Abstract
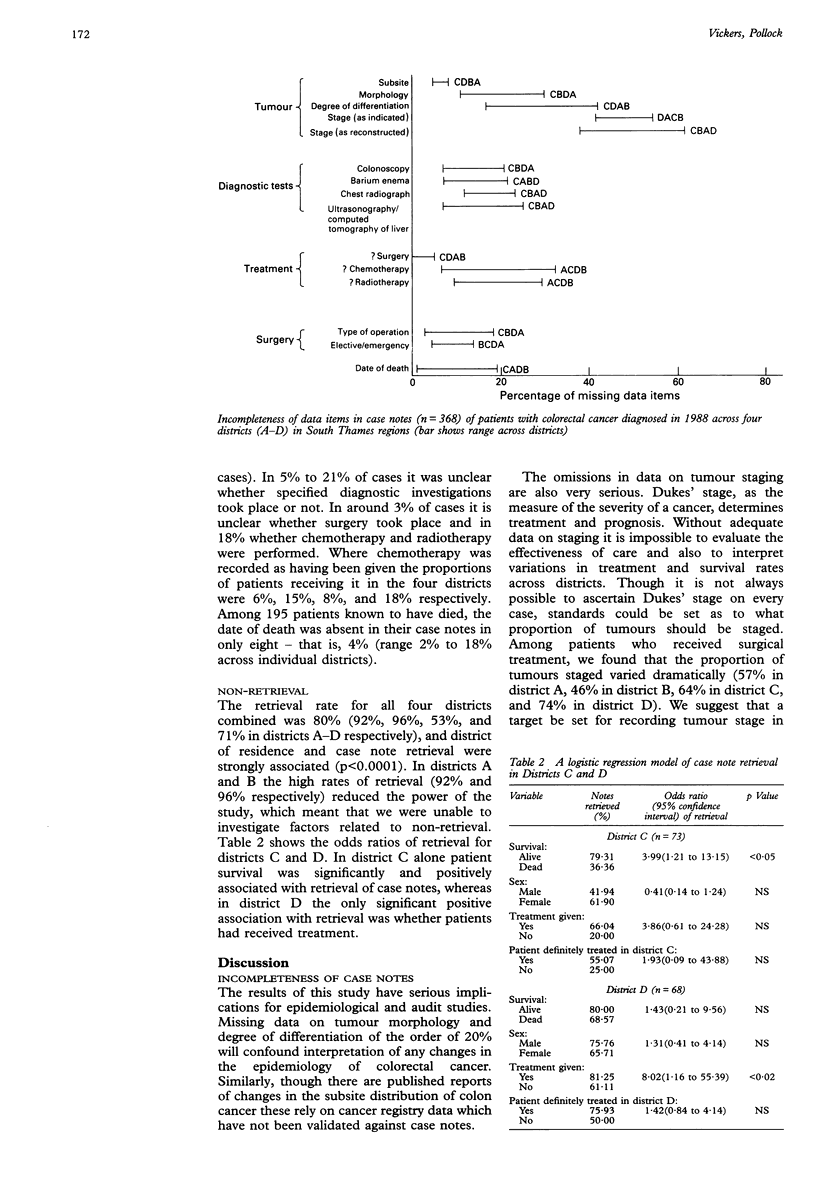
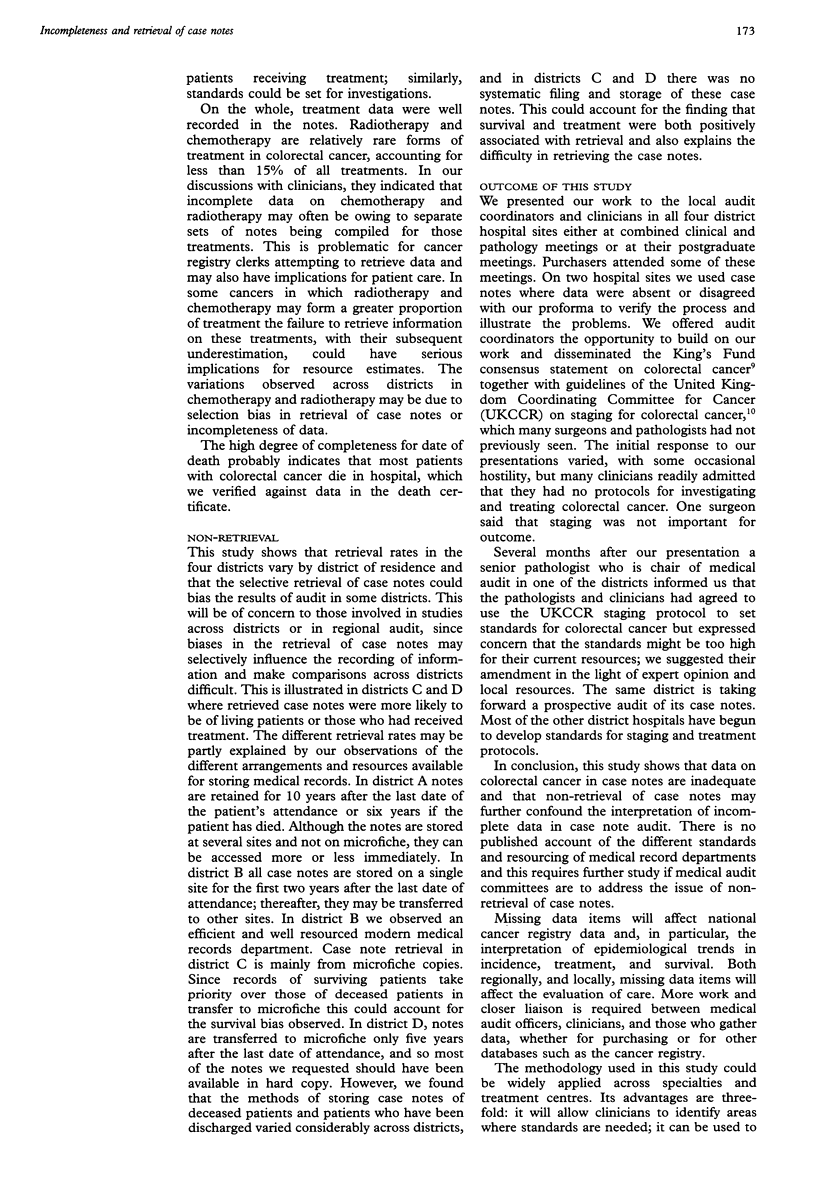
Hospital case notes are a crucial source of data but are subject to two major biases: incompleteness of data and non-retrieval. To assess these biases in relation to colorectal cancer a study was performed of all cases of colorectal cancer listed in the Thames cancer registry in patients resident in one of four districts in South Thames regions with a diagnosis in 1988. Five medical record sites were involved. Retrieval rate for all case notes for districts combined was 80%. In two districts the rates were too high for further investigation; in the other two respectively patient survival and whether treatment was given were positively associated with retrieval. Among the four districts incompleteness of notes ranged from 38% to 62% for staging, 8% to 40% for treatment, and 70% to 25% for diagnostic tests. Information about treatment was missing in 3% to 20%; survival data were omitted in less than 5%. In all districts completeness of case notes was inadequate and in some non-retrieval compounded the problem. Missing data reduce the quality of cancer registry data and potentially undermine interpretation of epidemiological studies and evaluation of care. Further research is warranted into the standards and resourcing of medical records departments and their effects on retrieval and data quality. Structured proformas could be applied across specialties to identify missing items in case notes, to identify areas where standards are required, or to audit notes where standards have already been agreed. A staging protocol to set standards for colorectal cancer has been adopted in one district, and a prospective audit is being established.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Gabbay J., McNicol M. C., Spiby J., Davies S. C., Layton A. J. What did audit achieve? Lessons from preliminary evaluation of a year's medical audit. BMJ. 1990 Sep 15;301(6751):526–529. doi: 10.1136/bmj.301.6751.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gulliford M. C., Petruckevitch A., Burney P. G. Hospital case notes and medical audit: evaluation of non-response. BMJ. 1991 May 11;302(6785):1128–1129. doi: 10.1136/bmj.302.6785.1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heath D. A. Random review of hospital patient records. BMJ. 1990 Mar 10;300(6725):651–652. doi: 10.1136/bmj.300.6725.651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krarup K. C., Lamont A. C. Hospital case notes and medical audit. BMJ. 1991 Jun 29;302(6792):1605–1606. doi: 10.1136/bmj.302.6792.1605-c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rai G. S. Lessons from preliminary evaluation of a year's medical audit. BMJ. 1990 Oct 13;301(6756):874–875. doi: 10.1136/bmj.301.6756.874-c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rai G. S., McInnes E., Phongsathorn V., Sharland D. E. Medical audit of case notes on one to one basis. J R Coll Physicians Lond. 1991 Oct;25(4):358–359. [PMC free article] [PubMed] [Google Scholar]


