Abstract
Background:
People using electricity-dependent durable medical equipment (DME) may be vulnerable to health effects from wildfire smoke, residence near wildfires, or residence in evacuation zones. To our knowledge, no studies have examined their healthcare utilization during wildfires.
Methods:
We obtained 2016–2020 counts of residential Zip Code Tabulation Area (ZCTA) level outpatient, emergency department (ED), and inpatient visits made by DME-using Kaiser Permanente Southern California members 45+. We linked counts to daily ZCTA-level wildfire PM2.5 and wildfire boundary and evacuation data from the 2018 Woolsey and 2019 Getty wildfires. We estimated the association of lagged (up to 7 days) wildfire PM2.5 and residence near a fire or in an evacuation zone and healthcare visit frequency with negative binomial and difference-in-differences models.
Results:
Among 236,732 DME users, 10 increases in wildfire PM2.5 concentration were associated with reduced rate (RR = 0.96, 95% CI: 0.94, 0.99) of all-cause outpatient visits one day after exposure and increased rate on 4 of 5 subsequent days (RR range 1.03–1.12). Woolsey Fire proximity (<20km) was associated with reduced all-cause outpatient visits, while evacuation and proximity were associated with increased inpatient cardiorespiratory visits (proximity RR = 1.45, 95% CI: 0.99, 2.12, evacuation RR = 1.72, 95% CI: 1.00, 2.96). Neither Getty Fire proximity nor evacuation was associated with healthcare visit frequency.
Conclusions:
Our results support the hypothesis that wildfire smoke or proximity interrupts DME users’ routine outpatient care, via sheltering in place. However, wildfire exposures were also associated with increased urgent healthcare utilization in this vulnerable group.
Keywords: Durable Medical Equipment, wildfire, wildfire smoke, wildfire evacuation, healthcare utilization, disaster evacuation, climate change
Introduction
Wildfires are widespread, have increased in severity because of climate change, and will worsen in coming decades1–5. Development in the wildland-urban interface has placed more communities in the path of these increasingly frequent disasters6. Immediate impacts of wildfire, such as evacuations, power outages, and destruction of infrastructure cause trauma, stress, financial strain, and physical injury in affected communities7,8. Simultaneously, 70% of the US population is exposed to wildfire smoke annually9–11
Among other hazardous components, wildfire smoke contains fine particulate matter (PM2.5). Of PM2.5 sources, wildfire PM2.5 may be particularly harmful because it consists of more organic and elemental carbon12–14. It also constitutes most extreme PM2.5 exposure in California, accounting for 71% of total PM2.5 on days that exceed US Environmental Protection Agency (USEPA) annual standard of 12 9.
Most studies examining wildfire PM2.5 exposure have focused on respiratory and cardiovascular disease outcomes. Exposure has been associated with asthma and chronic obstructive pulmonary disease symptom exacerbation15–17, increases in emergency department (ED) and inpatient visits related to cardiorespiratory disease18–21, and increased mortality risk22–24.
Proximity to wildfire or residence in an evacuation zone may not only cause visible smoke exposure or extreme wildfire-related air pollution, it may also involve possible evacuation, community disruption, loss of access to community services and housing, power outages, and stress co-occurring with and resulting from these events.
People who use durable medical equipment (DME) may be particularly vulnerable to both wildfire PM2.5 exposure and stress from wildfire proximity or evacuation. DME use is common among older adults and is associated with respiratory illness and other disabilities29. Prevalence of DME rentals at Kaiser Permanente Southern California (KPSC) increased from 2008–2018, with the highest prevalence among older adults30. DME types included bilevel positive airway pressure (BiPAP) machines, enteral feeding machines, infusion pumps, oxygen equipment, suction pumps, ventilators, and wheelchairs30.
This group may face unique challenges during wildfire events. The association between wildfire smoke exposure and respiratory and cardiovascular disease outcomes has may be stronger among older adults compared to younger populations16,31. Further, people using DME may have co-occurring medical conditions such as cardiovascular disease that make them more vulnerable to wildfire PM2.5 and wildfire-related stressors like threatened or actual evacuation. Limited mobility or need for electricity access may result in increased difficulty evacuating disaster zones30,35.
Our study has two unique components. First, we focus on a potentially vulnerable population by using 2016–2020 KPSC electronic health records from seven Southern California counties to examine the relationship between wildfire exposure and healthcare utilization in people who use DME. Second, we evaluate exposure to wildfire via (1) wildfire PM2.5 concentrations, and (2a) residential proximity to major active fires, and (2b) residence in an evacuated area. These proximity-based residential exposure estimates attempt to holistically assess the impact of wildfire exposure, including stress, rather than focusing only on air pollution. Our study period includes two major wildfire events in populated areas: the 400km2 Woolsey Fire, which burned from November 8–21 2018 in Los Angeles and Ventura counties, displacing 295,000 people and killing three36,37, and the 3km2 Getty Fire, which necessitated evacuations in densely populated Los Angeles, and burned from October 28-November 5, 201937,38.
Methods
Study population
We used electronic health record data from KPSC to identify all individuals who were 45 or older as of October 28 2019 and had rented DME in the year prior. KPSC patients represent the underlying population in the region, except for slight under-representation of individuals living in the highest and lowest socioeconomic status (SES) communities39. We excluded younger DME renters in order to focus on socially and medically vulnerable older adults, but also to exclude breast pump users, a healthy subgroup of the otherwise vulnerable DME using population, whom we did not hypothesize to be disproportionately vulnerable to wildfire exposure. Electronic health record data included each patient’s Zip Code Tabulation Area (ZCTA) of residence. We obtained daily counts of healthcare visits–not necessarily related to DME use–by this population by residential ZCTA in seven counties in Southern California from January 1 2016 to March 15 2020. 236,732 DME patients lived in the study area, which covered most of San Bernardino, Orange, Los Angeles, Riverside, San Diego, Ventura, and Kern counties (Figure 1). The area consisted of 582 ZCTAs, each containing 1–1773 patients. During 2018 and 2019, these seven counties experienced 23 wildfires that each burned over 3 km2 in California37,40, contributing to wildfire smoke in the area.
Figure 1:
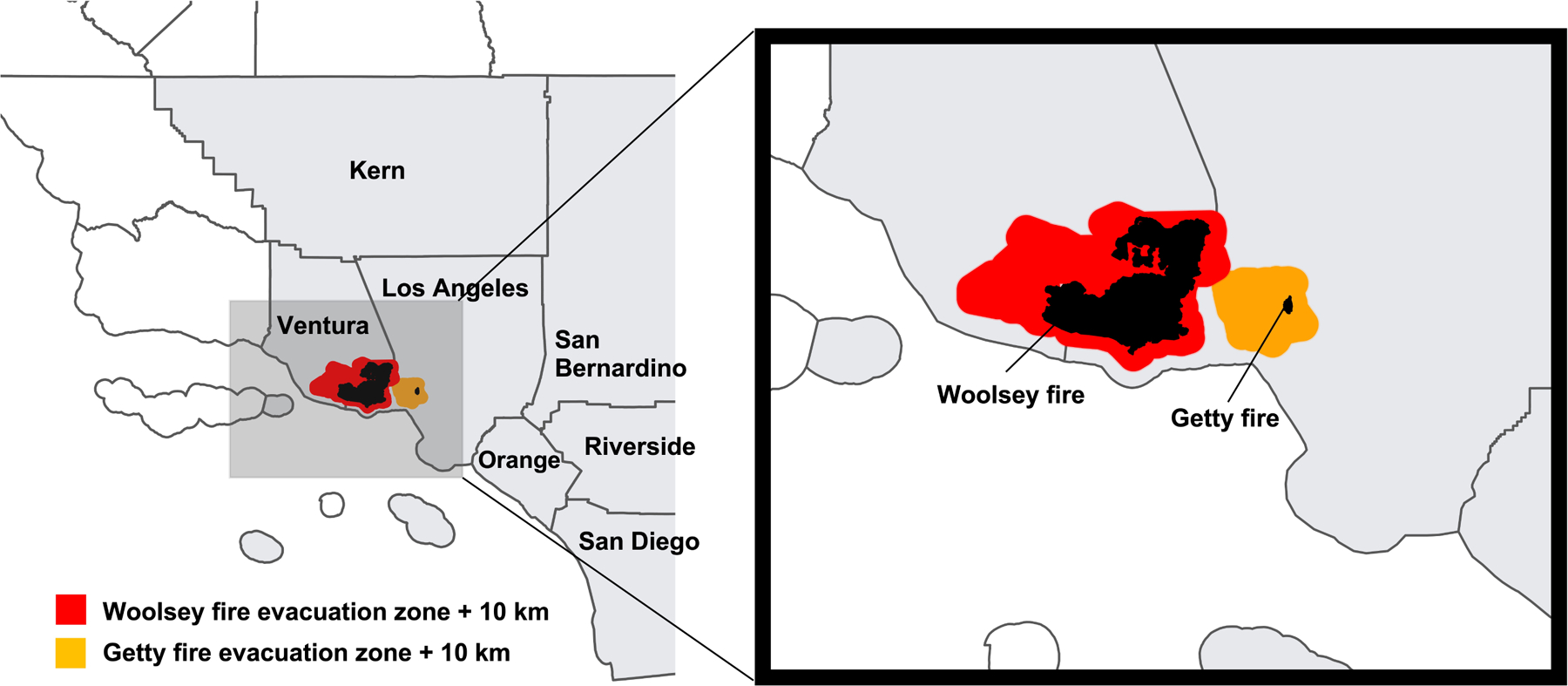
Map of Southern California study area, shaded in grey, with counties labelled in black. Woolsey and Getty fire burn areas are shaded in black.
