Abstract
Oxytocin is a peptide hormone that is most known for its role in reproduction. However, many effects other than reproduction have been defined. The lifetime prevalence of mental disorders is approximately 20%, and they have a significant ratio among the diseases that lead to disability. Treatment resistance may cause the mental disorder to become chronic and increase disability. With the examination of the oxytocinergic system, both the elucidation of the etiology of the diseases and their evaluation as a new treatment option have come to the fore. In various studies, it has been desired to create a more effective treatment model by measuring the level of oxytocin in psychiatric disorders, examining its receptor, and applying exogenous oxytocin in the treatment. In this review, an overview of oxytocin’s efficacy in treatment is presented by considering the relationship between psychiatric disorders and the oxytocinergic system.
Keywords: Psychiatric disorders, oxytocin, schizophrenia, resistance to treatment, autism
Abstract
Oksitosin peptid yapısında bir hormondur ve en fazla üremedeki rolü ile bilinir. Ancak üreme dışında da pek çok etkisi tanımlanmıştır. Ruhsal bozuklukların yaşam boyu yaygınlığı yaklaşık yüzde 20 oranlardadır ve yeti yitimine neden olan hastalıklar içerisinde azımsanmayacak düzeydedirler. Tedavilerde karşılaşılan direnç ruhsal bozukluğun kronikleşmesini sağlayıp yeti yitimini artırabilmektedir. Oksitosinerjik sistemin incelenmesi ile hastalıkların hem etiyolojisinin aydınlatılması hem de yeni bir tedavi seçeneği olarak değerlendirilmesi gündeme gelmiştir. Çeşitli çalışmalarda psikiyatrik bozukluklarda oksitosin düzeyinin ölçülmesi, reseptörünün incelenmesi ve tedavide eksojen oksitosin uygulanması ile daha etkin bir tedavi modeli oluşturulmak istenmiştir. Bu derlemede psikiyatrik bozukluklar ve oksitosinerjik sistem arasındaki ilişkiye yer verilerek oksitosinin tedavideki etkililiği hakkında genel bir bakış açısı sunulmaktadır.
Keywords: Psikiyatrik bozukluklar, oksitosin, şizofreni, tedaviye direnç, otizm
Introduction
Recently, neuropeptide hormones have become the focus of attention in investigating the relationships between the physiological and mental systems. One of the most studied of these peptides is the hormone oxytocin. Oxytocin functions as a hormone in the peripheral circulation and as a neurotransmitter in the central nervous system. The sensory and social effects of oxytocin on human behavior have been of interest for psychiatric disorders since its discovery. Because of these features, it has been investigated in terms of the pathophysiology and role in the treatment of various psychiatric diseases such as autism, anxiety disorders, depression, and eating disorders. Although it was found that oxytocin levels were different from those of healthy controls in many diseases such as autism, depression and schizophrenia. However, the results are not yet consistent because of method differences or insufficient sample sizes. The therapeutic use of oxytocin in many psychiatric disorders continues to be investigated. In this article, the relationship between oxytocin and psychiatric disorders will be examined and the treatment aspect will be evaluated. At the same time, it aimed to explain the inconsistent results in the literature and gain a holistic perspective.
Oxytocin Definition
Oxytocin is a peptide hormone. It is synthesized in the paraventricular and supraoptic nuclei of the magnocellular neurons of the hypothalamus. It exerts its effects through a uniform g protein-coupled oxytocin receptor. It is secreted from the posterior pituitary by childbirth, breastfeeding, and stress. Oxytocin receptors are found in many parts of the central nervous system, such as the prefrontal cortex, nucleus accumbens, lateral septum, hippocampus, amygdala, and stria terminalis. The hypothalamic-pituitary-adrenal (HPA) axis, acetylcholine, GABA, glutamate, opioid, cannabinoid, catecholamine, indoleamine, and steroid systems are related to the oxytocinergic system1.
Importance of Oxytocin
Oxytocin is mostly known for its role in reproduction. It is secreted by the contraction of the cervix during childbirth and stimulates contraction of the uterus. Thus, childbirth is facilitated. Oxytocin increases milk secretion with nipple stimulation after childbirth and supports breastfeeding. However, many effects other than reproduction have been described. Some studies affirm that oxytocin has effects in various areas such as social behaviors, attachment, empathy, psychological resilience, response to acute and chronic stress, fear response, processing of emotions and behavior, eating behavior, immunological and anti-inflammatory effects, and wound healing2. With the definition of various effects of oxytocin, its use for treating different diseases has come to the fore.
Prevalence of Psychiatric Disorders
The lifetime prevalence of psychiatric disorders varies by society, culture, and country. The lifetime prevalence of psychiatric disorders that meet the diagnostic criteria in adults worldwide was found to be 17.6 percent3.
Five of the first 20 diseases that may cause disability are psychiatric disorders. These include major depressive disorder (MDD), alcohol use disorder, schizophrenia, bipolar disorder, Alzheimer’s disease, and other dementia diseases4. Both the loss of labor and treatment resistance may lead to a serious financial burden for countries. Hence, the aim is to increase the rate of reaching remission and reduce disability with the search for new treatment options.
