Highlights
-
•
Preventable hospitalization rates decreased after Medicaid expansion in 2014.
-
•
Chronic obstructive pulmonary disease and asthma in older adults and bacterial pneumonia rates decreased after 2014.
-
•
These rates may be used as a quality indicator to measure access to primary care.
Keywords: Preventable hospitalizations, trends, Medicaid expansion, Affordable Care Act, policy
Abstract
Introduction
The Patient Protection and Affordable Care Act aimed to increase the number of individuals with health insurance, which may lead to adequate primary care management and reduced rates of preventable hospitalizations. To investigate the rates of preventable hospitalization after the passing of the Affordable Care Act in 2010 and Medicaid expansion in 2014 across 26 states, a population-based study was conducted using the Healthcare Cost and Utilization Project National Inpatient Sample database from 2005–2017.
Methods
A logistic regression and trend analysis was performed to assess the changes in preventable hospitalization rates over time and the impact of policy changes on the rate of preventable hospitalization. Individuals were included if they were aged between 18 and 64 years and had a preventable quality indicator International Classification of Diseases, Ninth or Tenth Revision code as determined by the Agency for Healthcare Research and Quality.
Results
More than 45 million preventable-hospitalization admissions were reported between 2005 and 2017. There was a significant decrease in preventable hospitalization rates after the passing of the Affordable Care Act from 12.0% to 10.8% (p<0.01) and from 11.5% to 10.6% (p<0.01) after Medicaid expansion. Bacterial pneumonia declined from 1.5% to 0.6% (p<0.01), along with chronic obstructive pulmonary disease and asthma in older adults from 1.9% to 1.7% (p=0.01) after the expansion.
Conclusions
States that have not implemented Medicaid expansion should make it a priority because it may lead to a reduction in preventable hospitalization rates. Furthermore, preventable hospitalization rates may be considered a quality measure to examine the accessibility and effectiveness of primary care intervention.
INTRODUCTION
More than $25 billion of healthcare expenses are attributable to preventable hospitalizations (PHs) each year.1,2 PHs, also referred to as ambulatory care sensitive conditions, are hospitalizations for specific acute and chronic conditions, such as bacterial pneumonia and diabetes complications. These hospitalizations occur when patients are unable to obtain and maintain primary care management.3 Billings et al.4 expand upon this understanding of PHs and state that outpatient care must be timely and effective to prevent the onset of symptoms and diseases for these chronic and acute conditions. Obstacles to accessing primary care in a timely manner include but are not limited to language barriers, disabilities, travel barriers, shortage of primary care physicians, and lack of health insurance.5, 6, 7, 8 Lack of health insurance leads to an underutilization of primary care resources because individuals are more likely to delay care and use the emergency department (ED) for treatment.5,9,10 However, PHs, particularly bacterial pneumonia, may occur in some individuals with adequate primary care access. Ultimately, an increase in insurance coverage should lead to a rise in primary care utilization, reducing the number of PHs.2,11,12
The Patient Protection and Affordable Care Act (ACA) was enacted in 2010 with the goal to expand healthcare coverage for Americans.13 However, the ACA was not implemented in >50% of the states (26 states) until 2014. The ACA reduced the number of uninsured individuals from 16% in 2010 to 9.1% in 2015.14 This reduction was achieved through the expansion of Medicaid eligibility and the addition of tax credits to increase accessibility to low-income individuals.14 Sommer et al.15 found that the expansion was associated with significantly increased access to primary care, reduced likelihood of ED visits, and increased screening and glucose monitoring rates for diabetes. They determined that PHs may be considered a quality measure to examine the effectiveness and accessibility of primary care.15 Although the effects of the ACA have been established, the relationship between PHs and the ACA has not been fully studied. Wen et al.3 evaluated the effects of Medicaid expansion from 2009 to 2015 in 36 states, obtaining 2 years of data after the expansion occurred, and found that adjusted PH rates decreased by approximately 3.5% among states that implemented Medicaid expansion. However, it is unclear whether these trends persist beyond 2 years after expansion.
Because of the implications that PH rates may have on patient mortality and healthcare expenses, they may be a primary focus for national and local policymakers working to reduce healthcare disparities. This study used a nationwide inpatient database to investigate the incidence and prevalence of PH after the passing of the ACA and Medicaid expansion across 26 states in 2014. We hypothesize that the rate of PH will decrease after the passing of the ACA and Medicaid expansion because of the requirement to have health insurance, ultimately granting individuals improved access to primary care.