The KPSC Institutional Review Board (IRB) approved this study, and the Columbia IRB did not consider it human subjects research, since the data were fully de-identified before researchers at Columbia received them.
Exposure Definition
Wildfire PM2.5
We measured wildfire smoke exposure by estimating daily wildfire and non-wildfire PM2.5 concentrations at the ZCTA level using a multistage approach described elsewhere and in the supplemental digital content, in eMethods 140.
We calculated daily wildfire and non-wildfire PM2.5 by averaging concentrations across the higher-level spatial groupings of several ZCTAs based on spatial proximity (hereafter ‘ZCTA groupings’; grouping method described in eMethods 2, in the eAppendix).
Proximity to wildfire
To measure direct exposure to wildfire, we obtained data on the fire boundaries and evacuation zones of two disastrous Southern California wildfires – the Woolsey Fire and the Getty Fire. We chose these fires because they affected a substantial number of people in our study area, during the study period. The Woolsey Fire, which burned from November 8 2018 until November 21 2018, required the evacuation of 295,000 people from Los Angeles and Ventura counties. It burned 1643 structures and almost 400 km2 of land, making it particularly destructive36,37. The Getty Fire, which ignited on October 28 2019 and burned until November 5th, 2019, was notable because it necessitated evacuations during its 9-day duration in densely populated Los Angeles37,38.
Notably, The Thomas Fire also burned over 1100 km2 during our study period42. However, most of the fire burned in the rural northern corner of Ventura County and outside the study area. Therefore, we did not include the Thomas Fire in the proximity analyses, since very few participants would have been exposed to it. Still, smoke from this fire contributed substantially to wildfire PM2.5 in Ventura County in December 2017, and therefore was included in our PM2.5 analyses (Figure 2).
Figure 2:

Daily mean non-wildfire PM2.5 concentrations by study area county from January 2016 – March 2020. Measurements are in. Dotted lines represent the US Environmental Protection Agency 35 standard. Colored time periods represent measurements made while a wildfire was burning.
We obtained shapefiles of the total areas burned during the Getty and Woolsey fires from the CALFIRE Fire and Resource Assessment Program43. These perimeters represented the approximately the maximum burned areas of each fire42 and we used them to define exposure. We considered ZCTAs exposed if their boundary was within 20km of a final fire perimeter on days that a fire was active. US-based studies have evaluated exposure to wildfire disasters in different ways, including self-reported impact44, wildfire damage to own home45, evacuation from own home46,47, residence in a community where structures burned48, residence in a county where a wildfire burned49, and residential proximity to a wildfire50. We selected the Getty and Woolsey wildfires a priori, then linked exposure via proximity to the wildfire boundaries, selecting a distance of 20km as one that could elicit a stress response; prior studies have found impacts on wellbeing and mental health at similar distances51.
Next, we created an evacuation exposure metric. GIS data on evacuation zones were not available for either fire. Therefore, we reviewed webpages (described in eMethods 3, in the eAppendix) containing maps of the evacuation zones and digitized boundaries around all areas ever evacuated during either fire in QGIS52 (Figure 1). Using these data, we considered ZCTAs exposed to evacuation stress if they were within 10 km of any evacuation zone boundary (Figure 1) on days where a fire was active. Like close residence to a wildfire burn area, evacuation and anticipating potential fire or evacuation can cause stress, which we aimed to capture with this exposure definition7,8,53. We chose a 10km buffer rather than the previous 20km buffer because evacuation zones themselves can be large.
By measuring proximity to wildfire or residence in an evacuation zone, we aimed to capture a mixture of exposures, including possible visible smoke exposure or extreme wildfire-related air pollution, possible evacuation, community disruption, loss of access to community services and housing, power outages, and stress co-occurring with and resulting from these events. Though not all people living near a wildfire experience every component of this mixture, we think the most important component is stress from the disaster. We have created a DAG (eFigure 1) describing this mixture.
Outcome Definition
We obtained daily counts of all-cause outpatient visits, all-cause emergency department (ED) visits, and all-cause inpatient admissions, as well as ED visits and inpatient admissions specifically for circulatory or respiratory disease outcomes made by KPSC members 45 and older who rented DME. Outpatient visits included both in-person and virtual synchronous visits (i.e., video or telephone visit with a provider), ED visits were those that terminated in the ED, and inpatient admissions consisted of all inpatient admissions (scheduled and unscheduled) as well as ED visits ending in an admission. Generally, outpatient visits are considered the lowest acuity, followed by ED visits, and inpatient visits are highest acuity. Recorded visits represent the universe of visits and were not necessarily related to DME use. We identified cause-specific visit counts using International Classification of Diseases 10 codes I00-I99 (circulatory) and J00-J99 (respiratory). We included visits from January 1 2016 to March 15 2020.
Daily visit counts by ZCTA were low and often zero [median outpatient visits = 1, interquartile range width (IQRw) = 3, median ED and inpatient visits = 0, IQRw = 0). For the wildfire PM2.5 analyses, to avoid zero-inflation in our models, and to increase statistical power, we could have aggregated ZCTA counts to the weekly level. However, prior studies of wildfire smoke exposure have found associations between same-day air pollution and healthcare visits over the course of the following week18–21. To evaluate a lagged temporal effect in our data, we required daily healthcare visit counts, therefore, we opted to aggregate our data into higher-level spatial groupings of several ZCTAs based on spatial proximity (hereafter ‘ZCTA groupings’; grouping method described in eMethods 2, the eAppendix).
For analyses measuring residence near a fire on in an evacuation zone, we used ZCTA level daily visit counts aggregated to the weekly level. We aggregated to the weekly level because we used last recorded fire boundaries and last recorded evacuation zones rather than daily PM2.5 concentrations as we had available for our air pollution. By aggregating, we also removed weekend–weekday patterns in outpatient visits, increased power, and reduced zero inflation. We considered a week exposed if the Woolsey or Getty fire burned any day that week.
Analysis
Wildfire PM2.5
To evaluate the relationship between daily wildfire PM2.5 and daily ZCTA grouping-level healthcare visit counts, we used negative binomial regression. Many studies on lagged effects of air pollution use constrained distributed lag models to estimate stable coefficients in the presence of highly autocorrelated (and therefore highly co-linear) lagged exposures54. We examined the autocorrelation of wildfire PM2.5 concentrations and found only weak autocorrelation (lags 1–7 days each had <0.25 correlation with lag 0). Unlike other sources of air pollution, wildfire PM2.5 concentrations increased dramatically on certain days, then decreased just as quickly (Figure 3). We therefore created unconstrained models, including separate terms for wildfire PM2.5 lags 0–7 days. We also performed an additional analysis examining weekly wildfire PM2.5 levels lagged up to two weeks. We created separate models for each healthcare visit type: all-cause outpatient, ED, and inpatient visits, and ED and inpatient visits for circulatory or respiratory disease endpoints.
