Abstract
Electronic health records have revolutionized the medical world by improving medical care, refining provider documentation, standardizing care, and minimizing sentinel events. Successful implementation of electronic health records remains a daunting task and requires careful strategic planning and buy-in from key stakeholders. Much has been published in resource-rich settings and high-income countries about implementations of electronic health records. However, little is known about the experience in resource-limited settings where challenges remain unique and distinct from other parts of the world. Our intention is to share lessons learned during implementation of a web-based electronic health record at a tertiary care center in Kenya.
Keywords: Electronic health record, Africa, implementation, low middle income country, resources
Introduction
Since the inception of medicine, healthcare providers have used paper or similar materials to help track patient symptoms and record their clinical progress. Technology has now taken over changing the way we practice, replacing paper with ever-advancing digital records via various easy-to-use and accessible platforms. Development of electronic health records (EHRs) began in the 1960s and the first EHR systems were known as clinical information systems. Around that time, many academic medical centers developed their own systems, but Lockheed (now known as Lockheed Martin Corporation), an American technology corporation with worldwide interests, pioneered a product that formed part of an EHR system now known as Allscripts. 1 The US federal government began using EHRs in the 1970s with implementation of VistA. In the 1980s, the Institute of Medicine was the first to argue on the need for using EHRs as a means to improve patient records. 2 Use of EHR systems still remained challenging at that time due to high costs, data entry errors, lack of acceptance by physicians, and a lack of real incentives. 3 In addition, many EHR systems were developed without full consideration of the user's experience. Due to cost implications, poor user interfaces, and siloed implementation strategies, EHRs ended up simply complementing paper records rather than replacing them.
In the 1990's computers became more powerful, faster, and portable which augmented better adoptions of EHRs across North America.4,5 Since then, large commercial vendors have replaced many EHRs that had been developed by academic institutions; and hence, it is not hard to comprehend that most EHR-related project and resulting publications are from North America and other western countries.6,7 In the USA and Canada, approximately 80.5% of all hospitals have adopted a basic EHR system.8,9
With the progression and improvement of EHR systems, three key functionalities that seem to be promising in improving quality of care as well as reducing cost and improving physician efficiency include: (1) Clinical decision support mechanisms that guide providers in decision making with regard to patient care, (2) computerized physician order entry which improves the efficiency of order administration related to patient care and, (3) health information exchanges where patient data is shared among different health facilities promoting safe and cost-effective care. 10 Over the course of time, EHR systems have revolutionized the medical world by improving access to patient information, improving patient safety and outcomes, and allowing for data interpretation that ultimately helps healthcare providers improve the way they practice medicine. In addition, EHRs have been shown to overcome poor penmanship that previously led to errors posing a threat to patient care. Despite the multiple benefits of a comprehensive EHR system, especially in regard to improving patient care, little is known about the adoption, implementation, and use of an EHR system in Africa.
Health care systems in Africa remain fragile, even though the burden of disease remains disproportionately higher when compared to other continents. Furthermore, despite the proven benefits of EHRs, 11 very few health care facilities in Africa have adopted EHR systems for various reasons including cost (implementation and maintenance), lack of incentives, poor internet and electricity services, and limited computer skills by the end user. 12
The Aga Khan University Hospital, located in Nairobi, Kenya, recently went live with an EHR system that required extensive planning toward successful clinical adoption. The University Hospital is a 300-bed hospital with all major services that cater to the local population as well as patients from neighboring countries. The University Hospital significantly promotes and contributes to academic and research missions in Kenya. In addition, there are over 50 outreach centers located all over the country that cater to the health needs of the local populations in their respective areas. To the best of our knowledge, we are now the only healthcare facility in the country, to be fully electronically integrated between all areas of care: Inpatient, ambulatory, and accident and emergency. Prior to this, the hospital used a system that was a hybrid with provider notes and orders recorded on paper while laboratory and radiology results were being posted on an archaic, non-interactive, non-web-based electronic system.
