Abstract
Context:
Educational interventions can help individuals increase their knowledge of available contraceptive methods, enabling them to make informed decisions and use contraception correctly. This review updates a previous review of contraceptive education.
Evidence acquisition:
Multiple databases were searched for articles published March 2011–November 2016. Primary outcomes were knowledge, participation in and satisfaction/comfort with decision making, attitudes toward contraception, and selection of more effective methods. Secondary outcomes included contraceptive behaviors and pregnancy. Excluded articles described interventions that had no comparison group, could not be conducted feasibly in a clinic setting, or were conducted outside the U.S. or similar country.
Evidence synthesis:
A total of 24,953 articles were identified. Combined with the original review, 37 articles met inclusion criteria and described 31 studies implementing a range of educational approaches (interactive tools, written materials, audio/videotapes, and text messages), with and without healthcare provider feedback, for a total of 36 independent interventions. Of the 31 interventions for which knowledge was assessed, 28 had a positive effect. Fewer were assessed for their effect on attitudes toward contraception, selection of more effective methods, contraceptive behaviors, or pregnancy—although increased knowledge was found to mediate additional outcomes (positive attitudes toward contraception and contraceptive continuation).
Conclusions:
This systematic review is consistent with evidence from the broader healthcare field in suggesting that a range of interventions can increase knowledge. Future studies should assess what aspects are most effective, the benefits of including provider feedback, and the extent to which educational interventions can facilitate behavior change and attainment of reproductive health goals.
Theme information:
This article is part of a theme issue entitled Updating the Systematic Reviews Used to Develop the U.S. Recommendations for Providing Quality Family Planning Services, which is sponsored by the Office of Population Affairs, U.S. Department of Health and Human Services.
CONTEXT
Despite the availability of a wide variety of effective contraceptive methods,1 nearly half of all pregnancies in the U.S. are unintended.2 Unintended pregnancy primarily occurs in women who do not use any contraception or use contraception incorrectly or inconsistently.3,4 Contraceptive counseling provided by trained healthcare professionals may help sexually active individuals and couples identify contraceptive methods that are the most appropriate and effective for their lifestyle and preferences. An essential component of the counseling process is education. Contraceptive education aims to provide clients the information they need to make informed decisions about their use of contraception and correctly use the contraceptive methods they have selected.
The importance of contraceptive education can be seen in the impact of knowledge on method selection and correct and consistent use of contraception. Many women indicate contraceptive effectiveness is among the most important considerations for selecting a method5–9; consistent with this priority, better knowledge of contraceptive effectiveness is associated with adoption of more effective methods.10,11 Conversely, inadequate knowledge of contraception is associated with incorrect perceptions of the risks and side effects of contraceptive methods, incorrect or inconsistent use, and method discontinuation.12–15 Despite the importance of education, gaps in contraceptive knowledge are frequently documented.11,16,17
In 2011, the Centers for Disease Control and Prevention (CDC) and the U.S. Office of Population Affairs conducted a systematic review to better understand the aspects of educational interventions that can promote acquisition of knowledge for informed decision making and correct and continued use of contraception.18 That review informed the development of the 2014 recommendations, Providing Quality Family Planning Services: Recommendations of CDC and the U.S. Office of Population Affairs.19 The objective of this updated review is to summarize the body of evidence that was published subsequently.
EVIDENCE ACQUISITION
Definition of Contraceptive Education
This review complements findings of the accompanying review on contraceptive counseling,20 defined as an interactive process between a provider and client intended to help the client achieve a reproductive health goal. This education review focuses more narrowly on the process of helping clients increase their knowledge of contraception so they can make informed decisions about using contraception, and then correctly and consistently use their chosen method.
Development of Key Questions and Search Strategy
This systematic review is reported according to the PRISMA checklist.21 The approach used was similar to that implemented in previous reviews22 guided by an analytic framework showing the logical relationships between the population of interest, the interventions, and the outcomes of interest (Figure 1). This review of education interventions primarily focused on short-term outcomes related to contraceptive knowledge and decision making; studies were excluded if the intervention they described focused only on skills or behaviors. Of seven key questions (KQs; Table 1), the first five (KQ1–KQ5) asked whether educational interventions affected the following: contraceptive knowledge, including correct method use, risks and benefits, side effects, and method effectiveness; participation in decision making; satisfaction/comfort with services and decision making; attitudes toward contraception; and for interventions providing education on the full range of methods, selection of more versus less effective methods (KQ5). KQ6 was expanded from a focus in the original review on health literacy and asked if there were any barriers or facilitators for clinics/clients; KQ7 was added to address unintended consequences.
Figure 1. Analytic framework for systematic review of impact of contraceptive education.
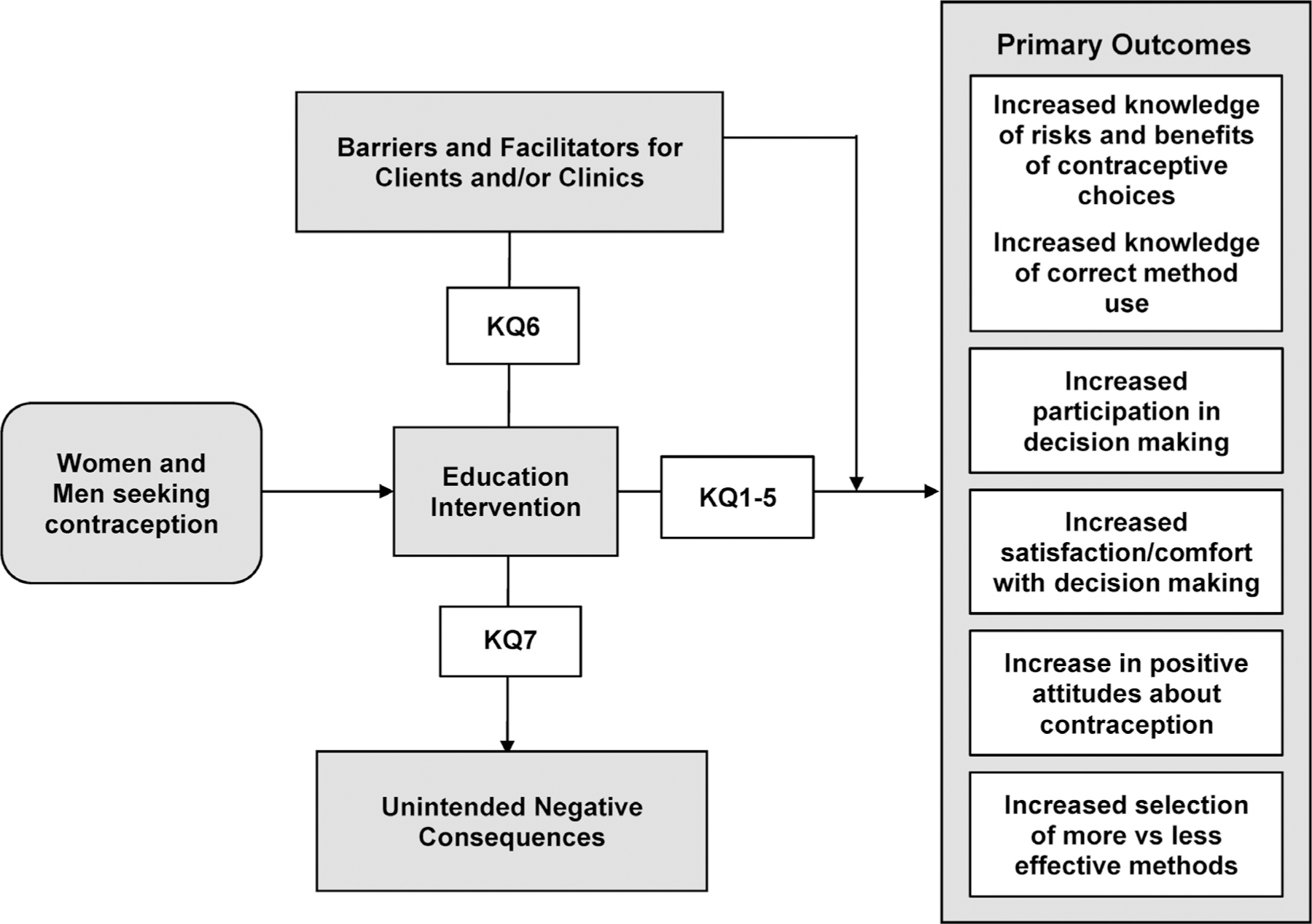
KQ, key question.