Figure 3:
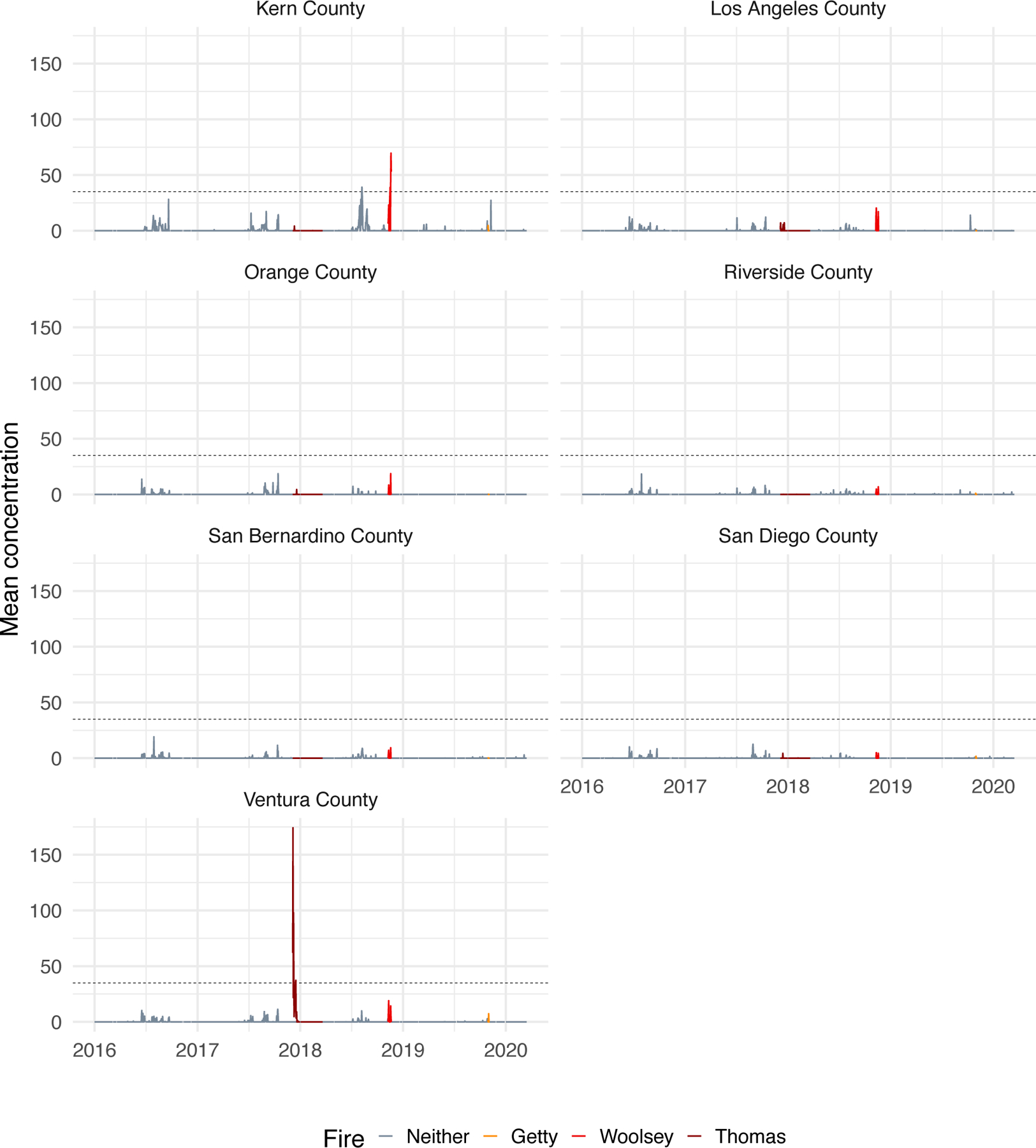
Daily mean wildfire PM2.5 concentrations by study area county from January 2016 – March 2020. Measurements are in . Dotted lines represent the US Environmental Protection Agency 35 standard. Colored time periods represent measurements made while a wildfire was burning.
We included offsets accounting for the number of KPSC members over 45 using DME in each ZCTA grouping. We controlled for temperature using a penalized spline term, as temperature can predict respiratory and cardiovascular healthcare utilization55 and wildfire56, using daily mean temperature data from the PRISM Climate Group57. We did not include any lags on temperature. We also controlled for long-term seasonal trends not caused by exposure with a natural spline term, and used the number of years in the study period (four) to determine the natural spline flexibility (12 degrees of freedom). We controlled for non-wildfire PM2.5, since non-wildfire PM2.5 concentrations were high during the study period: mean daily non-wildfire PM2.5 by grouping was 11.0 (SD = 6.69), just under the annual USEPA National Ambient Air Quality Standard of 12 (Figure 2). We also added a fixed effect for weekends to the outpatient visits model, accounting for fewer visits on weekend days.
We controlled for a comprehensive set of socioeconomic variables to account for correlation between ZCTA groupings. We obtained values by ZCTA from the 5-year 2015–2019 ACS58 including median household income, home ownership (% homes occupied by owner), poverty (percent households below threshold income), age structure (percent of population 20–64, and 65+ years), and racial and ethnic composition (percent Hispanic, percent non-Hispanic white, percent non-Hispanic Black). We took a simple mean within ZCTA groupings to obtain average covariate values by ZCTA grouping or summed within ZCTA groupings when appropriate (for example, we summed total population across groupings).
Proximity to wildfire and evacuation
To evaluate the association between proximity to and evacuation exposure related to wildfire and weekly ZCTA-level healthcare visit counts, we used a difference-in-differences (DID) analysis with negative binomial regression. We evaluated relationships separately for each fire, for evacuation and proximity, and for each type of healthcare visit. The DID estimators subtracted the change in weekly visit frequency when the Getty or Woolsey Fire was burning versus not burning among control ZCTAs (difference 1) from the change in visit frequency when the Getty or Woolsey Fire was burning versus not burning among ZCTAs exposed to the fire or evacuation zone (difference 2). If all models were specified correctly and parallel trends conditions were met, the DID estimator corresponded to the difference in visit frequency attributable to direct wildfire exposure. We assessed the parallel trends assumption visually in eFigure 2 in the supplemental digital content.
To avoid bias in our analyses due to exposure to fires, we excluded certain observations from specific ZCTAs from the control pool. If a ZCTA was exposed (i.e., boundary within 20km) to the Getty and Woolsey Fires or exposed to any other large fire that was declared a disaster by FEMA, burned a structure, or killed someone during the study period, we excluded observations from that ZCTA after the date the Getty, Woolsey, or other fire ignited. We used a CALFIRE fire perimeter data40 to identify all fires that met these criteria.
As in the wildfire PM2.5 models, we included offsets accounting for the population exposed and controlled for temperature with a penalized spline and non-wildfire PM2.5 with a linear term. We controlled for long-term seasonal trends not caused by exposure with a penalized spline term, as our data in these analyses were at the weekly level. We did not control for wildfire PM2.5 in a model describing residence proximate to a fire or in an evacuation zone, as we considered this part of our multifaceted exposure rather than a confounder.
We tested all models for sensitivity to parameterization of splines, by re-running all analyses with natural splines in place of penalized splines. We also tested all models for sensitivity to the size of the buffer around the wildfire perimeters and evacuation zones, by re-running analyses with a 30km buffer instead of a 20km buffer, expanding the exposed zone to include people further away from the fire or evacuation boundary. We conducted all analyses in R59, using the mgcv package60. All analysis code and model equations are available on GitHub at https://github.com/heathermcb/wildfires_DME.
Results
Health data description
The study population consisted of 236,732 KPSC DME users who between January 1, 2016 to March 15th, 2020 had a daily average of 2.5 (SD = 4.7) outpatient visits, 0.1 (SD = 0.5) ED visits, and 0.1 (SD = 0.4) inpatient visits per ZCTA grouping. There were on average 8 (SD = 8.9) outpatient visits per week per ZCTA, 0.5 (SD = 1.5) ED visits, and 0.2 (SD = 0.8) inpatient visits. The most common diagnoses were for circulatory or respiratory disease: of the 62,892 ED visits made over the study period, 49,364 (78%) were for circulatory or respiratory disease concerns, as were 30,325 (90%) of inpatient visits.
