Abstract
Individuals who have experienced more trauma throughout life have a heightened risk of developing posttraumatic stress disorder (PTSD) following injury. Although trauma history cannot be retroactively modified, identifying the mechanism(s) by which preinjury life events influence future PTSD symptoms may help clinicians mitigate the detrimental effects of past adversity. The current study proposed attributional negativity bias, the tendency to perceive stimuli/events as negative, as a potential intermediary in PTSD development. We hypothesized an association between trauma history and PTSD symptom severity following a new index trauma via heightened negativity bias and acute stress disorder (ASD) symptoms. Recent trauma survivors (N =189, 55.5% women, 58.7% African American/Black) completed assessments of ASD, negativity bias, and lifetime trauma 2-weeks postinjury; PTSD symptoms were assessed 6 months later. A parallel mediation model was tested with bootstrapping (10,000 resamples). Both negativity bias, Path b1: β = −.24, t(187) = −2.88, p = .004, and ASD symptoms, Path b2: β = .30, t(187) = 3.71, p < .001, fully mediated the association between trauma history and 6-month PTSD symptoms, full model: F(6, 182) = 10.95, p < .001, R 2= .27; Path c’: β = .04, t(187) = 0.54, p = .587. These results suggest that negativity bias may reflect an individual cognitive difference that can be further activated by acute trauma. Moreover, negativity bias may be an important, modifiable treatment target, and interventions addressing both acute symptoms and negativity bias in the early posttrauma period may weaken the link between trauma history and new-onset PTSD.
Trauma exposure occurs frequently, with estimates indicating that up to 70% of the world's population will experience at least one traumatic event in their lifetime (Kessler et al., 2017). In the early aftermath of trauma, many individuals experience heightened psychological and physiological reactions. For a subset of survivors (i.e., approximately 10%), the consequences of trauma exposure persist, and nonremitting symptoms develop into posttraumatic stress disorder (PTSD; American Psychological Association [APA], 2013). Trauma history is a prominent risk factor for chronic PTSD. As the number of lifetime traumatic experiences increases, the likelihood and severity of PTSD following a new-onset acute traumatic event have been shown to increase linearly (Irish et al., 2008; Kessler et al., 2018; Liu et al., 2017; Nishith et al., 2000; Weis et al., 2021).
One explanation as to why preexisting trauma strongly influences future psychopathology is the cumulative stress theory (Frodl & O’Keane, 2013). Although a single stressor or traumatic event may be disruptive of mental and/or physical health, the impact of experiencing a multitude of stressors and traumatic experiences is associated with the widespread disruption of normal biological responses to stress (E. D. Carlson & Chamberlain, 2005; Frodl & O’Keane, 2013; Seeman et al., 1997; Suglia et al., 2010). Prior work with traumatically injured participants indicates that lifetime trauma exposure is a robust predictor of future PTSD symptoms (E. B. Carlson et al., 2011; Weis et al., 2021). Unfortunately, individual preexisting trauma exposure cannot be changed; however, identifying potential mechanisms that explain how pretrauma events influence new-onset future PTSD symptoms may help mitigate the risk associated with cumulative lifetime trauma.
Negativity bias, a component of dysregulated affective information processing (Norris, 2021), is one such construct that may play a mechanistic role in the link between lifetime trauma history and the risk of adverse psychological outcomes following acute trauma. Operationalized as the tendency to perceive and/or expect negative events and outcomes, negativity bias can be essential and adaptive in aiding orientation toward safety (Lang et al., 1990; Norris, 2021). Naturally, attention and interest are more robustly captured by negative information to prioritize the mobilization of defensive responding and, thereby, survival (Lang et al., 1990; Norris, 2021; Norris et al., 2011). However, affective processing dysfunction can result in the overinterpretation of situations and stimuli as negative (e.g., through the accumulation of multiple traumatic experiences or stressful events), thereby reducing the allocation of attention and motivated behavior toward rewarding stimuli and goals (Gollan et al., 2016; Norris et al., 2011). Negativity bias is a broad umbrella term and can include both attentional (e.g., processing bias towards negative vs. neutral stimuli) and attributional (e.g., a cognitive tendency to view events more negatively) biases (Kimble & Hyatt, 2019). Herein, we focus on attributional negativity biases.
In general, maladaptive attributional negativity biases have long been considered in prevailing theories of depressive and anxiety disorders (Ehlers & Clark, 2000). Negative attributional styles may maintain symptoms of both depression and PTSD (i.e., increasing vulnerability through maladaptive or negative interpretations of life events or trauma; Abramson et al., 1989; Beck, 1987). Similarly, with anxiety disorders, this biased pattern denotes the interpretation of ambiguous stimuli and situations as either threatening or feared, causing hyperreactivity (Carlisi & Robinson, 2018; Williams et al., 2009). Indeed, these attributional biases are such prominent features of PTSD that they are embedded in the Diagnostic and Statistical Manual of Mental Disorder (5th ed.; DSM-5; APA, 2013) diagnostic criteria for the disorder, particularly Criterion D (i.e., negative alterations in cognitions and mood) and Criterion E (i.e., alterations in arousal and reactivity; Watters & Williams, 2011). Individuals with PTSD often exhibit biases toward negative emotional or trauma-related information (Kimble et al., 2018). This negativity bias is hypothesized to maintain and exacerbate symptoms by allocating cognitive resources to this emotional information. The misallocation of cognitive resources may disrupt the processing of other important environmental information, such as cues that signal safety and increase stress responses. Attributional negativity bias is associated with increased negative appraisals of traumatic experiences and, therefore, may actually drive the development of PTSD (Kimble & Hyatt, 2019).
