Abstract
Influenza virus neuraminidase (NA) can act as a receptor-binding protein, a role commonly attributed to hemagglutinin (HA). In influenza A(H3N2) viruses, three NA amino acid residues have previously been associated with NA-mediated hemagglutination: T148, D151, and more recently, H150. These residues are part of the 150-loop of the NA monomer. Substitutions at 148 and 151 arise from virus propagation in laboratory cell cultures, whereas changes at 150 occurred during virus evolution in the human host. In this study, we examined the effect of natural amino acid polymorphism at position 150 on NA-mediated hemagglutination. Using the A/Puerto Rico/8/34 backbone, we generated a comprehensive panel of recombinant A(H3N2) viruses that have different NAs but shared an HA that displays poor binding to red blood cells (RBCs). None of the tested substitutions at 150 (C, H, L, R, and S) promoted NA-binding. However, we identified two new determinants of NA-binding, Q136K and T439R, that emerged during virus culturing. Similar to T148I, both Q136K and T439R reduced NA enzyme activity by 48–86% and inhibition (14- to 173-fold) by the NA inhibitor zanamivir. NA-binding was observed when a virus preparation contained approximately 10% of NA variants with either T148I or T439R, highlighting the benefit of using deep sequencing in virus characterization. Taken together, our findings provide new insights into the molecular mechanisms underlying the ability of NA to function as a binding protein. Information gained may aid in the design of new and improved NA-targeting antivirals.
Keywords: Host cell selection, 150-Loop, 430-Loop, Receptor-binding, Neuraminidase inhibitors
1. Introduction
Influenza is a respiratory infectious disease that can annually affect millions of people worldwide. Among seasonal influenza viruses, the A (H3N2) subtype is associated with the most severe epidemics (Budd et al., 2019; Simonsen et al., 1997; Kaji et al., 2003). Influenza A viruses are also known to cause pandemics (Nelson and Holmes, 2007). Vaccines and antiviral medications are used to prevent and control influenza infections in humans. Various platforms are used to generate licensed and experimental influenza vaccines, many of which include neuraminidase (NA) as an antigen (Estrada and Schultz-Cherry, 2019). The target for influenza inhibitors oseltamivir, zanamivir, peramivir, and laninamivir is the NA active site. Apart from marketed inhibitors, other NA-targeting compounds are in the development pipeline (Jones et al., 2023). Both surface glycoproteins, hemagglutinin (HA) and NA, interact with sialic acid-containing receptors during the virus replication cycle. The interplay between HA and NA functions is rather intricate, but it is well-recognized that HA initiates virus infection by binding to receptors on the surface of host cells, whereas NA destroys receptors by cleaving off the terminal sialic acid moieties (Wright et al., 2007). This NA activity is also needed to promote virus mobility in the upper respiratory tract (Wright et al., 2007; Zanin et al., 2015).
The ability of HA to bind to receptors on red blood cells (RBCs) is utilized in the hemagglutination assay, which is widely used for virus characterization and other purposes. Accumulation of mutations in the HA of A(H3N2) viruses during evolution and adaptation to the human host has led to altered binding preferences with recent viruses having preference for extended, branched human-type receptors (Gulati et al., 2013; Lin et al., 2012; Nobusawa et al., 2000; Peng et al., 2017; Yang et al., 2015). One manifestation of these changes is poor binding of recently circulating viruses to RBCs. The altered HA binding preferences also pose challenges to virus isolation in chicken eggs and can lead to the selection of NA variants during virus culturing in Madin-Darby canine kidney (MDCK) cells, a commonly used laboratory cell line (Lin et al., 2010; Mohr et al., 2015; Tamura et al., 2013; Zhu et al., 2012a). A (H3N2) viruses with NA amino acid substitution at the highly conserved catalytic residue D151 (e.g., D151G) reportedly display hemagglutination, which can be prevented by addition of oseltamivir (Lin et al., 2010; Zhu et al., 2012a). D151G was shown to drastically reduce NA catalytic activity (Mishin et al., 2014; Zhu et al., 2012a) and is often found as a mixture with wild-type D151 in MDCK-grown viruses, where G151 acts as the binding protein and D151 acts as the enzyme (Lin et al., 2010; Xue et al., 2016). Another NA substitution, T148I, which also arises during virus propagation in cells, promotes NA-mediated binding, and simultaneously reduces enzyme activity (Mohr et al., 2015; Tamura et al., 2013). Viruses with mutations at position 148 or 151 were shown to affect the assessment of susceptibility to NA inhibitors (Mishin et al., 2014; Tamura et al., 2013). Both 148 and 151 belong to the 150-loop formed by residues 147–152, which is adjacent to the catalytic site (Russell et al., 2006; Wu et al., 2013).
Recently, an H150R substitution within the 150-loop was associated with NA-mediated hemagglutination that can be blocked by oseltamivir and NA-specific antibodies (Mogling et al., 2017). Contrary to the cell culture-selected substitutions that occurred at the highly conserved residues 148 and 151, H150R is a naturally occurring amino acid substitution (Mogling et al., 2017). However, Brown et al. (2020) more recently reported that an A(H3N2) virus with R150 did not agglutinate RBCs. Since H150R became predominant in recently circulating viruses, we wanted to investigate whether the ability of H150R to mediate agglutination depends on the NA genetic background. Understanding whether substitutions at 150 can affect key NA functions would improve virus characterization. Here, we used a comprehensive panel of recombinant influenza A(H3N2) viruses to assess the role of substitutions at 150 and other NA residues in NA-mediated agglutination of RBCs.
2. Materials and methods
2.1. Cells and compounds
MDCK-SIAT1 cells (kindly provided by M. Matrosovich) were used to grow influenza viruses and assess their infectious titers. Human embryonic kidney HEK-293T (American Type Culture Collection) cells were used to rescue recombinant influenza viruses.
The NA inhibitors oseltamivir carboxylate (oseltamivir), zanamivir, peramivir, and laninamivir (Biosynth) were dissolved in sterile distilled water, filter sterilized, and stored at ≤−30 °C until use.