METHODS
Study Population and Measures
We used the Healthcare Cost and Utilization Project (HCUP) National Inpatient Sample (NIS) database from 2005–2017 to retrieve PHs for patients aged 18–64 years. Individuals aged ≥65 years were not included because they are covered by Medicare and thus were minimally affected by the ACA and Medicaid expansion. By removing individuals aged ≥65 years, we are more accurately able to measure the impacts the ACA and Medicaid expansion had on PH. However, Medicare as an insurance group was not removed entirely because individuals aged <65 years with disabilities or end-stage renal disease can have Medicare insurance. The ACA provided many benefits to those with disabilities, including protection for those with pre-existing conditions, increased access to homecare-based services, and expanded eligible health conditions for Medicare and Medicaid. Eliminating Medicare from this study altogether would exclude a portion of the population that can benefit from the passing of the ACA. The NIS is the largest inpatient all-payer database in the U.S. From 2005 to 2011, the database was made up of approximately 8 million hospitalizations each year. In 2012, the database switched to a 20% stratified sample of admissions from participating acute-care hospitals (excluding federal hospitals, rehabilitation centers, and long-term care facilities) across the country. A total of 49 of 51 states’ (including Washington, District of Columbia) data are included within the sample. This 20% sample is designed to represent hospitals nationwide, even if a state's data may not be present within the database. Stratification for the NIS is based on 5 characteristics: hospital region, urban/rural status, ownership, number of beds, and teaching status. Sampling weights, as determined by the NIS, were applied each year to represent the entire U.S. population. Specific sampling weights were applied to 2005–2011 to account for changes that occurred in the redesign of the NIS database in 2012.16
Measures
A total of 10 Preventable Quality Indicator (PQI) conditions set forth by the Agency for Healthcare Research and Quality (AHRQ), Version 2019, were used to determine the PH rate each year between 2005 and 2017. PQI conditions included short-term diabetes complications, long-term diabetes complications, uncontrolled diabetes, lower extremity amputation related to diabetes, chronic obstructive pulmonary disease (COPD), asthma, hypertension, heart failure, community–acquired bacterial pneumonia, and urinary tract infection (UTI).17,18 PQI ICD-9-CM and ICD-10-CM diagnosis codes were identified by the AHRQ Evidence-Based Practice Center at Stanford University and the University of California, San Francisco through literature reviews and other evaluations. Patients must have one of the codes as the primary diagnosis.18
Statistical Analysis
A logistic regression and trend analysis were performed. Our outcome was binary: patients with a PH versus patients who did not have a PH. All records reported in NIS from 2005–2017 were included in the analysis. The NIS uses a record identifier instead of a person identifier; therefore, the analysis was based on record units. Given the size of the data set, a 0.01% weighted random sample without replacement was used for downstream analysis. Sampling without replacement ensures that an unbiased, representative sample was obtained. The sample demographic data were compared with the NIS demographics and were shown to be similar and thus were representative of the NIS sample itself. The sample data and descriptive statistics of covariates are shown as count (percentage) for categorical variables and mean (SD) for continuous variables. Covariates for this analysis include sex, age, race, income, and region. The income variable refers to the estimated median household income of residents in the patient's ZIP code. The quartiles are identified by values of 1–4, indicating the poorest to wealthiest populations. These values are derived from ZIP code‒demographic data obtained from Claritas.19 The income percentiles are updated annually; therefore, each year's income range and percentile vary. For example, in 2005, the 50th percentile was $45,999, but in 2017, it was $55,999. The statistics and distributions of each covariate were compared between patients with PH and patients without. A similar comparison was performed between the complete data and our randomly selected samples to ensure that our sample data were representative. A Student's t-test was used for continuous variables comparison, and a chi-square test was used to compare categorical variables. We showed the trajectory of PH rate and PQI condition rate changes each year in the sampled data. The association between PH rate and the passing of the ACA as well as the impact of Medicaid expansion on PH rate changes were evaluated through multiple logistic regression, adjusting for all other covariates. The corresponding adjusted p-values are reported. A p-value of <0.05 was considered statistically significant for all analyses, which were performed using R, Version 3.6.0. The University of Michigan Medical School IRB determined that this study was not regulated (HUM00171404).
RESULTS
A total of 45,119,586 PHs were reported in the U.S. between 2005 and 2017. We randomly selected a 0.01% weighted random sample for our statistical modeling and identified 40,647 hospitalizations (Figure 1). No statistically significant differences were found between the random sample and the whole population, showing that this random sample represented the whole population well. Of these hospitalizations, 3,155 (7.8%) were determined to be PHs according to the PQIs provided by AHRQ. Among these PHs, women made up 54.5% of records; approximately 30.1% of patients were covered by private insurance, whereas 27.1% were covered by Medicaid; and 64.5% of patients lived in an area with a median household income level that was in the 50th percentile or below. Table 1 provides a full list of the characteristics of our sample and PH records. Table 2 describes the sample size per PQI condition included within the sample by year.
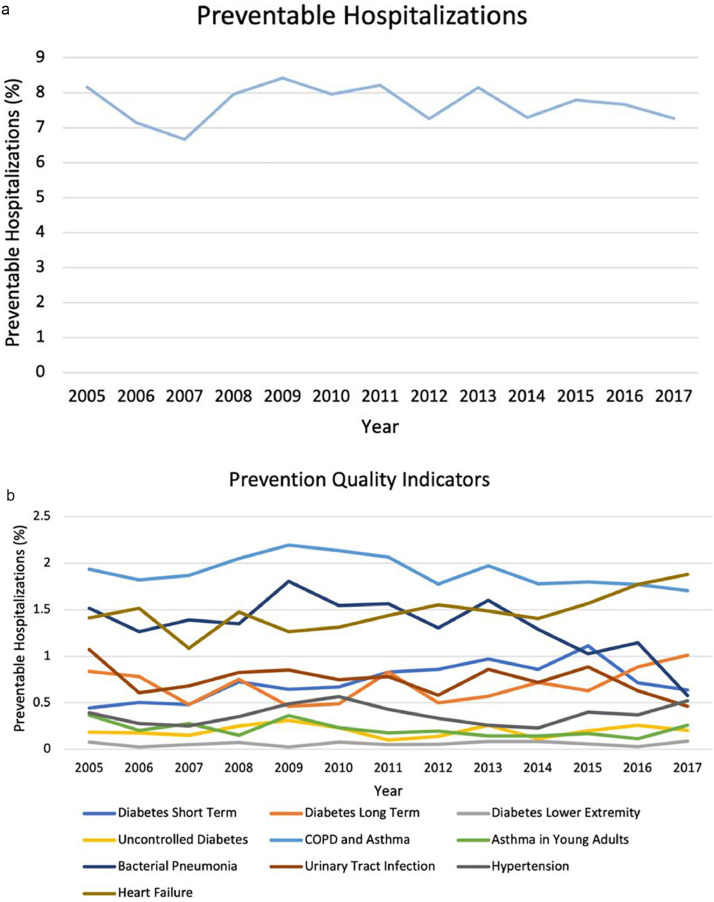
Figure 1.
Preventable hospitalizations between 2005 and 2017 and preventable quality indicator hospitalizations from 2005 to 2017.