Although trauma history is a known risk factor for PTSD, fewer studies have examined pathways explaining how lifetime trauma exposure influences PTSD outcomes. Given the literature demonstrating the formation of negativity bias through previous experience, negativity bias is a contender in the mechanisms underlying subsequent PTSD development. In addition to negativity bias, previous work suggests that posttraumatic stress symptoms (PTSS) that occur within 1 month of trauma exposure may also predict the development of PTSD. Although the PTSD diagnostic criteria do not consider PTSS until 1-month posttrauma, initial symptoms can be captured by the criteria for acute stress disorder (ASD; APA, 2013). ASD symptoms (i.e., PTSS that occur within 1-month posttrauma) may be useful in predicting who will develop PTSD (Bryant, 2010). In a sample of traumatically injured adults, ASD symptom severity, as measured using the PTSD Checklist for DSM-5 (PCL-5; Weathers, Litz, et al., 2013) and evaluated during hospitalization, was predictive of PTSD symptoms assessed 1-, 3-, and 6-months postinjury (deRoon-Cassini et al., 2010). Therefore, ASD symptoms may serve as a facilitator of subsequent symptom presentation.
The current study aimed to examine the associations among attributional negativity bias, trauma history, and PTSS in a sample of traumatically injured adults. We leveraged a prospective, longitudinal design to explore the role of attributional negativity bias, measured in the acute aftermath of trauma exposure, within the association between lifetime trauma history and future PTSD symptom severity. We anticipated that negativity bias and ASD symptoms (i.e., PTSS as assessed 2-weeks postinjury) would simultaneously mediate the association between preexisting lifetime trauma exposure and PTSD symptoms at 6-months posttrauma.
METHOD
Participants
In total, 232 individuals were recruited to participate in a prospective, longitudinal study examining risk and resilience following a traumatic injury (for additional detail see Bird et al., 2021; Webb et al., 2020; Weis et al., 2021). Adult participants aged 18–65 years were screened in the emergency department (ED) of a Level 1 trauma center. Individuals were eligible to participate if they spoke English and were able to schedule an appointment within 2 weeks of the injury. Previous work suggests that approximately 21% of traumatically injured patients recruited in an ED context go on to develop PTSD (Geier et al., 2019). Therefore, to identify higher-risk individuals, participants were screened and deemed eligible if they scored at least a 3 out of 5 on the Predicting PTSD Questionnaire (Rothbaum et al., 2013) or endorsed that the event leading to their ED visit was of near-death severity (Brasel et al., 2010; Rothbaum et al., 2013). Exclusion criteria were a spinal cord injury with neurological deficits, severe hearing or visual impairments, a history of psychotic or manic symptoms, being on police hold, having moderate-to-severe traumatic brain injury, or a positive alcohol test (i.e., a blood alcohol content greater than 0.08).
Procedure
Two weeks postinjury (Time [T] 1), participants completed a demographic assessment as well as self-report measures of negativity bias, new-onset PTSS severity (i.e., ASD symptoms), and lifetime trauma. Approximately 6 months postinjury (T2), participants completed a follow-up appointment to assess PTSS severity and PTSD diagnostic status in relation to the traumatic event that brought them to the ED. All procedures were approved by the Medical College of Wisconsin’s Institutional Review Board. Individuals provided informed consent and were financially compensated for study participation (i.e., up to $625 [USD] if all study visits and assessments were completed).
Measures
Attributional negativity bias
Participants completed an established self-report measure of emotional health, the mini–Brief Resilience Index for Screening (mini-BRISC; Rowe et al., 2007; Williams et al., 2009) as part of a computerized cognitive test battery (i.e., WebNeuro; Silverstein et al., 2007). The mini-BRISC is a validated 15-item questionnaire that has been used to identify individuals with depression, PTSD, and panic disorder (Williams et al., 2012). The mini-BRISC provides normalized scores for three domains: negativity bias, resilience, and social capacity.
In line with the current study’s hypotheses, only Negativity Bias subscale scores were included in this analysis. The negativity bias domain comprises five items evaluating sensitivity to and anticipation of negative events (e.g., “I tended to overreact to situations”; Williams et al., 2012). The negativity bias z scores used in the analyses were normalized to a nonclinical sample of over 1,300 participants, and scores were inverted such that a negative normalized score was indicative of a higher level of negativity bias (Williams et al., 2009). In the current sample, the z-score ranged from −2.87 to 2.37.
Adverse life experiences
The Life Events Checklist for the DSM-5 (LEC-5; Weathers, Blake, et al., 2013b) is a brief self-report assessment that is used to identify exposure to past potentially traumatic experiences that might meet DSM-5 PTSD Criterion A (Weathers, Blake, et al., 2013b). Respondents are asked to indicate their level of exposure (i.e., “happened to me,” “witnessed it,” “learned about it,” “part of my job,” “not sure,” or “does not apply”) to 17 potentially traumatic events. We employed a recently validated weighted scoring method that was developed in the current sample (Weis et al., 2022), which weights events based on exposure proximity such that events that a respondent directly experienced are weighted with a 3, witnessed events correspond with a 2, and events the respondent learned are weighted with a 1. The possible weighted total score ranges from 0 to 102 (current sample range: 0–78), with higher scores indicating higher degrees of exposure and proximity to traumatic events. In the present sample, Cronbach’s alpha was .91.
ASD symptoms
At T1, the PCL-5 (Weathers, Litz, et al., 2013) was used to assess symptoms of ASD linked to the recent injury. The PCL-5 consists of 20 self-report items that correspond with the DSM-5 PTSD diagnostic criteria. Participants rated how much each symptom had bothered them since experiencing the injury on a scale of 0 (not at all) to 4 (extremely). A total symptom severity score was created by summing item-level scores (Blevins et al., 2015; Weathers, Litz, et al., 2013). PCL-5 scores range from 0 to 80 (current sample range: 0–73), with higher scores indicating the presence of more severe PTSD symptoms. In the present sample, Cronbach’s alpha was .94.
PTSD symptoms
At T2 (i.e., 6-months postinjury), a trained member of the research staff administered the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5; Weathers, Blake, et al., 2013a) to evaluate PTSD symptoms in relation to the traumatic injury that precipitated the ED visit and establish PTSD diagnostic status. The CAPS-5 was used to assess the intensity and frequency of 30 items, 20 of which correspond with DSM-5 PTSD diagnostic criteria, with responses anchored to symptoms related to the traumatic injury. A single severity score was assigned to each of the 20 symptom items and a total score was created by summing severity ratings. Higher scores were indicative of higher levels of PTSD symptom severity (current sample range: 0–63). In the present sample, Cronbach’s alpha was .93.