2.2. Viruses
Human A(H3N2) viruses submitted to the Centers for Disease Control and Prevention (CDC), Atlanta, GA as part of the WHO global surveillance program were used in this study. Parent stock of the A/Victoria/261/2011 (H3N2) (VI/11) virus was obtained from the International Reagent Resource (IRR).
2.3. Plasmid constructs, reverse genetics, and recombinant virus propagation
Reverse genetics (RG) plasmids containing the A/Puerto Rico/8/34 (PR8) gene segments were provided by Dr. Bin Zhou (CDC). The HA and NA genes from A(H3N2) viruses were amplified and inserted into the pHW2000 plasmid as described (Hoffmann et al., 2000). NA-containing plasmids with single amino acid substitutions of interest were generated by site-directed mutagenesis (Thermo Fisher Scientific). All RG plasmids were confirmed by sequencing before use. Stocks of recombinant viruses were prepared in MDCK-SIAT1 cells and harvested at 48h post-infection. Codon-complete genome sequences of RG viruses were obtained using next generation sequencing (NGS, see below) to confirm identity to sequences submitted in the Global Initiative on Sharing All Influenza Data (GISAID) (see accession nos. in Table S1).
2.4. Hemagglutination assay with NA inhibitor and neuraminidase inhibition (NI) assay
Hemagglutination assay was performed using 0.75% guinea pig and 0.5% turkey RBCs (Lampire Biological Labs) (WHO, 2011). Viruses were two-fold serially diluted in PBS with or without oseltamivir (20 nM) and incubated at room temperature for 1h. RBCs were then added, and titers (hemagglutination units/50 μL, HAU/50 μL) were recorded after 1h incubation at room temperature.
NA inhibition (NI) assay was performed using the NA-Fluor™ kit (Applied Biosystems), as previously described (Okomo-Adhiambo et al., 2010b). Briefly, normalized virus preparations were incubated in the presence of NA inhibitors for 45min prior to the addition of 2-(4-(methylumbelliferyl)-a-D-N-acetylneuraminic acid (MUNANA) substrate. After 1h incubation at 37°C, the reaction was terminated by the addition of the NA-Fluor™ stop solution and the fluorescence (excitation = 360 nm; emission = 460 nm) produced by 4-metheylumbelliferone (4-MU), a product of MUNANA cleaved by NA, was measured using Cytation 7 (Agilent-BioTek). Curve-fitting and determination of IC50 (the drug concentration required to inhibit NA activity by 50%) were done as previously described (Okomo-Adhiambo et al., 2010b). Mean and standard deviation was calculated from results collected from at least three independent tests.
2.5. Pyrosequencing and NGS
Virus preparations were made by mixing the NA mutant T439R virus with wild-type virus (WT) at different proportions (1.25%, 2.5%, 5%, and 50%) based on infectious titer. Similar preparations were made for the NA mutant T148I. These virus preparations were subjected to pyrosequencing analysis essentially as previously described (Levine et al., 2011) using PyroMark Q96 ID instrument (Qiagen). Primers for the analysis of amino acid residue 439 were designed with the use of Pyrosequencing Assay Design software (Qiagen). RT-PCR and sequencing primers for analysis of codon 148 in NA were previously described (Tamura et al., 2013). Allele quantitation mode was utilized to determine the proportion of mutant in the mixture. The nucleotide dispensation order was generated by PyroMark software.
Codon-complete influenza genome was amplified using Uni/Inf primer set and Super-Script III One-Step RT-PCR with Platinum Taq High Fidelity enzyme (Invitrogen). Illumina MiSeq was used to generate sequences that were analyzed by the IRMA approach with singlenucleotide variant threshold of 2% (Shepard et al., 2016).
2.6. Infectious virus titer
Infectious virus titer was determined by counting virus-infected cells using a single-cycle replication as described (Jorquera et al., 2019). In 96-well microplates (black clear bottom, Agilent), recombinant viruses were 10-fold serially diluted (10−1 to 10−7) in virus growth medium (VGM) without TPCK-trypsin. MDCK-SIAT1 cells in suspension (~4 × 104 cells) were added into wells containing diluted viruses and microplates were incubated at 37°C in 5% CO2 for 20 h. Supernatants were aspirated and cells were then fixed and immuno-stained with a mouse anti-nucleoprotein (NP) monoclonal antibody (1:1000; IRR) followed by secondary staining with goat anti-mouse IgG antibody conjugated to Alexa Fluor™ 555 (1:1000; Thermo Fisher Scientific) mixed with the DNA dye Hoechst 33258 (1:5000; AnaSpec). Fluorescence measurements were done (excitation = 555 nm; emission = 580 nm for Alexa Fluor and excitation = 350 nm and emission = 461 nm for Hoechst 33258) and virus-infected cells identified and counted using a high-content quantitative imaging platform Cytation 7. The infected cell counts were then used to calculate infectious virus titer (expressed as log10 infectious units/milliliter, IU/mL).
2.7. Measurement of NA activity
Effect of NA mutations on enzyme activity was assessed using Cytation 7 (see above) according to the following procedure. Recombinant viruses were two-fold serially diluted in VGM lacking TPCK-trypsin in 96-well microplates (Agilent) followed by addition of MDCK-SIAT1 cells in suspension. Microplates were then incubated for 20 h at 37° C with 5% CO2. The infected cell monolayers were used to assess NA enzyme activity per virus-infected cell.
First, to measure the enzyme activity of NA molecules expressed on the surface of virus-infected cells, supernatants were removed and 50 μL of 200 μM MUNANA substrate were added to each well on top of the cell monolayer. After 1h incubation at 37°C, the liquid from each well was transferred into a different 96-well clear bottom microplate (NA activity microplate, Thermo Fisher Scientific) followed by addition of 50 μL of stop solution. Fluorescence produced by 4-MU was read using Cytation 7 (excitation = 360 nm; emission = 460 nm). NA enzyme activity was expressed as relative fluorescence unit (RFU).
