Abstract
Background
Pharmacological interventions are frequently used for people with autism spectrum disorder (ASD) to manage behaviours of concern, including irritability, aggression, and self‐injury. Some pharmacological interventions might help treat some behaviours of concern, but can also have adverse effects (AEs).
Objectives
To assess the effectiveness and AEs of pharmacological interventions for managing the behaviours of irritability, aggression, and self‐injury in ASD.
Search methods
We searched CENTRAL, MEDLINE, Embase, 11 other databases and two trials registers up to June 2022. We also searched reference lists of relevant studies, and contacted study authors, experts and pharmaceutical companies.
Selection criteria
We included randomised controlled trials of participants of any age with a clinical diagnosis of ASD, that compared any pharmacological intervention to an alternative drug, standard care, placebo, or wait‐list control.
Data collection and analysis
We used standard Cochrane methods. Primary outcomes were behaviours of concern in ASD, (irritability, aggression and self‐injury); and AEs. Secondary outcomes were quality of life, and tolerability and acceptability. Two review authors independently assessed each study for risk of bias, and used GRADE to judge the certainty of the evidence for each outcome.
Main results
We included 131 studies involving 7014 participants in this review. We identified 26 studies as awaiting classification and 25 as ongoing. Most studies involved children (53 studies involved only children under 13 years), children and adolescents (37 studies), adolescents only (2 studies) children and adults (16 studies), or adults only (23 studies). All included studies compared a pharmacological intervention to a placebo or to another pharmacological intervention.
Atypical antipsychotics versus placebo
At short‐term follow−up (up to 6 months), atypical antipsychotics probably reduce irritability compared to placebo (standardised mean difference (SMD) −0.90, 95% confidence interval (CI) −1.25 to −0.55, 12 studies, 973 participants; moderate‐certainty evidence), which may indicate a large effect. However, there was no clear evidence of a difference in aggression between groups (SMD −0.44, 95% CI −0.89 to 0.01; 1 study, 77 participants; very low‐certainty evidence). Atypical antipsychotics may also reduce self‐injury (SMD −1.43, 95% CI −2.24 to −0.61; 1 study, 30 participants; low‐certainty evidence), possibly indicating a large effect.
There may be higher rates of neurological AEs (dizziness, fatigue, sedation, somnolence, and tremor) in the intervention group (low‐certainty evidence), but there was no clear evidence of an effect on other neurological AEs. Increased appetite may be higher in the intervention group (low‐certainty evidence), but we found no clear evidence of an effect on other metabolic AEs. There was no clear evidence of differences between groups in musculoskeletal or psychological AEs.
Neurohormones versus placebo
At short‐term follow‐up, neurohormones may have minimal to no clear effect on irritability when compared to placebo (SMD −0.18, 95% CI −0.37 to −0.00; 8 studies; 466 participants; very low‐certainty evidence), although the evidence is very uncertain. No data were reported for aggression or self ‐injury.
Neurohormones may reduce the risk of headaches slightly in the intervention group, although the evidence is very uncertain. There was no clear evidence of an effect of neurohormones on any other neurological AEs, nor on any psychological, metabolic, or musculoskeletal AEs (low‐ and very low‐certainty evidence).
Attention‐deficit hyperactivity disorder (ADHD)‐related medications versus placebo
At short‐term follow‐up, ADHD‐related medications may reduce irritability slightly (SMD −0.20, 95% CI −0.40 to −0.01; 10 studies, 400 participants; low‐certainty evidence), which may indicate a small effect. However, there was no clear evidence that ADHD‐related medications have an effect on self‐injury (SMD −0.62, 95% CI −1.63 to 0.39; 1 study, 16 participants; very low‐certainty evidence). No data were reported for aggression.
Rates of neurological AEs (drowsiness, emotional AEs, fatigue, headache, insomnia, and irritability), metabolic AEs (decreased appetite) and psychological AEs (depression) may be higher in the intervention group, although the evidence is very uncertain (very low‐certainty evidence). There was no evidence of a difference between groups for any other metabolic, neurological, or psychological AEs (very low‐certainty evidence). No data were reported for musculoskeletal AEs.
Antidepressants versus placebo
At short‐term follow‐up, there was no clear evidence that antidepressants have an effect on irritability (SMD −0.06, 95% CI −0.30 to 0.18; 3 studies, 267 participants; low‐certainty evidence). No data for aggression or self‐injury were reported or could be included in the analysis.
Rates of metabolic AEs (decreased energy) may be higher in participants receiving antidepressants (very low‐certainty evidence), although no other metabolic AEs showed clear evidence of a difference. Rates of neurological AEs (decreased attention) and psychological AEs (impulsive behaviour and stereotypy) may also be higher in the intervention group (very low‐certainty evidence) although the evidence is very uncertain. There was no clear evidence of any difference in the other metabolic, neurological, or psychological AEs (very low‐certainty evidence), nor between groups in musculoskeletal AEs (very low‐certainty evidence).
Risk of bias
We rated most of the studies across the four comparisons at unclear overall risk of bias due to having multiple domains rated as unclear, very few rated as low across all domains, and most having at least one domain rated as high risk of bias.
Authors' conclusions
Evidence suggests that atypical antipsychotics probably reduce irritability, ADHD‐related medications may reduce irritability slightly, and neurohormones may have little to no effect on irritability in the short term in people with ASD. There was some evidence that atypical antipsychotics may reduce self‐injury in the short term, although the evidence is uncertain. There was no clear evidence that antidepressants had an effect on irritability. There was also little to no difference in aggression between atypical antipsychotics and placebo, or self‐injury between ADHD‐related medications and placebo. However, there was some evidence that atypical antipsychotics may result in a large reduction in self‐injury, although the evidence is uncertain. No data were reported (or could be used) for self‐injury or aggression for neurohormones versus placebo. Studies reported a wide range of potential AEs. Atypical antipsychotics and ADHD‐related medications in particular were associated with an increased risk of metabolic and neurological AEs, although the evidence is uncertain for atypical antipsychotics and very uncertain for ADHD‐related medications. The other drug classes had minimal or no associated AEs.
Keywords: Adolescent, Adult, Child, Humans, Aggression, Antidepressive Agents, Antidepressive Agents/therapeutic use, Antipsychotic Agents, Antipsychotic Agents/therapeutic use, Autism Spectrum Disorder, Autism Spectrum Disorder/drug therapy, Fatigue, Neurotransmitter Agents, Neurotransmitter Agents/pharmacology, Quality of Life, Self-Injurious Behavior, Self-Injurious Behavior/drug therapy
Plain language summary
Which medications reduce irritability, aggression or self‐harm in people with autism spectrum disorder (ASD)?
Key messages
• Only 3 classes of medications showed any reduction in irritability, aggression or self‐harm when compared to placebo (a dummy medication). Atypical (second‐generation) antipsychotic medications probably reduce irritability and aggression, but appear to have little to no effect on self‐injury. Attention deficit hyperactivity disorder (ADHD)‐related medications may reduce irritability, although the evidence is uncertain. Neurohormones (oxytocin and secretin) may also reduce irritability, but we are very uncertain about the evidence.
• Antidepressants appear to have no effect on irritability. Studies did not report on the effects of antidepressants, ADHD‐related medications and neurohormones on aggression or self‐injury.
• Studies reported a wide range of unwanted effects, but only atypical antipsychotics, ADHD‐related medications, and neurohormones showed evidence of a higher risk of any unwanted effects compared to placebo.
What is autism spectrum disorder (ASD)?
Autism is a disorder that affects a child's physical, mental and behavioural development. It is a lifelong disability that starts in childhood but continues throughout adulthood. People with autism may find it difficult to communicate and interact with the world. However, autism affects each person differently and may be more or less severe in different people, so it is described as a 'spectrum' disorder. Some people with autism spectrum disorder (ASD) may be irritable, angry or aggressive, or hurt themselves physically (self‐injury), which are 'behaviours of concern' that can be difficult to manage and distressing for the person.
How are behaviours of concern managed?
Behaviours of concern are frequently managed with various types of medications that have been developed to treat other conditions. This means that their effectiveness for behaviours of concern is largely unknown, and they may cause serious and varied unwanted effects that affect all parts of the body. For example:
• the heart and lungs;
• the stomach and digestive system;
• the immune system;
• movement, joints and bones; and
• mood and emotion.
What did we want to find out?
We wanted to know which types of medication were effective in reducing behaviours of concern in people with ASD and whether they caused unwanted effects.
What did we do?
We searched for studies that investigated any medication used to manage behaviours of concern. Studies compared the medication with placebo (a dummy medication) or another medication. People in the studies could be adults or children, but all had ASD with behaviours of concern. We compared and summarised the results of the studies and rated our confidence in the evidence, based on factors such as study methods and sizes.
What did we find?
We found 131 studies with 7014 people. Most studies involved children, although some studies involved both children and adults, or adults only. Studies looked at a wide range of medications, including those usually used to treat schizophrenia or bipolar disorder, depression, attention deficit hyperactivity disorder (ADHD), convulsions, emotional problems, heart and lungs, dementia, Parkinson's, and anxiety.
Atypical (second‐generation) antipsychotics are usually used to treat schizophrenia or bipolar disorder. They probably reduce irritability, but they may have little to no effect on aggression and self‐injury. People receiving antipsychotics might be more likely to experience unwanted effects such as increased appetite, dizziness, sedation (slowed thought and movement), sleepiness, tiredness and tremor compared to those receiving no treatment or other medications. People receiving antipsychotics may be no more or less likely than those receiving placebo to experience other unwanted effects.
Neurohormones (such as oxytocin and secretin) may have a minimal to small effect on irritability but no studies reported data for the effects of neurohormones on self‐harm or aggression. People receiving neurohormones may be no more or less likely than those receiving placebo to experience unwanted effects.
ADHD‐related medications may reduce irritability but may have no effect on self‐injury. No studies reported data for aggression. People receiving ADHD‐related medications might be more likely to experience unwanted effects such as drowsiness, tiredness, headache, difficulties sleeping, and decreased appetite. But they may be no more or less likely than those receiving placebo to experience other unwanted effects.
Antidepressants may have little to no effect on irritability. No studies reported useful data for aggression and self‐injury. People receiving antidepressants might be more likely to experience unwanted effects such as impulsive behaviour and making repetitive movements or sounds (stereotypy) compared to placebo. But they may be no more or less likely than those receiving placebo to experience other types of unwanted effects.
What are the limitations of the evidence?
Most of the studies lasted less than 3 months, and very few studies involved adults. Therefore, we are uncertain if the same effects would be seen over a longer period of time or in adults.
How up‐to‐date is the evidence?
The review authors searched for studies that had been published up to June 2022.
Summary of findings
Summary of findings 1. Atypical antipsychotics compared to placebo for irritability, aggression, and self‐injury in autism spectrum disorder (ASD).
| Atypical antipsychotics compared to placebo for irritability, aggression, and self‐injury in autism spectrum disorder (ASD) | |||||||
| Patient or population: participants (any age) with a clinical diagnosis of ASD who have displayed one or more unwanted or challenging behaviours at baseline assessment Setting: hospital inpatient or outpatient centres, education or disability settings, mental health settings, or clinics and research centres associated with universities Intervention: atypical antipsychotics Comparison: placebo | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | ||
| Risk with placebo | Risk with atypical antipsychotics | ||||||
|
Irritability Follow‐up: short term (up to 6 months) Measured via Aberrant Behaviour Checklist (Irritability subscale (ABC‐I), score range 0‐45; Aman 1985) and the Ritvo Freeman RealLife Rating Scale (RFRLRS; Freeman 1986). Lower scores indicate lower severity |
The mean score in the placebo group ranged from −8.40 to 25.5 | SMD 0.90 lower (95% CI 1.25 lower to 0.55 lower) | ‐ | 973 (12 studies: risperidone 6 studies; aripiprazole 5 studies; lurasidone 1 study) | ⊕⊕⊕⊝ Moderatea |
An SMD of 0.90 may represent a large effect (small = 0.2; medium = 0.5; and large = 0.8; Cohen 1988) |
|
|
Aggression Follow‐up: short term (up to 6 months) Measured via: Nisonger Child Behaviour Rating Form (conduct problem subscale; Aman 1996) Score range 0‐48: lower scores indicate lower severity |
The mean score in the placebo group was −6.6 | SMD 0.44 lower (95% CI 0.89 lower to 0.01 higher) | ‐ | 77 (1 study, risperidone) | ⊕⊝⊝⊝ Very lowb |
There was no clear evidence of a difference however, results are uncertain. | |
|
Self‐injury Follow‐up: short term (up to 6 months) Measured via: Self‐Injurious Behaviour Questionnaire (SIB‐Q Self‐injury subscale; Gualtieri 2002) Score range 0‐20; lower scores indicate lower severity |
The mean score in the placebo group was −4.90 | SMD 1.43 lower (95% CI 2.24 lower to 0.61 lower) | ‐ | 30 (1 study, risperidone) | ⊕⊕⊝⊝ Lowc |
An SMD of 1.43 may represent a large effect (small = 0.2; medium = 0.5; and large =0.8; Cohen 1988) | |
|
Adverse effects (AEs) Follow‐up: short term (up to 6 months) |
Neurological | There was evidence of a higher rate of AEs in the intervention group for dizziness (14% vs 3%, P = 0.04) | RR 4.19 (95% CI 1.10 higher to 16.00 higher; 2 studies, risperidone) | 974 (11 studies) |
⊕⊕⊝⊝ Lowd |
||
| There was evidence of a higher rate of AEs in the intervention group for fatigue (15% vs 5%, P < 0.001) | RR 2.58 (95% CI 1.68 higher to 3.97 higher; aripiprazole 2 studies; risperidone 4 studies) | ||||||
| There was evidence of a higher rate of AEs in the intervention group for sedation (18% vs 3%, P = 0.02) | RR 2.98 (95% CI 1.15 higher to 7.73 higher; aripiprazole 1 study; lurasidone 1 study; risperidone 4 studies) | ||||||
| There was evidence of a higher rate of AEs in the intervention group for somnolence (26% vs 6%, P < 0.00001) | RR 4.84 (95% CI 3.18 higher to 7.36 higher; aripiprazole 3 studies; lurasidone 1 study; risperidone 5 studies) | ||||||
| There was evidence of a higher rate of AEs in the intervention group for tremor (10% vs 1%, P = 0.003) | RR 5.99 (95% CI 1.87 higher to 19.19 higher; aripiprazole 3 studies; risperidone 2 studies) | ||||||
| There was little to no evidence of a difference between groups for: drowsiness (P = 0.06); extrapyramidal disorder (P = 0.15); hypersomnia (P = 0.29); lethargy (P = 0.19); restlessness (P = 0.98); or agitation (P = 0.23) | |||||||
| Psychological | There was little to no evidence of a difference between groups for anxiety (P = 0.42) or depression (P = 0.21). | 218 (4 studies) |
⊕⊝⊝⊝ Very lowe |
||||
| Metabolic | There was evidence of a higher rate of AEs in the intervention group for increased appetite | RR 2.38 (95% CI 1.69 higher to 3.34 higher; aripiprazole 3 studies; risperidone 5 studies) | 702 (8 studies) |
⊕⊕⊝⊝ Lowd |
|||
| There was little to no evidence of a difference between groups for decreased appetite (P = 0.11), weight gain (P = 0.10) or thirst (P = 0.39). | |||||||
| Musculoskeletal | There was little to no evidence of a difference between groups for rigidity (P = 0.13), movement disorder (P = 0.27) or dyskinesia (P = 0.28) | 182 (2 studies) |
⊕⊝⊝⊝ Lowf |
||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). AE: adverse effect; ASD: autism spectrum disorder; CI: confidence interval; RR: risk ratio; SMD: standardised mean difference | |||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||||||
aDowngraded 1 level for study limitations (high risk of bias across multiple domains). Not downgraded for inconsistency, as high I2 statistic (83%) can be attributed to 2 outlier studies. bDowngraded 1 level for study limitations (high risk of bias across multiple domains), 1 level for imprecision (small sample size of 77 participants) and 1 level for imprecision (95% confidence intervals includes both benefit and harm). cDowngraded 1 level for imprecision (small sample size of 30 participants), and 1 level for indirectness (available evidence relates to adults only). dDowngraded 1 level for study limitations (high risk of bias across multiple domains) and 1 level for inconsistency (direction of effect varies across studies). eDowngraded 1 level for study limitations (high risk of bias across multiple domains), 1 level for imprecision (small sample size of 79 participants), and 1 level for indirectness (available evidence relates to children only). fDowngraded 1 level for study limitations (high risk of bias across multiple domains), and 1 level for indirectness (available evidence relates to children only) and 1 level for imprecision (small sample size of 182 participants).
Summary of findings 2. Neurohormones compared to placebo for irritability, aggression, and self‐injury in autism spectrum disorder (ASD).
| Neurohormones compared to placebo for irritability, aggression, and self‐injury in autism spectrum disorder (ASD) | |||||||
| Patient or population: participants (any age) with a clinical diagnosis of ASD who have displayed one or more unwanted or challenging behaviours at baseline assessment Setting: hospital inpatient or outpatient centres, education or disability settings, mental health settings, or clinics and research centres associated with universities Intervention: neurohormones Comparison: placebo | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | ||
| Risk with placebo | Risk with neurohormones | ||||||
|
Irritability Follow‐up: short term (up to six months) Measured via Aberrant Behaviour Checklist (Irritability subscale) (ABC‐I) (Aman 1985, Score range (0‐45)). Lower scores indicate lower severity |
See comment | SMD 0.18 lower (95% CI 0.37 lower to 0.00 lower) | ‐ | 466 (8 studies: secretin 3 studies; ACTH 1 study; oxytocin 3 studies; vasopressin 1 study) | ⊕⊝⊝⊝ Very lowa |
An SMD of 0.18 may represent a small effect (small = 0.2; medium = 0.5; and large = 0.8; Cohen 1988) |
|
| Aggression | No data were reported for this outcome in this comparison | ||||||
| Self Injury | No data were reported for this outcome in this comparison | ||||||
|
Adverse effects Follow‐up: short term (up to six months) |
Neurological | There was evidence of a lower rate of AEs for headaches in the neurohormone group | RR 0.58 (95% CI 0.38 to 0.89) (7 studies: oxytocin 6 studies; balovaptan 1 study) | 863 participants (10 studies) |
⊕⊝⊝⊝ Very lowb |
‐ | |
| The was little to no evidence of a difference between groups for absence seizures (P = 0.52), aggression (P = 0.68), agitation (P = 0.67), decreased attention (P = 0.68), dizziness (P = 0.69), dysphoria (P = 0.49); excessive talking (P = 0.52), fatigue (P = 0.76), forgetfulness (P = 0.52), insomnia (P = 0.08), irritability (P = 0.22), leg shaking (P = 0.52), nervous sytem disorders (P = 0.47), oppositional (P = 0.69), restlessness (P = 0.67), seizure (P = 0.52), sedation (P = 0.16), somnolence (P = 0.22), tics (P = 0.49) | ‐ | ||||||
| Psychological | The was little to no evidence of a difference between groups for anxiety (P = 0.23), depression (P = 0.83), panic attacks (P = 0.45), psychiatric events (P = 0.21), or self‐injury (P = 1.00) | 570 participants (6 studies) |
⊕⊕⊝⊝ Lowc |
‐ | |||
| Metabolic | The was little to no evidence of a difference between groups for any of the metabolic AEs including decreased appetite (P = 0.19), increased appetite (P = 0.07), metabolism and nutrition disorders (P = 0.57), thirst (P = 0.62), weight change (P = 0.50), weight gain (P = 0.67), and weight loss (P = 0.20) | 515 participants (5 studies) |
⊕⊕⊝⊝ Lowc |
‐ | |||
| Musculoskeletal | The was little to no evidence of a difference between groups for muscle spasms (P = 0.52), musculoskeletal and connective tissues disorder (P = 0.50) and rhabdomyolysis (P = 0.81) | 355 participants (3 studies) |
⊕⊝⊝⊝ Very lowd |
‐ | |||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). AE: adverse effect; ASD: autism spectrum disorder; CI: confidence interval; RR: risk ratio; SMD: standardised mean difference | |||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||||||
aDowngraded 1 level for imprecision (95% CI includes both benefit and harm), 1 level for study limitations (all studies involved children) and 1 level for imprecision (95% confidence intervals includes both benefit and harm). bDowngraded 1 level for study limitations (high risk of bias across multiple domains), 1 level due to inconsistency (direction of effect varies across studies) and 1 level for imprecision (95% confidence intervals includes both benefit and harm). cDowngraded 1 level for study limitations (high risk of bias across multiple domains), and 1 level for imprecision (95% confidence intervals includes both benefit and harm). dDowngraded 1 level for imprecision (95% CI includes both benefit and harm), 1 level for study limitations (high risk of bias across multiple domains) and 1 level for imprecision (95% confidence intervals includes both benefit and harm).
Summary of findings 3. Attention deficit hyperactivity disorder (ADHD)‐related drugs compared to placebo for irritability, aggression, and self‐injury in autism spectrum disorder (ASD).
| ADHD‐related medications compared to placebo for irritability, aggression, and self‐injury in autism spectrum disorder (ASD) | ||||||
| Patient or population: participants (any age) with a clinical diagnosis of ASD who have displayed one or more unwanted or challenging behaviours at baseline assessment Setting: hospital inpatient or outpatient centres, education or disability settings, mental health settings, or clinics and research centres associated with universities Intervention: ADHD‐related medications Comparison: placebo | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with placebo | Risk with ADHD‐related drugs | |||||
|
Irritability All ADHD‐related medications Follow‐up: short term (up to six months) Measured via Aberrant Behaviour Checklist (Irritability subscale) (Score range (0‐45)) (Aman 1985) and the Ritvo‐Freeman Real Life Rating Scale (Freeman 1986 (score range 0‐15). Lower scores indicate lower severity. |
See comment | SMD 0.20 lower (95% CI 0.40 lower to 0.01 lower) | ‐ | 400 (10 studies: methylphenidate 2 studies; clonidine 2 studies; guanfacine 2 studies; atomoxetine 4 studies) | ⊕⊕⊝⊝ Lowa |
An SMD of 0.20 may represent a small effect size (small = 0.2; medium =0.5; large = 0.8, Cohen 1988). |
| Aggression | No data were reported for this outcome in this comparison | |||||
|
Self‐injury Follow‐up: short term (up to six months) Measured via the Repetitive Behaviour Scale ‐ Revised (self‐injury subscale) (Bodfish 2000) |
See comment | SMD 0.62 lower (95% CI 1.63 lower to 0.39 higher) | ‐ | 16 participants (1 study) | ⊕⊝⊝⊝ Very lowb |
There was no clear evidence of a difference, but results are uncertain. |
|
Adverse effects Follow‐up: short term (up to six months) |
Neurological | There was evidence of a higher rate of AEs in the intervention group for drowsiness | RR 3.42 (95% CI 1.54 higher to 7.59 higher); atomoxetine 2 studies; guanfacine 1 study; methylphenidate 1 study) | 511 (9 studies) |
⊕⊝⊝⊝ Very lowc |
‐ |
| There was evidence of a higher rate of AEs in the intervention group for emotional | RR 6.32 (95% CI 2.47 higher to 16.18 higher); methylphenidate 1 study; guanfacine 1 study | |||||
| There was evidence of a higher rate of AEs in the intervention group for fatigue | RR 3.73 (95% CI 1.98 higher to 7.03higher); atomoxetine 3 studies; guanfacine 1 study | |||||
| There was evidence of a higher rate of AEs in the intervention group for headache | RR 1.63 (95% CI 1.09 higher to 2.44 higher); atomoxetine 4 studies; methylphenidate 2 studies; guanfacine 1 study; amphetamine 1 study | |||||
| There was evidence of a higher rate of AEs in the intervention group for insomnia | RR 1.58 (95% CI 1.01 higher to 2.47 higher); methylphenidate 2 studies; atomoxetine 3 studies; guanfacine 1 study; amphetamine 1 study | |||||
| There was evidence of a higher rate of AEs in the intervention group for irritability | RR 1.61 (95% CI 1.25 to 2.07 higher); atomoxetine 3 studies; guanfacine 1 study; methylphenidate 2 studies | |||||
| There was little to no evidence of a difference between groups for aggression (P = 0.82), agitation (P = 0.85), dizziness (P = 0.22), drowsiness (P = 0.003), hyperactivity (P = 0.75), increased motor activity (P = 0.36), motor tics (P = 0.28), nightmares (P = 0.57), repetitive behaviour (P = 0.23), restlessness (P = 0.80), sleep disturbance (P = 0.76), talking excessively (P = 0.05), waking (P = 0.59), or tremor (P = 0.48). | ||||||
| Psychological | There was evidence of a higher rate of depression in the intervention group | RR 2.45 higher (95% CI 1.12 higher to 5.36 higher); methylphenidate 2 studies; guanfacine 1 study | 252 (5 studies) |
⊕⊝⊝⊝ Very lowd |
‐ | |
| There was little to no evidence of a difference between groups for anxiety (P = 0.30); mood change (P = 0.07), "silly behaviour" (P = 0.51), self‐injury (P = 0.19), or social withdrawal (P = 0.36). | ||||||
| Metabolic | There was evidence of a higher rate of AEs in the intervention group for decreased appetite | RR 2.15 (95% CI 1.55 higher to 2.99 higher); atomoxetine 5 studies; guanfacine 1 study; amphetamine 1 study; methylphenidate 2 studies | 511 (9 studies) |
⊕⊝⊝⊝ Very lowc |
‐ | |
| There was little to no evidence of a difference between groups for increased appetite (P = 0.63) and increased energy (P = 0.31). | ||||||
| Musculoskeletal | No data were reported for this outcome in this comparison. | |||||
| AE: adverse effect; ASD: autism spectrum disorder; CI: confidence interval; RR: risk ratio; SMD: standardised mean difference | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded 1 level due to study limitations (high risk of bias across multiple domains) and 1 level due to imprecision (95% confidence intervals includes both benefit and harm). bDowngraded 1 level due to study limitations (high risk of bias across multiple domains) and 1 level for indirectness (available evidence relates to children only) and 1 level for imprecision (small sample size of n = 16 and 95% confidence intervals includes both benefit and harm). cDowngraded 1 level due to study limitations (only involving children), 1 level due to inconsistency (direction of effect varies across studies) and 1 level due to imprecision (95% confidence intervals includes both benefit and harm). dDowngraded 1 level due to study limitations (high risk of bias across multiple domains), 1 level due to inconsistency (direction of effect varies across studies) and 1 level due to imprecision (95% confidence intervals includes both benefit and harm).
Summary of findings 4. Antidepressants compared to placebo for irritability, aggression, and self‐injury in autism spectrum disorder (ASD).
| Antidepressants compared to placebo for irritability, aggression, and self‐injury in autism spectrum disorder (ASD) | |||||||
| Patient or population: participants (any age) with a clinical diagnosis of ASD who have displayed one or more unwanted or challenging behaviours at baseline assessment Setting: hospital inpatient or outpatient centres, education or disability settings, mental health settings, or clinics and research centres associated with universities Intervention: antidepressants Comparison: placebo | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | ||
| Risk with placebo | Risk with antidepressants | ||||||
|
Irritability Follow‐up: short term (up to six months) Measured via Aberrant Behaviour Checklist (Irritability subscale) (ABC‐I) (Aman 1985), Score range (0‐45) Lower scores indicate lower severity |
The mean score in the placebo group ranged from 10.2 to 13.8 | SMD 0.06 lower (95% CI 0.30 lower to 0.18 higher) | ‐ | 267 (3 studies) | ⊕⊕⊝⊝ Lowa |
There was no evidence of a difference, but results are uncertain. | |
| Aggression | No data were reported for this outcome in this comparison | ||||||
| Self‐injurious behaviour ‐ no data could be used for this outcome because of skewness (see Table 5) | |||||||
|
Adverse effects Follow‐up: short term (up to six months) |
Neurological | There was evidence of a higher rate of decreased attention in the intervention group | RR 4.16 (95% CI 1.07 higher to 16.11 higher); citalopram 1 study; clomipramine 1 study; fluoxetine 5 studies; fluvoxamine 1 study; sertraline 1 study; tianeptine 1 study | 815 (10 studies) |
⊕⊕⊝⊝ Lowb |
||
| The was little to no evidence of a difference between groups for any of the other neurological adverse effects including activation syndrome (P = 0.64), agitation (P = 0.96), aggression or hostility (P = 0.83), anger or irritability (P = 0.35), autonomic disturbance (P = 0.83), CNS disturbance (P = 0.50), diaphoresis (sweating) (P = 0.49), drowsiness (P = 0.50), headache (P = 0.23), hyperactivity (P = 0.36), insomnia (P = 0.29), sedation (P = 0.16), sleep disturbance (P = 0.76), mood lability (P = 0.43), restlessness (P = 0.13), twitching (P = 0.17), tremor (P = 0.22), or vertigo (P = 0.65) | |||||||
| Psychological | The was evidence of a higher rate of AEs in the intervention
group for impulsive behaviour |
RR 2.92 (95% CI 1.11 higher to 7.68 higher); citalopram 1 study | 243 (4 studies) |
⊕⊝⊝⊝ Very lowc |
|||
| The was evidence of a higher rate of AEs in the intervention group for stereotypy | RR 8.33 (95% CI 1.07 higher to 64.95 higher); citalopram 1 study | ||||||
| The was little to no evidence of a difference between groups for anorexia (P = 0.42), verbal aggression (P = 0.36), suicidal ideation (P = 0.65), bad dreams (P = 0.28), unstable mood (P = 0.66), anxiety (P = 0.16) and depression (P = 0.79) | |||||||
| Metabolic | There was evidence of a higher rate of decreased energy in the antidepressant group | RR 1.94 (95% CI 1.13 higher to 3.33 higher); citalopram 1 study | 512 (7 studies) |
⊕⊝⊝⊝ Very lowd |
|||
| The was little to no evidence of a difference between groups for appetite disturbance (P = 0.40), decreased appetite (P = 0.39), increased appetite (P = 0.85), and weight gain (P = 0.80) | |||||||
| Musculoskeletal | The was little to no evidence of a difference between groups for motor disturbance (P = 0.30) or neck pain (P = 0.65) | 202 (2 studies) |
⊕⊝⊝⊝ Very lowe |
||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). AE: adverse effect; ASD: autism spectrum disorder; CI: confidence interval; CNS: central nervous system; RR: risk ratio; SMD: standardised mean difference | |||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||||||
aDowngraded 1 level for imprecision (95% confidence intervals includes both benefit and harm), and 1 level for imprecision (small sample size of n = 267). bDowngraded 1 level for study limitations (high risk of bias across multiple domains) and 1 level for imprecision (95% confidence intervals include both benefit and harm). cDowngraded 1 level for study limitations (high risk of bias across multiple domains), 1 level for inconsistency (direction of effect varied across studies) and 1 level for imprecision (small sample size of n = 279). dDowngraded 1 level for study limitations (high risk of bias across multiple domains), 1 level for inconsistency (direction of effect varied across studies and 1 level for imprecision (95% confidence intervals includes both benefit and harm). eDowngraded 1 level for study limitations (high risk of bias across multiple domains), 1 level for imprecision (small sample size of n=202), and 1 level for imprecision (95% confidence intervals includes both benefit and harm).
1. Antidepressant versus placebo: self‐injurious behaviour results that could not be used in meta‐analyses.
| Study name | Short‐/ medium‐/ long‐term outcomes | Group 1 | Group 2 | Group 1 sample size | Group 2 sample size | Group 1 results | Group 2 results | Other data | Notes |
| Carminati 2016 | Short‐term self‐injurious behaviour | Venlafaxine 18.75 mg/day | Placebo | 6 | 7 | Median 1 (range 0‐13) | Median 3 (range 0‐8) | ‐ | ‐ |
| King 2001 | Short‐term self‐injurious behaviour | Citalopram (max 20 mg/day) | Placebo | 73 | 76 | 2.4 (2.7) | 2.0 (2.6) | ‐ | Skewed |
| Mouti 2014 | Short‐term self‐injurious behaviour | Fluoxetine (max 20‐30 mg) | Placebo | 53 | 53 | 2.09 (3.01) | 3.55 (4.59) | ‐ | Skewed |
Background
Description of the condition
Autism spectrum disorder (ASD) is characterised by persistent deficits in social communication and social interaction across multiple contexts, as well as restricted repetitive patterns of behaviour, interests, or activities (DSM‐5 2013). There are currently five diagnostic criteria used by the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM‐5 2013), for the diagnosis of ASD, including 1) persistent deficits in social communication and social interaction across multiple contexts; 2) restricted, repetitive patterns of behaviour, interests, or activities; 3) presentation of symptoms in the early developmental period; 4) symptoms that cause clinically significant impairment in important areas of current functioning; and 5) disturbances that are not better explained by intellectual disability (intellectual developmental disorder) or global developmental delay (DSM‐5 2013).
Thirty years ago, research suggested that ASD was a rare categorical disorder with a prevalence of 4 in 10,000 (Baron‐Cohen 2008); more recent prevalence studies show it to be a common condition with a prevalence of approximately 1% of the population across most countries (Arora 2018; Cleaton 2018; Elsabbagh 2012; Ritchie 2020). However, prevalence varies between countries, with higher rates in high‐income countries such as the USA and UK, estimated to be 1% to 3%, whereas rates in lower‐income countries are 0.5% or less (Cleaton 2018; Ritchie 2020).
Some have attributed this rise to a true increase in the problems seen in ASD. Others have disputed this, attributing the rise to factors such as earlier diagnosis, broadening of diagnostic criteria (May 2020; Tantam 2012) and changes in diagnostic attribution (May 2017; Turowetz 2015). The prevalence of ASD in men is reported to exceed that in women, although the exact ratio may be impossible to specify; a recent review reported an overall male to female ratio of 3:1 (Loomes 2017).
The lower prevalence of ASD in lower‐income countries has been attributed to a relative lack of epidemiological studies in low‐income countries (Matos 2022), and multiple factors including community awareness, cost and capacity of health and other services, information seeking, and socio‐demographic factors (Zeidan 2022). In addition, some have suggested that due to financial restraints, low‐income countries often use their own or other criteria compared to more widely‐used criteria such as the DSM‐5 2013 to diagnose ASD (Peiris 2022). Because various ASD criteria and diagnostic tools are being used, this may explain the lack of consistency particularly between low‐income and high‐income countries.
The authors of this review are aware that a substantial proportion of the autistic community prefer to describe themselves as autistic, an autistic person, or on the spectrum, rather than person with autism or ASD (Autism Spectrum Australia 2023; Autistic Self Advocacy Network 2023; National Autistic Society 2023). However, preferences vary and throughout this review the authors will be using standard notation of 'person with ASD'.
Behaviours of concern
The terms 'challenging behaviour' (Emerson 1995), and 'behaviours that challenge' (NICE 2015), are widely used in the literature to describe behaviours such as irritability, aggression, and self‐injury. However, many behaviours seen as being challenging and framed as inherent to the person with autism could be better understood as legitimate responses to difficult environments and situations (Ramcharan 2009). 'Challenging behaviours', therefore, have also been described as reactive and responsive behaviours, distressed behaviours, expressions of unmet need, and in Australia, behaviours of concern. Throughout this review we use the term 'behaviours of concern', because it is a term that is increasingly being used internationally.
Irritability is an ambiguous term that is often not well‐defined. Irritability is defined by the DSM‐5 2013 as "persistent anger, a tendency to respond to events with angry outbursts or blaming others, an exaggerated sense of frustration over minor matters". Other emotions and behaviours such as anger and aggression are often associated with irritability, however, they are usually consequences of irritability rather than a trait of irritability (Benarous 2019; Toohey 2017).
In addition to the core symptoms, people with ASD may exhibit behaviours of concern. These can include behaviours such as agitation, aggression, self‐injury, destruction to property, disruptive behaviour, sexual misconduct, or arson (NICE 2015; Sheehan 2015). Neurodevelopmental disorders included in the DSM‐5 such as attention deficit hyperactivity disorder (ADHD), ASD, intellectual disability, specific learning disorders, or impairments in social interaction, communication, or movement are associated with behaviours of concern (Cleaton 2018; DSM‐5 2013), with increasing severity of disability associated with an increased likelihood, frequency, and severity of behaviours of concern (Emerson 2001; Matson 2009; McTiernan 2011).
The reported prevalence of behaviours of concern varies. It is estimated that between 5% and 15% of people with ASD develop behaviours of concern (NICE 2015), with a higher prevalence of greater than 25% reported in children (Hill 2014; Kanne 2011; Soke 2016). Prevalence tends to also be higher in particular circumstances such as in hospitals, amongst teenagers, people in their early twenties, men and boys, people with comorbid psychiatric diagnoses (NICE 2015), and people with dual diagnoses of intellectual disability and ASD (Fitzpatrick 2016; Kanne 2011; Tyrer 2006).
There appears to be a high co‐occurrence of other neurodevelopmental disorders with ASD, such as attention deficit hyperactivity disorder (ADHD; DSM‐5 2013). People with co‐occurring ASD and ADHD may have a higher incidence of behaviours of concern, which is not surprising given that such behaviours are reported in both disorders (Craig 2015; Ringer 2020). Furthermore, there is also co‐occurrence of mental health disorders with ASD, notably anxiety and depression (Hollocks 2019; Koritsas 2015; Lord 2018). Approximately 40% of children and 27% of adults with ASD are reported to also have at least one anxiety disorder (Hollocks 2019; Van Steensel 2011). Over 20% of adults with ASD are reported to have a current diagnosis of depression (Van Steensel 2011). When there are co‐occurring diagnoses, medications such as stimulants, anxiolytics or antidepressants may be prescribed to treat the co‐occurring condition.
The presence of behaviours of concern add complexity to living with and supporting people with ASD. Not only can this result in families and informal carers experiencing high levels of stress, they can also create barriers to adult independence and community involvement (Smith 2014).
Description of the intervention
Interventions that target core symptoms of ASD or co‐occurring difficulties can be associated with positive outcomes in areas such as cognitive functioning, language skills, social behaviours, and reduction of behaviours of concern (Seida 2009; Weitlauf 2014).
For individuals with ASD, environmental modifications, non‐pharmacological interventions (such as educational interventions and behavioural and psychological therapies) and pharmacological interventions (medication and other biological therapies) are commonly suggested treatments and can help reduce behaviours of concern such as irritability, aggression and self‐injury (Perez 2012; Posey 2001; Sengupta 2017).
This review will focus solely on pharmacological interventions that are used to target irritability, aggression or self‐injury in people with ASD. The major drug classes of interest were typical and atypical antipsychotics, ADHD‐related medications, anticonvulsants, anti‐dementia medications, antidepressants, antiparkinsonian medications, anxiolytics, neurohormones, and a number of drugs that did not fall into any of these classes and that we grouped under an 'experimental' category. These drug classes were based on the major classes listed in the review protocol (Livingstone 2015), as well as additional pharmacological classes identified from the search results (see Appendix 1 for search strategy).
Antipsychotics
Antipsychotics are medications that treat disorganised thinking and poor awareness of reality. The use of antipsychotics has also been associated with reduced irritability, social withdrawal, hyperactivity, and stereotypical behaviours in young people with ASD (Jesner 2007). First‐generation or 'typical antipsychotics' such as haloperidol were first used in the 1950s to treat people with schizophrenia. Second‐generation or 'atypical antipsychotics' such as aripiprazole and risperidone were introduced in the 1980s because of their reduced risk of long‐term and irreversible adverse effects (AEs) when compared to typical antipsychotics. Antipsychotic medications are psychotropic agents frequently prescribed for people with ASD (Coury 2012; Howes 2018; Loy 2017; Madden 2017; Murray 2014; Rasmussen 2019), often in the absence of a diagnosed mental disorder (Cvejic 2018; Deb 2009; Deb 2015; Sheehan 2015). Large‐scale studies have shown that around 5% to 15% of people with ASD are prescribed antipsychotics (Coury 2012; Howes 2018; Lake 2017; Murray 2014; Rasmussen 2019). Antipsychotics are commonly prescribed for hyperactivity, aggression, and other behaviours of concern (Dinnissen 2020; Henderson 2020), and antipsychotic prescribing is more prevalent amongst people with autism and/or intellectual disability compared to the general population (Glover 2015; Henderson 2020).
Although antipsychotics are not recommended for the treatment of core symptoms of ASD (Howes 2018), there is increasing evidence that antipsychotics decrease behaviours of concern in people with ASD (Howes 2018; Jesner 2007). Since publication of the protocol for this review (Livingstone 2015), seven systematic reviews reporting the effectiveness of antipsychotics on behaviours of concern in people with autism, predominantly children and adolescents, have been published (D’Alò 2021; Fallah 2019; Fung 2016; Hirsch 2016; Maneeton 2018a; Maneeton 2018b; Mano‐Sousa 2021). Although results were mixed, the majority of evidence for the effectiveness of antipsychotic medications in reducing behaviours of concern was reported for the atypical antipsychotics, aripiprazole and risperidone.
There is some concern regarding the long‐term health outcomes of antipsychotic use, such as significant weight gain (Alvarez‐Jiménez 2008; Bak 2014; Lake 2017), increased risk of diabetes mellitus (Holt 2019), increased prevalence of cardiovascular disease such as stroke and heart attack (Zivkovic 2019), and increased risk of all‐cause mortality (Simon 2015; Trifirò 2009). The National Institute for Health and Care Excellence (NICE) Guidelines recommend that antipsychotic medications should only be considered if behaviours of concern have not been reduced by psychological or other interventions, treatment for any co‐existing psychiatric disorders and the person or others are at severe risk of harm (NICE 2015). Other guidelines recommend that antipsychotics are only a short‐term option (up to 8 weeks) if non‐pharmacological interventions did not reduce the behaviours of concern. Effectiveness should be reviewed after three or four weeks on the drugs before continuing (SIGN 2016), and only one drug should be trialled at any one time to determine its effectiveness (Deb 2009).
ADHD‐related medications
ADHD‐related medications are often prescribed to people with ASD who exhibit behaviours of concern, at least in part due to some similarities between ASD and ADHD such as hyperactivity, inattention and social or communication deficits, or both (Cortese 2012; Hanson 2013; Mikami 2019; Rosello 2018), as well as the high comorbidity rates of ADHD amongst people with ASD (Antshel 2013; Sokolova 2017). In the past, stimulant medications have been prescribed to people with ASD who show behaviours of concern and have hyperactivity (Cortese 2012; Hanson 2013; Mikami 2019; Rosello 2018). Since 2013, when a dual diagnosis of ADHD and ASD was permitted, a high prevalence of co‐occurring ASD and ADHD has been reported (Antshel 2013; Sokolova 2017). Stimulants such as methylphenidate are the most commonly prescribed psychotropic medications for people with ASD aged six years and older, with prescribing rates up to 34% reported in large multinational studies (Houghton 2017; Hsia 2014; Murray 2014), and 17% in an Australian study (Rasmussen 2019).
Stimulants and non‐stimulants have also been reported to reduce symptoms of irritability and aggression in people with ASD (Banas 2020; Handen 2008; Ming 2008), and are some of the most prescribed psychotropics for people with ASD (Madden 2017). Stimulants such as methylphenidate, have also been recommended as adjuncts to behavioural interventions for hyperactivity in children or young people with co‐occurring ASD and ADHD (SIGN 2016). However, a narrative synthesis by Ghanizadeh 2019 concluded there was inadequate evidence to support or refute the effect of methylphenidate on irritability, while a Cochrane Review found no evidence that rates of treatment‐emergent irritability were different in children and adolescents with ASD taking methylphenidate (Sturman 2017).
Anticonvulsants
Anticonvulsants are primarily used to reduce seizures (Wassenaar 2013; Wlodarczyk 2012). Seizures associated with epilepsy are caused by abnormal and asynchronous firing of neurons (nerve cells) which usually end abruptly (DeLorenzo 2005; Geiger 2011; Kusmaker 2018; Proix 2018). Most anticonvulsants such as carbamazepine, phenobarbital and valproate block voltage‐gated sodium channels to reduce the firing of neurons (Verrotti 2010). Some anticonvulsants such as levetiracetam, topiramate or valproate also have a role in the release or modulation of the inhibitory neurotransmitter GABA (Cortes‐Altamirano 2016), decreasing the speed and firing of neurons. Some anticonvulsants are also used as mood stabilisers, for example, divalproex sodium, primarily in bipolar illness. Use of these medications has also been associated with reduction in affective instability, impulsivity and aggression in ASD (Hollander 2001).
In a systematic review of anticonvulsants for psychiatric disorders in children and adolescents, two trials of valproate and one of levetiracetam found no effect on aggression; however, an additional trial reported a decrease of irritability and aggression in the valproate group (Davico 2018). There was no difference in aggression in the remaining trial of participants with ASD, which compared to placebo. In another review of GABA modulators in autism by Brondino 2016, there was no difference in aggression and irritability in one study that evaluated valproate, while the other found valproate reduced irritability. Similarly, in the systematic review of the pharmacologic treatment of severe irritability and aggression in 2‐ to 17‐year‐olds with ASD by Fung 2016, one of the two small trials comparing valproate to placebo found it reduced the Aberrant Behaviour Checklist Irritability subscale (ABC‐I; Aman 1985) scores, with no apparent effect in the other.
Antidementia medications
Antidementia medications include cholinesterase inhibitors and N‐methyl‐D‐aspartate (NMDA) receptor antagonists, which are primarily used to treat individuals with Alzheimer’s dementia. Previous studies have shown that the cholinesterase inhibitor donepezil, has been associated with changes in aberrant behaviours of children with ASD (Chez 2003). Research also indicates that the NMDA receptor antagonist, memantine, could improve social behaviour, self‐stimulatory behaviours (Chez 2004), and irritability (Erickson 2007), in people with ASD.
Antidepressants
Antidepressants, such as selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants, are used to treat symptoms of depression, anxiety, and obsessionality and are commonly prescribed for people with ASD (Coury 2012; Howes 2018; Murray 2014); often in the absence of a diagnosed mental disorder (Cvejic 2018; Sheehan 2015; Tsouris 2013). Large‐scale studies involving people with ASD have found that antidepressants are prescribed at similar rates to antipsychotics and stimulants, and often concurrently (up to 40%) with antipsychotics (Branford 2019; Cvejic 2018; Esbensen 2009). In addition, the use of antidepressants amongst people with ASD in large‐scale studies is approximately eight times higher than in people without ASD (Madden 2017). However, there is no clear evidence of the effectiveness of antidepressants in reducing behaviours of concern in people with ASD (Branford 2019; Hurwitz 2012; Johnco 2015; Williams 2013).
Two Cochrane Reviews evaluated the effects of these two major classes of antidepressants on ASD. In one Cochrane Review of SSRIs for ASD (Williams 2013), there was limited evidence that citalopram reduced irritability but no evidence that fenfluramine and fluoxetine had an effect. In a Cochrane Review of tricyclic antidepressants for ASD in children and adolescents, there was no evidence that clomipramine and tianeptine improved irritability relative to placebo (Hurwitz 2012); however, the three included trials were very small. In an additional systematic review of antidepressant and antianxiety medications for people with ASD (Deb 2021), there was no evidence that citalopram, clomipramine, venlafaxine or fluoxetine decreased behaviours of concern, but one of two trials of fluvoxamine showed reduced aggression.
Antiparkinsonian medications
Antiparkinsonian medications are primarily used to treat individuals who have Parkinson's disease and Alzheimer’s dementia. Some antiparkinsonian medications, such as amantadine, have been studied for the treatment of people with ASD to address symptoms of irritability and aggression. A double‐blind, placebo‐controlled trial of children with ASD aged 5 to 19 years found that symptoms of irritability and aggression were reduced in those receiving amantadine as the active medication (King 2001). Other studies have reported that they may improve language function, social behaviour, and self‐stimulatory behaviours of some people with ASD (Chez 2004). A smaller improvement in irritability symptoms has also been reported (Erickson 2007). In a systematic review of pharmacologic treatment in 2‐ to 17‐year‐olds with ASD (Fung 2016), there was no evidence that amantadine decreased ABC‐I scores in the one small identified placebo‐controlled trial.
Anxiolytics
As anxiety is associated with behaviours of concern (Johnco 2015; Nadeau 2011;NICE 2015), anxiolytics may be effective in reducing behaviours of concern in people with ASD and anxiety (Bitsika 2016; Johnco 2015). Anxiolytics such as buspirone are commonly used to treat generalised anxiety disorder (Schmitt 2005). Compared to benzodiazepines, buspirone has a reduced risk of dependency, abuse and sedation, and so is sometimes considered a safer option for long‐term management of anxiety disorders, particularly amongst the young or elderly populations (Crocco 2017; Schmitt 2005). Buspirone is also considered a treatment for older adults or children with aggression, irritability, or agitation (Aronson 2016; Howland 2015), and as such, may be effective in reducing behaviours of concern in people with ASD. In the systematic review by Deb 2021, one of two parallel trials of buspirone showed a decrease in irritability.
Neurohormones
Neurohormones are hormones produced by nerve cells and secreted into the circulation with varying mechanisms of action and sites of origin. Two neurohormones have been investigated in ASD, namely oxytocin and secretin. Secretin has been suggested as potentially beneficial in the management of ASD and related behaviours of concern (McQueen 2002; Tanaka 2018). However, in an earlier Cochrane Review of intravenous secretin compared to placebo treatment in children or adults diagnosed with ASD, there was no effect of secretin in any of the three studies that reported irritability (Williams 2012).
Experimental
Effects have previously been reported for a range of medications that do not fall into any of the previously mentioned categories. A systematic review of trials of GABA modulators in autism evaluated acamprosate, arbaclofen, bumetanide, carnosine, flumazenil, riluzole and valproate (Brondino 2016). However, there was insufficient evidence to suggest that any of these medications were effective in people with autism (Brondino 2016). In a review of the drug riluzole, which also appears to regulate glutamate activity (De Boer 2019), two of three studies in children and young adults reported that single and adjunct use of riluzole decreased irritability, although there was no effect in the remaining trial. In a meta‐analysis of n‐acetylcysteine in ASD (Lee 2021), irritability scores were not different across all four identified studies, though a subgroup study indicated effects in one trial.
How the intervention might work
While each of these medications works differently, broadly speaking, medications may act by reducing co‐occurring conditions, like ADHD, anxiety or depression, or will act directly to reduce behaviours of concern. However, there is limited evidence for the effectiveness of these medications at this stage.
Antipsychotics
ASD has been associated with abnormalities in both the dopaminergic system and serotoninergic systems (Nakamura 2010). Dopamine over‐activation has also been linked with excessive motor activity and stereotyped behaviours, which are often observed in individuals with ASD (Previc 2007). Altered serotonin levels have been found to lead to changes in several psychological processes, which are also altered in individuals with ASD, including mood, irritability, and aggression (Young 2002). Typical or first‐generation antipsychotics exert their action by blocking dopamine receptors. However, atypical (second‐generation) antipsychotics also have a range of actions at other neurotransmitter systems, including systems that modulate serotonin and norepinephrine receptors.
Antidepressants
The two major classes of antidepressants prescribed for ASD (SSRIs and tricyclic antidepressants) have differing pharmacological actions. SSRIs exert their effects through increasing the availability of serotonin (Williams 2013), whereas tricyclic antidepressants increase the availability of the neurotransmitters serotonin and noradrenaline (Hurwitz 2012; Shojaie 2020). Altered serotonin levels have been found to lead to changes in several psychological processes, which are also altered in individuals with ASD, including mood, irritability, and aggression (Young 2002; Williams 2013). Antidepressants may be effective in treating some common comorbidities of ASD such as anxiety, depression, and obsessive compulsive disorder, which can in turn reduce behaviours of concern (Williams 2013; Zaboski 2018).
Anticonvulsants
The mechanism by which antiepileptic medications, such as carbamazepine and levetiracetam, could affect irritability and aggression remains unclear. What is known is that gabapentin reduces the excitability of nerve cells in the brain (Guglielmo 2013).
Anticonvulsants such as divalproex sodium are also used as mood stabilisers. It has been suggested that mood stabilisers, such as divalproex sodium, work by enhancing GABA, inhibiting glutamate, acting on serotonin and norepinephrine systems, and via limbic kindling (Hollander 2001).
ADHD‐related medications
These include stimulants such as methylphenidate and dexamphetamine that increase dopamine and noradrenaline activity; and non‐stimulants such as atomoxetine, clonidine and guanfacine, which primarily increase noradrenaline activity (Osland 2018).
Stimulant (Ghanizadeh 2019; Sturman 2017), and nonstimulant (Banas 2020; Ghanizadeh 2013; Patra 2019), ADHD‐related medications have been administered to children with ASD with the aim of improving symptoms. It is thought that any effects on behaviours of concern with ADHD‐related medications are likely to be secondary to improvements in attention, concentration and hyperactivity (Banas 2020).
ADHD is often associated with dopaminergic system dysfunction (Froehlich 2013; Huss 2016; Wu 2012). Dopamine plays an important role in planning, motor and motivational processes, which are abnormal in people with ADHD (Marinho 2018; Wu 2012). Stimulants such as amphetamine and methylphenidate are thought to improve symptoms of ADHD by increasing dopamine activity (Wu 2012).
The neurotransmitter, noradrenaline, may also decrease symptoms of ADHD as it has an important role in the prefrontal cortex, an area associated with attention and executive functioning (Patra 2019). Non‐stimulants such as atomoxetine, clonidine and guanfacine, which primarily increase noradrenaline activity, are sometimes prescribed as an alternative to stimulant ADHD‐related medications.
Atomoxetine is a dopamine and noradrenaline reuptake inhibitor (Froehlich 2013; Janak 2012). The increase in norepinephrine and dopamine in the pre‐frontal cortex by atomoxetine is thought to improve ADHD symptoms such as impaired attention and reduced executive function (Patra 2019; Ulke 2019). Clonidine and guanfacine are alpha‐2 adrenergic receptor agonists (Giovannitti 2015; Huss 2016), and are thought to improve ADHD symptoms by increasing noradrenergic activity in the prefrontal cortex (Caye 2019; Mechler 2022).
Antidementia medications
As described above, impairments in the dopaminergic system have been associated with behavioural characteristics of several neurodevelopmental disorders, including ASD (DiCarlo 2019). Amantadine is an NMDA receptor antagonist with an indirect dopaminergic agonist role (King 2001; Müller 2012).
The NMDA receptors play an important role in the cellular processes of the brain underlying learning and memory function (Chang 2021; Olivares 2012). NMDA also plays a role in regulating inflammation in the brain (Chang 2021), and it is thought that neuro inflammation is involved in neurological and neuropsychiatric disorders (Ricci 2013). The precise mechanisms by which NMDA receptor antagonists work is not well known, however, it has been found that people with ASD often have abnormally high glutamate and activity levels of NMDA receptors (Rojas 2014). Therefore, it is thought that NMDA receptor antagonists such as memantine may play a role in reducing the core symptoms of ASD.
Antiparkinsonian medications
Cholinergic neurotransmission, including nicotinic acetylcholine receptors, are involved in several functions including attention, memory, learning, social interactions, movement, and anxiety (Park 2022; Vallés 2021). The cholinergic system is thought to play a central role in Alzheimer's disease, particularly the associated cognitive decline (Sabri 2008), and nicotinic acetylcholine receptors are thought to have anti‐inflammatory and neuroprotective properties (Park 2022).
According to recent studies, acetylcholine and nicotinic receptor activity may be lower in brain samples of people with ASD. It has been suggested, therefore, that acetylcholinergic enhancement through the use of donepezil hydrochloride — an acetylcholinesterase inhibitor — may improve some behaviours associated with ASD (Chez 2003).
Anxiolytics
People with ASD commonly have elevated levels of blood serotonin (Anderson 1987), however, people with ASD also have an increased risk of alterations to serotonin receptors and synthesis (Veenstra‐VanderWeele 2012). Anxiolytics such as buspirone have a strong attraction to serotonin, both presynaptically and postsynaptically (Ceranoglu 2019; Poisbeau 2018), thereby increasing the availability of serotonin. Serotonin plays a role in regulating mood and sleep, and medications that increase serotonin are often prescribed for anxiety due to the anxiolytic effect of serotonin (Żmudzka 2018).
Neurohormones
Oxytocin is produced in the hypothalamus (Wilczyński 2019), with the primary role of promoting lactation, facilitating contractions, and promoting bonding between mother and infant (Andari 2010; Green 2010;Taylor 2018). Oxytocin has been found to be reduced in children with ASD (John 2021; Moerkerke 2021), and oxytocin is thought to have a role in ASD behaviours (Gottschalk 2017; Ooi 2017; Yamasue 2017; Yoon 2020). It has been suggested that increasing oxytocin will reduce ASD behaviours and this could lead to a reduction of behaviours of concern.
Secretin is produced in the gastrointestinal tract and has both digestive and neurological functions (Banko 2011; Welch 2004). Because secretin receptors are also located in areas of the brain associated with emotion and behaviour, such as in the amygdala, which regulates emotions and mood, and in the hippocampus, which is associated with memory formation (Banko 2011; Qi 2020), impairments or irregularities in brain neurohormones may be associated with ASD (Chaddad 2017; Gibbard 2018). Secretin has therefore been suggested as a potential intervention in the management of ASD (Krishnaswami 2011; McQueen 2002; Tanaka 2018).
Why it is important to do this review
To date, there have been five published Cochrane systematic reviews focusing on the use of pharmacological interventions in ASD. A review on risperidone found evidence that the medication may lead to significant improvements in irritability (Jesner 2007). Two reviews on aripiprazole also found evidence of improvements in irritability (Ching 2012; Hirsch 2016). A review of tricyclic antidepressants found small positive effects in children and adolescents with ASD, particularly in reducing irritability, although results were inconsistent (Hurwitz 2012). A review of SSRIs found evidence of improvement in an adult's aggression, but only from studies with a high risk of bias (Williams 2013). To date, no Cochrane Review has focused on any of the remaining pharmacological interventions that can be used to address behaviours of concern in ASD. These previously conducted reviews of single medications or single classes of medications have provided useful information regarding their effectiveness and safety, however, these reviews now require updating. Furthermore, this review includes studies of children and adults with ASD, whereas previous reviews had focused only on either children or adults.
Since the publication of the protocol (Livingstone 2015), 17 systematic reviews have been published. Seven of these were on antipsychotics, three each on anticonvulsants and 'experimental' interventions, and an additional four systematic reviews on antiparkinsonians, anxiolytics, dementia‐related medications, and antidepressants respectively. Each of the systematic reviews reported on the effectiveness of only one class of drug.
The extent to which the age of the person receiving the treatment will affect the intervention's efficacy remains unclear. ASD is a lifelong condition, and therefore it is important to understand the effect of interventions, including medication, across the lifespan (Tantam 2012).
Objectives
To assess the effectiveness and AEs of pharmacological interventions for managing the behaviours of irritability, aggression, and self‐injury in ASD.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs), including cross‐over studies, that compare pharmacological interventions to an alternative drug, standard care, placebo, or wait‐list control.
Types of participants
Studies were considered eligible for inclusion if they included participants of any age with a clinical diagnosis of ASD, who displayed one or more behaviours of concern at baseline assessment, specifically irritability, aggression and self‐injury. People with reported comorbidities were included in the analysis. We will also include studies that identify a subset of people with ASD.
We included studies where participants were diagnosed according to the criteria of the Diagnostic and Statistical Manual for Mental Disorders (DSM) Fourth (DSM‐IV (DSM‐4 1994); or DSM‐IV‐TR (DSM‐4‐TR 2000)) and Fifth (DSM‐5; DSM‐5 2013) Editions, or the International Classification of Diseases, 10th Revision (ICD‐10; ICD‐10 2004); and those who had been diagnosed through use of a standardised diagnostic instrument, including the Autism Diagnostic Observation Schedule (ADOS; Lord 2000) or the Autism Diagnostic Interview Revised (ADI‐R; Lord 1994).
Types of interventions
Any pharmacological intervention used to manage behaviours of concern in children, adolescents or adults with ASD, specifically irritability, aggression, or self‐injury. Interventions may have been given at any dosage, for any duration, and any frequency of administration. Relevant pharmacological interventions included first‐generation ('typical') antipsychotics such as haloperidol, second‐generation ('atypical') antipsychotics such as risperidone and aripiprazole, ADHD‐related medications, anticonvulsants, antidementia medications, antidepressants (including selective SSRIs and tricyclic antidepressants), antiparkinsonian medication, anxiolytics, neurohormones, and a number of other drugs that did not fall into any of these classes that we grouped under an experimental category.
It was possible that additional eligible interventions that review authors were not previously aware of may be identified in the course of the review. When we identified any pharmacological interventions that were not initially included, we considered them as eligible and included them in the review after assessing their comparability with those named above.
Because pharmacological interventions could be used in addition to non‐pharmacological therapies, we included any studies in which participants received concurrent non‐pharmacological therapies, provided that they were used in all intervention arms.
The interventions of interest for this review focus on the effectiveness and benefits and harms associated with pharmacological agents to address the behaviours of irritability, aggression and self‐injury for people with ASD. Interventions with different foci such as sleep interventions were not included in this review.
Types of outcome measures
We classified outcome measures as either primary or secondary outcomes.
Lower scores indicate a more positive response for all outcomes and measures used apart from quality of life, where higher scores indicate an improved quality of life.
Where data were insufficient, we provided a narrative account of the outcomes.
Where feasible, we made comparisons at the following specific follow‐up periods:
short‐term follow‐up (less than 6 months);
medium‐term follow‐up (6 to 12 months); and
long‐term follow‐up (over 12 months).
Primary outcomes
Behaviours of concern
Behaviours of concern in ASD, specifically:
irritability (including outcomes of irritability improvement and irritability relapse as defined by the study authors);
aggression; and
self‐injury.
These outcomes needed to be measured by standardised instruments such as the 'irritability' subscale of the Aberrant Behaviour Checklist (ABC‐I; Aman 1985). Where possible, preference was given to analysing each of these three specific challenging behaviours separately. Where this was not possible, we combined measures across studies to create a composite 'challenging behaviour' outcome. In the event that study authors reported several similar scales, we established a hierarchy of preferred scales/instruments where the ABC‐I was the preferred scale. This hierarchy was established through discussion with the full review group.
Adverse effects
AEs (including sedation and weight gain)
Due to the wide range of AE data that we collected during this review, we made a postprotocol decision to categorise available data into the following groups:
cardiovascular;
gastrointestinal;
immune;
metabolic system;
musculoskeletal;
neurological;
psychological;
respiratory system;
skin;
urinary; and
other.
Secondary outcomes
Quality of life
Quality of life for both the child and the parents or informal carers or family (as measured by standardised instruments such as the Pediatric Quality of Life Inventory (PedsQL; Varni 1999), or through quality‐of‐life questionnaires).
Tolerability and acceptability
Tolerability and acceptability of the intervention (as measured by self‐reported or clinician‐reported adherence to treatment).
Summary of findings tables
We used the following outcomes to populate the summary of findings tables for the main comparison:
irritability;
aggression;
self‐injury;
AEs.
Search methods for identification of studies
We ran searches in 2020 using the search strategies in Appendix 2. We also ran updated searches in 2022, in which we made changes to the original MEDLINE search strategy by adding the MeSH term for neurodevelopmental disorders to the population section, and included more search terms for pharmacological interventions. We adapted the revised MEDLINE search for all databases (Appendix 1), and ran the searches from inception for each source before de‐duplicating these with the records retrieved by the previous search.
Electronic searches
We searched all available years of the following databases.
Cochrane Central Register of Controlled Trials (CENTRAL; 2022, Issue 5), in the Cochrane Library. Searched 6 June 2022
MEDLINE Ovid (1946 to 6 June 2022)
MEDLINE In‐Process and Other Non‐indexed Citations Ovid (6 June 2022)
MEDLINE Epub Ahead of Print Ovid (6 June 2022)
Embase Ovid (1974 to 6 June 2022)
CINAHL EBSCOhost (1937 to 6 June 2022)
APA PsycINFO Ovid (1967 to 6 June 2022)
ERIC EBSCOhost (1966 to 6 June 2022)
Epistemonikos (www.epistemonikos.org/en/). Searched 6 June 2022
Sociological Abstracts Proquest, 1952 to 6 June 2022
Science Citation Index (SCI) Web of Science Clarivate (1970 to 6 June 2022)
Conference Proceedings Citation Index – Science (CPCI‐S) Web of Science Clarivate (1990 to 6 June 2022)
Cochrane Database of Systematic Reviews (CDSR; 2020, Issue 11), in the Cochrane Library. Searched 6 June 2022
Database of Abstracts of Reviews of Effects (DARE), in the Centre for Reviews and Dissemination (CRD) databases. Searched 6 June 2022
LILACS (lilacs.bvsalud.org/en/). Searched 6 June 2022
AutismData (autism.org.uk/autismdata). Not available 6 June 2022
ClinicalTrials.gov (clinicaltrials.gov/). Searched 6 June 2022
World Health Organization (WHO) International Clinical Trials Registry Platform (isrctn.com/). Searched 6 June 2022
We used search filters for RCTs where appropriate. We did not apply any language or date restrictions. We did not restrict by publication status, and we sought translation of documents where necessary.
Searching other resources
We scanned bibliographies of included and excluded studies for possible additional references of interest.
We contacted relevant pharmaceutical companies, authors, and key scholars to identify any additional ongoing or missed studies.
Data collection and analysis
The protocol of this review planned to conduct a network meta‐analysis on the available data. After assessing the plausibility of the transitivity assumption, we decided that a network meta‐analysis would not be appropriate with the available data.
This was due to the variation across studies in participants, interventions and comparators, that did not allow scope for linking nodes to produce a network for a network meta‐analysis. It was felt that the heterogeneity would have led to issues with transitivity that would have rendered the network unstable.
Network meta‐analyses may still be performed in future updates if more appropriate data become available. In the following sections, we have only reported the methods that were used in this version of the review. For unused methods, please refer to the published protocol for this review (Livingstone 2015), and Appendix 3.
Selection of studies
Two of the four review authors (DG, MI, MJ, NL) independently selected and assessed every study at abstract and title level and then full‐text level to determine whether they met the inclusion criteria for this review. We resolved any disagreements between the authors through discussion with the full review group. The selection process is presented in two PRISMA diagrams (Figure 1; Figure 2; Moher 2009).
1.

Original search November 2020
2.

Search update June 2022
Data extraction and management
Two review authors (DG, MI, MJ, NL) extracted data independently and entered them into a piloted data extraction form. We resolved any disagreements between the review authors through discussion with the full review group. We extracted the following data.
Outcome data
From each included study, we extracted relevant details on all primary and secondary outcome measures used, as defined by the review authors; and length of follow‐up and summary data, including means, standard deviations, confidence intervals and significance levels for continuous data, and proportions for dichotomous data. We extracted arm‐level data.
Data on potential effect modifiers
From each included study, we extracted data on the following study, participant, intervention, and comparison characteristics that may have acted as effect modifiers.
Study characteristics (study design, study duration, details of attrition, and risk of bias concerns)
Participant characteristics (number randomised, age of participants, specific diagnosis, comorbidities, gender distribution, geographical location of study)
Intervention characteristics (type of antidepressant or antipsychotic, dose, duration, frequency, age medication began, concurrent interventions)
Comparison characteristics (form, frequency, and duration of 'standard care')
Other data
From each included study, we extracted data on the following additional information.
Study author(s), year of publication, citation, and contact details
Sources of funding and other potential commercial interests
Assessment of risk of bias in included studies
Two of the four review authors (DG, MI, MJ, NL) independently assessed the seven risk of bias domains for each study and assigned each domain to one of the following categories as outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011):
high risk of bias;
low risk of bias; or
unclear or unknown risk of bias.
When determining quality of evidence, the overall risk of bias of each trial was assessed independently by two of the review authors and then agreed by consensus or referral to a third review author. Assessments of risk of bias for each study were based on the following criteria as outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Sequence generation (was the allocation sequence adequately generated?)
Allocation concealment (was allocation adequately concealed?)
Blinding of participants and personnel (was knowledge of the allocated intervention adequately prevented during the study?)
Blinding of outcome assessors (was knowledge of the allocated intervention adequately prevented during the study?)
Incomplete outcome data (were incomplete outcome data adequately addressed?)
Selective outcome reporting (are reports of the study free of suggestion of selective outcome reporting?)
Other sources of bias (was the study apparently free of other problems that could put it at a high risk of bias?)
We resolved any disagreements between the review authors through discussion with the full review group. We reached overall risk of bias judgements by considering the results from each relevant risk of bias domain for the outcome being considered.
Measures of treatment effect
Continuous data
We calculated standardised mean differences (SMDs) with 95% confidence intervals (CIs) for continuous outcome data (e.g. scores on standardised measures). We used Cohen's standards for interpreting effect sizes (small = 0.2, medium = 0.5, large = 0.8 (Cohen 1988)).
Dichotomous data
We estimated the pairwise relative treatment effects of the competing interventions by calculating effect sizes as odds ratios (ORs) with 95% CIs for dichotomous outcome data (e.g. adherence).
Unit of analysis issues
Cross‐over trials
We included cross‐over trials, in which all participants receive both the control and intervention treatment but in a random order. We had aimed only to use data reported during the first phase of the study, up to the point of the first cross‐over, to avoid any carry‐over effect from the first to second phase. However, the majority of studies did not differentiate data from first and second phases. Therefore, where first phase data were not reported in cross‐over studies, we included reported data from the study but undertook a sensitivity analysis to identify whether inclusion of these data had a differential effect on meta‐analytic estimates.
Multiple treatment groups
If two or more eligible intervention groups were compared to a single eligible control group, we split the sample size for the shared comparator group to prevent the same comparator participants being included twice. We clearly documented decisions made during this process in the review.
Dealing with missing data
We contacted the original investigators to request missing data. If we could not obtain the data, we made assumptions about whether the data appeared to be 'missing at random' or 'not missing at random' and followed the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2022a).
Data that are not missing at random are likely to be missing for reasons related to the outcomes of the missing data. For example, if a participant agrees to take part in a trial but is unhappy with the outcome of allocation, fails to adhere to the medication or experiences AEs as a result of the medication, then they may be unwilling to complete any follow‐up assessments. In such a situation, where dichotomous data are missing, we imputed data on the assumption that the participants experienced the less favourable outcome (e.g. 'participant did not adhere to the treatment').
When studies provided insufficient information regarding the exact number missing from each group, data imputation was not possible, in which case we analysed only the available data. Where continuous data were missing, we analysed only the available data.
Where studies had missing summary data, such as missing standard deviations, we derived these where possible using calculations provided in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2022a).
We specified the methods used to address any missing data in the Characteristics of included studies tables. If imputation was not possible, we outlined the reasons for this in the text.
Assessment of heterogeneity
We examined clinical heterogeneity within each pairwise comparison by inspecting each included study for variability in the participants, interventions or outcomes described. We examined methodological heterogeneity within each pairwise comparison by inspecting each included study for variability in the study design and risk of bias. We discussed in full any unexpected variability that arose. In pairwise analyses, we assessed statistically the presence of heterogeneity within each pairwise comparison using the Chi² statistic and its P value (Deeks 2022), and the I² statistic (Higgins 2003), and its 95% CI.
Assessment of reporting biases
We assessed publication bias and other reporting biases by visually inspecting the funnel plots of analyses with more than 10 trials and performing trim and fill analyses.
Data synthesis
We performed standard pairwise meta‐analyses on the results when data from at least two included studies were available for any treatment comparison. Due to expected heterogeneity amongst the included studies, we performed a random‐effects meta‐analysis using an inverse variance weighting method (Chi2 P value 0.05 or less) using Review Manager (RevMan) Web software (RevMan Web 2021). We used an inverse‐variance approach to meta‐analysis in order to increase the certainty of the pooled effect estimate, as larger studies with smaller standard errors are weighted more heavily than smaller studies with larger standard errors (Deeks 2022). When pooling the data was inappropriate, we provided a narrative description of the individual study results.
Subgroup analysis and investigation of heterogeneity
We conducted the following subgroup analyses for comparisons with a sufficient number of studies that provided specific details:
the differential effects of interventions by the age at which the drug was first administered; for example, infant/toddler (birth to six years of age) versus school age (6 to 12 years of age) versus adolescent (12 to 18 years of age), versus adult (18 years of age and over);
the differential effects of interventions by communication ability; for example, low communication ability versus high communication ability;
the differential effects of interventions by cognitive ability; for example, low cognitive ability versus high cognitive ability;
the differential effects of interventions by the gender of the participant; for example, male versus female.
Because most studies did not specify the ages of children, the subgroup analyses we conducted were children (up to 17 years of age) compared to children and adults, and adult‐only samples.
We also undertook subgroup analyses that were not planned in the protocol. This was because we wanted to identify whether there were differences within subclasses of each pharmacological class that had differing mechanisms of action, that is, each of the atypical antipsychotics that have differing mechanisms of action, stimulant versus non‐stimulant ADHD‐related medications, SSRI versus dibenzoxazepine antidepressants, different neurohormones, and between each of the different experimental drugs.
Sensitivity analysis
In the protocol (Livingstone 2015), we stated our aim to perform sensitivity analyses to assess whether the findings of this review were robust to the following:
reanalysis excluding studies according to study quality issues, including those with low sample size, high risk of bias, or high attrition;
reanalysis without imputing data for the missing participants;
reanalysis using a fixed‐effect model.
In addition, as the majority of cross‐over studies did not differentiate data from first and second phases, we aimed to undertake sensitivity analyses to identify whether inclusion of these data had a differential effect on meta‐analytic estimates.
We used the primary outcome irritability for the comparisons where there were significant differences between intervention and placebo groups.
We were only able to undertake sensitivity analyses on the comparisons of antipsychotics versus placebo, and neurohormone versus placebo as there were inadequate data for other comparisons. We were unable to do sensitivity analyses for cross‐over studies in atypical antipsychotics as there were no cross‐over studies included in those comparisons. Also, we did not use imputed data, therefore we undertook sensitivity analysis excluding studies at:
high risk of attrition bias;
high risk of other bias; and
with a sample size less than 50.
Summary of findings and assessment of the certainty of the evidence
We created summary of findings tables using the system developed by the GRADE Working Group (Schünemann 2013).
We used GRADEpro GDT to import data from RevMan Web to create summary of findings tables for the main comparisons and outcomes indicated under 'Types of outcome measures' (RevMan Web 2021).
Three review authors (NL, MI, DG) independently assessed the certainty of the evidence using GRADE. We resolved any disagreements through discussion.
For information regarding the GRADE approach, and factors that influence the assessment, see chapter 14 of the Cochrane Handbook for Systematic Reviews of Interventions (Schünemann 2022).
The main comparisons in this review as judged by clinical experts and for which we created summary of findings tables were as follows.
Atypical antipsychotics versus placebo
Neurohormones versus placebo
ADHD‐related drugs versus placebo
Antidepressants versus placebo
We used the following outcomes to populate the summary of findings tables for the main comparisons.
Irritability (short‐term)
Aggression (short‐term)
Self‐injury (short‐term)
AEs (metabolic, musculoskeletal, neurological, and psychological; short‐term)
During the course of this review, many different types of AEs were found to be reported by the included studies. To make the summary of findings tables more readable and useful, the clinical content experts on the review team were asked to prioritise the list of available AEs, to decide which should be presented in the summary of findings tables. The clinical experts were blinded to the type or availability of evidence available for each type of AE when they made this decision, to ensure their choice was based on clinical importance and not data availability. As a result of this prioritisation exercise, the decision was made to present a narrative summary of the most important AEs in the four most clinically important categories of AEs ‐ metabolic, musculoskeletal, neurological, and psychological.
Results
Description of studies
For more information please see Characteristics of included studies, Characteristics of excluded studies, Characteristics of studies awaiting classification; and Characteristics of ongoing studies.
Results of the search
An electronic search conducted in November 2020 yielded 7403 possible references. This was reduced to 5002 possible references once duplicates were removed. These 5002 references were screened at the title and abstract level; 4600 were irrelevant, and we excluded them for reasons such as they were not RCTs, they used an ineligible study design, were reviews, involved an irrelevant population or were non‐pharmacological interventions. This left 402 full‐text articles (376 studies) to screen, after which we excluded 76 references (as 72 studies), leaving 326 references: 281 references (121 studies) included in the analysis; 26 references (22 studies) awaiting classification; and 19 references (16 studies) for ongoing studies (Figure 1).
A top‐up electronic search was conducted in June 2022, which yielded 1809 possible references. This was reduced to 1294 possible references once duplicates were removed. After initial screening, this was reduced to 48 full‐text records that needed screening, after which we excluded 12 references (9 studies), leaving 36 references (as 23 studies). These were 10 included studies, five studies 'awaiting classification', eight 'ongoing studies' and 13 secondary references of these studies. See Figure 2 for a flow diagram of the search process.
We also contacted a number of study authors to request further information. See Table 6 for information about the studies and contact person.
2. Authors contacted.
| Study ID | Name of contact author | Response from author |
| Asadabadi 2013 | S. Akhonzadeh | No response |
| Belsito 2001 | K. Belsito | No response |
| Chugani 2016 | D. Chugani | No response |
| Ghaleiha 2013a | S. Akhonzadeh | No response |
| Ghaleiha 2015 | S. Akhonzadeh | No response |
| Ghaleiha 2016 | S. Akhonzadeh | No response |
| Handen 2000 | B. Handen | No response |
| Handen 2005 | B. Handen | No response |
| Handen 2008 | B. Handen | No response |
| Handen 2011 | B. Handen | No response |
| Mohammadi 2013 | S. Akhonzadeh | No response |
| Nikoo 2015 | S. Akhonzadeh | No response |
| Hollander 2012 | E. AnagNostou | No response |
| E. Hollander | No response | |
| Kern 2001a | J. Kern | No response |
| Kern 2002 | J. Kern | No response |
| King 2001 | B. King | No response |
| Mace 2001 | N. Blum | No response |
| McDougle 1996 | C. McDougle | Email bounced |
| Miral 2008 | S. Miral | No response |
| Molloy 2002 | C. Molloy | No response |
| Mouti 2014 | M. O'Sullivan | No response |
| A. Mouti | Received response but referred to another author | |
| D. Reddinhough | Was provided with a full‐text paper containing the additional data | |
| Munesue 2016 | T. Munesue | No response |
| Novotny 2004 | E. Hollander | No response |
| Remington 2001 | G. Remington | No response |
| Rezaei 2010 | S. Akhonzadeh | No response |
| Sandler 1999 | AD. Sandler | No response |
| Wasserman 2006 | S. Wasserman | No response |
| Wasserman 2006 | E. AnagNostou | No response |
Included studies
We have included 131 studies (291 reports and 149 datasets) involving 7014 participants in this review. We identified 25 studies as awaiting classification (see Studies awaiting classification) and 25 ongoing studies (see Ongoing studies). All included studies compared a pharmacological intervention to a placebo or to another pharmacological intervention.
The number of participants in each study ranged from 8 to 321 and most studies involved children, although some studies involved children and adults and some only adults; 53 studies involved only children under 13 years, 37 studies involved children and adolescents, two involved adolescents only, 16 involved children and adults, and 23 involved only adults.
Antipsychotics by comparison
Atypical or typical antipsychotics versus placebo or alternative medication class
Twenty‐four studies (59 reports, 1225 participants, 29 datasets) compared an atypical or typical antipsychotic to a placebo or other treatment (see Table 7 for further information). The number of participants ranged from nine (Dollfus 1992), to 128 (Loebel 2016), with an average age of 10.4 years. Apart from three studies that included a total of 44 adults (Mace 2001; McDougle 1998; Remington 2001), all participants were children (< 18 years). All the studies were short‐term (less than 6 months) and ranged from 34 days (Mace 2001), to 16 weeks (Findling 2014), although the average duration was between eight and 10 weeks. All trials were parallel RCTs apart from Dollfus 1992 and Remington 2001, which were cross‐over studies.
3. Summary of all antipsychotic comparisons.
| Antipsychotics | Placebo | Bromocriptine | Haloperidol | Memantine | Risperidone |
| Amisulpride | Dollfus 1992 (n = 9) | ||||
| Aripiprazole |
Findling
2014 (n = 85) Ichikawa 2017 (n = 92) Marcus 2009 (n = 105) NCT00198107 (n = 81) NCT00468130 (n=15) Owen 2009 (n = 98) 6 studies (n = 476) |
DeVane
2019 (n = 61) Ghanizadeh 2014 (n = 59) |
|||
| Haloperidol |
Mace
2001 (n = 7) Remington 2001 (n = 36) |
||||
| Lurasidone | Loebel 2016 (n = 148) | ||||
| Olanzapine | Hollander 2006b (n = 11) | Malone 2001 (n = 30) | |||
| Risperidone |
Kent
2013 (n = 66) Luby 2006 (n = 23) McCracken 2002 (n = 101) McDougle 1998 (n = 31) Research Units 2005 (n = 32) NCT01624675 (n = 39) Shea 2004 (n = 79) Troost 2005 (n = 24) 8 studies (n = 395) |
Miral 2008 (n = 30) | Nikvarz 2017 (n = 30) |
n: number of participants
Interventions: 16 studies compared an atypical antipsychotic to a placebo, two studies compared one atypical antipsychotic to another atypical antipsychotic, two studies compared a typical antipsychotic to a placebo, and two studies compared an atypical antipsychotic to a typical antipsychotic. A further two studies compared an atypical antipsychotic to an anti‐dementia drug and an atypical antipsychotic to an antiparkinsonian drug, respectively. Further information can be found in Table 7.
Setting: most (17) of the studies were conducted in the USA apart from Ghanizadeh 2014; and Nikvarz 2017, which were conducted in Iran, Ichikawa 2017 and NCT01624675 in Japan, Miral 2008 in Turkey, Remington 2001 in Canada, and Dollfus 1992 in France.
Inclusion criteria: all studies required a clinical diagnosis of ASD and some studies (DeVane 2019; Ichikawa 2017; Marcus 2009; McCracken 2002), also required co‐occurring behaviours of concern such as aggression, agitation, irritability, or self‐injury to be assessed at baseline.
Exclusion criteria: all studies excluded people with other DSM diagnoses or neurological disorders including schizophrenia, pervasive developmental disorder not otherwise specified (PDD‐NOS), Rett syndrome, psychosis, unstable seizure disorders, or other significant cardiac, renal or endocrine disorders. Some studies also excluded people who had previously been treated with the intervention or interventions of interest.
Participant intellectual ability: the intellectual ability of participants varied between trials, with some trials not providing specific details (DeVane 2019; Kent 2013). Most studies required participants to have a mental age of at least 18 months. Some studies included up to 83% of participants with an intellectual disability of varying severity (Ichikawa 2017; Malone 2001; McCracken 2002; Shea 2004).
Concomitant medications: most studies required participants to cease taking all psychotropic medications before commencing in the trial except for Findling 2014, which allowed the use of sleep medications, Troost 2005, which allowed stimulant use for co‐occurring ADHD, and Research Units 2005 and Hollander 2006b, both of which allowed anticonvulsants for participants with stable epilepsy.
Interventions
Amisulpride: one study compared amisulpride to an antiparkinsonian (bromocriptine; Dollfus 1992). Further details are provided below.
Aripiprazole: eight studies compared aripiprazole to a placebo or another atypical antipsychotic. Most studies administered the doses once daily in either a fixed or flexibly‐dosed manner to a maximum of 15 mg/day. The mean daily dose of aripiprazole was between 0.172 mg/day and 0.354 mg/kg/day.
Lurasidone: one study compared lurasidone to a placebo (Loebel 2016). Participants received either 20 mg or 60 mg once daily.
Olanzapine: two studies compared olanzapine to a placebo (Hollander 2006b), or a typical antipsychotic (Malone 2001). Participants who weighed less than 40 kg received a maximum of 2.5 mg of olanzapine once daily, and children 40 kg or heavier received a maximum of 5 mg of olanzapine once daily (Hollander 2006b). Malone 2001 administered olanzapine at 2.5 mg every second day for children who weighed 40 kg or less, and 2.5 mg once daily for children 41 kg and above with a maximum daily dose of 5 mg.
Risperidone: a total of 10 studies compared risperidone to a placebo or other treatment. Nine studies compared risperidone to a placebo, one study (Nikvarz 2017), compared risperidone to an antidementia medication, and one study compared risperidone to haloperidol (Miral 2008). Apart from the two discontinuation studies that required the intervention to be administered twice daily, doses were administered once daily. Mean daily dosage of risperidone for children who weighed less than 40 kg was 1.58 mg/day, 2.27 mg/day for children 40 kg or heavier, and 3.25 mg/day for adults.
Haloperidol: two studies (Mace 2001; Remington 2001), compared haloperidol (a typical antipsychotic) to a placebo. Both studies administered haloperidol two to three times daily, however, Remington 2001 used fixed doses (mean daily dose of 1.3 mg) while Mace 2001 initiated haloperidol at 0.25 mg/day for children who weighed 40 kg or less, and 0.5 mg/day for children who weighed 40 kg or more up to a maximum of 5 mg/day (mean daily dose 1.4 mg).
Comparator
Placebo: the majority of antipsychotic studies compared to a placebo, however, apart from NCT00468130, which used sugar pills, the study authors did not provide details regarding the ingredients of the placebo.
Haloperidol: two studies (Malone 2001; Miral 2008), compared an atypical antipsychotic (olanzapine and risperidone respectively) to haloperidol. Mean dose of haloperidol was 1.4 mg/day to 2.6 mg/day. Haloperidol was given up to twice daily.
Bromocriptine: one study (Dollfus 1992), compared amisulpride to bromocriptine. Bromocriptine was administered at 0.15 mg/kg/day to 0.20 mg/kg/day for all participants.
Primary outcomes
Irritability: 16 of the studies reported irritability; the majority used the ABC‐I subscale (Aman 1985). The exceptions were McDougle 1998 and Miral 2008, which both used the Ritvo Freeman Real Life Rating Scale (RFRLRS; Freeman 1986), to report irritability.
Improvement and relapse: amongst those taking risperidone (Kent 2013; McCracken 2002), or aripiprazole (Marcus 2009; Owen 2009), improvement was defined as a minimum of 25% improvement in ABC‐I (Kent 2013), in addition to a rating of much improved or very much improved on the Clinician Global Impression‐Irritability (CGI‐I) scale (Marcus 2009; McCracken 2002; Owen 2009). The two discontinuation studies (Research Units 2005; Troost 2005), reported relapse, defined as a minimum increase of 25% in ABC‐I scores during the discontinuation phase.
Aggression: one study (Shea 2004), reported aggression using the Nisonger Child Behavior Rating Form (conduct problem subscale; Aman 1996).
Self‐injury: three studies reported self‐injurious behaviour. One study (McDougle 1998), used the Self‐Injurious Behaviour Questionnaire (SIB‐Q; Gualtieri 2002), to measure self‐injurious behaviour, Shea 2004 used the Nisonger Child Behaviour Rating Form (Self‐injurious/ stereotypic subscale; Aman 1996), and Mace 2001 used their own scale to rate self‐injurious behaviour (self‐injurious behaviour per hour).
AEs: apart from three studies (Mace 2001; Research Units 2005; Troost 2005), all studies reported AEs. AEs were analysed and reported based on major categories including cardiovascular, metabolic, gastrointestinal, immune system, neurological, psychological, respiratory, skin, and urinary AEs. We could not include data from three studies in the analysis (Malone 2001; Marcus 2009; Owen 2009). Further details can be found in Effects of interventions.
Secondary outcomes
Quality of life: three trials comparing aripiprazole to a placebo reported quality‐of‐life outcomes (Findling 2014; Marcus 2009; Owen 2009). Each study used the Pediatric Quality of Life Inventory (PedsQL; Varni 2001).
Tolerability and acceptability (loss to follow‐up): 231 participants withdrew from studies involving an atypical antipsychotic versus a placebo and were not included in the relevant study analyses. Reasons for withdrawing included lack of efficacy (75), AEs (44), withdrew consent (32), other/not specified (18), lost to follow‐up (14), noncompliance (6), increased behaviours of concern or exacerbation of medical condition (5), missed visits (4), and physician decision (3).
Neurohormones versus placebo or other treatment
Twenty‐four studies (46 reports, 1640 participants, 27 datasets) compared a neurohormone to a placebo. Seven studies involved adult participants only (Anagnostou 2012; Bernaerts 2020; Jacob 2022; NCT01337687; NCT02940574; Squassante 2018; Yamasue 2020), one study involved adolescents and adults (15 to 45 years; Munesue 2016), one study involved children three to eight years of age (Le 2022), one study involved adolescents (12 to 18 years; Guastella 2015a), and fourteen studies involved only children (< 18 years). Fifteen studies were parallel trials and nine were cross‐over studies. Study duration ranged from four weeks to 24 weeks (Hollander 2020b; Jacob 2022; Sikich 2021). All but nine studies were conducted in the USA. The other studies were conducted in Australia, Belgium, China, two in Canada, the Netherlands, and three in Japan (Guastella 2015a; Bernaerts 2020; Le 2022; NCT01908205; NCT02940574; Buitelaar 1990; Munesue 2016; Takamitsu 2015a; Yamasue 2020) respectively.
-
Interventions
Adrenocorticotrophic hormone: one study involving 14 participants compared adrenocorticotrophic hormone to a placebo (Buitelaar 1990). Doses of either adrenocorticotrophic hormone or placebo were fixed (20 mg/day).
Balovaptan (RG7314): three studies involving 657 adult participants compared balovaptan to a placebo (Hollander 2020b; Jacob 2022; Squassante 2018). Doses were either 1.5 mg, 4 mg or 10 mg once daily of balovaptan in capsule form.
Oxytocin: 13 studies involving 709 participants compared oxytocin to a placebo. All but four studies required participants to take 12 IU of oxytocin twice daily (total of 24 IU daily). Munesue 2016 had a maximum of 8 IU of oxytocin twice daily, Guastella 2015a and Sikich 2013 had varying levels of oxytocin based on age (Guastella 2015a 18 IU twice daily for children < 16 years, and 24 IU twice daily for participants 16 to 18 years; Sikich 2013 administered up to 24 IU for children 3 to 10 years and a maximum of 32 IU for children 11 to 17 years), NCT01908205 involved 0.4 IU/kg taken twice daily up to a maximum of 24 IU per dose.
Secretin: five studies involving 211 participants compared secretin to a placebo. All studies were either single‐dose (Carey 2002; Levy 2003; Owley 2001; Unis 2002), or two doses separated by two months (Handen 2005). All studies used 2 IU/kg per infusion.
Vasopressin: two studies (Parker 2019; Umbricht 2017), involving 67 participants compared vasopressin to a placebo. Parker 2019 was a four‐week parallel study with vasopressin doses ranging from 4 IU to a maximum of 12 IU twice daily for children up to 12.9 years of age, and maximum of 16 IU twice daily for children over 12.9 years of age. Umbricht 2017 was a 20‐mg single‐dose cross‐over study involving male adults.
Comparators: all studies compared a neurohormone to a placebo. Apart from four studies that used saline solution (Anagnostou 2012; Carey 2002; NCT01337687; Owley 2001), the ingredients of placebo were not outlined.
Inclusion criteria: all studies required a clinical diagnosis of ASD, Asperger's, or PDD‐NOS to participate in the trial. Six studies also required a CGI severity score (Schopler 2009), above 4, four studies restricted participation to male participants only (Bernaerts 2020; Squassante 2018; Takamitsu 2015a; Yamasue 2020), four studies required participants to have an IQ above 70 (Munesue 2016; Sikich 2013; Squassante 2018; Yamasue 2020), and some required participants to either be on stable concomitant medication (Anagnostou 2012; Munesue 2016; Owley 2001; Sikich 2013), or not to have trialled the intervention previously (Carey 2002).
Exclusion criteria: most studies excluded people with a clinical diagnosis of psychosis, other mental disorders, or significant neurological or other medical conditions. Additional exclusion criteria included previous use of the intervention (Parker 2017; Parker 2019; Unis 2002), or use of psychotropic or other prohibited medications in the period before and during the trial.
Setting: apart from one study conducted in Australia (Guastella 2015a), two in Belgium (Bernaerts 2020; NCT02940574), one in Canada (NCT01908205), one in China (Le 2022), one in the Netherlands (Buitelaar 1990), and three in Japan (Munesue 2016; Takamitsu 2015a; Yamasue 2020), all studies were conducted in the USA. Studies were conducted at either outpatient clinics, hospitals or clinics and research centres associated with universities.
Concomitant medications: six studies provided details of concomitant medications. Bernaerts 2020 reported that 27% and 11% of those in the intervention and placebo groups respectively were taking psychostimulants concomitantly, as well as other medications including antidepressants, risperidone and aripiprazole. Guastella 2015a reported that approximately 35% of participants in both groups were taking other psychotropic medications. Levy 2003 reported that 10 participants out of 62 were taking one concurrent medication, including guanfacine, methylphenidate, fluoxetine (Prozac), and risperidone, and one participant was taking both guanfacine and Prozac concurrently. Squassante 2018 reported that antipsychotics were being taken concurrently by 15% to 28% of participants and concurrent stimulant use by 13% to 26% of participants. Parker 2017 reported concomitant medication use of up to 17% and included SSRIs, benzodiazepines, stimulants, anticonvulsants, and guanfacine, and Yamasue 2020 reported antidepressants, antipsychotics, anticonvulsants or hypnotics were being taken concurrently by 12 participants.
Participant cognitive status: reported IQ varied greatly between studies and ranged from 35 to 120.
Length of follow‐up: study duration ranged from four weeks to 12 weeks (Squassante 2018), although Guastella 2015a reported three‐month follow‐up data for primary and secondary outcomes.
Primary outcomes
Irritability: 10 of the studies reported irritability. All but one study used the ABC‐I scale (Aman 1985), whereas Levy 2003 used the Ritvo‐Freeman Real Life Rating Scale (affectual responses subscale; Freeman 1986) to measure irritability. Umbricht 2017 reported baseline ABC‐I (Aman 1985) but did not report endpoint data.
Self‐injury: Guastella 2015a reported self‐injurious behaviour using the Repetitive Behaviour Scale ‐ Revised (self‐injurious subscale) (Bodfish 2000).
AEs: 14 studies reported AEs, although Levy 2003 did not report AEs for both groups and therefore, the AE data from Levy 2003 could not be included.
Secondary outcomes
Quality of life: five studies (Anagnostou 2012; Bernaerts 2020; NCT01908205; Parker 2019; Takamitsu 2015a), reported quality of life. Anagnostou 2012, Bernaerts 2020 and Takamitsu 2015a used the WHO Quality of Life scale (WHOQoL; WHO 1998) and NCT01908205 and Parker 2019 used the Pediatric Quality of Life (PedQL) inventory (parent‐rated; Varni 2001).
Tolerability and acceptability (loss to follow‐up): 67 participants (7.6%) withdrew and were not included in the relevant study analyses. Reasons included withdrawing consent (26), loss to follow‐up (12), AEs (12), other (5), poor/non‐compliance (3), protocol violation (3), worsening of behaviours of concern (2), physician decision (1), and an administrative error (1).
ADHD‐related medications versus placebo or other treatment
Thirteen studies (28 reports, 482 participants, 18 datasets) compared an ADHD‐related medication to a placebo or other intervention. All studies included children (< 18 years) with study duration ranging from two weeks (Quintana 1995), to 11 weeks (NCT03242772); the mean was 5.5 weeks. Seven of the studies were cross‐overs and six were parallel (Eslamzadeh 2018; Handen 2015; Harfterkamp 2014;NCT03242772; NCT00498173; Scahill 2015).
-
Interventions
Amphetamine: one study involving 18 participants compared amphetamine to a placebo (NCT03242772). Amphetamine was initiated at 3.1 mg once daily for 11 weeks and titrated upwards if tolerated.
Atomoxetine: five studies involving 274 participants compared atomoxetine to a placebo (Arnold 2006; Eslamzadeh 2018; Handen 2015; Harfterkamp 2014; NCT00498173). Atomoxetine commenced at 0.3 mg/kg/day to 0.5 mg/kg/day up to a maximum of 1.8 mg/kg/day. Mean final doses were 1.2 mg/kg/day administered once daily (Harfterkamp 2014), 1.2 mg/kg/day twice daily (Eslamzadeh 2018), and 1.38 mg/kg/day administered twice daily (Handen 2015).
Clonidine: two studies (17 participants) compared clonidine to a placebo. Fankhauser 1992 administered clonidine via a weekly transdermal patch (approx 0.005 mg/kg/day) and Jaselskis 1992 administered 0.15 mg/kg/day to 0.20 mg/kg/day across three doses per day.
Guanfacine: two studies (73 participants) compared guanfacine to a placebo. The maximum daily dose of guanfacine was 3.0 mg/day across three daily doses (mean daily dose 2.68 mg/day; Handen 2008) or a maximum of 3 mg/day for children less than 25 kg and maximum 4 mg/day for children 25 kg or more (Scahill 2015).
Methylphenidate: three studies (7 datasets, 100 participants) compared methylphenidate to a placebo. Methylphenidate was administered two to three times daily using fixed doses. All studies were cross‐over studies: Posey 2005 administered three different doses (3 datasets) based on bodyweight (0.125 mg/kg/day, 0.250 mg/kg/day, 0.500 mg/kg/day); Quintana 1995 administered a mean methylphenidate dose of 0.397 mg/kg/day; and Pearson 2013 had mean doses of 0.21 mg/kg, 0.35 mg/kg and 0.48 mg/kg for low, medium and high doses respectively.
Comparators: all studies compared an ADHD‐related medication to a placebo. Only one study (Handen 2015), provided details of the placebo (sugar pill).
Inclusion criteria: all studies required participants to meet the DSM criteria for ASD, Asperger's or PDD‐NOS. Other criteria included a minimum mental age of 24 months, and symptoms of hyperactivity or impulsiveness for at least six months.
Exclusion criteria: prior exposure to ADHD‐related medication in the past two years, adverse reaction to the intervention, concurrent psychotropic medication use, other significant neurological, psychiatric, or medical conditions that may require medical management
Setting: apart from two trials that were conducted in Iran and the Netherlands respectively (Eslamzadeh 2018; Harfterkamp 2014), all studies were conducted in the USA, with participants recruited from either outpatient clinics or clinics and research centres associated with universities.
Concomitant medications: all studies required participants to be free of all psychotropic medications for up to one month prior to starting the study apart from Pearson 2013, which allowed stable (> 3 months) medications to be continued during the trial.
Participant cognitive status: the reported IQ ranged from severe intellectual disability to over 90.
Length of follow‐up: study duration was between one week (Pearson 2013), and 10 weeks (Handen 2015).
Primary outcomes
Irritability ‐ all studies apart from Eslamzadeh 2018 and NCT03242772 reported irritability. All studies apart from one used the ABC‐I (Aman 1985), however, Posey 2005 did not report endpoint ABC‐I scores. Fankhauser 1992 used the Ritvo‐Freeman Real Life Rating Scale (Freeman 1986).
Self‐injury ‐ only one study (Arnold 2006), reported self‐injurious behaviour using the Repetitive Behaviour Scale ‐ Revised (self‐injury subscale; Bodfish 2000).
AEs ‐ nine of the studies reported AEs.
Secondary outcomes
Tolerability and acceptability (loss to follow‐up)
Antidepressants versus placebo or other treatment
Ten studies (22 reports, 662 participants, 10 datasets) compared an antidepressant to a placebo or another intervention. An additional study (Remington 2001) compared clomipramine to a placebo, however, those numbers have already been included in a previous comparison. Three studies involved children only (< 12 years), four studies included children and adolescents (< 18 years), two studies included children, adolescent and adult participants (Gordon 1993; Remington 2001), and two studies included only adult participants (Hollander 2012; McDougle 1996). Seven studies were parallel and four were cross‐over studies (Gordon 1993; Hollander 2005; Niederhofer 2003; Remington 2001). Study duration ranged from five weeks (Gordon 1993) to 12 months (NCT00183339).
-
Interventions
Citalopram: one study involving 149 participants compared citalopram to a placebo (King 2009). Maximum citalopram was 20 mg/day (mean maximum dose was 16.5 mg/day (+/‐6.5 mg)).
Clomipramine: two studies compared clomipramine to a placebo. Remington 2001 (48 participants) commenced clomipramine at 25 mg once daily and increased incrementally up to 50 mg twice daily. Gordon 1993 (12 participants) commenced clomipramine at 25 mg/day up to a maximum of 5 mg/kg/day or maximum of 250 mg/day. The participants involved with Remington 2001 had previously been counted, so only the 12 participants from Gordon 1993 are included in the official count.
Fluoxetine: five studies involving 401 participants compared fluoxetine to a placebo (Herscu 2020; Hollander 2005; Hollander 2012; Mouti 2014; NCT00183339). Four of the studies involved only children (Herscu 2020; Hollander 2005; Mouti 2014; NCT00183339). They initiated fluoxetine at 2.0 mg/day to 8.0 mg/day depending on weight up to a maximum of 0.8 mg/kg/day (mean final dose 9.9 mg/day; Hollander 2005), a maximum of 20 mg/day and 30 mg/day for children under 40 kg and 40 kg and above (Mouti 2014; NCT00183339), or a maximum of 18 mg/day (mean final dose 11.8 mg ± 6.5; Herscu 2020). Hollander 2012, which involved adults, followed fixed doses of fluoxetine starting with 10 mg/day up to a maximum of 80 mg/day (mean final dose 64.76 mg/day). Most studies required participants to take fluoxetine once daily.
Fluvoxamine: one study involving 30 participants compared fluvoxamine to a placebo (McDougle 1996). Fluvoxamine was initiated at 50 mg once daily, increasing to a maximum of 300 mg/day if tolerated.
Sertraline: one study involving 58 participants compared sertraline to a placebo (Hagerman 2018). Sertraline was administered using fixed doses of 2.5 mg/day for children under four years of age, and 5.0 mg/day for children four years and over.
Tianeptine: one study involving 12 participants compared tianeptine to a placebo (Niederhofer 2003). Fixed doses of 37.5 mg/day were administered.
Comparators: all studies compared an antidepressant to a placebo. Details of placebo ingredients were not provided except for McDougle 1996, which described placebo as "lactose in identical‐looking tablets".
Inclusion criteria: all studies required participants to meet the DSM criteria for ASD, Asperger's or PDD‐NOS. Other criteria included being free of psychotropic medications for up to six weeks prior to the study (Hollander 2012; Niederhofer 2003; Remington 2001), and free of significant medical conditions (Niederhofer 2003).
Exclusion criteria: three studies excluded people with other DSM diagnoses or significant medical conditions including schizophrenia, hypersensitivity to or previous use of the intervention (Herscu 2020; Hollander 2005; Hollander 2012), three studies excluded people for concurrent use of psychotropic medications (Herscu 2020; Mouti 2014; Remington 2001), and two studies excluded people for positive serum pregnancy test results (McDougle 1996; Mouti 2014).
Setting: all studies were conducted in the USA apart from Mouti 2014 and Niederhofer 2003, which were conducted in Australia and Italy respectively. Participants were recruited from academic medical centres, tertiary hospitals, or research centres associated with universities.
Concomitant medications: three studies reported that some participants were taking medications such as anticonvulsants and stimulants concurrently (Hagerman 2018; Mouti 2014; Remington 2001), however, most studies did not permit concurrent medication use apart from sleep or antiparkinsonian medications (King 2009; Remington 2001).
Participant cognitive status: three of the studies reported that participants had an IQ of over 70, two studies reported that either all or some participants had an IQ of under 70 (Niederhofer 2003; Mouti 2014), one study included only adults who had an average IQ of over 100 (McDougle 1996), and the other four studies did not report cognitive status.
Length of follow‐up: ranged from seven weeks (Remington 2001), to 12 months (NCT00183339).
Primary outcomes
Irritability: all the studies reported irritability using the ABC‐I subscale (Aman 1985), except McDougle 1996.
Aggression: McDougle 1996 was the only study that reported aggression. The Brown Aggression Scale was used to measure aggression (Brown 1979).
Self‐injury: two studies (King 2009; Mouti 2014), reported self‐injurious behaviour using the Repetitive Behaviour Scale‐Revised (Bodfish 2000).
AEs: all the studies reported AEs.
Secondary outcomes
Tolerability and acceptability (loss to follow‐up): 159 participants (23.08%) withdrew and were not included in the relevant study analyses. Reasons included withdrew consent (66), loss to follow‐up (23), lack of efficacy (5), AEs (38), other/reason unknown (16), non‐compliance (3), protocol violation (3), clinician decision (4), and no longer met study criteria (1).
Atypical antipsychotic versus another atypical antipsychotic
Two studies involving 110 participants compared risperidone to aripiprazole (DeVane 2019; Ghanizadeh 2014). Participants were all children (< 18 years). The mean age was 9.6 and 9.5 years for aripiprazole and risperidone respectively. Both studies were parallel RCTs and were 10 weeks (DeVane 2019) and eight weeks (Ghanizadeh 2014) in duration.
-
Interventions
Risperidone: both studies used twice‐daily doses based on bodyweight. DeVane 2019 required participants who weighed 20 kg to 44 kg to take a maximum of 2.5 mg/day, and children 45 kg or more were allowed a maximum of 3 mg/day. Ghanizadeh 2014 required children up to 39 kg to take a maximum of 2 mg/day of risperidone, and children 40 kg and above a maximum of 3 mg/day (mean dose 1.12 mg/day).
Aripiprazole: Ghanizadeh 2014 allowed a maximum of 10 mg/day for children who weighed under 40 kg, and 15 mg/day for children who weighed 40 kg or more (mean dose 5.5 mg/day). DeVane 2019 allowed a maximum of 15 mg/day of aripiprazole regardless of weight.
Inclusion criteria: both studies required a clinical diagnosis of ASD and DeVane 2019 required participants to have an ABC‐I (Aman 1985), subscale score of > 18 at baseline, a CGI Severity score of 4 or greater (Guy 1976), and a mental age of at least 18 months.
Exclusion criteria: participants with a history of or current unstable medical conditions, prior use of risperidone or aripiprazole for more than two weeks within the last three years, medical conditions that may increase the risk of AEs including liver, renal or cardiovascular conditions, psychiatric disorders that are currently managed by psychotropic medications, or seizures within the past six months
Setting: DeVane 2019 was conducted in the USA whilst Ghanizadeh 2014 was conducted in Iran. All participants were recruited from either outpatient clinics, or clinics and research centres associated with universities.
Concomitant medications: one study (Ghanizadeh 2014), required participants to be off aripiprazole and risperidone for at least two weeks prior to and during the study, although other concomitant medications were allowed during the trial provided they were stable and commenced at least two weeks prior to the trial, while DeVane 2019 did not explicitly state medication requirements except that participants could not have taken either intervention for longer than two weeks in the last three years (DeVane 2019).
Participant cognitive status: neither study reported the cognitive status of participants.
Length of follow‐up: DeVane 2019 and Ghanizadeh 2014 were 10 and 8 weeks in duration respectively. Neither study followed up after the endpoint.
Primary outcomes
Irritability: both studies reported irritability using the ABC‐I subscale (Aman 1985). The baseline ABC‐I scores of all participants were above 20.
AEs: both studies reported AEs.
Secondary outcomes
Tolerability and acceptability (loss to follow‐up): 16 participants (14.5%) withdrew from their respective interventions and were not included in the relevant study analyses. Reasons for withdrawing from the risperidone groups included AEs (9), missed visits (4), increased behaviours of concern or exacerbation of medical condition (2), or physician decision (1).
Atypical antipsychotic versus an antidementia drug
One, eight‐week, parallel study involving 34 participants compared risperidone to memantine (Nikvarz 2017). Participants were all under 18 years (mean 6.7 years).
Interventions: once‐daily doses of risperidone commenced at 0.02 mg/kg/day, increasing to a maximum of 0.08 mg/kg/day or 3 mg/day. Memantine was administered in once‐daily doses of 20 mg if tolerated (mean daily dose of 0.4 mg/kg/day).
Inclusion criteria: participants were 5 to 17 years of age with a clinical diagnosis of ASD and had not received any pharmacological treatments for ASD or the treatments had been ineffective.
Exclusion criteria: people with a neurological disorder except for controlled epilepsy (defined as experiencing no seizures for at least one month prior to the study), history of substance abuse, any other significant medical conditions including cardiac, liver or kidney failure, pregnant or breastfeeding, previous allergic reactions to either risperidone or memantine, and currently taking stimulants.
Setting: an outpatient child and adolescent clinic associated with a university in Iran
Concomitant medications: details were not provided.
Participant cognitive status: details were not provided.
Primary outcomes
Irritability: irritability was reported using the ABC‐I subscale (Aman 1985). The baseline ABC‐I scores of all participants were above 20.
AEs: AEs were not reported fully for both groups apart from somnolence, which we included in the analyses.
Secondary outcomes
Tolerability and acceptability (loss to follow‐up): four participants (11.76%) withdrew and were not included in the relevant study analyses. Reasons included changing psychiatrist (1) and lack of efficacy (3).
Atypical antipsychotic versus an antiparkinsonian drug (bromocriptine)
One study involving nine participants compared amisulpride to bromocriptine (Dollfus 1992). The four‐week cross‐over study was conducted in France and involved children aged between 4 and 13 years of age.
Intervention (amisulpride plus placebo): amisulpride was administered at 1.5 mg/kg/day over a four‐week period with a six‐week washout period between the two phases.
Comparator (bromocriptine plus placebo): bromocriptine was administered at 0.15 mg/kg/day to 0.20 mg/kg/day plus placebo over a four‐week period with a six‐week washout period between the two phases.
Inclusion criteria: children aged 4 to 13 years with a clinical diagnosis of ASD, and a Childhood Autism Rating Scale (Schopler 2009), score of at least 36 indicating 'severely autistic'.
Exclusion criteria: no neuroleptic or other psychotropic medications were allowed during the trial, except for benzodiazepine, niaprazine, or hydroxyzine for severe sleep disorders.
Concomitant medications: three out of nine children were taking other permitted medications during the trial, including one child who was taking three different medications.
Outcomes
AEs was the only relevant outcome reported in this study.
Anticonvulsants versus placebo or other treatment
Six studies (12 reports, 165 participants, 6 datasets) compared an anticonvulsant to a placebo. All participants were children (< 18 years) apart from one adult in Hollander 2006a. All trials were parallel studies, with study duration ranging from eight to 18 weeks (Belsito 2001), (mean 10 weeks) and apart from one study (Rezaei 2010 (Iran)) all trials were conducted in the USA.
-
Interventions
Divalproex sodium: two trials involving 40 participants compared divalproex sodium to a placebo. Hollander 2010 commenced divalproex sodium at 125 mg/day once to twice daily for children up to 40 kg, and a maximum of 250 mg/day for children over 40 kg. Hollander 2006a increased divalproex sodium from 125 mg/day to a maximum of 30 mg/kg/day (mean final dose 822.92 mg/kg/day).
Lamotrigine: one study involving 35 participants compared lamotrigine to a placebo. Lamotrigine commenced at 0.5 mg/kg twice daily up to a maximum of 5.0 mg/kg twice daily (Belsito 2001).
Levetiracetam: one study involving 20 participants compared levetiracetam to a placebo. Wasserman 2006 commenced levetiracetam at 125 mg/day up to a maximum of 20 mg/kg/day to 30 mg/kg/day (mean maximum dose 862.50 mg/day).
Topiramate: one study involving 40 participants compared risperidone plus topiramate to risperidone plus placebo (Rezaei 2010). The analysis for this study is topiramate versus placebo. The maximum dose of topiramate was 100 mg/day for children under 30 kg or three to six years of age, and maximum of 200 mg/day for children 30 kg or more, or 7 to 12 years of age.
Valproate: one study involving 30 participants compared valproate to a placebo (Hellings 2005). The maximum valproate dose was 20 mg/kg/day.
Comparators: all studies compared an anticonvulsant to a placebo. Further details regarding placebo ingredients were not provided.
Inclusion criteria: all studies required participants to have a clinical diagnosis of ASD, Asperger's or PDD‐NOS, be free of other medications for at least two weeks prior to the study, and six of the studies required significant overactivity or inattention or a dual diagnosis of ADHD and ASD.
Exclusion criteria: most studies excluded people with unstable seizure disorders or other significant medical conditions including past or present psychotic disorders, and the concomitant use of psychotropic medications during the study.
Setting: apart from Rezaei 2010, all studies were conducted in the USA at either outpatient clinics, hospitals or clinics and research centres associated with universities. Rezaei 2010 was conducted at a hospital associated with a university in Iran.
Concomitant medications: all but two studies did not allow the use of psychoactive medications during the study. Handen 2008 had eight participants who were taking a range of psychotropic medications, including methylphenidate, risperidone, and anticonvulsants. Handen 2015 allowed the use of a single anticonvulsant for seizure disorders provided that seizures were stable, and the participant had been seizure‐free for at least six months.
Participant cognitive status: five of the studies reported IQ, all of which had a mean IQ of less than 90.
Length of follow‐up: length of follow‐up ranged from eight to 18 weeks (mean 10 weeks).
Primary outcomes
Irritability: all studies apart from one (Hollander 2006a), reported irritability. All studies used the ABC‐I subscale to measure irritability, however, Wasserman 2006 only reports baseline ABC‐I data.
Aggression: one study (Hellings 2005), reports aggression. The Overt Aggression Scale (parent‐rated; Yudofsky 2003), was used to measure aggression.
AEs: all six studies reported AEs.
Secondary outcomes
Tolerability and acceptability (loss to follow‐up): 21 participants (12.73%) withdrew and were not included in the relevant study analyses. Reasons included withdrawing consent (9), difficulty administering the medication (1); increased behavioural difficulties (4); increased symptoms associated with ASD (3); lack of efficacy (2); seizures (1); and skin rash (1).
Antidementia interventions versus placebo or other treatments
Eight studies (641 participants, 17 reports, 9 datasets) compared an antidementia intervention to a placebo or other treatment. Four studies compared memantine to a placebo, one study compared piracetam, one galantamine, and one compared donepezil to a placebo. All studies were parallel trials, were either 10 or 12 weeks in duration, and involved children (< 18 years). Four studies were conducted in the USA (Aman 2017; Handen 2011; NCT01972074; Soorya 2021), one study was conducted in multiple countries (Hardan 2019), and the other three were conducted in Iran. Most studies included children up to twelve years of age only, apart from Handen 2011 and NCT01972074, which involved children up to 17 years of age.
-
Interventions
Memantine: five studies involving 527 participants compared memantine to a placebo (Aman 2017; Ghaleiha 2013a; Hardan 2019; NCT01972074; Soorya 2021). All studies administered memantine once daily apart from NCT01972074, which involved twice‐daily doses. Two studies had maximum memantine doses of 15 mg/day (Ghaleiha 2013a; Hardan 2019), Aman 2017 administered 3 mg/day to 18 mg/day, depending on bodyweight, and children in NCT01972074 received a maximum of 20 mg/day.
Piracetam: one study involving 40 participants compared piracetam to a placebo (Akhondzadeh 2008). Piracetam was administered up to 800 mg/day in addition to 2 mg/day of risperidone for children up to 40 kg, and 3 mg/day for children 41 kg and above.
Galantamine: one study involving 40 participants compared galantamine to a placebo (Ghaleiha 2014). Galantamine was administered up to 12 mg/day for children up to 19 kg, 16 mg/day for children 20 kg to 30 kg, 20 mg/day for children 31 kg to 40 kg, and 24 mg/day for children over 40 kg. Risperidone was also administered up to 1 mg/day for children less than 20 kg, and 2 mg/day for children 20 kg and above.
Donepezil: one study involving 34 participants compared donepezil to a placebo (Handen 2011). The trial involved 5 mg/day of donepezil for four weeks and progressed to a maximum of 10 mg/day of donepezil for another four weeks if tolerated.
Comparators: three studies compared the intervention to a placebo plus risperidone, however, the analysis for these studies only included intervention versus placebo because risperidone was also added to the intervention (Akhondzadeh 2008; Ghaleiha 2013a; Ghaleiha 2014). None of the studies provided details of the placebo.
Inclusion criteria: all studies required participants to have a clinical diagnosis of ASD based on DSM criteria; two studies specified a minimum ABC‐I score of 12 (Ghaleiha 2013a; Ghaleiha 2014), and a maximum ABC‐I score of 16 (Hardan 2019). Two studies required either a minimum of 5 on the CGI‐Severity scale (NCT01972074), or presentation of severe symptoms related to ASD (Akhondzadeh 2008).
Exclusion criteria: most studies excluded people with co‐occurring psychiatric disorders, history of or current significant medical conditions including renal, cardiovascular, neurological, current or recent treatment with psychotropic medications or other medications prohibited for use during the study, and two studies excluded people with severe intellectual disabilities (Akhondzadeh 2008; Ghaleiha 2014).
Setting: four studies were primarily based in the USA at clinics and hospitals, three studies in Iran at clinics and hospitals associated with a university, and one study was conducted in 15 countries (Hardan 2019).
Concomitant medications: two studies provided details of concomitant medication use (Handen 2011; Hardan 2019). Handen 2011 allowed medications that did not interact with donepezil. Concurrent medication use included atomoxetine (1 participant in each group), stimulants (2 participants in each group), and sertraline (1 participant in intervention group) and citalopram (1 participant in intervention group). Hardan 2019 reported that approximately 10% of participants were taking risperidone, amongst other supplements and medications.
Participant cognitive status: not reported
Length of follow‐up: all studies were either 10 weeks or 12 weeks in duration and none of the studies followed up after the endpoint of the trial.
Primary outcomes
Irritability: three studies reported irritability (Ghaleiha 2013a; Ghaleiha 2014; Handen 2011). Two studies used the ABC‐I subscale (Aman 1985), to report irritability, while Handen 2011 used the Ritvo‐Freeman Real Life Rating Scale (affectual responses subscale; Freeman 1986) to report irritability.
Aggression: Handen 2011 reported aggression using the Child Behaviour Checklist (CBCL) (Achenbach 2000).
AEs: apart from Handen 2011, which reported no AEs associated with donepezil, all studies reported AEs.
Secondary outcomes
Tolerability and acceptability (loss to follow‐up): 54 participants (8.7%) withdrew from the studies and were not included in the relevant study analyses. Reasons included withdrawing consent (15); AEs (15), protocol violations (5); lost to follow‐up (4); lack of efficacy (5); no longer met inclusion/exclusion criteria (2); other (7); tolerability (2); and increased behaviours of concern (1).
Antiparkinsonian interventions versus placebo or other treatments
Two studies (3 reports, 79 participants, 2 datasets) compared an antiparkinsonian intervention to a placebo (King 2001; Mohammadi 2013). Both studies compared amantadine to a placebo, however, Mohammadi 2013 compared amantadine plus risperidone to placebo plus risperidone. The analysis for Mohammadi 2013 only included amantadine versus placebo. Both studies were parallel. King 2001 was five weeks in duration and was conducted in the USA at medical centres associated with universities. Mohammadi 2013 was 10 weeks in duration and was conducted in Iran at a hospital associated with a university. All participants were children and were approximately the same age (mean age 7.0 years).
Interventions: King 2001 required children to take 5 mg/kg/day of amantadine over two daily doses regardless of weight, whilst Mohammadi 2013 required children who weighed 30 kg to take 100 mg/day of amantadine or 150 mg/day over two daily doses for children 30 kg or over.
Comparators: both studies compared amantadine to a placebo however neither study described the ingredients of the placebo. Mohammadi 2013 compared amantadine to a placebo plus risperidone, although the analysis is only amantadine versus placebo.
Inclusion criteria: both studies required participants to have a diagnosis of ASD based on the DSM criteria and a score of 12 or higher on the ABC‐I subscale. Mohammadi 2013 also required presentation of severely disruptive symptoms associated with ASD.
Exclusion criteria: both studies excluded people with significant medical conditions requiring medications, allergies to the intervention, and psychotropic use in the six weeks prior to enrolment (Mohammadi 2013), or taking neuroleptic, anticonvulsant or stimulants (King 2001).
Concomitant medications: King 2001 allowed the use of SSRIs provided the dose had been stable for at least one month prior to the trial and the dose did not change during the trial. Mohammadi 2013 did not allow the use of any psychotropic medications.
Participant cognitive status: neither study provided details.
Length of follow‐up: King 2001 was five weeks and Mohammadi 2013 10 weeks in duration. Neither study followed up after the endpoint of the trial.
Primary outcomes
Secondary outcomes
Tolerability and acceptability (loss to follow‐up): Mohammadi 2013 excluded one participant (1.3%) from the analysis but did not provide the reason.
Anxiolytic interventions versus placebo or other treatment
Two studies (4 reports, 200 participants, 3 datasets) compared an anxiolytic to a placebo (Chugani 2016; Ghanizadeh 2015). Both studies compared buspirone, however, Ghanizadeh 2015 compared buspirone plus risperidone to placebo plus risperidone. The analysis for Ghanizadeh 2015 was buspirone versus placebo. Both studies were parallel, however Chugani 2016 was 24 weeks in duration and was based at six academic medical centres in the USA, and Ghanizadeh 2015 was eight weeks in duration and was conducted at a child and adolescent psychiatry clinic associated with a university in Iran. All participants were under 18 years old, however Chugani 2016 only included children under six years of age and Ghanizadeh 2015 included children up to 17 years of age.
Interventions: Chugani 2016 required participants to take buspirone twice daily at either 2.5 mg/dose (5 mg/day) or 5 mg/dose (10 mg/day). Ghanizadeh 2015 required children who weighed less than 40 kg to have a maximum of 5 mg twice daily (10 mg/day), or a maximum of 10 mg twice daily (20 mg/day) for children who weighed 40 kg or more.
Comparators: both studies compared buspirone to a placebo however Ghanizadeh 2015 compared buspirone plus risperidone to placebo plus risperidone. As mentioned previously, the analysis only involved buspirone versus placebo.
Inclusion criteria: both studies required participants to meet the DSM‐IV criteria for ASD; Ghanizadeh 2015 required participants to have at least a moderate rating on the CGI‐Severity score.
Exclusion criteria: both studies excluded people who had unstable medical conditions that required medication, including neurological, liver, kidney, cardiac or psychotic disorders. Chugani 2016 excluded people who were taking medications such as anticonvulsants, antidepressants, benzodiazepines, or neuroleptics in the six weeks prior to the trial, Ghanizadeh 2015 excluded people who had taken antipsychotics in the two months prior to the study.
Concomitant medications: Ghanizadeh 2015 allowed participants to take stable medications apart from antipsychotics provided that they were maintained at a constant dose throughout the trial.
Participant cognitive status: neither study provided details regarding cognitive status.
Length of follow‐up: Chugani 2016 was 24 weeks in duration and Ghanizadeh 2015 was eight weeks in duration.
Primary outcomes
Irritability: Ghanizadeh 2015 reported irritability using the ABC‐I subscale (Aman 1985). Baseline ABC‐I scores were above 24.
AEs: Chugani 2016 reported AEs.
Secondary outcomes
Tolerability and acceptability (loss to follow‐up): 30 participants (15%) withdrew and were not included in the relevant study analyses. Reasons included withdrawing consent (6); AEs (13), lost to follow‐up (5); no longer met inclusion/exclusion criteria (2); clinical decision (2); participant moved(1); other (1).
Experimental interventions versus placebo or other treatment:
Forty‐two studies (72 reports, 1920 participants, 43 datasets) compared an experimental interventional drug to a placebo. The majority of studies only included children, however, five studies included only adults (Chez 2020; Danforth 2018; Hollander 2020a; Lewis 2018; Willemsen‐Swinkels 1995), two studies included both adolescents (12 years and over) and adults (Veenstra‐VanderWeele 2017; Wink 2018), one study included only adolescents (11 to 17 years; Ayatollahi 2020), and one study involved children and adults up to 21 years of age (Aran 2021). Study duration ranged from seven days (Lewis 2018), to six months (Danfors 2005), with a mean duration of 10 weeks. Eighteen studies were conducted in Iran, 14 were conducted in the USA, four in the Netherlands (Sprengers 2021; VanAndel 2022; Willemsen‐Swinkels 1996; Willemsen‐Swinkels 1995), one in Israel (Aran 2021), China, Sweden, Australia, France and Austria respectively (Dai 2021; Danfors 2005; Dean 2019; Lemonnier 2017; Niederhofer 2002). All were parallel studies apart from 10, which were cross‐over studies.
-
Interventions
Arbaclofen: one study involving 150 participants compared arbaclofen to a placebo (Veenstra‐VanderWeele 2017). Mean age of participants was 11.6 years (range 5 years to 21 years). Arbaclofen was administered twice daily, up to maximum of 10 mg/day for children under 12 years and a maximum of 15 mg for participants 12 years and above.
Baclofen plus risperidone: one study involving 58 participants 4 to 12 years of age compared baclofen (plus risperidone) to a placebo (plus risperidone; Mahdavinasab 2019). Risperidone commenced at 0.5 mg/day to a maximum of 1.5 mg/day and baclofen was administered three times daily at 0.6 mg/kg. The analysis was baclofen compared to placebo.
Bumetanide: four studies involving 335 participants up to 18 years of age compared bumetanide to a placebo (Dai 2021; Lemonnier 2017; Sprengers 2021; VanAndel 2022). Participants in Lemonnier 2017 were allocated to either 0.5 mg, 1 mg, or 2 mg of bumetanide twice daily. Sprengers 2021 administered bumetanide in liquid form twice daily with a mean dose of 0.0482 mg/kg/day, and Dai 2021 administered 0.5 mg of bumetanide twice daily.
Cannabidiol: one cross‐over study involving 88 participants aged 5 to 21 years compared cannabidiol to a placebo (Aran 2021). Participants received 1 mg/kg of cannabidiol per day for 12 weeks.
Celecoxib plus risperidone: one study involving 40 participants compared celecoxib to a placebo (Asadabadi 2013). Maximum celecoxib was 200 mg/day plus 2 mg/day of risperidone for children who weighed 10 kg to 30 kg, and 30 mg/day of celecoxib plus 3 mg/day of risperidone for children 31 kg and over. Equivalent placebo plus risperidone was provided to participants in the placebo group. The analysis for this study is celecoxib versus placebo.
Cyproheptadine plus haloperidol: one study involving 40 participants compared cyproheptadine plus haloperidol to a placebo plus haloperidol (Akhondzadeh 2004). Maximum cyproheptadine was 0.2 mg/kg/day and maximum haloperidol was 0.05 mg/kg/day. The analysis for this study was cyproheptadine versus placebo.
D‐cycloserine plus social skills training: one study involving 67 participants compared D‐cycloserine plus social skills training to a placebo plus social skills training (Minshawi 2016). Participants received 50 mg of D‐cycloserine or placebo 30 minutes prior to weekly social skills training sessions.
Dextromethorphan: one study involving eight participants compared dextromethorphan to a placebo (sweetened syrup; Woodard 2007). Children aged 6 to 12 years and 13 years and over received 30 mg or 60 mg of dextromethorphan, respectively, every 12 hours.
Dextromethorphan plus quinidine: one study involving 14 participants compared dextromethorphan plus quinidine (Chez 2020). Participants received 20 mg of dextromethorphan plus 10 mg of quinidine in tablet form (Nuedexta) once daily for the first week and then twice daily for the following seven weeks.
Fenfluramine: one study involving 11 participants compared fenfluramine to a placebo (Campbell 1987). Fenfluramine was initiated at 1.0 mg/kg/day across two daily doses, increasing to a maximum of 60 mg/day.
Folinic acid plus risperidone: one study involving 55 participants compared folinic acid plus risperidone to a placebo plus risperidone (Batebi 2021). Folinic acid was administered at 2 mg/kg up to a maximum of 50 mg/day. Maximum risperidone for children who weighed up to 19 kg and 20 kg and over was 1 mg/day and 2 mg/day respectively. The analysis for this study was folinic acid versus placebo.
L‐carnosine plus risperidone: one study involving 42 participants compared L‐carnosine plus risperidone to a placebo plus risperidone (Hajizadeh‐Zaker 2018). Participants received 400 mg of L‐carnosine twice daily plus a maximum of 1 mg/day of risperidone (children under 20 kg) or 2 mg/day of risperidone (children over 20 kg). The analysis for this study was L‐carnosine versus placebo.
Lofexedine: one study involving 12 participants compared lofexedine to a placebo (Niederhofer 2002). Lofexedine commenced at 0.4 mg/day up to a maximum of 1.2 mg/day over three daily doses.
MDMA (methylenedioxymethamphetamine) plus psychotherapy: one study involving 12 adults compared MDMA plus psychotherapy to a placebo plus psychotherapy (Danforth 2018). Following three 60‐ to 90‐minute psychotherapy sessions, participants received either 75 mg to 125 mg of MDMA or placebo on two occasions approximately one month apart.
Mecamylamine: one study involving 20 participants compared mecamylamine to a placebo (Arnold 2012a). Mecamylamine was administered in fixed doses starting at 0.5 mg/day up to 5 mg/day if tolerated.
Minocycline plus risperidone: one study involving 46 participants compared minocycline plus risperidone to a placebo plus risperidone (Ghaleiha 2016). Minocycline was administered in fixed doses of 100 mg/day plus risperidone 1 mg/day (children under 20 kg) or 2 mg/day (children over 20 kg). The analysis for this study was minocycline versus placebo.
N‐acetylcysteine plus risperidone: two studies involving 71 participants compared N‐acetylcysteine plus risperidone to a placebo plus risperidone (Ghanizadeh 2013; Nikoo 2015).
N‐acetylcysteine: three studies involving 156 participants compared N‐acetylcysteine to a placebo (Dean 2019; Hardan 2012; Wink 2016).
Naltrexone: three studies involving 93 participants compared naltrexone to a placebo (Campbell 1993; Willemsen‐Swinkels 1995; Willemsen‐Swinkels 1996).
Nicotine: one study involving seven adult participants compared nicotine to a placebo (Lewis 2018). Participants applied 7 mg of nicotine or placebo daily via skin patches.
Palmitoylethanolamide plus risperidone: one study involving 62 participants compared palmitoylethanolamide plus risperidone to a placebo plus risperidone (Khalaj 2018); 600 mg of palmitoylethanolamide was administered twice daily in addition to 1 mg/day of risperidone (children under 20 kg) or 2 mg/day (children over 20 kg). The analysis for this study was palmitoylethanolamide versus placebo.
Pentoxifylline plus risperidone: one study involving 40 participants compared pentoxifylline plus risperidone to a placebo plus risperidone (Akhondzadeh 2010). Maximum pentoxifylline was 400 mg/day for children who weighed up to 40 kg, or a maximum of 600 mg/day for children 41 kg and above. Risperidone was administered up to 2 mg/day for children who weighed up to 40 kg, or a maximum of 3 mg/day for children above 40 kg. The analysis for this study was pentoxifylline versus placebo.
Pioglitazone plus risperidone: one study involving 44 participants compared pioglitazone plus risperidone to a placebo plus risperidone (Ghaleiha 2015); 15 mg of pioglitazone was administered twice daily in addition to an initial 0.5 mg/day of risperidone, increasing to 1 mg/day (children under 20 kg) or 2 mg/day (children over 20 kg). The analysis for this study was pioglitazone versus placebo.
Prednisolone plus risperidone: one study involving 26 participants compared prednisolone plus risperidone to a placebo plus risperidone (Malek 2020). Prednisolone was administered at 1 mg/kg/day in addition to an initial 0.5 mg/day of risperidone, increasing to 1 mg/day (children under 20 kg) or 2 mg/day (children over 20 kg). The analysis for this study was prednisolone versus placebo.
Pregnenolon plus risperidone: one study involving 59 participants compared pregnenolon plus risperidone to a placebo plus risperidone (Ayatollahi 2020). Pregnenolon was administered in fixed doses of 100 mg twice daily. Risperidone was administered at maximum doses of 2.5 mg/day for children who weighed 20 kg to 45 kg, or a maximum of 3.5 mg/day for children who weighed above 45 kg. The analysis for this study was pregnenolone versus placebo.
Propentofylline plus risperidone: one study involving 48 participants compared propentofylline to a placebo (Behmanesh 2019). Propentofylline commenced at 300 mg once daily and increased to 300 mg twice daily (children under 45 kg) or propentofylline increased to 300 mg three times daily (children 45 kg or over). Risperidone commenced at 0.5 mg/day and increased to 1 mg/day for children who weighed under 20 kg or 2 mg/day for those who weighed 20 kg or above. The analysis for this study was propentofylline versus placebo.
Resveratrol plus risperidone: one study involving 62 participants compared resveratrol plus risperidone to a placebo plus risperidone (Hendouei 2019). Resveratrol was administered as a fixed dose of 250 mg twice daily in addition to risperidone (initial dose of 0.5 mg/day increasing by 0.5 mg/day each week for the first three weeks). The analysis for this study was resveratrol versus placebo.
Riluzole: one study involving seven participants compared riluzole to a placebo (Wink 2018). Riluzole commenced at 50 mg/day and increased to 100 mg twice daily.
Riluzole plus risperidone: one study involving 40 participants compared riluzole plus risperidone to a placebo plus risperidone (Ghaleiha 2013b). Riluzole was administered 25 mg/day to 50 mg/day for children who weighed 10 kg to 40 kg, or a maximum of 100 mg/day for children over 40 kg. Maximum risperidone was 2 mg/day for children who weighed up to 40 kg and a maximum of 3 mg/day for children 41 kg and above.
Simvastatin plus risperidone: one study involving 66 participants compared simvastatin plus risperidone to a placebo plus risperidone (Moazen‐Zadeh 2018). Simvastatin was administered at either 20 mg/day for children under 10 years of age or 40 mg/day for children 10 years and over. The analysis for this study was simvastatin versus placebo.
Sulforaphane plus risperidone: one study involving 60 participants compared sulforaphane plus risperidone to a placebo plus risperidone (Montazmenesh 2020). Sulforaphane was administered at 50 μmol /day for children who weighed less than 45 kg, or 100 μmol for children 45 kg to 90 kg. Risperidone was administered at a maximum of 1 mg/day for children under 20 kg, 2.5 mg/day for children 20 kg to 45 kg, and 3.5 mg/day for children who weighed over 45 kg.
Tetrahydrobiopterin: two studies involving 58 participants compared tetrahydrobiopterin to a placebo (Danfors 2005; Klaiman 2013). Danfors 2005 administered tetrahydrobiopterin at a maximum of 3 mg/kg/day across two daily doses, while Klaiman 2013 administered tetrahydrobiopterin in tablet form at 20 mg/kg once daily (mean final dose was 385 mg/day).
Trichuris suis ova: one study involving 10 adult participants compared Trichuris suis ova to a placebo (Hollander 2020a). Participants received a dose of 2500 ova every two weeks.
Comparators: all studies compared an experimental intervention to a placebo, although 16 of the studies were compared to a placebo plus risperidone, one study was compared to a placebo plus haloperidol (Akhondzadeh 2004), and one study compared to placebo plus psychotherapy (Danforth 2018). Only three studies provided details of the placebo, sugar pill (Hardan 2012; Minshawi 2016) or sweetened syrup (Woodard 2007).
Inclusion criteria: all studies required participants to have a clinical diagnosis of ASD, and additional criteria included a minimum of 15 on the ABC‐I subscale (Asadabadi 2013; Ayatollahi 2020; Lewis 2018; Wink 2018; Woodard 2007), or a score of moderate or higher on the CGI‐Severity score (Minshawi 2016; Veenstra‐VanderWeele 2017), or the presentation of aggressive and disruptive behaviours (Akhondzadeh 2004; Akhondzadeh 2010; Behmanesh 2019; Ghaleiha 2015; Ghaleiha 2016; Malek 2020).
Exclusion criteria: the majority of studies excluded people with a history of or current medical or psychiatric conditions and also people who had been taking psychotropic medications or other prohibited medications in the period leading up to the trial. Some studies also excluded people with severe intellectual disabilities (Akhondzadeh 2010; Asadabadi 2013; Batebi 2021; Ghaleiha 2013b; Ghaleiha 2016; Hajizadeh‐Zaker 2018; Khalaj 2018; Montazmenesh 2020; Moazen‐Zadeh 2018), were pregnant or breastfeeding (Hollander 2020a), currently using tobacco or nicotine products (Lewis 2018), or had an allergy or intolerance to the intervention (Ayatollahi 2020; Behmanesh 2019; Nikoo 2015; Veenstra‐VanderWeele 2017).
Concomitant medications: studies required participants to have been off medications for at least one month and six months prior to the study (Niederhofer 2002; Batebi 2021), remain on stable psychotropic medications for at least three months (Arnold 2012a; Hollander 2020a), and two weeks prior to randomisation respectively (Campbell 1987; Hardan 2012; Minshawi 2016), or stable medication with no changes in the past 14 days (Lewis 2018). One study allowed the use of anticonvulsants, supplements, or sleep medications, however, any other psychotropic medications were not allowed (Klaiman 2013).
Participant cognitive status: most studies did not report the average IQ of participants apart from seven studies (Arnold 2012a; Danfors 2005; Dean 2019; Minshawi 2016; Niederhofer 2002; Sprengers 2021; Wink 2016). IQ ranged from 53 to 100 across these studies.
Length of follow‐up: study duration ranged from seven days (Lewis 2018), to six months (Danfors 2005). Mean duration was 9.6 weeks.
Primary outcomes
Irritability: 32 of the studies reported irritability and all used the ABC‐I subscale (Aman 1985), to measure irritability. Most studies required participants to have a minimum baseline ABC‐I of 12 or higher while some studies required a baseline ABC‐I of 15 or higher (Ayatollahi 2020; Lewis 2018; Mahdavinasab 2019; Wink 2018).
Self‐injury: five studies reported self‐injurious behaviour (Dai 2021; Dean 2019; Hardan 2012; Hollander 2020a; VanAndel 2022). Each study used the Repetitive Behaviour Scale ‐ Revised (self‐injury subscale; Bodfish 2000) to measure self‐injurious behaviour.
AEs: apart from five studies, all studies reported AEs (Chez 2020; Lewis 2018; Mahdavinasab 2019; Malek 2020; Willemsen‐Swinkels 1996).
Secondary outcomes
Tolerability and acceptability (loss to follow‐up): 230 participants (13%) withdrew and were not included in the relevant study analyses. Reasons included withdrawing consent (103); AEs (32), lost to follow‐up (23) ; poor/non‐compliance (20), protocol violations (10); lack of efficacy (9); due to an error (4); no longer met inclusion/exclusion criteria (4); clinical decision (2); participant moved (1); other (22).
Excluded studies
The full‐text screening resulted in 88 references (as 81 studies) being excluded due to ineligible criteria. Full‐text copies of the studies listed in this section were reviewed as it was not clear whether they met the inclusion criteria for the review based on title and abstract. Further screening of the full‐text reports of these studies found that they did not meet our inclusion criteria. Reasons for exclusion included: did not focus on population of interest; did not have a focus on unwanted behaviours (irritability, aggression, self‐injury); ineligible study design (non‐RCT); non‐pharmacological intervention; irrelevant comparator; and terminated studies.
Risk of bias in included studies
See Figure 3 for a risk of bias summary, and Figure 4 for a risk of bias graph.
3.