Difficulties in Treatments and New Treatment Search
Medical treatments for psychiatric disorders date back to the 1950s. With the discovery and use of chlorpromazine in the early 1950s, significant progress has been made in the fields of pharmacology, psychotherapy, neuromodulation, and psychosurgery. These treatment options are also effective in psychiatric disorders. However, 20%-60% of mental disorders can be unresponsive to treatments5. Despite the development of medical treatment options, treatment resistance is observed in approximately 30% of psychotic conditions such as schizophrenia6. Similarly, treatment resistance in depression can be seen at a rate of 30 percent7. The resistance encountered in the treatments can lead the psychiatric disorder to become chronic and increase disability. Therefore, the search for new treatment options is gaining importance. To increase the response to treatment, methods such as individual evaluation of the patient, choosing the appropriate treatment according to biomarkers, and determining the response to treatment are applied, apart from applying algorithmic diagnosis and treatment8. With the examination of the oxytocinergic system, both the elucidation of the etiology of the diseases and their evaluation as a treatment option have come to the fore. The social and behavioral effects of oxytocin have been defined as the increase in sociability, anxiolytic effect, reduction of fear, and anti-stress effects with intranasal oxytocin applications. Therefore, it was thought that mental disorders and the oxytocinergic system may be closely related. Thus, the etiology and treatment of psychiatric disorders have been investigated by measuring the plasma level of oxytocin, defining the oxytocin receptor, and administering exogenous oxytocin9.
Relationship Between Oxytocin and Psychiatric Diseases
Recently, biomarker studies have increased to clarify the biological basis of mental disorders. It is thought that oxytocin can also be evaluated as a biomarker of diseases10. In the oxytocin system, however, the oxytocin level and oxytocin receptor are mostly considered. Various studies have measured oxytocin levels in psychiatric disorders. At the same time, the relationship between oxytocin and the clinical manifestations of the disease is examined. Studies have shown that oxytocin levels in schizophrenic patients were lower than those in healthy controls and were inversely correlated with negative symptoms of the disease. Oxytocin levels were also found to be lower in patients with autism spectrum disorders (ASD) than in healthy controls. In addition, facial recognition and social communication skills were positively correlated with oxytocin levels. It was found that oxytocin levels were lower in patients with eating disorders than in healthy controls11. Lower oxytocin levels were found in patients with post-traumatic stress disorder (PTSD) than in healthy controls. This decrease in the oxytocin level was thought to be a biomarker of chronic stress12. Similarly, oxytocin levels were found to be lower in patients with MDD, anxiety disorder, bipolar disorder, and borderline personality disorder than in the healthy control group. A negative correlation was found between childhood trauma and oxytocin levels in patients with bipolar disorder. However, the higher level of oxytocin measured in patients with treatment-resistant depression compared with healthy controls has led to inconsistent results in the literature13. The oxytocin receptor has also been examined in terms of its relationship with psychiatric disorders. Genetic variations, epigenetic modifications, and methylation and polymorphisms in the oxytocin receptor gene may be related to the etiology of psychiatric disorders14. It has been reported that the quality of parental care, especially in childhood, is associated with rs53576 and rs2254298 oxytocin receptor gene polymorphisms, which are risk factors for depression, anxiety disorder, borderline personality disorder, and behavioral disorder15. Thus, it has been emphasized that the quality of parental care in the early period is a crucial factor in the development of mental disorders through the oxytocinergic system.
Use of Oxytocin for Treating Psychiatric Disorders
The first uses of oxytocin were for labor induction and bleeding control in the 1960s. After the modulatory effects of oxytocin in emotional, behavioral, and cognitive areas were defined, its use in mental disorders came to the fore16. The intranasal administration of oxytocin has been increased because of its higher bioavailability and blood-brain barrier crossing rates. At the same time, olfactory and trigeminal transport in the nasal region may contribute to the administration of oxytocin. The fact that intranasal administration is noninvasive and well tolerated and its side effects in children and adults are the same as those of placebo has led to the widespread use of oxytocin in practice. Studies have shown that there is no linear dose-response curve in oxytocin treatment, and this is due to the increased affinity of vasopressin to the receptors as the dose increases. It has been reported that the production of endogenous oxytocin increases with the administration of exogenous oxytocin17.
Oxytocin for Treating Schizophrenia
Schizophrenia is a mental disorder whose etiology has not yet been completely clarified. It includes positive symptoms such as delusions and hallucinations as well as negative symptoms such as affective bluntness, lack of pleasure and interest, difficulty in establishing interpersonal relationships, avoidance of social environments, and impaired social functioning. Although positive symptoms can be improved with antipsychotic treatment, negative symptoms show more complications. Resistance to treatment is a challenge in achieving remission. In some studies, oxytocin levels were found to be lower in schizophrenia patients; however, there are also some studies in which oxytocin levels are the same as those in healthy controls18. In a study conducted with clinical scales and cranial magnetic resonance imaging, follow-up was performed on 16 chronic schizophrenia patients with regular intranasal oxytocin administration for 3 months. Because of the follow-up, a decrease was found in the scores of positive and negative symptoms, especially in terms of negative scores. This reduction was inversely correlated with the gray volume of the right insula and the left cingulate cortex. In addition, an increase in verbal fluency was detected with oxytocin treatment. Clinical symptoms and cognitive functions improve with oxytocin administration in chronic schizophrenia, and this improvement may be related to the volume of the right insula and left cingulate cortex19. After 24 international unit (IU) intranasal oxytocin administration twice a day for 12 weeks with 68 patients diagnosed with schizophrenia and schizoaffective disorder, it was found that according to the positive and negative syndrome scale, the negative symptoms improved significantly in patients with schizophrenia, and better social functionality performing in the role play task was observed20. However, there are also studies reporting that clinical improvement is not achieved with oxytocin administration. In a meta-analysis of 10 randomized controlled trials investigating the clinical effects of oxytocin therapy in 344 schizophrenic patients, 40-80 IU oxytocin was administered to patients for 2-16 weeks on average, and it was reported that there was no significant improvement in symptomatology compared with the placebo group21. In the meta-analysis of variance of 10 randomized controlled studies conducted by considering the diversity of study groups, the difference in dosing, and the duration of administration, it was stated that oxytocin administration to schizophrenia patients does not provide clinically significant improvement22.