EHR implementation is a multidisciplinary approach with various key tasks (building documents, orders, workflows, configuration, training, etc.) that enables the institution to effectively adopt the new system. 13 Certainly, implementation of an EHR system across any healthcare institution remains a daunting task with high failure rates in various parts of the world. 14 Strategic planning with involvement of key stakeholders remains imperative to ensure that an implementation remains successful. As stated earlier, little is known or published about EHR systems implementations in low-middle-income countries (LMICs) that have limited financial resources and inexperienced staff. It is our aim to share key lessons learned from our journey transitioning from a paper-based system to a web-enabled EHR system. Our hope is to inform other health institutions in LMIC regions that may pursue implementation of an EHR system so that they may be better prepared. The key lessons learnt during our implementation journey include:
The core clinical informatics team
Identifying a champion or a group of champions who are trusted by peers and colleagues, have knowledge about the EHR system, and believe in it, remains key to a successful implementation. 15 This key team provides direction and creates trust in the system by communicating effectively with other healthcare providers. The Chief Medical Information Officer (CMIO) put together a core of physician and nurse-led clinical informatics team, from selected clinic areas that helped lead and develop various parts of the EHR system including the evidence-based order sets and documentation templates needed to provide patient care. Of note, this team had minimal experience to begin with, so guidance from a well-experienced CMIO was pivotal. The informatics team worked closely with all key stakeholders, especially the physician and nursing leadership, to ensure that they were involved in the development of the EHR system as well as fostering continuous communication, something shown to have success at other institutions. 16 We faced unique challenges in our setting, most notably a lack of experience in using and implementing an EHR system. Lack of experience was not limited to the core informatics team, but also the end-users and key leadership at the hospital and university; the majority of whom had never used an integrated EHR system before. Investing time and resources to help promote home-grown talent remained key to help build a strong and reliable core informatics team that, in turn, helped nurture teaching and learning vertically. This also remained cost-effective for the institution initially and seen as an investment for the long run.
Stakeholder buy-in
For the successful implementation of any EHR system, it remains crucial that the end-users including physicians, nurses, allied health, and other services buy into the usefulness, functionality and benefit of the EHR system. 17 Each provider should understand the importance of the EHR system and how such a system will help improve their productivity, patient satisfaction, and clinical efficiency. This can be a daunting and time-consuming task for the organization. The informatics team needs to develop various strategies that address such concerns per their institution's needs. Introduction to the EHR system must be planned strategically and done at the right time. If done too early, many providers can forget the basics before Go-Live and if done too late, this might not provide enough time to fully understand the system. 15 A fast track to project failure includes the absence to accommodate the emotional side to change. Interestingly, the best systems are often resisted by providers who have a low psychological ownership of the system and vice-versa. 15 Frequent communication and involvement early on in the process remain key to gain buy-in from various providers.15,16 About 6 months before Go-Live, we introduced the EHR system to all physicians and nurses and conducted various in-person as well as online sessions to demonstrate how the EHR system functions and how it would help providers with patient care and efficiency. We conducted various town halls and open question sessions so that providers could freely express their concerns to the leadership and the wider EHRs team. The clinical informatics team, consisting primarily of physicians and nurses, played a key role in conducting smaller and often one-to-one sessions with various departments as well as older providers who would potentially struggle with the new system. The CMIO, in conjunction with the hospital leadership and communications team, put together monthly newsletters focusing on the EHR system implementation process as well as short videos on provider views of how this would make patient care more efficient and safer in the long run.