To meet the criteria for a PTSD diagnosis, individuals had to report psychological disturbance for at least 1 month that was functionally and significantly impairing along with at least one symptom each from Criterion B (i.e., intrusion items) and Criterion C (i.e., avoidance items) and two symptoms each from Criterion D (i.e., negative alterations in cognitions and mood items) and Criterion E (i.e., alterations in arousal and reactivity; APA, 2013). Fewer than 20% of participants met the diagnostic threshold for PTSD. Approximately 20% of the assessments were subjected to reliability checks. There was excellent reliability across interviewer administration within the study, interclass correlation coefficient (ICC) = .96, 95% confidence interval (CI) [.93, .98].
Data analysis
All analyses were conducted using SPSS Statistics (Version 25.0). Only individuals who completed all measurements were included in the following analyses (n = 189 of N = 232, 81.4% retention). Bivariate associations between study variables were evaluated using Pearson’s correlation analyses. Dichotomous variables were dummy-coded before conducting the analyses. Using independent t tests, we evaluated whether negativity bias, T1 ASD symptoms, T2 PTSD symptoms, and lifetime trauma history significantly differed by gender (0 = male, 1 = female), trauma type (0 = nonassaultive, 1 = assaultive), and former psychiatric diagnosis and/or treatment (0 = no history, 1 = prior history).
To assess whether negativity bias and T1 ASD symptoms (i.e., PCL-5 total scores) explained the association between LEC-5 scores and T2 PTSD symptoms (i.e., CAPS-5 total scores), a parallel dual mediation model was conducted using the PROCESS macro (Version 3.4, 2019; Hayes, 2017) with bias-corrected bootstrapping (10,000 resamples). To examine the specificity of this path, we also examined whether the mediation model was significant if LEC-5 scores were replaced with a measure of childhood trauma (see Supplemental Materials). Continuous variables were grand mean centered. For all indirect, total, and conditional effects, 95% confidence intervals were estimated. A confidence interval that excluded the value 0 was considered statistically significant; p values are also reported.
RESULTS
Sample characteristics
Descriptive statistics and sample characteristics can be found in Table 1. Independent t tests indicated that men (n = 84) and women (n = 105) did not significantly differ regarding negativity bias, t(187) = 0.28, p = .703, d = 0.06; LEC-5 scores, t(187) = 1.24, p = .215, d = 0.18; or T2 CAPS-5 scores, t(187) = −1.40, p = .164, d = −0.21. T1 PCL-5 scores were trending higher for women (M = 30.97, SD = 19.13) than men (M = 26.00, SD = 17.70), t(187) = −1.84, p = .068, d = −0.27.
TABLE 1.
Sample characteristics and descriptive statistics
| Characteristic | % | M | SD |
|---|---|---|---|
| Age (years) | 33.63 | 10.74 | |
| Gender | |||
| Female | 55.5 | ||
| Race/ethnicity | |||
| African American/Black | 58.7 | ||
| White | 25.9 | ||
| More than one race | 6.9 | ||
| Other/unknown/not reported | 8.5 | ||
| Annual household income (USD) | |||
| $0–9,999 | 19.0 | ||
| $10–19,999 | 15.3 | ||
| $20–29,999 | 17.5 | ||
| $30–39,999 | 6.9 | ||
| $40–49,999 | 9.5 | ||
| $50–59,999 | 7.9 | ||
| $60–69,999 | 5.8 | ||
| $70–79,999 | 6.9 | ||
| $80–89,999 | < 5.0 | ||
| $90–99,999 | < 5.0 | ||
| ≥ $100,000 | < 5.0 | ||
| Mechanism of injury | |||
| Motor vehicle crash | 72.4 | ||
| Assault/altercation | 14.8 | ||
| Other | 12.8 | ||
| T1 ASD symptoms (PCL-5) | 28.8 | 18.6 | |
| T2 PTSD symptoms (CAPS-5) | 13.7 | 12.1 | |
| Trauma history (LEC-5)a | 32.2 | 17.1 | |
| Experienced (number endorsed) | 5.14 | 2.80 | |
| Witnessed (number endorsed) | 4.71 | 3.37 | |
| Learned of (number endorsed) | 7.35 | 4.36 | |
| Current depression | 9.0 | ||
| Negativity bias (Mini-BRISC) | −0.06 | 1.17 |
Note: N = 189. ASD = acute stress disorder; PTSD = posttraumatic stress disorder; LEC-5 = Life Events Checklist for DSM-5; PCL-5 = PTSD Checklist for DSM-5; CAPS-5 = Clinician-Administered PTSD Scale for DSM-5; Mini-BRISC = mini-Brief Resilience Index for Screening.
Weighted total.
There were no significant differences between trauma type (nonassaultive, n = 161, assaultive, n = 28) with regard to negativity bias, t(187) = 0.40, p = .687, d = 0.08; T1 PCL-5 score, t(187) = −1.07, p = .142, d = −0.22; LEC-5 score, t(187) = 1.69, p = .093, d = .35; or T2 CAPS-5 score, t(187) = −1.07, p = .288, d = −0.22.
Participants who indicated they had received a former psychiatric diagnosis or prior treatment for a psychiatric condition (n = 41) had significantly higher T1 PCL-5, t(187) = −3.06, p = .003, d = −0.54, and LEC-5 scores, t(187) = −2.59, p = .010, d = −0.45, compared to participants who did not endorse a previous psychiatric diagnosis or treatment. However, there was no significant difference between these two groups for negativity bias, t(187) = 1.81, p = .073, d = 0.32, or T2 CAPS-5 score, t(187) = −1.92, p = .061, d = −0.34.
Correlations between measures
Correlations between continuous study measures are provided in Table 2. Higher levels of negativity bias (i.e., negative normalized scores) were significantly correlated with higher LEC-5 scores, r(187) = −.21, p = .004; T1 PCL-5 scores, r(187) = −.62, p < .001; and T2 CAPS-5 scores, r(187) = −.44, p < .001. Higher weighted LEC-5 scores were significantly associated with higher T1 PCL-5, r(187) = .27, p < .001, and T2 CAPS-5 scores, r(187) = .17, p = .020. Finally, T1 PCL-5 scores and T2 CAPS-5 scores were significantly related, r(187) = .48, p < .001.