Oxytocin for Treating Mood Disorders
Oxytocin was thought to be closely related to MDD because of the lower oxytocin level in patients with MDD and those with the oxytocin receptor gene polymorphism. Simultaneously, its use for treatment in patients with MDD has come to the fore because oxytocin modulates the HPA axis and is associated with neurotransmitters such as serotonin23. However, there are conflicting results for oxytocin treatment in MDD. There are studies showing that the administration of 8 IU oxytocin in addition to escitalopram for a week reduces depressive symptoms and that the administration of 40 IU oxytocin in a single session increases neural activity in the limbic region of patients with MDD during rest. However, it was found that 24 IU of oxytocin, administered for one week in postpartum depression patients, increased the depressive symptoms24. It has been suggested that the effect of the oxytocin administered to postpartum depression patients on depressive symptoms is not significant, but it may improve their cognitions25. Lastly, there are no sufficient studies that investigate oxytocin use in bipolar disorder patients.
Oxytocin for Treating Autism Spectrum Disorders
ASD; is a heterogeneous group of neurodevelopmental syndromes with multiple genetic inheritances, characterized by limited and repetitive behavior patterns, interests, and activities, and chronic disability in social communication and interaction. After oxytocin’s effects were examined, its use for autism treatment came to the fore. ASD is the most studied field for the use of oxytocin in psychiatric disorders. The first trials of oxytocin for autism treatment were intravenous in the early 2000s. Some studies have shown that using oxytocin for the treatment of people with autism is widespread, but the results are inconsistent. In a randomized controlled study, a decrease in repetitive behaviors and an increase in eye contact fixation time were reported with 48 IU oxytocin treatment for 6 weeks in 106 adult individuals with ASD26. Again, after 4 weeks of 24 IU oxytocin administered in 40 adult patients with ASD, a decrease in repetitive behaviors and social avoidance and an increase in feeling more energetic and alive were observed compared with the placebo group. It has also been reported that this effect continued for one year after treatment27. However, in a comprehensive meta-analysis, it was stated that oxytocin administration provides a clinically insignificant improvement in repetitive behaviors, and therefore, its clinical effect may be limited28. In some studies conducted with pediatric patients with autism, it was stated that a significant social and cognitive well-being could not be achieved with oxytocin administration29. In another meta-analysis examining oxytocin levels, it was reported that oxytocin levels were lower in children with autism than in healthy controls, this difference was not observed in adolescence and adulthood, and there was no significant difference according to gender30. Thus, the first studies on oxytocin are more promising because oxytocin may be used for treating autism. However, current studies have shown that clinical improvement is not at a significant level.
Oxytocin for Treating Anxiety Disorders
After the anxiolytic effect of oxytocin was defined, its use in anxiety disorders came to the fore. In a study conducted with 40 patients with a diagnosis of social anxiety disorder, 24 IU of oxytocin was administered, and after 40 min, patients were able to perform the meeting task more easily when they entered the social environment, but the effect was limited31. In another study, it was determined that anxiety symptoms decreased after 5 days of low-dose oxytocin administration in 147 patients with anxiety disorder. In addition, a decrease in increased amygdala, insula, and prefrontal cortex activity has been observed during threats32. Based on these studies, it can be thought that a single dose of oxytocin administration has temporary effects on anxiety disorders, whereas chronic applications are more successful.
Oxytocin for Treating Post-traumatic Stress Disorder
Oxytocin therapy for PTSD was first applied to soldiers who participated in the Vietnam War, and it was suggested that it subjectively reduces re-experiencing and recalling traumatic memories. It has been suggested that it is particularly effective in extinguishing conditioned behavior. However, there are inconsistent results in these studies. Although oxytocin has relieving effect on PTSD symptoms, it has been reported that it is not clinically significant. However, it has been claimed that it can improve arousal and memory impairment when applied together with psychotherapy used in PTSD33,34.
Oxytocin for Treating Alcohol and Substance Use Disorders
When the relationship between the oxytocin system and alcohol and substance use disorders was examined, a bidirectional effect was suggested. Low oxytocin levels or oxytocin receptor gene polymorphisms increase susceptibility to alcohol and substance use disorders. In postmortem studies, oxytocin levels are lower in patients with alcohol and substance use disorders. Oxytocin has regulatory effects on the reward system, tolerance, memory, and stress responses. Oxytocin may have effects on impulsivity, reward seeking, negative affect, anxiety, and compulsive substance use, which are seen in alcohol and substance use disorders. However, there are conflicting results in clinical studies. Some studies have shown that intranasal oxytocin administration reduces the dose of lorazepam needed for detoxification, withdrawal, and craving symptoms in alcohol use disorder35. However, in a study, it was stated that the dose of oxazepam needed for detoxification with intranasal oxytocin administration of 24 IU twice a day for 3 days did not decrease compared with the placebo group36. In another study, it was found that alcohol craving and aggression were not decreased with a single dose of 40 IU oxytocin37. In oxytocin studies conducted with patients with alcohol use disorder, it can be stated that the clinical response may change with factors such as the patient’s compliance to the treatment, duration of treatment, and dose. Significant results cannot be obtained due to the shorter duration of the studies. In 42 patients with methamphetamine dependance it was reported that with 40 IU oxytocin administration for 4 weeks, the rate of craving for methamphetamine and depressive symptoms were decreased, while the level of anxiety was not different38. In another study, it was stated that a single dose of 40 IU oxytocin administration to heroin addicts reduced craving and withdrawal symptoms. Thus, oxytocin may be a promising treatment for heroin addiction39. There are more considerable results on the efficacy of oxytocin in substance use disorders, which gives hope for its use in substance use disorders.
