Abstract
Objective.
In the chronic phase after a stroke, limitations in activities of daily living (ADLs) and instrumental ADL (IADLs) initially plateau before steadily increasing. The benefits of pre-stroke physical activity on these limitations remain unclear. To clarify this relationship, we examined the effect of physical activity on the long-term evolution of functional limitations in a cohort of stroke survivors and compared it to a cohort of matched stroke-free adults.
Methods.
Longitudinal data from 2,143 stroke survivors and 10,717 stroke-free adults aged 50 years and older were drawn from a prospective cohort study based on the Survey of Health, Ageing and Retirement in Europe (2004–2022; 8 data collection waves). Physical activity was assessed in the pre-stroke wave. Functional limitations were assessed in the post-stroke waves. Each stroke survivor was matched with 5 stroke-free adults who had similar propensity scores computed on the basis of key covariates, including baseline age, sex, body mass index, limitations in ADL and IADL, chronic conditions and country of residence, before any of the participants from either cohort had experienced a stroke.
Results.
Results showed an interaction between stroke status and physical activity on ADL limitations (b = −0.076; 95% CI = −0.142 to −0.011), with the effect of physical activity being stronger in stroke survivors (b = −0.345, 95% CI = −0.438 to −0.252) than in stroke-free adults (b = −0.269, 95% CI = −0.269 to −0.241).
Conclusion.
The beneficial effect of pre-stroke physical activity on ADL limitations after stroke is stronger than its effect in matched stroke-free adults followed for a similar number of years.
Impact.
Physical activity, an intervention within the physical therapist’s scope of practice, is effective in reducing the risk of functional dependence after stroke. Moreover, pre-stroke levels of physical activity can inform the prognosis of functional dependence in stroke survivors.
Keywords: Cohort Studies, Comorbidity, Disability, Exercise, Functional Status, Health Behavior, Longitudinal Studies, Prognosis, Prospective Studies, Stroke Survivors
INTRODUCTION
The prevalence of stroke exceeds 100 million cases worldwide1. On average, each of these cases is associated with a loss of 1.4 years of full health1,2. Over the past three decades, the number of years of full health lost to stroke has increased by an average of 1.2 million per year1. This burden on stroke survivors is reflected in their functional limitations. Specifically, one year after a stroke, survivors experience at least slight (59%)3–17, moderate (33%)13–28, or severe (23%)11–13,15–20 dependency in activities of daily living (ADLs), such as dressing, walking, bathing, eating, and toileting (Supplemental Tables S1 to S3). Regarding instrumental ADLs (IADLs), 40%9,10,16,19,20 of stroke survivors are moderately active and 41%16,17,19–21 are inactive in household, leisure, work, and outdoor activities at 1 year (Supplemental Tables S4 and S5). Whether limitations in I/ADLs (ADLs and IADLs) plateau10,13,21,28,29 or increase11,12,19 in subsequent years depends on several factors, including age11,12,29,30, type of health insurance11, and severity of disability 1 to 2 years after stroke12.
The level of physical activity has been suggested as one of the factors influencing functional limitations after stroke31. Regarding ADLs, some studies have found an association between higher pre-stroke physical activity and lower post-stroke limitations in ADLs22,32–37. Specifically, higher pre-stroke physical activity was associated with higher independence in ADLs during the first22, 32–36 and second year37 after stroke. However, other studies found no evidence of this association between physical activity and functional independence in ADLs38–41. These mixed results could be explained by the use of a single-item rating scale22,32,33,35–41, the Modified Rankin Scale, which has been shown to be less reliable and more subjective than questionnaires assessing specific I/ADLs42. In addition, only one prospective study has examined the effect of pre-stroke physical activity on IADLs30. This study focused on vigorous physical activity and was based on a cohort of adults who were stroke-free at baseline. The results showed that higher vigorous physical activity at baseline was associated with a higher probability of being independent in I/ADLs after stroke, but this difference was similar before stroke. This result led the authors to conclude that “being physically active does not protect against the disabling effects of a stroke” on I/ADLs. Building on this previous study, we used a different approach by comparing the effect of physical activity on I/ADLs in a larger sample of stroke survivors (n = 2,143 vs. 1,374) with a sample of stroke-free adults matched for key covariates (n = 10,717). In addition, because moderate-intensity physical activity has been suggested to be at least as beneficial for brain plasticity as vigorous-intensity physical activity43,44, both intensities were included in our study.
The objective of this longitudinal case-control study was to examine the effect of pre-stroke physical activity on post-stroke functional limitations. We hypothesized that higher levels of pre-stroke physical activity would reduce post-stroke functional limitations in a cohort of stroke survivors. We further hypothesized that this beneficial effect of physical activity would be weaker in a cohort of stroke-free participants matched for baseline (i.e., before any of the stroke survivors had experienced a stroke) age, sex, body mass index, I/ADL limitations, and country of residence over a similar number of follow-up years, because stroke survivors are likely to have more functional limitations from which to recover.
METHODS
Study Sample and Design
Data were drawn from the Survey of Health, Ageing and Retirement in Europe (SHARE), a longitudinal population-based study of over 140,000 adults aged 50 years and older living in 28 European countries and one Middle East country45. Data were collected every 2 years between 2004 and 2022 for a total of 8 waves of measurement using computer-assisted personal interviewing (CAPI) in the participants’ homes. Physical activity, stroke events, and functional independence (ADLs, IADLs) were assessed at all measurement waves except wave 3 (2008–2009). To be included in the present study, participants had to be 50 years of age or older, have no reported history of stroke prior to study entry, and have participated in at least 4 waves. SHARE was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the University of Mannheim (waves 1–4) and the Ethics Council of the Max Planck Society (waves 4–8). All participants gave written informed consent.
Measures
Outcome Variable: Post-Stroke Functional Limitations
Functional dependence was assessed using the number of functional limitations in six ADLs (dressing, walking, bathing, eating, getting in and out of bed, and using the toilet) and seven IADLs (using a map, preparing a hot meal, shopping for groceries, making telephone calls, taking medication, gardening or doing housework, and managing money)46,47. Participants were presented with each activity and instructed to indicate whether they “have any difficulty with these activities because of a physical, mental, emotional or memory problem” (yes vs. no) and to “exclude any difficulties they expected to last less than three months”. A score representing the total number of functional dependencies was computed for ADLs (0–6) and IADLs (0–7), with higher scores indicating greater functional dependence.
Explanatory Variables: Stroke and Physical Activity
Information on stroke status during follow-up was collected at each wave using the following question: “Has a doctor told you that you have any of the conditions on this card [indicating history of health conditions including stroke]?”12.
