Key Points
Question
What is the frequency with which children diagnosed clinically with autism spectrum disorder (ASD) at 12 to 36 months of age continue to meet criteria for ASD based on functioning at 5 to 7 years of age, and what factors are associated with ASD persistence?
Findings
Of the 213 children in this cohort study, 79 (37%) had nonpersistent ASD. Higher baseline adaptive functioning and female sex were associated with nonpersistent ASD.
Meaning
These findings suggest that an ASD diagnosis in a child younger than 3 years may not persist, and child-specific factors may be associated with persistence.
This cohort study assesses the frequency with which children diagnosed with autism spectrum disorder at 12 to 36 months of age continued to meet diagnostic criteria based on functioning at 5 to 7 years of age.
Abstract
Importance
While the prevalence of autism spectrum disorder (ASD) continues to increase and early diagnosis is emphasized, there is limited information on outcomes for children diagnosed with ASD in early childhood using contemporary diagnostic criteria.
Objectives
To determine the frequency with which children who are clinically diagnosed with ASD at 12 to 36 months of age continue to meet diagnostic criteria for ASD at 5 to 7 years of age and to evaluate whether baseline child-specific and demographic characteristics and receipt of interventions are associated with ASD persistence.
Design, Setting, and Participants
In this natural history cohort study, children who received a clinical ASD diagnosis at 12 to 36 months of age underwent a research diagnostic assessment at 5 to 7 years of age. Research assessments occurred from August 14, 2018, to January 8, 2022.
Intervention
Children received community-based interventions, and parents provided details about interventions received.
Main Outcomes and Measures
The main outcome was persistence of ASD diagnosis based on current functioning. An experienced research psychologist assigned an ASD diagnosis (present or absent) according to criteria from the Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) after the research assessment. The research assessment included administration of the Autism Diagnostic Observation Schedule–2, Autism Diagnostic Interview–Research, and a cognitive measure.
Results
Of the 213 participants diagnosed with ASD at initial clinical assessment (mean [SD] age, 24.6 [3.9] months; 177 boys [83.1%]), 79 (37.1%) did not continue to meet diagnostic criteria for ASD (nonpersistent ASD) at research assessment (mean [SD] age, 74.3 [7.1] months). All children with nonpersistent ASD had IQ of at least 70, while there was a bimodal distribution of IQ for those with persistent ASD (46 with IQ <70 and 88 with IQ ≥70). All children received some interventions, and 201 (94.4%) received ASD-specific intervention, mostly applied behavioral analysis. In a multilevel logistic regression model, the only variables associated with increased odds of being in the nonpersistent ASD group at 6 years of age were higher baseline adaptive skills (b coefficient = −0.287 [SE, 0.108]) and female sex (b = 0.239 [SE, 0.064]).
Conclusions and Relevance
The findings of this cohort study suggest that among toddlers diagnosed with ASD, baseline adaptive function and sex may be associated with persistence of ASD.
Introduction
Autism spectrum disorder (ASD), which is estimated to occur in 1 of 36 children, is defined by deficits in social communication and restrictive, repetitive behaviors.1,2 In the past decade, there has been an emphasis on diagnosing ASD early (younger than 3 years) to facilitate access to intensive behavioral interventions.3 As the age of diagnosis decreases, the number of young children living with ASD increases, leading to the need for more nuanced understanding of the expected outcomes and factors associated with outcomes.
Prior studies4,5 have shown that rates of persistence of ASD for children diagnosed at a young age range from 68% to 100%. However, limitations of prior studies include small sample sizes, varying diagnostic categories and criteria (including the outdated pervasive developmental disorder not otherwise specified vs autistic disorder), differing outcomes (categorical diagnoses vs scales to rate ASD symptoms), use of research vs clinical samples, and limited follow-up duration.4,5,6,7,8,9,10,11,12 Thus, it is uncertain whether information from prior studies of the persistence of ASD diagnoses are applicable to children from contemporary clinical populations.
Additionally, the degree to which child-specific and demographic factors are associated with persistence of ASD is uncertain. Some studies have reported that higher baseline cognitive function is associated with an increased rate of persistence of ASD, while other studies have not found this association.4,5,10,13,14,15 Similarly, studies differ on whether baseline language and adaptive skills are associated with persistence of ASD.10,11,14 Furthermore, although one large study using data from the California Department of Developmental Services reported that children with well-educated mothers had better developmental trajectories,16 other smaller studies have reported that sociodemographic factors are not associated with outcomes.5,8,11
For children younger than 3 years diagnosed with ASD, both general interventions (eg, speech therapy, occupational therapy) and ASD-specific therapies, such as applied behavioral analysis (ABA),17 Early Start Denver Model (ESDM),18 and/or others, are often recommended.19 It is generally recommended that ASD-specific interventions occur at high levels of intensity (>20 h/wk).18,20 While older studies have reported that intervention was associated with robust developmental improvements,21 newer reports, including a Cochrane review,22 suggest that behavioral interventions for young children with ASD do not consistently reduce ASD severity. Thus, the extent to which general and ASD-specific interventions are associated with ASD persistence for young children is unclear.
With the increasing prevalence of ASD and emphasis on early diagnosis, it is imperative to better understand outcomes, and factors associated with outcomes, for a contemporary sample of young children clinically diagnosed with ASD.17 The objectives of this study were to (1) determine the frequency with which children previously diagnosed with ASD through a multidisciplinary clinical assessment at 12 to 36 months of age continued to meet diagnostic criteria for ASD based on functioning at 5 to 7 years of age and (2) evaluate the extent to which factors including baseline child-specific and demographic characteristics and interventions were associated with ASD persistence.
Methods
Recruitment and Study Subjects
In this cohort study, we recruited children aged 5 years 0 months to 7 years 11 months who had previously been diagnosed with Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) (DSM-5) ASD between 12 and 36 months of age.23 The ASD diagnosis occurred via a multidisciplinary clinical assessment at one outpatient developmental-behavioral pediatric clinic in a large academic hospital. Recruitment consisted of outreach via mail, telephone calls, and in-person recruitment when possible. We excluded children who were non–English speaking, in custodial care, and/or with known genetic conditions associated with developmental outcomes (eg, Down syndrome, Fragile X syndrome, PTEN variant). The Institutional Review Board of Boston Children’s Hospital approved this study, and caregivers gave written informed consent. This cohort study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline. We analyzed comparisons between study participants and a random subset of eligible nonparticipants and found no difference by age at diagnosis, cognitive ability, language, sex, race, or income, although participants had higher adaptive and communication scores and fewer were of Hispanic ethnicity, compared with nonparticipants (eTable in Supplement 1).