Training of end users
Effective training remains key to the successful implementation of an EHR system.17,18 Training allows the end-user to directly interact with the system, asking questions that reduce anxiety from anticipation of the new system.19,20 Training should be specific, brief, and timed appropriately to Go-Live which in turn helps build skill and buy-in, improve communication and involvement in improving the system. 15 Which type of training methods are best suited to transmit information still remains unclear at this time, but the initial training experience can influence the overall experience with any EHR system post-Go-Live. 21 We recruited an experienced EHR training manager; a nurse with a strong clinical background who had been involved in patient care. The training manager's sole responsibility was to develop a specific training schedule that catered to the needs of the various groups of providers. Training of multiple providers, in our case approximately 3000 providers, required much planning, time, space, and resources. The clinical informatics team and extra-trained super-users from various key clinical areas, as suggested in other studies, greatly helped in the training process which fostered trust not only in the team, but the EHR system itself. 22 Of the various methods to train end-users, our training manager in consultation with the informatics team chose a peer-peer training approach, where physicians trained physicians and nurses trained nurses and such a method has shown to be successful in previous studies. 23 End-users were also encouraged to view short videos on the functionality of the EHR system and how to use it better. These videos were available on demand and at the end-user's convenience, and greatly help enforce learning points. The training manager also arranged for multiple sessions, limited to 1 h, for re-training of various providers, especially for those struggling post Go-Live. 22 Even though some studies report starting their training process a few weeks before Go-Live, due to our limited resources and the sheer number of clinical providers and hospital staff, we started our training 60 days before Go-Live with ample opportunities to retrain. 22
Governance
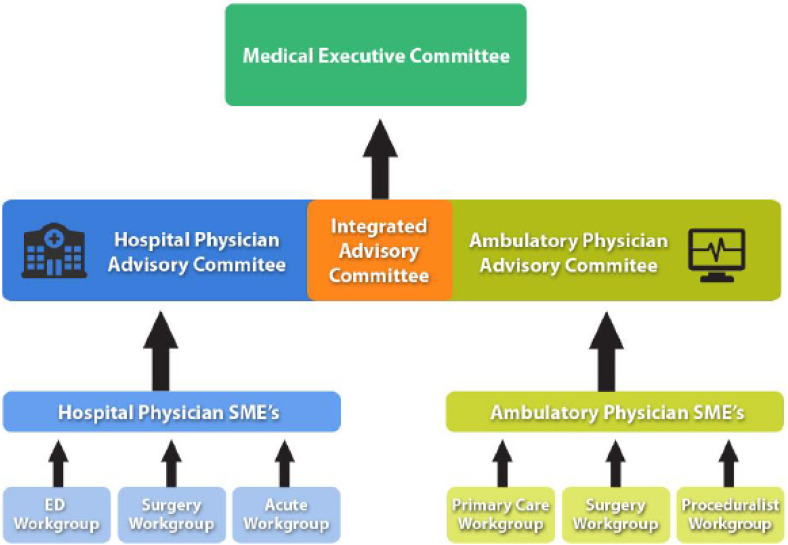
Governance during the implementation of any EHR system remains crucial not only to make key decisions but more importantly for effective communication with leadership and stakeholders. 18 There needs to be an objective way to discuss important decisions around the EHR system with key leaders and a way to make decisions that potentially affect patient care and provider efficiency. Many of the decisions were time-sensitive and required immediate action to resolve before Go-Live. We developed two strategic clinical committees chaired by the CMIO. (1) Clinical Leadership Standards Committee (CLSC) which consisted of the hospital leadership, department chairs, IT support, HIMS sections, and the clinical informatics team. It focused primarily on the physician and clinical components of the EHR; and (2) Enterprise Standards Committee (ESC) that focused on the non-physician aspects of EHR including patient registration, billing, pharmacy, and various nursing elements. We also had an EHR Steering Committee that met once a month to discuss other issues related to implementation of the EHR system such as space, IT support, wireless/internet services, software that complimented the EHRs, and other logistical issues. The stakeholders on both clinical committees had a chance to voice their concerns and ask specific questions to the appropriate team leads. Discussions on Go-Live plans, timeline updates, training schedules, internet services, hardware, and other key issues were discussed with projected turnaround times provided to all. Updates were also provided on the status of developing physician and nursing documentation as well as the number of order sets that were ready to be deployed. The CMIO remained the lynch pin in ensuring decisions were made, timelines were upheld, and communication stayed active. A quick schematic structure of how clinical governance can be organized is included in Figure 1. This structure was suggested by one of the authors and adopted at another institution in 2017. We adapted this structure to our institutional needs by choosing to combine both the hospital and ambulatory physician advisory committees into the CSLC and initiating a non-clinical committee; ESC that reported on the non-clinical matters related to the implementation.
