Abstract
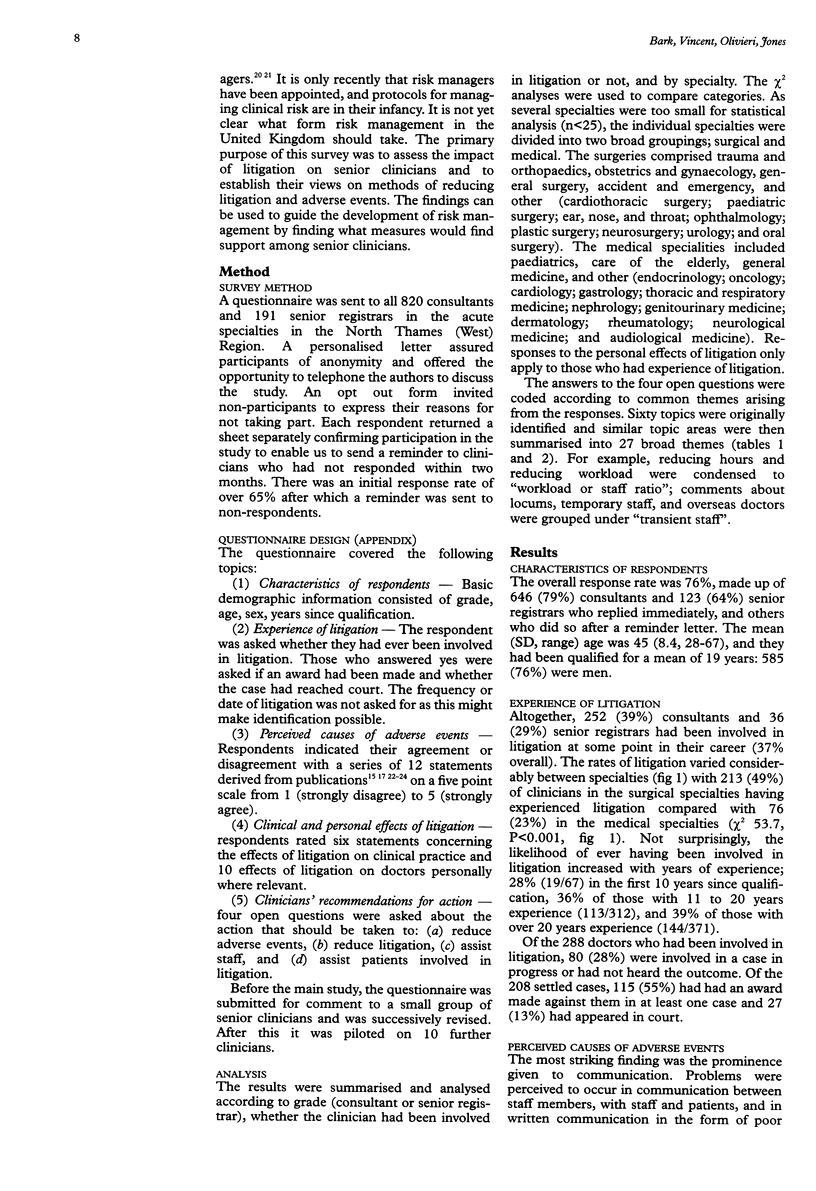
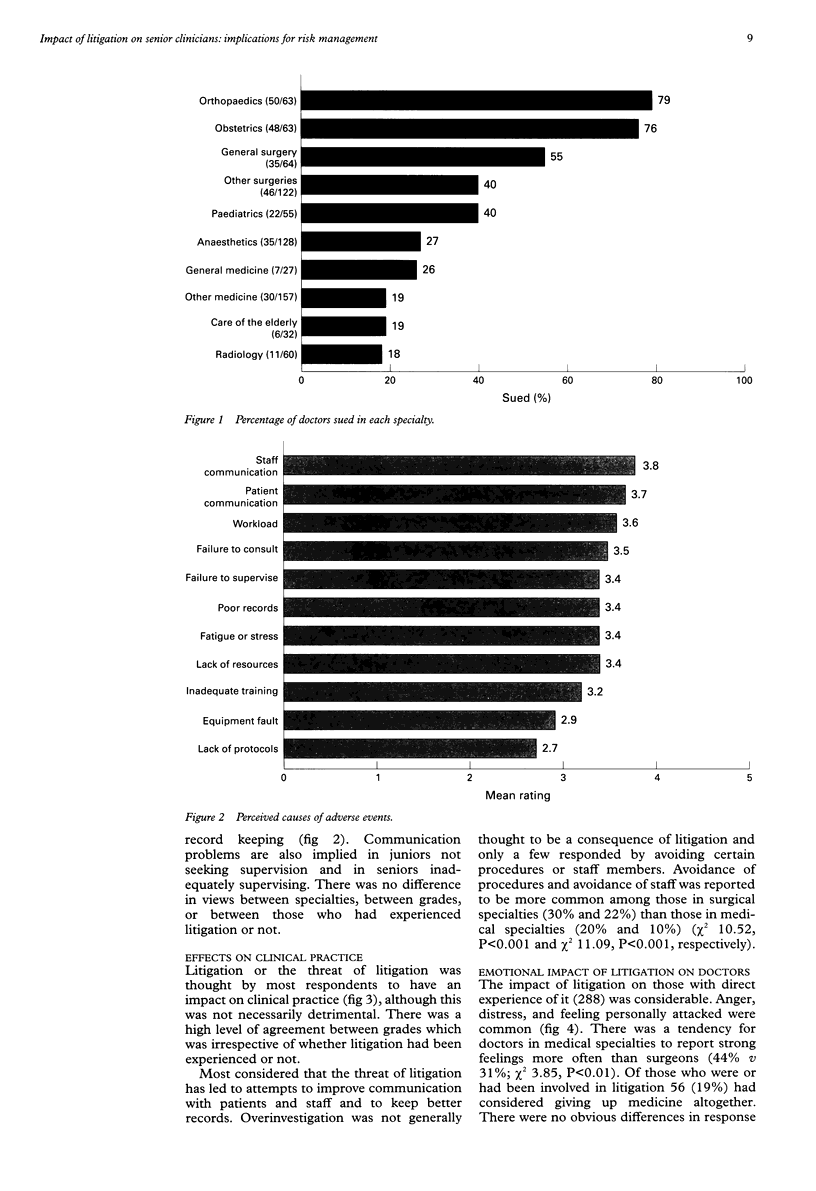
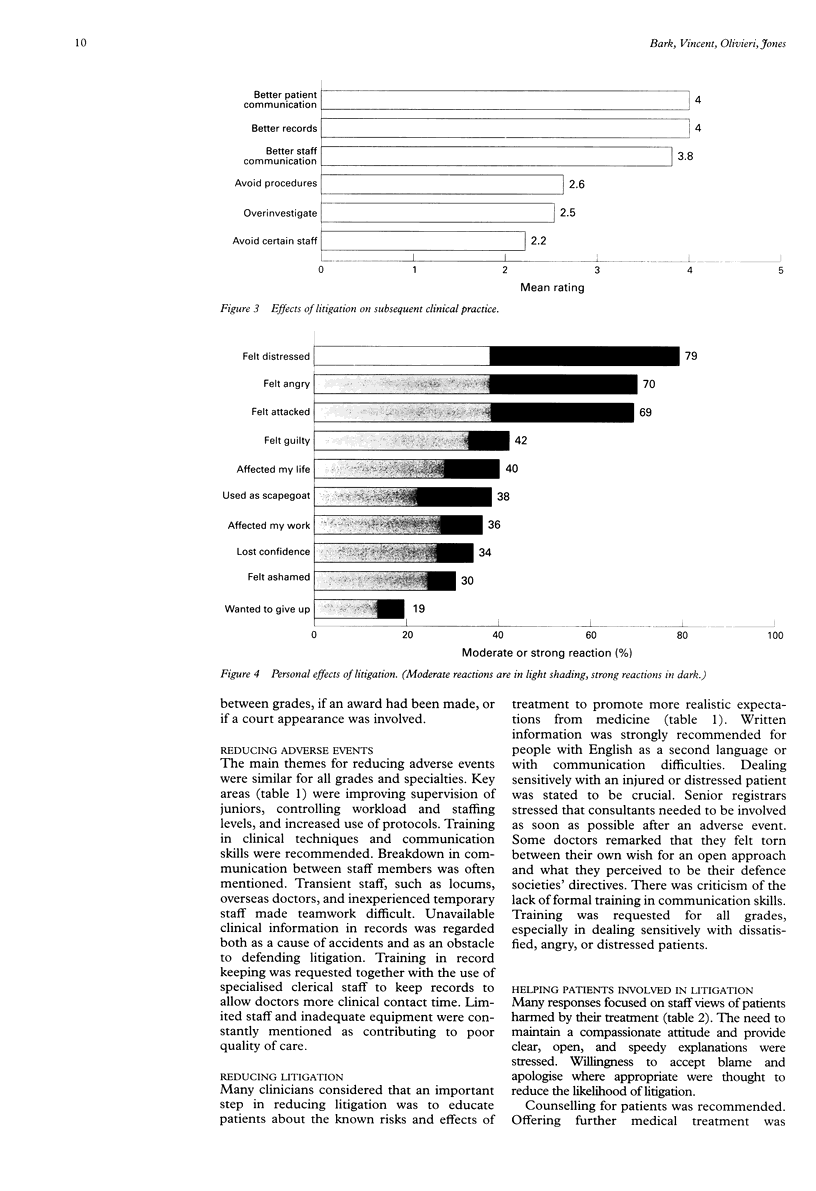
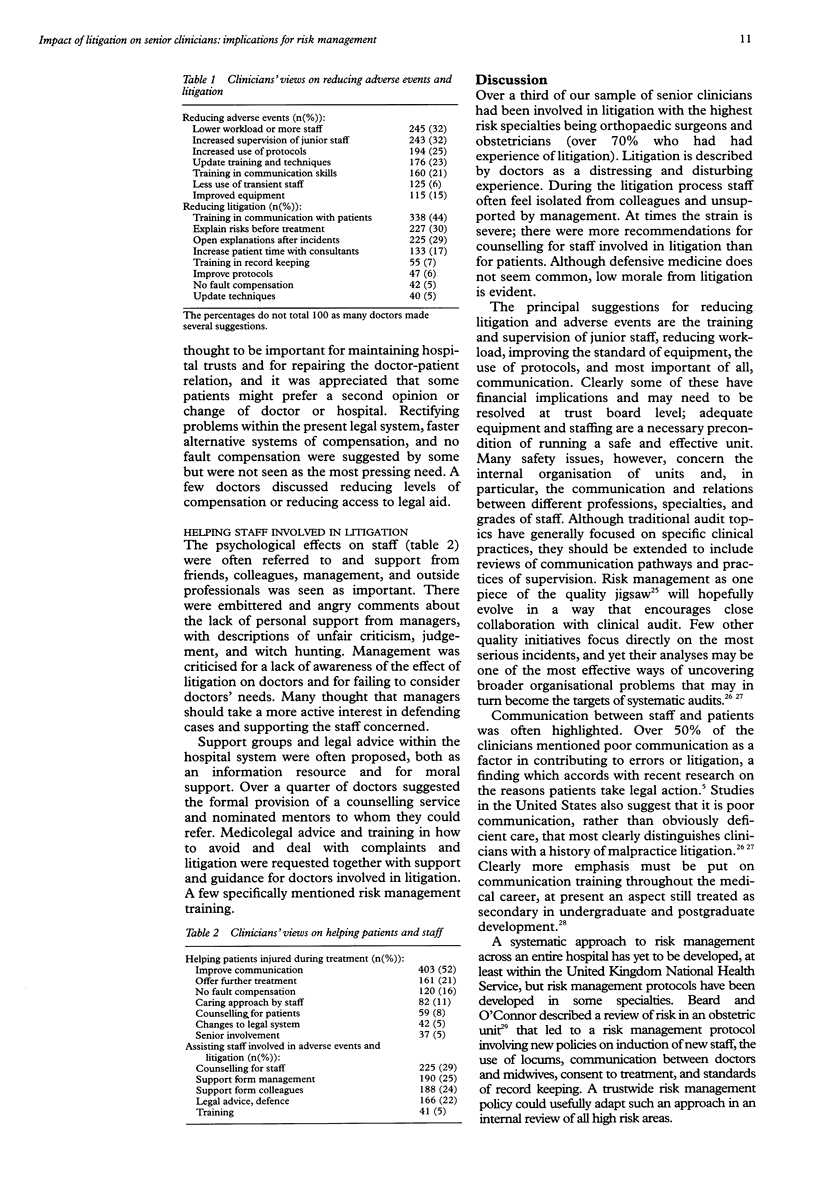
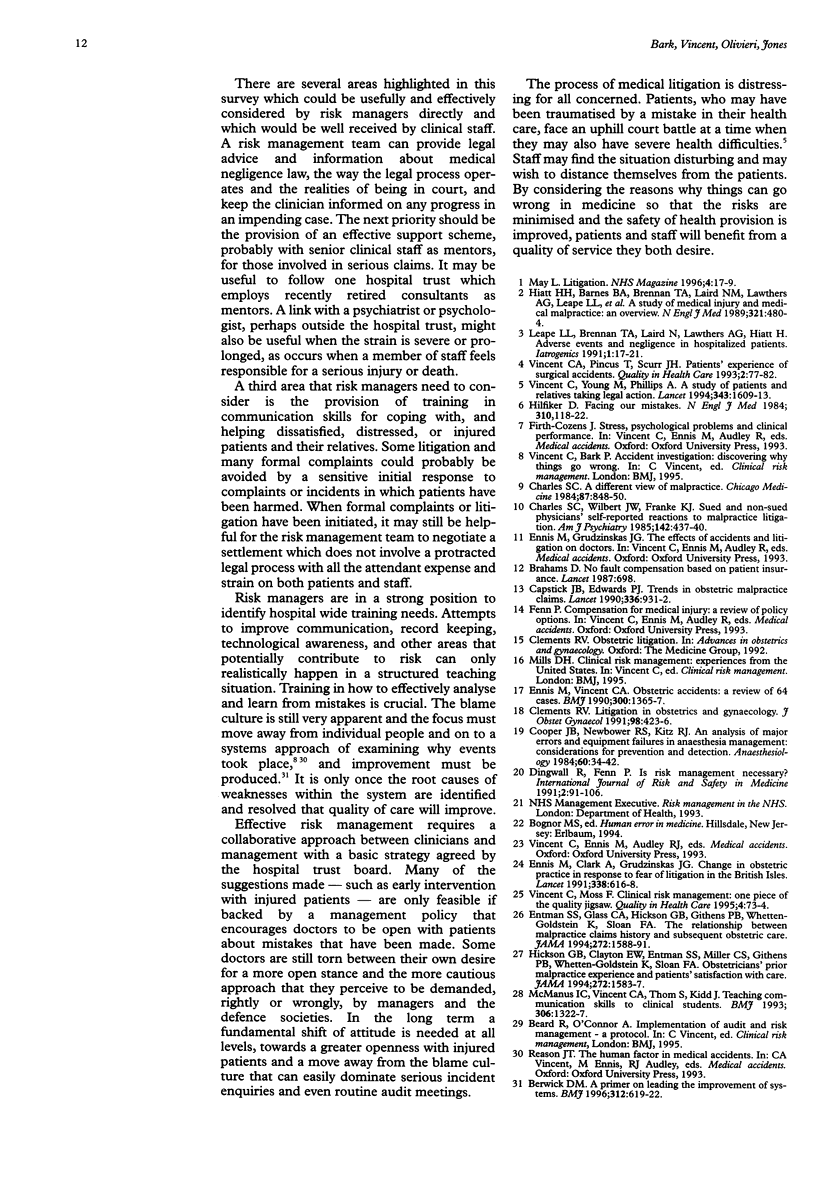
OBJECTIVES: To investigate the impact of litigation on consultants and senior registrars and to establish their views on methods of reducing adverse events and litigation. DESIGN: Postal survey. SETTING: Acute hospitals in the North Thames (West) Regional Health Authority. SUBJECTS: 1011 consultants and senior registrars in acute hospitals. MAIN MEASURES: Perceived causes and effects of adverse events; views on methods of reducing litigation and adverse events. RESULTS: 769 (76%) doctors responded. 288 (37%) had been involved in litigation at some point during their career; 213 surgeons (49%) and 75 (23%) doctors in the medical specialties. Anger, distress, and feeling personally attacked were common responses to litigation. Clinicians' views on reducing litigation emphasised the need for change at the clinical level. Supervision of junior staff, workload, and training in communication skills were to the fore. CONCLUSIONS: The high frequency of doctors who have experienced litigation and the emotional responses described indicate that clinicians require support at several levels. At a personal level, support can be offered to clinicians going through the litigation process or after an adverse event. Also, managerial support is needed by offering financial and practical help in correcting the factors that have been consistently identified as producing high risk situations to minimise the possibility of a reoccurrence. Accidents in medicine are, by their very nature, costly in human and financial terms and the root causes must be tackled. Recommendations are made for clinicians and risk management teams.