COPD, chronic obstructive pulmonary disease.
Table 1.
Summary Statistics on the Characteristics of the Study Cohort and the Subset of Subjects With Preventable Hospitalizations
| Characteristics | Sample (n=40,647) |
Preventable hospitalizations (n= 3,155) |
||
|---|---|---|---|---|
| n | (%) | n | (%) | |
| Age | ||||
| Mean age (SD) | 43.0 | (13.8) | 49.5 | (11.8) |
| Age range | 18–64 | 18–64 | ||
| Sex | ||||
| Men | 15,433 | (38.0) | 1,434 | (45.5) |
| Women | 25,214 | (62.0) | 1,721 | (54.5) |
| Race | ||||
| White | 25,229 | (62.1) | 1,811 | (57.4) |
| Black | 7,221 | (17.3) | 823 | (26.1) |
| Hispanic | 5,456 | (13.4) | 359 | (11.4) |
| Asian or pacific islander | 1,090 | (2.7) | 46 | (1.5) |
| Native American | 305 | (0.8) | 19 | (0.6) |
| Other | 1,346 | (3.3) | 97 | (3.1) |
| Income | ||||
| 0–25th percentile | 12,817 | (31.5) | 1,222 | (38.7) |
| 26th–50th percentile | 10,184 | (25.1) | 815 | (25.8) |
| 51st–75th percentile | 9,335 | (23.0) | 655 | (20.8) |
| 76th–100th percentile | 8,311 | (20.4) | 463 | (14.7) |
| Insurance | ||||
| Medicare | 6,123 | (15.1) | 865 | (27.4) |
| Medicaid | 10,847 | (26.7) | 854 | (27.1) |
| Private insurance | 18,199 | (44.8) | 949 | (30.1) |
| Self-pay | 3,246 | (8.0) | 335 | (10.6) |
| No charge | 363 | (0.9) | 40 | (1.3) |
| Other | 1,869 | (4.6) | 112 | (3.5) |
| Hospital region | ||||
| Northeast | 8,665 | (21.3) | 634 | (20.1) |
| Midwest | 7,228 | (17.8) | 536 | (17.0) |
| South | 16,523 | (40.6) | 1,460 | (46.3) |
| West | 8,231 | (20.2) | 525 | (16.6) |
| Hospital bed size | ||||
| Small | 5,423 | (13.3) | 559 | (17.7) |
| Medium | 10,900 | (26.8) | 887 | (28.1) |
| Large | 24,324 | (59.8) | 1,709 | (54.2) |
| Hospital location and teaching status | ||||
| Rural | 3,853 | (9.5) | 450 | (14.3) |
| Urban nonteaching | 14,792 | (36.4) | 1,234 | (39.1) |
| Urban teaching | 22,002 | (54.1) | 1,471 | (46.6) |
Table 2.
Sample Size per Prevention Quality Indicator Condition
| Conditions | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Short-term diabetes complications | 17 | 20 | 19 | 29 | 25 | 26 | 33 | 31 | 34 | 30 | 39 | 25 | 22 |
| Long-term diabetes complications | 32 | 31 | 19 | 30 | 18 | 19 | 33 | 18 | 20 | 25 | 22 | 31 | 35 |
| Lower extremity amputation for diabetes | <11 | <11 | <11 | <11 | <11 | <11 | <11 | <11 | <11 | <11 | <11 | <11 | <11 |
| Uncontrolled diabetes | <11 | <11 | <11 | <11 | 12 | <11 | <11 | <11 | <11 | <11 | <11 | <11 | <11 |
| COPD/asthma in older adults | 74 | 72 | 74 | 82 | 85 | 83 | 82 | 64 | 69 | 62 | 63 | 62 | 59 |
| Asthma in young adults | 14 | <11 | 11 | <11 | 14 | <11 | <11 | <11 | <11 | <11 | <11 | <11 | <11 |
| Bacterial pneumonia | 58 | 50 | 55 | 54 | 70 | 60 | 62 | 47 | 56 | 45 | 36 | 40 | 20 |
| Urinary tract infections | 41 | 24 | 27 | 33 | 33 | 29 | 31 | 21 | 30 | 25 | 31 | 22 | 16 |
| Hypertension | 15 | 11 | <11 | 14 | 19 | 22 | 17 | 12 | <11 | <11 | 14 | 13 | 18 |
| Heart failure | 54 | 60 | 43 | 59 | 49 | 51 | 57 | 56 | 52 | 49 | 55 | 62 | 65 |
| Total | 312 | 283 | 264 | 318 | 326 | 309 | 326 | 261 | 285 | 254 | 273 | 268 | 251 |
Note: The HCUP-NIS data use agreement requires that cells with <11 subjects cannot be published.
COPD, chronic obstructive pulmonary disease; HCUP, Healthcare Cost and Utilization Project; NIS, National Inpatient Sample.