Table 1.
Key Questions for Systematic Review on Impact of Education Interventions
| KQ no. | Question |
|---|---|
| 1 | Does contraceptive education increase comprehension of risks and benefits of contraceptive choices, including potential side effects, method effectiveness, and correct method use? |
| 2 | Does contraceptive education increase participation in the decision-making process? |
| 3 | Does contraceptive education increase satisfaction/comfort with services and decision making? |
| 4 | Does contraceptive education increase positive attitudes about contraception? |
| 5 | Does contraceptive education increase selection of more as compared with less effective methods? |
| 6 | What are the barriers and facilitators for clinics or clients related to the provision or receipt of education? |
| 7 | Are there any unintended negative consequences associated with contraceptive education? |
Note: The key questions are put into context by the analytic framework presented in Figure 1.
KQ, key question.
The search strategy included terms common to the other systematic reviews in this series on contraceptive counseling, reminder systems, and patient preferences for contraceptive counseling. Articles were identified from 16 electronic databases (Appendix Table 1, available online), and supplemented by hand searches of the bibliographies of identified articles. The initial and updated reviews identified articles published between January 1985–February 2011 and March 2011–November 2017, respectively.
Retrieval and inclusion criteria were developed a priori. Included studies were conducted in a clinic-based setting where family planning services: were provided or assessed an intervention that could be implemented feasibly in a clinic-based setting (e.g., not a multisession course series); contained a comparison group; were conducted in the U.S., Canada, Australia, New Zealand, or a European country categorized as “very high” on the Human Development Index23; and addressed at least one KQ. Studies focusing primarily on sexually transmitted infections were included only if they incorporated education on condom use to prevent pregnancy. For studies meeting inclusion criteria, outcomes of interest to other systematic reviews in this series (i.e., behavioral outcomes, such as contraceptive use, and long-term outcomes, such as pregnancy) also were evaluated because of their potential to be mediated by knowledge. Outcomes related to the KQs were considered primary outcomes; all other outcomes were considered secondary outcomes.
Data Abstraction
Detailed information was abstracted by a team of four abstractors and reviewed by two authors for relevance to contraceptive education; differences were reconciled by consensus. In provider-enhanced interventions, a healthcare provider/educator interacted with the intervention to help participants in at least one group understand or use the information presented. By contrast, in provider-independent interventions a healthcare provider/educator did not go beyond the standard of care to facilitate participant understanding; the participant received the intervention either before or after, rather than during their appointment, and providers were given no specific instructions to help participants understand or make use of information. Studies were classified as evaluating more than one intervention if they included distinct mediums (e.g., written materials versus audio/video) or a provider-independent and a provider-enhanced intervention, each of which was separately compared with a control arm.
Assessment of Study Quality and Data Synthesis
Study quality was assessed using a modification of the grading system developed by the U.S. Preventive Services Task Force.24 Studies were first rated based on the U.S. Preventive Services Task Force evidence scale and then specific criteria were used to judge whether the study had high, moderate, or low risk for bias.
Data synthesis was primarily qualitative. Meta-analysis was not performed because of the large degree of heterogeneity across studies with respect to study design, study populations, lengths of follow-up, and outcomes measured.
Evidence from the initial and updated systematic reviews (Figure 2), including primary and secondary outcomes, is summarized in Figure 3 and presented in detail in Appendix Table 2 (available online). Primary outcomes from the review update are further discussed in the text.
Figure 2.
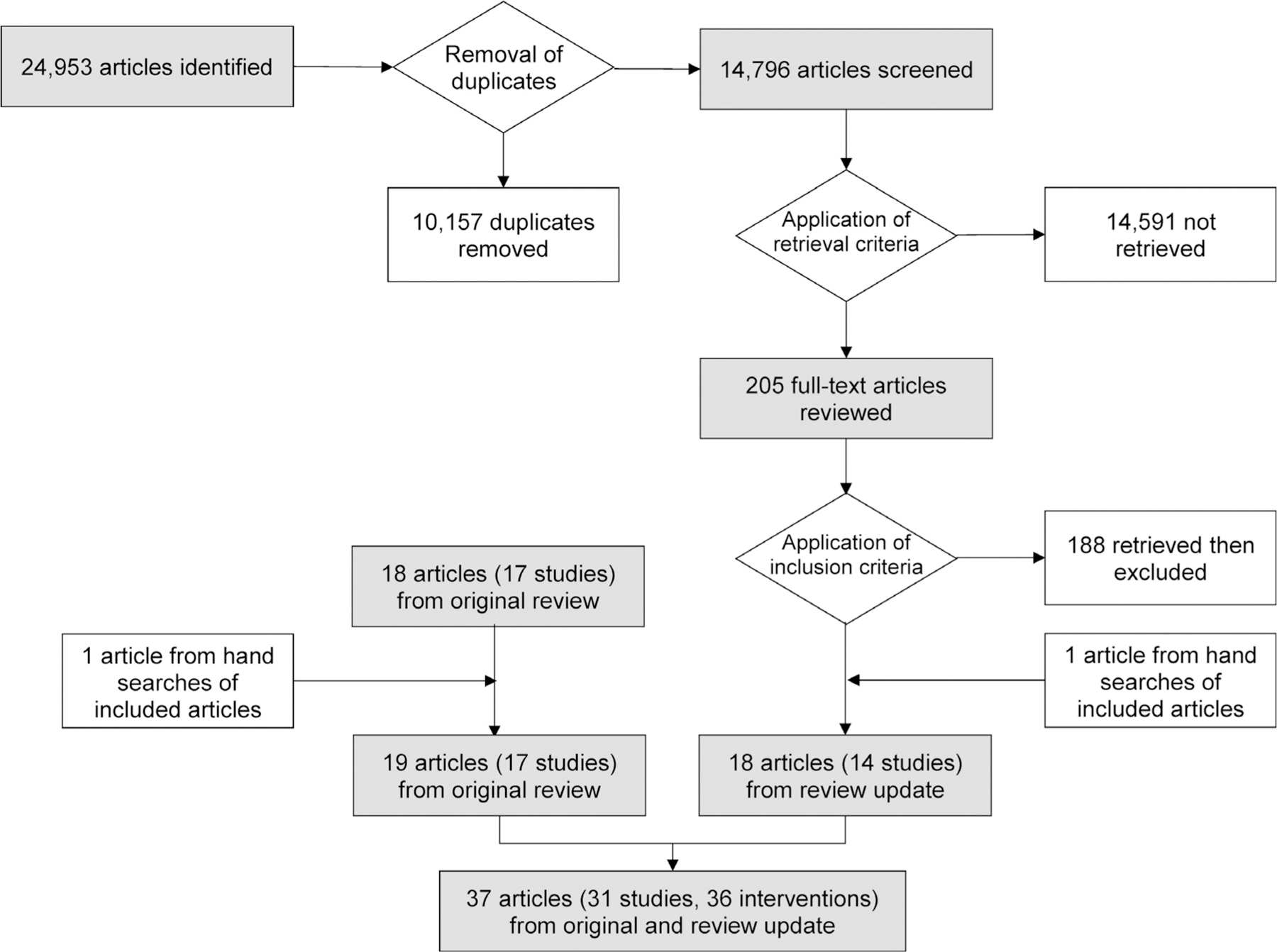
Flow diagram—process of identifying studies included.
Figure 3. Summary of evidence from systematic review on contraceptive education.