Full text
PDF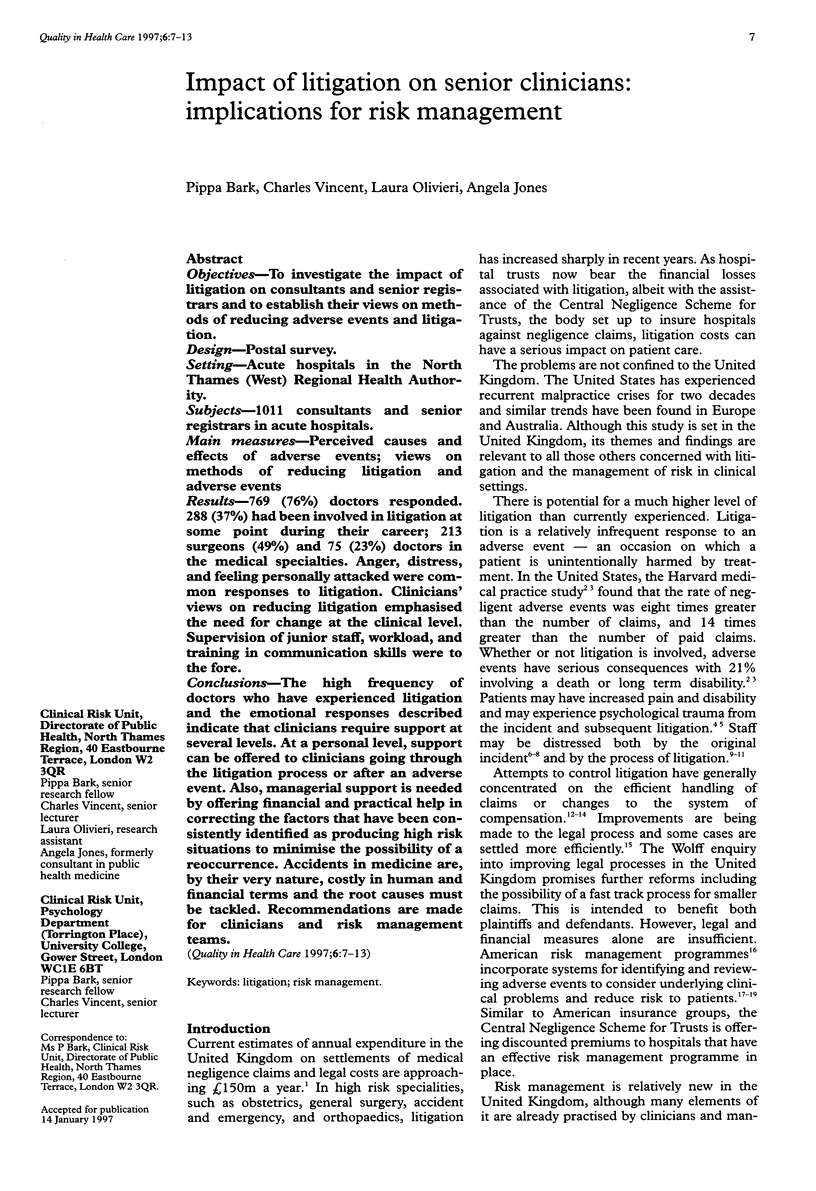
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Berwick D. M. A primer on leading the improvement of systems. BMJ. 1996 Mar 9;312(7031):619–622. doi: 10.1136/bmj.312.7031.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brahams D. No fault compensation based on patient insurance. Lancet. 1987 Mar 21;1(8534):698–698. doi: 10.1016/s0140-6736(87)90474-0. [DOI] [PubMed] [Google Scholar]
- Capstick J. B., Edwards P. J. Trends in obstetric malpractice claims. Lancet. 1990 Oct 13;336(8720):931–932. doi: 10.1016/0140-6736(90)92291-o. [DOI] [PubMed] [Google Scholar]
- Charles S. C., Wilbert J. R., Franke K. J. Sued and nonsued physicians' self-reported reactions to malpractice litigation. Am J Psychiatry. 1985 Apr;142(4):437–440. doi: 10.1176/ajp.142.4.437. [DOI] [PubMed] [Google Scholar]
- Clements R. V. Litigation in obstetrics and gynaecology. Br J Obstet Gynaecol. 1991 May;98(5):423–426. doi: 10.1111/j.1471-0528.1991.tb10334.x. [DOI] [PubMed] [Google Scholar]
- Cooper J. B., Newbower R. S., Kitz R. J. An analysis of major errors and equipment failures in anesthesia management: considerations for prevention and detection. Anesthesiology. 1984 Jan;60(1):34–42. doi: 10.1097/00000542-198401000-00008. [DOI] [PubMed] [Google Scholar]
- Ennis M., Clark A., Grudzinskas J. G. Change in obstetric practice in response to fear of litigation in the British Isles. Lancet. 1991 Sep 7;338(8767):616–618. doi: 10.1016/0140-6736(91)90616-w. [DOI] [PubMed] [Google Scholar]