Retrospective Data on Clinical Multidisciplinary ASD Diagnosis at 12 to 36 Months of Age
We abstracted medical record data from the initial clinical ASD diagnostic assessment at 12 to 36 months of age (all occurred >1 year before the COVID-19 pandemic), using a previously developed data abstraction protocol.24 Each child was seen by both a board-certified developmental-behavioral pediatrician (DBP; including E.H. and W.J.B.) and a postdoctoral level child psychologist, all of whom had clinical reliability training on the Autism Diagnostic Observation Schedule (ADOS). There were 44 different combinations of clinicians, including 12 DBPs and 11 psychologists. During the assessment, a DBP completed a detailed developmental history and obtained information from parents about the child’s behavior in naturalistic settings. The psychologist administered the Bayley Scales of Infant and Toddler Development, Third Edition (Bayley-III) and ADOS. Either the DBP or psychologist administered the Vineland Adaptive Behavior Scales, Second or Third Edition. For this study, standard scores from the Bayley-III and Vineland Adaptive Behavior Scales were abstracted from the medical records. Numeric ADOS scores from the initial clinical assessment were not in the medical records and were unavailable. All children had a DSM-5 ASD diagnosis made through a consensus team meeting with the DBP and psychologist immediately after the assessment.
Research Assessment at 5 to 7 Years of Age
The research assessment included the Autism Diagnostic Interview–Research (ADI-R),25 ADOS-2, Differential Abilities Scales–Second Edition26 or Bayley-III27 for children whose cognitive abilities precluded administration of the Differential Abilities Scales, Preschool Language Scales–Fifth Edition,28 and Vineland Adaptive Behavior Scales–Third Edition Parent Interview.29 Research psychologists (including E.H.) or supervised research assistants, all trained and research reliable in administration of the ADOS-2 and ADI-R, conducted the assessments. A research psychologist with over 20 years’ experience assessing children with ASD gave each participant an overall best estimate diagnosis of DSM-5 ASD (dichotomized to persistent ASD or nonpersistent ASD based on current functioning) using all available information, including psychometric test scores, DSM-5 diagnostic criteria, algorithm scores (ADI-R and ADOS), Vineland Adaptive Behavior Scales–Third Edition Parent Interview, and behavioral observations during testing. The psychologist assigned a 5-point ASD diagnostic certainty score (ranging from highly uncertain [1] to completely certain [5]). We conducted research assessments from August 14, 2018, to January 8, 2022, with 111 of the 213 assessments completed with the use of face masks (ADOS-2 administration and scoring are not validated using masks although procedures were as close to a standardized ADOS-2 as possible).
Demographics and Early Intervention
At the time of the research assessment, parents provided demographic data through a questionnaire completed for this study, including self-report of race and ethnicity by marking one of several provided categories, collected for descriptive purposes to provide information about the generalizability of the results of the study. Parents also reported specific type and hours per week of each intervention received from 1.5 years of age until research assessment, at 6-month intervals. Specific types of intervention recorded at each time interval were ABA, ESDM, Floortime, Social Communication/Emotional Regulation/Transactional Support (SCERTS), Relationship Developmental Intervention (RDI), speech-language therapy, physical therapy, occupational therapy, developmental specialist, and toddler playgroup. Interventions were analyzed in 3 categories: (1) total interventions, that is, all of the above-mentioned interventions; (2) ASD-specific interventions, including the ABA, ESDM, Floortime, SCERTS, and RDI; and (3) ABA alone.
Statistical Analysis
We used frequencies and descriptive statistics to describe the sample. We used independent sample 2-tailed t tests and χ2 tests when contrasting means and proportions. The study sample size allowed medium effect size difference power levels of 99.9% for t tests and greater than 95% for χ2 analyses.
We used a multilevel logistic regression model with predictive factors, including age at baseline and at research assessment, sex, maternal educational level, interventions received, and cognitive, language, and adaptive scores. The outcome variable was ASD persistence vs nonpersistence. We used a clustering variable (accounting for the 44 combinations of DBPs and psychologists who conducted the baseline assessments), and SE of estimates for the predictive factors were adjusted for the autocorrelation of observations nested within the DBP and psychologist groups. A multiple imputation procedure was implemented to account for missing data in baseline cognitive, language, and adaptive functioning (eMethods in Supplement 1).30
Power for the multilevel logistic regression model was estimated using a Monte Carlo simulation in Mplus, version 8.9 (Muthén & Muthén). We estimated power using a sample size of 200, a 2-category nominal outcome variable, a level of significance equal to 5% for a 2-tailed test and 1000 replicated samples. Differences between groups in the form of odds ratios were placed at 2.00 as indicative of an identifiable effect size. Results indicated that power ranged between 86.4% and 98.9% across replicated samples. Furthermore, coverage ranged between 93.9% and 95.1%. Ample levels of power were present when contrasting the 2 groups across independent variables. Two-sided P < .05 indicated statistical significance.