PM2.5 exposure
Mean daily wildfire PM2.5 concentration by ZCTA grouping throughout the study period was 0.22 (SD = 2.67) (Figure 2), since most groupings on most days (85% of days) had 0 wildfire PM2.5, while the maximum wildfire PM2.5 concentration was 551.53 . On the 366 days (23%) when study area wildfire PM2.5 was non-zero, the mean concentration in groupings with non-zero measurements was 5.6 (SD = 12.1). On days where wildfire PM2.5 exceeded USEPA air quality standards, in ZCTA groupings over the standard, wildfire PM2.5 made up 91% of total PM2.5.
In adjusted negative binomial models, a daily 10 increase in wildfire PM2.5 was associated with a decrease in rate of outpatient visits 1 day later (RR = 0.96, 95% CI: 0.94, 0.99), but increases on four of the five subsequent days (RR range 1.03–1.12, Table 1). Wildfire PM2.5 levels were not associated with the count of all-cause ED or inpatient visits or ED or inpatient visits for cardiorespiratory concerns.
Table 1:
Rate ratio and 95% confidence intervals from a negative binomial modela assessing the association between daily wildfire PM2.5 and healthcare utilization among KPSC DME users, daily lags.
| Rate ratios and [95% CI] for 10 increase in wildfire PM2.5 | |||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Outcome | lag 0 days | lag 1 day | lag 2 days | lag 3 days | lag 4 days | lag 5 days | lag 6 days |
| All-cause outpatient | 0.98 [0.96, 1.01] | 0.96 [0.94, 0.99] | 1.03 [1, 1.06] | 1.08 [1.05, 1.11] | 0.98 [0.95, 1.02] | 1.07 [1.04, 1.1] | 1.12 [1.09, 1.16] |
| All-cause ED | 0.97 [0.91, 1.04] | 1.02 [0.96, 1.08] | 0.98 [0.89, 1.07] | 0.96 [0.88, 1.06] | 0.95 [0.86, 1.04] | 1.03 [0.93, 1.13] | 0.92 [0.82, 1.02] |
| All-cause inpatient | 0.94 [0.84, 1.04] | 1.01 [0.93, 1.1] | 0.95 [0.84, 1.08] | 0.87 [0.76, 1] | 0.98 [0.87, 1.12] | 0.93 [0.81, 1.06] | 1.02 [0.89, 1.16] |
| ED: cardiorespiratory concerns | 0.99 [0.92, 1.07] | 0.99 [0.91, 1.08] | 0.96 [0.87, 1.07] | 0.99 [0.89, 1.1] | 0.92 [0.83, 1.03] | 1.01 [0.91, 1.13] | 0.89 [0.79, 1.01] |
| Inpatient: cardiorespiratory concerns | 0.91 [0.81, 1.02] | 1.03 [0.95, 1.12] | 0.93 [0.82, 1.07] | 0.91 [0.79, 1.05] | 0.97 [0.85, 1.1] | 0.91 [0.79, 1.05] | 0.99 [0.86, 1.14] |
Negative binomial models included fixed effects for wildfire PM2.5 lags 0–7 days, controlled for temperature, non-wildfire PM2.5, and time effects. We added a fixed effect to account for fewer visits on weekend days, and an offset to account for exposed population. We also included fixed effects for a set of ZCTA-level socioeconomic variables: median household income, home ownership (% homes occupied by owner), poverty (percent households below threshold income), age structure (percent of population under 5, 5–19, 20–64, and 65+ years), and racial/ethnic composition (percent Hispanic, percent non-Hispanic white, percent non-Hispanic Black). DME, electricity-dependent durable medical equipment; KPSC, Kaiser Permanente Southern California; ZCTA, Zip Code Tabulation Area.
In our additional analysis examining weekly wildfire PM2.5 levels lagged up to 2 weeks, a 10 increase in weekly wildfire PM2.5 concentration was associated with a next-week increase in outpatient visits (RR = 1.04, 95% CI: 1.00, 1.09), consistent with the daily outpatient visit model. Additionally, there were increases in weekly outpatient visits two weeks later (Table 2). We did not interpret the same-week coefficient due to issues with temporality – our outcome may have preceded the exposure. Weekly wildfire PM2.5 was not associated with the frequency of any other visits.
Table 2:
Rate ratio and 95% confidence intervals from a negative binomial modela assessing the association between weekly wildfire PM2.5 and healthcare utilization among KPSC DME users, weekly lags.
| Rate ratios and [95% CI] for 10 increase in wildfire PM2.5 | ||
|---|---|---|
|
| ||
| Outcome | lag 1 week | lag 2 weeks |
| All-cause outpatient | 1.04 [1.00, 1.09] | 1.05 [1.02, 1.09] |
| All-cause ED | 0.99 [0.88, 1.11] | 1.02 [0.92, 1.14] |
| All-cause inpatient | 1.08 [0.94, 1.23] | 0.99 [0.85, 1.15] |
| ED: cardiorespiratory concerns | 0.96 [0.84, 1.10] | 1.02 [0.91, 1.15] |
| Inpatient: cardiorespiratory concerns | 1.10 [0.96, 1.27] | 0.98 [0.85, 1.15] |
Negative binomial models included fixed effects for weekly mean wildfire PM2.5 lags 0–2 weeks, controlled for temperature, non-wildfire PM2.5, and time effects, and added an offset to account for exposed population. We also included fixed effects for a set of ZCTA-level socioeconomic variables: median household income, home ownership (% homes occupied by owner), poverty (percent households below threshold income), age structure (percent of population under 5, 5–19, 20–64, and 65+ years), and racial/ethnic composition (percent Hispanic, percent non-Hispanic white, percent non-Hispanic Black). CI, confidence interval; ED, emergency department; ZCTA, Zip Code Tabulation Area.
In additional analyses examining ED and inpatient visits, we also observed an 8% increase in rate of inpatient visits and a 10% increase in rate of cardiorespiratory inpatient visits 1 week following a 10 increase in weekly wildfire PM2.5 concentration (Table 2). Daily lag estimates were unstable, possibly owing to smaller sample sizes for inpatient and cardiorespiratory inpatient visits (Table 1).
Proximity to wildfire
There were 54 ZCTAs (9%) within 20 km of the Woolsey Fire boundary. We considered residents of these ZCTAs exposed to the fire. Despite the comparatively small size of the Getty Fire (3 km2 vs 400 km2), 98 ZCTAs (17%) met our exposure definition, as the Getty Fire was closer to population centers. We estimated that 20 and 21 ZCTAs overlapped with evacuation zones during the Woolsey and Getty fires, respectively. However, all ZCTAs overlapping with evacuation zones were also within 20km of the fire boundaries, meaning that the exposed ZCTAs were a subset of the wildfire proximate ZCTAs in both cases.
Woolsey Fire proximity and evacuation exposure
Residence in a ZCTA located within 20km of the Woolsey Fire boundary during the fire was associated with increased inpatient admissions for cardiorespiratory disease compared residence outside of it (RR = 1.45, 95% CI: 0.99, 2.12), and associated with decreased all-cause outpatient visits compared to residence outside of it (RR = 0.89, 95% CI: 0.79, 1.00), though the confidence intervals were wide (Figure 4). We observed similar associations, with wider confidence intervals, between Woolsey Fire evacuation exposure and healthcare visits. Residence in a ZCTA located in an evacuation zone of the Woolsey Fire during the fire was also associated with decreased all-cause outpatient and increased inpatient admissions for cardiorespiratory disease visits compared to residence outside of it (RR = 0.86, 95% CI: 0.72, 1.03, RR = 1.72, 95% CI: 1.00, 2.96, respectively), and was not associated with ED visit frequency (Figure 4). Detailed RRs for all visit types are outlined in eTable 1a and 1c.