Level of physical activity at entry in SHARE was derived from two questions: “How often do you engage in vigorous physical activity, such as sports, heavy housework, or a job that involves physical labor?” and “How often do you engage in activities that require a low or moderate level of energy such as gardening, cleaning the car, or doing a walk?”47–52. Participants responded on a four-point scale: 1 = Hardly ever or never; 2 = One to three times a month; 3 = Once a week; 4 = More than once a week. Participants who answered “more than once a week” to at least one of the questions were classified as physically active, whereas the other participants were classified as physically inactive to reduce a potential misclassification bias in which physically inactive participants would be incorrectly classified as physically active.
Covariates
Models were adjusted for baseline age, sex (male, female), time (survey waves), quadratic time, number of chronic conditions (none or 1 vs. 2 or more), and level of education (primary or less, secondary, tertiary), which has been shown to be associated with physical activity levels48,51,53–57.
Data Preprocessing
Matching Procedure
To select matched samples of stroke survivors and stroke-free participants with similar distributions of key covariates, a matching procedure based on the nearest neighbor method was conducted using the MatchIt R package58,59 with propensity scores obtained with a generalized linear model. This matching procedure used a 1:5 ratio to create groups including one stroke survivor and five stroke-free adults with similar propensity scores, thereby reducing the potential bias introduced by covariates. Propensity scores were calculated using the characteristics of the participants at their first SHARE interview, when none of them had experienced a stroke: Age, sex, number of chronic conditions (none or 1 vs. 2 or more), limitations in I/ADL, body mass index category [underweight (<18.5 kg/m2), normal (reference; 18.5 to 24.9 kg/m2), overweight (25 to 29.9 kg/m2), obese (30 kg/m2 and above)], country of residence, number of measurement waves, and wave number of the first interview.
Temporal Alignment of Data on the First Post-Stroke Wave
Using the lag() function of the dplyr R package, which allows the temporal alignment of the measurement waves to be shifted, the first wave in which a stroke was reported was set as Wave 1 in the analyses. Baseline data from stroke survivors used in the matching procedure (see below) were data collected during the wave preceding this Wave 1.
Statistical Analyses
Data were analyzed using linear mixed-effects models, which account for the nested structure of the data (i.e., repeated measures over time within a single participant), allow the use of incomplete and unbalanced data, and provide acceptable Type I error rates60,61. Models were built and fitted by maximum likelihood in R programming language62 using the lme463 and lmerTest64 packages. P-values were approximated using Satterthwaite method64. The effects of baseline physical activity on future I/ADL were compared between stroke survivors and stroke-free adults. The number of post-stroke measurement waves varied between participants in the stroke group and was matched to the number of measurement waves in the stroke-free adults. To examine the effect of pre-stroke physical activity on functional independence in stroke survivors and stroke-free adults, two dependent variables were tested: ADL and IADL limitations. The fitted models included stroke (stroke vs. no stroke), physical activity (active vs. inactive at baseline), linear time, quadratic time, and the covariates as fixed effects. The random structure included random intercepts for participants and for participants grouped together by the matching process, as well as random linear and quadratic slopes of wave within each participant61. These random effects estimated the functional independence of each participant and each matching group, as well as the rate of change of this independence across waves. The quadratic effect of wave was added to account for the potential accelerated (or decelerated) decline in functional independence across waves. An interaction term between stroke and physical activity conditions was added to formally test the moderating effect of stroke on the association between physical activity and functional dependence. In addition, interaction terms between stroke and wave (linear and quadratic) conditions were included to allow variations in I/ADL trajectories between the two groups. In summary, the equation of our models was as follows:
In this equation, is the jth participant’s number of limitations in ADLs or IADLs in condition , the are the fixed effect coefficients, is the random intercept for the participant, is the random slope of the wave for the participant, is the random slope of the quadratic wave for the participant, is a random intercept with coding for the matching group of the jth participant, the random effects are allowed to correlate freely (unstructured covariance matrix), and is the error term.
Sensitivity Analysis
In a sensitivity analysis, participants who responded “hardly ever or never” to one of the two physical activity questions were classified as physically inactive, whereas the other participants were classified as physically active. This categorization reduced a potential misclassification bias in which physically active participants would be incorrectly classified as physically inactive.
RESULTS
Descriptive Results
The study sample included 2,143 stroke survivors (mean age: 66.9 ± 9.1 years; 1,052 females) and 10,717 stroke-free adults (mean age: 66.9 ± 9.3 years, 5,126 females) from the SHARE study, whose characteristics at baseline are summarized in Table 1.
Table 1.
Baseline characteristics of the participants at their first interview for the Survey of Health, Ageing and Retirement in Europe (SHARE), when none of them had experienced a stroke, stratified by stroke-related status in the following waves.
| Variables | Stroke Survivors (N = 2,143) | Matched Stroke-Free Adults (N = 10,717) |
|---|---|---|
|
| ||
| Age, mean (SD) | 66.9 (9.1) | 66.9 (9.3) |
| Sex | ||
| Female, n (%) | 1052 (49.1) | 5126 (47.8) |
| Male, n (%) | 1091 (50.9) | 5591 (52.2) |
| Physical Activity | ||
| Physically active, n (%) | 1564 (72.5) | 8060 (74.6) |
| Physically inactive, n (%) | 595 (27.4) | 2720 (25.2) |
| Functional Limitations | ||
| ADL, mean (SD) | 0.2 (0.6) | 0.2 (0.7) |
| IADL, mean (SD) | 0.3 (0.8) | 0.3 (0.9) |
| Body Mass Index (kg/m2) | ||
| < 18.5 – Underweight, n (%) | 155 (1.5) | 590 (1.1) |
| 18.5–24.9 – Normal, n (%) | 3445 (33.9) | 16275 (31.7) |
| 25–29.9 – Overweight, n (%) | 4176 (41.0) | 22856 (44.5) |
| ≥ 30 – Obese, n (%) | 2401 (23.6) | 11647 (22.7) |
| Chronic Condition | ||
| < 2, n (%) | 3423 (32.7) | 22807 (43.5) |
| ≥ 2, n (%) | 7053 (67.3) | 29676 (56.5) |
| Education | ||
| Primary, n (%) | 666 (31.1) | 3027 (28.2) |
| Secondary, n (%) | 1081 (50.4) | 5415 (50.5) |
| Tertiary, n (%) | 396 (18.5) | 2275 (21.2) |
| Country | ||
| Austria, n (%) | 147 (6.9) | 764 (7.1) |
| Belgium, n (%) | 193 (9.0) | 965 (9.0) |
| Czech Republic, n (%) | 160 (7.5) | 818 (7.6) |
| Denmark, n (%) | 170 (7.9) | 810 (7.6) |
| Estonia, n (%) | 154 (7.2) | 870 (8.1) |
| France, n (%) | 161 (7.5) | 815 (7.6) |
| Germany, n (%) | 153 (7.1) | 831 (7.8) |
| Greece, n (%) | 106 (4.9) | 506 (4.7) |
| Israel, n (%) | 95 (4.4) | 460 (4.3) |
| Italy, n (%) | 161 (7.5) | 768 (7.2) |
| Luxembourg, n (%) | 20 (0.9) | 94 (0.9) |
| Netherlands, n (%) | 81 (3.8) | 384 (3.6) |
| Poland, n (%) | 73 (3.4) | 368 (3.4) |
| Slovenia, n (%) | 76 (3.5) | 379 (3.5) |
| Spain, n (%) | 141 (6.6) | 673 (6.3) |
| Sweden, n (%) | 167 (7.8) | 812 (7.6) |
| Switzerland, n (%) | 85 (4.0) | 404 (3.8) |
Notes. ADL = activities of daily living, IADL = instrumental activities of daily living, SD = standard deviation.