Results
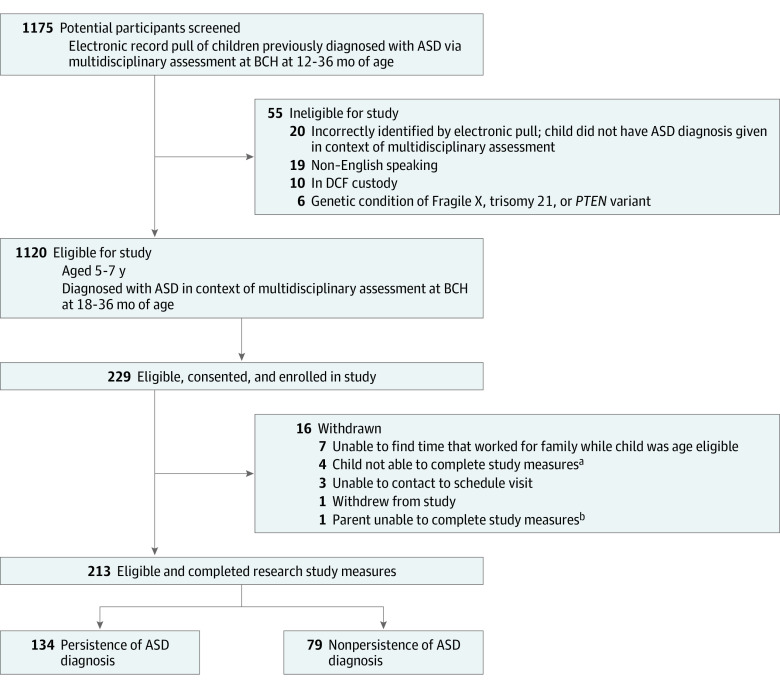
A total of 213 children (36 girls [16.9%] and 177 boys [83.1%]) clinically diagnosed with DSM-5 ASD at 12 to 36 months of age completed the research assessment at 5 to 7 years of age (Figure 1). In terms of race and ethnicity, 1 participant (0.5%) was American Indian or Alaska Native, 14 (6.6%) were Asian, 19 (8.9%) were Black, 30 (14.1%) were Hispanic or Latino, 171 (80.3%) were White, and 18 (8.5%) were of other race or ethnicity not further specified. The mean (SD) age was 24.6 (3.9) months at initial ASD diagnosis and 74.3 (7.1) months at research assessment. One hundred forty-nine children (70.0%) had private insurance, and 145 (68.1%) had maternal report of bachelor’s degree or higher level of education (Table 1). Of 191 caregivers who provided income data, 137 (71.7%) reported an income of $81 000 or greater, which is the median income in Massachusetts.31
Figure 1. Flow Diagram of the Recruitment Process.
Children were recruited from those diagnosed with autism spectrum disorder (ASD) via multidisciplinary assessment at Boston Children’s Hospital (BCH) at 12 to 36 months of age, and ultimately 213 completed research study measures. DCF indicates Department for Children and Families.
aThree children had a cognitive level of less than 13 months of age and were unable to engage in research measures; 1 child was nonadherent with testing and results were deemed to be not valid by research psychologists.
bResponses of 1 parent to the parent questionnaires were unreliable based on manual provided for survey instruments.
Table 1. Demographic and Sociodemographic Information for Total Sample and by ASD Status.
| Demographic and sociodemographic data | Diagnostic groupa | t Test or χ2 | P value | Effect size, Cohen d | ||
|---|---|---|---|---|---|---|
| All (n = 213) | Nonpersistent ASD (n = 79) | Persistent ASD (n = 134) | ||||
| Age at ASD clinical diagnosis, mo | ||||||
| Mean (SD) | 24.56 (3.85) | 25.01 (3.68) | 24.29 (3.94) | t = 1.324 | .19 | 0.19 |
| 12 to <18 | 5 (2.3) | 1 (1.3) | 4 (3.0) | χ2 = 0.653 | .72 | 0.11 |
| 18 to <24 | 81 (38.0) | 30 (38.0) | 51 (38.1) | |||
| 24-36 | 127 (59.6) | 48 (60.8) | 79 (59.0) | |||
| Age at research assessment, mean (SD), mo | 74.27 (7.10) | 73.61 (6.58) | 74.66 (7.34) | t = 1.053 | .29 | 0.15 |
| Sex | ||||||
| Girls | 36 (16.9) | 22 (27.8) | 14 (10.4) | χ2 = 10.714 | .001 | 0.46 |
| Boys | 177 (83.1) | 57 (72.2) | 120 (89.6) | |||
| Raceb | ||||||
| American Indian or Alaska Native | 1 (0.5) | 1 (1.3) | 0 | χ2 = 2.490 | .65 | NA |
| Asian | 14 (6.6) | 3 (3.8) | 11 (8.2) | |||
| Black | 19 (8.9) | 9 (11.4) | 10 (7.5) | |||
| White | 171 (80.3) | 64 (81.0) | 107 (79.9) | |||
| Other race or ethnicity not further specified | 18 (8.5) | 5 (6.3) | 13 (9.7) | |||
| Missing or prefer not to answer | 3 (1.4) | 1 (1.3) | 2 (1.5) | |||
| Ethnicity | ||||||
| Hispanic or Latino | 30 (14.1) | 10 (12.7) | 20 (14.9) | χ2 = 0.015 | .90 | 0.019 |
| Not Hispanic or Latino | 171 (80.3) | 67 (84.8) | 104 (77.6) | |||
| Prefer not to answer | 1 (0.5) | 1 (1.3) | 0 | |||
| Missing | 11 (5.2) | 1 (1.3) | 10 (7.5) | |||
| Insurance type | ||||||
| Private | 149 (70.0) | 61 (77.2) | 88 (65.7) | χ2 = 4.594 | .10 | 0.300 |
| Public | 49 (23.0) | 12 (15.2) | 37 (27.6) | |||
| Tri-Care | 11 (5.2) | 5 (6.3) | 6 (4.5) | |||
| Self-pay | 0 | 0 | 0 | |||
| Other or unknownc | 4 (1.9) | 1 (1.3) | 3 (2.2) | |||
| Premature (<37 wk) | ||||||
| No | 178 (83.6) | 64 (81.0) | 114 (85.1) | χ2 = 0.597 | .44 | 0.106 |
| Yes | 35 (16.4) | 15 (19.0) | 20 (14.9) | |||
| Maternal educational level | ||||||
| Did not attend high school | 0 | 0 | 0 | χ2 = 9.568 | .14 | NA |
| Some high school | 1 (0.5) | 1 (1.3) | 0 | |||
| High school graduate or GED | 17 (8.0) | 3 (3.8) | 14 (10.4) | |||
| Trade or vocational school | 3 (1.4) | 0 | 3 (2.2) | |||
| Associate’s degree | 18 (8.5) | 4 (5.1) | 14 (10.4) | |||
| Some college | 29 (13.6) | 10 (12.7) | 19 (14.2) | |||
| Bachelor’s degree | 68 (31.9) | 29 (36.7) | 39 (29.1) | |||
| Graduate or professional degree | 77 (36.2) | 32 (40.5) | 45 (33.6) | |||
| Prefer not to answer or missing | 0 | 0 | 0 | |||
| Annual household income | ||||||
| <$20 999 | 6 (2.8) | 3 (3.8) | 3 (2.2) | χ2 = 11.859 | .22 | NA |
| $21 000-$35 999 | 9 (4.2) | 4 (5.1) | 5 (3.7) | |||
| $36 000-$50 999 | 7 (3.3) | 4 (5.1) | 3 (2.2) | |||
| $51 000-$65 999 | 10 (4.7) | 1 (1.3) | 9 (6.7) | |||
| $66 000-$80 999 | 22 (10.3) | 9 (11.4) | 13 (9.7) | |||
| $81 000-$100 999 | 18 (8.5) | 2 (2.5) | 16 (11.9) | |||
| $101 000-$130 999 | 32 (15.0) | 13 (16.5) | 19 (14.2) | |||
| $131 000-$160 999 | 28 (13.1) | 10 (12.7) | 18 (13.4) | |||
| >$161 000 | 59 (27.7) | 26 (32.9) | 33 (24.6) | |||
| Prefer not to answer | 21 (9.9) | 7 (8.9) | 14 (10.4) | |||
| Missing | 1 (0.5) | 0 | 1 (0.7) | |||
Abbreviations: ASD, autism spectrum disorder; GED, General Educational Development; NA, not applicable.