The same microplates with the infected cell monolayers were also used to count virus-infected cells and to assess the viral protein synthesis. Cell monolayers were fixed and processed as described in section 2.6 by immuno-staining with anti-NP antibody (primary), followed by staining with the secondary conjugated anti-IgG antibody, and the DNA dye. Immuno-stained cells were digitally imaged using Cytation 7 to identify and count virus-infected cells (overlapped DNA and NP staining). In addition, Cytation 7 was used to quantify NP protein in individual virus-infected cells. Wells containing virus-infected cells in a range from 500 to 3000 and showing a similar quantity of NP protein were used to calculate NA activity per infected cell (expressed as RFU per cell).
3. Results
3.1. Selection of H3 HA donor with weak hemagglutination activity
To study N2 NA-mediated binding, we used a PR8-based RG approach. First, we sought to identify a donor of H3 HA with inherently weak hemagglutination activity. To this end, three recombinant A (H3N1) viruses were generated that contained HAs from the three main subclades (3C.2a, 3C.3a, and 3C.3b) circulating in 2013–2015 (Table S2). These A(H3N1) viruses were examined for their ability to agglutinate turkey and guinea pig RBCs. Only the recombinant virus with HA from A/Alaska/140/2015, belonging to clade 3C.2a, displayed poor binding to RBCs tested despite having the highest infectivity titer (Table S2). Therefore, A/Alaska/140/2015 was chosen to be the HA donor for all recombinant A(H3N2) viruses generated in subsequent experiments.
3.2. Role of residue 150 in NA-mediated hemagglutination activity
To assess the role of NA residue 150 in agglutination of RBCs, we generated recombinant A(H3N2) viruses containing the NAs of A/Wyoming/3/2003 (WY/03) and A/New York/07/2010 (NY/10). These NAs were chosen because their deduced amino acid sequences match those of viruses used to demonstrate the role of H150R in NA-binding (Mogling et al., 2017) (Table S1). Based on that study, introduction of H150R in WY/03-NA should have led to NA-mediated hemagglutination, and yet this was not observed (Table 1). Moreover, NY/10-NA with naturally occurring H150R also did not demonstrate detectable hemagglutination. Meanwhile, introduction of T148I, used as a positive control for NA-mediated binding, conferred hemagglutination when introduced in NAs of both WY/03 and NY/10. Expectedly, hemagglutination by these viruses was not observed in the presence of oseltamivir (Table 1).
Table 1.
Effect of NA substitutions at residues 148 and 150 on NA-mediated hemagglutination of recombinant A(H3N2) viruses.
| Source of NA | NA amino acid at residue | Infectivity (log10 IU/ml) | Hemagglutination titer (HAU/50 μl) |
NA-mediated binding | ||||
|---|---|---|---|---|---|---|---|---|
| |
Turkey RBCsc |
Guinea pig RBCs |
||||||
| 148 | 150 | − Osed | + Ose | − Ose | + Ose | |||
| A/Wyoming/3/2003a | T | H | 7.4 ± 0.1 | <2 | <2 | <2 | <2 | No |
| T | R | 7.8 ± 0.1 | <2 | <2 | <2 | <2 | No | |
|
|
I
|
H |
7.7 ± 0.1 |
16 |
<2 |
32 |
<2 |
Yes |
| A/New York/07/2010b | T | R | 8.1 ± 0.4 | <2 | <2 | <2 | <2 | No |
| I | R | 7.4 ± 0.4 | 128 | <2 | 256 | <2 | Yes | |
Recombinant A(H3N2) viruses containing the HA from A/Alaska/140/2015 (H3N2) and NA from designated viruses were generated in the background of A/Puerto Rico/8/34 (H1N1) through reverse genetics. Boldface amino acid indicates substitution.
NA amino acid sequence is identical to A/Netherlands/109/2003.
NA amino acid sequence is identical to A/Netherlands/761/2009.
RBCs, red blood cells.
Oseltamivir, 20 nM.
To further examine the role of residue 150, we generated a panel of 10 recombinant viruses with NAs displaying natural amino acid polymorphisms (C, H, L R, or S) at this position (Table S1). Only the one recombinant virus containing NA of A/Victoria/361/2011 (VI/11-NA) with R at 150 displayed hemagglutination (Table 2). Notably, hemagglutination activity of this virus was not observed in the presence of oseltamivir, confirming NA-mediated binding. However, R at 150 was not a determinant of NA-binding since the reversion to H (R150H) had no effect on hemagglutination (Table 2). Moreover, NGS analysis of VI/11-NA did not reveal substitutions at residue 148 or 151.
Table 2.
Identification of the molecular determinant responsible for the NA-mediated binding of the recombinant A/Victoria/361/2011(H3N2) virus.
| NA amino acid at residue | Infectivity (log10 IU/ml) | Hemagglutination titer (HAU/50 μl) |
NA-mediated binding | ||||||
|---|---|---|---|---|---|---|---|---|---|
| |
Turkey RBCsa |
Guinea pig RBCs |
|||||||
| 150 | 258 | 329 | 439 | − Oseb | + Ose | − Ose | + Ose | ||
| R | K | T | R | 8.1 ± 0.3 | 128 | <2 | 512 | 2 | Yes |
| H | K | T | R | 7.8 ± 0.5 | 128 | <2 | 512 | 2 | Yes |
| R | E | T | R | 7.6 ± 0.1 | 128 | <2 | 512 | 2 | Yes |
| R | K | N | R | 7.6 ± 0.2 | 128 | <2 | 512 | 2 | Yes |
| R |
K |
T |
T
|
8.2 ± 0.1 |
<2 |
<2 |
<2 |
2 |
No |
| R | K | T | A | 7.5 ± 0.1 | <2 | <2 | <2 | <2 | No |
| R | K | T | I | Not rescued | - | - | - | - | - |
| R | K | T | K | 7.6 ± 0.2 | 128 | <2 | 512 | <2 | Yes |
| R | K | T | P | Not rescued | - | - | - | - | - |
| R | K | T | S | 7.7 ± 0.1 | <2 | <2 | <2 | <2 | No |
| R | K | T | T | 8.2 ± 0.1 | <2 | <2 | <2 | <2 | No |
Recombinant PR8-based A(H3N2) viruses containing the NA from A/Victoria/361/2011 were generated by reverse genetics. Unique NA amino acid sequence at positions 258, 329, and 439 were sequentially reverted to wild-type sequences by site-directed mutagenesis. In addition, other naturally occurring mutations (boldface) at residue 439, identified from NA sequences deposited in GISAID, were also examined for their role in NA-binding. Dash lines (–) indicate no data to show as these variants failed to be rescued.
