Abstract
Background:
Falls are the leading cause of injuries among older adults in the United States (US). Falls are preventable and clinicians are advised to screen for fall risk yearly. There are many falls screening tools and not all have been validated for their ability to predict future falls.
Methods:
We enrolled 1905 community-dwelling older adults into a 13-month study using a probability-based representative panel of the US population recruited from NORC at the University of Chicago’s National Frame. Respondents completed a baseline survey, 11 monthly fall calendars, and a final survey. The baseline survey included six falls screening tools (the Stay Independent, Three Key Questions (3KQ), a modified American Geriatric/British Geriatric tool, the short Falls Efficacy-1[FES-I]) and two single screening questions (“I have fallen in the past year” and “How many times did you fall in the past 12 months?”). The baseline and final survey collected demographic and health information, including falls. Sensitivity, specificity, positive and negative likelihood ratios, and corresponding 95% confidence intervals were calculated in SAS using weighted proportions.
Results:
There were 1563 respondents who completed the final survey (completion rate 82%). Sensitivity estimates ranged from 22.5% for the short FES-I to 68.7% for the 3KQ. Specificity estimates ranged from 57.9% for the 3KQ to 89.4% for the short FES-I.
Conclusions:
Falls screening tools have varying sensitivity and specificity for predicting the occurrence of a fall in the following 12 months.
Keywords: Accidental falls, Older adults, Sensitivity and specificity, Screen
1. Background
Falls are the second leading cause of fatal injuries worldwide (James et al., 2020). Almost 30% of Americans, aged 65 and older (older adults) experienced a fall, resulting in 36 million falls, and 8 million fall related injuries (Moreland et al., 2020). Falls may lead to serious injuries including hip fractures (Haddad et al., 2020). In 2015, the total medical cost attributed to falls among older adults in the United States was $50 billion and that number will rise as the number of older adults in the United States increases (Florence et al., 2018; et al., 2016; Ortman et al., 2014).
There is substantial research on fall risk factors and interventions to reduce fall risk including in special populations such as cancer patients or those with cognitive impairment (Ambrose et al., 2013; Chantanachai et al., 2021; Dautzenberg et al., 2021; Gillespie et al., 2012; Grossman & Curry, 2018; Hammouda et al., 2021; Hopewell et al., 2018; Sherrington et al., 2020; Tinetti et al., 1986; Wildes et al., 2015). The likelihood of falling increases linearly with the number of fall risk factors present (Tinetti et al., 1986). Specific risk factors, like gait and balance, can be addressed during outpatient medical visits and through referrals to other members of the care team (e.g., physical therapists) or community exercise programs (American Geriatrics Society, 2001).
Determining who would benefit from interventions starts with screening for fall risk (American Geriatrics Society, 2001; Ganz et al., 2007). There are several fall risk screening tools used among community-dwelling adults. These tools include questionnaires (Tinetti et al., 1990; Yardley et al., 2005) used alone or combined with more time intensive functional assessments (Bergquist et al., 2019; Schoene & Wu, 2013). The Centers for Disease Control and Prevention (CDC) promotes the Stay Independent, a 12-item questionnaire, shown to offer similar results as a clinical evaluation of a patient’s fall risk (Rubenstein et al., 2011), and the Three Key Questions (3KQ), based on the American and British Geriatrics Societies’ (AGS/BGS) clinical practice algorithm for preventing falls in older persons (Stevens & Phelan, 2013). Tools vary in length and how they are administered. They range from one to more than twenty questions and can be administered by a clinician or self-administered by the patient. Functional assessments are administered by a clinician and can take one to twenty minutes to complete (Palumbo et al., 2019).
Studies have reported the sensitivity and specificity of falls screening tools and functional assessments in primary and emergency care settings or using survey data (Carpenter et al., 2014; Carpenter et al., 2009; Eckstrom et al., 2017; Gates et al., 2008; Lee et al., 2013; Lohman et al., 2017; Lusardi et al., 2017; Meekes et al., 2021; Mielenz et al., 2020; Nithman & Vincenzo, 2019; Panel on Prevention of Falls in Older Persons, 2011; Perell et al., 2001) One meta-analysis examined the predictive ability of several relevant medical questions, self-reported measures, and performance-based measures. They reported that no single question or assessment had strong predictive ability on its own (Palumbo et al., 2019) Few studies have evaluated the accuracy of a modified 3KQ and the Stay Independent (Lohman et al., 2017; Mielenz et al., 2020; Nithman & Vincenzo, 2019).
The purpose of this study was to validate how well fall risk screening questionnaires that can be self-administered, predict the occurrence of a future fall among community-dwelling older adults. A future fall is defined as the occurrence of a fall in the following 12 months.
2. Methods
2.1. Study design
The study was designed as a prospective longitudinal cohort. It included a baseline survey, 11 monthly surveys to collect information on falls that occurred after completing the baseline survey, and a final survey (13 total surveys). Monthly data collection is standard for falls research (Garcia et al., 2015; Lamb, Jørstad-Stein, Hauer, & Becker, 2005; Sanders, Stuart, Scott, Kotowicz, & Nicholson, 2015) and was used to retain respondents and minimize recall bias. We calculated that a total of 1520 respondents would need to complete the final survey to detect a minimum effect size of 3.6% with 80% power, considering the survey’s estimated prevalence of falls using different screening questions/tools and the approximate 29% of fallers reported in publications (Bergen, Stevens, & Burns, 2016). Based on previous AmeriSpeak Panel surveys, we estimated that 80% of enrolled panelists would complete the study, requiring 1900 panelists at baseline.
2.2. Sample population
Community-dwelling older adults were sampled from the AmeriSpeak® Panel, a large probability-based representative panel of the US population. The AmeriSpeak panel is recruited from the NORC sample frame (https://amerispeak.norc.org). The NORC sample frame contains almost 3 million households, including over 80,000 rural households not available from the US Postal Service Delivery Sequence File (USPS DSF) but identified by direct listing by field staff. Basic demographics (e.g., age, sex, race/ethnicity) are collected for all AmeriSpeak Panel members, which allows for oversampling of targeted populations. AmeriSpeak Panel members can participate in studies online or by telephone.
The analytic sample of community-dwelling older adults was selected using 24 demographic sampling strata to account for expected differential completion rates by demographic subgroups. In addition, if a household had more than one panel member aged 65 or older, only one was randomly selected. Panelists who did not respond to the initial survey invitation (post card and email) within three weeks received a reminder email emphasizing the importance of their participation.