Risk of bias in included studies
4.

Visual representation of risk of bias across all included studies
See below for more detailed information on risk of bias.
Allocation
Atypical or typical antipsychotics versus placebo or other treatment: we rated 16 studies as unclear risk of bias for randomisation and allocation concealment, mostly due to a lack of details regarding methods of randomisation and allocation concealment. We rated three studies (20%) as low because they conducted randomisation using a computer‐generated code, and one study as high due to a clear lack of randomisation and allocation concealment.
Neurohormones versus placebo or other treatment: we rated 12 studies as unclear and 12 studies as having a low risk of bias. Studies rated as unclear either did not provide details or provided very vague details regarding the randomisation and allocation of participants. We rated studies as low risk of bias because randomisation was conducted using a computer‐generated code.
ADHD‐related medications versus placebo or other treatment: we rated 10 studies as unclear risk of bias due to a lack of details regarding methods of randomisation and allocation concealment. We rated one study as low and two studies as high. The reason for the high ratings was because the investigators used 'sequential assignment'. The study rated as low randomised using a computer‐generated method.
Antidepressants versus placebo or other treatment: we rated eight studies as unclear due to a lack of details regarding methods of randomisation and allocation concealment. We rated the other two studies as low risk of bias as randomisation was conducted externally to the trial.
Atypical antipsychotic versus another atypical antipsychotic: we rated allocation concealment as unclear for both of the studies due to a lack of information.
Atypical antipsychotic versus an anti‐dementia drug: we rated allocation concealment as unclear for Nikvarz 2017 because although referred to as "simple balanced blocked randomisation", the study authors did not provide information on how allocation was concealed.
Atypical antipsychotic versus an antiparkinsonian drug (bromocriptine): we rated allocation concealment as unclear for Dollfus 1992 due to a lack of information.
Anticonvulsants versus placebo or other treatment: we rated five studies as having an unclear risk of bias due to a lack of details and one study as low because it conducted randomisation using a computer‐generated code.
Antidementia interventions versus placebo or other treatments: we rated six studies as low risk of bias because they conducted randomisation using a computer‐generated code, and the other two studies as unclear due to a lack of detail regarding the allocation process.
Antiparkinsonian interventions versus placebo or other treatments: we rated one study as low because it conducted randomisation using a computer‐generated code and the other study as having an unclear risk of bias due to insufficient details regarding allocation concealment.
Anxiolytic interventions versus placebo or other treatment: we rated one study as unclear due to a lack of details and the other study as low risk of bias because it conducted randomisation using a computer‐generated code.
Experimental interventions versus placebo or other treatment: we rated 24 studies as low risk of bias because they conducted randomisation using a computer‐generated code. We rated the remaining 18 studies as unclear, mainly due to a lack of details regarding randomisation methods and allocation concealment.
Blinding
Atypical or typical antipsychotics versus placebo or other treatment: we rated 14 studies as unclear risk of bias due to a lack of details regarding blinding and who was blinded, and the remaining six studies as low risk of bias.
Neurohormones versus placebo or other treatment: we rated 13 studies as unclear and the remaining 11 studies as having low risk of bias. Studies with an unclear risk of bias usually did not provide further details apart from stating that they used double‐blinding.
ADHD‐related medications versus placebo or other treatment: we rated eight studies as unclear risk of bias, three as low risk of bias and the remaining two studies as high risk of bias. This was due to investigators being unblinded.
Antidepressants versus placebo or other treatment: we rated seven studies as unclear risk of bias, with the remaining three studies at low risk of bias.
Atypical antipsychotic versus another atypical antipsychotic: we rated one study as a low risk of bias and the other as high due to some participants being unblinded and an unblinded clinician.
Atypical antipsychotic versus an anti‐dementia drug: we rated this study as having a high risk of bias due to being an open‐label (randomised) study and therefore lacking blinding.
Atypical antipsychotic versus an antiparkinsonian (bromocriptine): we rated this study as having an unclear risk of bias because it did not provide details regarding blinding.
Anticonvulsants versus placebo or other treatment: we rated three studies as being of low risk of bias and three studies as unclear, mainly due to lack of details.
Antidementia interventions versus placebo or other treatments: we rated six studies as having low risk of bias because they clearly stated the blinding methods that they used, and the other two studies as unclear risk of bias due to lack of further details apart from stating the study was double‐blinded.
Antiparkinsonian interventions versus placebo or other treatments: we rated one study as low risk of bias because different people were involved in the allocation of participants and the measurement of outcomes. We rated the other study as unclear risk of bias due to insufficient details regarding blinding.
Anxiolytic interventions versus placebo or other treatment: we rated one study as low risk of bias because an external person, who was not involved in enrolment or allocation, monitored outcomes. We rated the other study as unclear risk of bias because although the study stated that they used double‐blinding, the person who allocated participants to groups was unblinded.
Experimental interventions versus placebo or other treatment: we rated 30 studies as low risk of bias, 11 as unclear, and one as high risk of bias due to the use of single‐blinding only. The studies rated as unclear were due to a lack of details regarding blinding and who was blinded, and the high risk of bias was because the assessors were unblinded.
Incomplete outcome data
Atypical or typical antipsychotics versus placebo or other treatment: we rated 12 studies at low risk of bias, with a further four studies being rated as unclear and four studies as high risk of bias due to high rates of attrition, not including some participants in the analysis due to lack of efficacy, or lack of details regarding participants lost to follow‐up. We rated studies as unclear due to vague details regarding imputation of missing data, or an intention‐to‐treat analysis that did not include all participants.
Neurohormones versus placebo or other treatment: we rated 13 studies as low, six studies as unclear and five as high risk of bias. Studies rated as high had up to 50% missing data or did not provide reasons for loss to follow‐up. Studies rated as unclear did not provide reasons for participants lost to follow‐up, or some participants were not accounted for in analysis or numbers of participants lost to follow‐up. Studies rated as low had included all participants in the analysis and used an intention‐to‐treat analysis for any participants who did not complete the trial.
ADHD‐related medications versus placebo or other treatment: we rated five studies as unclear, two as low and six as high. We judged studies as high risk due to unexplained loss to follow‐up, incomplete data or lack of post‐baseline ratings. Ratings of unclear were because the study authors did not clearly report numbers of participants who completed the study and any who were lost to follow‐up throughout the study. Studies with ratings of low had included all participants in the final analysis or used an intention‐to‐treat analysis, or both.
Antidepressants versus placebo or other treatment: we rated four studies as having an unclear risk of bias, three studies as high and three studies as low risk of bias. 'Unclear' ratings were because it was not clear how many participants were included in the analysis, or loss to follow‐up was not reported by group. Reasons for a judgement of high risk of bias included high attrition of 20% to 25%, and not providing reasons for participant loss to follow‐up. The studies rated as low risk of bias used an intention‐to‐treat analysis and included all participants in the final analysis.
Atypical antipsychotic versus another atypical antipsychotic: we rated both studies as having a low risk of bias as all participants were included in the analysis.
Atypical antipsychotic versus an anti‐dementia drug: we rated the study as high risk of bias because data were not imputed for participants who discontinued.
Atypical antipsychotic versus an antiparkinsonian (bromocriptine): we rated the study as having a low risk of bias because only one participant did not complete the study, and it used a last observation carried forward.
Anticonvulsants versus placebo or other treatment: we rated three studies as unclear risk of bias and three studies as high risk of bias. The ratings of unclear were mainly due to unaccounted for participants, not imputing data where participants were lost to follow‐up, or lack of clarity regarding the number included in the analysis. The studies rated as high risk of bias were because of incomplete data.
Anti‐dementia interventions versus placebo or other treatments: we rated six studies as having low risk of bias, one study as high and one study as unclear risk of bias. The study with a high risk of bias had almost 50% attrition and the study rated as unclear provided vague details regarding loss to follow‐up and number analysed. Studies rated as low risk of bias included all participants in the analysis and used an intention‐to‐treat analysis for any participants who did not complete the trial.
Antiparkinsonian interventions versus placebo or other treatments: we rated one study as low risk of bias because all participants were included in the analysis, while we rated the other study as unclear due to imputation using last observation carried forward for all participants with at least one measurement post‐baseline.
Anxiolytic interventions versus placebo or other treatment: we rated one study as unclear and the other study as high risk of bias. The high risk of bias was due to not reporting outcome data at one of the prespecified time points and the study rated as unclear was due to "unavailable data" for almost half of the discontinued participants.
Experimental interventions versus placebo or other treatment: we rated 17 studies as low risk of bias, 14 as unclear and 11 studies as high risk of bias. The studies rated at high risk of bias were mainly due to significant attrition or not reporting reasons for loss to follow‐up. The ratings of unclear were because it was unclear how many were included in the analysis, or no further statistical measures such as intention‐to‐treat were used for those lost to follow‐up.
Selective reporting
Atypical or typical antipsychotics versus placebo or other treatment: we rated nine studies as high risk of bias, seven studies as low and four studies as unclear risk of bias. We rated the nine studies as high because of incomplete or absent reporting of outcomes, and not reporting AEs when it is highly likely they would have occurred. The studies rated as low were because all outcomes listed in the protocol or on the trial registry were reported in the published paper. The unclear ratings were due to lack of a protocol.
Neurohormones versus placebo or other treatment: we rated 11 studies as low risk of bias because outcomes reported matched those listed in the protocol, seven studies as unclear due to an absence of a published protocol or trial registration, and six as high risk of bias. Studies rated as high risk of bias did not report outcomes that were mentioned or listed on the clinical trials registry.
ADHD‐related medications versus placebo or other treatment: we rated seven studies as high risk of bias, three studies as low and two were unclear. The reasons for the high ratings were either incomplete or absent outcome data. The ratings of unclear were because of the absence of a published paper and details only provided on the trial registry. The ratings of low were because all outcomes listed in the protocol or on the trial registry were reported in the published paper.
Antidepressants versus placebo or other treatment: we rated four studies as low risk of bias, four studies as unclear and two studies as high risk of bias. Reasons for a rating of high were incomplete or absent outcome data. We rated studies as low because all outcomes listed in the protocol or on the trials registry were reported in the published paper. The unclear ratings were because of an absence of a published paper and details only provided on the trial registry.
Atypical antipsychotic versus another atypical antipsychotic: we rated one study as having a high risk of bias, due to conflicting statements that disagree with the statistics that they provided, and the other study as low risk of bias.
Atypical antipsychotic versus an antidementia drug: we rated this study as having an unclear risk of bias due to lack of a protocol.
Atypical antipsychotic versus an antiparkinsonian (bromocriptine): we rated this study as having an unclear risk of bias due to lack of a protocol.
Anticonvulsants versus placebo or other treatment: we rated five studies as high risk of bias and one as low risk. The ratings of high risk of bias were due to lack of outcome data, the use of P values or t‐values to report data, or differences between information in published papers and the clinical trials registry. The rating of low was because outcomes reported matched those listed in the protocol or on the trials registry.
Antidementia interventions versus placebo or other treatments: we rated three studies as having a high risk of bias, four studies as low and one study as having an unclear risk of bias. The unclear rating was because of an absence of a published protocol, and the low ratings were because all outcomes listed in a protocol or trial registry were reported by the study authors in the published paper. The ratings of high were because outcome data were not reported.
Antiparkinsonian interventions versus placebo or other treatments: we rated one study as low risk of bias and the other as unclear because it used last observation carried forward for any participant with at least one post‐baseline measure.
Anxiolytic interventions versus placebo or other treatment: we rated one study as low risk of bias because all outcomes listed in a protocol or trial registry were reported by the study authors in the published paper, and the study rated as high risk of bias was due to outcome measures not reported at the time points mentioned.
Experimental interventions versus placebo or other treatment: we rated 21 studies as low risk of bias because outcomes reported matched those listed in the protocol, 12 as unclear due to an absence of a published protocol or trial registry, and nine studies as high. The reasons for high risk of bias were failure to report outcomes mentioned in protocols or on trial registries, or reporting data at different time points to that mentioned in the protocol or trial registry.
Other potential sources of bias
Atypical or typical antipsychotics versus placebo or other treatment: we rated six studies as low risk of bias, eight as high risk of bias, and six as unclear. Most of the studies rated as high risk of bias were because of funding or other support by pharmaceutical companies, agreements between study authors and sponsors regarding the publishing of results, a small proportion of the sample with a diagnosis of autism despite the title mentioning autism spectrum disorder, or study authors' direct involvement in the ethics committee or funding process. The studies rated as unclear were because of some financial or other support from pharmaceutical companies. The six studies rated as low were because we identified no other sources of bias.
Neurohormones versus placebo or other treatment: we rated nine studies as high risk of bias, 10 as low and five studies as unclear risk of bias. All studies rated as high risk of bias were either funded by pharmaceutical companies, the pharmaceutical companies were involved in the analysis, or participants were responders to the intervention in a previous trial. Studies rated as low were because we did not identify any other sources of bias, and the studies rated as unclear were due to some involvement by pharmaceutical companies in the study.
ADHD‐related medications versus placebo or other treatment: we rated five studies as high risk of bias due to a lack of standardised measures, having received funding by pharmaceutical companies, or study authors' direct involvement in the ethics committee or funding process. We rated five studies as unclear due to highly divergent samples in addition to small sample sizes or lack of details regarding sponsorship or funding, and three studies as low because we did not identify any other sources of bias.
Antidepressants versus placebo or other treatment: we rated five studies as unclear risk of bias because of lack of details regarding funding, a published paper not being available, or a lack of baseline comparisons reported by group. We rated one study as low and four as high risk of bias. We rated studies as high risk of bias due to involvement or employment of study authors by pharmaceutical companies, study authors' direct involvement in the ethics committee or funding process, or an imbalance in baseline characteristics between the two groups. The one study rated as low was because we did not identify any other sources of bias.
Atypical antipsychotic versus another atypical antipsychotic: we rated both studies as having a low risk of bias because we did not identify any other sources of bias.
Atypical antipsychotic versus an antidementia drug: we rated this study as having a low risk of bias because we did not identify any other sources of bias.
Atypical antipsychotic versus an antiparkinsonian (bromocriptine): we rated this study as having an unclear risk of bias because we did not identify any other sources of bias. However, without a protocol or trial registry entry, it is difficult to know.
Anticonvulsants versus placebo or other treatment: we rated three studies as unclear risk of bias, two as high and one as low risk of bias. The studies rated as unclear were due to funding or other support from pharmaceutical companies, and the studies rated as high were due to a change in study duration without explanation or study authors' direct involvement in the ethics committee or funding process. The study rated as low was because we did not identify any other sources of bias.
Antidementia interventions versus placebo or other treatments: we rated one study as a low risk of bias because we did not identify any other sources of bias. We rated seven studies as high risk of bias due to funding and other involvement by pharmaceutical companies or study authors' direct involvement in the ethics committee or funding process.
Antiparkinsonian interventions versus placebo or other treatments: we rated one study as unclear risk of bias due to pharmaceutical companies providing funding and the unknown role they may have had in the study. We rated the other study as high risk of bias due to study authors' direct involvement in the ethics committee or funding process.
Anxiolytic interventions versus placebo or other treatment: we rated one study as unclear and the other as a high risk of bias because the study was retrospectively registered on the clinical trials website.
Experimental interventions versus placebo or other treatment: we rated six studies as low risk of bias because we did not identify any other sources of bias, six studies as unclear and 30 studies as high risk of bias. The reasons for high risk of bias were funding or other involvement by pharmaceutical companies in the studies, study authors being employed by the pharmaceutical companies funding the study, or study authors' direct involvement in the ethics committee or funding process. The reasons for an unclear rating were because of some involvement of pharmaceutical companies, or study authors did not provide baseline details regarding group differences.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
Atypical antipsychotics versus placebo
Primary outcomes
Behaviours of concern
Irritability
Atypical antipsychotics probably reduce irritability in the short term when compared to participants taking placebo (SMD −0.90, 95% CI −1.25 to −0.55; I2 = 83%; 12 studies, 973 participants; moderate‐certainty evidence; Analysis 1.1). The high level of heterogeneity across these 12 studies was reduced to 42% when we removed Ichikawa 2017 and Troost 2005 from the analysis (SMD −0.67, 95% CI −0.87 to −0.48; I2 = 42%; 10 studies; 857 participants). Please refer to Table 1 for more information.
1.1. Analysis.

Comparison 1: Atypical antipsychotic vs placebo, Outcome 1: Irritability
There were differences between types of atypical antipsychotics (P = 0.0005), however, there were no clear differences between atypical antipsychotics (P = 0.76) when we removed Loebel 2016 (lurasidone) from the analysis.
There were no clear differences between groups when we compared children only, and adults only (P = 0.87). There was insufficient information to conduct a subgroup analysis of irritability by cognitive or communication ability.
We were unable to include irritability data from one study in the meta‐analyses because the data were skewed (Findling 2014). Details can be found in Table 8.
4. Atypical antipsychotics versus placebo: irritability results that could not be used in meta‐analyses.
| Study name | Short‐/medium‐/long‐term outcomes | Group 1 | Group 2 | Group 1 sample size | Group 2 sample size | Group 1 results Mean (standard deviation) | Group 2 results Mean (standard deviation) | Other data | Notes |
| Findling 2014 | Short‐term irritability | Aripiprazole (max 15 mg/day) | Placebo | 39 | 43 | 5.2 (10.05) | 9.6 (10.23) | ‐ | Skewed |
As there were more than 10 studies in this analysis, we created a funnel plot for this outcome but found no evidence of asymmetry (Figure 5).
5.

SE: standard error; SMD: standardised mean difference
Atypical antipsychotics versus placebo (12 studies, 973 participants; Analysis 1.1)
Improvement
Participants were twice as likely to improve, defined as a minimum 25% decrease in the ABC‐I scores (RR 2.08, 95% CI 1.39 to 3.12; I2 = 53%; 4 studies, 470 participants; Analysis 1.3). There were no clear differences between groups when risperidone and aripiprazole were compared (P = 0.17).
1.3. Analysis.

Comparison 1: Atypical antipsychotic vs placebo, Outcome 3: Improvement
Relapse
Participants were less likely to relapse, defined as a minimum 25% increase in ABC‐I scores, if they received risperidone compared to the placebo group (RR 0.30, 95% CI 0.13 to 0.68; I2 = 0%; 2 studies, 56 participants; Analysis 1.2).
1.2. Analysis.

Comparison 1: Atypical antipsychotic vs placebo, Outcome 2: Relapse
Because both studies involved children, we could not conduct a subgroup analysis. There was insufficient information to conduct a subgroup analysis by communication or cognitive ability.
Aggression
There was no clear evidence of an effect of atypical antipsychotics (risperidone) on aggression in the short term (SMD −0.44; 95% CI −0.89 to 0.01; I2 = not applicable (NA); 1 study, 77 participants; very low‐certainty evidence; Analysis 1.4). Please refer to Table 1 for more information.
1.4. Analysis.

Comparison 1: Atypical antipsychotic vs placebo, Outcome 4: Aggression
Only one study provided data for this outcome, so we were unable to conduct subgroup analyses.
We could not include data from one study in the meta‐analyses because the paper did not report endpoint data (Hollander 2006b). Details can be found in Table 9.
5. Atypical antipsychotic versus placebo: aggression results that could not be used in meta‐analyses.
| Study name | Short‐/medium‐/ long‐term outcomes | Group 1 | Group 2 | Group sample size | Group 2 sample size | Group 1 results | Group 2 results | Other data | Notes |
| Hollander 2006a | Short‐term aggression | Olanzapine max 20 mg/day | Placebo | 6 | 5 | Not provided | Not provided | ‐ | "we did not find any evidence for significant change on the CY‐BOCS, the OAS‐M irritability measure, or the OAS‐M aggression measure" |
| CY‐BOCS: Children's Yale Bown Obsessive compulsive Scale; OAS‐M: Overt Aggression Scale ‐ Modified | |||||||||
Self‐injury
The evidence is very uncertain about the effect of atypical antipsychotics compared with placebo on self‐injurious behaviour in the short term (SMD −1.43 95% CI −2.24 to −0.61; P < 0.0001; I2 = NA; 1 study, 30 participants; very low‐certainty evidence; Analysis 1.5). Please refer to Table 1 for more information.
1.5. Analysis.

Comparison 1: Atypical antipsychotic vs placebo, Outcome 5: Self‐injury
We could not include data from one study in the meta‐analyses because the data were skewed. Please refer to Table 10 for more information.
6. Atypical antipsychotic versus placebo: self‐injurious behaviour results that could not be used in the meta‐analyses.
| Study name | Short‐/medium‐/long‐term outcomes | Group 1 | Group 2 | Group sample size | Group 2 sample size | Group 1 results Mean (standard deviation) | Group 2 results Mean (standard deviation) | Other data | Notes |
| Shea 2004 | Short‐term self‐injurious behaviour | Risperidone maximum 0.02 mg/kg/day | Placebo | 39 | 38 | −2.6 (3.3) | −1.3 (2.8) | ‐ | Skewed |
Only one study provided data for this outcome, so we could not conduct subgroup analyses.
Adverse effects
Cardiovascular
Participants were more likely to have tachycardia than those receiving placebo (RR 7.53, 95% CI 1.40 to 40.52; I2 = 0%; 2 studies, 179 participants; Analysis 1.6).
1.6. Analysis.

Comparison 1: Atypical antipsychotic vs placebo, Outcome 6: Adverse effects: cardiovascular
Gastrointestinal
There was no clear evidence of a difference between participants receiving atypical antipsychotics and those receiving placebo (Analysis 1.7), in the reported rates of:
1.7. Analysis.

Comparison 1: Atypical antipsychotic vs placebo, Outcome 7: Adverse effects: gastrointestinal
diarrhoea (RR 0.93, 95% CI 0.46 to 1.88; I2 = 0%; 5 studies, 318 participants; low‐certainty evidence);
dry mouth (RR 1.97, 95% CI 0.75 to 5.20; I2 = 0%; 2 studies, 131 participants; low‐certainty evidence);
dyspepsia (RR 3.19, 95% CI 0.14 to 72.69; I2 = NA; 1 study, 31 participants; low‐certainty evidence);
nausea (RR 1.47, 95% CI 0.61 to 3.56; I2 = 0%; 4 studies, 531 participants; low‐certainty evidence); or
stomach ache (RR 0.50, 95% CI 0.19 to 1.32; I2 = 0%; 2 studies, 166 participants; low‐certainty evidence)
However, participants receiving atypical antipsychotics were more likely to report:
abdominal pain (RR 2.70, 95% CI 1.04 to 7.07; I2 = 0%; 4 studies, 400 participants; low‐certainty evidence);
constipation (RR 2.36, 95% CI 1.28 to 4.34; 7 studies, 596 participants; I2 = 0%, low‐certainty evidence);
drooling (RR 9.64, 95% CI 1.29 to 72.10; 2 studies, 313 participants; I2 = 0%, low‐certainty evidence);
hypersalivation (RR 4.15, 95% CI 1.77 to 9.71; 5 studies, 449 participants; I2 = 0%, low‐certainty evidence); and
vomiting/nausea (RR 1.79, 95% CI 1.16 to 2.74; 9 studies, 920 participants; I2 = 0%, low‐certainty evidence).
Immune system
There was no clear evidence of a difference between atypical antipsychotics and placebo groups (Analysis 1.8), in:
1.8. Analysis.

Comparison 1: Atypical antipsychotic vs placebo, Outcome 8: Adverse effects: immune system
pyrexia (RR 1.81, 95% CI 0.85 to 3.86; I2 = 0%; 5 studies, 540 participants);
cough (RR 1.50, 95% CI 0.67 to 3.34; I2 = 0%; 3 studies, 444 participants);
flu‐like symptoms (RR 1.95, 95% CI 0.38 to 10.04; I2 = NA; 1 study, 79 participants);
sore throat (RR 5.20, 95% CI 0.63 to 42.96; I2 = NA; 1 study, 100 participants); and
earache (RR 0.52, 95% CI 0.10 to 2.71; I2 = NA; 1 study, 100 participants)
Metabolic
The antipsychotic group may be more likely to have an increase in appetite than the placebo group (RR 2.38, 95% CI 1.69 to 3.34; I2 = 0%; 8 studies, 702 participants; low‐certainty evidence; Analysis 1.9).
1.9. Analysis.

Comparison 1: Atypical antipsychotic vs placebo, Outcome 9: Adverse effects: metabolic (dichotomous)
There was no difference between groups in:
decreased appetite (RR 2.12, 95% CI 0.84 to 5.33; I2 = 0%; 4 studies, 426 participants; moderate‐certainty evidence; Analysis 1.9);
thirst (RR 1.51, 95% CI 0.59 to 3.87; I2 = 0%; 3 studies, 382 participants; Analysis 1.9);
weight gain (RR 2.30, 95% CI 0.84 to 6.30; I2 = 0%; 4 studies, 470 participants; Analysis 1.9); or
weight gain in kilograms (MD 2.35, 95% CI 0.73 to 3.97; I2 = NA; 1 study, 23 participants; Analysis 1.10).
1.10. Analysis.

Comparison 1: Atypical antipsychotic vs placebo, Outcome 10: Adverse effects: metabolic (continuous)
We could not include data from one study in the analysis because it did not report data for both groups, and described weight gain by change in BMI (Malone 2010). In addition, we could not include data from Owen 2009 and the three datasets from Marcus 2009 because the data were skewed. Further details can be found in Table 11.
7. Atypical antipsychotics versus placebo: adverse effects data that could not be used in the meta‐analyses.
| Study name | Short‐/medium‐/long‐term outcomes | Group 1 | Group 2 | Group 1 sample size | Group 2 sample size | Group 1 results Mean (standard deviation) | Group 2 results Mean (standard deviation) | Other data | Notes |
| Malone 2001 | Short‐term weight gain | Olanzapine 2.5‐2 mg/day | Placebo | Not described. 33 in total | Not described. 33 in total | Not outlined for each group. Weight gain was
described as change in BMI category from baseline
to endpoint and summarised as a group BMI
change. AEs were measured at baseline and after week 12 (not after blinded phase) |
Not outlined for each group. See Group 1 | At baseline, 70.3% of children were at a healthy weight, 21.6% were overweight, 2.7% were obese, and 5.4% were underweight. By week 12, 42.4% were healthy weight, 21.2% were overweight, and 36.4% were obese. | |
| Marcus 2009 | Short‐term weight gain (kg) | Aripiprazole 5 mg/day | Placebo | 44 | 13 | 1.5 (2.65) | 0.4 (1.85) | "All aripiprazole treatment groups were associated with significantly greater change in weight compared with the placebo at endpoint. Aripiprazole 5 mg/day and aripiprazole 15 mg/day were associated with a greater prevalence of clinically significant weight gain than the placebo, and aripiprazole 15 mg/day was also associated with significantly greater increases in body mass index than the placebo" | Skewed |
| Aripiprazole 10 mg/day | Placebo | 49 | 13 | 1.4 (2.1) | 0.4 (1.85) | ||||
| Aripiprazole 15 mg/day | Placebo | 47 | 13 | 1.6 (2.06) | 0.4 (1.85) | ||||
| Owen 2009 | Short‐term weight gain (kg) | Aripiprazole (2‐15 mg/day) |
Placebo | 47 | 50 | 2.0 (12.15) | 0.8 (12.15) | "Aripiprazole treatment was associated with significantly greater mean weight change compared with placebo at endpoint (LOCF: 2.0 vs 0.8 kg (P .005); observed case: 1.9 vs 0.5 kg (P .01)). Aripiprazole was also associated with a greater incidence of clinically significant weight gain (>7% increase from baseline) than placebo (LOCF: 28.9% vs 6.1%; P.01)" | Skewed |
| AE: adverse effect; BMI: body mass index; LOCF: Last observation carried forward | |||||||||
As there were more than 10 studies in this analysis, we created a funnel plot for this outcome but found no evidence of asymmetry (Figure 6).
6.

log: logarithm; SE: standard error; RR: risk ratio
Atypical antipsychotics versus placebo (8 studies, 702 participants; Analysis 1.9)
Musculoskeletal
In the one study with 100 participants that compared atypical antipsychotics and placebo (Analysis 1.11), there was no difference in:
1.11. Analysis.

Comparison 1: Atypical antipsychotic vs placebo, Outcome 11: Adverse effects: musculoskeletal
rigidity (RR 5.20, 95% CI 0.63 to 42.96; low‐certainty evidence);
movement disorder (RR 5.50, 95% CI 0.27 to 111.14; low‐certainty evidence); or
dyskinesia (RR 2.08, 95% CI 0.55 to 7.87; low‐certainty evidence).
Neurological
A number of neurological AEs may be more likely to be reported in participants receiving atypical antipsychotics compared with placebo (Analysis 1.12). These were:
1.12. Analysis.

Comparison 1: Atypical antipsychotic vs placebo, Outcome 12: Adverse effects: neurological
dizziness (RR 4.19, 95% CI 1.10 to 16.00; I2 = 0%; 2 studies, 139 participants, low‐certainty evidence);
fatigue (RR 2.58, 95% CI 1.68 to 3.97; I2 = 0%; 8 studies, 881 participants; low‐certainty evidence);
sedation (RR 2.98, 95% CI 1.15 to 7.73; I2 = 21%; 5 studies, 366 participants; low‐certainty evidence);
somnolence (RR 4.84, 95% CI 3.18 to 7.36; I2 = 0%; 9 studies, 869 participants, low‐certainty evidence); and
tremor (RR 5.99, 95% CI 1.87 to 19.19; I2 = 0%; 5 studies, 574 participants; low‐certainty evidence).
There was no clear evidence of a difference between atypical antipsychotics and placebo groups in:
agitation/excitation (RR 0.46, 95% CI 0.13 to 1.62; I2 = 0%; 2 studies, 97 participants);
aggression (dichotomous) (RR 0.34, 95% CI 0.12 to 0.98; I2 = 0%; 4 studies, 461 participants);
apathy (RR 10.73, 95% CI 0.61 to 187.79; P = 0.10; I2 = NA; 1 study, 79 participants);
drowsiness (RR 4.26, 95% CI 0.95 to 19.02; P = 0.06; I2 = NA; 1 study, 97 participants);
extrapyramidal disorder (RR 7.83, 95% CI 0.47 to 130.01; P = 0.15; I2 = NA; 1 study, 216 participants);
hypersomnia (RR 2.67, 95% CI 0.43 to 16.52; I2 = 0%; 2 studies, 282 participants);
insomnia (RR 0.72, 95% CI 0.50 to 1.04; I2 = 0%; 7 studies, 679 participants);
presyncope (RR 0.94, 95% CI 0.04 to 22.72; I2 = NA; 1 study, 216 participants);
headache (RR 1.17, 95% CI 0.63 to 2.15; I2 = 9%; 6 studies, 597 participants);
lethargy (RR 6.58, 95% CI 0.39 to 110.35; I2 = NA; 1 study, 216 participants);
hyperactivity (RR 0.47, 95% CI 0.13 to 1.70; I2 = 0%; 3 studies, 305 participants); and
restlessness (akathisia) (RR 0.99, 95% CI 0.40 to 2.43; I2 = 1%; 4 studies, 531 participants).
As there were more than 10 studies in this analysis, we created a funnel plot for this outcome but found no evidence of asymmetry (Figure 7).
7.

log: logarithm; RR: risk ratio; SE: standard error; SMD: standardised mean difference
Atypical antipsychotics versus placebo (11 studies, 974 participants; Analysis 1.12)
Psychological
There was no clear evidence of a difference between atypical antipsychotic and placebo groups in
anxiety (RR 1.34, 95% CI 0.65 to 2.76; I2 = 0%; 2 studies, 139 participants; very low‐certainty evidence); or
depression (RR 3.86, 95% CI 0.46 to 32.60; I2 = 0%; 2 studies, 79 participants; very low‐certainty evidence; Analysis 1.13).
1.13. Analysis.

Comparison 1: Atypical antipsychotic vs placebo, Outcome 13: Adverse effects: psychological
Respiratory
There was no clear evidence of a difference between the atypical antipsychotic and placebo groups in the respiratory symptoms of:
ear infection (RR 5.63, 95% CI 0.28 to 112.84; I2 = NA; 1 study, 66 participants);
epistaxis (RR 5.63, 95% CI 0.28 to 112.84; I2 = NA; 1 study, 66 participants);
nasal congestion (RR 2.39, 95% CI 0.52 to 11.00; I2 = 0%; 2 studies, 313 participants);
nasopharyngitis (RR 1.26, 95% CI 0.73 to 2.17; I2 = 0%; 6 studies, 702 participants);
pharyngolaryngeal pain (RR 0.31, 95% CI 0.06 to 1.48; I2 = NA; 1 study, 216 participants); or
rhinitis (RR 2.68, 95% CI 0.93 to 7.71; I2 = NA; 1 study, 79 participants).
However, there was a higher rate of upper respiratory tract infection in the antipsychotic group (RR 2.15, 95% CI 1.08 to 4.27; I2 = 8%; 6 studies, 640 participants; Analysis 1.14).
1.14. Analysis.

Comparison 1: Atypical antipsychotic vs placebo, Outcome 14: Adverse effects: respiratory
Skin
There was no clear evidence of a difference between groups in the likelihood of:
bruise (RR 0.32, 95% CI 0.03 to 2.96; I2 = NA; 1 study, 92 participants); or
rash (RR 0.79, 95% CI 0.14 to 4.62; I2 = 0%; 2 studies, 228 participants; Analysis 1.15).
1.15. Analysis.

Comparison 1: Atypical antipsychotic vs placebo, Outcome 15: Adverse effects: skin
Urinary
Enuresis was not different between the atypical antipsychotic and placebo groups (RR 1.12, 95% CI 0.67 to 1.86; I2 = 0%; 6 studies, 552 participants; Analysis 1.16).
1.16. Analysis.

Comparison 1: Atypical antipsychotic vs placebo, Outcome 16: Adverse effects: urinary
Other adverse effects
No other AEs were reported.
Secondary outcomes
Quality of life
Child, adolescent or adult with autism
Quality of life was not different at endpoint in participants receiving aripiprazole compared to those receiving placebo (SMD 0.95, 95% CI 0.14 to 1.76; I2 = 75%; 2 studies, 135 participants; Analysis 1.17).
1.17. Analysis.

Comparison 1: Atypical antipsychotic vs placebo, Outcome 17: Quality of life
We could not include two of the quality‐of‐life datasets (5 mg/day and 10 mg/day) from Marcus 2009 in the meta‐analysis because the data were skewed. Details can be found in Table 12.
8. Atypical antipsychotics versus placebo: quality‐of‐life results that could not be used in the meta‐analyses.
| Study name | Short‐/medium‐/long‐term outcomes | Group 1 | Group 2 | Group 1 sample size | Group 2 sample size | Group 1 results Mean (standard deviation) | Group 2 results Mean (standard deviation) | Other data | Notes |
| Marcus 2009 | Short‐term QoL | Aripiprazole 5 mg/day | Placebo | 43 | 12 | 14 (15.74) | 10.6 (15.82) | ‐ | "Although patients receiving aripiprazole 5 and 10 mg/day had improvement in these 3 (QoL) scale scores compared with those receiving placebo, the 95% CIs of the treatment differences included zero" |
| Aripiprazole 10 mg/day | Placebo | 41 | 12 | 10.4 (15.4) | 10.6 (15.82) | ‐ | |||
| QoL: Quality of Life | |||||||||
Tolerability/acceptability
Participants were less likely to be lost to follow‐up in the antipsychotic group than the placebo group (RR 0.54, 95% CI 0.41 to 0.71; I2 = 12%; 13 studies, 1004 participants; Analysis 1.18).
1.18. Analysis.

Comparison 1: Atypical antipsychotic vs placebo, Outcome 18: Tolerability/acceptability: loss to follow‐up
Apart from one study, all studies involved children and adolescents, and therefore, we could not conduct a subgroup analysis of differences in tolerability based on age.
Neurohormones versus placebo
Primary outcomes
Challenging behaviours
Irritability
At short‐term follow‐up, there was some evidence that neurohormones may have a minimal to no effect on irritability (SMD −0.18, 95% CI −0.37 to −0.00; I2 = 0%; 8 studies, 466 participants; low‐certainty evidence; Analysis 2.1).
2.1. Analysis.

Comparison 2: Neurohormone versus placebo, Outcome 1: Irritability
There were no differences between types of neurohormones (P = 0.54) or when male participants were compared to a mixed population of male and female participants (P = 0.94). There was insufficient information to conduct subgroup analyses of irritability by communication ability or cognitive ability.
We could not include data from three studies in the analysis because the data were skewed (Levy 2003; Squassante 2018; Unis 2002). Details can be found in Table 13.
9. Neurohormones versus placebo: irritability results that could not be used in the meta‐analyses.
| Study name | Short‐/medium‐/long‐term outcomes | Group 1 sample size | Group 2 sample size | Group 1 results Mean (standard deviation) | Group 2 results Mean (standard deviation) | Other data | Notes |
| Levy 2003 | Short‐term (single‐dose secretin (2 CU/kg)) | 31 | 31 | 0.01 (1.35) | −0.18 (0.79) | ‐ | Skewed |
| Squassante 2018 | Short‐term balovaptan 1.5 mg | 32 | 23 | −1.99 (14.92) | −2.85 (24.29) | ‐ | Skewed |
| Short‐term balovaptan 4 mg | 77 | 22 | −1.64 (24.15) | −1.07 (4.95) | |||
| Short‐term balovaptan 10 mg | 39 | 22 | −3.42 (34.79) | −2.99 (9.49) | |||
| Unis 2002 | Short‐term synthetic secretin (single infusion of 0.4 μg/kg) | 23 | 15 | −1.3 (3.93) | −1.5 (3.38) | ‐ | Skewed |
Please refer to Table 2 for further information.
Self‐injury
There was no clear evidence of a difference in self‐injury between participants receiving neurohormones compared to those receiving placebo at endpoint (SMD −0.37, 95% CI −0.93 to 0.19; I2 = NA; 1 study, 50 participants; Analysis 2.2) and at three‐month follow‐up (SMD −0.32, 95% CI −0.88 to 0.23; I2 = NA; 1 study, 50 participants; Analysis 2.2).
2.2. Analysis.

Comparison 2: Neurohormone versus placebo, Outcome 2: Self‐injury
We could not include data from one study in the analysis because the data were skewed (Guastella 2015a). Details can be found in Table 14.
10. Neurohormones versus placebo: adverse effects data that could not be used in the meta‐analysis.
| Name of study | Short‐/medium‐/long‐term outcomes | Group 1 sample size | Group 1 sample size | Group 1 results Mean (standard deviation) | Group 2 results Mean (standard deviation) | Other data | Notes |
| Sikich 2013 | Short‐term oxytocin (max 24 IU children 3‐10 years or max 32 IU children 11‐17 years) adverse effects (metabolic) | 11 | 13 | 0.64 (1.95) | 1.09 (1.14) | ‐ | Skewed |
Adverse effects
Cardiovascular
There was no clear evidence of a difference between participants receiving neurohormones compared to those receiving placebo in the likelihood of:
cardiac disorders (RR 1.45, 95% CI 0.23 to 9.05; I2 = 0%; 3 studies, 456 participants);
palpitations (RR 2.96, 95% CI 0.12 to 72.04; I2 = NA; 1 study, 290 participants); or
vascular disorders (RR 1.00, 95% CI 0.06 to 15.57; I2 = NA; 1 study, 106 participants Analysis 2.3).
2.3. Analysis.

Comparison 2: Neurohormone versus placebo, Outcome 3: Adverse effects: cardiovascular
Gastrointestinal
Only vomiting showed a difference between groups when oxytocin was compared to a placebo (RR 0.45, 95% CI 0.21 to 0.97; I2 = 0%; 4 studies, 409 participants, low‐certainty evidence; Analysis 2.4).
2.4. Analysis.

Comparison 2: Neurohormone versus placebo, Outcome 4: Adverse effects: gastrointestinal
There was no clear evidence of differences between the neurohormone and placebo groups in any of the other gastrointestinal AEs:
abdominal pain or discomfort (RR 0.42, 95% CI 0.17 to 1.07; I2 = NA; 1 study, 290 participants);
constipation (RR 0.89, 95% CI 0.46 to 1.73; 3 studies, 361 participants);
diarrhoea (RR 0.71, 95% CI 0.39 to 1.28; I2 = 0%; 5 studies, 450 participants);
dry mouth (RR 0.43, 95% CI 0.06 to 2.88; I2 = 0%; 2 studies, 350 participants);
encopresis (RR 0.74, 95% CI 0.17 to 3.25, I2 = NA; 1 study, 290 participants);
gastrointestinal disorders (RR 1.25, 95% CI 0.35 to 4.49; I2 = 0%; 2 studies, 166 participants);
nausea (RR 0.14, 95% CI 0.01 to 2.65; I2 = NA; 1 study, 60 participants);
salivary hypersecretion (RR 0.32, 95% CI 0.03 to 2.99; I2 = 0%; 2 studies 319 participants); and
stomatitis (RR 0.13, 95% CI 0.02 to 1.11; I2 = 0%; 2 studies, 321 participants, low‐certainty evidence Analysis 2.4).
Immune system
Infections and infestations were not different between groups (RR 2.00, 95% CI 0.81 to 4.93; I2 = NA; 1 study, 106 participants; Analysis 2.5).
2.5. Analysis.

Comparison 2: Neurohormone versus placebo, Outcome 5: Adverse effects: immune system
Metabolic
There was no clear evidence of a difference between neurohormone and placebo groups in any of the metabolic AEs. These included:
decreased appetite (RR 0.67, 95% CI 0.37 to 1.22; I2 = 0%; 4 studies, 409 participants; very low‐certainty evidence);
increased appetite (RR 1.74, 95% CI 0.96 to 3.16; I2 = 0%; 2 studies, 350 participants);
metabolism and nutrition disorders (RR 0.50, 95% CI 0.05 to 5.35; I2 = NA; 1 study, 106 participants; very low‐certainty evidence);
thirst (RR 1.42, 95% CI 0.35 to 5.67; I2 = 15%; 2 studies, 319 participants);
weight gain (RR 1.21, 95% CI 0.52 to 2.82; I2 = NA; 1 study, 290 participants);
weight change (RR ‐0.45, 95% CI ‐1.76 to 0.86; I2 = NA; 1 study, 24 participants) or
weight loss (RR 1.97, 95% CI 0.69 to 5.63; I2 = NA; 1 study, 290 participants; Analysis 2.6).
2.6. Analysis.

Comparison 2: Neurohormone versus placebo, Outcome 6: Adverse effects: metabolic (dichotomous)
We could not include one study in the analysis because the data were skewed (Sikich 2013). Details can be found in Table 14.
There was no clear evidence of a difference between neurohormones and placebo groups in mean change in weight in kilograms (SMD −0.45; 95% CI −1.76 to 0.86; 1 study, 24 participants; Analysis 2.7).
2.7. Analysis.

Comparison 2: Neurohormone versus placebo, Outcome 7: Adverse effects: metabolic (continuous)
Musculoskeletal
There was no difference between participants receiving neurohormones and those receiving placebo in:
muscle spasms (RR 2.81, 95% CI 0.12 to 63.83; I2 = NA; 1 study, 29 participants; very low‐certainty evidence);
musculoskeletal and connective tissue disorders (RR 3.00, 95% CI 0.12 to 72.02; I2 = NA; 1 study, 106 participants); and
rhabdomyolysis (RR 1.47, 95% CI 0.06 to 35.64; I2 = NA; 1 study, 220 participants); Analysis 2.8.
2.8. Analysis.

Comparison 2: Neurohormone versus placebo, Outcome 8: Adverse effects: musculoskeletal
Neurological
Numerous neurological AEs were reported in studies comparing neurohormones to placebo. We found low‐certainty evidence that neurohormones may decrease the risk of headaches (RR 0.58, 95% CI 0.38 to 0.89; I2 = 0%; 7 studies, 689 participants; Analysis 2.9).
2.9. Analysis.

Comparison 2: Neurohormone versus placebo, Outcome 9: Adverse effects: neurological
The other neurological AEs showed no differences between the groups and included:
absence seizures (RR 2.73, 95% CI 0.12 to 59.57; 1 study, 19 participants);
agitation (RR 1.12, 95% CI 0.65 to 1.94; I² = 0%; 3 studies, 344 participants; low‐certainty evidence);
aggression (dichotomous) (RR 0.91, 95% CI 0.57 to 1.44; I² = 9%; 3 studies, 356 participants; low‐certainty evidence);
decreased attention (RR 1.46, 95% CI 0.24 to 8.84; 3 studies, 108 participants);
dizziness (RR 0.65, 95% CI 0.08 to 5.27; I² = 44%; 3 studies, 369 participants; low‐certainty evidence);
excessive talking (RR 2.81, 95% CI 0.12 to 63.83; 1 study, 29 participants, low‐certainty evidence);
fatigue (RR 0.91, 95% CI 0.50 to 1.65; I2 = 0%; 3 studies, 120 participants; low‐certainty evidence);
insomnia (RR 0.72, 95% CI 0.50 to 1.04; I2 = 0%; 6 studies, 477 participants; low‐certainty evidence);
irritability (dichotomous) (RR 0.86, 95% CI 0.68 to 1.10; I2 = 0%; 6 studies, 655 participants);
leg shaking (RR 2.73, 95% CI 0.12 to 59.57; I2 = NA; 1 study, 19 participants; low‐certainty evidence);
nervous system disorders (RR 1.67, 95% CI 0.42 to 6.62; I2 = NA; 1 study, 106 participants);
oppositional behaviour (RR 0.72, 95% CI 0.14 to 3.61; I2 = NA; 1 study, 25 participants; low‐certainty evidence);
restlessness (RR 1.64, 95% CI 0.17 to 15.47; I² = 51%; 2 studies, 319 participants; low‐certainty evidence);
seizure (RR 2.81, 95% CI 0.12 to 63.83; I2 = NA; 1 study 29 participants; low‐certainty evidence);
sedation (RR 1.69, 95% CI 0.87 to 3.27; I2 = 0%; 2 studies, 350 participants; low‐certainty evidence);
somnolence (RR 3.81, 95% CI 0.44 to 32.96; I2 = 0%; 2 studies, 89 participants; low‐certainty evidence); or
tics (RR 0.63, 95% CI 0.16 to 2.38; I2 = 0%; 2 studies, 309 participants; low‐certainty evidence; Analysis 2.9).
As there were more than 10 studies in this analysis, we created a funnel plot for this outcome but found no evidence of asymmetry (Figure 8).
8.

log: logarithm; RR: risk ratio; SE: standard error; SMD: standardised mean difference
Neurohormone versus placebo (10 studies, 863 participants; Analysis 2.9)
Psychological
The psychological outcomes were not different between those receiving neurohormones and those receiving placebo. These included:
anxiety (RR 3.05, 95% CI 0.50 to 18.55; I2 = 0%; 2 studies, 97 participants);
depression (RR 0.89, 95% CI 0.29 to 2.68; I2 = 0%; 4 studies, 427 participants);
panic attack (RR 0.30, 95% CI 0.01 to 6.62; I2 = NA; 1 study, 19 participants);
psychiatric (RR 4.00, 95% CI 0.46 to 34.61; I2 = NA; 1 study, 106 participants); and
self‐injury (dichotomous) (RR 1.00, 95% CI 0.11 to 9.35; 2 studies, 118 participants; I2 = 0%; Analysis 2.10).
2.10. Analysis.

Comparison 2: Neurohormone versus placebo, Outcome 10: Adverse effects: psychological
Respiratory
There was no clear evidence of a difference between neurohormone and placebo groups in respiratory symptoms. These included:
cold symptoms (RR 0.65, 95% CI 0.26 to 1.65; ² = 0%; 2 studies, 73 participants);
cough (RR 1.35, 95% CI 0.81 to 2.25; I2 = 0%; 5 studies, 430 participants;);
croup (RR 3.23, 95% CI 0.14 to 72.46; I2 = NA; 1 study, 25 participants);
epistaxis (RR 1.21, 95% CI 0.63 to 2.31; I2 = 0%; 3 studies, 379 participants);
nasal congestion (RR 0.79, 95% CI 0.59 to 1.05; I2 = 0%; 5 studies, 468 participants);
nasal irritation/runny nose (RR 0.55, 95% CI 0.10 to 2.92; I2 = NA; 1 study, 40 participants);
nasopharyngitis (RR 0.93, 95% CI 0.15 to 5.76; I2 = NA; 1 study, 29 participants);
respiratory, thoracic and mediastinal disorders (RR 0.49, 95% CI 0.09 to 2.56; I² = 0%; 2 studies, 147 participants);
sinusitis (RR 0.47, 95% CI 0.05 to 4.60; I2 = NA; 1 study, 29 participants);
upper respiratory tract infection (RR 1.10, 95% CI 0.35 to 3.47; I2 = 0%; 2 studies, 273 participants; Analysis 2.11).
2.11. Analysis.

Comparison 2: Neurohormone versus placebo, Outcome 11: Adverse effects: respiratory
Skin
There was no clear evidence of a difference in the neurohormone group compared to placebo in:
general/systemic disorders and administration site conditions (RR 4.00, 95% CI 0.46 to 34.61; I2 = NA; 1 study, 106 participants); or
rash (RR 1.12, 95% CI 0.63 to 1.97; I2 = 0%; 4 studies, 416 participants; Analysis 2.12).
2.12. Analysis.

Comparison 2: Neurohormone versus placebo, Outcome 12: Adverse effects: skin
Urinary
There was no difference between the neurohormone group and the placebo group in renal and urinary disorders (RR 3.00, 95% CI 0.12 to 72.02; I2 = NA; 1 study, 106 participants). However, neurohormones (oxytocin) showed a reduced risk of enuresis when compared to placebo (RR 0.18, 95% CI 0.06 to 0.62; I2 = NA; 1 study, 290 participants; Analysis 2.13).
2.13. Analysis.

Comparison 2: Neurohormone versus placebo, Outcome 13: Adverse effects: urinary
Other adverse effects
There was no clear evidence of a difference in the neurohormone group compared to placebo in:
injury, poisoning, and procedural complications (RR 3.00, 95% CI 0.12 to 72.02; I2 = NA; 1 study, 106 participants);
investigations (RR 0.50, 95% CI 0.05 to 5.35; I2 = NA; 1 study, 106 participants);
lymphadenopathy (RR 0.33, 95% CI 0.01 to 7.87; I2 = NA; 1 study, 60 participants);
neoplasms benign, malignant, and unspecified (RR 3.00, 95% CI 0.12 to 72.02; I2 = NA; 1 study, 106 participants); or
increased troponin 1 (RR 1.47, 95% CI 0.06 to 35.64; I2 = NA; 1 study, 220 participants, Analysis 2.14).
2.14. Analysis.

Comparison 2: Neurohormone versus placebo, Outcome 14: Adverse effects: other
Please refer to Table 2 for further information.
Secondary outcomes
Quality of life
There was no clear evidence of a difference in quality of life between neurohormone and placebo groups in the short term (SMD 0.70, 95% CI −0.12 to 1.53; P = 0.001, I² = 81%; 4 studies, 191 participants; Analysis 2.15).
2.15. Analysis.

Comparison 2: Neurohormone versus placebo, Outcome 15: Quality of life
We were unable to include data from five studies because the data were skewed (Bernaerts 2020; Jacob 2022; NCT01908205; NCT02940574; Squassante 2018). Details can be found in Table 15
11. Neurohormones versus placebo: quality‐of‐life results that could not be used in the meta‐analyses.
| Study name | Short‐/medium‐/long‐term outcomes | Group 1 sample size | Group 2 sample size | Results Group 1 Mean (standard deviation) | Results Group 2 Mean (standard deviation) | Other data | Notes |
| Bernaerts 2020 | Short‐term oxytocin (24 IU once daily) | 22 | 17 | 1.77 (8.04) | ‐1.35 (6.74) | ‐ | Skewed |
| Jacob 2022 | Short‐term balovaptan (10 mg once daily) | 106 | 92 | 8.0 (13.7) | 6.0 (11.6) | ‐ | Skewed |
| NCT01908205 (2013) | Short‐term oxytocin (twice daily dose of max 24 IUs) | 25 | 29 | 14.2 (17.4) | 7.6 (21.3) | ‐ | Skewed |
| NCT02940574 (2016) | Short‐term oxytocin (24 IU once daily) | 22 | 17 | 1.14 (5.48) | 0.35 (4.53) | ‐ | Skewed |
| Squassante 2018 | Short‐term balovaptan (1.5 mg) | 26 | 22 | 2.0 (13.7) | 3.9 (13.0) | ‐ | Skewed |
| Short‐term balovaptan (4 mg) | 69 | 22 | 6.2 (10.8) | 3.9 (13) | ‐ | ||
| Short‐term balovaptan (10 mg) | 30 | 23 | 9.8 (10.0) | 3.98 (13.0) | ‐ |
Tolerability/acceptability
There was no clear evidence of a difference in loss to follow‐up between neurohormone and placebo groups (RR 1.10, 95% CI 0.87 to 1.40; I2 = 0%; 14 studies, 1312 participants; Analysis 2.16).
2.16. Analysis.

Comparison 2: Neurohormone versus placebo, Outcome 16: Tolerability/acceptability: loss to follow‐up
Outcomes not reported
No data were available for the outcome of aggression.
Comparison 3: ADHD‐related medications versus placebo
Primary outcomes
Challenging behaviours
Irritability
ADHD‐related medications may reduce irritability in the short term when compared to placebo (SMD −0.20, 95% CI −0.40 to −0.01; 10 studies, 400 participants; P = 0.86, I2 = 0%; low‐certainty evidence; Analysis 3.1). Please refer to Table 3 for further information.
3.1. Analysis.

Comparison 3: ADHD‐related medications vs placebo, Outcome 1: Irritability
There was no difference between groups when we compared stimulant to non‐stimulant ADHD‐related medication (P = 0.33), when we compared children only to children and adults (P = 0.74) and when we compared male participants to a mixed male and female sample (P = 0.58). There was insufficient information to conduct subgroup analyses of irritability by communication ability or cognitive ability.
Self‐injury
At short‐term follow‐up, there was no clear evidence that ADHD‐related medications have an effect on self‐injurious behaviour (SMD −0.62; 95% CI −1.63 to 0.39, I2 = NA; 1 study, 16 participants, very low‐certainty evidence; Analysis 3.2). Please refer to Table 3 for further information.
3.2. Analysis.

Comparison 3: ADHD‐related medications vs placebo, Outcome 2: Self‐injury
There was only one study, so we could not conduct a subgroup analysis.
Adverse effects
Cardiovascular
There was no clear evidence of a difference between groups in ADHD‐related medications AEs (bradycardia and tachycardia) (RR 0.64, 95% CI 0.16 to 2.54; 2 studies, 114 participants). There was no difference between the ADHD‐related medication and placebo groups in the likelihood of:
bradycardia (RR 0.36, 95% CI 0.09 to 1.37; I2 = NA; 1 study, 66 participants), or
tachycardia (RR 3.52, 95% CI 0.44 to 27.85; I2 = 0%; 2 studies, 48 participants; Analysis 3.3).
3.3. Analysis.

Comparison 3: ADHD‐related medications vs placebo, Outcome 3: Adverse effects: cardiovascular
Gastrointestinal
When ADHD‐related medications were compared to placebo (Analysis 3.4) there was no clear evidence of a difference in the gastrointestinal side effects of:
3.4. Analysis.

Comparison 3: ADHD‐related medications vs placebo, Outcome 4: Adverse effects: gastrointestinal
diarrhoea (RR 0.81, 95% CI 0.46 to 1.40; I2 = 0%; 6 studies, 426 participants);
stomach ache (RR 2.58, 95% CI 1.10 to 6.06; I2 = 0%; 2 studies, 86 participants; Analysis 3.4); or
vomiting (RR 1.35, 95% CI 0.81 to 2.25; I2 = 0%; 4 studies, 347 participants).
However, ADHD‐related medications may increase the risk of:
constipation (RR 2.68, 95% CI 1.61 to 4.45; I2 = 0%; 5 studies, 220 participants);
dry mouth (RR 5.92, 95% CI 1.86 to 18.81; I2 = 0%; 3 studies, 102 participants);
nausea (RR 3.08, 95% CI 1.51 to 6.29; I2 = 0%; 5 studies, 239 participants), and
stomach or abdominal discomfort (RR 2.26, 95% CI 1.41 to 3.63; I2 = 0%; 6 studies, 504 participants).
Immune system
There was no clear evidence of differences between groups on the immune effects of:
fever (RR 0.27, 95% CI 0.06 to 1.27; I2 = 0%; 3 studies, 183 participants);
influenza (RR 7.14, 95% CI 0.38 to 134.69; I2 = NA; 1 study, 97 participants);
myalgia (RR 4.72, 95% CI 0.56 to 39.55; I2 = 0%; 2 studies, 115 participants); or
weakness (RR 3.20, 95% CI 0.35 to 29.10; I2 = NA; 1 study, 62 participants; Analysis 3.5).
3.5. Analysis.

Comparison 3: ADHD‐related medications vs placebo, Outcome 5: Adverse effects: immune system
Metabolic
ADHD‐related medications may increase the risk of decreased appetite when compared to placebo (RR 2.15, 95% CI 1.55 to 2.99; I2 = 0%; 9 studies, 511 participants; low‐certainty evidence; Analysis 3.6).
3.6. Analysis.

Comparison 3: ADHD‐related medications vs placebo, Outcome 6: Adverse effects: metabolic (dichotomous)
There were no clear differences between groups in:
increased appetite (RR 0.67, 95% CI 0.14 to 3.34; I2 = 0%; 2 studies, 121 participants; low‐certainty evidence); and
increased energy (RR 1.60, 95% CI 0.65 to 3.95; I2 = NA; 1 study, 62 participants; Analysis 3.6).
We were unable to include one study in the analysis because the data were skewed (Jaselskis 1992). Details can be found in Table 16.
12. ADHD versus placebo: adverse effects data that could not be used in the meta‐analyses.
| Study name | Short‐/medium‐/long‐term outcomes | Group 1 sample size | Group 2 sample size | Group 1 results Mean (standard deviation) | Group 2 results Mean (standard deviation) | Other data | Notes |
| Jaselskis 1992 | Short‐term adverse effects (increased
thirst) clonidine (0.15‐0.20 mg/day) |
8 | 8 | 0.5 (0.8) | 0.3 (0.5) | ‐ | Skewed |
| Short‐term adverse effects (appetite
change) clonidine (0.15‐0.20 mg/day) |
8 | 8 | 1.6 (2.1) | 0.6 (0.7) | |||
| Short‐term adverse effects (sleep
disturbance) clonidine (0.15‐0.20 mg/day) |
8 | 8 | 1.6 (2.7) | 1.4 (2.3) | |||
| Short‐term adverse effects (depression) clonidine (0.15‐0.20 mg/day) |
8 | 8 | 1.4 (2.0) | 1.3 (1.4) |
Neurological
Very uncertain evidence shows that ADHD‐related medications compared to placebo may increase:
drowsiness (RR 3.42, 95% CI 1.54 to 7.59; I2 = 20%; 4 studies, 186 participants; very low‐certainty evidence);
emotion/tearfulness (RR 6.32, 95% CI 2.47 to 16.18; I2 = 0%; 2 studies, 128 participants; very low‐certainty evidence);
fatigue (RR 3.73, 95% CI 1.98 to 7.03; I2 = 0%; 4 studies, 235 participants; very low‐certainty evidence);
headache (RR 1.63, 95% CI 1.09 to 2.44; I2 = 0%; 8 studies, 383 participants; very low‐certainty evidence);
insomnia (RR 1.58, 95% CI 1.01 to 2.47; I2 = 5%; 7 studies, 411 participants; very low‐certainty evidence);
irritability (dichotomous) (RR 1.61, 95% CI 1.25 to 2.07; I2 = 0%; 6 studies, 336 participants; very low‐certainty evidence; Analysis 3.7).
3.7. Analysis.

Comparison 3: ADHD‐related medications vs placebo, Outcome 7: Adverse effects: neurological (dichotomous)
There was no clear evidence (all very low‐certainty evidence) of differences between groups in:
agitation (RR 0.95, 95% CI 0.56 to 1.60; I2 = NA; 1 study, 128 participants);
aggression (dichotomous) (RR 0.95, 95% CI 0.58 to 1.53; I2 = 0%; 5 studies, 365 participants);
dizziness (RR 2.17, 95% CI 0.63 to 7.53; I2 = 0%; 3 studies, 175 participants);
hyperactivity (RR 0.68, 95% CI 0.06 to 7.20; I2 = 39%; 2 studies, 115 participants);
increased motor activity (RR 1.89, 95% CI 0.48 to 7.47; I2 = NA; 1 study, 66 participants);
motor tics (RR 2.33, 95% CI 0.51 to 10.69; I2 = 20%; 3 studies, 118 participants);
nightmares (RR 1.48, 95% CI 0.38 to 5.75; I2 = 0%; 2 studies, 122 participants);
repetitive behaviour (RR 1.59, 95% CI 0.74 to 3.39; I2 = 0%; 2 studies, 128 participants);
restlessness (RR 1.52, 95% CI 0.06 to 40.44; I2 = 71%; 2 studies, 76 participants);
sleep disturbance (RR 1.12, 95% CI 0.54 to 2.31; I2 = 0%; 2 studies, 84 participants);
talking excessively (RR 0.24, 95% CI 0.06 to 1.01, I2 = NA; 1 study, 62 participants);
waking (RR 1.60, 95% CI 0.29 to 8.92, I2 = NA; 1 study, 62 participants); and
tremor (RR 3.00, 95% CI 0.14 to 64.26; I2 = NA; 1 study, 16 participants; Analysis 3.7).
There was also no clear evidence of a difference in the continuous neurological AEs of:
drowsiness (SMD 4.80, 95% CI 0.55 to 9.05; I2 = NA; 1 study, 8 participants); and
decreased activity (SMD 2.00, 95% CI −2.66 to 6.66; I2 = NA; 1 study, 8 participants; Analysis 3.8).
3.8. Analysis.

Comparison 3: ADHD‐related medications vs placebo, Outcome 8: Adverse effects: neurological (continuous)
Psychological
ADHD‐related medications may increase the risk of depression in the ADHD‐related medication group when compared to placebo although the evidence is very uncertain (RR 2.45, 95% CI 1.12 to 5.36; I2 = 0%; 3 studies, 152 participants, very low‐certainty evidence).
There was no clear evidence of differences between groups in:
anxiety (RR 1.39, 95% CI 0.74 to 2.62; I2 = 10%; 5 studies, 252 participants);
mood change (RR 13.00, 95% CI 0.78 to 216.39; I2 = NA; 1 study, 40 participants);
self‐injury (dichotomous) (RR 1.67, 95% CI 0.78 to 3.58; I² = 0%; 3 studies, 188 participants; moderate‐certainty evidence);
'silly' behaviour (RR 0.64, 95% CI 0.17 to 2.45; I2 = NA; 1 study, 62 participants); or
social withdrawal (RR 2.28, 95% CI 0.39 to 13.37; 2 studies, 126 participants; I2 = 43%) Analysis 3.9.
3.9. Analysis.

Comparison 3: ADHD‐related medications vs placebo, Outcome 9: Adverse effects: psychological (dichotomous)
Respiratory
There was no clear evidence of a difference between groups in cough (RR 0.81, 95% CI 0.26 to 2.46; I2 = 0%; 2 studies, 122 participants; Analysis 3.10).
3.10. Analysis.

Comparison 3: ADHD‐related medications vs placebo, Outcome 10: Adverse effects: respiratory
Skin
There was no clear evidence of a difference in the likelihood of:
rash (RR 2.21, 95% CI 0.79 to 6.16; I2 = 14%; 3 studies, 102 participants); or
skin picking (RR 0.36, 95% CI 0.04 to 3.23; I2 = NA; 1 study, 62 participants; Analysis 3.11).
3.11. Analysis.

Comparison 3: ADHD‐related medications vs placebo, Outcome 11: Adverse effects: skin
Urinary
Enuresis was not different between groups (RR 0.81, 95% CI 0.19 to 3.55; P = 0.65, I2 = 0%; 2 studies, 122 participants; Analysis 3.12).
3.12. Analysis.

Comparison 3: ADHD‐related medications vs placebo, Outcome 12: Adverse effects: urinary
Secondary outcomes
Quality of life
There was no clear evidence of a difference between groups in quality of life (SMD 0.21. 95% CI −0.33 to 0.75; I2 = NA; 1 study, 54 participants; Analysis 3.13).
3.13. Analysis.

Comparison 3: ADHD‐related medications vs placebo, Outcome 13: Quality of life
Tolerability/acceptability
Follow‐up was not different in the ADHD‐related and placebo groups (RR 0.91, 95% CI 0.50 to 1.69; I2 = 7%; 9 studies, 380 participants; Analysis 3.14).
3.14. Analysis.

Comparison 3: ADHD‐related medications vs placebo, Outcome 14: Tolerability/acceptability: loss to follow‐up
Outcomes not reported
No data were available for the outcomes of aggression, musculoskeletal AEs, or other AEs.
Antidepressants versus placebo
Primary outcomes
Challenging behaviours
Irritability
There was no clear evidence of a difference in irritability in the short term when antidepressants were compared to placebo (SMD −0.06, 95% CI −0.30 to 0.18; I2 = 0%, 3 studies, 267 participants; low‐certainty evidence; Analysis 4.1). There were no clear differences between groups when we compared types of antidepressants (P = 0.76), or when we compared male participants to a mixed population of male and female participants (P = 0.67).
4.1. Analysis.

Comparison 4: Antidepressant vs placebo, Outcome 1: Irritability
We were unable to include data from five studies in the analysis because data were either not reported, reported without standard deviation, reported as median and range, or were skewed (Carminati 2016; Gordon 1993; Hollander 2012; NCT00183339; Remington 2001). Details of these studies can be found in Table 17.
13. Antidepressant versus placebo: irritability results that could not be used in the meta‐analyses.
|
Study name Short‐/medium‐/ long‐term outcomes |
Group 1 | Group 2 | Group 3 | Group 1 sample size | Group 2 sample size | Group 3 sample size | Group 1 results Mean (standard deviation) | Group 2 results Mean (standard deviation) | Group 3 results Mean (standard deviation) | Notes | |
| Carminati 2016 | Short‐term irritability | Venlafaxine (18.75 mg/day) | Placebo | NA | 6 | 7 | NA | Median 10 (range 0‐40) | Median 9 (range 5‐17) | NA | Results presented as median and range |
| Gordon 1993 | Short‐term irritabilty | Clomipromine mean dose 4.3 mg/kg/day | Placebo | NA | 24 | 12 | NA | ABC‐I data not reported | ABC‐I data not reported | NA | Data not reported |
| Hollander 2012 | Short‐term Irritability | Fluoxetine (max 80 mg/day) | Placebo | Fluoxetine | 22 | 15 | NA | Not reported | Not reported | NA | Irritability was an outcome; however, it was not reported |
| NCT00183339 | Medium‐term irritability | Fluoxetine (max 20 mg/day) | Placebo | NA | 8 | 10 | NA | ABC‐I ‐8.5 (10.6) |
ABC‐I ‐0.7 (2.9) |
NA | Skewed |
| Remington 2001 | Short‐term irritability | Clompramine (max 150 mg/day) | Haloperidol (max 150 mg/day) |
Placebo | 13 | 13 | 10 | Mean 16 | Mean 12 | 17.5 | Results presented graphically without SD |
| ABC‐I: Aberrant Behaviour Checklist ‐ Irritability; SD: standard deviation | |||||||||||
Aggression
We were unable to pool data from two studies because the data were reported as a median and range or not reported fully (Carminati 2016; McDougle 1996). Details of the studies can be found in Table 18.
14. Antidepressant versus placebo: aggression results that could not be used in the meta‐analyses.
| Study name | Short‐/ medium‐/ long‐term outcomes | Group 1 | Group 2 | Group 1 sample size | Group 2 sample size | Group 1 results | Group 2 results | Other data | Notes |
| Carminati 2016 | Short‐term aggression | Venlafaxine 18.75 mg/day | Placebo | 6 | 7 | Median 3.5 (range 0‐18) | Median 4 (range 1‐9) | ‐ | Only median and range provided |
| McDougle 1996 | Short‐term aggression | Fluvoxamine max 300 mg/day | Placebo | 15 | 15 | Not reported; only t scores and P value | Not reported; only t scores and P value | As measured by total score on the Brown Aggression Scale, fluvoxamine was superior to placebo in reducing aggression (F = 4.57; d = 3.84; P < 0.03). | ‐ |
Self‐injury
We were unable to include data from three studies in the analysis because the data were reported as median and range or the data were skewed (Carminati 2016; Mouti 2014; King 2009). Details can be found in Table 5.
Adverse effects
Cardiovascular
There was no clear evidence of a difference between antidepressants and placebo in the cardiovascular AEs of:
flushing (RR 2.00, 95% CI 0.24 to 16.61; I2 = NA; 1 study 12 participants); or
tachycardia (RR 2.67, 95% CI 0.31 to 23.25; I2 = 0%; 2 studies, 35 participants; Analysis 4.2).
4.2. Analysis.

Comparison 4: Antidepressant vs placebo, Outcome 2: Adverse effects: cardiovascular
Gastrointestinal
Antidepressants were no more likely to be associated with gastrointestinal AEs than placebo. These included:
constipation (RR 0.95, 95% CI 0.09 to 10.03; I2 = 61%; 2 studies, 70 participants);
diarrhoea (RR 0.94, 95% CI 0.33 to 2.64; I2 = 81%; 4 studies, 409 participants);
dry mouth (RR 2.00, 95% CI 0.24 to 16.61; I2 = NA; 1 study, 12 participants);
gastrointestinal disturbance (RR 1.41, 95% CI 0.97 to 2.05; I2 = 0%; 3 studies, 341 participants);
nausea/abdominal pain (RR 1.67, 95% CI 0.85 to 3.27; I² = 0%; 5 studies, 251 participants); and
vomiting (RR 1.49, 95% CI 0.76 to 2.92; I2 = 17%; 5 studies, 400 participants; Analysis 4.3).
4.3. Analysis.

Comparison 4: Antidepressant vs placebo, Outcome 3: Adverse effects: gastrointestinal
Immune system
There were no differences between participants receiving antidepressants and those receiving placebo in:
allergies (RR 1.42, 95% CI 0.70 to 2.88; I2 = NA; 1 study, 149 participants);
cold, flu or other systemic infection (RR 1.24, 95% CI 0.82 to 1.87; I2 = NA; 1 study, 149 participants); and
infections (RR 1.15, 95% CI 0.85 to 1.56; I2 = 0%; 3 studies, 472 participants; Analysis 4.4).
4.4. Analysis.

Comparison 4: Antidepressant vs placebo, Outcome 4: Adverse effect: immune system
Metabolic
There was no clear evidence of a difference between antidepressant and placebo groups for:
appetite disturbance (RR 0.55, 95% CI 0.14 to 2.23; I2 = NA; 1 study, 165 participants; very low‐certainty evidence);
decreased appetite (RR 1.35, 95% CI 0.68 to 2.69; I2 = 0%; 4 studies, 242 participants; very low‐certainty evidence);
increased appetite (RR 0.91, 95% CI 0.35 to 2.38; I2 = NA; 1 study, 149 participants; very low‐certainty evidence); or
weight gain (RR 1.47, 95% CI 0.08 to 27.39; I2 = 46%; 2 studies, 93 participants; very low‐certainty evidence; Analysis 4.5).
4.5. Analysis.
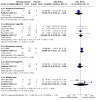
Comparison 4: Antidepressant vs placebo, Outcome 5: Adverse effects: metabolic
There may be higher levels of decreased energy (RR 1.94, 95% CI 1.13 to 3.33; P = 0.02; I2 = NA; 1 study, 149 participants, very low‐certainty evidence) in the antidepressant group although the evidence is very uncertain.
Musculoskeletal
There was no clear evidence of a difference between antidepressants and placebo in the musculoskeletal AEs of:
motor disturbance (RR 0.31, 95% CI 0.03 to 2.88; I2 = NA; 1 study, 165 participants; very low‐certainty evidence); or
neck pain (RR 2.09, 95% CI 0.09 to 48.04; I2 = NA; 1 study, 37 participants; Analysis 4.6).
4.6. Analysis.

Comparison 4: Antidepressant vs placebo, Outcome 6: Adverse effect: musculoskeletal
Neurological
There was no clear evidence of a difference between antidepressant and placebo groups in most of the reported neurological AEs (Analysis 4.7). These included:
4.7. Analysis.

Comparison 4: Antidepressant vs placebo, Outcome 7: Adverse effects: neurological
activation syndrome (RR 0.80, 95% CI 0.31 to 2.04; I2 = NA; 1 study, 159 participants);
agitation (RR 1.01, 95% CI 0.59 to 1.75; I2 = 40%; 2 studies, 197 participants; low‐certainty evidence);
aggression or hostility (dichotomous) (RR 1.07, 95% CI 0.59 to 1.95; I2 = 42%; 3 studies, 225 participants; low‐certainty evidence);
anger/irritability (dichotomous) (RR 1.31, 95% CI 0.75 to 2.29; I2 = 0%; 2 studies, 167 participants; low‐certainty evidence);
autonomic disturbance (RR 1.15, 95% CI 0.32 to 4.12; I2 = NA; 1 study, 165 participants; low‐certainty evidence);
central nervous system disturbance (RR 0.75, 95% CI 0.33 to 1.72; I2 = NA; 1 study, 165 participants; low‐certainty evidence);
diaphoresis (sweating) (RR 3.00, 95% CI 0.13 to 69.09; I2 = NA; 1 study, 36 participants; low‐certainty evidence);
drowsiness/fatigue (RR 1.25, 95% CI 0.65 to 2.41; I2 = 16%; 4 studies, 282 participants; low‐certainty evidence);
headache (RR 1.53, 95% CI 0.77 to 3.07; I2 = 0%; 3 studies, 244 participants; low‐certainty evidence);
hyperactivity (RR 1.93, 95% CI 0.47 to 7.82; I2 = 67%; 2 studies, 207 participants; low‐certainty evidence);
increased speech (RR 2.08, 95% CI 0.66 to 6.62; I2 = NA; 1 study, 149 participants; low‐certainty evidence);
insomnia (RR 1.19, 95% CI 0.87 to 1.63; I2 = 18%; 7 studies, 449 participants; low‐certainty evidence);
mood disturbance (RR 1.32, 95% CI 0.75 to 2.31; I2 = NA; 1 study, 165 participants; low‐certainty evidence);
mood lability (RR 0.69, 95% CI 0.27 to 1.74; I2 = 2%; 2 studies, 167 participants; low‐certainty evidence);
numbness (RR 2.09, 95% CI 0.09 to 48.04; I2 = NA; 1 study, 37 participants; low‐certainty evidence);
restlessness (RR 1.93, 95% CI 0.82 to 4.57; I2 = NA; 1 study, 149 participants; low‐certainty evidence);
sedation (RR 1.91, 95% CI 0.77 to 4.72; I2 = 0%; 3 studies, 117 participants; low‐certainty evidence);
sleep disturbance (RR 1.24, 95% CI 0.31 to 4.92; I2 = 75%; 2 studies, 223 participants; low‐certainty evidence);
tremor (RR 2.56, 95% CI 0.57 to 11.60; I2 = 0%; 3 studies, 85 participants; low‐certainty evidence);
twitching (RR 7.00, 95% CI 0.44 to 111.91; I2 = NA; 1 study, 12 participants; low‐certainty evidence); or
vertigo (RR 2.09, 95% CI 0.09 to 48.04; I2 = NA; 1 study, 37 participants; low‐certainty evidence).
There may be evidence of higher levels of decreased attention in the antidepressant group (RR 4.16, 95% CI 1.07 to 16.11; I2 = 0%; 2 studies, 207 participants; low‐certainty evidence; Analysis 4.7).
As there were more than 10 studies in this analysis, we created a funnel plot for this outcome (Figure 9) but found no evidence of asymmetry.
9.

log: logarithm; RR: risk ratio; SE: standard error; SMD: standardised mean difference
Antidepressant versus placebo (4 studies, 243 participants; Analysis 4.7)
Psychological
There was no clear evidence of a difference between antidepressant and placebo groups in the likelihood of:
anorexia (RR 1.58, 95% CI 0.53 to 4.74; I2 = NA; 1 study, 39 participants; very low‐certainty evidence);
anxiety/nervousness (RR 0.66, 95% CI 0.37 to 1.18; I2 = 0%; 2 studies, 188 participants; very low‐certainty evidence);
depression (RR 1.36, 95% CI 0.14 to 13.72; I2 = NA; 1 study, 37 participants; very low‐certainty evidence);
self‐injury (dichotomous) (RR 1.25, 95% CI 0.09 to 17.02; I2 = NA; 1 study, 18 participants, very low‐certainty evidence),
silliness (RR 0.94, 95% CI 0.40 to 2.17; I2 = NA; 1 study, 149 participants); very low‐certainty evidence;
suicidal ideation (RR 2.09, 95% CI 0.09 to 48.04; I2 = NA; 1 study, 37 participants; very low‐certainty evidence);
unstable mood (RR 0.81, 95% CI 0.32 to 2.06; I2 = NA; 1 study, 149 participants; very low‐certainty evidence);
verbal aggression (RR 0.23, 95% CI 0.01 to 5.34; I2 = NA; 1 study, 37 participants; very low‐certainty evidence); or
vivid or bad dreams (RR 4.87, 95% CI 0.27 to 87.94; I2 = NA; 1 study, 37 participants; very low‐certainty evidence).
There may be evidence in the antidepressant group of increased rates of:
impulsive/intrusive behaviour (RR 2.92, 95% CI 1.11 to 7.68; I2 = NA; 1 study, 149 participants; very low‐certainty evidence); and
stereotypy (RR 8.33, 95% CI 1.07 to 64.95; I2 = NA; 1 study, 149 participants; very low‐certainty evidence; Analysis 4.8)
4.8. Analysis.

Comparison 4: Antidepressant vs placebo, Outcome 8: Adverse effects: psychological
although the evidence is very uncertain.
As there were more than 10 studies in this analysis, we created a funnel plot for this outcome but found no evidence of asymmetry (Figure 10).
10.

log: logarithm; RR: risk ratio; SE: standard error; SMD: standardised mean difference
Antidepressant versus placebo (4 studies, 243 participants; Analysis 4.8)
Respiratory
There was no clear evidence of a difference between antidepressant and placebo groups in:
overall respiratory effects (RR 2.19, 95% CI 0.86 to 5.55; I2 = 0%; 2 studies, 314 participants);
upper respiratory infection (RR 0.98, 95% CI 0.73 to 1.31; I2 = 0%; 2 studies, 216 participants; or
cough (RR 1.67, 95% CI 0.52 to 5.39; 1 study, 18 participants; Analysis 4.9).
4.9. Analysis.

Comparison 4: Antidepressant vs placebo, Outcome 9: Adverse effects: respiratory
Skin
There was no clear evidence of a difference between antidepressant and placebo groups in the likelihood of rash or skin irritation (RR 1.00, 95% CI 0.36 to 2.78; I2 = 74%; 3 studies, 332 participants; Analysis 4.10).
4.10. Analysis.

Comparison 4: Antidepressant vs placebo, Outcome 10: Adverse effects: skin
Urinary
There was no clear evidence of a difference in:
enuresis (RR 3.13, 95% CI 0.81 to 12.06; I2 = NA; 1 study, 18 participants);
polyuria (RR 2.09, 95% CI 0.09 to 48.04; I2 = NA; 1 study, 37 participants); or
urinary tract infection (RR 0.60, 95% CI 0.21 to 1.73; I2 = NA; 1 study, 39 participants; Analysis 4.11).
4.11. Analysis.

Comparison 4: Antidepressant vs placebo, Outcome 11: Adverse effects: urinary
Other adverse effects
There was no clear evidence of a difference in:
salty taste (RR 2.09, 95% CI 0.09 to 48.04; I2 = NA; 1 study, 37 participants); or
mild trembling (RR 2.09, 95% CI 0.09 to 48.04; I2 = NA; 1 study, 37 participants; Analysis 4.12).
4.12. Analysis.

Comparison 4: Antidepressant vs placebo, Outcome 12: Adverse effects: other
Secondary outcomes
Tolerability/acceptability
Loss to follow‐up was not different in the antidepressant group compared to the placebo group (RR 1.22, 95% CI 0.93 to 1.59; I2 = 0%; 7 studies, 564 participants; Analysis 4.13).
4.13. Analysis.

Comparison 4: Antidepressant vs placebo, Outcome 13: Tolerability/acceptability: loss to follow‐up
Outcomes not reported
No data were available for the outcome of quality of life.
Atypical versus typical antipsychotics
Challenging behaviours
Irritability
There was no clear evidence of differences in irritability at endpoint when atypical antipsychotics were compared to typical antipsychotics (SMD −0.23, 95% CI −0.95 to 0.48; I2 = NA; 1 study, 30 participants; Analysis 5.1).
5.1. Analysis.

Comparison 5: Atypical vs typical antipsychotics, Outcome 1: Irritability
There were insufficient studies (1 study) to conduct subgroup analyses.
Adverse effects
Cardiovascular
There was no clear evidence of a difference between groups in tachycardia when atypical antipsychotics (olanzapine) were compared to typical antipsychotics (haloperidol) (RR 0.33, 95% CI 0.02 to 6.86; I2 = NA; 1 study 12 participants; Analysis 5.2).
5.2. Analysis.

Comparison 5: Atypical vs typical antipsychotics, Outcome 2: Adverse effects: cardiovascular (tachycardia)
Gastrointestinal
There was no clear evidence of differences in:
constipation (RR 1.00, 95% CI 0.24 to 4.18; I2 = NA; 1 study, 30 participants);
dry mouth (RR 1.00, 95% CI 0.08 to 12.56; I2 = NA; 1 study, 12 participants); or
nausea/vomiting (RR 5.00, 95% CI 0.29 to 86.43; I2 = NA; 1 study, 12 participants; Analysis 5.3).
5.3. Analysis.

Comparison 5: Atypical vs typical antipsychotics, Outcome 3: Adverse effects: gastrointestinal
Metabolic
There was no difference between atypical antipsychotics (olanzapine) compared to typical antipsychotics (haloperidol) in:
weight gain (RR 1.18, 95% CI 0.76 to 1.83; I2 = NA; 1 study, 12 participants); and
weight loss (RR 0.33, 95% CI 0.02 to 6.86; I2 = NA; 1 study, 12 participants; Analysis 5.4).
5.4. Analysis.

Comparison 5: Atypical vs typical antipsychotics, Outcome 4: Adverse effects: metabolic (dichotomous)
There was also no change in weight (SMD 0.26 kg, 95% CI −1.54 to 2.06; I2 = 83%; 2 studies, 42 participants; Analysis 5.5).
5.5. Analysis.

Comparison 5: Atypical vs typical antipsychotics, Outcome 5: Adverse effects: metabolic (continuous)
Neurological
There was no clear evidence of a difference between those receiving typical and atypical antipsychotics in the neurological AEs:
ataxia (RR 0.33, 95% CI 0.02 to 6.86; I2 = NA; 1 study, 12 participants);
blunted effect (RR 0.11, 95% CI 0.01 to 1.90; I2 = NA; 1 study, 30 participants);
insomnia (RR 3.00, 95% CI 0.15 to 61.74; I2 = NA; 1 study, 12 participants);
rigidity (RR 0.33, 95% CI 0.02 to 6.86; I2 = NA; 1 study, 12 participants); or
sedation (RR 2.50, 95% CI 0.76 to 8.19; I2 = NA; 1 study, 12 participants; Analysis 5.6).
5.6. Analysis.

Comparison 5: Atypical vs typical antipsychotics, Outcome 6: Adverse effects: neurological
Respiratory
There was no clear evidence of a difference between participants receiving typical (haloperidol) and atypical antipsychotics (risperidone) in the likelihood of respiratory tract infection (RR 0.88, 95% CI 0.43 to 1.80; 1 study, 30 participants; Analysis 5.7).
5.7. Analysis.

Comparison 5: Atypical vs typical antipsychotics, Outcome 7: Adverse effects: respiratory
Skin
There was no clear difference in rash between typical and atypical antipsychotic groups (RR 0.33, 95% CI 0.02 to 6.86; I2 = NA; 1 study, 12 participants; Analysis 5.8).
5.8. Analysis.

Comparison 5: Atypical vs typical antipsychotics, Outcome 8: Adverse effects: skin
Urinary
Enuresis was not different between groups (RR 1.00, 95% CI 0.29 to 3.48; I2 = 0%; 2 studies, 42 participants; Analysis 5.9).
5.9. Analysis.

Comparison 5: Atypical vs typical antipsychotics, Outcome 9: Adverse effects: urinary
Secondary outcomes
Tolerability/acceptability
There was no clear evidence of a difference between groups in follow‐up (RR 5.00, 95% CI 0.26 to 96.13; P = 0.29, I2 = 0%; 2 studies, 42 participants; Analysis 5.10).
5.10. Analysis.

Comparison 5: Atypical vs typical antipsychotics, Outcome 10: Tolerability/acceptability: loss to follow‐up
Outcomes not reported
No data were available for the outcomes of aggression, self‐injury and quality of life, or immune, musculoskeletal, psychological, or other AEs.
Atypical antipsychotics versus atypical antipsychotics
Primary outcomes
Challenging behaviours
Irritability
Compared to risperidone, there was evidence of an increased risk of irritability in the aripiprazole group at endpoint (SMD 0.40, 95% CI 0.02 to 0.78; P = 0.92, I2 = 0%; 2 studies, 110 participants; Analysis 6.1).
6.1. Analysis.

Comparison 6: Atypical vs atypical antipsychotics, Outcome 1: Irritability
There was insufficient information to conduct subgroup analyses of irritability by age, gender, communication ability, or cognitive ability.
Adverse effects
Cardiovascular
There was no clear evidence of a difference between different types of atypical antipsychotics in the likelihood of tachycardia (RR 1.07, 95% CI 0.16 to 7.04; I2 = 0%; 2 studies, 120 participants; Analysis 6.2).
6.2. Analysis.

Comparison 6: Atypical vs atypical antipsychotics, Outcome 2: Adverse effects: cardiovascular
Gastrointestinal
There was no clear evidence of differences between atypical antipsychotics in any of the gastrointestinal side effects:
abdominal pain (RR 3.10, 95% CI 0.34 to 28.15; 1 study, 59 participants);
constipation (RR 1.30, 95% CI 0.34 to 4.91; I2 = 0%; 2 studies, 120 participants);
diarrhoea (RR 3.10, 95% CI 0.13 to 73.14; 1 study, 59 participants);
drooling (RR 0.72, 95% CI 0.38 to 1.37; I2 = 0%; 2 studies, 120 participants);
dry mouth (RR 5.17, 95% CI 0.26 to 103.21; 1 study, 59 participants);
nausea (RR 0.52, 95% CI 0.05 to 5.40; 1 study, 59 participants); and
vomiting (RR 1.61, 95% CI 0.20 to 12.65; I2 = 0%; 2 studies, 120 participants; Analysis 6.3).
6.3. Analysis.

Comparison 6: Atypical vs atypical antipsychotics, Outcome 3: Adverse effects: gastrointestinal
Metabolic
There was no clear evidence of a difference between groups in:
decreased appetite (RR 1.67, 95% CI 0.56 to 4.96; I2 = 0%; 2 studies, 120 participants); and
increased appetite (RR 0.61, 95% CI 0.15 to 2.47; I2 = 30%; 2 studies, 120 participants).
However, there was a reduced risk of weight gain in the aripiprazole group when compared to risperidone (RR 0.37, 95% CI 0.19 to 0.70; 1 study, 61 participants; Analysis 6.4).
6.4. Analysis.

Comparison 6: Atypical vs atypical antipsychotics, Outcome 4: Adverse effects: metabolic
Musculoskeletal
There was no clear evidence of a difference between groups in muscle rigidity (RR 2.91, 95% CI 0.12 to 68.66; 1 study, 61 participants; Analysis 6.5).
6.5. Analysis.

Comparison 6: Atypical vs atypical antipsychotics, Outcome 5: Adverse effects: musculoskeletal
Neurological
There was no clear evidence of differences in neurological side effects including:
agitation (RR 4.84, 95% CI 0.24 to 96.89; 1 study, 61 participants);
difficulty sleeping (RR 6.78, 95% CI 0.37 to 125.95; 1 study, 61 participants);
dizziness (RR 0.73, 95% CI 0.10 to 5.39; I2 = 15%; 2 studies, 120 participants);
fatigue (RR 1.03, 95% CI 0.29 to 3.75; 1 study, 59 participants);
headache (RR 0.97, 95% CI 0.06 to 14.78; 1 study, 61 participants);
nausea (RR 2.91, 95% CI 0.12 to 68.66; 1 study, 61 participants);
nervousness (RR 2.07, 95% CI 0.20 to 21.60; 1 study, 59 participants);
restlessness (RR 0.44, 95% CI 0.07 to 2.88; I2 = 0%; 2 studies, 120 participants);
sedation (RR 3.39, 95% CI 0.76 to 15.02; 1 study, 61 participants);
somnolence (RR 8.72, 95% CI 0.49 to 155.27; 1 study, 61 participants); or
tremor (RR 1.55, 95% CI 0.28 to 8.62; 1 study, 59 participants; Analysis 6.6).
6.6. Analysis.

Comparison 6: Atypical vs atypical antipsychotics, Outcome 6: Adverse effects: neurological
Psychological
There was no clear evidence of a difference in depression when different atypical antipsychotics were compared (RR 0.34, 95% CI 0.01 to 8.13; 1 study, 59 participants; Analysis 6.7).
6.7. Analysis.

Comparison 6: Atypical vs atypical antipsychotics, Outcome 7: Adverse effects: psychological
Skin
The likelihood of rash was not different when different atypical antipsychotics were compared (RR 1.03, 95% CI 0.07 to 15.77; 1 study, 59 participants; Analysis 6.8).
6.8. Analysis.

Comparison 6: Atypical vs atypical antipsychotics, Outcome 8: Adverse effects: skin
Urinary
Enuresis did not differ between atypical antipsychotic groups (RR 1.37, 95% CI 0.04 to 53.78; I2 = 68%; 2 studies, 120 participants; Analysis 6.9).
6.9. Analysis.

Comparison 6: Atypical vs atypical antipsychotics, Outcome 9: Adverse effects: urinary
Secondary outcomes
Tolerability/acceptability
There was no clear evidence of a difference in loss to follow‐up between typical and atypical antipsychotic groups (MD 0.71, 95% CI 0.36 to 1.37; 2 studies, 120 participants; P = 0.31, I2 = 0%; Analysis 6.10).
6.10. Analysis.

Comparison 6: Atypical vs atypical antipsychotics, Outcome 10: Tolerability/acceptability: loss to follow‐up
Outcomes not reported
No data were available for the outcomes of aggression, self‐injury, and quality of life, or immune, respiratory, and other AEs.
Atypical antipsychotics versus antidementia medications
Primary outcomes
Challenging behaviours
Irritability
There was no clear evidence of a difference in irritability at endpoint when atypical antipsychotics (risperidone) were compared to antidementia medications (memantine) (SMD 0.46, 95% CI −0.27 to 1.19; 1 study, 30 participants; Analysis 7.1).
7.1. Analysis.

Comparison 7: Atypical antipsychotic vs antidementia, Outcome 1: Irritability
There were insufficient studies (1) to conduct subgroup analyses.
Adverse effects
Neurological
There was no clear evidence of a difference in somnolence when we compared atypical antipsychotics to antidementia medications (RR 1.30, 95% CI 0.86 to 1.96; 1 study, 30 participants; Analysis 7.2)
7.2. Analysis.

Comparison 7: Atypical antipsychotic vs antidementia, Outcome 2: Adverse effects: neurological
Secondary outcomes
Tolerability/acceptability
There was no clear evidence of a difference in loss to follow‐up between atypical antipsychotic and antidementia groups (RR 0.38, 95% CI 0.04 to 3.25; 1 study, 34 participants; Analysis 7.3).
7.3. Analysis.

Comparison 7: Atypical antipsychotic vs antidementia, Outcome 3: Tolerability
Outcomes not reported
No data were available for the outcomes of aggression, self‐injury, and quality of life, or cardiovascular, gastrointestinal, immune, metabolic, musculoskeletal, psychological, respiratory, skin, urinary, or other AEs.
Atypical antipsychotics versus antiparkinsonians
Primary outcomes
Challenging behaviours
None of the studies reported these outcomes.
Adverse effects
Gastrointestinal
There was no clear evidence of a difference in any of the gastrointestinal side effects when atypical antipsychotics (amulsipride) were compared to antiparkinsonians (bromocriptine):
diarrhoea (RR 3.00, 95% CI 0.14 to 65.16; 1 study, 9 participants);
increased salivation (RR 3.00, 95% CI 0.14 to 65.16; 1 study, 9 participants); or
vomiting (RR 0.20, 95% CI 0.01 to 3.66; 1 study, 9 participants; Analysis 8.1).
8.1. Analysis.

Comparison 8: Atypical antipsychotic vs antiparkinsonian, Outcome 1: Adverse effects: gastrointestinal
Metabolic
There was no clear evidence of a difference between those receiving atypical antipsychotics and antiparkinsonian medications in decreased appetite (RR 0.09, 95% CI 0.01 to 1.44; 1 study, 9 participants; Analysis 8.2).
8.2. Analysis.

Comparison 8: Atypical antipsychotic vs antiparkinsonian, Outcome 2: Adverse effects: metabolic
Neurological
There was no clear evidence of a difference between those receiving atypical antipsychotics and antiparkinsonian medications in any of the neurological side effects: agitation/ excitement (RR 1.50, 95% CI 0.32 to 6.94; 1 study, 9 participants); increased hyperactivity (RR 7.00, 95% CI 0.41 to 118.69; 1 study, 9 participants); insomnia (RR 2.00, 95% CI 0.48 to 8.31; 1 study, 9 participants); or sedation (RR 0.14, 95% CI 0.01 to 2.42; 1 study, 9 participants) Analysis 8.3.
8.3. Analysis.

Comparison 8: Atypical antipsychotic vs antiparkinsonian, Outcome 3: Adverse effects: neurological
Secondary outcomes
None of the studies reported these outcomes.
Outcomes not reported
No data were available for the outcomes of irritability, aggression, self‐injury, quality of life, or tolerability/acceptability, and cardiovascular, immune, musculoskeletal, psychological, respiratory, skin, urinary, and other AEs.
Anticonvulsants versus placebo
Primary outcomes
Challenging behaviours
Irritability
There was no clear evidence of a difference in measures of irritability at endpoint between participants receiving anticonvulsants and those receiving placebo (SMD −0.67, 95% CI −1.93 to 0.59; P = 0.30, I2 = 88%; 3 studies, 97 participants; Analysis 9.1).
9.1. Analysis.

Comparison 9: Anticonvulsant vs placebo, Outcome 1: Irritability
There was insufficient information to conduct subgroup analyses of irritability by age, gender, communication ability, or cognitive ability.
Aggression
There was no clear evidence of a difference in measures of aggression at endpoint between participants receiving anticonvulsants and those receiving placebo (SMD −0.18, 95% CI −0.71 to 0.35; I2 = 0%; 2 studies, 57 participants; Analysis 9.2).
9.2. Analysis.

Comparison 9: Anticonvulsant vs placebo, Outcome 2: Aggression
There was insufficient information to conduct subgroup analyses of aggression by age, gender, communication ability, or cognitive ability.
Adverse effects
Gastrointestinal
There was no clear evidence of a difference between anticonvulsants and placebo groups in:
abdominal pain (RR 1.75, 95% CI 0.38 to 8.15; 1 study 30 participants);
constipation (RR 0.58, 95% CI 0.11 to 3.00; 1 study, 30 participants);
diarrhoea (RR 3.50, 95% CI 0.44 to 27.75; 1 study, 30 participants);
nausea (RR 2.32, 95% CI 0.80 to 6.72; I2 = 0%; 2 studies, 70 participants); or
vomiting (RR 3.50, 95% CI 0.44 to 27.75; 1 study, 30 participants; Analysis 9.3).
9.3. Analysis.

Comparison 9: Anticonvulsant vs placebo, Outcome 3: Adverse effects: gastrointestinal
Immune system
There was no difference between anticonvulsant and placebo groups in:
chills (RR 2.63, 95% CI 0.31 to 22.46; 1 study, 30 participants); or
fever (RR 3.50, 95% CI 0.44 to 27.75; 1 study, 30 participants; Analysis 9.4).
9.4. Analysis.

Comparison 9: Anticonvulsant vs placebo, Outcome 4: Adverse effects: immune system
Metabolic
There were higher rates of decreased appetite in anticonvulsant groups when compared to placebo groups (RR 5.45, 95% CI 1.02 to 29.23; I2 = 0%; 2 studies, 60 participants).
There was no clear evidence of a difference between anticonvulsant and placebo groups in:
increased appetite (RR 0.99, 95% CI 0.05 to 18.14; I2 = 82%; 2 studies, 70 participants);
weight gain (RR 1.48, 95% CI 0.61 to 3.62; I2 = 0%; 3 studies, 77 participants);
weight loss (RR 3.00, 95% CI 0.14 to 65.90; 1 study, 20 participants; Analysis 9.5); or
weight gain in kilograms (SMD 0.48 kg, 95% CI −0.77 to 1.74; 1 study, 11 participants; Analysis 9.6).
9.5. Analysis.

Comparison 9: Anticonvulsant vs placebo, Outcome 5: Adverse effects: metabolic (dichotomous)
9.6. Analysis.

Comparison 9: Anticonvulsant vs placebo, Outcome 6: Adverse effects: metabolic (continuous)
Neurological
There was no clear evidence of a difference between anticonvulsant and placebo groups in any of the neurological AEs:
aggression (dichotomous) (RR 2.29, 95% CI 0.37 to 14.12; 2 studies, 48 participants);
agitation (RR 1.20, 95% CI 0.21 to 6.70; I2 = 0%; 2 studies, 47 participants);
dizziness (RR 4.00, 95% CI 0.49 to 32.72; 1 study, 40 participants);
drowsiness (RR 0.88, 95% CI 0.21 to 3.66; 1 study, 30 participants);
echolalia (RR 1.00, 95% CI 0.07 to 14.45; 1 study, 28 participants);
headache (RR 2.12, 95% CI 0.09 to 47.68; 1 study, 27 participants);
hyperactivity (RR 3.00, 95% CI 0.14 to 65.90; 1 study, 20 participants);
hypersomnolence (RR 0.10, 95% CI 0.01 to 1.78; 1 study, 27 participants);
insomnia (RR 1.69, 95% CI 0.44 to 6.56; I2 = 25%; 4 studies, 115 participants);
lethargy (RR 6.18, 95% CI 0.35 to 110.11; 1 study, 30 participants);
paresthesia (RR 5.00, 95% CI 0.64 to 39.06; 1 study 40 participants);
sedation (RR 0.25, 95% CI 0.03 to 2.05, 1 study, 40 participants);
self‐injurious behaviour (dichotomous) (RR 3.00, 95% CI 0.14 to 65.90; 1 study, 20 participants); or
somnolence (RR 7.00, 95% CI 0.95 to 51.80; 1 study, 20 participants; Analysis 9.7).
9.7. Analysis.

Comparison 9: Anticonvulsant vs placebo, Outcome 7: Adverse Effects: neurological
Psychological
There was no clear evidence of a difference in impulsivity when anticonvulsants were compared to placebo (RR 3.00, 95% CI 0.14 to 65.90; 1 study, 20 participants; Analysis 9.8).
9.8. Analysis.

Comparison 9: Anticonvulsant vs placebo, Outcome 8: Adverse effects: psychological
Skin
There was no difference in the risk of rash between anticonvulsant and placebo groups (RR 4.63, 95% CI 0.89 to 24.13; I2 = 0%; 2 studies, 57 participants; Analysis 9.9).
9.9. Analysis.

Comparison 9: Anticonvulsant vs placebo, Outcome 9: Adverse effects: skin
Urinary
Enuresis was not different between groups (RR 0.33, 95% CI 0.02 to 7.32; 1 study, 20 participants; Analysis 9.10).
9.10. Analysis.

Comparison 9: Anticonvulsant vs placebo, Outcome 10: Adverse effects: urinary
Secondary outcomes
Tolerability/acceptability
There was no clear evidence of a difference in loss to follow‐up between anticonvulsants and placebo groups (RR 1.98, 95% CI 0.84 to 4.66; I² = 0%; 6 studies, 167 participants; Analysis 9.11).
9.11. Analysis.

Comparison 9: Anticonvulsant vs placebo, Outcome 11: Tolerability/acceptability: loss to follow‐up
Outcomes not reported
No data were available for the outcomes of self‐injury or quality of life, or cardiovascular, respiratory, musculoskeletal, and other AEs.
Antidepressants versus antidepressants
Primary outcomes
Challenging behaviours
Irritability
One study with 36 participants compared two antidepressants, clomipramine and desipramine, but did not report any data on irritability.
Aggression
One study with 36 participants compared two antidepressants, clomipramine and desipramine, but did not report any data on aggression.
Self‐injury
One study with 36 participants compared two antidepressants, clomipramine and desipramine, but did not report any data on self‐injury.
Adverse effects
Cardiovascular
There was no clear evidence of a difference in tachycardia in the one study with 36 participants that compared clomipramine with desipramine (RR 2.60, 95% CI 0.13 to 50.25; 1 study, 24 participants; Analysis 10.1).
10.1. Analysis.

Comparison 10: Antidepressant vs antidepressant, Outcome 1: Adverse effects: cardiovascular
Gastrointestinal
There was no clear evidence of a difference in any gastrointestinal AEs when clomipramine was compared to desipramine. The effects that were reported were:
constipation (RR 1.50, 95% CI 0.35 to 6.35; 1 study, 36 participants);
dry mouth (RR 0.50, 95% CI 0.12 to 2.12; 1 study, 36 participants);
nausea/abdominal pain (RR 1.00, 95% CI 0.10 to 9.96; 1 study, 36 participants); and
vomiting (RR 1.56, 95% CI 0.07 to 35.67; 1 study, 36 participants; Analysis 10.2).
10.2. Analysis.

Comparison 10: Antidepressant vs antidepressant, Outcome 2: Adverse effects: gastrointestinal
Secondary outcomes
Quality of life
One study with 36 participants compared two antidepressants, clomipramine and desipramine, but did not report any data on quality of life.
Tolerability/acceptability
One study with 36 participants compared two antidepressants, clomipramine and desipramine, but did not report any data on loss to follow‐up.
Outcomes not reported
No data were available for the outcomes of irritability, aggression, or self‐injury, or immune, metabolic, musculoskeletal, neurological, psychological, respiratory, skin, urinary, and other AEs, or quality of life, and tolerability/acceptability.
Antidementia interventions versus placebo or other treatment
Primary outcomes
Challenging behaviours
Irritability
There was no clear evidence of a difference in continuous irritability scores at endpoint when antidementia medications were compared to placebo (SMD −0.40, 95% CI −1.31 to 0.52; I2 = 83%; 3 studies, 140 participants; Analysis 11.1).
11.1. Analysis.

Comparison 11: Antidementia versus placebo, Outcome 1: Irritability (continuous)
There was also no clear evidence of a difference in partial response (≥ 25% reduction in irritability score; RR 1.38, 95% CI 0.97 to 1.97; 1 study, 40 participants); or complete response (≥ 50% reduction in irritability score; RR 1.60, 95% CI 0.98 to 2.61; 1 study, 40 participants); or dichotomous irritability (RR 0.51, 95% CI 0.16 to 1.66; 1 study, 317 participants; Analysis 11.2).
11.2. Analysis.

Comparison 11: Antidementia versus placebo, Outcome 2: Irritability (dichotomous)
There was no clear evidence of a difference between groups when children were compared to adults (P = 0.40). There was insufficient information to conduct subgroup analyses of irritability by gender, communication ability, or cognitive ability.
Aggression
There was no clear evidence of a difference in aggression at endpoint when antidementia medications were compared to placebo (SMD 0.54, 95% CI ‐0.05 to 1.13; 1 study, 50 participants; Analysis 11.3).
11.3. Analysis.

Comparison 11: Antidementia versus placebo, Outcome 3: Aggression
There were insufficient studies (1 study) to conduct a subgroup analysis.
Adverse effects
Gastrointestinal
Gastrointestinal AEs were not increased in the group receiving antidementia medications. The reported gastrointestinal effects were:
abdominal pain (RR 0.97, 95% CI 0.21 to 4.50; I2 = 0%; 2 studies, 83 participants);
constipation (RR 0.33, 95% CI 0.04 to 3.01; I2 = 0%; 2 studies, 83 participants);
diarrhoea (RR 2.87, 95% CI 0.12 to 66.75; 1 study, 43 participants);
dry mouth (RR 0.14, 95% CI 0.01 to 2.60; 1 study, 40 participants);
gastroenteritis (RR 7.13, 95% CI 0.37 to 136.97; 1 study, 317 participants);
nausea (RR 2.00, 95% CI 0.41 to 9.71; 1 study, 40 participants);
vomiting (RR 0.54, 95% CI 0.18 to 1.67; I2 = 0%; 2 studies, 438 participants; Analysis 11.4).
11.4. Analysis.

Comparison 11: Antidementia versus placebo, Outcome 4: Adverse effects: gastrointestinal
Metabolic
There was no clear evidence of a difference in the effects of antidementia medications on:
decreased appetite (RR 0.99, 95% CI 0.24 to 4.07; I2 = 0%; 4 studies, 163 participants); or
increased appetite (RR 1.14, 95% CI 0.54 to 2.43; I2 = 0%; 4 studies, 163 participants; Analysis 11.5).
11.5. Analysis.

Comparison 11: Antidementia versus placebo, Outcome 5: Adverse events: metabolic
Musculoskeletal
There was no clear evidence of a difference in effects of antidementia medications compared to placebo on musculoskeletal pain (RR 0.32, 95% CI 0.01 to 7.42; 1 study, 43 participants; Analysis 11.6).
11.6. Analysis.

Comparison 11: Antidementia versus placebo, Outcome 6: Adverse effects: musculoskeletal pain
Neurological
Neurological AEs were not different between participants receiving antidementia medications and those receiving placebo. The neurological AEs that were reported included:
daytime drowsiness (RR 0.85, 95% CI 0.41 to 1.77; I2 = 0%; 2 studies, 80 participants);
decreased energy (RR 0.37, 95% CI 0.09 to 1.52, 1 study, 23 participants);
dizziness (RR 0.99, 95% CI 0.27 to 3.61; I2 = 0%; 2 studies, 83 participants);
fatigue (RR 1.39, 95% CI 0.48 to 4.02; I2 = 0%; 2 studies, 83 participants);
headache (RR 0.85, 95% CI 0.26 to 2.75; I2 = 0%; 2 studies, 438 participants);
hyperactivity (RR 0.35, 95% CI 0.07 to 1.73; I2 = 0%; 2 studies, 438 participants);
insomnia (RR 0.98, 95% CI 0.37 to 2.59; I2 = 2%; 4 studies, 227 participants);
morning drowsiness (RR 1.38, 95% CI 0.71 to 2.68; 1 study, 40 participants);
sedation (RR 1.34, 95% CI 0.30 to 5.98; I2 = 5%; 2 studies, 83 participants);
tremor (RR 3.00, 95% CI 0.13 to 69.52; 1 study, 40 participants; Analysis 11.7).
11.7. Analysis.

Comparison 11: Antidementia versus placebo, Outcome 7: Adverse effects: neurological
Psychological
Psychological AEs were not different between participants receiving antidementia medications and those receiving placebo. The psychological AEs that were reported included:
agitation (RR 1.89, 95% CI 0.45 to 8.05; I2 = 0%; 2 studies, 438 participants);
aggression (dichotomous) (RR 1.69, 95% CI 0.42 to 6.78; 1 study, 121 participants);
anger (RR 0.31, 95% CI 0.01 to 6.85; 1 study, 23 participants);
anxiety (RR 0.41, 95% CI 0.03 to 5.61; I2 = 67%; 3 studies, 478 participants);
emotional lability (RR 1.83, 95% CI 0.19 to 17.51, 1 study, 23 participants);
irritability (dichotomous) (RR 0.87, 95% CI 0.43 to 1.76; I2 = 0%; 3 studies, 461 participants);
mood changes (RR 1.68, 95% CI 0.95 to 2.96; 1 study, 23 participants);
self‐injurious behaviour (dichotomous) (RR 2.77, 95% CI 0.12 to 61.65, 1 study, 23 participants; Analysis 11.9).
11.9. Analysis.

Comparison 11: Antidementia versus placebo, Outcome 9: Adverse events: psychological
Respiratory
Respiratory AEs were not different between participants receiving antidementia medications and those receiving placebo. The respiratory AEs that were reported included:
cough (RR 1.83, 95% CI 0.63 to 5.34; I2 = 0%; 2 studies, 438 participants); and
nasopharyngitis (RR 0.61, 95% CI 0.08 to 4.35; I2 = 51%; 2 studies, 438 participants; Analysis 11.10).
11.10. Analysis.

Comparison 11: Antidementia versus placebo, Outcome 10: Adverse events: respiratory
Skin
There was no difference between participants receiving antidementia medications and those receiving placebo in:
rash (RR 2.00, 95% CI 0.20 to 20.33; 1 study, 40 participants); and
skin irritation (RR 0.46, 95% CI 0.15 to 1.40, 1 study, 23 participants; Analysis 11.11).
11.11. Analysis.

Comparison 11: Antidementia versus placebo, Outcome 11: Adverse effects: skin
Other adverse effects
Other AEs were not different between participants receiving antidementia medications and those receiving placebo. The other AEs reported were:
pyrexia (RR 0.68, 95% CI 0.19 to 2.41; I2 = 0%; 2 studies, 438 participants); and
increased infections (RR 0.69, 95% CI 0.35 to 1.35; 1 study, 23 participants).
Secondary outcomes
Tolerability/acceptability
There was no clear evidence of a difference in loss to follow‐up between antidementia and placebo groups (RR 0.95, 95% CI 0.83 to 1.09; P = 0.56, I² = 0%; 5 studies, 553 participants; Analysis 11.13).
11.13. Analysis.

Comparison 11: Antidementia versus placebo, Outcome 13: Tolerability/acceptability: loss to follow‐up
Outcomes not reported
No data were available for the outcomes of self‐injury, or cardiovascular, immune, and urinary AEs, or quality of life.
Antiparkinsonian medications versus placebo or other treatment
Primary outcomes
Challenging behaviours
Irritability
There was a reduction in irritability at endpoint in the one study with 40 participants that compared antiparkinsonians (amantadine) with placebo and reported this outcome (SMD −0.75, 95% CI −1.39 to −0.11; 1 study, 40 participants; Analysis 12.1).
12.1. Analysis.

Comparison 12: Antiparkinsonian vs placebo, Outcome 1: Irritability
There were insufficient studies (1 study) to conduct a subgroup analysis.
Adverse effects
Gastrointestinal
One study with 40 participants reported gastrointestinal AEs. There was no difference between the antiparkinsonian and placebo groups. Gastrointestinal effects reported included:
abdominal pain (RR 0.33, 95% CI 0.01 to 7.72; 1 study, 40 participants);
constipation (RR 0.20, 95% CI 0.01 to 3.92; 1 study, 40 participants); and
drooling (RR 0.33, 95% CI 0.01 to 7.72; 1 study, 40 participants; Analysis 12.2).
12.2. Analysis.

Comparison 12: Antiparkinsonian vs placebo, Outcome 2: Adverse effects: gastrointestinal
Metabolic
There was no clear evidence of an effect of antiparkinsonians compared with placebo on:
increased appetite (RR 3.00, 95% CI 0.69 to 13.12; 1 study, 40 participants); or
decreased appetite (RR 0.11, 95% CI 0.01 to 1.94; 1 study, 40 participants; Analysis 12.3).
12.3. Analysis.

Comparison 12: Antiparkinsonian vs placebo, Outcome 3: Adverse effects: metabolic
Neurological
Across two studies that compared antiparkinsonians (amantadine) to placebo, there was no difference in neurological AEs including:
daytime drowsiness (RR 3.00, 95% CI 0.13 to 69.52; 1 study, 40 participants);
insomnia (RR 2.26, 95% CI 0.55 to 9.26; I2 = 0%; 2 studies, 79 participants);
nervousness (RR 0.33, 95% CI 0.04 to 2.94; 1 study, 40 participants);
somnolence (RR 5.25, 95% CI 0.27 to 102.74; 1 study 39 participants); and
tremor (RR 3.00, 95% CI 0.13 to 69.52; 1 study, 40 participants; Analysis 12.4).
12.4. Analysis.

Comparison 12: Antiparkinsonian vs placebo, Outcome 4: Adverse effects: neurological
Psychological
There was no evidence of a change in adverse behaviour (dichotomous) (RR 0.53, 95% CI 0.11 to 2.55; 1 study, 39 participants) when antiparkinsonians were compared to placebo (Analysis 12.5).
12.5. Analysis.

Comparison 12: Antiparkinsonian vs placebo, Outcome 5: Adverse effects: psychological
Secondary outcomes
Tolerability/acceptability
There was no clear evidence of a difference in loss to follow‐up between antiparkinsonian and placebo groups (RR 0.33, 95% CI 0.01 to 7.72, 1 study, 40 participants; Analysis 12.6).
12.6. Analysis.

Comparison 12: Antiparkinsonian vs placebo, Outcome 6: Tolerability/acceptability: loss to follow‐up
Outcomes not reported
No data were available for the outcomes of aggression, self‐injury, quality of life, and cardiovascular, immune, musculoskeletal, respiratory, skin, urinary, and other AEs.
Anxiolytic interventions versus placebo or other treatment
Primary outcomes
Challenging behaviours
Irritability
There was no clear evidence of a difference in continuous measures of irritability at endpoint (SMD −0.20, 95% CI −0.88 to 0.47; 1 study, 34 participants; Analysis 13.1), although dichotomous measures of irritability (> 25% decrease in irritability score) showed a reduction in irritability (RR 1.83, 95% CI 1.04 to 3.22; 1 study, 34 participants; Analysis 13.2) when anxiolytics were compared to placebo.
13.1. Analysis.

Comparison 13: Anxiolytic versus placebo, Outcome 1: Irritabilty (continuous)
13.2. Analysis.

Comparison 13: Anxiolytic versus placebo, Outcome 2: Irritability (dichotomous)
There were insufficient studies (1 study) to conduct a subgroup analysis.
Adverse effects
Gastrointestinal
There was no clear evidence of differences between anxiolytics and placebo in any of the gastrointestinal AEs:
constipation (RR 0.97, 95% CI 0.35 to 2.67; 1 study, 166 participants);
diarrhoea (RR 1.04, 95% CI 0.68 to 1.61; 1 study, 166 participants); or
vomiting (RR 1.02, 95% CI 0.68 to 1.53; 1 study, 166 participants; Analysis 13.3).
13.3. Analysis.

Comparison 13: Anxiolytic versus placebo, Outcome 3: Adverse effects: gastrointestinal
Immune system
There was no difference between anxiolytic and placebo groups in the likelihood of:
nasopharyngitis (RR 0.87, 95% CI 0.33 to 2.28; 1 study, 166 participants); and
pyrexia (RR 1.00, 95% CI 0.73 to 1.37; 1 study, 166 participants).
However, upper respiratory tract infection was reduced in the anxiolytic group (RR 0.40, 95% CI 0.18 to 0.91; 1 study, 166 participants; Analysis 13.4).
13.4. Analysis.

Comparison 13: Anxiolytic versus placebo, Outcome 4: Adverse effects: immune System
Metabolic
There was no difference between anxiolytic and placebo groups in:
decreased appetite (RR 1.11, 95% CI 0.62 to 1.99; 1 study, 166 participants); and
increased appetite (RR 1.50, 95% CI 0.93 to 2.42; I2 = 0%; 2 studies, 200 participants; Analysis 13.5).
13.5. Analysis.

Comparison 13: Anxiolytic versus placebo, Outcome 5: Adverse effects: metabolic
Neurological
Neurological AEs were not different between anxiolytics and placebo groups in one study with 166 participants. These included:
hyperactivity (RR 0.79, 95% CI 0.47 to 1.30);
increased aggression (RR 0.91, 95% CI 0.60 to 1.38);
insomnia (RR 1.26, 95% CI 0.90 to 1.78); irritability (RR 0.84, 95% CI 0.48 to 1.47);
irritability (dichotomous) (RR 0.84, 95% CI 0.48 to 1.47); and
somnolence (RR 1.70, 95% CI 0.58 to 4.97; Analysis 13.6).
13.6. Analysis.

Comparison 13: Anxiolytic versus placebo, Outcome 6: Adverse effects: neurological
Psychological
Anxiety was not decreased in the anxiolytic group in one study with 166 participants (RR 2.76, 95% CI 0.48 to 15.83; Analysis 13.7).
13.7. Analysis.

Comparison 13: Anxiolytic versus placebo, Outcome 7: Adverse effects: psychological
Respiratory
There was no difference between anxiolytic and placebo groups in one study with 166 participants in:
cough (RR 0.90, 95% CI 0.64 to 1.26);
epistaxis (RR 0.52, 95% CI 0.19 to 1.43);
nasal congestion (RR 0.80, 95% CI 0.36 to 1.77);
rhinorrhea (RR 1.12, 95% CI 0.66 to 1.88); and
sinus congestion (RR 0.90, 95% CI 0.55 to 1.47; Analysis 13.8).
13.8. Analysis.

Comparison 13: Anxiolytic versus placebo, Outcome 8: Adverse effects: respiratory system
Skin
There was no difference in rash between anxiolytic and placebo groups in one study with 166 participants (RR 1.19, 95% CI 0.52 to 2.73; Analysis 13.9).
13.9. Analysis.

Comparison 13: Anxiolytic versus placebo, Outcome 9: Adverse effects: skin
Secondary outcomes
Tolerability/acceptability
There was no clear evidence of a difference in loss to follow‐up between anxiolytic and placebo groups (RR 0.88, 95% CI 0.45 to 1.73; I² = 0%; 2 studies, 206 participants; Analysis 13.11).
13.11. Analysis.

Comparison 13: Anxiolytic versus placebo, Outcome 11: Tolerability/acceptability: loss to follow‐up
Outcomes not reported
No data were available for the outcomes of aggression, self‐injury, or quality of life, and cardiovascular, musculoskeletal, urinary, and other AEs.
Experimental interventions versus placebo or other treatment
Primary outcomes
Challenging behaviours
Irritability
Studies compared a variety of interventions to placebo. As they covered a range of different pharmacological classes, we categorised them as experimental drugs. These interventions included: celecoxib (NSAID); d‐cycloserine; dextromethorphan; mecamylamine; riluzole; pioglitazone; n‐acetylcysteine; Trichuris suis ova; tetrahydrobiopterin; lofexedine; naltrexone; minocycline; propentofylline; sulforaphane; folinic acid; carnosine; prednisolone (corticosteroid); dextromethorphan/quinidine; pregnenolone; baclofen; palmitoylethanolamide; bumetanide; resveratrol; arbaclofen; simvastatin; and nicotine.
There was some evidence that irritability was reduced at endpoint in participants in the experimental intervention groups compared to placebo (SMD −0.30, 95% CI −0.53 to −0.07; I² = 72%, 28 studies, 1205 participants; Analysis 14.1). There were no differences between groups when we compared children to children and adults, and adults (P = 0.94), however, there was evidence of a difference between types of experimental interventions when we conducted a subgroup analysis of interventions by age group (children, children and adults, or adults; P < 0.00001). There was insufficient information to conduct subgroup analyses of irritability by gender, communication ability, or cognitive ability.
14.1. Analysis.

Comparison 14: Experimental versus placebo, Outcome 1: Irritability
We were unable to include data from three studies because the data were skewed (Arnold 2012a; Hollander 2020a; Minshawi 2016). Details can be found in Table 19.
15. Experimental versus placebo: irritability results that could not be used in the meta‐analyses.
| Study name | Short‐/medium‐/long‐term outcomes | Group 1 sample size | Group 2 sample size | Group 1 results Mean (standard deviation) | Group 2 results Mean (standard deviation) | Other data | Notes |
| Arnold 2012a | Short‐term mecamylamine (max 5 mg/day) | 12 | 8 | −3.17 (8.76) | −5.0 (10.78) | "No significant differences were found for age, weight, sex, diagnosis, IQ, or entry scores for the OACIS, RBS, ABC Irritability, ABC Hyperactivity, ABC Lethargy/ Social Withdrawal, ABC Inappropriate Speech, ADI‐R Qualitative Abnormalities in Reciprocal Social Interaction or ADI‐R Qualitative Abnormalities in Communication" | Skewed |
| Hollander 2020a | Short‐term Trichuris suis ova (a dose of 2500 Trichurissuis ova every 2 weeks) | 10 | 10 | −4.0 (18.5) | −0.14 (6.32) | P = 0.0687, 95% CI −4.82 to 91.32 | Skewed |
| Minshawi 2016 | Short‐term D‐cycloserine (50 mg once weekly) | 34 | 33 | −1.55 (6.11) | −1.23 (6.09) | "teacher‐rated ABC data was returned for 23.5 % of the DCS group, and 30.3 % of the placebo group with no significant difference noted for any of the ABC subscales (irritability p = 0.623, social withdrawal p = 0.845" | Skewed |
| ABC: Aberrant Behaviour checklist; DCS: D‐cycloserine; OACIS: Ohio Autism Clinical Impressions Scale; RBS: Repetitive Behaviour Scale | |||||||
Self‐injury
There was no clear evidence of a difference in self‐injurious behaviour at endpoint between participants receiving any of the experimental interventions compared to participants receiving placebo:
bumetanide (SMD 0.20, 95% CI −0.21 to 0.60, P = 0.34; I² = 22%, 2 studies, 148 participants;
N‐acetyl cysteine (SMD 0.08, 95% CI −0.29 to 0.44; P = 0.69; I² = 5%, 2 studies, 127 participants);
Trichuris suis ova (SMD −0.30, 95% CI −1.55 to 0.95; P = 0.64; 1 study, 10 participants; Analysis 14.2).
14.2. Analysis.

Comparison 14: Experimental versus placebo, Outcome 2: Self‐injury
We were unable to include data from three studies in the analysis because the data were skewed (Dean 2019; Hardan 2012; Hollander 2020a). Details can be found in Table 20.
16. Experimental versus placebo: self‐injurious behaviour results that could not be used in the meta‐analysis.
| Study name | Short‐/medium‐/long‐term outcomes | Group 1 sample size | Group 2 sample size | Group 1 results Mean (standard deviation) | Group 2 results Mean (standard deviation) | Other data | Notes |
| Dean 2019 | Short‐term self‐injurious behaviour (N‐acetylcysteine 500 mg/day) |
48 | 50 | 2.2 (2.9) | 1.7 (2.6) | "There were no differences between N‐acetyl cysteine and placebo‐treated groups on any of the outcome measures for either primary or secondary endpoints. There was no significant difference in the number and severity of adverse events between groups" | Skewed |
| Hardan 2012 | Short‐term self‐injurious behaviour (N‐acetylcysteine maz 900 mg/day 3 times daily) | 14 | 15 | 2.2 (2.3) | 3.0 (3.6) | "Compared with placebo, NAC resulted in significant improvements on ABC irritability subscale (F= 6.80; P <.001;d.= 0.96)" | Skewed |
| Hollander 2020a | Short‐term self‐injurious behaviour (Trichuris suis ova, dose of 2500 ova every 2 weeks) | 10 | 10 | −0.37 (2.5) | 0.42 (2.31) | "Trending improvements were observed in irritability using the overall percent change from baseline to endpoint on the Aberrant Behavior Checklist (ABC)–Irritability subscale" | Skewed |
| NAC: N‐acetylcysteine | |||||||
There was no clear evidence of a difference in self‐injury between groups when we compared interventions by age (children only versus adults; P = 0.65). There was insufficient information to conduct subgroup analyses of self‐injury by gender, communication ability, or cognitive ability.
Adverse effects
The AEs from one study (Ghanizadeh 2013), could not be included in the analysis because AEs were reported as a percentage of all participants who experienced an AE, rather than percentage by group. See Table 21.
17. Experimental versus placebo: adverse effects data that could not be used in the meta‐analysis.
| Study name | Short‐/medium‐/long‐term outcomes | Group 1 | Group 2 | Group 1 sample size | Group 2 sample size | Group 1 results Mean (standard deviation) | Group 2 results Mean (standard deviation) | Other data | Notes |
| Ghanizadeh 2013 | Short‐term adverse effects (NAC 1200 mg/day, risperidone 2‐3 mg/day depending on weight). 20+ AEs included fatigue, increased appetite, decreased appetite, diarrhoea, and constipation. | N‐acetylcysteine + risperidone | Placebo + risperidone | 17 | 14 | AEs were reported for each group although percentage was out of total number of participants, not participants for each group. | |||
| AE: adverse effect; NAC: N‐acetylcysteine | |||||||||
Gastrointestinal
There was some evidence of a difference between experimental interventions compared to placebo for thirst (RR 3.32, 95% CI 1.10 to 10.01; I² = 0%; 4 studies, 224 participants; Analysis 14.3).
14.3. Analysis.