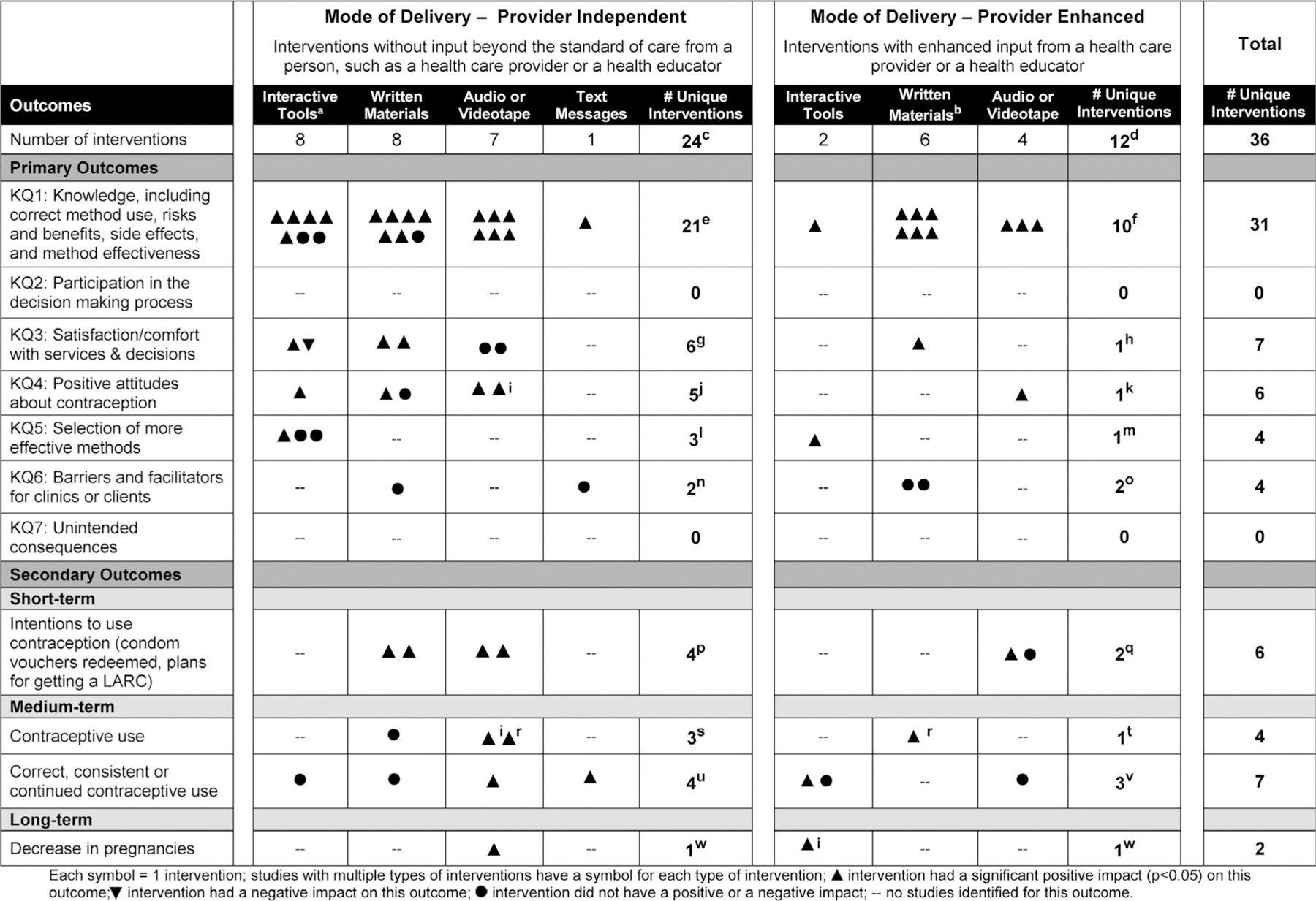
aIncludes decision aids, computer games, Facebook page, and smart phone apps.
bMaterials provided or read as a script.
cInterventions described in Kirby et al. 198949; Paperny and Starn 198954; Reis and Tymchyshyn 199256; O’Donnell et al. 199552,53; Smith and Whitfield 199559; Deijen and Kornaat 199746; Little 1998,44 200143; DeLamater et al. 200047; Lindenberg et al. 200250; Johnson et al. 200348; Mason et al. 200351; Steiner et al. 200360; Roberto et al. 200757; Schwarz et al. 200858; Castano et al. 201225; Hall et al. 2013,32 201442; Garbers et al. 201229,30; Vogt and Schaefer 201241; Schwarz et al. 201338; Gilliam et al. 201431; Kofinas et al. 201433; Davidson et al. 201526; Garbers et al. 201528; and Sridhar et al. 2015.40
dInterventions described in: O’Donnell et al. 199552,53; Little et al. 1998,44 200143; Chewning et al. 199945; DeLamater et al. 200047; Pedrazzini et al. 200055; Whitaker et al. 201061; Ragland et al. 201136; Garbers et al. 201229,30; Schwarz et al. 201439; Lee et al. 201534; Ragland et al. 201537; de Reilhac et al. 201627; and Michie et al. 2016.35
eInterventions described in: Kirby et al. 198949; Paperny and Starn 198954; Reis and Tymchyshyn 199256; O’Donnell et al. 199552,53; Smith and Whitfield 199559; Deijen and Kornaat 199746; Little 1998,44 200143; DeLamater et al. 200047; Lindenberg et al. 200250; Mason et al. 200351; Steiner et al. 200360; Roberto et al. 200757; Schwarz et al. 200858; Castano et al. 201225; Hall et al. 2013,32 201442; Vogt and Schaefer 201241; Schwarz et al. 201338; Gilliam et al. 201431; Kofinas et al. 201433; Garbers et al. 201528; and Sridhar et al. 2015.40
fInterventions described in O’Donnell et al. 199552,53; Little et al. 1998,44 200143; Chewning et al. 199945; DeLamater et al. 200047; Pedrazzini et al. 200055; Ragland et al. 201136; Schwarz et al. 201439; Lee et al. 201534; Ragland et al. 201537; de Reilhac et al. 201627; and Michie et al. 2016.35
gInterventions described in Johnson et al. 200348; Mason et al. 200351; Steiner et al. 200360; Kofinas et al. 201433; Davidson et al. 201526; and Sridhar et al. 2015.40
hIntervention described in: Schwarz et al. 201439; Lee et al. 2015.34
iIndicates intervention had a marginally significant effect on this outcome (0.05<p<0.1).
jInterventions described in Deijen and Kornaat 199746; Schwarz et al. 200858; Vogt and Schaefer 201241; and Kofinas et al. 2014.33
kIntervention described in Whitaker et al. 2010.61
lInterventions described in Garbers et al. 201230; Gilliam et al. 201431; and Sridhar et al. 2015.40
mIntervention described in Garbers et al. 2012.30
nInteraction with educational level described in Little et al. 200143 and Hall et al. 2013.32
oInteraction with educational level described in Little et al. 200143 and Regland et al. 2011.
pInterventions described in Kirby et al. 198949; O’Donnell et al. 199552,53; Vogt and Schaefer 201241; and Garbers et al. 2015.28
qInterventions described in O’Donnell et al. 199552,53 and Michie et al. 2016.35
rSignificant increase over baseline, but significance of increase relative to controls not reported.
sInterventions described in Kirby et al. 198949; DeLamater et al. 200047; and Schwarz et al. 2008.58
tIntervention described in DeLamater et al. 2000.47
uInterventions described in Deijen and Kornaat 199746; Garbers et al. 201229; and Castano et al. 201225; Hall et al. 2013,32 2014.42
vInterventions described in Chewning et al. 199945; Garbers et al. 201229; and Michie et al. 2016.35
wIntervention described in Schwarz et al. 2008.58
xIntervention described in Chewning et al. 1999.45
KQ, key question.
EVIDENCE SYNTHESIS
Search Results
The systematic review identified 14,796 unique abstracts. From the title and abstract review, 14,591 articles were excluded and 205 were retrieved; 17 met inclusion criteria.25–41 However, because three studies including the same population and intervention were described in multiple articles,25,29,30,32,34,39 these articles were counted as 14 independent studies. Hand searches of references from included articles identified one additional article42 providing further details on a study from the review update,25,32 and one article,43 providing further details on a study from the original review.44 Together with evidence from the original review,18 31 studies described in 37 articles are included in this review update (Figure 2).25–61
Of the included studies, 17 were RCTs, of which nine were classified as having low,27,29,30,33,43,44,47,49,52,53,58,60 six moderate,25,26,31,32,35,40,42,46 and two high38,51 risk for bias. Three were non-RCTs with separate groups of intervention and control participants; of these, two were classified as having moderate45,54 and one high57 risk for bias. Nine used a pre-/post-test study design, of which three were classified as having moderate36,37,41 and six high28,50,55,56,59,61 risk for bias. Two final studies, also with high risk for bias, used a sequential cohort analysis in which one set of participants was studied prior to implementation of an intervention and was compared with another set of participants studied during the intervention period.34,39,48
Of the 31 studies identified, five included two interventions (one included a written intervention and an audio/video intervention46; four included a provider-independent and a provider-enhanced intervention29,30,43,44,47,52,53) that were each separately compared with a control arm, for a total of 36 interventions. In addition to being assessed for their effects on the a priori outcomes of interest (Figure 3), for three interventions, knowledge gains were evaluated for their further effect on these outcomes, including positive attitudes toward oral contraceptives (OCs)41 and long-acting reversible contraceptives (LARC),33 intention to use OCs,41 and continued use of OCs.25,42
Knowledge
The review update identified 12 interventions25,27,28,31–42 assessed for their effect on knowledge (KQ1), including knowledge of correct method use, risks and benefits, side effects, and method effectiveness; of these, ten had a significant positive effect.25,27,28,31–37,39,41,42 Details are described separately for provider-independent and provider-enhanced interventions.