AmeriSpeak Panel members were eligible to be respondents in our survey if they were aged 65 and older, spoke English, and were able to pass a brief verbal memory three-word recall by correctly recalling all three words. Respondents were excluded if a member of their household was already participating in the survey.
2.3. Data collection process
Data collection began in April 2018 and ran until July 2019. Respondents were awarded points worth $5, $2, and $10 for completing the Baseline Survey, each Monthly Survey, and the Final Survey, respectively. Panelists who completed all 11 Monthly Surveys received bonus points worth $10. The greatest total amount of points a respondent could receive for participation were worth $47. Survey respondents completed the survey either via the Computer-Assisted Web Interview or Computer-Assisted Telephone Interview. If panelists had an email, they received email reminders before each monthly survey. Telephone panelists also received multiple follow-up call attempts at strategic times.
Respondents who missed a month of data collection could return to any prior month to complete the survey at any time. All respondents were asked to complete the final survey regardless of the number of monthly surveys they had completed.
Respondents were asked to designate a proxy in the event they could not be reached. Proxies would be asked to complete a short survey to assess the panelist’s reason for not responding (e.g., survey attrition, health issues, or mortality) and information about the respondents’ falls in the prior month.
2.4. Study variables
2.4.1. Fall risk screening tools
Screening tools were included in the baseline survey based on several steps. First, the Stay Independent and the 3KQ were included because they had not been evaluated for predictive accuracy at the time. Second, the AGS/BGS questions were included so we could compare how different the 3KQs performed compared to them. Third, NORC conducted a literature review and gray literature search to determine what tools/questionnaires were validated and translated for use in community settings. They identified 9 questionnaire-based tools, 25 performance-based assessment tools, and 2 quality reporting requirements that utilized 1–2 questions. Fourth, NORC contacted nine international subject matter experts for feedback on the literature review results. Subject matter experts were asked (1) if there were any other tools that were not included which they believed would be useful to include in the survey and (2) their thoughts on the nine questionnaire-based tools. They were reminded that the survey would be conducted over the phone or via a computer. Based on subject matter expert recommendations and the ability of the full tool to be conducted virtually, we included the FES-I. The single falls history questions were included based on literature supporting the importance of a fall history question (American Geriatrics Society, 2001).
The baseline survey included six fall risk screening tools or individual questions (Table 1). The additional functional assessments (Get Up and Go Test, Timed Up and Go Test, the Berg Balance Scale, the Performance Oriented Mobility Assessment) mentioned in the AGS/BGS algorithm were not included. A fall was defined as, “an event that resulted in a person unintentionally coming to rest on the ground, floor, or other lower level”.
Table 1.
Falls screening tools and questions included in baseline survey.
| Screening tool(n = number of questions) |
Question(s) | Scoring rubric |
|---|---|---|
| Three Key Questions (n = 3) | For each of the following statements, please select a yes or no answer. (1) I have fallen in the past year. (2) Sometimes I feel unsteady when I am walking. (3) I am worried about falling. |
A yes response to any question indicates fall risk. |
| Stay Independent (n = 12) | For each of the following statements, please select a yes or no answer. (1) I have fallen in the past year. (2) I use or have been advised to use a cane or walker to get around safely. (3) Sometimes I feel unsteady when I am walking. (4) I steady myself by holding onto furniture when walking at home. (5) I am worried about falling. (6) I need to push with my hands to stand up from a chair. (7) I have some trouble stepping up onto a curb. (8) I often have to rush to the toilet. (9) I have lost some feeling in my feet. (10) I take medicine that sometimes makes me feel light-headed or more tired than usual. (11) I take medicine to help me sleep or improve my mood. (12) I often feel sad or depressed. |
A yes response is worth 1 point except for questions 1 and 2 which are worth 2 points. Points are tallied and a total score of 4 or more indicates fall risk. Range 0–14 |
| American Geriatric/British Geriatric Screening Questions (n = 3) | Please answer the following questions with a number or select yes or no. (1) How many times have you fallen in the past 12 months? (2) Do you experience any issues with walking or with balance? (3) Did you seek medical care [for a fall injury]? |
Fall risk is indicated if an older adult reports having fallen two or more times in the past 12 months or if they replied yes to questions 2 or 3. |
| short Falls Efficacy Scale - International (n = 7) | For each of the following activities, please choose/tell me the response which is closest to your own opinion to show how concerned you are that you might fall if you did this activity: (1) Getting dressed or undressed (2) Taking a bath or shower (3) Getting in or out of a chair (4) Going up or down stairs (5) Reaching for something above your head or on the ground (6) Walking up or down a slope (7) Going out to a social event (e.g., religious service, family gathering, or club meeting). |
Response options for each question include: not at all concerned (1 point) somewhat concerned (2 points) fairly concerned (3 points) very concerned (4 points) Points are tallied and a total score of 14 or more indicates fall risk. Range 7–28 |
| Fell in the past year (n = 1) | (1) I have fallen in the past year. | A yes response indicates fall risk. |
| Fallen in the past 12 months (n = 1) | (1) How many times have you fallen in the past 12 months? | One or more falls indicates fall risk. |
Demographic characteristics.
Demographics included in the analysis were age, sex, race/ethnicity (White non-Hispanic, Black non-Hispanic, Hispanic, Asian non-Hispanic, and Other non-Hispanic), marital status, region of residence (Midwest, Northwest, South, West) and metropolitan status (urban, rural).
Outcomes.
In months 2–13 (with 13 being the final survey), respondents were asked to report on falls experienced in the past month. Respondents were prompted at the beginning of each survey with the definition of a fall. To indicate whether a respondent fell during the study period, a falls variable was created using the final survey. Monthly survey responses were used to prompt memory during the final survey if an older adult indicated a response incongruent with the monthly survey or if they reported not being sure if they fell.
Cognitive testing
Prior to launching the instrument, cognitive testing of the baseline survey was conducted with eight individuals to test the survey length and general comprehension of each question. These findings resulted in improvements to the baseline survey prior to the start of data collection.
2.5. Data analysis
We used descriptive analyses to describe demographics, the incidence of falls, the incidence of medically treated falls, and the percentage of respondents who screened at-risk using each tool. We performed logistic regression to calculate odds ratios for falling among those screening at-risk using each tool compared to screening not at-risk. We calculated sensitivity, specificity, positive and negative likelihood ratios, and corresponding 95% confidence intervals in SAS Enterprise Guide using the weighted proportions produced in SAS, overall and by sex and age-group.