TABLE 2.
Correlations between study measures
| Measure | Negativity bias (Mini-BRISC) |
Trauma history (LEC-5) |
ASD symptoms (PCL-5) |
PTSD symptoms (CAPS-5) |
|---|---|---|---|---|
| Negativity bias | – | −0.21* | −0.62* | −0.44* |
| Trauma history (LEC-5) | – | 0.27* | 0.17* | |
| ASD symptoms (PCL-5) | – | 0.48* | ||
| PTSD symptoms (CAPS-5) | – |
Note: N = 189. LEC-5 = Life Events Checklist for DSM-5; PCL-5 = PTSD Checklist for DSM-5; CAPS-5 = Clinician-Administered PTSD Scale for DSM-5; Mini-BRISC = mini-Brief Resilience Index for Screening.
Mediation model
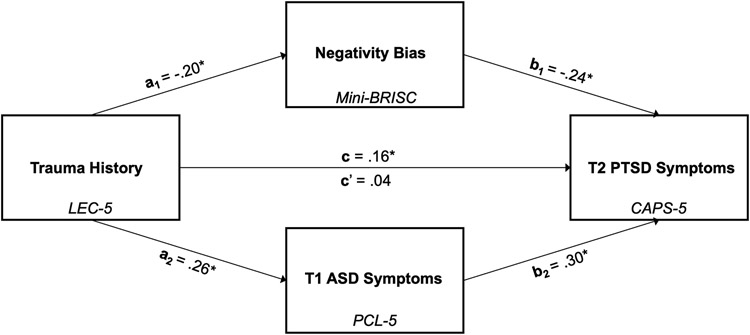
Results from the parallel mediation model (Figure 1) indicated that the effect of LEC-5 score was indirectly related to T2 PTSD symptoms through its association with negativity bias and T1 ASD symptoms. Higher LEC-5 scores predicted higher T2 CAPS-5 scores, Path c: β = .16, B = 0.11, SE = 0.05, t(187) = 2.19, p = .029, after adjusting for gender, age, and psychiatric history but before accounting for negativity bias and T1 PCL-5 scores, full model: F(4, 184) = 2.86, p = .025, R2 = .06.
FIGURE 1. The dual parallel mediating effects of negativity bias and Time (T) 1 acute stress disorder (ASD) symptoms in the association between trauma history and T2 posttraumatic stress disorder (PTSD) symptoms.
Note: All presented effects are standardized. The model was adjusted for gender, age, and former psychiatric diagnosis and/or treatment. LEC-5 = Life Events Checklist for DSM-5 (weighted score); PCL-5 = PTSD Checklist for the DSM-5; CAPS-5 = Clinician-Administered PTSD Scale for DSM-5; Mini-BRISC = mini-Brief Resilience Index for Screening.
*p < .05.
After adjusting for covariates (i.e., gender, age, and psychiatric history), higher weighted LEC-5 scores were associated with higher levels of negativity bias, Path a1: β = −.20, B = −0.01, SE = 0.01, t(187) = −2.68, p = .008; full model: F(4, 184) = 2.70, p = .032, R2 = .06, as well as higher T1 PCL-5 scores, Path a2: β = .26, B = 0.28, SE = 0.08, t(187) = 3.72, p = .003; full model: F(4, 184) = 9.11, p < .001, R2 = .17. Covariates were not associated with negativity bias, age: β = .04, B = 0.004, SE = 0.01, t(187) = 0.55, p = .582; gender: β = −.03, B = −0.08, SE = 0.17, t(187) = −0.47, p = .640; psychiatric history: β = −.09, B = −0.26, SE = 0.21, t(187) = −1.24, p = .215. However, these variables were associated with T1 PCL-5 scores, age: β = −.21, B = −0.37, SE = 0.11, t(187) = −3.14, p = .002; gender: β = .14, B = 5.17, SE = 2.56, t(187) = 2.02, p = .045; psychiatric history: β = .16, B = 7.38, SE = 3.13, t(187) = 2.36, p = .019.
Higher levels of negativity bias were subsequently related to higher T2 CAPS-5 scores Path b1: β = −.24, B = −2.43, SE = 0.84, t(187) = −2.88, p = .004; full model: F(6, 182) = 10.95, p < .001, R2 = 0.27, even after controlling for LEC-5 scores, PCL-5 scores, and covariates. Similarly, T1 PCL-5 scores were subsequently related to higher T2 CAPS-5 score, Path b2: β = .30, B = 0.20, SE = 0.06, t(187) = 3.71, p < .001, even after adjusting for LEC-5 scores, negativity bias, and covariates. After taking into account negativity bias and T1 PCL-5 scores, LEC-5 scores were no longer associated with T2 CAPS-5 scores Path c’: β = .04, B = 0.03, SE = 0.05, t(187) = 0.54, p = .587. Gender, β = .05, B = 1.32, SE = 1.58, t(187) = 0.83, p = .406;, age, β = −.01, B = −0.02, SE = 0.07, t(187) = −0.22, p = .828; and previous psychiatric history, β = .03, B = 0.83, SE = 1.94, t(187) = 0.43, p = .669, were not associated with T2 CAPS-5 scores after accounting for LEC-5, negativity bias, and T1 PCL-5 scores.
A 95% bias-corrected confidence interval based on 10,000 bootstrap samples indicated that the indirect effects of negativity bias (a1*b1), β = .05, standardized bootstrapped SE = 0.03, and T1 PCL-5 scores (a2*b2) β = .08, standardized bootstrapped SE = 0.03, were entirely above 0, standardized 95% CI [0.003, 0.106] and 95% CI [0.023, 0.149], respectively. After taking into account the mediators (i.e., negativity bias and T1 PCL-5 scores), the direct effect of LEC-5 scores on T2 CAPS-5 scores (B = 0.026, SE = 0.54) included 0, 95% CI [−0.068, 0.037].