Comparison 14: Experimental versus placebo, Outcome 3: Adverse effects: gastrointestinal
There was no clear evidence of a difference in any of the other gastrointestinal AEs including:
abdominal pain (RR 1.38, 95% CI 0.95 to 2.01; I² = 0%; 14 studies, 734 participants);
change in bowel habits (RR 0.39, 95% CI 0.05 to 3.26; I² = 25%; 2 studies, 54 participants);
constipation (RR 1.29, 95% CI 0.77 to 2.16; I² = 0%; 13 studies, 665 participants);
diarrhoea (RR 0.83, 95% CI 0.55 to 1.25; I² = 0%; 18 studies, 982 participants);
drooling (RR 0.29, 95% CI 0.01 to 5.79; 1 study, 11 participants);
dry mouth (RR 0.87, 95% CI 0.37 to 2.09; I² = 0%; 5 studies, 173 participants);
dyspepsia (RR 0.31, 95% CI 0.01 to 7.15; 1 study, 31 participants);
encopresis (RR 0.31, 95% CI 0.01 to 7.15; 1 study, 31 participants);
flatulence (RR 3.00, 95% CI 0.15 to 59.89; 1 study, 10 participants);
increased salivation (RR 1.00, 95% CI 0.39 to 2.58; 1 study, 40 participants);
nausea (RR 1.36, 95% CI 0.90 to 2.06; I² = 0%; 15 studies, 768 participants); or
vomiting (RR 1.34, 95% CI 0.91 to 1.98; I² = 0%; 13 studies, 793 participants; Analysis 14.3).
Immune system
There was no clear evidence of a difference between experimental and placebo groups in:
fever (RR 2.94, 95% CI 0.46 to 18.53; I² = 0%; 2 studies, 102 participants); or
influenza (RR 0.31, 95% CI 0.01 to 7.15; 1 study, 31 participants; Analysis 14.4).
14.4. Analysis.

Comparison 14: Experimental versus placebo, Outcome 4: Adverse effects: immune system
Metabolic
Participants receiving experimental interventions (bumetanide) compared to placebo were more likely to experience:
hypokalemia (RR 12.48, 95% CI 4.04 to 38.62, I2 = 0%; 4 studies, 331 participants); and
increased appetite (RR 1.42, 95% CI 1.02 to 1.98, I2 = 0%; 14 studies, 676 participants; Analysis 14.5).
14.5. Analysis.

Comparison 14: Experimental versus placebo, Outcome 5: Adverse effects: metabolic (dichotomous)
The other metabolic effects were no different to placebo:
decreased appetite (RR 1.62, 95% CI 0.95 to 2.75; I² = 0%; 15 studies, 806 participants);
hypoglycaemia (RR 0.71, 95% CI 0.09 to 5.68; I² = 21%; 2 studies, 120 participants);
hyponatremia (RR 3.00, 95% CI 0.13 to 69.31; 1 study, 38 participants);
weight gain (RR 0.32, 95% CI 0.04 to 2.77; I² = 0%; 2 studies, 39 participants);
weight loss (RR 1.49, 95% CI 0.50 to 4.39; I² = 0%; 4 studies, 306 participants);
weight loss (0.12 kg to 0.67 kg) (RR 9.43, 95% CI 0.65 to 137.77; 1 study, 11 participants); or
weight loss (0.45 kg to 2.19 kg) (RR 0.17, 95% CI 0.01 to 2.92; 1 study, 11 participants; Analysis 14.5);
weight change in kilograms (MD 0.13, 95% CI −0.24 to 0.50; 1 study, 23 participants; Analysis 14.6).
14.6. Analysis.

Comparison 14: Experimental versus placebo, Outcome 6: Adverse effects: metabolic (continuous)
Musculoskeletal
There was no clear evidence of a difference between any of the experimental medications compared to placebo for any musculoskeletal AEs including:
arthralgia (RR 0.33, 95% CI 0.02 to 6.65; 1 study, 10 participants);
difficulty walking (RR 0.20, 95% CI 0.01 to 3.92; 1 study, 40 participants);
impaired balance (RR 1.67, 95% CI 0.08 to 33.75; 1 study, 12 participants);
myalgia (RR 1.54, 95% CI 0.79 to 3.04; I² = 0%; 2 studies, 155 participants);
slow movement (RR 4.17, 95% CI 0.22 to 80.25; 1 study, 31 participants);
stiffness (RR 2.03, 95% CI 0.41 to 10.15; I² = 0%; 2 studies, 43 participants); or
weakness (RR 0.63, 95% CI 0.21 to 1.89; I² = 0%; 3 studies, 90 participants; Analysis 14.7).
14.7. Analysis.

Comparison 14: Experimental versus placebo, Outcome 7: Adverse effects: musculoskeletal
Neurological
There was some evidence of an increased risk of drowsiness in participants receiving an experimental intervention compared to placebo (RR 3.45, 95% CI 1.21 to 9.81, 5 studies, 298 participants).
There was no clear evidence of a difference between any of the experimental medications compared to placebo for any of the other neurological AEs including:
agitation/excitement (RR 0.76, 95% CI 0.39 to 1.48; I² = 0%; 5 studies, 220 participants);
anxiety (RR 1.06, 95% CI 0.44 to 2.57; I² = 0%; 3 studies, 250 participants);
daytime drowsiness (RR 1.57, 95% CI 0.75 to 3.28; I² = 0%; 6 studies, 172 participants);
dazed (RR 2.57, 95% CI 0.13 to 52.12; 1 study, 11 participants);
difficulty concentrating (RR 2.50, 95% CI 0.42 to 14.83; 1 study, 12 participants);
difficulty sleeping (RR 0.81, 95% CI 0.44 to 1.50; I² = 0%; 6 studies, 326 participants);
dizziness (RR 1.21, 95% CI 0.67 to 2.18; I² = 0%; 9 studies, 441 participants);
fatigue (RR 1.23, 95% CI 0.70 to 2.17; I² = 0%; 7 studies, 338 participants);
headache (RR 0.91, 95% CI 0.66 to 1.26; I² = 0%; 18 studies, 943 participants);
hypoactivity (RR 0.44, 95% CI 0.07 to 2.95; I² = 23%; 3 studies, 28 participants);
increased aggression (dichotomous) (RR 0.78, 95% CI 0.36 to 1.70; I² = 0%; 4 studies, 149 participants);
increased hyperactivity (RR 0.75, 95% CI 0.35 to 1.58; I² = 0%; 6 studies, 321 participants);
increased irritability (dichotomous) (RR 1.11, 95% CI 0.71 to 1.72; I² = 0%; 5 studies, 177 participants);
increased stereotypies (RR 0.52, 95% CI 0.10 to 2.80; 1 study, 41 participants);
insomnia (RR 1.04, 95% CI 0.66 to 1.65; I² = 0%; 8 studies, 488 participants);
migraine (RR 3.00, 95% CI 0.15 to 59.89; 1 study, 10 participants);
nervousness (RR 1.86, 95% CI 0.47 to 7.37; I² = 51%; 4 studies, 159 participants);
new onset seizures (RR 0.33, 95% CI 0.01 to 7.78; 1 study, 46 participants);
restlessness (RR 1.22, 95% CI 0.53 to 2.82; I² = 0%; 5 studies, 158 participants);
rocking (RR 0.29, 95% CI 0.01 to 5.79; 1 study, 11 participants);
sedation (RR 0.93, 95% CI 0.61 to 1.42; I² = 0%; 13 studies, 624 participants);
syncope (RR 2.80, 95% CI 0.30 to 25.94; 1 study, 89 participants);
tremor (RR1.80, 95% CI 0.44 to 7.37; I² = 0%; 4 studies, 140 participants); or
twitching (RR 3.60, 95% CI 0.42 to 31.04; I² = 0%; 2 studies, 71 participants; Analysis 14.8).
14.8. Analysis.

Comparison 14: Experimental versus placebo, Outcome 8: Adverse effects: neurological
Psychological
There was no clear evidence of a difference between any of the experimental medications compared to placebo for any psychological AEs including:
anorexia (RR 0.53, 95% CI 0.20 to 1.40; 1 study, 20 participants);
aggression (dichotomous) (RR 1.17, 95% CI 0.37 to 3.66; 1 study, 150 participants);
depression (RR 1.93, 95% CI 0.62 to 6.00; I² = 0%; 3 studies, 108 participants);
increased self‐injurious behaviour (RR 0.46, 95% CI 0.11 to 1.84; I² = 0%; 3 studies, 105 participants);
irritability (dichotomous) (RR 0.91, 95% CI 0.36 to 2.27; I² = 0%; 2 studies, 162 participants);
worsening of temper tantrums (dichotomous) (RR 1.88, 95% CI 0.30 to 11.83; I² = 0%; 2 studies, 52 participants);
mental symptoms (RR 1.00, 95% CI 0.41 to 2.45; 1 study, 20 participants); and
repetitive behaviour (RR 0.50, 95% CI 0.05 to 5.14; 1 study, 46 participants; Analysis 14.9).
14.9. Analysis.

Comparison 14: Experimental versus placebo, Outcome 9: Adverse effects: psychological
Respiratory
There was no clear evidence of a difference between any of the experimental medications when compared to placebo for any respiratory AEs including:
aggravation of asthma (RR 3.26, 95% CI 0.14 to 77.35; 1 study, 71 participants);
congestion/cold (RR 1.02, 95% CI 0.62 to 1.68; I² = 0%; 4 studies, 256 participants);
cough (RR 1.16, 95% CI 0.55 to 2.49; I² = 0%; 3 studies, 248 participants);
ear infection (RR 1.88, 95% CI 0.19 to 18.60; 1 study, 31 participants);
lung congestion (RR 1.00, 95% CI 0.60 to 1.68; 1 study, 20 participants) ;
nasopharyngitis (RR 0.78, 95% CI 0.22 to 2.79; 1 study, 150 participants); or
respiratory AEs (RR 5.43, 95% CI 0.27 to 109.19; 1 study, 71 participants; Analysis 14.10).
14.10. Analysis.

Comparison 14: Experimental versus placebo, Outcome 10: Adverse effects: respiratory
Skin
There was no clear evidence of a difference between experimental and placebo groups in:
hives (RR 0.31, 95% CI 0.01 to 7.15; 1 study, 31 participants);
itches (RR 0.55, 95% CI 0.07 to 4.19; I² = 0%; 2 studies, 62 participants);
rash (RR 0.76, 95% CI 0.30 to 1.92; I² = 0%; 7 studies, 440 participants);
skin lesion (RR 1.66, 95% CI 0.74 to 3.70; I² = 0%; 2 studies, 98 participants); or
overall skin AEs (RR 1.09, 95% CI 0.16 to 7.30; 1 study, 71 participants; Analysis 14.11).
14.11. Analysis.

Comparison 14: Experimental versus placebo, Outcome 11: Adverse effects: skin
Urinary
There was no clear evidence of a difference between experimental and placebo groups in:
diuresis (RR 0.93, 95% CI 0.25 to 3.51; 1 study, 89 participants);
enuresis (RR 2.70, 95% CI 0.82 to 8.87; I² = 0%; 3 studies, 205 participants);
urinary retention (RR 0.74, 95% CI 0.05 to 10.49; I² = 33%; 2 studies, 88 participants);
urinary tract infection (RR 0.31, 95% CI 0.01 to 7.15; 1 study, 31 participants; Analysis 14.12)
14.12. Analysis.

Comparison 14: Experimental versus placebo, Outcome 12: Adverse effects: urinary
Other adverse effects
There was no clear evidence of a difference between any of the experimental medications compared to placebo for any other AEs including:
blurred vision (RR 2.50, 95% CI 0.11 to 56.98; 1 study, 31 participants);
dilated pupils (RR 0.67, 95% CI 0.05 to 9.19; 1 study, 20 participants);
fever (RR 0.49, 95% CI 0.13 to 1.88; 1 study, 150 participants);
sweating (RR 0.75, 95% CI 0.15 to 3.86; I² = 0%; 3 studies, 129 participants)
conjunctivitis (RR 0.33, 95% CI 0.02 to 6.65; 1 study, 10 participants) Analysis 14.13.
14.13. Analysis.

Comparison 14: Experimental versus placebo, Outcome 13: Adverse effects: other
Secondary outcomes
Tolerability/acceptability
There was no clear evidence of a difference in loss to follow‐up between experimental and placebo groups (RR 1.07, 95% CI 0.89 to 1.28; 30 studies, 1913 participants; Analysis 14.14).
14.14. Analysis.

Comparison 14: Experimental versus placebo, Outcome 14: Tolerability/acceptability: loss to follow‐up
Outcomes not reported
No data were available for the outcomes of aggression, quality of life, and cardiovascular AEs.
Typical antipsychotics versus placebo
Primary outcomes
Challenging behaviours
Self‐injury
There was no clear evidence of a difference between haloperidol and placebo on levels of self‐injury in the short term (SMD −0.54, 95% CI −1.52 to 0.43; 1 study, 17 participants; Analysis 15.1).
15.1. Analysis.

Comparison 15: Typical antipsychotic vs placebo, Outcome 1: Self‐injury
There were insufficient studies (1 study) to conduct a subgroup analysis.
Adverse effects
Musculoskeletal
There was no clear evidence of a difference between haloperidol and placebo in risk of dystonia in the short term (RR 2.36, 95% CI 0.11 to 52.41; 1 study, 23 participants; Analysis 15.2).
15.2. Analysis.

Comparison 15: Typical antipsychotic vs placebo, Outcome 2: Adverse effects: musculoskeletal
Neurological
There was no clear evidence of a difference between haloperidol and placebo groups in risk of fatigue (RR 8.64, 95% CI 0.53 to 140.05; 1 study, 23 participants; Analysis 15.3).
15.3. Analysis.

Comparison 15: Typical antipsychotic vs placebo, Outcome 3: Adverse effects: neurological
Psychological
There was some evidence of a reduction in risk of behaviour problems in the haloperidol group compared to the placebo group (RR 0.34, 95% CI 0.16 to 0.73; 1 study, 23 participants; Analysis 15.4).
15.4. Analysis.

Comparison 15: Typical antipsychotic vs placebo, Outcome 4: Adverse effects: psychological
Secondary outcomes
Tolerability/acceptability
There was no difference in loss to follow‐up when participants receiving haloperidol were compared to those receiving placebo (RR 0.46, 95% CI 0.14 to 1.49; I2 = 0%; 2 studies, 40 participants; Analysis 15.5).
15.5. Analysis.

Comparison 15: Typical antipsychotic vs placebo, Outcome 5: Tolerability/acceptabiity: loss to follow‐up
Outcomes not reported
No data were available for the outcomes of irritability, aggression, quality of life, and cardiovascular, gastrointestinal, immune, metabolic, respiratory, skin, urinary, and other AEs.
Sensitivity analyses
Where we had sufficient data, we carried out sensitivity analyses on irritability data excluding studies at:
high risk of attrition bias;
high risk of other bias; and
with a sample size less than 50.
Atypical antipsychotics versus placebo
Aripiprazole
Ichikawa 2017 was at high risk of other bias. We found evidence of an effect of aripiprazole on irritability regardless of whether it was included in meta‐analysis (SMD −0.90, 95% CI −1.52 to −0.29) or excluded (SMD −0.64, 95% CI −0.86 to −0.42).
There was also evidence of an effect on irritability whether we included NCT00468130 in the analysis (SMD −0.90, 95% CI −1.52 to −0.29) or excluded it because it was at high risk of bias and had fewer than 50 participants (SMD −0.99, 95% CI −1.65 to −0.33).
Risperidone
Kent 2013 and Troost 2005 were both at high risk of attrition bias and Troost 2005 had multiple domains at high risk of bias. We found evidence of an effect of risperidone when we included both studies in meta‐analysis (SMD −1.11, 95% CI −1.47 to −0.76), when we excluded Kent 2013 from the meta‐analysis (SMD −1.17, 95% CI −1.62 to 0.72) and when we excluded Troost 2005 from the meta‐analysis SMD −1.00, 95% CI −1.23 to −0.76).
Shea 2004 had multiple domains at high risk of bias. We found evidence of an effect of risperidone on irritability whether it was excluded from the meta‐analysis or not (SMD −1.21, 95% CI −1.63 to −0.79).
Neurohormone versus placebo
The effect of neurohormone (oxytocin) on irritability compared with placebo with all three included oxytocin studies in the meta‐analysis was SMD −0.24 (95% CI −0.45 to −0.03). When we excluded Sikich 2021 (due to high risk of attrition bias) from the meta‐analysis, the effect was SMD −0.41 (95% CI −0.91 to 0.09), when we excluded Munesue 2016 and Parker 2017 (both because they included fewer than 50 participants) from the meta‐analysis, the effect was SMD −0.20 (95% CI −0.43 to 0.03), and when we excluded Munesue 2016 only (because it was a cross‐over study), the effect was SMD −0.21 (95% CI −0.43 to 0.01). This shows that, after removing the relevant studies, there was no longer any evidence of an effect of oxytocin.
Discussion
Summary of main results
This large review included 15 major comparisons with data from 131 studies. The major drug classes that the included studies compared to placebo were typical and atypical antipsychotics, ADHD‐related drugs, anticonvulsants, antidementia drugs, antidepressants, antiparkinsonian drugs, anxiolytics, neurohormones, and a number of drugs that did not fall into any of these classes, which we grouped under an 'experimental' category. Studies also compared atypical antipsychotics to typical antipsychotics, antidementia drugs, and antiparkinsonian drugs. They also compared three different types of antidepressants.
Antipsychotics
At short‐term follow‐up (up to 6 months), atypical antipsychotics compared with placebo probably reduce irritability (moderate‐certainty evidence) and may also reduce self‐injury (low‐certainty evidence). However, there was no clear evidence of a difference in aggression between groups (very low‐certainty evidence) in participants with ASD. Some AEs may be higher in participants who receive atypical antipsychotics. These include the neurological AEs of dizziness, fatigue, sedation, somnolence, and tremor (low‐certainty evidence), the metabolic AE of increased appetite (low‐certainty evidence), and the gastrointestinal AEs of abdominal pain, constipation, drooling, hypersalivation, and vomiting or nausea, but there was no clear evidence of a difference between groups for any of the other AEs.
Studies that investigated typical antipsychotics reported only self‐injury, with no clear evidence of a difference compared to placebo in the short term. Similarly, the two trials of typical antipsychotics versus placebo showed no clear differences in reported musculoskeletal, neurological or psychological AEs.
There was no clear evidence of a difference between typical and atypical antipsychotics on behaviours of concern or AEs.
Neurohormones
Eight studies reported irritability (466 participants). There was minimal to no clear evidence of a difference in irritability in the short term when neurohormones were compared to placebo (very low‐certainty evidence). None of the neurohormone studies reported aggression or self‐injury.
Neurohormones may reduce the risk of headaches (very low‐certainty evidence) but there were no clear differences between groups for any of the other neurological AEs. Neurohormones may decrease the rates of vomiting (low‐certainty evidence), but there were no clear differences between groups for any other gastrointestinal AEs. There were no clear differences between groups for any metabolic or psychological AEs (low‐certainty evidence), or musculoskeletal AEs (very low‐certainty evidence).
ADHD‐related medications
At short term follow‐up, ADHD‐related medications may reduce irritability when compared to placebo (low‐certainty evidence). There was no clear evidence of a difference in self‐injury between those receiving ADHD‐related medications compared to a placebo (very low‐certainty evidence). No data were reported for aggression.
We found very uncertain evidence that participants who receive ADHD‐related medications have higher rates of AEs compared to those who receive placebo. ADHD‐related medications may increase rates of drowsiness, emotion/tearfulness, fatigue, headache, insomnia, and irritability (very low‐certainty evidence) but there was no clear difference between groups for other neurological AEs: dizziness, motor tics, agitation, repetitive behaviour, or restlessness. ADHD‐related medications may increase rates of depression (very low‐certainty evidence) but there were no clear differences between groups for any of the other psychological AEs. ADHD‐related medications may lead to higher rates of decreased appetite (very low‐certainty evidence) but there were no clear differences between groups for the metabolic AEs of increased appetite or increased motor activity (very low‐certainty evidence). ADHD‐related medications may increase rates of constipation, dry mouth, and stomach or abdominal discomfort, but there were lower rates of diarrhoea in the ADHD‐related medication group compared to placebo. None of the studies in this comparison reported musculoskeletal AEs.
Antidepressants
At short‐term follow‐up, there was no clear evidence of a difference in irritability between those receiving antidepressants and those receiving placebo (low‐certainty evidence). Data for aggression and self‐injury were either not reported or could not be included in the analysis.
Antidepressants may lead to higher rates of decreased attention (low‐certainty evidence), but there was little to no difference between groups for the other neurological AEs. Antidepressants may increase rates of impulsive behaviour and stereotypy (very low‐certainty evidence) but there were no clear differences between groups for any of the other psychological AEs (very low‐certainty evidence). Antidepressants may increase the rates of decreased energy (very low‐certainty evidence) but there were no clear differences between groups for any of the other metabolic AEs. There were no clear differences between groups for any musculoskeletal AEs (very low‐certainty evidence).
Overall completeness and applicability of evidence
The included studies in this review were conducted over approximately a 30‐year period. Most of the studies were short term (less than 3 months) and as such it is unclear if these AEs and improvements would be observed beyond three months. Several antipsychotic studies did not report sedation as an AE when it is very likely to have occurred. However, sedation is usually a short‐term AE and the reporting and awareness of long‐term effects of antipsychotic use is more important considering the lack of long‐term studies and the risk of serious metabolic disorders such as diabetes mellitus and significant weight gain following antipsychotic use.
Prior to the DSM‐5 2013, the DSM did not permit a diagnosis of ADHD with an existing diagnosis of ASD or PDD‐NOS (Cortese 2012). The DSM‐5 has removed this criterion for an ADHD diagnosis (Antshel 2013; Epstein 2013). As such, there is uncertainty whether improvements in behaviours of concern with ADHD‐related medications in this review are due to improvements in concurrent ADHD symptoms that previously may not have been diagnosed in participants with ASD, rather than improvements in behaviours of concern associated with ASD.
Large studies have shown that people with ASD are at least two to three times more likely to have comorbid psychiatric conditions such as anxiety or depression (Brooks 2021; Schendel 2016; Vohra 2017). As such, there is uncertainty whether improvements in behaviours of concern observed with antipsychotics or other agents are due to improvements in undiagnosed or unreported psychiatric conditions rather than improvements in ASD‐related behaviours of concern.
The vast majority of the studies did not provide details such as severity of ASD, other diagnoses apart from ASD, or the presence of comorbid psychiatric conditions. Furthermore, only some of the studies reported baseline scores of behaviours of concern. Therefore, there are many varying factors and inconsistencies across both the population of interest and the included studies, and the heterogeneity creates a limitation in the synthesis of data.
There are also challenges associated with obtaining an accurate record of AEs in people with cognitive or communication limitations. Similarly, the outcome of quality of life is often reported by the family member or caregivers rather than self‐rated by the person with the disability. Although the studies often did not report the severity of ASD, this may introduce bias.
A lack of studies involving adults emerged as a major theme in the included trials, with only 22 of 131 trials involving adults as the target population. This highlights the need for more studies involving adults to identify the effectiveness and AEs associated with pharmacological intervention use amongst adults with ASD and behaviours of concern.
Quality of the evidence
Of the comparisons in the summary of findings tables, we downgraded the majority of results by at least one level due to study limitations (refer to Table 1; Table 2; Table 3; Table 4 for further details). Approximately only 25% of included studies appropriately detailed their random sequence generation and allocation concealment processes. The remaining studies in the review either provided insufficient information to allow us to make a judgement, or we judged them to be at high risk of bias due to 'sequential assignment' methods. We judged approximately 50% of the studies to be at either unclear or high risk of performance and detection bias. In addition, 25% to 30% of the studies were at high risk of attrition or reporting bias.
Despite the large number of included studies in this review, we downgraded many of the outcomes by at least one level due to imprecision. This was because important outcomes were often only reported by a few studies, providing a small evidence base of fewer than 200 participants. In addition, the 95% CIs of many of the results were wide and included the possibility of both benefit and harm.
As the focus of this review was the effect of these interventions on the ASD population regardless of age, we decided to downgrade some outcomes for indirectness if the only available evidence related to children, as these results may not be directly applicable to the population as a whole.
We downgraded many of the outcomes in this review due to inconsistency, based on the high I² statistic values in many of the analyses. We explored reasons for this heterogeneity via subgroup analyses, but the subjective nature of these analyses means we cannot be confident about their results, and therefore cannot attribute the high I² statistic values to these potential effect modifiers.
For many of the outcomes included in this review, it was not possible to create a funnel plot to assess publication bias due to an insufficient number of studies. When it was possible to construct these forest plots, there was no evidence of asymmetry, and therefore no reason to downgrade for publication bias.
Potential biases in the review process
Although we made every attempt to adhere to the protocol (Livingstone 2015), there remains the possibility of bias in this review process. The search was extensive, but there is a chance that we did not identify important unpublished evidence. Many of the included studies were lacking important details, and although we contacted some study authors to ask for clarification on these issues, in most cases we did not receive confirmation prior to publication. We judged many of the studies to be at unclear or high risk of bias, but we made the decision to pool together all evidence regardless of the results of the risk of bias assessment. If we had chosen to restrict analyses to low risk of bias studies only, the evidence base would be substantially smaller, but perhaps more certain. One aspect that we had not prepared for in our protocol was our choice of relevant 'adverse events'. Although we attempted to account for this post‐protocol, our ultimate choice of which AEs to prioritise may have been biased.
There are a number of included studies involving one research group that were conducted within a short period of time. We believe there are some conflicts of interests that have not been disclosed by the authors. It is also uncertain whether different participants are involved in each study due to the consistency of numbers reported and the same comparison used in all trials. We attempted to contact the study authors regarding some of these issues, but we did not receive any correspondence from the contact authors involved.
Agreements and disagreements with other studies or reviews
To our knowledge, this is the first systematic review that has assessed the effectiveness and AEs of multiple classes of drugs commonly prescribed for behaviours of concern in people with ASD. Two previous systematic reviews focused on the atypical antipsychotics aripiprazole (Ching 2012), and risperidone (Jesner 2007), and two systematic reviews focused on antidepressants, namely tricyclic antidepressants (Hurwitz 2012), and SSRIs (Williams 2013), for children and adults with ASDs.
Antipsychotics
Since the protocol for this review was published, seven systematic reviews of the effectiveness of antipsychotics in people with autism, predominantly children and adolescents, and reported behaviours of concern were published (D’Alò 2021; Fallah 2019; Fung 2016; Hirsch 2016; Maneeton 2018a; Maneeton 2018b; Mano‐Sousa 2021), in addition to the review by Jesner 2007. These included network meta‐analyses (Fallah 2019), meta‐analyses and narrative syntheses. Five of these systematic reviews were on the effectiveness of atypical antipsychotics, one systematic review was on multiple drug classes (Fung 2016), and the other review was on both typical and atypical antipsychotics (D’Alò 2021). All of these reviews involved children and adolescents, and the outcomes included irritability using the ABC‐I subscale (all reviews), aggression (Fung 2016), and AEs (all reviews). Across these reviews, as with our current review, there was evidence for the effectiveness of aripiprazole and risperidone in reducing irritability.
However, as with this current review, there was evidence for AEs across a range of systematic reviews. This included an overall increase (Alfageh 2019; D’Alò 2021), but also increased serious adverse events (D’Alò 2021), in children and adolescents with ASD.
Mean weight was also higher in trials of olanzapine, risperidone and aripiprazole (Fallah 2019; Fung 2016; Jesner 2007; Hirsch 2016; Maneeton 2018a; Mano‐Sousa 2021). Systematic reviews also found that haloperidol, risperidone, and aripiprazole were associated with somnolence or sedation (Fung 2016; Hirsch 2016; Maneeton 2018a; Maneeton 2018b). Extrapyramidal symptoms were also increased in the review by Fung 2016; and hypersalivation in the review by Maneeton 2018b.
Neurohormones
We found that neurohormones may have a minimal to small effect on behaviours of concern (irritability). In the Cochrane Review of intravenous secretin compared to a placebo treatment in children or adults diagnosed with ASD, there was no effect of secretin in any of the three studies that reported irritability (Williams 2012).
ADHD‐related medications
The current review found that there was low‐certainty evidence that overall ADHD‐related medications decreased irritability. Findings from two previous reviews did not find evidence that ADHD medications had an effect on irritability. A narrative synthesis by Ghanizadeh 2019 of clinical trials of stimulants in children and adolescents with both autism and ADHD, concluded inadequate evidence to support or refute their effect on irritability. While a Cochrane Review by Sturman 2017 found that methylphenidate did change reports of irritability that were reported as AEs in children and adolescents with ASD.
Antidepressants
We found no clear differences between antidepressants and placebo in behaviours of concern and this seems to be in line with previous evidence from trials of antidepressants.
In the Cochrane Review of SSRIs for ASD there was no evidence that fenfluramine and fluoxetine had an effect, and only limited evidence that citalopram reduced irritability (Williams 2013). In addition, citalopram and fenfluramine were associated with increased AEs.
A Cochrane Review of tricyclic antidepressants for ASD in children and adolescents also found no evidence that clomipramine or tianeptine improved irritability, although clomipramine was associated with cardiac and neurological AEs, and tianeptine with sedation (Hurwitz 2012).
A more recent systematic review by Deb 2021, found no evidence that citalopram, clomipramine, venlafaxine or the SSRI fluoxetine decreased behaviours of concern, though one of two trials of fluvoxamine reduced aggression.
Anticonvulsants
As with our findings, there is little evidence that anticonvulsants decrease behaviours of concern. In a systematic review of anticonvulsants in children and adolescents by Davico 2018, there was limited evidence of valproate having an effect on irritability and aggression in a single trial at 12 but not eight weeks, and no evidence that levetiracetam had any effect. In the narrative review by Brondino 2016 there were mixed findings with one of two trials finding no effect of valproate on aggression and irritability, while the other reported that valproate reduced irritability. Similarly, one of the two trials in the systematic review by Fung 2016 reported that valproate decreased irritability with no apparent effect in the other trial.
The review of valproate use in Brondino 2016 also reported mild side effects but no serious adverse events were reported. The review by Fung 2016 also reported that valproate was associated with weight gain.
Antiparkinsonians
As with the current review, there was no evidence that antiparkinsonians decreased behaviours of concern compared with placebo. The systematic review by Fung 2016 found no evidence that amantadine decreased irritability in the one small placebo‐controlled trial, and amantadine was also associated with somnolence and sedation.
Anxiolytics
A recent review showed contradictory findings for the effectiveness of anxiolytics on behaviours of concern. In the systematic review by Deb 2021, only one of two trials of buspirone showed a decrease in irritability. No major adverse events were reported, with the most common adverse events being changes in appetite, drowsiness, and fatigue.
Experimental
Systematic reviews were identified for several individual drugs or drug classes that we categorised as experimental for the purposes of this review. They were reviews of the GABA modulators acamprosate, arbaclofen, bumetanide, carnosine, flumazenil, riluzole and valproate in autism reviewed by Brondino 2016 (the findings with valproate are discussed under anticonvulsants); a review of riluzole by De Boer 2019; and a review of n‐acetylcysteine by Lee 2021.
As with our findings, in the systematic review by Brondino 2016, the authors concluded that there was insufficient evidence to suggest the use of the GABA modulators in autism. Though a later review of riluzole by De Boer 2019 found that riluzole decreased irritability in one trial with no apparent effect in the other trial.
In the meta‐analysis of N‐acetylcysteine by Lee 2021, there was no effect across all four identified studies in ASD, although mild AEs were reported. This was in line with our findings in this review.
Authors' conclusions
Implications for practice.
Based on data from all identified trials, atypical antipsychotics (risperidone and aripiprazole) appear to reduce behaviours of concern in people with autism spectrum disorder (ASD) by approximately 34% and attention deficit hyperactivity disorder (ADHD)‐related medications by approximately 32% in the short term. However, there was also evidence that certain adverse effects (e.g. sedation and weight gain) may be associated with their use. Consideration should be given to whether prescribing and administration is warranted given the risk of adverse events. There were inadequate data to draw conclusions about their effectiveness in the medium or long term.
There was little to no evidence of an effect of anticonvulsants, antidepressants, anxiolytics, antidementia medications, antiparkinsonian medications, neurohormones, or 'experimental' interventions on behaviours of concern (irritability, aggression or self‐injury) in the short term. In addition, there was little to no evidence of a difference in adverse effects between these intervention groups and placebo groups. There were inadequate data to draw conclusions about their effectiveness in the medium or long term.
Before considering medications to manage a person’s behaviour of concern, a comprehensive assessment to gain a functional understanding of their behaviours should be undertaken and non‐pharmacological interventions trialled, which supports the National Institute for Health and Care Excellence (NICE) guidance on interventions for people with intellectual disability and behaviours of concern (NICE 2015). In addition, clinicians should seek informed consent to use medications to manage behaviour from the person, or their substitute decision maker, and should discuss with them the risks and benefits associated with these medications to ensure that they are clearly understood.
Implications for research.
Length of follow‐up emerged as a major theme in the included studies, with only 12 studies following up participants for more than three months, one of which followed up participants for more than six months. This highlights the need for studies of longer than six months' duration to identify the long‐term health effects of pharmacological interventions in people with ASD.
Another major theme to emerge is the lack of studies involving adults; only 23 of 131 trials included adults as the target population. This highlights the need for more studies with adults to identify the effectiveness and adverse effects associated with pharmacological intervention use amongst adults with ASD and behaviours of concern.
A total of 95 (72%) of the included studies across all comparisons reported irritability as an outcome, whereas only four studies reported aggression and only 13 studies reported self‐injurious behaviour. This highlights the need for more studies to measure 'behaviour of concern' outcomes. Further, only 10 studies reported the outcome of quality of life. In addition, the consistent use of validated scales for each of these outcomes is important.
Adverse effects were reported by 110 (83%) of the studies, however, the inconsistency in reporting of adverse effects has highlighted the need for the use of consistent and validated scales particularly in relation to adverse effects associated with antipsychotic use. Consistent use of a validated adverse effect scale may lead to greater consistency in reporting and increase the relevance and usability of outcome data.
We downgraded certainty of evidence for most of the comparisons due to small sample sizes, as many of the studies included in this review involved fewer than 50 participants. Future studies should aim to involve at least 100 participants to increase the certainty of the evidence.
History
Protocol first published: Issue 7, 2015
Acknowledgements
We are very grateful for the invaluable support and advice provided to us by Cochrane Developmental, Psychosocial and Learning Problems.
We are very grateful for the advice provided to us by Deborah Caldwell on the feasibility of doing a network meta‐analysis.
-
Editorial and peer‐reviewer contributions: the following people conducted the editorial process for this article.
Sign‐off Editor (final editorial decision): Tari Turner, Cochrane Editorial Board, Cochrane Australia
Managing Editor (selected peer reviewers, collated peer‐reviewer comments, provided editorial guidance to review authors, edited the article): Samuel Hinsley, Cochrane Central Editorial Service
Editorial Assistant (conducted editorial policy checks and supported editorial team): Leticia Rodrigues, Cochrane Central Editorial Service
Copy Editor (copy editing and production): Denise Mitchell, Senior Production Editor, Cochrane Central Executive Team
Peer‐reviewers (provided comments and recommended an editorial decision): Benedetto Vitiello, M.D., University of Turin, Italy (clinical review), Robyn P. Thom, MD; Massachusetts General Hospital Lurie Center for Autism (clinical review), Lauren Ketteridge, University of Warwick (consumer review), Roses Parker, Cochrane Evidence Production and Methods Directorate, Central Editorial Service, (methods review), Jo Abbott, Cochrane Information Specialist (search review).
Appendices
Appendix 1. Search strategies used
CENTRAL
#1 [mh "child development disorders, pervasive"] #2 [mh ^"Developmental Disabilities"] #3 [mh ^"Neurodevelopmental disorders"] #4 (pervasive NEAR/3 child*) #5 pervasive NEXT development* NEXT disorder* #6 (PDD or PDDs or PDD NEXT NOS or ASD or ASDs) #7 autis* #8 asperger* #9 kanner* #10 childhood next schizophrenia #11 Rett* #12 {OR #1‐#11} #13 [mh ^"Drug therapy"] #14 ((pharma* or drug) NEAR/1 (intervention* or therap* or treat*)) #15 pharmacotherap* #16 [mh ^Psychopharmacology] #17 (psychopharmacol* or psycho next pharmacol*) #18 [mh ^"Off‐Label Use"] #19 (off next label ) #20 (novel NEAR/1 (drug* or medication* or pharma* or treatment*)) #21 (acetylcholinesterase or acetyl NEXT cholinesterase) #22 [mh ^Amisulpride] #23 (Analeptics or (Analeptic near agent*) or (Analeptic near drug*)) #24 [mh ^"Anti‐Anxiety Agents"] #25 (anxiolytic* or antianxiety NEXT agent* or antianxiety NEXT drug* or anti NEXT anxiety NEXT agent* or anti NEXT anxiety NEXT drug*) #26 [mh Anticonvulsants] #27 (Anticonvulsant* or anti next convulsant*) #28 (antiepileptic* or anti next epileptic*) #29 [mh "Antidepressive Agents"] #30 (antidepress* or anti NEXT depress*) #31 [mh "Antipsychotic Agents"] #32 (antipsychotic* or anti next psychotic*) #33 [mh "Antihypertensive Agents"] #34 [mh "Antiparkinson Agents"] #35 (antiparkinson or anti next parkinson) #36 [mh ^"Adrenergic Uptake Inhibitors"] #37 [mh ^"Atomoxetine Hydrochloride"] #38 [mh Bromocriptine] #39 [mh Buspirone] #40 [mh "Central Nervous System Stimulants"] #41 (CNS or central next nervous) next Stimulant* #42 [mh "Cholinesterase Inhibitors"] #43 Cholinesterase next Inhibitor* #44 [mh citalopram] #45 [mh Clomipramine] #46 [mh Clonidine] #47 [mh Fluoxetine] #48 [mh Fluvoxamine] #49 [mh guanfacine] #50 [mh Haloperidol] #51 [mh Imipramine] #52 [mh Levetiracetam] #53 [mh "Lurasidone Hydrochloride"] #54 [mh memantine] #55 [mh methylphenidate] #56 [mh Milnacipran] #57 mood next stabili*er* #58 (neurohormone* or neuro NEXT hormone*) #59 (NMDA NEAR/1 (antagonist* or receptor*)) #60 [mh Nortriptyline] #61 [mh oxytocin] #62 [mh Olanzapine] #63 [mh "Paliperidone Palmitate"] #64 [mh Paroxetine] #65 [mh "Quetiapine Fumarate"] #66 [mh Risperidone] #67 [mh Rivastigmine] #68 [mh Secretin] #69 [mh "Serotonin and Noradrenaline Reuptake Inhibitors"] #70 [mh "Serotonin Uptake Inhibitors"] #71 ((Serotonin NEAR/3 Uptake NEXT Inhibitor*) or (Serotonin NEAR/3 reuptake NEXT Inhibitor*) or (Serotonin NEAR/3 re NEXT uptake NEXT Inhibitor*)) #72 (SSRI or SSRIs) #73 [mh Sertraline] #74 Tetracyclic* #75 [mh Topiramate] #76 Tricyclic* #77 [mh "Venlafaxine Hydrochloride"] #78 [mh "Valproic Acid"] #79 (amantadine or amisulpride or aripiprazole or atomoxetine or bromocriptine or buspirone or Centedrin or Concerta or Daytrana or citalopram or clomipramine or clozapine or divalproex or donepezil or Equasym or escitalopram or fluoxetine or fluvoxamine or gabapentin or guanfacine or Haloperidol or imipramine or iamotrigine or lamotrigine or levetiracetam or lurasidone or memantine or Metadate or Methylin or Methylphenidat* or milnacipran or mirtazapine or nortriptyline or olanzapine or oxytocin or paliperidone or paroxetine or Phenidylate or quetiapine or risperidone or Ritalin* or rivastigmine or secretin or Sertraline or Tianeptine or Topiramate or Tsentedrin or valproate or Venlafaxine or Ziprasidone) #80 {or #13‐#79} #81 #12 and #80 in Trials
Ovid MEDLINE
1 exp child development disorders, pervasive/ 2 Developmental Disabilities/ 3 Neurodevelopmental disorders/ 4 pervasive development$ disorder$.tw,kf. 5 (pervasive adj3 child$).tw,kf. 6 (PDD or PDDs or PDD‐NOS or ASD or ASDs).tw,kf. 7 autis$.tw,kf. 8 asperger$.tw,kf. 9 kanner$.tw,kf. 10 childhood schizophrenia.tw,kf. 11 Rett$.tw,kf. 12 or/1‐11 13 Drug Therapy/ 14 ((pharma$ or drug) adj1 (intervention$ or therap$ or treat$)).tw,kf. 15 pharmacotherap$.tw,kf. 16 Psychopharmacology/ 17 (psychopharmacol$ or psycho‐pharmacol$).tw,kf. 18 "Off‐Label Use"/ 19 (off label or "off‐label").tw,kf. 20 (novel adj1 (drug$ or medication$ or pharma$ or treatment$)).tw,kf. 21 (acetylcholinesterase or acetyl‐cholinesterase).mp. 22 Amisulpride/ 23 (Analeptics or (Analeptic adj agent$) or (Analeptic adj drug$)).tw,kf. 24 Anti‐Anxiety Agents/ 25 (anxiolytic$ or antianxiety agent$ or antianxiety drug$ or anti anxiety agent$ or anti anxiety drug$).tw,kf. 26 exp Anticonvulsants/ 27 (Anticonvulsant$ or anti‐convulsant$).mp. 28 (antiepileptic$ or anti‐epileptic$).mp. 29 exp Antidepressive Agents/ 30 (antidepress$ or anti‐depress$).mp. 31 exp Antipsychotic Agents/ 32 (antipsychotic$ or anti‐psychotic$).mp. 33 exp Antihypertensive Agents/ 34 exp Antiparkinson Agents/ 35 (antiparkinson or anti‐parkinson).mp. 36 Adrenergic Uptake Inhibitors/ 37 Atomoxetine Hydrochloride/ 38 Bromocriptine/ 39 Buspirone/ 40 Central Nervous System Stimulants/ 41 CNS Stimulant$.tw,kf. 42 Cholinesterase Inhibitors/ 43 Cholinesterase Inhibitor$.tw,kf. 44 citalopram/ 45 Clomipramine/ 46 Clonidine/ 47 Fluoxetine/ 48 Fluvoxamine/ 49 guanfacine/ 50 Haloperidol/ 51 Imipramine/ 52 Levetiracetam/ (2193) 53 Lurasidone Hydrochloride/ 54 memantine/ 55 methylphenidate/ or dexmethylphenidate hydrochloride/ 56 Milnacipran/ 57 mood stabili#er$.mp. 58 (neurohormone$ or neuro hormone$).tw,kf. 59 (NMDA adj1 (antagonist$ or receptor$)).tw,kf. 60 Nortriptyline/ 61 oxytocin/ 62 Olanzapine/ 63 Paliperidone Palmitate/ 64 Paroxetine/ 65 Quetiapine Fumarate/ 66 Risperidone/ 67 Rivastigmine/ 68 Secretin/ 69 "Serotonin and Noradrenaline Reuptake Inhibitors"/ 70 Serotonin Uptake Inhibitors/ 71 ((Serotonin adj3 Uptake Inhibitor$) or (Serotonin adj3 reuptake Inhibitor$) or (Serotonin adj3 re‐uptake Inhibitor$)).tw,kf. 72 (SSRI or SSRIs).tw,kf. 73 Sertraline/ 74 Tetracyclic$.tw,kf. 75 Topiramate/ 76 Tricyclic$.tw,kf. 77 Venlafaxine Hydrochloride/ 78 Valproic Acid/ 79 (amantadine or amisulpride or aripiprazole or atomoxetine or bromocriptine or buspirone or Centedrin or Concerta or Daytrana or citalopram or clomipramine or clozapine or divalproex or donepezil or Equasym or escitalopram or fluoxetine or fluvoxamine or gabapentin or guanfacine or Haloperidol or imipramine or iamotrigine or lamotrigine or levetiracetam or lurasidone or memantine or Metadate or Methylin or Methylphenidat$ or milnacipran or mirtazapine or nortriptyline or olanzapine or oxytocin or paliperidone or paroxetine or Phenidylate or quetiapine or risperidone or Ritalin$ or rivastigmine or secretin or Sertraline or Tianeptine or Topiramate or Tsentedrin or valproate or Venlafaxine or Ziprasidone).mp. 80 or/13‐79 81 12 and 80 82 randomized controlled trial.pt. 83 controlled clinical trial.pt. 84 randomi#ed.ab. 85 placebo$.ab. 86 drug therapy.fs. 87 randomly.ab. 88 trial.ab. 89 groups.ab. 90 or/82‐89 91 exp animals/ not humans.sh. 92 90 not 91 93 81 and 92
MEDLINE In‐Process and Other Non‐Indexed Citations
1 pervasive development$ disorder$.tw,kf. 2 Developmental Disabilit$.tw,kf. 3 neurodevelopmental disorder$.tw,kf. 4 (pervasive adj3 child$).tw,kf. 5 (PDD or PDDs or PDD‐NOS or ASD or ASDs).tw,kf. 6 autis$.tw,kf. 7 asperger$.tw,kf. 8 kanner$.tw,kf. 9 childhood schizophrenia.tw,kf. 10 Rett$.tw,kf. 11 or/1‐10 12 ((pharma$ or drug) adj1 (intervention$ or therap$ or treat$)).tw,kf. 13 pharmacotherap$.tw,kf. 14 (psychopharmacol$ or psycho‐pharmacol$).tw,kf. 15 (off label or "off‐label").tw,kf. 16 (novel adj1 (drug$ or medication$ or pharma$ or treatment$)).tw,kf. 17 (acetylcholinesterase or acetyl‐cholinesterase).tw,kf. 18 (Analeptics or (Analeptic adj agent$) or (Analeptic adj drug$)).tw,kf. 19 (anxiolytic$ or antianxiety agent$ or antianxiety drug$ or anti anxiety agent$ or anti anxiety drug$).tw,kf. 20 (Anticonvulsant$ or anti‐convulsant$).tw,kf. 21 (antiepileptic$ or anti‐epileptic$).tw,kf. 22 (antidepress$ or anti‐depress$).tw,kf. 23 (antipsychotic$ or anti‐psychotic$).tw,kf. 24 (antiparkinson or anti‐parkinson).tw,kf. 25 CNS Stimulant$.tw,kf. 26 central nervous system stimulant$.tw,kf. 27 Cholinesterase Inhibitor$.tw,kf. 28 mood stabili#er$.tw,kf. 29 (neurohormone$ or neuro hormone$).tw,kf. 30 (NMDA adj1 (antagonist$ or receptor$)).tw,kf. 31 ((Serotonin adj3 Uptake Inhibitor$) or (Serotonin adj3 reuptake Inhibitor$) or (Serotonin adj3 re‐uptake Inhibitor$)).tw,kf. 32 (SSRI or SSRIs).tw,kf. 33 Tricyclic$.tw,kf. 34 (amantadine or amisulpride or aripiprazole or atomoxetine or bromocriptine or buspirone or Centedrin or Concerta or Daytrana or citalopram or clomipramine or clozapine or divalproex or donepezil or Equasym or escitalopram or fluoxetine or fluvoxamine or gabapentin or guanfacine or Haloperidol or imipramine or iamotrigine or lamotrigine or levetiracetam or lurasidone or memantine or Metadate or Methylin or Methylphenidat$ or milnacipran or mirtazapine or nortriptyline or olanzapine or oxytocin or paliperidone or paroxetine or Phenidylate or quetiapine or risperidone or Ritalin$ or rivastigmine or secretin or Sertraline or Tianeptine or Topiramate or Tsentedrin or valproate or Venlafaxine or Ziprasidone).tw,kf. 35 or/12‐34 36 11 and 35 37 (random$ or trial$ or control$ or group$ or placebo$ or blind$ or prospectiv$ or longitudinal$ or meta‐analys$ or systematic review$).tw. 38 36 and 37
MEDLINE EPub Ahead of Print
1 pervasive development$ disorder$.tw,kf. 2 Developmental Disabilit$.tw,kf. 3 neurodevelopmental disorder$.tw,kf. 4 (pervasive adj3 child$).tw,kf. 5 (PDD or PDDs or PDD‐NOS or ASD or ASDs).tw,kf. 6 autis$.tw,kf. 7 asperger$.tw,kf. 8 kanner$.tw,kf. 9 childhood schizophrenia.tw,kf. 10 Rett$.tw,kf. 11 or/1‐10 12 ((pharma$ or drug) adj1 (intervention$ or therap$ or treat$)).tw,kf. 13 pharmacotherap$.tw,kf. 14 (psychopharmacol$ or psycho‐pharmacol$).tw,kf. 15 (off label or "off‐label").tw,kf. 16 (novel adj1 (drug$ or medication$ or pharma$ or treatment$)).tw,kf. 17 (acetylcholinesterase or acetyl‐cholinesterase).tw,kf. 18 (Analeptics or (Analeptic adj agent$) or (Analeptic adj drug$)).tw,kf. 19 (anxiolytic$ or antianxiety agent$ or antianxiety drug$ or anti anxiety agent$ or anti anxiety drug$).tw,kf. 20 (Anticonvulsant$ or anti‐convulsant$).tw,kf. 21 (antiepileptic$ or anti‐epileptic$).tw,kf. 22 (antidepress$ or anti‐depress$).tw,kf. 23 (antipsychotic$ or anti‐psychotic$).tw,kf. 24 (antiparkinson or anti‐parkinson).tw,kf. 25 CNS Stimulant$.tw,kf. 26 central nervous system stimulant$.tw,kf. 27 Cholinesterase Inhibitor$.tw,kf. 28 mood stabili#er$.tw,kf. 29 (neurohormone$ or neuro hormone$).tw,kf. 30 (NMDA adj1 (antagonist$ or receptor$)).tw,kf. 31 ((Serotonin adj3 Uptake Inhibitor$) or (Serotonin adj3 reuptake Inhibitor$) or (Serotonin adj3 re‐uptake Inhibitor$)).tw,kf. 32 (SSRI or SSRIs).tw,kf. 33 Tricyclic$.tw,kf. 34 (amantadine or amisulpride or aripiprazole or atomoxetine or bromocriptine or buspirone or Centedrin or Concerta or Daytrana or citalopram or clomipramine or clozapine or divalproex or donepezil or Equasym or escitalopram or fluoxetine or fluvoxamine or gabapentin or guanfacine or Haloperidol or imipramine or iamotrigine or lamotrigine or levetiracetam or lurasidone or memantine or Metadate or Methylin or Methylphenidat$ or milnacipran or mirtazapine or nortriptyline or olanzapine or oxytocin or paliperidone or paroxetine or Phenidylate or quetiapine or risperidone or Ritalin$ or rivastigmine or secretin or Sertraline or Tianeptine or Topiramate or Tsentedrin or valproate or Venlafaxine or Ziprasidone).tw,kf. 35 or/12‐34 36 11 and 35 37 (random$ or trial$ or control$ or group$ or placebo$ or blind$ or prospectiv$ or longitudinal$ or meta‐analys$ or systematic review$).tw. 38 36 and 37
Embase Ovid
1 exp autism/ 2 developmental disorder/ 3 pervasive development$ disorder$.tw. 4 (PDD or PDDs or ASD or ASDs).tw. 5 autis$.tw. 6 asperger$.tw. 7 kanner$.tw. 8 childhood schizophreni$.tw. 9 Rett$.tw. 10 (pervasive adj3 child$).tw. 11 or/1‐10 12 drug therapy/ 13 ((pharma$ or drug) adj1 (intervention$ or therap$ or treat$)).tw,kw. 14 pharmacotherap$.tw,kw. 15 psychopharmacology/ 16 (psychopharmacol$ or psycho‐pharmacol$).tw,kw. 17 "off label drug use"/ 18 (off label or "off‐label").tw,kw. 19 (novel adj1 (drug$ or medication$ or pharma$ or treatment$)).tw,kw. 20 (acetylcholinesterase or acetyl‐cholinesterase).mp. 21 amisulpride/ 22 central stimulant agent/ 23 (Analeptics or (Analeptic adj agent$) or (Analeptic adj drug$)).tw,kw. 24 anxiolytic agent/ 25 (anxiolytic$ or antianxiety agent$ or antianxiety drug$ or anti anxiety agent$ or anti anxiety drug$).tw,kw. 26 anticonvulsive agent/ 27 (Anticonvulsant$ or anti‐convulsant$).mp. 28 (antiepileptic$ or anti‐epileptic$).mp. 29 exp antidepressant agent/ 30 (antidepress$ or anti‐depress$).mp. 31 (antipsychotic$ or anti‐psychotic$).mp. 32 exp antihypertensive agent/ 33 exp antiparkinson agent/ 34 (antiparkinson or anti‐parkinson).mp. 35 adrenergic receptor affecting agent/ ( 36 atomoxetine/ 37 bromocriptine/ 38 buspirone/ 39 central stimulant agent/ 40 ((CNS or central nervous system) adj Stimulant$).tw,kw. 41 cholinesterase inhibitor/ 42 Cholinesterase Inhibitor$.tw,kw. 43 citalopram/ 44 clomipramine/ 45 clonidine/ 46 fluoxetine/ 47 fluvoxamine/ 48 fluvoxamine maleate/ 49 guanfacine/ 50 Haloperidol/ 51 imipramine/ 52 levetiracetam/ 53 lurasidone/ 54 memantine/ 55 methylphenidate/ 56 milnacipran/ 57 mood stabilizer/ 58 mood stabili#er$.tw,kw. 59 neurohormone/ 60 (neurohormone$ or neuro hormone$).tw,kw. 61 (NMDA adj1 (antagonist$ or receptor$)).tw,kw. 62 nortriptyline/ 63 neuroleptic agent/ 64 oxytocin/ 65 Olanzapine/ 66 paliperidone/ 67 paroxetine/ 68 quetiapine/ 69 risperidone/ 70 rivastigmine/ 71 secretin/ 72 serotonin noradrenalin reuptake inhibitor/ 73 serotonin uptake inhibitor/ 74 ((Serotonin adj3 Uptake Inhibitor$) or (Serotonin adj3 reuptake Inhibitor$) or (Serotonin adj3 re‐uptake Inhibitor$)).tw,kw. 75 (SSRI or SSRIs).tw,kw. 76 sertraline/ 77 Tetracyclic$.tw,kw. 78 topiramate/ 79 Tricyclic$.tw,kw. 80 venlafaxine/ 81 valproic acid/ 82 (amantadine or amisulpride or aripiprazole or atomoxetine or bromocriptine or buspirone or Centedrin or Concerta or Daytrana or citalopram or clomipramine or clozapine or divalproex or donepezil or Equasym or escitalopram or fluoxetine or fluvoxamine or gabapentin or guanfacine or Haloperidol or imipramine or iamotrigine or lamotrigine or levetiracetam or lurasidone or memantine or Metadate or Methylin or Methylphenidat$ or milnacipran or mirtazapine or nortriptyline or olanzapine or oxytocin or paliperidone or paroxetine or Phenidylate or quetiapine or risperidone or Ritalin$ or rivastigmine or secretin or Sertraline or Tianeptine or Topiramate or Tsentedrin or valproate or Venlafaxine or Ziprasidone).mp. 83 or/12‐82 84 11 and 83 85 Randomized controlled trial/ 86 Controlled clinical study/ 87 random$.ti,ab. 88 randomization/ 89 intermethod comparison/ 90 placebo.ti,ab. 91 (compare or compared or comparison).ti. 92 ((evaluated or evaluate or evaluating or assessed or assess) and (compare or compared or comparing or comparison)).ab. 93 (open adj label).ti,ab. 94 ((double or single or doubly or singly) adj (blind or blinded or blindly)).ti,ab. 95 double blind procedure/ 96 parallel group$1.ti,ab. 97 (crossover or cross over).ti,ab. 98 ((assign$ or match or matched or allocation) adj5 (alternate or group$1 or intervention$1 or patient$1 or subject$1 or participant$1)).ti,ab. 99 (assigned or allocated).ti,ab. 100 (controlled adj7 (study or design or trial)).ti,ab. 101 (volunteer or volunteers).ti,ab. 102 human experiment/ 103 trial.ti. 104 or/85‐103 105 (random$ adj sampl$ adj7 ("cross section$" or questionnaire$1 or survey$ or database$1)).ti,ab. not (comparative study/ or controlled study/ or randomi?ed controlled.ti,ab. or randomly assigned.ti,ab.) 106 Cross‐sectional study/ not (randomized controlled trial/ or controlled clinical study/ or controlled study/ or randomi?ed controlled.ti,ab. or control group$1.ti,ab.) 107 (((case adj control$) and random$) not randomi?ed controlled).ti,ab. 108 (Systematic review not (trial or study)).ti. 109 (nonrandom$ not random$).ti,ab. 110 "Random field$".ti,ab. 111 (random cluster adj3 sampl$).ti,ab. 112 (review.ab. and review.pt.) not trial.ti. 113 "we searched".ab. and (review.ti. or review.pt.) 114 "update review".ab. 115 (databases adj4 searched).ab. 116 (rat or rats or mouse or mice or swine or porcine or murine or sheep or lambs or pigs or piglets or rabbit or rabbits or cat or cats or dog or dogs or cattle or bovine or monkey or monkeys or trout or marmoset$1).ti. and animal experiment/ 117 Animal experiment/ not (human experiment/ or human/) 118 or/105‐117 119 104 not 118 120 84 and 119
CINAHL EBSCOhost
S1 (MH "Child Development Disorders, Pervasive+") S2 (MH "Rett Syndrome") S3 (MH "Developmental Disabilities") S4 (MH "Mental Disorders Diagnosed in Childhood") S5 TI(autis* or asperger* or kanner* or "childhood schizophrenia" or Rett* or "pervasive development* disorder*" or PDD or PDDs or PDD‐NOS or ASD or ASDs) OR AB(autis* or asperger* or kanner* or "childhood schizophrenia" or Rett* or "pervasive development* disorder*" or PDD or PDDs or PDD‐NOS or ASD or ASDs) S6 S1 OR S2 OR S3 OR S4 OR S5 S7 (MH "Drug Therapy") S8 TI((pharma* or drug) N1 (intervention* or therap* or treat*)) OR AB((pharma* or drug) N1 (intervention* or therap* or treat*)) S9 TI(pharmacotherap* OR psychopharmacol* or psycho‐pharmacol*) OR AB(pharmacotherap* OR psychopharmacol* or psycho‐pharmacol*) S10 (MH "Psychopharmacology") S11 (MH "Drugs, Off‐Label") S12 TI("off label" or (novel N1 (drug* or medication* or pharma* or treatment*))) OR AB("off label" or (novel N1 (drug* or medication* or pharma* or treatment*))) S13 TI(acetylcholinesterase or acetyl‐cholinesterase) OR AB(acetylcholinesterase or acetyl‐cholinesterase) S14 (MH "Antianxiety Agents") OR (MH "Anticonvulsants") OR (MH "Antidepressive Agents+") OR (MH "Antipsychotic Agents+") OR (MH "Central Nervous System Stimulants+") S15 (MH "Antihypertensive Agents+") S16 (MH "Antiparkinson Agents") S17 (MH "Adrenergic Uptake Inhibitors") OR (MH "Serotonin Uptake Inhibitors") OR(MH "Cholinesterase Inhibitors") S18 (MH "Atomoxetine") S19 (MH "Bromocriptine") S20 (MH "Buspirone") S21 (MH "Citalopram") S22 (MH "Clomipramine") S23 (MH "Clonidine") S24 (MH "Fluoxetine") S25 (MH "Fluvoxamine Maleate") S26 (MH "Haloperidol") S27 (MH "Imipramine") S28 (MH "Memantine") S29 (MH "Methylphenidate") S30 (MH "Milnacipran Hydrochloride") S31 (MH "Nortriptyline") S32 (MH "Oxytocin") S33 (MH "Olanzapine") S34 (MH "Paliperidone") S35 (MH "Paroxetine") S36 (MH "Quetiapine") S37 (MH "Risperidone") S38 (MH "Rivastigmine") S39 (MH "Secretin") S40 (MH "Topiramate") S41 (MH "Venlafaxine") S42 (MH "Valproic Acid") S43 (MH "Sertraline Hydrochloride") S44 "(acetylcholinesterase or acetyl‐cholinesterase)" S45 (Analeptics or ("Analeptic agent*") or ("Analeptic Drug*") ) S46 (anxiolytic* or "antianxiety agent*" or "antianxiety drug*" or "anti anxiety agent*" or "anti anxiety drug*") S47 (Anticonvulsant* or "anti convulsant*") S48 (antiepileptic* or "anti epileptic*") S49 (antiepileptic* or "anti epileptic*") S50 (antidepress* or "anti depress*") S51 (antipsychotic* or "anti psychotic*") S52 (antiparkinson or "anti‐parkinson") S53 ("antiparkinson or "anti‐parkinson") S54 (CNS or "central nervous Stimulant*" ) S55 "Cholinesterase Inhibitor*" S56 ("mood stabili*er*") S57 neurohormone* or neuro‐hormone* S58 (NMDA N1 (antagonist* or receptor*)) S59 ((Serotonin N3 "Uptake Inhibitor*") or (Serotonin N3 "reuptake Inhibitor*") or ("Serotonin N3 "re‐uptake Inhibitor*")) S60 (SSRI or SSRIs) S61 Tricyclic* S62 (amantadine or amisulpride or aripiprazole or atomoxetine or bromocriptine or buspirone or Centedrin or Concerta or Daytrana or citalopram or clomipramine or clozapine or divalproex or donepezil or Equasym or escitalopram or fluoxetine or fluvoxamine or gabapentin or guanfacine or Haloperidol or imipramine or iamotrigine or lamotrigine or levetiracetam or lurasidone or memantine or Metadate or Methylin or Methylphenidat* or milnacipran or mirtazapine or nortriptyline or olanzapine or oxytocin or paliperidone or paroxetine or Phenidylate or quetiapine or risperidone or Ritalin* or rivastigmine or secretin or Sertraline or Tianeptine or Topiramate or Tsentedrin or valproate or Venlafaxine or Ziprasidone) S63 S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 OR S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 OR S52 OR S53 OR S54 OR S55 OR S56 OR S57 OR S58 OR S59 OR S60 OR S61 OR S62 S64 S6 AND S63 S65 MH ("Randomized Controlled Trials") S66 (MH "Double‐Blind Studies") S67 (MH "Single‐Blind Studies") S68 (MH "Random Assignment") S69 (MH "Pretest‐Posttest Design") S70 MH ("Cluster Sample") S71 TI (randomised OR randomized) S72 AB (random*) S73 TI (trial) S74 (MH "Sample Size") AND AB (assigned OR allocated OR control) S75 MH (Placebos) S76 PT (Randomized Controlled Trial) S77 AB (control W5 group) S78 MH ("Crossover Design") OR MH ("Comparative Studies") S79 AB (cluster W3 RCT) S80 (MH "Animals+") S81 MH ("Animal Studies") S82 TI (animal model*) S83 S80 OR S81 OR S82 S84 MH ("Human") S85 S83 NOT S84 S86 S65 OR S66 OR S67 OR S68 OR S69 OR S70 OR S71 OR S72 OR S73 OR S74 OR S75 OR S76 OR S77 OR S78 OR S79 S87 S86 NOT S85 S88 S64 AND S87
APA PsycInfo
1 exp autism spectrum disorders/ 2 neurodevelopmental disorders/ 3 Developmental disabilities/ 4 pervasive development$ disorder$.tw. 5 (pervasive adj3 child$).tw. 6 autis$.tw. 7 asperger$.tw. 8 (autis$ or ASD or ASDs).tw. 9 Rett$.tw. 10 Kanner$.tw. 11 (PDD or PDDs or PDD‐NOS or ASD or ASDs).tw. 12 childhood schizophreni$.tw. 13 or/1‐12 14 Drug Therapy/ 15 ((pharma$ or drug) adj1 (intervention$ or therap$ or treat$)).tw. 16 pharmacotherap$.tw. 17 psychopharmacology/ 18 (psychopharmacol$ or psycho‐pharmacol$).tw. 19 (off label or "off‐label").tw. 20 (novel adj1 (drug$ or medication$ or pharma$ or treatment$)).tw. 21 "prescribing (drugs)"/ 22 exp Acetylcholinesterase/ or exp Acetylcholine/ 23 (acetylcholinesterase or acetyl‐cholinesterase).mp. 24 analeptic drugs/ 25 (Analeptics or (Analeptic adj agent$) or (Analeptic adj drug$)).tw. 26 (anxiolytic$ or antianxiety agent$ or antianxiety drug$ or anti anxiety agent$ or anti anxiety drug$).tw. 27 Tranquilizing Drugs/ or sedatives/ 28 Anticonvulsive Drugs/ 29 (Anticonvulsant$ or anti‐convulsant$).tw. 30 (antiepileptic$ or anti‐epileptic$).tw. 31 Antidepressant Drugs/ or tricyclic antidepressant drugs/ 32 (antidepress$ or anti‐depress$).tw. 33 exp Neuroleptic Drugs/ 34 (antipsychotic$ or anti‐psychotic$).tw. 35 antihypertensive drugs/ 36 exp antihypertensive drugs/ 37 exp antitremor drugs/ 38 (antiparkinson or anti‐parkinson).tw. 39 atomoxetine/ 40 bromocriptine/ 41 buspirone/ 42 Cns stimulating drugs/ 43 ((Central Nervous System or CNS) adj stimulant$).tw. 44 cholinesterase inhibitors/ 45 Cholinesterase Inhibitor$.tw. 46 citalopram/ 47 chlorimipramine/ 48 clonidine/ 49 fluoxetine/ 50 fluvoxamine/ 51 haloperidol/ 52 imipramine/ 53 methylphenidate/ 54 mood stabilizers/ 55 mood stabili#er$.tw. 56 (neurohormone$ or neuro hormone$).tw. 57 (NMDA adj1 (antagonist$ or receptor$)).tw. 58 nortriptyline/ 59 oxytocin/ 60 olanzapine/ 61 paroxetine/ 62 quetiapine/ 63 risperidone/ 64 exp Serotonin Reuptake Inhibitors/ or exp Serotonin Norepinephrine Reuptake Inhibitors/ 65 neurotransmitter uptake inhibitors/ 66 ((Serotonin adj3 Uptake Inhibitor$) or (Serotonin adj3 reuptake Inhibitor$) or (Serotonin adj3 re‐uptake Inhibitor$)).tw. 67 (SSRI or SSRIs).tw. 68 Sertraline/ 69 Tetracyclic$.tw. 70 Venlafaxine/ 71 Valproic Acid/ 72 (amantadine or amisulpride or aripiprazole or atomoxetine or bromocriptine or buspirone or Centedrin or Concerta or Daytrana or citalopram or clomipramine or clozapine or divalproex or donepezil or Equasym or escitalopram or fluoxetine or fluvoxamine or gabapentin or guanfacine or Haloperidol or imipramine or iamotrigine or lamotrigine or levetiracetam or lurasidone or memantine or Metadate or Methylin or Methylphenidat$ or milnacipran or mirtazapine or nortriptyline or olanzapine or oxytocin or paliperidone or paroxetine or Phenidylate or quetiapine or risperidone or Ritalin$ or rivastigmine or secretin or Sertraline or Tianeptine or Topiramate or Tsentedrin or valproate or Venlafaxine or Ziprasidone).mp. 73 or/14‐72 74 13 and 73 75 clinical trials/ 76 longitudinal studies/ 77 exp program evaluation/ 78 exp Treatment Effectiveness Evaluation/ 79 random$.tw. 80 ((singl$ or doubl$ or trebl$ or tripl$) adj (blind$ or mask$)).tw. 81 (crossover$ or "cross over$").tw. 82 trial$.tw. 83 group$.ab. 84 treatment effectiveness evaluation/ 85 ((singl$ or doubl$ or tripl$ or trebl$) adj1 (blind$ or mask$)).tw. 86 prospective.tw. (60764) 87 factorial$.tw. 88 random$.tw. 89 (assign$ or allocat$).ab. 90 control.ab. 91 treatment as usual.ab. 92 placebo.ab. 93 (crossover or cross‐over).tw. 94 ((effectiveness or evaluat$) adj3 (stud$ or research$)).tw. 95 or/75‐94 96 74 and 95
ERIC EBSCOhost
S1 DE "Developmental Disabilities" S2 DE "Pervasive Developmental Disorders" OR DE "Asperger Syndrome" OR DE "Autism" S3 (pervasive development* disorder* or PDD or PDDs) S4 (autis* or ASD or ASDs) S5 Asperger* S6 Rett* S7 Kanner* S8 childhood schizophren* S9 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 S10 DE "Pharmacology" S11 (anxiolytic* or "antianxiety agent*" or "antianxiety drug*" or "anti anxiety agent*" or "anti anxiety drug*") S12 (Anticonvulsant* or "anti convulsant*") S13 (antiepileptic* or "anti epileptic*") S14 (antidepress* or "anti depress*") S15 (antipsychotic* or "anti psychotic*") S16 (antiparkinson or "anti‐parkinson") S17 (CNS or "central nervous Stimulant*" ) S18 "Cholinesterase Inhibitor*" S19 ("mood stabili*er*") S20 neurohormone* or neuro‐hormone* S21 (NMDA N1 (antagonist* or receptor*)) S22 ((Serotonin N3 "Uptake Inhibitor*") or (Serotonin N3 "reuptake Inhibitor*") or ("Serotonin N3 "re‐uptake Inhibitor*")) S23 (SSRI or SSRIs) S24 Tricyclic* S25 (amantadine or amisulpride or aripiprazole or atomoxetine or bromocriptine or buspirone or Centedrin or Concerta or Daytrana or citalopram or clomipramine or clozapine or divalproex or donepezil or Equasym or escitalopram or fluoxetine or fluvoxamine or gabapentin or guanfacine or Haloperidol or imipramine or iamotrigine or lamotrigine or levetiracetam or lurasidone or memantine or Metadate or Methylin or Methylphenidat* or milnacipran or mirtazapine or nortriptyline or olanzapine or oxytocin or paliperidone or paroxetine or Phenidylate or quetiapine or risperidone or Ritalin* or rivastigmine or secretin or Sertraline or Tianeptine or Topiramate or Tsentedrin or valproate or Venlafaxine or Ziprasidone) S26 S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 S27 S9 AND S26 S28 DE "Randomized Controlled Trials" S29 RCT* S30 *randomly or randomi*ed) N3 (allocated* or assign* or group* ) S31 control group* or experimental group* S32 placebo* or "treatment as usual" or TAU S33 S28 OR S29 OR S30 OR S31 OR S32 S34 S27 AND S33
Epistemonikos
title:(( amantadine OR amisulpride OR aripiprazole OR atomoxetine OR bromocriptine OR buspirone OR Centedrin OR Concerta OR Daytrana OR citalopram OR clomipramine OR clozapine OR divalproex OR donepezil OR Equasym OR escitalopram OR fluoxetine OR fluvoxamine OR gabapentin OR guanfacine OR Haloperidol OR imipramine OR iamotrigine OR lamotrigine OR levetiracetam OR lurasidone OR memantine OR Metadate OR Methylin OR Methylphenidat$ OR milnacipran OR mirtazapine OR nortriptyline OR olanzapine OR oxytocin OR paliperidone OR paroxetine OR Phenidylate OR quetiapine OR risperidone OR Ritalin$ OR rivastigmine OR secretin OR Sertraline OR Tianeptine OR Topiramate OR Tsentedrin OR valproate OR Venlafaxine OR Ziprasidone)) OR abstract:(( amantadine OR amisulpride OR aripiprazole OR atomoxetine OR bromocriptine OR buspirone OR Centedrin OR Concerta OR Daytrana OR citalopram OR clomipramine OR clozapine OR divalproex OR donepezil OR Equasym OR escitalopram OR fluoxetine OR fluvoxamine OR gabapentin OR guanfacine OR Haloperidol OR imipramine OR iamotrigine OR lamotrigine OR levetiracetam OR lurasidone OR memantine OR Metadate OR Methylin OR Methylphenidat$ OR milnacipran OR mirtazapine OR nortriptyline OR olanzapine OR oxytocin OR paliperidone OR paroxetine OR Phenidylate OR quetiapine OR risperidone OR Ritalin$ OR rivastigmine OR secretin OR Sertraline OR Tianeptine OR Topiramate OR Tsentedrin OR valproate OR Venlafaxine OR Ziprasidone))) OR title:(drug* OR pharma* OR medic*) AND (title:(ASD OR autis* OR asperg* OR rett* OR pervasive OR PDD*) OR abstract:(ASD OR autis* OR asperg* OR rett* OR pervasive OR PDD*))
Science Citation Index‐ Expanded Web of Science, Clarivate
# 26 #25 AND #22 # 25 #24 OR #23 # 24 ab=(randomi*sed or randomly or trial* or control* or RCT or placebo* or blind* or "treatment as usual" or TAU) # 23 ti=(random* or trial* or control* or RCT ) # 22 #21 AND #1 # 21 #20 OR #19 OR #18 OR #17 OR #16 OR #15 OR #14 OR #13 OR #12 OR #11 OR #10 OR #9 OR #8 OR #7 OR #6 OR #5 OR #4 OR #3 OR #2 # 20 ti=(amantadine or amisulpride or aripiprazole or atomoxetine or bromocriptine or buspirone or Centedrin or Concerta or Daytrana or citalopram or clomipramine or clozapine or divalproex or donepezil or Equasym or escitalopram or fluoxetine or fluvoxamine or gabapentin or guanfacine or Haloperidol or imipramine or iamotrigine or lamotrigine or levetiracetam or lurasidone or memantine or Metadate or Methylin or Methylphenidat* or milnacipran or mirtazapine or nortriptyline or olanzapine or oxytocin or paliperidone or paroxetine or Phenidylate or quetiapine or risperidone or Ritalin* or rivastigmine or secretin or Sertraline or Tianeptine or Topiramate or Tsentedrin or valproate or Venlafaxine or Ziprasidone) OR ab=(amantadine or amisulpride or aripiprazole or atomoxetine or bromocriptine or buspirone or Centedrin or Concerta or Daytrana or citalopram or clomipramine or clozapine or divalproex or donepezil or Equasym or escitalopram or fluoxetine or fluvoxamine or gabapentin or guanfacine or Haloperidol or imipramine or iamotrigine or lamotrigine or levetiracetam or lurasidone or memantine or Metadate or Methylin or Methylphenidat* or milnacipran or mirtazapine or nortriptyline or olanzapine or oxytocin or paliperidone or paroxetine or Phenidylate or quetiapine or risperidone or Ritalin* or rivastigmine or secretin or Sertraline or Tianeptine or Topiramate or Tsentedrin or valproate or Venlafaxine or Ziprasidone) # 19 ti=(Tricyclic*) or ab=(Tricyclic*) # 18 ti=(SSRI or SSRIs) or ab=(SSRI or SSRIs) # 17 ti=((Serotonin Near/3 "Uptake Inhibitor*") or (Serotonin Near/3 "reuptake Inhibitor*") or (Serotonin Near/3 "re‐uptake Inhibitor*") ) or ab=((Serotonin Near/3 "Uptake Inhibitor*") or (Serotonin Near/3 "reuptake Inhibitor*") or (Serotonin Near/3 "re‐uptake Inhibitor*") ) # 16 ti=(NMDA Near/0 (antagonist* or receptor*) ) or ab=(NMDA Near/0 (antagonist* or receptor*) ) # 15 ti=(neurohormone* or "neuro hormone*") or ab=(neurohormone* or "neuro hormone*") # 14 ti=("mood stabili*er*") or ab=("mood stabili*er*") # 13 ti=("Cholinesterase Inhibitor*") or ab=("Cholinesterase Inhibitor*") # 12 ti=("central nervous system stimulant*" or "CNS stimulant*") or ab=("central nervous system stimulant*" or "CNS stimulant*") # 11 ti=(antiparkinson or "anti parkinson") or ab=(antiparkinson or "anti parkinson") # 10 ti=(antipsychotic* or "anti psychotic*") or ab=(antipsychotic* or "anti psychotic*") # 9 ti=(antidepress* or "anti depress*") or ab=(antidepress* or "anti depress*") # 8 ti=(Anticonvulsant* or "anti convulsant*") or ab=(Anticonvulsant* or "anti convulsant*") # 7 ti=(anxiolytic* or "antianxiety agent*" or "antianxiety drug*" or "anti anxiety agent*" or "anti anxiety drug*") or ab=(anxiolytic* or "antianxiety agent*" or "antianxiety drug*" or "anti anxiety agent*" or "anti anxiety drug*") # 6 ti=(Analeptics or "Analeptic agent*" or "Analeptic drug*") or ab=(Analeptics or "Analeptic agent*" or "Analeptic drug*") # 5 ti=(acetylcholinesterase or "acetyl cholinesterase") or ab=(acetylcholinesterase or "acetyl cholinesterase") # 4 ti=("off label" or (novel NEAR/0 (drug* or medication* or pharma* or treatment*) )) OR ab=("off label" or (novel NEAR/0 (drug* or medication* or pharma* or treatment*) )) # 3 TI=(pharmacotherap* or psychopharmacol* or "psycho‐pharmacol*") or AB=(pharmacotherap* or psychopharmacol* or "psycho‐pharmacol*") # 2 TI=((pharma* or drug) Near/1 (intervention* or therap* or treat*) ) or AB=((pharma* or drug) Near/1 (intervention* or therap* or treat*) ) # 1 ti=(autis* or asperg* or Rett* or kanner* or "childhood schizophrenia" or "pervasive development* disorder*" or PDD or PDDs or "PDD‐NOS" or ASD or ASDs) OR ab=(autis* or asperg* or Rett* or kanner* or "childhood schizophrenia" or "pervasive development* disorder*" or PDD or PDDs or "PDD‐NOS" or ASD or ASDs)
Conference Proceedings Citation Index (Science ), Web of Science, Clarivate
# 26 #25 AND #22 # 25 #24 OR #23 # 24 ab=(randomi*sed or randomly or trial* or control* or RCT or placebo* or blind* or "treatment as usual" or TAU) # 23 ti=(random* or trial* or control* or RCT ) # 22 #21 AND #1 # 21 #20 OR #19 OR #18 OR #17 OR #16 OR #15 OR #14 OR #13 OR #12 OR #11 OR #10 OR #9 OR #8 OR #7 OR #6 OR #5 OR #4 OR #3 OR #2 # 20 ti=(amantadine or amisulpride or aripiprazole or atomoxetine or bromocriptine or buspirone or Centedrin or Concerta or Daytrana or citalopram or clomipramine or clozapine or divalproex or donepezil or Equasym or escitalopram or fluoxetine or fluvoxamine or gabapentin or guanfacine or Haloperidol or imipramine or iamotrigine or lamotrigine or levetiracetam or lurasidone or memantine or Metadate or Methylin or Methylphenidat* or milnacipran or mirtazapine or nortriptyline or olanzapine or oxytocin or paliperidone or paroxetine or Phenidylate or quetiapine or risperidone or Ritalin* or rivastigmine or secretin or Sertraline or Tianeptine or Topiramate or Tsentedrin or valproate or Venlafaxine or Ziprasidone) OR ab=(amantadine or amisulpride or aripiprazole or atomoxetine or bromocriptine or buspirone or Centedrin or Concerta or Daytrana or citalopram or clomipramine or clozapine or divalproex or donepezil or Equasym or escitalopram or fluoxetine or fluvoxamine or gabapentin or guanfacine or Haloperidol or imipramine or iamotrigine or lamotrigine or levetiracetam or lurasidone or memantine or Metadate or Methylin or Methylphenidat* or milnacipran or mirtazapine or nortriptyline or olanzapine or oxytocin or paliperidone or paroxetine or Phenidylate or quetiapine or risperidone or Ritalin* or rivastigmine or secretin or Sertraline or Tianeptine or Topiramate or Tsentedrin or valproate or Venlafaxine or Ziprasidone) # 19 ti=(Tricyclic*) or ab=(Tricyclic*) # 18 ti=(SSRI or SSRIs) or ab=(SSRI or SSRIs) # 17 ti=((Serotonin Near/3 "Uptake Inhibitor*") or (Serotonin Near/3 "reuptake Inhibitor*") or (Serotonin Near/3 "re‐uptake Inhibitor*") ) or ab=((Serotonin Near/3 "Uptake Inhibitor*") or (Serotonin Near/3 "reuptake Inhibitor*") or (Serotonin Near/3 "re‐uptake Inhibitor*") ) # 16 ti=(NMDA Near/0 (antagonist* or receptor*) ) or ab=(NMDA Near/0 (antagonist* or receptor*) ) # 15 ti=(neurohormone* or "neuro hormone*") or ab=(neurohormone* or "neuro hormone*") # 14 ti=("mood stabili*er*") or ab=("mood stabili*er*") # 13 ti=("Cholinesterase Inhibitor*") or ab=("Cholinesterase Inhibitor*") # 12 ti=("central nervous system stimulant*" or "CNS stimulant*") or ab=("central nervous system stimulant*" or "CNS stimulant*") # 11 ti=(antiparkinson or "anti parkinson") or ab=(antiparkinson or "anti parkinson") # 10 ti=(antipsychotic* or "anti psychotic*") or ab=(antipsychotic* or "anti psychotic*") # 9 ti=(antidepress* or "anti depress*") or ab=(antidepress* or "anti depress*") # 8 ti=(Anticonvulsant* or "anti convulsant*") or ab=(Anticonvulsant* or "anti convulsant*") # 7 ti=(anxiolytic* or "antianxiety agent*" or "antianxiety drug*" or "anti anxiety agent*" or "anti anxiety drug*") or ab=(anxiolytic* or "antianxiety agent*" or "antianxiety drug*" or "anti anxiety agent*" or "anti anxiety drug*") # 6 ti=(Analeptics or "Analeptic agent*" or "Analeptic drug*") or ab=(Analeptics or "Analeptic agent*" or "Analeptic drug*") # 5 ti=(acetylcholinesterase or "acetyl cholinesterase") or ab=(acetylcholinesterase or "acetyl cholinesterase") # 4 ti=("off label" or (novel NEAR/0 (drug* or medication* or pharma* or treatment*) )) OR ab=("off label" or (novel NEAR/0 (drug* or medication* or pharma* or treatment*) )) # 3 TI=(pharmacotherap* or psychopharmacol* or "psycho‐pharmacol*") or AB=(pharmacotherap* or psychopharmacol* or "psycho‐pharmacol*") # 2 TI=((pharma* or drug) Near/1 (intervention* or therap* or treat*) ) or AB=((pharma* or drug) Near/1 (intervention* or therap* or treat*) ) # 1 ti=(autis* or asperg* or Rett* or kanner* or "childhood schizophrenia" or "pervasive development* disorder*" or PDD or PDDs or "PDD‐NOS" or ASD or ASDs) OR ab=(autis* or asperg* or Rett* or kanner* or "childhood schizophrenia" or "pervasive development* disorder*" or PDD or PDDs or "PDD‐NOS" or ASD or ASDs)
Cochrane Database of Systematic Reviews
ID Search #1 [mh "child development disorders, pervasive"] #2 [mh ^"Developmental Disabilities"] #3 [mh ^"Neurodevelopmental disorders"] #4 (pervasive NEAR/3 child*):ti,ab,kw #5 (pervasive NEXT development* NEXT disorder*):ti,ab,kw #6 (PDD or PDDs or PDD NEXT NOS or ASD or ASDs):ti,ab,kw #7 autis*:ti,ab,kw #8 asperger*:ti,ab,kw #9 kanner*:ti,ab,kw #10 childhood next schizophrenia:ti,ab,kw #11 Rett*:ti,ab,kw #12 {OR #1‐#11} #13 [mh ^"Drug therapy"] #14 ((pharma* or drug) NEAR/1 (intervention* or therap* or treat*)):ti,ab,kw #15 pharmacotherap*:ti,ab,kw #16 [mh ^Psychopharmacology] #17 (psychopharmacol* or psycho next pharmacol*):ti,ab,kw #18 [mh ^"Off‐Label Use"] #19 (off next label ):ti,ab,kw #20 (novel NEAR/1 (drug* or medication* or pharma* or treatment*)):ti,ab,kw #21 (acetylcholinesterase or acetyl NEXT cholinesterase):ti,ab,kw #22 [mh ^Amisulpride] #23 (Analeptics or (Analeptic near agent*) or (Analeptic near drug*)):ti,ab,kw #24 [mh ^"Anti‐Anxiety Agents"] #25 (anxiolytic* or antianxiety NEXT agent* or antianxiety NEXT drug* or anti NEXT anxiety NEXT agent* or anti NEXT anxiety NEXT drug*):ti,ab,kw #26 [mh Anticonvulsants] #27 (Anticonvulsant* or anti next convulsant*):ti,ab,kw #28 (antiepileptic* or anti next epileptic*):ti,ab,kw #29 [mh "Antidepressive Agents"] #30 (antidepress* or anti NEXT depress*) #31 [mh "Antipsychotic Agents"] #32 (antipsychotic* or anti next psychotic*):ti,ab,kw #33 [mh "Antihypertensive Agents"] #34 [mh "Antiparkinson Agents"] #35 (antiparkinson or anti next parkinson):ti,ab,kw #36 [mh ^"Adrenergic Uptake Inhibitors"] #37 [mh ^"Atomoxetine Hydrochloride"] #38 [mh Bromocriptine] #39 [mh Buspirone] #40 [mh "Central Nervous System Stimulants"] #41 ((CNS or central next nervous) next Stimulant*):ti,ab,kw #42 [mh "Cholinesterase Inhibitors"] #43 (Cholinesterase next Inhibitor*):ti,ab,kw #44 [mh citalopram] #45 [mh Clomipramine] #46 [mh Clonidine] #47 [mh Fluoxetine] #48 [mh Fluvoxamine] #49 [mh guanfacine] #50 [mh Haloperidol] #51 [mh Imipramine] #52 [mh Levetiracetam] #53 [mh "Lurasidone Hydrochloride"] #54 [mh memantine] #55 [mh methylphenidate] #56 [mh Milnacipran] #57 (mood next stabili*er*):ti,ab,kw #58 (neurohormone* or neuro NEXT hormone*):ti,ab,kw #59 (NMDA NEAR/1 (antagonist* or receptor*)):ti,ab,kw #60 [mh Nortriptyline] #61 [mh oxytocin] #62 [mh Olanzapine] #63 [mh "Paliperidone Palmitate"] #64 [mh Paroxetine] #65 [mh "Quetiapine Fumarate"] #66 [mh Risperidone] #67 [mh Rivastigmine] #68 [mh Secretin] #69 [mh "Serotonin and Noradrenaline Reuptake Inhibitors"] #70 [mh "Serotonin Uptake Inhibitors"] #71 ((Serotonin NEAR/3 Uptake NEXT Inhibitor*) or (Serotonin NEAR/3 reuptake NEXT Inhibitor*) or (Serotonin NEAR/3 re NEXT uptake NEXT Inhibitor*)):ti,ab,kw #72 (SSRI or SSRIs):ti,ab,kw #73 [mh Sertraline] #74 Tetracyclic*:ti,ab,kw #75 [mh Topiramate] #76 Tricyclic*:ti,ab,kw #77 [mh "Venlafaxine Hydrochloride"] #78 [mh "Valproic Acid"] #79 (amantadine or amisulpride or aripiprazole or atomoxetine or bromocriptine or buspirone or Centedrin or Concerta or Daytrana or citalopram or clomipramine or clozapine or divalproex or donepezil or Equasym or escitalopram or fluoxetine or fluvoxamine or gabapentin or guanfacine or Haloperidol or imipramine or iamotrigine or lamotrigine or levetiracetam or lurasidone or memantine or Metadate or Methylin or Methylphenidat* or milnacipran or mirtazapine or nortriptyline or olanzapine or oxytocin or paliperidone or paroxetine or Phenidylate or quetiapine or risperidone or Ritalin* or rivastigmine or secretin or Sertraline or Tianeptine or Topiramate or Tsentedrin or valproate or Venlafaxine or Ziprasidone):ti,ab,kw #80 {or #13‐#79} #81 #12 and #80 in Cochrane Reviews, Cochrane Protocols
LILACS (lilacs.bvsalud.org/en/)
(ti:((drug* OR pharma* OR medic*) AND (asd OR autis* OR asperg* OR rett* OR pervasive OR pdd*))) OR (( amantadine OR amisulpride OR aripiprazole OR atomoxetine OR bromocriptine OR buspirone OR centedrin OR concerta OR daytrana OR citalopram OR clomipramine OR clozapine OR divalproex OR donepezil OR equasym OR escitalopram OR fluoxetine OR fluvoxamine OR gabapentin OR guanfacine OR haloperidol OR imipramine OR iamotrigine OR lamotrigine OR levetiracetam OR lurasidone OR memantine OR metadate OR methylin OR methylphenidat* OR milnacipran OR mirtazapine OR nortriptyline OR olanzapine OR oxytocin OR paliperidone OR paroxetine OR phenidylate OR quetiapine OR risperidone OR ritalin* OR rivastigmine OR secretin OR sertraline OR tianeptine OR topiramate OR tsentedrin OR valproate OR venlafaxine OR ziprasidone) AND (asd OR autis* OR asperg* OR rett* OR pervasive OR pdd*)) AND ( db:("LILACS") AND type_of_study:("clinical_trials"))
Sociological Abstracts (Proquest)
(SU.EXACT("Medications") OR( Psychopharmacology OR Amantadine OR Anticonvulsants OR Antidepressive Agents OR Antipsychotic Agents OR Antihypertensive Agents OR Antiparkinson Agents OR Central Nervous System Agents OR Cholinesterase Inhibitors OR Citalopram OR Clomipramine OR Clonidine OR Clozapine OR Fluoxetine OR Fluvoxamine OR Gabapentin OR Guanfacine OR Haloperidol OR Imipramine OR Memantine OR Nortriptyline OR Paroxetine OR Risperidone OR Serotonin Uptake Inhibitors OR Sertraline) OR (pharmacotherap* OR Amantadine OR Aripiprazole OR Cholinesterase Inhibitor* OR Citalopram OR Citalopram OR Clomipramine OR Clonidine OR Clozapine OR Divalproex OR Donepezil OR Escitalopram OR Fluoxetine OR Fluvoxamine OR Gabapentin OR Guanfacine OR Haloperidol OR Imipramine OR Lamotrigine OR Memantine OR Mirtazapine OR Nortriptyline OR Olanzapine OR Paliperidone OR Paroxetine OR Quetiapine OR Risperidone OR Rivastigmine OR Serotonin OR Sertraline OR Tetracyclic* OR Tianeptine OR Tricyclic* OR Venlafaxine OR Ziprasidone) OR ((pharma* OR drug) NEAR/1 (intervention* OR therap* OR treat*)) OR (psychopharmacol* OR psycho‐pharmacol*) OR (off label OR "off‐label") OR (novel NEAR/1 (drug* OR medication* OR pharma* OR treatment*)) OR (Anticonvulsant* OR anti‐convulsant* OR antiepileptic* OR anti‐epileptic* OR antidepress* OR anti‐depress* OR antipsychotic* OR anti‐psychotic* OR antiparkinson OR anti‐parkinson OR acetylcholinesterase OR acetyl‐cholinesterase) OR ("mood stabiliser" OR "mood stabilizer") OR (mood stabiliser) OR (mood stabilizer) OR (NMDA NEAR/1 (antagonist* OR receptor*)) OR (NMDA NEAR/1 antagonist*) OR (SSRI OR SSRIs) ) AND ((randomized controlled trial) OR (controlled clinical trial) OR (randomised OR randomized) OR placebo* OR (drug therapy) OR ab(randomly) OR ab(trial) OR ab(groups)) AND (su(child development disorders, pervasive) OR su(Developmental Disabilities) OR (PDD OR PDDs OR PDD‐NOS OR ASD OR ASDs) OR (pervasive development* disorder*) OR (pervasive NEAR/3 child*) OR (autis* OR asperger* OR kanner* OR Rett*) OR (childhood schizophrenia))
ClinicalTrials.gov
Advanced search
53 Studies found for: Interventional Studies | Autism OR Autism Spectrum Disorder OR ASPERGER OR RETT OR PDD‐NOS OR PERVASIVE DEVELOPMENT DISORDER | amantadine OR amisulpride OR aripiprazole OR atomoxetine OR bromocriptine OR buspirone OR Centedrin OR Concerta OR Daytrana OR citalopram OR clomipramine OR clozapine OR divalproex OR donepezil OR Equasym OR escitalopram OR fluoxetin
26 Studies found for: Interventional Studies | Autism OR Autism Spectrum Disorder OR ASPERGER OR RETT OR PDD‐NOS OR PERVASIVE DEVELOPMENT DISORDER | fluvoxamine OR gabapentin OR guanfacine OR Haloperidol OR imipramine OR iamotrigine OR lamotrigine OR levetiracetam OR lurasidone OR memantine OR Metadate OR Methylin OR Methylphenidate OR milnacipran OR mirtazapine OR nortriptyline
78 Studies found for: Interventional Studies | Autism OR Autism Spectrum Disorder OR ASPERGER OR RETT OR PDD‐NOS OR PERVASIVE DEVELOPMENT DISORDER | olanzapine OR oxytocin OR paliperidone OR paroxetine OR Phenidylate OR quetiapine OR risperidone OR Ritalin* OR rivastigmine OR secretin OR Sertraline OR Tianeptine OR Topiramate OR Tsentedrin OR valproate OR Venlafaxine OR Ziprasidone
29 Studies found for: Interventional Studies | Autism OR Autism Spectrum Disorder OR ASPERGER OR RETT OR PDD‐NOS OR PERVASIVE DEVELOPMENT DISORDER | drug OR pharmacological OR medicine
WHO ICTRP
The WHO ICTRP site was affected by heavy search traffic in November 2020 due to COVID, therefore an abbreviated form of the search was used.
BASIC SEARCH
autism AND amantadine OR autism AND amisulpride OR autism AND aripiprazole OR autism AND atomoxetine OR autism AND bromocriptine OR autism AND buspirone OR autism AND Centedrin OR autism AND Concerta OR autism AND Daytrana OR autism AND citalopram OR autism AND clomipramine OR autism AND clozapine OR autism AND divalproex OR autism AND donepezil OR autism AND Equasym OR autism AND escitalopram OR autism AND fluoxetin [49 RECORDS]
Autism AND fluvoxamine OR Autism AND gabapentin OR Autism AND guanfacine OR Autism AND Haloperidol OR Autism AND imipramine OR Autism AND iamotrigine OR Autism AND lamotrigine OR Autism AND levetiracetam OR Autism AND lurasidone OR Autism AND memantine OR Autism AND Metadate OR Autism AND Methylin OR Autism AND Methylphenidate OR Autism AND milnacipran OR Autism AND mirtazapine OR Autism AND nortriptyline [34 records]
Autism AND olanzapine OR Autism AND oxytocin OR Autism AND paliperidone OR Autism AND paroxetine OR Autism AND Phenidylate OR Autism AND quetiapine OR Autism AND risperidone OR Autism AND Ritalin OR Autism AND rivastigmine OR Autism AND secretin OR Autism AND Sertraline OR Autism AND Tianeptine OR Autism AND Topiramate OR Autism AND Tsentedrin OR Autism AND valproate OR Autism AND Venlafaxine OR Autism AND Ziprasidone [145 records]
Searching other resources
We contacted study authors when outcomes relevant to this review were either not reported fully or were reported using data not suitable for use in systematic reviews. Where contact details were no longer valid (such as an email bouncing) we made further attempts to find up‐to‐date details of the relevant researchers. We tried to contact study authors at least twice to request further information and noted if a reply had not been received. We requested information regarding the following studies.
| Study ID | Contact person |
| Asabadadi 2013 | Shahin Akhondzadeh |
| Belsito 2001 | Karin Belsito |
| Chugani 2016 | Diane Chugani |
| Ghaleiha 2013 | Shahin Akhondzadeh |
| Ghaleiha 2015 | Shahin Akhondzadeh |
| Ghaleiha 2016 | Shahin Akhondzadeh |
| Handen 2000 | Benjamin Handen |
| Handen 2005 | Benjamin Handen |
| Handen 2008 | Benjamin Handen |
| Handen 2011 | Benjamin Handen |
| Hollander 2012 | Eric Hollander |
| Evdokia Anagnostou | |
| Kern 2001a | Janet Kern |
| Kern 2002 | Janet Kern |
| KIng 2001 | Bryan King |
| Mace 2001 | Nathan Blum |
| McDougle 1996 | Christopher McDougle |
| Miral 2008 | Suha Miral |
| Mohammadi 2013 | Shahin Akhondzadeh |
| Molloy 2002 | Cynthia Molloy |
| Mouti 2014 | Molly O’Sullivan |
| Dinah Reddihough | |
| Munesue 2016 | Toshio Munesue |
| Nagaraj 2006 | Ravishankar Nagaraj |
| Nikoo 2015 | Shahin Akhondzadeh |
| Noone 2014 | Rachel Noone |
| Novotny 2004 | Eric Hollander |
| Posey 2005 | David Posey |
| Remington 2001 | Gary Remington |
| Rezaei 2010 | Shahin Akhondzadeh |
| Sandler 1999 | Adrian Sandler |
| Wasserman 2006 | Stacey Wasserman |
| Evdokia Anagnostou |
Appendix 2. Original search strategy
Ovid MEDLINE search strategy
1 exp child development disorders, pervasive/
2 Developmental Disabilities/
3 pervasive development$ disorder$.tw.
4 (pervasive adj3 child$).tw.
5 (PDD or PDDs or PDD‐NOS or ASD or ASDs).tw.
6 autis$.tw.
7 asperger$.tw.
8 kanner$.tw.
9 childhood schizophrenia.tw.
10 Rett$.tw.
11 or/1‐10
12 Drug Therapy/
13 ((pharma$ or drug) adj1 (intervention$ or therap$ or treat$)).tw.
14 pharmacotherap$.tw. 15 Psychopharmacology/ 16 (psychopharmacol$ or psycho‐pharmacol$).tw. 17 “Off‐Label Use”/ 18 (off label or “off‐label”).tw. 19 (novel adj1 (drug$ or medication$ or pharma$ or treatment$)).tw. 20 Amantadine/ 21 Amantadine.mp. 22 exp Anticonvulsants/ 23 (Anticonvulsant$ or anti‐convulsant$).mp. 24 (antiepileptic$ or anti‐epileptic$).mp. 25 exp Antidepressive Agents/ 26 (antidepress$ or anti‐depress$).mp. 27 exp Antipsychotic Agents/ 28 (antipsychotic$ or anti‐psychotic$).mp. 29 exp Antihypertensive Agents/ 30 exp Antiparkinson Agents/ 31 (antiparkinson or anti‐parkinson).mp. 32 Aripiprazole.mp. 33 Central Nervous System Agents/ 34 Cholinesterase Inhibitors/ 35 Cholinesterase Inhibitor$.mp. 36 (acetylcholinesterase or acetyl‐cholinesterase).mp. 37 citalopram/ 38 citalopram.mp. 39 Clomipramine/ 40 Clomipramine.mp. 41 Clonidine/ 42 Clonidine.mp. 43 Clozapine/ 44 Clozapine.mp. 45 divalproex.mp. 46 donepezil.mp. 47 Escitalopram.mp. 48 Fluoxetine/ 49 Fluoxetine.mp. 50 Fluvoxamine/ 51 Fluvoxamine.mp. 52 gabapentin.mp. 53 guanfacine/ 54 guanfacine.mp. 55 Haloperidol/ 56 Haloperidol.mp. 57 Imipramine/ 58 Imipramine.mp. 59 lamotrigine.mp. 60 memantine/ 61 memantine.mp. 62 Mirtazapine.mp. 63 mood stabili#er$.mp. 64 (NMDA adj1 (antagonist$ or receptor$)).mp. 65 Nortriptyline/ 66 Nortriptyline.mp.
67 Olanzapine.mp. 68 Paliperidone.mp. 69 Paroxetine/ 70 Paroxetine.mp. 71 Quetiapine.mp. 72 Risperidone/ 73 Risperidone.mp. 74 Rivastigmine.mp. 75 exp Serotonin Uptake Inhibitors/ 76 (SSRI or SSRIs).tw. 77 serotonin.mp. 78 Sertraline/ 79 Sertraline.mp. 80 Tetracyclic$.mp. 81 Tianeptine.mp. 82 Tricyclic$.mp. 83 Venlafaxine.mp. 84 Ziprasidone.mp. 85 or/12‐84 86 randomized controlled trial.pt. 87 controlled clinical trial.pt. 88 randomi#ed.ab. 89 placebo$.ab. 90 drug therapy.fs. 91 randomly.ab. 92 trial.ab. 93 groups.ab. 94 or/86‐93 95 exp animals/ not humans.sh. 96 94 not 95 97 11 and 85 and 96
Appendix 3. Unused methods
We did not use the following methods for a range of reasons including insufficient details to conduct the planned subgroup analyses, the characteristics of included studies, and following advice from a statistician we decided that a network meta‐analysis (NMA) was not feasible.
Criteria for considering studies for this review
Types of interventions
Had there been sufficient studies with direct comparisons of two or more interventions we would have primarily used these studies. However, the majority of studies compared one or more interventions to a placebo.
In the case of direct comparisons of two or more interventions, we would have assessed the plausibility of transitivity, and made indirect comparisons by including primary studies that compare relevant interventions to either placebo treatment, wait‐list or no‐treatment conditions, or an active common comparator. Transitivity requires the assumption that any patient that meets the inclusion criteria could reasonably be randomised among any selection of eligible interventions.
Measures of treatment effect
Relative treatment effects
We would have presented results from the network meta‐analysis (NMA) as summary relative effect sizes (standardised mean difference (SMD) or odds ratio (OR)) for each possible pair of treatments.
Relative treatment ranking
We would have estimated the ranking probabilities for each treatment. This is the probability that each treatment is the first, second, third, etc. best in the network. We would have obtained a treatment hierarchy using the surface under the cumulative ranking curve (SUCRA; Chaimani 2013), and mean ranks. SUCRA can also be expressed as a percentage and interpreted as the percentage of efficacy or safety of treatment that would be ranked first without uncertainty.
Unit of analysis issues
Studies with multiple intervention groups were anticipated in this area. Had we performed an NMA, data from any relevant multi‐arm trial could have been retained in their original form and entered into the model accordingly.
Dealing with missing data
Had continuous data been missing, we would have imputed data using a 'last observation carried forward' approach. Had cases been missing from the first outcome measure, we would have analysed only the available data.
Assessment of heterogeneity
We would have assessed the assumption of transitivity visually, by examining the distribution of potential effect modifiers extracted; for example, whether antidepressants were administered the same way in studies comparing antidepressants to placebo and in those comparing antidepressants to antipsychotics.
Assessment of reporting biases
Had we conducted an NMA, and had data been sufficient, we would have used the comparison‐adjusted funnel plot technique (Chaimani 2013).
Data synthesis
Methods for indirect and mixed comparisons
Had direct and indirect comparisons appeared to be in agreement, and had the assessment of transitivity seemed reasonable, we would have combined direct and indirect evidence to create mixed estimates of the relative effects of the different types of pharmacological interventions. We would have performed the NMA in STATA (Stata 2013), using the 'mvmeta' command (White 2012), and self‐programmed STATA routines (Chaimani 2013).
Assessment of statistical heterogeneity
Assumptions when estimating the heterogeneity
Had we conducted an NMA, we would have assumed a common estimate for heterogeneity variance across different comparisons.
Measures and tests for heterogeneity
The assessment of statistical heterogeneity in the NMA would have been based on the magnitude of the heterogeneity variance parameter (τ²) estimated from the NMA models. For dichotomous outcomes, the magnitude of the heterogeneity variance can then be compared with the empirical distribution described by meta‐epidemiological studies (Savović 2012; Turner 2012).
Assessment of statistical inconsistency
Local approaches for evaluating inconsistency
We would have used the loop‐specific approach to evaluate the presence of inconsistency locally. This method separately evaluates consistency in each closed loop of the network, where consistency is defined as the difference between direct and indirect estimates for a specific comparison in that loop (inconsistency factor). Then, the magnitude of the inconsistency factors and their 95% confidence intervals (CIs) can be used to infer the presence of inconsistency in each loop. We would have assumed a common heterogeneity estimate and presented the results of this approach graphically in a forest plot using the 'ifplot' command in STATA (Chaimani 2013).
Global approaches for evaluating inconsistency
Had we conducted a NMA, we would have conducted the following: check the assumption of consistency in the entire network, by using the ‘design‐by‐treatment’ model described by Higgins and colleagues (Higgins 2012). This method assesses different sources of inconsistency that can occur when studies with different designs (e.g. two‐arm trials versus three‐arm trials) give different results as well as disagreement between direct and indirect evidence. Using this approach, we would have inferred the presence of inconsistency from any source in the entire network based on a Chi² test. We would have performed the design‐by‐treatment model in STATA using the 'mvmeta' command.
Sensitivity analysis
Although we conducted some sensitivity analyses to assess whether the findings of this review are robust to the decisions made in the process of obtaining them, we could not perform some sensitivity analyses. Specifically, we could not conduct the following:
Reanalysis excluding studies according to study quality issues, including those with low sample size, high risk of bias, or high attrition and dropout rate
Reanalysis without imputing data for the missing participants
Reanalysis using a fixed‐effect model
Multiple treatment groups
If some studies had included more than one control group, each undergoing different yet equally eligible forms of 'management as usual' we would have combined the control groups to create a single pair‐wise comparison. Had this strategy posed a problem for the investigation of heterogeneity, we would have compared each group separately as part of the subgroup analyses.
Cluster‐randomised trials
We did not anticipate cluster‐randomised trials, in which allocation to the intervention group has occurred by school, hospital or by community as opposed to by individual, in this research area.
Had this review included cluster‐randomised trials we would have conducted the following: in the event that we had identified relevant cluster‐randomised trials, it is likely that study authors would have controlled for a clustering effect when presenting their results. When this information was unclear, we would contact study authors for further information. If the clustering effect was not controlled for, we would have requested individual participant data to calculate an estimate of the intracluster correlation coefficient (ICC). If individual participant data were not available, we would have searched for external estimates of the ICC from similar studies or available resources. If we could not find an appropriate ICC from any available resources, we would have sought statistical advice to obtain an estimate of the ICC and used this to reanalyse the trial data to obtain approximate correct analyses. We would then have entered these data into Review Manager Web software (RevMan Web 2021) to analyse effect sizes and CIs using the generic inverse variance method (Higgins 2022b).
Data and analyses
Comparison 1. Atypical antipsychotic vs placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Irritability | 12 | 973 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.90 [‐1.25, ‐0.55] |
| 1.1.1 Aripiprazole vs placebo | 5 | 492 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.90 [‐1.52, ‐0.29] |
| 1.1.2 Risperidone vs placebo | 6 | 333 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.11 [‐1.47, ‐0.76] |
| 1.1.3 Lurasidone vs placebo | 1 | 148 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.50, 0.19] |
| 1.2 Relapse | 2 | 56 | Risk Ratio (IV, Random, 95% CI) | 0.30 [0.13, 0.68] |
| 1.3 Improvement | 4 | 470 | Risk Ratio (IV, Random, 95% CI) | 2.08 [1.39, 3.12] |
| 1.3.1 Risperidone vs placebo | 2 | 167 | Risk Ratio (IV, Random, 95% CI) | 3.37 [1.21, 9.43] |
| 1.3.2 Ariprazole vs placebo | 2 | 303 | Risk Ratio (IV, Random, 95% CI) | 1.57 [1.09, 2.27] |
| 1.4 Aggression | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.4.1 Risperidone vs placebo | 1 | 77 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐0.89, 0.01] |
| 1.5 Self‐injury | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.43 [‐2.24, ‐0.61] |
| 1.5.1 Risperidone vs placebo | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.43 [‐2.24, ‐0.61] |
| 1.6 Adverse effects: cardiovascular | 2 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.6.1 Tachycardia | 2 | 179 | Risk Ratio (IV, Random, 95% CI) | 7.53 [1.40, 40.52] |
| 1.7 Adverse effects: gastrointestinal | 11 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.7.1 Abdominal pain | 4 | 400 | Risk Ratio (IV, Random, 95% CI) | 2.70 [1.04, 7.07] |
| 1.7.2 Constipation | 7 | 596 | Risk Ratio (IV, Random, 95% CI) | 2.36 [1.28, 4.34] |
| 1.7.3 Diarrhoea | 5 | 318 | Risk Ratio (IV, Random, 95% CI) | 0.93 [0.46, 1.88] |
| 1.7.4 Drooling | 2 | 313 | Risk Ratio (IV, Random, 95% CI) | 9.64 [1.29, 72.10] |
| 1.7.5 Dyspepsia (indigestion) | 1 | 31 | Risk Ratio (IV, Random, 95% CI) | 3.19 [0.14, 72.69] |
| 1.7.6 Dry mouth | 2 | 131 | Risk Ratio (IV, Random, 95% CI) | 1.97 [0.75, 5.20] |
| 1.7.7 Hypersalivation | 5 | 449 | Risk Ratio (IV, Random, 95% CI) | 4.15 [1.77, 9.71] |
| 1.7.8 Nausea | 4 | 531 | Risk Ratio (IV, Random, 95% CI) | 1.47 [0.61, 3.56] |
| 1.7.9 Stomach ache | 2 | 166 | Risk Ratio (IV, Random, 95% CI) | 0.50 [0.19, 1.32] |
| 1.7.10 Vomiting/nausea | 9 | 920 | Risk Ratio (IV, Random, 95% CI) | 1.79 [1.16, 2.74] |
| 1.8 Adverse effects: immune system | 7 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.8.1 Cough | 3 | 444 | Risk Ratio (IV, Random, 95% CI) | 1.50 [0.67, 3.34] |
| 1.8.2 Earache | 1 | 100 | Risk Ratio (IV, Random, 95% CI) | 0.52 [0.10, 2.71] |
| 1.8.3 Flu‐like symptoms | 1 | 79 | Risk Ratio (IV, Random, 95% CI) | 1.95 [0.38, 10.04] |
| 1.8.4 Pyrexia | 5 | 540 | Risk Ratio (IV, Random, 95% CI) | 1.81 [0.85, 3.86] |
| 1.8.5 Sore throat | 1 | 100 | Risk Ratio (IV, Random, 95% CI) | 5.20 [0.63, 42.96] |
| 1.9 Adverse effects: metabolic (dichotomous) | 10 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.9.1 Decreased appetite | 4 | 426 | Risk Ratio (IV, Random, 95% CI) | 2.12 [0.84, 5.33] |
| 1.9.2 Increased appetite | 8 | 702 | Risk Ratio (IV, Random, 95% CI) | 2.38 [1.69, 3.34] |
| 1.9.3 Weight gain | 4 | 470 | Risk Ratio (IV, Random, 95% CI) | 2.30 [0.84, 6.30] |
| 1.9.4 Thirst | 3 | 382 | Risk Ratio (IV, Random, 95% CI) | 1.51 [0.59, 3.87] |
| 1.10 Adverse effects: metabolic (continuous) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.10.1 Weight gain (kg) | 1 | 23 | Mean Difference (IV, Random, 95% CI) | 2.35 [0.73, 3.97] |
| 1.11 Adverse effects: musculoskeletal | 2 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.11.2 Dyskinesia | 1 | 100 | Risk Ratio (IV, Random, 95% CI) | 2.08 [0.55, 7.87] |
| 1.11.3 Movement disorder | 1 | 82 | Risk Ratio (IV, Random, 95% CI) | 5.50 [0.27, 111.14] |
| 1.11.4 Rigidity | 1 | 100 | Risk Ratio (IV, Random, 95% CI) | 5.20 [0.63, 42.96] |
| 1.12 Adverse effects: neurological | 11 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.12.1 Aggression | 4 | 461 | Risk Ratio (IV, Random, 95% CI) | 0.34 [0.12, 0.98] |
| 1.12.2 Agitation/excitation | 2 | 97 | Risk Ratio (IV, Random, 95% CI) | 0.46 [0.13, 1.62] |
| 1.12.3 Apathy | 1 | 79 | Risk Ratio (IV, Random, 95% CI) | 10.73 [0.61, 187.79] |
| 1.12.4 Dizziness | 2 | 139 | Risk Ratio (IV, Random, 95% CI) | 4.19 [1.10, 16.00] |
| 1.12.5 Drowsiness | 1 | 97 | Risk Ratio (IV, Random, 95% CI) | 4.26 [0.95, 19.02] |
| 1.12.6 Extrapyramidal disorder | 1 | 216 | Risk Ratio (IV, Random, 95% CI) | 7.83 [0.47, 130.01] |
| 1.12.7 Fatigue | 8 | 881 | Risk Ratio (IV, Random, 95% CI) | 2.58 [1.68, 3.97] |
| 1.12.8 Headache | 6 | 597 | Risk Ratio (IV, Random, 95% CI) | 1.17 [0.63, 2.15] |
| 1.12.9 Hyperactivity | 3 | 305 | Risk Ratio (IV, Random, 95% CI) | 0.47 [0.13, 1.70] |
| 1.12.10 Hypersomnia | 2 | 282 | Risk Ratio (IV, Random, 95% CI) | 2.67 [0.43, 16.52] |
| 1.12.11 Insomnia | 7 | 679 | Risk Ratio (IV, Random, 95% CI) | 0.72 [0.50, 1.04] |
| 1.12.12 Lethargy | 1 | 216 | Risk Ratio (IV, Random, 95% CI) | 6.58 [0.39, 110.35] |
| 1.12.13 Presyncope | 1 | 216 | Risk Ratio (IV, Random, 95% CI) | 0.94 [0.04, 22.72] |
| 1.12.14 Restlessness (akathisia) | 4 | 531 | Risk Ratio (IV, Random, 95% CI) | 0.99 [0.40, 2.43] |
| 1.12.15 Sedation | 5 | 366 | Risk Ratio (IV, Random, 95% CI) | 2.98 [1.15, 7.73] |
| 1.12.16 Somnolence | 9 | 869 | Risk Ratio (IV, Random, 95% CI) | 4.84 [3.18, 7.36] |
| 1.12.17 Tremor | 5 | 574 | Risk Ratio (IV, Random, 95% CI) | 5.99 [1.87, 19.19] |
| 1.13 Adverse effects: psychological | 4 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.13.1 Anxiety | 2 | 139 | Risk Ratio (IV, Random, 95% CI) | 1.34 [0.65, 2.76] |
| 1.13.2 Depression | 2 | 79 | Risk Ratio (IV, Random, 95% CI) | 3.86 [0.46, 32.60] |
| 1.14 Adverse effects: respiratory | 8 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.14.1 Ear infection | 1 | 66 | Risk Ratio (IV, Random, 95% CI) | 5.62 [0.28, 112.84] |
| 1.14.2 Epistaxis | 1 | 66 | Risk Ratio (IV, Random, 95% CI) | 5.62 [0.28, 112.84] |
| 1.14.3 Nasal congestion | 2 | 313 | Risk Ratio (IV, Random, 95% CI) | 2.39 [0.52, 11.00] |
| 1.14.4 Nasopharyngitis | 6 | 702 | Risk Ratio (IV, Random, 95% CI) | 1.26 [0.73, 2.17] |
| 1.14.5 Pharyngolaryngeal pain | 1 | 216 | Risk Ratio (IV, Random, 95% CI) | 0.31 [0.06, 1.48] |
| 1.14.6 Rhinitis | 1 | 79 | Risk Ratio (IV, Random, 95% CI) | 2.68 [0.93, 7.71] |
| 1.14.7 Upper respiratory tract infection | 6 | 640 | Risk Ratio (IV, Random, 95% CI) | 2.15 [1.08, 4.27] |
| 1.15 Adverse effects: skin | 3 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.15.1 Bruise | 1 | 92 | Risk Ratio (IV, Random, 95% CI) | 0.32 [0.03, 2.96] |
| 1.15.2 Rash | 2 | 228 | Risk Ratio (IV, Random, 95% CI) | 0.79 [0.14, 4.62] |
| 1.16 Adverse effects: urinary | 6 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.16.1 Enuresis | 6 | 552 | Risk Ratio (IV, Random, 95% CI) | 1.12 [0.67, 1.86] |
| 1.17 Quality of life | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.18 Tolerability/acceptability: loss to follow‐up | 13 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.19 Subgroup analysis: age ‐ irritability | 11 | 938 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.87 [‐1.24, ‐0.50] |
| 1.19.1 Adults only | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.94 [‐1.70, ‐0.18] |
| 1.19.2 Children only | 10 | 908 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.87 [‐1.26, ‐0.47] |
| 1.20 Subgroup analysis: age ‐ aggression | 1 | 77 | Mean Difference (IV, Random, 95% CI) | ‐3.80 [‐7.61, 0.01] |
| 1.20.1 Children only | 1 | 77 | Mean Difference (IV, Random, 95% CI) | ‐3.80 [‐7.61, 0.01] |
| 1.21 Subgroup analysis: cognitive ability ‐ irritability | 10 | 925 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.91 [‐1.29, ‐0.52] |
| 1.21.1 Mixed IQ | 10 | 925 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.91 [‐1.29, ‐0.52] |
1.19. Analysis.

Comparison 1: Atypical antipsychotic vs placebo, Outcome 19: Subgroup analysis: age ‐ irritability
1.20. Analysis.

Comparison 1: Atypical antipsychotic vs placebo, Outcome 20: Subgroup analysis: age ‐ aggression
1.21. Analysis.

Comparison 1: Atypical antipsychotic vs placebo, Outcome 21: Subgroup analysis: cognitive ability ‐ irritability
Comparison 2. Neurohormone versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Irritability | 8 | 466 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐0.37, ‐0.00] |
| 2.1.1 Secretin | 3 | 69 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.46, 0.49] |
| 2.1.2 ACTH | 1 | 14 | Std. Mean Difference (IV, Random, 95% CI) | 0.40 [‐0.66, 1.46] |
| 2.1.3 Oxytocin | 3 | 353 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.45, ‐0.03] |
| 2.1.4 Vasopressin | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐1.02, 0.43] |
| 2.2 Self‐injury | 1 | 100 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.74, 0.05] |
| 2.2.1 Endpoint | 1 | 50 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.93, 0.19] |
| 2.2.2 Three month follow‐up | 1 | 50 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.88, 0.23] |
| 2.3 Adverse effects: cardiovascular | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.3.1 Cardiac disorders | 3 | 456 | Risk Ratio (M‐H, Random, 95% CI) | 1.45 [0.23, 9.05] |
| 2.3.2 Vascular disorders | 1 | 106 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.06, 15.57] |
| 2.3.3 Palpitations | 1 | 290 | Risk Ratio (M‐H, Random, 95% CI) | 2.96 [0.12, 72.04] |
| 2.4 Adverse effects: gastrointestinal | 6 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 2.4.1 Abdominal pain or discomfort | 1 | 290 | Risk Ratio (IV, Random, 95% CI) | 0.42 [0.17, 1.07] |
| 2.4.2 Constipation | 3 | 361 | Risk Ratio (IV, Random, 95% CI) | 0.89 [0.46, 1.73] |
| 2.4.3 Diarrhoea | 5 | 450 | Risk Ratio (IV, Random, 95% CI) | 0.71 [0.39, 1.28] |
| 2.4.4 Dry mouth | 2 | 350 | Risk Ratio (IV, Random, 95% CI) | 0.43 [0.06, 2.88] |
| 2.4.5 Encopresis | 1 | 290 | Risk Ratio (IV, Random, 95% CI) | 0.74 [0.17, 3.25] |
| 2.4.6 Gastrointestinal disorders | 2 | 166 | Risk Ratio (IV, Random, 95% CI) | 1.25 [0.35, 4.49] |
| 2.4.7 Nausea | 1 | 60 | Risk Ratio (IV, Random, 95% CI) | 0.14 [0.01, 2.65] |
| 2.4.8 Salivary hypersecretion | 2 | 319 | Risk Ratio (IV, Random, 95% CI) | 0.32 [0.03, 2.99] |
| 2.4.9 Stomatitis | 2 | 321 | Risk Ratio (IV, Random, 95% CI) | 0.13 [0.02, 1.11] |
| 2.4.10 Vomiting | 4 | 409 | Risk Ratio (IV, Random, 95% CI) | 0.45 [0.21, 0.97] |
| 2.5 Adverse effects: immune system | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.5.1 infections and infestations | 1 | 106 | Risk Ratio (M‐H, Random, 95% CI) | 2.00 [0.81, 4.93] |
| 2.6 Adverse effects: metabolic (dichotomous) | 5 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 2.6.1 Decreased appetite | 4 | 409 | Risk Ratio (IV, Random, 95% CI) | 0.67 [0.37, 1.22] |
| 2.6.2 Increased appetite | 2 | 350 | Risk Ratio (IV, Random, 95% CI) | 1.74 [0.96, 3.16] |
| 2.6.3 Metabolism and nutrition disorders | 1 | 106 | Risk Ratio (IV, Random, 95% CI) | 0.50 [0.05, 5.35] |
| 2.6.4 Thirst | 2 | 319 | Risk Ratio (IV, Random, 95% CI) | 1.42 [0.35, 5.67] |
| 2.6.5 Weight gain | 1 | 290 | Risk Ratio (IV, Random, 95% CI) | 1.21 [0.52, 2.82] |
| 2.6.6 Weight loss | 1 | 290 | Risk Ratio (IV, Random, 95% CI) | 1.97 [0.69, 5.63] |
| 2.7 Adverse effects: metabolic (continuous) | 1 | 24 | Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐1.76, 0.86] |
| 2.7.1 Mean change in weight (kg) | 1 | 24 | Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐1.76, 0.86] |
| 2.8 Adverse effects: musculoskeletal | 3 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 2.8.1 Muscle spasms | 1 | 29 | Risk Ratio (IV, Random, 95% CI) | 2.81 [0.12, 63.83] |
| 2.8.2 Musculoskeletal and connective tissue disorders | 1 | 106 | Risk Ratio (IV, Random, 95% CI) | 3.00 [0.12, 72.02] |
| 2.8.3 Rhabdomyolysis | 1 | 220 | Risk Ratio (IV, Random, 95% CI) | 1.47 [0.06, 35.64] |
| 2.9 Adverse effects: neurological | 11 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 2.9.1 Absence seizures | 1 | 19 | Risk Ratio (IV, Random, 95% CI) | 2.73 [0.12, 59.57] |
| 2.9.2 Aggression | 3 | 356 | Risk Ratio (IV, Random, 95% CI) | 0.91 [0.57, 1.44] |
| 2.9.3 Agitation | 3 | 344 | Risk Ratio (IV, Random, 95% CI) | 1.12 [0.65, 1.94] |
| 2.9.4 Decreased attention | 3 | 108 | Risk Ratio (IV, Random, 95% CI) | 1.46 [0.24, 8.84] |
| 2.9.5 Dizziness | 3 | 369 | Risk Ratio (IV, Random, 95% CI) | 0.65 [0.08, 5.27] |
| 2.9.6 Dysphoria | 1 | 290 | Risk Ratio (IV, Random, 95% CI) | 0.33 [0.01, 8.00] |
| 2.9.7 Excessive talking | 1 | 29 | Risk Ratio (IV, Random, 95% CI) | 2.81 [0.12, 63.83] |
| 2.9.8 Fatigue | 3 | 120 | Risk Ratio (IV, Random, 95% CI) | 0.91 [0.50, 1.65] |
| 2.9.9 Forgetfulness | 1 | 19 | Risk Ratio (IV, Random, 95% CI) | 2.73 [0.12, 59.57] |
| 2.9.10 Headache | 7 | 689 | Risk Ratio (IV, Random, 95% CI) | 0.58 [0.38, 0.89] |
| 2.9.11 Insomnia | 6 | 477 | Risk Ratio (IV, Random, 95% CI) | 0.72 [0.50, 1.04] |
| 2.9.12 Irritability | 6 | 655 | Risk Ratio (IV, Random, 95% CI) | 0.86 [0.68, 1.10] |
| 2.9.13 Leg shaking | 1 | 19 | Risk Ratio (IV, Random, 95% CI) | 2.73 [0.12, 59.57] |
| 2.9.14 Nervous systems disorders | 1 | 106 | Risk Ratio (IV, Random, 95% CI) | 1.67 [0.42, 6.62] |
| 2.9.15 Oppositional | 1 | 25 | Risk Ratio (IV, Random, 95% CI) | 0.72 [0.14, 3.61] |
| 2.9.16 Restlessness | 2 | 319 | Risk Ratio (IV, Random, 95% CI) | 1.64 [0.17, 15.47] |
| 2.9.17 Seizure | 1 | 29 | Risk Ratio (IV, Random, 95% CI) | 2.81 [0.12, 63.83] |
| 2.9.18 Sedation | 2 | 350 | Risk Ratio (IV, Random, 95% CI) | 1.69 [0.87, 3.27] |
| 2.9.19 Somnolence | 2 | 89 | Risk Ratio (IV, Random, 95% CI) | 3.81 [0.44, 32.96] |
| 2.9.20 Tics | 2 | 309 | Risk Ratio (IV, Random, 95% CI) | 0.63 [0.16, 2.38] |
| 2.10 Adverse effects: psychological | 6 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 2.10.1 Anxiety | 2 | 97 | Risk Ratio (IV, Random, 95% CI) | 3.05 [0.50, 18.55] |
| 2.10.2 Depression | 4 | 427 | Risk Ratio (IV, Random, 95% CI) | 0.89 [0.29, 2.68] |
| 2.10.3 Panic attack | 1 | 19 | Risk Ratio (IV, Random, 95% CI) | 0.30 [0.01, 6.62] |
| 2.10.4 Psychiatric | 1 | 106 | Risk Ratio (IV, Random, 95% CI) | 4.00 [0.46, 34.61] |
| 2.10.5 Self‐injury | 2 | 118 | Risk Ratio (IV, Random, 95% CI) | 1.00 [0.11, 9.35] |
| 2.11 Adverse effects: respiratory | 10 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 2.11.1 Cold symptoms | 2 | 73 | Risk Ratio (IV, Random, 95% CI) | 0.65 [0.26, 1.65] |
| 2.11.2 Cough | 5 | 430 | Risk Ratio (IV, Random, 95% CI) | 1.35 [0.81, 2.25] |
| 2.11.3 Croup | 1 | 25 | Risk Ratio (IV, Random, 95% CI) | 3.23 [0.14, 72.46] |
| 2.11.4 Epistaxis | 3 | 379 | Risk Ratio (IV, Random, 95% CI) | 1.21 [0.63, 2.31] |
| 2.11.5 Nasal congestion | 5 | 468 | Risk Ratio (IV, Random, 95% CI) | 0.79 [0.59, 1.05] |
| 2.11.6 Nasal irritation/runny nose | 1 | 40 | Risk Ratio (IV, Random, 95% CI) | 0.55 [0.10, 2.92] |
| 2.11.7 Nasopharyngitis | 1 | 29 | Risk Ratio (IV, Random, 95% CI) | 0.93 [0.15, 5.76] |
| 2.11.8 Respiratory, thoracic and mediastinal disorders | 2 | 147 | Risk Ratio (IV, Random, 95% CI) | 0.49 [0.09, 2.56] |
| 2.11.9 Sinusitis | 1 | 29 | Risk Ratio (IV, Random, 95% CI) | 0.47 [0.05, 4.60] |
| 2.11.10 Upper respiratory tract infection | 2 | 273 | Risk Ratio (IV, Random, 95% CI) | 1.10 [0.35, 3.47] |
| 2.12 Adverse effects: skin | 5 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 2.12.1 General/systemic disorders and administration site conditions | 1 | 106 | Risk Ratio (IV, Random, 95% CI) | 4.00 [0.46, 34.61] |
| 2.12.2 Skin rash | 4 | 416 | Risk Ratio (IV, Random, 95% CI) | 1.12 [0.63, 1.97] |
| 2.12.3 Skin and subcutaneous tissue disorders | 1 | 106 | Risk Ratio (IV, Random, 95% CI) | 5.00 [0.25, 101.73] |
| 2.13 Adverse effects: urinary | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.13.1 Renal and urinary disorders | 1 | 106 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.12, 72.02] |
| 2.13.2 Enuresis | 1 | 290 | Risk Ratio (M‐H, Random, 95% CI) | 0.18 [0.06, 0.62] |
| 2.14 Adverse effects: other | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.14.1 Injury, poisoning, and procedural complications | 1 | 106 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.12, 72.02] |
| 2.14.2 Investigations | 1 | 106 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.05, 5.35] |
| 2.14.3 Lymphadenopathy | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 7.87] |
| 2.14.4 Neoplasms: benign, malignant, and unspecified | 1 | 106 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.12, 72.02] |
| 2.14.5 Troponin I increased | 1 | 220 | Risk Ratio (M‐H, Random, 95% CI) | 1.47 [0.06, 35.64] |
| 2.15 Quality of life | 4 | 191 | Std. Mean Difference (IV, Random, 95% CI) | 0.70 [‐0.12, 1.53] |
| 2.15.1 Oxytocin | 2 | 37 | Std. Mean Difference (IV, Random, 95% CI) | 0.24 [‐0.74, 1.21] |
| 2.15.2 Vasopressin | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | 0.55 [‐0.19, 1.29] |
| 2.15.3 Balovaptan | 1 | 124 | Std. Mean Difference (IV, Random, 95% CI) | 1.54 [1.14, 1.95] |
| 2.16 Tolerability/acceptability: loss to follow‐up | 14 | 1312 | Risk Ratio (IV, Random, 95% CI) | 1.10 [0.87, 1.40] |
| 2.17 Subgroup analyses: gender ‐ irritability | 10 | 654 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.28, 0.03] |
| 2.17.1 Male and female participants | 8 | 563 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.30, 0.03] |
| 2.17.2 Male participants only | 2 | 91 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.76, 0.54] |
2.17. Analysis.