Figure 1.
Schematic diagram of a proposed clinical governance (presentation by Dr K. Nadeem Ahmed 2017).
Post go-live support
Support during Go-Live and afterward remains a key part of a successful implementation and can greatly influence the willingness of providers to accept and adapt to an EHR system. 18 At our institution, we recruited 25 nurses as the front-line support staff. Before Go-Live, these nurses were taught how to use the physician and nursing portions of the EHR system and trained to support end-users within the live patient environment. These nurses were then deployed to key clinical areas wearing bright red shirts for easy identification and worked closely with end-users. These frontline support staffs were key in helping the clinical providers, within clinical areas, maneuver the EHR system as well as answering various clinical questions that arose during the first 3 months’ after Go-Live. The frontline support staff were a key element in improving the EHRs experience for all clinical providers, within the clinical areas. We also found that daily huddles to discuss challenges during Go-Live and Post Go-Live helped to quickly address many issues, update leadership, improve communications, and evaluate progress. 18 The core informatics team remained a key support for the frontline support staff, helping them navigate challenging scenarios as well as offering emotional support during the highly intense post-Go-Live period. 18 Residents and Fellows who easily adapted and learned the new EHR system remained a key source of support to help train others as well as notify the informatics team of any issues that might have been missed during the development of the order-sets or physician documentation templates. The frontline support team provided 24-h support with a dedicated smartphone assigned to the team. Providers could call at any time to help them address any clinical issues they faced. We also initiated a dedicated WhatsApp group to foster communication within the clinical and support teams; this helped solve many challenges as they arose. This also helped mobilize staff to areas that might not have been covered in person during the course of each day, which gave the providers a reassuring sense of support during the post-live period.
Conclusion
EHRs have been shown to help provide comprehensive and safe care to patients as well as improve the provider experience. Implementation of any EHR system, especially in the LMIC, remains understudied and challenging due to the lack of resources and inexperienced staff. Extensive planning of an implementation strategy remains key to successfully launch an EHR system. We found that the most important components for a successful EHR implementation included the following:
Development of a core informatics team to help build confidence and trust in the system, improve communication, as well as assist with the EHR system build.
Stake-holder buy in to help foster ownership of the EHR system.
Effective, specific, and ongoing training of end-users at the appropriate time before Go-Live, to lessen anxiety and smoothen the transition to an EHR system.
Establishing a governance structure, that addresses the various needs, both clinical and non-clinical of the institutions, to help make key decisions and improve communication between key stakeholders.
Providing key front-line support to end users, within the clinical areas to help providers better adapt and use the system, especially post-GO-live.
Footnotes
Contributorship: SKA developed the concept note and initial writing of the manuscript. All authors equally contributed to the development, writing, and editing of the manuscript.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: This study was approved by the Institutional Research Board at Aga Khan University, Nairobi, Kenya
ORCID iD: Sayed K Ali https://orcid.org/0000-0003-0750-2903
References
- 1.Amatayakul M. Electronic Health Records:: A Practical Guide for Professionals and Organizations. 2004.