Oxytocin for Treating Eating Disorders
The use of oxytocin in eating disorders has come to the fore because of its effects on diet choice and food intake, emotional regulation, and social cognition. The low oxytocin levels and oxytocin gene receptor polymorphism in patients with anorexia nervosa; indicate that the oxytocin system has a role in the development of eating disorders. However, this relationship could not be observed in patients with bulimia nervosa and binge eating disorder. At the same time, it has been suggested that oxytocin has an anorexigenic effect and that weight loss may occur with its use in obesity40.
There are limited studies examining the relationship between eating disorders and oxytocin. In a study conducted with patients with bulimia nervosa and binge eating disorder, it was observed that oxytocin did not have a significant effect in terms of eating behavior and stress41. In a different study conducted with patients with anorexia nervosa, it was found that eating anxiety and salivary cortisol levels, and cognitive rigidity decreased with 36 IU oxytocin treatment for 4-6 weeks42. In a meta-analysis study, it was stated that the clinical effects of oxytocin on eating disorders were not significant, but oxytocin may reduce food intake in healthy individuals43.
Oxytocin for Treating Personality Disorders
The role of oxytocin in personality disorders has been investigated. It has been noted that patients with borderline and antisocial personality disorders have low oxytocin levels and decreased oxytocin receptor gene expression. This alteration in the oxytocin system is thought to be related to childhood maltreatment, genetic-environment interaction, and plasticity44. Several studies have investigated the relationship between personality disorders and oxytocin, especially for borderline personality disorder. There are conflicting results in studies in which oxytocin treatment was used to reduce the clinical symptoms of borderline personality disorder. In one study, an increase in emotional empathy and social approach motivation was found with a single dose of 24 IU oxytocin administered to 51 patients with borderline personality disorder. In this study, a similar result was found by finding an increase in emotional empathy and social approach motivation in the healthy control group45. Thus, it can be stated that oxytocin is promising for correcting social behaviors. In another study, it was found that in oxytocin, individuals with borderline personality disorder noticed social threat cues more quickly, strengthened their avoidance behavior, and reduced impulsivity46. Although there are studies indicating the prosocial effects of oxytocin, the opposite effects have also been reported. It has been stated that confidence in patients with borderline personality disorder decreases with oxytocin administration47.
Oxytocin for Treating Chronic Pain Disorder
Chronic pain: is a symptom that is difficult to treat and manage clinically. Based on the view that oxytocin may have analgesic activity, its use for the treatment of chronic pain disorder has come to the fore and promising results have been obtained. The analgesic efficacy of oxytocin has been tested in conditions such as migraine, chronic low back pain, chronic pelvic pain, and wound pain. In one study, a reduction in pain was reported in approximately 30% of the participants with oxytocin administered to women with chronic pelvic pain, and no side effects were described48. In another study, it was reported that thermal pain decreased with oxytocin administration to patients with chronic low back pain, and this may be due to the caudate nucleus49. In a study conducted with migraine patients, it was stated that activation in the trigeminocervical region was decreased with the administration of in oxytocin. Thus, oxytocin could be used in the acute and prophylactic treatment of migraine50.
General Characteristics of the Studies
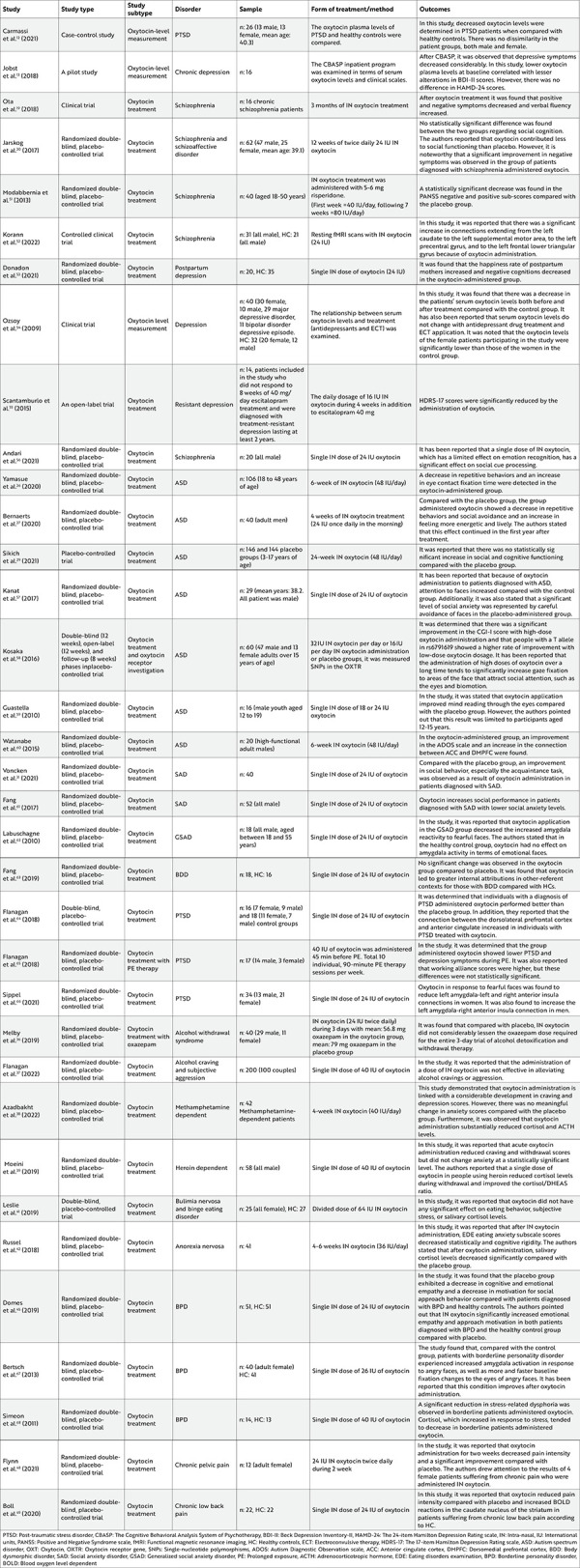
When open-label and placebo-controlled double-blind studies on the use of oxytocin for treating psychiatric disorders are examined, there are important limitations. The results obtained using different methods and measurement tools used in sample selection are inconsistent. Most studies on the use of oxytocin in treatment were conducted with patients diagnosed with PTSD, schizophrenia, and ASD. There are few studies on other psychiatric disorders. It is noteworthy that the studies have intensified, especially in recent years (2018-2021). In addition, to draw firm conclusions about the use of oxytocin for treating mental disorders, the results of short-term studies with small sample groups should be re-evaluated in randomized, placebo-controlled, long-term studies in larger study populations. The general characteristics of the open-label and double-blind, randomized, placebo-controlled studies performed so far are presented in Table 1.