RBCs, red blood cells.
Oseltamivir, 20 nM.
3.3. Role of residue 439 in NA-mediated hemagglutination activity
Comparison of NA sequences revealed that VI/11-NA differed in residues at positions 258, 329, and 439, none of which belong to the enzyme active site (Table S1). To identify which residue is responsible for NA-binding, we sequentially introduced mutations at each position. Neither K258E nor T329N affected NA-binding, however, R439T resulted in the loss of hemagglutination (Tables 2 and 3). To confirm the role of T439R in NA-binding, it was introduced into the NAs of A/Texas/50/2012 and A/Switzerland/9715293/2013. In both genetic backgrounds, T439R conferred hemagglutination, which was abrogated by oseltamivir (Table 3). Interestingly, NA-mediated binding was preserved when another basic, positively charged amino acid lysine (K) was introduced at 439 in VI/11-NA, underscoring the apparent significance of the side chain (Table 2).
Table 3.
Role of the cell culture-selected Q136K substitution in NA-mediated binding of recombinant A(H3N2) viruses.
| Source of NA | NA amino acid at residue | Infectivity (log10 IU/ml) | Hemagglutination titer (HAU/50 μl) |
NA-mediated binding | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| |
Turkey RBCsa |
Guinea pig RBCs |
||||||||
| 136 | 148 | 150 | 439 | − Oseb | + Ose | − Ose | + Ose | |||
| A/Victoria/361/2011 | Q | T | R | R | 8.1 ± 0.3 | 128 | <2 | 512 | 2 | Yes |
| Q | T | R | T | 8.2 ± 0.1 | <2 | <2 | <2 | <2 | No | |
| |
K
|
T |
R |
T |
7.7 ± 0.1 |
64 |
<2 |
256 |
<2 |
Yes |
| A/Texas/50/2012 | Q | T | H | T | 7.6 ± 0.3 | <2 | <2 | <2 | <2 | No |
| Q | T | H | R | 8.0 ± 0.3 | 128 | <2 | 512 | 2 | Yes | |
| |
K
|
T |
H |
T |
6.7 ± 0.1 |
32 |
<2 |
128 |
2 |
Yes |
| A/Switzerland/9715293/2013 | Q | T | R | T | 7.8 ± 0.3 | <2 | <2 | <2 | <2 | No |
| Q | T | H | R | 7.9 ± 0.3 | 128 | <2 | 512 | 2 | Yes | |
| K | T | R | T | 6.6 ± 0.3 | 32 | <2 | 128 | 2 | Yes | |
Recombinant PR8-based A(H3N2) viruses containing the NAs of the designated viruses were generated. Amino acid sequence at indicated positions were substituted (boldface) by site-directed mutagenesis.
RBCs, red blood cells.
Oseltamivir, 20 nM.
T439 is a highly conserved residue (Yasuhara et al., 2022) and analysis of 63,871 sequences from GISAID (1968–2022) showed that amino acid polymorphism at 439 was only seen in 11 other viruses (six A439, two I439, one P439, and two S439) (Table S3). Replacement of R with A or S at 439 in VI/11-NA abolished hemagglutination activity, while attempts to rescue viruses with I or P at 439 were unsuccessful (Table 2). It is worth noting that apart from the virus isolate used in our study, all other NA sequences of VI/11, a vaccine strain, deposited in GISAID contain T at 439 (Table S4). Using pyrosequencing, we determined that the virus isolate that was used as a donor of NA in this study contained a mixture of R (85%) and T (15%) at 439 (Fig. S1). Therefore, we believe that R439 is a cell-selected substitution that arose during the extended culturing of VI/11 in MDCK cells. Some NA sequences of this virus show substitution associated with NA-binding (e.g., 151 D/G), but such variants were not detected in our virus stock (Table S4).
3.4. Proportion of R439 variant population that confers NA-mediated hemagglutination
Next, we wanted to know at what proportion the presence of NA variants can manifest NA-mediated hemagglutination. To this end, RG viruses with T439 and R439 in VI/11-NA background were mixed, and the proportions of the mutant were determined using pyrosequencing and NGS analyses. These mixtures were then tested in hemagglutination assays. Hemagglutination (≥8 HAUs) was observed when as little as 6–7% of R439 NA variant was detected in the virus preparation.
Similarly, virus mixtures containing various proportions of T148 and I148 were prepared and tested. In this instance, 7–9% of the mutant I148 was sufficient to observe hemagglutination (8–16 HAUs) (Table S5).
3.5. Effect of T439R on NA enzyme activity and drug susceptibility
Because the hydrogen bond (H-bond) formed between the two threonines at 148 and 439 is implicated in the rigidity of the 150-loop (Wu et al., 2013), substitutions at either position should increase flexibility of the 150-loop, thereby producing a similar effect on NA function (Fig. 1B). Using recombinant NA proteins, we previously showed that T148I caused ~50% reduction in NA activity (Tamura et al., 2013). Therefore, we wanted to know whether the substitution at T439 would also reduce NA enzyme activity. Indeed, the enzyme activity of the recombinant virus with T439R in the VI/11-NA genetic background was reduced by ~86% (Fig. 1A, Table S6). Introduction of A or S at position 439 produced little or no effect, indicating the importance of the residue’s side chain. Similar to T439R, T148I was accompanied by ~53% reduction in enzyme activity. Both T148I and T439R substitutions conferred 5- to 14-fold reduced inhibition by zanamivir, while showing little or no effect on inhibition by the other three NA inhibitors (Table 4). Therefore, both T148I and T439R substitutions not only conferred NA-mediated binding, but also reduced NA enzyme activity and weakened interaction with zanamivir (Fig. 1A, Table 4). Conversely, substitutions at position 150 neither induced agglutination (Table S1) nor affected inhibition by zanamivir (Table 4). Although R150H and R150S substitutions did not affect enzyme activity of VI/11 NA, the later change reduced it by ~47% when introduced into the NA of A/Darwin/06/2021, a recent vaccine strain (Fig. 1A, Tables S6–S7).