Unless otherwise indicated, data are expressed as No. (%) of patients. Percentages have been rounded and may not total 100.
Twelve respondents reported more than 1 race. These categories were provided to the parent who then marked which of the categories best described their child.
Unknown and missing were grouped together on our survey.
ASD Persistence
Although 134 children (62.9%) continued to meet DSM-5 ASD criteria (persistent ASD), 79 (37.1%) did not (nonpersistent ASD). The research psychologist had a high level of diagnostic certainty for both children with persistent ASD (mean [SD], 4.6 [0.8]) and those with nonpersistent ASD (mean [SD], 4.3 [0.8]), although the certainty rating was statistically significantly higher for those with persistent ASD (independent samples 2-tailed t211 = 2.05; P = .02).
Baseline and Outcome Assessment Measures
At baseline clinical ASD assessment, the total sample mean (SD) Bayley-III cognitive standard score was 81.67 (14.03) and Vineland Adaptive Behavior Scales composite score was 73.52 (10.20). At research assessment, all children with nonpersistent ASD had an IQ of at least 70. In contrast, among those with persistent ASD, there was a bimodal distribution of IQ (46 with IQ <70 and 88 with IQ ≥70) (eFigure 1 in Supplement 1). Children with persistent ASD had significantly lower adaptive and language scores, compared with children with nonpersistent ASD (Table 2).
Table 2. Baseline and Outcome Functional Assessment Measures for Total Sample and by ASD Status.
| Standard scores | Diagnostic group, mean (SD) score | Statistical analysisa | Effect size, Cohen d | ||
|---|---|---|---|---|---|
| All (n = 213) | Nonpersistent ASD (n = 79) | Persistent ASD (n = 134) | |||
| Baseline clinical measures at 12-36 mo of age | |||||
| Cognitiveb | 81.67 (14.03) | 85.99 (11.39) | 79.11 (14.84) | t = 3.785 | 0.50 |
| Bayley-III Languagec | 65.49 (16.02) | 70.91 (16.47) | 62.25 (14.90) | t = 3.533 | 0.56 |
| Vineland Adaptive Behavior Scales composited | 73.52 (10.20) | 77.81 (9.77) | 71.04 (9.64) | t = 4.587 | 0.70 |
| Research-administered outcome measures at 5-7 y of age | |||||
| Cognitivee | 89.83 (26.42) | 105.22 (12.73) | 80.76 (28.18) | t = 8.657 | 1.12 |
| Score <70 | 46 | 0 | 46 | χ2 = 34.589 | 0.88 |
| Score >70 | 167 | 79 | 88 | ||
| Vineland Adaptive Behavior Scales | |||||
| Composite | 82.39 (18.34) | 94.68 (12.08) | 75.14 (17.55) | t = 9.597 | 1.24 |
| Communication | 82.27 (22.46) | 95.39 (12.55) | 74.53 (23.43) | t = 8.454 | 1.03 |
| Daily living skills | 82.78 (15.85) | 92.73 (12.50) | 76.92 (14.68) | t = 8.015 | 1.14 |
| Socialization | 85.52 (20.85) | 99.66 (10.40) | 77.18 (20.98) | t = 10.418 | 1.26 |
| Motorf | 87.11 (12.23) | 94.53 (8.84) | 82.71 (11.84) | t = 8.270 | 1.09 |
| PLS-5 standard scores | |||||
| Total languageg | 91.05 (24.35) | 108.33 (12.20) | 80.71 (23.97) | t = 11.059 | 1.36 |
| Auditory comprehensionh | 89.60 (22.40) | 105.09 (11.26) | 80.33 (22.31) | t = 10.678 | 1.31 |
| Expressive communication | 91.55 (25.12) | 108.80 (12.37) | 81.23 (25.18) | t = 10.617 | 1.29 |
Abbreviations: ASD, autism spectrum disorder; Bayley-III, Bayley Scales of Infant and Toddler Development, Third Edition; PLS-5, Preschool Language Scales–Fifth Edition.
P < .001 for all.
Two hundred eleven children completed Bayley-III Cognitive and 1 completed Differential Ability Scales (DAS) general cognitive ability at baseline clinical assessment; 1 was missing this variable.
Data were missing for 42 children.
Data were missing for 27 children.
One hundred ninety-seven children completed the DAS; for the 16 who completed Bayley-III, a developmental quotient was calculated as proxy for cognitive score. For cognitive scores at outcome, both mean (SD) and scores dichotomized to less than 70 vs 70 or greater are presented.
Data were missing for 1 child.
Data were missing for 3 children.
Data were missing for 2 children.