- 2.Io M. The Computer-Based Patient Record: An Essential Technology for Health Care. Revised Edition. Washington, DC: The National Academies Press, 1997. [PubMed] [Google Scholar]
- 3.Evans RS. Electronic health records: then, now, and in the future. Yearb Med Inform 2016; Suppl 1: S48–S61. PMID: 27199197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salenius SA, Margolese-Malin L, Tepper JE, et al. An electronic medical record system with direct data-entry and research capabilities. Int J Radiat Oncol Biol Phys 1992; 24: 369–376. [DOI] [PubMed] [Google Scholar]
- 5.Wormuth DW. SCUT: clinical data organization for physicians using pen computers. Proc Annu Symp Comput Appl Med Care 1992: 845–846. PMID: 1483012. [PMC free article] [PubMed] [Google Scholar]
- 6.Koppel R, Lehmann CU. Implications of an emerging EHR monoculture for hospitals and healthcare systems. J Am Med Inform Assoc 2015; 22: 465–471. [DOI] [PubMed] [Google Scholar]
- 7.Kim GR, Lehmann CU. In search of dialogue and discourse in applied clinical informatics. Appl Clin Inform 2009; 1–7. doi: 10.4338/ACI09-10-0002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adler-Milstein J, Holmgren AJ, Kralovec P, et al. Electronic health record adoption in US hospitals: the emergence of a digital “advanced use” divide. J Am Med Inform Assoc 2017; 24: 1142–1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gheorghiu B, Hagens S. Measuring interoperable EHR adoption and maturity: a Canadian example. BMC Med Inform Decis Mak 2016; 16: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Menachemi N, Collum TH. Benefits and drawbacks of electronic health record systems. Risk Manag Healthc Policy 2011; 4: 47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Advantages of Electronic Health Records Available: https://www.healthit.gov/faq/what-are-advantages-electronic-health-records.
- 12.Odekunle FF, Odekunle RO, Shankar S. Why sub-saharan Africa lags in electronic health record adoption and possible strategies to increase its adoption in this region. Int J Health Sci (Qassim) 2017; 11: 59–64. [PMC free article] [PubMed] [Google Scholar]
- 13.Electronic Health Record (EHR) Implementation. 2022.
- 14.Yogeswaran P, Wright G. EHR Implementation in South Africa: how do we get it right? Stud Health Technol Inform 2010; 160: 396–400. [PubMed] [Google Scholar]
- 15.Lorenzi NM, Kouroubali A, Detmer DE, et al. How to successfully select and implement electronic health records (EHR) in small ambulatory practice settings. BMC Med Inform Decis Mak 2009; 9: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sequeira L, Almilaji K, Strudwick G, et al. EHR “SWAT” teams: a physician engagement initiative to improve electronic health record (EHR) experiences and mitigate possible causes of EHR-related burnout. JAMIA Open 2021; 4: ooab018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Beeson K. EHR Implementation Plan: Your 8-Step Checklist Available: https://www.ehrinpractice.com/ehr-implementation-plan.html. Accessed February, 2023.
- 18.Lumetra IFfQHC. EHR Implementation Checklist. 2006. Available at: https://digital.ahrq.gov/sites/default/files/docs/workflowtoolkit/ehr_implementation_checklist.pdf
- 19.Lorenzi NM, Riley RT. Organizational aspects of health informatics: managing technological change. New York: Springer-Verlag, 1995. [Google Scholar]
- 20.Ash JS, Bates DW. Factors and forces affecting EHR system adoption: report of a 2004 ACMI discussion. J Am Med Inform Assoc 2005; 12: 8–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mishra V, Liebovitz D, Quinn M, et al. Factors that influence clinician experience with electronic health records. Perspect Health Inf Manag 2022; 19: 1f. [PMC free article] [PubMed] [Google Scholar]
- 22.Aguirre RR, Suarez O, Fuentes M, et al. Electronic health record implementation: a review of resources and tools. Cureus 2019; 11: e5649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dastagir MT, Chin HL, McNamara M, et al. Advanced proficiency EHR training: effect on physicians’ EHR efficiency, EHR satisfaction and job satisfaction. AMIA Annu Symp Proc 2012; 2012: 136–143. [PMC free article] [PubMed] [Google Scholar]