DISCUSSION
Individuals who have experienced a higher number of adverse life events are at a heightened risk of developing PTSD following a traumatic injury (Weis et al., 2021). We tested whether negativity bias and ASD symptoms explained the association between trauma history and future PTSD symptoms after new trauma exposure. By leveraging longitudinal data and applying a simultaneous mediation model, we found that, together, both variables fully mediated the effects of LEC-5 scores on PTSD assessed 6-months postinjury, suggesting that negativity bias and ASD symptoms help drive the relation between trauma history and PTSD after experiencing a new potentially traumatic event. Notably, these results align with prior work suggesting that evaluating ASD symptoms may be useful in identifying which trauma survivors are most at risk for developing PTSD (Bryant et al., 2011). The present work holds important implications for therapeutic interventions, suggesting that although prior trauma exposure cannot be absolved, targeting negativity bias and ASD symptoms in the acute aftermath of trauma exposure may offer an opportunity to mitigate the risk of PTSD.
Maladaptive negativity bias appears to be a consistent transdiagnostic marker of symptoms of psychopathology, evidenced in subclinical and clinical levels of depression and anxiety (Gollan et al., 2016; Nusslock & Alloy, 2017; Shook et al., 2007; Watters & Williams, 2011; Williams et al., 2009). Research also suggests that negativity bias maps onto a genetic vulnerability for psychopathology (Williams et al., 2009). Indeed, negativity bias is correlated specifically with polymorphisms in serotonin transporters (i.e., 5-HTTLPR), a risk factor for PTSD (Gressier et al., 2013; Williams et al., 2009; Xie et al., 2009). Importantly, although negativity bias may reflect an underlying vulnerability for the development of psychopathology, this bias is theorized to become “activated” or further elevated following acute trauma (Fani et al., 2012). That is, a predisposition toward negative interpretations may be exacerbated in the aftermath of a new-onset traumatic event and lead to maladaptive cognitive schemas (e.g., “the world is unsafe,” “I am bad”), a characteristic of PTSD.
The theory that negativity bias can be activated or further amplified by adverse life experiences is supported in the literature; for example, Braund et al. (2019) observed an association between increased chronic stress and higher levels of negativity bias. Past trauma exposure presents substantial stress, which is linked to aberrations in the detection, evaluation, attention, and recall of events (Barry et al., 2018; Snyder et al., 2015). The behavioral effects of negativity bias may partially stem from the activation of or hyperactivity within regions of the brain responsible for regulating emotion (Petro et al. 2018). The majority of work on negativity bias and its underlying mechanisms has specifically examined attentional negativity bias (for a review, see Browning et al., 2010). Excessive stress and/or input regarding negative events may “prime” brain regions critical for emotion regulation processes for attending to negative events and perceiving neutral events more negatively. This may result in the abnormal or improper evaluation and recall of events as being more negative than they were. We extended this work to suggest that attributional negativity bias, broadly defined, partially explains why lifetime trauma exposure is a risk factor and how PTSD symptoms are maintained over time. As traumatic experiences accumulate over an individual’s lifetime, it may place them at risk of increased negativity bias, or a tendency to view the world as unsafe or negative. In turn, this may confer a higher risk of PTSD when or if they are exposed to trauma in the future. In contrast to specific tasks used to quantify attentional biases (e.g., emotional Stroop paradigms, dot-probe tasks), the current study measured attributional negativity bias with a brief self-report measure. Though we view the employment of this measure as a study strength, we also recognize the need for future research to disentangle how attentional and attributional negativity bias contribute to PTSD trajectories.
A propensity toward perceiving events and stimuli more negatively may be tackled through cognitive reappraisal, an emotion regulation strategy that can be learned (Raio et al., 2021). Indeed, previous work has suggested that using cognitive reappraisal can promote resilience to poor mental health outcomes and decrease negativity bias (Browning et al., 2010). Further, there is some evidence indicating that cognitive bias modification paradigms that focus on changing one’s interpretation of stimuli can improve anxiety symptoms or reactions to a stressor, though there is variability across the literature (Jones & Sharpe, 2017). Yet, the theoretical underpinnings of cognitive therapy suggest that cognitive vulnerabilities (e.g., attribution biases) interact with external stressors, such as trauma exposure, leading to ongoing psychopathology (Clark & Beck, 2010). Related to PTSD specifically, cognitive processing therapy (CPT; Resick et al., 2016) has strong empirical support for reducing PTSD symptoms and aims to identify and reframe erroneous beliefs related to a traumatic experience. Intervention components in CPT that challenge unhelpful beliefs can also address attributional negativity biases. Understanding how negativity bias maintains and adds to PTSD symptoms, particularly maladaptive thought processes, may aid in tailoring interventions, especially in the aftermath of acute trauma, which can help improve posttrauma outcomes.
In the current study, most participants were traumatically injured during a motor vehicle crash. As such, this research question should be tested in more diverse samples of individuals exposed to trauma with a variety of mechanisms of injury. Lifetime trauma exposure, ASD symptoms, and negativity bias were all evaluated during the same study visit. Although the LEC-5 was used to evaluate all trauma exposure that occurred before the index traumatic injury and the T1 PCL-5 probed symptoms only related to the injury, acquiring these measures at the same time may have led to bias in responses. Perhaps more importantly, however, additional work is needed to explore how attributional negativity bias contributes, both through casual and maintenance pathways, to other posttrauma outcomes, such as chronic pain and major depressive disorder (MDD). Although negativity bias has been explored in these diagnoses, no studies to date, to our knowledge, have examined all three outcomes simultaneously. In the current study, we queried only PTSS and did not include assessments of MDD symptoms or chronic pain. A hallmark of MDD is negative cognitive schemas. Indeed, both attentional and attributional negativity bias have been documented in adults with MDD (Beevers et al., 2015; Ruhe et al., 2019). Attributional negativity bias, commonly known in the chronic pain literature as negative interpretation bias, is also associated with catastrophizing pain and increased pain chronicity (Heathcote et al., 2016; Vancleef et al., 2016). Taken together, this suggests that the tested mediation model should be evaluated in a larger sample of individuals with more diverse reported trauma types and extended to include multiple posttrauma outcomes, including MDD and chronic pain.