Figure 4:
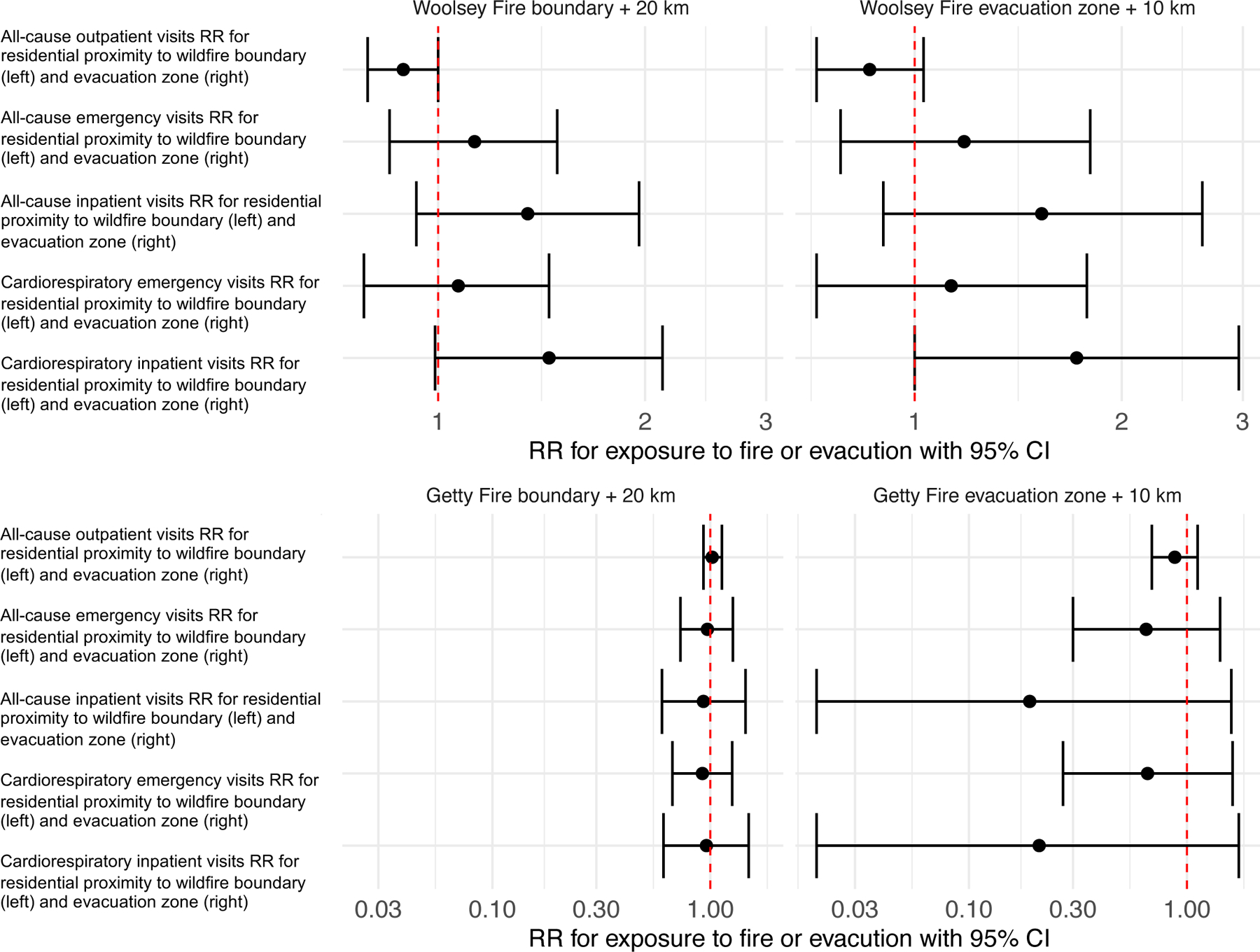
Plots of rate ratios and 95% confidence intervals from a negative binomial model assessing the association between residential proximity to wildfires and evacuation zones PM and healthcare utilization among KPSC DME users.
We used negative binomial regression to evaluate the effect of wildfire evacuation or proximity during an active fire. The difference-in-differences estimators subtracted the change in visit frequency when the Woolsey or Getty Fire was burning versus not burning among control ZCTAs (difference 1) from the change in visit frequency when the Woolsey or Getty Fire was burning versus not burning among ZCTAs exposed to the fire or evacuation zone (difference 2).We controlled for time effects, temperature, and non-wildfire PM2.5, and added an offset for the size of the exposed population. DME, electricity-dependent durable medical equipment; KPSC, Kaiser Permanente Southern California; RR, rate ratio; ZCTA, Zip Code Tabulation Area.
Getty Fire proximity and evacuation exposure
We observed no difference in frequency for any visit type during the Getty Fire for those living within 20 km of the fire compared to those living further away (Figure 4). Residence within an evacuation zone plus 10km was associated with reduced rate of all types of visits, though confidence intervals were very wide (Figure 4). Detailed RRs for all visit types are outlined in eTable 1b and 1d.
None of our results were sensitive to spline flexibility or the size of the buffer around exposures. Visual inspection of model residuals and Moran’s I results indicated that our model residuals were not exhibit spatial autocorrelation (plots included in eFigure 3, in the eAppendix).
Discussion
In this paper, we aimed to evaluate the relationship between daily wildfire PM2.5 exposure, residence near a wildfire, and residence in an evacuation zone, and daily ZCTA grouping-level healthcare visit counts. Using electronic health data describing 236,732 Kaiser Permanente DME-using patients from 2016–2020, we found that an increase in wildfire PM2.5 concentration was associated with brief (next-day) decreases in all-cause outpatient visits but increases in all-cause outpatient visits up to 2 weeks later in this population. Increases in wildfire PM2.5 were not associated with the frequency of daily ED or inpatient visits among DME users. However, in sensitivity analyses of 1-week lags, we did find elevated 1-week lag RRs for inpatient visits () and cardiorespiratory inpatient visits (RR=1.10). Residential proximity of DME users to the large Woolsey Fire was also associated with fewer all-cause outpatient visits, as well as more cardiorespiratory inpatient visits, but not with other visit types. Results for Woolsey Fire evacuation exposure were similar. Getty Fire evacuation or proximity was not associated with frequency of any kind of healthcare visit. Our study was unique in that we evaluated healthcare utilization among DME users, a group hypothesized to be susceptible to disaster and wildfire smoke exposures, included inpatient, ED, and outpatient visits, and examined residence near a wildfire or an evacuation zone in addition to wildfire PM2.5 exposure.
The literature describes a strong relationship between wildfire smoke exposure and respiratory health20, and a strong relationship between PM2.5 exposure and cardiovascular health61, though the relationship between wildfire PM2.5 and cardiovascular health is still being characterized. Large studies measure this association through healthcare utilization and have found increased risk of hospital admissions and ED visits for cardiorespiratory outcomes following wildfire PM2.5, PM10, or general smoke exposure in the U.S., Canada, Australia, and Brazil62–67. Fewer studies have examined wildfire PM2.5 exposure in vulnerable populations15,68. Of studies examining older adults, all have reported associations between smoke exposure and same or next-day increased inpatient and ED visit frequency62,66,69,70 and while some studies find older adults at elevated risk compared to younger adults16,64,69 others found no difference26,62. Surprisingly, we observed no association between wildfire PM2.5 and ED or inpatient visits among DME users. We hypothesized that older adult DME users would be particularly susceptible to wildfire PM2.5 due to probable high prevalence of underlying cardiorespiratory disease30. The observed null association between wildfire PM2.5 and ED or inpatient visits may indicate that DME users, especially those vulnerable to smoke, may take precautions to protect themselves from effects described in other studies or study limitations may obscure associations between smoke and more urgent healthcare use.
Limited studies have assessed outpatient care utilization during wildfire smoke exposure and most have focused on outpatient visits for respiratory concerns, reporting increases during smoke exposure62,71–74. None of those studies examined all-cause outpatient care use. Hutchinson et al. 201819 simultaneously reported decreases in all-cause outpatient visits during smoke exposure and increases in visits for respiratory concerns only, during a 5-day period following smoke exposure, suggesting that all or routine outpatient care may be disrupted, but respiratory care may be more needed and accessed during these exposures. Similarly, Henderson et al. 201161 found increased physician visits for asthma and all-respiratory outcomes related to same-day wildfire smoke exposure but no increase in physician visits for cardiovascular disease. In models with daily lags, we observed an initial same-day and next-day decrease in all-cause outpatient visits, and then a positive association between wildfire PM2.5 and all-cause outpatient visits among DME users for the week following exposure. In models with weekly lags, we observed increased outpatient visits in the 2 weeks following exposure, suggesting that there is overall an increase in all-cause outpatient visits among DME users following wildfire PM2.5 exposure. Very few prior studies have evaluated lags of short-term exposure to wildfire PM2.5 beyond 7 days,34 but our results indicate that outpatient visits among DME users remained elevated for up to 2 weeks. A decrease in healthcare utilization has been observed in previous studies of disaster-related exposures, including wildfires75 and extreme storms76. Our findings are consistent with theories that wildfire smoke may disrupt care immediately18,61, but at the same time exacerbate respiratory conditions leading to increased care use following smoke exposure among people (such as DME users) who have respiratory conditions.