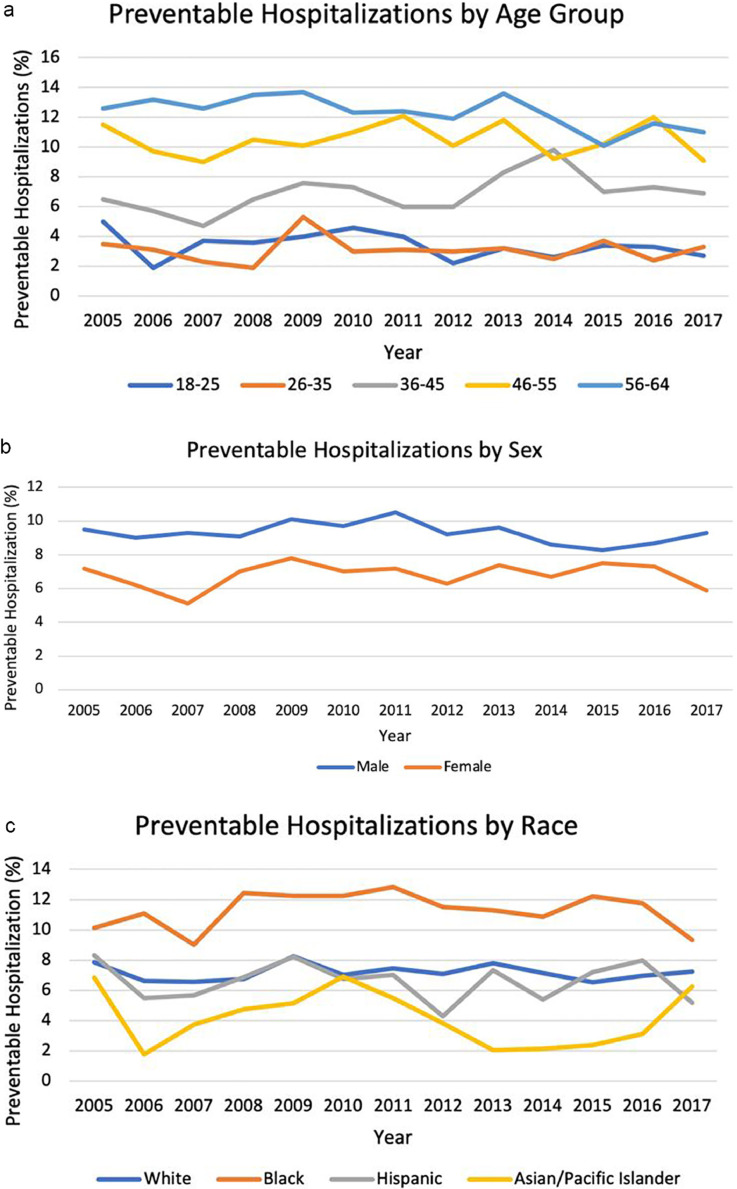
The overall PH rate decreased from 8.2% in 2005 to 7.7% in 2017 (p=0.05; OR=1; 95% CI= −0.989, 1.000) (Figure 1). In 2005, COPD and asthma were the most common PHs, making up 1.9% of all records that year. However, in 2017, heart failure (1.9%) was the most prevalent PH. Figure 1 reports the frequency of the PQI conditions between 2005 and 2017. Between 2005 and 2017, there was an overall significant decrease in the rate of PHs for bacterial pneumonia from 1.5% to 0.6% (p<0.01; OR=0.965; 95% CI=0.942, 0.989) and of COPD and asthma from 1.9% to 1.7% (p=0.01; OR=0.975; 95% CI=0.955, 0.995), whereas there was an increase in short-term diabetes complications from 0.2% to 0.5% (p=0.02; OR=1.04; 95% CI=1.007, 1.074). Thus, there was a significant decrease in the odds of experiencing PH owing to bacterial pneumonia by 3.5% per year from 2005–2017. The remaining 7 PQI conditions did not have significant changes in trends (Table 3). Figure 2 shows the differences among PHs by age groups, sex, and race. The only significant difference that occurred was between Black individuals and White individuals (p<0.01; OR=1.693; 95% CI=0.432, 0.621).
Table 3.
The Adjusted Estimated ORs of Preventable Hospitalizations Associated With Time or Passing of the ACA (2010) or Medicaid Expansion (2014)
| Changes over time during 2005–2017 | |||
|---|---|---|---|
| Condition | ORa | 95% CI | p-value |
| Short-term diabetes complications | 1.04 | 1.007, 1.074 | 0.02 |
| Long-term diabetes complications | 1.01 | 0.977, 1.044 | 0.54 |
| Lower extremity amputation for diabetes | 1.045 | 0.931, 1.172 | 0.45 |
| Uncontrolled diabetes | 1.026 | 0.964, 1.092 | 0.42 |
| COPD and asthma in older adults | 0.975 | 0.955, 0.995 | 0.01 |
| Asthma in young adults | 0.963 | 0.908, 1.021 | 0.21 |
| Bacterial pneumonia | 0.965 | 0.942, 0.989 | <0.01 |
| UTI | 0.98 | 0.950, 1.011 | 0.33 |
| Hypertension | 0.997 | 0.953, 1.042 | 0.89 |
| Heart failure | 0.999 | 0.976, 1.022 | 0.93 |
| Total preventable hospitalization | 0.989 | 0.979, 1.000 | 0.05 |
| Passing of the ACA (2010) (2005–February 2010 versus March 2010–2017) | |||
|---|---|---|---|
| Condition | ORa | 95% CI | p-value |
| Short-term diabetes complications | 1.349 | 1.052, 1.731 | 0.02 |
| Long-term diabetes complications | 1.021 | 0.794, 1.312 | 0.87 |
| Lower extremity amputation for diabetes | 2.028 | 0.746, 5.512 | 0.17 |
| Uncontrolled diabetes | 0.886 | 0.564, 1.393 | 0.60 |
| COPD and asthma in older adults | 0.814 | 0.700, 0.946 | <0.01 |
| Asthma in young adults | 0.771 | 0.505, 1.178 | 0.23 |
| Bacterial pneumonia | 0.883 | 0.738, 1.056 | 0.17 |
| UTI | 0.892 | 0.708, 1.123 | 0.33 |
| Hypertension | 0.9 | 0.649, 1.247 | 0.53 |
| Heart failure | 0.975 | 0.820, 1.160 | 0.78 |
| Total preventable hospitalization | 0.927 | 0.857, 1.002 | 0.06 |
| Medicaid Expansion (2014) (2005–2013 versus 2014–2017) | |||
|---|---|---|---|
| Condition | ORa | 95% CI | p-value |
| Short-term diabetes complications | 1.208 | 0.945, 1.544 | 0.13 |
| Long-term diabetes complications | 1.195 | 0.932, 1.531 | 0.16 |
| Lower extremity amputation for diabetes | 1.11 | 0.473, 2.606 | 0.81 |
| Uncontrolled diabetes | 1.104 | 0.682, 1.785 | 0.69 |
| COPD and asthma in older adults | 0.816 | 0.694, 0.959 | 0.01 |
| Asthma in young adults | 0.862 | 0.533, 1.395 | 0.55 |
| Bacterial pneumonia | 0.7 | 0.571, 0.859 | <0.01 |
| UTI | 0.866 | 0.673, 1.115 | 0.26 |
| Hypertension | 0.959 | 0.675, 1.363 | 0.81 |
| Heart failure | 1.026 | 0.862, 1.220 | 0.77 |
| Preventable hospitalization | 0.917 | 0.844, 0.995 | 0.04 |
Note: Boldface indicates statistical significance (p<0.05).