Fig. 1.
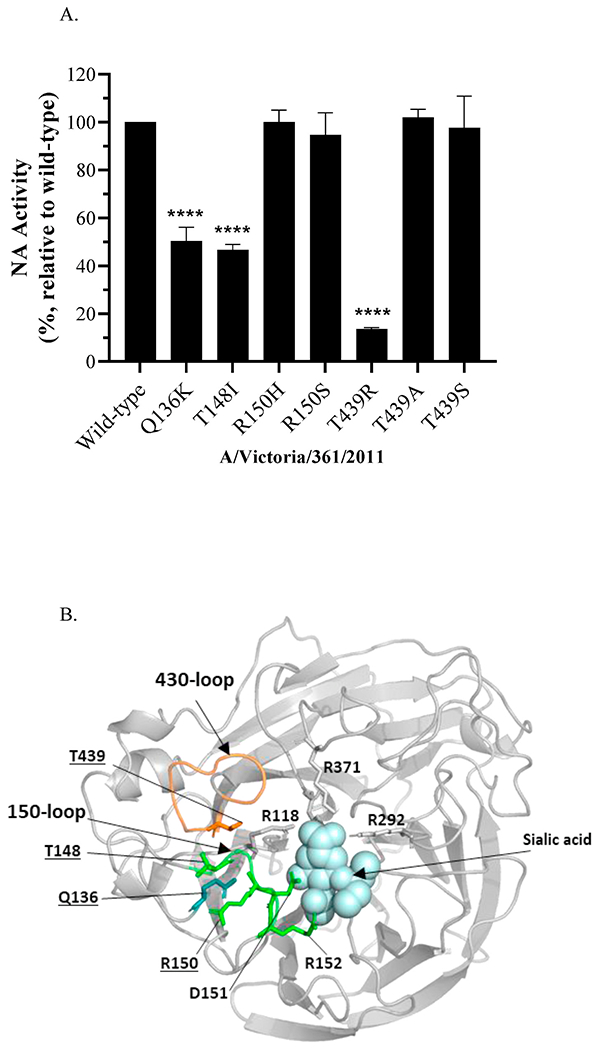
(A) Effect of NA substitutions on enzyme activity of recombinant PR8-based A(H3N2) viruses (see Table 1 footnote) containing the A/Victoria/361/2011 NA. The wild-type NA contains Q136, T148, R150, and T439 residues. Measurement of NA enzyme activity was performed in three independent experiments in three replicates. Differences in NA activity (presented as the percentage relative to wild-type) were compared using ordinary one-way analysis of variance, followed by Dunnett’s multiple comparison post hoc tests (GraphPad Prism v9). ****p < 0.0001, relative to wild-type. (B) The N2 NA monomer was visualized in a ribbon representation based on the structural information of the A/Tanzania/205/2010 (H3N2) NA protein (PDB ID: 4GZX) using PyMOL software. The residues examined in this study (136,148,150, and 439) are underlined and shown in stick representation. The following catalytic residues R118, D151, R152, R292, and R371 are shown. The residues located in the 150-loop and 430-loop are shown in green and orange, respectively.
Table 4.
Effect of NA substitutions on the drug susceptibility of recombinant A(H3N2) viruses carrying the NA from A/Victoria/361/2011.
| Amino acid at residue |
NA-mediated binding | IC50, nM (fold-change)a |
||||||
|---|---|---|---|---|---|---|---|---|
| 136 | 148 | 150 | 439 | Zanamivir | Oseltamivir | Peramivir | Laninamivir | |
| Q | T | R | T | No | 0.22 ± 0.02 | 0.13 ± 0.02 | 0.07 ± 0.01 | 0.28 ± 0.04 |
| Q | T | R | R | Yes | 3.15 ± 1.21 (14) | 0.16 ± 06 (1) | 0.24 ± 0.04 (3) | 1.15 ± 0.15 (4) |
| Q | I | R | T | Yes | 1.16 ± 0.20 (5) | 0.07 ± 0.01 (1) | 0.09 ± 0.01 (1) | 0.47 ± 0.03 (2) |
| Q | T | H | T | No | 0.24 ± 0.02 (1) | 0.14 ± 0.01 (1) | 0.08 ± 0.01 (1) | 0.33 ± 0.02 (1) |
| K | T | R | T | Yes | 37.96 ± 3.5 (173) | 0.06 ± 0.01 (1) | 0.56 ± 0.09 (8) | 11.23 ± 0.65 (40) |
Susceptibility of recombinant PR8-based A(H3N2) viruses containing A/Victoria/361/2011 NA with substitutions (boldface) of interest were examined in NA inhibition assay. Data shown are the average of four repeats ± standard deviation.
Based on comparing the IC50s of the virus containing wild-type NA sequence Q136, T148, R150, and T439.
3.6. Role of residue 136 in NA-mediated hemagglutination
Substitution of the conserved glutamine (Q) at position 136 with K or R has been reported in MDCK-grown A(H3N2) viruses (Little et al., 2015; Okomo-Adhiambo et al., 2014). Like the T148-T439 interaction, the H-bond between Q136 and H150 was also implicated in the rigidity of the 150-loop (Wu et al., 2013) (Fig. 1B). This prompted us to investigate whether substitution at residue 136 can also promote NA-mediated hemagglutination. Indeed, introduction of Q136K resulted in efficient agglutination of RBCs that was prevented by oseltamivir (Table 4). Furthermore, NA-mediated hemagglutination was also observed when Q136K was introduced into the NAs of two other viruses, indicating that this observed property was not strain-specific (Table 3). These results show for the first time that Q136K can independently promote NA-mediated hemagglutination. Moreover, as with T148I and T439R, introduction of Q136K decreased enzyme activity by ~48% and resulted in 173-fold reduced inhibition by zanamivir; 8- to 40-fold reduced inhibition by peramivir and laninamivir was also observed (Fig. 1 and Table 3).