Provider-independent interventions.
The review update identified seven provider-independent interventions.25,28,31–33,38,40–42 Of these, three were non-interactive, assessing either a video,28 written materials,41 or text messages25,32,42; all three had a significant positive effect. The first28 used a pre-/post-test analysis to assess the effect of a single online video session; the video was based on social and cognitive theories and provided information on intrauterine devices (IUDs). Immediately following the video, participants showed an increase from baseline in their knowledge that the IUD is more effective than the pill (p<0.001) and that women who have never had a child can use an IUD (p<0.001). The second intervention41 also used a pre-/post-test analysis to examine knowledge among participants who received a comprehensive information brochure on OCs using either a standard evidence-based or a mental models approach. Participants receiving either type of brochure were combined into one group for analysis, which showed an increase in knowledge from baseline to immediate post-test (p<0.001), and from baseline to 3 months (p<0.001). The third intervention25,32,42 was evaluated through an RCT and used daily text messages to address key domains of information for OCs (mechanism of action, effectiveness, use, side effects, risks, and benefits). From baseline to 6 months, knowledge scores increased 7% in the intervention versus 3% in the control group (p<0.001). While the groups were similar at baseline, at 6 months intervention participants had higher scores related to mechanisms of action (p=0.004); side effects (p=0.03); effectiveness (p<0.001); and potential OC benefits (p<0.001).
The remaining four provider-independent interventions were interactive tools, each evaluated through an RCT.31,33,38,40 Of these, two had a significant positive effect.31,33 The first31 was based on the theory of planned behavior and was intended to fill gaps in knowledge of LARC, while also providing information on the full range of methods. Knowledge among intervention participants increased from baseline to immediate post-intervention (p=0.001).31 The second33 presented information from American College of Obstetricians and Gynecologists contraceptive education pamphlets through an interactive Facebook page with videos, diagrams, and games; control participants were given the same amount of time to review the education pamphlets on the American College of Obstetricians and Gynecologists webpage. Although control participants had higher knowledge scores at baseline (p=0.04), Facebook participants showed greater knowledge gains (p<0.001) and higher post-test scores (p<0.001). Of the two interactive tools that did not have a significant effect, the first38 was based on CDC’s U.S. Medical Eligibility Criteria; it allowed participants to explore their contraceptive options and then request a prescription if they wanted a method requiring one; control participants were provided a similar tool with information on chlamydia infection. Immediately following use of their respective tools, intervention and control participants did not differ in their knowledge of relative method effectiveness (LARC versus tubal ligation, p=0.26; patch/ring versus birth control pills, p=0.16), or the effectiveness of condoms for preventing pregnancy (p=0.49). The second tool40 was a smartphone app that allowed participants to access information on a range of contraceptive options. Control participants received standard-of-care counseling from a health educator. Mean scores for knowledge related to the participant’s selected method did not differ between the intervention and control groups immediately post-intervention (p=0.30).
In combination with the original review,18 21 provider-independent interventions were evaluated for their effect on knowledge. Only one50 of 1425,28,41,43,44,46,47,49–53,58–60 non-interactive and two38,40 of seven31,33,38,40,54,56,57 interactive interventions did not have a positive effect on at least one outcome (Figure 3; Appendix Table 2, available online). Only one study compared delivery of the same information in an interactive and a non-interactive format, with participants in the interactive group showing greater knowledge gains.33
Provider-enhanced interventions.
The review update identified five provider-enhanced interventions evaluated for their effect on knowledge.27,34–37,39 Of these, one included a video intervention35 and four used written materials delivered as a script from a healthcare provider.27,34,36,37,39 The video intervention,35 evaluated through an RCT, was a 9-minute DVD presenting information on Nexplanon to abortion patients considering use of this method for the first time. During their appointment, intervention participants viewed the DVD and were then given the opportunity to ask their provider questions. Immediately post-intervention, a higher percentage of intervention versus control participants correctly responded to the effect of implants on mood and skin changes (p=0.004), although they did not differ in knowledge related to duration of effectiveness, mechanisms of action, or return to fertility.
The first provider-enhanced intervention using written materials27 also was evaluated through an RCT. Providers used a checklist to deliver information determined through a Delphi interview process of 100 gynecologists to be essential for women considering OCs for the first time. Compared with the control group, the intervention group had a higher median knowledge score (p<0.001), and for 15 of 22 questions, a higher percentage of participants with correct responses (range by response, p<0.05–p<0.0001). The next two interventions36,37 similarly included the use of a flip chart to deliver information about emergency contraception during a 5-minute session; the first36 was delivered in the waiting room of a women’s clinic, and the second37 was delivered at a grocery store pharmacy; both were evaluated through a pre-/post-test analysis. With the clinic-based intervention, knowledge scores increased from baseline to immediate post-test (p<0.001), and remained elevated at 1–5 months (p-value not reported). With the pharmacy-based intervention, knowledge scores also increased from baseline to immediate post-test (p<0.001); at 1–3 months follow-up, knowledge scores remained higher than at baseline (p=0.014), although they were lower than immediate post-test scores (p<0.001). The final provider-enhanced intervention using written materials34,39 was evaluated through a sequential cohort analysis. During, but not prior to, the intervention period, providers used a checklist as a reminder to ask patients seeking walk-in services for pregnancy testing or emergency contraception about their pregnancy intentions and any unprotected sex in the past week. Providers then read a short script describing the effectiveness of LARCs relative to other methods, and offered participants emergency contraception or same-day LARC insertion, as appropriate. Immediately following their appointment, participants in the intervention versus the pre-intervention cohort had greater knowledge of LARC effectiveness and duration relative to other methods (p<0.05, both outcomes). However, findings related to knowledge of the reversibility of LARCs were mixed, as were findings related to knowledge at 3 months.
In combination with the original review,18 a total of ten provider-enhanced interventions were assessed for their effect on knowledge; all ten had a significant positive effect (Figure 3, Appendix Table 2, available online).27,34–37,39,43–45,47,52,55
Satisfaction/Comfort With Services and Decision Making
Four interventions in the review update were assessed for their effect on satisfaction/comfort with services and decision making (KQ3): three were provider-independent interventions assessed through an RCT,26,33,40 and one was a provider-enhanced intervention assessed through a sequential cohort analysis.34,39 Of the provider-independent interventions, the first33 found that intervention participants given the opportunity to interact with a Facebook page, versus control participants allowed to view pamphlets with the same information, had higher composite scores for satisfaction with the counseling they received (p<0.001). By contrast, the second intervention40 found a lower percentage of intervention participants using a smartphone app, versus control participants receiving standard-of-care counseling from a health educator, who reported they were very satisfied with the counseling they received (p<0.001). The third provider-independent intervention26 was a video informed by the transtheoretical model of behavioral change designed to increase awareness and dispel misconceptions about LARC. Intervention and control participants did not differ as to whether they reported that they had been given sufficient information (p=0.94); they had been able to make their own decision (p=0.21); staff had respected their decision (p=0.54); or that they were satisfied with their decision (p=0.94) and counseling received (p=0.82). The one provider-enhanced intervention assessed for its effect on satisfaction was the sequential cohort analysis that was previously described.34,39 In this analysis, a higher percentage of participants in the intervention versus the pre-intervention cohort, having been read a short script on LARC effectiveness, reported that all their questions about birth control had been answered (p<0.001), and that they were satisfied with the discussion (p=0.03).