OR estimates associated with each year. OR<1 is a decrease, and OR>1 is an increase. For example, from 2005 to 2017, preventable hospitalizations because of short-term diabetes complications significantly increased by 4% per year.
ACA, Affordable Care Act; COPD, chronic obstructive pulmonary disease; UTI, urinary tract infection.
Figure 2.
Preventable hospitalizations 2005 and 2017 by age group, sex, and race.
A logistic regression model was used, to assess whether there is a decrease in the overall PH rate and PQI condition rates before (2005-February 2010) and after (March 2010–2017) the passing of the ACA, adjusting for other covariates (Table 3). After the passing of the ACA, the overall PH rate decreased from 8.0% to 7.7% (p=0.06; OR=0.927; 95% CI=0.857, 1.002). Comparing 2005–February 2010 (before the ACA was passed) with March 2010–March 2017 (after the ACA was passed), the rates for COPD and asthma significantly decreased (p<0.01; OR=0.814; 95% CI=0.7, 0.946), and the rates for short-term diabetes complications increased from 0.6% to 0.9% (p=0.02; OR=1.349; 95% CI=1.052, 1.731). Adjusting for other covariates, the odds of having PH owing to short-term diabetes complications increased by 4% per year during the study period 2005–2017 (p=0.02; OR=1.04; 95% CI=1.007, 1.074). Hypertension, UTIs, bacterial pneumonia, uncontrolled diabetes, and lower extremity amputations among patients with diabetes trended downward but not significantly (Table 3 and Figure 2). The remaining conditions—heart failure, long-term diabetes complications, and asthma in young adults—increased in rate but not significantly (Table 3 and Figure 2).
Although the ACA was passed in 2010, Medicaid expansion did not occur in more than half of the states until 2014. Therefore, we performed a subgroup analysis to evaluate whether there was a change in PH rates before (2005–2013) and after (2014–2017) Medicaid expansion (Table 3). Overall PH rates decreased significantly after Medicaid expansion (p=0.04; OR=0.917; 95% CI=0.844, 0.995). For condition-specific rates, we again found a significant decrease in COPD and asthma in older adults (p=0.01; OR=0.816; 95% CI=0.694, 0.959) and bacterial pneumonia (p<0.01; OR=0.7; 95% CI=0.571, 0.859) after Medicaid expansion. More specifically, the odds of having a PH owing to bacterial pneumonia dropped significantly by 30% after Medicaid expansion. The rates of short-term diabetes complications and UTIs decreased too, although they were not statistically significant. The rates of long-term diabetes complications, lower extremity amputation among patients with diabetes, uncontrolled diabetes, hypertension, asthma in young adults, and heart failure increased after Medicaid expansion but not significantly (Figure 2).
DISCUSSION
Before the passing of the ACA in 2010, more than 20 million Americans did not have health insurance, thus limiting their access to primary care.20 Individuals without health insurance are less likely to use primary care services and are more likely to have poor health outcomes, have a delay in care, and be hospitalized for manageable conditions.5,8,9 Primary care provides services such as screening for diseases, blood pressure readings, and acute and chronic care management.21 Medicaid expansion increased insurance coverage by 14.9% in states.22 Therefore, we conducted a population-based study to determine whether the passing of the ACA and expansion of Medicaid led to a decrease in PH rates.
The results of this population-based study found a significant decrease in total PH rates after Medicaid expansion in 2014 across 26 states. In addition, the rates of bacterial pneumonia and COPD and asthma in older adults decreased substantially after the expansion. We suspect that the decline in bacterial pneumonia is associated with increase in primary care access to avert more serious infection. Bacterial pneumonia occurs more frequently in patients with multiple comorbidities; therefore, the increase in primary care access is likely to improve the overall health of a patient to mount a more effective immune response.23 COPD and asthma likely decreased because of the development of treatments, an increase in areas that prohibit smoking in public places, and improvements in disease management.24 Next, long-term diabetes complications, asthma in young adults, UTIs, and hypertension had sizable decreases in hospitalization rates, but they were not significant. The decline in hospitalizations for these conditions is likely related to improved access to primary care, which provides patients with access to antibiotics, inhalers, blood pressure readings, and blood glucose screenings. In contrast, the remaining 3 diabetes conditions and heart failure had increased hospitalization rates but not significantly. These are chronic conditions that may be prevented in the earlier phases of the disease rather than the terminal events that may be difficult to control. Short-term diabetes complications began to rise in 2007 and continued until 2015 before declining to the previous PH rates for short-term diabetes complications. Many factors lead to an increased risk for diabetes, such as lack of exercise, but the decline from 2015 to 2017 is promising because individuals may be reverting to previous practices and receiving earlier intervention from primary care visits to reduce the overall rate of diabetes. Finally, a downward trend in PH rates occurred before 2010. This decline in PH is likely caused by the economic crash that started in late 2007. This economic crash left many without insurance because individuals lost their jobs. Individuals with insurance experienced increased premiums and copays, further deterring them from seeking care. Therefore, the passing of the ACA and Medicaid expansion appears to be instrumental in the reduction of PH rates and the decline in hospitalizations for PQI conditions set forth by the AHRQ. Future researchers may seek to investigate the level of contribution the ACA and Medicaid expansion have had on the decreasing rate of PH compared with the public health policies that have been enacted over time and the changes in care management that have occurred since the passing of the ACA and Medicaid expansion.