Interventions Received
All 213 children (100%) received at least 1 type of intervention between clinical ASD diagnosis and research assessment. Most children (201 [94.4%]) received ASD-specific interventions, as follows: ABA (n = 197); ESDM (n = 5); Floortime (n = 7); SCERTS (n = 1); and RDI (n = 1) (10 children received >1 type). The mean highest number of hours per week of total intervention was received between 12 and 18 months after ASD diagnosis. Subsequently, children with nonpersistent ASD received a mean fewer hours per week of intervention than children with persistent ASD (Figure 2). Therefore, considering that intervention is most effective when provided at younger ages, and to assess potential differences in maximal intensity of intervention following ASD diagnosis between those with persistent vs nonpersistent ASD, for each participant we used the highest number of hours per week of intervention received in any of the first three 6-month intervals after ASD diagnosis to characterize intervention receipt in the predictor model. Importantly, there was no correlation between the amount of ASD-specific early intensive behavioral intervention and income (r = 0.07 [95% CI, −0.06 to 0.21]; P = .29).
Figure 2. Mean Weekly Hours of Services Following Autism Spectrum Disorder (ASD) Diagnosis.
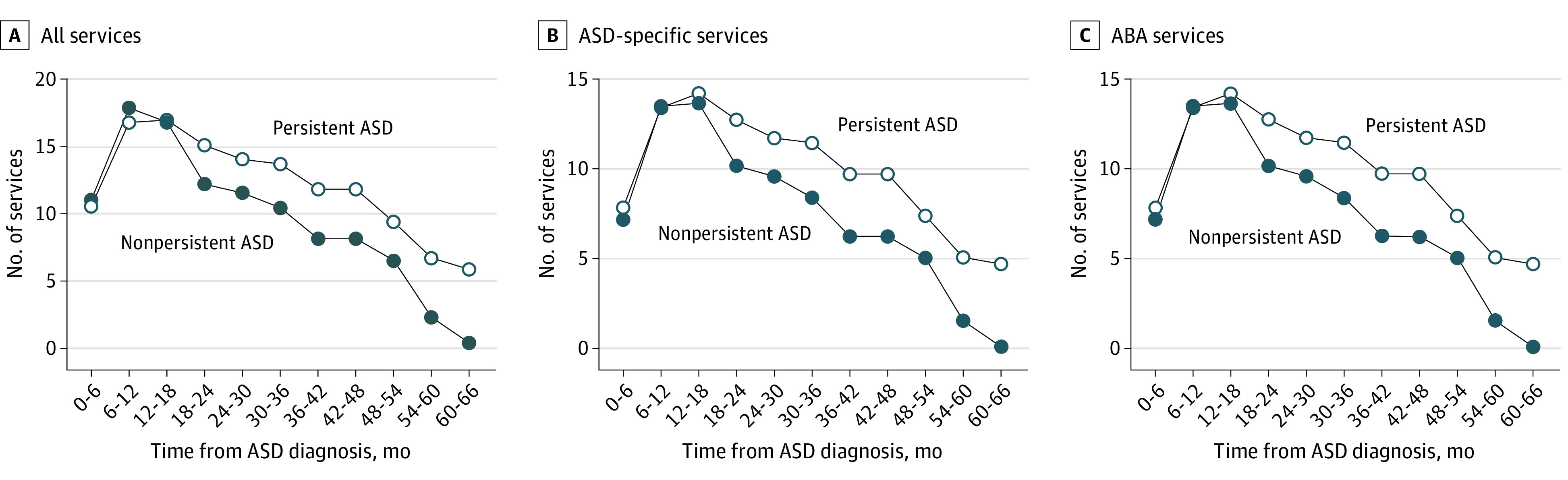
Service receipt by 6-month blocks from clinical ASD diagnosis to research assessment, separately for all services, ASD-specific services, and applied behavioral analysis (ABA) only.
Factors Associated With ASD Persistence
In a multilevel logistic regression model, children who were more likely to have nonpersistent ASD at research assessment had higher baseline adaptive skills (b coefficient = −0.287 [SE, 0.108]) and were more likely to be female (b = 0.239 [SE, 0.064]) compared with children with persistent ASD (Table 3). Among the total sample, baseline adaptive scores were less than 70 for 68 children (31.9%); 70 to 85 for 121 (56.8%); and greater than 85 for 24 (11.3%). In group-level analyses, for every 15 points higher baseline adaptive skills, the probability of having persistent ASD decreases by 20% to 26%, depending on the level of adaptive skills (notably, there was a wide 95% CI for probability of persistence in those with adaptive scores >70). For example, a child with a baseline Vineland Adaptive Behavior Scale score of 85 would have a 44.72% (95% CI, 28.52%-60.13%) likelihood of having persistent ASD, while for a child with a baseline score of 70, there would be a 70.43% (95% CI, 67.50%-71.80%) likelihood of having persistent ASD (eFigure 2 in Supplement 1 shows probabilities given baseline Vineland Adaptive Behavioral Scale scores between 60 and 100). Besides sex and adaptive scores, no other factors exceeded conventional significance levels.
Table 3. Logistic Regression Associated With Nonpersistent vs Persistent ASD.
| Predictive factors | Nonpersistent vs persistent ASD | |||
|---|---|---|---|---|
| b Coefficient (SE)a | z Test | P value | OR (95% CI) | |
| Age at clinical ASD diagnosis | −0.116 (0.069) | −1.669 | .09 | 0.94 (0.87-1.01) |
| Age at research assessment | 0.067 (0.072) | 0.930 | .35 | 1.02 (0.98-1.07) |
| Sex, male | −0.239 (0.064) | −3.756 | <.001 | 0.27 (0.13-0.53) |
| Maternal education level | −0.088 (0.077) | −1.150 | .25 | 0.89 (0.72-1.09) |
| Baseline Bayley-III cognitive standard score | 0.041 (0.120) | −0.337 | .74 | 0.99 (0.96-1.03) |
| Baseline Bayley-III language standard score | −0.081 (0.114) | −0.710 | .48 | 0.99 (0.96-1.02) |
| Baseline Vineland Adaptive Behavior Scales composite standard score | −0.287 (0.108) | −2.651 | .008 | 0.94 (0.90-0.99) |
| Insurance status | −0.029 (0.076) | −0.381 | .70 | 0.90 (0.52-1.56) |
| Receipt of total interventionsb | −0.056 (0.066) | −0.855 | .39 | 0.99 (0.97-1.01) |
| Receipt of ASD-specific interventions | −0.003 (0.059) | −0.052 | .96 | 1.00 (0.98-1.02) |
| Receipt of ABA interventions | −0.039 (0.056) | −0.702 | .48 | 0.99 (0.97-1.01) |
Abbreviations: ASD, autism spectrum disorder; ABA, applied behavioral analysis; Bayley-III, Bayley Scales of Infant and Toddler Development, Third Edition; OR, odds ratio.