A true positive (TP) was defined as a respondent who screened at risk for a future fall at baseline and reported one or more falls during the follow-up period. A true negative (TN) was defined as a respondent who screened not at risk for a future fall at baseline and did not report a fall during the follow-up period. A false negative (FN) was defined as a respondent who screened not at risk for a future fall at baseline but did report one or more falls during the follow-up period. A false positive (FP) was defined as a respondent who screened at risk for a future fall but did not report a fall during the follow-up period.
2.6. Sample weights
Respondents were compared to the Current Population Survey (Current Population Survey (CPS) (census.gov)) to produce weights that allowed the sample to be more representative of US older adult population based on race/Hispanic ethnicity, sex, age-group and census division, education, housing tenure and household telephone status. The falls survey sample weights also reflect the following design features from both the AmeriSpeak Panel: (a) probability of selection of the housing unit in the panel, (b) adjustments for unknown eligibility of the housing unit in the panel, (c) nonresponse associated with panel recruitment, (d) panel attrition, (e) nonresponse from eligible adults in households where at least one adult was recruited, (f) probability of selection of the falls survey sample from the panel, (g) nonresponse associated with the selected sample for the survey.
2.7. Missing data
Only respondents who completed the baseline and final survey were included in the analysis. Respondents who only partially completed the survey were contacted and prompted to complete it. All respondents had complete demographic information in order to participate in the AmeriSpeak Panel. Respondents were excluded from analysis if they did not respond to the screening questions or provide falls outcome data.
2.8. Institutional review board
This study was approved by NORC’s Institutional Review Board (IRB00000967).
3. Results
There were 1905 respondents who completed the baseline survey. For the final survey, 1563 interviews were completed. The cooperation for the monthly surveys ranged from 81.8 to 88.7% and did not differ significantly by mode of survey (data not shown). Proxy surveys were administered to those who had missed one or more surveys during survey months 4, 8, and 12. Proxy response rates ranged from 5 to 14% (data not shown) and none indicted a respondent was deceased, hospitalized, or unable to participate due to a fall (data not shown). The majority of the final sample was female (n = 820, 52.5%) aged 65–74 (n = 1066, 68.2%), White non-Hispanic (n = 1245,79.7%) and lived in a metro area (n = 1361, 87.1%) (Table 2). At baseline, 30.2% of respondents reported at least one fall in the past 12 months, compared to 47.0% during the final survey. The percentage reporting a fall did not differ significantly by survey mode (data not shown).
Table 2.
Demographic characteristics of respondents for the baseline, final, and weighted sample.
| Baseline |
Final1 |
||||
|---|---|---|---|---|---|
|
n = 1905 |
% |
n = 1563 |
% | Weighted % |
|
| Sex | |||||
| Male | 889 | 46.7 | 743 | 47.5 | 45.0 |
| Female | 1016 | 53.3 | 820 | 52.5 | 55.0 |
| Age | |||||
| 65–74 | 1266 | 66.5 | 1066 | 68.2 | 59.3 |
| 75–84 | 520 | 27.3 | 414 | 26.5 | 32.5 |
| 85+ | 119 | 6.3 | 83 | 5.3 | 8.2 |
| Race/Ethnicity | |||||
| White, non-Hispanic | 1482 | 77.8 | 1245 | 79.7 | 77.0 |
| Black, non-Hispanic | 210 | 11.0 | 154 | 9.9 | 8.9 |
| Hispanic | 106 | 5.6 | 84 | 5.4 | 8.2 |
| Asian, non-Hispanic | 25 | 1.3 | 20 | 1.3 | 0.9 |
| Other, non-Hispanic | 82 | 4.3 | 60 | 3.9 | 5.0 |
| Marital Status | |||||
| Married | 941 | 49.4 | 795 | 50.9 | 48.7 |
| Widowed | 382 | 20.1 | 282 | 18.0 | 24.1 |
| Divorced/Separated | 383 | 20.1 | 317 | 20.3 | 18.2 |
| Never married | 154 | 8.1 | 128 | 8.2 | 6.4 |
| Living with partner | 45 | 2.4 | 41 | 2.6 | 2.6 |
| Region | |||||
| Northeast | 302 | 15.9 | 243 | 15.5 | 18.6 |
| Midwest | 509 | 26.7 | 411 | 26.3 | 21.5 |
| South | 676 | 35.5 | 564 | 36.1 | 37.3 |
| West | 418 | 21.9 | 345 | 22.1 | 22.6 |
| Metropolitan Status | |||||
| Non-Metro Area | 255 | 13.4 | 202 | 12.9 | 14.6 |
| Metro Area | 1650 | 86.6 | 1361 | 87.1 | 85.4 |
| Interview mode | |||||
| Web-based | 1287 | 67.6 | 1115 | 71.3 | 62.9 |
| Telephone | 618 | 32.4 | 448 | 28.7 | 37.1 |
| Fall (Baseline) | |||||
| In past year | 561 | 29.5 | 26.3 | ||
| In past 12 months | 636 | 33.5 | 30.2 | ||
| Medically treated fall in past | 143 | 7.5 | 6.0 | ||
| Fall (Follow-up) | |||||
| I have fallen in the past year | 603 | 38.6 | 35.9 | ||
| How many times have you fallen in past 12 months2 | 766 | 49.0 | 47.0 | ||
| Medically treated fall in past year | 187 | 12.0 | 11.7 | ||
Includes all respondents who completed the final survey. Some respondents included did not complete all the monthly surveys.
When asked about the number of falls in the last 12 months, respondents were asked to refer to a memory aid (calendar) provided to them to recall prior falls they reported in the monthly surveys. The percentage reflects those who answered one or more times.