In stroke survivors, the average level of functional limitation at the first wave after stroke was 0.17 for ADLs and 0.28 for IADLs and increased to 1.05 and 1.72 at the eighth wave after stroke, respectively (Supplemental Table S6). In stroke-free adults, the average level of functional limitation on the first wave after stroke was 0.15 for ADLs and 0.25 for IADLs and increased to 0.41 and 0.73 on the eighth wave after stroke, respectively (Supplemental Table S6). The similar level of functional limitation between groups at the first poststroke wave was expected because the propensity score used for the matching procedure included the number of I/ADL limitations at baseline.
At baseline, 258 stroke survivors engaged in moderate physical activity “hardly ever or never”, 127 “one to three times a month”, 274 “once a week”, and 1,500 “more than once a week” (Supplemental Table S7). In addition, 951 engaged in vigorous physical activity “hardly ever or never”, 216 “one to three times a month”, 306 “once a week”, and 706 “more than once a week” (Supplemental Table S7). In total, 1,564 stroke survivors were considered physically active (i.e., answered “more than once a week” to at least one of the two questions) and 595 were considered physically inactive (Supplemental Table S8).
Statistical Results
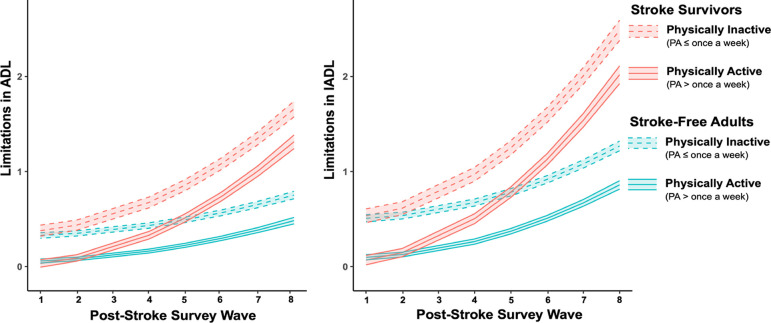
Results of the mixed-effects models showed an interaction effect between stroke status and physical activity on ADL limitations (b = −0.076, 95% confidence interval [CI]: −0.142 to −0.011, p = 0.022; Table 2, Figure 1). The simple effects of the terms in this interaction confirmed that the effect of physical activity was stronger in stroke survivors (b = −0.345, 95% CI: −0.438, −0.252, p < 2.0 × 10−16) than in stroke-free adults (b = −0.269, 95% CI: −0.296 to −0.241, p < 2.0 × 10−16), with physically active participants (i.e., physical activity > once a week) showing fewer limitations in ADLs than physically inactive participants (i.e., physical activity ≤ once a week). Similarly, a main effect showed that physically active participants showed fewer limitations in IADLs (b = −0.410, 95% CI: −0.445 to −0.375, p < 2.0 × 10−16; Table 2, Figure 1). However, results showed no evidence of an interaction effect of stroke status and physical activity on limitations in IADLs (b = −0.057, 95% CI: −0.140 to 0.026, p = 0.178; Table 2, Figure 1).
Table 2.
Results of the mixed-effects models testing the interaction between stroke-related status and physical activity (PA; once a week or less vs. more than once a week) on limitations in activities of daily living (ADL) and instrumental activities of daily living (IADL).
| Exposures | ADL | IADL | ||
|---|---|---|---|---|
|
| ||||
| b (95 CI) | P | b (95 CI) | P | |
|
| ||||
| Intercept | −0.379 (−0.472 to −0.286) | 1.3 × 10−15 | −0.849 (−0.971 to −0.727) | < 2.0 × 10−16 |
| Stroke | 0.051 (−0.011 to 0.113) | 0.105 | 0.027 (−0.050 to 0.104) | 0.495 |
| Physical Activity | −0.269 (−0.296 to −0.241) | < 2.0 × 10−16 | −0.410 (−0.445 to −0.375) | < 2.0 × 10−16 |
| Wave | 0.016 (0.005 to 0.027) | 0.005 | 0.015 (0.001 to 0.029) | 0.030 |
| Wave2 | 0.006 (0.005 to 0.008) | 5.7 × 10−15 | 0.013 (0.011 to 0.015) | < 2.0 × 10−16 |
| Age | 0.008 (0.007 to 0.009) | < 2.0 × 10−16 | 0.014 (0.013 to 0.016) | < 2.0 × 10−16 |
| Sex | 0.073 (0.051 to 0.095) | 1.1 × 10−10 | 0.204 (0.175 to 0.232) | < 2.0 × 10−16 |
| Education | ||||
| Primary (vs. Secondary) | 0.115 (0.090 to 0.141) | < 2.0 × 10−16 | 0.219 (0.187 to 0.251) | < 2.0 × 10−16 |
| Tertiary (vs. Secondary) | −0.024 (−0.053 to 0.004) | 0.094 | −0.043 (−0.079 to −0.007) | 0.020 |
| Chronic Conditions | 0.115 (0.101 to 0.130) | < 2.0 × 10−16 | 0.180 (0.162 to 0.198) | < 2.0 × 10−16 |
| Stroke × Physical Activity | −0.076 (−0.142 to −0.011) | 0.022 | −0.057 (−0.140 to 0.026) | 0.178 |
| Stroke × Wave | 0.020 (−0.006 to 0.047) | 0.128 | 0.031 (−0.002 to 0.064) | 0.066 |
| Stroke × Wave2 | 0.015 (0.011 to 0.018) | 4.9 × 10−13 | 0.020 (0.015 to 0.025) | 3.9 × 10−15 |
Notes. 95 CI = 95% confidence interval, ADL = activities of daily living, IADL = instrumental activities of daily living
Figure 1.