The SE of estimates were adjusted for the autocorrelation induced by the nesting of participants within 44 different combinations of developmental-behavioral pediatrician and psychologist assessment groups at baseline ASD clinical diagnoses.
The intervention variables have been included separately in the model as they were colinear (rs > 0.95). Thus, the coefficients in the model reflect a multivariate model with total interventions. The estimates for ASD-specific and ABA interventions reflect different model runs, albeit with almost identical estimates for the rest of the variables. Intervention variables represent maximal intensity of intervention following ASD diagnosis, operationalized as the highest number of hours per week of intervention for each participant received in any of the first three 6-month blocks after ASD diagnosis.
Discussion
In this study assessing outcomes of 213 children who were clinically diagnosed with ASD at 12 to 36 months of age, 37.1% had nonpersistent ASD at 5 to 7 years of age based on their current functioning. Children with higher baseline adaptive functioning scores and girls were more likely to have nonpersistent vs persistent ASD. While all children in this sample received interventions, and most received ASD-specific interventions, intensity of interventions in the 18 months after ASD diagnosis was not associated with ASD persistence.
The 37.1% rate of nonpersistent ASD at 5 to 7 years of age is higher than may have been expected based on prior research. A study of 207 children initially diagnosed with Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition, Text Revision) criteria for ASD at 2 years of age and re-evaluated at 4 years of age10 reported 17% did not retain their ASD diagnosis. In a more recent study of children with diverse backgrounds (79.7% from racial and ethnic minority groups) who received a DSM-5 ASD diagnosis before 3 years of age,11 7 of 60 (11.7%) had nonpersistent ASD at a mean (SD) age of 51.3 (7.0) months during follow-up. In that study, for every additional month between initial and follow-up evaluations, children showed a 1.3-fold increase in likelihood of losing the ASD diagnosis. Thus, the older age of our sample at follow-up (mean [SD], 74.3 [7.1] months), as well as differences in demographics, could be associated with higher rates of nonpersistent ASD in our study.
The high rate of apparent ASD resolution by school age may raise questions about accuracy of the initial diagnosis. However, baseline ASD diagnoses were made via team consultations and included developmental testing and administration of the ADOS, which replicates clinical experiences for children referred to a specialized diagnostic center. Alternatively, these outcomes may reflect the developmental trajectory for children with an early ASD diagnosis. A complete description of the characteristics of the nonpersistent ASD group is outside this study’s scope, with functional outcomes to be described in future reports. Other research suggests that even when ASD is nonpersistent, some developmental challenges may remain.32,33 It is also uncertain how the development of these children will progress over time, since they are only 5 to 7 years of age at research assessment.
Our findings are consistent with other recent research indicating that an early ASD diagnosis may not be stable over time.34 A longitudinal study of autism symptom trajectories for 155 children evaluated at various points into adulthood (aged 2-25 years) reported that diagnoses can shift, with some individuals retaining the diagnosis during childhood but not in adulthood. If our findings are replicated in other samples, it may be appropriate to conceptualize ASD at a young age as an “early ASD profile” that requires treatment and monitoring, rather than an immutable diagnosis. Also, if a substantial percentage of young children diagnosed with ASD ultimately do not retain the diagnosis, genetic and biomarker studies of young children with ASD will need to consider this additional complicating factor to describe the already heterogeneous nature of ASD among toddlers.35
Among child-specific baseline characteristics, higher adaptive functioning was associated with nonpersistent ASD, which is consistent with prior findings.10,36 Stronger daily living skills may reflect unmeasured factors, such as ability to learn.10,37 Adaptive skills may capture overall developmental abilities better than 1-time structured assessments such as the Bayley-III cognitive standard score, which incorporates play and language skills, and may not be a sensitive enough measure to differentiate baseline functioning in children aged 12 to 36 months with ASD. The finding that girls were more likely to have nonpersistent ASD than boys aligns with recent studies reporting that girls have decreasing symptoms of ASD over time.38,39 Although unclear, possible explanations include that the social and cultural environment tends to emphasize social-emotional learning for girls more than boys, leading to more naturalistic interventions, or that girls tend to have more subtle symptoms that may lead to less likelihood of receiving a clinical ASD diagnosis.40,41
The methods of this study did not allow us to determine whether children with nonpersistent ASD improved because of inherent differences in their developmental trajectories or because of interventions they received. However, statistical analyses revealed no association between the highest number of hours per week of interventions received in the first 18 months after ASD diagnosis and ASD persistence. Furthermore, children with nonpersistent ASD had gradually decreasing intensity of intervention over time in comparison with those with persistent ASD. All children in this study received some interventions and most received ASD-specific interventions. This study focused on ASD persistence, and it is possible that interventions facilitate other outcomes and provide crucial child and family support in the years after an ASD diagnosis. Thus, these findings should not be interpreted to suggest that interventions do not matter. More nuanced and individualized treatment recommendations are needed and a sequential multiple assignment randomized trials design, in which interventions are adapted based on the child’s developmental progress, could be an ethical and pragmatic approach for future studies.42
Limitations
The findings of this study should be interpreted in the context of some limitations. All participants initially received a clinical diagnosis of DSM-5 ASD at a single multidisciplinary developmental clinic of an academic medical center. It is possible that differences between baseline clinical assessment (team consensus diagnosis, no ADI-R) and research assessment (solo research psychologist rather than team) account for some diagnostic differences. We obtained data on interventions received via parental recall from 3 to 5 years ago. While the children who participated in the study were broadly representative of those seen in this clinic, they were less likely to be of Hispanic ethnicity and had higher baseline cognitive and language or communication scores than nonparticipants, and most of the mothers had higher educational levels and were affluent and White. Thus, it is unclear how well these findings would generalize to more diverse groups of children. The study was conducted in the context of the COVID-19 pandemic and thus about half the sample had research assessments completed with the use of face masks. However, research staff completed assessments consistent with expert opinion during the pandemic.