Few studies have evaluated proximity to wildfire boundaries or wildfire evacuation as risk factors for healthcare utilization or adverse health outcomes74,77,78. Proximity to wildfires can affect health through a stress pathway, on top of risks related to smoke exposure. Qualitative studies emphasize this point, and several have documented the immense stress experienced by those displaced by wildfire7,8,53. After the 2014 Canadian Northwest Territory wildfires, one interviewee said: “Well, it took a toll on me because being stressed out from the fires and never knowing when we had to leave to be evacuated we didn’t know if we were going to come home to a community or to our houses.”28 Agyapong et al. 2021 estimated the likely prevalence of post-traumatic stress disorder among Canadian Fort McMurray wildfire survivors at 12.8%, twice the baseline population prevalence79. We attempted to assess this proximity/evacuation pathway for two major fires in our study area using a difference-in-differences analysis.
We found no association between exposure and healthcare visits during the Getty Fire. However, during the Woolsey Fire, we observed an increase in cardiorespiratory inpatient visits and a decrease in all-cause outpatient visits with both residential proximity to fire and residence in an evacuation among DME users. The 400 km2 Woolsey Fire, which caused $3 billion in damages,80 was much larger than the 3 km2 Getty Fire, which destroyed 10 homes39, that null associations between Getty proximity exposure and all visit types could be due to its smaller size; it may have not been large enough to produce a detectable effect in visit changes. A larger analysis examining several wildfires, rather than two, could be informative. As in our discussion of wildfire PM2.5 exposure, the Woolsey Fire may have decreased outpatient care as has been documented during other disaster scenarios,75, 76 while inpatient visits may have increased because of respiratory disease worsening with exposure.
However, study limitations could have influenced our results. First, we identified KPSC members who rented DME in the year prior to October 29, 2019. This meant that some study participants may not have been using DME at the time of wildfire exposure or healthcare visit but were nonetheless likely socially or medically vulnerable. KPSC patients would be highly motivated to seek care at Kaiser, given their membership status; however, they may have sought urgent care at other clinics or hospitals. Such alternate utilization would have produced artificially reduced visit counts, especially for inpatient and emergency visits. If patients sought care at other clinics only during wildfires (whether during evacuations or while a fire was burning nearby) this could have biased association estimates towards the null.
Second, we lacked individual-level information on participants. Therefore, we did not know if patients sought care for DME-related issues and only used prior DME use as a vulnerability metric. We also were not able to assess differences in healthcare use by type of DME or stratify by age group or sex beyond limiting our study population to those age 45 or older. Excluding younger people excluded most breast pump users, a generally healthy subpopulation who constitute 30% of DME users of all ages at KPSC30. Subgroups such as those using ventilators or those using breast pumps likely have vastly different health needs and outcomes. We chose to focus on DME users overall aged 45 and older who were likely the most susceptible to wildfire. However, users of specific types of DME, such as oxygen concentrators, or DME users of different ages, such as those over 75 years, may have unique needs and differing outcomes; future research may wish to examine these sub-groups in detail.
Third, days with 0 visits made by patients living in a spatial grouping were common. Inpatient and ED visits were much less frequent over the study period (both mean = 0.1 daily visits) than outpatient visits (mean = 2.5 daily visits). All models may have been underpowered to detect visit changes. For example, during the Woolsey Fire, we observed decreased outpatient visits in ZCTAs proximate to the fire and among evacuation exposed ZCTAs but, for both, confidence intervals were wide, likely due to sample size.
Last, as in any observational study, residual confounding could affect our results. We attempted to account for residual spatial confounding by including a set of ZCTA-level covariates that measured different facets of socioeconomic status.
Conclusion
This study evaluated the relationship between short-term exposure to wildfire PM2.5 and residential proximity and residence in a disaster zone, as a proxy for a mixture of health-harming exposures such as community disruption, smoke exposure, and stress and outpatient, ED, and inpatient visits among DME users in Southern California. Observed associations pointed to disruption of daily lives among those more exposed to wildfire, with missed outpatient care visits. We observed an association between elevated wildfire PM2.5 concentrations and decreased next-day rate followed by increased rate of all-cause outpatient visits over 4/5 subsequent days as well as reduced all-cause outpatient visits among those living in proximity to the Woolsey Fire. Wildfire PM2.5 was not associated with ED or inpatient visits, but Woolsey Fire proximity was associated with increased inpatient cardiorespiratory visits. This study adds to a literature on the health of vulnerable populations exposed to wildfires, which becomes more critical as wildfires frequency and severity increases with climate change. Protecting vulnerable populations that may be harmed by exposures which others can avoid or endure is essential. More work is needed to understand the timing of health risks for vulnerable populations affected by smoke, fire, and evacuation.
Supplementary Material
Acknowledgments
This paper is supported by the National Institute on Aging RF1AG071024.
We acknowledge Dr. Robbie Parks for his publicly downloadable temperature processing scripts used in our data pipeline.
Footnotes
No authors have a conflict of interest.
All of our code is publicly available for download at github.comheathermcb/wildfires_and_DME, but our data is privately shared from Kaiser Permanente Southern California, and therefore cannot be made public.