Comparison 2: Neurohormone versus placebo, Outcome 17: Subgroup analyses: gender ‐ irritability
Comparison 3. ADHD‐related medications vs placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Irritability | 10 | 400 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.40, ‐0.01] |
| 3.1.1 Irritability: non‐stimulant ADHD‐related drugs | 8 | 342 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.38, 0.05] |
| 3.1.2 Irritability: stimulant ADHD‐related drugs | 2 | 58 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐0.97, 0.08] |
| 3.2 Self‐injury | 1 | 16 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.62 [‐1.63, 0.39] |
| 3.3 Adverse effects: cardiovascular | 3 | 114 | Risk Ratio (IV, Random, 95% CI) | 0.64 [0.16, 2.54] |
| 3.3.1 Bradycardia | 1 | 66 | Risk Ratio (IV, Random, 95% CI) | 0.36 [0.09, 1.37] |
| 3.3.2 Tachycardia | 2 | 48 | Risk Ratio (IV, Random, 95% CI) | 3.52 [0.44, 27.85] |
| 3.4 Adverse effects: gastrointestinal | 9 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 3.4.1 Constipation | 5 | 220 | Risk Ratio (IV, Random, 95% CI) | 2.68 [1.61, 4.45] |
| 3.4.2 Diarrhoea | 6 | 426 | Risk Ratio (IV, Random, 95% CI) | 0.81 [0.46, 1.40] |
| 3.4.3 Dry mouth | 3 | 102 | Risk Ratio (IV, Random, 95% CI) | 5.92 [1.86, 18.81] |
| 3.4.4 Nausea | 5 | 239 | Risk Ratio (IV, Random, 95% CI) | 3.08 [1.51, 6.29] |
| 3.4.5 Stomachache | 2 | 86 | Risk Ratio (IV, Random, 95% CI) | 2.58 [1.10, 6.06] |
| 3.4.6 Stomach or abdominal discomfort | 6 | 504 | Risk Ratio (IV, Random, 95% CI) | 2.26 [1.41, 3.63] |
| 3.4.7 Vomiting | 4 | 347 | Risk Ratio (IV, Random, 95% CI) | 1.35 [0.81, 2.25] |
| 3.5 Adverse effects: immune system | 4 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 3.5.1 Fever | 3 | 183 | Risk Ratio (IV, Random, 95% CI) | 0.27 [0.06, 1.27] |
| 3.5.2 Influenza | 1 | 97 | Risk Ratio (IV, Random, 95% CI) | 7.14 [0.38, 134.69] |
| 3.5.3 Myalgia | 2 | 115 | Risk Ratio (IV, Random, 95% CI) | 4.72 [0.56, 39.55] |
| 3.5.4 Weakness | 1 | 62 | Risk Ratio (IV, Random, 95% CI) | 3.20 [0.35, 29.10] |
| 3.6 Adverse effects: metabolic (dichotomous) | 9 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 3.6.1 Decreased appetite | 9 | 511 | Risk Ratio (IV, Random, 95% CI) | 2.15 [1.55, 2.99] |
| 3.6.2 Increased appetite | 2 | 122 | Risk Ratio (IV, Random, 95% CI) | 0.67 [0.14, 3.34] |
| 3.6.3 Increased energy | 1 | 62 | Risk Ratio (IV, Random, 95% CI) | 1.60 [0.65, 3.95] |
| 3.7 Adverse effects: neurological (dichotomous) | 9 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 3.7.1 Aggression | 5 | 365 | Risk Ratio (IV, Random, 95% CI) | 0.95 [0.58, 1.53] |
| 3.7.2 Agitation | 1 | 128 | Risk Ratio (IV, Random, 95% CI) | 0.95 [0.56, 1.60] |
| 3.7.3 Dizziness | 3 | 175 | Risk Ratio (IV, Random, 95% CI) | 2.17 [0.63, 7.53] |
| 3.7.4 Drowsiness | 4 | 186 | Risk Ratio (IV, Random, 95% CI) | 3.42 [1.54, 7.59] |
| 3.7.5 Emotional / tearful | 2 | 128 | Risk Ratio (IV, Random, 95% CI) | 6.32 [2.47, 16.18] |
| 3.7.6 Fatigue | 4 | 235 | Risk Ratio (IV, Random, 95% CI) | 3.73 [1.98, 7.03] |
| 3.7.7 Headache | 8 | 383 | Risk Ratio (IV, Random, 95% CI) | 1.63 [1.09, 2.44] |
| 3.7.8 Hyperactivity | 2 | 115 | Risk Ratio (IV, Random, 95% CI) | 0.68 [0.06, 7.20] |
| 3.7.9 Increased motor activity | 1 | 66 | Risk Ratio (IV, Random, 95% CI) | 1.89 [0.48, 7.47] |
| 3.7.10 Insomnia | 7 | 411 | Risk Ratio (IV, Random, 95% CI) | 1.58 [1.01, 2.47] |
| 3.7.11 Irritability | 6 | 336 | Risk Ratio (IV, Random, 95% CI) | 1.61 [1.25, 2.07] |
| 3.7.12 Motor tics | 3 | 118 | Risk Ratio (IV, Random, 95% CI) | 2.33 [0.51, 10.69] |
| 3.7.13 Nightmares | 2 | 122 | Risk Ratio (IV, Random, 95% CI) | 1.48 [0.38, 5.75] |
| 3.7.14 Repetitive behaviour | 2 | 128 | Risk Ratio (IV, Random, 95% CI) | 1.59 [0.74, 3.39] |
| 3.7.15 Restless | 2 | 76 | Risk Ratio (IV, Random, 95% CI) | 1.52 [0.06, 40.44] |
| 3.7.16 Sleep disturbance | 2 | 84 | Risk Ratio (IV, Random, 95% CI) | 1.12 [0.54, 2.31] |
| 3.7.17 Talking excessively | 1 | 62 | Risk Ratio (IV, Random, 95% CI) | 0.24 [0.06, 1.01] |
| 3.7.18 Waking | 1 | 62 | Risk Ratio (IV, Random, 95% CI) | 1.60 [0.29, 8.92] |
| 3.7.19 Tremor | 1 | 16 | Risk Ratio (IV, Random, 95% CI) | 3.00 [0.14, 64.26] |
| 3.8 Adverse effects: neurological (continuous) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.8.1 Drowsiness | 1 | 8 | Mean Difference (IV, Random, 95% CI) | 4.80 [0.55, 9.05] |
| 3.8.2 Decreased activity | 1 | 8 | Mean Difference (IV, Random, 95% CI) | 2.00 [‐2.66, 6.66] |
| 3.9 Adverse effects: psychological (dichotomous) | 5 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 3.9.1 Anxiety | 5 | 252 | Risk Ratio (IV, Random, 95% CI) | 1.39 [0.74, 2.62] |
| 3.9.2 Depression | 3 | 152 | Risk Ratio (IV, Random, 95% CI) | 2.45 [1.12, 5.36] |
| 3.9.3 Mood change | 1 | 40 | Risk Ratio (IV, Random, 95% CI) | 13.00 [0.78, 216.39] |
| 3.9.4 Self‐injury | 3 | 188 | Risk Ratio (IV, Random, 95% CI) | 1.67 [0.78, 3.58] |
| 3.9.5 Silly behaviour | 1 | 62 | Risk Ratio (IV, Random, 95% CI) | 0.64 [0.17, 2.45] |
| 3.9.6 Social withdrawal | 2 | 126 | Risk Ratio (IV, Random, 95% CI) | 2.28 [0.39, 13.37] |
| 3.10 Adverse effects: respiratory | 2 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 3.10.1 Cough | 2 | 122 | Risk Ratio (IV, Random, 95% CI) | 0.81 [0.26, 2.46] |
| 3.11 Adverse effects: skin | 3 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 3.11.1 Rash | 3 | 102 | Risk Ratio (IV, Random, 95% CI) | 2.21 [0.79, 6.16] |
| 3.11.2 Skin picking | 1 | 62 | Risk Ratio (IV, Random, 95% CI) | 0.36 [0.04, 3.23] |
| 3.12 Adverse effects: urinary | 2 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 3.12.1 Enuresis | 2 | 122 | Risk Ratio (IV, Random, 95% CI) | 0.81 [0.19, 3.55] |
| 3.13 Quality of life | 1 | 54 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [‐0.33, 0.75] |
| 3.14 Tolerability/acceptability: loss to follow‐up | 9 | 380 | Risk Ratio (IV, Random, 95% CI) | 0.91 [0.50, 1.69] |
| 3.14.1 ADHD‐related drugs: loss to follow‐up | 9 | 380 | Risk Ratio (IV, Random, 95% CI) | 0.91 [0.50, 1.69] |
| 3.15 Subgroup analyses: gender ‐ irritability | 9 | 291 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.48, ‐0.01] |
| 3.15.1 Male participants only | 2 | 17 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐1.50, 0.47] |
| 3.15.2 Male and female participants | 7 | 274 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.47, 0.01] |
| 3.16 Subgroup analyses: age ‐ irritability | 9 | 293 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.48, ‐0.02] |
| 3.16.1 Adults and children | 1 | 9 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.48 [‐1.83, 0.87] |
| 3.16.2 Children only | 8 | 284 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.48, ‐0.01] |
3.15. Analysis.

Comparison 3: ADHD‐related medications vs placebo, Outcome 15: Subgroup analyses: gender ‐ irritability
3.16. Analysis.

Comparison 3: ADHD‐related medications vs placebo, Outcome 16: Subgroup analyses: age ‐ irritability
Comparison 4. Antidepressant vs placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Irritability | 3 | 267 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.30, 0.18] |
| 4.1.1 SSRIs | 2 | 255 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.29, 0.20] |
| 4.1.2 Dibenzoxazepine | 1 | 12 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐1.37, 0.91] |
| 4.2 Adverse effects: cardiovascular | 2 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 4.2.1 Flushing | 1 | 12 | Risk Ratio (IV, Random, 95% CI) | 2.00 [0.24, 16.61] |
| 4.2.2 Tachycardia | 2 | 35 | Risk Ratio (IV, Random, 95% CI) | 2.67 [0.31, 23.25] |
| 4.3 Adverse effects: gastrointestinal | 10 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 4.3.1 Constipation | 2 | 70 | Risk Ratio (IV, Random, 95% CI) | 0.95 [0.09, 10.03] |
| 4.3.2 Diarrhoea | 4 | 409 | Risk Ratio (IV, Random, 95% CI) | 0.94 [0.33, 2.64] |
| 4.3.3 Dry mouth | 1 | 12 | Risk Ratio (IV, Random, 95% CI) | 2.00 [0.24, 16.61] |
| 4.3.4 Gastrointestinal disturbance | 3 | 341 | Risk Ratio (IV, Random, 95% CI) | 1.41 [0.97, 2.05] |
| 4.3.5 Nausea/abdominal pain | 5 | 251 | Risk Ratio (IV, Random, 95% CI) | 1.67 [0.85, 3.27] |
| 4.3.6 Vomiting | 5 | 400 | Risk Ratio (IV, Random, 95% CI) | 1.49 [0.76, 2.92] |
| 4.4 Adverse effect: immune system | 3 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 4.4.1 Allergies | 1 | 149 | Risk Ratio (IV, Random, 95% CI) | 1.42 [0.70, 2.88] |
| 4.4.2 Cold, flu or other systemic infection | 1 | 149 | Risk Ratio (IV, Random, 95% CI) | 1.24 [0.82, 1.87] |
| 4.4.3 Infections | 3 | 472 | Risk Ratio (IV, Random, 95% CI) | 1.15 [0.85, 1.56] |
| 4.5 Adverse effects: metabolic | 7 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 4.5.1 Appetite disturbance | 1 | 165 | Risk Ratio (IV, Random, 95% CI) | 0.55 [0.14, 2.23] |
| 4.5.2 Decreased appetite | 4 | 242 | Risk Ratio (IV, Random, 95% CI) | 1.35 [0.68, 2.69] |
| 4.5.3 Decreased energy | 1 | 149 | Risk Ratio (IV, Random, 95% CI) | 1.94 [1.13, 3.33] |
| 4.5.4 Increased appetite | 1 | 149 | Risk Ratio (IV, Random, 95% CI) | 0.91 [0.35, 2.38] |
| 4.5.5 Weight gain | 2 | 93 | Risk Ratio (IV, Random, 95% CI) | 1.47 [0.08, 27.39] |
| 4.6 Adverse effect: musculoskeletal | 2 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 4.6.1 Motor disturbance | 1 | 165 | Risk Ratio (IV, Random, 95% CI) | 0.31 [0.03, 2.88] |
| 4.6.2 Neck pain | 1 | 37 | Risk Ratio (IV, Random, 95% CI) | 2.09 [0.09, 48.04] |
| 4.7 Adverse effects: neurological | 10 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 4.7.1 Activation syndrome | 1 | 158 | Risk Ratio (IV, Random, 95% CI) | 0.80 [0.31, 2.04] |
| 4.7.2 Agitation | 2 | 197 | Risk Ratio (IV, Random, 95% CI) | 1.01 [0.59, 1.75] |
| 4.7.3 Aggression or hostility | 3 | 225 | Risk Ratio (IV, Random, 95% CI) | 1.07 [0.59, 1.95] |
| 4.7.4 Anger/irritability | 2 | 167 | Risk Ratio (IV, Random, 95% CI) | 1.31 [0.75, 2.29] |
| 4.7.5 Autonomic disturbance | 1 | 165 | Risk Ratio (IV, Random, 95% CI) | 1.15 [0.32, 4.12] |
| 4.7.6 CNS disturbance | 1 | 165 | Risk Ratio (IV, Random, 95% CI) | 0.75 [0.33, 1.72] |
| 4.7.7 Decreased attention | 2 | 207 | Risk Ratio (IV, Random, 95% CI) | 4.16 [1.07, 16.11] |
| 4.7.8 Diaphoresis (sweating) | 1 | 36 | Risk Ratio (IV, Random, 95% CI) | 3.00 [0.13, 69.09] |
| 4.7.9 Drowsiness/fatigue | 4 | 282 | Risk Ratio (IV, Random, 95% CI) | 1.25 [0.65, 2.41] |
| 4.7.10 Headache | 3 | 244 | Risk Ratio (IV, Random, 95% CI) | 1.53 [0.77, 3.07] |
| 4.7.11 Hyperactivity | 2 | 207 | Risk Ratio (IV, Random, 95% CI) | 1.93 [0.47, 7.82] |
| 4.7.12 Increased speech | 1 | 149 | Risk Ratio (IV, Random, 95% CI) | 2.08 [0.66, 6.62] |
| 4.7.13 Insomnia | 7 | 449 | Risk Ratio (IV, Random, 95% CI) | 1.19 [0.87, 1.63] |
| 4.7.14 Mood disturbance | 1 | 165 | Risk Ratio (IV, Random, 95% CI) | 1.32 [0.75, 2.31] |
| 4.7.15 Mood lability | 2 | 167 | Risk Ratio (IV, Random, 95% CI) | 0.69 [0.27, 1.74] |
| 4.7.16 Numbness | 1 | 37 | Risk Ratio (IV, Random, 95% CI) | 2.09 [0.09, 48.04] |
| 4.7.17 Restlessness | 1 | 149 | Risk Ratio (IV, Random, 95% CI) | 1.93 [0.82, 4.57] |
| 4.7.18 Sedation | 3 | 117 | Risk Ratio (IV, Random, 95% CI) | 1.91 [0.77, 4.72] |
| 4.7.19 Sleep disturbance | 2 | 223 | Risk Ratio (IV, Random, 95% CI) | 1.24 [0.31, 4.92] |
| 4.7.20 Tremor | 3 | 85 | Risk Ratio (IV, Random, 95% CI) | 2.56 [0.57, 11.60] |
| 4.7.21 Twitching | 1 | 12 | Risk Ratio (IV, Random, 95% CI) | 7.00 [0.44, 111.91] |
| 4.7.22 Vertigo | 1 | 37 | Risk Ratio (IV, Random, 95% CI) | 2.09 [0.09, 48.04] |
| 4.8 Adverse effects: psychological | 4 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 4.8.1 Anorexia | 1 | 39 | Risk Ratio (IV, Random, 95% CI) | 1.58 [0.53, 4.74] |
| 4.8.2 Anxiety/nervousness | 2 | 188 | Risk Ratio (IV, Random, 95% CI) | 0.66 [0.37, 1.18] |
| 4.8.3 Depression | 1 | 37 | Risk Ratio (IV, Random, 95% CI) | 1.36 [0.14, 13.72] |
| 4.8.4 Impulsive/intrusive behaviour | 1 | 149 | Risk Ratio (IV, Random, 95% CI) | 2.92 [1.11, 7.68] |
| 4.8.5 Self‐injury | 1 | 18 | Risk Ratio (IV, Random, 95% CI) | 1.25 [0.09, 17.02] |
| 4.8.6 Silliness | 1 | 149 | Risk Ratio (IV, Random, 95% CI) | 0.94 [0.40, 2.17] |
| 4.8.7 Stereotypy | 1 | 149 | Risk Ratio (IV, Random, 95% CI) | 8.33 [1.07, 64.95] |
| 4.8.8 Suicidal ideation | 1 | 37 | Risk Ratio (IV, Random, 95% CI) | 2.09 [0.09, 48.04] |
| 4.8.9 Unstable mood | 1 | 149 | Risk Ratio (IV, Random, 95% CI) | 0.81 [0.32, 2.06] |
| 4.8.10 Verbal aggression | 1 | 37 | Risk Ratio (IV, Random, 95% CI) | 0.23 [0.01, 5.34] |
| 4.8.11 Vivid or bad dreams | 1 | 37 | Risk Ratio (IV, Random, 95% CI) | 4.87 [0.27, 87.94] |
| 4.9 Adverse effects: respiratory | 5 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 4.9.1 Cough | 1 | 18 | Risk Ratio (IV, Random, 95% CI) | 1.67 [0.52, 5.39] |
| 4.9.2 Respiratory | 2 | 314 | Risk Ratio (IV, Random, 95% CI) | 2.19 [0.86, 5.55] |
| 4.9.3 Upper respiratory infection (URI) | 2 | 216 | Risk Ratio (IV, Random, 95% CI) | 0.98 [0.73, 1.31] |
| 4.10 Adverse effects: skin | 3 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 4.10.1 Rash or skin irritation | 3 | 332 | Risk Ratio (IV, Random, 95% CI) | 1.00 [0.36, 2.78] |
| 4.11 Adverse effects: urinary | 3 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 4.11.1 Enuresis | 1 | 18 | Risk Ratio (IV, Random, 95% CI) | 3.12 [0.81, 12.06] |
| 4.11.2 Polyuria | 1 | 37 | Risk Ratio (IV, Random, 95% CI) | 2.09 [0.09, 48.04] |
| 4.11.3 Urinary tract infection (UTI) | 1 | 39 | Risk Ratio (IV, Random, 95% CI) | 0.60 [0.21, 1.73] |
| 4.12 Adverse effects: other | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 4.12.1 Salty taste | 1 | 37 | Risk Ratio (IV, Random, 95% CI) | 2.09 [0.09, 48.04] |
| 4.12.2 Trembling (mild) | 1 | 37 | Risk Ratio (IV, Random, 95% CI) | 2.09 [0.09, 48.04] |
| 4.13 Tolerability/acceptability: loss to follow‐up | 7 | 564 | Risk Ratio (IV, Random, 95% CI) | 1.22 [0.93, 1.59] |
| 4.14 Subgroup analyses: gender ‐ irritability | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.14.1 Male and female participants | 2 | 255 | Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐2.79, 1.90] |
| 4.14.2 Male participants only | 1 | 12 | Mean Difference (IV, Random, 95% CI) | ‐1.50 [‐8.37, 5.37] |
| 4.15 Serious adverse events | 2 | 76 | Risk Ratio (IV, Random, 95% CI) | 0.98 [0.11, 8.85] |
| 4.15.1 Hospitalisation for dehydration | 1 | 58 | Risk Ratio (IV, Random, 95% CI) | 2.45 [0.10, 57.85] |
| 4.15.2 Severe diarrhoea | 1 | 18 | Risk Ratio (IV, Random, 95% CI) | 0.41 [0.02, 8.84] |
4.14. Analysis.

Comparison 4: Antidepressant vs placebo, Outcome 14: Subgroup analyses: gender ‐ irritability
4.15. Analysis.

Comparison 4: Antidepressant vs placebo, Outcome 15: Serious adverse events
Comparison 5. Atypical vs typical antipsychotics.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Irritability | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.95, 0.48] |
| 5.2 Adverse effects: cardiovascular (tachycardia) | 1 | 12 | Risk Ratio (IV, Random, 95% CI) | 0.33 [0.02, 6.86] |
| 5.3 Adverse effects: gastrointestinal | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.3.1 Constipation | 1 | 30 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.24, 4.18] |
| 5.3.2 Dry mouth | 1 | 12 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.08, 12.56] |
| 5.3.3 Nausea/vomiting | 1 | 12 | Risk Ratio (M‐H, Random, 95% CI) | 5.00 [0.29, 86.43] |
| 5.4 Adverse effects: metabolic (dichotomous) | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 5.4.1 Weight gain | 1 | 12 | Risk Ratio (IV, Random, 95% CI) | 1.18 [0.76, 1.83] |
| 5.4.2 Weight loss | 1 | 12 | Risk Ratio (IV, Random, 95% CI) | 0.33 [0.02, 6.86] |
| 5.5 Adverse effects: metabolic (continuous) | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.5.1 Weight gain (kg) | 2 | 42 | Std. Mean Difference (IV, Random, 95% CI) | 0.26 [‐1.54, 2.06] |
| 5.6 Adverse effects: neurological | 2 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 5.6.1 Ataxia | 1 | 12 | Risk Ratio (IV, Random, 95% CI) | 0.33 [0.02, 6.86] |
| 5.6.2 Blunted effect | 1 | 30 | Risk Ratio (IV, Random, 95% CI) | 0.11 [0.01, 1.90] |
| 5.6.3 Insomnia | 1 | 12 | Risk Ratio (IV, Random, 95% CI) | 3.00 [0.15, 61.74] |
| 5.6.4 Rigidity | 1 | 12 | Risk Ratio (IV, Random, 95% CI) | 0.33 [0.02, 6.86] |
| 5.6.5 Sedation | 1 | 12 | Risk Ratio (IV, Random, 95% CI) | 2.50 [0.76, 8.19] |
| 5.7 Adverse effects: respiratory | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 5.7.1 Respiratory tract infection | 1 | 30 | Risk Ratio (IV, Random, 95% CI) | 0.88 [0.43, 1.80] |
| 5.8 Adverse effects: skin | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 5.8.1 Rash | 1 | 12 | Risk Ratio (IV, Random, 95% CI) | 0.33 [0.02, 6.86] |
| 5.9 Adverse effects: urinary | 2 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 5.9.1 Enuresis | 2 | 42 | Risk Ratio (IV, Random, 95% CI) | 1.00 [0.29, 3.48] |
| 5.10 Tolerability/acceptability: loss to follow‐up | 2 | 42 | Risk Ratio (IV, Random, 95% CI) | 5.00 [0.26, 96.13] |
Comparison 6. Atypical vs atypical antipsychotics.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Irritability | 2 | 110 | Std. Mean Difference (IV, Random, 95% CI) | 0.40 [0.02, 0.78] |
| 6.2 Adverse effects: cardiovascular | 2 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 6.2.1 Tachycardia | 2 | 120 | Risk Ratio (IV, Random, 95% CI) | 1.07 [0.16, 7.04] |
| 6.3 Adverse effects: gastrointestinal | 2 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 6.3.1 Abdominal pain | 1 | 59 | Risk Ratio (IV, Random, 95% CI) | 3.10 [0.34, 28.15] |
| 6.3.2 Constipation | 2 | 120 | Risk Ratio (IV, Random, 95% CI) | 1.30 [0.34, 4.91] |
| 6.3.3 Diarrhoea | 1 | 59 | Risk Ratio (IV, Random, 95% CI) | 3.10 [0.13, 73.14] |
| 6.3.4 Drooling | 2 | 120 | Risk Ratio (IV, Random, 95% CI) | 0.72 [0.38, 1.37] |
| 6.3.5 Dry mouth | 1 | 59 | Risk Ratio (IV, Random, 95% CI) | 5.17 [0.26, 103.21] |
| 6.3.6 Nausea | 1 | 59 | Risk Ratio (IV, Random, 95% CI) | 0.52 [0.05, 5.40] |
| 6.3.7 Vomiting | 2 | 120 | Risk Ratio (IV, Random, 95% CI) | 1.61 [0.20, 12.65] |
| 6.4 Adverse effects: metabolic | 2 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 6.4.1 Decreased appetite | 2 | 120 | Risk Ratio (IV, Random, 95% CI) | 1.67 [0.56, 4.96] |
| 6.4.2 Increased appetite | 2 | 120 | Risk Ratio (IV, Random, 95% CI) | 0.61 [0.15, 2.47] |
| 6.4.3 Weight gain | 1 | 61 | Risk Ratio (IV, Random, 95% CI) | 0.37 [0.19, 0.70] |
| 6.5 Adverse effects: musculoskeletal | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.5.1 Muscle rigidity | 1 | 61 | Risk Ratio (M‐H, Random, 95% CI) | 2.91 [0.12, 68.66] |
| 6.6 Adverse effects: neurological | 2 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 6.6.1 Agitation | 1 | 61 | Risk Ratio (IV, Random, 95% CI) | 4.84 [0.24, 96.89] |
| 6.6.2 Difficulty sleeping | 1 | 61 | Risk Ratio (IV, Random, 95% CI) | 6.78 [0.37, 125.95] |
| 6.6.3 Dizziness | 2 | 120 | Risk Ratio (IV, Random, 95% CI) | 0.73 [0.10, 5.39] |
| 6.6.4 Fatigue | 1 | 59 | Risk Ratio (IV, Random, 95% CI) | 1.03 [0.29, 3.75] |
| 6.6.5 Headache | 1 | 61 | Risk Ratio (IV, Random, 95% CI) | 0.97 [0.06, 14.78] |
| 6.6.6 Nausea | 1 | 61 | Risk Ratio (IV, Random, 95% CI) | 2.91 [0.12, 68.66] |
| 6.6.7 Nervousness | 1 | 59 | Risk Ratio (IV, Random, 95% CI) | 2.07 [0.20, 21.60] |
| 6.6.8 Restlessness | 2 | 120 | Risk Ratio (IV, Random, 95% CI) | 0.44 [0.07, 2.88] |
| 6.6.9 Tremor | 1 | 59 | Risk Ratio (IV, Random, 95% CI) | 1.55 [0.28, 8.62] |
| 6.6.10 Sedation | 1 | 61 | Risk Ratio (IV, Random, 95% CI) | 3.39 [0.76, 15.02] |
| 6.6.11 Somnolence | 1 | 61 | Risk Ratio (IV, Random, 95% CI) | 8.72 [0.49, 155.27] |
| 6.7 Adverse effects: psychological | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.7.1 Depression | 1 | 59 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.01, 8.13] |
| 6.8 Adverse effects: skin | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 6.8.1 Rash | 1 | 59 | Risk Ratio (IV, Random, 95% CI) | 1.03 [0.07, 15.77] |
| 6.9 Adverse effects: urinary | 2 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 6.9.1 Enuresis | 2 | 120 | Risk Ratio (IV, Random, 95% CI) | 1.37 [0.04, 53.78] |
| 6.10 Tolerability/acceptability: loss to follow‐up | 2 | Risk Ratio (IV, Random, 95% CI) | Subtotals only |
Comparison 7. Atypical antipsychotic vs antidementia.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 Irritability | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | 0.46 [‐0.27, 1.19] |
| 7.2 Adverse effects: neurological | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 7.2.1 Somnolence | 1 | 30 | Risk Ratio (IV, Random, 95% CI) | 1.30 [0.86, 1.96] |
| 7.3 Tolerability | 1 | 34 | Risk Ratio (IV, Random, 95% CI) | 0.38 [0.04, 3.25] |
Comparison 8. Atypical antipsychotic vs antiparkinsonian.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 8.1 Adverse effects: gastrointestinal | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 8.1.1 Diarrhoea | 1 | 18 | Risk Ratio (IV, Random, 95% CI) | 3.00 [0.14, 65.16] |
| 8.1.2 Increased salivation | 1 | 18 | Risk Ratio (IV, Random, 95% CI) | 3.00 [0.14, 65.16] |
| 8.1.3 Vomiting | 1 | 18 | Risk Ratio (IV, Random, 95% CI) | 0.20 [0.01, 3.66] |
| 8.2 Adverse effects: metabolic | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 8.2.1 Decreased appetite | 1 | 18 | Risk Ratio (IV, Random, 95% CI) | 0.09 [0.01, 1.44] |
| 8.3 Adverse effects: neurological | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 8.3.1 Agitation/excitement | 1 | 18 | Risk Ratio (IV, Random, 95% CI) | 1.50 [0.32, 6.94] |
| 8.3.2 Increased hyperactivity | 1 | 18 | Risk Ratio (IV, Random, 95% CI) | 7.00 [0.41, 118.69] |
| 8.3.3 Insomnia | 1 | 18 | Risk Ratio (IV, Random, 95% CI) | 2.00 [0.48, 8.31] |
| 8.3.4 Sedation | 1 | 18 | Risk Ratio (IV, Random, 95% CI) | 0.14 [0.01, 2.42] |
Comparison 9. Anticonvulsant vs placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 9.1 Irritability | 3 | 97 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.67 [‐1.93, 0.59] |
| 9.2 Aggression | 2 | 57 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐0.71, 0.35] |
| 9.3 Adverse effects: gastrointestinal | 2 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 9.3.1 Abdominal pain | 1 | 30 | Risk Ratio (IV, Random, 95% CI) | 1.75 [0.38, 8.15] |
| 9.3.2 Constipation | 1 | 30 | Risk Ratio (IV, Random, 95% CI) | 0.58 [0.11, 3.00] |
| 9.3.3 Diarrhoea | 1 | 30 | Risk Ratio (IV, Random, 95% CI) | 3.50 [0.44, 27.75] |
| 9.3.4 Nausea | 2 | 70 | Risk Ratio (IV, Random, 95% CI) | 2.32 [0.80, 6.72] |
| 9.3.5 Vomiting | 1 | 30 | Risk Ratio (IV, Random, 95% CI) | 3.50 [0.44, 27.75] |
| 9.4 Adverse effects: immune system | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 9.4.1 Chills | 1 | 30 | Risk Ratio (IV, Random, 95% CI) | 2.62 [0.31, 22.46] |
| 9.4.2 Fever | 1 | 30 | Risk Ratio (IV, Random, 95% CI) | 3.50 [0.44, 27.75] |
| 9.5 Adverse effects: metabolic (dichotomous) | 4 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 9.5.1 Decreased appetite | 2 | 60 | Risk Ratio (IV, Random, 95% CI) | 5.45 [1.02, 29.23] |
| 9.5.2 Increased appetite | 2 | 70 | Risk Ratio (IV, Random, 95% CI) | 0.99 [0.05, 18.14] |
| 9.5.3 Weight gain | 3 | 77 | Risk Ratio (IV, Random, 95% CI) | 1.48 [0.61, 3.62] |
| 9.5.4 Weight loss | 1 | 20 | Risk Ratio (IV, Random, 95% CI) | 3.00 [0.14, 65.90] |
| 9.6 Adverse effects: metabolic (continuous) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 9.6.1 Weight gain (kg) | 1 | 11 | Std. Mean Difference (IV, Random, 95% CI) | 0.48 [‐0.77, 1.74] |
| 9.7 Adverse Effects: neurological | 5 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 9.7.1 Aggression | 2 | 48 | Risk Ratio (IV, Random, 95% CI) | 2.29 [0.37, 14.12] |
| 9.7.2 Agitation | 2 | 47 | Risk Ratio (IV, Random, 95% CI) | 1.20 [0.21, 6.70] |
| 9.7.3 Dizziness | 1 | 40 | Risk Ratio (IV, Random, 95% CI) | 4.00 [0.49, 32.72] |
| 9.7.4 Drowsiness | 1 | 30 | Risk Ratio (IV, Random, 95% CI) | 0.88 [0.21, 3.66] |
| 9.7.5 Echolalia | 1 | 28 | Risk Ratio (IV, Random, 95% CI) | 1.00 [0.07, 14.45] |
| 9.7.6 Headache | 1 | 27 | Risk Ratio (IV, Random, 95% CI) | 2.12 [0.09, 47.68] |
| 9.7.7 Hyperactivity | 1 | 20 | Risk Ratio (IV, Random, 95% CI) | 3.00 [0.14, 65.90] |
| 9.7.8 Hypersomnolence | 1 | 27 | Risk Ratio (IV, Random, 95% CI) | 0.10 [0.01, 1.78] |
| 9.7.9 Insomnia | 4 | 115 | Risk Ratio (IV, Random, 95% CI) | 1.69 [0.44, 6.56] |
| 9.7.10 Lethargy | 1 | 30 | Risk Ratio (IV, Random, 95% CI) | 6.18 [0.35, 110.11] |
| 9.7.11 Paraesthesia | 1 | 40 | Risk Ratio (IV, Random, 95% CI) | 5.00 [0.64, 39.06] |
| 9.7.12 Sedation | 1 | 40 | Risk Ratio (IV, Random, 95% CI) | 0.25 [0.03, 2.05] |
| 9.7.13 Self‐injury | 1 | 20 | Risk Ratio (IV, Random, 95% CI) | 3.00 [0.14, 65.90] |
| 9.7.14 Somnolence | 1 | 40 | Risk Ratio (IV, Random, 95% CI) | 7.00 [0.95, 51.80] |
| 9.8 Adverse effects: psychological | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 9.8.5 Impulsivity | 1 | 20 | Risk Ratio (IV, Random, 95% CI) | 3.00 [0.14, 65.90] |
| 9.9 Adverse effects: skin | 2 | 57 | Risk Ratio (IV, Random, 95% CI) | 4.63 [0.89, 24.13] |
| 9.9.1 Rash | 2 | 57 | Risk Ratio (IV, Random, 95% CI) | 4.63 [0.89, 24.13] |
| 9.10 Adverse effects: urinary | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 9.10.1 Enuresis | 1 | 20 | Risk Ratio (IV, Random, 95% CI) | 0.33 [0.02, 7.32] |
| 9.11 Tolerability/acceptability: loss to follow‐up | 6 | 167 | Risk Ratio (IV, Random, 95% CI) | 1.98 [0.84, 4.66] |
Comparison 10. Antidepressant vs antidepressant.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 10.1 Adverse effects: cardiovascular | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 10.1.1 Tachycardia | 1 | 36 | Risk Ratio (IV, Random, 95% CI) | 2.60 [0.13, 50.25] |
| 10.2 Adverse effects: gastrointestinal | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 10.2.1 Constipation | 1 | 36 | Risk Ratio (IV, Random, 95% CI) | 1.50 [0.35, 6.35] |
| 10.2.2 Dry mouth | 1 | 36 | Risk Ratio (IV, Random, 95% CI) | 0.50 [0.12, 2.12] |
| 10.2.3 Nausea/abdominal pain | 1 | 36 | Risk Ratio (IV, Random, 95% CI) | 1.00 [0.10, 9.96] |
| 10.2.4 Vomiting | 1 | 36 | Risk Ratio (IV, Random, 95% CI) | 1.56 [0.07, 35.67] |
Comparison 11. Antidementia versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 11.1 Irritability (continuous) | 3 | 130 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐1.31, 0.52] |
| 11.2 Irritability (dichotomous) | 2 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 11.2.1 Partial response (≥ 25% reduction in irritability score) | 1 | 40 | Risk Ratio (IV, Random, 95% CI) | 1.38 [0.97, 1.97] |
| 11.2.2 Complete response (≥ 50% reduction in irritability score) | 1 | 40 | Risk Ratio (IV, Random, 95% CI) | 1.60 [0.98, 2.61] |
| 11.2.3 Irritability | 1 | 317 | Risk Ratio (IV, Random, 95% CI) | 0.51 [0.16, 1.66] |
| 11.3 Aggression | 1 | 50 | Std. Mean Difference (IV, Random, 95% CI) | 0.54 [‐0.05, 1.13] |
| 11.4 Adverse effects: gastrointestinal | 6 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 11.4.1 Abdominal pain | 2 | 83 | Risk Ratio (IV, Random, 95% CI) | 0.97 [0.21, 4.50] |
| 11.4.2 Constipation | 2 | 83 | Risk Ratio (IV, Random, 95% CI) | 0.33 [0.04, 3.01] |
| 11.4.3 Diarrhoea | 1 | 43 | Risk Ratio (IV, Random, 95% CI) | 2.87 [0.12, 66.75] |
| 11.4.4 Dry mouth | 1 | 40 | Risk Ratio (IV, Random, 95% CI) | 0.14 [0.01, 2.60] |
| 11.4.5 Gastroenteritis | 1 | 317 | Risk Ratio (IV, Random, 95% CI) | 7.13 [0.37, 136.97] |
| 11.4.6 Nausea | 1 | 40 | Risk Ratio (IV, Random, 95% CI) | 2.00 [0.41, 9.71] |
| 11.4.7 Vomiting | 2 | 438 | Risk Ratio (IV, Random, 95% CI) | 0.54 [0.18, 1.67] |
| 11.5 Adverse events: metabolic | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 11.5.1 Decreased appetite | 4 | 163 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.24, 4.07] |
| 11.5.2 Increased appetite | 4 | 163 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.54, 2.43] |
| 11.6 Adverse effects: musculoskeletal pain | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 11.7 Adverse effects: neurological | 7 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 11.7.1 Daytime drowsiness | 2 | 80 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.41, 1.77] |
| 11.7.2 Dizziness | 2 | 83 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.27, 3.61] |
| 11.7.3 Fatigue | 2 | 83 | Risk Ratio (M‐H, Random, 95% CI) | 1.39 [0.48, 4.02] |
| 11.7.4 Headache | 2 | 438 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.26, 2.75] |
| 11.7.5 Hyperactivity | 2 | 438 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.07, 1.73] |
| 11.7.6 Insomnia | 4 | 227 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.37, 2.59] |
| 11.7.7 Morning drowsiness | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 1.38 [0.71, 2.68] |
| 11.7.8 Sedation | 2 | 83 | Risk Ratio (M‐H, Random, 95% CI) | 1.34 [0.30, 5.98] |
| 11.7.9 Tremor | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.13, 69.52] |
| 11.7.10 Decreased energy | 1 | 23 | Risk Ratio (M‐H, Random, 95% CI) | 0.37 [0.09, 1.52] |
| 11.8 Adverse events: other | 3 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 11.8.1 Pyrexia | 2 | 438 | Risk Ratio (IV, Random, 95% CI) | 0.68 [0.19, 2.41] |
| 11.8.2 Increased infections | 1 | 23 | Risk Ratio (IV, Random, 95% CI) | 0.69 [0.35, 1.35] |
| 11.9 Adverse events: psychological | 4 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 11.9.1 Agitation | 2 | 438 | Risk Ratio (IV, Random, 95% CI) | 1.89 [0.45, 8.05] |
| 11.9.2 Aggression | 1 | 121 | Risk Ratio (IV, Random, 95% CI) | 1.69 [0.42, 6.78] |
| 11.9.3 Anxiety | 3 | 478 | Risk Ratio (IV, Random, 95% CI) | 0.41 [0.03, 5.61] |
| 11.9.4 Irritability | 3 | 461 | Risk Ratio (IV, Random, 95% CI) | 0.87 [0.43, 1.76] |
| 11.9.5 Mood changes | 1 | 23 | Risk Ratio (IV, Random, 95% CI) | 1.68 [0.95, 2.96] |
| 11.9.6 Emotional lability | 1 | 23 | Risk Ratio (IV, Random, 95% CI) | 1.83 [0.19, 17.51] |
| 11.9.7 Anger | 1 | 23 | Risk Ratio (IV, Random, 95% CI) | 0.31 [0.01, 6.85] |
| 11.9.8 Self‐injury | 1 | 23 | Risk Ratio (IV, Random, 95% CI) | 2.77 [0.12, 61.65] |
| 11.10 Adverse events: respiratory | 2 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 11.10.1 Cough | 2 | 438 | Risk Ratio (IV, Random, 95% CI) | 1.83 [0.63, 5.34] |
| 11.10.2 Nasopharyngitis | 2 | 438 | Risk Ratio (IV, Random, 95% CI) | 0.61 [0.08, 4.35] |
| 11.10.3 Upper respiratory tract infection | 1 | 317 | Risk Ratio (IV, Random, 95% CI) | 7.13 [0.37, 136.97] |
| 11.11 Adverse effects: skin | 2 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 11.11.1 Rash | 1 | 40 | Risk Ratio (IV, Random, 95% CI) | 2.00 [0.20, 20.33] |
| 11.11.2 Skin irritation | 1 | 23 | Risk Ratio (IV, Random, 95% CI) | 0.46 [0.15, 1.40] |
| 11.12 Serious adverse events | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 11.12.1 Affective disorder | 1 | 121 | Risk Ratio (IV, Random, 95% CI) | 3.05 [0.13, 73.40] |
| 11.13 Tolerability/acceptability: loss to follow‐up | 5 | 553 | Risk Ratio (IV, Random, 95% CI) | 0.95 [0.83, 1.09] |
| 11.14 Subgroup analysis: age ‐ irritability (continuous) | 4 | 140 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐1.24, 0.33] |
| 11.14.1 Children only | 3 | 130 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐1.31, 0.52] |
| 11.14.2 Adults only | 1 | 10 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.75 [‐2.06, 0.56] |
11.8. Analysis.

Comparison 11: Antidementia versus placebo, Outcome 8: Adverse events: other
11.12. Analysis.

Comparison 11: Antidementia versus placebo, Outcome 12: Serious adverse events
11.14. Analysis.

Comparison 11: Antidementia versus placebo, Outcome 14: Subgroup analysis: age ‐ irritability (continuous)
Comparison 12. Antiparkinsonian vs placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 12.1 Irritability | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.75 [‐1.39, ‐0.11] |
| 12.2 Adverse effects: gastrointestinal | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 12.2.1 Abdominal pain | 1 | 40 | Risk Ratio (IV, Random, 95% CI) | 0.33 [0.01, 7.72] |
| 12.2.2 Constipation | 1 | 40 | Risk Ratio (IV, Random, 95% CI) | 0.20 [0.01, 3.92] |
| 12.2.3 Drooling | 1 | 40 | Risk Ratio (IV, Random, 95% CI) | 0.33 [0.01, 7.72] |
| 12.3 Adverse effects: metabolic | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 12.3.1 Decreased appetite | 1 | 40 | Risk Ratio (IV, Random, 95% CI) | 0.11 [0.01, 1.94] |
| 12.3.2 Increased appetite | 1 | 40 | Risk Ratio (IV, Random, 95% CI) | 3.00 [0.69, 13.12] |
| 12.4 Adverse effects: neurological | 2 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 12.4.1 Daytime drowsiness | 1 | 40 | Risk Ratio (IV, Random, 95% CI) | 3.00 [0.13, 69.52] |
| 12.4.2 Insomnia | 2 | 79 | Risk Ratio (IV, Random, 95% CI) | 2.26 [0.55, 9.26] |
| 12.4.3 Nervousness | 1 | 40 | Risk Ratio (IV, Random, 95% CI) | 0.33 [0.04, 2.94] |
| 12.4.4 Somnolence | 1 | 39 | Risk Ratio (IV, Random, 95% CI) | 5.25 [0.27, 102.74] |
| 12.4.5 Tremor | 1 | 40 | Risk Ratio (IV, Random, 95% CI) | 3.00 [0.13, 69.52] |
| 12.5 Adverse effects: psychological | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 12.5.2 Adverse behaviour | 1 | 39 | Risk Ratio (IV, Random, 95% CI) | 0.53 [0.11, 2.55] |
| 12.6 Tolerability/acceptability: loss to follow‐up | 1 | 40 | Risk Ratio (IV, Random, 95% CI) | 0.33 [0.01, 7.72] |
Comparison 13. Anxiolytic versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 13.1 Irritabilty (continuous) | 1 | 34 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.88, 0.47] |
| 13.1.1 Anxiolytics vs placebo | 1 | 34 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.88, 0.47] |
| 13.2 Irritability (dichotomous) | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 13.2.1 Response rate (> 25% decrease in irritability score) | 1 | 34 | Risk Ratio (IV, Random, 95% CI) | 1.83 [1.04, 3.22] |
| 13.3 Adverse effects: gastrointestinal | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 13.3.1 Constipation | 1 | 166 | Risk Ratio (IV, Random, 95% CI) | 0.97 [0.35, 2.67] |
| 13.3.2 Diarrhoea | 1 | 166 | Risk Ratio (IV, Random, 95% CI) | 1.04 [0.68, 1.61] |
| 13.3.3 Vomiting | 1 | 166 | Risk Ratio (IV, Random, 95% CI) | 1.02 [0.68, 1.53] |
| 13.4 Adverse effects: immune System | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 13.4.1 Nasopharyngitis | 1 | 166 | Risk Ratio (IV, Random, 95% CI) | 0.87 [0.33, 2.28] |
| 13.4.2 Pyrexia | 1 | 166 | Risk Ratio (IV, Random, 95% CI) | 1.00 [0.73, 1.37] |
| 13.4.3 Upper respiratory tract infection | 1 | 166 | Risk Ratio (IV, Random, 95% CI) | 0.40 [0.18, 0.91] |
| 13.5 Adverse effects: metabolic | 2 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 13.5.1 Decreased appetite | 1 | 166 | Risk Ratio (IV, Random, 95% CI) | 1.11 [0.62, 1.99] |
| 13.5.2 Increased appetite | 2 | 200 | Risk Ratio (IV, Random, 95% CI) | 1.50 [0.93, 2.42] |
| 13.6 Adverse effects: neurological | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 13.6.1 Hyperactivity | 1 | 166 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.47, 1.30] |
| 13.6.2 Increased aggression | 1 | 166 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.60, 1.38] |
| 13.6.3 Insomnia | 1 | 166 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [0.90, 1.78] |
| 13.6.4 Irritability | 1 | 166 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.48, 1.47] |
| 13.6.5 Somnolence | 1 | 166 | Risk Ratio (M‐H, Random, 95% CI) | 1.70 [0.58, 4.97] |
| 13.7 Adverse effects: psychological | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 13.7.1 Anxiety | 1 | 166 | Risk Ratio (M‐H, Random, 95% CI) | 2.76 [0.48, 15.83] |
| 13.8 Adverse effects: respiratory system | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 13.8.1 Cough | 1 | 166 | Risk Ratio (IV, Random, 95% CI) | 0.90 [0.64, 1.26] |
| 13.8.2 Epistaxis | 1 | 166 | Risk Ratio (IV, Random, 95% CI) | 0.52 [0.19, 1.43] |
| 13.8.3 Nasal congestion | 1 | 166 | Risk Ratio (IV, Random, 95% CI) | 0.80 [0.36, 1.77] |
| 13.8.4 Rhinorrhoea | 1 | 166 | Risk Ratio (IV, Random, 95% CI) | 1.12 [0.66, 1.88] |
| 13.8.5 Sinus congestion | 1 | 166 | Risk Ratio (IV, Random, 95% CI) | 0.90 [0.55, 1.47] |
| 13.9 Adverse effects: skin | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 13.9.1 Rash | 1 | 166 | Risk Ratio (IV, Random, 95% CI) | 1.19 [0.52, 2.73] |
| 13.10 Other adverse effects | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 13.10.1 Ear infection | 1 | 166 | Risk Ratio (IV, Random, 95% CI) | 1.10 [0.50, 2.41] |
| 13.10.2 Ear and labyrinth disorders | 1 | 166 | Risk Ratio (IV, Random, 95% CI) | 2.92 [0.51, 16.72] |
| 13.10.3 Eye disorders | 1 | 166 | Risk Ratio (IV, Random, 95% CI) | 3.11 [0.72, 13.44] |
| 13.10.4 Renal and urinary disorders | 1 | 166 | Risk Ratio (IV, Random, 95% CI) | 0.97 [0.41, 2.30] |
| 13.11 Tolerability/acceptability: loss to follow‐up | 2 | 206 | Risk Ratio (IV, Random, 95% CI) | 0.88 [0.45, 1.73] |
13.10. Analysis.

Comparison 13: Anxiolytic versus placebo, Outcome 10: Other adverse effects
Comparison 14. Experimental versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 14.1 Irritability | 28 | 1205 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.53, ‐0.07] |
| 14.1.1 Arbaclofen | 1 | 130 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.68, 0.02] |
| 14.1.2 Baclofen | 1 | 58 | Std. Mean Difference (IV, Random, 95% CI) | 0.88 [0.34, 1.42] |
| 14.1.3 Bumetanide | 2 | 104 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.74 [‐1.84, 0.37] |
| 14.1.4 Celecoxib | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.27 [‐1.95, ‐0.58] |
| 14.1.5 Dextromethorphan | 1 | 8 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐1.52, 1.26] |
| 14.1.6 Dextromethorphan/quinidine | 1 | 14 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐1.43, 0.69] |
| 14.1.7 Folinic acid | 1 | 55 | Std. Mean Difference (IV, Random, 95% CI) | 0.63 [0.08, 1.17] |
| 14.1.8 Lofexedine | 1 | 12 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐1.66, 0.66] |
| 14.1.9 L‐carnosine | 1 | 42 | Std. Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.41, 0.80] |
| 14.1.10 Minocycline | 1 | 46 | Std. Mean Difference (IV, Random, 95% CI) | 0.89 [0.28, 1.50] |
| 14.1.11 N‐acetylcysteine | 4 | 125 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐1.16, ‐0.06] |
| 14.1.12 Naltrexone | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐0.80, 0.44] |
| 14.1.13 Nicotine | 1 | 8 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.72 [‐2.19, 0.75] |
| 14.1.14 Pioglitazone | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.77 [‐1.42, ‐0.13] |
| 14.1.15 Palmitoylethanolamide | 1 | 62 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.49 [‐1.00, 0.01] |
| 14.1.16 Prednisolone (steroid) | 1 | 26 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.96, 0.58] |
| 14.1.17 Pregnenolone | 1 | 59 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.55 [‐1.07, ‐0.03] |
| 14.1.18 Propentofylline | 1 | 48 | Std. Mean Difference (IV, Random, 95% CI) | 0.56 [‐0.01, 1.14] |
| 14.1.19 Resveratol | 1 | 62 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.79, 0.21] |
| 14.1.20 Riluzole | 2 | 54 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐1.10, 0.42] |
| 14.1.21 Simvastatin | 1 | 66 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.88 [‐1.38, ‐0.37] |
| 14.1.22 Sulforaphane | 1 | 60 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.86 [‐1.39, ‐0.33] |
| 14.1.23 Tetrahydrobiopterin | 1 | 46 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.68, 0.48] |
| 14.2 Self‐injury | 5 | 285 | Std. Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.09, 0.38] |
| 14.2.1 Bumetanide | 2 | 148 | Std. Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.21, 0.60] |
| 14.2.2 N‐acetylcysteine | 2 | 127 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.29, 0.44] |
| 14.2.3 Trichuris suris ova | 1 | 10 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐1.55, 0.95] |
| 14.3 Adverse effects: gastrointestinal | 32 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 14.3.1 Abdominal pain | 14 | 734 | Risk Ratio (IV, Random, 95% CI) | 1.38 [0.95, 2.01] |
| 14.3.2 Change in bowel habits | 2 | 54 | Risk Ratio (IV, Random, 95% CI) | 0.39 [0.05, 3.26] |
| 14.3.3 Constipation | 13 | 665 | Risk Ratio (IV, Random, 95% CI) | 1.29 [0.77, 2.16] |
| 14.3.4 Diarrhoea | 18 | 982 | Risk Ratio (IV, Random, 95% CI) | 0.83 [0.55, 1.25] |
| 14.3.5 Drooling | 1 | 11 | Risk Ratio (IV, Random, 95% CI) | 0.29 [0.01, 5.79] |
| 14.3.6 Dry mouth | 5 | 173 | Risk Ratio (IV, Random, 95% CI) | 0.87 [0.37, 2.09] |
| 14.3.7 Dyspepsia | 1 | 31 | Risk Ratio (IV, Random, 95% CI) | 0.31 [0.01, 7.15] |
| 14.3.8 Encopresis | 1 | 31 | Risk Ratio (IV, Random, 95% CI) | 0.31 [0.01, 7.15] |
| 14.3.9 Flatulance | 1 | 10 | Risk Ratio (IV, Random, 95% CI) | 3.00 [0.15, 59.89] |
| 14.3.10 Increased salivation | 1 | 40 | Risk Ratio (IV, Random, 95% CI) | 1.00 [0.39, 2.58] |
| 14.3.11 Nausea | 15 | 768 | Risk Ratio (IV, Random, 95% CI) | 1.36 [0.90, 2.06] |
| 14.3.12 Thirst | 4 | 224 | Risk Ratio (IV, Random, 95% CI) | 3.32 [1.10, 10.01] |
| 14.3.13 Vomiting | 13 | 793 | Risk Ratio (IV, Random, 95% CI) | 1.34 [0.91, 1.98] |
| 14.4 Adverse effects: immune system | 2 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 14.4.1 Fever | 2 | 102 | Risk Ratio (IV, Random, 95% CI) | 2.94 [0.46, 18.53] |
| 14.4.2 Influenza | 1 | 31 | Risk Ratio (IV, Random, 95% CI) | 0.31 [0.01, 7.15] |
| 14.5 Adverse effects: metabolic (dichotomous) | 27 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 14.5.1 Decreased appetite | 15 | 806 | Risk Ratio (IV, Random, 95% CI) | 1.62 [0.95, 2.75] |
| 14.5.2 Hypoglycemia | 2 | 120 | Risk Ratio (IV, Random, 95% CI) | 0.71 [0.09, 5.68] |
| 14.5.3 Hypokalemia | 4 | 331 | Risk Ratio (IV, Random, 95% CI) | 12.48 [4.04, 38.62] |
| 14.5.4 Hyponatremia | 1 | 38 | Risk Ratio (IV, Random, 95% CI) | 3.00 [0.13, 69.31] |
| 14.5.5 Increased appetite | 14 | 676 | Risk Ratio (IV, Random, 95% CI) | 1.42 [1.02, 1.98] |
| 14.5.6 Weight gain | 2 | 39 | Risk Ratio (IV, Random, 95% CI) | 0.32 [0.04, 2.77] |
| 14.5.7 Weight loss | 4 | 306 | Risk Ratio (IV, Random, 95% CI) | 1.49 [0.50, 4.39] |
| 14.5.8 Weight loss (0.12‐0.67 kg) | 1 | 11 | Risk Ratio (IV, Random, 95% CI) | 9.43 [0.65, 137.77] |
| 14.5.9 Weight loss (0.45‐2.19 kg) | 1 | 11 | Risk Ratio (IV, Random, 95% CI) | 0.17 [0.01, 2.92] |
| 14.6 Adverse effects: metabolic (continuous) | 1 | 23 | Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.24, 0.50] |
| 14.6.1 Change in weight (kg) | 1 | 23 | Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.24, 0.50] |
| 14.7 Adverse effects: musculoskeletal | 8 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 14.7.1 Arthralgia | 1 | 10 | Risk Ratio (IV, Random, 95% CI) | 0.33 [0.02, 6.65] |
| 14.7.2 Difficulty walking | 1 | 40 | Risk Ratio (IV, Random, 95% CI) | 0.20 [0.01, 3.92] |
| 14.7.3 Impaired balance | 1 | 12 | Risk Ratio (IV, Random, 95% CI) | 1.67 [0.08, 33.75] |
| 14.7.4 Myalgia | 2 | 155 | Risk Ratio (IV, Random, 95% CI) | 1.54 [0.79, 3.04] |
| 14.7.5 Slow movement | 1 | 31 | Risk Ratio (IV, Random, 95% CI) | 4.17 [0.22, 80.25] |
| 14.7.6 Stiffness | 2 | 43 | Risk Ratio (IV, Random, 95% CI) | 2.03 [0.41, 10.15] |
| 14.7.7 Weakness | 3 | 90 | Risk Ratio (IV, Random, 95% CI) | 0.63 [0.21, 1.89] |
| 14.8 Adverse effects: neurological | 33 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 14.8.1 Agitation/excitement | 5 | 220 | Risk Ratio (IV, Random, 95% CI) | 0.76 [0.39, 1.48] |
| 14.8.2 Anxiety | 3 | 250 | Risk Ratio (IV, Random, 95% CI) | 1.06 [0.44, 2.57] |
| 14.8.3 Daytime drowsiness | 6 | 172 | Risk Ratio (IV, Random, 95% CI) | 1.57 [0.75, 3.28] |
| 14.8.4 Dazed | 1 | 11 | Risk Ratio (IV, Random, 95% CI) | 2.57 [0.13, 52.12] |
| 14.8.5 Difficulty concentrating | 1 | 12 | Risk Ratio (IV, Random, 95% CI) | 2.50 [0.42, 14.83] |
| 14.8.6 Difficulty sleeping | 6 | 326 | Risk Ratio (IV, Random, 95% CI) | 0.81 [0.44, 1.50] |
| 14.8.7 Dizziness | 9 | 441 | Risk Ratio (IV, Random, 95% CI) | 1.21 [0.67, 2.18] |
| 14.8.8 Drowsiness | 5 | 298 | Risk Ratio (IV, Random, 95% CI) | 3.45 [1.21, 9.81] |
| 14.8.9 Fatigue | 7 | 338 | Risk Ratio (IV, Random, 95% CI) | 1.23 [0.70, 2.17] |
| 14.8.10 Headache | 18 | 943 | Risk Ratio (IV, Random, 95% CI) | 0.91 [0.66, 1.26] |
| 14.8.11 Hypoactivity | 3 | 28 | Risk Ratio (IV, Random, 95% CI) | 0.44 [0.07, 2.95] |
| 14.8.12 Increased aggression | 4 | 149 | Risk Ratio (IV, Random, 95% CI) | 0.78 [0.36, 1.70] |
| 14.8.13 Increased hyperactivity | 6 | 321 | Risk Ratio (IV, Random, 95% CI) | 0.75 [0.35, 1.58] |
| 14.8.14 Increased irritability | 5 | 177 | Risk Ratio (IV, Random, 95% CI) | 1.11 [0.71, 1.72] |
| 14.8.15 Increased stereotypies | 1 | 41 | Risk Ratio (IV, Random, 95% CI) | 0.52 [0.10, 2.80] |
| 14.8.16 Insomnia | 8 | 488 | Risk Ratio (IV, Random, 95% CI) | 1.04 [0.66, 1.65] |
| 14.8.17 Migraine | 1 | 10 | Risk Ratio (IV, Random, 95% CI) | 3.00 [0.15, 59.89] |
| 14.8.18 Nervousness | 4 | 159 | Risk Ratio (IV, Random, 95% CI) | 1.86 [0.47, 7.37] |
| 14.8.19 New onset seizures | 1 | 46 | Risk Ratio (IV, Random, 95% CI) | 0.33 [0.01, 7.78] |
| 14.8.20 Restlessness | 5 | 158 | Risk Ratio (IV, Random, 95% CI) | 1.22 [0.53, 2.82] |
| 14.8.21 Rocking | 1 | 11 | Risk Ratio (IV, Random, 95% CI) | 0.29 [0.01, 5.79] |
| 14.8.22 Sedation | 13 | 624 | Risk Ratio (IV, Random, 95% CI) | 0.93 [0.61, 1.42] |
| 14.8.23 Syncope | 1 | 89 | Risk Ratio (IV, Random, 95% CI) | 2.80 [0.30, 25.94] |
| 14.8.24 Tremor | 4 | 140 | Risk Ratio (IV, Random, 95% CI) | 1.80 [0.44, 7.37] |
| 14.8.25 Twitching | 2 | 71 | Risk Ratio (IV, Random, 95% CI) | 3.60 [0.42, 31.04] |
| 14.9 Adverse effects: psychological | 10 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 14.9.1 Anorexia | 1 | 20 | Risk Ratio (IV, Random, 95% CI) | 0.53 [0.20, 1.40] |
| 14.9.2 Aggression | 1 | 150 | Risk Ratio (IV, Random, 95% CI) | 1.17 [0.37, 3.66] |
| 14.9.3 Depression | 3 | 108 | Risk Ratio (IV, Random, 95% CI) | 1.93 [0.62, 6.00] |
| 14.9.4 Increased self‐injurious behaviour | 3 | 105 | Risk Ratio (IV, Random, 95% CI) | 0.46 [0.11, 1.84] |
| 14.9.5 Irritability | 2 | 162 | Risk Ratio (IV, Random, 95% CI) | 0.91 [0.36, 2.27] |
| 14.9.6 Mental symptoms | 1 | 20 | Risk Ratio (IV, Random, 95% CI) | 1.00 [0.41, 2.45] |
| 14.9.7 Repetitive behaviour | 1 | 46 | Risk Ratio (IV, Random, 95% CI) | 0.50 [0.05, 5.14] |
| 14.9.8 Worsening of temper tantrums | 2 | 52 | Risk Ratio (IV, Random, 95% CI) | 1.88 [0.30, 11.83] |
| 14.10 Adverse effects: respiratory | 6 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 14.10.1 Aggravation of asthma | 1 | 71 | Risk Ratio (IV, Random, 95% CI) | 3.26 [0.14, 77.35] |
| 14.10.2 Congestion/cold | 4 | 256 | Risk Ratio (IV, Random, 95% CI) | 1.02 [0.62, 1.68] |
| 14.10.3 Cough | 3 | 248 | Risk Ratio (IV, Random, 95% CI) | 1.16 [0.55, 2.49] |
| 14.10.4 Ear infection | 1 | 31 | Risk Ratio (IV, Random, 95% CI) | 1.88 [0.19, 18.60] |
| 14.10.5 Lung congestion | 1 | 20 | Risk Ratio (IV, Random, 95% CI) | 1.00 [0.60, 1.68] |
| 14.10.6 Nasopharyngitis | 1 | 150 | Risk Ratio (IV, Random, 95% CI) | 0.78 [0.22, 2.79] |
| 14.10.7 Respiratory adverse effects | 1 | 71 | Risk Ratio (IV, Random, 95% CI) | 5.43 [0.27, 109.19] |
| 14.11 Adverse effects: skin | 12 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 14.11.1 Hives | 1 | 31 | Risk Ratio (IV, Random, 95% CI) | 0.31 [0.01, 7.15] |
| 14.11.2 Itches | 2 | 62 | Risk Ratio (IV, Random, 95% CI) | 0.55 [0.07, 4.19] |
| 14.11.3 Rash | 7 | 440 | Risk Ratio (IV, Random, 95% CI) | 0.76 [0.30, 1.92] |
| 14.11.4 Skin adverse effects | 1 | 71 | Risk Ratio (IV, Random, 95% CI) | 1.09 [0.16, 7.30] |
| 14.11.5 Skin lesion | 2 | 98 | Risk Ratio (IV, Random, 95% CI) | 1.66 [0.74, 3.70] |
| 14.12 Adverse effects: urinary | 5 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 14.12.1 Diuresis | 1 | 89 | Risk Ratio (IV, Random, 95% CI) | 0.93 [0.25, 3.51] |
| 14.12.2 Enuresis | 3 | 205 | Risk Ratio (IV, Random, 95% CI) | 2.70 [0.82, 8.87] |
| 14.12.3 Urinary retention | 2 | 88 | Risk Ratio (IV, Random, 95% CI) | 0.74 [0.05, 10.49] |
| 14.12.4 Urinary tract infection | 1 | 31 | Risk Ratio (IV, Random, 95% CI) | 0.31 [0.01, 7.15] |
| 14.13 Adverse effects: other | 7 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 14.13.1 Blurred vision | 1 | 31 | Risk Ratio (IV, Random, 95% CI) | 2.50 [0.11, 56.98] |
| 14.13.2 Dilated pupils | 1 | 20 | Risk Ratio (IV, Random, 95% CI) | 0.67 [0.05, 9.19] |
| 14.13.3 Fever | 1 | 150 | Risk Ratio (IV, Random, 95% CI) | 0.49 [0.13, 1.88] |
| 14.13.4 Sweating | 3 | 129 | Risk Ratio (IV, Random, 95% CI) | 0.75 [0.15, 3.86] |
| 14.13.5 Vision: conjunctivitis | 1 | 10 | Risk Ratio (IV, Random, 95% CI) | 0.33 [0.02, 6.65] |
| 14.14 Tolerability/acceptability: loss to follow‐up | 30 | 1913 | Risk Ratio (IV, Random, 95% CI) | 1.07 [0.89, 1.28] |
| 14.15 Subgroup analyses: age ‐ irritability (option 1) | 28 | 1242 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.42, ‐0.00] |
| 14.15.1 Children only | 23 | 1014 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.46, 0.04] |
| 14.15.2 Adults only | 3 | 84 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.69, 0.17] |
| 14.15.3 Children and adults | 2 | 144 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.61, 0.05] |
| 14.16 Subgroup analyses: age ‐ irritability (option 2) | 28 | 1179 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.42, 0.01] |
| 14.16.1 Celecoxib: children only | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.27 [‐1.95, ‐0.58] |
| 14.16.2 D‐cycloserine: children only | 1 | 67 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.53, 0.43] |
| 14.16.3 Dextromethorphan: children only | 1 | 8 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐1.52, 1.26] |
| 14.16.4 Mecamylamine: children only | 1 | 20 | Std. Mean Difference (IV, Random, 95% CI) | 0.18 [‐0.71, 1.08] |
| 14.16.5 Riluzole: children only | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.63 [‐1.27, 0.00] |
| 14.16.6 Riluzole: children and adults | 1 | 14 | Std. Mean Difference (IV, Random, 95% CI) | 0.18 [‐0.87, 1.23] |
| 14.16.7 Pioglitazone: children only | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.77 [‐1.42, ‐0.13] |
| 14.16.8 N‐acetylcysteine: children only | 4 | 125 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐1.16, ‐0.06] |
| 14.16.9 Trichuris suis ova: adults only | 1 | 10 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐1.50, 1.00] |
| 14.16.10 Tetrahydrobiopterin: children only | 1 | 46 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.68, 0.48] |
| 14.16.11 Lofexedine: children only | 1 | 12 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐1.66, 0.66] |
| 14.16.12 Naltrexone: adults only | 1 | 20 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐1.05, 0.70] |
| 14.16.13 Minocycline: children only | 1 | 46 | Std. Mean Difference (IV, Random, 95% CI) | 0.89 [0.28, 1.50] |
| 14.16.14 Propentofylline: children only | 1 | 48 | Std. Mean Difference (IV, Random, 95% CI) | 0.56 [‐0.01, 1.14] |
| 14.16.15 Sulforaphane: children only | 1 | 60 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.86 [‐1.39, ‐0.33] |
| 14.16.16 Folinic acid: children only | 1 | 55 | Std. Mean Difference (IV, Random, 95% CI) | 0.63 [0.08, 1.17] |
| 14.16.17 L‐carnosine: children only | 1 | 42 | Std. Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.41, 0.80] |
| 14.16.18 Prednisolone (steroid): children only | 1 | 26 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.96, 0.58] |
| 14.16.19 Dextromethorphan/quinidine: adults only | 1 | 14 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐1.43, 0.69] |
| 14.16.20 Pregnenolone: children only | 1 | 59 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.55 [‐1.07, ‐0.03] |
| 14.16.21 Baclofen: children only | 1 | 58 | Std. Mean Difference (IV, Random, 95% CI) | 0.88 [0.34, 1.42] |
| 14.16.22 Palmitoylethanolamide: children only | 1 | 62 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.49 [‐1.00, 0.01] |
| 14.16.23 Bumetanide: children only | 1 | 75 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.55, 0.35] |
| 14.16.24 Resveratol: children only | 1 | 62 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.79, 0.21] |
| 14.16.25 Arbaclofen: children and adults | 1 | 130 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.68, 0.02] |
| 14.17 Subgroup analyses: age ‐ self‐injury (option 1) | 3 | 147 | Std. Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.30, 0.35] |
| 14.17.1 Children only | 2 | 127 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.29, 0.44] |
| 14.17.2 Adults only | 1 | 20 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.31 [‐1.20, 0.57] |
| 14.18 Subgroup analyses: age ‐ self‐injury (option 2) | 5 | 285 | Std. Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.09, 0.38] |
| 14.18.1 N‐acetylcysteine: children only | 1 | 98 | Std. Mean Difference (IV, Random, 95% CI) | 0.18 [‐0.22, 0.58] |
| 14.18.2 N‐acetylcysteine: children only | 1 | 29 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.99, 0.48] |
| 14.18.3 Trichuris suis ova: adults only | 1 | 10 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐1.55, 0.95] |
| 14.18.4 Bumetanide: children only | 2 | 148 | Std. Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.21, 0.60] |
14.15. Analysis.

Comparison 14: Experimental versus placebo, Outcome 15: Subgroup analyses: age ‐ irritability (option 1)
14.16. Analysis.

Comparison 14: Experimental versus placebo, Outcome 16: Subgroup analyses: age ‐ irritability (option 2)
14.17. Analysis.

Comparison 14: Experimental versus placebo, Outcome 17: Subgroup analyses: age ‐ self‐injury (option 1)
14.18. Analysis.