- Ennis M., Vincent C. A. Obstetric accidents: a review of 64 cases. BMJ. 1990 May 26;300(6736):1365–1367. doi: 10.1136/bmj.300.6736.1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Entman S. S., Glass C. A., Hickson G. B., Githens P. B., Whetten-Goldstein K., Sloan F. A. The relationship between malpractice claims history and subsequent obstetric care. JAMA. 1994 Nov 23;272(20):1588–1591. [PubMed] [Google Scholar]
- Hiatt H. H., Barnes B. A., Brennan T. A., Laird N. M., Lawthers A. G., Leape L. L., Localio A. R., Newhouse J. P., Peterson L. M., Thorpe K. E. A study of medical injury and medical malpractice. N Engl J Med. 1989 Aug 17;321(7):480–484. doi: 10.1056/NEJM198908173210725. [DOI] [PubMed] [Google Scholar]
- Hickson G. B., Clayton E. W., Entman S. S., Miller C. S., Githens P. B., Whetten-Goldstein K., Sloan F. A. Obstetricians' prior malpractice experience and patients' satisfaction with care. JAMA. 1994 Nov 23;272(20):1583–1587. [PubMed] [Google Scholar]
- Hilfiker D. Facing our mistakes. N Engl J Med. 1984 Jan 12;310(2):118–122. doi: 10.1056/NEJM198401123100211. [DOI] [PubMed] [Google Scholar]
- McManus I. C., Vincent C. A., Thom S., Kidd J. Teaching communication skills to clinical students. BMJ. 1993 May 15;306(6888):1322–1327. doi: 10.1136/bmj.306.6888.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent C. A., Pincus T., Scurr J. H. Patients' experience of surgical accidents. Qual Health Care. 1993 Jun;2(2):77–82. doi: 10.1136/qshc.2.2.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent C., Moss F. Clinical risk management: one piece of the quality jigsaw. Qual Health Care. 1995 Jun;4(2):73–74. doi: 10.1136/qshc.4.2.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent C., Young M., Phillips A. Why do people sue doctors? A study of patients and relatives taking legal action. Lancet. 1994 Jun 25;343(8913):1609–1613. doi: 10.1016/s0140-6736(94)93062-7. [DOI] [PubMed] [Google Scholar]