Table 1. General characteristics of the studies.
Conclusion
After the effects of oxytocin, apart from its effects on reproduction, were defined, its use in psychiatric disorders came to the fore. In many disorders such as schizophrenia, ASD, mood disorders, eating disorders, and personality disorders, oxytocin levels were measured and its receptor was examined. Its use as a treatment has been tried and different results have been obtained. Although some studies have reported that the clinical response is better with treatment, there are also studies stating that it has no effect. Many factors are responsible for these inconsistent results in oxytocin studies. Age and gender differences are the most important factors. It has been stated that women in the menstrual cycle may show different oxytocin levels and responses to treatment. In addition, it was stated that childhood trauma can also determine the level of oxytocin, and this factor should be considered. The lack of standardization in the dose and duration of oxytocin therapy may also affect the response to treatment. The presence of additional medical and psychiatric disorders may also affect the oxytocin system. The explanation of many heterogeneities and factors affecting oxytocin level and response to treatment shows the limited aspects of studies. Thus, inconsistent results are obtained, and the evaluation of oxytocin’s efficacy is weakened. However, because studies with a larger sample group are conducted in autism and schizophrenia diseases in the literature, the relationship between oxytocin and diseases has been discussed in a broader framework and has given more explanatory information about its use for therapeutic purposes. Demonstration of the effect of oxytocin on stress response and social behaviors in psychiatric diseases and evidence that it can be used for therapeutic purposes show the strengths of oxytocin studies. In particular, in autism and other psychiatric diseases where medical treatment options are limited, there is a need for studies in which the oxytocin level, its relationship with clinical symptoms, and response to oxytocin treatment are evaluated and oxytocin is examined holistically. To reduce heterogeneity and evaluate the efficacy of oxytocin treatment more objectively, the holistic approach stands out in the fact that studies should be conducted with a larger number of patients, with appropriate dosage and duration. Thus, more answers can be obtained regarding oxytocin’s relationship with psychiatric diseases.
Footnotes
Ethics
Peer-review: Externally peer-reviewed.
Author Contributions
Concept: S.C.K., C.H., Design: S.C.K., C.H., Data Collection and/or Processing: S.C.K., C.H., Analysis and/or Interpretation: S.C.K., C.H., Literature Search: S.C.K., C.H., Writing: S.C.K., C.H.
Conflict of Interest: The authors have no conflict of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Jurek B, Neumann ID. The Oxytocin Receptor: From Intracellular Signaling to Behavior. Physiol Rev. 2018;98:1805–908. doi: 10.1152/physrev.00031.2017. [DOI] [PubMed] [Google Scholar]
- 2.Carter CS, Kenkel WM, MacLean EL, et al. Is Oxytocin “Nature’s Medicine”? Pharmacol Rev. 2020;72:829–61. doi: 10.1124/pr.120.019398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Steel Z, Marnane C, Iranpour C, et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980-2013. Int J Epidemiol. 2014;43:476–93. doi: 10.1093/ije/dyu038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Depression W. Other common mental disorders: global health estimates. Geneva: World Health Organization. 2017;24. [Google Scholar]
- 5.Howes OD, Thase ME, Pillinger T. Treatment resistance in psychiatry: state of the art and new directions. Mol Psychiatry. 2022;27:58–72. doi: 10.1038/s41380-021-01200-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Potkin SG, Kane JM, Correll CU, et al. The neurobiology of treatmentresistant schizophrenia: paths to antipsychotic resistance and a roadmap for future research. NPJ Schizophr. 20207;6:1. doi: 10.1038/s41537-019-0090-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kverno KS, Mangano E. Treatment-Resistant Depression: Approaches to Treatment. J Psychosoc Nurs Ment Health Serv. 2021;59:7–11. doi: 10.3928/02793695-20210816-01. [DOI] [PubMed] [Google Scholar]
- 8.Arns M, van Dijk H, Luykx JJ, van Wingen G, Olbrich S. Stratified psychiatry: Tomorrow’s precision psychiatry? Eur Neuropsychopharmacol. 2022;55:14–9. doi: 10.1016/j.euroneuro.2021.10.863. [DOI] [PubMed] [Google Scholar]
- 9.Tabak BA, Leng G, Szeto A, et al. Advances in human oxytocin measurement: challenges and proposed solutions. Mol Psychiatry. 2023;28:127–40. doi: 10.1038/s41380-022-01719-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Caicedo Mera JC, Cárdenas Molano MA, García López CC, Acevedo Triana C, Martínez Cotrina J. Discussions and perspectives regarding oxytocin as a biomarker in human investigations. Heliyon. 2021;7:e08289. doi: 10.1016/j.heliyon.2021.e08289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferreira AC, Osório FL. Peripheral oxytocin concentrations in psychiatric disorders - A systematic review and methanalysis: Further evidence. Prog Neuropsychopharmacol Biol Psychiatry. 2022;117:110561. doi: 10.1016/j.pnpbp.2022.110561. [DOI] [PubMed] [Google Scholar]