Comparison 14: Experimental versus placebo, Outcome 18: Subgroup analyses: age ‐ self‐injury (option 2)
Comparison 15. Typical antipsychotic vs placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 15.1 Self‐injury | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 15.2 Adverse effects: musculoskeletal | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 15.2.1 Dystonia | 1 | 23 | Risk Ratio (IV, Random, 95% CI) | 2.36 [0.11, 52.41] |
| 15.3 Adverse effects: neurological | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 15.3.2 Fatigue/lethargy | 1 | 23 | Risk Ratio (IV, Random, 95% CI) | 8.64 [0.53, 140.05] |
| 15.4 Adverse effects: psychological | 1 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 15.4.1 Behaviour problems | 1 | 23 | Risk Ratio (IV, Random, 95% CI) | 0.34 [0.16, 0.73] |
| 15.5 Tolerability/acceptabiity: loss to follow‐up | 2 | 40 | Risk Ratio (IV, Random, 95% CI) | 0.46 [0.14, 1.49] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Akhondzadeh 2004.
| Study characteristics | ||
| Methods | Parallel trial of haloperidol + cyproheptadine versus haloperidol + placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: speciality clinic for children at Roozbeh Psychiatric teaching hospital, Tehran, Iran Sample size: 40 Number of withdrawals/dropouts: none reported Gender: 24 boys, 16 girls Mean age: haloperidol + cyproheptadine = 6.4 years; haloperidol + placebo = 6.9 years IQ: not reported Baseline ABC‐I scores or other behaviours of concern: not reported Concomitant medications: not reported History of previous medications: not reported |
|
| Interventions | Intervention (haloperidol + cyproheptadine) for 8
weeks (20 participants): cyproheptadine was titrated
up to 0.2 mg/kg/day; haloperidol was titrated up to
0.05 mg/kg/day Comparator (haloperidol + placebo) for 8 weeks (20 participants): haloperidol was titrated up to 0.05 mg/kg/day; placebo was not described |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: not reported Timing of outcome assessment: baseline, 2, 4, 6 and 8 weeks |
|
| Notes | Study start date: January 2002 Study end date: January 2003 Funding source: Tehran University of Medical Sciences Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised to receive cyproheptadine or placebo in a 1: 1 ratio using a computer‐generated code. |
| Allocation concealment (selection bias) | Low risk | The assignments were kept in sealed, opaque envelopes until the point of allocation. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Throughout the study, the person who administered the medications, the rater and the patients were blind to assignments." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Throughout the study, the person who administered the medications, the rater and the patients were blind to assignments." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All 40 randomised patients completed the trial. No loss to follow up reported |
| Selective reporting (reporting bias) | Low risk | All primary outcomes appear to have been reported. |
| Other bias | High risk |
|
Akhondzadeh 2008.
| Study characteristics | ||
| Methods | Parallel trial of piracetam + risperidone versus placebo + risperidone | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: outpatient clinic of Roozbeh psychiatric hospital, Iran Sample size: 40 (20 each group) Number of withdrawals/dropouts: none reported Gender: 30 boys, 10 girls Mean age: piracetam = 6.9 years; placebo = 6.75 years IQ: not reported Baseline ABC‐I scores or other behaviours of concern: not reported Concomitant medications: not reported History of previous medications: piracetam: 8/20 had taken risperidone, 4/20 had taken haloperidol; placebo: 10/20 had taken risperidone, 3/20 had taken haloperidol |
|
| Interventions | Intervention (piracetam + risperidone) for 10 weeks:
piracetam dose was titrated up to 800 mg/day (200
mg/day starting dosage with 200 mg increments every
2 days). Risperidone was titrated up to 2 mg/day as
fixed dose for children 10‐40 kg or 3 mg/day for
children ≥ 41 kg. Comparator (placebo + risperidone) for 10 weeks: risperidone was titrated up to 2 mg/day as fixed dose for children 10‐40 kg or 3 mg/day for children ≥ 41 kg. Placebo was not described. |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: none reported Timing of outcome assessment: baseline, 2, 4, 6, 8 and 10 weeks |
|
| Notes | Study start date:January 2004 Study end date: January 2006 Funding source: grant from Tehran University of Medical Sciences Conflicts of interest: none reported Trial registry ‐ none reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomised to receive piracetam or placebo in a 1:1 ratio using a computer‐generated code." |
| Allocation concealment (selection bias) | Low risk | Quote: "The assignments were kept in sealed, opaque envelopes until the point of data analysis" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Throughout the study, the person who administered the medications, the rater and the patients were blind to assignments." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Throughout the study, the person who administered the medications, the rater and the patients were blind to assignments." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | All participants were reported to have completed the
entire study, however other details are vague such
as "about 18 patients were excluded from the study".
Some detail is provided about this exclusion, "they
were receiving other psychotropic medications or had
other significant active medical problems such as
epilepsy". LTFU: no dropouts reported |
| Selective reporting (reporting bias) | High risk | Endpoint data were not reported despite the ABC being the primary outcome measure and apparently measured 6 times throughout the study. |
| Other bias | High risk |
|
Akhondzadeh 2010.
| Study characteristics | ||
| Methods | Parallel trial of pentoxifylline + risperidone versus placebo + risperidone | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: children's outpatient clinic of Roozbeh Psychiatric Hospital, Tehran, Iran Sample size: 40 Number of withdrawals/dropouts: none reported Gender: 29 boys, 11 girls Mean age: risperidone + pentoxifylline = 8.05 years; placebo = 7.37 years IQ: not reported Baseline ABC‐I scores or other behaviours of concern: risperidone + pentoxifylline = 16.67; risperidone + placebo = 16.06 Concomitant medications: 0% History of previous medications: risperidone + pentoxifylline: 12/20 participants had previously received risperidone, 2/20 participants had previously received haloperidol; risperidone + placebo: 13/20 participants had previously received risperidone, 3/20 had previously received haloperidol |
|
| Interventions | Pentoxifylline + risperidone for 10 weeks (n = 20):
pentoxifylline titrated up to 400 mg/day for
children between 10 and 40 kg; or up to 600 mg for
children weighing > 40 kg. The dose of
risperidone was titrated up to 2 mg/day (0.5 mg
starting dosage with 0.5 mg increments in weekly
dosage for the first 3 weeks) for children between
10 and 40 kg and 3 mg/day for children weighting
above 40 kg. Risperidone + placebo for 10 weeks (n = 20): risperidone was titrated up to 2 mg/day (0.5 mg starting dosage with 0.5 mg increments in weekly dosage for the first 3 weeks) for children between 10 and 40 kg and 3 mg/day for children weighing > 40 kg. |
|
| Outcomes | Primary outcomes ‐ irritability, measured using the
Abberant Behaviour Checklist and five subscales
(Aman
1985); AEs Secondary outcomes: none reported Timing of outcome assessment: baseline, 2, 4, 6, 8 and 10 weeks |
|
| Notes | Study start date: April 2007 Study end date: 2009 Funding source: Tehran University of Medical Sciences Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised to receive pentoxifylline or placebo in a 1:1 ratio using a computer‐generated code. |
| Allocation concealment (selection bias) | Low risk | The assignments were kept in sealed, opaque envelopes until the point of data analysis. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Throughout the study, the person who administered the medications, the rater and the patients were blind to assignments. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Throughout the study, the person who administered the medications, the rater and the patients were blind to assignments. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | LTFU: none reported. All participants completed the trial and there were no missing data. |
| Selective reporting (reporting bias) | Low risk | Outcomes match protocol http://www.irct.ir/trial/857 |
| Other bias | High risk |
|
Aman 2017.
| Study characteristics | ||
| Methods | 12‐week parallel trial of memantine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: USA Sample size: 121 randomised (61 memantine, 60 placebo) Reasons for withdrawals/ dropouts: memantine, 6 discontinued (3 AEs, 2 LTFU, 1 withdrew consent); placebo: 11 discontinued (4 AEs, 1 insufficient response, 1 protocol violation, 3 withdrew consent, 2 LTFU) Gender: 80% and 87% male participants in the memantine and placebo groups, respectively Mean age: not reported IQ: not reported Baseline ABC‐I or other BoC scale: not reported Concomitant medications: not reported Previous medications: not reported |
|
| Interventions | Intervention (memantine): once daily oral
administration of memantine extended release for 12
weeks. Memantine = 3 mg and 6 mg capsules, dose
ranging 3‐18 mg/day in 4 weight groups Comparator (placebo): once daily oral administration of placebo for 12 weeks Timing of outcome assessments: baseline, weeks 2, 4, 6, 8, 10 and 12 |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: tolerability |
|
| Notes | Study start date: April 2009 Study end date: February 2013 Funding: "This study was supported by funding from Forest Laboratories, LLC, (Jersey City, New Jersey), Allergan. The study sponsor was involved in the study design, data collection (via contracted clinical investigator sites), analysis and interpretation of data, and the decision to present these results." Conflicts of interest: involvement with pharmaceutical companies either in advisory roles, research grants from pharmaceutical companies, or being employed by study sponsor. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomization codes were generated and securely retained by the Statistical Programming and Drug Safety Surveillance Department at Forest Research Institute, Inc" |
| Allocation concealment (selection bias) | Low risk | Quote: "The randomization codes were generated and securely retained by the Statistical Programming and Drug Safety Surveillance Department at Forest Research Institute, Inc" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk |
|
| Blinding of outcome assessment (detection bias) All outcomes | Low risk |
|
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants were accounted for and an ITT analysis was used |
| Selective reporting (reporting bias) | High risk | ABC was listed as an outcome and measured at baseline, weeks 6 and 12. None were reported |
| Other bias | High risk | Pharma funded and involved in analysis etc |
Anagnostou 2012.
| Study characteristics | ||
| Methods | 6‐week parallel trial of oxytocin versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: New York, USA Sample size: 19 adults Number of withdrawals/dropouts: oxytocin = 1 discontinued at week 4 because of staring spells; placebo = 2 discontinued, 1 at week 4 due to increased tics, and the other at baseline for not tolerating intranasal formulation Gender: 16 male participants, 3 female participants Mean age: 33.2 (SD 13.29) IQ: oxytocin = 99; placebo = 118 Baseline ABC‐I or other behaviours of concern: quality of life: oxytocin = 47.8; placebo = 65.2 Concomitant medications: not reported History of previous medications: not reported |
|
| Interventions | Intervention (oxytocin) for 6 weeks: oxytocin
(Syntocinon; NOVARTIS) dosage was 24 IU (6
intranasal spray puffs) twice‐daily for 6 weeks Comparator (placebo) for 6 weeks: placebo was saline solution in an identical bottle and label to oxytocin |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: QoL, measured using the WHOQOL emotional (WHO 1998); tolerability Timing of outcome assessment: AEs were recorded every 2 weeks. QoL was measured twice during the 6‐week study: at baseline and at conclusion of the study. |
|
| Notes | Study start date: June 2006 Study end date: April 2012 Funding: a hospital and an autism centre funded the study Conflicts of interest: the primary author (EA) at the time of the study was receiving funding for other studies relating to the same pharmacological intervention, the other authors were also receiving funding for other clinical trials involving people with ASD. Trial registry ‐ NCT00490802 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A computer‐generated randomisation table was created by the research pharmacist and used to randomise participants. |
| Allocation concealment (selection bias) | Unclear risk | No details provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No details provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants were anlaysed using an ITT anlaysis and baseline and endpoint QoL scores were recorded. |
| Selective reporting (reporting bias) | Low risk | The primary and secondary outcomes of interest were recorded on clinicaltrials.gov and all results were provided. |
| Other bias | Unclear risk | No information |
Aran 2021.
| Study characteristics | ||
| Methods | 12‐week cross‐over trial of cannabidiol versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: Shaare Zedek Medical Center, Jerusalem, Israel Sample size: pure cannabis (44), placebo (44) Reasons for withdrawals/dropouts:
Gender: 80% male, 20% female Mean age: 11.8 (SD4.1) years IQ: not reported Baseline ABC‐I or other BoC scale: Concomitant medications: any medication 72%; antipsychotics 54%; SSRIs 15%; antiepileptics 12%; stimulants 12%; benzodiazepines 7%; alpha‐2 agonists 4% Previous medications: details not provided |
|
| Interventions | Intervention (pure cannabinoids): 99% pure
cannabidiol (CBD) and 99% pure tetrahydrocannabinol
in a 20:1 ratio at 1 mg/kg cannabidiol/d,
up‐titrated until intolerance or to a maximum dose
of 10 mg/kg CBD/d, divided to 3 daily doses, for 3
months Comparator (placebo): oral olive oil and flavors that mimic in texture and flavour the cannabinoid solution. |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: none reported Timing of outcome assessments: 1 month, 2 months, and 3 months (endpoint) |
|
| Notes | Study start date: January 2017 Study end date: December 2018 Funding: the study was funded by BOL Pharma, Revadim, Israel and the National Institute for Psychobiology in Israel (#203‐17‐18). Conflicts of interest: details not provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Allocation to treatment arm was based on a randomisation list. Randomisation scheme was generated by BioStats Statistical Consulting Ltd. |
| Allocation concealment (selection bias) | Low risk | Allocation to treatment arm was based on a randomisation list. Randomisation scheme was generated by BioStats Statistical Consulting Ltd. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The code key was kept by BioStats Statistical Consulting Ltd. until study end. Neither the principal investigator nor any other team member or individual had access to the codes until study end. No unblinding occurred during the study. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The code key was kept by BioStats Statistical Consulting Ltd. until study end. Neither the principal investigator nor any other team member or individual had access to the codes until study end. No unblinding occurred during the study. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 12% overall attrition, doesn't appear to be bias in dropout reason |
| Selective reporting (reporting bias) | Low risk | it appears that all outcomes listed on trial registry have been reported |
| Other bias | High risk | The study was funded by BOL Pharma, Revadim, Israel. |
Arnold 2006.
| Study characteristics | ||
| Methods | 6‐week cross‐over trial of atomoxetine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria: "cardiovascular disease, glaucoma, unstable seizure disorder, other significant physical illness, psychosis, severe mood disorder, substance abuse, or pregnancy." Location/setting: details not provided Sample size: 16 Reasons for withdrawals/dropouts: 3 terminated early, 1 each after the 3rd, 4th, and 5th weeks of the second condition (1 on atomoxetine, 2 on placebo). The last observation was carried forward to endpoint for anyone who discontinued the trial. Gender: 12 male, 4 female Mean age: 9.26 years (SD2.93) IQ: details not provided Baseline ABC‐I or other BoC scale: ABC‐Irritability 16.00 (intervention group); 14.18 (placebo group) Concomitant medications: 6 participants were taking psychotropics during the trial (risperidone (3), aripiprazole (1), sertraline (1), divalproex (1), ziprasidone (1), and paroxetine (1). Previous medications: details not provided |
|
| Interventions | Intervention (atomoxetine) for 6 weeks: "Atomoxetine
in six sizes from 2.5 to 40 mg were supplied by the
manufacturer (Eli Lilly). They were administered in
split doses, morning and afternoon, starting at 0.25
mg/kg/day and increased every 4 to 5 days by
increments of 0.3 to 0.4 mg/kg/day, unless limiting
side effects or satisfactory clinical results
occurred first. The maximum daily dose was 1.4
mg/kg/day, not to exceed 100 mg/day total. For
subjects also taking a significant CYP2D6 inhibitor
(such as antidepressants or neuroleptics), the dose
increments were 0.2 to 0.3 mg/kg/day and dose was
capped at 1.2 mg/kg/day." Comparator (placebo) for 6 weeks: equivalent placebo |
|
| Outcomes | Primary outcomes: irritability (measured using the
ABC‐I subscale (Aman 1985), self‐injurious behaviour
(measured using the Repetitive Behaviour Checklist
(self‐injury subscale) (Bodfish 2000),
AEs Secondary outcomes: none reported Timing of outcome assessments: baseline, week 6 (endpoint) |
|
| Notes | Study start date: details not provided Study end date: details not provided Funding: "The authors receive research funding from Lilly, Shire, Janssen, and PediaMed and are on speakers_ bureaus of and/or consult for Shire, Novartis, Janssen, Sigma Tau, and Forest Laboratories." Conflicts of interest: details not provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "randomization to order of conditions and stratification on autistic disorder versus other ASD diagnoses" |
| Allocation concealment (selection bias) | High risk | "randomization to order of conditions and stratification on autistic disorder versus other ASD diagnoses" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Apart from saying it was a double‐blinded study, no further details were provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Apart from saying it was a double‐blinded study, no further details were provided. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No info on 2 out of 3 of the dropouts |
| Selective reporting (reporting bias) | Unclear risk | Without a protocol it is difficult to know if all outcomes were reported. |
| Other bias | High risk | Matched placebo and atomoxetine in 6 sizes from 2.5 to 40 mg were supplied by the manufacturer (Eli Lilly) and Eli Lilly supported the study. |
Arnold 2012a.
| Study characteristics | ||
| Methods | Parallel trial of mecamylamine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: not reported Sample size: 20 Number of withdrawals/dropouts: 2 in Intervention group dropped out after 4 weeks Gender: treatment = 11 male participants, 1 female participant; placebo = 6 male participants, 2 = female participants Mean age: mecamylamine = 6.76 (SD 2.24); placebo = 8.36 (SD 2.83) years IQ: an IQ of > 36 or mental age of > 18 months. Mean IQ mecamylamine group = 77.58, placebo mean IQ = 62.62 Baseline ABC‐I scores or other BoC scale: mecamylamine = 12.75, placebo = 12.88 Concomitant medications: medications were allowed except for antipsychotic medications in the 3 months prior to the study and medications for unstable seizure disorders History of previous medications: not reported |
|
| Interventions | Mecamylamine for 14 weeks (n = 12): fixed dosages
starting at 0.5 mg/day oral mecamylamine increasing
in week 6 to 2.5 mg/day for 2 weeks, and increasing
again to 5 mg/day for a further 6 weeks if
tolerated Placebo for 14 weeks (n = 8): matched placebo starting at 0.5 mg/day, increasing in week 6 to 2.5 mg/day for 2 weeks, and increasing again to 5 mg/day for a further 6 weeks if tolerated |
|
| Outcomes | Primary outcomes:
Secondary outcomes: tolerability Timing of outcome assessments: baseline and weeks 2, 6, 8, 10, and 14 |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: a grant from Autism Speaks Conflicts of interest: Dr Arnold receives or has recently received research support or consulting honoraria from Lilly, Shire, Curemark, Neuropharm,Noven, Organon, Seaside Therapeutics, Targacept, Biomarin, and Astra Zeneca. Dr Aman has received consulting honoraria or research support from Bristol‐Myers Squibb, Johnson and Johnson,Forrest, Novartis, and Supernus. Dr Anand, Ms Bates, Ms Farmer, Ms Hollway, Dr Hurt, Dr Li, Dr Ramadan, MsThompson, and Dr Williams have no affiliations to report. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Details not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | LOCF was used for the 2 participants who did not complete the entire trial. |
| Selective reporting (reporting bias) | Unclear risk | ABC data collected each fortnight not reported ‐ only change from baseline weeks 6, 8, 14 |
| Other bias | Unclear risk | Quote: "Dr. Arnold receives or has received recently research support or consulting honoraria from Lilly, Shire, Curemark, Neuropharm, Noven, Organon, Seaside Therapeutics, Targacept, BioMarin, and AstraZeneca. Dr. Aman has received consulting honoraria or research support from Bristol‐Myers Squibb, Johnson and Johnson, Forrest, Novartis and Supernus". |
Asadabadi 2013.
| Study characteristics | ||
| Methods | Parallel, placebo‐controlled trial of celecoxib + risperidone versus placebo + risperidone | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: children's outpatient clinic at Roozbeh hospital, Tehran, Iran Sample size: 40 Number of withdrawals/dropouts: none reported Gender: 25 boys, 15 girls Mean age: celcoxib = 7.6 (1.7) years; placebo = 7.5 (1.5) years IQ: not reported Baseline ABC‐I scores or other BoC scale: celecoxib = 17.3; placebo = 17.6 Concomitant medications: not reported History of previous medications: celecoxib + risperidone: 19/20 had previously taken risperidone, 1/20 had taken haloperidol previously; placebo + risperidone: 18/20 had taken risperidone previously, 2/20 had taken haloperidol previously |
|
| Interventions | Intervention (celecoxib + risperidone) for 10 weeks:
celecoxib (100 mg capsules) titrated up to 200
mg/day for children weighing < 30 kg and 300
mg/day for > 30 kg. Risperidone (0.5 mg tablets)
was titrated up to 2 mg/day (starting dose of 0.5 mg
with subsequent dose increase in 0.5 mg increments
in the weekly dosage for the first 3 weeks) for
children between 10 kg and 40 kg and 3 mg/day for
children weighing above 40 kg Comparator (placebo + risperidone) for 10 weeks: placebo not described. Risperidone (0.5 mg tablets) was titrated up to 2 mg/day (starting dose of 0.5 mg with subsequent dose increase in 0.5 mg increments in the weekly dosage for the first 3 weeks) for children between 10 kg and 40 kg and 3 mg/day for children weighing above 40 kg |
|
| Outcomes | Primary outcomes
Secondary outcome: none reported |
|
| Notes | Study start date: November 2009 Study end date: January 2012 Funding source: grant from Tehran University of Medical Sciences to Prof Shahin Akhondzadeh (grant No:. 8144) Conflict of interest: none reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomized in a 1:1 ratio using a computer‐generated code" |
| Allocation concealment (selection bias) | Low risk | Quote: "The assignments were kept in sealed, opaque envelopes until data analysis". "Separate persons were responsible for random allocation and interviewing the patients." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Throughout the study, the person who administered the medications, the rater, and the patients and their parents were blind to assignments". |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Throughout the study, the person who administered the medications, the rater, and the patients and their parents were blind to assignments". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No LTFU reported. All children included in the
analysis. Quote: "All patients completed the trial and there were no missing data." |
| Selective reporting (reporting bias) | Low risk | The ABC was reported at baseline and weeks 2, 4, 6, 8 and 10. |
| Other bias | High risk | Study was reduced from 10 weeks to 8 weeks and
|
Ayatollahi 2020.
| Study characteristics | ||
| Methods | 10‐week parallel trial of pregnenolone + risperidone or placebo + risperidone | |
| Participants | Inclusion criteria: "drug‐naive 11‐ to 17‐year‐old
adolescents who had met the Diagnostic and
Statistical Manual of Mental Disorders, Fifth
Edition' (DSM‐5
2013) who also display aggression,
over‐reactivity or repetitive behaviours,
ABC‐Irritability scores of at least 15 at
screening" Exclusion criteria:
Location/setting: psychiatric hospital in Iran Sample size: 64 (32 to each group) Reason for dropouts/withdrawals: 5; 2 withdrew from pregnenolone group due to withdrawing consent (prior to week 5), 3 from placebo group withdrew consent prior to week 5 Gender: placebo = 10/19 male participants, pregnenolone = 13/17 male participants Mean age: 13.5 years IQ: not reported Baseline ABC‐I or other BoC scores: pregnenolone = 23.23 (4.88), placebo = 23.24 (6.0) Concomitant medications ‐ not reported Previous medications: not reported |
|
| Interventions | Intervention: pregnenolone 100 mg twice daily +
risperidone 0.4 mg/day for those weighing 20‐45 kg,
up to a maximum of 2.5 mg/day for 10 weeks.
Participants weighing > 45 kg a maximum dose of
3.5 mg/day of risperidone Comparator: placebo capsules containing starch + risperidone 0.4 mg/day for those weighing 20‐45 kg, up to a maximum of 2.5 mg/day for 10 weeks. Participants weighing > 45 kg a maximum dose of 3.5 mg/day of risperidone |
|
| Outcomes | Primary outcomes: ABC‐Irritability (Aman 1985);
AEs Secondary outcomes: tolerability |
|
| Notes | Study start date: August 2018 Study end date: January 2020 Funding: "This study was supported by a grant from Tehran University of Medical Sciences to S.A. (Grant Number: 38138)." Conflicts of interest: "The authors have no conflicts of interest to declare." Trial registry ‐ IRCT20090117001556N112 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Using a computer‐generated code, patients were randomly allocated to 2 treatment arms by the permuted randomisation block method in a 1:1 ratio. |
| Allocation concealment (selection bias) | Low risk | The assigned group number for each participant was kept hidden in a sealed opaque envelope until data analysis. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Pregnenolone and matching placebo capsules were identical in terms of shape, colour, size, and smell. All measures were under management of an independent group not involved elsewhere in the study. Both participants and the research team were blinded to the group assignments. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All measures were under management of an independent group not involved elsewhere in the study. Both participants and the research team were blinded to the group assignments." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition, no other obvious issues with outcome data reporting |
| Selective reporting (reporting bias) | High risk | CARS noted in registration but not reported |
| Other bias | High risk |
|
Batebi 2021.
| Study characteristics | ||
| Methods | 10‐week parallel trial of folinic acid + risperidone versus placebo + risperidone | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: outpatient children with ASD attending Roozbeh Hospital, Tehran, Iran Sample size: 66 Reason for dropouts/withdrawals: folinic acid + risperidone: 5 withdrew consent prior to week 5; placebo + risperidone: 6 withdrew consent prior to week 5 (all withdrew consent) Mean age: folinic acid average age 8.36; placebo group average age 7.52 Mean IQ: not reported Gender: folinic acid 42.9% female, placebo group 29.6% female Baseline ABC‐I or other BoC scores: folinic acid 22.82, placebo 22.67 Concomitant medications: folinic acid and risperidone were initiated simultaneously. No other concomitant medication was allowed for neither of the trial groups. Previous medications: not reported |
|
| Interventions | Intervention: risperidone twice daily initiating at a
dose of 0.5 mg with a dose increase of 0.5 mg/week
(for the first 3 weeks). The maximum risperidone
dose for children < 20 kg was 1 mg/day, and for
children 20 kg or heavier was 2 mg/day,
respectively. Folinic acid (C20H23N7O7) dosage was 2
mg/kg up to 50 mg/day for the entire course of the
study. At the same time, the control group received
placebo capsules. Comparator: placebo + risperidone (1‐3.5 mg/day) for 10 weeks |
|
| Outcomes | Primary outcomes: irritability, measured using the
ABC‐Irritability subscale (Aman 1985);
adverse events Secondary outcomes: tolerability |
|
| Notes | Study start date: November 2018 Study end date: April 2019 Funding: "This study was funded by Tehran University of Medical Sciences and Health Services (Grant number 38898)." Conflicts of interest: "The authors declare that they have no conflict of interest" trial registry: IRCT20090117001556N114 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Using the Microsoft Office Excel software, a specific random code was allocated to each patient. The randomisation and allocation were conducted using block randomisation (with blocks of size 4) by the primary investigator of the study, who was not involved in the diagnosis and follow‐ups. |
| Allocation concealment (selection bias) | Low risk | The allocations were kept in confidential and sealed opaque envelops and were exposed at the end of the trial. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Separate individuals implemented randomizations, drug administration, rating, data entry, and statistical analysis. Moreover, patients, parents, and researchers were blinded to the allocations." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Separate individuals implemented randomizations, drug administration, rating, data entry, and statistical analysis. Moreover, patients, parents, and researchers were blinded to the allocations." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 17% dropout without actual reasons given (just says "consent withdrawal"), thus can't assess whether reasons for incomplete data could be related to outcome |
| Selective reporting (reporting bias) | High risk | The 2 primary outcomes listed on the trials registry were ABC and subscales, and CARS. CARS was not reported. |
| Other bias | High risk |
|
Behmanesh 2019.
| Study characteristics | ||
| Methods | 12‐week parallel study of propentofylline + risperidone versus placebo + risperidone | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: children attending Roozbeh Hospital, Iran Sample size: 48 (24 in each group) Mean age: 7 years Mean IQ: not reported Gender: 75% of all participants were boys Baseline ABC‐I scores: intervention 25.79 (5.39); placebo 26.29 (4.70) Reason for dropouts/withdrawals: 9 discontinued from each group. Propentofylline + risperidone: 5 withdrew consent and 4 excluded due to "lack of collaboration of their parents". Placebo + risperidone: 6 withdrew consent, 3 excluded due to "lack of collaboration of their parents" Concomitant medications: "no other concomitant intervention or medication was permitted neither for the propentofylline nor the placebo group" Previous medications: not reported |
|
| Interventions | Intervention (propentofylline + risperidone): 300 mg
propentofylline once daily in capsule form. The
dosage of propentofylline was increased to 600
mg/day (300 mg twice daily) after week 2, and for
those heavier than 45 kg, the dose was increased to
900 mg/day (300 mg thrice daily). Risperidone began
at a dose of 0.5 mg with a dose increase of 0.5 mg
each week for the first 3 weeks. The maximum dose
for participants < 20 kg was 1 mg/day and for
participants ≥ 20 kg was 2 mg/day. Comparator (placebo + risperidone): risperidone began at a dose of 0.5 mg with a dose increase of 0.5 mg each week for the first 3 weeks. The maximum dose for participants < 20 kg was 1 mg/day and for participants ≥ 20 kg was 2 mg/day. |
|
| Outcomes | Primary outcomes: irritability (change from baseline)
using the ABC‐I (Aman 1985); AEs Secondary outcomes ‐ tolerability |
|
| Notes | Study start date: November 2018 Study end date: April 2019 Funding: this study was supported by a grant from Tehran University of Medical Sciences to Prof Shahin Akhondzadeh (grant number 3899). Conflicts of interest: "The authors have no conflict of interest to disclose." Trial registry: IRCT20090117001556N113 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Using the Microsoft Office Excel software, the participants of the study were randomly assigned into 2 groups |
| Allocation concealment (selection bias) | Low risk | The assignments were retained in confidential and sealed opaque envelops and were unveiled at the study endpoint for statistical analysis |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Separate individuals were responsible for randomisations, drug administration, rating, data entry, and statistical analysis. The participants research investigators, nurses, and interviewers were all blinded to the treatment allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Separate individuals were responsible for randomisations, drug administration, rating, data entry, and statistical analysis. The participants, research investigators, nurses, and interviewers were all blinded to the treatment allocation. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 27% dropout from each group /missing outcome data |
| Selective reporting (reporting bias) | Low risk | ABC‐C and CARS prespecified outcomes, though trial endpoint timing different (10 weeks vs 12 weeks in protocol) |
| Other bias | High risk |
|
Belsito 2001.
| Study characteristics | ||
| Methods | Placebo‐controlled trial of lamotrigine versus placebo | |
| Participants | Inclusion criteria: "children 3‐11 years with a
primary diagnosis of autistic disorder, either with
early signs or following regression after a period
of normal development were enrolled." Exclusion criteria included "children with autistic disorder associated with comorbid medical etiologies, such as Fragile X syndrome or metabolic disorders" Location/setting: John Hopkins medical institutions Sample size: 35 Number of withdrawals/dropouts: lamotrigine 5; placebo 2 Gender: 33 boys, 2 girls Mean age: median age 5.8 (1.75) IQ: not reported Baseline ABC‐I scores or other BoC: not reported Concomitant medications: not reported History of previous medications: not reported |
|
| Interventions | Intervention (lamotrigine) for 18 weeks: 0.5 mg/kg
lamotrigine twice daily titrated to a maximum of 5.0
mg/kg twice daily over 12 weeks or placebo twice
daily Comparator (placebo) for 18 weeks: "participants received a placebo twice daily prepared in identically appearing tablets (shape, size, color, and taste)" |
|
| Outcomes | Primary outcomes: irritability, measured as change in
ABC‐ I subscale scores (Aman 1985);
AEs Secondary outcomes: none reported Timing of outcome assessment: baseline, 4, 8, 12 and 18 weeks |
|
| Notes | Study start date: not reported Study end date: not reported Funding source: Glaxo Wellcome Conflicts of interest: none declared Trial registry ‐ not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "the blinded sequence by which each patient received lamotrigine or placebo was determined by randomization at the end of baseline evaluations. Subjects were randomised via a computer‐generated cluster method which made user‐selected block assignments. Within each block, an equal number of patients received placebo or drug". |
| Allocation concealment (selection bias) | Low risk | Quote: "Codes were accessible to the investigational drug pharmacists and to the appointed safety committee". |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described apart from, "Codes were accessible to the investigational drug pharmacists and to the appointed safety committee." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described apart from, "Codes were accessible to the investigational drug pharmacists and to the appointed safety committee." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 22% LTFU ‐ lamotrigine: 4 children (3 due to insomnia, and 1 due to increased stereotypies; 2 LTFU in placebo group: 1 increased stereotypies, and 1 for increased echolalia |
| Selective reporting (reporting bias) | High risk | The paper reports that outcome measures were completed at baseline, 4, 8, 12 and 18 weeks. Results were only presented graphically. Paper reports to measure changes in ABC‐I and other subscales however "changes in irritability, lethargy, and hyperactivity were also insignificant between the groups" and only P values provided. |
| Other bias | Unclear risk | Quote: "The trial was supported by GlaxoWellcome". |
Bernaerts 2020.
| Study characteristics | ||
| Methods | 4‐week parallel trial of oxytocin versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria: any neurological or genetic disorder, or contraindication for MRI Location/ setting: autism centre at the Leuven University Hospital, Belgium Sample size: oxytocin 22; placebo 18 Reasons for dropouts/withdrawal: the reason was not provided for the 1 participant from the placebo group who was not included in the analysis. Mean IQ: approx 103 for both groups Mean age: 24.5 years Gender: details not provided Baseline ABC‐I or other BoC scale: oxytocin: WHO QoL 82.91 (14.04); placebo 85.24 (9.63) Concomitant medications: 6/22 in oxytocin group were on psychostimulants. Other medications included antidepressants, aripiprazole, unspecified antipsychotics and carbamazepine (Tegretol). 2/18 in placebo group were on psychostimulants. Other medications included antidepressants, and risperidone. Previous medications ‐ not reported |
|
| Interventions | Intervention (oxytocin): 4 weeks of intranasal
oxytocin (24 IU), once daily in the morning Comparator (placebo): nasal spray for 4 weeks, once daily in the morning Timing of outcome assessments: baseline and endpoint (4 weeks) |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: QoL (change from baseline) measured using the WHO QoL scale (WHO 1998) |
|
| Notes | Study start date: April 2015 Study end date: December 2016 Funding: this research was supported by the Branco Weiss fellowship of the Society in Science ‐ ETH Zurich and by grants from the Flanders Fund for Scientific Research (FWO projects KAN 1506716N, KAN 1521313N, G040112 & G079017N). Conflicts of interest: S.B. is supported by a fund of the Marguerite‐Marie Delacroix foundation. Trial registry: European Clinical Trial Registry (Eudract 2014‐000586‐45) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomised order |
| Allocation concealment (selection bias) | Unclear risk | Details regarding allocation concealment not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Except for the manager of randomisation, all research staff conducting the trial, participants, and their parents and/or partners were blinded to treatment allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Except for the manager of randomisation, all research staff conducting the trial, participants, and their parents and/or partners were blinded to treatment allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Data were analysed using an ITT format with LOCF to replace missing data |
| Selective reporting (reporting bias) | Low risk | All primary and secondary outcomes listed on clinical registry were reported. |
| Other bias | Low risk | No other obvious sources of bias identified |
Buitelaar 1990.
| Study characteristics | ||
| Methods | 4‐week crossover trial of adrenocorticotrophic hormone (synthetic analog of ACTH 4‐9 (Org 2766)) versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria: "patients who suffered from gross neurological disorders, and internal and endocrinological diseases were excluded". Location/setting: child psychiatry outpatient clinic at Utrecht university hospital, The Netherlands Sample size: 14 Number of withdrawals/ dropouts: none reported Gender: 12 male, 2 female Mean age: 8.5 years IQ: Group 1 (Org 2766/ placebo): 65.3; Group 2 (placebo/Org 2766): 62.3 Concomitant medications: not reported History of previous medications: not reported Baseline ABC‐I scores or other BoC: parent‐rated ABC‐I: 9.4 (6.8) Exclusion criteria included "having gross neurological disorders, and internal and endocrinological diseases; used psychotropic, or had used anticonvulsive or related medications 3 months prior to or during the trial". |
|
| Interventions | Adrenocorticotrophic hormone (4‐9) for 4 weeks: Org
2766 was given at 20 mg/day for 4 weeks, after a
2‐week placebo period Placebo for 4 weeks: equivalent placebo |
|
| Outcomes | Primary outcomes: irritability, measured using the
ABC‐Irritability subscale (Aman 1985) Secondary outcomes: none reported Timing of outcome assessment: baseline, after intervention phase and after placebo phase |
|
| Notes | Study start date: not reported Study end date: not reported Funding source: not reported Conflicts of interest: none reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient details provided |
| Allocation concealment (selection bias) | High risk | Tablets of Org 2766 or identical matching placebo tablets were provided by Organon International B.V. and labelled by the local pharmacy. Assignment to treatment order occurred at random |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "During the trial the behavior of the child was rated once every 2 weeks at home by the parents or caretakers, and at school or day care unit by teacher or nurse". |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | All children completed the trial however Quote: "because of intermittant physical illness one child could not visit his day care unit for several periods of time. Behaviour checklist ratings from teachers were dismissed for this child". |
| Selective reporting (reporting bias) | Low risk | The primary outcome measures were play observations and the ABC (all subscales), which were all measured and reported in full. |
| Other bias | High risk | Tablets of Org 2766 and identical matching placebo tablets were provided by Organon International B.V. |
Campbell 1987.
| Study characteristics | ||
| Methods | Parallel trial of fenfluramine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria: "children who had a known cause of autism" Location/setting: children's psychiatric inpatient service, USA Sample size: 11 (6 fenfluramine, 5 placebo) Number of withdrawals/dropouts: none reported Gender: 9 male, 2 female Mean age: 4.48 (1.16) years IQ: "adaptive developmental quotients ranged from 34‐83” Baseline ABC‐I scores or other BoC: not reported/ applicable Concomitant medications: 0% History of previous medications: not reported |
|
| Interventions | Intervention (fenfluramine) for 8 weeks: fenfluramine
was started at 1.0 mg/kg/day in 2 daily doses. The
maximum dose would not exceed 60 mg/day Comparator (placebo) for 8 weeks: "for placebo, the optimal doses ranged from 1.8‐3.3 mg/kg/day (mean = 2.2); the maximum explored dose was 3.3 mg/kg/day.’ |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: none reported Timing of outcome assessment: baseline, week 4, week 8 |
|
| Notes | Study start date: not reported Study end date: not reported Funding source: supported, in part, by USPHS grant MH‐32212 from the National Institute of Mental Health Conflicts of interest: none reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Details not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition |
| Selective reporting (reporting bias) | High risk | Only selected items from the CGI and CPRS were reported. "None of the items on the CPRS nor their sum produced a statistically significant interaction. The effects of fenfluramine were thus indistinguishable from those of placebo". |
| Other bias | Unclear risk | No group differences published |
Campbell 1993.
| Study characteristics | ||
| Methods | 3‐week parallel trial of naltrexone versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria: “children with identifiable causes of autism (eg. congenital rubella, inborn errors of metabolism, etc.), tardive or withdrawal dyskinesia or those who had other associated movement disorders (eg. Tourette's syndrome, chorea), systemic disease (renal, vascular), history of cardiac disease or nephrosis, seizure disorder or history of seizure disorder, history of hyperthyroidism or hypothyroidism, concurrent administration of any psychoactive medication, hypersensitivity to naltrexone, and opioid dependence”. Location/setting: pediatric inpatient clinic, Bellevue Hospital Centre, USA Sample size: 41 participants (naltrexone 23, placebo 18) Number of withdrawals/dropouts: 4 from naltrexone group "because error was made in labelling the blood samples for naltrexone levels." Gender: 34 boys, 7 girls Mean age: 4.9 years IQ: naltrexone group mean adaptive developmental quotient was 56.8; placebo group mean adaptive developmental quotient was 44.9 Baseline ABC‐I or other BoC: not reported Concomitant medications: 0% History of previous medications: not reported |
|
| Interventions | Intervention (naltrexone) for 3 weeks: naltrexone
maximum 1.0 mg/kg/day Comparator (placebo) for 3 weeks: placebo equivalent |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: none reported Timing of outcome assessment: once/week an hour after drug administration |
|
| Notes | Study start date: not reported Study end date: not reported Funding source: "supported in part by USPHS grants MH‐32212 and MH‐18915 from the NIMH, the Hirschell and Deanna E. Levine Foundation, and the Marion O. and Maximilian E. Hoffman Foundation, Inc Conflicts of interest: none declared Trial registry: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | These ratings were done independently by 2 child psychiatrists (CPRS; CGI) and a research nurse (Nurses' Global Impressions [NGIl and Aggression Rating Scale) who were all blinded to the child's treatment condition. "The teacher, also blinded, rated the children in the classroom." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 45 children completed the study; the data of 4 were not analysed because error was made in labeling the blood samples for naltrexone levels |
| Selective reporting (reporting bias) | Unclear risk | Several scales were used to measure outcomes and all were reported on, however only comparisons between baseline and endpoint were given (as F values and P values) and the aggression scale reported as absent/mild etc |
| Other bias | High risk | Quote: "New York Health and Hospitals Corporation, I.E. du Pont de Nemours & Company for supplying naltrexone (Trexan) and matching placebo tablets and for supporting in part the statistical analyses" |
Carey 2002.
| Study characteristics | ||
| Methods | 48‐week cross‐over trial of secretin versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria: not reported Location/setting: Developmental and Behavioral Pediatrics Division at the Medical College of Ohio, USA Sample size: 8 in total Number of withdrawals/dropouts: not reported Gender: 8 boys Mean age: 5 years IQ: "general developmental level based on parent report on the Child Development Inventory ranged from 16 to 39 months". Baseline ABC‐I or other BoC: ABC‐I secretin 24.5, placebo 15.5 Concurrent drug use: details not provided History of previous medications: details not provided |
|
| Interventions | Intervention (single dose of secretin): single dose
of 2 IU of secretin/kg of body weight Comparator (single dose of placebo): equivalent single dose of placebo |
|
| Outcomes | Primary outcomes: irritability, measured using the
ABC‐I subscale (Aman 1985); AEs Secondary outcomes: none reported Timing of outcome assessment: ABC‐I: prior to infusion and then weekly for 8 weeks |
|
| Notes | Study start date: not reported Study end date: not reported Funding source: not reported Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | All participants were randomised into 2 groups. |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Double‐blinded, however no further details provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Details not provided |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Complete parent and teacher data were obtained for 8 of the total 21 project participants. |
| Selective reporting (reporting bias) | Unclear risk | Protocol was not provided so unclear if all outcomes were reported |
| Other bias | High risk | Participants were recruited from a list of children whose parents contacted the Developmental and Behavioral Pediatrics Division at the Medical College of Ohio to request a trial of secretin for their child. |
Chez 2020.
| Study characteristics | ||
| Methods | 8‐week cross‐over trial of dextromethorphan + quinidine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/ setting: single‐centre study in the USA Sample size: 15 were randomised although 7 in each group received at least 1 dose of intervention or placebo. Reasons for dropouts: 2 participants withdrew after 17 weeks. Both had collateral informants who decided to withdraw from the study due to behavior deterioration. Mean IQ: details not provided Mean age: 21.92 (3.30) years Gender: 3/14 were female Baseline ABC‐I or other BoC scale: dextromethorphan + quinidine 17.42 (9.23); placebo 17.5 (11.74) Concomitant medications: participants were not allowed to use MAOI antidepressants, lamotrigine, felbamate or other NMDA agonists or antagonists. Previous medications: not reported |
|
| Interventions | Intervention: participants received 20 mg
dextromethorphan/10 mg quinidine in tablet form
(Nuedexta) once daily for 7 days and then every 12 h
for the next 7 weeks. Comparator: equivalent placebo for 8 weeks |
|
| Outcomes | Primary outcomes: ABC‐Irritability (Aman 1985) Secondary outcomes: tolerability Timing of outcome assessments: phase 1: baseline and week 8 Phase 2: baseline (after 4 week washout) and week 8 |
|
| Notes | Study start date ‐ details not provided Study end date ‐ details not provided Funding: "This study was supported by an investigator initiated research Grant from Avanir Corporation (Grant No. 947135‐1107629)" Conflicts of interest: "Dr. Michael Chez has been a speaker for pediatric epilepsy issues for Eisai, Lundbeck, UCB, and Sunnovion for the past 2 years. No other authors have any conflicts of interest". |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The parents, neuropsychologists, clinical research coordinators (CRC), and investigators were blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The parents, neuropsychologists, clinical research coordinators (CRC), and investigators were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition and all participants accounted for |
| Selective reporting (reporting bias) | Unclear risk | Without a clinical trial record or protocol, it is difficult to know if all outcomes were reported. |
| Other bias | High risk | Pharma funded ‐ Avanir Corporation |
Chugani 2016.
| Study characteristics | ||
| Methods | 24‐week parallel trial of 2.5 mg buspirone and 5.0 mg buspirone versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: “6 academic medical centres: Wayne State University School of Medicine, Children's Hospital of Michigan; Case Western Reserve University, Rainbow Babies Hospital; University of Texas South Western; Cleveland Clinic Foundation; University of California Davis; an New York University School of Medicine”. USA Sample size: 166 (2.5 mg buspiraone n = 54; 5.0 mg buspirone n = 55; placebo n = 57) Number of withdrawals/ dropouts: "twenty‐four participants (14%) discontinued the study during the treatment phase (adverse event [n = 12, 6 in the placebo group, 3 in the 2.5‐mg group, 3 in the 5.0‐mg group], withdrew consent [n = 3], lost to follow‐up [n = 3], started exclusionary medication [n = 2], clinical decision [n = 2], participant moved [n = 1], time commitments [n = 1])." Gender: 137 male, 29 female Mean age: 4.4 years IQ: not reported Baseline ABC‐I or other BoC scores: Repetitive Behaviour Scale (self‐injurious behaviour), 2.5 mg buspirone 46.9 (3.5), 5.0 mg buspirone 31.5 (3.5), placebo 36.7 (3.5) Concurrent medications: “participants who used a stable dose of melatonin for sleep before entry into the study were allowed to continue use during the study." History of previous medications: not reported |
|
| Interventions | Buspirone 2.5 mg/day for 24 weeks: liquid, 2.5 mg in
1 mL, once/day in the evening for the first week of
administration and thereafter twice a day 12 h apart
for the entire study Buspirone 5.0 mg/day for 24 weeks: buspirone liquid, 5.0 mg in 1 mL, once/day in the evening for the first week of administration and thereafter twice a day 12 h apart for the entire study Placebo for 24 weeks: “placebo liquid, in 1 mL, once/day in the evening for the first week of administration and thereafter twice a day 12 h apart for the entire study” |
|
| Outcomes | Primary outcomes: AEs; self‐injurious behaviour,
measured with the Repetitive Behaviour Scale (Bodfish
2000) Secondary outcomes: tolerability Timing of outcome assessments: AEs were assessed twice monthly. Self‐injurious behaviour was measured at baseline, 24 weeks and 48 weeks. |
|
| Notes | Study start date: 14 July 2009 Study end date: 8 January 2013 Source of funding: supported by the National Institute of Neurological Disorders and Stroke Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Exact method not mentioned. Quote: "Within each site, participants were randomised in blocks for age groups (2 to <4 years, and 4 to <6 years) to treatment groups of 2.5mg, 5mg, or placebo". |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "all site personnel were blinded to treatment during both phases of treatment. A medical monitor at a different site not involved in the enrollment of participants evaluated the adverse events" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Details not provided although an external person evaluated the adverse effects |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Outcome data could not be obtained for 11 of 24 participants who discontinued early because families declined to return for the final visit testing or were lost to follow‐up, however an ITT analysis was used. |
| Selective reporting (reporting bias) | Low risk | The main outcome reported on clinicaltrials.gov was "To evaluate the effects of twice‐daily oral buspirone on core features of autism in autistic children 2‐6 years measuring the change from baseline in ADOS (Autism Diagnostic Observation Schedule) Composite Total scores compared to placebo at 6 months". the ADOS total scores were reported for each intervention group. |
| Other bias | Unclear risk | We contacted study authors for details on Repetitive Behaviour Scale subscale 4 results but no reply |
Dai 2021.
| Study characteristics | ||
| Methods | ||
| Participants | Inclusion criteria: "The patients, aged from 3 to 6
years old, were given the diagnosis of ASD according
to the Diagnostic and Statistical Manual of Mental
Disorders, Fifth Edition (DSM‐5) , by a team of
autism experts; Scores for Children Autism Rating
Scale (CARS) were more than 30; Signed Informed
Consents were provided by parents." Exclusion criteria: "Liver and kidney dysfunction; With a history of allergy to sulfa drugs; abnormal ECG; chromosomal abnormality; suffering from nervous system diseases (such as epilepsy, schizophrenia, and so on); using the melatonin treatment for sleep disorders or withdrawal less than three weeks." Location/setting: Shanghai, China Sample size: bumetanide 59; placebo 60 (119 in total) Reasons for withdrawals/dropouts: bumetanide 1 dropped out due to non‐adherence; placebo 2 dropped out (1 due to hand and foot disease, the other "met the criteria for withdrawal") Gender: bumetanide group 51 male, 8 female; placebo group 49 male, 11 female Mean age: bumetanide group 4.03 years; placebo 4.22 years IQ: details not provided except that 75% in the intervention and 65% placebo groups had ASD plus intellectual or developmental disability Baseline ABC‐I or other BoC scale: not an outcome Concomitant medications: details not provided Previous medications: details not provided |
|
| Interventions | Intervention (bumetanide) for 3 months: bumetanide
tablets, oral intake, 0.5 mg, twice daily,
respectively at 8 am and 4 pm Comparator (placebo) for 3 months: "placebo tablets, oral intake, 0.5 mg, twice daily, respectively at 8 am and 4 pm" |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: self‐injurious behaviour, change from baseline; measured using the Repetitive Behaviour Scale (Bodfish 2000) Timing of outcome assessments: not clear |
|
| Notes | Study start date: May 2017 Study end date: July 2019 Funding: various grants Conflicts of interest: details not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Participants were randomly assigned in a 1:1 ratio to receive 0.5 mg oral bumetanide or placebo twice daily for 3 months by using a block randomization scheme." "The generation of random allocation sequence and the preparation of trial medication were done by investigators in an external consultancy who do not participate in other aspects of the study." |
| Allocation concealment (selection bias) | Unclear risk | "The study medication (bumetanide or placebo tablet) was provided in sequentially numbered envelopes" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "The study medication (bumetanide or placebo tablet) was provided in sequentially numbered envelopes" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Stated that "Patients and their caregivers, investigators, experienced psychiatrists, and data analysts remained masked to the treatment allocation until the study database was locked" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 1 withdrew because "they met the criteria for withdrawal" |
| Selective reporting (reporting bias) | Unclear risk | 2 of the outcomes on the trial registry have not been reported. |
| Other bias | High risk | The baseline Repetitive Behaviour Scale (self‐injury) scores were double that in the placebo group. |
Danfors 2005.
| Study characteristics | ||
| Methods | 6‐month cross‐over trial of tetrahydrobiopterin versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: outpatients from 4 different departments of child and adolescent psychiatry in Sweden Sample size: 12 in total Number of withdrawals/dropouts: "all 12 children completed the tetrahydrobiopterin treatment study". Gender: 11 male, 1 female Mean age: 5.3 years IQ: 32‐93 Concurrent medications: participants could not have taken pharmacological treatments for ASD prior to or during the study. History of previous medications: see above |
|
| Interventions | Intervention (tetrahydrobiopterin): individual doses
of tetrahydrobiopterin at 3 mg/kg of body weight
were prescribed in capsule form (in single‐dose
pack) to be taken twice daily. Comparator (placebo): twice‐daily capsules |
|
| Outcomes | Primary outcomes: adverse events Secondary outcomes: none reported |
|
| Notes | Study start date: details not provided Study end date: details not provided Funding: "This research was supported by grants from the Subfemtomole Biorecognition Project, ICORP, Japan Science and Technology Agency (JST), The Swedish Research Council (grant 8645) the Sven Jerring Fund, Holmia insurance company, the Gillbergska Foundation, the Samaritan Foundation, the Linnea and Josef Carlssons Foundation, and the child‐neurology fund of Uppsala University" Conflicts of interest: none declared Trial registry: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The local hospital pharmacy produced the capsules and performed the randomisation of the patients |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind; the assessors remained blinded throughout the study. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blind; the assessors remained blinded throughout the study. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | AEs were not provided for both groups despite being recorded every 3 months. |
| Selective reporting (reporting bias) | Unclear risk | Difficult to determine without a protocol |
| Other bias | Low risk | None identified |
Danforth 2018.
| Study characteristics | ||
| Methods | 4‐week parallel trial of MDMA + psychotherapy versus placebo + psychotherapy | |
| Participants | Inclusion criteria:
Exclusion criteria: psychiatric exclusion criteria included family history in first‐degree relatives of schizophrenia or bipolar I disorder, or participant diagnoses of active or past psychotic disorder, borderline personality disorder, dissociative identity disorder, eating disorder or active suicidal ideation. Setting: Los Angeles Biomedical Research Institute in Torrance, CA, USA Sample size: placebo (n = 4); MDMA (n = 8) Reason for dropouts/withdrawals: from MDMA group, 1 treatment discontinuation due to not meeting inclusion criteria Current or previous medications: previous medications MDMA: antidepressants (5), anxiolytics (1), antipsychotics (1), stimulant (3), other (3). Placebo: antidepressants (2), antipsychotics (1), stimulant (1) Mean age: placebo mean age 28.3 years, MDMA mean age 32.8 years Mean IQ: details not provided Gender: MDMA 25% female, placebo all male Baseline ABC‐Irritability scores: not an outcome Concomitant medications ‐ not reported Previous medications: previous medications: MDMA antidepressants (5), anxiolytics (1), antipsychotics (1), stimulant (3), other (3). Placebo antidepressants (2), antipsychotics (1), stimulant (1) |
|
| Interventions | Intervention (MDMA + psychotherapy): "after three 60‐
to 90‐min non‐drug preparatory psychotherapy
sessions, participants received two blinded
experimental sessions with MDMA or placebo, spaced
approximately 1 month apart. Following each
experimental session, three 60‐ to 90‐min non‐drug
integrative psychotherapy sessions occurred over 3
weeks" Comparator (placebo + psychotherapy): "after three 60‐ to 90‐min non‐drug preparatory psychotherapy sessions, participants received two blinded experimental sessions with MDMA or placebo, spaced approximately 1 month apart. Following each experimental session, three 60‐ to 90‐min non‐drug integrative psychotherapy sessions occurred over 3 weeks" |
|
| Outcomes | Primary outcomes: adverse events Secondary outcomes: tolerability Timing of outcome assessments: baseline, post‐intervention, and 6 months |
|
| Notes | Study start date: February 2014 Study end date: April 2017 Funding: "The trial was sponsored and funded by the Multidisciplinary Association for Psychedelic Studies (MAPS), a 501(c)(3) nonprofit organization. MAPS Public Benefit Corporation (MPBC), wholly owned by MAPS, was the trial organizer." Conflicts of interest: in receipt of various grants and some authors were eployed by the funder of the study. Other: clinical trial registry ‐ NCT02008396 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Participants, therapists, and IR [Independent Rater] were blinded to drug assignment" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | An independent rater (IR) administered the Leibowitz Social Anxiety Scale (LSAS) at baseline, 1 day, 2 weeks, and 4 weeks after each experimental session and readministered it before the blind was broken at 6 months. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | ITT analysis, only one dropout |
| Selective reporting (reporting bias) | Low risk | Same primary outcomes on clinical trial registration |
| Other bias | High risk | The trial was sponsored and funded by the Multidisciplinary Association for Psychedelic Studies. |
Dean 2019.
| Study characteristics | ||
| Methods | 24‐week trial of N‐acetyl cysteine (NAC) versus placebo | |
| Participants | Inclusion criteria: "diagnosis of Autistic Disorder
according to DSM‐4‐TR (Diagnostic and Statistical
Manual of Mental Disorders, Fourth Edition, Text
Revision) criteria (American Psychiatric
Association, 2000) and were aged between 3 and 9
years, inclusive". Exclusion criteria: "had a known or suspected clinically relevant systemic medical disorder or known genetic or metabolic cause of developmental delay, such as fragile X or Rett syndrome; had a prior sensitivity or allergy to NAC were considered likely to be unable to comply with the treatment protocol, e.g., having a highly restricted diet leading to refusal to take NAC; had parents/guardians who were non‐fluent in English; had a history of asthma or epilepsy, as these are equivocally influenced by NAC, or were already receiving any treatment containing NAC, glutathione or their precursors". Location/setting: Australia Sample size: ITT sample was 98: NAC 48; placebo 50 Reason for dropouts/withdrawals:
Mean age: 6.4 years Mean IQ: 73 Gender: 79 male, 19 female Baseline ABC‐Irritability scores: Repetitive Behaviour Scale (self‐injury) 2.2 (2.9) in intervention group, 1.7 (2.6) in placebo group Current or previous medications: "children undergoing any pharmacological treatment for autistic disorder were allowed to continue with that treatment, as usual". Not specified per group but outlined 26.5% on a psychotropic medication (most commonly; melatonin 12/2% and risperidone 5.1%). Other medications included health supplements (most commonly fish oil 19.4%), anti‐allergy medication (total use 5.1%), skin medication (total use 4.1%) and 9.1% of children were on a range of other medications (e.g. paracetamol). |
|
| Interventions | Intervention: fixed dose 500 mg once daily of
N‐acetyl cysteine Comparator: equivalent placebo |
|
| Outcomes | Primary outcomes: self‐injurious behaviour, measured
with the Repetitive Behaviour Scale (Bodfish 2000);
AEs Secondary outcomes: tolerability Timing of outcome assessments: baseline, week 4, 12 and 24 |
|
| Notes | Study start date: details not provided Study end date: details not provided Funding: "This work was supported by the Simons Foundation Autism Research Initiative (SFARI) [Grant 201473]. A pilot award and scholarship support for Kristi‐Ann Villagonzalo was obtained from Australian Rotary Health. Michael Berk is supported by an NHMRC Senior Principal Research Fellowship (1059660)". Conflicts of interest: "No potential conflict of interest was reported by the authors". Trial registry: ACTRN12610000635066 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were randomised sequentially into either the NAC or placebo groups using a computer program designed for clinical trial randomisation (randomization.com)". "An independent researcher, who had no contact with any participants, coordinated the computer‐generated randomisation codes" |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants, their parents/guardians, trial staff and the statistician were blind to treatment arm allocation for the duration of the study. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants, their parents/guardians, trial staff and the statistician were blind to treatment arm allocation for the duration of the study |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Large amount of attrition by 6 months (> 25% in both groups). Not clear if AEs is for all participants or just those at 6 months' follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Outcomes have not been listed on the clinical trials registry and so it is difficult to know if all outcomes have been reported. |
| Other bias | Unclear risk | The study medication was gifted by BioMedica |
DeVane 2019.
| Study characteristics | ||
| Methods | 10‐week trial of aripiprazole versus risperidone | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: 3 academic medical centres and a single private paediatric practice in the USA Mean age: range 6‐15.1 years in aripiprazole group; 6.3‐17.5 years in risperidone group IQ: details not provided Gender: 19% and 23% of aripiprazole and risperidone groups were female. Current or previous medications: aripiprazole, 4/31 had previously taken the study drug (but not within the last 3 years), risperidone, 1/31 had previously taken the study drug (but not within the last 3 years). Baseline ABC‐Irritability scores: > 18 at baseline Sample size: 61 (31 aripiprazole; 30 risperidone) Number analysed: aripiprazole 31, risperidone 30 Reason for dropouts: aripiprazole, 4 discontinued all due to AEs, risperidone, 6 discontinued (3 due to missed visits, 2 AEs, and 1 withdrew on physician's advice) Timing of outcome assessments: "safety, physical, and psychological assessment were recorded at clinic visits that took place weekly or every 2 weeks". |
|
| Interventions | Intervention (risperidone): "children weighing 20‐45
kg will receive an initial dose of 0.5 mg daily that
will be increased to twice daily on day 4 (morning
and bedtime). The dosage will be gradually increased
in 0.5 mg increments to a maximum dose of 2.5 mg per
day (1.0 mg in the morning and 1.5 mg at bedtime) by
the fourth treatment week. A slightly accelerated
dosage will be allowed for children who weigh more
than 45 kg for a maximum dosage of 3.5 mg /day" Comparator (aripiprazole): starting dosage of 2.0 mg/day. "The dosage will be allowed to increase to 5.0 mg/day on day 4 and can be increased thereafter to a maximum dosage of 15 mg/day. The dosage will only be increased in 5.0 mg intervals. No dosage adjustments will be allowed for either drug after 4 weeks". |
|
| Outcomes | Primary outcomes: ABC‐Irritability (Aman 1985);
AEs Secondary outcomes: tolerability |
|
| Notes | Study start date: September 2011 Study end date: June 2015 Funding: "The study was funded by Grant No. R01HD62550 from the National Institute of Child Health and Human Development, National Institutes of Health". Conflicts of interest: "The authors have declared no conflicts of interest for this article". Trial registry: NCT01333072 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details given on how random sequence was generated |
| Allocation concealment (selection bias) | Unclear risk | No details given on allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | All research personnel blinded except for RA who prepared meds and study pharmacist who checked meds |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Physicians (who conducted physical neurological evaluation) and caregiver (who completed questionnaires) were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants were accounted for and included in the analysis. |
| Selective reporting (reporting bias) | High risk | Protocol available at ClinicalTrials.gov Identifier: NCT01333072 Primary outcome was "Changes in the Irritability Subscale of the Larger ABC (Abberent Behavior Checklist) That Occur From Baseline to 10 Weeks" but they've tested for P values at each week as there was no statistically significant difference at 10 weeks. This is reported misleadingly in the abstract Quote: "Improvement was greatest in the risperidone group at every assessment period" |
| Other bias | Low risk | None identified |
Dollfus 1992.
| Study characteristics | ||
| Methods | Cross‐over trial of amisulpride versus bromocriptine | |
| Participants | Inclusion criteria: "children 4‐13 years inclusive
who meet the DSM‐III diagnostic criteria for
infantile autism. Severity of autism according to
the Childhood Autism Rating Scale was at least 36
indicating 'severely autistic'." Exclusion criteria: details not provided Location/setting: inpatients and outpatients at Salpetriere hospital, Paris Sample size: 9 in total (cross‐over study). Amisulpride first group (5); bromocriptine first group (4) Number of withdrawals/dropouts: none in first phase of cross‐over. Only one dropped out of the study during the second treatment phase (amisulpride) on week 12 for reasons unrelated to the treatment Gender: 4 girls, 5 boys Mean age: 6.9 years IQ: "the severity of the autistic syndrome did not allow IQ tests to be given. It may be presumed, therefore, that the children are likely to have been severely mentally retarded". Baseline ABC‐I or other BoC: not an outcome Concurrent medications: "two of the nine children had received neuroleptic treatment at the time of selection. Therefore, a 45‐day neuroleptic washout period was required". No neuroleptic or other psychotropic drugs were allowed during the trial, except benzodiazepine, niaprazine, or hydroxyzine for severe sleep disorders, which 3 participants took concurrently during the trial (1 participant niaprazine; 1 participant niaprazine and flunitrazepam‐hydroxyzine; 1 participant hydroxyzine) History of previous medications: not reported |
|
| Interventions | Intervention (amisulpride): 1.5 mg/kg/day for 4
weeks Comparator (bromocriptine): 0.15‐0.20 mg/kg/day for 4 weeks |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: none reported Timing of outcome assessment: baseline and then every 2 weeks for 14 weeks |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: research protocol subsidised by MUSTELA Foundation (under the aegis of the Foundation of France) Conflicts of interest: none declared Trial registry: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Double‐blinding was used although specific details not provided |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The raters were blind to the treatment" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Only 9 participants were involved in the trial, with only 1 person withdrawing from the trial during the second phase of the crossover trial. A LOCF was used for the analysis of this participant. |
| Selective reporting (reporting bias) | Unclear risk | The BSE was reported fully at baseline and endpoint for both phases of the cross‐over, however the BSE is not relevant to the outcomes of interest. Non‐specific BSE measures include items on aggressiveness which not reported specifically, rather included as part of total score. |
| Other bias | Unclear risk | No other sources identified but difficult to know without a protocol or trial registry |
Eslamzadeh 2018.
| Study characteristics | ||
| Methods | 8‐week parallel trial of atomoxetine + risperidone versus placebo + risperidone | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: outpatient clinic of Ibnesina hospital, Iran Mean IQ: details not provided Mean age: 8.0 years Gender: 6 female, 34 male Sample size: 40‐20 each group Number analysed: 20 in each group completed the trial Reasons for dropouts: 3 from atomoxetine group discontinued due to withdrawing consent (1) and AEs (2) and 1 from placebo group did not start the trial. Baseline ABC‐I or other BoC scale: not reported Timing of outcome assessments: "patients were evaluated at baseline, 4 weeks and 8 weeks after the administration of the drug". Concomitant medications: apart from risperidone, participants could not be taking any other psychotropic drugs. Previous medications ‐ not reported |
|
| Interventions | Intervention (atomoxetine + risperidone): atomoxetine
was given at 0.5 mg/kg/day at the start and
increasing every 5 days up to a maximum of 1.2
mg/kg/day for 8 weeks. All participants were
currently taking risperidone ranging from 1‐4
mg/day Comparator (placebo + risperidone): placebo plus usual intake of risperidone for 8 weeks |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: tolerability |
|
| Notes | Study start date: August 2015 Study end date: September 2016 Funding: "This work was extracted from a residency thesis in the Mashhad University of Science. There was no organizational financial support". Conflicts of interest: "There are no conflicts of interest". Other: trial registry IRCT2016022826802N1 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "double blind". No further details provided |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | The trial registry stated that investigators were not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The numbers that discontinued in the treatment group do not match what was analysed (i.e they report 3 dropouts but 4 not included in the analysis). |
| Selective reporting (reporting bias) | Low risk | The outcomes listed on the clinical registry were reported |
| Other bias | High risk |
|
Fankhauser 1992.
| Study characteristics | ||
| Methods | Cross‐over trial of clonidine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: USA Sample size: 9 in total (cross‐over) Number of withdrawals/dropouts: 2 from clonidine group Gender: all male Mean age: 12.9 years IQ: not reported Baseline ABC‐I or other BoC: baseline RFRLRS (affectual responses: 1.02) Concurrent medications: 0% History of previous medications: 0% |
|
| Interventions | Intervention (clonidine): weekly patch delivering
approximately 0.005 mg/kg /day for 4 weeks Comparator (placebo): transdermal placebo patch for 4 weeks |
|
| Outcomes | Primary outcomes: irritability, measured using the
RFRLRS (Freeman
1986) Secondary outcomes: tolerability Timing of outcome assessment: baseline, 2 weeks, 4 weeks |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: Boehringer Ingelheim Pharmaceuticals supplied the patches Conflicts of interest: none declared Trial registry: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 2 of 9 participants were lost to follow‐up, 1 because
of irritability and sedation while on clonidine LTFU: 2 unexplained |
| Selective reporting (reporting bias) | High risk | AEs were not reported. |
| Other bias | Unclear risk | This was highly divergent sample (5‐33 years) with low sample numbers (9) |
Findling 2014.
| Study characteristics | ||
| Methods | Parallel trial of aripiprazole versus placebo | |
| Participants | Inclusion criteria
Exclusion criteria
Location/setting: child and adolescent psychiatry, Johns Hopkins Hospital, USA Sample size: 85 (41 aripiprazole, 44 placebo) Number of withdrawals/dropouts: 19 dropouts in aripiprazole group due to: withdrawal (5), LTFU (1), lack of efficacy (13); 25 dropouts in placebo group due to: adverse event (1), lack of efficacy (23), noncompliance (1) Mean age: aripiprazole 10.1 years, placebo 10.8 years IQ: mental age of at least 24 months Gender: aripiprazole male 30/41; placebo 38/44 male Baseline ABC‐I or other BoC: not reported (only change from baseline) Concurrent medications: "allowed antipsychotics apart from aripiprazole include antidepressants, benzodiazepines (for procedures only), stimulants, alpha‐agonists, mood stabilizers, and atomoxetine. Diphenhydramine for sleep or serious behaviur problems, nonbenzodiazepine sleep aids for insomnia, and melotonin for insomnai were permitted". History of previous medications: not reported |
|
| Interventions | Intervention (aripiprazole): "Phase 1 (single
blind): Participants received an initial dose of
aripiprazole 2 mg daily, titered up to 5, 10, or 15
mg once daily to optimize clinical benefit, for a
maximum of 26 weeks. Phase 2 (randomised):
Aripiprazole was continued at the (fixed) dose
prescribed at the end of Phase 1, once daily for 16
weeks. The dose (within the range of 2‐15 mg/day)
could have been adjusted based on efficacy and
tolerability". Comparator (placebo): equivalent placebo for 16 weeks |
|
| Outcomes | Primary outcomes: irritability (change from
baseline), measured using the ABC‐Irritability
subscale (Aman
1985); AEs Secondary outcomes: QoL, measured with the PedsQL Timing of outcome assessment: ABC‐I and AEs were assessed every 2 weeks and PedsQL every 4 weeks |
|
| Notes | Study start date: March 2011 Study end date: June 2012 Source of funding: Bristol‐Myers Squibb Conflicts of interest: "Dr Findling receives or has received research support from, acted as a consultant to, received royalties from, and/or served on a speaker’s bureau for Abbott, Addrenex, Alexza, American Psychiatric Press, AstraZeneca, Biovail, Bracket, Bristol‐Myers Squibb, Dainippon Sumitomo Pharma, Forest, GlaxoSmithKline, Guilford Press, Johns Hopkins University Press, Johnson & Johnson, KemPharm, Lilly, Lundbeck, Merck, National Institutes of Health, Neuropharm, Novartis, Noven, Organon, Otsuka, Pfizer, Physicians Postgraduate Press, Rhodes Pharmaceuticals, Roche, Sage, Sanofi‐Aventis, Schering‐Plough, Seaside Therapeutics, Sepracore, Shionogi, Shire, Solvay, Stanley Medical Research Institute, Sunovion, Supernus, Transcept, Validus, WebMD and Wyeth". |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided about sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Details not provided about allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided about blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Details not provided about blinding |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Paper mentions the PedQoL and Caregiver Strain
Questionnaire that were administered every 4 weeks
in the double‐blind phase. Neither outcome was
reported in the paper. LTFU: aripiprazole 19/39 did not complete the trial (withdrawal (5); LTFU (1); Lack of efficacy (13)) Placebo: 25/43 did not complete the trial (adverse event (1), poor/noncompliance (1), lack of efficacy (23)) |
| Selective reporting (reporting bias) | High risk | Quote: "Safety assessments were made every 2 weeks in the double blind phase". Relatively few AEs reported for double‐blind phase suggesting reporting bias. |
| Other bias | High risk | There is an agreement between Principal Investigators and the Sponsor (or its agents) that restricts the PI's rights to discuss or publish trial results after the trial is completed". |
Ghaleiha 2013a.
| Study characteristics | ||
| Methods | Parallel trial of memantine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: speciality clinic for autism in the children’s outpatient clinic, Iran Sample size: 40 (20 memantine/risperidone; 20 placebo/risperidone) Number of withdrawals/ dropouts: none reported Gender: memantine 11 boys, 9 girls; placebo 12 boys, 8 girls Mean age: memantine 7.42 years; placebo 7.97 years IQ: not reported Baseline ABC‐I or other BoC: ABC‐I memantine 18.25, placebo 17.65 Concurrent medications: 0% (participants had to be drug‐treatment‐free in 6 months prior to trial) History of previous medications: not reported |
|
| Interventions | Intervention (memantine + risperidone) for 10 weeks:
participants started on 5 mg (tablets) once daily,
which was titrated up or down in 5 mg increments
each week up to a maximum of 15 mg/day for children
10‐40 kg and 20 mg/day for children > 40 kg.
Risperidone was titrated up to 2 mg/day (starting at
0.5 mg with dose increases of 0.5 mg increments
weekly for the first 3 weeks) for children weighing
10‐40 kg, titrated up to 3 mg/day for children >
40 kg Comparator (placebo + risperidone) for 10 weeks: placebo was identical to memantine in appearance, shape, size, colour and taste. Risperidone was titrated up to 2 mg/day (starting at 0.5 mg with dose increases of 0.5 mg increments weekly for the first 3 weeks) for children weighing 10‐40 kg, titrated up to 3 mg/day for children > 40 kg |
|
| Outcomes | Primary outcomes: irritability, measured using the
ABC‐Irritability subscale (Aman 1985);
AEs Secondary outcomes: none reported Timing of outcome assessments: ABC‐I was rated at baseline, weeks 2, 4, 6, 8 and 10; AEs were recorded every 2 weeks |
|
| Notes | Study start date: January 2009 Study end date: January 2011 Source of funding: Tehran University of Medical Sciences Conflicts of interest: none declared Trial registry ‐ IRCT1138901151556N10 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "patients were randomised to receive memantine or placebo in a 1:1 ratio using a computer‐generated code" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "the assignments were kept in sealed, opaque envelopes until data analysis." But it is not clear how they were allocated. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Throughout the study the person who administered the medications, the rater and the patients were blind to assignments. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Throughout the study, the person who administered the medications, the rater and the patients were blind to assignments. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There appeared to be no LTFU |
| Selective reporting (reporting bias) | Low risk | All data appear to have been reported |
| Other bias | High risk |
|
Ghaleiha 2013b.
| Study characteristics | ||
| Methods | Parallel trial of riluzole + risperidone versus placebo + risperidone | |
| Participants | Inclusion criteria: "male and female outpatients aged
5‐12 years with a diagnosis of autistic disorder
based on the DSM‐4‐TR criteria and a score of >12
on the ABC‐C irritability subscale who had
discontinue other medication because of lack of
efficacy". Participants also had to be drug‐free for
at least 6 weeks prior to study entry". Exclusion criteria:
Location/ Setting: autism speciality clinic in the children’s outpatient clinic of Roozbeh Hospital, Iran Sample size: riluzole + risperidone 25; placebo + risperidone 24 Number of withdrawals/dropouts: riluzole + risperidone: 3 restlessness, 2 no improvement. Placebo + risperidone: 1 restlessness; 3 withdrew consent Gender: 17/20 male riluzole/risperidone group; 16/20 male placebo/risperidone group Mean age: riluzole + risperidone 8.4 years; placebo + risperidone 7.6 years IQ: not reported Baseline ABC‐I or other BoC: ABC‐I of ≥ 12 Concurrent medications: 0% on psychotropic medications History of previous medications: 16/20 and 18/20 (riluzole and placebo group respectively) risperidone; Ritalin (methylphenidate) 6 and 7/20; biperiden 5 and 3/20; haloperidol 1 and 2/20; clonidine 2 and 3/20; fluoxetine 2 in both groups; levocarnitine 2 in riluzole group; valproic acid 1 in both groups; lamatrogine 1 and 2/20; lithium 1 in riluzole group; perphanazine 1 in placebo group; ginseng 1 in riluzole group; desmopressin 1 in riluzole group; pentoxifylline 1 in placebo group |
|
| Interventions | Intervention (riluzole + risperidone) for 10 weeks:
riluzole (Rilutek; Sanofi‐Aventis) was titrated from
25 mg/day to 50 mg/day for children weighing between
10 kg and 40 kg or 100 mg/day for children weighing
> 40 kg. Risperidone (Risperdal; Janssen
Pharmaceuticals) was titrated from 0.5 mg/day up to
2 mg/day for children weighing up to 40 kg or 3
mg/day for children weighing > 40 kg. Comparator (placebo + risperidone) for 10 weeks: risperidone (Risperdal; Janssen Pharmaceuticals) was titrated from 0.5 mg/day up to 2 mg/day for children weighing up to 40 kg or 3 mg/day for children weighing more than 40 kg. |
|
| Outcomes | Primary outcomes: irritability, measured using the
ABC‐Irritability subscale (Aman 1985);
AEs Secondary outcomes: tolerability Timing of outcome assessments: baseline, week 5, week 10 |
|
| Notes | Study start date: August 2011 Study end date: September 2012 Source of funding: supported by a grant from Tehran University of Medical Sciences to Prof Shahin Akhonzadeh (grant number 14037) Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A computer‐generated code was used in order to randomly assign the patients to the riluzole or placebo group in a 1:1 ratio" |
| Allocation concealment (selection bias) | Low risk | Quote: "The assignments were kept in sequentially numbered, sealed, opaque envelopes until the end of the study." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "The patients, their parents, and the physicians who referred them were all blind to the treatment assignments, as were the rater and the person who administered the medications. Separate persons were responsible for random allocation and rating of the patients" Quote: "The placebo was identical in appearance (shape, size, color, and taste) to riluzole and was dispensed by the investigational drug pharmacist." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: 'The patients, their parents, and the physicians who referred them were all blind to the treatment assignments, as were the rater and the person who administered the medications. Separate persons were responsible for random allocation and rating of the patients'. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | All 40 participants who completed at least one post‐baseline visit were included in the analysis. 9 of 49 randomised participants did not attend a post‐baseline visit, 5 in the riluzole group and 4 in the placebo group. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported (ICRT checked) |
| Other bias | High risk |
|
Ghaleiha 2014.
| Study characteristics | ||
| Methods | Parallel trial of galantamine + risperidone versus placebo + risperidone | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: psychiatric academic hospital affiliated with Tehran University of Medical Sciences Sample size: galantamine 25; placebo 23 Number of withdrawals/dropouts: galantamine (5) because of withdrawn consent; placebo (3) because of withdrawn consent Gender: galantamine 17/20 male; placebo 18/20 male Mean age: galantamine 6.85 years; placebo 5.9 years IQ: galantamine 6 had mild intellectual disability, 2 had moderate intellectual disability; placebo 5 had mild intellectual disability, 4 had moderate intellectual disability Baseline ABC‐I or other BoC: ABC‐I baseline of ≥ 12 Concurrent medications: none permitted History of previous medications: galantamine 1 had taken valproic acid; placebo 1 sodium valproate, 1 carbamazepine, 1 vigabatrin, 1 phenobarbital |
|
| Interventions | Intervention (galantamine + risperidone) for 10
weeks: the initial dosage of galantamine was 2
mg/day and increased weekly in increments of 2 mg if
tolerated and clinically indicated. The maximum dose
was 12 mg/day for children weighing < 20 kg, 16
mg/day for children weighing 20–30 kg, 20 mg/day for
children weighting 30–40 kg and 24 mg/day for
children weighing ≥ 40 kg. Risperidone: titrated up
to 1 mg/day for children weighing < 20 kg, and 2
mg/day for children weighing ≥ 20 kg Comparator (placebo + risperidone) for 10 weeks: risperidone was titrated up to 1 mg/day for children weighing < 20 kg, and 2 mg/day for children weighing ≥ 20 kg. The equivalent placebo was also administered. |
|
| Outcomes | Primary outcomes:
Secondary outcomes: tolerability Timing of outcome assessments: baseline, week 5, week 10 |
|
| Notes | Study start date: April 2012 Study end date: January 2013 Source of funding: Tehran University of Medical Sciences (grant number 13216 to SA) Conflicts of interest: none declared Trial registry: IRCT201204081556N40 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomization codes were generated by excel software by an independent person who was not involved elsewhere in the research project" |
| Allocation concealment (selection bias) | Low risk | Quote: "assignments were kept in sequentially‐numbered, sealed, opaque envelopes and were opened sequentially, only after the participant details were written on the envelope" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "the patients, their parents and the physicians who referred them were all blind to the treatment assignments, so were the research investigators and the person who administered the medications. Placebo capsules and their ingredients were made to be identical to galantamine capsules" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The research investigators were blinded to the treatment assignments. Separate people were responsible for rating and random allocation of the patients. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data analysed for 20 participants completing in each group |
| Selective reporting (reporting bias) | Low risk | All ABC domains reported |
| Other bias | High risk |
|
Ghaleiha 2015.
| Study characteristics | ||
| Methods | Parallel trial of pioglitazone + risperidone versus placebo + risperidone | |
| Participants | Inclusion criteria:
Location/setting: autism speciality clinic of the children's outpatient clinic of Roozbeh Psychiatric Hospital, Tehran University of Medical Sciences, Iran Sample size: 22 in each group. Number of withdrawals/dropouts: 2 in each group withdrew consent Gender: treatment 15/20 male; placebo 17/20 male Mean age: treatment group 6.95 years; placebo 6.2 years IQ: not reported Baseline ABC‐I or other BoC: ABC‐I 18.25; placebo 19.00 Concurrent medications: not reported History of previous medications: treatment group: risperidone 15/20 participants, Ritalin (methylphenidate) 4, valproic acid 2, lamotrigine 1. Placebo: risperidone 16/20, Ritalin (methylphenidate) 6, valproic acid 2, lamotrigine 2 Exclusion criteria: any active medical condition, diagnosis of DSM‐IV axis I or II disorder, use of any psychotropics in previous 6 weeks, history of hepatic disease or seizure; having insulin‐dependent diabetes, liver disease, or congestive heart failure Number randomised: pioglitazone 22; placebo 22 Number analysed: pioglitazone 20; placebo 20 |
|
| Interventions | Intervention (pioglitazone + risperidone) for 10
weeks: pioglitazone (Actos, Takeda/Eli Lilly) 30
mg/day (15 mg twice/day) fixed dose.
Risperidone(Risperdal; Janssen Pharmaceuticals,
Belgium) initial dose 0.5 mg/day increased by 0.5 mg
every week to a maximum of 1 mg/day for participants
weighing < 20 kg and 2 mg/day for those who were
≥ 20 kg Comparator (placebo + risperidone) for 10 weeks: placebo tablets with identical appearance. Risperidone (Risperdal; Janssen Pharmaceuticals, Belgium) initial dose 0.5 mg/day increased by 0.5 mg every week to a maximum of 1 mg/day for participants weighing < 20 kg and 2 mg/day for those who were ≥ 20 kg |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: baseline, week 5, week 10 |
|
| Notes | Study start date: March 2012 Study end date: February 2014 Source of funding: "This study was supported by a grant from Tehran University ofMedical Sciences to Prof Shahin Akhondzadeh (grant number16043). The funding organization had no role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript and the decision to submit the paper for publication." Conflicts of interest: none declared Trial registry: IRCT201204081556N40 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation codes were generated by Microsoft Office excel software and each participant was assigned to one specific code" |
| Allocation concealment (selection bias) | Low risk | Quote: "Assignments were kept in confidential sealed opaque envelopes and were disclosed after the end of the study for statistical analysis" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The participants, parents and referring physicians were totally blinded to the assignments. Additionally, responsible individuals for administration of the medications, rating and statistical analysis were also blinded to the assignments. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The participants, parents and referring physicians were totally blinded to the assignments. Additionally, responsible individuals for administration of the medications, rating and statistical analysis were also blinded to the assignments. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Two of 22 were LTFU in both groups |
| Selective reporting (reporting bias) | Low risk | All data were reported. |
| Other bias | High risk |
|
Ghaleiha 2016.
| Study characteristics | ||
| Methods | 10‐week parallel study of minocycline + risperidone versus placebo + risperidone | |
| Participants | Inclusion criteria:
Exclusion criteria: "Children with concomitant psychotic disorders, severe intellectual disability that made the diagnosis inconclusive (based on clinical judgment and reviewing prior neurocognitive testing and records), other DSM‐IV axis I or II disorders, seizure disorder, a history of alcohol or drug abuse, tardive dyskinesia, administration of antipsychotic medications within the past 6 months, as well as behavior therapy, and the presence of any significant active medical condition were excluded from the study". Setting: psychiatric hospital Dropouts/withdrawals: 2 participants in each group withdrew consent prior to week 5 (1st outcome measurement point) Sample size: 50 (25 each group) Mean age: 7.6 years Gender: minocycline 17/23 male; placebo 18/23 male IQ: details not provided Baseline ABC‐I or other BoC: ABC‐I intervention group 21.26 (4.82), comparator group 19.91 (7.20) Concomitant medications: participants were not allowed to be taking antipsychotics concomitantly. Previous medications: details not provided |
|
| Interventions | Intervention (minocycline + risperidone): minocycline
100 mg/day + tablet risperidone 1‐2 mg/day as
intervention 10 weeks Comparator (placebo + risperidone): risperidone 1‐2 mg/day + capsule placebo as control for 10 weeks. The maximum target dose of risperidone was defined as 1 mg/day for children weighing < 20 kg and 2 mg/day for those weighing ≥ 20 kg |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported |
|
| Notes | Study start date: March 2013 Study end date: March 2015 Funding: "This study was supported by a grant from Tehran University of Medical Sciences to Dr. Shahin Akhondzadeh (Grant No. 20288)". Also, "The authors also affirm that there was no source of funding" Conflicts of interest: 'the authors do not have any conflicts of interest" Trial registry: IRCT201302201556N50 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Patients were randomised to receive either minocycline or placebo in a 1:1 ratio using a computer‐generated code. |
| Allocation concealment (selection bias) | Low risk | The assignments were kept in sealed opaque envelopes until data analysis. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Throughout the study, the person who administered the medications, the rater, the participants, and parents were blind to assignments. Independent people were responsible for treatment allocation and participant interviews. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Placebo was identical to the intervention medication (minocycline) in shape, size, colour, and taste and was dispensed by the investigational drug pharmacist. Throughout the study, the person who administered the medications, the rater, the participants, and parents were blind to assignments. Independent people were responsible for treatment allocation and participant interviews |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 2 participants in each group discontinued (8% each group) and imputation was not used |
| Selective reporting (reporting bias) | Low risk | Outcomes reported match protocol |
| Other bias | High risk |
|
Ghanizadeh 2013.
| Study characteristics | ||
| Methods | Parallel trial of N‐acetylcysteine (NAC) + risperidone versus placebo + risperidone | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: child and adolescent psychiatry clinics affiliated with Shiraz University of Medical Sciences Sample size: 40 (20 to each group) Number of withdrawals/dropouts: NAC: lack of efficacy 0, declined to return 3, severe sedation 1. Placebo: lack of efficacy 3, declined to return 4, severe sedation 0 Gender: NAC 13/17 boys; placebo 12/14 boys Mean age: NAC 8.8 years; placebo 7.9 years IQ: not reported Baseline ABC‐I or other BoC: ABC‐I NAC + risperidone 13.2; placebo + risperidone 16.7 Concurrent medications: clonidine NAC (5), placebo (3); folic acid NAC (2), placebo 0; imipramine NAC (1), placebo (0); biperiden 1 each group; nortriptyline 1 (NAC group); topiramate NAC (0), placebo (2) History of previous medications: not reported |
|
| Interventions | Intervention (NAC + risperidone) for 8 weeks: 1200
mg/day in twice‐daily doses. Risperidone started at
the dose of 0.5 mg/day, titrated up to 2 mg/day
during 3 weeks for children weighing < 30 kg. The
dose for children > 30 kg was up to 3 mg/day. Comparator (placebo + risperidone) for 8 weeks: placebo tablets were administered in the form of effervescent. The shape, size, taste, and colour of NAC and placebo were identical. Risperidone started at the dose of 0.5 mg/day, titrated up to 2 mg/day during 3 weeks for children weighing < 30 kg. The dose for children > 30 kg was up to 3 mg/day. |
|
| Outcomes | Primary outcomes:
Secondary outcomes: tolerability Timing of outcome assessments: baseline, 4 weeks and 8 weeks (endpoint) |
|
| Notes | Study start date: 2011 Study end date: 2012 Source of funding: "This study was supported by a grant from Shiraz University of Medical Sciences (Grant No: 5545)." Conflicts of interest: none declared Trial registry: IRCT201106103930N6 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "patients were randomly allocated into one of the two groups using a random number generator" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "The patients, parents, and independent assessor were blind to the allocation of patients" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "the independant assessor was blind to the allocation of patients" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Data analysed for 17/20 in NAC group and 14/20 in placebo group |
| Selective reporting (reporting bias) | Low risk | Relevant ABC domains reported |
| Other bias | Unclear risk | Unclear whether there were differences in the dose of risperidone between groups. 5 in the NAC group and 3 in the placebo group also received clonidine. 2 in the placebo group but none in the NAC group received topiramate. |
Ghanizadeh 2015.
| Study characteristics | ||
| Methods | Parallel trial of buspirone + risperidone versus placebo + risperidone | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: "child and adolescent psychiatry clinic affiliated with Shiraz University of Medical Sciences [Iran] clinics specializing in the treatment of child and adolescent psychiatry problems". Sample size: 40 (20 in each group) Number of withdrawals/dropouts: 16 completing trial in the busperone group; 18 in placebo group Gender: buspirone 12/16 boys, placebo 15/18 boys Mean age: buspirone 7.05 years, placebo 7.5 years IQ: not reported Baseline ABC‐I or other BoC: ABC‐I buspirone 25.7, placebo 24.7 Concomitant medications: not reported History of previous medications: not reported |
|
| Interventions | Intervention (buspirone + risperidone) for 8 weeks:
buspirone was titrated to a maximum 10 mg/day given
twice daily for children weighing < 40 kg, and up
to 20 mg/day for children weighing > 40 kg. The
dose of risperidone was up to 2 mg/day for children
weighing < 40 kg and up to 3 mg/day for children
weighing > 40 kg. The dosage was increased to
this target/maximum dose from week 1 to week 2, and
modified at any time in response to clinical
efficacy and AEs. Comparator (placebo + risperidone) for 8 weeks: the dose of risperidone was up to 2 mg/day for children weighing < 40 kg and up to 3 mg/day for children weighing > 40 kg. The dosage was increased to this target/maximum dose from week 1 to week 2, and modified at any time in response to clinical efficacy and AEs. |
|
| Outcomes | Primary outcomes:
Secondary outcomes: tolerability Timing of outcome assessment: baseline, week 4, week 8 |
|
| Notes | Study start date: 2012 Study end date: 2013 Source of funding: supported by a grant from Shiraz University of Medical Sciences to Professor Ahmad Ghanizadeh (grant no. 6978) Conflicts of interest: none declared Trial registry: IRCT201307303930N28 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A random number list provided by a random number generator was used for the allocation of the patients into the groups". |
| Allocation concealment (selection bias) | Unclear risk | Quote: "both risperidone and placebo were administered in the form of similar tablets" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Reported to be double‐blinded however, the "physician who interviewed the patients and allocated the patients into the groups was not blinded". |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The person who allocated the patients into the group and the person who rated the outcome measure were different. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Mentioned assessment at week 4 but these outcomes
were not reported LTFU: 2 people did not respond to calls (1 in each group). 1 person's symptoms of crying and isolation were exacerbated (buspirone group) |
| Selective reporting (reporting bias) | High risk | The Iranian clinical trial registry does not include results (neither does the paper include week 4 measures) and the trial was retrospectively registered online. |
| Other bias | High risk | The study authors retrospectively registered the trial on the Iranian clinical trials website ‐ it is unknown whether 8 weeks was the original length of the trial or not. |
Ghanizadeh 2014.
| Study characteristics | ||
| Methods | Parallel trial of aripiprazole versus risperidone | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: child psychiatry outpatient clinic affiliated with Shiraz University of Medical Sciences, Iran Sample size: 59 were randomised (29 aripiprazole, 30 risperidone) Number of withdrawals/dropouts: 3 children dropped out of aripiprazole group because of severity of symptoms (1), exacerbation of epilepsy (1) and severe sedation (1). 3 children dropped out of the risperidone group due to lack of efficacy (1), refused to return (1), agitation and crying (1) Gender: aripiprazole 25/29 male; risperidone 23/30 male Mean age: aripiprazole 9.6 years, risperidone 9.5 years IQ: not reported Baseline ABC‐I or other BoC: ABC‐I aripiprazole 26.2; risperidone 21.5 Concomitant medications: concurrent medications were allowed apart from antipsychotics provided they were stable throughout the trial and commenced at least two weeks prior to the trial. History of previous medications: details not provided |
|
| Interventions | Intervention (aripiprazole) for 8 weeks: maximum dose
of aripiprazole for children weighing < 40 kg was
up to 10 mg/day and up to 15 mg/day for children
> 40 kg. The dose of aripiprazole was titrated
over 2 weeks (1.25 mg/day starting dose); mean daily
dose of 5.5 mg/day (approximately 0.163
mg/kg/day) Comparator (risperidone) for 8 weeks: maximum dose for children weighing < 40 kg was 2 mg, and for those > 40 kg was up to 3 mg/day. Risperidone was titrated over 2 weeks (0.25 mg starting dose); risperidone mean daily dose 1.12 mg/day (or 0.033 mg/kg/day) |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: baseline, 1 month and 2 months (endpoint) |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: "grant (No: 3135) from Shiraz University of Medical Sciences to Professor Ahmad Ghanizadeh. MB is supported by the Simons Autism Foundation. MB has received Grant/Research Support from the NIH, Cooperative Research Centre, Simons Autism Foundation, Cancer Council of Victoria, Stanley Medical Research Foundation, MBF, NHMRC, Beyond Blue, Rotary Health, Geelong Medical Research Foundation, Bristol Myers Squibb, Eli Lilly, Glaxo SmithKline, Organon, Novartis, Mayne Pharma and Servier, has been a speaker for Astra Zeneca, Bristol Myers Squibb, Eli Lilly, Glaxo SmithKline, Janssen Cilag, Lundbeck, Merck, Pfizer, Sanofi Synthelabo, Servier, Solvay and Wyeth, and served as a consultant to Astra Zeneca, Bristol Myers Squibb, Eli Lilly, Glaxo SmithKline, Janssen Cilag, Lundbeck Merck and Servier, and is a co‐inventor of two provisional patents regarding the use of NAC and related compounds for psychiatric indications". Conflicts of interest: none declared Trial registry ‐ IRCT201110233930N15 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The clinician who administered the medications was not blind to assignment and "about 7 of the parents (12%) of the parents were not blinded to the group assignment because they could correctly guess the group allocation or requested to be not blinded to it". |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Some parents knew of their allocation and contamination could have occurred. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants completed both the first and second
follow‐up and an ITT analysis was used. LTFU aripiprazole: severity of symptoms (1); exacerbation of epilepsy (1); and severe sedation (1) LTFU risperidone: lack of efficacy (1); refused to return (1); agitation and crying (1) |
| Selective reporting (reporting bias) | High risk | The most common AEs associated with risperidone were not reported (sedation and weight gain) |
| Other bias | Low risk | None identified |
Gordon 1993.
| Study characteristics | ||
| Methods | Cross‐over trial of clomipramine, desipramine, and placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: outpatient clinic, USA Sample size: 24 in total (cross‐over) Number of withdrawals/dropouts: 1 in clomipramine group and 1 other dropout although group was not specified. Gender: 15/24 male Age range: 6‐18 years IQ range: 30‐107 Baseline ABC‐I or other BoC: not reported Concomitant medications: not reported History of previous medications: not reported |
|
| Interventions | Intervention 1 (clomipramine) for 5 weeks: mean final
dose was 152 mg/day (SD 56), 4.3 mg/kg/day (SD 0.8).
The initial dosage was 25 mg/day, and titrated to a
maximum of 5 mg/kg per day or 250 mg/day usually
between weeks 2 and 3 Intervention 2 (desipramine) for 5 weeks: mean final dose was 127 mg/day (SD 52). 4.0 mg/kg/day (SD 1.2). The initial dosage was 25 mg/day, titrated to a maximum of 5 mg/kg per day or 250 mg/day usually between weeks 2 and 3 Comparator (placebo) for 5 weeks: equivalent placebo |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: none reported Timing of outcome assessment: week 5 (endpoint) |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: not reported Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomisation was performed by the National Institutes of Health pharmacy using a random‐number table". |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details of blinding were not provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Details not provided |
| Incomplete outcome data (attrition bias) All outcomes | High risk | LTFU: clomipramine/desipramine 2; 1 in the clomipramine/ desipramine group because of violent outbursts and 1 because the group home administered his medicine to the wrong participant. |
| Selective reporting (reporting bias) | Unclear risk | Outcomes that were mentioned in the paper were reported. No protocol was available. |
| Other bias | Unclear risk | No baseline comparisons were reported by group. |
Guastella 2015a.
| Study characteristics | ||
| Methods | 8‐week parallel trial of oxytocin versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria: "females, severe depressive or psychotic symptoms, including suicidal thoughts and/or actions, cardiovascular disease, kidney disease, smoking more than 15 cigarettes a day, substance dependence, or sensitivity to preservatives (in particular, E 216, E 218, and chlorobutanol hemihydrate)". Location/setting: autism clinic at the Brain & Mind Research Institute, University of Sydney, Australia Sample size: oxytocin (26), placebo (24) Number of withdrawals/dropouts: placebo, 1, parent unwilling to attend follow‐up assessment, 2 discontinued (1 parent withdrew, 1 AEs) Gender: all male Age range: oxytocin 13.85. placebo 14.00 years IQ range: mean IQ oxytocin 80.04, placebo 93.14 Baseline ABC‐I or other BoC: self‐injurious behaviour (measured using the Repetitive Behaviour Scale (self‐injurious subscle), oxytocin baseline 1.96 (2.27); placebo 3.13 (3.75) Concurrent medications: adjunctive psychotropic medication use (oxytocin = 9, placebo = 9) included stimulants (35.7%), antipsychotics (28.6%), antidepressants (25%), mood stabilisers (7.1%), and benzodiazepines (3.6%) History of previous medications: not reported |
|
| Interventions | Intervention (oxytocin nasal spray): either 18 or 24
IU, administered twice daily for 8 weeks Comparator (placebo nasal spray): administered twice daily for 8 weeks. |
|
| Outcomes | Primary outcomes: self‐injurious behaviour measured
using the Repetitive Behaviour Scale (Bodfish
2000) Secondary outcomes: tolerability Timepoints ‐ baseline, endpoint and 3‐month follow‐up |
|
| Notes | Study start date: February 2009 Study end date: January 2012 Funding: "This study was funded by a National Health and Medical Research Council Project Grant to authors A.J.G., K.M.G., N.J.R., and S.L.E. (632625)" Conflicts of interest: most authors were also receiving funding for other trials. Other: trial registry ACTRN12609000513213 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Nasal sprays were developed and randomised by a compounding chemist with an identical placebo containing all ingredients except the active oxytocin |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Double‐blinded ‐ no further details provided |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Data were entered by research assistants blind to drug assignment" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low dropout. Analysed in ITT format, although "last‐observations‐carried‐forward to replace missing data" was used which is a dubious method. |
| Selective reporting (reporting bias) | Low risk | Same primary outcome and measurement timepoints as clinical trial reg |
| Other bias | Low risk | No other sources of bias identified |
Hagerman 2018.
| Study characteristics | ||
| Methods | 6‐month trial of sertraline versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: USA Sample size: 58 (32 sertraline, 26 placebo) Number of withdrawals/dropouts: sertraline (8, 2 lost to follow‐up, 6 withdrew consent); placebo (5, 1 lost to follow‐up, 4 withdrew consent) Gender: details not provided Average age (SD) : 4.3 (0.8) and 3.7 (1.1) years in the sertraline and placebo groups IQ range: details not provided Baseline ABC‐I or other BoC: N/A Concurrent medications: sertraline (9.38%); placebo (7.69%) History of previous medications: details not provided |
|
| Interventions | Intervention: the study drug was administered orally
in liquid form (20 mg/mL), and dose was assigned
based on age at enrolment: participants under 4
years received sertraline or placebo liquid in a
dose of 2.5 mg/day (0.125 mL) for the duration of
the trial, and participants ≥ 4 years received 5.0
mg/day (0.25 mL). Comparator: placebo was administered orally in liquid form for 6 months. |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: tolerability |
|
| Notes | Study start date: April 2015 Study end date: July 2018 Funding: "This project was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number R40MCH 27701". Conflicts of interest: "RH has carried out treatment studies in fragile X syndrome and autism spectrum disorder by Roche, Novartis, Neuren, Marinus, Alcobra, and Curemark and has also consulted with Zynerba and Fulcrum. FT received funds from Asuragen, Roche, and Zynerba. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest". Trial registry: NCT02385799 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The UC Davis Investigational Drug Services independently carried out randomization". No information on sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "The UC Davis Investigational Drug Services independently carried out randomization" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Apart from "double‐blinded" no further details were provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Apart from "double‐blinded" no further details were provided. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropout < 20% and reasons reported |
| Selective reporting (reporting bias) | Low risk | Same primary outcomes as trial reg (MSEL expressive language raw score and age equivalent combined score) |
| Other bias | Low risk | No other sources of bias identified |
Hajizadeh‐Zaker 2018.
| Study characteristics | ||
| Methods | 10‐week trial of L‐carnosine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: speciality clinic for autism in the children’s outpatient clinic (Iran) Sample size: 50 Number of withdrawals/dropouts: risperidone + L‐carnosine (n = 4) 4 discontinued treatment (withdrew consent), risperidone + placebo (n = 4) 4 discontinued treatment (withdrew consent) Gender: 35 male, 7 female Mean age: L‐carnosine + risperidone 8.24 (2.22), placebo + risperidone 7.90 (1.89) Mean IQ: details not provided Baseline ABC‐I or other BoC: ABC‐I > 22.0 at baseline Concurrent medications: details not provided History of previous medications: details not provided |
|
| Interventions | Intervention (L‐carnosine + risperidone): L‐carnosine
was administered in tablet form, 400 mg twice daily,
+ tablet form of risperidone, 1‐3.5 mg/day, for 10
weeks Comparator (placebo + risperidone): risperidone was administered in tablet form, 1‐3.5 mg/day, plus placebo in tablet form for 10 weeks. |
|
| Outcomes | Primary outcomes:
Secondary outcomes: tolerability |
|
| Notes | Study start date: December 2015 Study end date: November 2016 Funding: "This study was supported by a grant from Tehran University of Medical Sciences to Prof. S.A. (Grant No. 29571). This study was supported by a grant from Tehran University of Medical Sciences (Grant No. 29571)". Conflicts of interest: "No competing financial interests exist". Other ‐ trial registry: IRCT201512081556N83 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A computerised random number generator (allocation ratio 1:1) was applied to generate randomisation codes |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes were used to keep the assignments to mask the allocation throughout the study. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "The children, parents, the physician who referred the children, the physician who arranged the medications, the rater, and the statistician were all blinded to the allocated treatment." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The children, parents, the physician who referred the children, the physician who arranged the medications, the rater, and the statistician were all blinded to the allocated treatment." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 16% dropout in both groups. |
| Selective reporting (reporting bias) | Low risk | Outcome measures reported per protocol |
| Other bias | High risk |
|
Handen 2005.
| Study characteristics | ||
| Methods | Cross‐over trial of secretin versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: research centre at the Children’s Hospital of Pittsburgh Sample size: 8 in total (cross‐over) Number of withdrawals/dropouts: none reported Gender: 7 male, 1 female Mean age: 7 years, 6 months IQ: "IQs ranged from moderate mental retardation [intellectual disability] to gifted (with two subjects functioning within the moderate range of mental retardation, three within the mild range, one with borderline intellectual functioning, one with average abilities and one functioning within the gifted range)". Baseline ABC‐I or other BoC: ABC‐I 11.4 Concurrent medications: not reported History of previous medications: not reported |
|
| Interventions | Intervention (porcine secretin): 2 infusions of
porcine secretin at a dose of 2 IU/kg at the start
of the secretin phase and 2 months later Comparator (placebo): single 2 IU/kg dose of placebo |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessment: baseline, 1 month and 2 months post‐infusion |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: "this research was supported by a small grant to the authors from the General Clinical Research Center at Children's Hospital of Pittsburgh" Conflicts of interest: none disclosed Trial registry: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Allocated by hospital pharmacist |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not clear how many participants were originally randomised to the study |
| Selective reporting (reporting bias) | Unclear risk | The primary outcomes mentioned at the start of the paper are the ABC (and 5 subscales), the CGI, the Dosage Record and Treatment Emergent Symptom Scale (DOTES), and the Gilliam Autism Rating Scale (GARS). Adverse events were not recorded, although the other 3 scales were recorded in full. |
| Other bias | Unclear risk | Cross‐over study and all participants appear to have completed both phases of the study |
Handen 2008.
| Study characteristics | ||
| Methods | Cross‐over trial of guanfacine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: outpatient speciality clinic serving children with developmental disorders Sample size: 11 in total Number of withdrawals/dropouts: 1 from placebo group due to non‐compliance Gender: 10 male, 1 female Mean age: 7.3 years IQ: cognitive functioning ranged from severe intellectual disability to average IQ. Baseline ABC‐I or other BoC: details not provided Concomitant medications: Adderall (2), mirtazapine (1); risperidone, zolpidem, tartrate and carbamazepine (1); nortriptyline (1); lamotrigine (1); methylphenidate (1); and bupropion and clonidine (1) History of previous medications: details not provided |
|
| Interventions | Intervention (guanfacine): began on a maximum of 3.0
mg/day titrated doses over a 19‐day period. After 8
days on the highest dose, a 6‐day washout period
commenced (1.5 mg/day for 3 days and 0 mg/kg per day
for 3 days) Comparator (placebo): equivalent placebo for 8 days |
|
| Outcomes | Primary outcomes: irritability, measured using the
parent‐rated ABC‐I subscale (Aman 1985) Secondary outcomes: tolerability Timing of outcome assessments: baseline then at 4 additional visits |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: not reported Conflicts of interest: not reported Trial registry: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided, only that it is a double‐blinded trial |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Details not provided |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "we did not have complete sets of parent and/or teacher data for some subjects (e.g., one parent whose child was in the summer program was unreliable in completing questionnaires; some trials that occurred across a school vacation resulted in incomplete teacher data). Our solution was to use parent data as our primary source when available and to use teacher data if parent data were missing." |
| Selective reporting (reporting bias) | High risk | The authors note that the ABC was measured at baseline and an additional four visits. Neither baseline nor additional visit scores were recorded. |
| Other bias | High risk | Quote: "no standardized instruments were used to assess autistic disorder and comorbid psychiatric diagnoses" (among other limitations) |
Handen 2011.
| Study characteristics | ||
| Methods | Parallel trial of donepezil versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria: not reported Location/setting: not reported Sample size: 34 (donepezil 18, placebo 16) Number of withdrawals/dropouts: "one subject terminated due to an increase in aggression and irritability. Two other subjects were unable to tolerate the 10mg/day dose and were maintained on a 5mg/day dose". Gender: details not provided Mean age: treatment group 8 years 7 months, placebo group 9 years 7 months IQ: mean 96.8 (treatment group), 96.7 (placebo group) Baseline ABC‐I or other BoC: baseline CBCL (aggression) 9.72; RFRLRS (affectual responses i.e. irritability) 0.90 Concurrent medications: concurrent psychotropic medications allowed provided the dose levels are maintained during the trial. 5 participants were taking SSRIs, 4 were taking stimulants and 2 were taking atomoxetine. History of previous medications: not reported |
|
| Interventions | Intervention ‐ donepezil max 5 mg/day for 4 weeks
followed by donepezil maximum 10 mg/day for 4 weeks
if tolerated. Participants began on 2.5 mg/day
increasing to 5 mg/day after 1 week. After 4 weeks
at 5 mg/day doses were increased to 7.5 mg/day for 1
week, up to a maximum of 10 mg/day for the remaining
for 4 weeks (for 16/18 who could tolerate higher
doses). Comparator (placebo) for 10 weeks: equivalent placebo |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: "following randomisation, subjects were seen for a total of 4 clinic visits (following one week on 2.5mg/day, following four weeks on 5.0mg/day, one week on 7.5mg/day, and four weeks at 10mg/day". |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: NIMH Grant 5R21 MH64941‐03 as well as a gift by Pfizer and Eisai Pharmaceutical companies Conflicts of interest: none declared Trial registry: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The study pharmacist conducted the randomization for each subject" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described though study authors stated the trial was double‐blind |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | LOCF analysis used for the one of 34 randomised participants who did not complete the trial |
| Selective reporting (reporting bias) | Low risk | All outcome data appear to have been reported |
| Other bias | High risk | A gift was given by Pfizer and Eisai Pharmaceutical companies (who also provided the medication and placebo for this trial). The placebo group were one year older (9 years 7 months) compared to the donepezil group (8 years 7 months). Baseline scores for aggression (9.72 vs 7.47) and irritability (0.90 vs 0.80) were also higher for the donepezil group. |
Handen 2015.
| Study characteristics | ||
| Methods | Parallel trial of atomoxetine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: University of Pittsburgh Medical Centre, Ohio State University, and University of Rochester, USA Sample size: atomoxetine 32, placebo 32 Number of withdrawals/dropouts: inadequate improvement (2 placebo group); behavioural AEs especially irritability 2 atomoxetine group, 3 placebo group; physical AE 2 placebo group; LTFU 1 from each group; other LTFU/unknown 3 placebo group Gender: atomoxetine 26/32 boys; placebo 24/32 boys Mean age: atomoxetine 8.6 years; 8.2 years placebo IQ: atomoxetine group: 78.7; placebo group: 86.7 Baseline ABC‐I or other BoC: ABC‐I atomoxetine group: 16.00; placebo group 16.97 Concomitant medications: “a single anticonvulsant for seizure control was allowed, provided that stable doses and seizure‐free status had been 6 months or more”. History of previous medications: details not reported |
|
| Interventions | Intervention (atomoxetine) for 10 weeks: the initial
dose was 0.3 mg/kg/day (rounded to the nearest 5 mg)
with weekly escalations by 0.3 mg/kg/day, unless
there were limiting side effects or no further
improvement, to a target dose of 1.2 mg/kg/day, but
could be increased to a maximum of 1.8 mg/kg/day.
Mean final dose of atomoxetine was 1.38
mg/kg/day. Comparator (placebo) for 10 weeks: sugar pill administered twice daily |
|
| Outcomes | Primary outcomes:
Secondary outcomes: tolerability Timing of outcome assessment: “study visits occurred weekly to assess medication response, to monitor adverse events (AEs), and to adjust doses. Final dose adjustments were made at week 6, with subsequent monitoring visits at weeks 8 and 10" |
|
| Notes | Study start date: October 2008 Study end date: April 2014 Source of funding: grants from the National Institute of Mental Health to Ohio State University (5R01MH079080), University of Pittsburgh (5R01MH079082‐05), and University of Rochester (5R01 MH083247), by Eli Lilly and Co, who provided atomoxetine and placebo, and by the University of Rochester CTSA (UL1 RR024160) and Ohio State University CTSA (UL1TR001070) from the National Center for Research Resources and the National Center for Advancing Translational Sciences of the National Institutes of Health Conflicts of interest: none declared Trial registry: NCT00844753 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The study biostatistician generated the randomisation sequence using a computer algorithm" |
| Allocation concealment (selection bias) | Low risk | Quote: "a designated team member at each site obtained the assignment for each participant via a Web portal maintained by the data centre" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "ATX [atomoxetine] assignment was double‐blinded" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "ATX [atomoxetine] assignment was double‐blinded". Independent evaluators blinded to treatment assignment until completion of the study rated participants on the CGI scale. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | High LTFU across groups 29/128 although data were estimated from Missing At Random models and sensitivity tested using LOCF. |
| Selective reporting (reporting bias) | Unclear risk | Protocol and archived versions available NCT00844753 |
| Other bias | Unclear risk | More than twice as many (72%) in special education compared to placebo group (34%) |
Hardan 2012.
| Study characteristics | ||
| Methods | Parallel trial of N‐acetylcysteine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Setting/location: autism clinic at Stanford University, USA Sample size: 33 (15 randomised to NAC and 18 to placebo) Number of withdrawals/dropouts: 2 from NAC group (1 AE, 1 dislike taste); 6 from placebo group (3 dislike the taste, 2 withdrawal, 1 LTFU) Gender: 31 male, 2 female Mean age: NAC group 7.0 years, placebo 7.2 years IQ: details not provided Baseline ABC‐I or other BoC: NAC group ABC‐I 16.9, repetitive behaviour scale (Scales of Independent Behaviour) 3.9; placebo group ABC‐I 14.8, Repetitive Behaviour Scale (Scales of Independent Behaviour) 3.4 Concomitant medications: "14 subjects were on at least on psychotropic medication with three being on more than one. The most commonly prescribed classes of medication were second generation antipsychotics and SSRIs". History of previous medications: details not provided |
|
| Interventions | Intervention (N‐Acetylcysteine) for 12 weeks: NAC was
initiated at 900 mg/day for the first 4 weeks, then
900 mg twice/day for 4 weeks, then 900 mg 3
times/day for 4 weeks (or matching placebo) Comparator (placebo) for 12 weeks: sugar pill |
|
| Outcomes | Primary outcomes:
Secondary outcomes: tolerability Timing of outcome assessment: baseline, 4, 8 and 12 weeks |
|
| Notes | Study start date: March 2009 Study end date: September 2010 Source of funding: "grant from the Escher Family Fund at the Silicon Valley Community Foundation to AYH. Dr AY Hardan has received research support from the companies: Bristol‐Myers Squibb Company and Forest Pharmaceuticals. Dr Frazier has received research support from, acted as a consultant to, or received travel support from Shire Development, Inc. and Bristol‐Myers Squibb Company. Dr LA Herzenberg and Dr R Tirouvanziam are listed as inventors on two patents licensed by Bioadvantex, Inc, the supplier of the N‐acetylcysteine and placebo for this study, covering the use of N‐acetylcysteine in cystic fibrosis". Conflicts of interest: none declared Trial registry: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomisation was done by the Stanford pharmacist using www.randomization.com, which randomises each subject by using the method of randomly permuted blocks" |
| Allocation concealment (selection bias) | Low risk | Quote: "each participant received a supply of the compound (NAC or placebo) labeled with a reference number" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Parents and investigators involved in the study were blinded to participant status". "The study coordinator was not involved in randomisation and clinical ratings, received information about the group assignments and distribute the compound to the parents" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "investigators involved in the study were blinded to participants' status" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Participants did not complete intervention after randomisation ‐ unclear if ITT analysis or other approach was used to account for these losses. |
| Selective reporting (reporting bias) | Unclear risk | Without knowing what was in the trial protocol, it is difficult to know if outcomes and measures originally undertaken were reported |
| Other bias | High risk | Pharmaceutical company provided both active treatment and placebo for study. 2 study authors are inventors of two patents listed with this same company. |
Hardan 2019.
| Study characteristics | ||
| Methods | ‐week trial of memantine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Setting/location: paediatric outpatient settings at multiple study sites (92 sites in 15 countries) Sample size: 158 and 160 randomised to memantine and placebo groups respectively and 108 and 116 completed the trial Number of withdrawals/dropouts: 8 (placebo 1 protocol violation, 1 consent withdrawal; memantine reduced dose 1 did not meet eligibility criteria; memantine full dose 1 did not meet eligibility criteria, 3 protocol violation, 1 LTFU) Gender: placebo 88.8% were male, memantine 84.1% were male Mean age: placebo mean age 8.9 years, memantine mean age 9.2 years IQ: placebo mean IQ 93.3, memantine mean IQ 91.1 Baseline ABC‐I or other BoC: not reported Concomitant medications: "83.8% of participants were taking concomitant medications and supplements, most commonly (≥ 10.0%) melatonin (17.0%), multivitamin (15.9%), ibuprofen (11.4%), risperidone (10.6%), and paracetamol (10.3%)" History of previous medications: not reported |
|
| Interventions | Intervention (memantine): doses were based on weight;
≥ 60 kg maximum 15 mg/day, 40‐59 kg maximum 9
mg/day, 20‐39 kg maximum 6 mg/day, < 20 kg
maximum 3 mg/day. These doses were reduced to 6
mg/day, 3 mg/day, 3 mg/day and 3 mg every other day,
for each respective group. Comparator (placebo): matching placebo for 12 weeks |
|
| Outcomes | Primary outcomes:
Secondary outcomes: tolerability |
|
| Notes | Study start date: May 2009 Study end date: August 2012 Funding: "Funding for these studies was provided by Forest Research Institute (Jersey City, NJ), the sponsor at the time the studies were conducted." Conflicts of interest: none declared Trial registry: NCT00872898 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Premier, Inc. provided Interactive Web Response System (IWRS) services for randomization." |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Double‐blind ‐ no further details provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Double‐blind ‐ no further details provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low dropout; an ITT analysis was used that included all participants with at least 1 post‐baseline outcome assessment. |
| Selective reporting (reporting bias) | High risk | ABC‐I (change from baseline) was mentioned as an outcome in the paper, but it was not reported, only "At week 12, no clinically meaningful changes from baseline were observed between treatment groups on the additional efficacy variables, CGI‐I and CGI‐S, ABC‐C, or SRS [Social Responsiveness Scale] subscales and SRS total raw score." |
| Other bias | High risk | Funding for these studies was provided by Forest Research Institute (Jersey City, NJ), the sponsor at the time the studies were conducted. Writing support was funded by Allergan plc (formerly Forest Research Institute; Madison, NJ). Two of the listed study authors were employed by the sponsor. |
Harfterkamp 2014.
| Study characteristics | ||
| Methods | Parallel trial of atomoxetine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: 9 Dutch child and adolescent psychiatry centres, 6 university centres, (Amsterdam, Groningen, Leiden, Maastricht, Nijmegen, and Utrecht), and 3 non‐university centres (The Hague, Hoorn, an Oosterhout). Sample size: 48 in atomoxetine group, 49 in placebo group Number of withdrawals/dropouts: placebo group: protocol violation (2), physician decision (1). Atomoxetine group: AE (1), protocol violation (2), lack of efficacy (1), parent/ caregiver decision (1) Gender: atomoxetine 42/48 male, placebo 41/49 Mean age: atomoxetine 9.9 years, placebo 10.0 years IQ: atomoxetine 91, placebo 94.6 Baseline ABC‐I or other BoC: atomoxetine ABC‐I 17.3, placebo ABC‐I 16.2 Concomitant medications: participants were not permitted to be using psychoactive medications prior to study on an ongoing basis History of previous medications: atomoxetine 18/48 and placebo 18/49 had not received any prior psychopharmacological treatment |
|
| Interventions | Intervention (atomoxetine) for 8 weeks: maximum of
1.2 mg/kg/day daily dose. First week 0.5 mg/kg/day;
2nd week 0.8 mg/kg/day; 1.2 mg/kg/day for 6
weeks Comparator (placebo) for 8 weeks: maximum of 1.2 mg/kg/day daily dose. First week 0.5 mg/kg/day; 2nd week 0.8 mg/kg/day; 1.2 mg/kg/day for 6 weeks |
|
| Outcomes | Primary outcomes:
Secondary outcomes: tolerability Timing of outcome assessments: baseline and 8 weeks (endpoint) |
|
| Notes | Study start date: October 2006 Study end date: March 2008 Source of funding: funded by Eli Lilly and company. "Myriam Harfterkamp has accepted invitations for congress travels from Eli Lilly and Eurocept. Ruud B. Minderaa was advisor for Eli Lilly. Jan K. Buitelaar has been a consultant to/member of advisory board of, and/or speaker for Bristol‐Myer Squibb, Eli Lilly, Janssen Cilag BV, Medice, Organon/Shering Plough, Servier, Shire, and Union Chimique Belge (UCB). Gigi van de LooNeus has received honoraria for a presentation from Eli Lilly and wasmember oftheadvisory boardforUCBPharma B.V. andShire. Rutger‐Jan van der Gaag has no financial disclosures. Pieter J. Hoekstra has received honoraria for presentations or advice from Desitin, Eli Lilly, and Shire". Conflicts of interest: none declared Trial registry: NCT00380692 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Details were not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | An ITT analysis was used and all participants who received at least 1 dose of the drugs were included in the analysis |
| Selective reporting (reporting bias) | Low risk | Results reported on clinicaltrials.gov (NCT00380692) |
| Other bias | High risk | Sponsor: Eli Lilly and Company Information provided by: Eli Lilly and Company |
Hellings 2005.
| Study characteristics | ||
| Methods | Parallel trial of valproate versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: recruitment was through University of Kansas MR/Autism outpatient, USA Sample size: 30 in total (16 to valproate, 14 to placebo) Number of withdrawals/dropouts: 13/16 valproate participants completed the trial, 12/14 in placebo group completed the trial. 1 severely hyperactive and 1 spreading skin rash dropped out on advice from principal investigator and unblinded child psychiatrist, remaining 3 dropped out due to "manifested dangerous aggression". Gender: 20 boys, 10 girls Mean age: 11.2 years Mean IQ: 54 Baseline ABC‐I or other BoC: ABC‐I valproate 23.33, placebo 21.93; aggression valproate 10.05, placebo 10.50. Concomitant medications: psychotropic or anticonvulsant medications were not allowed to be taken concurrently. History of previous medications: details not provided |
|
| Interventions | Intervention (valproate acid 20 mg/kg/day) for 8
weeks: after an initial 1‐week placebo lead‐in
phase, valproate liquid (250 mg/5 mL) was gradually
introduced with an additional 250 mg added every 3rd
day, replacing the equivalent amount of placebo
liquid, to achieve a dosage of 20 mg/kg/day. Comparator (placebo) for 8 weeks: placebo administered in a liquid form resembling valproate for 8 weeks |
|
| Outcomes | Primary outcomes:
Secondary outcomes: tolerability Timing of outcome assessments: weekly |
|
| Notes | Study start date: 1998 Study end date: 2003 Source of funding: "funding sources for this work were the National Institute of Mental Health (1K08MH01561‐01), National Institute of Child Health and Human Development (HD26927, HD02528), and Abbott Pharmaceuticals, Abbott Park, Illinois (Unrestricted $5,000 grant)." Conflicts of interest: none declared Trial registry: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "an 8‐week trial of two parallel groups of subjects, randomised to liquid VPA or placebo by the study pharmacist." |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "The investigators, parents, and teachers were blinded regarding medication or PBO [placebo] status" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "The investigators were blinded regarding medication or PBO [placebo] status" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | An ITT analysis was used however 1 participant is not
accounted for LTFU: 1 in valproate group and 1 in placebo group discontinued due to AEs, and 1 in valproate group withdrew due to non‐efficacy |
| Selective reporting (reporting bias) | Low risk | The ABC‐I was measured and reported at baseline and endpoint. |
| Other bias | Unclear risk | Potential bias with pharmaceutical company funding but "unrestricted" implies no involvement beyond financial. No significant differences in age, gender, current placement home, day placement school, years in current placement, parental marriage status, and aggression as the worst presenting symptom. |
Hendouei 2019.
| Study characteristics | ||
| Methods | 10‐week trial of resveratrol + risperidone versus placebo + risperidone | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: autism clinic in children's outpatient clinic of Roozbeh Hospital (Tehran University of Medical Sciences, Tehran, Iran) Sample size: resveratrol (35); placebo (35) Number of withdrawals/dropouts: resveratrol (4, 2 ineligible to continue, 2 consent withdrawn); placebo (4, 4 consent withdrawn) Gender: 50 male, 12 female Mean age: resveratrol 7.8 (2.1); placebo: 8.1 (1.9) IQ: details not provided Baseline ABC‐I or other BoC: ABC‐I of > 22 at baseline across both groups Concomitant medications: apart from resveratrol and risperidone no other concomitant medications were allowed in either group. History of previous medications: antipsychotics could not be taken in month prior to the study and any anticonvulsant use could not have changed in month prior to study |
|
| Interventions | Intervention (resveratrol + risperidone): both groups
were treated with risperidone twice daily, starting
at a dose of 0.5 mg, with a dose increase of 0.5 mg
per week (for the first 3 weeks). Resveratrol dosage
was 250 mg twice per day from the beginning of the
study. Comparator (placebo + risperidone): both groups were treated with risperidone twice daily, starting at a dose of 0.5 mg with a dose increase of 0.5 mg/week (for the first 3 weeks) plus placebo for 10 weeks. |
|
| Outcomes | Primary outcomes:
Secondary outcomes: tolerability Timing of outcome assessments: baseline, week 5 and week 10 (endpoint) |
|
| Notes | Study start date: January 2018 Study end date: April 2019 Funding: "This study was supported by a grant from Tehran University of Medical Sciences to Prof. Shahin Akhondzadeh (Grant No: 36420)" Conflicts of interest: "None of the authors in this study had conflict of interest of any kind with the parties that might be involved." Trial registry: IRCT20090117001556N104 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Using the Microsoft Office Excel software, each patient was assigned to a specific random code." |
| Allocation concealment (selection bias) | Low risk | The assignments were retained in confidential and sealed opaque envelops and were unveiled at the study endpoint for statistical analysis. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "all individuals involved in this study, such as patients and researchers, were blinded to the assignments." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Separate individuals were responsible for randomisations, drug administration, rating, data entry and statistical analysis. Furthermore, all individuals involved in this study, such as patients and researchers, were blinded to the assignments. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition, and all participants were accounted for |
| Selective reporting (reporting bias) | High risk | Doesn't report CARS (primary outcome on trial reg) and measurement time points different to trial reg |
| Other bias | High risk |
|
Herscu 2020.
| Study characteristics | ||
| Methods | 14‐week parallel trial of fluoxetine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria: "diagnosis of Asperger Syndrome or Pervasive Developmental Disorder Not Otherwise Specified, Rett Syndrome, Childhood Disintegrative Disorder, Patients planning to commence cognitive behaviour therapy during the period of the study or those who have begun cognitive behaviour therapy within 8 weeks prior to enrolment, or Patients who are currently taking fluoxetine or who have previously taken it". Location/setting: an autism network consisting of 18 centres Sample size: 158 (78 fluoxetine, 80 placebo) Reason for dropouts/withdrawals: fluoxetine 22 withdrawn (7 AEs, 6 withdrew consent, 1 sponsor decision, 2 lack of efficacy, 6 LTFU); placebo 15 withdrawn (5 AEs, 7 withdrew consent, 2 lack of efficacy, 1 LTFU). Mean age: 9.0 years Mean IQ: not reported Gender: 13% and 16% of the fluoxetine and placebo groups respectively were female Baseline ABC‐Irritability or other BoC: not reported Concomitant medications: participants were not allowed to be taking psychotropic medications. Previous medications: not reported |
|
| Interventions | Intervention (fluoxetine): all randomised
participants initiated treatment with 2 mg/day
fluoxetine, which could be titrated flexibly every 2
weeks to 4 mg, 6 mg, 9 mg, 13 mg, and a maximum of
18 mg/day. Comparator (placebo): all randomised participants initiated treatment with 2 mg/day placebo, which could be titrated flexibly every 2 weeks to 4 mg, 6 mg, 9 mg, 13 mg, and a maximum of 18 mg/day |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: tolerability Timing of outcome assessments: weeks 2, 4, 8, 10, 12 and 14 (endpoint) |
|
| Notes | Study start date: September 2007 Study end date: January 2009 Funding: "This study was funded by Neuropharm Plc. in collaboration with the Autism Speaks Autism Clinical Trials Network." Conflicts of interest: various consulting with and funding by pharmaceutical companies Trial registry: NCT00515320 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Treatment group was assigned centrally through the use of an automated clinical trials database. |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Double‐blinded ‐ no further details provided |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Scoring was by a site clinician who was blind both to drug/placebo assignment and to AEs (which could have biased the rater). |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High dropout (23%); ITT analysis based on percent change from baseline to endpoint (Week 14 or the **last assessment for those withdrawing**) |
| Selective reporting (reporting bias) | Low risk | Same primary outcome as clinical trial reg |
| Other bias | High risk | Funded by Neuropharm Plc. One person dropped out due to "sponsor decision" to withdraw from treatment group |
Hollander 2005.
| Study characteristics | ||
| Methods | Cross‐over trial of fluoxetine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: details not provided Sample size: 44 children or adolescents Number of withdrawals/dropouts: "three subjects were dropped due to noncompliance and one was dropped because of lack of efficacy, all prior to week 4". Gender: 30 boys, 9 girls Mean age: 8.18 +/‐ 3.04 IQ: 63.7 Baseline ABC‐I or other BoC: not reported Concomitant medications: none were allowed History of previous medications: details not provided |
|
| Interventions | Intervention (fluoxetine) for 8 weeks: fluoxetine was
started at 2.5 mg/day for a week, then titrated
based on weight to a maximum dose of 0.8 mg/kg/day;
0.3 mg/kg for week 2, 0.5 mg/kg/day for week 3, and
0.8 mg/kg/day for weeks 4–8. Dose prescribed on day
28 (end of week 4) was maintained for the remainder
of the 8‐week phase unless indicated due to side
effects, in which case the stable dose was lowered.
This was followed by a 4‐week washout period before
cross‐over to placebo. Comparator (placebo) for 8 weeks: the dosing schedule began at 2.5 mg/day of placebo once a day for 1 week. The following 7 weeks followed a flexible titration schedule up to a maximum of 0.8 mg/kg/day (0.3 mg/kg for week 2, 0.5 mg/kg/day for week 3, and 0.8 mg/kg/day weeks 4‐8) |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: tolerability Timing of outcome assessments: baseline and every 4 weeks until week 20 |
|
| Notes | Study start date: not reported Study end date: not reported Funding: "this work was supported by Orphan Products Division of the Food and Drug Administration Grant # FD‐R‐00152001‐03, NIH STAART Center of Excellence Grant #1U54 MM066673‐01A1, NARSAD Young Investigator Award for Dr Novotny, and the Seaver Foundation. Lilly Research Laboratories provided liquid fluoxetine and matching placebo for the study" Conflicts of interest: none declared Trial registry: NCT00004486 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "subjects were monitored and assessed weekly by the treating physician, who was blind to treatment condition, during the first 4 weeks of each fluoxetine/placebo phase of the study". "In addition, all CY‐BOCS and CGI‐AD outcome assessments were completed by an independent evaluator (IE) who did not have access to side effect data and who was blind to treatment condition, at baseline and every 4 weeks throughout the study, until week 20 or termination." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | All participants were accounted for and an ITT
analysis was used on the 39 participants who
completed the trial. LTFU: 1 participant not included in the analysis because of "lost pharmacy records, which made it impossible to be certain of the subject’s randomization condition" and three participants were dropped due to noncompliance and 1 was dropped because of lack of efficacy, all prior to week 4. |
| Selective reporting (reporting bias) | Unclear risk | The CY‐BOCS, CGI, the Vineland Adaptive Behavior Scale, Wechsler Preschool and Primary Intelligence Scale‐Revised (WPPSIR), Wechsler Intelligence Scale for Children (WISC‐III) (ages 7–16) or the Wechsler Adult Intelligence Scale‐Third Edition (WAIS‐III) (age 17). The CY‐BOCS was reported in full at weeks 0, 4 and 8, however the CGI scores were only reported at endpoint. |
| Other bias | Unclear risk | "This work was supported by Orphan Products Division of the Food and Drug Administration Grant # FD‐R‐001520‐ 01‐03, NIH STAART Center of Excellence Grant #1U54 MM066673‐01A1, NARSAD Young Investigator Award for Dr Novotny, and the Seaver Foundation. Lilly Research Laboratories provided liquid fluoxetine and matching placebo for the study. We acknowledge Charles Cartwright MD, Katherine Delaney PhD, and Sallie Jo Hadley MD for their clinical contributions to this study." |
Hollander 2006a.
| Study characteristics | ||
| Methods | 8‐week parallel study of divalproex sodium versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria: "medical illnesses (with the exception of stable seizure disorder), past history of psychotic disorders, and recent or current use of divalproex, terfenadine (Seldane), or astemizole (Hismanal). Subjects using any psychoactive medication were allowed to participate in the trial only if the dose remained stable for at least 3 months prior to and during the trial". Location/setting: "patients were recruited and screened for the presence of ASDs at the Seaver and New York Autism Center of Excellence" (USA) Number and reason for discontinuing: "one subject dropped out in week 5 due to lack of efficacy (on medication) and 12 subjects completed the trial". Mean IQ: IQ scores for the majority of participants were in the mild to moderate intellectual disability range, with a mean IQ score of 60 (range = 30–104) Gender: details not provided Mean age: 9.5 years (12 were children or adolescents (< 18 years), and 1 adult was aged 40) Baseline ABC‐I or other BoC: not an outcome Concomitant medications: "only one participant was on a stable dose of risperidone prior to the study and continued throughout the 8 wk of the study. No other participant was on concomitant medications." Previous medications: not reported |
|
| Interventions | Intervention (divalproex sodium) for 8 weeks: started
with 125 mg/day and was increased by 125 mg every 4
days during the first 2 weeks of treatment. The
recommended divalproex serum level was 50–100 mg/mL
by week 2, and the maximum dose was 30
mg/kg/day. Comparator (placebo) for 8 weeks: started with 125 mg/day and was increased by 125 mg every 4 days during the first 2 weeks of treatment. The recommended serum level was 50–100 mg/mL by week 2, and the maximum dose was 30 mg/kg/day. |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: tolerability Timing of outcome assessments: baseline, weeks 1, 2, 3, 4, 6, and 8 (endpoint) |
|
| Notes | Study start date: details not provided Study end date: details not provided Funding: "Funding was received from Abbott Laboratories as an investigator‐initiated study, the Seaver Foundation, and STAART Autism Center of Excellence Grant no. 5 U54 MH06673‐02". Conflicts of interest "Dr Hollander has served on an advisory board of Abbott Laboratories." Trial registry: NCT00211757 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The randomisation schedule had a goal of establishing a 2:1 ratio of patients in the active vs placebo groups |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Reported to be double‐blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | An unblinded person reported serum divalproex levels of < 50 mg/mL or > 100 mg/mL to the investigators so that the dose of study drug could be adjusted appropriately. In order to preserve the study blind, sham divalproex levels were reported for selected placebo participants. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear if > 13 were randomised and thus selective reporting. Quote: "Twenty‐five subjects were screened. Thirteen subjects were randomized, had at least one post‐treatment outcome measure, and were included in the intent‐to‐treat (ITT) group" |
| Selective reporting (reporting bias) | High risk | The CGI and ABC were reported as outcomes on trial registry however not reported in the paper. The primary outcome (CYBOCS) was reported graphically and using t‐scores. |
| Other bias | Low risk | No other sources identified |
Hollander 2006b.
| Study characteristics | ||
| Methods | Parallel trial of olanzapine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: details not provided Sample size: 11 in total, 6 olanzapine group, 5 placebo Number of withdrawals/dropouts: "one child dropped out right after randomization due to parental disagreement regarding study participation. Two others dropped out during the study because their parents were noncompliant with their follow up appointments." Gender: all were male in the olanzapine group, placebo 3/5 were male Mean age: olanzapine 9.25 years, placebo 8.9 years IQ: 2 in olanzapine group had severe intellectual disability, 5 participants had mild intellectual disability (2 and 3 in placebo), 4 had normal cognitive function (2 in each group) Baseline ABC‐I or other BoC: not applicable Concomitant medications: 0% History of previous medications: not reported |
|
| Interventions | Intervention (olanzapine) for 8 weeks: "in children
weighing less than 40kg, the dosage started with
2.5mg of olanzapine every other day; after 3 days,
the dose increased to 2.5mg every day. In children
weighing more than 40kg, the dose started at 2.5mg
every day and was increased to 5mg/day after 3 days/
Thereafter, the dosage for both weight groups was
increased in 5‐mg increments weekly to a maximum of
20mgday" Comparator (placebo) for 8 weeks: equivalent placebo |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: none reported Timing of outcome assessments: baseline, weekly for 1st 4 weeks then biweekly for last 4 weeks |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: "this study was supported by an investigator‐initiated research grant from Lilly Research Laboratories. Olanzapine and matching placebo were supplied by Lilly Research Laboratories" Conflicts of interest: "Dr Hollander serves on the advisory board of Abbott, Wyeth, Solvay, Somaxon Pharmaceuticals and receives research grants from Lilly, Abbott, Pfizer, UCB‐Pharma, and OrthoMcNeil Pharmaceuticals. All other authors have no financial relationships to disclose". Trial registry: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided except for, quote: "Patients were evaluated weekly for the first 4 weeks and biweekly for the next 4 weeks in a double‐blind fashion by the treating psychiatrist." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Paper reports that a secondary outcome is the Overt Aggression Scale irritability and aggression subscales however scores are not reported (only P values and z scores) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Available data from this relatively small sample of 11 participants (6 treatment and 5 control), we used mixed regression analysis to assess differences in the improvement ratings between the treatment and control groups. This analysis did not eliminate participants, but instead estimated effects using the data available for each participant. The reasons for missing data were children who discontinued the study before 8 weeks and missed treatment visits. |
| Selective reporting (reporting bias) | High risk | Quote: "The Overt Aggression Scale as listed as one of the outcome measures", however, "we did not find any evidence for significant change on the CYBOCS, the OAS‐M [Overt Aggression Scale‐Modified] irritability measure, or the OAS‐M [Overt Aggression Scale ‐ Modified] aggression measure". |
| Other bias | High risk | Both active treatment and placebo supplied by the same pharmaceutical company that financially supported the study |
Hollander 2010.
| Study characteristics | ||
| Methods | Parallel trial of divalproex sodium versus placebo | |
| Participants | Inclusion criteria: aged
Exclusion criteria:
Location/setting: not mentioned Sample size: 16 (intervention group), 11 (placebo group) Number of withdrawals/dropouts: placebo group 1 withdrawal; intervention group 1 withdrawal for lack of efficacy. Gender: 23 male, 4 female Mean age: 9.46 years IQ: placebo 76.1, intervention 52.92. Overall mean IQ 63.3 Baseline ABC‐I or other BoC: ABC‐I intervention group 20.3, placebo 22 Concomitant medications: 0% History of previous medications: details not provided |
|
| Interventions | Intervention (divalproex sodium) for 12 weeks:
started at 125 mg/day for children weighing up to 40
kg and titrated to a maximum of 250 mg twice/day
over 1 week. For children weighing ≥ 40 kg, the
starting dose was 250 mg/day and titrated to a
maximum of 500 mg twice/day over 1 week. Comparator (placebo) for 12 weeks: participants received a placebo comparative to the study drug divalproex sodium |
|
| Outcomes | Primary outcomes:
Secondary outcomes: tolerability Timing of outcome assessments: AEs recorded at baseline then weekly for 4 weeks then biweekly for next 4 weeks |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: funded by NINDS R21 NS4 3979‐01, E Hollander, PI. Grant no. M01‐RR00071 from the National Centre for Research Resources (NCRR) Conflicts of interest: "Eric Hollander received consultation fees from Abbott, Neuropharm, Nastech, BMS, and Forest; received research grants from Abbott, and UBS Pharma; and has intellectual property related to oxytocin and memantine and ASD. Evdokia Anagnostou received a consultation fee by InteGragen. The rest of the authors have nothing to disclose". Trial registry: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The children were randomised in a 1:1 fashion |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided except, quote: "all clinicians involved in efficacy or safety assessments were blinded to the randomisation condition", and "feedback on subjects randomised to placebo was based on a blocked schedule, so that all study clinicians remained blinded to the condition of randomisation." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Details not provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No direct mention of ITT methods to account for 3 participants who didn't complete intervention, however implied in the total number analysed |
| Selective reporting (reporting bias) | Low risk | Final ABC‐I scores were not provided however were on the clinicaltrials.gov website |
| Other bias | High risk | Quote: "adverse event monitoring took place every week for the first four weeks and every 2 weeks thereafter. Questions were focused on known side effects of divalproex sodium, followed by open‐ended questions." |
Hollander 2012.
| Study characteristics | ||
| Methods | Parallel trial of fluoxetine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: details not provided Sample size: 37 (fluoxetine 22, placebo 15) Number of withdrawals/dropouts: 2 dropouts did not comply with study procedures, 1 discontinued because of relocation, and 1 discontinued because of poor tolerability Gender: 26 male, 11 female Mean age: 34.31 years IQ: 103.25 Baseline ABC‐I or other BoC: not applicable Concomitant medications: 0% History of previous medications: not reported |
|
| Interventions | Intervention (fluoxetine) for 12 weeks: dosage
followed a fixed schedule, starting at 10 mg/day and
increasing, as tolerated, up to 80 mg/day; mean
final dose 9.9 mg/day Comparator (placebo) for 12 weeks: equivalent placebo |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: AEs were measured biweekly |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: "funded by Food and Drug Administration orphan product g rant FD‐R‐0 0 2 0 2 6 ‐0 1 and supported by Studies to Advance Autism Research and Treatment (STAART) Center of Excellence grant 1U5 4 MH‐ 0 6 6 6 7 3 from NIMH, by the Seaver Foundation, and by the Mount Sinai General Clinical Research Center. Mount Sinai School of Medicine licensed an orphan designation for fluoxetine in autism to Neuropharm, Ltd". Conflicts of interest: "Dr Hollander has been a consultant to Abbott, Forest, and Neuropharm in the past. Dr Anagnostou has consulted without fees to Neuropharm, Novartis, and Proximagen. The other authors report no financial relationships with commercial interests". Trial registry ‐ NCT00004486 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Loss to follow‐up by group not reported for all outcomes |
| Selective reporting (reporting bias) | High risk | ABC irritability data not reported |
| Other bias | High risk | Higher proportion of men (80%) in placebo group compared to fluoxetine group (64%); higher proportion who were white (86%) in the fluoxetine group compared to placebo group (53%); higher proportion had Asperger's (rather than ASD) (73%) in the fluoxetine group compared to placebo group (53%). No other differences in age, IQ, and baseline scores |
Hollander 2020a.
| Study characteristics | ||
| Methods | Cross‐over trial of Trichuris suis ova versus placebo | |
| Participants | Inclusion criteria: "age 18‐35, inclusive, at the
time of consent, Outpatient, meet criteria for the
diagnosis of Autism Spectrum Disorder according to
the DSM‐4‐TR, and supported by the ADOS or ADI‐R,
have an IQ of 70 or greater, participants who are
taking other medications prior to enrollment had to
be on a stable dose of concomitant medication,
including psychotropic, anticonvulsant, or sleep aid
for at least 3 months prior to baseline ratings.
Other inclusion criteria included being judged
reliable for medication compliance and agree to keep
appointments for study contacts and tests as
outlined in the protocol (both subjects and
guardians) and have a personal or family history of
allergies". Exclusion criteria
Location/setting: autism programme at Montefiore Medical Center, Albert Einstein College of Medicine, USA Sample size: 10 total (cross‐over) Number of withdrawals/ dropouts: none reported Gender: 9 male, 1 female Mean age: 21.15 years IQ: 87.89 Baseline ABC‐I or other BoC: parent‐rated ABC‐I 12.5 Concomitant medications: details not provided History of previous medications: details not provided |
|
| Interventions | Intervention (Trichuris suis ova) for 12
weeks: Trichuris suis ova were administered
in vials prepared by Coronado Biosciences. Vials
were diluted with a commercial drink and given to
participants orally to ingest. Participants received
a dose of 2500 ova every 2 weeks for 12 weeks. Comparator (placebo) for 12 weeks: placebo was administered on site every 2 weeks. |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessment: baseline and every 2 weeks for 12 weeks |
|
| Notes | Study start date: November 2012 Study end date: June 2014 Source of funding: funding provided by the Simons Foundation. Drug/placebo and consulting provided by Coronado Biosciences: "Coronado Biosciences also provided both TSO and the matching placebo". Conflicts of interest: none declared Trial registry: NCT01040221 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Other than "double‐blinded", details not provided |
| Incomplete outcome data (attrition bias) All outcomes | High risk | No dropouts were reported although only 9 were analysed for CGI scale |
| Selective reporting (reporting bias) | High risk | The ABC was apparently measured at baseline, 2, 4, 6, 8, 10, 12, 14, 16 weeks. Only pooled baseline and mean change from baseline to endpoint were reported |
| Other bias | High risk | No study results posted on ClinicalTrials.gov for this study even though it was completed July 2014. Active treatment prepared by pharmaceutical company |
Hollander 2020b.
| Study characteristics | ||
| Methods | 24‐week parallel trial of balovaptan versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria
Location/setting: 44 sites across the USA Sample size: 134 Number of withdrawals/dropouts: placebo, 26 dropped out (AEs (3); lack of efficacy (1); LTFU (3); physician decision (1); withdrawal by participant (18)). Balovaptan, unclear, groups are not clearly defined. Gender: 83% and 84% were male in the intervention and placebo groups respectively. Mean age: approximately 12 years in both groups IQ: not reported Baseline ABC‐I scores or other BoC: not reported Concomitant medications: not reported History of previous medications: not reported |
|
| Interventions | Intervention (balovaptan) for 24 weeks: participants
received age‐adjusted total daily oral dose
approximately equivalent to the adult dose of 10
mg/day of balovaptan (RO5285119). Approximate
treatment duration was up to 24 weeks (up to 52
additional weeks for those enroled in the open‐label
extension). Comparator: participants received a matching placebo orally. Approximate treatment duration was up to 24 weeks. |
|
| Outcomes | Primary outcomes: none reported Secondary outcomes: QoL (change from baseline) measured using the PedsQL (Varni 2001). Higher scores suggest a higher QoL Timing of outcome assessments: baseline, weeks 12 and 24 (endpoint) |
|
| Notes | Study start date: 2016 Study end date: 2020 Source of funding: F. Hoffmann‐La Roche Ltd (pharmaceutical company) Conflicts of interest: various grants and other support from pharmaceutical companies |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided apart from "randomised study" |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided apart from "Masking: Double (Participant, Investigator)" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Details not provided apart from "Masking: Double (Participant, Investigator)" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Difficult to understand participant flow |
| Selective reporting (reporting bias) | High risk | The paper/presentation mentions the ABC‐Irritability however, it wasn't reported and was not listed on the trial registry. Also, the study was "Terminated (The 24‐week analysis indicated no clinical or statistical benefit for the primary endpoint for the overall study population. No new safety concerns identified.)" |
| Other bias | High risk | List of disclosures included payment by pharma company, for many of the study authors |
Ichikawa 2017.
| Study characteristics | ||
| Methods | 8‐week parallel trial of aripiprazole versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: 50 sites in Japan Sample size: 47 aripiprazole, 45 placebo Number of withdrawals/dropouts: 3 from placebo discontinued, 1 due to AEs and 2 due to a physician decision Gender: 75 male, 17 female Mean age: approx 10 years IQ: approximately 35% in both groups had mild intellectual disability, 15% had moderate intellectual disability, and 13% had severe intellectual disability Baseline ABC‐I or other BoC: aripiprazole ABC‐I 27.1 (7.2); placebo 26.8 (6.5) Concomitant medications: concomitant psychotropic medications were not permitted during the trial. History of previous medications: not provided |
|
| Interventions | Intervention: aripiprazole was initiated at 1 mg/day,
with a target dosage of 1, 3, 6, 9, 12, or 15
mg/day Placebo: equivalent placebo once daily for 8 weeks |
|
| Outcomes | Primary outcomes:
Secondary outcomes: tolerability |
|
| Notes | Study start date: June 2012 Study end date: June 2015 Funding: "This study was funded by Otsuka Pharmaceutical Co, Ltd (Tokyo, Japan)" Conflicts of interest: various authors received funding and other support from pharmaceutical companies. Trial registry: NCT01617447 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information on method of generating this sequence |
| Allocation concealment (selection bias) | Low risk | Quote: "Clinicians were required to input information regarding eligible patients on the Interactive Web Response System (IWRS), and then the registration center assigned a trial drug code to each patient" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Double‐blind ‐ doesn't specify exactly who was blind |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Double‐blind ‐ doesn't specify exactly who was blind |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition was low and all participants were accounted for. |
| Selective reporting (reporting bias) | Low risk | The trial registry reports that the ABC‐Irritability and AEs were outcomes. Both of these were reported in full. |
| Other bias | High risk | A pharmaceutical company funded the study and 2 of the study authors are employees of the pharma company. |
Jacob 2022.
| Study characteristics | ||
| Methods | 24‐week parallel trial of balovaptan versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: 46 sites across 6 countries (the USA, the UK, France, Italy, Spain, and Canada) Sample size: 321 (balovaptan group 163; placebo group 158) Number of withdrawals/dropouts:
Gender: 64 females, 257 males Mean age: 27.6 years IQ: approx 105 Baseline ABC‐I scores or other BoC: Concomitant medications: details not provided History of previous medications: details not provided |
|
| Interventions | Intervention: 10 mg of oral balovaptan once daily for
24 weeks Comparator: equivalent placebo for 24 weeks |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: QoL, measured using the PedsQL, (Varni 2001) Timing of outcome assessments: AEs week 24 (endpoint); QoL: baseline, week 12 and 24 (endpoint) |
|
| Notes | Study start date: August 2018 Study end date: July 2020 Source of funding: Pharmaceutical company (Hoffmann‐La Roche) Conflicts of interest: |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly allocated (1:1) to receive balovaptan or placebo with an independent interactive voice or web‐based response system (IxRS) using permuted blocks of four. Knowledge of block size was controlled to avoid randomisation predictability. Sites enroling a participant entered the participant’s data in the IxRS, and the system assigned the participant to a trial group according to the allocation sequence. The randomisation provider was Signant Health; the sponsor did not have access to the live allocation sequence while the study was ongoing. |
| Allocation concealment (selection bias) | Low risk | Participants were randomly allocated (1:1) to receive balovaptan or placebo with an independent interactive voice or web‐based response system (IxRS) using permuted blocks of four. Knowledge of block size was controlled to avoid randomisation predictability. Sites enroling a participant entered the participant’s data in the IxRS, and the system assigned the participant to a trial group according to the allocation sequence. The randomisation provider was Signant Health; the sponsor did not have access to the live allocation sequence while the study was ongoing. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Apart from "Participants, study site personnel, and the sponsor were masked to treatment assignment" no further details were provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Apart from "Participants, study site personnel, and the sponsor were masked to treatment assignment" no further details were provided. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Over half of all dropouts in both groups were "terminated by the sponsor". |
| Selective reporting (reporting bias) | Unclear risk | It appears that all outcomes listed on trial registry were reported however, with the early termination it is unclear if other factors contributed to the study terminating (especially with the involvement of the sponsor). |
| Other bias | High risk | The funder of the study had a role in study design, data collection, data analysis, data interpretation, and writing of the report. |
Jaselskis 1992.
| Study characteristics | ||
| Methods | Cross‐over trial of clonidine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: outpatients clinic, USA Sample size: 8 in total (cross‐over) Number of withdrawals/dropouts:none reported Gender: 8 male Mean age: 8.1 years IQ: 59 Baseline ABC‐I or other BoC: none reported Concomitant medications: 0% History of previous medications: medications were not allowed in the month prior to the study. |
|
| Interventions | Intervention (clonidine) for 6 weeks: clonidine was
provided at 0.025 mg strength. Clonidine was tapered
up over 2 weeks to a dose of 4‐10 ug/kg/day
(0.15‐0.20 mg/day) in 3 doses per day. Comparator (placebo) for 6 weeks: identical placebo tablets were provided in a 0.025 mg strength. Placebo was tapered up over 2 weeks to a dose of 4‐10 ug/kg per day (0.15‐0.20 mg/day) in 3 doses per day. |
|
| Outcomes | Primary outcomes: irritability, measured using the
ABC‐I subscale (Aman 1985) Secondary outcomes: none reported Timing of outcome assessment: ABC‐I rated weekly by teachers; AEs recorded weekly however not reported |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: "supported in part by the Harris Center for Developmental Studies (Chicago, IL) and National Institute of Mental Health Child and Adolescent Mental Health Academic Award K07 MH00822 (to E.C.)" … "Catapres and matched placebo tablets were provided as a gift from Boehringer Ingelheim Pharmaceuticals Inc. (Ridgefield, CT)". Conflicts of interest: none declared Trial registry: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided except for, quote: "The subjects were randomly assigned by a non‐rating clinician whose only clinical contact with patients and parents occurred during the diagnostic phase and after the completion of the study for each patient." |
| Allocation concealment (selection bias) | Unclear risk | "Tablets were placed in sealed envelopes designated for each day of the study" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "All raters (parents, teachers and clinicians) were blind to drug order until ratings were completed" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "all raters (parents, teachers, and clinicians) were blind to drug order until ratings were completed" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only 8 participants were analysed in the trial and individual data were not recorded. |
| Selective reporting (reporting bias) | High risk | No baseline scores were recorded despite "three sessions that were done at baseline". "Clinician ratings were only made at the end of each treatment period" and "none of the clinician ratings showed significant differences between placebo and clonidine" and "weekly teacher ratings included the Abberant Behaviour Checklist". Side effects were monitored weekly however not reported. |
| Other bias | High risk | Quote: "clonidine and identical placebo tablets were provided...by Boehringer Ingelheim Pharmaceuticals, Inc" |
Kent 2013.
| Study characteristics | ||
| Methods | Parallel trial of risperidone versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Setting: multicenter study including "16 clinical and investigative settings", USA Sample size: 66 (risperidone 31, placebo 35) Number of withdrawals/dropouts: placebo 8 (AE 0, LTFU 0, withdrew consent 1, insufficient response 6, medication noncompliance 1, other 0). Risperidone 6 (AE 1, LTFU 1, withdrew consent 3, insufficient response 0, medication noncompliance 0, other 1) Gender: placebo 31 male, 4 female; risperidone 28 male, 3 female Mean age: all were aged under 18 years IQ: not reported Baseline ABC‐I or other BoC: ABC‐I risperidone 28.0; placebo 28.9 Concomitant medications: participants were not allowed to be taking psychotropic medications for at least 1 week before baseline. Anticholinergics and antihistamines for the treatment of emergent extrapyramidal symptoms were restricted to the lowest dose and for the shortest duration possible. Similarly, hypnotic or sedative medications (lorazepam, 0.25–2 mg; or diphenhydramine up to 50 mg) were allowed if the patient had been stable on a particular dose for at least 30 days before study start. Antihistaminic drugs were the most commonly used concomitant medication; a higher percentage of participants in placebo (20%; n = 7) than risperidone group 3%, n = 1) were treated with these drugs. History of previous medications: not reported |
|
| Interventions | Intervention (risperidone) for 6 weeks: 1.25 mg/day
children < 45 kg; or 1.75 mg/day children > 45
kg Comparator (placebo) for 6 weeks: placebo oral solution for 6 weeks |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessment: baseline and the 6 weeks (endpoint) |
|
| Notes | Study start date: December 2007 Study end date: March 2010 Source of funding: Johnson & Johnson Pharmaceutical Research & Development, LLC Conflicts of interest: "Dr Aman was an investigator for this study and has received research support or been a consultant for Janssen Research & Development, LLC, Bristol‐Myers Squibb, Pfizer, Forest Research, and Hoffman La Roche. Drs. Ness, Singh, Hough and Kent and Mr. Karcher are employees of Janssen Research & Development, LLC. Drs Ning and Kushner were employed by Janssen Research & Development, LLC during the design and conduct of this study. Dr Ning is currently employed by Purdue Pharma and Dr Kushner is at CFG Health Systems, LLC. All authors met ICMJE criteria and all those who fulfilled those criteria are listed as authors". Trial registry" NCT00576732 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "the randomisation was conducted by using randomly permuted blocks and was stratified by centre and baseline weight" |
| Allocation concealment (selection bias) | Low risk | Quote: "To maintain blinding, the study drugs supplied were identical in appearance and packed in identical child‐resistant containers." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "Patients, parents or primary caregivers, and the site personnel were all blinded to treatment assignment." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not mentioned apart from "site personnel were all blinded" |
| Incomplete outcome data (attrition bias) All outcomes | High risk |
|
| Selective reporting (reporting bias) | Unclear risk | All outcomes mentioned were reported however without a trial protocol it is difficult to know if other outcomes were originally measured but not reported. Data were collected at 4 days, and weeks 1, 2, 4 and 6, or at the time of early withdrawal but only endpoint data were reported. |
| Other bias | Unclear risk | Participants were recruited from the investigators' practices There were no apparent differences in age, gender, race, BMI, diagnosis, symptoms or baseline scores. |
Khalaj 2018.
| Study characteristics | ||
| Methods | 10‐week parallel trial of palmitoylethanolamide versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: 2 Children's Outpatient Clinics at tertiary hospitals in Iran Sample size: 70 (35 each group) Number analysed: risperidone plus palmitoylethanolamide (n = 31), risperidone plus placebo (n = 31) Number of withdrawals/dropouts: risperidone plus palmitoylethanolamide (n = 4), risperidone plus placebo (n = 4). No reasons reported Gender: 47 male, 15 female Mean age: 6.84 (2.1); placebo 7.42 (2.35) years IQ: details not provided Baseline ABC‐I or other BoC: ABC‐I intervention group 21.97 (5.06); placebo 20.97 (6.8) Concomitant medications: only children who were drug‐free for at least 6 weeks before beginning of the study due to other reasons (discontinuation of drugs by their parents) were included. History of previous medications: details not provided |
|
| Interventions | Intervention (palmitoylethanolamide + risperidone):
participants in both groups similarly received
risperidone. It was started with an initial dose of
0.5 mg and stepwise 0.5 mg weekly increases for the
first 3 weeks were implemented. Maximum dose of
risperidone was 1 mg/d for children weighing < 20
kg and 2 mg/d for those with a body weight ≥ 20 kg.
Additionally, individuals were administered 600 mg
palmitoylethanolamide twice daily for 10 weeks. Comparator (placebo + risperidone): risperidone was started with an initial dose of 0.5 mg and stepwise 0.5 mg weekly increases for the first 3 weeks were implemented. Maximum dose of risperidone was 1 mg/d for children weighing < 20 kg and 2 mg/d for those with a body weight ≥ 20 kg. Additionally, individuals were administered 600 mg of placebo twice daily for 10 weeks. |
|
| Outcomes | Primary outcomes:
Secondary outcomes: tolerability |
|
| Notes | Study start date: February 2017 Study end date: October 2017 Funding: this study was funded by Tehran University of Medical Sciences and Health Services (grant number 33135). Conflicts of interest: "Authors declare no conflict of interest" Trial registry: IRCT201702171556N96 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear if random number generator or quasi Quote: "Randomization was performed by a radomization operator who was not otherwise involved in this trial" |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomization was performed by a radomization operator who was not otherwise involved in this trial." "Randomization codes were kept secure until data curation was completed." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind; participants and their parents were blinded to group allocations. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blind ; participants and their parents were blinded to group allocations. "Randomization codes were kept secure until data curation was completed" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Reason for withdrawals not described |
| Selective reporting (reporting bias) | Unclear risk | Difficult to know without a protocol |
| Other bias | High risk |
|
King 2001.
| Study characteristics | ||
| Methods | Parallel trial of amantadine hydrochloride versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: 6 university medical centres, USA Sample size: 19 amantadine hydrochloride, 20 placebo Number of withdrawals/dropouts: none post‐randomisation Gender: amantadine: 15/19 male; placebo: 19/20 male Mean age: 7 years IQ: > 35 Baseline ABC‐I or other BoC: ABC‐I amantadine 19.1; ABC‐I placebo 18.7 Concomitant medications: SSRIs ("provided the dose had been stable for greater than 1 month prior to entry, and the dose did not change during the study period") amantadine group: 4/19; placebo 6/20 History of previous medications: not reported |
|
| Interventions | Intervention (amantadine hydrochloride) for 5 weeks:
after a week‐long placebo baseline phase, amantadine
hydrochloride was started at 2.5 mg/kg once/day for
first week of active treatment. "For each of the
three remaining weeks of the treatment phase,
amantadine hydrochloride as two doses of 0.25 mL/kg
(i.e., 5 mg/kg per day)" Comparator (placebo) for 5 weeks: "taste and color‐matched placebo was started as 0.25 mL/kg per day for a week during baseline phase. During the first week of the treatment phase, under double‐blind conditions, subjects received placebo at a single dose of 0.25 mL/kg per day. For each of the three remaining weeks, the subject was given placebo as two doses of 0.25 mL/kg (i.e., 0.5 mL/kg per day)". |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: none reported Timing of outcome assessments: screening, baseline start of the week, baseline end of the week, visits in weeks 2, 3, 4, 5 |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: "funded by Cerebrus plc, Winnersh, UK" Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided except, "Treatment allocation was randomized and supplied in a blind manner" |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Details not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants were accounted for and included in the analysis. The only participants who withdrew from the study did so before randomisation. |
| Selective reporting (reporting bias) | High risk | ABC‐I endpoint scores not reported |
| Other bias | Unclear risk | Study was funded by Cerebus plc ‐ unclear parameters around this funding. No significant differences in age, gender, weight, race, concomitant SSRI, CGI‐rated illness severity, ABC irritability and hyperactivity scores at baseline |
King 2009.
| Study characteristics | ||
| Methods | Parallel trial of citalopram versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria: details not provided Location/setting: s6 academic medical centres in the USA Sample size: 149 (73 children were randomised to citalopram and 76 to placebo) Number of withdrawals/dropouts: placebo: 13 withdrew (7 AEs, 1 protocol violation, 5 withdrew consent) Citalopram hydrobromide: 13 withdrew (1 serious AE, 8 AEs, 2 protocol violations, 2 withdrew consent) Mean age: 9.4 years Gender: 128/149 boys IQ: 43% had nonverbal IQ > 70 Baseline ABC‐I or other BoC: citalopram ABC‐I 13.2; placebo 11.2; self‐injurious behaviour 2.8 (citalopram); 2.6 (placebo) Concomitant medications: psychotropic medication not allowed during the study. Only sleep medications allowed History of previous medications: details not provided |
|
| Interventions | Intervention (citalopram hydrobromide) for 12 weeks:
10 mg/5 mL. Mean maximum dose was 16.5 mg/day (± 6.5
mg) Comparator (placebo) for 12 weeks: equivalent placebo |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: AEs assessed at bi‐weekly visits; ABC‐I and self‐injury measured at baseline and endpoint |
|
| Notes | Study start date: April 2004 Study end date: October 2006 Source of funding: all authors received salary contributions from the National Institutes of Health, which supported this study. Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomly assigned to citalopram or placebo using permuted blocks with randomly varying block sizes stratified by site and by age (5‐11 vs 12‐17 years) |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Two masked clinicians met with participants during each scheduled evaluation |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The evaluating clinician monitored efficacy and was blinded to AEs |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | LTFU citalopram: 13 withdrew, 1 due to serious AE; 8
AEs; 2 protocol violations; 2 consent withdrawn LTFU placebo: 13 withdrawn, 7 AEs; 1 protocol violation; 5 consent withdrawn |
| Selective reporting (reporting bias) | Low risk | The trial protocol was recorded on Clinicaltrials.gov and outcomes were reported in the paper. |
| Other bias | High risk | Study authors all work with/for pharmaceutical companies |
Klaiman 2013.
| Study characteristics | ||
| Methods | Parallel trial of tetrahydrobiopterin versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: Children’s Health Council in Palo Alto, California, USA Sample size: 46 (23 in both groups) Number of withdrawals/dropouts: tetrahydrobiopterin (BH4) AEs (2) and lack of efficacy (1), placebo lack of efficacy (1) Gender: tetrahydrobiopterin (BH4) 20 male, 3 female, 18 male, 5 female Mean age: 5 years IQ: not reported Baseline ABC‐I or other BoC: ABC‐I BH4 11.1, placebo 11.9 Concomitant medications: participants could not have been taking psychotropic drugs in 6 months prior to trial and not start any new medications during the trial. History of previous medications: not reported |
|
| Interventions | Intervention (tetrahydrobiopterin) for 16 weeks:
"individual doses of BH4 were prescribed in tablet
form at 20mg/kg of body weight and taken once daily.
The form of BH4 prescribed was given as
tetrahydrobiopterin dihydrochloride. "The mean dose
of BH4 at endpoint was 385mg/day or 19mg/kg/day" Comparator (placebo) for 16 weeks: matching placebo |
|
| Outcomes | Primary outcomes:
Secondary outcomes: tolerability Timing of outcome assessments: baseline, week 8 and week 16 (endpoint) |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: "study drugs and matching placebo were provided by BioMarin Pharmaceutical, Inc" Conflicts of interest: none declared Trial registry: NCT00850070 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Group assignment was generated by a randomization program on Microsoft Excel" |
| Allocation concealment (selection bias) | Low risk | One member of the research team (LH) was responsible for all randomisation; randomisation records were kept on a password‐protected computer in a locked office. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | BH4 and placebo were supplied by the pharmacist as matching pills in identical packaging. "Participants, parents, and evaluators (GRE and CK) responsible for assessing the children all were blind to assignment; they remained blind until the final participant completed the trial." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Participants, parents, and evaluators (GRE and CK) responsible for assessing the children all were blind to assignment; they remained blind until the final participant completed the trial." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants were included in the analysis and an ITT analysis was used, including using LOCF. All outcomes were reported in full. |
| Selective reporting (reporting bias) | Low risk | All measures were reported in full. |
| Other bias | High risk | This research was funded by BioMarin Pharmaceutical, Inc. as an investigator‐initiated study (#CHC0901). |
Le 2022.
| Study characteristics | ||
| Methods | 6 week cross‐over trial of oxytocin versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: China Sample size: 41 (21 oxytocin, 20 placebo) Number of withdrawals/dropouts: none were lost to follow‐up in the first phase of the cross‐over trial Gender: male (38), female (3) Mean age: 5.0 years across both groups IQ: not reported Baseline ABC‐I or other BoC scores: not an outcome Concurrent medications: details not provided History of previous medications: details not provided |
|
| Interventions | Intervention (oxytocin) followed by placebo: oxytocin
nasal spray 24 IU every 2nd day for 6 weeks,
followed by a 2‐week wash‐out period before starting
the 2nd phase of the cross‐over trial Comparator (placebo) followed by oxytocin: equivalent placebo (24 IU) every 2nd day for 6 weeks, followed by a 2‐week wash‐out period before starting the 2nd phase of the cross‐over trial |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: not reported Timing of outcome assessments: unclear |
|
| Notes | Source of funding: University of Electronic Science
and Technology of China, UESTC high‐level research
fostering project Conflicts of interest: "The authors have no conflicts of interest to declare" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 1:1 computer‐generated randomisation |
| Allocation concealment (selection bias) | Unclear risk | Intranasal spay bottles for oxytocin or placebo were identical in appearance and labelling with each having a unique code. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Intranasal spray bottles were labelled and distributed to carers by an individual not involved in any other aspect of the trial who was responsible for finally unmasking the treatment details at the end of the trial. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Intranasal spray bottles were labelled and distributed to carers by an individual not involved in any other aspect of the trial who was responsible for finally unmasking the treatment details at the end of the trial. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1 of 21 LTFU in oxytocin group and 1 in 22 in placebo group |
| Selective reporting (reporting bias) | Unclear risk | There were no serious AEs in either group but the only other AE that was reported was urination frequency. |
| Other bias | Low risk | No differences in age, gender, baseline scores of autism subtype |
Lemonnier 2017.
| Study characteristics | ||
| Methods | 3‐month parallel trial of bumetanide versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: France; the patients were enroled in six French specialised centres (hospitals of Brest, Limoges, Rouen, Nice, Lyon and Marseilles) Mean IQ: details not provided Mean age: 7.8 ± 4.1 (0.5 mg), 7.9 ± 4.6 (1.0 mg), 8.4 ± 4.6 (2.0 mg) and 8.8 ± 4.5 (placebo) Gender: 78 male, 10 female Sample size: 88 Reasons for dropouts: 0.5 mg ‐ no LTFU reported, 1.0 mg ‐ 3 AEs and 1 LTFU, 2.0 mg ‐ 6 AEs, 3 LTFU; placebo ‐ 1 AE, 2 LTFU Baseline ABC‐I or other BoC scale: not an outcome Timing of outcome assessments: end of month 4 Concomitant medications: psychotropic medications (including antipsychotic, psychostimulant, antidepressant, anxiolytics, mood stabilisers and neuroleptic agents) had to be discontinued at least 4 weeks before entering the trial Previous medications: not reported |
|
| Interventions | Intervention (bumetanide) 0.5 mg, 1 mg or 2 mg twice
daily for 90 days Comparator: equivalent placebo for 90 days |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: tolerability |
|
| Notes | Study start date: January 2014 Study end date: March 2015 Funding: "The study was sponsored by Neurochlore, a biotech company dedicated to the development of novel therapies to autism and other developmental disorders'. 'Funding of the trial comes from an investment of Symmetry Capital, a grant from France's Agence Nationale de la Recherche (ANR‐12‐ RPIB‐0001‐01) and French Government loans". Conflicts of interest: "Three of the authors are founders and shareholders of the company funding the study. The remaining authors declare no conflicts of interest" Trial registry: NCT01078714 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated age‐stratified randomisation schedule prepared by Amatsi group used |
| Allocation concealment (selection bias) | Unclear risk | No information beyond "randomised" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Double‐blinded ‐ no further details provided |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Each patient was seen and assessed by two clinicians who were unaware of the treatment assignment. Quote "Finally, the diuretic actions of bumetanide also impact the blinding procedure. To reduce this impact, the psychiatrist was separated from the pediatrician who treated the children and was thus blinded to the treatment." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | LTFU participants included in final analyses |
| Selective reporting (reporting bias) | Unclear risk | Protocol not published |
| Other bias | High risk | Quote: "The study was sponsored by Neurochlore, a biotech company dedicated to the development of novel therapies to autism and other developmental disorders. EL, DR and YB‐A are founders and shareholders of the company" |
Levy 2003.
| Study characteristics | ||
| Methods | Cross‐over trial of single‐dose secretin versus single‐dose placebo | |
| Participants | Inclusion criteria: diagnosis of ASD confirmed using
the ADI‐R. No other inclusion criteria outlined Exclusion criteria:
Location/setting: Children's Hospital of Philadelphia, USA Sample size: 62 total (31 in each group) Number of withdrawals/dropouts: 2 participants dropped out post‐randomisation however reasons were not provided Gender: all participants were male Mean age: secretin 6.4 years; placebo 5.9 years. IQ: not reported Baseline ABC‐I or other behaviours of concern: RFRLRS (subscale3) 0.74 (secretin), 0.64 (placebo). Concomitant medications: 7/31 (secretin) were on either prozac (1), Adderall (2), guanfacine (2), methylphenidate (2). Placebo: either prozac, guanfacine or risperidone with 1 child taking prozac and guanfacine History of previous medications: not reported |
|
| Interventions | Intervention (single‐dose secretin)with 6‐week
washout before placebo (or vice versa): single
intravenous dose of human secretin (2 CU/kg).
Initially, a test dose of 0.2 uh was given and if no
reaction was noted after 1 min, the remaining dose
of 2 CU/kg up to a maximum of 75 CU was injected
slowly over 1 min Comparator (placebo): single intravenous dose of saline placebo (2 CU/kg) |
|
| Outcomes | Primary outcomes: irritability, measured using the
RFRLRS Affectual Responses subscale (Freeman 1986);
adverse effects although data were not reported for
both groups and so could not be included. Secondary outcomes: none reported Timing of outcome assessments: baseline, 2 and 4 weeks postinfusion |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: ChiRhoClin Corporation donated the human secretin used for the study. Otherwise, sponsorship was through research grants. Conflicts of interest: none declared Trial registry: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "the 62 subjects were randomly assigned to two groups using a computerised randomisation assignment" |
| Allocation concealment (selection bias) | Unclear risk | Details were not provided on how the placebo was administered. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Each participant was separated from his or her parents during the infusion (since secretin may cause a transient skin rash—the presence of which may unblind the parent to the treatment condition). |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All personnel involved in clinical and neurodevelopmental assessments were blinded to subject's allocation" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 2 participants did not complete both phases of the trial (1 in each group) however reasons were not provided and information not given if an ITT analysis was used or LOCF |
| Selective reporting (reporting bias) | Low risk | The outcome measures were the Global Behavior Rating Scale, Communication and Symbolic Behavior Scale and the Real Life Ritvo Behavior Scale. All outcomes were reported at baseline and at the end of each phase of the cross‐over trial. |
| Other bias | Unclear risk | "ChiRhoClin Corporation donated the human synthetic secretin used for the study". Only a single dose of secretin was used |
Lewis 2018.
| Study characteristics | ||
| Methods | 3‐week cross‐over trial of nicotine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/ setting: Yale Child Study Center in New Haven, CT, USA Sample size: 8 in total Reason for dropouts: 1 participant did not complete the first phase of the trial because of a protocol violation. Mean age: 21 years Mean IQ: not reported Gender: 7 male, 1 female Baseline ABC‐I or other BoC scale: 25.0 (8.0) Concomitant medications: divalproex (3), risperidone (4), desipramine (1), methylphenidate (1), clonidine (2), lamotrigine (1), buspirone (1), olanzapine (1), aripiprazole (1), fluoxetine (1), clonazepam (1), propranol (1), gabapentin (1) Previous medications: not reported |
|
| Interventions | Intervention: skin patches containing 7 mg of
nicotine were applied for 7 days with a washout
period of 7 days between each phase Comparator: skin patches containing 7 mg of placebo were applied for 7 days |
|
| Outcomes | Primary outcomes: ABC‐I (Aman 1985) Secondary outcomes: none reported Timing of outcome assessments: baseline, completion of weeks 1 and 3 |
|
| Notes | Study start date: May 2015 Study end date: November 2017 Funding: "This work was supported by Autism Speaks grant #9699, National Institutes of Health grants R01DA14241, R01MH077681, R25MH071584, T32MH019961, and T32MH14276, and the Yale Child Study Center Associates and the AACAP Pilot Award for General Psychiatry Residents". Conflicts of interest: "The authors declare no conflicts of interest". Trial registry: NCT02552147 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details on sequence generation beyond, "Randomization and preparation of patches was performed by the Yale Investigational Drug Service." |
| Allocation concealment (selection bias) | Unclear risk | No details on allocation concealment beyond "Randomization and preparation of patches was performed by the Yale Investigational Drug Service" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No details apart from double‐blind |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details apart from double‐blind |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Large % of people missing data for primary outcome |
| Selective reporting (reporting bias) | High risk | Doesn't report State‐Trait Anxiety Inventory, State‐Trait Anger Expression Inventory‐2 etc |
| Other bias | Unclear risk | Early stoppage of trial before sample size reached |
Loebel 2016.
| Study characteristics | ||
| Methods | 6‐week, double‐blind RCT, parallel trial of lurasidone (20 mg/day or 60 mg/day) versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: not reported Sample size: 148 (lurasidone 60 mg/day 51, 20 mg/day lurasidone 48, placebo 49) Number of withdrawals/dropouts: placebo: lack of efficacy (1), AEs (4), lost to follow‐up (1), withdrew consent (4); lurasidone 60 mg/day: lack of efficacy (1), AEs (2), miscellaneous (1); lurasidone 20 mg/day: AEs (2), lack of efficacy (1), lost to follow‐up (2), withdrawal by participant (1) Gender: placebo 40/49 male, lurasidone 60 mg/day 43/51 male, lurasidone 20 mg/day 38/48 male Mean age: placebo 11 years, lurasidone 20 mg/day 10.5 years, lurasidone 60 mg/day 10.5 years IQ: not reported Baseline ABC‐I or other BoC: irritability, placebo 29.0, lurasidone 60 mg/day 27.0 Concurrent medications: not reported History of previous medications: any antipsychotic: placebo 19/49, lurasidone 20 mg/day 17/48, lurasidone 60 mg/day 16/51. Any psychostimulant: placebo 18/49, lurasidone 20 mg/day 11/48, lurasidone 60 mg/day 16/51. Any antidepressant: placebo 6/49, lurasidone 60 mg/day 5/51 |
|
| Interventions | Intervention 1 (lurasidone 60 mg/day) for 6 weeks:
study participants randomised to the 60
mg/day arm received lurasidone 20 mg/day from days
1–3, 40 mg/day from days 4–6, and 60 mg/day from day
7 to week 6. If the participant was not able to
tolerate the 60 mg/day dose, a one‐time dose
reduction to 40 mg/day was permitted (between days 8
and 29); the 40 mg/day dose was then maintained for
the remainder of the study. Intervention 2 (lurasidone 20 mg/day) for 6 weeks: mean of 0.476 mg/kg/day Comparator (placebo) for 6 weeks: matching placebo |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: weekly |
|
| Notes | Study start date: August 2013 Study end date: November 2014 Source of funding: researchers were employed by Sunovion Pharmaceuticals. Conflicts of interest: "Drs Loebel, Goldman, Silva, Hernandez, Mankoski, and Deng are employees of Sunovion Pharmaceuticals Inc. Dr Brams has been a speaker, consultant, and served on advisory boards for Novartis Pharmaceuticals Corp and Shire; and has received grant‐research support from Novartis Pharmaceuticals Corp, Shire, and Eli Lilly. Dr Findling receives or has received research support, acted as a consultant and/or served on a speaker’s bureau for Alcobra, American Academy of Child & Adolescent Psychiatry, American Physician Institute, American Psychiatric Press, AstraZeneca, Bracket, Bristol‐Myers Squibb, CogCubed, Cognition Group, Coronado Biosciences, Dana Foundation, Elsevier, Forest, GlaxoSmithKline, Guilford Press, Johns Hopkins University Press Johnson and Johnson, Jubilant Clinsys, KemPharm, Lilly, Lundbeck, Merck, NIH, Neurim, Novartis, Noven, Otsuka, Oxford University Press, Pfizer, Physicians Postgraduate Press, Purdue, Rhodes Pharmaceuticals, Roche, Sage, Shire, Sunovion, Supernus Pharmaceuticals, Transcept Pharmaceuticals, Validus, and WebMD". Trial registry: NCT01911442 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised via an interactive voice/web response system |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Double‐blinding although details not explicitly provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Double‐blinding although details not explicitly provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The ITT population consisted of randomised study participants who received at least 1 dose of study medication and had at least 1 postbaseline efficacy assessment. |
| Selective reporting (reporting bias) | Low risk | The trial was registered on clinicaltrials.gov and all outcomes were reported. |
| Other bias | High risk | "The sponsor was involved in the design, collection, and analysis of the data." "Drs. Loebel, Goldman, Silva, Hernandez, Mankoski, and Deng are employees of Sunovion Pharmaceuticals Inc." |
Luby 2006.
| Study characteristics | ||
| Methods | Parallel trial of risperidone versus placebo | |
| Participants | Inclusion criteria:
Exclusions:
Location/setting: "psychiatric outpatient clinic at Washington University School of Medicine", USA Sample size: 23 (11 risperidone, 12 placebo) Number of withdrawals/dropouts: 1 exclusion from risperidone group as the "child did not meet the threshold for an ASD on the CARS or GARS [Gilliam Autism Rating Scale] at baseline, despite having been referred with a clinical diagnosis, and was excluded from analyses". 1 dropout from placebo group due to parent report of severe hyperactivity Gender: risperidone 9/11 male, placebo 8/12 male Mean age: risperidone 4.1 years, placebo 4 years IQ: not reported Baseline ABC‐I or other BoC: not an outcome Concomitant medications: not reported History of previous medications: not reported. |
|
| Interventions | Intervention (risperidone) for 6 months: the majority
of participants started risperidone at 0.5 mg once
daily; mean starting dose was 0.03 mg/kg/day. 81.8%
of risperidone participants took 1 mg (0.5 mg twice
daily) after 4 weeks; 27.3% of risperidone
participants were dispensed total daily doses of 1.5
mg after 8 weeks, whereas all others received total
daily doses of 1 mg. The final risperidone mean dose
was 0.05 mg/kg/day and mean daily final dose was
1.14 mg (SD 0.32). Comparator (placebo) for 6 months: placebo participants were dispensed 0.5 mg daily doses. Mean final daily dose was 1.38 mg (0.57), which was comparable to risperidone. |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: none reported Timing of outcome assessments: at baseline visit, weekly visits during the 1st study month, biweekly visits during the 2nd month, followed by monthly visits for months 3–6 |
|
| Notes | Study start date: November 1999 Study end date: November 2002 Source of funding: "this study was funded by Janssen Pharmaceutica as an investigator initiated project to Dr. Luby". Conflicts of interest: none disclosed Trial registry: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Patients were consecutively assigned by an unblinded child psychiatrist (J.L) to risperidone or placebo treatment using a randomisation table obtained from the WUSM pharmacy and derived using a standard software package |
| Allocation concealment (selection bias) | High risk | Quote: "Patients were consecutively assigned by an unblinded child psychiatrist" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Parents and raters who conducted all standardized assessments were blind to treatment group" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Parents and raters who conducted all standardized assessments were blind to treatment group" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants, apart from one who did not meet the
required baseline threshold for ASD on the CARS or
Gilliam Autism Rating Scale, were included in the
analysis. LTFU: 1 participant withdrew from placebo group due to staring spells. No other LTFU reported |
| Selective reporting (reporting bias) | High risk | All children were previously diagnosed and referred by a clinician. "the treating psychiatrist (J.L) was unblinded and conducted regular clinical assessments over the 6‐month period". The unblinded child psychiatrist was also the lead investigator. |
| Other bias | High risk | All children were previously diagnosed and referred by a clinician. "the treating psychiatrist (J.L) was unblinded and conducted regular clinical assessments over the 6‐month period". The unblinded child psychiatrist was also the lead investigator. |
Mace 2001.
| Study characteristics | ||
| Methods | Parallel trial of haloperidol versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: inpatient unit in the USA Sample size: 7 in total who had autism Number of withdrawals/dropouts: none reported Gender: 3 male, 4 female Mean age: 11 years IQ: details not reported Baseline ABC‐I or other BoC: self‐injurious behaviour per hour at baseline, haloperidol 125; placebo 146.4 Concomitant medications: participants were not permitted to take psychotropic medications during the trial. History of previous medications: "participants were taking zero to three psychotropic medications upon admission to the inpatient unit. These medications were discontinued before completion of the functional analysis (except for Subjects 5 and 9), and individuals remained off these medications throughout the remainder of the study." |
|
| Interventions | Intervention: (haloperidol) for minimum 34 days:
"started at 0.025 mg/kg/day for people
weighing below 20 kg or 0.5 mg/day for those above
20 kg. The doses were titrated up to the maximum of
the lower dose of 0.1 mg/kg/day or 4 mg/day, or
until there was a 75% decrease in SIB or significant
side effects to the medication. Individuals who did
not have a positive response to haloperidol were
weaned from the medication by decreasing the total
daily dose by 0.25‐0.5 mg every 3‐5 days until the
individual was off the medication. Once the
haloperidol was stopped, a placebo was started and
data reported for the placebo condition were
collected after the individual was entirely off
haloperidol for at least 14 days". Comparator (placebo) for minimum 34 days: matching placebo capsules |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: not reported Trial registry: not reported |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: supported, in part, by a grant from the National Institute of Mental Health (MH50358‐8) Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "All behaviour analysts, nurses, and inpatient unit staff were blind to the medication assignments. The physician was aware of the medication assignment" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All behaviour analysts, nurses and inpatient unit staff were blind to the medication assignments". "To keep staff blinded to the different patterns of medication adjustment for behavioural treatment versus medication non‐responders, the letters used to identify the medication could be changed by the physician even if the medication was not changed". |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The data for the 15 participants were recorded in
regards to response to behavioural treatment (%
change in SIB), max dose haloperidol (mg/day),
response to haloperidol (% change in SIB) and
response to placebo (% change in SIB). ABC
Irritability baseline and endpoint data were not
provided for placebo despite being measured
weekly. Other participants had placebo condition measured after 14 days off haloperidol; unclear whether there was any ITT analysis for these missing data. |
| Selective reporting (reporting bias) | High risk | ABC baseline and endpoint data were not provided for placebo at all. |
| Other bias | Low risk | None identified |
Mahdavinasab 2019.
| Study characteristics | ||
| Methods | 10‐week parallel trial of baclofen versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: children’s outpatient clinic at a tertiary hospital in Iran Mean IQ: details not provided Mean age: baclofen + risperidone 8.04 (SD = 2.33); placebo + risperidone 7.9 (SD = 2.0) Gender: 46 male, 12 female Sample size: baclofen (2); placebo (32). Number analysed: baclofen (29); placebo (29) Reasons for dropouts: baclofen (3), physician's choice (1), refusal of further therapy (2); placebo (3), refusal of further therapy (3) Baseline ABC‐I or other BoC scale: ABC‐I baclofen + risperidone 22.76 (8.56); placebo + risperidone 22.62 (9.24) Timing of outcome assessments: baseline, week 5, week 10 Concomitant medications: details not provided Previous medications: excluded if history of antipsychotic medication within the past 6 months before enrolment. |
|
| Interventions | Baclofen + risperidone: initial dose of 0.5 mg and
stepwise 0.5 mg weekly increases for the first 3
weeks + 0.6 mg kg; 1 baclofen 3 times/day Risperidone: initial dose of 0.5 mg and stepwise 0.5 mg weekly increases for the first 3 weeks + placebo |
|
| Outcomes | Primary outcomes:
Secondary outcomes: tolerability |
|
| Notes | Study start date: April 2016 Study end date: August 2018 Funding: "This study was supported by a grant from Tehran University of Medical Sciences to Prof. Shahin Akhondzadeh (Grant No: 32601)". Conflicts of interest" "Authors declare no conflict of interest". Trial registry: IRCT201701131556N95 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomization was performed by a randomization operator who was not otherwise involved in this trial." |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomization codes were kept secure until data curation was completed." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. "Randomization codes were kept secure until data curation was completed... Participants and their parents were blinded to group allocations." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Double‐blind. "Randomization codes were kept secure until data curation was completed... No specific details about outcome assessors." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition and all participants were accounted for |
| Selective reporting (reporting bias) | High risk | Trial reg lists additional primary outcome not reported: Childhood autism rating scale (CARS) |
| Other bias | High risk |
|
Malek 2020.
| Study characteristics | ||
| Methods | 12‐week parallel trial of prednisolone versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria: from those diagnosed with regressive ASD,
Location/setting: paediatric outpatient clinic at a hospital in Iran Sample size: prednisolone (n = 19); placebo (n = 18) Reasons for dropouts: prednisolone (n = 6) 6 withdrawn consent; placebo (n = 5) 4 withdrawn consent, 1 dropped out due to severe irritability Mean IQ: details not provided Mean age: prednisolone 5.81 ± 2.5; placebo.34 ± 2.07 Gender: 25 male, 1 female Baseline ABC‐I or other BoC scale: ABC‐I prednisolone 30.15 (9.62); placebo 25.31 (10.46) Timing of outcome assessments: end of week 12 Concomitant medications: participants could not have taken any antipsychotic medication in past 6 months. Previous medications: details not outlined |
|
| Interventions | Intervention (prednisolone + risperidone) for 12
weeks: initial dose of risperidone was 0.5 mg/day
during the first week of study and stepwise 0.5 mg
weekly increases to maximum dose of 1 mg/d or 2
mg/day. Prednisolone given at 1 mg/kg/day Comparator (placebo + risperidone) for 12 weeks: initial dose of risperidone was 0.5 mg/day during the first week of study and stepwise 0.5 mg weekly increases to maximum dose of 1 mg/day or 2 mg/day. Placebo was administered in placebo pills. |
|
| Outcomes | Primary outcomes: irritability measured using the
ABC‐I (Aman
2017) Secondary outcomes: none reported Timing of outcome assessments: baseline, weeks 4, 8 and 12 (endpoint) |
|
| Notes | Study start date: January 2018 Study end date: February 2019 Funding: "This study was supported by a grant from Tehran University of Medical Sciences to Prof. Shahin Akhondzadeh (Grant Number: 36362)". Conflicts of interest ‐ "The authors have no conflicts of interest to declare". Trial registry ‐ IRCT20090117001556N102 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Patients were randomly assigned to treatment groups by the permuted randomisation block method in a 1:1 ratio using a computer‐generated code. |
| Allocation concealment (selection bias) | Low risk | "The participants were kept ignorant of either the groups to which they have been assigned. Prednisolone and placebo were identical in appearance" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Single‐blind (only participants blinded) |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Single‐blind (only participants blinded) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition and all participants were accounted for |
| Selective reporting (reporting bias) | Low risk | All outcomes reported on clinical trials registry were reported in full |
| Other bias | High risk |
|
Malone 2001.
| Study characteristics | ||
| Methods | Parallel trial of olanzapine versus haloperidol | |
| Participants | Inclusion criteria:
Exclusion criteria: "major medical problems such as cardiac, liver, endocrine, or renal diseases, or seizure disorders or gross neurological deficit, treatment with concomitant psychotropic medication, or a history of previous treatment with haloperidol or olanzapine". Location/setting: not reported Sample size: 12 Number of withdrawals/dropouts: none reported Gender: olanzapine 4/6 male both groups Mean age: 7.8 years IQ: 2/6 and 3/6 (olanzapine and haloperidol) had severe intellectual disability, 3 and 2 had moderate intellectual disability, 1 in haloperidol had mild intellectual disability, and 1 in olanzapine had normal cognitive functioning. Baseline ABC‐I or other BoC: not an outcome Concomitant medications: psychotropic drug use during trial was not permitted History of previous medications: 4 participants had no history of prior psychotropic drug use |
|
| Interventions | Intervention (olanzapine) for 6 weeks: the starting
dosage of olanzapine was 2.5 mg every other day for
participants who weighed ≤ 40 kg and 2.5 mg/day for
participants who weighed > 40 kg. In general,
dosages could be increased in 2.5‐mg increments up
to 5 mg a week, as needed. The maximum dosage for
olanzapine permitted by the study protocol was 20
mg/day. Comparator (haloperidol) for 6 weeks: the starting dosage of haloperidol was 0.25 mg/day for participants who weighed ≤ 40 kg and 0.5 mg for participants who weighed > 40 kg. In general, dosages could be increased as clinically indicated in 0.5‐mg increments up to 1 mg a week, as needed. The maximum dosage for haloperidol permitted by the study protocol was 5 mg/day. Mean daily dose 1.4 mg/day (+/‐0.7) |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: none reported Timing of outcome assessments: baseline and endpoint |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: supported, in part, by a grant from Lilly Research Laboratories (Investigator‐Initiated Study) Conflicts of interest: none disclosed |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation was performed by use of a computer‐generated list" |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Details not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 13 were originally enrolled in the study and 1 withdrew consent before beginning study medication. 12 were included in the analysis. |
| Selective reporting (reporting bias) | Low risk | The CGI and the Children's Psychiatric Rating Scale were the primary outcomes and were reported for both groups. |
| Other bias | Low risk | Treatment groups did not differ significantly on demographic variables such as age, race, gender, socioeconomic status, severity of illness, or level of cognitive functioning. |
Marcus 2009.
| Study characteristics | ||
| Methods | 8‐week RCT, double‐blind, placebo‐controlled trial of aripiprazole versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: 35 independent research centres and research centres with a hospital affiliation Sample size: 218 children in total; placebo (52); 5 mg aripiprazole (53), 10 mg aripiprazole (59) and 15 mg aripiprazole (54) Number of withdrawals/dropouts: placebo (14), 5 mg aripiprazole (17), 10 mg aripiprazole (10) and 15 mg aripiprazole (7) Gender: placebo 48/52 male, 5 mg aripiprazole 47/53 male, 10 mg aripiprazole 50/59 male and 15 mg aripiprazole 50/54 male Mean age: placebo 10.2 years, 5 mg aripiprazole 9.0 years, 10 mg aripiprazole 10.0 years and 15 mg aripiprazole 9.5 years IQ: not reported Baseline ABC‐I or other BoC: placebo 28.0, 5 mg aripiprazole 28.6, 10 mg aripiprazole 28.2 and 15 mg aripiprazole 28.9 Concurrent medications: "psychotropic medications including antipsychotics, antidepressants, anxiolytics, mood stabilisers and neuroleptics were prohibited during the study". History of previous medications: aripiprazole 5 mg/day 24/52 had taken any nervous system medications, 9/52 had taken antipsychotics with 1 of those taking aripiprazole, 8/52 had taken anxiolytics, 8/52 had taken antidepressants, and 3/52 had taken psychostimulants previously. Placebo: 22/51 had taken any nervous system medications, 11/51 had taken antipsychotic and 3 of those had taken aripiprazole previously, 8/51 had taken anxiolytics, 3/51 had taken antidepressants, and 5/51 had taken psychostimulants |
|
| Interventions | All participants randomised to aripiprazole started
on 2 mg/day for the 1st week, which was increased to
5 mg/day for the 2nd week. Aripiprazole 5 mg/day for 8 weeks: 5 mg tablet once daily for 8 weeks (mean 0.129 mg/kg/day) Aripiprazole 10 mg/day for 8 weeks: weekly 5 mg increments until 10 mg/day was reached. 10 mg tablets once daily for 8 weeks (mean 0.223 mg/kg/day) Aripiprazole 15 mg/day for 8 weeks: weekly 5 mg increments until 15 mg/day was reached. 15 mg tablet once daily for 8 weeks (mean 0.354 mg/kg/day) Placebo for 8 weeks: equivalent placebo |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
Timing of outcome assessments: baseline, weeks 1, 2, 3, 4, 5, 6 and 8 |
|
| Notes | Study start date: June 2006 Study end date: June 2008 Source of funding: "This study was supported by Bristol‐Myers Squibb (Princeton, NJ) and Otsuka Pharmaceutical Co, Ltd (Tokyo, Japan). Editorial support for the preparation of this article was provided by Ogilvy Healthworld Medical Education." Conflicts of interest: "this study was supported by Bristol‐Myers Squibb (Princeton, NJ) and Otsuka Pharmaceutical Co., Ltd. (Tokyo, Japan). Editorial support for the preparation of this article was provided by Ogilvy Healthworld Medical Education". "Drs Marcus, Owen, Kamen, and Manos are with Bristol‐Myers Squibb; Drs McQuade and Carson are with Otsuka Pharmaceutical Developmental and Commercialization and Dr Aman is with Ohio State University". Trial registry" not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Details not provided. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided, only that double‐blinding occurred |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Details not provided, only that double‐blinding occurred |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants were accounted for and details
recorded on www.clinicaltrials.gov Analyses were based on LOCF. LTFU 5 mg/day aripiprazole: AE (5), withdrew consent (2), LTFU (1), poor/ non‐compliance (1) |
| Selective reporting (reporting bias) | High risk | Response defined as a ≥ 25% reduction from baseline to endpoint in the ABC‐I Subscale score, and a CGI‐I score of 1 or 2 at endpoint was not reported |
| Other bias | Unclear risk | The proportion of participants who were moderately ill (compared to, markedly, severely and extremely) was 25% lower in the aripiprazole 10 mg/day group compared to the placebo group. |
McCracken 2002.
| Study characteristics | ||
| Methods | Parallel trial of risperidone versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: University of California at Los Angeles, Ohio State University, Indiana University, Yale University, and the Kennedy Krieger Institute at Johns Hopkins University, USA Sample size: 101: 49 risperidone group, 51 placebo Number of withdrawals/dropouts: risperidone 3/49; placebo 18/52 (risperidone: 3 lack of efficacy; placebo: severe headache and seizure (1); withdrawal of consent (1); LTFU (3); non‐compliance (1); lack of efficacy (12)). Gender: 82 boys, 19 girls Mean age: 8.6 years IQ: 13/101 had profound intellectual disability, 18/101 had severe intellectual disability, 18/101 had a moderate intellectual disability, 25/101 had a mild intellectual disability Baseline ABC‐I or other BoC: ABC‐I risperidone 26.2, placebo 25.5 Concomitant medications: participants had to be free of all psychotropic drugs at least 2 weeks prior to randomisation (4 weeks for antipsychotics and fluoxetine). History of previous medications: antipsychotics 5/101, SSRIs 16/101, stimulant 21/101, alpha‐2‐agonist 16/101 |
|
| Interventions | Risperidone for 8 weeks: children who weigh 20‐45 kg
commenced on 0.5 mg at bedtime, increased to 0.5 mg
twice daily on day 4. The dose was gradually
increased in 0.5 mg increments of 2.5 mg/day (1.0 mg
in the morning and 1.5 mg at bedtime) by day 29.
Children weighing > 45 kg had a maximum dose of
1.5 mg in the morning and 2.0 mg at bedtime.
Children weighing < 20 kg were given an initial
dose of 0.25 mg/ day. Dose increases could be
delayed because of adverse effects or significant
improvement on lower doses. No dose increases after
day 29. Mean daily dose of 1.8 mg/day or maximum
daily dose of 2.5 mg/day children < 45 kg or 3.5
mg/day children > 45 kg Placebo for 8 weeks: placebo equivalent of 2.4 ± 0.6 mg/day |
|
| Outcomes | Primary outcomes
Secondary outcomes: none reported Timing of outcome assessments: weekly for 8 weeks |
|
| Notes | Study start date: June 1999 Study end date: April 2001 Source of funding: "supported by contracts from the National Institute of Mental Health (N01MH70009), to Dr Scahill; N01MH70010 to Dr McCracken; N01MH70001 to Dr McDougle ; and N01MH80011 to Dr Aman, General Clinical Research Centre grants from the National Institute of Health (M01 RR00750 to Indiana University; M01 RR00052 to Johns Hopkins University; M01 RR00034 to Ohio State University; and M01 RR06022 to Yale University, and a grant from the Korczak Foundation to Dr Scahill". Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient details |
| Allocation concealment (selection bias) | Unclear risk | Insufficient details |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Each child was seen weekly by two clinicians who were unaware of the treatment assignment." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Each child was seen weekly by two clinicians who were unaware of the treatment assignment: a primary clinician, who reviewed side effects and adjusted the dose of medication, and a clinical evaluator, who assessed the response to treatment." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | LTFU risperidone: treatment ineffective (3) 46 of original 49 in risperidone group completed trial (3 withdrew "because the study was not effective") 18 children in placebo group withdrew: severe headaches and a seizure (1); withdrawal of consent (1); nonadherence (1); LTFU (3) and lack of efficacy (12) 4 were identified as having an ABC‐I that fell below the ABC‐I score of 18 and were included in theITT analysis. Authors noted that zero participants withdrew from study due to AEs. An ITT analysis was used, and all participants were included in the analysis. |
| Selective reporting (reporting bias) | High risk | Sedation not reported as an AE |
| Other bias | Low risk | No concerns |
McDougle 1996.
| Study characteristics | ||
| Methods | Parallel trial of fluvoxamine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: a neuroscience research centre at the Connecticut Mental Health Center, New Haven, and the Adult Pervasive Developmental Disorders Clinic at the same neuroscience research centre, USA Sample size: fluvoxamine 15; placebo 15 Number of withdrawals/dropouts: none reported Gender: 27 men, 3 women Mean age: 30.1 years IQ: not reported Baseline ABC‐I or other BoC: aggression (Brown Aggression Scale; Brown 1979) fluvoxamine 9.3, placebo 12.3 Concomitant medications: participants were required to be psychotropic drug‐free before the trial History of previous medications: not reported |
|
| Interventions | Intervention (fluvoxamine for 12 weeks): started at
50 mg every night. "The dosage could then be
increased by 50 mg daily every 3 or 4 days to a
maximum dosage of 300 mg/day, as tolerated, if
maximal clinical response was not obtained. Thus,
the maximum dosage of fluvoxamine was attained
within 3 weeks, and patients received this dose for
at least 9 weeks." maximum 300 mg/day Comparator (placebo for 12 weeks): equivalent placebo, "lactose in identical‐looking tablets" |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: baseline, 4, 8 and 12 weeks |
|
| Notes | Study start date: September 1990 Study end date: December 1993 Source of funding: "this work was supported by a National Alliance for Research on Schizophrenia and Depression Young Investigator Award (Dr McDougle), the State of Connecticut Department of Mental Health and Addiction Services, The Korczak Foundation for Autism and Related Disorders, and grants MOI RR06022‐33, P50 MH30929‐18, HD 0300827, and POI MH25642from the National Institutes of Health, Bethesda, Md. Fluvoxamine and financial support were provided by Solvay Pharmaceuticals, Marietta, Ga". Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "The prescribing psychiatrist (C.J.M.), the nurse (S.T.N.) who performed the behavioral ratings, the patients, and all family and other members of the patients' treatment teams were unaware of drug assignment" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "The prescribing psychiatrist (C.J.M.), the nurse (S.T.N.) who performed the behavioral ratings, the patients, and all family and other members of the patients' treatment teams were unaware of drug assignment.". Apart from that it was not described how the outcome assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants were accounted for and included in the analysis. Quote: "All patients who complete at least two weeks of drug treatment will be included in the analysis. The final rating scores of any patient who terminates the study prematurely will be carried forward to the end of the study." |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Unclear risk | No significant differences were seen in age, sex distribution, Autism Behavior Checklist scores, or full‐scale IQ scores between the 2 groups. |
McDougle 1998.
| Study characteristics | ||
| Methods | Parallel trial of risperidone versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: all participants were evaluated and treated within the outpatient (24) and inpatient (7) divisions of the neuroscience research centre at the Connecticut Mental Health Centre, New Haven, USA Sample size: risperidone 15, placebo 16 Number of withdrawals/dropouts: 7 withdrew: 3 from risperidone group (1 withdrew after 1 week due to "notable agitation"; 1 developed an "abnormal gait" after 4 weeks; and 1 withdrew "because of a lack of significant improvement in symptoms"); 4 from placebo group withdrew: 2 with PDD and 2 with autism withdrew "because of interfering agitation after 4 weeks" Gender: risperidone 13 male, 2 female; placebo 9 male, 7 female Mean age: 26.4 years IQ: risperidone mean 55.5; placebo 52.9 Baseline ABC‐I or other BoC: irritability (using the RFRLRS subscale 3) risperidone 1.02, placebo 0.78; SIB (Self‐Injurious Behaviour Questionnaire) risperidone 47.8, placebo 24.2 Concomitant medications: participants could not have taken any psychotropic drugs for at least 4 weeks before the start of the trial. History of previous medications: 24 had received psychotropic medications previously |
|
| Interventions | Risperidone for 12 weeks: risperidone was started at
1 mg every night. The dosage was then increased by 1
mg daily every 3‐4 days to a maximum dosage of 10
mg/day. Patients received the maximum dose (based on
tolerability) for at least 7 weeks. Mean dose of 2.9
mg/day Placebo for 12 weeks: placebo started at 1 mg every night. The dosage was then increased by 1 mg daily every 3‐4 days to a maximum dosage of 10 mg/day. Patients received the maximum dose (based on tolerability) for at least 7 weeks. |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: baseline, weeks 4, 8 and 12 |
|
| Notes | Study start date: June 1994 Study end date: February 1997 Source of funding: grants MH‐30929 and HD‐03008 from the Public Health Service, Bethesda Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Patients were randomly allocated according to a computer‐generated list. |
| Allocation concealment (selection bias) | Low risk | Risperidone or placebo (lactose) in identical‐appearing capsules |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The prescribing psychiatrist, the research nurse clinician who performed the behavioural ratings, the patients, and all family and other members of the patients’ treatment teams were unaware of the drug assignment (blind). |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The research nurse clinician who performed the behavioural ratings...were unaware of the drug assignment (blind) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | LOCF and ITT analysis used LTFU: risperidone (3), AEs (agitation) (1); developed abnormal gait (1); lack of efficacy (1) |
| Selective reporting (reporting bias) | Low risk | The measures were the CGI, the RFRLRS, Yale‐Brown Obsessive Compulsive Scale and the Self‐Injurious Behaviour Questionnaire. All scales were reported at both baseline and endpoint for both risperidone and placebo group. Sedation not reported as an AE |
| Other bias | Low risk | No concerns |
Minshawi 2016.
| Study characteristics | ||
| Methods | Parallel trial of D‐cycloserine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: "Indiana University School of Medicine and Cincinnati Children’s Hospital Medical Center". Sample size: D‐cycloserine 34; placebo 33 Number of withdrawals/dropouts: no dropouts postrandomisation Gender: D‐cycloserine 28/34 male; placebo 27/33 male Mean age: D‐cycloserine 8.4 years; placebo 8.3 years IQ: D‐cycloserine 92.4; placebo 87.3 Baseline ABC‐I or other BoC: treatment: ABC‐I 11.06; placebo 12.67 Concomitant medications: antipsychotics 8/34, 8/33 placebo, alpha‐2 agonist 6/34, 8/33, stimulants 14/34 and 11/33, sleep aids 9/34 and 7/33, mood stabilisers 1 and 2, glutamatergic modulators 1 in D‐cycloserine group, other 3 and 1 History of previous medications: not reported |
|
| Interventions | D‐cycloserine for 10 weeks: given at a 50 mg dose 30
min prior to weekly group social skills training
over 10 weeks Placebo for 10 weeks: placebo pill (sugar pill) administered 30 min prior to each of the 10 social skills training sessions |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: baseline, week 6 and week 10 (endpoint) |
|
| Notes | Study start date: March 2010 Study end date: January 2014 Source of funding: "funding for this study was provided by the United States Department of Defense Award Number W81XWH‐09‐1‐0091." Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Children with ASD were randomised to receive 10 weeks (10 doses) of D‐cycloserine or placebo in a 1:1 ratio |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details on parents and teachers completing ABC questionnaire |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts were reported and all 67 were included in the analysis. |
| Selective reporting (reporting bias) | Low risk | Baseline and endpoint data reported for all outcomes mentioned |
| Other bias | Low risk | No significant group differences, or pharmaceutical company funding |
Miral 2008.
| Study characteristics | ||
| Methods | Parallel trial of risperidone versus haloperidol | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: Turkey Sample size: 30 (15 in each group) Number of withdrawals/dropouts: 2 in risperidone group excluded from final analysis from the week 12 evaluation because of the lack of efficacy data Gender: risperidone 11/15 male; haloperidol 13/15 male Mean age: risperidone 10 years, haloperidol 10.9 years IQ: not reported Baseline ABC‐I or other BoC: irritability (using the RFRLRS) risperidone 1.09, haloperidol 1.05 Concomitant medications: details not provided History of previous medications: details not provided |
|
| Interventions | Intervention (risperidone) for 12 weeks: risperidone
was initiated at a dosage of 0.01 mg/kg/day and the
dosage was increased to 0.04 mg/kg/day until the end
of the 2nd week. If tolerated, then it was increased
to a maximum dosage of 0.08 mg/kg/day. Mean daily
dose 2.6 mg/day or maximum 0.08 mg/kg; haloperidol
mean dose 2.6 mg/day Comparator (haloperidol) for 12 weeks: haloperidol was initiated at a dosage of 0.01 mg/kg/day and the dosage was increased to 0.04 mg/kg/day until the end of the 2nd week. If tolerated, then it was increased to a maximum dosage of 0.08 mg/kg/day. |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: baseline, weeks 2, 4, 8 and 12 |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: "this research was supported in part by Janssen and Cilag Drug company". Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding not discussed Quote: "two experienced clinicians performed all of the measures" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "two subjects who were being administered
risperidone were excluded from our final analysis
from the week 12 evaluation because of lack of
efficacy data" LTFU: 2 in risperidone group were excluded from analysis due to lack of efficacy data ITT analysis or LOCF not noted by study authors |
| Selective reporting (reporting bias) | High risk | RFRLRS subscores and weight were outlined for both baseline and endpoint, as well as other outcomes reported in the paper. However, the CGI baseline scores were not reported despite being a primary outcome measure. |
| Other bias | Unclear risk | The research was supported in part by Janssen and Cilag Drug Company. |
Moazen‐Zadeh 2018.
| Study characteristics | ||
| Methods | 10‐week parallel trial of simvastatin versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: speciality outpatient autism clinic at Roozbeh Psychiatry Hospital, Iran Sample size: 35 in each group Number of withdrawals/dropouts: 2 from each group (simvastatin: 1 no longer met criteria, 1 withdrew consent; placebo: 2 withdrew consent) Gender: 53 male, 13 female Mean age: simvastatin 7.06 years (2.33); placebo 7.61 (2.74) years IQ: details not provided Baseline ABC‐I or other BoC: ABC‐I simvastatin 20.97 (5.37); placebo 19.97 (7.24) Concomitant medications: children did not have a history of psychotropic drug use History of previous medications: children did not have a history of psychotropic drug use |
|
| Interventions | Intervention (simvastatin + risperidone): risperidone
(Risperdal; Janssen Pharmaceuticals, Belgium) plus
simvastatin (Osveh, Iran) for 10 weeks. Risperidone
starting dose was 0.5 mg/day in 0.5 mg tablets, and
in the absence of clinically significant AEs it was
increased by 0.5 mg per week to the target dose of 1
mg/day for children weighing < 20 kg and 2 mg/day
for those weighing at least 20 kg. Simvastatin was
administered in the form of a 20 mg tablet/day for
children < 10 years of age and a 40 mg tablet per
day for those at least 10 years of age. Comparator (placebo + risperidone): risperidone (Risperdal; Janssen Pharmaceuticals, Belgium) plus placebo for 10 weeks. Risperidone starting dose was 0.5 mg/day in 0.5 mg tablets, and in the absence of clinically significant AEs it was increased by 0.5 mg/week to the target dose of 1 mg/day for children weighing < 20 kg and 2 mg/day for those weighing at least 20 kg. Placebo was administered in the form of a 20 mg tablet/day for children < 10 years of age and a 40 mg tablet per day for those at least 10 years of age. |
|
| Outcomes | Primary outcomes:
Secondary outcomes: tolerability Timing of outcome assessments: baseline, weeks 5 and 10 (endpoint) |
|
| Notes | Study start date: February 2016 Study end date: December 2016 Funding: "This study was supported by a grant to Prof. Shahin Akhondzadeh (Grant number 30327) from Tehran University of Medical Sciences (TUMS)" Conflicts of interest: "No competing financial interests exist" Trial registry: IRCT201602041556N86 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised random number generator |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Simvastatin and placebo tablets were identical in shape, size, texture, colour, and taste, and they were dispensed in identical containers by an investigational drug pharmacist. Quote: "During the trial, the physicians, other healthcare personnel, participants, and parents were blinded to treatment assignments." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "During the trial, the physicians, other healthcare personnel, participants, and parents were blinded to treatment assignment" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No further statistical methods such as data imputation or ITT analysis were conducted for participants who were lost to follow‐up or dropped out. |
| Selective reporting (reporting bias) | Low risk | All outcomes on the trial registry were reported in the paper. |
| Other bias | High risk |
|
Mohammadi 2013.
| Study characteristics | ||
| Methods | Parallel trial of amantadine + risperidone versus placebo + risperidone | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: a psychiatric academic hospital affiliated with Tehran University of Medical Sciences, Iran Sample size: 40 (20 in each group) Number of withdrawals/dropouts: 1 participant in the risperidone plus placebo group discontinued after week 5. Gender: amantadine 16/20 boys; placebo 17/20 boys Mean age: amantadine 6.4 years; placebo 7.1 years IQ: not reported Baseline ABC‐I or other BoC: ABC‐I amantadine group 20; ABC‐I placebo 20.9 Concomitant medications: not reported History of previous medications: not reported |
|
| Interventions | Amantadine + risperidone for 10 weeks: amantadine was
given twice a day at 100 mg/d for children < 30
kg, and 150 mg/d for those ≥ 30 kg. Risperidone was
started at 0.5 mg/day, and titrated up to 2.0 mg/day
in a 0.5 mg/week rate if there were no
complications. Placebo + risperidone for 10 weeks: risperidone was started at 0.5 mg/day, and titrated up to 2.0 mg/day in a 0.5 mg/week rate if there were no complications. Placebo was identical in appearance (shape, size, colour, and taste) and dispensed by investigational drug pharmacist, alongside risperidone, which started at 0.5 mg/day, and was titrated up to 2.0 mg/day in a 0.5 mg/week rate if there were no complications. |
|
| Outcomes | Primary outcomes:
Secondary outcomes: not reported Timing of outcome assessments: baseline, 5 weeks, 10 weeks (endpoint) |
|
| Notes | Study start date: June 2011 Study end date: May 2012 Source of funding: supported by a grant from Tehran University of Medical Sciences (grant 10797) Conflicts of interest: "no conflict of interest exists for any of the authors associated with the manuscript and there was no source of extra‐institutional commercial funding". |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was accomplished using a computerised random number generator in a 1:1 ratio and blocks of 4 |
| Allocation concealment (selection bias) | Low risk | Quote: "treatment allocation was concealed from the patients and the rating psychiatrists using sequentially numbered, opaque, sealed, and stapled envelopes" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Separate persons were responsible for random allocation and rating of the patients. The patients, the psychiatrists who referred them, the clinician who assessed the patients and prescribed the drugs, and the statistician were blind to the allocations." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The patients, the psychiatrists who referred them, the clinician who assessed the patients and prescribed the drugs, and the statistician were blind to the allocations." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | All analyses were based on the ITT sample and were performed using LOCF procedure on participants with at least 1 post‐baseline visit. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported in the trial protocol on the Iranian Registry of Clinical trials were reported in the paper. |
| Other bias | High risk |
|
Montazmenesh 2020.
| Study characteristics | ||
| Methods | 10‐week parallel trial of sulforaphane versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: autism clinic in the children’s outpatient clinic of Roozbeh Hospital (Iran) Sample size: sulforaphane group (34), placebo group (34) Number of withdrawals/dropouts: sulforaphane group (4), 4 discontinued intervention; placebo group (4), 4 discontinued intervention Mean age: sulforaphane 6.87 years (2.06), placebo 7.67 (2.35) Gender: 40 male, 20 female IQ: details not provided Baseline ABC‐I or other BoC: sulforaphane ABC‐I 22.50 (4.89); placebo 21.30 (6.13) Concomitant medications: only children who had been drug‐free for at least 6 months were included. No other concomitant intervention or medication was permitted during the trial History of previous medications: details not provided |
|
| Interventions | Sulforaphane + risperidone: participants in both
groups received risperidone in a similar manner. The
starting daily dose of risperidone was 0.25 mg in
children weighing < 20 kg and 0.5 mg in children
weighing ≥ 20 kg. The dosage was increased stepwise
by 0.5 mg weekly up to a maximum dose of 1 mg for
children weighing < 20 kg, 2.5 mg for those
weighing 20–45 kg, and 3.5 mg for those weighing
> 45 kg. Sulforaphane
(1‐isothiocyanato‐4‐methylsulfinylbutane; ACER,
Tehran, Iran) was prescribed at 50 μmol and 100 μmol
(approximately 10 mg and 20 mg) per day for children
weighing < 45 kg and 45–90 kg, respectively. Placebo + risperidone: participants in both groups received risperidone in a similar manner. The starting daily dose of risperidone was 0.25 mg in children weighing < 20 kg and 0.5 mg in children weighing ≥ 20 kg. The dosage was increased stepwise by 0.5 mg weekly up to a maximum dose of 1 mg for children weighing < 20 kg, 2.5 mg for those weighing 20–45 kg, and 3.5 mg for those weighing > 45 kg. The placebo group received placebo capsule. |
|
| Outcomes | Primary outcomes:
Secondary outcomes: tolerability |
|
| Notes | Study start date: April 2018 Study end date: November 2019 Funding: "This study was funded by Tehran University of Medical Sciences and Health Services (Grant number 37048)" Conflicts of interest: "The authors declare no conflict of interest" Trial registry: IRCT20090117001556N107 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Allocation of the treatment groups using block randomisation (with blocks of size 4) |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes were unveiled at the study end‐point for statistical analysis. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Sealed opaque envelopes were unveiled at the study end‐point for statistical analysis. "Randomizations, drug administration, rating, data entry, and statistical analysis were implemented by separate individuals." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Randomizations, drug administration, rating, data entry, and statistical analysis were implemented by separate individuals. Placebo capsules were identical to sulforaphane based on shape, size, color, and taste." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | ~12% attrition |
| Selective reporting (reporting bias) | High risk | CARS is a primary outcome in trial registration but not in paper |
| Other bias | High risk |
|
Mouti 2014.
| Study characteristics | ||
| Methods | Parallel study of fluoxetine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: 3 tertiary hospitals in Australia Sample size: 146 participants Number of withdrawals/dropouts: 31 in fluoxetine, 21 in placebo dropped out or did not complete treatment. Mean age: 11.2 years Gender: 124 boys, 22 girls IQ: 46/146 had an intellectual disability Baseline ABC‐I or other BoC: fluoxetine ABC‐I 18.57; placebo 17.87 Concomitant medications: 62/146 were on concurrent medications and a further 2 were receiving stimulant medications History of previous medications:details not provided |
|
| Interventions | Fluoxetine for 16 weeks: commenced at 4 or 8 mg/day
for the first week depending on weight and then
titrated to a maximum of 20 mg/day for children
weighing < 40 kg or 30 mg/day if ≥ 40 kg Placebo for 16 weeks: equivalent placebo |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: AEs assessed weekly and other primary outcomes at baseline and endpoint |
|
| Notes | Study start date: November 2010 Study end date: August 2017 Source of funding: "Drs Reddihough and Lee and Ms Orsini report receiving grants from NHMRC and the Royal Children's Hospital Foundation during the conduct of the study. Dr Hazell reports that his employer has received payment from Shire for speaker’s fees. Dr Whitehouse reports receiving grants from NHMRC during the conduct of the study." Conflicts of interest: none declared Comment: Study authors were contacted for further information and they emailed a separate published paper providing all the details (Reddinhough). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Low risk | Quote: "The randomization schedule was provided to the clinical trials pharmacist at each site, who arranged a sequential stock of trial medication for each stratum, labeled with only the study number, strata, and instructions for use" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "This schedule remained confidential throughout the study. The independent statistician retained a copy of the master randomization schedule to check for any discrepancies. Participants and their families, clinicians, and the research team assessing outcomes remained blind to the randomization schedule throughout the study." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "This schedule remained confidential throughout the study. The independent statistician retained a copy of the master randomization schedule to check for any discrepancies. Participants and their families, clinicians, and the research team assessing outcomes remained blind to the randomization schedule throughout the study." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | A large number from each group withdrew from the
trial (31 fluoxetine and 21 placebo) and
"Twenty‐five percent of the participants did not
provide data on the primary outcome (n = 21 and n =
16 in the fluoxetine and placebo groups,
respectively) however where outcome data was
reported at least once an ITT analysis was used.
There was a chance baseline imbalance in some of the
key behavioral measures of ASDs, indicating that the
placebo group had a comparatively more severe
behavioral phenotype than the fluoxetine group". LTFU fluoxetine group: 31 discontinued (20 parent or caregiver withdrew consent; 5 AEs; 2 clinician decisions to discontinue; 1 used other ineligible drugs; and 3 others withdrew for personal reasons) LTFU placebo group: 21 discontinued (12 parent or caregiver withdrew; 4 AEs; 2 clinician decisions to discontinue; 3 others withdrew for personal reasons) |
| Selective reporting (reporting bias) | Unclear risk | All scales mentioned in the protocol were reported in the final paper, however the subscales of the Repetitive Behaviour Scale were not reported, only the total score however, more information was provided by the study authors. |
| Other bias | High risk | Quote: "The active and placebo medication will be produced by Richard Stenlake Chemists (Bondi Junction, Australia)". "PH and MK have received payment from Eli Lilly (the manufacturer of fluoxetine) for participation in consultancies, advisory boards, speaker’s bureau, and the conduct of clinical trials" |
Munesue 2016.
| Study characteristics | ||
| Methods | Cross‐over trial of oxytocin versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: outpatient setting of the Department of Child and Adolescent Psychiatry of Kanazawa University Hospital in Kanazawa, Japan Sample size: 29, 15 oxytocin‐placebo; 14 placebo‐oxytocin Number of withdrawals/dropouts: none reported Gender: all participants were male Mean age: range 15‐40 years IQ: oxytocin first: 24.9; placebo first: 37.5 Baseline ABC‐I or other BoC: ABC‐I oxytocin first: 11.9; placebo first: 17.4 Concomitant medications: not reported History of previous medications: 22 participants (75.9%) received psychotropic medications at stable doses during the 3 weeks prior to randomisation. |
|
| Interventions | Intervention (oxytocin) for 6 weeks: oxytocin dosage
was 8 IU twice‐daily for 6 weeks (16 IU per
day). Comparator (placebo) for 6 weeks: equivalent placebo |
|
| Outcomes | Primary outcomes:
Secondary outcomes: WHOQOL (WHO 1998) Timing of outcome assessments: every 2 weeks |
|
| Notes | Study start date: February 2012 Study end date: October 2013 Source of funding: "this work was supported by the Strategic Research Program for Brain Sciences from the Ministry of Education, Culture, Sports, Science, and Technology, Japan (MEXT) and from the Japan Agency for Medical Research and Development and also by the Industry‐Academia Collaborative R&D Programs [Center of Innovation (COI) Program] from MEXT." Conflicts of interest: none declared Trial registry: UMIN000007250 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "a computer generated randomization table was created by the research pharmacist and used to randomise participants" |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All efficacy assessments were carried out by an independent evaluator who was blinded to both side effects and group assignment" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants were analysed using an ITT analysis and baseline and endpoint QoL scores were recorded. |
| Selective reporting (reporting bias) | Low risk | The primary and secondary outcomes of interest were recorded on clinicaltrials.gov and all results were provided. |
| Other bias | Unclear risk | No significant differences in gender, race, age. Perhaps a slight difference in IQ ‐ oxytocin group 99 (22) and placebo 118 (19) however, several study authors are connected to many pharmaceutical companies |
NCT00183339.
| Study characteristics | ||
| Methods | 12‐month parallel trial of fluoxetine versus placebo | |
| Participants | Inclusion criteria: diagnosis of autism Exclusion criteria:
Location/setting: details not provided on clinical registry Sample size: 18 Number of withdrawals/dropouts: 4/8; 6/10 (reasons not provided) Mean age: 44 months Gender: details not provided IQ: details not provided Baseline ABC‐I or other BoC: baseline ABC‐I not provided Concomitant medications: details not provided History of previous medications: details not provided |
|
| Interventions | Fluoxetine: "between 2 mg per day and 20 mg per day
of liquid fluoxetine will be given in the morning
using a flexible dosing strategy, following a
36‐week dose titration schedule" Placebo: "between 0.5ml per day and 5ml per day of liquid placebo will be given in the morning using a flexible dosing strategy, following a 36‐week dose titration schedule" |
|
| Outcomes | Primary outcomes:
Secondary outcomes: tolerability |
|
| Notes | Study start date: September 2005 Study end date: March 2014 Funding: details not provided Conflicts of interest: details not provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided apart from, "Masking: quadruple (Participant, Care Provider, Investigator, Outcomes Assessor)" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Details not provided apart from, "Masking: quadruple (Participant, Care Provider, Investigator, Outcomes Assessor)" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | This study primarily aimed to look at rate of attrition and recruitment but doesn't provide data on reason for dropout. |
| Selective reporting (reporting bias) | Unclear risk | Primary outcome is rate of recruitment however without a protocol we can't be sure. |
| Other bias | Unclear risk | Paper has not been published as yet, so greater details have not been provided. |
NCT00198107.
| Study characteristics | ||
| Methods | 48‐week parallel trial of aripiprazole versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: USA (Riley Hospital for Children, Christian Sarkine Autism Treatment Center, Indiana University School of Medicine) Sample size: 81 randomised, 40 aripiprazole, 41 placebo Mean IQ: details not provided Mean age: details not provided Gender: 4/38 female in aripiprazole group, 7/40 female in placebo group Reasons for dropouts: 6 from placebo group discontinued, AE (1), lack of efficacy (2), LTFU (2), doctor decision (1); 3 from aripiprazole group discontinued, AE (1), LTFU (1), withdrawal by participant (1) Baseline ABC‐I or other BoC scale: details not provided Concomitant medications: details not provided Previous medications: details not provided |
|
| Interventions | Intervention (aripiprazole) for 8 weeks: participants
≤ 49 kg will receive maximum dose of 10 mg/day of
aripiprazole over 8 weeks. Participants weighing ≥
50 kg will receive a maximum dose of 15 mg/day
aripiprazole over 8 weeks. Comparator (placebo) for 8 weeks: matching placebo pill for 8 weeks |
|
| Outcomes | Primary outcomes:
Secondary outcomes: tolerability Timing of outcome assessments: ABC‐I measured in weeks 1, 2, 3, 4, 6, and 8 (endpoint) |
|
| Notes | Study start date: September 2005 Study end date: April 2019 Funding: details not provided Conflicts of interest: details not provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Only details provided were on the trials registry, "Masking: Quadruple (Participant, Care Provider, Investigator, Outcomes Assessor)" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Only details provided were on the trials registry, "Masking: Quadruple (Participant, Care Provider, Investigator, Outcomes Assessor)" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropout < 15%, reasons reported |
| Selective reporting (reporting bias) | Unclear risk | No information |
| Other bias | Unclear risk | Not stated |
NCT00468130.
| Study characteristics | ||
| Methods | 8‐week parallel trial of aripiprazole versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Setting/location: the USA Sample size: 15 in total Number and reason for dropouts: 2 in each group dropped out, 3 due to AEs and 1 withdrew Mean age: 12.4 years Gender: 2 female, 11 male Mean IQ: details not provided Previous or current medications: details not provided |
|
| Interventions | Intervention (aripiprazole): participants weighing
< 40 kg will receive a maximum of 10 mg/day of
aripiprazole, and a maximum of 20 mg/day for
children ≥ 40 kg for 8 weeks Comparator (placebo): equivalent placebo (sugar pills) for 8 weeks |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: every second week |
|
| Notes | Source of funding: University of Medicine and
Dentistry of New Jersey Conflicts of interest: unclear |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Apart from, "Masking: Quadruple (Participant, Care Provider, Investigator, Outcomes Assessor)", no other details provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Apart from "Masking: Quadruple (Participant, Care Provider, Investigator, Outcomes Assessor)", no other details provided. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 8‐week data appear to be reported for all participants, but study authors note 2 dropouts due to AEs in treatment group (i.e. nearly 30% dropout). Unclear if outcome data are really complete. |
| Selective reporting (reporting bias) | Unclear risk | Protocol is available and all prespecified outcomes of interest reported in the prespecified way |
| Other bias | High risk | The baseline ABC‐I scores were twice that in the intervention group compared to placebo. |
NCT00498173.
| Study characteristics | ||
| Methods | 8‐week parallel trial of atomoxetine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: details not described Mean IQ: details not described Mean age: atomoxetine 9.3 years, placebo 8.4 years Gender: 54 male, 6 female Sample size: 60 Reasons for dropouts: no postbaseline ratings for 2 people in atomoxetine group and 1 in placebo group Baseline ABC‐I or other BoC scale: PedsQL atomoxetine 56.3 (18.8); placebo 60.5 (19.6) Concomitant medications: atomoxetine (34.5%) were taking concomitant medications; placebo 41.9% were taking concomitant medications Previous medications: details not provided |
|
| Interventions | Intervention (atomoxetine) for 8 weeks: available
tablet strengths of atomoxetine: 5 mg, 10 mg, 25 mg,
40 mg. Week 1, participant takes 0.5 mg/kg/day; week
2, 0.8 mg/kg/day; week 3, 1.2 mg/kg/day. Potential
exists for dose increase at week 4 to 1.8 mg/kg/day
based on CGI improvement rating at week 4. Comparator (placebo) for 8 weeks: participants will receive blinded, matched placebo for 8 weeks. Dosage can be increased over the first 4 weeks of study participation and will then be held constant for the remainder of the 8‐week trial. Placebo tablets dosages: 5 mg, 10 mg, 25 mg, 40 mg |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
Timing of outcome assessments: details not described |
|
| Notes | Study start date: July 2007 Study end date: August 2017 Source of funding: details not provided Conflicts of interest: details not provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Sequential Assignment" |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Only details provided were on the trial registry, "Masking: triple (participant, care provider, investigator)" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Only details provided were on the trial registry, "Masking: triple (participant, care provider, investigator)" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 3 participants were not included in the analysis all due to "no post‐baseline ratings" |
| Selective reporting (reporting bias) | Unclear risk | Only relying on Clinical trials reg |
| Other bias | Unclear risk | Difficult to know without a published paper and protocol |
NCT01337687.
| Study characteristics | ||
| Methods | 6‐week parallel trial of oxytocin versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: Montefiore Medical Center, USA Mean IQ: not reported Mean age: 33.2 years Gender: 16 male, 3 female Sample size: 19 in total Reasons for dropouts/withdrawals: none reported Baseline ABC‐I or other BoC scale: not reported Concomitant medications: details not provided Previous medications: details not provided |
|
| Interventions | Intervention (oxytocin) for 6 weeks: administered
intranasally twice a day via 1 x 12 unit puff to
each nostril, totalling 48 IU a day Comparator (saline) for 6 weeks: administered intranasally twice a day via 1 puff per nostril, totalling 48 IU a day |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: none reported Timing of outcome assessments: baseline and 6 weeks (endpoint) |
|
| Notes | Study start date: April 2011 Study end date: February 2020 Funding: details not provided Conflicts of interest: details not provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Only details provided were on the trial registry, "Masking: quadruple (participant, care provider, investigator, outcomes assessor)" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Only details provided were on the trial registry, "Masking: quadruple (participant, care provider, investigator, outcomes assessor)" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropout reported |
| Selective reporting (reporting bias) | Unclear risk | No peer‐reviewed paper |
| Other bias | Low risk | No other sources of bias identified |
NCT01624675.
| Study characteristics | ||
| Methods | 8‐week parallel trial of risperidone versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: 18 study centres in Japan Mean IQ: not reported Mean age: not reported Gender: not reported Sample size 39: risperidone (21); placebo (18) Reasons for dropouts/withdrawals: no dropouts reported Baseline ABC‐I or other BoC scale: ABC‐I risperidone 28.2 (6.36); placebo 27.5 (5.26) Concomitant medications: not reported Previous medications: not reported |
|
| Interventions | Intervention (risperidone) for 8 weeks: participants
weighing < 20 kg received risperidone 0.25 mg/day
up to day 4. On day 4, dose was titrated in
increments of 0.25 mg/day (up to a daily dose of 1.0
mg) at the regular study visit thereafter until week
8. Participants weighing ≥ 20 kg received
risperidone 0.5 mg/day up to day 4. On day 4, dose
was titrated in increments of 0.5 mg/day (up to a
daily dose of 2.5 mg) at the regular visit
thereafter until week 8. The maximum daily dose for
participants weighing ≥ 45 kg was 3.0 mg. Comparator (placebo) for 8 weeks: matching placebo |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: unclear |
|
| Notes | Study start date: June 2012 Study end date: October 2015 Funding: details not provided Conflicts of interest: details not provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information beyond double‐blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information beyond double‐blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data available for all participants |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | Outcomes matched those on clinical trials registry |
NCT01908205.
| Study characteristics | ||
| Methods | 12‐week trial of oxytocin versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: Canada Mean IQ: not stated Mean age: all under 18 years Gender: 47 male, 7 female Sample size: 60 Reasons for dropouts/withdrawals: oxytocin 5, placebo 1 (2 LTFU, 4 withdrew) Baseline ABC‐I or other BoC scale: not an outcome Concomitant medications: details not provided Previous medications: details not provided |
|
| Interventions | Intervention (oxytocin) for 12 weeks: the proposed
dosing schedule is 0.4 IU/kg oxytocin, taken twice
daily, for a maximum of 24 IUs per dose for 12
weeks Comparator (placebo) for 12 weeks: the proposed dosing schedule is 0.4 IU/kg, taken twice daily, for a maximum of 24 IUs per dose for 12 weeks |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes:
Timing of outcome assessments: baseline and 12 weeks (endpoint) |
|
| Notes | Study start date: July 2013 Study end date: November 2020 Funding: details not provided Conflicts of interest: details not provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information. Quote: "Allocation: Randomized\" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information. Quote: "Allocation: Randomized" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Only details provided were on the trials registry Quote: "Masking: Quadruple (Participant, Care Provider, Investigator, Outcomes Assessor)" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Only details provided were on the trials registry Quote: "Masking: Quadruple (Participant, Care Provider, Investigator, Outcomes Assessor)" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 2 LTFU, and 4 withdrew ‐ no further information |
| Selective reporting (reporting bias) | Unclear risk | Without a published paper or protocol it is difficult to know if all outcomes were reported |
| Other bias | Low risk | No other sources of bias identified |
NCT01972074.
| Study characteristics | ||
| Methods | 12‐week trial of memantine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: Massachusetts General Hospital. USA Mean IQ: details not provided Mean age: details not provided Gender: details not provided Sample size: memantine, 22 randomised; placebo, 21 randomised Reasons for dropouts/withdrawals: memantine, 6 did not complete (4 due to AEs, 1 lack of efficacy, and 1 withdrawal by participant); placebo, 4 did not complete (1 due to AEs, 1 LTFU, 1 lack of efficacy, and 1 withdrawal by participant). Baseline ABC‐I or other BoC scale: not an outcome Concomitant medications: details not provided Previous medications: details not provided |
|
| Interventions | Intervention (memantine) for 12 weeks: given in
capsule form twice daily. It will be administered
twice daily for 12 weeks (including a 4‐week
titration phase to a maximum dose of 20 mg/day).
Participants will undergo neuroimaging before and
after the 12‐week treatment phase. Comparator (placebo) for 12 weeks: no active ingredients; given in capsule form twice daily. It will be administered twice daily for 12 weeks. Participants will undergo neuroimaging before and after the 12‐week treatment phase. |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: tolerability Timing of outcome assessments: unclear |
|
| Notes | Study start date: October 2013 Study end date: September 2019 Funding: details not provided Conflicts of interest: details not provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "ASD subjects will be randomized to either active memantine or placebo in a 1:1 ratio after they have been determined to meet all eligibility criteria. Randomization lists stratified by gender and racial/ethnic minority status (minority vs Caucasian) will be generated by the statistician and passed to the investigational pharmacy for assignment". |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Only details provided were on the trials registry Quote: "Masking: quadruple (participant, care provider, Investigator, outcomes assessor)" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Only details provided were on the trials registry Quote: "Masking: quadruple (participant, care provider, Investigator, outcomes assessor)" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants included in analyses |
| Selective reporting (reporting bias) | Unclear risk | It is difficult to know without a protocol |
| Other bias | Low risk | No other sources identified |
NCT02940574.
| Study characteristics | ||
| Methods | 4‐week trial of oxytocin versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: Belgium Mean IQ: details not provided Mean age: 18‐40 year olds Gender: all participants were male. Sample size: 40 (oxytocin 22, placebo 18) Reasons for dropouts/withdrawals: 1 in oxytocin group withdrew from the study, 1 from placebo not included in analysis due to "excessive in‐scanner head motion" Baseline ABC‐I or other BoC scale: not an outcome Concomitant medications: details not provided Previous medications: details not provided |
|
| Interventions | Intervention (oxytocin) for 4 weeks: single dose of
24 IU oxytocin (Syntocinon) nasal spray (3 puffs of
4 IU per nostril), followed by 4 weeks of a daily
single dose (24 IU; 3 puffs of 4 IU per nostril) of
nasal spray. Comparator (placebo) for 4 weeks: placebo (physiological water (solution of sodium chloride (NaCl) in water)) administered via nasal spray. A single dose (24 IU) of nasal spray (3 puffs of 4 IU per nostril), followed by 4 weeks of a daily single dose (24 IU; 3 puffs of 4 IU per nostril) of nasal spray. |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes:
Timing of outcome assessments: baseline and 4 weeks (endpoint) |
|
| Notes | Study start date: October 2016 Study end date: February 2020 Funding: details not provided Conflicts of interest: details not provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient detail: "allocation: randomized" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient detail. Quote: "allocation: randomised" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Only details provided were on the trials registry Quote: "masking: quadruple (participant, care provider, investigator, outcomes assessor)" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Only details provided were on the trials registry Quote: "masking: quadruple (participant, care provider, investigator, outcomes assessor)" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "1 subject lost in Syntocinon group due to subject withdrawal. 1 subject lost in placebo group due to low data quality (excessive in‐scanner head motion)" |
| Selective reporting (reporting bias) | Unclear risk | Difficult to know without a protocol |
| Other bias | Low risk | No other apparent sources of bias |
NCT03242772.
| Study characteristics | ||
| Methods | 11‐week parallel trial of amphetamine plus parent training versus placebo plus parent training | |
| Participants | Inclusion criteria:
Exclusion criteria:
History of epilepsy or seizure disorder (except for history of simple febrile seizures or if the child is seizure free (regardless of seizure type) for the past year) Location/setting: Duke Center for Autism and Brain Development, USA Number of withdrawals/dropouts: amphetamine group 3 dropped out (2. LTFU, 1 withdrew); placebo group 1 dropped out due to "physician decision" Gender: 12 male, 6 female Mean age: intervention group 86.83 (SD20.80) months; placebo group 103.00 (18.88) months IQ: not reported Baseline ABC‐I scores or other BoC: not an outcome Concomitant medications:details not provided History of previous medications: details not provided |
|
| Interventions | Intervention:
Comparator:
|
|
| Outcomes | Primary outcomes: adverse effects Secondary outcomes: none reported Timing of outcome assessments: 11 weeks (endpoint) |
|
| Notes | Study start date: December 2018 Study end date: results submitted online December 2021 Funding: Duke University Conflicts of interest: details not provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Only information "Allocation: Randomized" |
| Allocation concealment (selection bias) | Unclear risk | Only information "Allocation: Randomized" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information apart from, "Masking: Quadruple (Participant, Care Provider, Investigator, Outcomes Assessor)" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information apart from, "Masking: Quadruple (Participant, Care Provider, Investigator, Outcomes Assessor)" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Primary outcome data not reported. "This variable required behavioral coding of videotaped caregiver‐child interactions collected at two time points. This coding were not conducted due to the fact that the study was terminated and time 2 data were not collected for participants due to safety concerns related to Covid‐19." |
| Selective reporting (reporting bias) | High risk | Primary outcome data not reported. "This variable required behavioral coding of videotaped caregiver‐child interactions collected at two time points. This coding were not conducted due to the fact that the study was terminated and time 2 data were not collected for participants due to safety concerns related to Covid‐19." |
| Other bias | Low risk | "Principal Investigators are NOT employed by the organization sponsoring the study." "There is NOT an agreement between Principal Investigators and the Sponsor (or its agents) that restricts the PI's rights to discuss or publish trial results after the trial is completed." |
Niederhofer 2002.
| Study characteristics | ||
| Methods | Cross‐over trial of lofexidine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria: details not provided Location/setting: Austria Sample size: 12 in total (cross‐over) Number of withdrawals/dropouts: details not provided Gender: all participants were male. Mean age: lofexidine group 7.3 years; placebo group 9.2 years Mean IQ: lofexidine 59; placebo 48 Baseline ABC‐I or other BoC: details not provided Concomitant medications: participants had been off medications for at least 1 month prior to the study. History of previous medications: details not provided |
|
| Interventions | Intervention (lofexidine) for 13 weeks: lofexidine
was started at 0.4 mg/day, and tapered up over 2
weeks to 0.8‐1.2 mg/day in 3 doses. Comparator (placebo) for 13 weeks: identical placebo tablets were given. |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: ABC‐ I and AEs assessed weekly |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: not reported Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Tablets for each subject were placed in sealed envelopes designated for each day of the study" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "All raters (parents, teachers, and clinicians) were blind to drug order until ratings were completed" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details on how clinicians were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No baseline data reported. Not clear how many included in the analysis |
| Selective reporting (reporting bias) | Unclear risk | Unclear outcomes for 2 arms of active treatment (10 mg and 20 mg doses) |
| Other bias | Unclear risk | Funding and author affiliations unknown |
Niederhofer 2003.
| Study characteristics | ||
| Methods | Cross‐over trial of tianeptine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Sample size: 7 in tianeptine group, 6 placebo (13 in total) Reason for withdrawals/dropouts: "a thirteenth subject entered the study but was dropped because of noncompliance with medication" Location/setting: Italy Mean age: 7.3 years Gender: all participants were male. Mean IQ: ranged from 35‐84 Baseline ABC‐I or other BoC: tianeptine ABC‐I 13.9; placebo 14.1 Concomitant medications: participants had been off medication for at least 1 month before the study. History of previous medications: "all these children had been treated with either methylphenidate, neuroleptics or desipramine before entry into the study. In each case, these medications had either not been effective or caused intolerable side effects." |
|
| Interventions | Intervention (tianeptine) for 12 weeks: 37.5 mg/day
dose for 12 weeks Comparator (placebo) for 12 weeks: identical placebo tablets |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: weekly ABC ratings and AEs |
|
| Notes | Study start date: 2002 Study end date: not reported Source of funding: not reported Conflicts of interest: none disclosed |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "subjects were randomly assigned by a nonrating clinician to begin tianeptine or placebo." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | All raters were blind to drug order until ratings were completed. However, the authors note of "possible unblinding of parents and teachers because of side effects" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No details about participation and dropouts |
| Selective reporting (reporting bias) | Unclear risk | Adverse effects not reported. Without a trial protocol it is difficult to know if any outcomes were measured but not reported. |
| Other bias | Unclear risk | Details not provided |
Nikoo 2015.
| Study characteristics | ||
| Methods | Parallel trial of N‐acetylcysteine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: Tehran, Iran Sample size: 20 in N‐acetylcysteine + risperidone, 20 placebo + risperidone (40 in total) Number of withdrawals/dropouts: no reported dropouts after first post‐baseline measurements Gender: 33 male, 7 female Mean age: 7.5 years (N‐acetylcysteine), 7.6 years (placebo) IQ: not reported Baseline ABC‐I or other BoC: ABC‐I NAC 21.2, placebo 19.7 Concomitant medications: concomitant drug during course of trial not allowed History of previous medications: details not provided |
|
| Interventions | Intervention (N‐acetylcysteine) for 10 weeks:
administered at 200 mg 3 times/day for children
weighing < 20 kg. For children weighing ≥ 20 kg,
N‐acetylcysteine was given at 300 mg 3
times/day. Risperidone was also started at 0.5 mg and titrated weekly by 0.5 mg to a maximum of 1.0 mg/day for children weighing < 20 kg. For children weighing ≥ 20 kg, risperidone was given at the same starting dose and titration rate, but to a maximum of 2.0 mg/day. Comparator (placebo) for 10 weeks: equivalent placebo |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: baseline, week 5, week 10 |
|
| Notes | Study start date: November 2011 Study end date: November 2013 Source of funding: "this study was supported by a grant from Tehran University of Medical Sciences to Shahin Akhondzadeh, PhD, (grant no. 15155)." Conflicts of interest: none disclosed |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random allocation of the patients into 2 groups in a 1:1 ratio with the help of computer‐generated codes |
| Allocation concealment (selection bias) | Low risk | Quote: "the assignments were kept in consecutively numbered, confidential, and sealed envelopes until the statistical analysis step" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided except double‐blinding used |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "during the study, separate persons held the responsibility of randomisation and rating of the patients. Resultant data were also entered in a database by a person not involved in other parts of the study" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Appears to have been no LTFU |
| Selective reporting (reporting bias) | Low risk | The trial was registered on http://irct.ir/trial/879 and all outcomes reported in the protocol were reported. |
| Other bias | High risk |
|
Nikvarz 2017.
| Study characteristics | ||
| Methods | 8‐week parallel trial of risperidone versus memantine | |
| Participants | Inclusion criteria:
Exclusion criteria:
Setting/location: Roozbeh Psychiatric Hospital, Iran Sample size: 34, memantine (18 participants), risperidone (16 participants) Number of dropouts/withdrawals: 1 participant in the risperidone group did not complete the trial due to a change in psychiatrist. 3 participants in the memantine group did not complete the trial ‐ all reportedly due to a lack of therapeutic response in first 2 weeks of trial. Mean age: 6.7 years IQ: details not provided Gender: memantine 13/15 male; risperidone 10/15 male Baseline ABC‐I scores: 21.8 Concomitant medications: details not provided Previous medications: risperidone: 2 in risperidone group and 4 in memantine group had previously taken risperidone; aripiprazole: 2/15 in memantine group and zero from risperidone group had previously taken aripiprazole. |
|
| Interventions | Intervention (memantine) for 8 weeks: started at a
once‐daily dose of 0.2 mg/kg/day then increased to
0.3 mg/kg/day in the 2nd week and ultimately to 0.4
mg/kg/day in the 3rd week. The maximum daily dose of
memantine was 20 mg/day. Comparator (risperidone) for 8 weeks: "Risperidone was started at 0.02 mg/kg/day then increased to 0.04 mg/kg/day at week 2" up to a maximum of "0.06mg/kg/day at the third week." The maximum daily dose of risperidone was 3mg/day. |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: baseline, week 4 and week 8 (endpoint) |
|
| Notes | Study start date: April 2012 Study end date: March 2013 Funding: "This study was supported by Tehran University of Medical Sciences (TUMS) (Grant number: 91‐01‐33‐16991)." Conflicts of interest: "The authors declare no conflict of interest." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sample size was 30. Patients were randomly allocated to receive risperidone or memantine based on simple, balanced, blocked randomisation. |
| Allocation concealment (selection bias) | Unclear risk | Although referred to as "simple balanced blocked randomisation", no information on how allocation was concealed |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label trial |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No information beyond it being "open label", so assume unblinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Data not imputed for participants who discontinued |
| Selective reporting (reporting bias) | Unclear risk | Difficult to know for certain without seeing study protocol |
| Other bias | Low risk | No other sources of bias identified |
Owen 2009.
| Study characteristics | ||
| Methods | Parallel trial of aripiprazole versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: USA Sample size: 98 participants were randomised (aripiprazole 47; placebo 51) Number of withdrawals/dropouts: placebo group discontinued (15): lack of efficacy (6), AEs (3), withdrew consent (2), LTFU (4). Aripiprazole group discontinued (8): lack of efficacy (1), AEs (5), withdrew consent (1), LTFU (1) Gender: 44/51 and 42/47 were male Mean age: placebo 8.8 years, aripiprazole 9.7 years IQ: not reported Baseline ABC‐I or other BoC: placebo ABC‐I 30.2; aripiprazole 29.6 Concomitant medications: not reported History of previous medications: 50% had previously received psychotropic medications. The most commonly received medications were antipsychotic agents (placebo: 30.0%; aripiprazole: 17.0%), psychostimulant agents (placebo: 26.0%; aripiprazole: 17.0%), anxiolytic agents (placebo: 16.0%; aripiprazole: 17.0%), and antidepressant agents (placebo: 10.0%; aripiprazole: 6.4%) |
|
| Interventions | Intervention (aripiprazole) for 8 weeks:
approximately 7.5 mg/day or 0.172 mg/kg/day Comparator (placebo) for 8 weeks: equivalent to 5, 10, or 15 mg/day doses |
|
| Outcomes | Primary outcomes:
Secondary outcomes: QoL, measured using the PedsQL (WHO 1998) Timing of outcome assessments: baseline, weeks 1, 2, 3, 4, 5, 6 and 8, with telephone call in week 7 |
|
| Notes | Study start date: June 2006 Study end date: February 2008 Source of funding: "Drs Owen, Corey‐Lisle, Manos, and Marcus are employees of Bristol‐Myers Squibb. This study was supported by Bristol‐ Myers Squibb (Princeton, NJ) and Otsuka Pharmaceutical Co, Ltd (Tokyo, Japan). Editorial support for the preparation of this manuscript was provided by Ogilvy Healthworld Medical Education; funding was provided by Bristol‐Myers Squibb." Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Computer‐generated randomisation schedule prepared by Bristol Myers Squibb using a permuted block design |
| Allocation concealment (selection bias) | Low risk | Investigational sites accessed a call‐in interactive voice response system. The system assigned a medication bottle number to each participant. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | LOCF LTFU aripiprazole: discontinued (8); lack of efficacy (1); AEs (5); withdrew consent (1); LTFU (1) LTFU placebo: discontinued (15); lack of efficacy (6); AEs (3); withdrew consent (2); LTFU (4) |
| Selective reporting (reporting bias) | Low risk | The trial was registered on clinicaltrials.gov and the outcomes registered were reported |
| Other bias | Unclear risk | No differences in age, gender, ethnicity, weight or baseline scores but previous antipsychotic use (51% across groups) was not reported by group |
Owley 2001.
| Study characteristics | ||
| Methods | Cross‐over trial of porcine secretin versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: University of Chicago, University of California‐Irvine, University of Utah, USA Sample size: 56 in total (28 to secretin‐placebo, 28 to placebo‐secretin) Number of withdrawals/dropouts: none reported Gender: 48 boys, 8 girls Mean age: 6.7 years IQ: mental age ≥ 24 months Baseline ABC‐I or other BoC: ABC‐I placebo‐secretiin 10.1. secretin‐placebo 11.6 Concomitant medications: 14 participants were taking a total of 15 psychotropic medications (at stable doses) during the study, including SSRIs (3), atypical neuroleptics (3), α‐adrenergic agonist (1), and psychostimulants (8) History of previous medications: participants on stable doses of psychotropic medications were included but they were asked not to change the dosages of these medications for the duration of the trial. |
|
| Interventions | Intervention (secretin) for 4 weeks: secretin was
administered at 2 CU/kg/day Comparator (placebo) for 4 weeks: placebo (infused saline) that was indistinguishable from the active treatment |
|
| Outcomes | Primary outcomes: irritability, measured using the
ABC‐Irritability subscale (Aman 1985) Secondary outcomes: none reported Timing of outcome assessments: baseline and then at the end of weeks 2, 4, 6 and 8 |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: "this work was supported in part by the University of California at Davis Medical Investigation of Neurodevelopmental Disorders Institute (WM, EHC, PAF). Additional support was provided by grants from the NIMH (R01 MH52223, K02 MH01389, EC), the Jean Young and Walden W. Shaw Foundation (BLL), and the Irving B. Harris Foundation (BLL). This work was conducted as part of the NICHD/NIDCD Collaborative Network on the Neurobiology and Genetics of Autism." Conflicts of interest: none disclosed |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Randomisation was done by the investigational pharmacy at each site". Unclear as to the method and whether the same method was used across all sites. |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "All patients, their parents, all members of the assessment team were blind to drug assignments until all subjects at that site had completed the trial." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Members of the assessment team were blind to drug assignments until all subjects at that site had completed the trial. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants were accounted for and where particular assessments were missed, the number of participants who were analysed were indicated in brackets (). |
| Selective reporting (reporting bias) | Low risk | All outcomes reported at cross‐over endpoints |
| Other bias | High risk | Only a single dose of secretin was used. |
Parker 2017.
| Study characteristics | ||
| Methods | 4‐week parallel trial of oxytocin versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: study was conducted in the Autism and Developmental Disabilities Clinic in the Division of Child and Adolescent Psychiatry at Stanford University, USA Sample size: 32 Number of withdrawals/dropouts: 2/16; 0/18 (1 LTFU, 1 withdrew) Gender: 27 male, 5 female Mean age: 6‐12 years IQ: approx 35‐90 Baseline ABC‐I or other BoC: baseline scores not reported Concomitant medications: participants were allowed to take concurrent psychotropic medications provided they do not interact with oxytocin, were on a stable dose before study entry and medication use did not differ between groups. History of previous medications: details not provided |
|
| Interventions | Intervention (oxytocin): twice‐daily each participant
will have 3 puffs per nostril of 4 IU/puff (24 IU
twice daily) for 4 weeks Comparator (placebo): placebo nasal spray 3 puffs per nostril of 4 IU/puff (24 IU twice daily) for 4 weeks |
|
| Outcomes | Primary outcomes:
Secondary outcomes: tolerability Timing of outcome assessments: baseline, week 4 (endpoint) |
|
| Notes | Study start date: June 2012 Study end date: April 2016 Funding: "K.J.P. and A.Y.H. provided funding for the research" Conflicts of interest: "The authors declare no conflict of interest" Trial registry: NCT01624194 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization was performed by an IDS pharmacist using www.randomization.com, which allocates each participant to an intervention by using the method of randomly permuted blocks" |
| Allocation concealment (selection bias) | Low risk | "Randomization was performed by an IDS pharmacist using www.randomization.com, which allocates each participant to an intervention by using the method of randomly permuted blocks" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. Quote: "the research team to remain blinded throughout the trial’s duration" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "This practice allowed the research team to remain blinded throughout the trial’s duration... A technician blinded to treatment condition performed sample preparation and OXT quantification following established procedures" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants were accounted for. |
| Selective reporting (reporting bias) | High risk | Some outcomes from clinicaltrials.gov not reported in the peer‐reviewed paper |
| Other bias | Low risk | No other sources of bias identified |
Parker 2019.
| Study characteristics | ||
| Methods | 4‐week trial of vasopressin versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: autism disorders clinic, USA Sample size: 30 Number of withdrawals/dropouts: none reported Gender: 25 male, 5 female Mean age: 6‐12.9 years of age (outpatients) IQ: approximately 77‐98 Baseline ABC‐I or other BoC: baseline ABC‐I 8.29 (7.4); baseline QoL 64.53 (13.86) Concomitant medications: details not provided History of previous medications: details not provided |
|
| Interventions | Intervention (vasopressin nasal spray): 4 IU twice
daily of vasopressin during week 1 and 8 IU twice
daily of vasopressin during week 2. Participants
aged 6‐9.5 years then received 12 IU twice daily of
vasopressin during weeks 3 and 4, whereas
participants aged 9.6‐12.9 years received 16 IU
twice daily of vasopressin during weeks 3 and 4. Comparator (placebo nasal spray): matching placebo for 4 weeks |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
Timing of outcome assessments: ABC‐I and QoL were measured at baseline and week 4 (endpoint). Participants underwent weekly safety/tolerability assessments in the clinic to monitor for AEs. |
|
| Notes | Study start date: December 2013 Study end date: May 2017 Funding: various grants to the researchers Conflicts of interest: financial compensation by pharmaceutical companies and other involvement with pharmaceutical companies Trial registry: NCT01962870 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was performed by an unblinded investigator using a machine‐generated treatment schedule, which allocated each participant to an intervention. |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Research team, parents/legal guardians, and child participants remained blind throughout the trial's duration. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Research team, parents/legal guardians, and child participants remained blind throughout the trial's duration. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no dropouts reported and all were included in the analysis. |
| Selective reporting (reporting bias) | High risk | PedsQL and ABC not reported in peer‐reviewed paper. The Overt Aggression Scale was mentioned as an outcome but not reported. |
| Other bias | Low risk | No other sources identified |
Pearson 2013.
| Study characteristics | ||
| Methods | 1‐week cross‐over trial of methylphenidate (3 doses) versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/ setting: University of Texas Medical School at Houston, USA Sample size: 24 Number of withdrawals/dropouts: none reported Gender: details not provided Mean age: 8.8 years (1.7) IQ: 85.0 (16.8) Baseline ABC‐I or other BoC: not reported Concomitant medications: 7 children were stable on long‐term (> 3 months) medications that they continued (at a constant dose) during the trial: risperidone (n = 3), aripiprazole (n = 1), sertraline (n = 1), bupropion (n = 1), and trazodone (n = 1). History of previous medications: 13 children had previously taken stimulant medication, which was discontinued 1 week prior to entry into the trial. |
|
| Interventions | Intervention (methylphenidate): each child received 1
week each of the four MPH dosing regimens (placebo,
low‐dose methylphenidate, medium‐dose
methylphenidate, and high‐dose methylphenidate). The
children received Ritalin long‐acting (LA;
extended‐release methylphenidate) at breakfast and
immediate‐release methylphenidate in the afternoon,
with dosing based on body weight. The mean
immediate‐release methylphenidate per dose
equivalents of the Ritalin LA (given in the morning)
were 0.21 mg/kg methylphenidate in the low‐dose,
0.35 mg/kg in medium‐dose, and 0.48 mg/kg in the
high‐dose. The immediate‐release methylphenidate
dose (given in the afternoon) was approximately half
of each single‐dose equivalent of the morning’s
Ritalin LA. Comparator: not described apart from "Participants will take a placebo for 1 full week of the randomized drug trial. They will take one capsule in the morning and one capsule in the afternoon." |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported |
|
| Notes | Study start date: September 2005 Study end date: May 2013 Funding: "This study was funded by grant number MH072263 from the National Institute of Mental Health (NIMH)." Conflicts of interest: "Dr. Pearson and Ms. Mansour have received travel reimbursement and research support from the Forest Research Institute and Curemark LLC." Trial registry: NCT00178503 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Study personnel were unblinded to placebo. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Study personnel were unblinded to placebo. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Reported no dropouts, however 5 of the 24 children discontinued the afternoon immediate‐release methylphenidate dose because of behaviour concerns in late afternoon/evening ‐ unclear if ITT |
| Selective reporting (reporting bias) | High risk | Primary outcome in trial reg not reported ‐ Mean Continuous Performance Test (CPT)‐Commission Errors by Dose |
| Other bias | Low risk | No other sources of bias identified |
Posey 2005.
| Study characteristics | ||
| Methods | Cross‐over trial of methylphenidate versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: 5 centres, Indiana University (Indianapolis), the Kennedy Krieger Institute at John Hokins University (Baltimore), The Ohio State University (Columbus), the University of California (Los Angeles), Yale University (New Haven), USA Sample size: 66 Number of withdrawals/dropouts: 8 exited cross‐over phase, 7 due to AEs (3 from high dose, 3 medium dose and 1 low dose), 1 due to other reasons, withdrawing consent prior to receiving treatment. Gender: 59/66 male Mean age: 7.5 years IQ: mental age of at least 18 months Baseline ABC‐I or other BoC: ABC‐I 16.5 Concomitant medications: no concurrent psychotropic medications for at least 1‐3 weeks (1 week for stimulants and clonidine hydrochloride; 2 weeks for antidepressants except fluoxetine and citalopram hydrobromide; 3 weeks for fluoxetine, citalopram hydrobromide, or antipsychotics) prior to baseline visit. History of previous medications: not described |
|
| Interventions | Intervention (methylphenidate) for 4 weeks: dosage
levels were varied depending on the weight of the
child. The low‐dosage level approximate 0.125 mg/kg
per dose. The medium‐dosage level approximate 0.250
mg/kg per dose. The high‐dosage level approximate
0.500 mg/kg per dose. Each participant received 1
week placebo and 1 week each of 3 different doses in
random order (except high dose never followed
placebo). Each dose was received 3 times daily (8
am, 12 pm, 4 pm). Comparator (placebo) for 4 weeks: equivalent placebo |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: details not provided |
|
| Notes | Study start date: November 2001 Study end date: September 2003 Source of funding: research supported by authors' contracts with National Institute of Mental Health, and grants with various universities, the General Clinical Research Centers, National Center for Research Resources, National Institutes of Health, Bethesda, and by the Korczak Foundation, Amsterdam Conflicts of interest: none declared Trial registry: NCT00025779 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation lists were generated centrally and were held by an investigational pharmacist at each site. |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Clinicians, the patient, and the caregiver were blind to treatment assignment during this phase. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The rating clinician was also kept blinded to any information about AEs or changes in vital signs or weight. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Consistent with ITT principles, all of the data from
participants receiving 2 medium doses (owing to the
inability to tolerate a high dose) were analysed. No
significant differences were found between these 2
weeks of receiving the medium dose, so the data were
combined. LTFU unclear as they did not report for intervention and placebo groups. |
| Selective reporting (reporting bias) | High risk | ABC‐I was reported in baseline scores however it was not reported in the endpoint scores (only ABC hyperactivity). |
| Other bias | Low risk | None identified |
Quintana 1995.
| Study characteristics | ||
| Methods | Cross‐over trial of methylphenidate versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: USA Sample size: 10 Number of withdrawals/dropouts: none reported Gender: 6 boys, 4 girls Mean age: 8.5 years IQ: mean Developmental Quotient was 64.3 Baseline ABC‐I or other BoC: ABC‐I 11.8 Concomitant medications: participants were required to have been off neuroleptics for a period of at least 1 month prior to the study. History of previous medications: all the children had been on neuroleptic medications (haloperidole etc) at some point in their lives but had not been previously treated with methylphenidate |
|
| Interventions | Intervention (methylphenidate) for 2 weeks: started
at 10 mg/kg twice a day for the 1st week, then 20
mg/kg twice a day in the 2nd week Placebo for 2 weeks: equivalent placebo |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: unclear |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: not reported Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No other comments apart from, "These investigators, the children, and the parents were blind to drug and drug dose." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 10 total participants mentioned, without detail as to
dosage allocation, completion of study and
individual outcome measures LTFU was not mentioned |
| Selective reporting (reporting bias) | Low risk | All outcomes measured were reported at baseline and endpoint. Published baseline and endpoint data on all outcome measures |
| Other bias | Unclear risk | No mention of funding sources or conflicts of interest |
Remington 2001.
| Study characteristics | ||
| Methods | Cross‐over trial of clomipramine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria: with the exception of "antiparkinsonian medication in the form of benztropine...no other psychotropic medications were permitted during the study." Location/setting: "recruited from the Autism and Pervasive Developmental Disorder Clinic at the Centre for Addiction and Mental Health, Clarke Division, a teaching hospital associated with the University of Toronto." (Canada) Sample size: 36 (phase 1) Number of withdrawals/dropouts: 5 withdrew from placebo group because of behaviour; 5 withdrew from clomipramine group, 2 because of behaviour and AEs, and 3 because of AEs alone Gender: 31/36 male Mean age: 16.3 years IQ: not reported Baseline ABC‐I or other BoC: ABC‐I 19.0 Concomitant medications: 13/36 were taking other medications such as trifluoperazine, methylphenidate, fluvoxamine or carbamazepine History of previous medications: not reported |
|
| Interventions | Intervention 1 (clomipramine) for 7 weeks: 25 mg at
bedtime for 2 days, 25 mg twice a day for 2 days, 25
mg 3 times/day for 2 days, and 50 mg twice a day Intervention 2 (haloperidol): 0.25 mg at bedtime for 2 days, 0.25 mg twice a day for 2 days, 0.25 mg 3 times/day for 2 days, and 0.5 mg twice a day Comparator (placebo) for 7 weeks: placebo equivalent |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: not reported |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: grant from the Ontario Mental Health Foundation Conflicts of interest: none declared Trial registry: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomly assigned to one of three treatment groups as part of a Latin square design (clomipramine‐placebo‐haloperidol, placebo‐haloperidol‐clomipramine, and haloperidol‐clomipramine‐placebo) |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Medications and placebo were packaged in similar capsules to maintain the double‐blind component" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Details not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | LTFU clomipramine: 20 in total withdrew:
LTFU haloperidol: 10 in total withdrew from haloperidol group.
LTFU placebo: 10 in total withdrew
|
| Selective reporting (reporting bias) | High risk | Outcomes including ABC subscales measured every 2 weeks, however these results were not reported. |
| Other bias | Low risk | No other sources identified |
Research Units 2005.
| Study characteristics | ||
| Methods | 8‐week discontinuation phase of McCracken 2002 study | |
| Participants | Inclusion criteria:
Exclusion criteria: no concomitant treatment with psychotropic medication was allowed during any phase of the study, except anticonvulsant treatment for seizure control if the child had been taking a stable dose for 4 weeks and had been free of seizures for 6 months. Location/setting: the 5 clinical sites included the University of California Los Angeles, Ohio State University, Indiana University, Yale University, and Kennedy Krieger Institute (Johns Hopkins University), USA Sample size: 38 participants Number analysed: 32 (16 from each group) Number of withdrawals/dropouts: 2 not included in the analyses however reasons were not provided Gender: 81% were male in the original McCracken study. Mean age: 8.6 years IQ: 73% of participants had a mild to profound intellectual disabilities Baseline ABC‐I or other BoC: following McCracken study ABC‐I was 11.3 Concomitant medications: participants had to be free of all psychotropic drugs at least 2 weeks prior to randomisation (4 weeks for antipsychotics and fluoxetine). History of previous medications: details not reported |
|
| Interventions | Risperidone for 8 weeks: the maintenance risperidone
dose was reduced by 25% each week until only placebo
in the fourth week Placebo for 8 weeks: equivalent placebo |
|
| Outcomes | Primary outcomes: relapse rates, measured in % Secondary outcomes: none reported. Apart from relapse rates, no other outcomes or new data were provided. Timing of outcome assessments: all participants were seen weekly for a total of 8 weeks in the discontinuation phase. |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: "NIMH contracts to principal investigators Dr McCracken (grant N01 MH‐70010), Dr Scahill (N01 MH‐70009), Dr McDougle (N01 MH‐70001) and Dr Aman (N01 MH‐80011); NIH Division of Research Resources General Clinical Research Center grants to Indiana University (M01 RR00750), Johns Hopkins University (M01 RR‐00052), Ohio State University (M01 RR‐00034) and to Yale University (M01 RR‐06022). Funding was also received by Dr Scahill from the Korczak Foundation and study medications were donated by Janssen Pharmaceutica." Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided about outcome assessors or clinicians |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "subjects were randomly assigned again, this time either to continued risperidone at the same dose or to gradual placebo substitution, in a double‐blind fashion" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Details not provided |
| Selective reporting (reporting bias) | Unclear risk | Only relapse reported |
| Other bias | Unclear risk | Details not provided |
Rezaei 2010.
| Study characteristics | ||
| Methods | Parallel trial of topiramate + risperidone versus placebo + risperidone | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: paediatric outpatient clinic in Iran Sample size: 40 (20 to each group) Number of withdrawals/dropouts: none reported Gender: 27 boys, 13 girls Mean age: topiramate + risperidone: 8.17 years; placebo + risperidone: 7.85 years IQ: not reported Baseline ABC‐I or other BoC: topiramate + risperidone: 17.25; placebo + risperidone: 16.80 Concomitant medications: not reported History of previous medications: not reported |
|
| Interventions | Topiramate + risperidone for 8 weeks: maximum
topiramate dose of 100 mg/day for children < 30
kg or 3‐6 years of age. Maximum of 200 mg/day for
children 7‐12 years or ≥ 30 kg. Maximum risperidone
dose of 2 mg/day for children 10‐40 kg or 3 mg/day
for children > 40 kg Risperidone + placebo for 8 weeks: maximum risperidone of 2 mg/day for children 10‐40 kg or 3 mg/day for children > 40 kg |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessment: AEs recorded at weeks 1, 2, 4, 6 and 8 |
|
| Notes | Study start date: April 2008 Study end date: January 2010 Source of funding: grant from Tehran University of Medical Sciences to Prof Shahin Akhondzadeh (Grant No: 6550) Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Patients were randomised to receive topiramate or placebo in a 1:1 ratio using a computer‐generated code. |
| Allocation concealment (selection bias) | Low risk | The assignments were kept in sealed, opaque envelopes until data analysis. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Throughout the study, the person who administered the medications, the rater and the patients were blind to assignments" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Throughout the study, the person who administered the medications, the rater and the patients were blind to assignments" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Patients will be randomly allocated to
topiramate + risperidone (Group A) or placebo +
risperidone (Group B) for a 10‐week, double‐blind,
placebo‐controlled study" only 8‐weeks of the trial
was reported in the paper LTFU: none reported |
| Selective reporting (reporting bias) | High risk | The ABC and the 5 subscales were the primary outcome measure and were reported, however it is unexplained why the Iranian clinical trials website and the paper are different in terms of length of study. "Timepoint weeks 2‐4‐6‐8‐10 after beginning of trial". |
| Other bias | High risk | The Iranian clinical trial website says that
timepoints are weeks 2‐4‐6‐8‐10 after beginning of
trial, however, week 10 is not recorded in the paper
and neither is a 2‐week follow‐up period. "Patients
will be randomly allocated to topiramate +
risperidone (Group A) or placebo + risperidone
(Group B) for a 10‐week, double‐blind,
placebo‐controlled study. The contact author is also on the ethics committee at the university funding the study and is a peer‐reviewer for one of the journals in which some of their studies are published. |
Scahill 2015.
| Study characteristics | ||
| Methods | 8‐week parallel trial of guanfacine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Setting/ location: University of California (Los Angeles), Emory University, Massachusets General Hospital, University of Washington at Seattle, and Yale University, USA Sample size: guanfacine 30; placebo 32 Number of withdrawals/dropouts: 4 from guanfacine group (2 lack of efficacy, 2 AEs); 4 from placebo group all due to lack of efficacy Gender: 26/30 male in guanfacine group; 27/32 male in placebo group Mean age: 8.4 years IQ: not reported Baseline ABC‐I or other BoC: guanfacine ABC‐I 20.3; placebo 18.06 Concomitant medication: not reported Previous medications: not reported |
|
| Interventions | Intervention (guanfacine) for 8 weeks: starting dose
for all children was 1 mg/day. Children < 25kg
remained on 1 mg/day until day 14 and then increased
to 2 mg/day until day 28, and increased again to 3
mg/day for the remaining 4 weeks. Children 25 kg or
more increased to 2 mg/day at day 7 up to a maximum
of 4 mg/day by day 21 or 28 of the trial. Comparator (placebo) for 8 weeks: placebo administered for up to 8 weeks |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessment: weekly for the first 4 weeks, then week 6 and week 8 |
|
| Notes | Study start date: December 2011 Study end date: March 2014 Source of funding: "supported by NIMH grants to Dr. Scahill (R01MH083707), Dr. McDougle (RO1MH83739), Dr.McCracken (RO1MH083747), and Dr. King (R01MH86927); by a Yale Clinical and Transitional Science Award (UL1 RR024139) from the NIH National Center for Research Resources; and by Atlanta Clinical and Translational Science Institute, Emory University, which is supported by the NIH National Center for Advancing Translational Sciences under award UL1TR000454. Shire Pharmaceuticals provided active extended‐release guanfacine and placebo." Conflicts of interest: none declared Trial registry: NCT01238575 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Using permeated blocks to conceal allocation, eligible subjects were randomly assigned within site without stratification in a 1:1 ratio to extended‐release guanfacine or placebo for 8 weeks." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "Two blinded clinicians followed each subject: a treating clinician and an independent evaluator....To protect the blind, the independent evaluator did not discuss adverse effects or dosing". |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The treatment mask was broken for subjects who did not show a positive response. The blind was broken by the treating clinician, and treatment status was not disclosed to independant evaluators" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Consort diagram was provided outlining numbers at each stage of the trial, including the number analysed and number that completed the trial. All randomly assigned participants were included in the ITT analyses. |
| Selective reporting (reporting bias) | Unclear risk | Although the ABC‐hyperactivity was the primary outcome measure, other secondary measures such as the CGI were not reported. |
| Other bias | Unclear risk | Shire pharmaceuticals provided active extended‐release guanfacine and placebo. |
Shea 2004.
| Study characteristics | ||
| Methods | Parallel trial of risperidone versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: 7 investigational sites in Canada Sample size: 79 participants Number of withdrawals/dropouts: risperidone (2 total), "1 withdrew because of an adverse event (the result of an accidental overdose on day 2) and 1 withdrew because of insufficient response". Placebo (5 total) "1 withdrew because of an adverse event (an accidental medication overdose on day 16), 2 withdrew because of insufficient response, and 2 withdrew consent." Gender: 29/40 boys (risperidone); 32/39 placebo Mean age: 7.6 years (risperidone, 7.3 years (placebo) IQ: 14 participants had IQ > 85; 10 had IQ 71‐84, 20 had IQ 50‐70, and 22 had IQ 35‐49 Baseline ABC‐I or other BoC: ABC‐I 18.9 risperidone, 21.2 placebo Concurrent and previous medications: during the trial, anticholinergics could be initiated to treat emergent extrapyramidal symptoms after the Extrapyramidal Symptom Rating Scale (ESRS) had been completed. Prohibited medications included antipsychotics other than the study medication, antidepressants, lithium, _2‐antagonists, clonidine, guanfacine, cholinesterase inhibitors, psychostimulants, and naltrexone. A single anticonvulsant and/or medications for sleep or anxiety were permitted only in the case in which the participant was already taking them at a stable dose for the 30 days before enrolment. Similar restrictions were placed on the use of behaviour intervention therapy. Medications for pre‐existing organic disorders were allowed provided that the dose and schedule of administration were kept as constant as possible. |
|
| Interventions | Intervention (risperidone) for 8 weeks:
"risperidone oral solution 1.0mg/mL was
administered once daily in the morning at
0.01mg/kg/day on treatment days 1 and 2 and
increased to 0.02mg/kg/day on day 3. The dose could
be increased from day 8 by a maximal increment of
0.02mg/kg/day. After that, the dose could be
adjusted at the investigator's discretion at weekly
intervals by increments/ decrements not to exceed
0.02mg/kg/day. The maximal allowable dosage was
0.06mg/kg/day. (mean dose 0.06mg/day; mean
1.48mg/day)" Comparator (placebo) for 8 weeks: 1 mg/mL once daily increasing to 0.02 mg/kg/day |
|
| Outcomes | Primary outcomes
Secondary outcomes: none reported Timing of outcome assessments: baseline, and weeks 1, 2, 3, 5, 7 and 8 |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: Janssen‐Ortho Inc, Canada, and Johnson & Johnson Pharmaceutical Research and Development Conflicts of interest: none declared Trial registry: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Inadequate details |
| Allocation concealment (selection bias) | Unclear risk | Inadequate details |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient details |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient details |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Used an ITT analysis (participants who had received
at least 1 dose of study medication) LTFU: 2 in treatment group withdrew because of AE and 1 withdrew due to insufficient response |
| Selective reporting (reporting bias) | High risk | Sedation not reported as an AE |
| Other bias | High risk | Study authors note that measurements were made 7 times throughout the study however only baseline and endpoint data were reported. |
Sikich 2013.
| Study characteristics | ||
| Methods | Parallel trial of oxytocin versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: not stated Sample size: 25 (12 in oxytocin/oxytocin sequence; 13 in placebo/oxytocin) Number of withdrawals/dropouts: 1 in oxytocin/oxytocin group due to AEs Gender: oxytocin 12/12 were male; placebo 11/13 were male Mean age: oxytocin 10.6 years; placebo 10.0 years IQ: oxytocin: 4/12 had IQ < 70; placebo 10/13 had IQ < 70 Baseline ABC‐I or other BoC: not reported Concurrent medications: details not provided History of previous medications: details not provided |
|
| Interventions | Intervention (oxytocin) for 6 weeks: oxytocin
(Syntocinon; NOVARTIS) dosage was up to 32 IU (8
intranasal spray puffs) twice‐daily for 6 weeks.
Participants aged 3‐10 years titrated up to a
maximum dose of 24 IU. Participants aged 11‐17 years
titrated up to a maximum dose of 32 IU Comparator (placebo) for 6 weeks: placebo nasal spray |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: none reported Timing of outcome assessments: not reported |
|
| Notes | Study start date: March 2011 Study end date: April 2013 Source of funding: University of North Carolina, Chapel Hill Autism Speaks, USA Conflicts of interest: none declared Trial registry: NCT01944046 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "a computer generated randomization table was created by the research pharmacist and used to randomise participants" |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All efficacy assessments were carried out by an independent evaluator who was blinded to both side effects and group assignment" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants were analysed using an ITT analysis and baseline and endpoint QoL scores were recorded. |