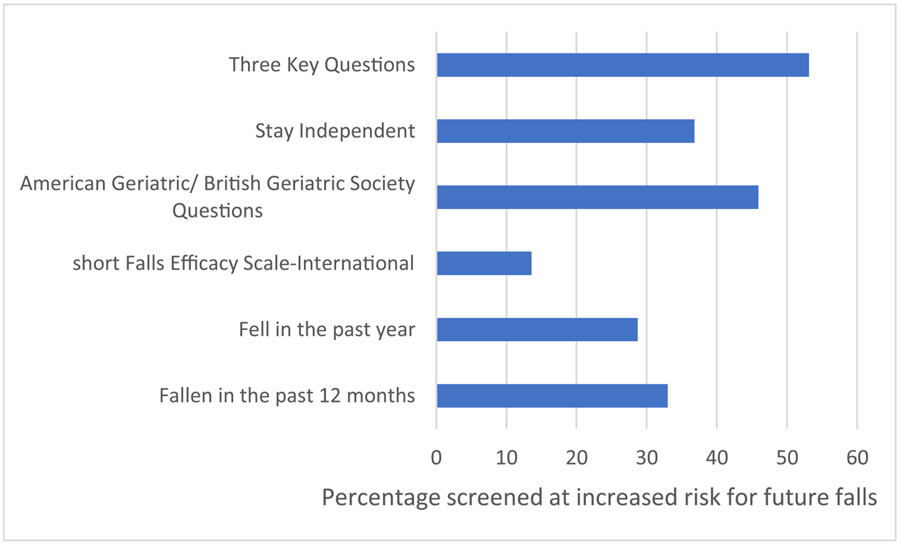
At baseline, the percentage of older adults who would be classified as at-risk for a future fall differed by screening tool. The 3KQ designated the most older adults at-risk (53.1%). The short FES-I classified the fewest number of older adults at-risk (13.6%) (Fig. 1). The percentage was also different by sex and across age-group (Table 3). More women were identified at increased risk for a future fall compared to men by every screening tool and a higher percentage of those aged 85 and older were identified as at increased risk compared to those 74–85 and 65–74.
Fig. 1.
Baseline percentage1 of older adults at increased risk for a future fall, by screening question or tool2 1Percentage is unweighted and is comprised of the 1563 respondents who completed the final survey. 2Cut-off values for screening at increased risk for future fall are described in Table 1.
Table 3.
Baseline percentage1 of older adults at increased risk for a future fall, by screening question or tool,2 by sex and age-group.
| Tool | N | % | Tool | n | % | |
|---|---|---|---|---|---|---|
| Sex | Three Key Questions | Stay Independent | ||||
| Male | 351 | 47.2 | 238 | 32.0 | ||
| Female | 479 | 58.4 | 337 | 41.1 | ||
| Age | ||||||
| 65–74 | 536 | 34.3 | 353 | 33.1 | ||
| 75–84 | 231 | 55.8 | 169 | 40.8 | ||
| 85+ | 63 | 75.9 | 53 | 63.9 | ||
| Sex | American Geriatric/ British Geriatric Society Questions | short Falls Efficacy Scale-International | ||||
| Male | 312 | 42.0 | 81 | 10.9 | ||
| Female | 405 | 49.4 | 132 | 16.1 | ||
| Age | ||||||
| 65–74 | 465 | 43.6 | 125 | 11.7 | ||
| 75–84 | 203 | 49.0 | 65 | 15.7 | ||
| 85+ | 49 | 59.0 | 23 | 27.7 | ||
| Sex | Fell in the past year | Fallen in the past 12 months | ||||
| Male | 203 | 27.3 | 237 | 31.9 | ||
| Female | 245 | 29.9 | 273 | 33.4 | ||
| Age | ||||||
| 65–74 | 291 | 27.3 | 333 | 31.2 | ||
| 75–84 | 118 | 28.5 | 133 | 32.1 | ||
| 85+ | 39 | 47.0 | 44 | 53.0 |
Percentage is unweighted and includes the 1563 respondents who completed the final survey.
Cut-off values for screening at increased risk for future fall are described in Table 1.
At baseline, screening at-risk of falls on every screening tool or question was associated with increased odds of falling during the subsequent follow-up period (Table 4). Odds ratios ranged from 3.0 time higher for the 3KQ and the AGS/BGS questions to 4.2 times higher for both “I have fallen in the past year/past 12 months” questions.
Table 4.
Association of screening positive for each fall risk questions or tools and falling during the study follow-up period 1.
| Odds Ratio |
95% Confidence Interval |
|
|---|---|---|
| Tool | ||
| Three Key Questions | 3.0 | 2.3, 4.1 |
| Stay Independent | 3.9 | 2.9, 5.3 |
| American Geriatric/British Geriatric Questions | 3.0 | 2.2, 4.0 |
| short Falls Efficacy Scale-International | 2.5 | 1.6, 3.8 |
| Fell in the past year | 4.2 | 3.1, 5.8 |
| Fallen in the past 12 months | 4.2 | 3.0, 5.7 |
Calculated using population weights.
Overall screening test sensitivity estimates ranged from 22.5% for the short FES-I to 68.7% for the 3KQ (Table 5). The 3KQ had a significantly higher sensitivity than all but the AGS/BGS questions. Positive likelihood ratios ranged from 1.6 (3KQ) to 2.9 (“I have fallen in the past year.”) (Table 3). Negative likelihood ratios ranged from 0.5 (3KQ) to 0.9 (short FES-I). Specificity estimates ranged from 57.9% for the 3KQ to 89.4% for the short FES-I (Table 5). The 3KQ had a significantly lower specificity than the questions “Did you fall in the past year,” “Did you fall in the past 12 months,” the Stay Independent, and the short FES-I. Sensitivity for most tools was higher among those aged 85+ compared to younger age groups (Table 6). The 3KQ and the Stay Independent had higher specificity when screening men for fall risk.
Table 5.
Sensitivity and specificity of fall risk questions and tools1.
| Sensitivity |
Specificity |
Positive Likelihood Ratio |
Negative Likelihood Ratio |
|||||
|---|---|---|---|---|---|---|---|---|
| % | 95% Confidence Interval |
% | 95% Confidence Interval |
% | 95% Confidence Interval |
% | 95% Confidence Interval |
|
| Tool | ||||||||
| Three Key Questions | 68.7 | 64.0, 73.4 | 57.9 | 53.2, 62.6 | 1.6 | 1.4, 2.0 | 0.5 | 0.5, 0.6 |
| Stay Independent | 55.7 | 50.7, 60.7 | 75.9 | 71.8, 79.9 | 2.3 | 1.8, 3.0 | 0.6 | 0.4, 0.8 |
| American Geriatric/British Geriatric | 60.1 | 55.1, 65.0 | 66.4 | 61.9, 70.9 | 1.8 | 1.4, 2.2 | 0.6 | 0.5, 0.7 |
| short Falls Efficacy Scale | 22.5 | 18.3, 26.7 | 89.4 | 86.5, 92.3 | 2.1 | 1.3, 3.4 | 0.9 | 0.5, 1.4 |
| Fell in the past year | 40.3 | 35.4, 45.2 | 86.2 | 82.9, 89.5 | 2.9 | 2.0, 4.2 | 0.7 | 0.5, 1.0 |
| Fallen in the past 12 months | 45.3 | 40.3, 50.3 | 83.4 | 79.8, 86.9 | 2.7 | 2.0, 3.8 | 0.7 | 0.5, 0.9 |
Calculated using population weights.