- 12.Carmassi C, Marazziti D, Mucci F, et al. Decreased Plasma Oxytocin Levels in Patients With PTSD. Front Psychol. 2021;12:612338. doi: 10.3389/fpsyg.2021.612338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jobst A, Sabaß L, Hall D, Brücklmeier B, Buchheim A, Hall J, Sarubin N, Zill P, Falkai P, Brakemeier EL, Padberg F. Oxytocin plasma levels predict the outcome of psychotherapy: A pilot study in chronic depression. J Affect Disord. 2018;227:206–13. doi: 10.1016/j.jad.2017.10.037. [DOI] [PubMed] [Google Scholar]
- 14.Wei J, Zheng H, Li G, Chen Z, Fang G, Yan J. Involvement of oxytocin receptor deficiency in psychiatric disorders and behavioral abnormalities. Front Cell Neurosci. 2023;17:1164796. doi: 10.3389/fncel.2023.1164796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cataldo I, Azhari A, Lepri B, Esposito G. Oxytocin receptors (OXTR) and early parental care: An interaction that modulates psychiatric disorders. Res Dev Disabil. 2018;82:27–38. doi: 10.1016/j.ridd.2017.10.007. [DOI] [PubMed] [Google Scholar]
- 16.Uvnäs Moberg K, Handlin L, Kendall-Tackett K, Petersson M. Oxytocin is a principal hormone that exerts part of its effects by active fragments. Med Hypotheses. 2019;133:109394. doi: 10.1016/j.mehy.2019.109394. [DOI] [PubMed] [Google Scholar]
- 17.Quintana DS, Lischke A, Grace S, Scheele D, Ma Y, Becker B. Advances in the field of intranasal oxytocin research: lessons learned and future directions for clinical research. Mol Psychiatry. 2021;26:80–91. doi: 10.1038/s41380-020-00864-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goh KK, Chen CH, Lane HY. Oxytocin in Schizophrenia: Pathophysiology and Implications for Future Treatment. Int J Mol Sci. 2021;22:2146. doi: 10.3390/ijms22042146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ota M, Yoshida S, Nakata M, Yada T, Kunugi H. The effects of adjunctive intranasal oxytocin in patients with schizophrenia. Postgrad Med. 2018;130:122–8. doi: 10.1080/00325481.2018.1398592. [DOI] [PubMed] [Google Scholar]
- 20.Jarskog LF, Pedersen CA, Johnson JL, et al. A 12-week randomized controlled trial of twice-daily intranasal oxytocin for social cognitive deficits in people with schizophrenia. Schizophr Res. 2017;185:88–95. doi: 10.1016/j.schres.2017.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zheng W, Zhu XM, Zhang QE, et al. Adjunctive intranasal oxytocin for schizophrenia: A meta-analysis of randomized, double-blind, placebo-controlled trials. Schizophr Res. 2019;206:13–20. doi: 10.1016/j.schres.2018.12.007. [DOI] [PubMed] [Google Scholar]
- 22.Martins D, Paduraru M, Paloyelis Y. Heterogeneity in response to repeated intranasal oxytocin in schizophrenia and autism spectrum disorders: A meta-analysis of variance. Br J Pharmacol. 2022;179:1525–43. doi: 10.1111/bph.15451. [DOI] [PubMed] [Google Scholar]
- 23.Jiang J, Yang M, Tian M, Chen Z, Xiao L, Gong Y. Intertwined associations between oxytocin, immune system and major depressive disorder. Biomed Pharmacother. 2023;163:114852. doi: 10.1016/j.biopha.2023.114852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kirsch P. Oxytocin in the socioemotional brain: implications for psychiatric disorders. Dialogues Clin Neurosci. 2015;17:463–76. doi: 10.31887/DCNS.2015.17.4/pkirsch. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhu J, Jin J, Tang J. Oxytocin and Women Postpartum Depression: A Systematic Review of Randomized Controlled Trials. Neuropsychiatr Dis Treat. 2023;19:939–47. doi: 10.2147/NDT.S393499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yamasue H, Okada T, Munesue T, et al. Effect of intranasal oxytocin on the core social symptoms of autism spectrum disorder: a randomized clinical trial. Mol Psychiatry. 2020;25:1849–58. doi: 10.1038/s41380-018-0097-2. [DOI] [PubMed] [Google Scholar]
- 27.Bernaerts S, Boets B, Bosmans G, Steyaert J, Alaerts K. Behavioral effects of multiple-dose oxytocin treatment in autism: a randomized, placebo-controlled trial with long-term follow-up. Mol Autism. 2020;11:6. doi: 10.1186/s13229-020-0313-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhou MS, Nasir M, Farhat LC, Kook M, Artukoglu BB, Bloch MH. Meta-analysis: Pharmacologic Treatment of Restricted and Repetitive Behaviors in Autism Spectrum Disorders. J Am Acad Child Adolesc Psychiatry. 2021;60:35–45. doi: 10.1016/j.jaac.2020.03.007. [DOI] [PubMed] [Google Scholar]