One of the aims of the ACA was to reduce healthcare costs. Chronic conditions, along with technology and lifestyle choices, are some of the reasons for rising healthcare costs. Approximately 75% of healthcare costs are because of chronic conditions, including diabetes, which is a PQI condition.25 Concentrating efforts to minimize chronic conditions is one of the most feasible ways to reduce healthcare costs. Researchers have found that the most disadvantaged (Area Deprivation Index, Quintile 5) counties had a higher proportion of their healthcare costs going to potentially preventable care.26 Individuals living in the poorest neighborhoods are twice as likely to be hospitalized as those who live in wealthy neighborhoods.27 Thus, some recommend that local governments should spend more on health and social services to increase early intervention, educate the community on the importance of routine care visits, and potentially prevent hospitalization.28 Some social services, such as education and housing, have been associated with improvements in community health.29 Therefore, national and local policymakers in geographic locations with high rates of PHs should work together to implement policies to reduce healthcare disparities.
Although this study did not analyze data beyond 2017, it is critical to mention the impact severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) or coronavirus disease 2019 (COVID-19) has had on the ED and outpatient care, because future studies may assess these impacts and the rates of PH. The COVID-19 pandemic has exacerbated health disparities and conditions across the country, limited outpatient care because non-emergency cases were delayed, and pushed EDs further beyond their limits. The limited access to outpatient centers has led many individuals to seek care from the ED, but the ED is filled with patients with COVID-19, leading to increased wait times. Before COVID-19, wait times in the ED had already increased or worsened after Medicaid expansion because wait times for primary care appointments also increased. Increased wait times for primary care are promising because they show that more individuals are seeking care now that they have insurance.30 Lyu and Wehby found that the rate of cancer screenings among low-income individuals has increased in states participating in Medicaid expansion with a high supply of primary care physicians, but the rates have not increased in states with a low supply of physicians, thus leading patients to seek care from the ED instead.31 To minimize the physician shortage, Congress should seek to expand the number of residency spots, whereas state governments may offer financial rewards to physicians who accept Medicaid insurance to increase the supply of physicians. It is reasonable to believe that future data will continue to show an increase in wait times for both the ED and primary care appointments because the physician shortage continues to increase, and non-essential healthcare was placed on hold during the initial stages of COVID-19. It is unclear the level of impact and the long-term implications wait times will have on PH rates in the future as the healthcare system aims to return to prepandemic levels of care. Future work should aim to understand how the COVID-19 pandemic and increased post-expansion wait times will impact the rate of PH over time.
Limitations
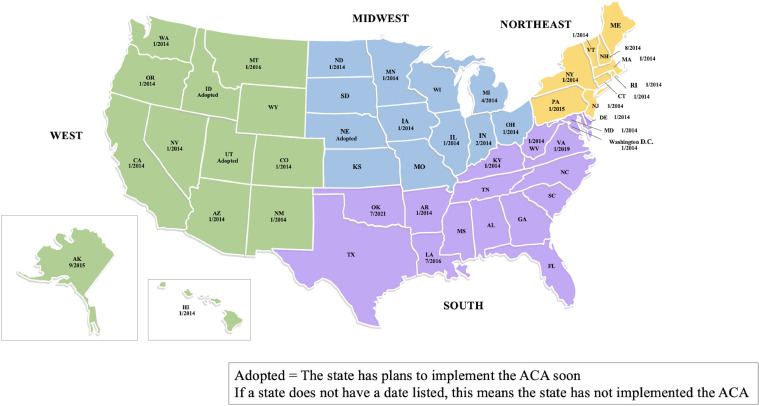
This study has limitations. First, the use of a single database cannot capture all the variables related to PHs. The HCUP database does not include government hospitals, long-term care facility patients, and rehabilitation centers and only represents 20% of all hospitals in the U.S. Including PH rates from these centers and hospitals could skew the overall rate of PH because these patients are more susceptible to complications given their previous experiences and comorbidities. However, the database covers a wide range geographically and stratifies the data on the basis of region, bed count, location, teaching status, and ownership to build a comprehensive database. Second, the analysis is not able to account for the full impact of Medicaid expansion on the U.S. As of 2014, only 26 states had implemented the ACA. However, each year, more states have put plans in place to implement the legislation, and we have found a significant decrease in PH rates after the expansion of Medicaid in 26 states in 2014. As of 2021, 37 states (including Washington DC) had adopted or implemented the expansion, and 14 states had not adopted the expansion (Figure 3).32 Therefore, we anticipate a further decline in PH rates as more states implement the ACA. Third, a state-by-state analysis was not performed because of limited access to consistent data sets. The State Inpatient Database includes 36 states, but there are gaps within the data for some states, and other states do not have data available for 2005‒2017. For instance, data from California are only available from 2003–2011 to 2018–2020, data from Indiana are only available from 2017 to 2020, and those from Wisconsin are not available for purchase. Therefore, the NIS database was selected because it provided a sample that represented hospitalizations nationwide. Future researchers who want to investigate state differences and report on state policies should ensure that the assumption of similarity can be maintained across states participating in the analysis. Failure to do so could provide a false representation of the trends over time. Fourth, the NIS does not identify patients who were admitted for observation only nor does the NIS include patients who are treated within the ED and discharged. Therefore, it could not be determined whether the increasing practice of admitting individuals for observation was leading to a decrease in PHs. Fifth, we are not able to assess causality between the decrease in PH rates and the impact of the ACA. However, since 1981, it has been theorized that low-income and uninsured individuals were more likely to be hospitalized than those in high-income areas or who had private insurance.17,33,34 As research on PH continues, it has been agreed upon by researchers and national organizations, such as the Centers for Disease Control and Prevention, that PH can be reduced by successful primary care management.35 Finally, the sample size was limited to a 0.01% sample. Including a larger sample size for this analysis would have overestimated small differences and led to statistically significant and misleading results. Despite the small sample size, the sample population was representative of the HCUP-NIS database. Future researchers should be cautious with overestimating the differences within a database and should use additional databases or sources of data if restricted by small sample size.