Conclusions
The findings of this cohort study suggest that a substantial percentage of individuals clinically diagnosed with ASD in early childhood no longer met criteria for ASD at school age, and that higher baseline adaptive scores and female sex were associated with nonpersistent ASD. Most children received ASD-specific interventions after diagnosis, but intensity of intervention was not associated with ASD persistence. Children with an early ASD diagnosis require ongoing developmental monitoring over time for diagnostic clarification and to provide ongoing treatment recommendations.
eTable. Differences Between Study Participants and a Subset of Eligible Nonparticipants
eMethods. Description of Imputation Methods
eFigure 1. IQ Distributions for Children With Nonpersistent ASD and Persistent ASD, Separately
eFigure 2. Probability of Persistent ASD at Research Assessment as a Function of Baseline Vineland Adaptive Scores
Data Sharing Statement
References
- 1.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013. [Google Scholar]
- 2.Maenner MJ, Warren Z, Williams AR, et al. Prevalence and characteristics of autism spectrum disorder among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2020. MMWR Surveill Summ. 2023;72(2):1-14. doi: 10.15585/mmwr.ss7202a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zwaigenbaum L, Bauman ML, Stone WL, et al. Early Identification of autism spectrum disorder: recommendations for practice and research. Pediatrics. 2015;136(suppl 1):S10-S40. doi: 10.1542/peds.2014-3667C [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chawarska K, Klin A, Paul R, Macari S, Volkmar F. A prospective study of toddlers with ASD: short-term diagnostic and cognitive outcomes. J Child Psychol Psychiatry. 2009;50(10):1235-1245. doi: 10.1111/j.1469-7610.2009.02101.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Turner LM, Stone WL. Variability in outcome for children with an ASD diagnosis at age 2. J Child Psychol Psychiatry. 2007;48(8):793-802. doi: 10.1111/j.1469-7610.2007.01744.x [DOI] [PubMed] [Google Scholar]
- 6.Kleinman JM, Ventola PE, Pandey J, et al. Diagnostic stability in very young children with autism spectrum disorders. J Autism Dev Disord. 2008;38(4):606-615. doi: 10.1007/s10803-007-0427-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Malhi P, Singhi P. Follow up of children with autism spectrum disorders: stability and change in diagnosis. Indian J Pediatr. 2011;78(8):941-945. doi: 10.1007/s12098-011-0370-8 [DOI] [PubMed] [Google Scholar]
- 8.Anderson DK, Liang JW, Lord C. Predicting young adult outcome among more and less cognitively able individuals with autism spectrum disorders. J Child Psychol Psychiatry. 2014;55(5):485-494. doi: 10.1111/jcpp.12178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Howlin P, Goode S, Hutton J, Rutter M. Adult outcome for children with autism. J Child Psychol Psychiatry. 2004;45(2):212-229. doi: 10.1111/j.1469-7610.2004.00215.x [DOI] [PubMed] [Google Scholar]
- 10.Moulton E, Barton M, Robins DL, Abrams DN, Fein D. Early characteristics of children with ASD who demonstrate optimal progress between age two and four. J Autism Dev Disord. 2016;46(6):2160-2173. doi: 10.1007/s10803-016-2745-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Giserman-Kiss I, Carter AS. Stability of autism spectrum disorder in young children with diverse backgrounds. J Autism Dev Disord. 2020;50(9):3263-3275. doi: 10.1007/s10803-019-04138-2 [DOI] [PubMed] [Google Scholar]
- 12.Solomon M, Iosif AM, Reinhardt VP, et al. What will my child’s future hold? phenotypes of intellectual development in 2-8-year-olds with autism spectrum disorder. Autism Res. 2018;11(1):121-132. doi: 10.1002/aur.1884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zachor DA, Ben-Itzchak E. From toddlerhood to adolescence, trajectories and predictors of outcome: long-term follow-up study in autism spectrum disorder. Autism Res. 2020;13(7):1130-1143. doi: 10.1002/aur.2313 [DOI] [PubMed] [Google Scholar]
- 14.Barbaro J, Dissanayake C. Diagnostic stability of autism spectrum disorder in toddlers prospectively identified in a community-based setting: behavioural characteristics and predictors of change over time. Autism. 2017;21(7):830-840. doi: 10.1177/1362361316654084 [DOI] [PubMed] [Google Scholar]
- 15.Lord C, Risi S, DiLavore PS, Shulman C, Thurm A, Pickles A. Autism from 2 to 9 years of age. Arch Gen Psychiatry. 2006;63(6):694-701. doi: 10.1001/archpsyc.63.6.694 [DOI] [PubMed] [Google Scholar]
- 16.Fountain C, Winter AS, Bearman PS. Six developmental trajectories characterize children with autism. Pediatrics. 2012;129(5):e1112-e1120. doi: 10.1542/peds.2011-1601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zwaigenbaum L, Bauman ML, Choueiri R, et al. Early intervention for children with autism spectrum disorder under 3 years of age: recommendations for practice and research. Pediatrics. 2015;136(Suppl 1)(suppl 1):S60-S81. doi: 10.1542/peds.2014-3667E [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dawson G, Rogers S, Munson J, et al. Randomized, controlled trial of an intervention for toddlers with autism: the Early Start Denver Model. Pediatrics. 2010;125(1):e17-e23. doi: 10.1542/peds.2009-0958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shire SY, Chang YC, Shih W, Bracaglia S, Kodjoe M, Kasari C. Hybrid implementation model of community-partnered early intervention for toddlers with autism: a randomized trial. J Child Psychol Psychiatry. 2017;58(5):612-622. doi: 10.1111/jcpp.12672 [DOI] [PubMed] [Google Scholar]