In combination with the original review,18 seven interventions were assessed for their effect on satisfaction/comfort with services and decision making (Figure 3, Appendix Table 2, available online). Findings remained mixed. Six of the seven interventions were provider-independent interventions, with three finding a significant positive effect,33,48,60 two finding no effect,26,51 and one finding a significant negative effect40; only one provider-enhanced intervention was identified.34,39
Positive Attitudes Toward Contraception
Two provider-independent interventions were identified in the review update that assessed attitudes toward contraception (KQ4), both with a positive effect. The first,41 evaluated through a pre-/post-test analysis of a comprehensive information brochure, as described earlier, resulted in an immediate post-test increase in participants’ scores for a positive attitude about OCs (p<0.001); although scores dropped after 3 months, they remained higher than at baseline (p=0.036). Moreover, the increase was positively associated with knowledge scores, both immediately post-test (r=0.284, p=0.001) and at the 3-month follow-up (r=0.206, p=0.022). The second intervention,33 also described earlier, resulted in a significantly greater proportion of participants in the interactive Facebook group expressing a preference for implants in particular (p<0.01), or LARC in general (p<0.01). Moreover, knowledge was again an important factor. For both study arms combined, greater increases in knowledge (4%, 12%, 24%, and 36%) were associated with a greater increase in the RR of stating a preference for LARC (RRs: 1.06, 1.19, 1.43, and 1.71, respectively, 95% CIs in Appendix Table 2, available online).
In combination with the original review,18 six different interventions assessed the effect of educational tools on attitudes toward contraception (Figure 3, Appendix Table 2, available online). Except for one intervention using written materials alone,46 each had a positive effect.33,41,46,58,61
Selection of More Effective Contraceptive Methods
The review update identified four interventions, assessed through three RCTs30,31,40 that addressed the selection of more versus less effective contraceptive methods and also provided education on the full range of contraceptive options (KQ5; Figure 3, Appendix Table 2, available online). Two of these interventions were provider-independent interactive tools described previously: one filled gaps in knowledge of LARC, while also providing information on the full range of contraceptive options,31 and the other presented methods in the order of effectiveness.40 Neither resulted in differences in LARC uptake among intervention versus control participants (Gilliam et al.31: p=0.77, Sridhar and colleagues40: p=0.75). The final study30 found a positive effect of both a provider-independent and a provider-enhanced intervention. This study assessed a computer-based contraceptive assessment module in which intervention participants received either a generic list of methods (provider-independent), or a list of methods tailored to their responses, which they were instructed to share with their healthcare provider (provider-enhanced). Among participants in the control group who were not exposed to any tool, 65% selected an effective method (i.e., injectables, pills, patches, or rings), and 15% selected a highly effective method (i.e., IUD or implant); in comparison to these percentage for the control group, selection of effective and highly effective methods, respectively, was greater in both the generic (78% and 24%, p<0.001) and tailored information arm (75% and 22%, p<0.001), and both intervention arms had increased odds relative to controls of selecting an effective method (generic vs control: OR=1.74, 95% CI=1.35, 2.25; tailored vs control: OR=1.56, 95% CI=1.23, 1.98).
No studies from the original review18 evaluated the effect of educational interventions on selection of more effective methods.
Educational Attainment as a Facilitator or Barrier
The review update identified four interventions (two provider-independent32,43 and two provider-enhanced36,43), assessed through two RCTs32,43 and one pre-/post-test analysis,36 that asked whether a participant’s education level impacted knowledge gains (KQ6; Figure 3, Appendix Table 2, available online). One study assessed the interaction of patient education with use of text messages,32 one with written materials delivered by a provider using a flip chart,36 and one with use of either a summary card or full-length brochure, delivered with or without interactive questions delivered by a provider.43 With three of the interventions, knowledge gains were similar across education categories (text messages: p=0.49; summary card or full-length brochure without interactive questions: p=0.9; or with interactive questions: p=0.6).32,43 Education interacted with the final intervention in which providers delivered information using a flip chart: Increases in knowledge were greater for participants with a high school education versus those with some college education or above (136% vs 51%, p=0.016).36
No studies from the original review18 assessed the effect of educational attainment on knowledge gains.
DISCUSSION
The initial and updated reviews identified 31 independent educational interventions using a variety of mediums (i.e., written materials, audio/videotapes, text messages, and interactive tools) assessed for their effect on knowledge.25,27,28,31–47,49–52,54–60 All but three38,40,50 of the 31 interventions had a significant positive effect, and 1625,27,32,33,35,42–44,46,47,49,52–54,58,60 of those with a positive effect were evaluated through RCTs characterized by low/moderate risk for bias. These findings are consistent with the initial review18 and other systematic reviews from the broader healthcare field,62,63 in suggesting a wide range of educational interventions can help increase client understanding.
Although the original review18 did not identify any interventions assessed for their interaction with client educational attainment, the review update identified four such interventions. With three,32,36,43 increases in knowledge did not differ by educational attainment; the benefit of the fourth was greater for participants with less versus more education.36 Although the educational level targeted by these interventions was not described, it is possible they were effective across educational levels because they were designed for individuals with lower levels of educational attainment. This would be consistent with recommendations from evidence-based tool kits from the broader healthcare field suggesting that health education materials be easy to interpret by clients with a fourth- to sixth-grade reading level,64–66 and that certain basic strategies can be used to simplify information and promote comprehension for all clients. These strategies include appropriately presenting numeric quantities (e.g., by using common denominators and natural frequencies, such as “1 in 100 versus 5 in 100”),67–79 limiting the amount of information presented, and highlighting important facts by placing them first.80–82 Given the initial review identified only two studies that assessed the use of such strategies for simplifying the presentation of information (both of which had mixed results),44,60 and no additional studies were identified in the review update, more detailed research specific to contraception is warranted.
Few conclusions can be drawn with respect to the secondary outcomes. For intentions to use contraception, the one secondary outcome considered a short-term outcome in the accompanying reviews, there was a positive effect in all but one35 of six interventions.28,35,41,49,52,53 However, with respect to medium- and long-term outcomes (i.e., contraceptive use, including correct, consistent, or continued use, and pregnancy), a positive effect was found in a smaller proportion of interventions, which may be because broader counseling interventions are needed to address outcomes associated with behavioral change and reproductive health goals.83 Nonetheless, with three interventions, knowledge mediated additional outcomes of interest, including positive attitudes toward OCs41 or LARCs,33 intentions to use OCs,41 and continued use of OCs.25,42
Finally, this update adds to evidence about the extent to which educational interventions are more effective with input from a health provider/educator. With respect to knowledge (KQ1), all ten provider-enhanced versus 18 of 21 provider-independent interventions had a significant positive effect. However, for satisfaction/comfort with decision making and services (KQ3), positive attitudes (KQ4), and selection of more effective methods (KQ5), only one provider-enhanced intervention was identified, thus providing little basis for comparison. Of note, however, four RCTs with low risk for bias (three from the original review44,47,52,53 and one from the review update29,30) were identified comparing the same intervention with and without feedback from a healthcare provider. Results were mixed. In the first, participants who attended a face-to-face session with a health educator, versus those who received similar information through a video, made greater knowledge gains relative to controls.47 In the second, participants who received either a simplified tool or a standard leaflet showed increases in knowledge relative to controls; however, although the increase relative to controls was even greater when the simplified tool was paired with interactive questions from a provider, there was no additive effect with the standard leaflet.44 In the third RCT, the addition of a facilitator-led discussion session was no more effective than a videotape alone for increasing knowledge relative to controls,52 but did result in a higher proportion of participants redeeming vouchers for free condoms.53 The final RCT, described above,30 found that a contraceptive assessment tool was similarly effective at promoting selection of more effective methods with and without provider enhancement. However, only participants in the provider enhanced group showed higher odds relative to controls of using their selected method correctly and continuing at 4 months.29
One reason for the mixed results on provider feedback may be that educational tools by themselves are only effective for some types of learning. Research from other areas of health care has demonstrated the effectiveness of active learning techniques.84–87 Such learning can be readily incorporated into interactive tools, many of which have been developed recently for contraception and included in this review, with mixed results.29–31,33,38,40 However, these tools may not enhance more complex interactions. For instance, the teach-back method, in which clients restate the most important messages in their own words, has been shown to ensure comprehension,88,89 and was recently used to lower IUD discontinuation rates.90 Similarly, interactive tools by themselves may not be sufficient for other components of counseling that build upon knowledge, such as skill building or evaluating options in light of individual needs and preferences. More recently, contraceptive decision aids have been developed as provider tools for improving contraceptive counseling.91,92 Research is needed to assess whether contraceptive decision aids developed for this purpose can further promote satisfaction with services, and attainment of behavioral and reproductive health goals.