Table 6.
Sensitivity and specificity of fall risk questions and tools, by sex and age group1.
| Sensitivity |
Specificity |
Positive Likelihood Ratio |
Negative Likelihood Ratio |
||||||
|---|---|---|---|---|---|---|---|---|---|
| % | 95% Confidence Interval |
% | 95% Confidence Interval |
% | 95% Confidence Interval |
% | 95% Confidence Interval |
||
| Tool | |||||||||
| Three Key Questions | Sex | ||||||||
| Male | 64.0 | 56.6, 71.4 | 66.5 | 60.0, 73.0 | 1.9 | 1.4, 2.6 | 0.5 | 0.4, 0.7 | |
| Female | 72.2 | 66.2, 78.1 | 50.2 | 43.7, 56.8 | 1.4 | 1.2, 1.8 | 0.6 | 0.4, 0.7 | |
| Age | |||||||||
| 65–74 | 65.2 | 59.0, 71.4 | 64.2 | 58.3, 70.2 | 1.8 | 1.4, 2.4 | 0.5 | 0.4, 0.7 | |
| 75–84 | 67.8 | 59.4, 76.2 | 48.2 | 40.0, 56.4 | 1.3 | 1.0, 1.7 | 0.7 | 0.5, 0.9 | |
| 85+ | 95.5 | 88.4, 100.0 | 52.4 | 35.2, 69.6 | 2.0 | 1.2, 3.4 | 0.1 | 0.1, 0.1 | |
| Stay Independent | Sex | ||||||||
| Male | 51.1 | 43.4, 58.8 | 83.0 | 77.8, 88.2 | 3.0 | 1.9, 4.8 | 0.6 | 0.4, 0.9 | |
| Female | 59.0 | 52.5, 65.5 | 69.4 | 63.4, 75.5 | 1.9 | 1.4, 2.6 | 0.6 | 0.4, 0.8 | |
| Age | |||||||||
| 65–74 | 47.7 | 41.2, 54.2 | 78.9 | 73.8, 84.0 | 2.3 | 1.5, 3.3 | 0.7 | 0.5, 1.0 | |
| 75–84 | 61.4 | 52.6, 70.2 | 73.6 | 66.4, 80.8 | 2.3 | 1.5, 3.6 | 0.5 | 0.3, 0.8 | |
| 85+ | 89.3 | 78.8, 99.7 | 62.1 | 45.4, 78.9 | 2.4 | 1.2, 4.5 | 0.2 | 0.1, 0.3 | |
| American Geriatric/ British Geriatric | Sex | ||||||||
| Male | 56.2 | 48.6, 63.9 | 72.4 | 66.3, 78.6 | 2.0 | 1.4, 2.9 | 0.6 | 0.4, 0.9 | |
| Female | 62.9 | 56.5, 69.3 | 61.0 | 54.6, 67.4 | 1.6 | 1.2, 2.1 | 0.6 | 0.5, 0.8 | |
| Age | |||||||||
| 65–74 | 55.8 | 49.3, 62.2 | 68.3 | 62.5, 74.0 | 1.8 | 1.3, 2.4 | 0.6 | 0.5, 0.9 | |
| 75–84 | 62.4 | 53.7, 71.1 | 62.4 | 54.4, 70.3 | 1.7 | 1.2, 2.4 | 0.6 | 0.4, 0.9 | |
| 85+ | 80.8 | 67.5, 94.1 | 70.1 | 54.3, 85.9 | 2.7 | 1.3, 5.8 | 0.3 | 0.1, 0.6 | |
| short Falls Efficacy Scale | Sex | ||||||||
| Male | 16.3 | 10.6, 22.0 | 92.6 | 88.9, 96.2 | 2.2 | 1.0, 5.1 | 0.9 | 0.4, 2.1 | |
| Female | 27.1 | 21.2, 33.0 | 86.6 | 82.1, 91.0 | 2.0 | 1.2, 3.5 | 0.8 | 0.5, 1.5 | |
| Age | |||||||||
| 65–74 | 17.9 | 12.9, 22.9 | 91.6 | 88.1, 95.0 | 2.1 | 1.1, 4.2 | 0.9 | 0.5, 1.8 | |
| 75–84 | 26.0 | 18.1, 33.9 | 84.5 | 78.6, 90.4 | 1.7 | 0.9, 3.3 | 0.9 | 0.4, 1.7 | |
| 85+ | 41.0 | 24.4, 57.5 | 94.4 | 86.5, 100.0 | 7.3 | 0.9, 57.2 | 0.6 | 0.1, 4.9 | |
| Fell in the past year | Sex | ||||||||
| Male | 39.9 | 32.3, 47.5 | 86.0 | 81.2, 90.8 | 2.8 | 1.7, 4.9 | 0.7 | 0.4, 1.2 | |
| Female | 40.6 | 34.1, 47.1 | 86.4 | 81.9, 90.9 | 3.0 | 1.8, 5.0 | 0.7 | 0.4, 1.1 | |
| Age | |||||||||
| 65–74 | 40.1 | 33.8, 46.5 | 87.8 | 83.8, 91.9 | 3.3 | 2.0, 5.5 | 0.7 | 0.4, 1.1 | |
| 75–84 | 36.7 | 28.0, 45.4 | 84.9 | 79.0, 90.8 | 2.4 | 1.3, 4.6 | 0.7 | 0.4, 1.4 | |
| 85+ | 53.9 | 37.1, 70.7 | 79.2 | 65.3, 93.2 | 2.6 | 0.9, 7.3 | 0.6 | 0.2, 1.6 | |
| Fallen in the past 12 months | Sex | ||||||||
| Male | 43.8 | 36.2, 51.5 | 83.1 | 77.9, 88.2 | 2.6 | 1.6, 4.2 | 0.7 | 0.4, 1.1 | |
| Female | 46.4 | 39.7, 53.0 | 83.7 | 78.8, 88.5 | 2.8 | 1.8, 4.5 | 0.6 | 0.4, 1.0 | |
| Age | |||||||||
| 65–74 | 43.2 | 36.8, 49.7 | 85.1 | 80.7, 89.5 | 2.9 | 1.8, 4.6 | 0.7 | 0.4, 1.1 | |
| 75–84 | 43.1 | 34.2, 52.0 | 83.6 | 77.6, 89.7 | 2.6 | 1.5, 4.7 | 0.7 | 0.4, 1.2 | |
| 85+ | 67.1 | 51.2, 83.1 | 69.1 | 53.1, 85.1 | 2.2 | 1.0, 4.8 | 0.5 | 0.2, 1.1 | |
Calculated using population weights.