References
- 1.Spracklen DV, Mickley LJ, Logan JA, et al. Impacts of climate change from 2000 to 2050 on wildfire activity and carbonaceous aerosol concentrations in the western united states. Journal of Geophysical Research: Atmospheres 2009;114(D20). doi: 10.1029/2008JD010966 [DOI] [Google Scholar]
- 2.Fried JS, Torn MS, Mills E. The impact of climate change on wildfire severity: A regional forecast for northern california. Climatic Change 2004;64(1):169–191. doi: 10.1023/B:CLIM.0000024667.89579.ed [DOI] [Google Scholar]
- 3.Westerling AL, Hidalgo HG, Cayan DR, Swetnam TW. Warming and earlier spring increase western u.s. Forest wildfire activity. Science 2006;313(5789):940–943. 10.1126/science.1128834 [DOI] [PubMed] [Google Scholar]
- 4.Abatzoglou JT, Williams AP. Impact of anthropogenic climate change on wildfire across western US forests. Proc Natl Acad Sci U S A 2016;113(42):11770–11775. doi: 10.1073/pnas.1607171113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Williams AP, Abatzoglou JT, Gershunov A, et al. Observed impacts of anthropogenic climate change on wildfire in california. Earth’s Future 2019;7(8):892–910. [Google Scholar]
- 6.Radeloff VC, Helmers DP, Kramer HA, et al. Rapid growth of the US wildland-urban interface raises wildfire risk. Proceedings of the National Academy of Sciences 2018;115(13):3314–3319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Belleville G, Ouellet MC, Morin CM. Post-traumatic stress among evacuees from the 2016 fort McMurray wildfires: Exploration of psychological and sleep symptoms three months after the evacuation. International Journal of Environmental Research and Public Health 2019;16(9). doi: 10.3390/ijerph16091604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McCaffrey Sarah, S M, Rhodes Alan. Wildfire evacuation and its alternatives: Perspectives from four united states’ communities. International Journal of Wildland Fire 2014;24:170–178. [Google Scholar]
- 9.Liu JC, Mickley LJ, Sulprizio MP, et al. Particulate air pollution from wildfires in the western US under climate change. Clim Change 2016;138(3):655–666. doi: 10.1007/s10584-016-1762-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O’Dell K, Bilsback K, Ford B, et al. Estimated mortality and morbidity attributable to smoke plumes in the united states: Not just a western US problem. GeoHealth 2021;5(9):e2021GH000457. doi: 10.1029/2021GH000457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lassman W, Ford B, Gan RW, et al. Spatial and temporal estimates of population exposure to wildfire smoke during the washington state 2012 wildfire season using blended model, satellite, and in situ data. GeoHealth 2017;1(3):106–121. doi: 10.1002/2017GH000049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nakayama Wong LS, Aung HH, Lamé MW, Wegesser TC, Wilson DW. Fine particulate matter from urban ambient and wildfire sources from california’s san joaquin valley initiate differential inflammatory, oxidative stress, and xenobiotic responses in human bronchial epithelial cells. Toxicology in Vitro 2011;25(8):1895–1905. doi: 10.1016/j.tiv.2011.06.001 [DOI] [PubMed] [Google Scholar]
- 13.Aguilera R, Corringham T, Gershunov A, Benmarhnia T. Wildfire smoke impacts respiratory health more than fine particles from other sources: Observational evidence from southern california. Nature Communications 2021;12(1):1493. doi: 10.1038/s41467-021-21708-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu JC, Peng RD. The impact of wildfire smoke on compositions of fine particulate matter by ecoregion in the western US. Journal of exposure science & environmental epidemiology 2019;29(6):765–776. [DOI] [PubMed] [Google Scholar]
- 15.Colleen Reid MMM. Wildfire smoke exposure under climate change. Pulmonary Medicine Published online 2019. [DOI] [PMC free article] [PubMed]
- 16.Anjali Haikerwal, A DM, Muhammad Akram, Dennekamp M. Impact of fine particulate matter (PM2.5) exposure during wildfires on cardiovascular health outcomes. JAHA Published online 2015. [DOI] [PMC free article] [PubMed]
- 17.Yao J, Brauer M, Wei J, McGrail KM, Johnston FH, Henderson SB. Sub-daily exposure to fine particulate matter and ambulance dispatches during wildfire seasons: A case-crossover study in British Columbia, Canada. Environ Health Perspect 2020;128(6):67006. doi: 10.1289/EHP5792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reid CE, Considine EM, Watson GL, Telesca D, Pfister GG, Jerrett M. Associations between respiratory health and ozone and fine particulate matter during a wildfire event. Environ Int 2019;129:291–298. doi: 10.1016/j.envint.2019.04.033 [DOI] [PubMed] [Google Scholar]
- 19.Hutchinson JA, Vargo J, Milet M, et al. The san diego 2007 wildfires and medi-cal emergency department presentations, inpatient hospitalizations, and outpatient visits: An observational study of smoke exposure periods and a bidirectional case-crossover analysis. PLoS Med 2018;15(7):e1002601. doi: 10.1371/journal.pmed.1002601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reid CE, Brauer M, Johnston FH, Jerrett M, Balmes JR, Elliott CT. Critical review of health impacts of wildfire smoke exposure. Environ Health Perspect 2016;124(9):1334–1343. doi: 10.1289/ehp.1409277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu JC, Wilson A, Mickley LJ, et al. Who Among the Elderly Is Most Vulnerable to Exposure to and Health Risks of Fine Particulate Matter From Wildfire Smoke? American Journal of Epidemiology 2017;186(6):730–735. doi: 10.1093/aje/kwx141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kollanus V, Tiittanen P, Niemi JV, Lanki T. Effects of long-range transported air pollution from vegetation fires on daily mortality and hospital admissions in the helsinki metropolitan area, finland. Environ Res 2016;151:351–358. doi: 10.1016/j.envres.2016.08.003 [DOI] [PubMed] [Google Scholar]
- 23.Doubleday A, Schulte J, Sheppard L, et al. Mortality associated with wildfire smoke exposure in washington state, 2006–2017: A case-crossover study. Environ Health 2020;19(1):4. doi: 10.1186/s12940-020-0559-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu JC, Pereira G, Uhl SA, Bravo MA, Bell ML. A systematic review of the physical health impacts from non-occupational exposure to wildfire smoke. Environ Res 2015;136:120–132. doi: 10.1016/j.envres.2014.10.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Davies Ian P., CR J, Haugo Ryan D.. The unequal vulnerability of communities of color to wildfire. PLOS ONE Published online 2018. [DOI] [PMC free article] [PubMed]
- 26.Rappold AG, Reyes J, Pouliot G, Cascio WE, Diaz-Sanchez D. Community vulnerability to health impacts of wildland fire smoke exposure. Environmental Science & Technology 2017;51(12):6674–6682. doi: 10.1021/acs.est.6b06200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aguilera R, Corringham T, Gershunov A, Leibel S, Benmarhnia T. Fine particles in wildfire smoke and pediatric respiratory health in california. Pediatrics 2021;147(4). doi: 10.1542/peds.2020-027128 [DOI] [PubMed] [Google Scholar]
- 28.Dodd W, Scott P, Howard C, et al. Lived experience of a record wildfire season in the northwest territories, canada. Canadian Journal of Public Health 2018;109(3):327–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jacobs BC, Lee JA. Durable medical equipment: Types and indications. Medical Clinics 2014;98(4):881–893. [DOI] [PubMed] [Google Scholar]
- 30.Casey JA, Mango M, Mullendore S, et al. Trends from 2008 to 2018 in electricitydependent durable medical equipment rentals and sociodemographic disparities. Epidemiology 2021;32(3):327–335. doi: 10.1097/EDE.0000000000001333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mahsin MD, Cabaj J, Saini V. Respiratory and cardiovascular condition-related physician visits associated with wildfire smoke exposure in Calgary, Canada, in 2015: a population-based study. International Journal of Epidemiology Published online September 2021. doi: 10.1093/ije/dyab206 [DOI] [PubMed]
- 32.Santana Francisca N., Gonzalez David JX, and Wong-Parodi Gabrielle. “Psychological factors and social processes influencing wildfire smoke protective behavior: Insights from a case study in Northern California.” Climate Risk Management 34 (2021): 100351. [Google Scholar]
- 33.Hamideh Sara, Sen Payel, and Fischer Erica. “Wildfire impacts on education and healthcare: Paradise, California, after the Camp Fire.” Natural hazards 111, no. 1 (2022): 353–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wong-Parodi Gabrielle. “Support for public safety power shutoffs in California: Wildfire-related perceived exposure and negative outcomes, prior and current health, risk appraisal and worry.” Energy Research & Social Science 88 (2022): 102495. [Google Scholar]
- 34.Kivimaki SM Effects of stress on the development and progression of cardiovascular disease. Nat Rev Cardiol Published online 2018. [DOI] [PubMed]
- 35.Los Angeles Fire Department. LAFD news: Woolsey fire Published 2019. https://www.lafd.org/news/woolsey-fire
- 36.Fire Cal 2018 Incident Archive Published 2018. https://www.fire.ca.gov/incidents/2018
- 37.Los Angeles Fire Department. LAFD news: Getty fire Published 2018. https://www.lafd.org/news/getty-fire
- 38.Fire Cal 2019 Incident Archive Published 2019. https://www.fire.ca.gov/incidents/2019/