- 29.Sikich L, Kolevzon A, King BH, et al. Intranasal Oxytocin in Children and Adolescents with Autism Spectrum Disorder. N Engl J Med. 2021;385:1462–73. doi: 10.1056/NEJMoa2103583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moerkerke M, Peeters M, de Vries L, et al. Endogenous Oxytocin Levels in Autism-A Meta-Analysis. Brain Sci. 2021;11:1545. doi: 10.3390/brainsci11111545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Voncken MJ, Dijk C, Stöhr F, Niesten IJM, Schruers K, Kuypers KPC. The effect of intranasally administered oxytocin on observed social behavior in social anxiety disorder. Eur Neuropsychopharmacol. 2021;53:25–33. doi: 10.1016/j.euroneuro.2021.07.005. [DOI] [PubMed] [Google Scholar]
- 32.Kou J, Zhang Y, Zhou F, et al. Anxiolytic Effects of Chronic Intranasal Oxytocin on Neural Responses to Threat Are Dose-Frequency Dependent. Psychother Psychosom. 2022;91:253–64. doi: 10.1159/000521348. [DOI] [PubMed] [Google Scholar]
- 33.Preckel K, Trautmann S, Kanske P. Medication-Enhanced Psychotherapy for Posttraumatic Stress Disorder: Recent Findings on Oxytocin’s Involvement in the Neurobiology and Treatment of Posttraumatic Stress Disorder. Clin Psychol Eur. 2021;3:e3645. doi: 10.32872/cpe.3645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dumont GJH. Oxytocine voor de behandeling van PTSS? [Oxytocin for the treatment of PTSD?] Ned Tijdschr Geneeskd. 2021;165:D5925. [PubMed] [Google Scholar]
- 35.King CE, Gano A, Becker HC. The role of oxytocin in alcohol and drug abuse. Brain Res. 2020;1736:146761. doi: 10.1016/j.brainres.2020.146761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Melby K, Gråwe RW, Aamo TO, Salvesen Ø, Spigset O. Effect of intranasal oxytocin on alcohol withdrawal syndrome: A randomized placebo-controlled double-blind clinical trial. Drug Alcohol Depend. 2019;197:95–101. doi: 10.1016/j.drugalcdep.2019.01.003. [DOI] [PubMed] [Google Scholar]
- 37.Flanagan JC, Nietert PJ, Sippel L, et al. A randomized controlled trial examining the effects of intranasal oxytocin on alcohol craving and intimate partner aggression among couples. J Psychiatr Res. 2022;152:14–24. doi: 10.1016/j.jpsychires.2022.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Azadbakht A, Salehi M, Maracy MR, Banafshe HR. The Effects of Oxytocin on Craving, Mental Health Parameters, and Stress Hormones in Methamphetamine-Dependent Patients Undergoing Matrix Treatment Model: A Randomized, Double-Blind Clinical Trial. Eur Addict Res. 2022;28:340–9. doi: 10.1159/000525443. [DOI] [PubMed] [Google Scholar]
- 39.Moeini M, Omidi A, Sehat M, Banafshe HR. The Effects of Oxytocin on Withdrawal, Craving and Stress Response in Heroin-Dependent Patients: A Randomized, Double-Blind Clinical Trial. Eur Addict Res. 2019;25:41–7. doi: 10.1159/000496194. [DOI] [PubMed] [Google Scholar]
- 40.Plessow F, Eddy KT, Lawson EA. The Neuropeptide Hormone Oxytocin in Eating Disorders. Curr Psychiatry Rep. 2018;20:91. doi: 10.1007/s11920-018-0957-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Leslie M, Leppanen J, Paloyelis Y, Treasure J. The influence of oxytocin on eating behaviours and stress in women with bulimia nervosa and binge eating disorder. Mol Cell Endocrinol. 2019;497:110354. doi: 10.1016/j.mce.2018.12.014. [DOI] [PubMed] [Google Scholar]
- 42.Russell J, Maguire S, Hunt GE, et al. Intranasal oxytocin in the treatment of anorexia nervosa: Randomized controlled trial during re-feeding. Psychoneuroendocrinology. 2018;87:83–92. doi: 10.1016/j.psyneuen.2017.10.014. [DOI] [PubMed] [Google Scholar]
- 43.Chen CY, Chiang YC, Kuo TC, Tam KW, Loh EW. Effects of intranasal oxytocin in food intake and craving: A meta-analysis of clinical trials. Clin Nutr. 2021;40:5407–16. doi: 10.1016/j.clnu.2021.08.011. [DOI] [PubMed] [Google Scholar]
- 44.Zhang M, Liu N, Chen H, Zhang N. Oxytocin receptor gene, childhood maltreatment and borderline personality disorder features among male inmates in China. BMC Psychiatry. 2020;20:332. doi: 10.1186/s12888-020-02710-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Domes G, Ower N, von Dawans B, et al. Effects of intranasal oxytocin administration on empathy and approach motivation in women with borderline personality disorder: a randomized controlled trial. Transl Psychiatry. 2019;9:328. doi: 10.1038/s41398-019-0658-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schneider I, Boll S, Volman I, et al. Oxytocin Normalizes Approach- Avoidance Behavior in Women With Borderline Personality Disorder. Front Psychiatry. 2020;11:120. doi: 10.3389/fpsyt.2020.00120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jawad MY, Ahmad B, Hashmi AM. Role of Oxytocin in the Pathogenesis and Modulation of Borderline Personality Disorder: A Review. Cureus. 2021;13:e13190. doi: 10.7759/cureus.13190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Flynn MJ, Campbell TS, Robert M, Nasr-Esfahani M, Rash JA. Intranasal oxytocin as a treatment for chronic pelvic pain: A randomized controlled feasibility study. Int J Gynaecol Obstet. 2021;152:425–32. doi: 10.1002/ijgo.13441. [DOI] [PubMed] [Google Scholar]
- 49.Boll S, Ueltzhoeffer K, Roth C, et al. Pain-modulating effects of oxytocin in patients with chronic low back pain. Neuropharmacology. 2020;171:108105. doi: 10.1016/j.neuropharm.2020.108105. [DOI] [PubMed] [Google Scholar]