Effect of physical activity (PA ≤ once a week vs. PA > once a week) on limitations in activities of daily living (ADL, left panel) and instrumental activities of daily living (IADL, right panel) in stroke survivors and matched stroke-free adults.
An interaction between stroke status and quadratic wave indicated that limitations in ADLs (b = 0.015, 95% CI: 0.011 to 0.018, p = 4.9 × 10−13) and IADLs (b = 0.020, 95% CI: 0.015 to 0.025, p = 3.9 × 10−15) increased across waves at a higher rate in stroke survivors than in stroke-free adults (Figure 1).
Results of the sensitivity analyses based on a different threshold for classifying physically active (i.e., physical activity ≥ once a month) and inactive participants (i.e., hardly ever or never active) were consistent with the results of the main analyses (Supplemental Table S9; Supplemental Figure S1).
DISCUSSION
Main Results
The objective of this longitudinal case-control study was to examine the effect of pre-stroke physical activity on post-stroke functional limitations in stroke survivors and matched stroke-free adults. Consistent with our hypothesis, the results suggest that the beneficial effect of pre-stroke physical activity on post-stroke ADL limitations is stronger than its effect in stroke-free adults matched for age, sex, body mass index, limitations in I/ADLs, number of chronic conditions, and country of residence, number of measurement waves, and wave number of the first interview.
Comparison With Other Studies
Our results in stroke survivors showed that higher levels of pre-stroke physical activity were associated with fewer ADL limitations, which is consistent with the existing literature22,32–37. Most importantly, our results reveal that the effect of pre-stroke physical activity on in ADL limitations after stroke is statistically stronger than its effect in matched stroke-free adults. Although the study by Ris et al.30 also examined the effect of physical activity in both stroke survivors and stroke-free adults (without the matching procedure we conducted), this potential interaction effect was not considered. Several mechanisms could explain how physical activity improves functional independence after stroke, such as an association between pre- and post-stroke physical activity. Previous studies have shown that this level of physical activity is similar in 41 to 42% of stroke survivors activity66,67. Post-stroke engagement in physical activity could increase brain plasticity processes such as angiogenesis, synaptogenesis, and neurogenesis, primarily through the upregulation of growth factors (e.g., brain-derived neurotrophic factor; BDNF)68–70. However, the same studies also showed that 33 to 39% of stroke survivors reported lower levels of physical activity after stroke compared to before stroke, and 20 to 25% reported higher levels of physical activity66,67. Another explanation could be the beneficial effect of pre-stroke physical activity on depression66, which has been shown to be associated with ADL limitations47,71,72.
Strengths and Limitations
The present study has several strengths including results presented for a long follow-up period (up to 16 years) and a large international post-stroke population (17 countries), which allowed us to robustly examine the effects of physical activity on I/ADL limitations. The number of I/ADL limitations was used to assess changes in functional limitation over time, which is more reliable than single-item ratings and more sensitive to identifying differences in functional trajectories between stroke survivors and stroke-free adults. Sensitivity results using a different categorization of physical activity were consistent with the main results.
However, our results should be considered in the light of several limitations. (1) There was a lack of information on stroke characteristics, which is common in and inherent to large-scale longitudinal studies. Differences in stroke subtypes (i.e., ischemic, hemorrhagic, cryptogenic, transient ischemic attack) or in the type of impairment resulting from the stroke (e.g., motor, sensory, visual, cognitive) may partly explain the discrepancy in our findings between ADL and IADL. The different behaviors that comprise ADL (which rely more on basic motor functions) and IADL (which rely more on cognitive functions) may interact with stroke characteristics. However, data specifying stroke characteristics is not available in SHARE. Future studies should be supported by medical records to provide a more specific understanding of the relationship between physical activity and specific aspects of functional independence by stroke characteristics. (2) The outcome (i.e., stroke) was self-reported. Therefore, a memory bias cannot be excluded. However, the agreement between self-reported stroke and medical records ranges from 79%73 to 96%74. (3) Physical activity was self-reported, which may not have accurately captured the actual levels of physical activity, as correlations between self-report and direct measures of physical activity are low to moderate75,76. Future studies should assess physical activity using device-based measures, which have been shown to have greater validity and reliability77.
Conclusions
Our results support a stronger long-term beneficial effect of physical activity on independence in ADLs in stroke survivors compared with stroke-free adults. These findings underscore the beneficial role of moderate-to-vigorous physical activity in mitigating stroke-related limitations in ADLs. In addition, these findings highlight the need to consider the pre-stroke levels of physical activity in the prognosis of stroke-related functional independence.
As movement specialists and primary care practitioners, physical therapists are key healthcare professionals in the prevention of physical inactivity, which falls within their scope of practice78,79. As such, the expertise of physical therapists should be used to help people achieve the recommendations of physical activity, thereby optimizing their functional independence in the event of a stroke. While physical therapists feel confident in providing general advice to patients and clients about a physically active lifestyle and suggesting specific physical activity programs, they also perceive some barriers in providing this comprehensive care, including the lack of time, counseling skills, and reimbursement80. Such reimbursement may lead to the emergence of certified clinical specialists who can develop mor in-depth knowledge and skills related to physical inactivity.
Supplementary Material
Acknowledgements
Based on the Contributor Roles Taxonomy (CRediT)81,82, individual author contributions to this work are as follows: Zack van Allen: Formal Analysis; Visualization; Data Curation; Writing – Review and Editing; Dan Orsholits: Methodology; Formal Analysis; Visualization; Data Curation; Writing – Review and Editing; Matthieu P. Boisgontier: Conceptualization; Methodology; Formal Analysis; Visualization; Data Curation; Writing – Original Draft; Writing – Review and Editing; Supervision; Project Administration; Funding Acquisition.
The authors are grateful to Dr. Olivier Renaud (University of Geneva, Switzerland) for his help in transcribing the R code of our statistical models into a scientific equation.