Limitations
This evidence summarizing the impact of educational interventions has several limitations, which should be considered when interpreting the evidence. Although several high-quality studies were identified for assessing the impact of educational interventions on knowledge, fewer were identified for the remaining primary outcomes targeted by contraceptive education. Seven studies assessed satisfaction/comfort with services and decision making, of which four were RCTs with low/moderate risk,26,33,40,60 and three had high risk for bias.34,39,48,51 Of the five studies assessing positive attitudes toward contraception, three were RCTs with low/moderate risk for bias,33,46,58 and two had a high risk for bias or a less rigorous design.41,61 Only three studies were identified that assessed selection of more effective methods, although all were RCTs with low/moderate risk for bias.30,31,40 The authors were unable to identify any studies that addressed participation in the decision-making process. Additionally, as noted above, there was insufficient evidence to assess strategies for simplifying the presentation of information or the importance of input from a healthcare provider. Lastly, it is possible that additional articles meeting the inclusion criteria for this systematic review have been published since the updated search of the literature.
CONCLUSIONS
This systematic review provides clear evidence that a wide range of educational interventions can effectively increase client understanding. Although the small number of studies addressing the remaining outcomes limited additional conclusions, some studies demonstrated that increases in knowledge can mediate additional outcomes of interest. Future studies should assess what aspects of interventions for increasing knowledge and promoting informed decision making are most effective with respect to contraception, the benefits of including provider feedback, and the extent to which educational interventions can facilitate behavior change and attainment of reproductive health goals.
Supplementary Material
ACKNOWLEDGMENTS
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the Office of Population Affairs.
This product was supported, in part, by a contract between the Office of Population Affairs and Atlas Research, Inc. (HHSP233201500126I, HHSP233201450040A).
Footnotes
No conflicts of interest or financial disclosures were reported by the authors of this paper.
THEME NOTE
This article is part of a theme issue entitled Updating the Systematic Reviews Used to Develop the U.S. Recommendations for Providing Quality Family Planning Services, which is sponsored by the Office of Population Affairs, U.S. Department of Health and Human Services.
SUPPLEMENTAL MATERIAL
Supplemental materials associated with this article can be found in the online version at doi:10.1016/j.amepre.2018.07.012.
REFERENCES
- 1.Hatcher R, Trussell J, Nelson A, Cates W, Kowal D, Policar M. Contraceptive Technology Atlanta, GA: Ardent Media, 2011. [Google Scholar]
- 2.Finer LB, Zolna MR. Declines in unintended pregnancy in the United States, 2008–2011. N Engl J Med 2016;374(9):843–852. 10.1056/NEJMsa1506575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gold RB, Sonfield A, Richards CL, Frost JJ. Next Steps for America’s Family Planning Program: Leveraging the Potential of Medicaid and Title X in an Evolving Health Care System New York, NY: Guttmacher Institute, 2009. [Google Scholar]
- 4.Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception 2011;84(5):478–485. 10.1016/j.contraception.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stanwood NL, Bradley KA. Young pregnant women’s knowledge of modern intrauterine devices. Obstet Gynecol 2006;108(6):1417–1422. 10.1097/01.AOG.0000245447.56585.a0. [DOI] [PubMed] [Google Scholar]
- 6.Grady WR, Klepinger DH, Nelson-Wally A. Contraceptive characteristics: the perceptions and priorities of men and women. Fam Plann Perspect 1999;31(4):168–175. 10.2307/2991589. [DOI] [PubMed] [Google Scholar]
- 7.Forrest JD. U.S. women’s perceptions of and attitudes about the IUD. Obstet Gynecol Surv 1996;51(12):(suppl)S30–S34. 10.1097/00006254-199612000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Steiner MJ, Trussell J, Mehta N, Condon S, Subramaniam S, Bourne D. Communicating contraceptive effectiveness: a randomized controlled trial to inform a World Health Organization family planning handbook. Am J Obstet Gynecol 2006;195(1):85–91. 10.1016/j.ajog.2005.12.053. [DOI] [PubMed] [Google Scholar]
- 9.Jackson AV, Karasek D, Dehlendorf C, Foster DG. Racial and ethnic differences in women’s preferences for features of contraceptive methods. Contraception 2016;93(5):406–411. 10.1016/j.contraception.2015.12.010. [DOI] [PubMed] [Google Scholar]
- 10.Dempsey AR, Billingsley CC, Savage AH, Korte JE. Predictors of long-acting reversible contraception use among unmarried young adults. Am J Obstet Gynecol 2012;206(6):526.e1–526.e5. 10.1016/j.ajog.2012.02.014. [DOI] [PubMed] [Google Scholar]
- 11.Eisenberg DL, Secura GM, Madden TE, Allsworth JE, Zhao Q, Peipert JF. Knowledge of contraceptive effectiveness. Am J Obstet Gynecol 2012;206(6):479.e1–479.e9. 10.1016/j.ajog.2012.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gardner J, Miller L. Promoting the safety and use of hormonal contraceptives. J Womens Health (Larchmt) 2005;14(1):53–60. 10.1089/jwh.2005.14.53. [DOI] [PubMed] [Google Scholar]
- 13.Grimes DA, Schulz KF. Nonspecific side effects of oral contraceptives: nocebo or noise? Contraception 2011;83(1):5–9. 10.1016/j.contraception.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 14.Frost JJ, Duberstein Lindberg L, Finer LB. Young adults’ contraceptive knowledge, norms and attitudes: associations with risk of unintended pregnancy. Perspect Sex Reprod Health 2012;44(2):107–116. 10.1363/4410712. [DOI] [PubMed] [Google Scholar]
- 15.Rickert VI, Berenson AB, Williamson AJ, Wiemann CM. Immediate recall of oral contraceptive instructions: implications for providers. Am J Obstet Gynecol 1999;180(6, pt 1):1399–1406. 10.1016/S0002-9378(99)70025-6. [DOI] [PubMed] [Google Scholar]
- 16.Rocca CH, Harper CC. Do racial and ethnic differences in contraceptive attitudes and knowledge explain disparities in method use ? Perspect Sex Reprod Health 2012;44(3):150–158. 10.1363/4415012. [DOI] [PubMed] [Google Scholar]
- 17.Hall KS, Castaño PM, Stone PW, Westhoff C. Measuring oral contraceptive knowledge: a review of research findings and limitations. Patient Educ Couns 2010;81(3):388–394. 10.1016/j.pec.2010.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pazol K, Zapata LB, Tregear SJ, Mautone-Smith N, Gavin LE. Impact of contraceptive education on contraceptive knowledge and decision making: a systematic review. Am J Prev Med 2015;49(2):(suppl)S46–S56. 10.1016/j.amepre.2015.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention (CDC). Providing quality family planning services: recommendations of the CDC and the U.S. Office of Population Affairs. MMWR Recomm Rep 2014;63(4):1–54. [PubMed] [Google Scholar]
- 20.Zapata LB, Pazol K, Dehlendorf C, et al. Contraceptive counseling in clinical settings: an updated systematic review. Am J Prev Med 2018;55(5):677–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tregear SJ, Gavin LE, Williams JR. Systematic review evidence methodology: providing quality family planning services. Am J Prev Med 2015;49(2):(suppl) S23–S30. 10.1016/j.amepre.2015.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.UN Development Programme. Human development report 2016: human development for everyone http://hdr.undp.org/en/2016-report/. Published 2016. Accessed October 31, 2017.