- 20.Autism Speaks. Applied Behavior Analysis (ABA). Updated May 1, 2023. Accessed May 2, 2023. https://www.autismspeaks.org/applied-behavior-analysis
- 21.Lovaas OI. Behavioral treatment and normal educational and intellectual functioning in young autistic children. J Consult Clin Psychol. 1987;55(1):3-9. doi: 10.1037/0022-006X.55.1.3 [DOI] [PubMed] [Google Scholar]
- 22.Reichow B, Hume K, Barton EE, Boyd BA. Early intensive behavioral intervention (EIBI) for young children with autism spectrum disorders (ASD). Cochrane Database Syst Rev. 2018;5(5):CD009260. doi: 10.1002/14651858.CD009260.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Boston outcomes of autism in toddlers study (BOAT). ClinicalTrials.gov identifier: NCT03517163. Updated July 6, 2023. Accessed July 6, 2023. https://classic.clinicaltrials.gov/ct2/show/NCT03517163
- 24.Harris HK, Lee C, Sideridis GD, Barbaresi WJ, Harstad E. Identifying subgroups of toddlers with DSM-5 autism spectrum disorder based on core symptoms. J Autism Dev Disord. 2021;51(12):4471-4485. doi: 10.1007/s10803-021-04879-z [DOI] [PubMed] [Google Scholar]
- 25.Lord C, Rutter M, Le Couteur A. Autism Diagnostic Interview–Revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J Autism Dev Disord. 1994;24(5):659-685. doi: 10.1007/BF02172145 [DOI] [PubMed] [Google Scholar]
- 26.Elliott CD, Salerno JD, Dumont R, Willis JO. Contemporary intellectual assessment: Theories, tests, and issues. In: Flanagan DP, McDonough EM, eds. The Differential Ability Scales. 2nd ed. The Guilford Press; 2018:360-382. [Google Scholar]
- 27.Albers CA, Grieve AJ. Test review: Bayley, N. (2006). Bayley Scales of Infant and Toddler Development–Third Edition. J Psychoed Assess. 2007;25(2):180-190. doi: 10.1177/0734282906297199 [DOI] [Google Scholar]
- 28.Zimmerman IL, Steiner VG, Pond RE. Preschool Language Scales. 5th ed. Pearson; 2011. Accessed February 22, 2023. https://psycnet.apa.org/doiLanding?doi=10.1037%2Ft15141-000 [Google Scholar]
- 29.Sparrow SS, Cicchetti DV, Saulnier CA. Vineland Adaptive Behavior Scales. 3rd ed. Pearson; 2016. Accessed February 22, 2023. https://www.pearsonassessments.com/store/usassessments/en/Store/Professional-Assessments/Behavior/Adaptive/Vineland-Adaptive-Behavior-Scales-%7C-Third-Edition/p/100001622.html [Google Scholar]
- 30.Enders CK. Applied Missing Data Analysis. 2nd ed. Guilford Press; 2022. [Google Scholar]
- 31.US Census Bureau B19013 . Median household income in Massachusetts in 2020. 2020. Accessed February 22, 2023. https://www.census.gov/quickfacts/fact/table/MA#
- 32.Suh J, Orinstein A, Barton M, et al. Ratings of broader autism phenotype and personality traits in optimal outcomes from autism spectrum disorder. J Autism Dev Disord. 2016;46(11):3505-3518. doi: 10.1007/s10803-016-2868-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Troyb E, Rosenthal M, Eigsti IM, et al. Executive functioning in individuals with a history of ASDs who have achieved optimal outcomes. Child Neuropsychol. 2014;20(4):378-397. doi: 10.1080/09297049.2013.799644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Elias R, Lord C. Diagnostic stability in individuals with autism spectrum disorder: insights from a longitudinal follow-up study. J Child Psychol Psychiatry. 2022;63(9):973-983. doi: 10.1111/jcpp.13551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Thapar A, Rutter M. Genetic advances in autism. J Autism Dev Disord. 2021;51(12):4321-4332. doi: 10.1007/s10803-020-04685-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Georgiades S, Tait PA, McNicholas PD, et al. Trajectories of symptom severity in children with autism: variability and turning points through the transition to school. J Autism Dev Disord. 2022;52(1):392-401. doi: 10.1007/s10803-021-04949-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sutera S, Pandey J, Esser EL, et al. Predictors of optimal outcome in toddlers diagnosed with autism spectrum disorders. J Autism Dev Disord. 2007;37(1):98-107. doi: 10.1007/s10803-006-0340-6 [DOI] [PubMed] [Google Scholar]
- 38.Szatmari P, Georgiades S, Duku E, et al. ; Pathways in ASD Study Team . Developmental trajectories of symptom severity and adaptive functioning in an inception cohort of preschool children with autism spectrum disorder. JAMA Psychiatry. 2015;72(3):276-283. doi: 10.1001/jamapsychiatry.2014.2463 [DOI] [PubMed] [Google Scholar]
- 39.Waizbard-Bartov E, Ferrer E, Young GS, et al. Trajectories of autism symptom severity change during early childhood. J Autism Dev Disord. 2021;51(1):227-242. doi: 10.1007/s10803-020-04526-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lai MC, Lombardo MV, Chakrabarti B, et al. ; MRC AIMS Consortium . Neural self-representation in autistic women and association with “compensatory camouflaging”. Autism. 2019;23(5):1210-1223. doi: 10.1177/1362361318807159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lai MC, Szatmari P. Sex and gender impacts on the behavioural presentation and recognition of autism. Curr Opin Psychiatry. 2020;33(2):117-123. doi: 10.1097/YCO.0000000000000575 [DOI] [PubMed] [Google Scholar]
- 42.Kasari C, Sturm A, Shih W. SMARTer approach to personalizing intervention for children with autism spectrum disorder. J Speech Lang Hear Res. 2018;61(11):2629-2640. doi: 10.1044/2018_JSLHR-L-RSAUT-18-0029 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Differences Between Study Participants and a Subset of Eligible Nonparticipants
eMethods. Description of Imputation Methods
eFigure 1. IQ Distributions for Children With Nonpersistent ASD and Persistent ASD, Separately
eFigure 2. Probability of Persistent ASD at Research Assessment as a Function of Baseline Vineland Adaptive Scores
Data Sharing Statement