Funding
Dr Boisgontier is supported by the Canada Foundation for Innovation (CFI), Mitacs, and the Banting Research Foundation. Zack van Allen is supported by a Mitacs-Banting Discovery Postdoctoral Fellowship. The SHARE data collection was primarily funded by the European Commission through FP5 (QLK6-CT-2001–00360), FP6 (SHARE-I3: RII-CT-2006–062193, COMPARE: CIT5-CT-2005–028857, SHARELIFE: CIT4-CT-2006–028812) and FP7 (SHARE-PREP: no.211909, SHARE-LEAP: no.227822, SHARE M4: no.261982). Additional funding from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, the U.S. National Institute on Aging (U01_AG09740–13S2, P01_AG005842, P01_AG08291, P30_AG12815, R21_AG025169, Y1-AG-4553–01, IAG_BSR06–11, OGHA_04–064, HHSN271201300071C) and from various national funding sources is gratefully acknowledged (see www.share-project.org).
Nonstandard abbreviations and acronyms:
- ADL
activities of daily living
- IADL
instrumental activities of daily living
- SHARE
Survey of Health, Ageing and Retirement in Europe
Footnotes
Reporting Guidelines
This manuscript conforms to the STROBE guidelines for observational studies (http://www.strobe-statement.org)86.
Ethical approval: This study was part of the Survey of Health, Ageing and Retirement in Europe (SHARE), which was approved by the relevant research ethics committees. The University of Ottawa’s Office of Research Ethics and Integrity has formally confirmed that the study does not require review by a Research Ethics Board because it relies exclusively on publicly available information that is legally available to the public and appropriately protected by law. All participants provided written informed consent.
Data and Code Sharing
In accordance with good research practices83, the R code used to analyze the data is publicly available online84. A non-peer-reviewed version of this manuscript is publicly available online85. The SHARE dataset is available at http://www.share-project.org/data-access.html and the DOIs for the waves used in the current study are the following: https://doi.org/10.6103/SHARE.w1.600, https://doi.org/10.6103/SHARE.w2.600, https://doi.org/10.6103/SHARE.w4.600, https://doi.org/10.6103/SHARE.w5.600, https://doi.org/10.6103/SHARE.w6.600, https://doi.org/10.6103/SHARE.w7.711, https://doi.org/10.6103/SHARE.w8cabeta.001.
REFERENCES
- 1.GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021;20(10):795–820. 10.1016/S1474-4422(21)00252-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Indicator metadata registry list: Disability-Adjusted Life Years (DALYs). Accessed January 29, 2022. https://www.who.int/data/gho/indicator-metadata-registry/imr-details/158
- 3.Carolei A, Marini C, Di Napoli M, et al. High stroke incidence in the prospective community-based L’Aquila registry (1994–1998). First year’s results. Stroke. 1997;28(12):2500–2506. 10.1161/01.str.28.12.2500 [DOI] [PubMed] [Google Scholar]
- 4.Hartman-Maeir A, Soroker N, Ring H, Avni N, Katz N. Activities, participation and satisfaction one-year post stroke. Disabil Rehabil. 2007;29(7):559–566. 10.1080/09638280600924996 [DOI] [PubMed] [Google Scholar]
- 5.Leśniak M, Bak T, Czepiel W, Seniów J, Członkowska A. Frequency and prognostic value of cognitive disorders in stroke patients. Dement Geriatr Cogn Disord. 2008;26(4):356–363. 10.1159/000162262 [DOI] [PubMed] [Google Scholar]
- 6.Minelli C, Fen LF, Minelli DP. Stroke incidence, prognosis, 30-day, and 1-year case fatality rates in Matão, Brazil: a population-based prospective study. Stroke. 2007;38(11):2906–2911. 10.1161/STROKEAHA.107.484139 [DOI] [PubMed] [Google Scholar]
- 7.Skånér Y, Nilsson GH, Sundquist K, Hassler E, Krakau I. Self-rated health, symptoms of depression and general symptoms at 3 and 12 months after a first-ever stroke: a municipality-based study in Sweden. BMC Fam Pract. 2007;8:61. 10.1186/1471-2296-8-61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van de Port IG, Kwakkel G, van Wijk I, Lindeman E. Susceptibility to deterioration of mobility long-term after stroke: a prospective cohort study. Stroke. 2006;37(1):167–171. 10.1161/01.STR.0000195180.69904.f2 [DOI] [PubMed] [Google Scholar]
- 9.Sveen U, Wyller TB, Ljunggren AE, Bautz-Holter E. Predictive validity of early cognitive assessment in stroke rehabilitation, Scand J Occup Ther. 1996;3(1):20–27. 10.3109/11038129609106678 [DOI] [Google Scholar]
- 10.Ayerbe L, Ayis S, Rudd AG, Heuschmann PU, Wolfe CD. Natural history, predictors, and associations of depression 5 years after stroke: the South London Stroke Register. Stroke. 2011;42(7):1907–1911. 10.1161/STROKEAHA.110.605808 [DOI] [PubMed] [Google Scholar]
- 11.Dhamoon MS, Moon YP, Paik MC, et al. Long-term functional recovery after first ischemic stroke: the Northern Manhattan Study. Stroke. 2009;40(8):2805–2811. 10.1161/STROKEAHA.109.549576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gil-Salcedo A, Dugravot A, Fayosse A, et al. Long-term evolution of functional limitations in stroke survivors compared with stroke-free adults: findings from 15 years of follow-up across 3 international surveys of aging. Stroke. 2022;53(1):228–237. 10.1161/STROKEAHA.121.034534 [DOI] [PubMed] [Google Scholar]
- 13.Willey JZ, Disla N, Moon YP, et al. Early depressed mood after stroke predicts long-term disability: the Northern Manhattan Stroke Study (NOMASS). Stroke. 2010;41(9):1896–1900. 10.1161/STROKEAHA.110.583997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Taub NA, Wolfe CD, Richardson E, Burney PG. Predicting the disability of first-time stroke sufferers at 1 year. 12-month follow-up of a population-based cohort in southeast England. Stroke. 1994;25(2):352–357. 10.1161/01.str.25.2.352 [DOI] [PubMed] [Google Scholar]
- 15.Wong GK, Lam SW, Wong A, et al. MoCA-assessed cognitive function and excellent outcome after aneurysmal subarachnoid hemorrhage at 1 year. Eur J Neurol. 2014;21(5):725–730. 10.1111/ene.12363 [DOI] [PubMed] [Google Scholar]