| Selective reporting (reporting bias) | Low risk | The primary and secondary outcomes of interest were recorded on clinicaltrials.gov and all results were provided. |
| Other bias | Unclear risk | No significant differences in gender, race, age. Perhaps a slight difference in IQ ‐ oxytocin group 99 (22) and placebo 118 (19) however, several study authors are connected to many pharmaceutical companies. |
Sikich 2021.
| Study characteristics | ||
| Methods | 24‐week parallel trial of oxytocin versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: USA Sample size: oxytocin 146; placebo 144 Reasons for withdraws/dropouts: oxytocin 21 (AEs (5), clinical worsening (3), LTFU (3), participant withdrew (2), physician decision (1), did not have baseline ABC‐SW (2), did not have a postbaseline ABC SW (5)); placebo 19 (AEs (2), clinical worsening (2), LTFU (3), participant withdrew (4), physician decision (2), did not have a postbaseline ABC SW (6)) Gender: 242 male, 35 female Mean age: approximately 10.5 years across both groups IQ: details not provided Baseline ABC‐I or other BoC scale (mean and SD): oxytocin ABC‐Irritability 10.9 (SD7.83); placebo 12.6 (8.94) Concomitant medications: participants must be on stable psychotropic medication in the month prior to and during the study. Anticonvulsants and stimulants were allowed. Previous medications: details not provided |
|
| Interventions | Intervention (oxytocin) for 24 weeks: "Each
insufflation will deliver 8 IU or 24 IU of oxytocin.
A maximum of 3 insufflations at a time will be
required. Dosing will be flexible between 8 IU/day
and 80 IU/day, typically in two divided doses
delivered in the morning and in the afternoon. Doses
will typically increase by 8 IU twice daily (BID) at
week 2 and weeks 4 and 8 until achieving the target
dose of 24 IU BID at week 8. Subsequently doses may
be increased in 8 IU BID increments ONLY at each
visit until a maximum dose of 40 IU BID is
achieved.Each bottle's label will have its own
unique nonsequential randomly assigned number and
not a lot number to facilitate masking". Comparator (placebo) for 24 weeks: "This nasal spray will contain all of the ingredients that are in the active oxytocin spray in the same quantities, except oxytocin will NOT be added to the solution. It will be packaged using the same container system as the active oxytocin nasal spray. Each bottle's label will have its own unique nonsequential randomly assigned number and not a lot number to facilitate masking. Dose titration will occur using exactly the same criteria and procedures as for active study drug." |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: endpoint (24 weeks) |
|
| Notes | Study start date: August 2014 Study end date: June 2017 Funding: “Supported by a grant (U01HD073984) from the Eunice Ken[1]nedy Shriver National Institute of Child Health and Human Development through the Autism Centers of Excellence Program and the Department of Psychiatry and Behavioral Sciences at Duke University. The data and safety monitoring board was funded by a grant (UL1TR002489) from the National Center for Advancing Translational Sciences.” Conflicts of interest: details not provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly assigned in a 1:1 ratio, by means of a centralised randomisation table |
| Allocation concealment (selection bias) | Unclear risk | Participants were randomly assigned in a 1:1 ratio, by means of a centralised randomisation table |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind; "the trial physician, who was unaware
of the participant’s trial‐group assignment,
completed a physical examination, systematically
elicited a history of adverse events, verified
concomitant treatments, and, at visits after the
baseline visit, assessed current symptoms of autism
spectrum disorder using the Clinical Global
Impressions" "Scale of Improvement. Parents or guardians completed the Aberrant Behavior Checklist (ABC) and the Pervasive Developmental Disorders Behavior Inventory–Screening Version (PDDBI‐SV) at each visit..." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blind; "the trial physician, who was unaware
of the participant’s trial‐group assignment,
completed a physical examination, systematically
elicited a history of adverse events, verified
concomitant treatments, and, at visits after the
baseline visit, assessed current symptoms of autism
spectrum disorder using the Clinical Global
Impressions" "Scale of Improvement. Parents or guardians completed the Aberrant Behavior Checklist (ABC) and the Pervasive Developmental Disorders Behavior Inventory–Screening Version (PDDBI‐SV) at each visit..." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Several exclusions for "not having data" e.g. "2 Had no baseline ABC‐mSW data" |
| Selective reporting (reporting bias) | High risk | At least one of the outcomes on trials registry was not reported in the paper (CGI) |
| Other bias | Low risk | Nothing else identified |
Soorya 2021.
| Study characteristics | ||
| Methods | 6‐month parallel trial of memantine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: 2 outpatient clinics in the USA Sample size: 23 in total (memantine (12); placebo (11)) Reasons for withdrawals/dropouts: 5 in memantine group discontinued (AEs (1), time constraints (1), lack of efficacy (2), LTFU (1)); 3 in placebo group discontinued (time constraints (1), AEs (2)) Gender: 20 male, 3 female Mean age: approximately 9.5 years across both groups IQ: approximately 77 across both groups Baseline ABC‐I or other BoC scale: ABC‐I was < 17 at baseline Concomitant medications: "stable on up to two concomitant psychotropic medications 30 days before randomization" Previous medications: details not provided |
|
| Interventions | Intervention (memantine) for 6 months: "memantine
will be initiated at 3 mg. The dose will be
increased every week by 3 mg for a maximum of 12mg
for subjects weighing ≥ 60kg, 9mg for subjects
weighing ≥ 40 kg but <60 kg, and 6 mg for
subjects weighing ≥ 20 kg but < 40kg." Comparator (placebo): equivalent placebo for 6 months |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: tolerability Timing of outcome assessments: every 2 weeks |
|
| Notes | Study start date: December 2011 Study end date: October 2015 Funding:"No funding was received for this article." Conflicts of interest: study medication was provided through an in‐kind contribution from Forest Pharmaceuticals. Most of the study authors received consultation fees or other support from pharmaceutical companies. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information on how the sequence was generated. Quote: "Participants (n = 23), ages 6–12, were randomized at a 1:1 ratio to treatment with memantine or placebo by the study pharmacist at the Icahn School of Medicine at Mount Sinai (original coordinating site)." |
| Allocation concealment (selection bias) | Unclear risk | Randomisation process unclear, pharmacist may have known the next allocation Quote: "Participants (n = 23), ages 6–12, were randomized at a 1:1 ratio to treatment with memantine or placebo by the study pharmacist at the Icahn School of Medicine at Mount Sinai " |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | All participants and investigators were blind to group assignment until the blind was broken by the study statistician at the end of the study. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All participants and investigators were blind to group assignment until the blind was broken by the study statistician at the end of the study. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Large attrition from treatment group (near 50%), denominator unclear for outcomes reported |
| Selective reporting (reporting bias) | Low risk | Appears to match registry |
| Other bias | High risk | Study medication was provided through an in‐kind contribution from Forest Pharmaceuticals. |
Sprengers 2021.
| Study characteristics | ||
| Methods | 13‐week parallel trial of bumetanide versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: a tertiary hospital in the Netherlands Mean age: 10.5 years Mean IQ: 101 Gender: bumetanide 68% male; placebo 69% male Sample size: 47 randomised to bumetanide group, 45 randomised to placebo group Reasons for dropouts: 4 participants (2 from each group) discontinued prior to collecting the first outcome data. "One participant in the placebo arm stopped because of nonspecific somatic complaints and another because of intractable resistance to venipunctures. The two discontinued treatments in the bumetanide arm were because of inability to adhere to potassium supplementation and one because of a school crisis requiring immediate psychiatric intervention." Baseline ABC‐Irritability scores: bumetanide 14.3 (8.2); placebo 14.5 (7.9) Concomitant medications: details not provided Previous medications: 30% had received stimulants and 6% antipsychotics in the bumetanide group while 24% and 11% from the placebo group had received stimulants and antipsychotics respectively. |
|
| Interventions | Intervention (bumetanide) for 13 weeks: twice daily
bumetanide liquid with a concentration of 0.5 mg/mL
for 91 days (13 weeks). The mean dose of bumetanide
was 0.0482 mg/kg/day. Comparator (placebo) for 13 weeks: twice daily placebo liquid with a concentration of 0.5 mg/mL |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: baseline, day 4, day 7, day 14, day 28, day 56, day 91 (endpoint) |
|
| Notes | Study start date: June 2016 Study end date: December 2018 Funding: "The study was funded by the Netherlands Organisation for Health Research and Development (ZonMw; GGG ‐ #836041015)" Conflicts of interest: some study authors received grants for other studies. Trial registry: details not provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The sequence was generated with restricted randomisation using permuted block design with block sizes randomly varying from 2 to 4 to 6 participants |
| Allocation concealment (selection bias) | Low risk | Undistinguishable medication kits were numbered accordingly by Neurochlore, the company who provided the study medication, and were shipped to the local trial pharmacy where a sealed copy of the randomisation sequence was stored for emergency unmasking. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants, parents, healthcare providers, and outcome assessors were masked for randomisation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | To secure masking of the outcome assessors for possible (diuretic) side effects of bumetanide, medical checks and handling of AEs during the treatment and wash‐out phase were performed by a team at the paediatric nephrology department of the nearby Wilhelmina Children’s Hospital who were also masked for randomisation. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Modified ITT with a high (relative) number of dubious exclusions. Quote: "Outcome measures of six participants had to be excluded from analysis. One participant appeared to have started extensive dyslexia training during the medication phase. The outcomes of the other five participants were excluded because parents explicitly mentioned unreliable reporting on outcome measures due to stress of, for example, pending divorce lawsuits or conflicts to obtain access to health care provisions." |
| Selective reporting (reporting bias) | Low risk | Prespecified primary outcomes reported (Social Responsiveness Scale‐2 at 91 days) |
| Other bias | Low risk | No obvious other sources of bias |
Squassante 2018.
| Study characteristics | ||
| Methods | 12‐week parallel trial of balovaptan versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: 26 sites across USA Sample size: placebo (5), balovaptan 1.5 mg (32), balovaptan 4 mg (77), balovaptan 10 mg (39) Number of withdrawals/dropouts: missing postbaseline efficacy assessment placebo (3), balovaptan 1.5 mg (2), balovaptan 4 mg (4), balovaptan 10 mg (1) Gender: all paticipants were male Mean age: placebo 24.7 (6.3); balovaptan 1.5 mg 28.2 (7.8); balovaptan 4.0 mg 24.5 (6.6); balovaptan 10 mg 23.9 (5.0) IQ: details not provided Baseline ABC‐I or other BoC: baseline scores not reported Concomitant medications: "before enrollment and throughout the study, 81 to 86% of participants across treatment groups were on concomitant pharmacological treatments, with the most common being selective serotonin reuptake inhibitors (28 to 35% across groups). Antipsychotic agents were taken by 15 to 28% of participants across treatment groups, and central nervous system stimulants were taken by 13 to 26% of participants. There were no imbalances in the percentage of participants taking psychotropic drugs across the treatment arms." Previous medications: details not provided |
|
| Interventions | Intervention (balovaptan) for 12 weeks: 1.5 mg, 4.0
mg, or 10 mg: balovaptan or placebo was administered
orally daily for 12 weeks, with the first dose on
day 1 after predose and baseline assessments, with a
6‐ to 7‐week follow‐up period after the last dose.
Study medication was provided as balovaptan 0.5‐,
4‐, and 5‐mg hard capsules or matching placebo
capsules. Comparator (placebo) for 12 weeks: matching placebo |
|
| Outcomes | Primary outcomes:
Secondary outcomes: QoL, measured using the PedsQL (WHO 1998) Timing of outcome assessments: baseline and week 12 (endpoint) |
|
| Notes | Study start date: February 2013 Study end date: February 2017 Funding: "Funding was provided by F. Hoffmann‐La Roche Ltd. for the study and third‐party writing assistance, which was provided by Dinakar Sambandan, PhD, of Envision Pharma Group". Conflicts of interest: the majority of the study authors were employees of the funder (F.Hoffmann‐La Roche Ltd.). Trial registry: NCT01793441 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants, site personnel, and the sponsor were blinded to treatment assignments, with the exception of the individual responsible for pharmacokinetic data analysis and the internal monitoring committee/scientific oversight committee for specified data reviews. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants, site personnel, and the sponsor were blinded to treatment assignments, with the exception of the individual responsible for pharmacokinetic data analysis and the internal monitoring committee/scientific oversight committee for specified data reviews. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition |
| Selective reporting (reporting bias) | High risk | Percentage of participants with suicidality, as measured by the Columbia‐Suicide Severity Rating Scale (C‐SSRS) was a primary outcome on trial reg (NCT01793441) but is not reported. Doesn't report PedsQL at baseline. |
| Other bias | High risk | Pharma company funded the study and was involved in the analysis. 'F. Hoffmann–La Roche AG, Basel, Switzerland provided support for the study and participated in the study design, conducted the study, undertook data collection, management, and interpretation as well as preparation, review, and approval of the manuscript. Funding was provided by F. Hoffmann–La Roche Ltd. for the study and third‐party writing assistance, which was provided by K. H. Condon of Envision Pharma Group' |
Takamitsu 2015a.
| Study characteristics | ||
| Methods | 6‐week cross‐over trial of oxytocin versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: outpatient clinic of The University of Tokyo Hospital, Japan Sample size: oxytocin‐placebo (10), placebo‐oxytocin (10) Number of withdrawals/dropouts: oxytocin‐placebo (1), placebo‐oxytocin (1) ‐ both due to self‐termination Gender: all participants were male Mean age: oxytocin‐placebo = 35.1, placebo‐oxytocin = 29.3 IQ: details not provided Baseline ABC‐I or other BoC: oxytocin‐placebo QoL 3.25 (0.65); placebo‐oxytocin 2.68 (0.82) Concomitant medications: details not provided History of previous medications: "moreover, a comparable effect size was also seen in psychotropic‐free participants after excluding one participant with continual medication of serotonin‐norepinephrine reuptake inhibitors for his recurrent major depression (d = 0.74)." |
|
| Interventions | Intervention (oxytocin) for 6 weeks: the participants
received oxytocin (24 IU, Syntocinon‐Spray;
Novartis) in the morning and afternoon over 6
consecutive weeks (i.e. 48 IU/day). Comparator (placebo) for 6 weeks: in the same way (24 IU placebo Syntocinon‐Spray; Novartis) in the morning and afternoon over 6 consecutive weeks (i.e. 48 IU/day). |
|
| Outcomes | Primary outcomes: none reported Secondary outcomes: QoL (WHO‐QoL) (WHO 1998) |
|
| Notes | Study start date: March 2012 Study end date: April 2013 Funding: "A part of this study is a result of the ‘Development of biomarker candidates for social behaviour’ project under the Strategic Research Program for Brain Sciences by the MEXT (K.K. and H.Y.) and the Centre of Innovation Program from Japan Science and Technology Agency (HY)". Conflicts of interest: "The authors declare no conflict of interests". Trial registry: UMIN000007122 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomised order |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The manager completely covered the bottle labels to keep drug types unknown to all participants, their families, experimenters, clinicians and assessors including ADOS administrators and assessors" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Details not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants were accounted for and included in the analysis. |
| Selective reporting (reporting bias) | Low risk | Primary outcome measures reported per trial reg ‐ https://rctportal.niph.go.jp/en/detail?trial_id=UMIN000007122 |
| Other bias | Low risk | No other sources of bias identified |
Troost 2005.
| Study characteristics | ||
| Methods | Parallel discontinuation trial of risperidone versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria: on effective psychotropic drug treatment for disruptive behaviour Location/setting: "study participants were recruited from Groningen and Utrecht University Child and Adolescent Psychiatry Centres", the Netherlands Sample size: 24 Number of withdrawals/dropouts: Gender: 22/24 were male Mean age: risperidone 9 years; placebo 8 years IQ: mental age of ≥ 18 months Baseline ABC‐I or other BoC: ABC‐I risperidone 11.1, placebo 12.7 Concomitant medications: provided that no changes in dose during the study would occur. Anticonvulsants used for the treatment of a seizure disorder were permitted if the dose had been stable for at least 4 weeks and the patient was seizure‐free for at least 6 months. 20/24 were not taking any medications concurrently. 3 were on stimulants and 1 was on stimulants and anticonvulsants. History of previous medications: 19/24 had not received any prior psychotropic drugs, 3 had been on stimulants, 1 on antipsychotics and 1 on a stimulant and anticonvulsant. |
|
| Interventions | Intervention (risperidone) for 8 weeks: risperidone
mean daily dose of 1.8 mg/day or maximum daily dose
of 2.5 mg (children weighing < 45 kg) or 3.5 mg
(children ≥ 45 kg) Comparator (placebo) for 8 weeks: "for the placebo group, entry doses were reduce by 25% per week for 3 consecutive weeks. After full placebo substitution, the placebo group remained on placebo for 8 weeks." |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: weekly during the discontinuation phase |
|
| Notes | Study start date: details not reported Study end date: details not reported Source of funding: "Korczak Foundation" ‐ EBMH publication Conflicts of interest: "Dr. Buitelaar is a paid consultant to or has received support from Janssen Cilag BV, Abbott, VCB, Shire, Medice, and Eli Lilly; Dr. Minderaa is a paid consultant to Eli Lilly and Janssen Cilag BV; and Dr. Scahill is a paid consultant to Janssen Pharmaceutica Inc., Bristol‐Myers Squibb, and Pfizer."Study medications were donated by Janssen Cilag BV." Trial registry: not reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation sequence was generated by an outside vendor and was stratified by investigational site. |
| Allocation concealment (selection bias) | Low risk | Risperidone and placebo were supplied by the pharmacist at each site as matching capsules in identical packages. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Patients, parents and evaluators all were unaware of assignment to placebo or risperidone. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Patients, parents and evaluators all were unaware of assignment to placebo or risperidone. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Sedation was not reported as an AE. No LTFU reported
by the study authors. ITT analysis: an ITT analysis was used for all participants enroled by using the LOCF for all measures. |
| Selective reporting (reporting bias) | High risk | The ABC‐I scores were reported in full for both the open‐label and discontinuation phases of the trial. However, the CGI scores were only reported at baseline. |
| Other bias | High risk | Dr. Buitelaar is a paid consultant to or has received
support from Janssen Cilag BV, Abbott, VCB, Shire,
Medice, and Eli Lilly; Dr. Minderaa is a paid
consultant to Eli Lilly and Janssen Cilag BV; and
Dr. Scahill is a paid consultant to Janssen
Pharmaceutica Inc., Bristol‐Myers Squibb, and
Pfizer. Only 8/24 with autism were in discontinuation phase despite title mentioning ASD. Baseline ABC‐I was relatively low. |
Umbricht 2017.
| Study characteristics | ||
| Methods | Cross‐over study of vasopressin versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: multicenter (3 sites, universities in the USA) Sample size: first phase vasopressin followed by placebo, 9 were randomised first phase; placebo followed by RG7713, 10 were randomised. 1 participant was excluded from the vasopressin analysis. Number of withdrawals/dropouts: none reported Gender: all participants were male Mean age: 23.4 years (5.1) IQ: 100 (14.5) Baseline ABC‐I or other BoC: intervention ABC‐I 3.0 (3.9); placebo 3.0 (3.9) Concomitant medications: prohibited medications included all medications except those for ongoing treatment of symptoms of irritability, mood disorders, anxiety and hypertension, and paracetamol/acetaminophen for treatment of AEs. CYP3A4 inhibitors and inducers, or P‐gp substrates must not be taken ≤ 4 weeks before the study. History of previous medications: details not provided |
|
| Interventions | Vasopressin‐placebo: sequence 1. Participants
received a single dose of 20 mg vasopressin during
treatment visit 1 followed by placebo during
treatment visit 2. "A single 20 mg dose of
vasopressin or placebo was administered
intravenously as a 2‐h infusion to each subject on
two different days (treatment visits 1 and 2)
separated by a 7–14‐ day washout period." Placebo‐vasopressin: sequence 2. Participants received a single dose of placebo followed by vasopressin. |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: Timing of outcome assessments: baseline and at the end of each phase of cross‐over study |
|
| Notes | Study start date: December 2011 Study end date: March 2013 Source of funding: the study was funded by a pharmaceutical company (F. Hoffmann‐La Roche) and the drug was also supplied by this company. Conflicts of interest: none declared Trial registry: NCT01474278 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Subjects were randomized to sequence 1 or 2 using a randomized treatment schedule that was developed by the study sponsor for each site and incorporated into double‐blind (investigator and subject) treatment labelling" |
| Allocation concealment (selection bias) | Low risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "Subjects were randomized to sequence 1 or 2 using a randomized treatment schedule that was developed by the study sponsor for each site and incorporated into double‐blind (investigator and subject) treatment labeling." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Subjects were randomized to sequence 1 or 2 using a randomized treatment schedule that was developed by the study sponsor for each site and incorporated into double‐blind (investigator and subject) treatment labeling." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All were included in the analysis |
| Selective reporting (reporting bias) | Unclear risk | ABC‐I was reported at baseline but only total ABC was reported at endpoint. |
| Other bias | High risk | The study was funded by pharma companies and the drug was also supplied by them. |
Unis 2002.
| Study characteristics | ||
| Methods | 4‐week parallel study of secretin versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Setting: not described Sample size: 85 Number of dropouts: 4 participants discontinued, the infusion was not given (2), decided against the infusion (1), did not return for follow‐up assessment (1). Another child developed illness and a fever after infusion and did not complete the study. Mean age: 6.5 years Gender: details not provided IQ: mean IQ of 55 Baseline ABC‐I or other BoC: scores were > 57 at baseline Concomitant medications: psychotropic medications were not permitted during the study or in the 6 months prior to the study except for "occasional symptomatic use for sleep, etc" Previous medications: details not provided |
|
| Interventions | Intervention (secretin): single infusion of 0.4 ug/kg
synthetic secretin given intravenously over a
2‐minute period, or single infusion of 2 CU/kg
biologic secretin given intravenously over a
2‐minute period Comparator (placebo): single infusion of placebo intravenously over a 2‐minute period |
|
| Outcomes | Primary outcomes: ABC‐I (change from baseline) (Aman 1985) Secondary outcomes: none reported Timing of outcome assessments: baseline and week 4 (endpoint) |
|
| Notes | Study start date: June 1999 Study end date: May 2000 Funding: "Unis, Munson, Abbott, and Dawson were supported by a grant from the NICHD and the NIDCD (PO1HD34565). Dr. Rogers was supported by a grant from the NICHD (PO1HD35468). Drs. Rogers, Gabriels, and Goldson were also supported by ADD grant 90dd041401 and MCH grant MCJ08941301. Dr. Goldson was also supported by a grant from the NCRR (MO1‐RR00069)". Conflicts of interest: none declared Trial registry: NCT00065962 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Children were then randomly assigned to treatment group" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Children were then randomly assigned to treatment group" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "parents, teachers and investigators were all blind to treatment (allocation)" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "parents, teachers and investigators were all blind to treatment (allocation)" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 5 participants were reported to have not completed the study however only 77/85 results were reported for ABC‐I. Up to 40% missing data (see table 1) for teacher‐reported ABC‐I |
| Selective reporting (reporting bias) | Low risk | Outcome measures included in trials registry reported |
| Other bias | High risk | All participants were responders to secretin from previous open‐label trial |
VanAndel 2022.
| Study characteristics | ||
| Methods | 13‐week parallel trial of bumetanide versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: The Netherlands Sample size: 38 (19 to each group) Reasons for withdrawals/dropouts: 4 in each group dropped out (bumetanide: discontinued treatment (3), excluded due to incomplete parent reports (1); placebo group discontinued treatment (2), excluded due to incomplete or unreliable parent reports (2)) Gender: 22 male, 8 female Mean age: bumetanide group 10.9 years, placebo group 8.7 years IQ: approx 99 in both groups Baseline ABC‐I or other BoC scale: bumetanide group 13.1, placebo group 17.1 Diagnoses: 22/30 participants had an ASD diagnosis, of whom 15 only had an ASD diagnosis (another 6 had ASD and ADHD, and 1 participant had ASD and epilepsy) Concomitant medications: during the trial 68.4% in both groups did not receive any other medications. Of those who were taking other medications 15.8% in bumetanide group and 5.3% in placebo group were taking antipsychotics; 5.3% in placebo group were taking a benzodiazepine in addition to an antipsychotic; 15.8% in the placebo group were taking an anticonvulsant; 10.5% in the bumetanide group were taking an SSRI; and 5.3% in both groups were taking an SSRI in addition to an antipsychotic. Previous medications: 47.4% in both groups did not take medications prior to the trial. Of those who took medications 21.1% in bumetanide group and 10.5 in placebo group were taking antipsychotics; 5.3% in the placebo group were taking a benzodiazepine; 5.3% and 31.6% in the bumetanide and placebo groups respectively were taking an anticonvulsant; 10.5% and 5.3% in the bumetanide and placebo groups respectively were taking an SSRI; 31.6% and 26.3% in the bumetanide and placebo groups respectively were taking stimulants; 5.3% and 10.5% in the bumetanide and placebo groups respectively were taking an alpha adrenergic agonist. |
|
| Interventions | Intervention (bumetanide) for 13 weeks: maximum of 1
mg bumetanide twice daily followed by a 28‐day
washout period Comparator (placebo) for 13 weeks: equivalent placebo twice daily followed by a 28‐day washout period |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: AEs were monitored on days 4, 7, 14, 28, 56, 91, and 119; other outcomes were measured at day 91 (endpoint) and day 119 following washout |
|
| Notes | Study start date: June 2017 Study end date: June 2019 Funding: "This study was supported by a grant from Dutch Brain Foundation (Hersenstichting #HA2015‐01‐04)." Conflicts of interest: HB (the contact author) has reported being a shareholder of Aspect Neuroprofiles BV, which provides EEG‐analysis services for clinical trials. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Sequence generation, concealment, and treatment allocation was overseen by a third‐party not involved in the study (i.e., Julius Center, a consultant support agency for clinical research and trials located in the UMC Utrecht). Restricted randomization was used with permuted block design randomly varying between two, four, and six participants. Treatment allocation was done automatically using minimization with a probability of 0.75 on the participant factors active epilepsy (y/n), IQ (55–75; 76–110; >110) and study center (UMC/Jonx)" |
| Allocation concealment (selection bias) | Low risk | "Sequence generation, concealment, and treatment allocation was overseen by a third‐party not involved in the study" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants, parents, healthcare providers, and outcome assessors were blinded for randomisation |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants, parents, healthcare providers, and outcome assessors were blinded for randomisation |
| Incomplete outcome data (attrition bias) All outcomes | High risk | > 25% dropout, "one participant was excluded from analyses as questionnaires were not reliable" |
| Selective reporting (reporting bias) | Unclear risk | Can't find outcomes on either trial reg (EudraCT trial registry (2016‐002875‐81) and Dutch trial registry (NL6178) |
| Other bias | Low risk | Funder had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript |
Veenstra‐VanderWeele 2017.
| Study characteristics | ||
| Methods | 12‐week parallel trial of arbaclofen versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: 25 sites across USA Sample size: 150 were randomised, arbaclofen 76, placebo 74 Mean age: 11.6 years (range 5‐21 years) Mean IQ: IQ > 70 in approximately 50% of participants Gender: arbaclofen 63% were male; placebo 61% were male Baseline ABC‐I scores: arbaclofen group 17.2; placebo 15.6 Reasons for dropouts: arbaclofen 15 discontinued (LTFU (1), AEs (8), protocol violation (1), withdrew consent (4), other (1)). Placebo 5 discontinued (AE (2), withdrew consent (2), other (1)) Concomitant medications: arbaclofen 14 were on concomitant psychoactive medication; placebo: 12 were on concomitant psychoactive medication Previous medications: details not provided |
|
| Interventions | Intervention (arbaclofen) for 12 weeks: starting dose
of arbaclofen was 5 mg twice daily increasing to 10
mg twice daily up to a maximum dose of 10 mg 3 times
daily for children < 12 years. Children ≥ 12
years could have 15 mg 3 times daily Comparator (placebo) for 12 weeks: matching placebo tablets |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: baseline and week 12 (endpoint) |
|
| Notes | Study start date: May 2011 Study end date: September 2012 Funding: Seaside Therapeutics (pharmaceutical company) Conflicts of interest: various study authors received funding from and consulted with pharmaceutical companies. Trial registry: NCT01288716 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised 1: 1 to either arbaclofen or placebo according to a centrally generated randomisation list, with stratification by age (5–11 or 12–21 years) and concomitant use of psychoactive medication. |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Blinding was maintained by utilizing identical tablets containing either STX209 or placebo" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Apart from "Double‐blinded" details were not provided. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Large dropout (20%) with many dropping out in treatment group due to AEs |
| Selective reporting (reporting bias) | Low risk | Same primary outcome on trial reg |
| Other bias | High risk | Funded by Seaside Therapeutics and the team has interests in a range of pharma companies |
Wasserman 2006.
| Study characteristics | ||
| Methods | Parallel trial of levetiracetam versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/ Setting: autism centre, USA Sample size: 20 (10 in each group) Number of withdrawals/dropouts: 1 from placebo group dropped out due to increased hyperactivity and 1 dropped out of levetiracetam group after having a seizure, and another due to lack of efficacy. Gender: 8 male levetiracetam group, 9 male in placebo group Mean age: 8.72 IQ: 75.75 Baseline ABC‐I or other BoC: not reported adequately Concomitant medications: patients were free of any psychotropic medications for 4 weeks before participation and no concomitant psychiatric medications or initiation of new behavioral therapies was allowed during the study. History of previous medications: details not provided |
|
| Interventions | Intervention (levetiracetam) for 10 weeks: commenced
at 125 mg/day up to maximum of 20‐30 mg/kg/day (mean
maximum dose 862.50 ± 279.19 mg/day) Comparator (placebo) for 10 weeks: equivalent placebo |
|
| Outcomes | Primary outcomes: ABC‐I (although not reported) Secondary outcomes: none reported Timing of outcome assessments: assessed weekly for first 4 weeks then bi‐weekly for next 6 weeks |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: supported by a grant from UCB Pharma Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Levetiracetam and placebo were distributed in identical forms" no further details |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided. Only that it was double‐blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Details not provided |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Primary outcomes were the CGI and the parent and teacher‐rated ABC subscales. Data were not supplied, only "there were no significant findings on ABC subscale of irritability" (and Z score, SE, and P value provided). |
| Selective reporting (reporting bias) | High risk | ABC‐I baseline not reported, and endpoint figures only reported as standard score, rather than by group. |
| Other bias | Unclear risk | Study supported by pharmaceutical company ‐ nature and extent of their involvement is unclear |
Willemsen‐Swinkels 1995.
| Study characteristics | ||
| Methods | Cross‐over trial of naltrexone versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria: details not provided Location/setting: the Netherlands Sample size: 33 Number of withdrawals/dropouts: one 28‐year old woman (with autism and self‐injurious behaviour) "manifested an acute and severe increase in SIB and acting out behavior. She had to be isolated for several weeks, and her condition improved only gradually after naltrexone treatment was stopped and lithium treatment was instituted" Gender: 27 men, 6 women Mean age: 29 years IQ: details not provided Baseline ABC‐I or other BoC: not an outcome Concomitant medications: details not provided History of previous medications: details not provided |
|
| Interventions | Intervention (naltrexone) for 4 weeks: after 2
weeks of placebo capsule taken once daily,
naltrexone hydrochloride was given at 100 mg (mean
1.61 (0.24) mg/kg) in 1 dose at the start of week 3.
For the remainder of that week, the participant
received a placebo capsule every morning. From week
4, naltrexone was given at 50 mg per day for 4
weeks. This was followed by a 4‐week washout period
then cross‐over to continue on placebo. Comparator (placebo) for 4 weeks: matching placebo tablets |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: none reported Timing of outcome assessments: participants were observed twice at baseline, 6 and 24 h after the single‐dose administration, and after 2 and 4 weeks of daily treatment |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: Janusz Korczak Foundation, Huizen Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided apart from "double‐blinding used" |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Treatment doses were changed for second cross‐over phase after review of outcome measures, implying that assessors or investigators knew which group was being given naltrexone in first phase ‐ i.e. not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 1 participant didn't complete trial due to AEs detailed ‐ data were excluded due to early discontinuation (week 2 of 16) |
| Selective reporting (reporting bias) | High risk | Self‐injurious behaviour was measured using the ABC‐Stereotypies subscale. The authors mention that "it included three items on SIB". Incorrect. The ABC‐Stereotypies subscale does not. |
| Other bias | High risk | Active treatment was provided in part by employee of pharmaceutical company. Nature of funding support unclear. Participant details were not provided in terms of age, gender, diagnosis, rate of SIB etc, in addition to incorrectly claiming to have assessed SIB using the ABC |
Willemsen‐Swinkels 1996.
| Study characteristics | ||
| Methods | Cross‐over trial of naltrexone versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria: details not provided Location/ Setting: the Netherlands Sample size: 20 total (23 originally randomised) Number of withdrawals/dropouts: 2 children were excluded from analysis because "they had taken up the habit of chewing the capsules", and 1 participant dropped out after the first treatment due to parents withdrawing consent. Gender: 16 male, 4 female Mean age: 5.5 years IQ: details not provided Baseline ABC‐I or other BoC: naltrexone ABC‐I 18.5, placebo 14 Concomitant medications: participants were free of psychotropic drugs for at least 6 weeks before the study. 1 participant with epilepsy was treated with carbamazepine in a fixed dosage during the study period. None of the participants had previously been treated with psychotropic drugs. History of previous medications: details not provided |
|
| Interventions | Intervention (single‐dose naltrexone) for 4 weeks:
naltrexone was given at 40 mg (approximately 2
mg/kg) in a single‐dose capsule. After 11 weeks,
this group was given a placebo in a matched capsule.
Long‐term daily dose study 1996: after a 2‐week
baseline period, naltrexone was given at 20 mg per
day (approximately 1 mg/kg) over 4 weeks, with the
exception of 1 participant with the weight of 42 kg
who was given 40 mg per day over 4 weeks. Comparator (placebo) for 4 weeks: matching placebo tablet was given daily over 4 weeks |
|
| Outcomes | Primary outcomes: irritability, measured using the
ABC‐Irritability subscale (Aman 1985) Secondary outcomes: none reported Timing of outcome assessments: 2 weeks before baseline, baseline, day 1 and day 2 (for each phase) |
|
| Notes | Study start date: details not reported Study end date: details not reported Source of funding: supported by Janusz Korczak Foundation. Du Pont Pharma supplied part of the drug required. Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Further details not provided |
| Allocation concealment (selection bias) | Unclear risk | Further details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Details not provided |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Baseline ABC‐I scores were significantly higher in the naltrexone group compared to placebo. |
| Selective reporting (reporting bias) | Unclear risk | Results only graphically presented |
| Other bias | High risk | Only single dosage used. Active treatment supplied in part by pharmaceutical company. The nature of foundation support is unclear. |
Wink 2016.
| Study characteristics | ||
| Methods | Parallel trial of N‐acetylcysteine versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: USA Sample size: N‐acetylcysteine 13; placebo 12 Number of withdrawals/dropouts: N‐acetylcysteine 3 (2 lLTFU, 1 AE); placebo 3 ( 2 LTFU, 1 AE) Gender: 24/31 male Mean age: N‐acetylcysteine 7.6 and 8.2 years IQ: 86 Baseline ABC‐I or other BoC: ABC‐I N‐acetylcysteine 17.0, placebo 18.3 Concomitant medications: 16/31 were taking other medications. Participants taking concomitant psychotropic medications, must be taking the medication at a constant dose for 60 days with no dose changes planned for the duration of the trial. History of previous medications: details not provided |
|
| Interventions | Intervention (N‐acetylcysteine) for 12 weeks: started
at 300 mg/day for people weighing 15‐30 kg. For
people weighing > 30 kg, NAC was started at 600
mg/day. This was titrated to the target dose of 60
mg/kg/day in 3 divided doses and a maximum dose of
4200 mg/day over the first 3 weeks, then remained
stable in the last 9 weeks of the study. Dose
reductions due to AEs were permitted at any
time. Comparator (placebo) for 12 weeks: equivalent placebo |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: baseline, and weeks 4, 8 and 12 |
|
| Notes | Study start date: December 2006 Study end date: November 2009 Source of funding: "Dr. Wink’s current research is supported by the Simons Research Foundation, Autism Speaks, Riovant Sciences Ltd, and Cures Within Reach. Dr. Wink has also served as a past consultant for Otsuka. Dr. Erickson is a past consultant to Alcobra Pharmaceuticals, the Roche Group, and Novartis. Dr. Erickson holds non‐related IP held by CCHMC and Indiana University. Dr. Erickson receives research grant support from the John Merck Fund, Cincinnati Children’s Hospital Medical Center, Autism Speaks, the National Fragile X Foundation, The Roche Group, Neuren Pharmaceuticals, and Riovant Sciences Ltd. Dr. Adams, Dr. Wang, Dr. Klaunig, Dr. Plawecki, Dr. Posey, and Dr. McDougle report no potential conflicts of interest. This study was funded by the Autism Speaks." Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Following screening and baseline measures, participants were randomised 1:1 via computer ‐ by the investigational pharmacy". |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "all participants, guardians and investigators remained blind to study assignment" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "all participants guardians and investigators remained blind to study assignment" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 6 participants from a total of 31 (19%) withdrew from the study after baseline and 25 participants were included in the final analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported at baseline and endpoint in both the paper and clinical trials registry. |
| Other bias | Low risk | None identified |
Wink 2018.
| Study characteristics | ||
| Methods | 5‐week cross‐over study of riluzole versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria: "participants prescribed > 2 psychotropic drugs targeting irritability, taking medications with known interactions with riluzole or prescribed concomitant glutamatergic or GABA (A) modulating drugs." Location/setting: the USA Mean IQ: details not reported Mean age: 16.0 years Gender: 6/7 were male Sample size: 8 in total Number analysed: 7 in total Reasons for dropouts: "one participant withdrew due to worsening aggressive behavior necessitating adjustment of his concomitant psychotropic medications after receiving five doses of study drug." Baseline ABC‐I or other BoC scale: riluzole ABC‐I 24.29 (6.2); placebo 25.71 (7.3) Current or previous medications:
|
|
| Interventions | Intervention (riluzole): initially dosed at 50
mg/day. Dosing was then increased by 50 mg weekly to
a maximum potential optimal dose of 200 mg/day (100
mg twice daily) by week 4. Comparator (placebo): initially dosed at 50 mg/day. Dosing was then increased by 50 mg weekly to a maximum potential optimal dose of 200 mg/day (100 mg twice daily) by week 4 |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: screening, baseline, weeks 3, 5, 7, and 12 |
|
| Notes | Study start date: September 2013 Study end date: May 2015 Funding: "This study was funded by the Center for Clinical and Translational Science and Training at the University of Cincinnati via an Institutional Clinical and Translational Science Award, NIH/NCRR Grant No. 8UL1TR000077‐04" Conflicts of interest: "The authors declare that they have no interests that compete directly with this work, though LKW, CRT, RSC, EVP, and CAE do receive research support from various sources for other work". Trial registry: NCT02081027 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Participants were randomized by the CCHMC investigational pharmacy" |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Participants, guardians, and investigators remained blind to study assignment throughout the study" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Participants, guardians, and investigators remained blind to study assignment throughout the study" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The 7 participants who completed the trial were included in all the analyses. |
| Selective reporting (reporting bias) | Low risk | The ABC‐I and CGI were the only outcomes listed on the trials registry. They were reported in full. |
| Other bias | Low risk | No other bias sources identified |
Woodard 2007.
| Study characteristics | ||
| Methods | 4‐week cross‐over trial of dextromethorphan versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria: details not provided Location/setting: an educational treatment programme for people with autism and related developmental disorders (USA) Sample size: 8 in total (cross‐over). Number of withdrawals/dropouts: none reported Gender: 7 male, 1 female Mean age: 13 years IQ: not reported Baseline ABC‐I or other BoC: ABC‐I of > 16 Concomitant medications: 3 were prescribed Risperdal and 1 participant received Depakote, Risperdal, Zoloft, and Seroquel. History of previous medications: not reported |
|
| Interventions | Intervention (dextromethorphan) for 4 weeks:
each participant was administered
dextromethorphan (Delsym) at the recommended dosage
of 30 mg dextromethorphan, hydrobromide) every 12 h
for ages 6‐12, or 60 mg dextromethorphan
hydrobromide every 12 h for ages 12 and over. Comparator (placebo) for 4 weeks: each participant was administered an identical volume of a similar sweetened syrup, packaged by a pharmacist in the same brown bottles as the Delsym. |
|
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessment: baseline, week 4, endpoint (end of 2nd phase) |
|
| Notes | Study start date: not reported Study end date: not reported Source of funding: "this research was supported by a grant from Celltech Pharmaceuticals, Inc., a grant from the John Trimble Fund of The Groden Center, and NICHD grant HD30615." Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not provided |
| Allocation concealment (selection bias) | Unclear risk | Details not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Details not provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | There were only 8 participants and while individual endpoint data are provided for the ABC and each subscale, as well as the CGI, baseline data were not provided at all. |
| Selective reporting (reporting bias) | Unclear risk | The primary outcome measures were the ABC (and 5 subscales), the CGI‐S, and the Treatment Emergent Side Effects Scale. All three of these measures were reported at endpoint, however baseline scores were not provided. Only that participants were required to have ≥ 16 on ABC‐I. |
| Other bias | High risk | This research was supported by a grant from Celltech Pharmaceuticals, Inc. |
Yamasue 2020.
| Study characteristics | ||
| Methods | 6‐week parallel trial of oxytocin versus placebo | |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: The University of Tokyo Hospital, Nagoya University Hospital, Kanazawa University, and University of Fukui Hospital in Japan Sample size: 53 were randomised to oxytocin and 53 to placebo groups Number of withdrawals/dropouts: 2 in oxytocin group were LTFU, 1 withdrew due to tumoural swelling of breast; 1 LTFU in placebo group due to worsening of repetitive behaviours Gender: all participants were male Mean age: 18‐54 years, mean age oxytocin 27.6 years, mean age placebo 26.3 years IQ: details not provided Baseline ABC‐I scores or other BoC: baseline scores not reported Concomitant medications: "12 continued their psychotropic medications throughout the period (4 antidepressants, 4 antipsychotics, 2 anticonvulsants (mood stabilizers), 2 hypnotics)". Previous medications: details not provided |
|
| Interventions | Intervention (oxytocin): 24 IU (Syntocinon Spray;
Novartis, Switzerland) in the morning and afternoon
for 6 consecutive weeks Comparator (placebo): 24 IU in the morning and afternoon for 6 consecutive weeks |
|
| Outcomes | Primary outcomes: AEs Secondary outcomes: tolerability Timing of outcome assessments: baseline and week 6 (endpoint) |
|
| Notes | Study start date: January 2015 Study end date: March 2016 Funding: "the Strategic Research Program for Brain Sciences from Japan Agency for Medical Research and Development" Conflicts of interest: "Neither the funder nor the sponsor, the Strategic Research Program for Brain Sciences from Japan Agency for Medical Research and Development, had any involvement in the data collection, analyses, writing, or interpretation of the study. However, the sponsor participated in the discussion regarding which sites should be included in the trial and how to best interpret the results" Trial registry: JPRN‐UMIN000015264 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were randomly assigned to receive oxytocin or placebo at a one‐to‐one ratio using a computer‐generated minimization design." |
| Allocation concealment (selection bias) | Low risk | "The registration, allocation, and data management procedures were defined separately... The following procedures were performed by the individual in charge of allocating and coding the test drug... confidentiality of the test drug allocation code table until the end of the trial and until the inclusion of each participant was fixed The registration, allocation, and data management procedures were defined separately." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Details not provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Apart from "double blinded" no further details were provided. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Number of dropouts described don't add up to difference in randomised/analysed (see fig 1) |
| Selective reporting (reporting bias) | Low risk | All outcomes listed on trials registry were reported in the paper or journal website. |
| Other bias | High risk | The sponsor participated in the discussion regarding which sites should be included in the trial and how to best interpret the results |
ABC: Aberrant Behaviour Checklist; ABC‐I: Aberrant Behaviour Checklist Irritability subscale; ADHD: Attention Deficit Hyperactivity Disorder; ADI‐R: Autism Diagnostic Interview‐Revised; ADOS‐2: Autism Diagnostic Observation Schedule, 2nd edition; AE: adverse effects; ASD: autism spectrum disorder; BoC: behaviours of concern; BSE: Behavioral Summarized Evaluation; CARS: Childhood Autism Rating scale; CBCL: Child Behaviour Checklist; CGI‐S: Clinical Global Impression Scale—Severity; CPRS: Conners' Parent Rating Scale; CYBOCS‐PDD: Children's Yale‐Brown Obsessive Compulsive Scale modified for pervasive developmental disorders; DSM‐4:Diagnostic and Statistical Manual of Mental Disorders(4th edition );DSM‐4 (TR):Diagnostic and Statistical Manual of Mental Disorders(4th edition ‐ text revision); DSM‐5:Diagnostic and Statistical Manual of Mental Disorders(5th edition); ECG: electrocardiogram; EEG: electroencephalogram; ICD‐10: International Classification of Diseases‐10; IQ: intelligience quotient; ITT: intention‐to‐treat; IU: International Units; LOCF: last observation carried forward; LTFU: lost to follow‐up; MAOI: monoamine oxidase inhibitor; MDMA: 3,4‐methylenedioxy‐methamphetamine; MRI: magnetic resonance imaging; MSEL: Mullen Scales of Early Learning; NAC: N‐acetylcysteine; PedsQL: Pediatric Quality of Life inventory; PDD‐NOS: pervasive developmental disorder not otherwise specified; QoL: quality of life; RCT: randomised controlled trial; RFRLRS: Ritvo Freeman Real Life Rating Scale; SD: standard deviation; SNAP: Swanson, Nolan and Pelham; SSRI: selective serotonin reuptake inhibitor; TSO:Trichuris suis ova; WHO: World Health Organization; WHOQOL: World Health Organization Quality of Life scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Althaus 2015 | Ineligible comparator |
| Aman 1997 | Non‐RCT |
| Aman 2009 | Ineligible comparator |
| Anderson 1984 | Focus not on unwanted behaviours (irritability, aggression, self‐injury) |
| Anderson 1989 | Focus not on unwanted behaviours (irritability, aggression, self‐injury) |
| Anderson 1997 | Non‐RCT |
| Anderson 2007 | Ineligible outcomes |
| Arman 2003 | Non‐RCT |
| Arnold 2012b | Ineligible comparator |
| August 1987 | Focused on core symptoms of ASD |
| Bachmann 2013 | Non‐RCT |
| Barnard‐Brak 2016 | Non‐RCT |
| Beeghly 1987 | Focused on core symptoms of ASD |
| Castellanos 2019 | Foccused on core symptoms of ASD |
| Chez 2002 | Non‐pharmacological |
| Chez 2003 | Focused on core symptoms of ASD |
| Du 2015 | Focused on core symptoms of ASD |
| Duker 1991 | Focused on core symptoms of ASD |
| Dunn‐Geier 2000 | Focused on core symptoms of ASD |
| Ekman 1989 | Focused on core symptoms of ASD |
| Fahmy 2013 | Focused on core symptoms of ASD |
| Fang 2018 | Non‐pharmacological intervention (e.g. herbal etc.) |
| Findling 1997a | Non‐pharmacological intervention (e.g. herbal etc.) |
| Groden 1987 | Non‐RCT |
| Guglielmo 2013 | Non‐RCT |
| Handen 2013 | Did not focus on BoC |
| Hellings 2006a | Non‐RCT |
| Hellings 2010 | Non‐RCT |
| Hellings 2015 | Non‐RCT |
| Hess 2010 | Non‐RCT |
| Hollander 2003 | Focus not on BoC |
| Hollander 2006c | Did not focus on people with ASD |
| Hollander 2020c | Retracted study |
| Horovitz 2012 | Non‐RCT |
| Horrigan 1997 | Non‐RCT |
| Hughes 2002 | Non‐RCT |
| Jacob 2020 | Terminated study |
| Jordan 2012 | Non‐RCT |
| JPRN‐UMIN000007250 2012 | Terminated study |
| Jun 2000 | Focused on core symptoms of ASD |
| Kolmen 1995 | Focused on core symptoms of ASD |
| Kolmen 1997 | Non‐RCT |
| Krusch 2004 | Focus not on BoC |
| Leboyer 1993 | Non‐RCT |
| Lemonnier 2012 | Focused on core symptoms of ASD |
| Leventhal 1993 | Focus not on BoC (irritability, aggression, self‐injury) |
| Levine 1997 | Non‐RCT |
| Malone 2002 | Non‐RCT |
| Moharreri 2017 | Focused on core symptoms of ASD |
| Nagaraj 2006 | Scales ineligible and AEs were not specified for each group |
| NCT00198120 2005 | Focused on lethargy and improvement in CGI |
| NCT01078844 | Terminated study |
| Nickels 2008 | Non‐RCT |
| Niederhofer 2007 | Non‐RCT |
| Posey 2004 | Focused on core symptoms of ASD |
| Preckel 2016 | Focused on core symptoms of ASD |
| Purdon 1994 | Non‐RCT |
| Radzivil 2006 | Non‐RCT |
| Ratcliff‐Schaub 2005 | Focus not on BoC (irritability, aggression, self‐injury) |
| Ritvo 1971 | Non‐RCT |
| Ritvo 1983 | Non‐RCT |
| Ritvo 1984 | Non‐RCT |
| Roberts 2001 | Focus not on BoC (irritability, aggression, self‐injury) |
| Scifo 1996 | Ineligible outcomes |
| Sponheim 2002 | Focus not on BoC (irritability, aggression, self‐injury) |
| Steiner 1999 | Focus not on BoC (irritability, aggression, self‐injury) |
| Stubbs 1986 | Focus not on BoC (irritability, aggression, self‐injury) |
| Sugie 2003 | Non‐RCT |
| Sugiyama 1998 | Ineligible outcomes and measures used were not specific to BoC (e.g. CGI) |
| Tachibana 2013 | Non‐RCT |
| Taylor 1993 | Did not focus on people with ASD |
| Tolbert 1993 | Ineligible outcomes |
| Troost 2006 | Non‐RCT |
| Volkmar 1983 | Non‐RCT |
| Volkmar 2009 | Ineligible study design |
| Wasserman 2005 | Focus not on BoC |
| Wei 2011 | Non‐RCT |
| Witwer 2005 | Did not focus on BoC |
| Yarbrough 1987 | Outcomes ‐ insufficient data reported |
| Yui 2012 | Focus not on BoC (irritability, aggression, self‐injury) |
| Zingarelli 1992 | Non‐RCT |
ABC‐I: Aberrant Behaviour Checklist (Irritability subscale); AE: adverse effect; ASD: autism spectrum disorder; BoC: behaviours of concern; CGI: Clinical Global Impression; RCT: randomised controlled trial
Characteristics of studies awaiting classification [ordered by study ID]
Anagnostou 2018.
| Methods | 12‐week trial of tideglusib versus placebo |
| Participants | Inclusion criteria: not specified apart from aged
12‐18 years Exclusion criteria: details not provided (conference poster) Location/setting: not specified but assumed to be either the USA or Canada Number of participants randomly assigned: not specified apart from 83 were randomised in a 1:1 manner Number of withdrawals/dropouts: not reported Gender: not reported Mean age: not reported IQ: not reported Concomitant medications: not reported History of previous medications: not reported |
| Interventions | Intervention (tideglusib): once‐daily oral
administration of tideglusib commenced at 400 mg
increasing to 1000 mg (1g) Comparator (placebo): not described Timing of outcome assessments: baseline and 12 weeks (endpoint) |
| Outcomes | Primary outcomes:
|
| Notes | Study start date: not reported Study end date: not reported Funding: not reported Conflicts of interest: not reported |
Buitelaar 1996.
| Methods | Parallel trial of ORG 2766, an ACTH‐(4–9) analog versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria: taking concurrent psychotropic medications Location/setting: outpatient clinic of the Department of Child and Adolescent Psychiatry of the Utrecht University Hospital, The Netherlands Sample size: 50 (30 to ORG2766 group, 20 to placebo group) Number analysed: 30 ORG 2766; 20 placebo Number of withdrawals/dropouts: 2 on placebo and 1 on ORG 2766 dropped out because of "an increase in anxiety, nervousness and irritability after they had ingested the tablets for 3 weeks, 4 days and 2 days respectively" Gender: not reported Mean age: "aged between 7 and 15 years" IQ: "a performance IQ of more than 60". Concurrent medications: participants could not have been on any concurrent psychotropic medications History of previous medications: details not provided Baseline ABC‐I or other BoC: parent‐rated total ABC score: ORG2766 responders 51.0 (18.5), ORG2766 non‐responders 46.9 (29.5); placebo responders 42.3 (16.4), placebo non‐responders 46.5 (22.5) |
| Interventions | Intervention: (ORG 2766) for 6 weeks: 40 mg/day of
ORG 2766 Comparator: (placebo) for 6 weeks: 40 mg/day of placebo |
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: baseline, week 2, 4, and 6 (endpoint) |
| Notes | Study start date: not reported Study end date: not reported Source of funding: not reported Conflicts of interest: not reported |
Campbell 1982a.
| Methods | 4‐week trial haloperidol versus placebo |
| Participants | Inclusion criteria: meet the DSM criteria for
autism Exclusion criteria: not reported Location/Setting: appears to be in the USA Number of participants randomly assigned: 40 in total Number of withdrawals/dropouts: Gender: not reported Mean age: 4.7 years (range 2.3‐7.9 years) IQ: not reported Concomitant medications: not reported History of previous medications: not reported |
| Interventions | Intervention (haloperidol): mean 1.12 mg/day (0.5
mg‐3.0 mg/day) Comparator (placebo): equivalent placebo |
| Outcomes | No relevant outcomes reported (behaviours were stereotypies, fidgeting, hyperactivity, and withdrawal) |
| Notes | Comment: insufficient information provided and scales used were not relevant (CGI, Children's Psychiatric Rating Scale) |
Carminati 2016.
| Methods | Parallel trial of venlafaxine versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: University Hospitals of Geneva, Switzerland Sample size: 14 in total, 13 analysed Number of withdrawals/dropouts: 3 participants withdrew consent: 2 at day 14, 1 day 28 but were included in analysis; 1 was not included in analysis due to taking paroxetine during the study Gender: 11/13 were male Mean age: median age venlafaxine group: 22 years (range 18‐30); median age placebo group: 19 (range 19‐32) IQ: all participants had a mild, moderate or severe intellectual disability Baseline ABC‐I or other BoC: ABC‐I median 18.0, self‐injurious behaviour median 8.5; aggression median 5.5 Concomitant medications: psychotropic treatment were prohibited during the trial History of previous medications: not reported |
| Interventions | Intervention (venlafaxine) for 8 weeks: 18.75 mg/day
of venlafaxine Comparator (placebo) for 8 weeks: matching placebo |
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcomes assessment: baseline, and weeks 2 and 8 |
| Notes | Study start date: not reported Study end date: not reported Source of funding: “the Unit of Mental Development of the Department of Mental Health and Psychiatry of the Geneva University Hospitals, Geneva, Switzerland and the Foundation Handicap Mental & Société (FHMS), Geneva, Switzerland, (N. CGR 73166 PS‐Venlafaxine). The funding sources had no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication." Conflicts of interest: none declared |
Gabis 2019.
| Methods | 12‐week cross‐over trial of donepezil versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: Israel Sample size: target of 84 participants Number randomised: 60 in total (donepezil + choline (29) or placebo (31)) Number analysed: 48 (intervention (23), placebo (25)) Number and reason for dropouts: 14 were reported to have dropped out ("Six subjects dropped out after the first assessment due to lack of compliance, and three additional subjects subsequently failed to attend follow‐up for the second assessment. Three subjects (one in the placebo group and two in the treatment group) were excluded during treatment due to side effects"). Gender: not reported Mean age: not reported IQ: not reported Concomitant medications: not reported Previous medications: not reported |
| Interventions | Intervention (donepezil + choline) for 12 weeks:
maximum donepezil 5 mg/day taken once daily, choline
250 mg/day (children up to 40 kg) or 500 mg/day
(children 40 kg and over) Comparator (placebo) for 12 weeks: equivalent placebo |
| Outcomes | Primary outcomes: AEs Secondary outcomes: none reported Timing of outcome assessments: baseline, weeks 4, 8 and 12 (endpoint) |
| Notes | Study start date: March 2010 Study end date: December 2017 Source of funding: not reported Conflicts of interest: not reported |
Handen 2000.
| Methods | Cross‐over trial of 0.3 mg/kg methylphenidate, 0.6 mg/kg methylphenidate or placebo |
| Participants | Inclusion criteria:
Exclusion criteria: not reported Location/setting: participants were recruited from either special education programmes, a psychiatric inpatient unit, or intensive day‐treatment programme. Sample size: 13 in total (cross‐over) Number of withdrawals/dropouts: 1 person was not included in the analysis; however, reasons were not provided. Gender: 10 male participants, 3 female participants Mean age: median 7.4 years IQ: 3 had severe/profound disability, 5 had moderate intellectual disability, 4 had mild intellectual disability, 1 had average IQ Baseline ABC‐I or other BoC: not reported Concomitant medications: not reported History of previous medications: not reported |
| Interventions | Intervention 1 (0.3 mg/kg methylphenidate for 7
days): 0.3 mg/kg doses of methylphenidate rounded to
the nearest 2.5 mg was given 2‐3 times/day for 7
consecutive days. Doses were given at breakfast and
4 h later with lunch. Intervention 2 (0.6 mg methylphenidate for 7 days): 0.6 mg/kg doses of methylphenidate rounded to the nearest 2.5 mg was given 2‐3 times/day for 7 consecutive days. Doses were given at breakfast and 4 h later with lunch. Comparator (placebo for 7 days): equivalent placebo doses |
| Outcomes | Primary outcomes:
Secondary outcomes: not reported Timing of outcome assessment: not reported |
| Notes | Study start date: not reported Study end date: not reported Source of funding: "This research was supported by a grant to the third author from the Fanny Pushin Rosenberg Research Foundation." Conflicts of interest: none declared |
IRCT2017041333406N1.
| Methods | 12‐week parallel trial of donepezil versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria: "patients who have been treated with other psychotropic drugs and also patients with other psychiatric disorders" Location/setting: Iran Sample size: target sample size is 66 Number of withdrawals/dropouts: it is unknown if the trial has been completed or not, as there is insufficient information on the trial registry. Gender: not reported Mean age: not reported IQ: > 50 based on the Weiland test Concurrent medications: only risperidone was allowed History of previous medications: not reported |
| Interventions | Intervention (donepezil + risperidone) for 12 weeks:
maximum of 10 mg/day of donepezil taken twice daily;
maximum of 2 mg/day of risperidone Comparator (placebo + risperidone) for 12 weeks: placebo + maximum of 2 mg/day of risperidone |
| Outcomes | Primary outcomes: AEs Secondary outcomes: none reported Timing of outcome assessments: baseline, week 6, week 12 (endpoint) |
| Notes | Study start date: September 2017 Study end date: not reported Source of funding: not reported Conflicts of interest: not reported |
IRCT20190714044199N1.
| Methods | 10‐week parallel trial of N‐acetylcysteine versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: Iran Number randomised: target sample size of 66 Number of withdrawals/dropouts: not reported Gender: not reported Mean age: not reported IQ: > 50 Baseline ABC‐I or other BoC: not reported Concomitant medications: not reported History of previous medications: not reported |
| Interventions | Intervention (N‐acetylcysteine + risperidone) for 10
weeks: maximum of 600 mg/day + risperidone (maximum
of 1.5 mg/day) Comparator (placebo + risperidone) for 10 weeks: placebo + risperidone (maximum of 1.5 mg/day) Timing of outcome assessments: baseline, week 5, week 10 (endpoint) |
| Outcomes | Primary outcomes: AEs Secondary outcomes: not reported |
| Notes | Study start date: November 2019 Study end date: not reported Source of funding: not reported Conflicts of interest: not reported |
JPRN‐JMA‐IIA00438.
| Methods | 8‐week parallel trial of pyridoxamine versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria
Target sample size: 78 |
| Interventions | Intervention 1: high‐dose pyridoxamine plus 20 mg
vitamin B1 Intervention 2: low‐dose pyridoxamine plus 20 mg vitamin B1 Comparator: placebo plus 2 0mg vitamin B1 |
| Outcomes | Primary outcomes irritability, measured using the
ABC‐Japanese version Secondary outcomes: none reported Timing of outcome assessments: baseline, 4 and 8 weeks |
| Notes | Contact name: Mitugu Uematsu Contact details: not provided Other clinical trial numbers: UMIN000035172; jRCT2021200001 |
Jung 2000.
| Methods | 4‐week cross‐over trial of dimethylglycine versus placebo |
| Participants | Inclusion and exclusion criteria: unclear, details
not provided Location/setting: China Sample size: 106 (unclear how many in each group) Number of dropouts/withdrawals: 61 participants in total "(At the end of the first 4 weeks 22 cases (21%) were lost. At the end of 10 weeks 61 cases (58%) were lost which was inadequate for analysis. Therefore we decided to use the data from the first 4 weeks for our main analysis." |
| Interventions | Phase one Intervention (dimethylglycine): participants received between 6.94 mg and 10.41 mg/kg body weight for 4 weeks. This was followed by a 2‐week wash‐out period before commencing placebo. Comparator: equivalent placebo for 4 weeks. This was followed by a 2‐week wash‐out period before commencing dimethylglycine. |
| Outcomes | Primary outcomes:
Secondary outcomes: it appears that none were reportd although it is difficult to know Timing of outcome assessments: details not provided |
| Notes | Contact person: details not provided Contact details: details not provided |
Jørgensen 2002.
| Methods | Written in Danish, and we have not found an abstract or full‐text copy in either Danish or English. No further information on participants, interventions or outcomes. |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes |
Kern 2001a.
| Methods | Parallel trial N, N‐dimethylglycine versus placebo |
| Participants | Inclusion criteria: diagnosis of autism and/or PDD
according to DSM‐IV criteria Exclusion criteria: not reported Location/Setting: USA Sample size: placebo 19, dimethylglycine 18 Number of withdrawals/dropouts: 1 discontinued due to negative behavioural effects in dimethylglycine group; 1 child discontinued due to damage to the tablets in the placebo group Gender: not reported Mean age: 3‐11 years IQ: not reported Baseline ABC‐I or other BoC: not reported Concomitant medications: 7 children were on psychoactive medication (clonidine, thioridazine, paroxetine, imipramine, methylphenidate and fluoxetine) History of previous medications: not reported |
| Interventions | Intervention (dimethylglycine) for 4 weeks: started
at 1 x 125 mg tablet/day for children weighing <
40 lbs (approx 18 kg) for 4 weeks. The dosage was 2
tablets (250 mg/day) for children weighing 41‐70 lbs
(approx 18‐32 kg), 3 tablets (375 mg/day) for 71‐100
lbs (approx 32‐45 kg), 4 tablets (500 mg/day) for
101‐130 lbs (approx 45‐59 kg), and 5 tablets (725
mg/day) for > 131 lbs (approx 59 kg). Comparator (placebo) for 4 weeks: 1 x 125 mg tablet each morning for 4 weeks for children weighing < 40 lbs (approx 18 kg), 2 tablets for 41‐70 lbs (approx 18‐32 kg), 3 tablets for 71‐100 lbs (approx 32‐45 kg), 4 tablets for 101‐130 lbs (approx 45‐59 kg), and five tablets for > 131 lbs (approx 59 kg) |
| Outcomes | Primary outcomes: irritability, measured using the
ABC‐I subscale (Aman 1985); however, it was not reported
fully (only t‐scores) Secondary outcomes: none reported Timing of outcome assessments: before treatment and 4 weeks after treatment |
| Notes | Study start date: 1998 Study end date: 1999 Source of funding: supported by FoodScience Corporation Conflicts of interest: none declared |
Kern 2002.
| Methods | Cross‐over trial of secretin versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: a neurology clinic at Children's Medical Centre of Dallas, USA Sample size: 19 children in total Number of withdrawals/dropouts: none reported Gender: 15 boys, 4 girls Mean age: 6.3 years IQ: not reported Baseline ABC‐I or other BoC: not reported Concomitant medications: not reported History of previous medications: not reported |
| Interventions | Intervention (secretin) for 3 weeks: "each
Secretin‐Ferring vial contained 75 CU porcine
secretin, 1mg L‐cysteine hydrochloride, and 20mg
mannitol. The dose was 2 CUs/kg" Comparator (placebo) for 3 weeks: placebo was sterile normal saline and identical in appearance to the porcine secretin |
| Outcomes | Primary outcomes: irritability, measured using the
ABCt‐I subscale (Aman 1985) Secondary outcomes: none reported Timing of outcome assessments: baseline and weeks 3 and 6 (not reported) |
| Notes | Study start date: not reported Study end date: not reported Source of funding: not reported Conflicts of interest: none declared Comments: study authors divided participants into normal GI and participants with chronic diarrhea. Outcome scores could not be used. |
Li 2016.
| Methods | 8‐week parallel trial of paliperidone versus aripiprazole |
| Participants | Inclusion criteria: unknown (the only available
details are in the abstract) Exclusion criteria: unknown Location/setting: unknown, but assumed to be China Number randomised: 62 (31 to each group) Number of withdrawals/dropouts: unknown (the only available details are in the abstract) Gender: details not provided Mean age: not known ‐ unable to find the full‐text paper IQ: not known ‐ unable to find the full‐text paper Baseline ABC‐I or other BoC: unknown Concurrent medications: unknown History of previous medications: unknown |
| Interventions | Intervention (paliperidone) for 8 weeks: details not
reported Comparator (aripiprazole) for 8 weeks: details not reported |
| Outcomes | Primary outcomes: AEs Timing of outcome assessments: baseline, weeks 4,6, 8 (endpoint) |
| Notes | Study start date: details not reported Study end date: details not reported Source of funding: details not reported Conflicts of interest: details not reported |
Malone 2010.
| Methods | Parallel trial of olanzapine versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: Drexel University, College of Medicine, Philadelphia, PA, USA Sample size: 33 Number of withdrawals/dropouts: none reported Gender: 25 male participants, 8 female participants Mean age: 6.58 years IQ: not reported Baseline ABC‐I or other BoC: not reported Concomitant medications: not reported History of previous medications: not reported |
| Interventions | Intervention (olanzapine) for 6 weeks: olanzapine
tablets given twice daily at a dosage of 2.5‐20
mg/day for up to 12 weeks Comparator (placebo) for 6 weeks: matching placebo treatment |
| Outcomes | Primary outcomes: AEs Secondary outcomes: none reported Timing of outcome assessments: baseline and week 12 |
| Notes | Study start date: May 2003 Study end date: September 2005 Source of funding: Food and Drug Administration (FD‐R‐002190), National Institute of Mental Health (MH073524). Placebo and drugs were provided by Eli Lilly Conflicts of interest: none declared |
Martsenkovsky 2016.
| Methods | 16‐week parallel trial of memantine versus placebo |
| Participants | Inclusion criteria: children 18−36 months old with
ASD (based on DSM‐IV criteria) Exclusion criteria: not reported Location/setting: not specifically mentioned but assumed to be in the Ukraine Sample size: 76 Number of withdrawals/dropouts Gender: not reported Mean age: 18‐36 months of age IQ: not reported Baseline ABC‐I or other BoC: unknown Concomitant medications: not reported History of previous medications: not reported |
| Interventions | Intervention (memantine) for 16 weeks: maximum of 15
mg/day (mean daily dose of 7.5 mg/day for children
18‐25 months, 10.3 mg/day for children 26‐36
months) Comparator (placebo) for 16 weeks: equivalent placebo |
| Outcomes | Primary outcomes: AEs ABC (subscales unknown or if the measure is the Aberrant Behaviour Checklist or a different ABC scale) |
| Notes | Study start date: details not reported Study end date: details not reported Source of funding: details not reported Conflicts of interest: details not reported Comments: only F values provided |
Miller 1979.
| Methods | Unable to obtain abstract or full‐text. The paper is written in German and published in 1979. If we obtained at least an abstract we could have had it translated but it is not available (partly due to the fact it was published over 40 years ago). No further information on methods, participants, interventions (except Sulpiride) or outcomes |
| Participants | |
| Interventions | Intervention: Sulpiride Comparator: unclear |
| Outcomes | |
| Notes |
Molloy 2002.
| Methods | Cross‐over trial of single dose secretin versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria: "had known chromosomal or other genetic disorders, a structural abnormality on neuroimaging, had previously received secretin, had acute or chronic pancreatic disease or a medical condition that might make participation in the study unsafe". Location/setting: Children's Hospital Medical Centre, Cincinnati, Ohio, USA Sample size: 60 Number analysed: secretin first: 19, placebo first: 23 Number of withdrawals/dropouts: 18 dropped out from original 60, although reasons for only 1 participant provided (from placebo/secretin group) ‐ they did not return for the final assessment. Gender: 37/42 analysed were male participants Mean age: 6.8 years IQ: not reported Baseline ABC‐I or other BoC: not reported Concurrent medications: not reported History of previous medications: not reported |
| Interventions | Intervention (single dose secretin): a single dose of
2 IU/kg of intravenous synthetic human secretin was
given at the first visit of the phase. Comparator (single dose placebo): a single dose of 2 IU/kg of placebo was given at first visit of the phase. |
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: baseline, and weeks 1, 3, 6, 9 and 12 |
| Notes | Study start date: not reported Study end date: not reported Source of funding: "supported by Grant #4 T73 MC 00032‐10 awarded by the Maternal and Child Health Bureau, Health Resources and Service Administration, DHHS and by Grant #M01 RR‐08084, NIH. The human synthetic secretin used in the study was supplied by ChiRoClin (Silver Spring, MD) free of charge". Conflicts of interest: none declared Comment: author was contacted for information but no reply |
Naruse 1982.
| Methods | Cross‐over trial of pimozide versus haloperidol versus placebo |
| Participants | 87 children (3‐16 years), 69 boys and 18 girls from
12 hospitals; 34 with autistic disturbance, 27 with
behaviour disturbance caused by organic damage, 17
with mental retardation, 5 with neurosis and 4 with
psychosis Location/setting: 12 hospitals in Germany Sample size: 87 Number of withdrawals/dropouts: not reported (unable to obtain full text) Gender: 69 boys, 18 girls Mean age: 3‐16 years IQ: not reported Concurrent medications: not reported History of previous medications: not reported Baseline ABC‐I or other BoC: not reported |
| Interventions | Intervention 1 (pimozide) for 8 weeks: the initial
dose was pimozide 1 tablet (1 mg). The maximum daily
dose was 9 tablets (pimozide 9 mg). Intervention 2 (haloperidol) for 8 weeks: 1 tablet (0.75 mg). The maximum daily dose was 9 tablets (haloperidol 6.75 mg). Comparator (placebo) for 8 weeks: equivalent placebo |
| Outcomes | Primary outcomes: anger/aggression/injury and
violence to others Secondary outcomes: none reported Timing of outcome assessments: not reported |
| Notes | Study start date: not reported Study end date: not reported Source of funding: not reported Conflicts of interest: not reported Comment: not able to obtain the full text |
Noone 2014.
| Methods | Parallel trial of milnacipran versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: USA Sample size: 10 in total Number of withdrawals/dropouts: not reported Gender: not reported Mean age: 19‐41 years IQ: > 70 Baseline ABC‐I or other BoC: not reported Concomitant medications: not reported, although comorbid neurological, psychiatric and medical condition excluded except for ADHD or OCD History of previous medications: not reported |
| Interventions | Intervention (milnacipran) for 12 weeks: participants
were given a titrated dose of milnacipran increasing
to a maximum of 100 mg a day over the 12‐week study
period. Dosing was based on a fixed schedule that
was monitored using a side‐effect profile. Comparator (placebo) for 12 weeks: participants were given placebo tablets at dosing corresponding to the fixed schedule between 12.5 mg and 100 mg. |
| Outcomes | Primary outcomes: ABC‐I (Aman 1985) (not
reported in paper or clinicaltrials.gov website) Secondary outcomes: none reported Timing of outcome assessments: twice‐weekly |
| Notes | Study start date: February 2011 Study end date: July 2014 Source of funding: "funded by an investigator initiated grant from Forest Pharmaceuticals, Inc" Conflicts of interest: none declared |
Novotny 2004.
| Methods | Parallel trial of single‐dose M‐chlorophenylpiperazine (m‐cpp) versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria: "meeting criteria for current or past psychotic disorders diagnosed by SCID – Axis disorders; reporting a history of seizures or medical illnesses" Location/setting: USA Sample size: oral m‐CPP 11, placebo 8 Number of withdrawals/dropouts: no LTFU reported Gender: 10 male participants, 1 female participant Mean age: 34.3 years IQ: not reported Baseline ABC‐I or other BoC: not reported Concomitant medications: participants were required to be drug‐free for 2 weeks prior to study. History of previous medications: not reported |
| Interventions | Intervention (single dose of oral m‐CPP): 0.5 mg/kg
at least 48 h apart from the placebo single dose,
and after a drug‐free period of at least 2 weeks or
6 weeks for those on fluoxetine, and a 72‐h low
monoamine diet Comparator (single‐dose placebo): equivalent placebo |
| Outcomes | Primary outcomes: self‐injurious behaviours (not
reported) Secondary outcomes: none reported Timing of outcome assessments: baseline and at 60, 120, 180, 240 min (single dose) |
| Notes | Study start date: not reported Study end date: not reported Source of funding: "supported in part by grants from the Seaver Foundation, National Alliance for Research on Schizophrenia and Depression, Cure Autism Now, National Alliance for Autism Research and grant 5 MO1 RR00071 for the Mount Sinai General Clinical Research Center from the National Center for Research Resources, National Institutes of Health.: Conflicts of interest: none declared |
Sandler 1999.
| Methods | Parallel trial of single‐dose secretin versus single‐dose placebo |
| Participants | Inclusion criteria:
Location/setting: Department of Psychiatry, University of North Carolina. Children were referred by the Treatment and Evaluation of Autism and Communication Handicaps program of the Department of Psychiatry at the University of North Carolina or whose parents responded to notices about this study placed in the newsletter of an autism‐support group. Sample size: 60 children were randomised Number of withdrawals/dropouts: 4 could not be evaluated (2 received secretin outside the study, and 2 did not return for follow‐up) Gender: not reported Mean age: secretin 7.6 years, placebo 7.4 years IQ: secretin 65.6, placebo 60.1 Baseline ABC‐I or other BoC: not reported Concomitant medications: secretin 8/30, placebo 11/30 were taking psychotropic medications History of previous medications: not reported |
| Interventions | Intervention (single‐dose secretin): 0.4 ug per kg of
body weight Comparator (single‐dose placebo): saline placebo |
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: baseline, weeks 1, 2 and 4 postinfusion |
| Notes | Study start date: not reported Study end date: not reported Source of funding: Thoms Health Services Foundation and by a Public Health Service grant (30615) from the National Institutes of Child Health and Human Development Conflicts of interest: none declared Comment: study author contacted twice for information about AEs but no reply |
Stern 1990.
| Methods | Cross‐over trial of fenfluramine versus placebo |
| Participants | Inclusion criteria: "infantile autism with or without
mental retardation [intellectual disability]"
diagnosis based on DSM‐III, previously under the
care of paediatricians and paediatric
neurologists Exclusion criteria: chromosomal anomalies, including the fragile X chromosome Location/setting: Adelaide Children's hospital, Australia Sample size: 20 in total Number of withdrawals/dropouts: "one child moved to another state half way through the trial" Gender: 14 boys, 6 girls Mean age: 10 years IQ: not reported Baseline ABC‐I or other BoC: not reported Concomitant medications: 15/20 were on no medications, 3 were on anticonvulsants, 1 was on benzodiazepine and 1 was on the contraceptive pill History of previous medications: not reported |
| Interventions | Intervention (fenfluramine) for 5 months: "the dose
of Fenfluramine was 1.5mg/kg/day given twice daily
for a 5 month period". At the end of the period all
children were given placebo for 2 months before the
groups crossed over for a second 5‐month period. Comparator (placebo) for 5 months: All children were given placebo for a month to get used to the routine of taking tablets regularly. The children were then randomised to either fenfluramine or placebo for a 5‐month period. At the end of the period all children were given placebo for 2 months before the groups crossed over for a second 5‐month period. |
| Outcomes | Primary outcomes: AEs (weight change, measured in
kgs) Secondary outcomes: none reported Timing of outcome assessments: not reported |
| Notes | Study start date: not reported Study end date: not reported Source of funding: "this study was supported by a grant from the Apex Foundation. The authors thank Dr Grant Sutherland for the karyotypes and Mrs Robyn Clements for the manuscript preparation. Fenfluramine and placebo tablets were supplied by Servier Laboratories (Australia) Pty, Ltd." Conflicts of interest: none declared |
Wink 2020.
| Methods | 6 week cross‐over trial of ketamine versus placebo |
| Participants | Inclusion criteria: Aged 12‐30 years old * Weight of at least 50kg *general good health as determined by physical exam, medical history, laboratory work up, and EKG, diagnostic and Statistical Manual of Mental Disorders 5th Edition diagnosis of autism spectrum disorder (not associated with Fragile X Syndrome or other known genetic syndrome) as confirmed by the Autism Diagnostic Observation Schedule at screen or previous (within last 5 years) if available; IQ of at least 50 as confirmed via testing (Leiter‐3) at screen or previous (within last 5 years, any valid testing acceptable); clinical Global Impressions‐Severity score of 4 (Moderately Ill); score of 10 on the Social Withdrawal subscale of the Aberrant Behavior Checklist; stable dosing of all concomitant psychotropic medications for five half‐lives prior to screening visit and during the study; presence of parent/guardian or significant other or caregiver willing to serve as informant for behavioral outcome measures" Exclusion criteria: "Presence of co‐morbid schizophrenia, schizoaffective disorder, bipolar disorder with psychosis, bipolar disorder or psychosis not otherwise specified; comorbid diagnoses determined by psychiatrist clinical interview and use of Diagnostic and Statistical Manual of Mental Disorders 5th Edition diagnostic criteria; history of drug or alcohol abuse; presence of cardiac disease including coronary artery disease, congestive heart failure, or uncontrolled hypertension per medical history (individuals with ≥ 2 blood pressure readings of ≥140/90 during screen/baseline will be excluded); airway instability, tracheal surgery, or tracheal stenosis per medical history; central nervous system masses or hydrocephalus per medical history; porphyria, thyroid disorder, or thyroid medication use per medical history; glaucoma or other cause of increased intraocular pressure per medical history; allergy to ketamine; current use of drugs with concomitant modification of non‐competitive N‐methyl‐D‐aspartate glutamate activity (acamprosate, amantadine, memantine, d‐cycloserine etc.); for female subjects of child bearing potential, a positive pregnancy test; any major chronic medical or chronic respiratory illness considered to be uncontrolled by the Principal Investigator; inability to tolerate study procedures or study drug per the discretion of the Principal Investigator." Location/setting: "Cincinnati Children’s Hospital Medical Center (CCHMC)". USA Sample size: 21 in total Number analysed: 17 Number of withdrawals/dropouts: "Four subjects withdrew from the study, one due to emesis following frst dose of study drug (ketamine), one due to seizure during the two‐week washout period (seven days post‐ketamine; determined unrelated to study drug), and two due to scheduling issues after Phase 1 (one ketamine, one placebo)". Gender: 19 male, 2 female Mean age (SD): 9.48 (3.83) Mean IQ (SD): 102.14 (23.62) Concurrent medications: History of previous medications: details not provided Baseline ABC‐I or other BoC: Mean ABC‐I (and standard deviation) 10.05 (5.86) |
| Interventions | Intervention: 2 doses of intranasal ketamine (30 mg and 50 mg) provided 1 week apart followed by a 2‐week washout period before starting phase 2 of the trial Comparator: 2 equivalent doses of placebo (saline spray) provided 1 week apart followed by a 2‐week washout period before starting phase 2 of the trial. |
| Outcomes | Primary outcomes: AEs Secondary outcomes: none reported Timing of outcomes assessment: baseline and endpoint |
| Notes | Study start date: December 22, 2015 Study end date: May 7, 2018 Funding: "Funding for this project was provided by Cures Within Reach and Roivant Sciences." Conflicts of interest: "The authors report no competing financial interests related to the work described". Trial registry: NCT02611921 |
Yatawara 2016.
| Methods | 14‐week cross‐over trial of oxytocin versus placebo |
| Participants | Inclusion criteria: "children aged between 3 and 8
years of age who met the DSM‐IV‐TR (Diagnostic and
Statistical Manual of Mental Disorders, 4th Edition,
Text Revision) criteria for Autistic Disorder,
Asperger’s Disorder or Pervasive Developmental
Disorder‐Not Otherwise Specified (PDD‐NOS)." Exclusion criteria: "Exclusion criteria included known sensitivity to preservatives in the nasal spray (in particular, E216, E218 and chlorobutanol hemihydrates)." Location/setting: "The study was conducted at the Brain and Mind Centre (BMC), The University of Sydney (Australia)". Number of participants: 39 were randomised, 17 to oxytocin (phase 1); 22 to placebo (phase 1). Number of withdrawals/dropouts: phase 1, 2 were excluded from oxytocin group (adverse reaction (1), competing time commitments (1)); 5 in placebo were excluded (intolerance of nasal spray (2); adverse reaction (1); competing time commitments (1); respiratory illness (1)). An additional person was excluded during phase 2 (oxytocin group). Gender: 27 male, 4 female Mean age (SD) in years: 6.2 (1.7) Mean IQ (SD): non‐verbal IQ 83.6 (24.2) Concomitant medications: atomoxetine (1); melatonin (1); anticonvulsant (2); risperidone (2); selective serotonin reuptake inhibitor (sertraline) (2) History of previous medications: not reported |
| Interventions | Intervention: oxytocin nasal spray 12 IU twice daily
(24 IU daily) for 5 weeks with a 4‐week wash‐out
period before starting phase 2 of the trial. Comparator (placebo): equivalent placebo nasal spray twice‐daily for 5 weeks with a 4‐week wash‐out period before starting phase 2 of the trial. |
| Outcomes | Primary outcomes: repetitive behaviour scale (not
clear which subscales); adverse effects Secondary outcomes: none reported Timing of outcome assessments: baseline and endpoint of each phase |
| Notes | Study start date: October 2010 Study end date:October 2012 Funding: "We acknowledge an National Health Medical Research Council Australian Fellowship (APP 511921) to IBH, an NHMRC Career Development Fellowship (APP 1061922) to AJG and a generous donation by Mr Geoff Stein toward the completion of this trial. These funders had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; and decision to submit the manuscript for publication." Conflicts of interest: "the authors declare no conflict of interest" |
ABC: Aberrant Behaviour Checklist; AE: adverse effect; BoC: behaviours of concern; CARS: Child Autism Rating Scale; CDC: Centers for Disease Control; CGI: Clinical Global Impression; ICD‐10: International Classification of Diseases, 10th revision; IQ: intelligence quotient; LTFU: loss to follow‐up; M: median; PDD‐(NOS): pervasive developmental disorders (not otherwise specified); SD: standard deviation
Characteristics of ongoing studies [ordered by study ID]
ACTRN12617000441314.
| Study name | A course of oxytocin to improve social communication in young children with autism |
| Methods | 15‐week parallel trial of oxytocin versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria: "known to be hypersensitive to the preservatives in the nasal spray (E216, E218, and chlorobutanol hemihydrates). Participants with severe nasal obstruction/blockage will be excluded as this is likely to reduce the efficacy of the nasal spray medication. Further, participants whose caregivers report that they have a serious medical condition from one of the following categories will be excluded (evidenced through medical examination): 1. severely compromised cardiac function 2. severely compromised hepatic function 3. severely compromised renal function". Setting/location: Sydney and Perth (Australia) Target sample size: details not provided |
| Interventions | Intervention: oxytocin basal spray 16 IU twice daily
(32 IU in total) for 12 weeks Comparator: equivalent placebo for 12 weeks |
| Outcomes | Primary outcomes: AEs Secondary outcomes: none reported Timing of outcome assessments: 6 weeks and 12 weeks (endpoint) |
| Starting date | April 2017 |
| Contact information | Contact name: Adam Guastella Contact details: adam.guastella@sydney.edu.au. |
| Notes | Source of funding: University of Sydney Conflicts of interest |
ChiCTR1800017720.
| Study name | A random, double‐blind, placebo controlled trial for oxytocin nasal spray in the treatment for ASD social dysfunction |
| Methods | Parallel trial of oxytocin versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria:
Setting/location: unclear although assumed to be in China Sample size: unclear |
| Interventions | Intervention (oxytocin): 12 IU morning and night Comparator (placebo): equivalent placebo morning and night |
| Outcomes | Primary outcomes:
Secondary outcomes: unclear Timing of outcome assessments: unclear |
| Starting date | Registered in August 2018 |
| Contact information | Name: Xu Chen E‐mail: yinuo0311@163.com |
| Notes | Source of funding: Beijing Anding Hospital Capital
Medical University Conflicts of interest: unclear |
Crutel 2020.
| Study name | Bumetanide oral liquid formulation for the treatment of children and adolescents with autism spectrum disorder: design of two phase III studies (SIGN Trials) |
| Methods | 6‐month parallel trial of bumetanide versus placebo |
| Participants | Inclusion criteria: "a primary diagnosis of ASD as
per DSM‐5 criteria, plus ASD criteria met on ADOS‐2
and ADI‐R", aged 7‐17 years (study 1) or 2‐6 years
(study 2), moderate to severe ASD according to CGI
score of at least 4, CARS2 total score of at least
34 Exclusion criteria: "concomitant participation in another study, or previous participation in a study of another medicinal product for 3 months prior to enrollment; known monogenic syndrome (e.g. Fragile X, Rett Syndrome); high suicide risk or psychiatric conditions considered likely to interfere with the conduct of the study; chronic hepatic disease, renal dysfunction or cardiac dysfunction; unstable psychotherapy, behavioral, cognitive, or cognitive‐behavioral therapy; concomitant psychotropic medication (exceptions: aripiprazole and risperidone in study 1, which are permitted if a stable dose is used between selection and inclusion, and up to Week 26; methylphenidate, atomoxetine, or guanfacine, which are permitted in both studies if stabilized for at least 4 weeks prior to inclusion and not planned to be modifed or stopped up to Week 26) or other contraindicated medication; and previous treatment with bumetanide that was not effective for the treatment of ASD symptoms" Setting/ location: across 13 countries Sample size: 170 per trial |
| Interventions | Intervention (bumetanide) for 6 months: oral solution
of 0.04 mL/kg twice daily for participants weighing
< 25 kg; participants ≥ 25 kg will receive 0.5 mg
twice daily Comparator (placebo) for 6 months: equivalent placebo, twice daily depending on weight |
| Outcomes | Primary outcomes: AEs Secondary outcomes: QoL measured using the Pediatric Quality of Life Inventory (Varni 2001) and the WHOQoL (WHO 1998). Timing of outcome assessments: unclear |
| Starting date | Unclear |
| Contact information | Simon Kyaga E‐mail: simon.kyaga@servier.com |
| Notes | Source of funding: Servier (pharmaceutical
company) Conflicts of interest: most study authors are employees of the funder (pharmaceutical company) |
CTRI/2021/12/038721.
| Study name | Comparison of the efficacy of oral risperidone and aripiprazole in children with autism spectrum disorders (ASDs) aged 6‐18 years: a double blind randomized controlled trial ‐ RAAT |
| Methods | 12‐week parallel trial of risperidone versus aripiprazole |
| Participants | Inclusion criteria :
Exclusion criteria:
Location/setting: India Target sample size: 120 participants |
| Interventions | Intervention (risperidone in tablet form): 0.5 mg/day
daily for 12 weeks Comparator (aripiprazole in tablet form): 2.5 mg/day daily for 12 weeks |
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: baseline and endpoint (week 12) |
| Starting date | Unclear: was not recruiting as at February 2022 |
| Contact information | Contact person: Prateek Kumar Panda Contact details: drprateekpanda@gmail.com |
| Notes | Source of funding Conflicts of interest |
EUCTR2008‐003712‐36‐FR.
| Study name | Etude de la réponse clinique et neurofonctionnelle à la fluoxétine dans l'autisme infantile |
| Methods | 20‐week parallel trial of fluoxetine versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria:
Location: France Setting: unclear Target sample size: unclear |
| Interventions | Intervention (fluoxetine) for 20 weeks, 20 mg/5
mL Comparator (placebo) for 20 weeks, equivalent oral solution of placebo |
| Outcomes | Primary outcomes: BoC (total score of ABC) Secondary outcomes: unclear Timing of outcome assessments: baseline and 20 weeks |
| Starting date | Registered November 2008 |
| Contact information | Contact name: not reported Contact details: not reported |
| Notes | Source of funding: Public Assistance ‐ Hopitaux De
Paris (AP‐HP) Conflicts of interest: unclear |
EUCTR2010‐024202‐34‐DE.
| Study name | Effect of oxytocin on therapy results of a group based social skill training in adolescents with autism spectrum disorder |
| Methods | Parallel trial of oxytocin versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: Germany Sample size: not known |
| Interventions | Intervention (oxytocin): 40 IU oxytocin nasal spray
(trial registry does not state the frequency) Comparator (placebo): equivalent placebo nasal spray |
| Outcomes | Primary outcomes: unclear Secondary outcomes: QoL (scale not reported) Timing of outcome assessments: unclear |
| Starting date | Registered December 2013 |
| Contact information | Contact name: Tanja Schad‐Hansjosten E‐mail: tanja.schad@zi‐mannheim.de |
| Notes | Source of funding: appears to be a pharmaceutical
company (Universitätsmedizin Göttingen,
Georg‐August‐Universität, Klinik für Kinder‐ und
Jugendpsychiatrie/Psychotherapie) Conflicts of interest: unclear |
EUCTR2014‐003080‐‐38‐DE.
| Study name | Glutamatergic medication in the treatment of obsessive compulsive disorder (OCD) and autism spectrum disorder (ASD) |
| Methods | 12‐week parallel trial of memantine versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria:
Setting/location: 4 centres across England, Germany, and the Netherlands Sample size: target is 50 participants each group (100 in total), 50% with ASD, 50% with OCD |
| Interventions | Intervention (memantine + regular treatment) for 12
weeks: 5‐15 mg/day, administered once daily Comparator (placebo + regular treatment) for 12 weeks: equivalent placebo |
| Outcomes | Primary outcomes:
Secondary outcomes: unclear Timing of outcome assessments: unclear |
| Starting date | Registered July 2014 |
| Contact information | Name: Alexander Häge E‐mail: alexander.haege@zi‐mannheim.de |
| Notes |
Source of funding: "European Community's
Seventh Framework Programme (FP7/2007‐2013) under
grant agreement number 278948, TACTICS
(Translational Adolescent and Childhood Therapeutic
Interventions in Compulsive Syndromes)". Conflicts of interest: unclear |
IRCT20090117001556N124.
| Study name | Cilostazol as adjunctive treatment of autism: a double blind and placebo controlled trial in children 5 to 11 years old |
| Methods | 10‐week parallel trial of cilostazol versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria:
|
| Interventions | Intervention (cilostazol + risperidone): 100 mg
cilostazol morning and night plus risperidone 1‐3
mg/day Comparator (placebo + risperidone): 1‐3 mg/day of risperidone plus placebo |
| Outcomes | Primary outcomes: irritability, measured using the
ABC‐I (Aman
1985) Secondary outcomes: unclear Timing of outcome assessments: baseline, week 5 and 10 (endpoint) |
| Starting date | 30 May 2020 |
| Contact information | Contact name: S. Akhondzadeh E‐mail: s.akhond@sina.tums.ac.ir |
| Notes | Source of funding: Tehran University of Medical
Sciences Conflicts of interest: not reported |
IRCT20200317046801N2.
| Study name | Effect of ondansetron combination therapy with risperidone in children with autism spectrum disorder in a randomized, double‐blind, placebo‐controlled clinical trial |
| Methods | 8‐week parallel trial of ondansetron versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria:
Setting: Roozbeh Hospital, Tehran, Iran Target sample size: 40 |
| Interventions | Intervention: risperidone and ondansetron (05
mg/kg/day for children > 40 kg) for 8 weeks Comparator: risperidone and placebo for 8 weeks ‐ the dosage of risperidone is unclear. Ondansetron: 05 mg/kg/day for children > 40 kg; placebo is 05 mg/kg/day for children > 40 kg |
| Outcomes | Primary outcomes: irritability, measured using the
ABC‐I (Aman
1985) Secondary outcomes: unclear Timing of outcome assessments: baseline, weeks 4 and 8 (endpoint) |
| Starting date | 11 September 2020 |
| Contact information | Name: Rahim Badrfam E‐mail: rbadrfam@gmail.com |
| Notes | Source of funding: Tehran University of Medical
Sciences Conflicts of interest: unclear |
ISRCTN15984604.
| Study name | Sertraline for anxiety in adults with a diagnosis of autism |
| Methods | 14‐week parallel trial of sertraline versus placebo |
| Participants | Inclusion criteria: "Aged ≥18 years and have a
diagnosis of autism (including autism spectrum
disorder/condition or other variations, Asperger
syndrome, or pervasive developmental disorder);
experience anxiety for which participants are
willing to try treatment with medication; able to
complete online or paper‐based questionnaires about
things such as anxiety, other symptoms, and
healthcare usage; able to provide informed consent
to take part". Exclusion criteria: "currently taking medication(s) for depression and/or anxiety, or have taken them in the past 8 weeks, or are using St John’s Wort; have a moderate or severe learning disability which means they may not be able to provide informed consent and/or understand and complete the study questionnaires; have/had other mental health conditions such as bipolar disorder or psychosis; have epilepsy that is not well controlled; have current problematic use of alcohol or illicit drugs; have allergies to sertraline or placebo; have/had severe liver problems, bleeding disorders, some heart problems; have swallowing difficulties or are unable to take medication in capsule form; taking part in another clinical trial; or are pregnant, planning pregnancy during the study period, or breastfeeding." Location/setting: the UK and Australia Target sample size: 306 participants |
| Interventions | Intervention (sertraline): the first 2 weeks
participants will receive 25 mg of sertraline in
tablet form, increasing to 25 mg twice daily for the
next 4 weeks. Dose can be increased by 50 mg every 4
weeks until the optimal dose is reached. Comparator: the first 2 weeks participants will receive 25 mg of placebo in tablet form, increasing to 25 mg twice daily for the next 4 weeks. Dose can be increased by 50 mg every 4 weeks until the optimal dose is reached. |
| Outcomes | Primary outcomes: AEs Secondary outcomes: health‐related QoL measured using EQ‐5D‐5L questionnaire Timing of outcome assessments: baseline, 12, 16, 24 and 52 weeks |
| Starting date | October 2019 |
| Contact information | Contact name: Adam Taylor Contact details: research‐governance@bristol.ac.uk |
| Notes | Source of funding: National Institute for Health
Research Health Technology Assessment programme
(NIHR HTA) (UK) and the National Health and Medical
Research Council (NHMRC) (Australia) Conflicts of interest: details not reported |
JPRN‐UMIN000017876.
| Study name | Effects of long‐term administration of intranasal oxytocin in children with autism spectrum disorder |
| Methods | 14‐week cross‐over trial of oxytocin versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria
Location/setting: Japan Target sample size: 10 in total |
| Interventions | Intervention: intranasal oxytocin 24 IU twice daily,
followed by a 1‐week wash‐out period before phase 2
of the trial. Comparator: equivalent intranasal placebo twice daily, followed by a 1‐week wash‐out period before phase 2 of the trial. |
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: baseline and endpoint of phase |
| Starting date | First registered June 2015 |
| Contact information | Contact person: Masako Taniike Contact details: masako@ped.med.osaka‐u.ac.jp |
| Notes | Source of funding: sponsored by the United Graduate School of Child Development, Osaka University Conflicts of interest: details not provided |
NCT00198120.
| Study name | Safety and effectiveness of D‐cycloserine in children with autism |
| Methods | 8‐week parallel trial of D‐cycloserine versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria:
Setting/location: assumed to be in the USA Sample size: target sample size is 80 |
| Interventions | Intervention (D‐Cycloserine) for 8 weeks: maximum 1.7
mg/kg/day Comparator (placebo) for 8 weeks: equivalent placebo |
| Outcomes | No relevant outcomes |
| Starting date | Trial registry last updated 2016 |
| Contact information | Name: Christopher J McDougle Contact details: not provided |
| Notes | Source of funding: Indiana University Conflicts of interest: unclear |
NCT01914939.
| Study name | A randomized, controlled trial of intranasal oxytocin as an adjunct to behavioral therapy for autism spectrum disorder |
| Methods | 12‐week parallel trial of oxytocin versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria:
Setting/location: Boston, USA Sample size: target is 92 participants |
| Interventions | Intervention (oxytocin) for 12 weeks: intranasal
spray of oxytocin 24 IU (unclear how often) Comparator (placebo) for 12 weeks: intranasal placebo |
| Outcomes | Primary outcomes: AEs Secondary outcomes: QoL (measured using the Quality of Life Enjoyment and Satisfaction Questionnaire) Timing of outcome assessments: unclear |
| Starting date | First registered in 2013 |
| Contact information | Name: John Gabrieli Address: Massachusetts General Hospital/MIT |
| Notes | Source of funding: Massachusetts General Hospital Conflicts of interest: not reported |
NCT01970345.
| Study name | A pilot treatment study of insulin‐like growth factor‐1 (IGF‐1) in autism spectrum disorder |
| Methods | 12‐week cross‐over trial of insulin‐like growth factor‐1 (IGF‐1) versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria:
Setting/location: unknown, although assumed to be in the USA Number of participants: target is 10 |
| Interventions | Intervention (insulin‐like growth factor‐1 (IGF‐1))
for 12 weeks: initiated at 0.04 mg/kg twice daily by
injection, increasing to maximum of 0.12 mg/kg twice
daily Comparator (placebo) for 12 weeks: equivalent placebo |
| Outcomes | Primary outcomes: BoC (measured using the Repetitive
Behaviour Scale (Bodfish 2000) (subscales unknown)) Secondary outcomes: unclear Timing of outcome assessments: unclear |
| Starting date | First registered in 2013 and expected to be completed in 2022 |
| Contact information | Name: Bonnie Lerman E‐mail: bonnie.lerman@mssm.edu |
| Notes | Source of funding: Icahn School of Medicine at Mount
Sinai, Autism Science Foundation Conflicts of interest: unclear |
NCT03553875.
| Study name | Memantine for the treatment of social deficits in youth with disorders of impaired social interactions |
| Methods | 12‐week parallel trial of memantine hydrochloride versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: Massachusetts General Hospital, USA Target sample size: 100 participants |
| Interventions | Intervention (memantine) for 12 weeks: maximum daily
dose of 20 mg, administered twice daily for 12
weeks Comparator (placebo) for 12 weeks: equivalent placebo pill twice daily |
| Outcomes | Primary outcomes: CGI‐Improvement Scale Secondary outcomes: unclear Timing of outcome assessments: not known |
| Starting date | First registered in November 2018 |
| Contact information | Name: Chloe Hutt Vater E‐mail: chuttvater@mgh.harvard.edu |
| Notes | Source of funding: Massachusetts General Hospital Conflicts of interest: unclear |
NCT03887676.
| Study name | Arbaclofen versus placebo in the treatment of children and adolescents with ASD |
| Methods | 16‐week parallel trial of arbaclofen versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria:
Setting/ location: Canada Sample size: 90 participants |
| Interventions | Intervention: arbaclofen administered orally in
tablet form in the following doses 5 mg, 10 mg, 15
mg and 20 mg for 16 weeks Comparator: equivalent placebo for 16 weeks |
| Outcomes | Primary outcomes: AEs Secondary outcomes: none reported Timing of outcome assessments: 16 weeks (endpoint) |
| Starting date | March 2019 |
| Contact information | Evdokia Anagnostou Contact details: not provided |
| Notes | Source of funding: Holland Bloorview Kids
Rehabilitation Hospital; McMaster University;
University of Western Ontario, Canada; Queen's
University; Unity Health Toronto; University of
Toronto Conflicts of interest: details not provided |
NCT04520685.
| Study name | CASCADE: CAnnabidiol Study in Children with Autism spectrum DisordEr (CASCADE) |
| Methods | 12‐week cross‐over trial of cannabidiol versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria:
Setting/location: University of Colorado, Denver Sample size: target is 70 participants |
| Interventions | Intervention (cannabidiol) for 12 weeks then placebo
for 15 weeks: "Each study period is 12 weeks and
dose will be titrated up for 1 week at the beginning
of a treatment period and titrated down for 1 week
at the end of a treatment period, with a two week
placebo washout between periods for Arms 1 and 2.
The titration dose will be 5mg/kg/day and the
treatment dose will be 10mg/kg/day" Comparator (placebo) for 15 weeks then cannabidiol for 12 weeks: participants will begin placebo in period 1 and receive cannabidiol in period 2 (same as above) |
| Outcomes | Primary outcomes:
Secondary outcomes: QoL (measured using the PedsQL ‐ Core Scale) (Varni 2001) Timing of outcome assessments ‐ baseline, week 12 (endpoint) |
| Starting date | First registered in August 2020 |
| Contact information | Name: Nana Welnick E‐mail: CBDinAutismStudy@childrenscolorado.org |
| Notes | Source of funding: University of Colorado, Denver Conflicts of interest: unclear |
NCT04725383.
| Study name | Amitriptyline for repetitive behaviors in autism spectrum disorders |
| Methods | 12‐week parallel trial of amitripyline versus placebo |
| Participants | Inclusion criteria
Exclusion criteria:
Target sample size: 30 participants Location/setting: USA |
| Interventions | Intervention: "Subjects will receive active
amitriptyline compounded into look‐alike capsules to
resemble placebo capsules. Dosing will be as
tolerated, up to a maximum of 100mg/day or
1.5mg/kg/day, for 12 weeks." Comparator: "Subjects in this arm will receive placebo compounded into capsules that resemble the compounded amitriptyline capsules, up to 4 capsules a day, for 12 weeks." |
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: baseline and 12 weeks (endpoint) |
| Starting date | First registered January 2021 |
| Contact information | Jessica Hellings Jessica.Hellings@tmcmed.org |
| Notes | Source of funding: sponsored by the University of
Missouri, Kansas City Conflicts of interest: details not provided |
NCT04745026.
| Study name | An exploratory, phase 2, randomized, double‐blind, placebo‐controlled trial to investigate the safety and efficacy of cannabidiol oral solution (GWP42003‐P; CBD‐OS) in children and adolescents with autism spectrum disorder |
| Methods | 12‐week parallel trial of GWP42003‐P (cannabidiol) versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria
Setting/location: 7 sites in the USA, and 2 sites in both Canada and the UK Sample size: 160 participants |
| Interventions | Intervention GWP42003‐P (100 mg/mL cannabidiol (CBD)
in sesame oil with anhydrous ethanol, ethanol
sweetener [sucralose], and strawberry flavouring),
administered twice a day (morning and evening) Comparator: "Oral placebo to match GWP42003‐P oral solution containing sesame oil with anhydrous ethanol, sweetener (sucralose), strawberry flavoring, and beta carotene, administered twice a day (morning and evening)". |
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: baseline, endpoint |
| Starting date | May 2021 |
| Contact information | Contact person: not provided Contact details: ClinicalTrialDisclosure@JazzPharma.com; info@gwpharm.com (UK contact) |
| Notes | Source of funding Conflicts of interest |
NCT04895215.
| Study name | A three‐arm, parallel group, randomized, double‐blind, placebo‐controlled study of the efficacy, safety, and tolerability of AB‐2004 in a 13 to 17 year‐old autism spectrum disorder population |
| Methods | 8‐week parallel trial of two doses of AB‐2004 versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria:
Setting/location: "13 sites in the U.S., and two sites in Australia/New Zealand combined." Sample size: target sample size is 195 |
| Interventions | Intervention: AB‐2004 (high‐dose) taken 3 times
daily; or AB‐2004 (low‐dose) taken 3 times daily Comparator: equivalent placebo taken 3 times daily |
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: baseline and endpoint (week 8) |
| Starting date | August 2021 |
| Contact information | Name:Jeffrey Young E‐mail: jeffrey@axialtx.com |
| Notes | Source of funding: details not reported Conflicts of interest: not reported |
NCT05015439.
| Study name | Cannabidiol (CBD) in adults with ASD |
| Methods | 14‐week cross‐over trial of cannabiodiol versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria: "history of alcohol or substance use disorder; positive urine tetrahydrocannabinol screen at onset of study; positive urine tetrahydrocannabinol screen at onset of study; individuals with unstable liver disease; individuals taking medications where CBD interaction might significantly alter drug levels, such as clobazam". Setting/location: USA Sample size: target sample size is 40 |
| Interventions | Intervention (cannabidiol): 100 mg cannabidiol twice
daily in capsule form, increasing to 200 mg twice
daily by week 3. This is followed by a 2‐week
wash‐out period before starting phase 2 of the
cross‐over. Comparator (placebo): equivalent placebo for 6 weeks. This is followed by a 2‐week wash‐out period before starting phase 2 of the cross‐over. |
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: baseline and six weeks (end of phase) |
| Starting date | Estimated start date: September 2022 |
| Contact information | Contact name: Elizabeth Wise Contact details: ewise11@jhmi.edu |
| Notes | Source of funding: Johns Hopkins University; Canopy
Growth Corporation Conflicts of interest: details not provided |
NCT05163717.
| Study name | INP105 proof‐of‐concept study for the acute treatment of agitation in adolescents with ASD (CALM 201) |
| Methods | Cross‐over trial of single‐dose INP105 (olanzapine) versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria:
Location/setting: USA Target sample size: 32 participants Gender: details not provided Mean age: details not provided IQ: details not provided Concomitant medications: details not provided Previous medications: details not provided |
| Interventions | Intervention (olanzapine): a single dose of 5 mg of
olanzapine Comparator (placebo): a single dose of equivalent placebo |
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: AEs measured up to 48 h post‐dose; aggression and irritability measured 30 minutes post‐dose. |
| Starting date | |
| Contact information | Contact name: Stephen Shrewsbury Contact details: sshrewsbury@impelpharma.com |
| Notes | Study start date: June 2022 Study end date: estimated to be January 2023 Source of funding: Impel NeuroPharma Inc. Conflicts of interest: details not provided |
NCT05182697.
| Study name | SCI‐210 in the treatment of children and young adults with autism evaluate the safety, tolerability and efficacy of SCI‐210 in children with autism spectrum disorder (ASD) |
| Methods | Cross‐over trial of palmitoylethanolamide versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria:
Setting/location: Israel Sample size: |
| Interventions | Intervention: oral cannabidiol oil plus pills of
CannAmide (palmitoylethanolamide (PEA) 400 mg twice
daily Comparator: active cannabidiol oil with twice‐daily placebo pills matched in appearance and taste to CannAmide active pill |
| Outcomes | Primary outcomes:
Secondary outcomes: none reported Timing of outcome assessments: the ABC will be measured at baseline and weeks 4 and 8 of each phase |
| Starting date | Approximately October 2022 |
| Contact information | Contact person: Gal Meiri Contact details: not provided |
| Notes |
Parellada 2021.
| Study name | Arbaclofen in children and adolescents with ASD (AIMS2‐CT1) |
| Methods | 16‐week parallel trial of arbaclofen versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria:
Setting/location: France, Spain and the UK Sample size: target sample size is 130 |
| Interventions | Intervention (arbaclofen) for 16 weeks: maximum of 15
mg 3 times daily for children aged 5‐11 years, and a
maximum of 20 mg/day for children aged 12‐17
years Comparator (placebo for 16 weeks): equivalent placebo |
| Outcomes | Primary outcomes:
Secondary outcomes: health‐related QoL (unclear the measure used) Timing of outcome assessments: unclear |
| Starting date | September 2019 |
| Contact information | Contact person: Inge Winter Contact details: I.Winter@umcutrecht.nl |
| Notes | Source of funding: "This project has received funding
from the Innovative Medicines Initiative 2 Joint
Undertaking under the grant agreement No. 777394 for
the project AIMS‐2‐TRIALS. This Joint Undertaking
receives support from the European Union's Horizon
2020 research and innovation program, EFPIA, Autism
Speaks, Autistica, and the Simons Foundation". Conflicts of interest: various authors had a consultancy or other working relationship with pharmaceutical companies Trial registry ‐ NCT03682978 |
UMIN000017876.
| Study name | Effects of long‐term administration of intranasal oxytocin in children with autism spectrum disorder |
| Methods | 4‐week cross‐over trial of oxytocin versus placebo |
| Participants | Inclusion criteria:
Exclusion criteria:
Setting/location: Japan Sample size: target sample size is 10 |
| Interventions | Intervention (oxytocin for 4 weeks followed by
placebo): 24 IU of oxytocin twice daily for 4 weeks,
then 1‐week washout followed by 4 weeks of
placebo Comparator (placebo for 4 weeks followed by oxytocin): placebo for 4 weeks followed by 1‐week washout period then 4 weeks of 24 IU oxytocin twice daily |
| Outcomes | Primary outcomes:
Secondary outcomes: unclear Timing of outcome assessments: unclear |
| Starting date | Registered in 2015 |
| Contact information | Name: Masako Taniike E‐mail: masako@ped.med.osaka‐u.ac.jp |
| Notes | Source of funding: unclear |
ABC‐I: Aberrant Behaviour Checklist: Irritability subscale; ADOS: Autism Diagnostic Observation Schedule; AE: adverse effect; ASD: Autism Spectrum Disorder; BoC: behaviours of concern; DSM:IV: Diagnostic and statistical Manual of Mental disorders (4th edition); DSM‐V: Diagnostic and statistical Manual of Mental disorders (5th edition); ICD‐10: International classification of diseases (10th edition); IGF‐1: insulin‐like growth factor‐1; PedsQL: Pediatric Quality of Life inventory; QoL: quality of life
Differences between protocol and review
Description of the intervention
The original classifications of medications for this review were to include: antidepressants, antipsychotics, cholinesterase inhibitors, mood stabilisers, and N‐methyl‐D‐aspartate (NMDA) receptor antagonists. However, because these categories were based on both function and pharmacological receptor activity, we modified these categories based on function and, where possible, conducted subgroup analyses based on pharmacological action. The major drug classes that were used, therefore, were typical and atypical antipsychotics, ADHD‐related drugs (both stimulant and non‐stimulant), anticonvulsants, antidementia drugs, antidepressants, antiparkinsonian drugs, anxiolytics, neurohormones, and a number of drugs that did not fall into any of these classes that we grouped under an experimental category.
Objectives
"To generate a clinically useful ranking of available pharmacological interventions for BoC in autism, according to their safety, efficacy, and tolerability." After consultation with a statistician (who was not involved in the review in any other way), it was decided that a network meta‐analysis was not feasible.
Unit of analysis issues
We originally planned to only include data from the first phase of cross‐over trials in the analysis. We found that only a very small percentage of cross‐over trials reported phase one data and as such, we decided to include data from all cross‐over trials provided the participants were randomised. This was due to the large number of studies that would have been excluded from the review had we only included trials that reported phase data.
As the majority of cros‐sover studies did not differentiate data from first and second phases we undertook sensitivity analyses to identify whether inclusion of these data had a differential effect on meta‐analytic estimates.
Types of outcome measures
Due to the wide range of adverse effect data that we collected during this review, a post‐protocol decision was made to categorise available data into the following groups; neurological, psychological, metabolic, musculoskeletal, cardiovascular, gastrointestinal, immune system, respiratory system, skin, urinary, and other.
We also decided to include improvement and relapse as outcomes because a few study authors reported either at least a 25% decrease (improvement) or a 25% increase (relapse) in ABC‐Irritability scores. We included these outcomes because they are related to the primary outcome of irritability.
Summary of findings and assessment of the certainty of the evidence
During the course of this review, a very large number of different types of 'adverse effects' were found to be reported by the included studies. To make the summary of findings table more readable and useful, the clinical content experts on the review team were asked to prioritise the list of available adverse effects, to decide which should be presented in the summary of findings table. The clinical experts were blinded to the type or availability of evidence available for each type of adverse effect when they made this decision, to ensure their choice was based on clinical importance and not data availability. As a result of this prioritisation exercise, the decision was made to present a narrative summary of the most important adverse effects in the four most clinically important categories: neurological, psychological, metabolic, and musculoskeletal.
Contributions of authors
Conception of the review: NL and authors of the protocol
Design of the review: NL and authors of the protocol
Co‐ordination of the review: NL, DG
Search and selection of studies for inclusion in review: DG, MI, MJ, NL
Collection of data for the review: DG, MI, MJ, NL
Assessment of the risk of bias, DG, MI, NL, MJ
Analysis of data: MI, NL, DG
Assessment of the certainty of the evidence: MI, DG, NL
Interpretation of data: MI, DG, NL
Writing of review: MI, DG, NL
Author of protocol and revising final draft: PH
All review authors contributed to the drafting and revising of the draft for important intellectual content.
Sources of support
Internal sources
-
Queen’s University Belfast, UK
Salary (Nuala Livingstone)
-
University of Melbourne, Australia
Salary (Katrina Williams)
-
University of Bristol, UK
Salary (Deborah M Caldwell)
-
Royal Children's Hospital, Australia
Salary (Louise Baker)
-
NDIS Quality and Safeguards Commission, Australia
Salary (Donna Gillies, Michelle Iffland and Mikaela Jorgensen)
External sources
-
Health and Social Care (HSC) Research & Development Division, Public Health Agency, Northern Ireland (NI), UK
Cochrane Fellowship (Nuala Livingstone)
-
UK Medical Research Council, Other
Population Health Scientist Fellowship award (G0902118) (Deborah M Caldwell)
Declarations of interest
Michelle Iffland is a Research Officer with the NDIS Quality and Safeguards Commission, NSW. The NDIS Quality and Safeguards Commission is committed to reducing and eliminating the use of restrictive practices in people with a disability.
Donna Gillies is the Director for Research and Practice Evidence with the NDIS Quality and Safeguards Commission, Penrith, NSW. The NDIS Quality and Safeguards Commission is committed to reducing and eliminating the use of restrictive practices in people with a disability.
Nuala Livingstone is a Quality Assurance Editor with the Cochrane Evidence Production and Methods Directorate, Central Editorial Service, and an Editor with Cochrane Developmental, Psychosocial and Developmental Problems (DPLP); UK. Nuala Livingstone was not involved in the editorial process for this article
Mikaela Jorgensen is the Assistant Director of Research with the NDIS Quality and Safeguards Commission, NSW, which is committed to the reduction and elimination of restrictive practices for people with disability.
Philip Hazell (PH) reports payments for lectures, for Lilly, Janssen, Pfizer and Shire, and advisory boards for Lilly, Janssen and Shire related to the pharmacological management of child and adolescent mental disorders in general; paid to Sydney Local Health District; PH is a Consultant Psychiatrist for Sydney Local Health District, NSW, and an Editor with Cochrane Developmental, Psychosocial and Learning Problems, UK. PH reports being involved in a study eligible for inclusion in this review: Multisite randomised control trail of fluoxetine for children and adolescents with autism; the study was funded by NHMRC and hosted by Murdoch Children's Research Institute, VIC. The researchers retained complete control over the study design, methods, data analysis and reporting. PH was not involved in assessing the studies for eligibility, extracting data from the studies, or assessing the risk of bias or grading the certainty of the evidence; these methods were completed by two independent review authors (DG, MI, MJ, NL).
New
References
References to studies included in this review
Akhondzadeh 2004 {published data only}
- Akhondzadeh S, Erfani S, Mohammadi MR, Tehrani-Doost M, Amini H, Gudarzi SS, et al. Cyproheptadine in the treatment of autistic disorder: a double‐blind placebo‐controlled trial. Journal of Clinical Pharmacy and Therapeutics 2004;29(2):145-50. [DOI: 10.1111/j.1365-2710.2004.00546.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Akhondzadeh 2008 {published data only}
- Akhondzadeh S, Tajdar H, Mohammadi M-R, Mohammadi M, Nouroozinejad G-H, Shabstari OL, et al. A double-blind placebo controlled trial of piracetam added to risperidone in patients with autistic disorder. Child Psychiatry and Human Development 2008;39(3):237-45. [DOI: 10.1007/s10578-007-0084-3] [PMID: ] [DOI] [PubMed] [Google Scholar]
Akhondzadeh 2010 {published data only}
- Akhondzadeh S, Fallah J, Mohammadi M-R, Imani R, Mohammadi M, Salehi B, et al. Double-blind placebo-controlled trial of pentoxifylline added to risperidone: effects on aberrant behavior in children with autism. Progress in Neuro-Psychopharmacology and Biological Psychiatry 2010;34(1):32-6. [DOI: 10.1016/j.pnpbp.2009.09.012] [PMID: ] [DOI] [PubMed] [Google Scholar]
Aman 2017 {published data only}
- Aman MG, Findling RL, Hardan AY, Hendren RL, Melmed RD, Kehinde-Nelson OK, et al. Safety and efficacy of memantine in children with autism: randomized, placebo-controlled study and open-label extension. Journal of Child and Adolescent Psychopharmacology 2017;27(5):403-12. [DOI: 10.1089/cap.2015.0146] [PMCID: PMC5510039] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT00872898. Study of pharmacokinetics, safety, efficacy, and tolerability of memantine in children with autism [An open-label (part one) and a randomized, double-blind, placebo-controlled (part two) study of the pharmacokinetics, safety, efficacy, and tolerability of memantine in pediatric patients with autism]. clinicaltrials.gov/ct2/show/NCT00872898 (first received 31 March 2009).
Anagnostou 2012 {published data only}
- Anagnosou E, Soorya L, Chaplin W, Bartz J, Halpern D, Wasserman S, et al. Intranasal oxytocin versus placebo in the treatment of adults with autism spectrum disorders: a randomized controlled trial. Molecular Autism 2012;3(1):16. [DOI: 10.1186/2040-2392-3-16] [PMCID: PMC3539865] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT00490802. Intranasal oxytocin in the treatment of autism. clinicaltrials.gov/ct2/show/NCT00490802 (first received 25 June 2007).
Aran 2021 {published data only}
- Aran A, Harel M, Cassuto H, Polyansky K, Schnapp A, Wattad1 N, et al. Cannabinoid treatment for autism: a proof-of-concept randomized trial. Molecular Autism 2021;12(6):6-6. [DOI: 10.1186/s13229-021-00420-2] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT02956226. Cannabinoids for behavioral problems in children with ASD (CBA). (first received 2 November 2016).
Arnold 2006 {published data only}
- Arnold LE, Aman M, Cook AM, Witwer AN, Hall KL, Thompson S, et al. Atomoxetine for hyperactivity in autism spectrum disorders: placebo-controlled crossover pilot trial. Journal of the American Academy of Child and Adolescent Psychiatry 2006;45(10):1196-205. [DOI: 10.1097/01.chi.0000231976.28719.2a] [PMID: ] [DOI] [PubMed] [Google Scholar]
Arnold 2012a {published data only}
- Arnold LE, Aman MG, Hollway J, Hurt E, Bates B, Li X, et al. Placebo-controlled pilot trial of mecamylamine for treatment of autism spectrum disorders. Journal of Child and Adolescent Psychopharmacology 2012;22(3):198-205. [DOI: 10.1089/cap.2011.0056] [PMCID: PMC3417385] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT00773812. Placebo-controlled pilot trial of mecamylamine for treatment of autism spectrum disorders [Neuronal nicotinic receptor modulation in the treatment of autism: a pilot trial of mecamylamine]. clinicaltrials.gov/ct2/show/NCT00773812 (first received 16 October 2008).
Asadabadi 2013 {published data only}IRCT138711091556N2
- Akhondzadeh S, Asadabadi M. Risperidone plus celecoxib in children with autistic disorder: a double-blind, randomized trial. British Journal of Clinical Pharmacology 2012;73(6):983-4. [DOI: 10.1111/j.1365-2125.2012.04253.x] [DOI] [Google Scholar]
- Asadabadi M, Mohammadi M-R, Ghanizadeh A, Modabbernia A, Ashrafi M, Hassanzadeh E, et al. Celecoxib as adjunctive treatment to risperidone in children with autistic disorder: a randomized, double-blind, placebo-controlled trial. Psychopharmacology 2013;225(1):51-9. [DOI: 10.1007/s00213-012-2796-8] [PMID: ] [DOI] [PubMed] [Google Scholar]
- IRCT138711091556N2. Celecoxib and autism [A double-blind placebo controlled trial of celecoxib added to risperidone in patients with autistic disorder]. www.irct.ir/trial/852 (first received 12 February 2009).
Ayatollahi 2020 {published data only}IRCT20090117001556N112
- Ayatollahi A, Bagheri S, Ashraf-Ganjouei A, Moradi K, Mohammadi M-R, Akhondzadeh S. Does pregnenolone adjunct to risperidone ameliorate irritable behavior in adolescents with autism spectrum disorder: a randomized, double-blind, placebo-controlled clinical trial? Clinical Neuropharmacology 2020;43(5):139-45. [DOI: 10.1097/WNF.0000000000000405] [PMID: ] [DOI] [PubMed] [Google Scholar]
- IRCT20090117001556N112. Efficacy of pregnenolon in treatment of irritability in teenagers with autism [Efficacy of pregnenolon in treatment of irritability in teeanagers with autism; a double blind and placebo controlled triall]. www.irct.ir/trial/32775 (first received 25 July 2018).
Batebi 2021 {published data only}IRCT20090117001556N114
- Batebi N, Moghaddam HS, Hasanzadeh A, Fakour Y, Mohammadi MR, Akhondzadeh S. Folinic acid as adjunctive therapy in treatment of inappropriate speech in children with autism: a double-blind and placebo-controlled randomized trial. Child Psychiatry & Human Development 2021;52(5):928-38. [DOI: 10.1007/s10578-020-01072-8] [PMID: ] [DOI] [PubMed] [Google Scholar]
- IRCT20090117001556N114. Folinic acid in the treatment of autism spectrum disorder [Folinic acid add on therapy to risperidone in symptoms of children with autism: a randomized double-blind placebo-controlled clinical trial]. www.irct.ir/trial/35172 (first received 15 November 2018).
Behmanesh 2019 {published data only}IRCT20090117001556N113
- Behmanesh H, Moghaddam HS, Mohammadi M-R, Akhondzadeh S. Risperidone combination therapy with propentofylline for treatment of irritability in autism spectrum disorders: a randomized, double-blind, placebo-controlled clinical trial. Clinical Neuropharmacology 2019;42(6):189-96. [DOI: 10.1097/WNF.0000000000000368] [PMID: ] [DOI] [PubMed] [Google Scholar]
- IRCT20090117001556N113. Effect of propentofylline in children with autism [Effect of propentofylline add on therapy to risperidon in children with autism: a randomized double-blind placebo-controlled clinical trial]. www.irct.ir/trial/35171 (first received 15 November 2018).
Belsito 2001 {published data only (unpublished sought but not used)}
- Belsito KM, Law PA, Kirk KS, Landa RJ, Zimmerman AW. Lamotrigine therapy for autistic disorder: a randomised, double-blind, placebo-controlled trial. Journal of Autism and Developmental Disorders 2001;31(2):175-81. [DOI: 10.1023/A:1010799115457] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Belsito K, Kirk K, Landa R, Law P, Zimmerman A. Lamotrigine therapy for childhood autism: a randomized, double-blind, placebo-controlled trial. Neurology 1998;50(4):A85. [DOI] [PubMed] [Google Scholar]
Bernaerts 2020 {published data only}
- Bernaerts S, Boets B, Bosmans G, Steyaert J, Alaerts K. Behavioral effects of multiple-dose oxytocin treatment in autism: a randomized, placebo-controlled trial with long-term follow-up. Molecular Autism 2020;11(1):6. [DOI: 10.1186/s13229-020-0313-1] [PMCID: PMC6964112] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernaerts S, Dillen C, Steyaert J, Alaerts K. The effects of four weeks of intranasal oxytocinon social responsiveness and repetitive and restricted behaviors in autism spectrum disorders: a randomized controlled trial. Biological Psychiatry 2020;81(10):S349-50. [ABSTRACT NO: 864] [DOI: 10.1016/j.biopsych.2017.02.589] [DOI] [Google Scholar]
- Eudract 2014-000586-45. Oxytocin-based pharmacotherapy for autism spectrum disorders: Investigating the neural and behavioral effects of a promising intervention approach. https://www.clinicaltrialsregister.eu/ctr-search/search?query=2014-000586-45 (first registered May 2014).
Buitelaar 1990 {published data only}
- Buitelaar JK, Van Engeland H, De Kogel KH, De Vries H, Van Hooff JA, Van Ree JM. The use of adrenocorticotrophic hormone (4-9) analog ORG 2766 in autistic children: effects on the organization of behavior. Biological Psychiatry 1992;31(11):1119-29. [DOI: 10.1016/0006-3223(92)90156-T] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Buitelaar JK, Van Engeland H, Van Ree JM, De Wied D. Behavioral effects of Org 2766, a synthetic analog of the adrenocorticotrophic hormone (4–9), in 14 outpatient autistic children. Journal of Autism and Developmental Disorders 1990;20(4):467-78. [DOI: 10.1007/BF02216053] [PMID: ] [DOI] [PubMed] [Google Scholar]
Campbell 1987 {published data only}
- Campbell M, Adams P, Small AM, Curren EL, Overall JE, Anderson LT, et al. Efficacy and safety of fenfluramine in autistic children. Journal of the American Academy of Child & Adolescent Psychiatry 1988;27(4):434-9. [DOI: 10.1097/00004583-198807000-00010] [PMID: ] [DOI] [PubMed] [Google Scholar]
Campbell 1993 {published data only}
- Campbell M, Anderson LT, Small AM, Adams P, Gonzalez NM, Ernst E. Naltrexone in autistic children: behavioral symptoms and attentional learning. Journal of the American Academy of Child and Adolescent Psychiatry 1993;32(6):1283-91. [DOI: 10.1097/00004583-199311000-00024] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Gonzalez NM, Campbell M, Small AM, Shay J, Bluhm LD, Adams PB, et al. Naltrexone plasma levels, clinical response and effect on weight in autistic children. Psychopharmacology Bulletin 1994;30(2):203-8. [PMID: ] [PubMed] [Google Scholar]
Carey 2002 {published data only}
- Carey T, Ratcliff-Schaub K, Funk J, Weinle C, Myers M, Jenks J, et al. Double-blind placebo-controlled trial of secretin: effects on aberrant behavior in children with autism. Journal of Autism and Developmental Disorders 2002;32(3):161-7. [DOI: 10.1023/A:1015493412224] [PMID: ] [DOI] [PubMed] [Google Scholar]
Chez 2020 {published data only}
- Chez M, Kile S, Lepage C, Parise C, Benabides B, Hankins A. A randomized, placebo-controlled, blinded, crossover, pilot study of the effects of dextromethorphan/quinidine for the treatment of neurobehavioral symptoms in adults with autism. Journal of Autism and Developmental Disorders 2020;50(5):1532-8. [DOI: 10.1007/s10803-018-3703-x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Chugani 2016 {published data only (unpublished sought but not used)}
- Chugani DC, Chugani HT, Wiznitzer M, Parikh S, Evans PA, Hansen RL, et al. Efficacy of low-dose buspirone for restricted and repetitive behavior in young children with autism spectrum disorder: a randomized trial. Journal of Pediatrics 2016;170:45-53.e1-4. [DOI: 10.1016/j.jpeds.2015.11.033] [PMID: ] [DOI] [PubMed] [Google Scholar]
- NCT00873509. Buspirone in the treatment of 2-6 year old children with autistic disorder (B-ACE) [A randomized, placebo-controlled, double-masked clinical trial of buspirone in the treatment of 2- 6 year old children with autistic disorder]. (first received 1 April 2009).
Dai 2021 {published data only}
- Dai Y, Zhang L, Yu J, Zhou X, He H, Ji Y, et al. Improved symptoms following bumetanide treatment in children aged 3-6 years with autism spectrum disorder: a randomized, double-blind, placebo-controlled trial. Science Bulletin 2021;66(15):1591-8. [DOI: 10.1016/j.scib.2021.01.008] [DOI] [PubMed] [Google Scholar]
- NCT03156153. A study of bumetanide for the treatment of autism spectrum disorders. (first received 15 May 2017).
Danfors 2005 {published data only}
- Danfors T, Von Knorring A-L, Hartvig P, Langstrom B, Moulder R, Stromberg B, et al. Tetrahydrobiopterin in the treatment of children with autistic disorder: a double-blind placebo-controlled crossover study. Journal of Clinical Psychopharmacology 2005;25(5):485-9. [DOI: 10.1097/01.jcp.0000177667.35016.e9] [PMID: ] [DOI] [PubMed] [Google Scholar]
Danforth 2018 {published data only}
- Danforth AL, Grob CS, Struble C, Feduccia AA, Walker N, Jerome L, et al. Reduction in social anxiety after MDMA-assisted psychotherapy with autistic adults: a randomized, double-blind, placebo-controlled pilot study. Psychopharmaology 2018;235(11):3137-48. [DOI: 10.1007/s00213-018-5010-9] [PMCID: PMC6208958] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT02008396. Phase 2 pilot safety study of MDMA-assisted therapy for socail anxiety in autistic adults. (first received 6 December 2013).
Dean 2019 {published data only}ACTRN12610000635066
- ACTRN12610000635066. Efficacy Of N-acetyl cysteine in autism: a double-blind, placebo-controlled randomised trial [Efficacy of n-acetyl cysteine on social skills, communication and behaviour in autistic children: a double-blind, placebo-controlled randomised trial]. www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=320918 (first received 3 August 2010).
- Dean OM, Gray K, Dodd S, Villagonzalo K-A, Brown E, Tonge B, et al. Does N-acetylcysteine improve behaviour in children with autism?: a mixed-methods analysis of the effects of N-acetylcysteine. Journal of Intellectual & Developmental Disability 2019;44(4):474-80. [DOI: 10.3109/13668250.2017.1413079] [DOI] [Google Scholar]
- Dean OM, Gray KM, Villagonzalo K-A, Dodd S, Mohebbi M, Vick T, et al. A randomised, double blind, placebo-controlled trial of a fixed dose of N-acetyl cysteine in children with autistic disorder. Australian and New Zealand Journal of Psychiatry 2017;51(3):241-9. [DOI: 10.1177/0004867416652735] [PMID: ] [DOI] [PubMed] [Google Scholar]
DeVane 2019 {published data only}
- DeVane CL, Charles JM, Abramson RK, Williams JE, Carpenter LA, Raven S, et al. Pharmacotherapy of autism spectrum disorder: results from the randomized BAART clinical trial. Pharmacotherapy 2019;39(6):626-35. [DOI: 10.1002/phar.2271] [PMCID: PMC6555676] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT01333072. Biomarkers in autism of aripiprazole and risperidone treatment (BAART) [Biomarkers in autism of aripiprazole and risperidone treatment]. clinicaltrials.gov/ct2/show/NCT01333072 (first received 11 April 2011).
Dollfus 1992 {published data only}
- Dollfus S, Petit M, Menard JF, Lesieur P. Amisulpride versus bromocriptine in infantile autism: a controlled crossover comparative study of two drugs with opposite effects on dopaminergic function. Journal of Autism and Developmental Disorders 1992;22(1):47-60. [DOI: 10.1007/BF01046402] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Dollfus S, Petit P, Menard JF. Pharmacoclinical study of an agonist and an antagonist of dopamine in early infantile autism. Neuropsychiatrie de l'Enfance et de l'Adolescence 1992;40(5-6):300-309. [Google Scholar]
Eslamzadeh 2018 {published data only}IRCT2016022826802N1
- Eslamzadeh M, Hebrani P, Behdani F, Moghadam MD, Panaghi L, Mirzadeh M, et al. Assessment the efficacy of atomoxetine in autism spectrum disorders: a randomized, double-blind, placebo-controlled trial. Iranian Journal of Psychiatry and Behavioral Sciences 2018;12(2):e10596. [DOI: 10.5812/ijpbs.10596] [DOI] [Google Scholar]
- IRCT2016022826802N1. Assessment the efficacy of atomoxetin(stramox) in autism spectrum disorders 6-17 years old. www.irct.ir/trial/22109 (first received 31 August 2016).
Fankhauser 1992 {published data only}
- Fankhauser MP, Karamanchi VC, German ML, Yates A, Karamanchi SD. A double-blind, placebo-controlled study of the efficacy of transdermal clonidine in autism. Journal of Clinical Psychiatry 1992;53(3):77-82. [PMID: ] [PubMed] [Google Scholar]
Findling 2014 {published data only}
- Findling RL, Mankoski R, Timko K, Lears K, McCartney T, McQuade RD, et al. A randomized controlled trial investigating the safety and efficacy of aripiprazole in the long-term maintenance treatment of pediatric patients with irritability associated with autistic disorder. Journal of Clinical Psychiatry 2014;75(1):22-30. [DOI: 10.4088/JCP.13m08500] [PMID: ] [DOI] [PubMed] [Google Scholar]
- NCT01227668. Phase IV long-term maintenance study of aripiprazole in the treatment of irritability associated with autistic disorder. https://clinicaltrials.gov/ct2/show/NCT01227668?term=NCT01227668&draw=2&rank=1 (first received October 2010).
Ghaleiha 2013a {published data only}IRCT1138901151556N10
- Ghaleiha A, Asababadi M, Mohammadi M-R, Shahei M, Tabrizi M, Hajiaghaee R, et al. Memantine as adjunctive treatment to risperidone in children with autistic disorder: a randomized, double-blind, placebo-controlled trial. International Journal of Neuropsychopharmacology 2013;16(4):783-9. [DOI: 10.1017/S1461145712000880] [PMID: ] [DOI] [PubMed] [Google Scholar]
- IRCT1138901151556N10. A double-blind placebo-controlled trial of memantine added to risperidone in patients with autistic disorder. https://www.irct.ir/trial/860 (first received May 2010).
Ghaleiha 2013b {published data only}IRCT201107281556N27
- Ghaleiha A, Mohammadi E, Mohammadi M-R, Farokhnia M, Modabbernia A, Yekehtaz H, et al. Riluzole as an adjunctive therapy to risperidone for the treatment of irritability in children with autistic disorder: a double-blind, placebo-controlled, randomized trial. Pediatric Drugs 2013;15(6):505-14. [DOI: 10.1007/s40272-013-0036-2] [PMID: ] [DOI] [PubMed] [Google Scholar]
- IRCT201107281556N27. Riluzole in the treatment of autism [Riluzole added to risperidone in the treatment of autism: a double blind and placebo controlled trial]. en.irct.ir/trial/877 (first received 30 July 2011).
Ghaleiha 2014 {published data only}IRCT201204081556N40
- Ghaleiha A, Ghyasvand M, Mohammadi M-R, Farokhnia M, Yadegari N, Tabrizi M, et al. Galantamine efficacy and tolerability as an augmentative therapy in autistic children: a randomized, double-blind, placebo-controlled trial. Journal of Psychopharmacology 2014;28(7):677-85. [DOI: 10.1177/0269881113508830] [PMID: ] [DOI] [PubMed] [Google Scholar]
- IRCT201204081556N40. Galantamine in the treatment of autism [Galantamine added to risperidone in the treatment of autism: a double blind and placebo controlled trial]. en.irct.ir/trial/890 (first received 14 April 2012).
Ghaleiha 2015 {published data only}IRCT201202281556N37
- Ghaleiha A, Rasa SM, Nikoo M, Farokhnia M, Mohammadi M-R, Akhondzadeh S. A pilot double-blind placebo-controlled trial of pioglitazone as adjunctive treatment to risperidone: effects on aberrant behavior in children with autism. Psychiatry Research 2015;229(1-2):181-7. [DOI: 10.1016/j.psychres.2015.07.043] [PMID: ] [DOI] [PubMed] [Google Scholar]
- IRCT201202281556N37. Pioglitazone in the treatment of autism [Pioglitazone added to risperidone in the treatment of autism: a double blind and placebo controlled trial]. en.irct.ir/trial/887 (first received 1 March 2012).
Ghaleiha 2016 {published data only}IRCT201302201556N50
- Ghaleiha A, Alikhani R, Kazemi M-R, Mohammadi M-R, Mohammadinejad P, Zeinoddini A, et al. Minocycline as adjunctive treatment to risperidone in children with autistic disorder: a randomized, double-blind placebo-controlled trial. Journal of Child and Adolescent Psychopharmacology 2016;26(9):784-91. [DOI: 10.1089/cap.2015.0175] [PMID: ] [DOI] [PubMed] [Google Scholar]
- IRCT201302201556N50. Minocycline in the treatment of autism [Minocycline added to risperidone in the treatment of autism: a double blind and placebo controlled trial ]. en.irct.ir/trial/900 (first received 21 February 2013).
Ghanizadeh 2013 {published data only}IRCT201106103930N6
- Ghanizadeh A, Moghimi-Sarani E. A randomized double blind placebo controlled clinical trial of N-acetylcysteine added to risperidone for treating autistic disorders. BMC Psychiatry 2013;13:196. [DOI: 10.1186/1471-244X-13-196] [PMCID: PMC3737121] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- IRCT201106103930N6. N-acetylcysteine augmentation with risperidone in treatment of autism in children [N-acetylcysteine augmentation with rispridone in treatment of autism in children: a double blind randomized placebo controlled clinical trial]. www.irct.ir/trial/4085 (first received 8 July 2011).
Ghanizadeh 2014 {published data only}IRCT201110233930N15
- Ghanizadeh A, Sahraeizadeh A, Berk M. A head-to-head comparison of aripiprazole and risperidone for safety and treating autistic disorders, a randomized double blind clinical trial. Child Psychiatry and Human Development 2014;45(2):185-92. [DOI: 10.1007/s10578-013-0390-x] [PMID: ] [DOI] [PubMed] [Google Scholar]
- IRCT201110233930N15. Aripiprazole versus risperidone for treatment of autism. www.irct.ir/trial/4094 (first received 12 December 2011).
Ghanizadeh 2015 {published data only}IRCT201307303930N28
- Ghanizadeh A, Ayoobzadehshirazi A. A randomized double-blind placebo-controlled clinical trial of adjuvant buspirone for irritability in autism. Pediatric Neurology 2015;52(1):77-81. [DOI: 10.1016/j.pediatrneurol.2014.09.017] [PMID: ] [DOI] [PubMed] [Google Scholar]
- IRCT201307303930N28. A randomized double blind placebo controlled clinical trial of buspirone for treating autism spectrum disorders. www.irct.ir/trial/4107 (first received 4 April 2014).
Gordon 1993 {published data only}
- Gordon CT, Rapoport JL, Hamburger SD, State RC, Mannheim GB. Differential response of seven subjects with autistic disorder to clomipramine and desipramine. American Journal of Psychiatry 1992;149(3):363-6. [DOI: 10.1176/ajp.149.3.363] [DOI] [PubMed] [Google Scholar]
- Gordon CT, State RC, Nelson JE, Hamburger SD, Rapoport JL. A double-blind comparison of clomipramine, desipramine, and placebo in the treatment of autistic disorder. JAMA 1993;50(6):2441-7. [DOI: 10.1001/archpsyc.1993.01820180039004] [DOI] [PubMed] [Google Scholar]
Guastella 2015a {published data only}ACTRN12609000513213
- ACTRN12609000513213. A course of oxytocin nasal spray (OT) to treat social problems in youth with autism spectrum disorders [A double blind randomised controlled trial of oxytocin nasal spray to treat social problems in autistic youth]. www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=83655 (first received 29 June 2009).
- Guastella AJ, Gray KM, Rinehart NJ, Alvares GA, Tonge BJ, Hickie IB, et al. The effects of a course of intranasal oxytocin on social behaviors in youth diagnosed with autism spectrum disorders: a randomized controlled trial. Journal of Child Psychology and Psychiatry 2015;56(4):444-52. [DOI: 10.1111/jcpp.12305] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hagerman 2018 {published data only}
- Hagerman R, Potter L, Biag H, Scholze D, Schneider A, Rivera S, et al. A controlled trial of sertraline in children 2 to 6 with ASD without fragile X syndrome. Journal of Intellectual Disability Research 2018;62(8):667-8. [DOI: 10.1111/jir.12512] [DOI] [Google Scholar]
- NCT02385799. A trial of sertraline in young children with autism spectrum disorder (Sert2). https://clinicaltrials.gov/ct2/show/NCT02385799?term=NCT02385799&draw=2&rank=1 (first received March 2015).
- Potter LA, Scholze DA, Biag HM, Schneider A, Chen Y, Nguyen DV, et al. A randomized controlled trial of sertraline in young children with autism spectrum disorder. Frontiers in Psychiatry 2019;10:810. [DOI: 10.3389/fpsyt.2019.00810] [PMCID: PMC6851992] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hajizadeh‐Zaker 2018 {published data only}IRCT201512081556N83
- Hajizadeh-Zaker R, Ghajar A, Mesgarpour B, Afarideh M, Mohammadi M-R, Akhondzadeh S. L-carnosine as an adjunctive therapy to risperidone in children with autistic disorder: a randomized, double-blind, placebo-controlled trial. Journal of Child and Adolescent Psychopharmacology 2018;28(1):74-81. [DOI: 10.1089/cap.2017.0026] [PMID: ] [DOI] [PubMed] [Google Scholar]
- IRCT201512081556N83. L carnosine in the treatment of autism [L carnosine added to risperidone in the treatment of autism: a double blind and placebo controlled trial]. www.irct.ir/trial/932 (first received 9 December 2015).
Handen 2005 {published data only}
- Handen BL, Hofkosh D. Secretin in children with autistic disorder: a double-blind, placebo-controlled trial. Journal of Developmental and Physical Disabilities 2005;17(2):95-107. [DOI: 10.1007/s10882-005-3682-7] [DOI] [Google Scholar]
Handen 2008 {published data only}
- Handen BL, Sahl R, Hardan AY. Guanfacine in children with autism and/or intellectual disabilities. Journal of Developmental & Behavioral Pediatrics 2008;29(4):303-8. [DOI: 10.1097/DBP.0b013e3181739b9d] [PMID: ] [DOI] [PubMed] [Google Scholar]
Handen 2011 {published data only}
- Handen BL, Johnson CR, McAuliffe-Bellin S, Hardan A. Safety and efficacy of donepezil in children - behavioural measures. International public health journal 2010;2(1):125-34. [Google Scholar]
- Handen BL, Johnson CR, Mcauliffe-Bellin S, Murray PJ, Hardan AY. Safety and efficacy of donepezil in children and adolescents with autism: neuropsychological measures. Journal of Child and Adolescent Psychopharmacology 2011;21(1):43-50. [DOI: 10.1089/cap.2010.0024] [PMCID: PMC3037196] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardan A, Johnson C, Handen BL. Preliminary findings from a double-blind placebo=controlled study of donepezil in pervasive developmental disorders. Biological Psychiatry 2006;59(8):50S-50S. [Google Scholar]
- NCT00047697. Donepezil HCl and cognitive deficits in autism. https://clinicaltrials.gov/ct2/show/results/NCT00047697?term=NCT00047697&draw=2&rank=1 (first received October 2002).
Handen 2015 {published data only}
- Arnold LE, Ober N, Aman MG, Handen B, Smith T, Pan X, et al. A 1.5-year follow-up of parent training and atomoxetine for attention-deficit/hyperactivity disorder symptoms and noncompliant/disruptive behavior in autism. Journal of Child and Adolescent Psychopharmacology 2018;28(5):322-30. [DOI: 10.1089/cap.2017.0134] [PMCID: PMC5994674] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handen BL, Aman MG, Arnold LE, Hyman SL, Tumuluru RV, Lecavalier L, et al. Atomoxetine, parent training, and their combination in children with autism spectrum disorder and attention-deficit/hyperactivity disorder. Journal of the American Academy of Child & Adolescent Psychiatry 2015;54(11):905-15. [DOI: 10.1016/j.jaac.2015.08.013] [PMCID: PMC4625086] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lecavalier L, Pan X, Smith T, Handen BL, Arnold LE, Silverman L, et al. Parent stress in a randomized clinical trial of atomoxetine and parent training for children with autism spectrum disorder. Journal of Autism and Developmental Disorders 2018;48(4):980-7. [DOI: 10.1007/s10803-017-3345-4] [PMCID: PMC6070148] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT00844753. Atomoxetine, placebo and parent management training in autism (Strattera) [Atomoxetine, placebo and parent management training in autism]. clinicaltrials.gov/ct2/show/NCT00844753 (first received 16 February 2016).
- Smith T, Aman MG, Arnold LE, Silverman LB, Lecavalier L, Hollway J, et al. Atomoxetine and parent training for children with autism and attention-deficit/hyperactivity disorder: a 24-week extension study. Journal of the American Academy of Child and Adolescent Psychiatry 2016;55(10):868-76.e2. [DOI: 10.1016/j.jaac.2016.06.015] [PMCID: PMC5108566] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tumuluru RV, Corbett-Dick P, Aman MG, Smith T, Arnold LE, Pan X, et al. Adverse events of atomoxetine in a double-blind placebo-controlled study in children with autism. Journal of Child and Adolescent Psychopharmacology 2017;27(8):708-14. [DOI: 10.1089/cap.2016.0187] [PMCID: PMC5651962] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hardan 2012 {published data only}
- Hardan A. Psychopharmacological treatment of anxiety symptoms in autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry 2016;55(10):S325-6. [DOI: 10.1016/j.jaac.2016.07.369] [ABSTRACT NO: 42.4] [DOI] [Google Scholar]
- Hardan AY, Fung LK, Libove RA, Obukhanych TV, Nair S, Herzenberg LA, et al. A randomised controlled pilot trial of N-acetylcysteine in children with autism. Biological Psychiatry 2012;71(11):956-61. [DOI: 10.1016//j.biopsych.2012.01.014] [PMCID: PMC4914359] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hardan 2019 {published data only}
- EUCTR 2012-001568-31. A double-blind, placebo-controlled, randomized withdrawal study of the safety and efficacy of memantine in pediatric patients with autism, Asperger’s disorder, or pervasive developmental disorder not otherwise specified (PDD-NOS) previously treated with memantine. www.clinicaltrialsregister.eu/ctr-search/trial/2012-001568-31/results (first posted November 2012).
- Hardan AY, Hendren RL, Aman MG, Robb A, Melmed RD, Andersen KA, et al. Efficacy and safety of memantine in children with autism spectrum disorder: results from three phase 2 multicenter studies. Autism 2019;23(8):2096-111. [DOI: 10.1177/1362361318824103] [PMCID: PMC6779018] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT01592747. Withdrawal study of memantine in pediatric patients with autism, Asperger's disorder, or pervasive developmental disorder not otherwise specified previously treated with memantine [A double-blind, placebo-controlled, randomized withdrawal study of the safety and efficacy of memantine in pediatric patients with autism, Asperger's disorder, or pervasive developmental disorder not otherwise specified (pdd-nos) previously treated with memantine]. clinicaltrials.gov/ct2/show/results/NCT01592747 (first received 7 May 2012).
Harfterkamp 2014 {published data only}
- Harfterkamp M, Buitelaar JK, Minderaa RB, Van de Loo-Neus G, Van De Gaag R-J, Hoekstra PJ. Atomoxetine in autism spectrum disorder: no effects on social functioning; some beneficial effects on stereotyped behaviours; inappropriate speech and fear of change. Journal of Child and Adolescent Psychopharmacology 2014;24(9):481-5. [DOI: 10.1089/cap.2014.0026] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Harfterkamp M, Van Der Meer J. Randomized double-blind study of atomoxetine vs. placebo followed by an open label extension period of treatment with atomoxetine for ADHD symptoms in children with ASD. European Child and Adolescent Psychiatry 2013;22(2):S216-17. [DOI: 10.1007/s00787-013-0423-9] [ABSTRACT NO: PS-012] [DOI] [Google Scholar]
- Harfterkamp M, Van de Loo-Neus G, Minderaa RB, Van der Gaag R-J, Escobar R, Schacht A, et al. A randomized double-blind study of atomoxetine versus placebo for attention-deficit/hyperactivity disorder symptoms in children with autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry 2012;51(7):733-41. [DOI: 10.1016/j.jaac.2012.04.011] [PMID: ] [DOI] [PubMed] [Google Scholar]
- NCT00380692. Atomoxetine versus placebo for symptoms of attention-deficit/hyperactivity disorder (ADHD) in children and adolescents with autism spectrum disorder [A randomized, double-blind comparison of atomoxetine hydrochloride and placebo for symptoms of attention-deficit/hyperactivity disorder in children and adolescents with autism spectrum disorder]. clinicaltrials.gov/ct2/show/NCT00380692 (first received 26 September 2006).
Hellings 2005 {published data only}
- Hellings JA, Weckbaugh M, Nickel EJ, Cain SE, Zarcone JR, Reese RM, et al. A double-blind, placebo-controlled study of valproate for aggression in youth with pervasive developmental disorders. Journal of Child and Adolescent Psychopharmacology 2005;15(4):682-92. [DOI: 10.1089/cap.2005.15.682] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hendouei 2019 {published data only}IRCT20090117001556N104