Figure 3.
Medicaid expansion across the U.S. through 2021.
ACA, Affordable Care Act.
CONCLUSIONS
Our study indicates that the passing of the ACA and the expansion of Medicaid are associated with decreased rates of PH overall, bacterial pneumonia, and COPD and asthma in older adults. Of the 50 states and Washington, DC, 37 states have implemented or adopted the Medicaid expansion as of 2021. Therefore, we suggest that the remaining 14 states expand Medicaid. Furthermore, policymakers should use PH rates as a quality measure to examine the accessibility and effectiveness of primary care in a given region. In addition, policymakers may reconsider modifying the ACA to include lower copays, encourage more physicians to accept government insurance to improve access to providers, and increase the number of residency spots to reduce the physician shortage and ultimately minimize the rates of PHs in the future. State and local government leaders should work together to improve health and social services for their communities and educate community members because SES plays a role in health outcomes.
ACKNOWLEDGMENTS
Molin Yue worked at the Department of Biostatistics, School of Public Health, University of Michigan at the time of the research.
KCC receives funding from the National Institutes of Health, book royalties from Wolters Kluwer and Elsevier, and a research grant from Sonex to study carpal tunnel outcomes.No other disclosures were reported.
CRediT AUTHOR STATEMENT
Shannon M. Wood: Conceptualization, Formal analysis, Resources, Visualization, Writing–original draft, Writing–review and editing. Molin Yue: Data curation, Formal analysis, Methodology, Software, Writing–original draft. Sandra V. Kotsis: Conceptualization, Formal analysis, Methodology, Project administration, Resources, Supervision, Writing–review and editing. Anne V. Seyferth: Writing–original draft. Lu Wang: Formal analysis, Methodology, Software, Writing–review and editing. Kevin C. Chung: Conceptualization, Project administration, Supervision, Writing–review and editing.
REFERENCES
- 1.Bair YA, García JA, Romano PS, Siefkin AD, Kravitz RL. Does “mainstreaming” guarantee access to care for Medicaid recipients with asthma? J Gen Intern Med. 2001;16(7):475–481. doi: 10.1046/j.1525-1497.2001.016007475.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nyweide DJ, Anthony DL, Bynum JP, et al. Continuity of care and the risk of preventable hospitalization in older adults. JAMA Intern Med. 2013;173(20):1879–1885. doi: 10.1001/jamainternmed.2013.10059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wen H, Johnston KJ, Allen L, Waters TM. Medicaid expansion associated with reductions in preventable hospitalizations. Health Aff (Millwood) 2019;38(11):1845–1849. doi: 10.1377/hlthaff.2019.00483. [DOI] [PubMed] [Google Scholar]
- 4.Billings J, Zeitel L, Lukomnik J, Carey TS, Blank AE, Newman L. Impact of socioeconomic status on hospital use in New York City. Health Aff (Millwood) 1993;12(1):162–173. doi: 10.1377/hlthaff.12.1.162. [DOI] [PubMed] [Google Scholar]
- 5.Ayanian JZ, Weissman JS, Schneider EC, Ginsburg JA, Zaslavsky AM. Unmet health needs of uninsured adults in the United States. J Am Med Assoc. 2000;284(16):2061–2069. doi: 10.1001/jama.284.16.2061. [DOI] [PubMed] [Google Scholar]
- 6.Cheng EM, Chen A, Cunningham W. Primary language and receipt of recommended health care among Hispanics in the United States. J Gen Intern Med. 2007;22(suppl 2):283–288. doi: 10.1007/s11606-007-0346-6. 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krahn GL, Hammond L, Turner A. A cascade of disparities: health and health care access for people with intellectual disabilities. Ment Retard Dev Disabil Res Rev. 2006;12(1):70–82. doi: 10.1002/mrdd.20098. [DOI] [PubMed] [Google Scholar]
- 8.Bodenheimer T, Pham HH. Primary care: current problems and proposed solutions. Health Aff (Millwood) 2010;29(5):799–805. doi: 10.1377/hlthaff.2010.0026. [DOI] [PubMed] [Google Scholar]
- 9.Brown ER, Ojeda VD, Wyn R, Levan R. Racial and ethnic disparities in access to health insurance and health care. Popul Res Policy Rev. 2017;36(2):181–201. doi: 10.1007/s11113-016-9416-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zuvekas SH, Taliaferro GS. Pathways to access: health insurance, the health care delivery system, and racial/ethnic disparities, 1996–1999. Health Aff (Millwood) 2003;22(2):139–153. doi: 10.1377/hlthaff.22.2.139. [DOI] [PubMed] [Google Scholar]
- 11.Kao YH, Lin WT, Chen WH, Wu SC, Tseng TS. Continuity of outpatient care and avoidable hospitalization: a systematic review. Am J Manag Care. 2019;25(4):e126–e134. [PubMed] [Google Scholar]
- 12.Mahmoudi E, Kamdar N, Furgal A, Sen A, Zazove P, Bynum J. Potentially preventable hospitalizations among older adults: 2010–2014. Ann Fam Med. 2020;18(6):511–519. doi: 10.1370/afm.2605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adkinson JM, Chung KC. The patient protection and affordable care act: A primer for hand surgeons. Hand Clin. 2014;30(3):345–352. doi: 10.1016/j.hcl.2014.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ward BW, Clarke TC, Nugent CN, Schiller JS. National Center for Health Statistics, Centers for Disease Control and Prevention; Atlanta, GA: May 2016. Early release of selected estimates based on data from the 2015 National Health Interview Survey.https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwiAv8m0ouv5AhVjUHwKHRsuBycQFnoECA8QAQ&url=https%3A%2F%2Fwww.cdc.gov%2Fnchs%2Fdata%2Fnhis%2Fearlyrelease%2Fearlyrelease201605.pdf&usg=AOvVaw1BSDqBaoSLTo0TeedE00cl [Google Scholar]
- 15.Sommers BD, Blendon RJ, Orav EJ, Epstein AM. Changes in utilization and health among low-income adults after Medicaid expansion or expanded private insurance. JAMA Intern Med. 2016;176(10):1501–1509. doi: 10.1001/jamainternmed.2016.4419. [DOI] [PubMed] [Google Scholar]
- 16.Overview of the National (Nationwide) Inpatient Sample (NIS). Agency for Healthcare Research and Quality. https://www.hcup-us.ahrq.gov/nisoverview.jsp. Updated September 13, 2021. Accessed November 17, 2021.