- 16.Appelros P. Characteristics of the Frenchay Activities Index one year after a stroke: a population-based study. Disabil Rehabil. 2007;29(10):785–790. 10.1080/09638280600919715 [DOI] [PubMed] [Google Scholar]
- 17.Mar J, Masjuan J, Oliva-Moreno J, et al. Outcomes measured by mortality rates, quality of life and degree of autonomy in the first year in stroke units in Spain. Health Qual Life Outcomes. 2015;13:36. 10.1186/s12955-015-0230-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Broussy S, Saillour-Glenisson F, García-Lorenzo B, et al. Sequelae and quality of life in patients living at home 1 year after a stroke managed in stroke units. Front Neurol. 2019;10:907. 10.3389/fneur.2019.00907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patel MD, Coshall C, Rudd AG, Wolfe CD. Cognitive impairment after stroke: clinical determinants and its associations with long-term stroke outcomes. J Am Geriatr Soc. 2002;50(4):700–706. 10.1046/j.1532-5415.2002.50165.x [DOI] [PubMed] [Google Scholar]
- 20.Patel M, Coshall C, Rudd AG, Wolfe CD. Natural history of cognitive impairment after stroke and factors associated with its recovery. Clin Rehabil. 2003;17(2):158–166. 10.1191/0269215503cr596oa [DOI] [PubMed] [Google Scholar]
- 21.Wolfe CD, Crichton SL, Heuschmann PU, et al. Estimates of outcomes up to ten years after stroke: analysis from the prospective South London Stroke Register. PLoS Med. 2011;8(5):e1001033. 10.1371/journal.pmed.1001033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Urbanek C, Gokel V, Safer A, et al. Low self-reported sports activity before stroke predicts poor one-year-functional outcome after first-ever ischemic stroke in a population-based stroke register. BMC Neurol. 2018;18(1):181. 10.1186/s12883-018-1189-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jokinen H, Melkas S, Ylikoski R, et al. Post-stroke cognitive impairment is common even after successful clinical recovery. Eur J Neurol. 2015;22(9):1288–1294. 10.1111/ene.12743 [DOI] [PubMed] [Google Scholar]
- 24.López-Cancio E, Jovin TG, Cobo E, et al. Endovascular treatment improves cognition after stroke: a secondary analysis of REVASCAT trial. Neurology. 2017;88(3):245–251. 10.1212/WNL.0000000000003517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Santus G, Ranzenigo A, Caregnato R, Inzoli MR. Social and family integration of hemiplegic elderly patients 1 year after stroke. Stroke. 1990;21(7):1019–1022. 10.1161/01.str.21.7.1019 [DOI] [PubMed] [Google Scholar]
- 26.Verhoeven CL, Post MW, Schiemanck SK, van Zandvoort MJ, Vrancken PH, van Heugten CM. Is cognitive functioning 1 year poststroke related to quality of life domain? J Stroke Cerebrovasc Dis. 2011;20(5):450–458. 10.1016/j.jstrokecerebrovasdis.2010.02.018 [DOI] [PubMed] [Google Scholar]
- 27.Wafa HA, Wolfe CDA, Bhalla A, Wang Y. Long-term trends in death and dependence after ischaemic strokes: a retrospective cohort study using the South London Stroke Register (SLSR). PLoS Med. 2020;17(3):e1003048. 10.1371/journal.pmed.1003048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.de Campos LM, Martins BM, Cabral NL, et al. How many patients become functionally dependent after a stroke? A 3-year population-based study in Joinville, Brazil. PLoS One. 2017;12(1):e0170204.. 10.1371/journal.pone.0170204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rejnö Å, Nasic S, Bjälkefur K, Bertholds E, Jood K. Changes in functional outcome over five years after stroke. Brain Behav. 2019;9(6):e01300. 10.1002/brb3.1300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rist PM, Capistrant BD, Mayeda ER, Liu SY, Glymour MM. Physical activity, but not body mass index, predicts less disability before and after stroke. Neurology. 2017;88(18):1718–726. 10.1212/WNL.0000000000003888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Viktorisson A, Reinholdsson M, Danielsson A, Palstam A, S Sunnerhagen K. Pre-stroke physical activity in relation to post-stroke outcomes - linked to the International Classification of Functioning, Disability and Health (ICF): A scoping review. J Rehabil Med. 2022;54:jrm00251. 10.2340/jrm.v53.51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ursin MH, Ihle-Hansen H, Fure B, Tveit A, Bergland A. Effects of premorbid physical activity on stroke severity and post-stroke functioning. J Rehabil Med. 2015;47(7):612–617. 10.2340/16501977-1972 [DOI] [PubMed] [Google Scholar]
- 33.Deplanque D, Masse I, Lefebvre C, Libersa C, Leys D, Bordet R. Prior TIA, lipid-lowering drug use, and physical activity decrease ischemic stroke severity. Neurology. 2006;67(8):1403–1410. 10.1212/01.wnl.0000240057.71766.71 [DOI] [PubMed] [Google Scholar]
- 34.Stroud N, Mazwi TM, Case LD, et al. Prestroke physical activity and early functional status after stroke. J Neurol Neurosurg Psychiatry. 2009;80(9):1019–1022. 10.1136/jnnp.2008.170027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wen CP, Liu CH, Jeng JS, et al. Pre-stroke physical activity is associated with fewer post-stroke complications, lower mortality and a better long-term outcome. Eur J Neurol. 2017;24(12):1525–1531. 10.1111/ene.13463 [DOI] [PubMed] [Google Scholar]
- 36.Ricciardi AC, López-Cancio E, Pérez de la Ossa N, et al. Prestroke physical activity is associated with good functional outcome and arterial recanalization after stroke due to a large vessel occlusion. Cerebrovasc Dis. 2014;37(4):304–311. 10.1159/000360809 [DOI] [PubMed] [Google Scholar]
- 37.Krarup LH, Truelsen T, Gluud C, et al. Prestroke physical activity is associated with severity and long-term outcome from first-ever stroke. Neurology. 2008;71(17):1313–1318. 10.1212/01.wnl.0000327667.48013.9f [DOI] [PubMed] [Google Scholar]
- 38.Morovatdar N, Di Napoli M, Stranges S, et al. Regular physical activity postpones age of occurrence of first-ever stroke and improves long-term outcomes. Neurol Sci. 2021;42(8):3203–3210. 10.1007/s10072-020-04903-7 [DOI] [PubMed] [Google Scholar]