4. Discussion
This study evaluated how well commonly used fall risk screening questionnaires predict a future fall among community-dwelling older adults. Among the tools tested, screening at-risk at baseline was associated with a higher odds of falling during follow-up. The 3KQ and the modified AGS/BGS questions ranked highest on sensitivity and the two single questions, and the short FES-I ranked highest on specificity. However, there was minimal difference among the likelihood ratios for all questionnaires.
Variation in sensitivity and specificity was expected given the different characteristics used to assess risk. For example, both single-question tools assign risk based on whether the respondent previously fell. A prior fall is a risk factor for future falls (Ganz et al., 2007). However, neither of these single question tools consider other common risk factors. Therefore, it was expected that single question tools would result in more false negatives or lower sensitivity than tools that assess more than one fall risk factor. The 3KQ considers risk from past falls, gait and balance issues, and fear of falling. As a result, the 3KQ has a higher sensitivity but is likely to result in more false positives.
Clinicians may want to consider the age distribution of their patient population when selecting a fall risk screening tool. The prevalence of falls, falls requiring a hospitalization, and fall deaths increase with age. The sensitivity and positive likelihood ratio of most tools increased with age; in populations 85 and older, both the Stay Independent and the 3KQ had sensitivities over 89% and likelihood ratios ≥2. Therefore, a practice that serves a large population of adults 85 and older may benefit from a tool with a higher sensitivity.
Clinicians report time and competing priorities as barriers to conducting fall prevention (Howland et al., 2018; van Rhyn & Barwick, 2019, Jan) While each of the six tools studied could be self-administered electronically before a medical appointment or given to the patient to complete while waiting for their appointment, the different levels of sensitivity and specificity would impact the number of patients who require a more comprehensive fall risk assessment (e.g., comprehensive review of the patient’s medications, functional assessments). Therefore, when deciding which screening tool to use, a clinician will have to balance the additional time commitment of false positives (lower specificity) against missing a proportion of patients who are truly at-risk (lower sensitivity). Eckstrom et al. (2017), compared the Stay Independent to the 3KQ. They found 95% of patients categorized as high-risk by the Stay Independent would have also been categorized as high-risk using the 3KQ. Using the 3KQ versus the 12-question Stay Independent could potentially reduce the amount of time needed to screen. However, the higher sensitivity of the 3KQ would have resulted in 18% more patients who were screened at-risk and in need of additional fall risk assessment.
Clinicians may consider staffing in addition to time when choosing a screening tool. Fall risk screening does not need to be conducted by the physician (Carpenter, Griffey, Stark, Coopersmith, & Gage, 2011; Stevens et al., 2017). Staff at a regional healthcare system added fall risk screening questions to their nursing staff’s existing intake forms (Stevens et al., 2017). Patients aged 65 and older were automatically asked the fall screening questions at the beginning of their appointment (Stevens et al., 2017). Clinicians may also be able to delegate falls care management by working with other members of the healthcare team to assess and intervene to reduce fall risk. For instance, the Stay Independent was validated against a full clinical assessment (Rubenstein et al., 2011) so a clinician could use the responses to direct their follow-up assessments to other members of the healthcare team. For example, a physical therapist could conduct functional assessments if the patient indicates they “sometimes feel unsteady when walking.”
Any screening tool will result in some false positives and false negatives. Sensitivity and specificity are inversely related so a test may have a high sensitivity and low specificity (Trevethan, 2017). While a more accurate screening tool would be beneficial in correctly identifying those at risk and managing time and resources there is utility in using a quick tool to screen. For instance, the Geriatric Depression Scale-4 (GDS-4) which is commonly used to screen for depression in older adults, has a positive likelihood ratio of 2.6 and a negative likelihood ratio of 0.4 (Krishnamoorthy et al., 2020).
Results from this study should be interpreted with potential limitations. First, all data were based on self-report. While we collected data monthly to reduce recall bias in accordance with Prevention of Falls Network Europe (ProFaNE) recommendations (Lamb, Jørstad-Stein, Hauer, & Becker, 2005), our study population was older and memory issues may be common. To mitigate this, we screened for verbal memory issues at baseline and only included older who were able to pass a three-word recall. However, adults 85 and older had the highest percentage of loss to follow-up (30%). It is possible that some falls were missed in this age group, thus impacting the overall sensitivity and specificity among the oldest age group. We attempted to enroll proxies who could be contacted if the older adult failed to respond to three surveys in a row. However, the proxy designation was unpopular, and we were unable to confirm a designee for 75% of respondents. No proxies indicted a respondent was deceased, hospitalized or unable to participate due to a fall. Second, we were not able to evaluate the functional assessments that are associated with the AGS/BGS algorithm so our estimates for the predictiveness of that tool to predict future falls should be interpreted cautiously. Thirdly, our study may have confounders that are associated with fall risk that were not adjusted for in our estimates such as frailty; our unweighted study population was slightly younger, more likely to be white, married, and live in a metro area than the US population, which could limit generalizability. Fourth, while we found that the sensitivity and the specificity of the tools differed by sex and age-group, there were fewer adults in the age 85 and older group than others. However, it is likely that all the tools do have a higher sensitivity at older ages given the higher prevalence of falling.
Falls are common among older adults, but they can be prevented. Screening is a necessary first step. Current falls screening tools have low-moderate predictive ability, and more research is needed to determine more accurate tools. The CDC STEADI initiative (www.cdc.gov/steadi) offers guidance to clinicians who want to integrate falls screening, assessment, and intervention in their practice.