- 24.Harris RP, Helfand M, Woolf SH, et al. Current methods of the U.S. Preventive Services Task Force: a review of the process. Am J Prev Med 2001;(suppl)20(3):21–35. 10.1016/S0749-3797(01)00261-6. [DOI] [PubMed] [Google Scholar]
- 25.Castano PM, Bynum JY, Andres R, Lara M, Westhoff C. Effect of daily text messages on oral contraceptive continuation: a randomized controlled trial. Obstet Gynecol 2012;119(1):14–20. 10.1097/AOG.0b013e31823d4167. [DOI] [PubMed] [Google Scholar]
- 26.Davidson AS, Whitaker AK, Martins SL, et al. Impact of a theory-based video on initiation of long-acting reversible contraception after abortion. Am J Obstet Gynecol 2015;212(3):310.e1–310.e7. 10.1016/j.ajog.2014.09.027. [DOI] [PubMed] [Google Scholar]
- 27.de Reilhac P, Plu-Bureau G, Serfaty D, Letombe B, Gondry J, Christin-Maitre S. The CORALIE study: improving patient education to help new users better understand their oral contraceptive. Eur J Contracept Reprod Health Care 2016;21(5):388–394. 10.1080/13625187.2016.1217323. [DOI] [PubMed] [Google Scholar]
- 28.Garbers S, Chiasson MA, Baum R, Tobier N, Ventura A, Hirshfield S. Get It and Forget It”: online evaluation of a theory-based IUD educational video in English and Spanish. Contraception 2015;91(1):76–79. 10.1016/j.contraception.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 29.Garbers S, Meserve A, Kottke M, Hatcher R, Chiasson MA. Tailored health messaging improves contraceptive continuation and adherence: results from a randomized controlled trial. Contraception 2012;86(5):536–542. 10.1016/j.contraception.2012.02.005. [DOI] [PubMed] [Google Scholar]
- 30.Garbers S, Meserve A, Kottke M, Hatcher R, Ventura A, Chiasson MA. Randomized controlled trial of a computer-based module to improve contraceptive method choice. Contraception 2012;86(4):383–390. 10.1016/j.contraception.2012.01.013. [DOI] [PubMed] [Google Scholar]
- 31.Gilliam ML, Martins SL, Bartlett E, Mistretta SQ, Holl JL. Development and testing of an iOS waiting room “app” for contraceptive counseling in a Title X family planning clinic. Am J Obstet Gynecol 2014;211(5):481.e1–481.e8. 10.1016/j.ajog.2014.05.034. [DOI] [PubMed] [Google Scholar]
- 32.Hall KS, Westhoff CL, Castano PM. The impact of an educational text message intervention on young urban women’s knowledge of oral contraception. Contraception 2013;87(4):449–454. 10.1016/j.contraception.2012.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kofinas JD, Varrey A, Sapra KJ, Kanj RV, Chervenak FA, Asfaw T. Adjunctive social media for more effective contraceptive counseling: a randomized controlled trial. Obstet Gynecol 2014;123(4):763–770. 10.1097/AOG.0000000000000172. [DOI] [PubMed] [Google Scholar]
- 34.Lee J, Papic M, Baldauf E, Updike G, Schwarz EB. A checklist approach to caring for women seeking pregnancy testing: effects on contraceptive knowledge and use. Contraception 2015;91(2):143–149. 10.1016/j.contraception.2014.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Michie L, Cameron ST, Glasier A, Johnstone A. Giving information about the contraceptive implant using a DVD: is it acceptable and informative? A pilot randomised study. J Fam Plann Reprod Health Care 2016;42(3):194–200. 10.1136/jfprhc-2015-101186. [DOI] [PubMed] [Google Scholar]
- 36.Ragland D, Payakachat N, Ounpraseuth S, Pate A, Harrod SE, Ott RE. Emergency contraception counseling: an opportunity for pharmacists. J Am Pharm Assoc (2003) 2011;51(6):756–761. 10.1331/JAPhA.2011.10157. [DOI] [PubMed] [Google Scholar]
- 37.Ragland D, Payakachat N, Stafford RA. Emergency contraception counseling in a retail pharmacy setting: a pilot study. J Pharm Pract 2015;28(3):261–265. 10.1177/0897190013516507. [DOI] [PubMed] [Google Scholar]
- 38.Schwarz EB, Burch EJ, Parisi SM, et al. Computer-assisted provision of hormonal contraception in acute care settings. Contraception 2013;87 (2):242–250. 10.1016/j.contraception.2012.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schwarz EB, Papic M, Parisi SM, Baldauf E, Rapkin R, Updike G. Routine counseling about intrauterine contraception for women seeking emergency contraception. Contraception 2014;90(1):66–71. 10.1016/j.contraception.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 40.Sridhar A, Chen A, Forbes ER, Glik D. Mobile application for information on reversible contraception: a randomized controlled trial. Am J Obstet Gynecol 2015;212(6):774.e1–774.e7. 10.1016/j.ajog.2015.01.011. [DOI] [PubMed] [Google Scholar]
- 41.Vogt C, Schaefer M. Knowledge matters—impact of two types of information brochure on contraceptive knowledge, attitudes and intentions. Eur J Contracept Reprod Health Care 2012;17(2):135–143. 10.3109/13625187.2011.643837. [DOI] [PubMed] [Google Scholar]
- 42.Hall KS, Castano PM, Westhoff CL. The influence of oral contraceptive knowledge on oral contraceptive continuation among young women. J Womens Health (Larchmt) 2014;23(7):596–601. 10.1089/jwh.2013.4574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Little P, Griffin S, Dickson N, Sadler C, Kelly J. Unwanted pregnancy and contraceptive knowledge: identifying vulnerable groups from a randomized controlled trial of educational interventions. Fam Pract 2001;18(4):449–453. 10.1093/fampra/18.4.449. [DOI] [PubMed] [Google Scholar]
- 44.Little P, Griffin S, Kelly J, Dickson N, Sadler C. Effect of educational leaflets and questions on knowledge of contraception in women taking the combined contraceptive pill: randomised controlled trial. BMJ 1998;316(7149):1948–1952. 10.1136/bmj.316.7149.1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chewning B, Mosena P, Wilson D, et al. Evaluation of a computerized contraceptive decision aid for adolescent patients. Patient Educ Couns 1999;38(3):227–239. 10.1016/S0738-3991(99)00014-2. [DOI] [PubMed] [Google Scholar]
- 46.Deijen JB, Kornaat H. The influence of type of information, somatization, and locus of control on attitude, knowledge, and compliance with respect to the triphasic oral contraceptive Tri-Minulet. Contraception 1997;56(1):31–41. 10.1016/S0010-7824(97)00071-1. [DOI] [PubMed] [Google Scholar]
- 47.DeLamater J, Wagstaff DA, Havens KK. The impact of a culturally appropriate STD/AIDS education intervention on black male adolescents’ sexual and condom use behavior. Health Educ Behav 2000;27 (4):454–470. 10.1177/109019810002700408. [DOI] [PubMed] [Google Scholar]
- 48.Johnson LK, Edelman A, Jensen J. Patient satisfaction and the impact of written material about postpartum contraceptive decisions. Am J Obstet Gynecol 2003;188(5):1202–1204. 10.1067/mob.2003.308. [DOI] [PubMed] [Google Scholar]
- 49.Kirby D, Harvey PD, Claussenius D, Novar M. A direct mailing to teenage males about condom use: its impact on knowledge, attitudes and sexual behavior. Fam Plann Perspect 1989;21(1):12–18. 10.2307/2135413. [DOI] [PubMed] [Google Scholar]
- 50.Lindenberg CS, Solorzano RM, Bear D, Strickland O, Galvis C, Pittman K. Reducing substance use and risky sexual behavior among young, low-income, Mexican-American women: comparison of two interventions. Appl Nurs Res 2002;15(3):137–148. 10.1053/apnr.2002.34141. [DOI] [PubMed] [Google Scholar]
- 51.Mason V, McEwan A, Walker D, Barrett S, James D. The use of video information in obtaining consent for female sterilisation: a randomised study. BJOG 2003;110(12):1062–1071. 10.1111/j.1471-0528.2003.03041.x. [DOI] [PubMed] [Google Scholar]
- 52.O’Donnell L, San Doval A, Duran R, O’Donnell CR. The effectiveness of video-based interventions in promoting condom acquisition among STD clinic patients. Sex Transm Dis 1995;22(2):97–103. 10.1097/00007435-199503000-00004. [DOI] [PubMed] [Google Scholar]
- 53.O’Donnell LN, Doval AS, Duran R, O’Donnell C. Video-based sexually transmitted disease patient education: its impact on condom acquisition. Am J Public Health 1995;85(6):817–822. 10.2105/AJPH.85.6.817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Paperny DM, Starn JR. Adolescent pregnancy prevention by health education computer games: computer-assisted instruction of knowledge and attitudes. Pediatrics 1989;83(5):742–752. [PubMed] [Google Scholar]
- 55.Pedrazzini AE, McGowan H, Lucking L, Johanson RJ. The trouble with sex—it always gets in the way”: an evaluation of a peer-produced teenage pregnancy video. Br J Fam Plann 2000;26(3):131–135. 10.1783/147118900101194544. [DOI] [PubMed] [Google Scholar]
- 56.Reis J, Tymchyshyn P. A longitudinal evaluation of computer-assisted instruction on contraception for college students. Adolescence 1992;27 (108):803–811. [PubMed] [Google Scholar]
- 57.Roberto AJ, Zimmerman RS, Carlyle KE, Abner EL, Cupp PK, Hansen GL. The effects of a computer-based pregnancy, STD, and HIV prevention intervention: a nine-school trial. Health Commun 2007;21 (2):115–124. 10.1080/10410230701306990. [DOI] [PubMed] [Google Scholar]
- 58.Schwarz EB, Gerbert B, Gonzales R. Computer-assisted provision of emergency contraception a randomized controlled trial . J Gen Intern Med 2008;23(6):794–799. 10.1007/s11606-008-0609-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Smith LF, Whitfield MJ. Women’s knowledge of taking oral contraceptive pills correctly and of emergency contraception: effect of providing information leaflets in general practice. Br J Gen Pract 1995;45(397):409–414. [PMC free article] [PubMed] [Google Scholar]
- 60.Steiner MJ, Dalebout S, Condon S, Dominik R, Trussell J. Understanding risk: a randomized controlled trial of communicating contraceptive effectiveness. Obstet Gynecol 2003;102(4):709–717. 10.1097/00006250-200310000-00012. [DOI] [PubMed] [Google Scholar]
- 61.Whitaker AK, Terplan M, Gold MA, Johnson LM, Creinin MD, Harwood B. Effect of a brief educational intervention on the attitudes of young women toward the intrauterine device. J Pediatr Adolesc Gynecol 2010;23(2):116–120. 10.1016/j.jpag.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 62.Trevena LJ, Davey HM, Barratt A, Butow P, Caldwell P. A systematic review on communicating with patients about evidence. J Eval Clin Pract 2006;12(1):13–23. 10.1111/j.1365-2753.2005.00596.x. [DOI] [PubMed] [Google Scholar]
- 63.Stacey D, Bennett CL, Barry MJ, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 2011;10 CD001431 10.1002/14651858.CD001431.pub3. [DOI] [PubMed] [Google Scholar]
- 64.Centers for Medicare and Medicaid Services. Toolkit for making written material clear and effective. www.cms.gov/WrittenMaterialsTool-kit/01_Overview.asp#TopOfPage. Published 2011.