4. Discussion
Observations made in this study provide new insights into molecular determinants responsible for altering the functional activities of NA. It is known that propagation of influenza A(H3N2) viruses in laboratory cell cultures can lead to mutations that allow NA to play the non-classical role of a receptor-binding protein, a function typically associated with HA. NA-mediated attachment to cell receptors is needed to achieve optimal virus replication when HA exhibits weak binding, but it consequently results in lower enzyme activity. Unlike what is found in nature, strong NA activity is not required for viruses propagated in MDCK cells, as this laboratory cell line does not produce mucins that would entrap virus particles with a defective enzyme. Therefore, MDCK cells provide an environment that is permissive to the re-distribution of the receptor-binding function between HA and NA. Several studies have revealed that D151G and T148I confer NA-binding (Brown et al., 2020; Lin et al., 2010; Mohr et al., 2015; Tamura et al., 2013). D151 is a catalytic residue that directly participates in the cleavage of the substrate (Colman et al., 1983). Zhu et al. (2012a) showed that D151G increases sialic acid binding affinity while decreasing catalytic activity of NA. Here we discovered two new determinants, Q136K and T439R, that are also responsible for NA-mediated hemagglutination. The effect of Q136K on enzyme activity and antiviral susceptibility was previously reported (Dapat et al., 2010; Little et al., 2015; Okomo-Adhiambo et al., 2014), but no association was made with respect to NA-dependent hemagglutination.
Other than D151G, the exact mechanisms by which the identified substitutions at other residues lead to receptor-binding remain unknown. NA-mediated hemagglutination can be prevented by NA inhibitors, indicating the involvement of the enzyme active site (Mohr et al., 2015). The NA catalytic and receptor-binding sites overlap, but are not the same, since different concentrations of NA inhibitor is needed to affect enzyme activity and binding (Mohr et al., 2015). Like D151, T148 belongs to the 150-loop adjacent to the catalytic site. The conformation of this loop is implicated in forming the 150-cavity, a target for structure-based drug design (reviewed in Grienke et al., 2012). It was reported that T148 contributes to the rigidity of the 150-loop by making an H-bond with T439 (Wu et al., 2013), which belongs to the neighboring 430-loop (Amaro et al., 2007; Zhu et al., 2012b). Amaro et al. (2007) also described how the coordinated movements of the 150-and 430-loops can significantly expand the cavity of the active site. In addition to T148 and T439, Q136 also contributes to the rigidity of the 150-loop by participating in the network of interactions with nearby amino acids (Wu et al., 2013). All three NA-binding determinants examined in this study, Q136K, T148I, and T439R, reduced NA enzyme activity and inhibition by zanamivir. Therefore, it is tempting to assume that each of these substitutions can independently increase the flexibility of the 150-loop, thereby allowing for structural changes (e.g., formation of 150-cavity that expands the enzyme active site) resulting in the dual NA functionality.
Residue 150, which is non-catalytic, is located on the edge of the active site (Russell et al., 2006; Wu et al., 2013). Because it is flanked by 148 and 151, it was reasonable to suspect that 150 could also play a role in NA-mediated hemagglutination (Mogling et al., 2017). However, our introduction of H150R into different backgrounds did not lead to NA-binding. Moreover, our data showed that other substitutions at 150 that are found in recently circulating viruses, including vaccine strains (e.g., S150 in A/Darwin/9/2021), also did not confer NA-binding. The misidentification of H150R as an NA-binding determinant most likely stemmed from the use of Sanger sequence analysis, which lacks the necessary sensitivity to detect minor virus populations. Indeed, we and others (Mohr et al., 2015) show that a minor population of T148I (<10%) was sufficient to produce hemagglutination titers. In this study we also showed that 6–12% of T439R was sufficient to agglutinate RBCs. Hence, our findings underscore the importance of sequence confirmation after virus culturing, preferably using deep sequencing methods.
Brown et al. (2020) showed that A(H3N2) viruses that acquire NA-binding mutations T148I or D151G revert to wild-type after a single passage in human airway epithelial cells, a mucin-rich environment where NA activity is needed to prevent entrapment of virus particles. In our study, we did not assess replicative fitness of NA-binding mutants with Q136K and T439R in human airway epithelial cells. However, it is likely that their fitness would also be compromised due to reduced NA enzyme activity. Importantly, NA-binding mutants encoding these substitutions (Q136K, T148, D151G, and T439R) are very rare in original human specimens but are found in MDCK cell-propagated viruses (Dapat et al., 2010; Mohr et al., 2015; Tamura et al., 2013; this study).
Apart from A(H3N2) viruses, cell-selected NA variants can also emerge during propagation of A(H1N1) and type B viruses (Brown et al., 2022; Hurt et al., 2016; McKimm-Breschkin et al., 2003; Okomo-Adhiambo et al., 2010a), including those implicated in NA-binding (Hooper and Bloom, 2013). Virus propagation in genetically modified MDCK cell lines has been shown to help mitigate the selection of cell culture-associated NA mutations (Oh et al., 2008; Takada et al., 2019; Tamura et al., 2013) and thus, are preferred for virus isolation and propagation. Alternatively, it was demonstrated that human airway epithelial cells can select against NA-binding variants, thereby reverting the virus population to wild-type (Brown et al., 2020). Additional studies, using molecular dynamics and other approaches, are needed to elucidate the precise mechanisms by which the NA substitutions described here are able to promote NA-binding. Observations made in this study may provide information that could be used for structure-based design of new or improved NA-targeting antivirals.
Supplementary Material
Acknowledgements
We acknowledge Juan De La Cruz and other colleagues from the Virology Surveillance and Diagnosis Branch, Influenza Division, CDC, for their valuable support and contributions to this project. We also thank our collaborators in the U.S. public health laboratories for the submission of influenza virus isolates and clinical specimens.
Financial Support
This work was supported by the Influenza Division, CDC.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention.
Footnotes
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.antiviral.2023.105719.
Data availability
Data will be made available on request.
