Abstract
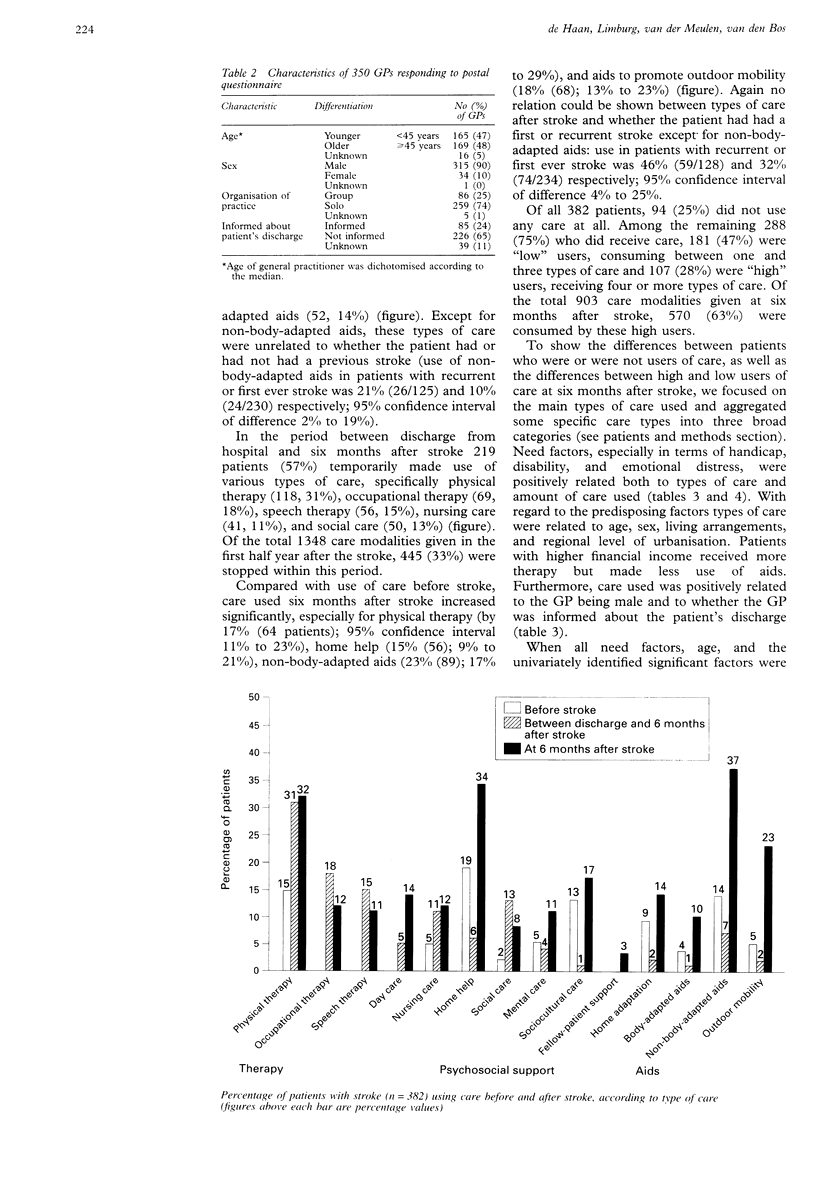
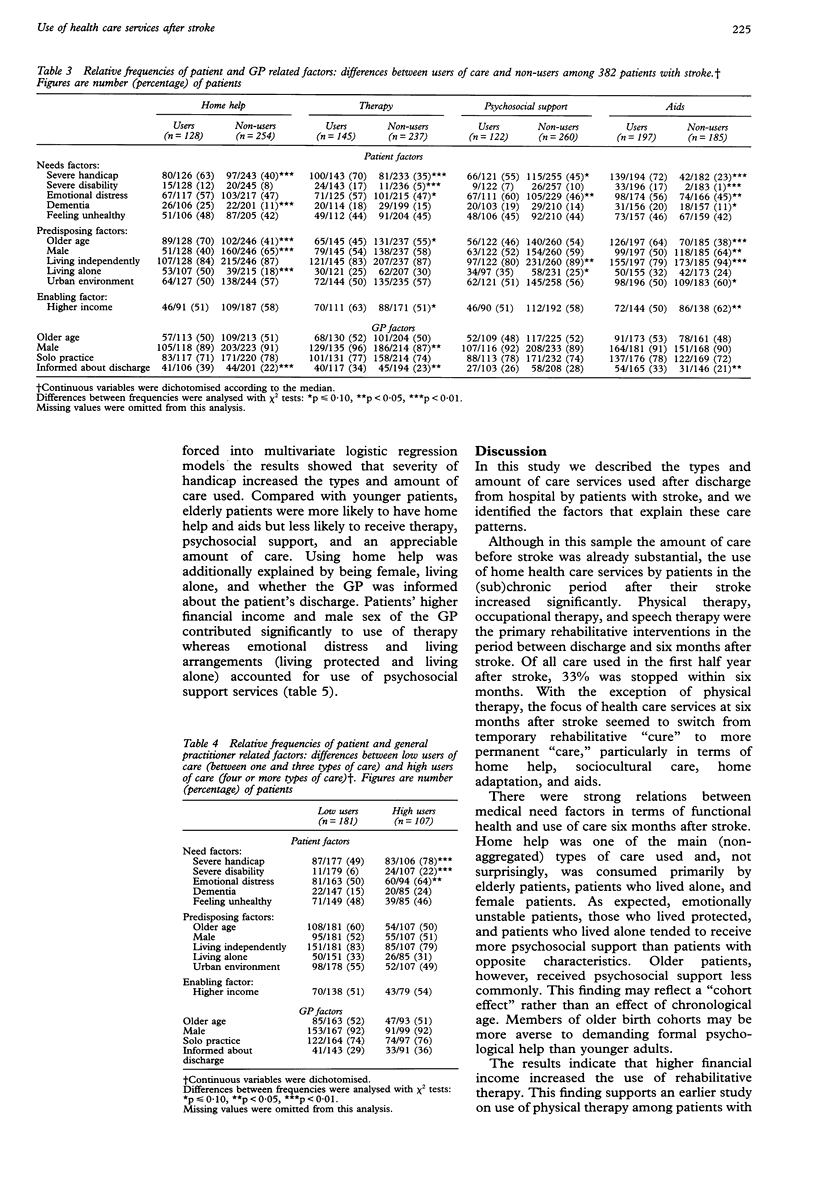
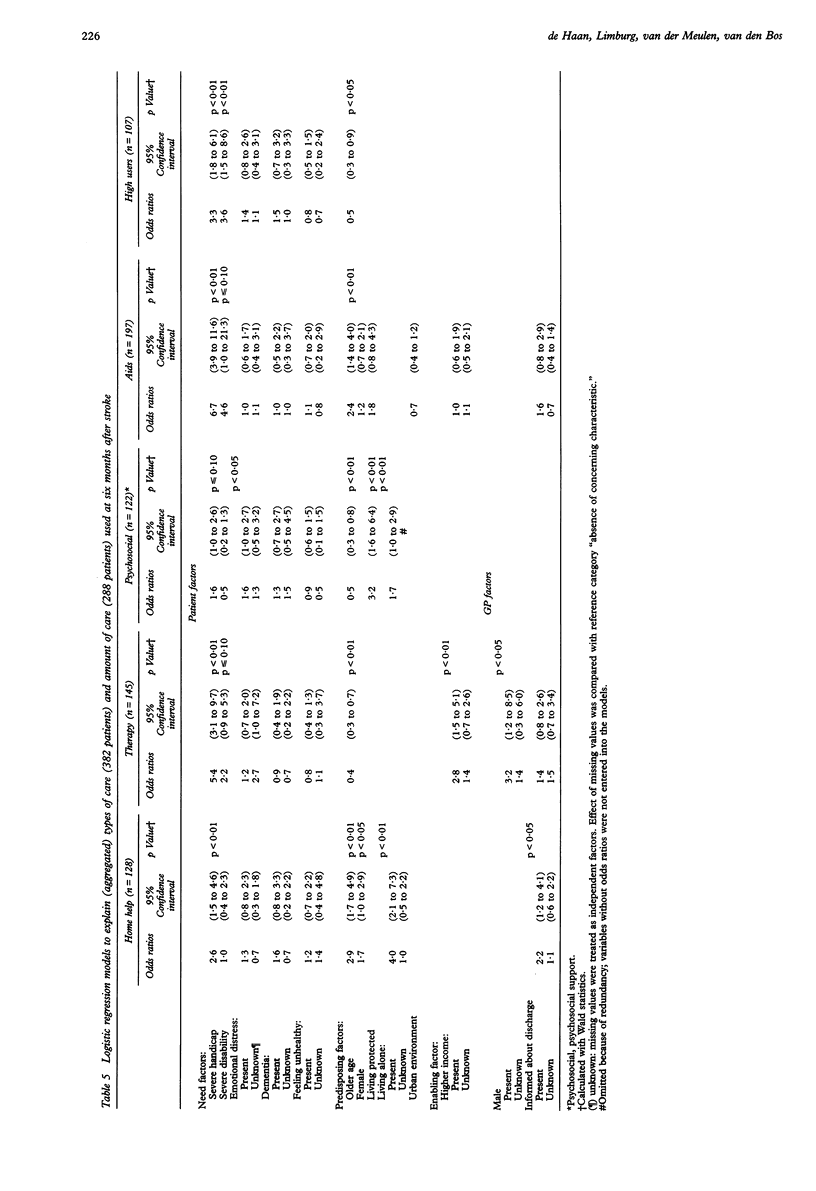
OBJECTIVES--To describe the use of care before and after stroke and to evaluate equity in access to health care services after stroke. DESIGN--Cross sectional study. SETTING--The Netherlands. PATIENTS--382 patients living in the community who had been admitted to hospital with a stroke six months before. MAIN MEASURES--Sociodemographic status and functional health status according to The Barthel index, Rankin scale, and sickness impact profile, assessed during interview, and general practitioner (GP) characteristics obtained by postal questionnaire. Univariate and multivariate analyses of the relation between patient and GP related factors and use of care. RESULTS--Compared with the period before stroke the use of care six months after stroke increased significantly, especially use of physical therapy, home help, and aids. Multivariate analyses showed that impaired functional health increased the use of care (range in odds ratios 1.6 to 6.7). Compared with younger patients, elderly patients were more likely to have home help (odds ratio 2.9) and aids (2.4) but less likely to receive therapy (0.4), psychosocial support (0.5), and an appreciable amount of care (0.5). Being female (1.7), living alone (4.0), and whether the GP was informed about patients' discharge (2.2) increased the use of home help. Higher financial income (2.8) and having a male GP (3.2) contributed to use of therapy. Emotional distress (1.6), living protected (3.2), and living alone (1.7) accounted for psychosocial support. CONCLUSIONS--Although older age, lower income, and poor discharge information to the GP decreased the use of some types of care, there is equity in access to care after stroke, primarily determined by needs in terms of functional health status and predisposing factors such as living arrangement and social circumstances. IMPLICATIONS--Patient oriented studies focusing on care processes and care outcomes in terms of subjective needs, perceived care deficits, and satisfaction with care are still required.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bamford J. M., Sandercock P. A., Warlow C. P., Slattery J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1989 Jun;20(6):828–828. doi: 10.1161/01.str.20.6.828. [DOI] [PubMed] [Google Scholar]
- Bergner M., Bobbitt R. A., Carter W. B., Gilson B. S. The Sickness Impact Profile: development and final revision of a health status measure. Med Care. 1981 Aug;19(8):787–805. doi: 10.1097/00005650-198108000-00001. [DOI] [PubMed] [Google Scholar]
- Browne G. B., Arpin K., Corey P., Fitch M., Gafni A. Individual correlates of health service utilization and the cost of poor adjustment to chronic illness. Med Care. 1990 Jan;28(1):43–58. doi: 10.1097/00005650-199001000-00006. [DOI] [PubMed] [Google Scholar]
- Dove H. G., Schneider K. C., Wallace J. D. Evaluating and predicting outcome of acute cerebral vascular accident. Stroke. 1984 Sep-Oct;15(5):858–864. doi: 10.1161/01.str.15.5.858. [DOI] [PubMed] [Google Scholar]