- Hendouei F, Moghaddam HS, Mohammadi MR, Taslimi N, Rezaei F, Akhondzadeh S. Resveratrol as adjunctive therapy in treatment of irritability in children with autism: a double‐blind and placebo‐controlled randomized trial. Journal of Clinical Pharmacy and Therapeutics 2020;45(2):324-34. [DOI: 10.1111/jcpt.13076] [PMID: ] [DOI] [PubMed] [Google Scholar]
- IRCT20090117001556N104. Resveratrol in treatment of autism [Resveratrol add on therapy to risperidone in irritibility of children with autism: a randomized double-blind placebo-controlled clinical trial]. www.irct.ir/trial/28378 (first received 25 December 2012).
Herscu 2020 {published data only}
- Herscu P, Handen BL, Arnold LE, Snape MF, Bregman JD, Ginsberg L, et al. The SOFIA Study: negative multi‑center study of low dose fluoxetine on repetitive behaviors in children and adolescents with autistic disorder. Journal of Autism and Developmental Disorders 2020;50(9):3233-44. [DOI: 10.1007/s10803-019-04120-y] [PMID: ] [DOI] [PubMed] [Google Scholar]
- NCT00515320. Study of fluoxetine in autism (SOFIA) [Study of fluoxetine in autism: a randomised, double-blind, placebo-controlled, parallel-group 14-week study to investigate the effect of fluoxetine orally dissolving tablet (odt) on repetitive behaviors in childhood and adolescent autistic disorder]. clinicaltrials.gov/ct2/show/NCT00515320 (first received 13 August 2007).
Hollander 2005 {published data only}
- Hollander E, Swanson E, Anagnostou E, Phillips A, Chaplin W, Wasserman S. Liquid fluoxetine versus placebo for repetitive behaviors in childhood autism. Progress in Neurotherapeutics and Neuropsychopharmacology 2006;1(1):105-13. [DOI: 10.1017/S1748232105000108] [DOI] [Google Scholar]
- HollanderE, Phillips A, Chaplin W, Zagursky K, Novotny S, Wasserman S, et al. A placebo controlled crossover trial of liquid fluoxetine on repetitive behaviours in childhood and adolescent autism. Neuropsychopharmacology 2005;30(3):582-9. [DOI: 10.1038/sj.npp.1300627] [PMID: ] [DOI] [PubMed] [Google Scholar]
- NCT00004486. Randomized study of fluoxetine in children and adolescents with autism. clinicaltrials.gov/ct2/show/NCT00004486 (first received 19 October 1999).
Hollander 2006a {published data only}
- Hollander E, Soorya L, Wasserman S, Esposito K, Chaplin W, Anagnostou E. Divalproex sodium vs placebo in the treatment of repetitive behaviours in autism spectrum disorder. International Journal of Neuropsychopharmacology 2006;9(2):209-13. [DOI: 10.1017/S1461145705005791] [PMID: ] [DOI] [PubMed] [Google Scholar]
- NCT00211757. Divalproex sodium versus placebo in childhood/adolescent autism. https://clinicaltrials.gov/ct2/show/results/NCT00211757?term=NCT00211757&draw=2&rank=1 (first received September 2005).
Hollander 2006b {published data only}
- Hollander E, Wasserman S, Swanson EN, Chaplin W, Schapiro ML, Zagursky K, et al. A double-blind placebo-controlled pilot study of olanzapine in childhood/adolescent pervasive developmental disorder. Journal of Child and Adolescent Psychopharmacology 2006;16(5):541-8. [DOI: 10.1089/cap.2006.16.541] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hollander 2010 {published data only}
- Anagnostou E, Soorya L, Swanson E, Rusoff J, Chaplin W, Wasserman S, et al. Divalproex sodium vs placebo for the treatment of child and adolescent autism. European Neuropsychopharmacology 2006;16:S74-5. [DOI: 10.1016/S0924-977X(06)80088-X] [DOI] [Google Scholar]
- Hollander E, Chaplin W, Soorya L, Wasserman S, Novotny S, Rusoff J, et al. Divalproex sodium vs placebo for the treatment of irritability in children and adolescents with autism spectrum disorders. Neuropsychopharmacology 2010;35(4):990-8. [DOI: 10.1038/npp.2009.202] [PMCID: PMC2846602] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollander E, Soorya L, Wasserman S, Esposito K, Chaplin W, Anagnostou E. Divalproex sodium vs placebo in the treatment of repetitive behaviours in autism spectrum disorder. International Journal of Neuropsychopharmacology 2006;9(2):209-13. [DOI: 10.1017/S1461145705005791] [PMID: ] [DOI] [PubMed] [Google Scholar]
- NCT00211757. Divalproex sodium vs. placebo in childhood/adolescent autism. https://clinicaltrials.gov/ct2/show/NCT00211757?term=NCT00211757&draw=1&rank=1 (first received September 2005).
Hollander 2012 {published data only (unpublished sought but not used)}
- Hollander E, Soorya L, Chaplin W, Anagnostou E, Taylor BP, Ferretti CJ, et al. A double-blind placebo-controlled trial of fluoxetine for repetitive behaviors and global severity in adult autism spectrum disorders. American Journal of Psychiatry 2012;169(3):292-9. Erratum in: American Journal of Psychiatry. 2012 May;169(5):540. [DOI: 10.1176/appi.ajp.2011.10050764] [PMID: ] [DOI] [PubMed] [Google Scholar]
- NCT00004486. Randomized study of fluoxetine in children and adolescents with autism. https://clinicaltrials.gov/show/NCT00004486 (first received 19 October 1999).
Hollander 2020a {published data only}
- Hollander E, Ferretti CJ, Taylor BP, Noone RH, Racine E. P.7.d.006 Trichuris suis ova (TSO) as an immune-inflammatory treatment for repetitive behaviors in autism spectrum disorders (ASD). European Neuropsychopharmacology 2014;24(2):S723. [DOI: 10.1016/S0924-977X(14)71165-4] [DOI] [Google Scholar]
- Hollander E, Uzunova G, Taylor BP, Noone R, Racine E, Doernberg E, et al. Randomized crossover feasibility trial of helminthic Trichuris suis ova versus placebo for repetitive behaviors in adult autism spectrum disorder. World Journal of Biological Psychiatry 2020;21(4):291-9. [DOI: 10.1080/15622975.2018.1523561] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Hollander E, Ferretti C, Taylor B, Noone R, Kirsch J, Racine E. Trichuris suis ova (TSO) as an immune inflammatory treatment for repetitive behaviors in ASD. Neuropsychopharmacology 2013;38:S391-2. [DOI: 10.1038/npp.2013.280] [DOI] [Google Scholar]
- Hollander E, Uzunova G, Taylor BP, Noone R, Racine E, Doernberg E, et al. Randomized crossover feasibility trial of helminthic Trichuris suis ova versus placebo for repetitive behaviors in adult autism spectrum disorder. World Journal of Biological Psychiatry 2020;21(4):291-9. [DOI: 10.1080/15622975.2018.1523561] [PMID: ] [DOI] [PubMed] [Google Scholar]
- NCT01040221. Trichuris suis ova in autism spectrum disorders (TSO) [Trichuris suis ova in autism spectrum disorders ]. www.clinicaltrials.gov/ct2/show/NCT01040221 (first received November 2012).
- Stark FS, Chavanne C, Lennon-Chrimes S, Diack C, Derks M, Smith J. Paediatric dosing of balovaptan for the treatment of the core symptoms of autism spectrum disorder: data from a Phase 2 study (aV1ation; NCT02901431). European Neuropsychopharmacology 2020;40:S82-S83. [DOI: 10.1016/j.euroneuro.2020.09.110] [DOI] [Google Scholar]
Hollander 2020b {published data only}
- Hollander E, Jacob S, Jou R, McNamara N, Sikich L, Tobe R, et al. A phase 2 randomized controlled trial (RCT) of balovaptan (BAL) in pediatric participants with autism spectrum disorder (ASD). Neuropsychopharmacology 2021;46:152. [DOI: 10.1038/s41386-021-01236-7] [DOI] [Google Scholar]
- Hollander E, Jacob S, Jou RJ, McNamara N, Sikich L, Tobe R, et al. Phase 2 randomized controlled trial of balovaptan in pediatric participants with autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry 2020;59(10):S262-S263. [DOI: 10.1016/j.jaac.2020.08.458] [DOI] [Google Scholar]
- NCT02901431. A study to investigate the efficacy and safety of balovaptan (RO5285119) in participants with autism spectrum disorder (ASD). www.clinicaltrials.gov/ct2/show/NCT02901431?term=NCT02901431&draw=2&rank=1 (first received 21 November 2016).
Ichikawa 2017 {published data only}
- Ichikawa H, Mikami K, Okada T, Yamashita Y, Ishizaki Y, Tomoda A, et al. Aripiprazole in the treatment of irritability in children and adolescents with autism spectrum disorder in Japan: a randomized, double-blind, placebo-controlled study. Child Psychiatry & Human Development 2017;48(5):796-806. [DOI: 10.1007/s10578-016-0704-x] [PMCID: PMC5617873] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT01617447. A short treatment study of aripiprazole in pediatric patients with autistic disorder [A short-term administration study of aripiprazole in children and adolescents (age: 6 to 17 years) with autistic disorder]. clinicaltrials.gov/ct2/show/NCT01617447 (first received 12 June 2012).
Jacob 2022 {published data only}
- Jacob S, Veenstra-VanderWeele J, Murphy D, McCracken J, Smith J, Sanders K, et al. Efficacy and safety of balovaptan for socialisation and communication difficulties in autistic adults in North America and Europe: a phase 3, randomised, placebo-controlled trial. Lancet 2022;9(3):199-210. [DOI: 10.1016/S2215-0366(21)00429-6] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Jacob S, Veenstra-VanderWeele J, Murphy D, McCracken J, Smith J, Sanders K, et al. Phase three randomised controlled trial of balovaptan in adults with autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry 2020;59(10):S163-S163. [DOI: 10.1016/j.jaac.2020.08.108] [DOI] [Google Scholar]
- NCT03504917. A study of balovaptan in adults with autism spectrum disorder with a 2-year open-label extension. clinicaltrials.gov/ct2/show/NCT03504917?term=NCT03504917&draw=2&rank=1 (first received 8 August 2018).
Jaselskis 1992 {published data only}
- Jaselskis CA, Cook EH, Fletcher KE, Leventhal BL. Clonidine treatment of hyperactive and impulsive children with autistic disorder. Journal of Clinical Psychopharmacology 1992;12(5):322-7. [PMID: ] [PubMed] [Google Scholar]
Kent 2013 {published data only}
- Kent JM, Kushner S, Ning X, Karcher K, Ness S, Aman M, et al. Risperidone dosing in children and adolescents with autistic disorder: a double-blind placebo-controlled study. Journal of Autism and Developmental Disorders 2013;43(8):1773-83. [DOI: 10.1007/s10803-012-1723-5] [PMID: ] [DOI] [PubMed] [Google Scholar]
- NCT00576732. A study of the effectiveness and safety of two doses of risperidone in the treatment of children and adolescents with autistic disorder [Risperidone in the treatment of children and adolescents with autistic disorder: a double-blind, placebo-controlled study of efficacy and safety, followed by an open-label extension study of safety]. clinicaltrials.gov/ct2/show/NCT00576732 (first received 19 December 2007).
Khalaj 2018 {published data only}IRCT201702171556N96
- IRCT201702171556N96. Palmitoylethanolamide as adjunctive treatment of autism: a double blind and placebo controlled trial. en.irct.ir/trial/945 (first received 20 February 2017).
- Khalaj M, Saghazadeh A, Shirazi E, Shalbafan M-R, Alavi K, Shooshtari MH, et al. Palmitoylethanolamide as adjunctive therapy for autism: efficacy and safety results from a randomized controlled trial. Journal of Psychiatric Research 2018;103:104-11. [DOI: 10.1016/j.jpsychires.2018.04.022] [PMID: ] [DOI] [PubMed] [Google Scholar]
King 2001 {published data only (unpublished sought but not used)}
- King BH, Wright DM, Handen BL, Sikich L, Zimmerman AW, Mcmahon W, et al. Double-blind, placebo-controlled study of amantadine hydrochloride in the treatment of children with autistic disorder. Journal of the American Academy of Child & Adolescent Psychiatry 2001;40(6):658-65. [DOI: 10.1097/00004583-200106000-00010] [PMID: ] [DOI] [PubMed] [Google Scholar]
King 2009 {published data only}
- King BH, Hollander E, Sikich L, McCracken JT, Scahill L, Bregman JD, et al. Lack of efficacy of citalopram in children with autism spectrum disorders and high levels of repetitive behavior: citalopram ineffective in children with autism. Archives of General Psychiatry 2009;66(6):583-90. [DOI: 10.1001/archgenpsychiatry.2009.30] [PMCID: PMC4112556] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers SM. Citalopram not effective for repetitive behavior in autistic spectum disorders. Evidence-Based Mental Health 2010;13(1):22. [DOI: 10.1136/ebmh.13.1.22] [PMID: ] [DOI] [PubMed] [Google Scholar]
- NCT00086645. Citalopram for children with autism and repetitive behavior (STAART Study 1) [Citalopram treatment in children with autism spectrum disorders and high levels of repetitive behavior]. clinicaltrials.gov/ct2/show/NCT00086645 (first received 13 July 2004).
- Scahill L, McCracken JT, Bearss K, Robinson F, Hollander E, King B, et al. Design and subject characteristics in the federally-funded citalopram trial in children with pervasive developmental disorders. Journal of Autism and Developmental Disorders 2012;42(3):432-40. [DOI: 10.1007/s10803-011-1251-8] [PMID: ] [DOI] [PubMed] [Google Scholar]
Klaiman 2013 {published data only}
- Klaiman C, Huffman L, Masaki L, Elliott GR. Tetrahydrobiopterin as a treatment for autism spectrum disorders: a double-blind, placebo-controlled trial. Journal of Child and Adolescent Psychopharmacology 2013;13(5):320-8. [DOI: 10.1089/cap.2012.0127] [PMID: ] [DOI] [PubMed] [Google Scholar]
- NCT00850070. Sapropterin as a treatment for autistic disorder. https://clinicaltrials.gov/ct2/show/results/NCT00850070?term=NCT00850070&draw=2&rank=1 (first received February 2009).
Le 2022 {published data only}ChiCTR1900023774
- ChiCTR1900023774. The effects of chronic intranasal oxytocin combined with positive social interaction in the treatment of young children with autism. www.chictr.org.cn/showproj.aspx?proj=39640 (first received 11 June 2019).
- Le J, Zhang L, Zhao W, Zhi S, Lan C, Kou J, et al. Infrequent intranasal oxytocin followed by positive social interaction improves symptoms in autistic children: a pilot randomized clinical trial. Psychotherapy and Psychosomatics 2022;91(5):335-47. [DOI: 10.1159/000524543] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lemonnier 2017 {published data only}
- Lemonnier E, Villeneuve N, Sonie S, Rosier A, Roue M, Brosset P, et al. Effects of bumetanide on neurobehavioral function in children and adolescents with autism spectrum disorders. Translational Psychiatry 2017;7(3):e1056. [DOI: 10.1038/tp.2017.10] [PMCID: PMC5416661] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT01078714. Efficiency of bumetanide in autistic children (BUMEA). https://clinicaltrials.gov/ct2/show/NCT01078714?term=NCT01078714&draw=1&rank=1 (first received March 2010).
Levy 2003 {published data only}
- Levy SE, Souders MC, Wray J, Jawad AF, Gallagher PR Coplin J, et al. Children with autistic spectrum disorders. I: comparison of placebo and single dose of human synthetic secretin. Archives of Disease in Childhood 2003;88(8):731-6. [DOI: 10.1136/adc.88.8.731] [PMCID: PMC1719589] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lewis 2018 {published data only}
- Lewis AS, Van Schalkwy GI, Lopez MO, Volkmar FR, Picciotto MR, Sukhodolsky DG. An exploratory trial of transdermal nicotine for aggression and irritability in adults with autism spectrum disorder. Journal of Autism and Developmental Disorders 2018;48(8):2748-57. [DOI: 10.1007/s10803-018-3536-7] [PMCID: PMC6394231] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT02552147. Nicotinic cholinergic modulation as a novel treatment strategy for aggression associated with autism [Nicotinic cholinergic modulation as a novel treatment strategy for aggression associated with autism]. clinicaltrials.gov/ct2/show/NCT02552147 (first received 16 September 2015).
Loebel 2016 {published data only}
- Loebel A, Brams M, Goldman RS, Silva R, Hernandez D, Deng L, et al. Lurasidone for the treatment of irritability associated with autistic disorder. Journal of Autism and Developmental Disorders 2016;46(4):1153-63. [DOI: 10.1007/s10803-015-2628-x] [PMCID: PMC4786592] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT01911442. Lurasidone pediatric autism study. https://clinicaltrials.gov/ct2/show/results/NCT01911442?term=NCT01911442&draw=2&rank=1 (first received July 2013).
Luby 2006 {published data only}
- Luby J, Mrakotsky C, Stalets MM, Belden A, Heffelfinger A, Williams M, et al. Risperidone in preschool children with autistic spectrum disorders: an investigation of safety and efficacy. Journal of Child and Adolescent Psychopharmacology 2006;16(5):575-87. [DOI: 10.1089/cap.2006.16.575] [PMID: ] [DOI] [PubMed] [Google Scholar]
Mace 2001 {published data only (unpublished sought but not used)}
- Mace CF, Blum NJ, Sierp BJ, Delaney BA, Mauk JE. Differential response of operant self-Injury to pharmacologic versus behavioral treatment. Journal of Developmental & Behavioral Pediatrics 2001;22(2):85-91. [DOI: 10.1097/00004703-200104000-00001] [PMID: ] [DOI] [PubMed] [Google Scholar]
Mahdavinasab 2019 {published data only}IRCT201701131556N95
- IRCT201701131556N95. Baclofen in the treatment of autism [Baclofen as adjunctive treatment of autism: a double blind and placebo controlled trial]. www.irct.ir/trial/944 (first received 13 January 2017).
- Mahdavinasab S-M, Saghazadeh A, Motamed-Gorji N, Vaseghi S, Mohammadi M-R, Alichani R, et al. Baclofen as an adjuvant therapy for autism: a randomized, double-blind, placebo-controlled trial. European Child & Adolescent Psychiatry 2019;28(12):1619-28. [DOI: 10.1007/s00787-019-01333-5] [PMID: ] [DOI] [PubMed] [Google Scholar]
Malek 2020 {published data only}IRCT20090117001556N102
- IRCT20090117001556N102. Prednisolone in autism spectrum disorders [Prednisolone in regressive autism spectrum disorders: a randomized double-blind placebo-controlled clinical trial]. www.irct.ir/trial/28026 (first received 9 December 2017).
- Malek M, Ashraf-Ganjouei A, Moradi K, Bagheri S, Mohammadi M-R, Akhonzadeh S. Prednisolone as adjunctive treatment to risperidone in children with regressive type of autism spectrum disorder: a randomized, placebo-controlled trial. Clinical Neuropharmacology 2020;43(2):39-45. [DOI: 10.1097/WNF.0000000000000382] [PMID: ] [DOI] [PubMed] [Google Scholar]
Malone 2001 {published data only}
- Malone RP, Cater J, Sheikh RM, Choudhury MS, Delaney MA. Olanzapine versus haloperidol in children with autistic disorder: an open pilot study. Journal of the American Academy of Child and Adolescent Psychiatry 2001;40(8):887-94. [DOI: 10.1097/00004583-200108000-00009] [PMID: ] [DOI] [PubMed] [Google Scholar]
Marcus 2009 {published data only}
- Benton TD. Aripiprazole to treat irritability associated with autism: a placebo-controlled, fixed-dose trial. Current Psychiatric Reports 2011;13(2):77-9. [DOI: 10.1007/s11920-010-0172-0] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Curran MP. Aripiprazole in the treatment of irritability associated with autistic disorder in paediatric patients: profile report. CNS Drugs 2011;25(9):801-2. [DOI: 10.2165/11208280-000000000-00000] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Lewis D, Couch D, Marcus R, Manos G, Mankoski R, Carson W, et al. Efficacy and safety of fixed-dose aripiprazole for the treatment of irritability associated with autistic disorder in children and adolescents (6-17 years). Annals of Neurology 2009;66:S110. [Google Scholar]
- Mankosky R, Stockton G, Manos G, Marler S, McQuade R, Forbes RA, et al. Aripiprazole treatment of irritability associated with autistic disorder and the relationship between prior antipsychotic exposure, adverse events, and weight change. Journal of Child and Adolescent Psychopharmacology 2013;23(8):572-6. [DOI: 10.1089/cap.2012.0075] [PMCID: PMC3804231] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus RN, Owen R, Kamen L, Manos G, McQuade RD, Carson WH, et al. A placebo-controlled, fixed-dose aripiprazole in children and adolescents with irritability associated with autistic disorder. Journal of the American Academy of Child and Adolescent Psychiatry 2009;48(11):1110-9. [DOI: 10.1097/CHI.0b013e3181b76658] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Varni JW, Handen BL, Corey-Lisle PK, Guo Z, Manos G, Ammerman DK, et al. Effect of aripiprazole 2 to 15 mg/day on health-related quality of life in the treatment of irritability associated with autistic disorder in children: a post-hoc analysis of two controlled trials. Clinical Therapeutics 2012;34(4):980-92. [DOI: 10.1016/j.clinthera.2012.02.023] [PMID: ] [DOI] [PubMed] [Google Scholar]
McCracken 2002 {published data only}
- Aman M, Rettiganti M, Nagaraja HN, Hollway JA, McCracken J, McDougle CJ, et al. Tolerability, safety, and benefits of risperidone in children and adolescents with autism: 21-month follow-up after 8-week placebo-controlled trial. Journal of Child & Adolescent Psychopharmacology 2015;25(6):482-93. [DOI: 10.1089/cap.2015.0005] [PMCID: PMC4545698] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aman MG, Arnold LE, McDougle CJ, Vitiello B, Scahill L, Davies MD, et al. Acute and long-term safety and tolerability of risperidone in children with autism. Journal of Child and Adolescent Psychopharmacology 2005;15(6):869-84. [DOI: 10.1089/cap.2005.15.869] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Aman MG, Hollway JA, McDougle CJ, Scahill L, Tierney E, McCracken JT, et al. Cognitive effects of risperidone in children with autism and irritable behavior. Journal of Child and Adolescent Psychopharmacology 2008;18(3):227-36. [DOI: 10.1089/cap.2007.0133] [PMCID: PMC2935828] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold LE, Aman MG, Martin A, Collier-Crespin A, Vitiello B, Tierney E, et al. Assessment in multisite randomized clinical trials of patients with autistic disorder: the Autism RUPP Network. Research Units on Pediatric Psychopharmacology. Journal of Autism and Developmental Disorders 2000;30(2):99-111. [DOI: 10.1023/a:1005451304303] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Arnold LE, Farmer C, Kraemer HC, Davies M, Witwer A, Chuang S, et al. Moderators, mediators, and other predictors of risperidone response in children with autistic disorder and irritability. Journal of Child & Adolescent Psychopharmacology 2010;20(2):83-93. [DOI: 10.1089/cap.2009.0022] [PMCID: PMC2865212] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold LE, Vitiello B, McDougle C, Scahill L, Shah B, Gonzalez NM, et al. Parent-defined target symptoms respond to risperidone in RUPP autism study: customer approach to clinical trials. Journal of the American Academy of Child and Adolescent Psychiatry 2003;42(12):1443-50. [DOI: 10.1097/00004583-200312000-00011] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Caicedo C, Williams SH. Risperidone improves behavior in children with autism. Journal of Family Practice 2002;51(11):915. [PMID: ] [PubMed] [Google Scholar]
- Fombonne E. Risperidone improves restricted, repetitive, and stereotyped behaviour in autistic children and adolescents. Evidence-Based Mental Health 2006;9(1):6. [DOI: 10.1136/ebmh.9.1.6] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Levine SZ, Kodesh A, Goldberg Y, Reichenberg A, Furukawa TA, Kolevzon A, et al. Initial severity and efficacy of risperidone in autism: results from the RUPP trial. European Psychiatry 2016;32:16-20. [DOI: 10.1016/j.eurpsy.2015.11.004] [PMID: ] [DOI] [PubMed] [Google Scholar]
- McCracken JT, McGough J, Shah B, Cronin P, Hong D, Aman MG, et al. Risperidone in children with autism and serious behavioural problems. New England journal of medicine 2002;347(5):314-21. [DOI: 10.1056/NEJMoa013171] [PMID: ] [DOI] [PubMed] [Google Scholar]
- McDougle C, Aman M, McCracken J, Scahill L, Tierney E, Vitiello B. A double-blind placebo-controlled trial of risperidone in autistic disorder. European Neuropsychopharmacology 2003;13:S327-8. [DOI: 10.1016/S0924-977X(03)92062-1] [POSTER NO: P.2.109] [DOI] [Google Scholar]
- McDougle CJ, Scahill L, Aman MG, McCracken JT, Tierney E, Davies M, et al. Risperidone for the core symptom domains of autism: results from the study by the Autism Network of the Research Units on Pediatric Psychopharmacology. American Journal of Psychiatry 2005;16(2):1142-8. [DOI: 10.1176/appi.ajp.162.6.1142] [PMID: ] [DOI] [PubMed] [Google Scholar]
- NCT00005014. Treatment of autism in children and adolescents [Placebo-controlled study of risperidone for the treatment of children and adolescents with autism and negative behavioral symptoms]. www.clinicaltrials.gov/ct2/show/NCT00005014 (first received 3 April 2000).
- Research Units on Pediatric Psychopharmacology Autism Network. Risperidone treatment of autistic disorder: longer-term benefits and blinded discontinuation after 6 months. American Journal of Psychiatry 2005;162(7):1361-9. [DOI: 10.1176/appi.ajp.162.7.1361] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Scahill L, Hallett V, Aman MG, McDougle CJ, Arnold LE, McCracken JT, et al. Brief report: social disability in autism spectrum disorder: results from Research Units on Pediatric Psychopharmacology (RUPP) Autism Network trials. Journal of Autism and Developmental Disorders 2013;43(3):739-46. [DOI: 10.1007/s10803-012-1689-3] [PMCID: PMC3886122] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scahill L, Koenig, Carroll DH, Pachler M. Risperidone approved for the treatment of serious behavioral problems in children with autism. Journal of Child & Adolescent Psychiatric Nursing 2007;20(3):188-90. [DOI: 10.1111/j.1744-6171.2007.00112.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Study of risperidone with autistic children finds no detrimental cognitive effects. Brown University Child & Adolescent Psychopharmacology Update 2008;10(9):3. [DOI: 10.1002/cpu.20075] [DOI]
- Williams SK, Scahill L, Vitiello B, Aman MG, Arnold LE, McDougle CJ, et al. Risperidone and adaptive behavior in children with autism. Journal of the American Academy of Child & Adolescent Psychiatry 2006;45(4):431-9. [DOI: 10.1097/01.chi.0000196423.80717.32] [PMID: ] [DOI] [PubMed] [Google Scholar]
McDougle 1996 {published data only (unpublished sought but not used)}
- Huffman G. Fluvoxamine for the treatment of autistic disorders in adults. American Family Physician 1997;55(4):1375-4. [Google Scholar]
- McDougle CJ, Naylor ST, Cohen DJ, Volkmar FR, Heninger GR, Price LH. A double-blind, placebo-controlled study of fluvoxamine in adults with autistic disorder. Archives of General Psychiatry 1996;53(11):1001-8. [DOI: 10.1001/archpsyc.1996.01830110037005] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Vegso SJ. A double-blind placebo-controlled study of fluvoxamine in treating the symptoms of autism [Master's thesis]. New Haven (CT): Southern Connecticut State University, 1995. [Google Scholar]
McDougle 1998 {published data only}
- McDougle CJ, Holmes JP, Carlson DC, Pelton GH, Cohen DJ, Price LH. A double-blind, placebo-controlled study of risperidone in adults with autistic disorder and other pervasive developmental disorders. Archives of General Psychiatry 1998;55(7):633-41. [DOI: 10.1001/archpsyc.55.7.633] [PMID: ] [DOI] [PubMed] [Google Scholar]
Minshawi 2016 {published data only}
- Minshawi NF, Wink LK, Shaffer R, Plawecki MH, Posey DJ, Liu H, et al. A randomized, placebo-controlled trial of D-cycloserine for the enhancement of social skills training in autism spectrum disorders. Molecular Autism 2016;7(3):2. [DOI: 10.1186/s13229-015-0062-8] [PMCID: PMC4712595] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT01086475. D-cycloserine and social skills training in autism spectrum disorders. https://clinicaltrials.gov/ct2/show/NCT01086475?term=NCT01086475&draw=1&rank=1 (first received March 2010).
- Wink LK, Minshawi NF, Shaffer RC, Plawecki MH, Posey DJ, Horn PS, et al. D-cycloserine enhances durability of social skills training in autism spectrum disorder. Molecular Autism 2017;8:2. [DOI: 10.1186/s13229-017-0116-1] [PMCID: PMC5264460] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Miral 2008 {published data only (unpublished sought but not used)}
- Miral S, Gencer O, Inal-Emiroglu FN, Baykara B, Baykara A, Dirik E. Risperidone versus haloperidol in children and adolescents with AD: a randomized, controlled, double-blind trial. European Child & Adolescent Psychiatry 2008;17(1):1-8. [DOI: 10.1007/s00787-007-0620-5] [PMID: ] [DOI] [PubMed] [Google Scholar]
Moazen‐Zadeh 2018 {published data only}
- IRCT201602041556N86. Simvastatin added to risperidone in the treatment of autism: a double blind and placebo controlled trial. https://www.irct.ir/trial/935 (first received February 2016).
- Moazen-Zadeh E, Shirzad F, Karkhaneh-Yousefi M-A, Khezri R, Mohammadi M-R, Akhondzadeh S. Simvastatin as an adjunctive therapy to risperidone in treatment of autism: a randomized, double-blind, placebo-controlled clinical trial. Journal of Child and Adolescent Psychopharmacology 2018;28(1):82-9. [DOI: 10.1089/cap.2017.0055] [PMID: ] [DOI] [PubMed] [Google Scholar]
Mohammadi 2013 {published data only}IRCT201106101556N25
- IRCT201106101556N25. Amantadine in the treatment of autism [A double - blind placebo controlled traial of amantadine added to risperidone in patint with autistic disorder]. www.irct.ir/trial/875 (first received 12 June 2011).
- Mohammadi M-R, Yadegari N, Hassanzadeh E, Farokh M, Yekehtaz H, Mirshafiee O, et al. Double-blind, placebo-controlled trial of risperidone plus amantadine in children with autism: a 10-week randomized study. Clinical Neuropharmacology 2013;36(6):179-84. [DOI: 10.1097/WNF.0b013e3182a9339d] [PMID: ] [DOI] [PubMed] [Google Scholar]
Montazmenesh 2020 {published data only}IRCT20090117001556N107
- IRCT20090117001556N107. Sulforaphane as adjunctive treatment of irritability in children with autism spectrum disorder [Sulforaphane treatment of autism spectrum disorder: a double blind controlled trial]. www.irct.ir/trial/30363 (first received 6 April 2018).
- Montazmenesh S, Amirimoghaddam-Yazdi Z, Moghaddam HS, Mohammadi MR, Akhondzadeh S. Sulforaphane as an adjunctive treatment for irritability in children with autism spectrum disorder: a randomized, double-blind, placebo-controlled clinical trial. Psychiatry and Clinical Neurosciences 2020;74(7):398-405. [DOI: 10.1111/pcn.13016] [PMID: ] [DOI] [PubMed] [Google Scholar]
Mouti 2014 {published and unpublished data}
- Mouti A, Reddihough D, Marraffa C, Hazell P, Wray J, Lee KL, et al. Fluoxetine for autistic behaviors (FAB trial): study protocol for a randomized controlled trial in children and adolescents with autism. Trials 2014;15:230. [DOI: 10.1186/1745-6215-15-230] [PMCID: PMC4067505] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddihough DS, Marraffa C, Mouti A, O'Sullivan M, Lee KJ, Orsini F, et al. Effect of fluoxetine on obsessive-compulsive behaviours in children and adolescents with autism spectrum disorders: a randomized clinical trial. JAMA 2019;322(16):1561-9. [DOI: 10.1001/jama.2019.14685] [PMCID: PMC6806436] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Munesue 2016 {published data only (unpublished sought but not used)}UMIN000007250
- Munesue T, Nakamura H, Kikuchi M, Miura Y, Takeuchi N, Anme T, et al. Oxytocin for male subjects with autism spectrum disorder and comorbid intellectual disabilities: a randomized pilot study. Frontiers in Psychiatry 2016;7:2. [DOI: 10.3389/fpsyt.2016.00002] [PMCID: PMC4720778] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- UMIN000007250. A randomized, double-blind, placebo-controlled, cross-over trial of oxytocin in patients with autism spectrum disorder. center6.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno=R000008548 (first received 9 February 2012).
NCT00183339 {published data only}
- NCT00183339. Early intervention with fluoxetine in autism [A randomized, placebo-controlled trial of fluoxetine in preschool children]. clinicaltrials.gov/ct2/show/NCT00183339 (first received 16 September 2005).
NCT00198107 {published data only}
- NCT00198107. Evaluating the effectiveness of aripiprazole and D-cycloserine to treat symptoms associated with autism [Novel pharmacological strategies in autism]. clinicaltrials.gov/ct2/show/NCT00198107 (first received 20 September 2005).
NCT00468130 {published data only}
- NCT00468130. Efficacy of aripiprazole versus placebo in the reduction of aggressive and aberrant behavior in autistic children (Abilify) [Efficacy of aripiprazole versus placebo in the reduction of aggressive and aberrant behavior in autistic children]. clinicaltrials.gov/ct2/show/NCT00468130 (first received 2 May 2007).
NCT00498173 {published data only}
- NCT00498173. Effectiveness of atomoxetine in treating ADHD symptoms in children and adolescents with autism [Targeted pharmacologic interventions for autism: a double-blind, placebo-controlled trial of atomoxetine in children and adolescents with autism]. clinicaltrials.gov/ct2/show/NCT00498173 (first received 9 July 2007).
NCT01337687 {published data only}
- NCT01337687. Intranasal oxytocin for the treatment of autism spectrum disorders (INOT) [Intranasal oxytocin for the treatment of autism spectrum disorders]. clinicaltrials.gov/ct2/show/NCT01337687 (first received 19 April 2011).
NCT01624675 {published data only}
- NCT01624675. A study to evaluate the efficacy and safety of risperidone (R064766) in children and adolescents with irritability associated with autistic disorder [A double-blind, placebo-controlled study, followed by an open-label extension study evaluating the efficacy and safety of risperidone (r064766) in children and adolescents with irritability associated with autistic disorder]. clinicaltrials.gov/ct2/show/NCT01624675 (first received 21 June 2012).
NCT01908205 {published data only}
- NCT01908205. Intranasal oxytocin for the treatment of children and adolescents with autism spectrum disorders (ASD) (OXY-R) [Intranasal oxytocin for the treatment of children and adolescents with autism]. clinicaltrials.gov/ct2/show/NCT01908205 (first received 25 July 2013).
NCT01972074 {published data only}
- NCT01972074. Behavioral and neural response to memantine in adolescents with autism spectrum disorder. clinicaltrials.gov/ct2/show/NCT01972074 (first received 30 October 2013).
NCT02940574 {published data only}
- NCT02940574. Neural and behavioral effects of oxytocin in autism spectrum disorders [Oxytocin-based pharmacotherapy for autism spectrum disorders: investigating the neural and behavioral effects of a promising intervention approach]. clinicaltrials.gov/ct2/show/NCT02940574 (first received 21 October 2016).
NCT03242772 {published data only}
- Impact of combined medication and behavioral treatment for ASD & ADHD. clinicaltrials.gov/ct2/NCT03242772?term=NCT03242772&draw=2&rank=1 (first received 14 December 2018).
Niederhofer 2002 {published data only}
- Niederhofer H, Staffen W, Mair A. Lofexidine In hyperactive and impulsive children with autistic disorder. Journal of the American Academy of Child & Adolescent Psychiatry 2002;41(12):1396-7. [DOI: 10.1097/00004583-200212000-00010] [PMID: ] [DOI] [PubMed] [Google Scholar]
Niederhofer 2003 {published data only}
- Niederhofer H, Staffen W, Mair A. Tianeptine: a novel strategy of psychopharmacological treatment of children with autistic disorder. Human Psychopharmacology 2003;18(5):389-93. [DOI: 10.1002/hup.491] [PMID: ] [DOI] [PubMed] [Google Scholar]
Nikoo 2015 {published data only}IRCT201110281556N29
- IRCT201110281556N29. N-acetylcysteine in the treatment of autism [N-acetyl cysteine added to risperidone in the treatment of autism: a double blind and placebo controlled trial]. en.irct.ir/trial/879 (first received 29 October 2011).
- Nikoo M, Radnia H, Farokhnia M, Mohammadi M-R, Akhondzadeh S. N-acetylcysteine as an adjunctive therapy to risperidone for treatment of irritability in autism: a randomized, double-blind, placebo-controlled clinical trial of efficacy and safety. Clinical Neuropharmacology 2015;38(1):11-7. [DOI: 10.1097/WNF.0000000000000063] [PMID: ] [DOI] [PubMed] [Google Scholar]
Nikvarz 2017 {published data only}IRCT201204037202N5
- IRCT201204037202N5. Comparing efficacy and side effects of memantine and risperidone in treating autistic patients. www.irct.ir/trial/7627 (first received 20 June 2012).
- Nikvarz N, Alaghband-Rad J, Tehrani-Doost M, Alimadadi A, Ghaeli P. Comparing efficacy and side effects of memantine vs risperidone in the treatment of autistic disorder. Pharmacopsychiatry 2017;50(1):19-25. [DOI: 10.1055/s-0042-108449] [PMID: ] [DOI] [PubMed] [Google Scholar]
Owen 2009 {published data only}EUCTR2016‐005111‐40
- EUCTR2016-005111-40. Study of aripiprazole in the treatment of serious behavioral problems in children and adolescents with autistic disorder (AD) [A multicenter, double-blind, randomized, placebo-controlled, flexible-dosed parallel-group study of aripiprazole flexibly dosed in thetreatment of children and adolescents with autistic disorder]. www.clinicaltrialsregister.eu/ctr-search/trial/2016-005111-40/results (first received 7 April 2017).
- Lewis D, Couch D, Marcus R, Manos G, Mankoski R, Carson W, et al. Efficacy and safety of flexibly-dosed aripiprazole for the treatment of irritability associated with autistic disorder in children and adolescents (6-17 years). Annals of Neurology 2009;66:S110-1. [DOI: 10.1002/ana.21853] [DOI] [Google Scholar]
- Lewis D, Owen R, Couch D. Efficacy and safety of aripiprazole for the treatment of irritability associated with autistic disorder in children and adolescents (6-17 years): results from two 8-week randomized, double-blind, placebo-controlled trials. Neurology 2009;72(11 (Supp 3)):A428. [ABSTRACT NO: S50.005] [Google Scholar]
- Mankoski R, Stockton G, Manos G, Marlor S, McQuade R, Forbes RA, et al. Aripiprazole treatment of irritability associated with autistic disorder and the relationship between prior antipsychotic exposure, adverse events, and weight change. Journal of Child and Adolescent Psychopharmacology 2013;23(8):572-6. [DOI: 10.1089/cap.2012.0075] [PMCID: PMC3804231] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT00365859. Study of aripiprazole in the treatment of serious behavioral problems in children and adolescents with autistic disorder (AD) [A 52-week, open-label, multicenter study of the safety and tolerability of aripiprazole flexibly dosed in the treatment of children and adolescents with autistic disorder]. clinicaltrials.gov/ct2/show/NCT00365859 (first received 18 August 2006).
- Owen R, Sikich L, Marcus RN, Corey-Lisle P, Manos G, McQuade RD, et al. Aripiprazole in the treatment of irritability in children and adolescent with autistic disorder. Pediatrics 2009;124(6):1533-40. [DOI: 10.1542/peds.2008-3782] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Robb AS, Andersson C, Bellocchio EE, Manos G, Rojas-Fernandez C, Mathew S, et al. Safety and tolerability of aripiprazole in the treatment of irritability associated with autistic disorder in pediatric subjects (6-17 years old): results from a pooled analysis of 2 studies. Primary Care Companion for CNS Disorders 2011;13(1):PCC.10m01008. [DOI: 10.4088/PCC.10m01008gry] [PMCID: PMC3121213] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varni JW, Handen BL, Corey-Lisle PK, Guo Z, Manos G, Ammerman DK, et al. The effect of aripiprazole 2 to 15mg/day on health-related quality of life in the treatment of irritability associated with autistic disorder in children: a post-hoc analysis of two controlled trials. Clinical Therapeutics 2012;34(4):980-92. [DOI: 10.1016/j.clinthera.2012.02.023] [PMID: ] [DOI] [PubMed] [Google Scholar]
Owley 2001 {published data only}
- Owley T, Macmahon W, Cook EH, Laulhere T, South M, Mays LZ, et al. Multisite, double-blind, placebo-controlled trial of porcine secretin in autism. Journal of the American Academy of Child and Adolescent Psychiatry 2001;40(11):1293-9. [DOI: 10.1097/00004583-200111000-00009] [PMID: ] [DOI] [PubMed] [Google Scholar]
Parker 2017 {published data only}
- NCT01624194. Intranasal oxytocin treatment for social deficits in children with autism [Double-blind, randomized, placebo controlled trial of intranasal oxytocin treatment for social deficits in children with autism]. clinicaltrials.gov/ct2/show/NCT01624194 (first received 20 June 2012).
- Parker KJ, Oztan O, Libove RA, Sumiyoshi RD, Jackson LP, Karhson DS, et al. Intranasal oxytocin treatment for social deficits and biomarkers of response in children with autism. Proceedings of the National Academy of Sciences of the United States of America 2017;114(30):8119‐24. [DOI: 10.1073/pnas.1705521114] [PMCID: PMC5544319] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Parker 2019 {published data only}
- NCT01962870. The role of vasopressin in the social deficits of autism [Randomized placebo-controlled trial of vasopressin treatment for social deficits in children with autism]. clinicaltrials.gov/ct2/show/NCT01962870 (first receceived 14 October 2013).
- Parker KJ, Oztan O, Libove RA, Mohsin N, Karhson DS, Sumiyoshi RD, et al. A randomized placebo-controlled pilot trial shows that intranasal vasopressin improves social deficits in children with autism. Science Translational Medicine 2019;11(491):eaau7356. [DOI: 10.1126/scitranslmed.aau7356] [PMCID: PMC6716148] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pearson 2013 {published data only}
- NCT00178503. Methylphenidate for attention deficit hyperactivity disorder and autism in children [ADHD symptoms in autism: cognition, behavior, treatment]. www.clinicaltrials.gov/ct2/show/NCT00178503 (first received 15 September 2005).
- Pearson DA, Santos CW, Aman MG, Arnold LE, Casat CD, Mansour R, et al. Effects of extended release methylphenidate treatment on ratings of attention-deficit/hyperactivity disorder (ADHD) and associated behavior in children with autism spectrum disorders and ADHD symptoms. Journal of Child and Adolescent Psychopharmacology 2013;23(5):337-51. [DOI: 10.1089/cap.2012.0096] [PMCID: PMC3689935] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Posey 2005 {published data only (unpublished sought but not used)}
- NCT00025779. Methylphenidate in children and adolescents with pervasive developmental disorders [Methylphenidate for hyperactivity and impulsiveness in children and adolescents with pervasive developmental disorders]. clinicaltrials.gov/ct2/show/NCT00025779 (first received 24 October 2001).
- Research Units on Pediatric Psychopharmacology (RUPP) Autism Network. Randomized, controlled, crossover trial of methylphenidate in pervasive developmental disorders with hyperactivity. Archives of General Psychiatry 2005;62(11):1266-74. [DOI: 10.1001/archpsyc.62.11.1266] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Scahill L, Bearss K, Sarhangian R, McDougle CJ, Arnold LE, Aman MG, et al. Using a patient-centered outcome measure to test methylphenidate versus placebo in children with autism spectrum disorder. Journal of Child and Adolescent Psychopharmacology 2017;27(2):125-31. [DOI: 10.1089/cap.2016.0107] [PMCID: PMC5367913] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Quintana 1995 {published data only}
- Quintana H, Birmaher B, Stedge D, Lennon S, Freed J, Bridge J, et al. Use of methylphenidate in the treatment of children with autistic disorder. Journal of Autism and Developmental Disorders 1995;25(3):283-94. [DOI: 10.1007/BF02179289] [PMID: ] [DOI] [PubMed] [Google Scholar]
Remington 2001 {published data only (unpublished sought but not used)}
- Remington G, Sloman L, Konstantareas M, Parker K, Gow R. Clomipramine versus haloperidol in the treatment of autistic disorder: a double-blind, placebo-controlled, crossover study. Journal of Clinical Psychopharmacology 2001;21(4):440-4. [DOI: 10.1097/00004714-200108000-00012] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Sloman L, Remington G, Konstantareas M, Parker K. Haloperidol versus clomipramine in autistic disorder. In: 151st Annual Meeting of the American Psychiatric Association; 1998 May 30 to June 4; Toronto (ON), Canada. Vol. 17. 1998. [PRESENTATION NO: 17]
Research Units 2005 {published data only}
- Research Units on Pediatric Psychopharmacology Autism Network. Risperidone treatment for autistic disorder: longer-term benefits and blinded discontinuation after 6 months. American Journal of Psychiatry 2005;162(7):1361-9. [DOI: 10.1176/appi.ajp.162.7.1361] [PMID: ] [DOI] [PubMed] [Google Scholar]
Rezaei 2010 {published data only}IRCT138901141556N9
- IRCT138901141556N9. Topiramate in the treatment of autism [Tpoiramate added to risperidone in patint with autistic disorder: a double-blind placebo controlled trial]. www.irct.ir/trial/859 (first received 29 April 2010).
- Rezaei V, Mohammadi M-R, Ghanizadeh A, Sahraian A, Tabrizi M, Rezazadeh S-A, et al. Double-blind, placebo-controlled trial of risperidone plus topiramate in children with autistic disorder. Progress in Neuro-Psychopharmacology and Biological Psychiatry 2010;34(7):1269-72. [DOI: 10.1016/j.pnpbp.2010.07.005] [PMID: ] [DOI] [PubMed] [Google Scholar]
Scahill 2015 {published data only}
- Munoz Martinez V, Nuevo Fernandez L, Mella Dominguez L, Mata Saenz B, Asensio Aguerri L. Guanfacine as an alternative for autism spectrum disorder with hyperactivity symptoms. European Neuropsychopharmacology 2017;27(4):S607. [DOI: 10.1016/S0924-977X(17)31154-9] [POSTER NO: P.1.c.006] [DOI] [Google Scholar]
- NCT01238575. Guanfacine for the treatment of hyperactivity in pervasive developmental disorder. clinicaltrials.gov/ct2/show/NCT01238575 (first received 10 November 2010).
- Politte LC, Scahill L, Figueroa J, McCracken JT, King B, McDougle CJ. A randomized, placebo-controlled trial of extended-release guanfacine in children with autism spectrum disorder and ADHD symptoms: an analysis of secondary outcome measures. Neuropsychopharmacology 2018;43(8):1772-8. [DOI: 10.1038/s41386-018-0039-3] [PMCID: PMC6006142] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scahill L, McCracken JT, King BH, Rockhill C, Shah B, Politte L, et al. Extended-release guanfacine for hyperactivity in children with autism spectrum disorder. American Journal of Psychiatry 2015;172(12):1197-206. [DOI: 10.1176/appi.ajp.2015.15010055] [PMID: ] [DOI] [PubMed] [Google Scholar]
Shea 2004 {published data only}
- Light M, Dunbar E, Shea S. P2.104 Efficacy and safety of risperidone in the treatment of children with autistic and other pervasive developmental disorders (PDD): a randomized, double-blind, placebo controlled trial. European Neuropsychopharmacology 2004;14(Suppl 3):S278. [DOI: 10.1016/S0924-977X(04)80324-9] [DOI] [Google Scholar]
- Light M, Dunbar F, Shea M. Efficacy and safety of risperidone in the treatment of children with autistic and other pervasive developmental disorders (PDD): a randomized, double-blind, placebo controlled trial. International Journal of Neuropsychopharmacology 2004;7:S275. [DOI: 10.1016/S0924-977X(04)80324-9] [DOI] [Google Scholar]
- Pandina GJ, Bossie CA, Youssef E, Zhu Y, Dunbar F. Risperidone improves behavioural symptoms in children with autism in a randomized, double-blind, placebo-controlled trial. Journal of Autism and Developmental Disorders 2007;37(2):367-73. [DOI: 10.1007/s10803-006-0234-7] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Shea S, Turgay A, Carroll A, Schulz M, Orlik H, Smith I, et al. Risperidone in the treatment of disruptive behavioral symptoms in children with autistic and other pervasive developmental disorders. Pediatrics 2004;114(5):e634-41. [DOI: 10.1542/peds.2003-0264-F] [PMID: ] [DOI] [PubMed] [Google Scholar]
Sikich 2013 {published data only}
- NCT01944046. Study of oxytocin in autism to improve reciprocal social behaviours (SOARS-B) [Phase II study of oxytocin in autism to improve reciprocal social behaviors]. clinicaltrials.gov/ct2/show/NCT01944046 (first received 17 September 2013).
- Sikich L, Alderman C, Hazzard L, Bethea T, Gregory S, Johnson J. Pilot study of sustained oxytocin treatment in children and adolescents with autistic disorder. Biological Psychiatry 2013;73(9):145S. [Google Scholar]
Sikich 2021 {published data only}
- NCT01944046. Study of Oxytocin in Autism to Improve Reciprocal Social Behaviors (SOARS-B). clinicaltrails.gov/ct2/show/study/NCT01944046?term=NCT01944046&draw=2&rank=1 (first received 1 August 2014).
- Sikich L, Kolevzon A, King B, McDougle C, Sanders K, Kim S-J, et al. Intranasal oxytocin in children and adolescents with autism spectrum disorder. New England Journal of Medicine 2021;385(16):1462-73. [DOI: 10.1056/NEJMoa2103583] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spanos M, Bethea T, Alderman C, Johnson J, Chandrasekhar T, Sikich L. Randomized, placebo-controlled trial with open-label extension of intranasal oxytocin for autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry 2021;60(10):S162. [DOI: 10.1016/j.jaac.2021.09.087] [DOI] [Google Scholar]
Soorya 2021 {published data only}
- NCT01372449. A multi-site double-blind placebo-controlled trial of memantine versus placebo in children with autism (MEM). clinicaltrials.gov/ct2/show/NCT01372449?term=NCT01372449&draw=1&rank=1 (first received December 2011).
- Soorya L, Fogg L, Ocampo E, Printen M, Youngkin S, Halpern D, et al. Neurocognitive outcomes from memantine: a pilot, double-blind, placebo-controlled trial in children with autism spectrum disorder. Journal of Child and Adolescent Psychopharmacology 2021;31(7):475-84. [DOI: 10.1089/cap.2021.0010] [PMID: ] [DOI] [PubMed] [Google Scholar]
Sprengers 2021 {published data only}
- Sprengers J, Van Andel D, Zuithoff N, Keijzer-Veen M, Scheepers F, Lilien M, et al. Bumetanide versus placebo for core symptoms of autism spectrum disorder at 91 days (BAMBI): a single-centre, double-blinded, patient-randomized, placebo-controlled, phase-2-trial. European Neuropsychopharmacology 2020;40:S80-S81. [DOI: 10.1016/j.euroneuro.2020.09.108] [DOI] [PubMed] [Google Scholar]
- Sprengers JJ, Van Andel DM, Zuithoff NP, Keijzer-Veen MG, Schulp AJ, Scheepers FE, et al. Bumetanide for core symptoms of autism spectrum disorder (BAMBI): a single center, double-blinded, participant-randomized, placebo-controlled, phase-2 superiority trial. Journal of the American Academy of Child and Adolescent Psychiatry 2021;60(7):865-76. [DOI: 10.1016/j.jaac.2020.07.888] [PMID: ] [DOI] [PubMed] [Google Scholar]
Squassante 2018 {published data only}
- NCT01793441. A study of RG7314 to investigate efficacy and safety in individuals with autism spectrum disorders (ASD) [A multi-center, randomized, double-blind, 12-week, parallel group, placebo-controlled proof of concept study to investigate the efficacy and safety of rg7314 in individuals with autism spectrum disorders (ASD)]. clinicaltrials.gov/ct2/show/NCT01793441 (first received 15 February 2013).
- Squassante L, Bolognani F, Smith J, Murtagh L, Fontoura P, Khwaja O, et al. Effects of balovaptan on health-related quality of life of adult men with ASD: results from a phase 2 randomized double-blind placebo controlled study (Vanilla). Journal of the American Academy of Child and Adolescent Psychiatry 2018;57(10):S231. [DOI: 10.1016/j.jaac.2018.09.308] [PRESENTATION NO: 5.13] [DOI] [Google Scholar]
Takamitsu 2015a {published data only}UMIN000007122
- UMIN000007122. A randomized, double-blind and cross-over trial to examine effects of continuous administration of intranasal oxytocin on social dysfunction in subjects with autism spectrum disorders. center6.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno=R000008388 (first received 1 February 2012).
- Watanabe T, Kuroda M, Kuwabara H, Aoki Y, Iwashiro N, Tatsunobu N, et al. Clinical and neural effects of six-week administration of oxytocin on core symptoms of autism. Brain 2015;138(11):3400-12. [DOI: 10.1093/brain/awv249] [PMID: ] [DOI] [PubMed] [Google Scholar]
Troost 2005 {published data only}
- Malone RP. Discontinuing risperidone results in relapse in children with autism spectrum disorders. Evidence-Based Mental Health 2006;9(2):56. [DOI: 10.1136/ebmh.9.2.56] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Troost PW, Althaus M, Lahuis BE, Buitelaar JK, Minderaa RB, Hoekstra PJ. Neuropsychological effect of risperidone in children with pervasive developmental disorders: a blinded discontinuation study. Journal of Child and Adolescent Psychopharmacology 2006;16(5):561-73. [DOI: 10.1089/cap.2006.16.561] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Troost PW, Lahuis BE, Steenhuis M-P, Ketelaars CE, Buitelaar JK, Van Engeland H, et al. Long-term effects of risperidone in children with autism spectrum disorders: a placebo discontinuation study. Journal of the American Academy of Child and Adolescent Psychiatry 2005;44(11):1137-44. [DOI: 10.1097/01.chi.0000177055.11229.76] [PMID: ] [DOI] [PubMed] [Google Scholar]
Umbricht 2017 {published data only}
- NCT01474278. A study of RO5028442 in adult male high-functioning autistic patients. https://clinicaltrials.gov/ct2/show/NCT01474278?term=NCT01474278&draw=2&rank=1 (first registered December 2011).
- Umbricht D, Del Valle Rubido M, Hollander E, McCracken JT, Shic F, Scahill L, et al. A single dose, randomized, controlled proof-of-mechanism study of a novel vasopressin 1a receptor antagonist (RG7713) in high-functioning adults with autism spectrum disorder. Neuropsychopharmacology 2017;42(9):1914-23. [DOI: 10.1038/npp.2016.232] [PMCID: PMC5520775] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Unis 2002 {published data only}
- NCT00065962. Secretin for the treatment of autism [Multisite controlled secretin trial in autism]. clinicaltrials.gov/ct2/show/NCT00065962 (first received 5 August 2003).
- Unis AS, Munson JA, Rogers SJ, Goldson E, Osterling J, Gabriels R, et al. A randomized, double-blind, placebo-controlled trial of porcine versus synthetic secretin for reducing symptoms of autism. Journal of the American Academy of Child and Adolescent Psychiatry 2002;41(11):1315-21. [DOI: 10.1097/00004583-200211000-00012] [PMID: ] [DOI] [PubMed] [Google Scholar]
VanAndel 2022 {published data only}
- VanAndel D, Sprengers J, Keijzer-Veen M, Schulp A, Lillien M, Scheepers F, et al. Bumetanide for irritability in children with sensory processing problems across neurodevelopmental disorders: a pilot randomized controlled trial. Frontiers in Psychiatry 2022;13:780281. [DOI: 10.3389/fpsyt.2022.780281] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Veenstra‐VanderWeele 2017 {published data only}
- NCT01288716. Study of arbaclofen for the treatment of social withdrawal in subjects with autism spectrum disorders. https://clinicaltrials.gov/ct2/show/NCT01288716?term=NCT01288716&draw=2&rank=1 (first received February 2011).
- Veenstra-VanderWeele J, Cook EH, King BH, Zarevics P, Cherubini M, Walton-Bowen K, et al. Arbaclofen in children and adolescents with autism spectrum disorder: a randomized, controlled, phase 2 trial. Neuropsychopharmacology 2017;42(7):1390-8. [DOI: 10.1038/npp.2016.237] [PMCID: PMC5436109] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wasserman 2006 {published data only (unpublished sought but not used)}
- Wasserman S, Iyengar R, Chaplin WF, Watner D, Waldoks SE, Anagnostou E, et al. Levetiracetam versus placebo in childhood and adolescent autism: a double-blind placebo-controlled study. International Clinical Psychopharmacology 2006;21(6):363-7. [DOI: 10.1097/01.yic.0000224787.13782.0f] [PMID: ] [DOI] [PubMed] [Google Scholar]
Willemsen‐Swinkels 1995 {published data only}
- Willemsen-Swinkels SH, Buitelaar JK, Nijhof GJ, Van Engeland H. Failure of naltrexone hydrochloride to reduce self-injurious and autistic behaviour in mentally retarded adults. Double-blind placebo-controlled studies. Archives of General Psychiatry 1995;52(9):766-73. [DOI: 10.1001/archpsyc.1995.03950210060011] [PMID: ] [DOI] [PubMed] [Google Scholar]
Willemsen‐Swinkels 1996 {published data only}
- Willemsen-Swinkels SH, Buitelaar JK, Van Engeland H. The effects of chronic naltrexone treatment in young autistic children: a double-blind placebo-controlled crossover study. Biological Psychiatry 1996;39(12):1023-31. [DOI: 10.1016/0006-3223(95)00297-9] [PMID: ] [DOI] [PubMed] [Google Scholar]
Wink 2016 {published data only}
- NCT00453180. A study of oral N-acetylcysteine in children with autism spectrum disorders. https://clinicaltrials.gov/ct2/show/NCT00453180?term=NCT00453180&draw=2&rank=1 (first received March 2007).
- Wink LK, Adams R, Wang Z, Klaunig JE, Plawecki MH, Posey DJ, et al. A randomized placebo-controlled pilot study of N-acetylcysteine in youth with autism spectrum disorder. Molecular Autism 2016;7:26. [DOI: 10.1186/s13229-016-0088-6] [PMCID: PMC4839099] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wink 2018 {published data only}
- NCT02081027. Pilot study of riluzole for drug-refractory irritability in autism spectrum disorders. https://clinicaltrials.gov/ct2/show/NCT02081027?term=NCT02081027&draw=2&rank=1 (first received March 2014). [DOI] [PubMed]
- Wink LK, Adams R, Horn PS, Tessier CR, Bantel AP, Hong M, et al. A randomized placebo-controlled cross-over pilot study of riluzole for drug-refractory irritability in autism spectrum disorder. Journal of Autism and Developmental Disorders 2018;48(9):3051-60. [DOI: 10.1007/s10803-018-3562-5] [PMID: ] [DOI] [PubMed] [Google Scholar]
Woodard 2007 {published data only}
- Woodard C, Groden J, Goodwin M, Bodfish J. A placebo double-blind pilot study of dextromethorphan for problematic behaviors in children with autism. Autism 2007;11(1):29-41. [DOI: 10.1177/1362361307070989] [PMID: ] [DOI] [PubMed] [Google Scholar]
Yamasue 2020 {published data only}
- JPRN‐UMIN000015264. A multicenter, parallel group, placebo-controlled, double blind, confirmatory trial of intranasal oxytocin in participants with autism spectrum disorders. https://trialsearch.who.int/Trial2.aspx?TrialID=JPRN-UMIN000015264 (first received March 2019).
- Yamasue H, Okada T, Munesue T, Kuroda M, Fujioka T, Uno Y, et al. Effect of intranasal oxytocin on the core social symptoms of autism spectrum disorder: a randomized clinical trial. Molecular Psychiatry 2020;25(8):1849-58. [DOI: 10.1038/s41380-018-0097-2] [PMID: ] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Althaus 2015 {published data only}
- Althaus M, Groen Y, Wijers A, Noltes H, Tucha O, Hoekstra P. Oxytocin enhances orienting to social information in a selective group of high-functioning male adults with autism spectrum disorder. Neuropsychologia 2015;79:53-69. [DOI: 10.1016/j.neuropsychologia.2015.10.025] [DOI] [PubMed] [Google Scholar]
Aman 1997 {published data only}
- Aman M, Van Bourgondien M, Osborne P, Sarphare G. Side effects associated with psychoactive medication in individuals with autism. Journal of Autism & Developmental Disorders 1997;27(3):342-4. [PubMed] [Google Scholar]
Aman 2009 {published data only}
- Aman M, McDougle C, Scahill L, Handen B, Arnold L, Johnson C. Medication and parent training in children with pervasive developmental disorders and serious behavior problems: results from a randomized clinical trial. Journal of the American Academy of Child and Adolescent Psychiatry 2009;48(12):1143-54. [ISSN: 0890-8567] [DOI] [PMC free article] [PubMed] [Google Scholar]
Anderson 1984 {published data only}
- Anderson L, Campbell M, Grega D. Haloperidol in the treatment of infantile autism: Effects on learning and behavioral symptoms. American Journal of Psychiatry 1984;141(10):1195-202. [DOI] [PubMed] [Google Scholar]
Anderson 1989 {published data only}
- Anderson L, Campbell M, Adams P, Small A, Perry R, Shell J. The effects of haloperidol on discrimination learning and behavioral symptoms in autistic children. Journal of Autism and Developmental Disorders 1989;19(2):227-39. [DOI] [PubMed] [Google Scholar]
Anderson 1997 {published data only}
- Anderson S, Hanson R, Malecha M, Oftelie A, Erickson C, Clark J. The effectiveness of naltrexone in treating task attending, aggression, self-injury and stereotypic mannerisms of six young males with autism or pervasive developmental disorders. Journal of Developmental and Physical Disabilities 1997;9(3):211-42. [Google Scholar]
Anderson 2007 {published data only}
- Anderson G, Scahill L, McCracken J, Aman M, Tierney E, Arnold L. Effects of short- and long-term risperidone treatment on prolactin levels in children with autism. Biological Psychiatry 2007;61(4):515-50. [DOI: ] [DOI] [PubMed] [Google Scholar]
Arman 2003 {published data only}
- Arman A, Yazgan Y, Berkem M, Campbell M. The effects of risperidone on behaviors seen in children with pervasive developmental disorder and mental retardation in an educational setting. Bulletin of Clinical Psychopharmacology 2003;13(4):174-8. [Google Scholar]
Arnold 2012b {published data only}
- Arnold L, Aman M, Li X, Butter E, Humphries K, Scahill L. Research Units of Pediatric Psychopharmacology (RUPP) autism network randomized clinical trial of parent training and medication: one-year follow-up. Journal of the American Academy of Child and Adolescent Psychiatry 2012;51(11):1173-84. [DOI: 10.1016/j.jaac.2012.08.028] [DOI] [PMC free article] [PubMed] [Google Scholar]
August 1987 {published data only}
- August G, Raz N, Baird T. Fenfluramine response in high and low functioning autistic children. Journal of the American Academy of Child & Adolescent Psychiatry 1985;26(3):342-6. [DOI: 10.1097/00004583-198705000-00011] [DOI] [PubMed] [Google Scholar]
Bachmann 2013 {published data only}
- Bachmann C, Manthey T, Kamp-Becker I, Glaeske G, Hoffmann F. Psychopharmacological treatment in children and adolescents with autism spectrum disorders in Germany. Research in Developmental Disabilities 2013;34(9):2551-63. [DOI: 10.1016/j.ridd.2013.05.028] [DOI] [PubMed] [Google Scholar]
Barnard‐Brak 2016 {published data only}
- Barnard-Brak L, Davis T, Schmidt M, Richman D. Effects associated with on- and off-label stimulant treatment of core autism and ADHD symptoms exhibited by children with autism spectrum disorder. Developmental neurorehabilitation 2016;19(1):46-53. [DOI: ] [PMID: ] [DOI] [PubMed] [Google Scholar]
Beeghly 1987 {published data only}
- Beeghly J, Kuperma S, Perry P, Wright G, Tsai L. Fenfluramine treatment of autism: relationship of treatment response to blood levels of fenfluramine and norfenfluramine. Journal of Autism and Developmental Disorders 1987;17(4):541-8. [DOI: 10.1007/BF01486969] [DOI] [PubMed] [Google Scholar]
Castellanos 2019 {published data only}
- Castellanos F. A placebo-controlled double-blind trial of cannabinoids in children and adolescents with autism spectrum disorder. Neuropsychopharmacology 2019;44(1):61-2. [DOI: 10.1038/s41386-019-0544-z] [DOI] [Google Scholar]
Chez 2002 {published data only}
- Chez M, Buchanan C, Aimonovitch M, Becker M, Schaefer K, Black C. Double-blind, placebo-controlled study of L-carnosine supplementation in children with autistic spectrum disorders. Journal of Child Neurology 2002;17(11):833-7. [DOI: 10.1177/08830738020170111501] [DOI] [PubMed] [Google Scholar]
Chez 2003 {published data only}
- Chez M, Buchanan T, Becker M, Jessler J, Aimonovitch M, Mrazek S. Donepezil hydrochloride: a double-blind study in autistic children. Journal of Pediatric Neurology 2003;1(2):83-8. [DOI: 10.1055/s-0035-1557175] [DOI] [Google Scholar]
Du 2015 {published data only}
- Du L, Shan L, Wang B, Li H, Xu Z, Staal W. A pilot study on the combination of applied behavior analysis and bumetanide treatment for children with autism. Journal of Child and Adolescent Psychopharmacology 2015;25(7):585-8. [DOI: 10.1089/cap.2015.0045] [DOI] [PubMed] [Google Scholar]
Duker 1991 {published data only}
- Duker P, Welles K, Seys D, Rensen H, Vis A, Berg G. Brief report: effects of fenfluramine on communicative, stereotypic, and inappropriate behaviors of autistic-type mentally handicapped individuals. Journal of Autism and Developmental Disorders 1991;21(3):355-63. [DOI: 10.1007/BF02207332] [DOI] [PubMed] [Google Scholar]
Dunn‐Geier 2000 {published data only}
- Dunn-Geier J, Ho H, Auersperg E, Doyle D, Eaves L, Matsuba C. Effect of secretin on children with autism: a randomized controlled trial. Developmental Medicine and Child Neurology 2000;42(12):796-802. [DOI: 10.1017/S0012162200001481] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ekman 1989 {published data only}
- Ekman G, Miranda-Linne F, Gillberg C, Garle M, Wetterberg L. Fenfluramine treatment of twenty children with autism. Journal of Autism & Developmental Disorders 1989;19(4):511-32. [DOI: 10.1007/BF02212855] [PMID: ] [DOI] [PubMed] [Google Scholar]
Fahmy 2013 {published data only}
- Fahmy S, El-Hamamsy M, Zaki O, Badary O. L-carnitine supplementation improves the behavioral symptoms in autistic children. Research in Autism Spectrum Disorders 2013;7(1):159-66. [DOI: 10.1016/j.rasd.2012.07.006] [DOI] [Google Scholar]
Fang 2018 {published data only}
- Fang L, Jiang X, Huang Y, Sun Y, Xie Y, Wang L. Efficacy of vitamin D combined with ω-3 fatty acid in treatment of children with autism spectrum disorder. Pharmaceutical Care and Research 2018;18(5):347-50. [DOI: 10.5428/pcar20180508] [DOI] [Google Scholar]
Findling 1997a {published data only}
- Findling R, Maxwell K, Scotese-Wojtila L, Huang J, Yamashita T, Wiznitzer M. High-dose pyridoxine and magnesium administration in children with autistic disorder: an absence of salutary effects in a double-blind, placebo-controlled study. Journal of Autism and Developmental Disorders 1997;27(4):467-78. [DOI: 10.1023/A:1025861522935] [DOI] [PubMed] [Google Scholar]
Groden 1987 {published data only}
- Groden G, Groden J, Dondey, M, Zane T, Pueschel S. Effects of fenfluramine on the behavior of autistic individuals. Research in Developmental Disabilities 1987;8(2):203-11. [DOI] [PubMed] [Google Scholar]
Guglielmo 2013 {published data only}
- Guglielmo R, Ioime L, Grandinetti P, Janiri L. Managing disruptive and compulsive behaviors in adult with autistic disorder with gabapentin. Journal of Clinical Psychopharmacology 2013;33(2):273-4. [DOI: 10.1097/JCP.0b013e318285680c] [DOI] [PubMed] [Google Scholar]
Handen 2013 {published data only}
- Handen B, Johnson C, Butter E, Lecavalier L, Scahill L, Aman M. Use of a direct observational measure in a trial of risperidone and parent training in children with pervasive developmental disorders. Journal of Developmental & Physical Disabilities 2013;25(3):355-71. [DOI: 10.1007/s10882-012-9316-y] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hellings 2006a {published data only}
- Hellings JA, Zarcone JR, Crandall K, Wallace D, Schroeder SR. Weight gain in a controlled study of risperidone in children, adolescents and adults with mental retardation and autism. Journal of Child and Adolescent Psychopharmacology 2001;11(3):228-38. [DOI: 10.1089/10445460152595559] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Hellings JA, Zarcone JR, Reese RM, Valdovinos MG, Marquis JG, Fleming KK, et al. A crossover study of risperidone in children, adolescents and adults with mental retardation. Journal of Autism and Developmental Disorders 2006;36(3):401-11. [DOI: 10.1007/s10803-006-0078-1] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Napolitano D. The effects of risperidone on the self-injury, aggression, and stereotypy of persons with developmental disabilities: observer agreement using direct observations and the aberrant behavior checklis during a double-blind placebo-controlled clinical. Dissertation Abstracts International: Section B: The Sciences and Engineering 2001;61(8-B):4384. [ISBN: 978-0-599-91735-4]
- Zarcone JR, Hellings JA, Crandell K, Reese RM, Marquis J, Fleming K, et al. Effects of risperidone on aberrant behavior of persons with developmental disabilities: I. A double blind crossover study using multiple measures. American Journal of Mental Retardation 2001;106(6):525-38. [DOI: ] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hellings 2010 {published data only}
- Hellings J, Cardona A, Schroeder S, Aman M, Buitelaar J, Findling R. Long-term safety and adverse events of risperidone in children, adolescents, and adults with pervasive developmental disorders. Journal of Mental Health Research in Intellectual Disabilities 2010;3(3):132-44. [Google Scholar]
Hellings 2015 {published data only}
- Hellings J, Reid G, Cain S, Zhou X, Barth F, Aman M. Loxapine add-on for adolescents and adults with autism spectrum disorders and irritability. Journal of Child & Adolescent Psychopharmacology 2015;25(2):150-9. [DOI: 10.1089/cap.2014.0003] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hess 2010 {published data only}
- Hess J, Matson J, Neal D, Mahan S, Fodstad J, Bamburg J. A comparison of psychotropic drug side effect profiles in adults diagnosed with intellectual disabilities and autism spectrum disorders. Journal of Mental Health Research in Intellectual Disabilities 2010;3(2):85-96. [DOI: 10.1080/19315861003690588] [DOI] [Google Scholar]
Hollander 2003 {published data only}
- Hollander E, Novotny S, Hanratty M, Yaffe R, DeCaria C, Aronowitz B. Oxytocin infusion reduces repetitive behaviors in adults with autistic and Asperger's disorders. Neuropsychopharmacology 2003;28(1):193-8. [DOI: 10.1038/sj.npp.1300021] [DOI] [PubMed] [Google Scholar]
Hollander 2006c {published data only}
- Hollander E, Wasserman S, Swanson E, Chaplin W, Schapiro M, Zagursky K. A double-blind placebo-controlled pilot study of olanzapine in childhood/adolescent pervasive developmental disorder. Journal of Child and Adolescent Psychopharmacology October 2006;16(5):541-8. [DOI: 10.1089/cap.2006.16.541] [DOI] [PubMed] [Google Scholar]
Hollander 2020c {published data only}
- Hollander E, Jacob S, Jou R, McNamara N, Sikich L, Tobe R. A phase 2 randomized controlled trial of balovaptan in pediatric participants with autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry 2020;59(10):S262-S263. [DOI: 10.1016/j.jaac.2020.08.458] [DOI] [Google Scholar]
Horovitz 2012 {published data only}
- Horovitz M, Matson J, Barker A. The relationship between symptoms of autism spectrum disorders and psychotropic medication use in infants and toddlers. Research in Autism Spectrum Disorders 2013;6(4):1406-11. [DOI: 10.1016/j.rasd.2011.05.013] [DOI] [Google Scholar]
Horrigan 1997 {published data only}
- Horrigan J, Barnhill L. Risperidone and explosive aggressive autism. Journal of Autism & Developmental Disorders 1997;27(3):313-23. [DOI: 10.1023/A:1025854532079] [DOI] [PubMed] [Google Scholar]
Hughes 2002 {published data only}
- Hughes D, Cunningham M, Libretto S. Risperidone in children and adolescents with autistic disorder and aggressive behaviour. British Journal of Developmental Disabilities 2002;48(95):113-22. [DOI: 10.1179/096979502799104229] [DOI] [Google Scholar]
Jacob 2020 {published data only}
- Jacob S, Veenstra-VanderWeele J, Murphy D, McCracken J, Smith J. Phase 3 randomized controlled trial of balovaptan in adults with autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry 2020;59(10):S163-S164. [DOI: 10.1016/j.jaac.2020.08.108] [DOI] [Google Scholar]
Jordan 2012 {published data only}
- Jordan I, Robertson D, Catani M, Craig M, Murphy D. Aripiprazole in the treatment of challenging behaviour in adults with autism spectrum disorder. Psychopharmacology 2012;223(3):357-60. [DOI: 10.1007/s00213-012-2723-z] [DOI] [PubMed] [Google Scholar]
JPRN‐UMIN000007250 2012 {published data only}
- JPRN-UMIN000007250. A randomized, double-blind, placebo-controlled, cross-over trial of oxytocin in patients with autism spectrum disorder. http://www.who.int/trialsearch/Trial2.aspx?TrialID=JPRN-UMIN000007250 2012. [http://www.who.int/trialsearch/Trial2.aspx?TrialID=JPRN-UMIN000007250]
Jun 2000 {published data only}
- Jun S-S, Kao C-H, Lee Y-C. Double blind crossover study of secretin/secrepan treatment for children with autistic symptoms. Tzu Chi Medical Journal 2000;12(3):173-81. [Google Scholar]
Kolmen 1995 {published data only}
- Kolmen B, Feldman H, Handen B, Janosky J. Naltrexone in young autistic children: a double-blind, placebo-controlled crossover study. Journal of the American Academy of Child and Adolescent Psychiatry 1995;34(2):223-31. [DOI: 10.1097/00004583-199502000-00018] [DOI] [PubMed] [Google Scholar]
Kolmen 1997 {published data only}
- Kolmen B, Feldman H, Handen B, Janosky J. Naltrexone in young autistic children: replication study and learning measures. Journal of the American Academy of Child and Adolescent Psychiatry 1997;36(11):1570-8. [DOI: 10.1016/S0890-8567(09)66567-9] [DOI] [PubMed] [Google Scholar]
Krusch 2004 {published data only}
- Krusch D. Effects of repeated secretin administration on a subset of children with pervasive developmental disorder. Dissertation Abstracts International: Section B: The Sciences and Engineering 2004;65(2-B):1032. [ISBN: 9780496695942] [Google Scholar]
Leboyer 1993 {published data only}
- Leboyer M, Bouvard M, Recasens J, Plumet M, Waller P, Tabuteau F. Opioid hypothesis in infantile autism? Therapeutic trials with naltrexone [Une hypothese opiacee dans l'autisme infantile? Essais therapeutiques avec la naltrexone]. Encephale 1993;19:95-102. [PubMed] [Google Scholar]
Lemonnier 2012 {published data only}
- Lemonnier E, Degrez C, Phelep M, Tyzio R, Josse R, Grandgeorge M. A randomised controlled trial of bumetanide in the treatment of autism in children. Translational Psychiatry 2012;2:e202. [DOI: 10.1038/tp.2012.124] [DOI] [PMC free article] [PubMed] [Google Scholar]
Leventhal 1993 {published data only}
- Leventhal B, Cook E, Morford M, Ravitz A, Heller W, Freedman D. Clinical and neurochemical effects of fenfluramine in children with autism. Journal of Neuropsychiatry and Clinical Neurosciences 1993;5(3):307-15. [DOI: 10.1176/jnp.5.3.307] [DOI] [PubMed] [Google Scholar]
Levine 1997 {published data only}
- Levine J, Aviram A, Holan A, Ring A, Barak A, Belmaker R. Inositol treatment of autism. Journal of Neural Transmission 1997;104(2-3):307-10. [DOI] [PubMed] [Google Scholar]
Malone 2002 {published data only}
- Malone R, Maislin G, Choudhrey M, Gifford. Risperidone treatment in children and adolescents with autism: short- and long-term safety and effectiveness. Journal of the American Academy of Child & Adolescent Psychiatry 2002;41(2):140-7. [DOI] [PubMed] [Google Scholar]
Moharreri 2017 {published data only}
- IRCT201108155280N5. A comparative study on the effectiveness of risperidone versus risperidone plus naltrexone in treatment of autistic spectrum disorder in children with 6-12 years old. www.irct.ir/trial/5631 (first received 10 February 2013).
- Moharreri F, Abdollahian E, Hosseini SA, Mirzadeh M. Comparative study on the effect of risperidone and its combination with naltrexone in pediatric patients with autistic spectrum disorders: a clinical trial study. International Journal of Pediatrics 2017;5(12):6375-82. [DOI: 10.22038/ijp.2017.18557.1516] [DOI] [Google Scholar]
Nagaraj 2006 {published data only (unpublished sought but not used)}
- Nagaraj R, Singhi P, Malhi P. Risperidone in children with autism: randomized, placebo-controlled, double-blind study. Journal of Child Neurology 2006;21(6):450-5. [DOI] [PubMed] [Google Scholar]
NCT00198120 2005 {published data only}
- NCT00198120. Safety and effectiveness of D-Cycloserine in children with autism. https://clinicaltrials.gov/ct2/show/NCT00198120?term=NCT00198120&draw=2&rank=1 (first received February 2004).
NCT01078844 {published data only}
- NCT01078844. Memantine in adult autism spectrum disorder. https://clinicaltrials.gov/study/NCT01078844 (not published - terminated) (first received 1 March 2010).
Nickels 2008 {published data only}
- Nickels K, Katusic S, Colligan R, Weaver A, Voigt R, Barbaresi W. Stimulant medication treatment of target behaviors in children with autism: a population-based study. Journal of Developmental & Behavioral Pediatrics 2008;29(2):75-81. [DOI: 10.1097/DBP.0b013e31815f24f7] [DOI] [PMC free article] [PubMed] [Google Scholar]
Niederhofer 2007 {published data only}
- Niederhofer H. Glutamate antagonists seem to be slightly effective in psychopharmacologic treatment of autism. Journal of Clinical Psychopharmacology 2007;27(3):317-8. [DOI: 10.1097/01.jcp.0000270082.30500.69] [DOI] [PubMed] [Google Scholar]
Posey 2004 {published data only}
- Posey D, Kem D, Swiezy N, Sweeten T, Wiegand R, McDougle C. A pilot study of D-cycloserine in subjects with autistic disorder. The American journal of psychiatry 2004;161(11):2115-7. [DOI: 10.1176/appi.ajp.161.11.2115] [DOI] [PubMed] [Google Scholar]
Preckel 2016 {published data only}
- DRKS00008952. Oxytocin-induced enhancement of Social Skills Training in Adolescents with ASD. http://www.who.int/trialsearch/Trial2.aspx?TrialID=DRKS00008952 2015 2015.
- Mayer A, Preckel K, Ihle K, Piecha F, Junghanns K, Reiche S. No support for oxytocin modulation of reward-related brain function in autism: evidence from a randomized controlled trial. https://www.medrxiv.org/content/10.1101/2021.03.19.21253900v1 2021. [DOI: 10.1101/2021.03.19.21253900] [DOI]
- Preckel K, Kanske P, Singer T, Paulus F, Krach S. Clinical trial of modulatory effects of oxytocin treatment on higher-order social cognition in autism spectrum disorder: a randomized, placebo-controlled, double-blind and crossover trial. BMC Psychiatry 2016;16(1):329-39. [DOI: 10.1186/s12888-016-1036-x] [DOI] [PMC free article] [PubMed] [Google Scholar]
Purdon 1994 {published data only}
- Purdon S, Lit W, Labelle A, Jones B. Risperidone in the Treatment of Pervasive Developmental Disorder. Canadian Journal of Psychiatry 1994;39(7):400-05. [DOI] [PubMed] [Google Scholar]
Radzivil 2006 {published data only}
- Radzivil M, Bashina V. An effect of long-term cerebrolysin therapy in combination with neuroleptics on behavioral and cognitive disturbances in endogenous childhood autism. Zhurnal Nevrologii i Psikhiatrii Imen 2006;106(2):21-5. [PMID: ] [PubMed] [Google Scholar]
Ratcliff‐Schaub 2005 {published data only}
- Ratcliff-Schaub K, Carey T, Reeves G, Rogers M. Randomized controlled trial of transdermal secretin on behavior of children with autism. the international journal of research and practice 2005;9(3):256-65. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ritvo 1971 {published data only}
- Ritvo E, Yuwiler A, Geller E, Kales E, Rashkis S, Schicor, A. Effects of L-dopa in autism. Journal of Autism & Childhood Schizophrenia 1971;1(2):190-205. [DOI] [PubMed] [Google Scholar]
Ritvo 1983 {published data only}
- Ritvo E, Freeman B, Geller E, Yuwiler A. Effects of fenfluramine on 14 outpatients with the syndrome of autism. Journal of the American Academy of Child Psychiatry 1983;22(6):549-58. [DOI: 10.1097/00004583-198311000-00006] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ritvo 1984 {published data only}
- Ritvo E, Freeman B, Yuwiler, A, Geller E, Yokota A, Schroth P. Study of fenfluramine in outpatients with the syndrome of autism. The Journal of pediatrics 1984;105(5):823-8. [DOI] [PubMed] [Google Scholar]
Roberts 2001 {published data only}
- Roberts W, Weaver L, Brian J, Bryson S, Emelianova S, Griffiths A. Repeated doses of porcine secretin in the treatment of autism: a randomized, placebo-controlled trial. Pediatrics 2001;107(5):E71. [DOI: 10.1542/peds.107.5.e71] [DOI] [PubMed] [Google Scholar]
Scifo 1996 {published data only}
- Scifo R, Batticane N, Quattropani N, Spoto G. A double-blind trial with naltrexone in autism. Brain Dysfunction 1991;4(6):301-7. [Google Scholar]
- Scifo R, Cioni M, Nicolosi A, Batticane N, Tirolo C, Testa N. Opioid-immune interactions in autism: behavioural and immunological assessment during a double-blind treatment with naltrexone. Annali dell'Istituto superiore di sanità 1996;32(3):351-9. [PubMed] [Google Scholar]
Sponheim 2002 {published data only}
- Sponheim E, Oftedal G, Helverschou S. Multiple doses of secretin in the treatment of autism: a controlled study. Acta paediatrica 2002;91(5):540-5. [DOI: 10.1111/j.1651-2227.2002.tb03274.x] [DOI] [PubMed] [Google Scholar]
Steiner 1999 {published data only}
- Steiner M, Babcock S, Steinberg S, Stewart D, Carter D, Berger C. Fluoxetine's efficacy in improving physical symptoms associated with pdd: results from a multisite, randomized, placebo-controlled trial. Proceedings of the 152nd annual meeting of the American Psychiatric Association 1999:15-20. [Google Scholar]
Stubbs 1986 {published data only}
- Stubbs E, Budden S, Jackson R, Terdal L, Ritvo E. Effects of fenfluramine on eight outpatients with the syndrome of autism. Developmental medicine and child neurology 1986;28(2):229-35. [DOI: 10.1111/j.1469-8749.1986.tb03859.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Sugie 2003 {published data only}
- Sugie Y, Sugie H, Fukuda T, Ito M, Ohzeki T. Studies on the adverse effects of fluvoxamine treatment in children with autistic disorder: correlation with genetic polymorphism in serotonin related genes. No to Hattatsu [Brain & Development] 2003;35(3):233-7. [PubMed] [Google Scholar]
Sugiyama 1998 {published data only (unpublished sought but not used)}
- Sugiyama N, Sugie H, Igarashi Y, Ito M, Fukuda T. Low-dose levodopa therapy of autistic disorder: evaluation of clinical effectiveness. No to Hattatsu [Brain and Development] 1998;30(1):51-5. [ISSN: 0029-0831] [PubMed] [Google Scholar]
Tachibana 2013 {published data only}
- Tachibana M, Kagitani-Shimono K, Mohri I, Yamamoto T, Sanefuji W, Nakamura A. Long-term administration of intranasal oxytocin is a safe and promising therapy for early adolescent boys with autism spectrum disorders. Journal of Child and Adolescent Psychopharmacology 2013;23(2):123-7. [DOI: 10.1089/cap.2012.0048] [PMID: ] [DOI] [PubMed] [Google Scholar]
Taylor 1993 {published data only}
- Taylor D, Sandman C, Touchette P, Hetrick W, Barron J. Naltrexone improves learning and attention in self-injurious individuals with developmental disabilities. Pharmacotherapy 1993;5(1):29-42. [DOI: 10.1007/BF01046596] [DOI] [Google Scholar]
Tolbert 1993 {published data only}
- Tolbert L, Haigler T, Waits M, Dennis T. Fluoxetine in autism. Journal of Autism and Developmental Disorders 1993;23(1):193-9. [DOI: 10.1007/BF01066428] [PMID: ] [DOI] [PubMed] [Google Scholar]
Troost 2006 {published data only}
- Troost P, Steenhuis M, Tuynman-Qua H, Kalverdijk L, Buitelaar J, Minderaa R. Atomoxetine for attention-deficit/hyperactivity disorder symptoms in children with pervasive developmental disorders: a pilot study. Journal of Child and Adolescent Psychopharmacology October 2006;16(5):611-19. [DOI: 10.1089/cap.2006.16.611] [DOI] [PubMed] [Google Scholar]
Volkmar 1983 {published data only}
- Volkmar F, Paul R, Cohen D, Shaywitz B. Irritability in autistic children treated with fenfluramine. New England Journal of Medicine 1983;309(3):187. [DOI] [PubMed] [Google Scholar]
Volkmar 2009 {published data only}
- Volkmar F. Citalopram treatment in children with autism spectrum disorders and high levels of repetitive behavior. Archives of General Psychiatry 2009;66(6):581-2. [DOI: 10.1001/archgenpsychiatry.2009.42] [DOI] [PubMed] [Google Scholar]
Wasserman 2005 {published data only}
- Wasserman S. Divalproex sodium vs. placebo in the treatment of repetitive behaviors and the treatment of activation associated with fluoxetine in autism spectrum disorder. Biological Psychiatry 2005;57(8):166S-167S. [DOI: 10.1017/S1461145705005791] [PMID: ] [DOI] [PubMed] [Google Scholar]
Wei 2011 {published data only}
- Wei B, Huang F, Qin X, Liang Q. Treatment of behavioral disorders by risperidone in children with autism. Zhongguo Dangdai Erke Zazhi 2011;13(3):216-8. [PubMed] [Google Scholar]
Witwer 2005 {published data only}
- Witwer A, Lecavalier L. Treatment incidence and patterns in children and adolescents with autism spectrum disorders. Journal of Child & Adolescent Psychopharmacology 2005;15(4):671-81. [PMID: ] [DOI] [PubMed] [Google Scholar]
Yarbrough 1987 {published data only}
- Yarbrough E, Santat U, Perel I, Webster C, Lombardi R. Effects of fenfluramine on autistic individuals residing in a state developmental centre. Journal of autism and developmental disorders 1987;17(3):303-14. [DOI: 10.1007/BF01487062] [DOI] [PubMed] [Google Scholar]
Yui 2012 {published data only}
- Yui K. Useful pharmacologic treatment in impaired social interaction in autism spectrum disorders. Seishin Shinkeigaku Zasshi - Psychiatria et Neurologia Japonica 2012;114(8):934-40. [PubMed] [Google Scholar]
Zingarelli 1992 {published data only}
- Zingarelli G, Ellman G, Hom A, Wymore M. Clinical effects of naltrexone on autistic behavior. American Journal on Mental Retardation 1992;97(1):57-63. [PubMed] [Google Scholar]
References to studies awaiting assessment
Anagnostou 2018 {published data only}
- Anagnostou E, Bennett TA, Thorpe K, Nicolson R. A phase 2 randomized, placebo-controlled trial of tideglusib, an orally administered GSK-3 beta inhibitor, in the treatment of adolescents with ASD. Journal of the American Academy of Child and Adolescent Psychiatry 2018;57(10):S232. [DOI: 10.1016/j.jaac.2018.09.311] [DOI] [Google Scholar]
Buitelaar 1996 {published data only}
- Buitelaar JK, Dekker ME, Van Ree JM, Van Engeland H. A controlled trial with ORG 2766, an ACTH-(4-9) analog, in 50 relatively able children with autism. European Neuropsychopharmacology 1996;6(1):13-9. [DOI: 10.1016/0924-977x(95)00049-u] [PMID: ] [DOI] [PubMed] [Google Scholar]
Campbell 1982a {published data only}
- Campbell M, Anderson L, Cohen I. Haloperidol in autistic children: effects on learning, behavior, and abnormal involuntary movements. Psychopharmacology Bulletin 1982;18(1):110-11. [Google Scholar]
Carminati 2016 {published data only}
- Carminati GG, Gerber F, Darbellay B, Kosel MM, Deriaz N, Chabert J, et al. Using venlafaxine to treat behavioral disorders in patients with autism spectrum disorder. Progress in Neuro-Psychopharmacology & Biological Psychiatry 2016;65:85-95. [DOI: 10.1016/j.pnpbp.2015.09.002] [PMID: ] [DOI] [PubMed] [Google Scholar]
Gabis 2019 {published data only}
- Gabis LV, Ben-Hur R, Shefer S, Jokel A, Shalom DB. Improvement of language in children with autism with combined donepezil and choline treatment. Journal of Molecular Neuroscience 2019;69(2):224-34. [DOI: 10.1007/s12031-019-01351-7] [PMID: ] [DOI] [PubMed] [Google Scholar]
- NCT01098383. Treatment with acetyl-choline esterase inhibitors in children with autism spectrum disorders [Treatment with acetyl-choline esterase inhibitors in children with autism ]. clinicaltrials.gov/ct2/show/NCT01098383 (first received 2 April 2010).
Handen 2000 {published data only}
- Handen BL, Johnson CR, Lubetsky M. Efficacy of methylphenidate among children with autism and symptoms of attention-deficit hyperactivity disorder. Journal of Autism and Developmental Disorders 2000;30(3):245-55. [DOI: 10.1023/A:1005548619694] [PMID: ] [DOI] [PubMed] [Google Scholar]
IRCT2017041333406N1 {published data only}IRCT2017041333406N1
- IRCT2017041333406N1. The efficacy of augmentation donepezil to risperidon in treatment of autism spectrum disorders [Assessment the efficacy of augmentation donepezil to risperidon in treatment of autism spectrum disorders]. www.irct.ir/trial/25769 (first received 20 September 2017).
IRCT20190714044199N1 {published data only}IRCT20190714044199N1
- IRCT20190714044199N1. Efficacy of N-acetyl cysteine in patients with autism spectrum disorder [Evaluating the efficacy of adding N-acetyl cysteine to risperidone treatment regimen in patients with autism spectrum disorder]. www.irct.ir/trial/41209 (first received 10 November 2019).
JPRN‐JMA‐IIA00438 {published data only}
- JPRN-JMA-IIA00438. The efficacy and safety of pyridoxamine in patients with autism spectrum disorder; exploratory physician-led Phase 2 trial. ww.trialsearch.who.int/Trial2.aspx?trialID=JPRN-JMA-IIA00438 (first received March 2020).
Jung 2000 {published data only}
- Jung S, Lee Y. A double blind study of dimethylglycine treatment in children with autism. A double blind study of dimethylglycine treatment in children with autism 2000;12(2):111-21. [Google Scholar]
Jørgensen 2002 {published data only}
- Jørgensen M, Thomsen PH, Henriksen JH. Secretin treatment of autism? Ugeskrift for Laeger 2002;164(12):1676. [PMID: ] [PubMed] [Google Scholar]
Kern 2001a {published data only (unpublished sought but not used)}
- Kern JK, Miller VS, Cauller L, Kendall R, Mehta J, Dodd M. Effectiveness of N,N-Dimethylglycine in autism and pervasive developmental disorder. Journal of Child Neurology 2000;16(3):169-73. [DOI: 10.2310/7010.2001.17515] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kern 2002 {published data only}
- Kern JK, Van Miller S, Evans PA, Travedi MH. Efficacy of porcine secretin in children with autism and pervasive developmental disorder. Journal of Autism and Developmental Disorders 2002;32(3):153-60. [DOI: 10.1023/A:1015441428154] [PMID: ] [DOI] [PubMed] [Google Scholar]
Li 2016 {published data only}
- Li Y-C, Ma J, Xu H-M, Yang G-Y, Zhang J-C. Efficacy and safety of paliperidone and aripiprazole in the treatment of autism. Chinese Journal of New Drugs 2016;25(16):1893-7. [Google Scholar]
Malone 2010 {published data only}
- Malone R, West S, Ghaffari M, Delaney M, Hardison H. Metabolic effects of olanzapine in children with autistic disorder. Journal of Child and Adolescent Psychopharmacology 2010;20(6):531-2. [DOI: 10.1089/cap.2010.2064] [DOI] [Google Scholar]
- NCT00057408. A controlled sudy of olanzapine in children with autism. clinicaltrials.gov/ct2/show/NCT00057408 (first received 2 April 2003).
Martsenkovsky 2016 {published data only}
- Martsenkovsky I, Martsenkovska I. The safety and efficacy of memantine hydrochloride versus placebo for children under 3 years old with autism spectrum disorders. European Neuropsychopharmacology 2016;26(2):S729. [DOI: 10.1016/S0924-977X(16)31879-X] [EISSN: 1873-786] [ABSTRACT NO: P.7.d.002] [DOI] [Google Scholar]
Miller 1979 {published data only}
- Miller B, Wallis H. Mode of action of sulpiride in autistic children. A double blind study. Münchener Medizinische Wochenschrift 1979;121(19):667-9. [PMID: ] [PubMed] [Google Scholar]
Molloy 2002 {published data only (unpublished sought but not used)}
- Molloy CA, Manning-Courtney P, Swayne S, Bean J, Brown JM, Murray DS, et al. Lack of benefit of intravenous synthetic human secretin in the treatment of autism. Journal of Autism and Developmental Disorders 2002;32(6):545-51. [DOI: 10.1023/A:1021202930206] [PMID: ] [DOI] [PubMed] [Google Scholar]
Naruse 1982 {published data only}
- Hyoka R. A multi centered double blind trial of pimozide (Orap), haloperidol and placebo for abnormal behavior in children using crossover design. Clinical Evaluation 1980;8(3):629-73. [Google Scholar]
- Naruse H, Nagahata M, Nakane Y, Shirahashi K, Takesada M, Yamazaki K. A multi-center double-blind trial of pimozide (Orap), haloperidol and placebo in children with behavioral disorders, using crossover design. Acta Paedopsychiatrica 1982;48(4):173-84. [PMID: ] [PubMed] [Google Scholar]
Noone 2014 {published data only}
- Noone R, Ferretti C, Taylor B, Racine E, Hollander E. Milnacipran vs placebo in adult autism spectrum disorder: impact on hyperactivity. Neuropsychopharmacology 2014;39:S291-S472. [DOI: 10.1038/npp.2014.281] [DOI] [Google Scholar]
Novotny 2004 {published data only (unpublished sought but not used)}
- Novotny S, Hollander E, Phillips A, Allen A, Wasserman S, Iyengar R. Increased repetitive behaviours and prolactin responsivity to oral m-chlorophenylpiperazine in adults with autism spectrum disorders. International Journal of Neuropsychopharmacology 2004;7(3):249-54. [DOI: 10.1017/S146114570400433X] [PMID: ] [DOI] [PubMed] [Google Scholar]
Sandler 1999 {published data only (unpublished sought but not used)}
- Sandler AD, Sutton KA, DeWesse J, Girardi MA, Sheppard V, Bodfish JW. Lack of benefit of a single dose of synthetic human secretin in the treatment of autism and pervasive developmental disorder. New England Journal of Medicine 1999;341(24):1801-6. [DOI: 10.1056/NEJM199912093412404] [PMID: ] [DOI] [PubMed] [Google Scholar]
Stern 1990 {published data only (unpublished sought but not used)}
- Stern LM, Walker MK, Sawyer MG, Oades RD, Badcock NR, Spence JG. A controlled crossover trial of fenfluramine in autism. Journal of Child Psychology and Psychiatry 1990;31(4):569-85. [DOI: 10.1111/j.1469-7610.1990.tb00798.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Wink 2020 {published data only}
- NCT02611921. Study of intranasal ketamine for social impairment in autism spectrum disorder. Search of: NCT02611921 - List Results - ClinicalTrials.gov First received January 2021.
- Wink L, Reisinger, DL, Horn P, Shaffer R, O'Brien K, Schmitt L. Brief Report: intranasal Ketamine in Adolescents and Young Adults with Autism Spectrum Disorder—Initial Results of a Randomized, Controlled, Crossover, Pilot Study. Journal of Autism and Developmental Disorders 2020;51(4):1392-99. [DOI: 10.1007/s10803-020-04542-z] [PMID: ] [DOI] [PubMed] [Google Scholar]
Yatawara 2016 {published data only}
- Yatawara C, Einfeld S, Hickie I, Davenport T, Guastella A. The effect of oxytocin nasal spray on social interaction deficits observed in young children with autism: a randomized clinical crossover trial. Molecular Psychiatry September 2016;21(9):1225-31. [DOI: 10.1038/mp.2015.162] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
ACTRN12617000441314 {published data only}
- ACTRN12617000441314. The feasibility of magnetic resonance imaging in a non-selective comprehensive clinical trial in pediatric autism spectrum disorder. australianclinicaltrials.gov.au/anzctr/trial/ACTRN12617000441314 (first received in 2017).
ChiCTR1800017720 {published data only}
- ChiCTR1800017720. A random, double-blind, placebo controlled trial for oxytocin nasal spray in the treatment for ASD social dysfunction. www.chictr.org.cn/showprojen.aspx?proj=29953 (first received 10 August 2018).
Crutel 2020 {published data only}
- Crutel V, Lambert E, Penelaud P-F, Albarran Severo C, Fuentes J, Rosier A, et al. Bumetanide oral liquid formulation for the treatment of children and adolescents with autism spectrum disorder: design of two phase III studies (SIGN Trials). Journal of Autism and Developmental Disorders 2020;51(8):2959-72. [DOI: 10.1007/s10803-020-04709-8] [PMCID: PMC8254707] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
CTRI/2021/12/038721 {published data only}
- CTRI/2021/12/038721. Comparison of the efficacy of oral risperidone and aripiprazole in children with autism spectrum disorders (ASDs) aged 6-18 years: a double blind randomized controlled trial - RAAT. www.trialsearch.who.int/Trial2.aspx?TrialID=CTRI/2021/12/038721 (first received December 2021).
EUCTR2008‐003712‐36‐FR {published data only}
- EUCTR2008-003712-36-FR. Study of the clinical and neurofunctional response to fluoxetine in childhood autism (FAIR) [Etude de la réponse clinique et neurofonctionnelle à la fluoxétine dans l'autisme infantile (FAIR)]. www.clinicaltrialsregister.eu/ctr-search/trial/2008-003712-36/FR (first received 19 June 2008).
EUCTR2010‐024202‐34‐DE {published data only}EUCTR2010‐024202‐34‐DE
- EUCTR2010-024202-34-DE. Group-therapy, autism and oxytocin - an investigation with the question "Does oxytocin (OT) enhance therapy effects in autism?" [Effekt von oxytocin auf den therapieerfolg eines sozialen kompetenztrainings bei jugendlichen mit autismus-spektrum-störung (Effect of oxytocin on therapy results of a group based social skill training in adolescents with autism spectrum disorder)]. www.clinicaltrialsregister.eu/ctr-search/trial/2010-024202-34/DE (first received 9 December 2013).
EUCTR2014‐003080‐‐38‐DE {published data only}EUCTR2014‐003080‐‐38‐DE
- Häge A, Banaschewski T, Buitelaar JK, Dijkhuizen RM, Franke B, Lythgoe DJ, et al. Glutamatergic medication in the treatment of obsessive compulsive disorder (OCD) and autism spectrum disorder (ASD) – study protocol for a randomised controlled trial. Trials 2016;17(1):141. [DOI: 10.1186/s13063-016-1266-8] [PMCID: PMC4794817] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
IRCT20090117001556N124 {published data only}IRCT20090117001556N124
- IRCT20090117001556N124. Cilostazol in the treatment of autism [Cilostazol as adjunctive treatment of autism: a double blind and placebo controlled trial in children 5 to 11 years old cilostazol in the treatment of autism]. www.irct.ir/trial/48108 (first received 16 May 2020).
IRCT20200317046801N2 {published data only}IRCT20200317046801N2
- IRCT20200317046801N2. The effect of ondansetron on autism [Effect of ondansetron combination therapy with risperidone in children with autism spectrum disorder in a randomized, double-blind, placebo-controlled clinical trialThe effect of ondansetron on autism]. www.irct.ir/trial/46589 (first received 13 April 2020).
ISRCTN15984604 {published data only}
- ACTRN12621000801819. Sertraline for anxiety in adults with a diagnosis of autism (STRATA) a randomised controlled trial. Australianclinicaltrials.gov.au/anzctr/trial/ACTRN12621000801819 (first received 9 February 2022).
- ISRCTN15984604. Sertraline for anxiety in adults with a diagnosis of autism. www.isrtcn.com/ISRTCN15984604.
JPRN‐UMIN000017876 {published data only}
- UMIN000017876. Effects of long-term administration of intranasal oxytocin in children with autism spectrum disorder. https://center6.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno=R000020712 (first registered June 2015).
NCT00198120 {published data only}
- NCT00198120. Safety and effectiveness of D-cycloserine in children with autism [A randomized controlled trial of D-cycloserine in autism]. clinicaltrials.gov/ct2/show/NCT00198120 (first received 20 September 2005).
NCT01914939 {published data only}
- NCT01914939. A randomized, controlled trial of intranasal oxytocin as an adjunct to behavioral therapy for autism spectrum disorder. clinicaltrials.gov/ct2/show/NCT01914939 (first received 2 August 2013).
NCT01970345 {published data only}
- NCT01970345. A pilot treatment study of insulin-like growth factor-1 (IGF-1) in autism spectrum disorder. clinicaltrials.gov/ct2/show/NCT01970345 (first received 28 October 2013).
NCT03553875 {published data only}
- NCT03553875. Memantine for the treatment of social deficits in youth with disorders of impaired social interactions [Memantine for the treatment of social deficits in youth with disorders of impaired social interactions: a randomized controlled trial]. clinicaltrials.gov/show/NCT03553875 (first received 12 June 2018).
NCT03887676 {published data only}
- NCT03887676. Arbaclofen vs. Placebo in the Treatment of Children and Adolescents With ASD. clinicaltrials.gov/ct2/show/NCT03887676?term=NCT03887676%draw=2&rank=1 (first received 18 March 2019).
NCT04520685 {published data only}
- NCT04520685. CASCADE: CAnnabidiol Study in Children with Autism Spectrum DisordEr [CAnnabidiol Study in Children With Autism Spectrum DisordEr (CASCADE): a double-blind, placebo-controlled study to investigate efficacy and safety of cannabidiol in children and adolescents with autism]. clinicaltrials.gov/ct2/show/NCT04520685 (first received 20 August 2020).
NCT04725383 {published data only}
- NCT04725383. Amitriptyline for repetitive behaviors in autism spectrum disorders. www.clinicaltrails.gov/ct2/showNCT04725383?term=NCT04725383&draw=2&rank=1 (first received 1 July 2023).
NCT04745026 {published data only}
- EUCTR2020-002819-21. An exploratory, Phase 2, randomized, double-blind, placebo-controlled trial to investigate the safety and efficacy of cannabidiol oral solution (GWP42003-P; CBD-OS) in children and adolescents with autism spectrum disorder. clinicaltrialregister.eu/ctr-search/trial/2020-002819-21/DE (first received April 2021).
- NCT04745026. Trial to investigate the safety and efficacy of cannabidiol oral solution (GWP42003-P; CBD-OS) in children and adolescents with autism spectrum disorder. clinicaltrials.gov/ct2/show/NCT04745026?term=NCT04745026&draw=2&rank=1 (first received February 2021).
NCT04895215 {published data only}
- NCT04895215. AB-2004 in Treatment of adolescents with irritability associated with autism spectrum sisorder (ASD). AB-2004 in Treatment of adolescents with irritability associated with autism spectrum disorder (ASD) - full text view - ClinicalTrials.gov (first received May 2021).
NCT05015439 {published data only}
- NCT05015439. Cannabidiol (CBD) in adults With ASD. Cannabidiol (CBD) in adults With ASD - full text view - ClinicalTrials.gov (first received August 2021).
NCT05163717 {published data only}
- NCT05163717. INP105 proof-of-concept study for the acute treatment of agitation in adolescents with ASD (CALM 201). www.clinicaltrials.gov/ct2/show/NCT05163717 (first received 20 December 2021).
NCT05182697 {published data only}
- NCT05182697. SCI-210 in the treatment of children and young adults with autism evaluate the safety, tolerability and efficacy of SCI-210 in children with autism spectrum disorder (ASD). www.clinicaltrials.govct/show/NCT05182697?term=NCT05182697&draw=2&rank=1 (first received January 2022).
Parellada 2021 {published data only}
- NCT03682978. Arbaclofen in children and adolescents with ASD (AIMS2-CT1). clinicaltrials.gov/ct2/show/NCT03682978?term=NCT03682978&draw=2&rank=1 (first received 25 March 2019).
- Parellada M, Cáceres AS, Palmer M, Delorme R, Jones EJ, Parr JR, et al. A phase II randomised, double-blind, placebo-controlled study of the efficacy, safety and tolerability of arbaclofen administered for the treatment of social function in children and adolescents with autism spectrum disorders - study protocol for AIMS-2-TRIALS-CT1. Frontiers in Psychiatry 2021;12:701729. [DOI: 10.3389/fpsyt.2021.701729] [DOI] [PMC free article] [PubMed] [Google Scholar]
UMIN000017876 {published data only}UMIN000017876
- UMIN000017876. Effects of long-term administration of intranasal oxytocin in children with autism spectrum disorder. upload.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno=R000020712 (first received 19 June 2015).
Additional references
Achenbach 2000
- Achenbach TM, Rescorla L. Manual for the ASEBA preschool forms and profiles. Burlington, Vermont: University of Vermont, Research Center for Children, 2000. [Google Scholar]
Alfageh 2019
- Alfageh BH, Wang Z, Mongkhon P, Besag FM, Alhawassi TM, Brauer R, et al. Safety and tolerability of antipsychotic medication in individuals with autism spectrum disorder: a systematic review and meta-analysis. Pediatric Drugs 2019;21(3):153-67. [DOI: 10.1007/s40272-019-00333-x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Alvarez‐Jiménez 2008
- Alvarez-Jiménez M, González-Blanch C, Crerco-Facorro B, Hetrick S, Rodríguez-Sánchez JM, Pérez-Iglesias R, et al. Antipsychotic-induced weight gain in chronic and first-episode psychotic disorders: a systematic critical reappraisal. CNS Drugs 2008;22(7):547-62. [DOI: 10.2165/00023210-200822070-00002] [PMID: ] [DOI] [PubMed] [Google Scholar]
Aman 1985
- Aman M, G, Singh NN, Stewart AW, Field CJ. The Aberrant Behavior Checklist: a behavior rating scale for the assessment of treatment effects. American Journal of Mental Deficiency 1985;89(5):485-91. [PMID: ] [PubMed] [Google Scholar]
Aman 1996
- Aman MG, Tasse MJ, Rojahn J, Hammer D. The Nisonger CBRG: a child behavior rating form for children with developmental disabilities. Research in Developmental Disabilities 1996;17(1):41-57. [DOI: 10.1016/0891-4222(95)00039-9] [PMID: ] [DOI] [PubMed] [Google Scholar]
Andari 2010
- Andari E, Duhamel J-R, Zalla T, Herbrecht E, Leboyer M, Sirigu A. Promoting social behaviour with oxytocin in high-functioning autism spectrum disorders. Proceedings of the National Academy of Sciences of the United States of America 2010;107(9):4389-94. [DOI: 10.1073/pnas.0910249107] [PMCID: PMC2840168] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Anderson 1987
- Anderson GM, Freedman DX, Cohen DJ, Volkmar FR, Hoder EL, McPhedran P. Whole blood serotonin in autistic and normal subjects. Journal of Child Psychology and Psychiatry and allied disciplines 1987;28(6):885-900. [DOI] [PubMed] [Google Scholar]
Antshel 2013
- Antshel KM, Zhang-James Y, Faraone SV. The comorbidity of ADHD and autism spectrum disorder. Expert Review of Neurotherapeutics 2013;13(10):1117-28. [DOI: 10.1586/14737175.2013.840417] [PMID: ] [DOI] [PubMed] [Google Scholar]
Aronson 2016
- Aronson JK. Buspirone. In: Aronson JK, editors(s). Meyler's Side Effects of Drugs: The International Encyclopedia of Adverse Drug Reactions and Interactions. 16th edition. Amsterdam: Elsevier, 2016:1096-99. [DOI: 10.1016/B978-0-444-53717-1.00423-6] [DOI] [Google Scholar]
Arora 2018
- Arora NK, Nair MK, Gulati S, Deshmukh V, Mohapatra A, Mishra D, et al. Neurodevelopmental disorders in children aged 2-9 years: population-based burden estimates across five regions in India. PloS Medicine 2018;15(7):e1002615-e. [DOI: 10.1371/journal.pmed.1002615] [PMCID: PMC6057634] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Autism Spectrum Australia 2023
- Autism Spectrum Australia. How do we describe autism? https://www.autismspectrum.org.au/blog/how-do-we-describe-autism .
Autistic Self Advocacy Network 2023
- Identity-first language. https://autisticadvocacy.org/about-asan/identity-first-language/.
Bak 2014
- Bak M, Fransen A, Janssen J, Van Os J, Drukker M. Almost all antipsychotics result in weight gain: a meta-analysis. PloS One 2014;9(4):e94112. [DOI: 10.1371/journal.pone.0094112] [PMCID: PMC3998960] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Banas 2020
- Banas K, Sawchuk B. Clonidine as a treatment of behavioural disturbances in autism spectrum disorder: a systematic literature review. Journal of the Canadian Academy of Child and Adolescent Psychiatry 2020;29(2):110-20. [PMCID: PMC7213918] [PMID: ] [PMC free article] [PubMed] [Google Scholar]
Banko 2011
- Banko JL, TrotterJ, Weeber EJ. Insights into synaptic function from mouse models of human cognitive disorders. Future Neurology 2011;6(1):113-25. [DOI: 10.2217/fnl.10.80] [PMCID: PMC4114080] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Baron‐Cohen 2008
- Baron-Cohen S. Autism and Asperger Syndrome. New York: Oxford University Press, 2008. [Google Scholar]
Benarous 2019
- Benarous X, Consoli A, Cohen D, Renaud J, Lahaye H, Guilé J-M. Suicidal behaviors and irritability in children and adolescents:a systematic review of the nature and mechanisms of the association. European Child and Adolescent Psychiatry October 2018;28(5):667-83. [DOI: 10.1007/s00787-018-1234-9] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bitsika 2016
- Bitsika V, Sharpley CF. Which aspects of challenging behaviour are associated with anxiety across two age groups of young males with an autism spectrum disorder? Journal of Developmental and Physical Disabilities 2016;28(5):685-701. [DOI: 10.1007/s10882-016-9502-4] [DOI] [Google Scholar]
Bodfish 2000
- Bodfish JW, Symons FS, Parker DE, Lewis MH. Varieties of repetitive behavior in autism: comparisons to mental retardation. Journal of Autism and Developmental Disorders 2000;30(3):237-43. [DOI: 10.1023/A:1005596502855] [PMID: ] [DOI] [PubMed] [Google Scholar]
Branford 2019
- Branford D, Gerrard D, Saleem N, Shaw C, Webster A. Stopping over-medication of people with intellectual disability, autism or both (STOMP) in England part 1 – history and background of STOMP. Advances in Mental Health and Intellectual Disabilities 2019;13(1):31-40. [DOI: 10.1108/AMHID-02-2018-0004] [DOI] [Google Scholar]
Brondino 2016
- Brondino N, Fusar-Poli L, Panisi C, Damiani S, Barale F, Politi P. Pharmacological modulation of GABA function in autism spectrum disorders: a systematic review of human studies. Journal of Autism and Developmental Disorders 2016;46(3):825-39. [DOI: 10.1007/s10803-015-2619-y] [PMID: ] [DOI] [PubMed] [Google Scholar]
Brooks 2021
- Brooks J, Bronskill S, Fu L, Saxena F, Arneja J, Pinzaru V, et al. Identifying children and youth with autism spectrum disorder in electronic medical records: examining health system utilisation and comorbidities. Autism Research 2021;14(2):400-410. [DOI: 10.1002/aur.2419] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brown 1979
- Brown GL, Goodwin FK, Ballenger JC, Goyer PF, Major LF. Aggression in humans correlates with cerebrospinal fluid amine metabolites. Psychiatry Research 1979;1(2):131-9. [DOI: 10.1016/0165-1781(79)90053-2] [PMID: ] [DOI] [PubMed] [Google Scholar]
Caye 2019
- Caye A, Swanson JM, Coghill D, Rohde LA. Treatment strategies for ADHD: an evidence-based guide to select optimal treatment. Molecular Psychiatry 2019;24(3):390–408. [DOI: 10.1038/s41380-018-0116-3] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ceranoglu 2019
- Ceranoglu TA, Wozniak J, Fried R, Galdo M, Hoskova B, DeLeon Fong M, et al. A retrospective chart review of buspirone for the treatment of anxiety in psychiatrically referred youth with high-functioning autism spectrum disorder. Journal of Child and Adolescent Psychopharmacology 2019;29(1):28-33. [DOI: 10.1089/cap.2018.0021] [PMCID: PMC6354602] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chaddad 2017
- Chaddad A, Desrosiers C, Hassan L, Tanougast C. Hippocampus and amygdala radiomic biomarkers for the study of autism spectrum disorder. BMC Neuroscience 2017;18(1):52. [DOI: 10.1186/s12868-017-0373-0] [PMCID: PMC6389224] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chaimani 2013
- Chaimani A, Higgins JP, Mavridis D, Spyridonos P, Salanti G. Graphical tools for network meta-analysis in STATA. PLoS One 2013;8(10):e76654. [DOI: 10.1371/journal.pone.0076654] [PMCID: PMC3789683] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chang 2021
- Chang C-H, Liu C-Y, Chen S-J, Tsai H-C. Effect of N‑Methyl‑D‑Aspartate receptor enhancing agents on cognition in dementia: an exploratory systematic review and meta‑analysis of randomized controlled trials. Scientific Reports 2021;11(1):22996-22996. [DOI: 10.1038/s41598-021-02040-5] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chez 2003
- Chez MG, Buchanon TM, Becker M, Kessler J, Aimonovitch MC, Mrazek SR. Donepezil hydrochloride: a double-blind study in autistic children. Journal of Pediatric Neurology 2003;1(2):83-8. [DOI: 10.1055/s-0035-1557175] [DOI] [Google Scholar]
Chez 2004
- Chez MG, Hung PC, Chin K, Memon S, Kirschner S. Memantine experience in children and adolescents with autistic spectrum disorders. Annals of Neurology 2004;56(Suppl 8):S109. [DOI: 10.1002/ana.20263] [DOI] [Google Scholar]
Ching 2012
- Ching H, Pringsheim T. Aripiprazole for autism spectrum disorders (ASD). Cochrane Database of Systematic Reviews 2012, Issue 5. Art. No: CD009043. [DOI: 10.1002/14651858.CD009043.pub2] [PMID: ] [DOI] [PubMed] [Google Scholar]
Cleaton 2018
- Cleaton MA, Kirby A. Why do we find it so hard to calculate the burden of neurodevelopmental disorders? Journal of Childhood and Developmental Disorders 2018;4(3):10-20. [DOI: 10.4172/2472-1786.100073] [DOI] [Google Scholar]
Cohen 1988
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd edition. Hillsdale (NJ): Erlbaum, 1988. [ISBN: 0-8058-0283-5] [Google Scholar]
Cortes‐Altamirano 2016
- Cortes-Altamirano JL, Olmes-Hernández A, Bonilla-Jaime H, Bandala C, González-Maciel A, Alfaro-Rodríguez A. Levetiracetam as an antiepileptic, neuroprotective, and hyperalgesic drug. Neurology India 2016;64(6):1266-75. [DOI: 10.4103/0028-3886.193801] [PMID: ] [DOI] [PubMed] [Google Scholar]
Cortese 2012
- Cortese S, Castelnau P, Morcillo C, Roux S, Bonnet-Brilhault F. Psychostimulants for ADHD-like symptoms in individuals with autism spectrum disorders. Expert Review of Neurotherapeutics 2012;12(4):461-73. [DOI: 10.1586/ern.12.23] [PMID: ] [DOI] [PubMed] [Google Scholar]
Coury 2012
- Coury DL, Anagnostou E, Manning-Courtney P, Reynolds A, Cole L, McCoy R, et al. Use of psychotropic medication in children and adolescents with autism spectrum disorders. Pediatrics 2012;130(Suppl 2):S69-76. [DOI: 10.1542/peds.2012-0900D] [PMID: ] [DOI] [PubMed] [Google Scholar]
Craig 2015
- Craig F, Lamanna AL, Margari F, Matera E, Simone M, Margari L. Overlap between autism spectrum disorders and attention deficit hyperactivity disorder: searching for distinctive/common clinical features. 2015 8;3:328-37. [DOI: 10.1002/aur.1449] [PMCID: PMC4654237] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Crocco 2017
- Crocco EA, Jaramillo S, Cruz-Ortiz C, Camfield K. Pharmacological management of anxiety disorders in the elderly. Current Treatment Options in Psychiatry 2017;4(1):33-46. [DOI: 10.1007/s40501-017-0102-4] [PMCID: PMC5609714] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cvejic 2018
- Cvejic RC, Arnold SR, Foley K-R, Troller Jn. Neuropsychiatric profile and psychotropic medication use in adults with autism spectrum disorder: results from the Australian Longitudinal Study of Adults with Autism. BJPsych Open 2018;4(6):461-6. [DOI: 10.1192/bjo.2018.64] [PMCID: PMC6235990] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Davico 2018
- Davico C, Canavese C, Vittorini R, Gandione M, Vitiello B. Anticonvulsants for psychiatric disorders in children and adolescents: a systematic review of their efficacy. Frontiers in Psychiatry 2018;9:270. [DOI: 10.3389/fpsyt.2018.00270] [PMCID: PMC6024111] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
De Boer 2019
- De Boer JN, Vingerhoets C, Hirdes M, McAlonan GM, Amelsvoort TV, Zinkstok JR. Efficacy and tolerability of riluzole in psychiatric disorders: a systematic review and preliminary meta-analysis. Psychiatry Research 2019;278:294-302. [DOI: 10.1016/j.psychres.2019.06.020] [PMID: ] [DOI] [PubMed] [Google Scholar]
Deb 2009
- Deb S, Kwok H, Bertelli M, Salvador-Carulla L, Bradley E, Torr J, et al. International guide to prescribing psychotropic medication for the management of problem behaviours in adults with intellectual disabilities. World Psychiatry 2009;8(3):181-6. [DOI: 10.1002/j.2051-5545.2009.tb00248.x] [PMCID: PMC2758582] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Deb 2015
- Deb S, Unwin G, Deb T. Characteristics and the trajectory of psychotropic medication use in general and antipsychotics in particular among adults with an intellectual disability who exhibit aggressive behaviour. Journal of Intellectual Disability Research 2015;59(1):11-25. [DOI: 10.1111/jir.12119] [PMID: ] [DOI] [PubMed] [Google Scholar]
Deb 2021
- Deb S, Roy M, Lee R, Majid M, Limbu B, Santambrogio J, et al. Randomised controlled trials of antidepressant and anti-anxiety medications for people with autism spectrum disorder: systematic review and meta-analysis. BJPsych Open 2021;7(6):e179. [DOI: 10.1192/bjo.2021.1003] [PMCID: PMC8503912] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2022
- Deeks JJ, Higgins JP, Altman DG editor(s). Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (updated February 2022). Cochrane, 2022. Available from www.training.cochrane.org/handbook.
DeLorenzo 2005
- DeLorenzo RJ, Sun DA, Deshpande LS. Cellular mechanisms underlying acquired epilepsy: the calcium hypothesis of the induction and maintainance of epilepsy. Pharmacology & Therapeutics 2005;105(3):229-66. [DOI: 10.1016/j.pharmthera.2004.10.004] [PMCID: PMC2819430] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
DiCarlo 2019
- DiCarlo GE, Aguilar JI, Matthies HJ, Harrison FE, Bundschuh KE, West A, et al. Autism-linked dopamine transporter mutation alters striatal dopamine neurotransmission and dopamine dependent behaviors. Journal of Clinical Investigation 2019;129(8):3407-19. [DOI: 10.1172/JCI127411] [PMCID: PMC6668686] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dinnissen 2020
- Dinnissen M, Dietrich A, Van der Molen JH, Verhallen AM, Buiteveld Y, Jongejan S. Prescribing antipsychotics in child and adolescent psychiatry - guideline adherence. European Child and Adolescent Psychiatry 2020;29(12):1717-27. [DOI: 10.1007/s00787-020-01488-6] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
DSM‐4 1994
- American Psychiatric Association. DSM-4. Diagnostic and Statistical Manual of Mental Disorders. 4th edition. Arlington (VA): American Psychiatric Association, 1994. [Google Scholar]
DSM‐4‐TR 2000
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4-TR edition. Arlington (VA): American Psychiatric Association, 2000. [Google Scholar]
DSM‐5 2013
- American Psychiatric Association. DSM-5. Diagnostic and Statistical Manual of Mental Disorders. 5th edition. Arlington (VA): American Psychiatric Association, 2013. [Google Scholar]
D’Alò 2021
- D’Alò GL, De Crescenzo F, Amato L, Cruciani F, Davoli M, Fulceri F, et al. Impact of antipsychotics in children and adolescents with autism spectrum disorder: a systematic review and meta-analysis. Health and Quality of Life Outcomes 2021;19(1):33. [DOI: 10.1186/s12955-021-01669-0] [PMCID: PMC7831175] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Elsabbagh 2012
- Elsabbagh M, Divan G, Koh Y-J, Kim YS, Kauchali S, Marcín C, et al. Global prevalence of autism and other pervasive developmental disorders. Autism Research 2012;5(3):160-79. [DOI: 10.1002/aur.239] [PMCID: PMC3763210] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Emerson 1995
- Emerson E, Bromley J. The form and function of challenging behaviours. Journal of Intellectual Disability Research 1995;39(5):388-98. [DOI: 10.1111/j.1365-2788.1995.tb00543.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Emerson 2001
- Emerson E, Kiernan C, Alborz A, Reeves D, Mason H, Swarbrick R, et al. The prevalence of challenging behaviours: a total population study. Research in Developmental Disabilities 2001;22(1):77-93. [DOI: 10.1016/S0891-4222(00)00061-5] [PMID: ] [DOI] [PubMed] [Google Scholar]
Epstein 2013
- Epstein JN, Loren RE. Changes in the definition of ADHD in DSM-5: subtle but important. Neuropsychiatry 2013;3(5):455-8. [DOI: 10.2217/npy.13.59] [PMCID: PMC3955126] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Erickson 2007
- Erickson CA, Posey DJ, Stigler KA, Mullett J, Katschke AR, McDougle CJ. A retrospective study of memantine in children and adolescents with pervasive developmental disorders. Psychopharmacology 2007;191(1):141-7. [DOI: 10.1007/s00213-006-0518-9] [PMID: ] [DOI] [PubMed] [Google Scholar]
Esbensen 2009
- Esbensen AJ, Greenberg JS, Seltzer MM, Aman MG. A longitudinal investigation of psychotropic and non-psychotropic medication use among adolescents and adults with autism spectrum disorders. Journal of Autism and Developmental Disorders 2009;39(9):1339-49. [PMCID: PMC2829244] [PMID: 10.1007/s10803-009-0750-3] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fallah 2019
- Fallah MS, Shaikh MR, Neupane B, Rusiecki D, Bennett TA, Beyene J. Atypical antipsychotics for irritability in pediatric autism: a systematic review and network meta-analysis. Journal of Child and Adolescent Psychopharmacology 2019;29(3):168-80. [DOI: 10.1089/cap.2018.0115] [PMID: ] [DOI] [PubMed] [Google Scholar]
Fitzpatrick 2016
- Fitzpatrick SE, Srivorakiat L, Wink LK, Pedapati EV, Erickson CA. Aggression in autism spectrum disorder: presentation and treatment options. Neuropsychiatric Disease and Treatment 2016;12:1525-38. [DOI: 10.2147/NDT.S84585] [PMCID: PMC4922773] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Freeman 1986
- Freeman BJ, Ritvo ER, Yokota A, Ritvo A. A scale for rating symptoms of patients with the syndrome of autism in real life settings. Journal of the American academy of child psychiatry 1986;25(1):130-6. [DOI: 10.1016/S0002-7138(09)60610-5] [PMID: ] [DOI] [PubMed] [Google Scholar]
Froehlich 2013
- Froehlich TE, Delgado SV, Anixt JS. Psychostimulant and non-stimulant agents address the symptoms of ADHD substantial evidence shows. Current Psychiatry 2013;12(12):21-9. [ISSN: 1537-8276] [URL: www.mdedge.com/psychiatry/article/78793/neurology/expanding-medication-options-pediatric-adhd] [PMC free article] [PubMed] [Google Scholar]
Fung 2016
- Fung LK, Mahajan R, Nozzolillo A, Bernal P, Krasner A, Jo B, et al. Pharmacologic treatment of severe irritability and problem behaviors in autism: a systematic review and meta-analysis. Pediatrics 2016;137(Suppl 2):S124-5. [DOI: 10.1542/peds.2015-2851K] [PMID: ] [DOI] [PubMed] [Google Scholar]
Geiger 2011
- Geiger WJ, Nievera CC, Musil B, Goldstein JT. Managing seizures: achieving control while minimizing risk. Journal of Family Practice 2011;60(8):464-72. [PMID: ] [PubMed] [Google Scholar]
Ghanizadeh 2013
- Ghanizadeh A. Atomoxetine for treating ADHD symptoms in autism: a systematic review. Journal of Attention Disorders 2013;17(8):635-40. [DOI: 10.1177/1087054712443154] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ghanizadeh 2019
- Ghanizadeh A, Molla M, Olanga GJ. The effect of stimulants on irritability in autism comorbid with ADHD: a systematic review. Neuropsychiatric Disease and Treatment 2019;15:1547-55. [DOI: 10.2147/NDT.S194022] [PMCID: PMC6559223] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gibbard 2018
- Gibbard CR, Ren J, Skuse DH, Clayden JD, Clark CA. Structural connectivity of the amygdala in young adults with autism spectrum disorder. Human Brain Mapping 2018;39(3):1270-82. [DOI: 10.1002/hbm.23915] [PMCID: PMC5838552] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Giovannitti 2015
- Giovannitti JA Jr, Thoms SM, Crawford JJ. Alpha-2 adrenergic receptor agonists: a review of current clinical applications. Anesthesia Progress 2015;62(1):31-9. [DOI: 10.2344/0003-3006-62.1.31] [PMCID: PMC4389556] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Glover 2015
- Glover G, Williams R, Branford D, Avery R, Chauhan U, Hoghton M. Prescribing of psychotropic drugs to people with learning disabilities and/or autism by general practitioners in England. Public Health England 2015.
Gottschalk 2017
- Gottschalk MG, Domschke K. Oxytocin and anxiety disorders. In: Hurelmann R, Grinevich V, editors(s). Behavioral Pharmacology of Neuropeptides: Oxytocin. Cham: Springer International Publishing, 2017:467-98. [DOI: 10.1007/7854_2017_25] [DOI] [Google Scholar]
GRADEpro GDT [Computer program]
- GRADEpro. 3.2 for Windows. Brozek J, Oxman A, Schünemann H, Version accessed 27 April 2022. Hamilton (ON): McMaster University (developed by Evidence Prime). Available at gradepro.org.
Green 2010
- Green JJ, Hollander E. Autism and oxytocin: new developments in translational approaches to therapeutics. Neurotherapeutics 2010;7(3):250-7. [DOI: 10.1016/j.nurt.2010.05.006] [PMCID: PMC5084228] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gualtieri 2002
- Gualtieri CT. Psychopharmacology of brain injured and mentally retarded patients. Philadelphia: Lippincott Williams and Wilkins, 2002. [Google Scholar]
Guglielmo 2013
- Guglielmo R, Ioime L, Grandinetti P, Janiri L. Managing disruptive and compulsive behaviors in adult with autistic disorder with gabapentin. Journal of Clinical Psychopharmacology 2013;33(2):273-4. [DOI: 10.1097/JCP.0b013e318285680c] [PMID: ] [DOI] [PubMed] [Google Scholar]
Guy 1976
- Guy W (editor). ECDEU Assessment Manual for Psychopharmacology. Rockville, MD, U.S.: Department of Health, Education, and Welfare, 1976. [Google Scholar]
Handen 2008
- Handen BL, Sahl R, Hardan AY. Guanfacine in children with autism and/or intellectual disabilities. Journal of Developmental and Behavioral Pediatrics 2008;29(4):303–8. [DOI: 10.1097/DBP.0b013e3181739b9d] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hanson 2013
- Hanson E, Cerban BM, Slater CM, Caccamo LM, Bacic J, Chan E. Brief report: prevalence of attention deficit/ hyperactivity disorder among individuals with an autism spectrum disorder. Journal of Autism and Developmental Disorders 2013;43(6):1459-64. [DOI: 10.1007/s10803-012-1677-7] [PMID: ] [DOI] [PubMed] [Google Scholar]
Henderson 2020
- Henderson A, Kinnear D, Fleming M, Stanley B, Greenlaw N, Young-Southward G, et al. Antipsychotic and antidepressant prescribing for 704 297 children and young people with and without intellectual disabilities: record linkage study. Brtish Journal of Psychiatry 2020;218(1):58-62. [DOI: 10.1192/bjp.2020.232] [PMID: ] [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Altman DG, Sterne JA editor(s). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. https://training.cochrane.org/handbook/archive/v5.1/.
Higgins 2012
- Higgins JP, Jackson D, Barrett JK, Lu G, Ades AE, White IR. Consistency and inconsistency in network meta-analysis: concepts and models for multi-arm studies. Research Synthesis Methods 2012;3(2):98–110. [DOI: 10.1002/jrsm.1044] [PMCID: PMC4433772] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2022a
- Higgins JP, Li T, Deeks JJ editor(s). Chapter 6: Choosing effect measures and computing estimates of effect. In: Higgins JP Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (updated February 2022). Cochrane, 2022. Available from www.training.cochrane.org/handbook.
Higgins 2022b
- Higgins JP, Eldridge S, Li T editor(s). Chapter 23: Including variants on randomized trials. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (updated February 2022). Cochrane, 2022. Available from training.cochrane.org/handbook.
Hill 2014
- Hill AP, Zuckerman KE, Hagen AD, Kriz DJ, Duvall SW, Van Santen J, et al. Aggressive behaviour problems in children with autism spectrum disorders: prevalence and correlates in a large clinical sample. Research in Autism Spectrum Disorders 2014;8(9):1121-33. [DOI: 10.1016/j.rasd.2014.05.006] [PMCID: PMC4160737] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hirsch 2016
- Hirsch LE, Pringsheim T. Aripiprazole for autism spectrum disorders (ASD). Cochrane Database of Systematic Reviews 2016, Issue 6. Art. No: CD009043. [DOI: 10.1002/14651858.CD009043.pub3] [PMCID: PMC7120220] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hollander 2001
- Hollander E, Dolgoff-Kaspar R, Cartwright C, Rawitt R, Novotny S. An open trial of divalproex sodium in autism spectrum disorders. Journal of Clinical Psychiatry 2001;62(7):530-4. [DOI: 10.4088/jcp.v62n07a05] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hollocks 2019
- Hollocks MJ, Lerh JW, Magiati I, Meiser-Stedman R, Brugha TS. Anxiety and depression in adults with autism spectrum disorder: a systematic review and meta-analysis. Psychological Medicine 2019;49(4):559-72. [DOI: 10.1017/S0033291718002283] [PMID: ] [DOI] [PubMed] [Google Scholar]
Holt 2019
- Holt RI. Association between antipsychotic medication use and diabetes. Current Diabetes Reports 2019;19(10):96. [DOI: 10.1007/s11892-019-1220-8] [PMCID: PMC6718373] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Houghton 2017
- Houghton R, Ong RC, Bolognani F. Psychiatric comorbidities and use of psychotropic medications in people with autism spectrum disorder in the United States. Autism Research 2017;10(12):2037-47. [DOI: 10.1002/aur.1848] [PMID: ] [DOI] [PubMed] [Google Scholar]
Howes 2018
- Howes OD, Rogdaki M, Findon JL, Wiches RH, Charman T, King BH, et al. Autism spectrum disorder: consensus guidelines on assessment, treatment and research from the British Association for Psychopharmacology. Journal of Psychopharmacology 2018;32(1):3-29. [DOI: 10.1177/0269881117741766] [PMCID: PMC5805024] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Howland 2015
- Howland RH. Buspirone: back to the future. Journal of Psychosocial Nursing and Mental Health Services 2015;53(11):21-4. [DOI: 10.3928/02793695-20151022-01] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hsia 2014
- Hsia Y, Wong AY, Murphy DG, Simonoff E, Buitelaar JK, Wong IC. Psychopharmacological prescriptions for people with autism spectrum disorder (ASD): a multinational study. Psychopharmacology 2014;231(6):999-1009. [DOI: 10.1007/s00213-013-3263-x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hurwitz 2012
- Hurwitz R, Blackmore R, Hazell P, Williams K, Woolfenden S. Tricyclic antidepressants for autism spectrum disorders (ASD) in children and adolescents. Cochrane Database of Systematic Reviews 2012, Issue 3. Art. No: CD008372. [DOI: 10.1002/14651858.CD008372.pub2] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Huss 2016
- Huss M, Chen W, Ludolph AG. Guanfacine extended release: a new pharmacological treatment option in Europe. Clinical Drug Investigation 2016;36(1):1-25. [DOI: 10.1007/s40261-015-0336-0] [PMCID: PMC4706844] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
ICD‐10 2004
- World Health Organization. ICD-10: International Classification of Diseases for Mortality and Morbidity Statistics. 10th edition. Geneva: World Health Organization, 2004. [Google Scholar]
Janak 2012
- Janak P, Scott Bowers M, Corbit L. Compound stimulus presentation and the norepinephrine reuptake inhibitor atomoxetine enhance long-term extinction of cocaine-seeking behavior. Neuropsychopharmacology 2012;37(4):975-85. [DOI: 10.1038/npp.2011.281] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jesner 2007
- Jesner OS, Aref-Adib M, Coren E. Risperidone for autism spectrum disorder. Cochrane Database of Systematic Reviews 2007, Issue 1. Art. No: CD005040. [DOI: 10.1002/14651858.CD005040.pub2] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
John 2021
- John S, Jaeggi AV. Oxytocin levels tend to be lower in autistic children: a meta-analysis of 31 studies. Autism 2021;25(8):2152-61. [DOI: 10.1177/13623613211034375] [PMID: ] [DOI] [PubMed] [Google Scholar]
Johnco 2015
- Johnco C, Storch EA. Anxiety in youth with autism spectrum disorders implications for treatment. Expert Review of Neurotherapeutics 2015;15(11):1343-52. [DOI: 10.1586/14737175.2015.1111762] [PMCID: PMC4886863] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kanne 2011
- Kanne SM, Mazurek MO. Aggression in children and adolescents with ASD: prevalence and risk factors. Journal of Autism and Developmental Disorders 2011;41(7):926-37. [DOI: 10.1007/s10803-010-1118-4] [PMID: ] [DOI] [PubMed] [Google Scholar]
King 2001
- King BH, Wright DM, Handen BL, Sikich L, Zimmerman AW, McMahon W, et al. Double-blind, placebo-controlled study of amantadine hydrochloride in the treatment of children with autistic disorder. Journal of the American Academy of Child and Adolescent Psychiatry 2001;40(6):658–65. [DOI: 10.1097/00004583-200106000-00010] [PMID: ] [DOI] [PubMed] [Google Scholar]
Koritsas 2015
- Koritsas S, Iacono T. Predictors of challenging behaviour in adults with intellectual disability. Advances in Mental Health and Intllectual Disabilities 2015;9(6):312-26. [DOI: 10.1108/AMHID-06-2015-0029] [DOI] [Google Scholar]
Krishnaswami 2011
- Krishnaswami S, McPheeters ML, Veenstra-Vanderweele J. A systematic review of secretin for children with autism spectrum disorders. Pediatrics 2011;127(5):e1322-5. [DOI: 10.1542/peds.2011-0428] [PMCID: PMC3387870] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kusmaker 2018
- Kusmaker S, Karmaker CK, Yan B, O'Brien TJ, Mathuganapathy R, Palaniswarmi M. Onset detection of epileptic seizures from acceloerometry signal. In: 40th Annual Internal Conference of the IEEE Engineering in Medicine and Biology Society (EMBC); 2018 Jul 18-12; Honolulu (HI), USA. 2018:1-4. [DOI: 10.1109/EMBC.2018.8513669] [DOI] [PubMed]
Lake 2017
- Lake JK, Denton D, Lunsky Y, Shui AM, Veenstra-VanderWheele J, Anagnostou E. Medical conditions and demographic, service and clinical factors associated with atypical antipsychotic medication use among children with an autism spectrum disorder. Journal of Autism and Developmental Disorders 2017;47(5):1391-402. [DOI: 10.1007/s10803-017-3058-8] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lee 2021
- Lee T-M, Lee K-M, Lee C-Y, Lee H-C, Tam K-W, Loh E-W. Effectiveness of N-acetylcysteine in autism spectrum disorders: a meta-analysis of randomized controlled trials. Australian and New Zealand Journal of Psychiatry 2021;55(2):196-206. [DOI: 10.1177/0004867420952540] [PMID: ] [DOI] [PubMed] [Google Scholar]
Loomes 2017
- Loomes R, Hull L, Mandy WP. What is the male-to-female ratio in autism spectrum disorder? A systematic review and meta-analysis. Journal of the American Academy of Child and Adolescent Psychiatry 2017;56(6):466-74. [DOI: 10.1016/j.jaac.2017.03.013] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lord 1994
- Lord C, Rutter M, Le Couteur A. Autism Diagnostic Interview Revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders 1994;24(5):659-85. [DOI: 10.1007/BF021172145] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lord 2000
- Lord C, Risi S, Lambrecht L, Cook EH Jr, Leventhal BL, DiLavore PC. Autism Diagnostic Interview Revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders 2000;30(3):205-23. [PMID: ] [PubMed] [Google Scholar]
Lord 2018
- Lord C, Elsabbagh M, Baird G, Veenstra-Vanderweele J. Autism Spectrum Disorder. Lancet 2018;392(10146):508-20. [DOI: 10.1016/S0140-6736(18)31129-2] [PMCID: PMC7398158] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Loy 2017
- Loy JH, Merry SN, Hetrick AE, Stasiak K. Atypical antipsychotics for disruptive behaviour disorders in children and youths. Cochrane Database of Systematic Reviews 2017, Issue 8. Art. No: CD008559. [DOI: 10.1002/14651858.CD008559.pub3] [PMCID: PMC6483473] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Madden 2017
- Madden JM, Lakoma MD, Lynch FL, Rusinak D, Owen-Smith AA, Coleman KJ, et al. Psychotropic medication use among insured children with autism spectrum disorder. Journal of Autism and Developmental Disorders 2017;47(1):144-54. [DOI: 10.1007/s10803-016-2946-7] [PMCID: PMC5328123] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Maneeton 2018a
- Maneeton N, Maneeton B, Putthisri S, Suttajit S, Likhitsathian S, Srisurapanont M. Aripiprazole in acute treatment of children and adolescents with autism spectrum disorder: a systematic review and meta-analysis. Neuropsychiatric Disease and Treatment 2018;14:3063-72. [PMCID: PMC6237245] [PMID: 10.2147/NDT.S174622] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Maneeton 2018b
- Maneeton N, Maneeton B, Putthisri S, Woottiluk P, Narkpongphun A, Srisurapanont M. Risperidone for children and adolescents with autism spectrum disorder: a systematic review. Neuropsychiatric Disease and Treatment 2018;14:1811-20. [DOI: 10.2147/NDT.S151802] [PMCID: PMC6045903] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mano‐Sousa 2021
- Mano-Sousa BJ, Pedrosa AM, Alves BC, Galduróz JC, Belo VS, Chaves VE, et al. Effects of risperidone in autistic children and young adults: a systematic review and meta-analysis. Current Neuropharmacology 2021;19(4):538-52. [DOI: 10.2174/1570159X18666200529151741] [PMCID: PMC8206457] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Marinho 2018
- Marinho V, Oliveira T, Rocha K, Robeiro J, Magalhães F, Bento T, et al. The dopaminergic system dynamic in the time perception: a review of the evidence. International Journal of Neuroscience 2018;128(3):262-82. [DOI: 10.1080/00207454.2017.1385614] [PMID: ] [DOI] [PubMed] [Google Scholar]
Matos 2022
- Matos MB, Bara TS, Cordiero ML. Autism spectrum disorder diagnoses: a comparison of countries with different income levels. Clinical Epidemiology December 2022;14:959-69. [DOI: 10.2147/CLEP.S373186] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Matson 2009
- Matson JL, Boisjoli JA. Restraint procedures and challenging behaviours in intellectual disability: an analysis of causative factors. Journal of Applied Research in Intellectual Disabilities 2009;22(2):111-7. [DOI: 10.1111/j.1468-3148.2008.00477.x] [DOI] [Google Scholar]
May 2017
- May T, Sciberras E, Brignell A, Williams K. Autism spectrum disorder: updated prevalence and comparison of two birth cohorts in a nationally representative Australian sample. BMJ Open 2017;7(5):e015549. [DOI: 10.1136/bmjopen-2016-015549] [PMCID: PMC5623420] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
May 2020
- May T, Brignell A, Williams K. Autism spectrum disorder prevalence in children aged 12-13 years from the Longitudinal Study of Australian Children. Autism Research 2020;13(5):821-7. [DOI: 10.1002/aur.2286] [PMID: ] [DOI] [PubMed] [Google Scholar]
McQueen 2002
- McQueen JM, Heck AM. Secretin for the treatment of autism. Annals of Pharmacotherapy 2002;36(2):305-11. [DOI: 10.1345/aph.19113] [PMID: ] [DOI] [PubMed] [Google Scholar]
McTiernan 2011
- McTiernan A, Leader G, Healy O, Mannion A. Analysis of risk factors and early predictors of challenging behavior for children with autism spectrum disorder. Research in Autism Spectrum Disorders 2011;5(3):1215-22. [DOI: 10.1016/j.rasd.2011.01.009] [DOI] [Google Scholar]
Mechler 2022
- Mechler K, Banaschewski T, Hohmann S, Häge A. Evidence-based pharmacological treatment options for ADHD in children and adolescents. Pharmacology & therapeutics 2022 ;230:107940. [DOI: 10.1016/j.pharmthera.2021.107940] [PMID: ] [DOI] [PubMed] [Google Scholar]
Mikami 2019
- Mikami AY, Miller M, Lerner MD. Social functioning in youth with attention-deficit/hyperactivity disorder and autism spectrum disorder: transdiagnostic commonalities and differences. Clinical Psychology Review 2019;68:54-70. [DOI: 10.1016/j.cpr.2018.12.005] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ming 2008
- Ming X, Gordon E, Kang N, Wagner GC. Use of clonidine in children with autism spectrum disorders. Brain & Development 2008;30(7):454–60. [DOI: 10.1016/j.braindev.2007.12.007] [PMID: ] [DOI] [PubMed] [Google Scholar]
Moerkerke 2021
- Moerkerke M, Peeters M, De Vries L, Daniels N, Steyaert J, Alaerts K, et al. Endogenous oxytocin levels in autism—a meta-analysis. Brain Sciences 2021;11(11):1545. [DOI: 10.3390/brainsci11111545] [PMCID: PMC8615844] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG, for the PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Murray 2014
- Murray ML, Hsia Y, Glaser K, Simonoff E, Murphy DG, Asherson PJ, et al. Pharmacological treatments prescribed to people with autism spectrum disorder (ASD) in primary health care. Psychopharmacology 2014;231(6):1011-21. [DOI: 10.1007/s00213-013-3140-7] [PMCID: PMC3932167] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Müller 2012
- Müller T. Drug therapy in patients with Parkinson’s disease. Translational Neurodegeneration 2012;1(1):10. [DOI: 10.1186/2047-9158-1-10] [PMCID: PMC3514092] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nadeau 2011
- Nadeau J, Sulkowski ML, Ung D, Wood JJ, Lewin AB, Murphy TK, et al. Treatment of comorbid anxiety and autism spectrum disorders. Neuropsychiatry 2011;1(6):567-78. [DOI: 10.2217/npy.11.62] [PMCID: PMC3809000] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nakamura 2010
- Nakamura K, Sekine Y, Ouchi Y, Tsujii M, Yoshikawa E, Futatsubashi M, et al. Brain serotonin and dopamine transporter bindings in adults with high-functioning autism. Archives of General Psychiatry 2010;67(1):59-68. [DOI: 10.1001/archgenpsychiatry.2009.137] [PMID: ] [DOI] [PubMed] [Google Scholar]
National Autistic Society 2023
- National Autistic Society. How to talk and write about autism. https://www.autism.org.uk/what-we-do/help-and-support/how-to-talk-about-autism.
NICE 2015
- National Institute for Health and Care Excellence. Challenging behaviour and learning disabilities: prevention and interventions for people with learning disabilities whose behaviour challenges. NICE guideline (NG11); May 2015. Available at www.nice.org.uk/guidance/ng11. [PubMed]
Olivares 2012
- Olivares D, Deshpande VK, Shi K, Lahiri DK, Greig NH, Rogers JT. N-Methyl D-Aspartate (NMDA) receptor antagonists and memantine treatment for Alzheimer's disease, vascular dementia, and Parkinson's disease. Current Alzheimer Research 2012;9(6):746-58. [DOI: 10.2174/156720512801322564] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ono 1996
- Ono Y. Factor validity and reliability for the Aberrant Behavior Checklist-Community in a Japanese population with mental retardation. Research in Developmental Disabilities 1996;17(4):303-09. [DOI: 10.1016/0891-4222(96)00015-7] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ooi 2017
- Ooi YP, Weng S-J, Kossowsky J, Gerger H, Sung M. Oxytocin and autism spectrum disorders: a systematic review and meta-analysis of randomized controlled trials. Pharmacopsychiatry 2017;50(1):5-13. [DOI: 10.1055/s-0042-109400] [PMID: ] [DOI] [PubMed] [Google Scholar]
Osland 2018
- Osland ST, Steeves TD, Pringsheim T. Pharmacological treatment for attention deficit hyperactivity disorder (ADHD) in children with comorbid tic disorders. Cochrane Database of Systematic Reviews 2018, Issue 6. Art. No: CD007990. [DOI: 10.1002/14651858.CD007990.pub3] [PMCID: PMC6513283] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Park 2022
- Park J-E, Leem Y-H, Park J-S, Kim D-Y, Kang J-L, Kim H-S. Anti-inflammatory and neuroprotective mechanisms of GTS-21, an α7 nicotinic acetylcholine receptor agonist, in neuroinflammation and Parkinson’s disease mouse models. International Journal of Molecular Sciences 2022;23(8):4420. [DOI: 10.3390/ijms23084420] [DOI] [PMC free article] [PubMed] [Google Scholar]
Patra 2019
- Patra S, Nebhinani N, Viswanathan A, Kirubakaran R. Atomoxetine for attention deficit hyperactivity disorder in children and adolescents with autism: a systematic review and meta-analysis. Autism Research 2019;12(4):542-52. [DOI: 10.1002/aur.2059] [PMID: ] [DOI] [PubMed] [Google Scholar]
Peiris 2022
- Peiris H, Wickramarachchi DS, Samarasinghe P, Vance P, Dahanayake D, Kulasekara V. Diagnosing autism in low-income countries: clinical record-based analysis in Sri Lanka. Autism Research 2022;15(7):1358-67. [DOI: 10.1002/aur.2765] [PMID: ] [DOI] [PubMed] [Google Scholar]
Perez 2012
- Perez M, Carlson G, Ziviani J, Cuskelly M. Contribution of occupational therapists in positive behaviour support. Australian Occupational Therapy Journal 2012;59(6):428-36. [DOI: 10.1111/j.1440-1630.2012.01036.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Poisbeau 2018
- Poisbeau P, Gazzo G, Calvel L. Anxiolytics targeting GABAA receptors: insights on etifoxine. World Journal of Biological Psychiatry 2018;19(Suppl 1):S36-S45. [DOI: 10.1080/15622975.2018.1468030] [PMID: ] [DOI] [PubMed] [Google Scholar]
Posey 2001
- Posey DJ, McDougle CJ. Pharmacotherapeutic management of autism. Expert Opinion on Pharmacotherapy 2001;2(4):587-600. [DOI: 10.1517/14656566.2.4.587] [PMID: ] [DOI] [PubMed] [Google Scholar]
Previc 2007
- Previc FH. Prenatal influences on brain dopamine and their relevance to the rising incidence of autism. Medical Hypotheses 2007;68(1):46-60. [DOI: 10.1016/j.mehy.2006.06.041] [PMID: ] [DOI] [PubMed] [Google Scholar]
Proix 2018
- Proix T, Jirsa VK, Bartolomei F, Guye M, Truccolo W. Predicting the spatiotemporal diversity of seizure propagation and termination in human focal epilepsy. Nature Communications 2018;9(1):1088. [DOI: 10.1038/s41467-018-02973-y] [PMCID: PMC5852068] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Qi 2020
- Qi X-R, Zhang L. The potential role of gut peptide hormones in autism spectrum disorder. Frontiers in Cellular Neuroscience 2020;14:73. [DOI: 10.3389/fncel.2020.00073] [PMCID: PMC7136424] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ramcharan 2009
- Ramcharan P, Nankervis K, Strong M, Robertson A. Experiences of restrictive practices: a view from people with disabilities and family carers. A final research report to the office of the Senior Practitioner; May 2009. Available at vgls.sdp.sirsidynix.net.au/client/search/asset/1297931 .
Rasmussen 2019
- Rasmussen L, Pratt N, Roughead E, Moffat A. Prevalence of psychotropic medicine use in Australian children with autism spectrum disorder: a drug utilization study based on children enrolled in the longitudinal study of Australian children. Journal of Autism and Developmental Disorders 2019;49(1):227-35. [DOI: 10.1007/s10803-018-3718-3] [PMID: ] [DOI] [PubMed] [Google Scholar]
RevMan Web 2021 [Computer program]
- Review Manager Web (RevMan Web). Version 3.13.0. The Cochrane Collaboration, 2021. Available at revman.cochrane.org.
Ricci 2013
- Ricci S, Businaro R, Ippoliti F, Lo Vasco VR, Massoni F, Onofri E, et al. Altered cytokine and BDNF levels in autism spectrum disorder. Neurotoxicity Research 2013;24(4):491-501. [DOI: 10.1007/s12640-013-9393-4] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ringer 2020
- Ringer N, Wilder J, Scheja M, Gustavsson A. Managing children with challenging behaviours. Parents' meaning-making processes in relation to their children's ADHD diagnosis. International journal of disability, development and education 2020;67(4):376-92. [DOI: 10.1080/1034912X.2019.1596228] [DOI] [Google Scholar]
Ritchie 2020
- Ritchie H. Neurodevelopmental disorders. www.ourworldindata.org/neurodevelopmental-disorders (accessed 27th April 2022).
Rojahn 2001
- Rojahn J, Matson J, Lott D, Esbensen AJ, Smalls Y. The behaviour problems inventory - an instrument for the assessment of self-injury, stereotyped behaviour, and aggression/destruction in individuals with developmental disabilities. Journal of Autism and Developmental Disorders 2001;31(6):577-88. [DOI: 10.1023/A:1013299028321] [PMID: ] [DOI] [PubMed] [Google Scholar]
Rojas 2014
- Rojas DC. The role of glutamate and its receptors in autism and the use of glutamate receptor antagonists in treatment. Journal of Neural Transmission 2014;121(8):891-905. [DOI: 10.1007/s00702-014-1216-0] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rosello 2018
- Rosello B, Berenguer C, Baixauli I, Colomer C, Miranda A. ADHD symptoms and learning behaviors in children with ASD without intellectual disability. A mediation analysis of executive functions. PloS one 2018;13(11):e0207286. [DOI: 10.1371/journal.pone.0207286] [PMCID: PMC6241124] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sabri 2008
- Sabri O, Kendziorra K, Wolf H, Gertz H-J, Brust P. Acetylcholine receptors in dementia and mild cognitive impairment. European Journal of Nuclear Medicine and Molecular Imaging 2008;35(Suppl 1):30-45. [DOI: 10.1007/s00259-007-0701-1] [PMID: ] [DOI] [PubMed] [Google Scholar]
Savović 2012
- Savović J, Jones H, Altman D, Harris R, Jűni P, Pildal J, et al. Influence of reported study design characteristics on intervention effect estimates from randomised controlled trials: combined analysis of meta-epidemiological studies. Health Technology Assessment 2012;16(35):1-82. [DOI: 10.3310/hta16350] [PMID: ] [DOI] [PubMed] [Google Scholar]
Schendel 2016
- Schendel DA, Overgaard M, Christensen J, Jorgensen M, Vestergaard M, Parner ET. Association of psychiatric and neurologic comorbidity with mortality among persons with autism spectrum disorder in a Danish population. JAMA Pediatrics 2016;170(3):243-50. [DOI: 10.1001/jamapediatrics.2015.3935] [PMID: ] [DOI] [PubMed] [Google Scholar]
Schmitt 2005
- Schmitt R, Gazalle FK, Lima MS, Cunha A, Souza J, Kapczinski F. The efficacy of antidepressants for generalized anxiety disorder: a systematic review and meta-analysis. Revista Brasileira de Psiquiatria 2005;27(1):18-24. [DOI: 10.1590/S1516-44462005000100007] [PMID: ] [DOI] [PubMed] [Google Scholar]
Schopler 2009
- Schopler E, Van Bourgondien ME, Wellman J, Love S. Childhood Autism Rating Scale-second edition (CARS2): Manual. Childhood Autism Rating Scale, Second Edition (CARS-2) | Pearson Clinical Australia & New Zealand 2009.
Schünemann 2013
- Schünemann H, Brożek J, Guyatt G, Oxman A, editor(s). Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach (updated October 2013). GRADE Working Group, 2013. Available from https://gdt.gradepro.org/app/handbook/handbook.html.
Schünemann 2022
- Schünemann HJ, Higgins JP, Vist GE, Glasziou P, Akl EA, Skoetz N, et al. Completing ‘Summary of findings’ tables and grading the certainty of the evidence. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (updated February 2022). Cochrane, 2022. Available from training.cochrane.org/handbook.
Seida 2009
- Seida JK, Ospina MB, Karkhaneh M, Hartling L, Smith V, Clark B. Systematic reviews of psychosocial interventions for autism: an umbrella review. Developmental Medicine and Child Neurology 2009;51(2):95-104. [DOI: 10.1111/j.1469-8749.2008.03211.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Sengupta 2017
- Sengupta K, Lobo L, Krishnamurthy V. Educational and behavioral interventions in management of autism spectrum disorder. Indian Journal of Pediatrics 2017;84(1):61-7. [DOI: 10.1007/s12098-015-1967-0] [PMID: ] [DOI] [PubMed] [Google Scholar]
Sheehan 2015
- Sheehan R, Hassiotis A, Walters K, Osborn D, Strydom A, Horsfall L. Mental illness, challenging behaviour, and psychotropic drug prescribing in people with intellectual disability: UK population based cohort study. BMJ 2015;351:h4326. [DOI: 10.1136/bmj.h4326] [PMCID: PMC4556752] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shojaie 2020
- Shojaie F. Quantum computations of interactions of most reactive tricyclic antidepressant drug with carbon nanotube, serotonin, and norepinephrin. Chemical Methodologies 2020;4(4):447-66. [DOI: 10.33945/SAMI/CHEMM.2020.4.7] [DOI] [Google Scholar]
SIGN 2016
- Scottish Intercollegiate Guidelines Network. SIGN145. Assessment, diagnosis and interventions for autism spectrum disorders: a national clinical guideline; June 2016. Available at www.sign.ac.uk/assets/sign145.pdf.
Simon 2015
- Simon G. ACP Journal Club: new use of atypical antipsychotics was linked to acute kidney injury and all-cause mortality at 90 days. Annals of Internal Medicine 2015;162(4):JC12. [DOI: 10.7326/ACPJC-2015-162-4-012] [PMID: ] [DOI] [PubMed] [Google Scholar]
Smith 2014
- Smith LE, Greenberg JS, Mailick MR. The family context of autism spectrum disorders: influence on the behavioral phenotype and quality of life. Child and Adolescent Psychiatric Clinics of North America 2014;23(1):143-55. [DOI: 10.1016/j.chc.2013.08.006] [PMCID: PMC3891371] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Soke 2016
- Soke GN, Rosenberg SA, Hamman RF, Fingerlin T, Robinson C, Carpenter L, et al. Brief report: prevalence of self-injurious behaviors among children with autism spectrum disorder—a population-based study. Journal of Autism and Developmental Disorders 2016;46(11):3607-14. [DOI: 10.1007/s10803-016-2879-1] [PMCID: PMC5392775] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sokolova 2017
- Sokolova E, Oerlemans AM, Rommelse NN, Groot P, Hartman CA, Glennon JC, et al. A causal and mediation analysis of the comorbidity between attention deficit hyperactivity disorder (ADHD) and autism spectrum disorder (ASD). Journal of Autism and Developmental Disorders 2017;47(6):1595-604. [DOI: 10.1007/s10803-017-3083-7] [PMCID: PMC5432632] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Stata 2013 [Computer program]
- Stata. Version 13. College Station, TX, USA: StataCorp , 2013. Available at www.stata.com.
Sturman 2017
- Sturman N, Deckx L, Van Driel ML. Methylphenidate for children and adolescents with autism spectrum disorder. Cochrane Database of Systematic Reviews 2017, Issue 11. Art. No: CD011144. [DOI: 10.1002/14651858.CD011144.pub2] [PMCID: PMC6486133] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tanaka 2018
- Tanaka A, Furubayashi T, Arai M, Inoue D, Kimura S, Kiriyama A, et al. Delivery of oxytocin to the brain for the treatment of autism spectrum disorder by nasal application. Molecular Pharmaceutics 2018;15(3):1105-11. [DOI: 10.1021/acs.molpharmaceut.7b00991] [PMID: ] [DOI] [PubMed] [Google Scholar]
Tantam 2012
- Tantam D. Autism Spectrum Disorders through the Life Span. Philadelphia (PA): Jessica Kingsley Publishers, 2012. [Google Scholar]
Taylor 2018
- Taylor JH, Schulte NA, French JA, Toews ML. Binding characteristics of two oxytocin variants and vasopressin at oxytocin receptors from four primate species with different social behaviour patterns. Journal of Pharmacology and Experimental Therapeutics 2018;367(1):101-7. [DOI: 10.1124/jpet.118.250852] [PMCID: PMC7250472] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Toohey 2017
- Toohey MJ, DiGiuseppe R. Defining and measuring irritability: construct clarification and differentiation. Clinical Psychology Review 2017;53:93-108. [DOI: 10.1016/j.cpr.2017.01.009] [PMID: ] [DOI] [PubMed] [Google Scholar]
Trifirò 2009
- Trifirò G, Spina E, Gambassi G. Use of antipsychotics in elderly patients with dementia: do atypical and conventional agents have a similar safety profile? Pharmacological Research 2009;59(1):1-12. [DOI: 10.1016/j.phrs.2008.09.017] [PMID: ] [DOI] [PubMed] [Google Scholar]
Tsouris 2013
- Tsouris JA, Kim S-Y, Brown WT, Pettinger J, Cohen IL. Prevalence of psychotropic drug use in adults with intellectual disability: positive and negative findings from a large scale study. Journal of Autism and Developmental Disorders 2013;43(3):719-31. [DOI: 10.1007/s10803-012-1617-6] [PMID: ] [DOI] [PubMed] [Google Scholar]
Turner 2012
- Turner RM, Davey J, Clarke MJ, Thompson SG, Higgins JP. Predicting the extent of heterogeneity in meta-analysis, using empirical data from the Cochrane Database of Systematic Reviews. International Journal of Epidemiology 2012;41(3):818-27. [DOI: 10.1093/ije/dys041] [PMCID: PMC3396310] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Turowetz 2015
- Turowetz J, Maynard DW. Category attribution as a device for diagnosis: fitting children to the autism spectrum. Sociology of Health & Illness 2015;38(4):610-26. [DOI: 10.1111/1467-9566.12382] [PMID: ] [DOI] [PubMed] [Google Scholar]
Tyrer 2006
- Tyrer F, McGrother CW, Thorp CF, Donaldson M, Bhaumik S, Watson JM, et al. Physical aggression towards others in adults with learning disabilities: prevalence and associated factors. Journal of Intellectual Disability Research 2006;50(4):295-304. [DOI: 10.1111/j.1365-2788.2005.00774.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ulke 2019
- Ulke C, Rullmann M, Huang J, Ludhardt J, Becker G-A, Patt M, et al. Adult attention-deficit/hyperactivity disorder is associated with reduced norepinephrine transporter availability in right attention networks: a (S,S)-O-[11C]methylreboxetine positron emission tomography study. Translational Psychiatry 2019;9(1):301. [DOI: 10.1038/s41398-019-0619-y] [PMCID: PMC6858438] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vallés 2021
- Vallés AS, Barrantes FJ. Dysregulation of neuronal nicotinic acetylcholine receptor - cholesterol crosstalk in autism spectrum disorder. Frontiers in Molecular Neuroscience 2021;14:744597. [DOI: 10.3389/fnmol.2021.744597] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Steensel 2011
- Van Steensel FJ, Bögels SM, Perrin S. Anxiety disorders in children and adolescents with autistic spectrum disorders: a meta-analysis. Clinical Child and Family Psychology Review 2011;14(3):302-17. [DOI: 10.1007/s10567-011-0097-0] [PMCID: PMC3162631] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Varni 1999
- Varni JW, Seid M, Rode CA. The PedsQL - measurement model for the pediatric quality of life inventory. Medical care 1999;37(2):126-39. [DOI: 10.1097/00005650-199902000-00003] [PMID: ] [DOI] [PubMed] [Google Scholar]
Varni 2001
Veenstra‐VanderWeele 2012
- Veenstra-VanderWeele J, Blakely RD. Networking in autism: leveraging genetic, biomarker, and model system findings in the search for new treatments. Neuropsychopharmacology 2012;37(1):196-212. [DOI: 10.1038/npp.2011.185] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Verrotti 2010
- Verrotti A, Coppola G, Parisi P, Mohn A, Chiarelli F. Bone and calcium metabolism and antiepileptic drugs. Clinical Neurology and Neurosurgery 2010;112(1):1-10. [DOI: 10.1016/j.clineuro.2009.10.011] [PMID: ] [DOI] [PubMed] [Google Scholar]
Vohra 2017
- Vohra R, Madhaven S, Sambamoorthi U. Comorbidity prevalence, healthcare utilization, and expenditures of Medicaid enrolled adults with autism spectrum disorders. Autism 2017;21(8):995-1009. [DOI: 10.1177/1362361316665222] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wassenaar 2013
- Wassenaar M, Van Heijl I, Leijten FS, Van der Linden P, Uijl SG, Egberts AC, et al. Treatment of epilepsy in daily clinical practice: have outcomes improved over the past 10 years?. Journal of Neurology 2013;260(11):2736-43. [DOI: 10.1007/s00415-013-7058-0] [PMID: ] [DOI] [PubMed] [Google Scholar]
Weitlauf 2014
- Weitlauf AS, McPheeters ML, Peters B, Sathe N, Travis R, Aiello R, et al. Therapies for Children with Autism Spectrum Disorder: Behavioral Interventions Update. Rockville (MD): Agency for Healthcare Research and Quality (US), 2014. [BOOKSHELF ID: NBK241444] [PMID: ] [PubMed] [Google Scholar]
Welch 2004
- Welch MG, Keune JD, Welch-Horan TB, Anwar N, Anwar M, Ludwig RJ, et al. Secretin: hypothalamic distribution and hypothesized neuroregulatory role in autism. Cellular and Molecular Neurobiology 2004;24(2):219-41. [DOI: 10.1023/B:CEMN.0000018618.59015.a2] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
White 2012
- White IR, Barrett JK, Jackson D, Higgins JP. Consistency and inconsistency in network meta-analysis: model estimation using multivariate meta-regression. Research Synthesis Methods 2012;3(2):111-25. [DOI: 10.1002/jrsm.1045] [PMCID: PMC4433771] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 1998
- World Health Organization. WHO Quality of Life user manual. file:///U:/Downloads/WHO_HIS_HSI_Rev.2012.03_eng%20(1).pdf 1998.
Wilczyński 2019
- Wilczyński KM, Zasada I, Siwiec A, Janas-Kozik M. Differences on oxytocin and vasopressin levels in individuals suffering from the autism spectrum disorders vs general population – a systematic review. Neuropsychiatric Disease and Treatment 2019;15:2613-20. [DOI: 10.2147/NDT.S207580] [PMCID: PMC6750159] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Williams 2012
- Williams K, Wray JA, Wheeler DM. Intravenous secretin for autism spectrum disorders (ASD). Cochrane Database of Systematic Reviews 2012, Issue 4. Art. No: CD003495. [DOI: 10.1002/14651858.CD003495.pub3] [PMCID: PMC7154585] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Williams 2013
- Williams K, Brignell A, Randall M, Silove N, Hazell P. Selective serotonin reuptake inhibitors (SSRIs) for autism spectrum disorders (ASD). Cochrane Database of Systematic Reviews 2013, Issue 8. Art. No: CD004677. [DOI: 10.1002/14651858.CD004677.pub3] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wlodarczyk 2012
- Wlodarczyk BJ, Palacios AM, George TM, Finnell RH. Antiepileptic drugs and pregnancy outcomes. American Journal of Medical Genetics. Part A 2012;158A(8):2071-90. [DOI: 10.1002/ajmg.a.35438] [PMCID: PMC3402584] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wu 2012
- Wu J, Xiao H, Sun H, Zou L, Zhu L-Q. Role of dopamine receptors in ADHD: a systematic meta-analysis. Molecular Neurobiology 2012;45(3):605-20. [DOI: 10.1007/s12035-012-8278-5] [PMID: ] [DOI] [PubMed] [Google Scholar]
Yamasue 2017
- Yamasue H, Domes G. Oxytocin and autism spectrum disorders. In: Hurlemann R, Grinevich V, editors(s). Behavioral Pharmacology of Neuropeptides: Oxytocin. Cham: Springer International Publishing, 2017:449-65. [DOI: 10.1007/7854_2017_24] [DOI] [Google Scholar]
Yoon 2020
- Yoon S, Kim YK. The role of the oxytocin system in anxiety disorders. In: Kim YK, editors(s). Anxiety Disorders: Rethinking and Understanding Recent Discoveries. Advances in Experimental Medicine and Biology. Vol. 1191. Singapore: Springer, 2020:103-20. [DOI: 10.1007/978-981-32-9705-07] [DOI] [PubMed] [Google Scholar]
Young 2002
- Young SN, Leyton M. The role of serotonin in human mood and social interaction: insight from altered tryptophan levels. Pharmacology, Biochemistry and Behavior 2002;71(4):857-65. [DOI: 10.1016/s0091-3057(01)00670-0] [PMID: ] [DOI] [PubMed] [Google Scholar]
Yudofsky 2003
- Yudofsky SC, Silver JM, Jackson W, Endicott J, Williams D. The Overt Aggression Scale for the objective rating of verbal and physical aggression. American Journal of Psychiatry 2003;143(1):35-9. [DOI: 10.1176/ajp.143.1.35] [DOI] [PubMed] [Google Scholar]
Zaboski 2018
- Zaboski BA, Storch EA. Comorbid autism spectrum disorder and anxiety disorders: a brief review. Future Neurology 2018;13(1):31-7. [DOI: 10.2217/fnl-2017-0030] [PMCID: PMC5772195] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zeidan 2022
- Zeidan J, Fombonne E, Scorah J, Ibrahim A, Durkin MS, Saxena S. Global prevalence of autism: a sysyematic review update. Autism Research February 2022;15(5):778-90. [DOI: 10.1002/aur.2696] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zivkovic 2019
- Zivkovic S, Koh CH, Kaza N, Jackson CA. Antipsychotic drug use and risk of stroke and myocardial infarction: a systematic review and meta-analysis. BMC Psychiatry 2019;19(1):189-203. [DOI: 10.1186/s12888-019-2177-5] [PMCID: PMC6585081] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Żmudzka 2018
- Żmudzka E, Sałaciak K, Sapa J, Pytka K. Serotonin receptors in depression and anxiety: insights from animal studies. Life Sciences 2018;210:106-24. [DOI: 10.1016/j.lfs.2018.08.050] [PMID: ] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Livingstone 2015
- Livingstone N, Macdonald G, Williams K, Caldwell DM, Baker LB, Hazell P. Pharmacological intervention for irritability, aggression, and self‐injury in Autism Spectrum Disorders (ASD). Cochrane Database of Systematic Reviews 2015, Issue 7. Art. No: CD011769. [DOI: 10.1002/14651858.CD011769] [DOI] [PMC free article] [PubMed] [Google Scholar]