- 65.HHS, Office of Disease Prevention and Health Promotion. Health literacy online: a guide for simplifying the user experience. https://health.gov/healthliteracyonline/. Published 2016.
- 66.DeWalt D, Callahan L, Hawk V, et al. Health Literacy Universal Precautions Toolkit AHRQ Publication No. 10-0046-EF. http://nchealth-literacy.org/toolkit/. Published 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Berry DC. Informing people about the risks and benefits of medicines: implications for the safe and effective use of medicinal products. Curr Drug Saf 2006;1(1):121–126. 10.2174/157488606775252638. [DOI] [PubMed] [Google Scholar]
- 68.Berry DC, Raynor DK, Knapp P, Bersellini E. Patients’ understanding of risk associated with medication use: impact of European Commission guidelines and other risk scales. Drug Saf 2003;26(1):1–11. 10.2165/00002018-200326010-00001. [DOI] [PubMed] [Google Scholar]
- 69.Edwards A, Elwyn G, Mulley A. Explaining risks: turning numerical data into meaningful pictures. BMJ 2002;324(7341):827–830. 10.1136/bmj.324.7341.827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Galesic M, Gigerenzer G, Straubinger N. Natural frequencies help older adults and people with low numeracy to evaluate medical screening tests. Med Decis Making 2009;29(3):368–371. 10.1177/0272989X08329463. [DOI] [PubMed] [Google Scholar]
- 71.Garcia-Retamero R, Galesic M. Communicating treatment risk reduction to people with low numeracy skills: a cross-cultural comparison. Am J Public Health 2009;99(12):2196–2202. 10.2105/AJPH.2009.160234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Garcia-Retamero R, Galesic M, Gigerenzer G. Do icon arrays help reduce denominator neglect? Med Decis Making 2010;30(6):672–684. 10.1177/0272989X10369000. [DOI] [PubMed] [Google Scholar]
- 73.Gigerenzer G, Edwards A. Simple tools for understanding risks: from innumeracy to insight. BMJ 2003;327(7417):741–744. 10.1136/bmj.327.7417.741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Knapp P, Gardner PH, Raynor DK, Woolf E, McMillan B. Perceived risk of tamoxifen side effects: a study of the use of absolute frequencies or frequency bands, with or without verbal descriptors. Patient Educ Couns 2010;79(2):267–271. 10.1016/j.pec.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 75.Kurz-Milcke E, Gigerenzer G, Martignon L. Transparency in risk communication: graphical and analog tools. Ann N Y Acad Sci 2008;1128:18–28. 10.1196/annals.1399.004. [DOI] [PubMed] [Google Scholar]
- 76.Lipkus IM. Numeric, verbal, and visual formats of conveying health risks: suggested best practices and future recommendations. Med Decis Making 2007;27(5):696–713. 10.1177/0272989X07307271. [DOI] [PubMed] [Google Scholar]
- 77.Paling J Strategies to help patients understand risks. BMJ 2003;327 (7417):745–748. 10.1136/bmj.327.7417.745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Skolbekken JA. Communicating the risk reduction achieved by cholesterol reducing drugs. BMJ 1998;316(7149):1956–1958. 10.1136/bmj.316.7149.1956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Visschers VH, Meertens RM, Passchier WW, de Vries NN. Probability information in risk communication: a review of the research literature. Risk Anal 2009;29(2):267–287. 10.1111/j.1539-6924.2008.01137.x. [DOI] [PubMed] [Google Scholar]
- 80.McGee J Toolkit for making written material cear and effective, CMS Product No. 11476 Centers for Medicare aned Medicaid Services. 2010. [Google Scholar]
- 81.Peters E, Dieckmann N, Dixon A, Hibbard JH, Mertz CK. Less is more in presenting quality information to consumers. Med Care Res Rev 2007;64(2):169–190. 10.1177/10775587070640020301. [DOI] [PubMed] [Google Scholar]
- 82.Berry DC, Michas IC, Rosis Fd Evaluating explanations about drug prescriptions: effects of varying the nature of information about side effects and its relative position in explanations. Psychol Health 1998;13(5):767–784. 10.1080/08870449808407431. [DOI] [Google Scholar]
- 83.Zapata LB, Tregear SJ, Curtis KM, et al. Impact of contraceptive counseling in clinical settings: a systematic review. Am J Prev Med 2015;49(2): (suppl) S31–S45. 10.1016/j.amepre.2015.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Belcher L, Kalichman S, Topping M, et al. A randomized trial of a brief HIV risk reduction counseling intervention for women. J Consult Clin Psychol 1998;66(5):856–861. 10.1037/0022-006X.66.5.856. [DOI] [PubMed] [Google Scholar]
- 85.Eldridge GD, St Lawrence JS, Little CE, et al. Evaluation of the HIV risk reduction intervention for women entering inpatient substance abuse treatment. AIDS Educ Prev 1997;9(1):62–76 (suppl). [PubMed] [Google Scholar]
- 86.Jaccard J Unlocking the Contraceptive Conundrum Washington, DC: The National Campaign to Prevent Teen and Unplanned Pregnancy, 2009. [Google Scholar]
- 87.Berkman ND, Sheridan SL, Donahue KE, et al. Health Literacy Interventions and Outcomes: An Updated Systematic Review Rockville, MD: Agency for Healthcare Research and Quality, 2011 Evidence Report/Technology Assesment No. 199. AHRQ Publication Number; 11–E006. [Google Scholar]
- 88.Schillinger D, Piette J, Grumbach K, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med 2003;163(1):83–90. 10.1001/archinte.163.1.83. [DOI] [PubMed] [Google Scholar]
- 89.McMahon SR, Rimsza ME, Bay RC. Parents can dose liquid medication accurately. Pediatrics 1997;100(3, pt 1):330–333. 10.1542/peds.100.3.330. [DOI] [PubMed] [Google Scholar]
- 90.Garbers S, Haines-Stephan J, Lipton Y, Meserve A, Spieler L, Chiasson MA. Continuation of copper-containing intrauterine devices at 6 months. Contraception 2013;87(1):101–106. 10.1016/j.contraception.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 91.Dehlendorf C, Fitzpatrick J, Steinauer J, et al. Development and field testing of a decision support tool to facilitate shared decision making in contraceptive counseling. Patient Educ Couns 2017;100(7):1374–1381. 10.1016/j.pec.2017.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Koo HP, Wilson EK, Minnis AM. A computerized family planning counseling aid: a pilot study evaluation of smart choices. Perspect Sex Reprod Health 2017;49(1):45–53. 10.1363/psrh.12016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