Attributional negativity bias is an individual difference that can become activated in the aftermath of stressful or traumatic events (Clark & Beck, 2010). The combination of a propensity to view events as more negative and ASD symptoms appears to mediate the association between lifetime trauma history and future PTSD symptoms after new trauma exposure. This is a promising finding, as it suggests a mechanism by which therapeutic interventions targeting negativity bias during the acute aftermath of a traumatic event may reduce the risk of PTSD development bestowed by trauma history.
Supplementary Material
Acknowledgments
Support for the research, authorship, and/or publication of this article was provided by the National Institutes of Health (NIH; R01-M1H106574; Christine L. Larson), a Medical College of Wisconsin CTSI Pilot Award (Terri A. deRoon-Cassini) and the NIH National Center for Advancing Translational Sciences (TL1TR001437; E. Kate Webb). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
The authors extend their gratitude to the participants who generously shared their time and experiences.
Footnotes
OPEN PRACTICES STATEMENT
The analysis reported in this article was not formally preregistered. Deidentified data along with a code book are shared via the National Institutes of Mental Health Data Archive at https://nda.nih.gov/edit_collection.html?id=2297; access to the data is limited to qualified researchers. The materials used in these studies are widely publicly available.
REFERENCES
- Abramson LY, Metalsky GI, & Alloy LB (1989). Hopelessness depression: A theory-based subtype of depression. Psychological Review, 96(2), 358–372. 10.1037/0033-295X.96.2.358 [DOI] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). 10.1176/appi.books.9780890425596 [DOI] [Google Scholar]
- Barry TJ, Lenaert B, Hermans D, Raes F, & Griffith JW (2018). Meta-Analysis of the association between autobiographical memory specificity and exposure to trauma. Journal of Traumatic Stress, 31(1), 35–46. 10.1002/jts.22263 [DOI] [PubMed] [Google Scholar]
- Beck AT (1987). Cognitive models of depression. Journal of Cognitive Psychotherapy, 1(1), 5–37. [Google Scholar]
- Beevers CG, Clasen PC, Enock PM, & Schnyer DM (2015). Attention bias modification for major depressive disorder: Effects on attention bias, resting state connectivity, and symptom change. Journal of Abnormal Psychology, 124(3), 463–475. 10.1037/abn0000049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird CM, Webb EK, Schramm AT, Torres L, Larson C, & deRoon-Cassini TA (2021). Racial discrimination is associated with acute posttraumatic stress symptoms and predicts future posttraumatic stress disorder symptom severity in trauma-exposed Black adults in the United States. Journal of Traumatic Stress, 34(5), 995–1004. 10.1002/jts.22670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blevins CA, Weathers FW, Davis MT, Witte TK, & Domino JL (2015). The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and Initial Psychometric Evaluation. Journal of Traumatic Stress, 28(6), 489–498. 10.1002/jts.22059 [DOI] [PubMed] [Google Scholar]
- Brasel KJ, Deroon-Cassini T, & Bradley CT (2010). Injury severity and quality of life: Whose perspective is important? Journal of Trauma, 68(2), 263–268. 10.1097/TA.0b013e3181caa58f [DOI] [PubMed] [Google Scholar]
- Braund TA, Palmer DM, Tillman G, Hanna H, & Gordon E (2019). Increased chronic stress predicts greater emotional negativity bias and poorer social skills but not cognitive functioning in healthy adults. Anxiety, Stress, and Coping, 32(4), 399–411. 10.1080/10615806.2019.1598555 [DOI] [PubMed] [Google Scholar]
- Browning M, Holmes EA, & Harmer CJ (2010). The modification of attentional bias to emotional information: A review of the techniques, mechanisms, and relevance to emotional disorders. Cognitive, Affective, & Behavioral Neuroscience, 10(1), 8–20. 10.3758/CABN.10.1.8 [DOI] [PubMed] [Google Scholar]
- Bryant RA (2011). Acute stress disorder as a predictor of posttraumatic stress disorder: A systematic review. Journal of Clinical Psychiatry, 72(2), 233–239. 10.4088/JCP.09r05072blu [DOI] [PubMed] [Google Scholar]
- Carlson EB, Smith SR, Palmieri PA, Dalenberg C, Ruzek JI, Kimerling R, Burling TA, & Spain DA (2011). Development and validation of a brief self-report measure of trauma exposure: The Trauma History Screen. Psychological Assessment, 23(2), 463–477. 10.1037/a0022294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson ED, & Chamberlain RM (2005). Allostatic load and health disparities: A theoretical orientation. Research in Nursing & Health, 28(4), 306–315. 10.1002/nur.20084 [DOI] [PubMed] [Google Scholar]
- Carlisi CO, & Robinson OJ (2018). The role of prefrontal–subcortical circuitry in negative bias in anxiety: Translational, developmental and treatment perspectives. Brain and Neuroscience Advances, 8(2), Article 239821281877422. 10.1177/2398212818774223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark DA, & Beck AT (2010). Cognitive theory and therapy of anxiety and depression: Convergence with neurobiological findings. Trends in cognitive sciences, 14(9), 418–424. 10.1016/j.tics.2010.06.007 [DOI] [PubMed] [Google Scholar]
- deRoon-Cassini TA, Mancini AD, Rusch MD, & Bonanno GA (2010). Psychopathology and resilience following traumatic injury: A latent growth mixture model analysis. Rehabilitation Psychology, 55(1), 1–11. 10.1037/a0018601 [DOI] [PubMed] [Google Scholar]
- Ehlers A, & Clark DM (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38(4), 319–345. 10.1016/S0005-7967(99)00123-0 [DOI] [PubMed] [Google Scholar]