- 50.García-Boll E, Martínez-Lorenzana G, Condés-Lara M, González-Hernández A. Inhibition of nociceptive dural input to the trigeminocervical complex through oxytocinergic transmission. Exp Neurol. 2020;323:113079. doi: 10.1016/j.expneurol.2019.113079. [DOI] [PubMed] [Google Scholar]
- 51.Modabbernia A, Rezaei F, Salehi B, et al. Intranasal oxytocin as an adjunct to risperidone in patients with schizophrenia : an 8-week, randomized, double-blind, placebo-controlled study. CNS Drugs. 2013;27:57–65. doi: 10.1007/s40263-012-0022-1. [DOI] [PubMed] [Google Scholar]
- 52.Korann V, Jacob A, Lu B, et al. Effect of Intranasal Oxytocin on Resting-state Effective Connectivity in Schizophrenia. Schizophr Bull. 2022;48:1115–24. doi: 10.1093/schbul/sbac066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Donadon MF, Martin-Santos R, L Osório F. Oxytocin effects on the cognition of women with postpartum depression: A randomized, placebo-controlled clinical trial. Prog Neuropsychopharmacol Biol Psychiatry. 2021;111:110098. doi: 10.1016/j.pnpbp.2020.110098. [DOI] [PubMed] [Google Scholar]
- 54.Ozsoy S, Esel E, Kula M. Serum oxytocin levels in patients with depression and the effects of gender and antidepressant treatment. Psychiatry Res. 2009;169:249–52. doi: 10.1016/j.psychres.2008.06.034. [DOI] [PubMed] [Google Scholar]
- 55.Scantamburlo G, Hansenne M, Geenen V, Legros JJ, Ansseau M. Additional intranasal oxytocin to escitalopram improves depressive symptoms in resistant depression: an open trial. Eur Psychiatry. 2015;30:65–8. doi: 10.1016/j.eurpsy.2014.08.007. [DOI] [PubMed] [Google Scholar]
- 56.Andari E, Massa NM, Fargotstein MD, et al. Effects of Oxytocin on Emotion Recognition in Schizophrenia: A Randomized Double-Blind Pilot Study. J Clin Psychopharmacol. 2021;41:103–13. doi: 10.1097/JCP.0000000000001367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kanat M, Spenthof I, Riedel A, van Elst LT, Heinrichs M, Domes G. Restoring effects of oxytocin on the attentional preference for faces in autism. Transl Psychiatry. 2017;7:e1097. doi: 10.1038/tp.2017.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kosaka H, Okamoto Y, Munesue T, et al. Oxytocin efficacy is modulated by dosage and oxytocin receptor genotype in young adults with high-functioning autism: a 24-week randomized clinical trial. Transl Psychiatry. 2016;6:e872. doi: 10.1038/tp.2016.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Guastella AJ, Einfeld SL, Gray KM, et al. Intranasal oxytocin improves emotion recognition for youth with autism spectrum disorders. Biol Psychiatry. 2010;67:692–4. doi: 10.1016/j.biopsych.2009.09.020. [DOI] [PubMed] [Google Scholar]
- 60.Watanabe T, Kuroda M, Kuwabara H, et al. Clinical and neural effects of six-week administration of oxytocin on core symptoms of autism. Brain. 2015;138:3400–12. doi: 10.1093/brain/awv249. [DOI] [PubMed] [Google Scholar]
- 61.Fang A, Treadway MT, Hofmann SG. Working hard for oneself or others: Effects of oxytocin on reward motivation in social anxiety disorder. Biol Psychol. 2017;127:157–62. doi: 10.1016/j.biopsycho.2017.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Labuschagne I, Phan KL, Wood A, et al. Oxytocin attenuates amygdala reactivity to fear in generalized social anxiety disorder. Neuropsychopharmacology. 2010;35:2403–13. doi: 10.1038/npp.2010.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fang A, Lawson EA, Wilhelm S. Intranasal oxytocin modulates higher order social cognition in body dysmorphic disorder. Depress Anxiety. 2019;36:153–61. doi: 10.1002/da.22876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Flanagan JC, Hand A, Jarnecke AM, et al. Effects of oxytocin on working memory and executive control system connectivity in posttraumatic stress disorder. Exp Clin Psychopharmacol. 2018;26:391–402. doi: 10.1037/pha0000197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Flanagan JC, Sippel LM, Wahlquist A, Moran-Santa Maria MM, Back SE. Augmenting Prolonged Exposure therapy for PTSD with intranasal oxytocin: A randomized, placebo-controlled pilot trial. J Psychiatr Res. 2018;98:64–9. doi: 10.1016/j.jpsychires.2017.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sippel LM, Flanagan JC, Holtzheimer PE, Moran-Santa-Maria MM, Brady KT, Joseph JE. Effects of intranasal oxytocin on threat-and reward-related functional connectivity in men and women with and without childhood abuse-related PTSD. Psychiatry Res Neuroimaging. 2021;317:111368. doi: 10.1016/j.pscychresns.2021.111368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bertsch K, Gamer M, Schmidt B, et al. Oxytocin and reduction of social threat hypersensitivity in women with borderline personality disorder. Am J Psychiatry. 2013;170:1169–77. doi: 10.1176/appi.ajp.2013.13020263. [DOI] [PubMed] [Google Scholar]
- 68.Simeon D, Bartz J, Hamilton H, et al. Oxytocin administration attenuates stress reactivity in borderline personality disorder: a pilot study. Psychoneuroendocrinology. 2011;36:1418–21. doi: 10.1016/j.psyneuen.2011.03.013. [DOI] [PubMed] [Google Scholar]