References
- Amaro RE, Minh DD, Cheng LS, Lindstrom WM Jr., Olson AJ, Lin JH, Li WW, McCammon JA, 2007. Remarkable loop flexibility in avian influenza N1 and its implications for antiviral drug design. J. Am. Chem. Soc 129, 7764–7765. [DOI] [PubMed] [Google Scholar]
- Brown JC, Barclay WS, Galiano M, Harvey R, 2020. Passage of influenza A/H3N2 viruses in human airway cells removes artefactual variants associated with neuraminidase-mediated binding. J. Gen. Virol 101, 456–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SK, Tseng YY, Aziz A, Baz M, Barr IG, 2022. Characterization of influenza B viruses with reduced susceptibility to influenza neuraminidase inhibitors. Antivir. Res 200, 105280. [DOI] [PubMed] [Google Scholar]
- Budd AP, Beacham L, Smith CB, Garten RJ, Reed C, Kniss K, Mustaquim D, Ahmad FB, Cummings CN, Garg S, Levine MZ, Fry AM, Brammer L, 2019. Birth cohort effects in influenza surveillance data: evidence that first influenza infection. Affects Later Influenza-Associated Illness 220, 820–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colman PM, Varghese JN, Laver WG, 1983. Structure of the catalytic and antigenic sites in influenza virus neuraminidase. Nature 303, 41–44. [DOI] [PubMed] [Google Scholar]
- Dapat C, Suzuki Y, Saito R, Kyaw Y, Myint YY, Lin N, Oo HN, Oo KY, Win N, Naito M, Hasegawa G, Dapat IC, Zaraket H, Baranovich T, Nishikawa M, Saito T, Suzuki H, 2010. Rare influenza A (H3N2) variants with reduced sensitivity to antiviral drugs. Emerg. Infect. Dis 16, 493–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estrada LD, Schultz-Cherry S, 2019. Development of a universal influenza vaccine. J. Immunol 202, 392–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grienke U, Schmidtke M, von Grafenstein S, Kirchmair J, Liedl KR, Rollinger JM, 2012. Influenza neuraminidase: a druggable target for natural products. Nat. Prod. Rep 29, 11–36. [DOI] [PubMed] [Google Scholar]
- Gulati S, Smith DF, Cummings RD, Couch RB, Griesemer SB, St George K, Webster RG, Air GM, 2013. Human H3N2 influenza viruses isolated from 1968 to 2012 show varying preference for receptor substructures with No apparent consequences for disease or spread. PLoS One 8, e66325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann E, Neumann G, Kawaoka Y, Hobom G, Webster RG, 2000. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc. Natl. Acad. Sci. U. S. A 97, 6108–6113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooper KA, Bloom JD, 2013. A mutant influenza virus that uses an N1 neuraminidase as the receptor-binding protein. J. Virol 87, 12531–12540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurt AC, Besselaar TG, Daniels RS, Ermetal B, Fry A, Gubareva L, Huang W, Lackenby A, Lee RT, Lo J, Maurer-Stroh S, Nguyen HT, Pereyaslov D, Rebelo-de-Andrade H, Siqueira MM, Takashita E, Tashiro M, Tilmanis D, Wang D, Zhang W, Meijer A, 2016. Global update on the susceptibility of human influenza viruses to neuraminidase inhibitors, 2014-2015. Antivir. Res 132, 178–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jorquera PA, Mishin VP, Chesnokov A, Nguyen HT, Mann B, Garten R, Barnes J, Hodges E, De La Cruz J, Xu X, Katz J, Wentworth DE, Gubareva LV, 2019. Insights into the antigenic advancement of influenza A(H3N2) viruses, 2011-2018. Sci. Rep 9, 2676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones JC, Yen HL, Adams P, Armstrong K, Govorkova EA, 2023. Influenza antivirals and their role in pandemic preparedness. Antivir. Res 210, 105499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaji M, Watanabe A, Aizawa H, 2003. Differences in Clinical Features between Influenza A H1N1, A H3N2, and B in Adult Patients, 8, pp. 231–233. [DOI] [PubMed] [Google Scholar]
- Levine M, Sheu TG, Gubareva LV, Mishin VP, 2011. Detection of hemagglutinin variants of the pandemic influenza A (H1N1) 2009 virus by pyrosequencing. J. Clin. Microbiol 49, 1307–1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin YP, Gregory V, Collins P, Kloess J, Wharton S, Cattle N, Lackenby A, Daniels R, Hay A, 2010. Neuraminidase receptor binding variants of human influenza A(H3N2) viruses resulting from substitution of aspartic acid 151 in the catalytic site: a role in virus attachment? J. Virol 84, 6769–6781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin YP, Xiong X, Wharton SA, Martin SR, Coombs PJ, Vachieri SG, Christodoulou E, Walker PA, Liu J, Skehel JJ, Gamblin SJ, Hay AJ, Daniels RS, McCauley JW, 2012. Evolution of the receptor binding properties of the influenza A(H3N2) hemagglutinin. Proc. Natl. Acad. Sci. U. S. A 109, 21474–21479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little K, Leang SK, Butler J, Baas C, Harrower B, Mosse J, Barr IG, Hurt AC, 2015. Zanamivir-resistant influenza viruses with Q136K or Q136R neuraminidase residue mutations can arise during MDCK cell culture creating challenges for antiviral susceptibility monitoring. Euro Surveill. 20. [DOI] [PubMed] [Google Scholar]
- McKimm-Breschkin J, Trivedi T, Hampson A, Hay A, Klimov A, Tashiro M, Hayden F, Zambon M, 2003. Neuraminidase sequence analysis and susceptibilities of influenza virus clinical isolates to zanamivir and oseltamivir. Antimicrob. Agents Chemother 47, 2264–2272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishin VP, Sleeman K, Levine M, Carney PJ, Stevens J, Gubareva LV, 2014. The effect of the MDCK cell selected neuraminidase D151G mutation on the drug susceptibility assessment of influenza A(H3N2) viruses. Antivir. Res 101, 93–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mogling R, Richard MJ, Vliet SV, Beek RV, Schrauwen EJA, Spronken MI, Rimmelzwaan GF, Fouchier RAM, 2017. Neuraminidase-mediated haemagglutination of recent human influenza A(H3N2) viruses is determined by arginine 150 flanking the neuraminidase catalytic site. J. Gen. Virol 98, 1274–1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr PG, Deng YM, McKimm-Breschkin JL, 2015. The neuraminidases of MDCK grown human influenza A(H3N2) viruses isolated since 1994 can demonstrate receptor binding. Virol. J 12, 67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson M, Holmes EC, 2007. The evolution of epidemic influenza. Nat. Rev. Genet 8, 196–205. [DOI] [PubMed] [Google Scholar]