- Fani N, Tone EB, Phifer J, Norrholm SD, Bradley B, Ressler KJ, Kamkwalala A, & Jovanovic T (2012). Attention bias toward threat is associated with exaggerated fear expression and impaired extinction in PTSD. Psychological Medicine, 42(3), 533–543. 10.1017/S0033291711001565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frodl T, & O’Keane V (2013). How does the brain deal with cumulative stress? A review with focus on developmental stress, HPA axis function and hippocampal structure in humans. Neurobiology of Disease, 52, 24–37. 10.1016/j.nbd.2012.03.012 [DOI] [PubMed] [Google Scholar]
- Geier TJ, Hunt JC, Nelson LD, Brasel KJ, & deRoon-Cassini TA (2019). Detecting PTSD in a traumatically injured population: The diagnostic utility of the PTSD Checklist for DSM-5. Depression and Anxiety, 36(2), 170–178. 10.1002/da.22873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gollan JK, Hoxha D, Hunnicutt-Ferguson K, Norris CJ, Rosebrock L, Sankin L, & Cacioppo J (2016). Twice the negativity bias and half the positivity offset: Evaluative responses to emotional information in depression. Journal of Behavior Therapy and Experimental Psychiatry, 52, 166–170. 10.1016/j.jbtep.2015.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gressier F, Calati R, Balestri M, Marsano A, Alberti S, Antypa N, & Serretti A (2013). The 5-HTTLPR polymorphism and posttraumatic stress disorder: A meta-analysis. Journal of Traumatic Stress, 26(6), 645–653. 10.1002/jts.21855 [DOI] [PubMed] [Google Scholar]
- Hayes AF (2017). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Publications. [Google Scholar]
- Heathcote L, Koopmans M, Eccleston C, Fox E, Jacobs K, Wilkinson N, & Lau JY (2016). Negative interpretation bias and the experience of pain in adolescents. Journal of Pain, 17(9), 972–981. 10.1016/j.jpain.2016.05.009 [DOI] [PubMed] [Google Scholar]
- Irish L, Ostrowski SA, Fallon W, Spoonster E, Dulmen MV, Sledjeski EM, & Delahanty DL (2008). Trauma history characteristics and subsequent PTSD symptoms in motor vehicle accident victims. Journal of Traumatic Stress, 21(4), 377–384. 10.1002/jts.20346 [DOI] [PubMed] [Google Scholar]
- Jones EB, & Sharpe L (2017). Cognitive bias modification: A review of meta-analyses. Journal of Affective Disorders, 223, 175–183. 10.1016/j.jad.2017.07.034 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Aguilar-Gaxiola S, Alonso J, Benjet C, Bromet EJ, Cardoso G, Degenhardt L, de Girolamo G, Dinolova RV, Ferry F, Florescu S, Gureje O, Haro JM, Huang Y, Karam EG, Kawakami N, Lee S, Lepine J-P, Levinson D, … Koenen KC (2017). Trauma and PTSD in the WHO World Mental Health Surveys. European Journal of Psychotraumatology, 8(supp5), Article 1353383. 10.1080/20008198.2017.1353383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Aguilar-Gaxiola S, Alonso J, Bromet EJ, Gureje O, Karam EG, Koenen KC, Lee S, Liu H, Pennell B-E, Petukhova MV, Sampson NA, Shahly V, Stein DJ, Atwoli L, Borges G, Bunting B, de Girolamo G, Gluzman SF, … Zaslavsky AM (2018). The associations of earlier trauma exposures and history of mental disorders with PTSD after subsequent traumas. Journal of Molecular Psychiatry, 23(9), 1892–1899. 10.1038/mp.2017.194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimble M, Sripad A, Fowler R, Sobolewski S, & Fleming K (2018). Negative world views after trauma: Neurophysiological evidence for negative expectancies. Psychological Trauma: Theory, Research, Practice, and Policy, 10(5), 576–584. 10.1037/tra0000324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimble MO, & Hyatt AS (2019). Vigilance/avoidance to expected and presented stimuli in trauma survivors: An eye-tracking study. Journal of Trauma & Dissociation, 20(2), 228–241. 10.1080/15299732.2019.1572041 [DOI] [PubMed] [Google Scholar]
- Lang PJ, Bradley MM, & Cuthbert BN (1990). Emotion, attention, and the startle reflex. Psychological Review, 97(3), 377–395. 10.1037/0033-295X.97.3.377 [DOI] [PubMed] [Google Scholar]
- Liu H, Petukhova MV, Sampson NA, Aguilar-Gaxiola S, Alonso J, Andrade LH, Bromet EJ, de Girolamo G, Haro JM, Hinkov H, Kawakami N, Koenen KC, Kovess-Masfety V, Lee S, Medina-Mora ME, Navarro-Mateu F, O’Neill S, Piazza M, Posada-Villa J, … Kessler RC (2017). Association of DSM-IV posttraumatic stress disorder with traumatic experience type and history in the world health organization world mental health surveys. JAMA Psychiatry, 74(3), 270–281. 10.1001/jamapsychiatry.2016.3783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris CJ (2021). The negativity bias, revisited: Evidence from neuroscience measures and an individual differences approach. Social Neuroscience, 16(1), 68–82. 10.1080/17470919.2019.1696225 [DOI] [PubMed] [Google Scholar]
- Norris C, Larsen J, Crawford LE, & Cacioppo J (2011). Better (or worse) for some than others: Individual differences in the positivity offset and negativity bias. Journal of Research in Personality, 45(1), 100–111. 10.1016/j.jrp.2010.12.001 [DOI] [Google Scholar]
- Nusslock R, & Alloy LB (2017). Reward processing and mood-related symptoms: An RDoC and translational neuroscience perspective. Journal of Affective Disorders, 216, 3–16. 10.1016/j.jad.2017.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishith P, Mechanic MB, & Resick PA (2000). Prior interpersonal trauma: The contribution to current PTSD symptoms in female rape victims. Journal of Abnormal Psychology, 109(1), 20–25. 10.1037/0021-843X.109.1.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petro NM, Tong TT, Henley DJ, & Neta M (2018). Individual differences in valence bias: fMRI evidence of the initial negativity hypothesis. Social Cognitive and Affective Neuroscience, 13(7), 687–698. 10.1093/scan/nsy049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raio CM, Harp NR, Brown CC, & Neta M (2021). Reappraisal—but not suppression—tendencies determine negativity bias after laboratory and real-world stress exposure. Affective Science, 2(4), 455–467. 10.1007/s42761-021-00059-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Monson CM, & Chard KM (2016). Cognitive processing therapy for PTSD: A comprehensive manual. Guilford Publications. [Google Scholar]