Funding
Data collection for the Test Predictability of Falls Screening Tools project was funded by a contract between NORC at the University of Chicago and the CDC under contract number HHSD2002013M53955B
We would like to thank Lieutenant Commander Erin Parker, PhD, from the Centers for Disease Control and Prevention for her contributions to the study concept and design of this project.
Footnotes
CRediT authorship contribution statement
Elizabeth R. Burns: Conceptualization, Methodology, Writing – original draft, Validation, Supervision. Robin Lee: Writing – review & editing, Supervision. Sarah E. Hodge: Methodology, Investigation, Writing – review & editing. Vicki J. Pineau: Methodology, Formal analysis, Writing – review & editing. Bess Welch: Methodology, Investigation, Writing – review & editing, Project administration. Meimeizi Zhu: Formal analysis, Investigation, Data curation, Writing – review & editing.
Declaration of Competing Interest
None of the authors have relevant financial interests, activities, relationships, or affiliations, or other potential conflicts of interest to report.
Previous presentations of the work
The protocol for this study was described during an oral symposium session at the Gerontological Society of America’s annual meeting in 2019.
References
- Ambrose AF, Paul G, & Hausdorff JM (2013). Risk factors for falls among older adults: A review of the literature. Maturitas, 75(1), 51–61. [DOI] [PubMed] [Google Scholar]
- American Geriatrics Society. (2001). British geriatrics society, and american academy of orthopaedic surgeons panel on falls prevention. Guideline for the prevention of falls in older persons. Journal of the American Geriatrics Society, 49(5), 664–672. [PubMed] [Google Scholar]
- Bergen G, Stevens MR, & Burns ER (2016). Falls and fall injuries among adults aged ≥65 years - United States, 2014. MMWR Morbidity and Mortality Weekly Report, 65(37), 993–998. [DOI] [PubMed] [Google Scholar]
- Bergquist R, Weber M, Schwenk M, et al. (2019). Performance-based clinical tests of balance and muscle strength used in young seniors: A systematic literature review. BMC Geriatrics, 19(1), 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter CR, Avidan MS, Wildes T, Stark S, Fowler SA, & Lo AX (2014). Predicting geriatric falls following an episode of emergency department care: A systematic review. Academic Emergency Medicine: Official Journal of the Society for Academic Emergency Medicine, 21(10), 1069–1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter CR, Griffey RT, Stark S, Coopersmith CM, & Gage BF (2011). Physician and nurse acceptance of technicians to screen for geriatric syndromes in the emergency department. Western Journal of Emergency Medicine, 12(4), 489–495.. kl. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter CR, Scheatzle MD, D’Antonio JA, Ricci PT, & Coben JH (2009). Identification of fall risk factors in older adult emergency department patients. Academic Emergency Medicine: Official Journal of the Society for Academic Emergency Medicine, 16(3), 211–219. [DOI] [PubMed] [Google Scholar]
- Chantanachai T, Sturnieks DL, Lord SR, Payne N, Webster L, & Taylor ME (2021). Risk factors for falls in older people with cognitive impairment living in the community: Systematic review and meta-analysis. Ageing Research Reviews, 71, Article 101452. [DOI] [PubMed] [Google Scholar]
- Dautzenberg L, Beglinger S, Tsokani S, et al. (2021). Interventions for preventing falls and fall-related fractures in community-dwelling older adults: A systematic review and network meta-analysis. Journal of The American Geriatrics Society, 69(10), 2973–2984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckstrom E, Parker EM, Lambert GH, Winkler G, Dowler D, & Casey CM (2017). Implementing STEADI in academic primary care to address older adult fall risk. Innovation in Aging, 1(2). IGx028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Florence CS, Bergen G, Atherly A, Burns E, Stevens J, & Drake C (2018). Medical costs of fatal and nonfatal falls in older adults. Journal of The American Geriatrics Society, 66(4), 693–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganz DA, Bao Y, & Shekelle PG (2007). Rubenstein LZ. Will my patient fall? JAMA, 297(1), 77–86. [DOI] [PubMed] [Google Scholar]
- Garcia PA, Dias JM, Silva SL, & Dias RC (2015). Prospective monitoring and self-report of previous falls among older women at high risk of falls and fractures: A study of comparison and agreement. Brazilian Journal of Physical Therapy, 19(3), 218–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gates S, Smith LA, Fisher JD, & Lamb SE (2008). Systematic review of accuracy of screening instruments for predicting fall risk among independently living older adults. Journal of Rehabilitation Research and Development, 45(8), 1105–1116. [PubMed] [Google Scholar]
- Gillespie LD, Robertson MC, Gillespie WJ, et al. (2012). Interventions for preventing falls in older people living in the community. The Cochrane Database of Systematic Reviews, 2012(9), Article CD007146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Preventive Services Task Force, Grossman DC, Curry SJ, et al. (2018). Interventions to prevent falls in community-dwelling older adults: US preventive services task force recommendation statement. JAMA, 319(16), 1696–1704. [DOI] [PubMed] [Google Scholar]
- Haddad YK, Shakya I, Moreland BL, Kakara R, & Bergen G (2020). Injury diagnosis and affected body part for nonfatal fall-related injuries in community-dwelling older adults treated in emergency departments. Journal of Aging and Health, 32(10), 1433–1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammouda N, Carpenter CR, Hung WW, et al. (2021). Moving the needle on fall prevention: A geriatric emergency care applied research (GEAR) network scoping review and consensus statement. Academic Emergency Medicine: Official Journal of The Society for Academic Emergency Medicine, 28(11), 1214–1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopewell S, Adedire O, Copsey BJ, et al. (2018). Multifactorial and multiple component interventions for preventing Falls In Older People living in the community. The Cochrane database of Systematic Reviews, 7(7), Article CD012221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houry D, Florence C, Baldwin G, Stevens J, & McClure R (2016). The CDC injury center’s response to the growing public health problem of falls among older adults. American Journal of Lifestyle Medicine, 10(1), 74–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howland J, Hackman H, Taylor A, O’Hara K, Liu J, & Brusch J (2018). Older adult fall prevention practices among primary care providers at accountable care organizations: A pilot study. PloS One, 13(10), Article E0205279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James SL, Lucchesi LR, Bisignano C, et al. (2020). The global burden of falls: Global, regional and national estimates of morbidity and mortality from the global burden of disease study 2017. Injury Prevention, 26(Supp 1). I3–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnamoorthy Y, Rajaa S, & Rehman T (2020). Diagnostic accuracy of various forms of geriatric depression scale for screening of depression among older adults: Systematic review and meta-analysis. Archives of Gerontology and Geriatrics, 87, Article 104002. [DOI] [PubMed] [Google Scholar]