- Nobusawa E, Ishihara H, Morishita T, Sato K, Nakajima K, 2000. Change in receptor-binding specificity of recent human influenza A viruses (H3N2): a single amino acid change in hemagglutinin altered its recognition of sialyloligosaccharides. Virology 278, 587–596. [DOI] [PubMed] [Google Scholar]
- Oh DY, Barr IG, Mosse JA, Laurie KL, 2008. MDCK-SIAT1 cells show improved isolation rates for recent human influenza viruses compared to conventional MDCK cells. J. Clin. Microbiol 46, 2189–2194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okomo-Adhiambo M, Nguyen HT, Abd Elal A, Sleeman K, Fry AM, Gubareva LV, 2014. Drug susceptibility surveillance of influenza viruses circulating in the United States in 2011-2012: application of the WHO antiviral working group criteria. Influenza Other Respir Viruses 8, 258–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okomo-Adhiambo M, Nguyen HT, Sleeman K, Sheu TG, Deyde VM, Garten RJ, Xu X, Shaw MW, Klimov AI, Gubareva LV, 2010a. Host cell selection of influenza neuraminidase variants: implications for drug resistance monitoring in A (H1N1) viruses. Antivir. Res 85, 381–388. [DOI] [PubMed] [Google Scholar]
- Okomo-Adhiambo M, Sleeman K, Ballenger K, Nguyen HT, Mishin VP, Sheu TG, Smagala J, Li Y, Klimov AI, Gubareva LV, 2010b. Neuraminidase inhibitor susceptibility testing in human influenza viruses: a laboratory surveillance perspective. Viruses 2, 2269–2289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng W, de Vries RP, Grant OC, Thompson AJ, McBride R, Tsogtbaatar B, Lee PS, Razi N, Wilson IA, Woods RJ, Paulson JC, 2017. Recent H3N2 viruses have evolved specificity for extended, branched human-type receptors, conferring potential for increased avidity. Cell Host Microbe 21, 23–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell RJ, Haire LF, Stevens DJ, Collins PJ, Lin YP, Blackburn GM, Hay AJ, Gamblin SJ, Skehel JJ, 2006. The structure of H5N1 avian influenza neuraminidase suggests new opportunities for drug design. Nature 443, 45–49. [DOI] [PubMed] [Google Scholar]
- Shepard SS, Meno S, Bahl J, Wilson MM, Barnes J, Neuhaus E, 2016. Viral deep sequencing needs an adaptive approach: IRMA, the iterative refinement meta-assembler. BMC Genom. 17, 708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonsen L, Clarke MJ, Williamson GD, Stroup DF, Arden NH, Schonberger LB, 1997. The impact of influenza epidemics on mortality: introducing a severity index. Am. J. Publ. Health 87, 1944–1950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takada K, Kawakami C, Fan S, Chiba S, Zhong G, Gu C, Shimizu K, Takasaki S, Sakai-Tagawa Y, Lopes TJS, Dutta J, Khan Z, Kriti D, van Bakel H, Yamada S, Watanabe T, Imai M, Kawaoka Y, 2019. A humanized MDCK cell line for the efficient isolation and propagation of human influenza viruses. Nat Microbiol 4, 1268–1273. [DOI] [PubMed] [Google Scholar]
- Tamura D, Nguyen HT, Sleeman K, Levine M, Mishin VP, Yang H, Guo Z, Okomo-Adhiambo M, Xu X, Stevens J, Gubareva LV, 2013. Cell culture-selected substitutions in influenza A(H3N2) neuraminidase affect drug susceptibility assessment. Antimicrob. Agents Chemother 57, 6141–6146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO), 2011. Global Influenza Surveillance Network: Manual for the Laboratory Diagnosis and Virological Surveillance of influenza. Geneva, Switzerland. [Google Scholar]
- Wu Y, Qin G, Gao F, Liu Y, Vavricka CJ, Qi J, Jiang H, Yu K, Gao GF, 2013. Induced opening of influenza virus neuraminidase N2 150-loop suggests an important role in inhibitor binding. Sci. Rep 3, 1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright P, Neumann G, Kawaoka Y, 2007. Orthomyxoviruses. In: Howley PM, Knipe DM (Eds.), Fields Virology, fifth ed., Wolters Kluwer. Lippincott, Williams, Philadelphia, pp. 1785–1837. [Google Scholar]
- Xue KS, Hooper KA, Ollodart AR, Dingens AS, Bloom JD, 2016. Cooperation between distinct viral variants promotes growth of H3N2 influenza in cell culture. Elife 5, e13974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang H, Carney PJ, Chang JC, Guo Z, Villanueva JM, Stevens J, 2015. Structure and receptor binding preferences of recombinant human A(H3N2) virus hemagglutinins. Virology 477, 18–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yasuhara A, Yamayoshi S, Kiso M, Sakai-Tagawa Y, Okuda M, Kawaoka Y, 2022. A broadly protective human monoclonal antibody targeting the sialidase activity of influenza A and B virus neuraminidases. Nat. Commun 13, 6602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanin M, Marathe B, Wong SS, Yoon SW, Collin E, Oshansky C, Jones J, Hause B, Webby R, 2015. Pandemic swine H1N1 influenza viruses with almost undetectable neuraminidase activity are not transmitted via aerosols in ferrets and are inhibited by human mucus but not swine mucus. J. Virol 89, 5935–5948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu X, McBride R, Nycholat CM, Yu W, Paulson JC, Wilson IA, 2012a. Influenza virus neuraminidases with reduced enzymatic activity that avidly bind sialic Acid receptors. J. Virol 86, 13371–13383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu X, Yang H, Guo Z, Yu W, Carney PJ, Li Y, Chen LM, Paulson JC, Donis RO, Tong S, Stevens J, Wilson IA, 2012b. Crystal structures of two subtype N10 neuraminidase-like proteins from bat influenza A viruses reveal a diverged putative active site. Proc. Natl. Acad. Sci. U. S. A 109, 18903–18908. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.