- 17.Bindman AB, Grumbach K, Osmond D, et al. Preventable hospitalizations and access to health care. J Am Med Assoc. 1995;274(4):305–311. doi: 10.1001/jama.274.4.305. [DOI] [PubMed] [Google Scholar]
- 18.Prevention quality indicators technical specifications. Agency for Healthcare Research and Quality. https://qualityindicators.ahrq.gov/archive/pqi_techspec/icd10_v2019. Accessed November 17, 2021.
- 19.Description of data elements. Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality.https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwj3j9ympOv5AhUS9zgGHacICHsQFnoECAsQAQ&url=https%3A%2F%2Fwww.hcup-us.ahrq.gov%2Fdb%2Fnation%2Fnis%2Fnisdde.jsp&usg=AOvVaw15Yg7hB8ZdMQ-zGAorPhfO. Updated October 14, 2021. Accessed November 17, 2021.
- 20.Kominski GF, Nonzee NJ, Sorensen A. The Affordable Care Act's impacts on access to insurance and health care for low-income populations. Annu Rev Public Health. 2017;38:489–505. doi: 10.1146/annurev-publhealth-031816-044555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Courtemanche C, Marton J, Ukert B, Yelowitz A, Zapata D. Effects of the Affordable Care Act on health care access and self-assessed health after 3 years. Inq J Health Care Organ Provision Financ. 2018;55 doi: 10.1177/0046958018796361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.De Alba I, Amin A. Pneumonia readmissions: risk factors and implications. Ochsner Journal. 2014;14(4):649–654. PMID: 25598730. [PMC free article] [PubMed] [Google Scholar]
- 24.Librero J, Ibañez-Beroiz B, Peiró S, et al. Trends and area variations in Potentially Preventable Admissions for COPD in Spain (2002–2013): a significant decline and convergence between areas. BMC Health Serv Res. 2016;16(1):367. doi: 10.1186/s12913-016-1624-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Norbeck TB. Drivers of health care costs: a physicians foundation white paper-second of a three-part series. Mo Med. 2013;110(2):113–118. PMID: 23724476. [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang Y, Ancker JS, Hall J, Khullar D, Wu Y, Kaushal R. Association between residential neighborhood social conditions and health care utilization and costs. Med Care. 2020;58(7):586–593. doi: 10.1097/MLR.0000000000001337. [DOI] [PubMed] [Google Scholar]
- 27.Doshi RP, Aseltine RH, Sabina AB, Graham GN. Racial and ethnic disparities in preventable hospitalizations for chronic disease: prevalence and risk factors. J Racial Ethn Health Disparities. 2017;4(6):1100–1106. doi: 10.1007/s40615-016-0315-z. [DOI] [PubMed] [Google Scholar]
- 28.McCullough JM, Curwick K. Local health and Social Services spending to reduce preventable hospitalizations. Popul Health Manag. 2020;23(6):453–458. doi: 10.1089/pop.2019.0195. [DOI] [PubMed] [Google Scholar]
- 29.McCullough JM, Leider JP. Government spending in health and nonhealth sectors associated with improvement in county health rankings. Health Aff (Millwood) 2016;35(11):2037–2043. doi: 10.1377/hlthaff.2016.0708. [DOI] [PubMed] [Google Scholar]
- 30.Allen L, Gian CT, Simon K. The impact of Medicaid expansion on emergency department wait times. Health Serv Res. 2022;57(2):294–299. doi: 10.1111/1475-6773.13892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lyu W, Wehby GL. The impacts of the ACA Medicaid expansions on cancer screening use by primary care provider supply. Med Care. 2019;57(3):202–207. doi: 10.1097/MLR.0000000000001053. [DOI] [PubMed] [Google Scholar]
- 32.Kaiser Family Foundation. Status of state Medicaid expansion decision: interactive Map. San Francisco, CA: Kaiser Family Foundation. https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/. Accessed June 21, 2022.
- 33.Kleinman JC, Gold M, Makuc D. Use of ambulatory medical care by the poor: another look at equity. Med Care. 1981;19(10):1011–1029. doi: 10.1097/00005650-198110000-00004. [DOI] [PubMed] [Google Scholar]
- 34.Freeman HE, Blendon RJ, Aiken LH, Sudman S, Mullinix CF, Corey CR. Americans report on their access to health care. Health Aff (Millwood) 1987;6(1):6–8. doi: 10.1377/hlthaff.6.1.6. [DOI] [PubMed] [Google Scholar]
- 35.Moy E, Chang E, Barrett M. Centers for Disease Control and Prevention (CDC). Prevention. Potentially preventable hospitalizations—United States, 2001–2009. MMWR Suppl. 2013;62(3):139–143. PMID: 24264504. [PubMed] [Google Scholar]