- Lamb SE, Jørstad-Stein EC, Hauer K, Becker C, &The Prevention of Falls Network Europe Outcomes Consensus Group. (2005). Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. Journal of the American Geriatrics Society, 53(9), 1618–1622. [DOI] [PubMed] [Google Scholar]
- Lee J, Geller AI, & Strasser DC (2013). Analytical review: Focus on fall screening assessments. PM&R, 5(7), 609–621. the journal of injury, function, and rehabilitation. [DOI] [PubMed] [Google Scholar]
- Lohman MC, Crow RS, DiMilia PR, Nicklett EJ, Bruce ML, & Batsis JA (2017). Operationalisation and validation of the stopping elderly accidents, deaths, and injuries (STEADI) fall risk algorithm in a nationally representative sample. Journal of Epidemiology and Community Health, 71(12), 1191–1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lusardi MM, Fritz S, Middleton A, et al. (2017). Determining risk of falls in community dwelling older adults: a systematic review and meta-analysis using posttest probability. Journal of Geriatric Physical Therapy, 40(1), 1–36, 2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meekes WM, Korevaar JC, Leemrijse CJ, & van de Goor IA (2021). Practical and validated tool to assess falls risk in the primary care setting: A systematic review. BMJ Open, 11(9), Article E045431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mielenz TJ, Kannoth S, Jia H, et al. (2020). Evaluating a two-level vs. Three-level fall risk screening algorithm for predicting falls among older adults. Frontiers in Public Health, 8, 373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreland B, Kakara R, & Henry A (2020). Trends in Nonfatal Falls and Fall-Related Injuries Among Adults Aged ≥65 Years - United States, 2012–2018. MMWR Morbidity and Mortality Weekly Report, 69(27), 875–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nithman RW, & Vincenzo JL (2019). How steady is the STEADI? Inferential analysis of the CDC fall risk toolkit. Archives of Gerontology and Geriatrics, 83, 185–194. [DOI] [PubMed] [Google Scholar]
- Ortman J, Velkoff V, & Hogan H (2014). An aging nation: The older population in the United States. Washington, DC: US Department of Commerce, US Census Bureau. Available at: Https://www.census.gov/content/dam/Census/library/publications/2014/demo/p25-1140.pdf. [Google Scholar]
- Palumbo P, Becker C, Bandinelli S, & Chiari L (2019). Simulating the effects of a clinical guidelines screening algorithm for fall risk in community dwelling older adults. Aging Clinical and Experimental Research, 31(8), 1069–1076. 10.1007/S40520-018-1051-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panel on Prevention of Falls in Older Persons. (2011). American geriatrics society and british geriatrics society. Summary of the updated american geriatrics society/British geriatrics society clinical practice guideline for prevention of falls in older persons. Journal of The American Geriatrics Society, 59(1), 148–157. [DOI] [PubMed] [Google Scholar]
- Perell KL, Nelson A, Goldman RL, Luther SL, Prieto-Lewis N, & Rubenstein LZ (2001). Fall risk assessment measures: An analytic review. The Journals of Gerontology Series A Biological Sciences and Medical Sciences, 56(12), M761–M766. [DOI] [PubMed] [Google Scholar]
- Rubenstein LZ, Vivrette R, Harker JO, Stevens JA, & Kramer BJ (2011). Validating an evidence-based, self-rated fall risk questionnaire (FRQ) for older adults. Journal of Safety Research, 42(6), 493–499. [DOI] [PubMed] [Google Scholar]
- Sanders KM, Stuart AL, Scott D, Kotowicz MA, & Nicholson GC (2015). Validity of 12-month falls recall in community-dwelling older women participating in a clinical trial. International Journal of Endocrinology, 2015, 210527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoene D, Wu SM, et al. (2013). Discriminative ability and predictive validity of the timed up and go test in identifying older people who fall: Systematic review and meta-analysis. Journal of The American Geriatrics Society, 61(2), 202–208. [DOI] [PubMed] [Google Scholar]
- Sherrington C, Fairhall N, Kwok W, et al. (2020). Evidence on physical activity and falls prevention for people aged 65+ years: Systematic review to inform the WHO guidelines on physical activity and sedentary behaviour. The International Journal of Behavioral Nutrition and Physical Activity, 17(1), 144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens JA, & Phelan EA (2013). Development of STEADI: A fall prevention resource for health care providers. Health Promotion Practice, 14(5), 706–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens JA, Smith ML, Parker EM, Jiang L, & Floyd FD (2017). Implementing a clinically based fall prevention program. American Journal of Lifestyle Medicine, 14 (1), 71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinetti ME, Richman D, et al. (1990). Falls efficacy as a measure of fear of falling. Journal of Gerontology, 45(6), 239–243. [DOI] [PubMed] [Google Scholar]
- Tinetti ME, Williams TF, & Mayewski R (1986). Fall risk index for elderly patients based on number of chronic disabilities. The American Journal of Medicine, 80(3), 429–434. [DOI] [PubMed] [Google Scholar]
- Trevethan R, & Sensitivity, Specificity, and Predictive Values: Foundations, Pliabilities, and Pitfalls in Research and Practice. Frontiers in public health, 5, 307.. (2017). Sensitivity, Specificity, and Predictive Values: Foundations, Pliabilities, and Pitfalls in Research and Practice. Frontiers in Public Health, 5, 307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Rhyn B, & Barwick A (2019). Health practitioners’ perceptions of falls and fall prevention in older people: A metasynthesis. Qualitative Health Research, 29(1), 69–79. [DOI] [PubMed] [Google Scholar]
- Wildes TM, Dua P, Fowler SA, et al. (2015). Systematic review of falls in older adults with cancer. Journal of Geriatric Oncology, 6(1), 70–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yardley L, Beyer N, Hauer K, Kempen G, Piot-Ziegler C, & Todd C (2005). Development and initial validation of the falls efficacy scale-international (FES-I). Age and Ageing, 34(6), 614–619. [DOI] [PubMed] [Google Scholar]