- 39.Rist PM, Lee IM, Kase CS, Gaziano JM, Kurth T. Physical activity and functional outcomes from cerebral vascular events in men. Stroke. 2011;42(12):3352–3356. 10.1161/STROKEAHA.111.619544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Damsbo AG, Mortensen JK, Kraglund KL, Johnsen SP, Andersen G, Blauenfeldt RA. Prestroke physical activity and poststroke cognitive performance. Cerebrovasc Dis. 2020;49(6):632–638. 10.1159/000511490 [DOI] [PubMed] [Google Scholar]
- 41.Decourcelle A, Moulin S, Sibon I, et al. Influence of previous physical activity on the outcome of patients treated by thrombolytic therapy for stroke. J Neurol. 2015;262(11):2513–2519. 10.1007/s00415-015-7875-4 [DOI] [PubMed] [Google Scholar]
- 42.Wolfe CD, Taub NA, Woodrow EJ, Burney PG. Assessment of scales of disability and handicap for stroke patients. Stroke. 1991;22(10):1242–1244. 10.1161/01.str.22.10.1242 [DOI] [PubMed] [Google Scholar]
- 43.Szuhany KL, Bugatti M, Otto MW. A meta-analytic review of the effects of exercise on brain-derived neurotrophic factor. J Psychiatr Res. 2015;60:56–64. 10.1016/j.jpsychires.2014.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Marin Bosch B, Bringard A, Logrieco MG, Lauer E, Imobersteg N, Thomas A, Ferretti G, Schwartz S, Igloi K. A single session of moderate intensity exercise influences memory, endocannabinoids and brain derived neurotrophic factor levels in men. Sci Rep. 2021;11(1):14371. 10.1038/s41598-021-93813-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Börsch-Supan A, Brandt M, Hunkler C, et al. Data Resource Profile: the Survey of Health, Ageing and Retirement in Europe (SHARE). Int J Epidemiol. 2013;42(4):992–1001. 10.1093/ije/dyt088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Landös A, von Arx M, Cheval B, et al. Childhood socioeconomic circumstances and disability trajectories in older men and women: a European cohort study. Eur J Public Health. 2019;29(1):50–58. 10.1093/eurpub/cky166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Boisgontier MP, Orsholits D, von Arx M, et al. Adverse childhood experiences, depressive symptoms, functional dependence, and physical activity: a moderated mediation model. J Phys Act Health. 2020;17(8):790–799. 10.1123/jpah.2019-0133 [DOI] [PubMed] [Google Scholar]
- 48.Cheval B, Maltagliati S, Saoudi I, Fessler L, Farajzadeh A, Sieber S, Cullati S, Boisgontier MP. Physical activity mediates the effect of education on mental health trajectories in older age. J Affect Disord. 2023;336:64–73. 10.1016/j.jad.2023.05.052 [DOI] [PubMed] [Google Scholar]
- 49.Cheval B, Orsholits D, Sieber S, Courvoisier D, Cullati S, Boisgontier MP. Relationship between decline in cognitive resources and physical activity. Health Psychol. 2020;39(6):519–528. 10.1037/hea0000857 [DOI] [PubMed] [Google Scholar]
- 50.Cheval B, Rebar AL, Miller MW, Sieber S, Orsholits D, Baranyi G, Courvoisier D, Cullati S, Sander D, Chalabaev A, Boisgontier MP. Cognitive resources moderate the adverse impact of poor perceived neighborhood conditions on self-reported physical activity of older adults. Prev Med. 2019;126:105741. 10.1016/j.ypmed.2019.05.029 [DOI] [PubMed] [Google Scholar]
- 51.Cheval B, Saoudi I, Maltagliati S, Fessler L, Farajzadeh A, Sieber S, Cullati S, Boisgontier MP. Initial status and change in cognitive function mediate the association between academic education and physical activity in adults over 50 years of age. Psychol Aging. 2023;38(6):494–507. 10.1037/pag0000749 [DOI] [PubMed] [Google Scholar]
- 52.Cheval B, Sieber S, Guessous I, Orsholits D, Courvoisier DS, Kliegel M, Stringhini S, Swinnen SP, Burton-Jeangros C, Cullati S, Boisgontier MP. Effect of early- and adult-life socioeconomic circumstances on physical inactivity. Med Sci Sports Exerc. 2018;50(3):476–485. 10.1249/MSS.0000000000001472 [DOI] [PubMed] [Google Scholar]
- 53.Beenackers MA, Kamphuis CB, Giskes K, et al. Socioeconomic inequalities in occupational, leisure-time, and transport related physical activity among European adults: a systematic review. Int J Behav Nutr Phys Act. 2012;9:116. 10.1186/1479-5868-9-116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Clouston SA, Richards M, Cadar D, Hofer SM. Educational inequalities in health behaviors at midlife: is there a role for early-life cognition? J Health Soc Behav. 2015;56(3):323–340. 10.1177/0022146515594188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Droomers M, Schrijvers CT, Mackenbach JP. Educational level and decreases in leisure time physical activity: predictors from the longitudinal GLOBE study. J Epidemiol Community Health. 2001;55(8):562–568. 10.1136/jech.55.8.562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kari JT, Viinikainen J, Böckerman P, et al. Education leads to a more physically active lifestyle: evidence based on Mendelian randomization. Scand J Med Sci Sports. 2020;30(7):1194–1204. 10.1111/sms.13653 [DOI] [PubMed] [Google Scholar]
- 57.O’Donoghue G, Kennedy A, Puggina A, et al. Socio-economic determinants of physical activity across the life course: a “DEterminants of DIet and Physical ACtivity” (DEDIPAC) umbrella literature review. PLoS One. 2018;13(1):e0190737. 10.1371/journal.pone.0190737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ho DE, Imai K, King G, Stuart EA. Matching as nonparametric preprocessing for reducing model dependence in parametric causal inference. Political Anal. 2007;15(3):199–236. 10.1093/pan/mpl013 [DOI] [Google Scholar]
- 59.Ho D, Imai K, King G, Stuart E, Whitworth A, Greife N. MatchIt: Nonparametric preprocessing for parametric causal inference [R package]. Version 4.5.4; 2023. https://cran.r-project.org/web/packages/MatchIt/MatchIt.pdf [Google Scholar]
- 60.Boisgontier MP, Cheval B. The anova to mixed model transition. Neurosci Biobehav Rev. 2016;68:1004–1005. 10.1016/j.neubiorev.2016.05.034 [DOI] [PubMed] [Google Scholar]
- 61.Lohse K, Kozlowski A, Strube MJ. Model specification in mixed-effects models: a focus on random effects. Commun Kinesiol. 2023;1(5):1–28. 10.51224/cik.2023.52 [DOI] [Google Scholar]
- 62.R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2021. https://www.r-project.org [Google Scholar]