- Folstein M. F., Folstein S. E., McHugh P. R. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975 Nov;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Herman B., Leyten A. C., van Luijk J. H., Frenken C. W., Op de Coul A. A., Schulte B. P. Epidemiology of stroke in Tilburg, the Netherlands. The population-based stroke incidence register: 2. Incidence, initial clinical picture and medical care, and three-week case fatality. Stroke. 1982 Sep-Oct;13(5):629–634. doi: 10.1161/01.str.13.5.629. [DOI] [PubMed] [Google Scholar]
- Hulka B. S., Wheat J. R. Patterns of utilization. The patient perspective. Med Care. 1985 May;23(5):438–460. doi: 10.1097/00005650-198505000-00009. [DOI] [PubMed] [Google Scholar]
- Malmgren R., Bamford J., Warlow C., Sandercock P., Slattery J. Projecting the number of patients with first ever strokes and patients newly handicapped by stroke in England and Wales. BMJ. 1989 Mar 11;298(6674):656–660. doi: 10.1136/bmj.298.6674.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silliman R. A., Wagner E. H., Fletcher R. H. The social and functional consequences of stroke for elderly patients. Stroke. 1987 Jan-Feb;18(1):200–203. doi: 10.1161/01.str.18.1.200. [DOI] [PubMed] [Google Scholar]
- Thorngren M., Westling B. Utilization of health care resources after stroke. A population-based study of 258 hospitalized cases followed during the first year. Acta Neurol Scand. 1991 Oct;84(4):303–310. doi: 10.1111/j.1600-0404.1991.tb04959.x. [DOI] [PubMed] [Google Scholar]
- Wade D. T., Collin C. The Barthel ADL Index: a standard measure of physical disability? Int Disabil Stud. 1988;10(2):64–67. doi: 10.3109/09638288809164105. [DOI] [PubMed] [Google Scholar]