- 39.Koebnick C, Langer-Gould AM, Gould MK, et al. Sociodemographic characteristics of members of a large, integrated health care system: comparison with US Census Bureau data. Perm J 2012; 16:37–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Aguilera R, Luo N, Basu R, Wu J, Clemesha R, Gershunov A, & Benmarhnia T (2023). A novel ensemble-based statistical approach to estimate daily wildfire-specific PM2. 5 in California (2006–2020). Environment International, 171, 107719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.National Interagency Fire Center. Historic wildland fire open data Published 2022. https://datanifc.opendata.arcgis.com/search?tags=Category%2Chistoric_wildlandfire_opendata
- 42.CALFIRE Fire and Resource Assessment Program. Published 2022. https://frap.fire.ca.gov/mapping/gis-data/
- 43.Tally Steven, Levack Ashley, Sarkin Andrew J., Gilmer Todd, and Groessl Erik J.. “The impact of the San Diego wildfires on a general mental health population residing in evacuation areas.” Administration and Policy in Mental Health and Mental Health Services Research 40, no. 5 (2013): 348–354. [DOI] [PubMed] [Google Scholar]
- 44.Kirsch Katie R., Feldt Bonnie A., Zane David F., Haywood Tracy, Jones Russell W., and Horney Jennifer A.. “Longitudinal community assessment for public health emergency response to wildfire, Bastrop County, Texas.” Health security 14, no. 2 (2016): 93–104. [DOI] [PubMed] [Google Scholar]
- 45.Marshall Grant N., Schell Terry L., Elliott Marc N., Rayburn Nadine R., and Jaycox Lisa H.. “Psychiatric disorders among adults seeking emergency disaster assistance after a wildland-urban interface fire.” Psychiatric services 58, no. 4 (2007): 509–514. [DOI] [PubMed] [Google Scholar]
- 46.Felix Erika D., and Afifi Walid. “The role of social support on mental health after multiple wildfire disasters.” Journal of Community Psychology 43, no. 2 (2015): 156–170. [Google Scholar]
- 47.Jones Russell T., Ribbe David P., Cunningham Phillippe B., David Weddle J, and Langley Audra K.. “Psychological impact of fire disaster on children and their parents.” Behavior modification 26, no. 2 (2002): 163–186. [DOI] [PubMed] [Google Scholar]
- 48.Jones Russell T., Ribbe David P., Cunningham Phillippe, and David Weddle J. “Psychosocial correlates of wildfire disaster: Post disaster adult reactions.” Fire technology 39, no. 2 (2003): 103–117. [Google Scholar]
- 49.Jones Benjamin A., and Berrens Robert P.. “Prescribed Burns, Smoke Exposure, And Infant Health.” Contemporary Economic Policy 39, no. 2 (2021): 292–309. [Google Scholar]
- 50.Johnston David W., Kürşat Önder Yasin, Habibur Rahman Muhammad, and Ulubaşoğlu Mehmet A.. “Evaluating wildfire exposure: Using wellbeing data to estimate and value the impacts of wildfire.” Journal of Economic Behavior & Organization 192 (2021): 782–798. [Google Scholar]
- 51.Team QD. QGIS geographic information system Published online 2009. http://qgis.org
- 52.Christianson AC, McGee TK. Wildfire evacuation experiences of band members of whitefish lake first nation 459, Alberta, Canada. Natural Hazards 2019;98(1):9–29. [Google Scholar]
- 53.Westerling AL, Hidalgo HG, Cayan DR, Swetnam TW. Warming and earlier spring increase western u.s. Forest wildfire activity. Science 2006;313(5789):940–943. 10.1126/science.1128834 [DOI] [PubMed] [Google Scholar]
- 54.Rochelle S Green BM Rupa Basu. The effect of temperature on hospital admissions in nine california counties. International Journal of Public Health 2010;55:113–121. [DOI] [PubMed] [Google Scholar]
- 55.Vlassova L, Perez-Cabello F, Mimbrero MR, Lloverıá RM, Garcıá -Martıń A. Analysis of the relationship between land surface temperature and wildfire severity in a series of landsat images. Remote Sensing 2014;6(7):6136–6162. doi: 10.3390/rs6076136 [DOI] [Google Scholar]
- 56.Group PC. PRISM climate group daily temperature data Published 2021. https://prism.oregonstate.edu/
- 57.Bureau UC. American community survey 5-year public use samples Published online 2016–2020.
- 58.Team RC. R: A language and environment for statistical computing Published online 2021. https://www.R-project.org/
- 59.Wood S Generalized Additive Models: An Introduction with r 2nd ed. Chapman; Hall/CRC; 2017. [Google Scholar]
- 60.Yu Yu, Wei William Zou Michael Jerrett, and Meng Ying-Ying. “Acute Health Impact of Convectional and Wildfire-related PM2. 5: a narrative review.” Environmental Advances (2022): 100179.
- 61.Henderson SB, Brauer M, MacNab YC, Kennedy SM. Three measures of forest fire smoke exposure and their associations with respiratory and cardiovascular health outcomes in a population-based cohort. Environmental health perspectives 2011;119(9):1266–1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Thelen B, French NH, Koziol BW, et al. Modeling acute respiratory illness during the 2007 san diego wildland fires using a coupled emissions-transport system and generalized additive modeling. Environmental Health 2013;12(1):1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Delfino RJ, Brummel S, Wu J, et al. The relationship of respiratory and cardiovascular hospital admissions to the southern california wildfires of 2003. Occupational and environmental medicine 2009;66(3):189–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Johnston FH, Purdie S, Jalaludin B, Martin KL, Henderson SB, Morgan GG. Air pollution events from forest fires and emergency department attendances in sydney, australia 1996–2007: A case-crossover analysis. Environmental health 2014;13(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Morgan G, Sheppeard V, Khalaj B, et al. Effects of bushfire smoke on daily mortality and hospital admissions in sydney, australia. Epidemiology Published online 2010:47–55. [DOI] [PubMed]
- 66.Ye T, Guo Y, Chen G, et al. Risk and burden of hospital admissions associated with wildfire-related PM2 5 in brazil, 2000–15: A nationwide time-series study. The Lancet Planetary Health 2021;5(9):e599–e607. [DOI] [PubMed] [Google Scholar]
- 67.Xi Y, Kshirsagar AV, Wade TJ, et al. Mortality in US hemodialysis patients following exposure to wildfire smoke. Journal of the American Society of Nephrology 2020;31(8):1824–1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ignotti E, Valente JG, Longo KM, Freitas SR, Hacon S de S, Artaxo Netto P. Impact on human health of particulate matter emitted from burnings in the brazilian amazon region. Revista de saude publica 2010;44:121–130. [DOI] [PubMed] [Google Scholar]
- 69.DeFlorio-Barker S, Crooks J, Reyes J, Rappold AG. Cardiopulmonary effects of fine particulate matter exposure among older adults, during wildfire and non-wildfire periods, in the united states 2008–2010. Environmental health perspectives 2019;127(3):037006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sheldon TL, Sankaran C. The impact of indonesian forest fires on singaporean pollution and health. American Economic Review 2017;107(5):526–529. [DOI] [PubMed] [Google Scholar]
- 71.Lee TS, Falter K, Meyer P, Mott J, Gwynn C. Risk factors associated with clinic visits during the 1999 forest fires near the hoopa valley indian reservation, california, USA. International journal of environmental health research 2009;19(5):315–327. [DOI] [PubMed] [Google Scholar]
- 72.Moore D, Copes R, Fisk R, Joy R, Chan K, Brauer M. Population health effects of air quality changes due to forest fires in british columbia in 2003. Canadian journal of public health 2006;97(2):105–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mott JA, Mannino DM, Alverson CJ, et al. Cardiorespiratory hospitalizations associated with smoke exposure during the 1997 southeast asian forest fires. International journal of hygiene and environmental health 2005;208(1–2):75–85. [DOI] [PubMed] [Google Scholar]
- 74.Binet É, Ouellet MC, Lebel J, et al. A portrait of mental health services utilization and perceived barriers to care in men and women evacuated during the 2016 fort McMurray wildfires. Administration and Policy in Mental Health and Mental Health Services Research 2021;48(6):1006–1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sorensen Cecilia, et al. “Associations between wildfire‐related PM2. 5 and intensive care unit admissions in the United States, 2006–2015.” GeoHealth 5.5 (2021): e2021GH000385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Parks Robbie M., et al. “Tropical cyclone exposure is associated with increased hospitalization rates in older adults.” Nature communications 12.1 (2021): 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Park BY, Boles I, Monavvari S, et al. The association between wildfire exposure in pregnancy and foetal gastroschisis: A population-based cohort study. Paediatric and perinatal epidemiology 2022;36(1):45–53. [DOI] [PubMed] [Google Scholar]
- 78.Tally S, Levack A, Sarkin AJ, Gilmer T, Groessl EJ. The impact of the san diego wildfires on a general mental health population residing in evacuation areas. Administration and Policy in Mental Health and Mental Health Services Research 2013;40(5):348–354. [DOI] [PubMed] [Google Scholar]
- 79.Agyapong VI, Juhas M, Omege J, et al. Prevalence rates and correlates of likely post-traumatic stress disorder in residents of fort mcmurray 6 months after a wildfire. International Journal of Mental Health and Addiction 2021;19(3):632–650. [Google Scholar]
- 80.Holland E. $6 Billion In Real Estate Destroyed In Woolsey Fire: Report. https://patch.com/california/malibu/6-billion-real-estate-destroyed-woolsey-fire-report.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