- Rothbaum BO, Kearns MC, Reiser E, Davis JS, Kerley KA, Rothbaum AO, Mercer KB, Price M, Houry D, & Ressler KJ (2014). Early intervention following trauma may mitigate genetic risk for PTSD in civilians: A pilot prospective emergency department study. Journal of Clinical Psychiatry, 75(12), 1380–1387. 10.4088/JCP.13m08715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe DL, Cooper NJ, Liddell BJ, Clark CR, Gordon E, & Williams LM (2007). Brain structure and function correlates of general and social cognition. Journal of Integrative Neuroscience, 6(1), 35–74. 10.1142/S021963520700143X [DOI] [PubMed] [Google Scholar]
- Ruhe HG, Mocking RJT, Figueroa CA, Seeverens PWJ, Ikani N, Tyborowska A, Browning M, Vrijsen JN, Harmer CJ, & Schene AH (2019). Emotional biases and recurrence in major depressive disorder: Results of 2.5 years follow-up of drug-free cohort vulnerable for recurrence. Frontiers in Psychiatry, 10, Article 145. 10.3389/fpsyt.2019.00145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman TE, Singer BH, Rowe JW, Horwitz RI, & McEwen BS (1997). Price of adaptation—allostatic load and its health consequences: MacArthur Studies of Successful Aging. Archives of Internal Medicine, 157(19), 2259–2268. 10.1001/archinte.1997.00440400111013 [DOI] [PubMed] [Google Scholar]
- Silverstein SM, Berten S, Olson P, Paul R, Willams LM, Cooper N, & Gordon E (2007). Development and validation of a world-wide-web-based neurocognitive assessment battery: WebNeuro. Behavior Research Methods, 39(4), 940–949. 10.3758/BF03192989 [DOI] [PubMed] [Google Scholar]
- Shook NJ, Fazio RH, & Vasey MW (2007). Negativity bias in attitude learning: A possible indicator of vulnerability to emotional disorders? Journal of Behavior Therapy and Experimental Psychiatry, 38(2), 144–155. 10.1016/j.jbtep.2006.10.005 [DOI] [PubMed] [Google Scholar]
- Snyder KP, Barry M, & Valentino RJ (2015). Cognitive impact of social stress and coping strategy throughout development. Psychopharmacology, 232(1), 185–195. 10.1007/s00213-014-3654-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suglia SF, Staudenmayer J, Cohen S, Enlow MB, Rich-Edwards JW, & Wright RJ (2010). Cumulative stress and cortisol disruption among Black and Hispanic pregnant women in an urban cohort. Psychological Trauma: Theory, Research, Practice and Policy, 2(4), 326–334. 10.1037/a0018953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watters AJ, & Williams LM (2011). Negative biases and risk for depression; integrating self-report and emotion task markers. Depression and Anxiety, 28(8), 703–718. 10.1002/da.20854 [DOI] [PubMed] [Google Scholar]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, & Keane TM (2013a). The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5). https://www.ptsd.va.gov/professional/assessment/adult-int/caps.asp [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, & Keane TM (2013b). The Life Events Checklist For DSM-5 (LEC-5). https://www.ptsd.va.gov/professional/assessment/te-measures/life_events_checklist.asp [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmier PA, Marx BP, & Schnurr PP (2013). The PTSD Checklist for DSM-5 (PCL-5). https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp [Google Scholar]
- Weathers FW, Bovin MJ, Lee DJ, Sloan DM, Schnurr PP, Kaloupek DG, Keane TM, & Marx BP (2018). The Clinician-Administered PTSD Scale for DSM–5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychological Assessment, 30(3), 383–395. 10.1037/pas0000486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb EK, Weis CN, Huggins AA, Parisi EA, Bennett KP, Miskovich T, Krukowski J, deRoon-Cassini TA, & Larson CL (2020). Neighborhood disadvantage is associated with stable deficits in neurocognitive functioning in traumatically-injured adults. Health & Place, 67, Article 102493. 10.1016/j.healthplace.2020.102493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weis CN, Webb EK, Huggins AA, Kallenbach M, Miskovich TA, Fitzgerald JM, Bennett KP, Krukowski JL, deRoon-Cassini TA, & Larson CL (2021). Stability of hippocampal subfield volumes after trauma and relationship to development of PTSD symptoms. NeuroImage, 236, Article 118076. 10.1016/j.neuroimage.2021.118076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weis CN, Webb EK, Stevens SK, Larson CL, & deRoon-Cassini TA (2022). Scoring the Life Events Checklist: Comparison of three scoring methods. Psychological Trauma, 14(4), 714–720. 10.1037/tra0001049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams LM, Cooper NJ, Wisniewski SR, Gatt JM, Koslow SH, Kulkarni J, DeVarney S, Gordon E, & John Rush A (2012). Sensitivity, specificity, and predictive power of the “Brief Risk-resilience Index for SCreening,” a brief pan-diagnostic web screen for emotional health. Brain and Behavior, 2(5), 576–589. 10.1002/brb3.76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams LM, Gatt JM, Schofield PR, Olivieri G, Peduto A, & Gordon E (2009). "Negativity bias" in risk for depression and anxiety: Brain–body fear circuitry correlates, 5-HTT-LPR and early life stress. NeuroImage, 47(3), 804–814. 10.1016/j.neuroimage.2009.05.009 [DOI] [PubMed] [Google Scholar]
- Vancleef LMG, Hanssen MM, & Peters ML (2016). Are individual levels of pain anxiety related to negative interpretation bias? An examination using an ambiguous word priming task. European Journal of Pain, 20(5), 833–844. 10.1002/ejp.809 [DOI] [PubMed] [Google Scholar]
- Xie P, Kranzler HR, Poling J, Stein MB, Anton RF, Brady K, Weiss RD, Farrer L, & Gelernter J (2009). Interactive effect of stressful life events and the serotonin transporter 5-HTTLPR genotype on posttraumatic stress disorder diagnosis in 2 independent populations. Archives of General Psychiatry, 66(11), 1201–1209. 10.1001/archgenpsychiatry.2009.153 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.