- 63.Bates D, Maechler M, Bolker B, Walker S, Christensen RHB, Singmann H, Dai B, Scheipl F, Grothendieck G, Green P, Fox J, Bauer A, Krivitsky PN. lme4: linear mixed-effects models using ‘eigen’ and S4 [R package]. Version 1.1–27.1; 2021. https://cran.r-project.org/web/packages/lme4/lme4.pdf [Google Scholar]
- 64.Kuznetsova A, Brockhoff PB, Christensen RHB. lmerTest: tests in linear mixed effects models [R package]. Version 3.1–3; 2016. https://cran.r-project.org/web/packages/lmerTest/lmerTest.pdf [Google Scholar]
- 65.Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67:1–48. 10.18637/jss.v067.i01 [DOI] [Google Scholar]
- 66.Bovim MR, Indredavik B, Hokstad A, Cumming T, Bernhardt J, Askim T. Relationship between pre-stroke physical activity and symptoms of post-stroke anxiety and depression: an observational study. J Rehabil Med. 2019;51(10):755–760. 10.2340/16501977-2610 [DOI] [PubMed] [Google Scholar]
- 67.Viktorisson A, Andersson EM, Lundström E, Sunnerhagen KS. Levels of physical activity before and after stroke in relation to early cognitive function. Sci Rep. 2021;11(1):9078. 10.1038/s41598-021-88606-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cotman CW, Berchtold NC, Christie LA. Exercise builds brain health: key roles of growth factor cascades and inflammation. Trends Neurosci. 2007;30(9):464–472. 10.1016/j.tins.2007.06.011 [DOI] [PubMed] [Google Scholar]
- 69.Gibbons TD, Cotter JD, Ainslie PN, Abraham WC, Mockett BG, Campbell HA, Jones EMW, Jenkins EJ, Thomas KN. Fasting for 20 h does not affect exercise-induced increases in circulating BDNF in humans. J Physiol. 2023;601(11):2121–2137. 10.1113/JP283582 [DOI] [PubMed] [Google Scholar]
- 70.Hillman CH, Erickson KI, Kramer AF. Be smart, exercise your heart: exercise effects on brain and cognition. Nat Rev Neurosci. 2008;9(1):58–65. 10.1038/nrn2298 [DOI] [PubMed] [Google Scholar]
- 71.Hadidi N, Treat-Jacobson DJ, Lindquist R. Poststroke depression and functional outcome: a critical review of literature. Heart Lung. 2009;38(2):151–162. 10.1016/j.hrtlng.2008.05.002 [DOI] [PubMed] [Google Scholar]
- 72.Lai SM, Duncan PW, Keighley J, Johnson D. Depressive symptoms and independence in BADL and IADL. J Rehabil Res Dev. 2002;39(5):589–596. [PubMed] [Google Scholar]
- 73.Engstad T, Bonaa KH, Viitanen M. Validity of self-reported stroke: the Tromso Study. Stroke. 2000;31(7):1602–1607. 10.1161/01.str.31.7.1602 [DOI] [PubMed] [Google Scholar]
- 74.van den Akker M, van Steenkiste B, Krutwagen E, Metsemakers JF. Disease or no disease? Disagreement on diagnoses between self-reports and medical records of adult patients. Eur J Gen Pract. 2015;21(1):45–51. 10.3109/13814788.2014.907266 [DOI] [PubMed] [Google Scholar]
- 75.Lee PH, Macfarlane DJ, Lam TH, Stewart SM. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): a systematic review. Int J Behav Nutr Phys Act. 2011;8:115. 10.1186/1479-5868-8-115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Prince SA, Adamo KB, Hamel ME, Hardt J, Connor Gorber S, Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Act. 2008;5:56. 10.1186/1479-5868-5-56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Dowd KP, Szeklicki R, Minetto MA, Murphy MH, Polito A, Ghigo E, van der Ploeg H, Ekelund U, Maciaszek J, Stemplewski R, Tomczak M, Donnelly AE. A systematic literature review of reviews on techniques for physical activity measurement in adults: a DEDIPAC study. Int J Behav Nutr Phys Act. 2018;15(1):15. 10.1186/s12966-017-0636-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Boisgontier MP, Iversen MD. Physical inactivity: a behavioral disorder in the physical therapist’s scope of practice. Phys Ther. 2020;100(5):743–746. 10.1093/ptj/pzaa011 [DOI] [PubMed] [Google Scholar]
- 79.APTA House of Delegates. Physical therapist’s scope of practice HOD P06–17-09–16/HOD P06–17-08–07. Accessed February 15, 2024. https://www.apta.org/contentassets/a400d547ca63438db1349c4a69bf7ead/position-pt-scope-practice.pdf
- 80.Shirley D, van der Ploeg HP, Bauman AE. Physical activity promotion in the physical therapy setting: perspectives from practitioners and students. Phys Ther. 2010;90:1311–1322. 10.2522/ptj.20090383 [DOI] [PubMed] [Google Scholar]
- 81.Allen L, O’Connell A, Kiermer V. How can we ensure visibility and diversity in research contributions? How the Contributor Role Taxonomy (CRediT) is helping the shift from authorship to contributorship. Learn Publ. 2019;32(1):71–74. 10.1002/leap.1210 [DOI] [Google Scholar]
- 82.Brand A, Allen L, Altman M, Hlava M, Scott J. Beyond authorship: attribution, contribution, collaboration, and credit. Learn Publ. 2015;28:151–155. 10.1087/20150211 [DOI] [Google Scholar]
- 83.Boisgontier MP. Research integrity requires to be aware of good and questionable research practices. Eur Rehabil J. 2022;2(1):1–3. 10.52057/erj.v2i1.24 [DOI] [Google Scholar]
- 84.Orsholits D, van Allen Z, Boisgontier MP. Pre-stroke physical activity matters for functional limitations (v1.2). Zenodo. 2024. 10.5281/zenodo.10668778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.van Allen Z, Orsholits D, Boisgontier MP. Functional limitations in stroke survivors: pre-stroke physical activity matters. MedRxiv. 2023. 10.1101/2023.09.14.23295576 [DOI] [Google Scholar]
- 86.von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4(10):e296. 10.1371/journal.pmed.0040296 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
In accordance with good research practices83, the R code used to analyze the data is publicly available online84. A non-peer-reviewed version of this manuscript is publicly available online85. The SHARE dataset is available at http://www.share-project.org/data-access.html and the DOIs for the waves used in the current study are the following: https://doi.org/10.6103/SHARE.w1.600, https://doi.org/10.6103/SHARE.w2.600, https://doi.org/10.6103/SHARE.w4.600, https://doi.org/10.6103/SHARE.w5.600, https://doi.org/10.6103/SHARE.w6.600, https://doi.org/10.6103/SHARE.w7.711, https://doi.org/10.6103/SHARE.w8cabeta.001.