Abstract
Aims: Skipping breakfast is known as a cardiovascular disease (CVD) risk. Recently, eating and dietary patterns have been varied in many countries, however, the mechanisms of promoting CVD are still unclear. Our goal was to assess the effects of eating and dietary patterns on CVD risk factors, with a focus on lipid parameters including serum concentration of small dense low-density lipoprotein cholesterol (sdLDL-C).
Methods: Subjects consisted of 27,997 Japanese men and women, who had medical check-up. Lipid parameters including sdLDL-C levels in breakfast skippers were compared with those in breakfast eaters. Lipid parameters in staple foods skippers were also compared with those in staple foods eaters.
Results: Breakfast skippers had significantly (p<0.01) higher serum levels of median sdLDL-C than breakfast eaters in both genders (34.7 versus 32.0 mg/dL in men, 25.4 versus 24.9 mg/dL in women, respectively), and the same was true for sdLDL-C/LDL-C ratio (0.276 versus 0.260 in men, 0.218 versus 0.209 in women, respectively). Similarly, staple foods skippers had significantly higher sdLDL-C level than staple foods eaters in both genders (34.1 versus 31.6 mg/dL in men, 25.8 versus 24.7 mg/dL in women), and the same went for sdLDL-C/LDL-C ratio (0.278 versus 0.256 in men, 0.215 versus 0.208 mg/dL in women, respectively).
Conclusion: Our data indicate that both skipping breakfast and having meals without staple foods increase serum sdLDL-C concentration and cause unfavorable lipid profiles, and then may promote CVD. These finding provide evidence for the importance of having breakfast and meals with staple foods for preventing CVD.
Keywords: Breakfast skipper, Staple foods skipper, Dyslipidemia, Small dense LDL-C, Cardiovascular disease risk
See editorial vol. 30: 1313-1314
Introduction
Cardiovascular disease (CVD) is the leading cause of death in Japan and worldwide 1) . Diet is strongly associated with CVD. Recently, the American Heart Association (AHA) has issued statements on modification of irregular eating patterns such as skipping breakfast and poor dietary patterns such as unbalanced combination of foods 2 , 3) . The AHA statement declared that poor diet quality is strongly associated with elevated risk of CVD morbidity and mortality and irregular eating patterns appear less favorable for achieving a healthy cardiometabolic profile. The Japan Atherosclerosis Society has also recommended diet improvement for preventing CVD 4 , 5) . Currently over 20% of US adults do not eat breakfast, and breakfast consumption has declined in recent decades 3) . Similarly, according to the National Health and Nutrition Survey 2019, 15% of Japanese men and 10% of Japanese women are also breakfast skippers 6) . Although several studies have shown that skipping breakfast is associated with CVD, the mechanisms of promoting CVD are still unknown 3 , 7 - 10) .
The traditional Japanese diet consists of staple foods (e.g., rice, noodles, bread), main dishes (e.g., meat, fish, soy products, eggs), and side dishes (e.g., vegetables, mushrooms, seaweed). According to the Ministry of Agriculture, Forestry and Fisheries of Japan, Japanese dietary pattern means a nutritionally-balanced diet 11) . Some reports suggested that the Japanese diet pattern contributes to weight control and prevention of lifestyle diseases 11 - 13) . However, in recent years, low-carbohydrate diets have become prevalent as a method to reduce body weight 14 - 17) . Some people practice having meal without staple foods in order to demonstrate low-carbohydrate diets, however, they may also lose the good balance of the Japanese diet 11 , 13) .
Dyslipidemia is one of the major risk factors for CVD and associated with diet. The association between dyslipidemia and diet has been explained mostly via nutrients such as omega-3 polyunsaturated fatty acid or saturated fatty acid 18 - 23) . In contrast, the association between dyslipidemia and dietary and eating patterns is still unclear. Elevated levels of low-density lipoprotein cholesterol (LDL-C) has been known for developing CVD and stroke 24 - 26) . Especially, small dense LDL (sdLDL), a smaller and denser subfraction of LDL, has been known as more atherogenic lipoprotein particles, and serum sdLDL-cholesterol (sdLDL-C) concentration has been reported to be a more sensitive risk marker for CVD than serum LDL-C concentration 27 - 31) .
Therefore, we assessed the association of eating patterns such as skipping breakfast and dietary patterns such as having meal without staple foods with CVD risk factors with focus on lipid parameters including serum concentration of sdLDL-C.
Aims
Our aims in this investigation were to assess the association of eating and dietary patterns with lipid parameters in a large Japanese population study. We tested our main hypothesis that 1) lipid parameters are more favorable in breakfast eaters than those in breakfast skippers, and 2) lipid parameters are more favorable in staple foods eaters than those in staple foods skippers through this investigation.
Methods
The study population consisted of 27,997 men and women who received a medical examination at the health evaluation centers in Osaka, Japan, from April 2019 to March 2020. All subjects agreed to participate in this study and the study protocol had previously been approved by the Medical Research Ethics Committee of Tokyo Medical and Dental University, Tokyo, Japan (M2000-2209). If subjects who had more than once visit during the study period, data on only first visit was used for this study. Subjects on lipid lowering medication and those with missing data were excluded from the analysis. The data for eating and dietary patterns of participants were collected using the self-administered questionnaire, along with their lifestyle factors such as smoking, alcohol drinking and snacking habits. Daily nutrient intakes were estimated using data collected dietary record by the same method with the National Health and Nutrition Survey 6) .
Regarding eating patterns, subjects were divided into two groups: breakfast skippers (BS) or breakfast eaters (BE). BS consumed breakfast less than 6 times a week, while BE consumed breakfast almost every day. Characteristics and laboratory data including lipid parameters in BS were compared with those in BE. In addition, the relationship between the frequency of consuming breakfast and serum concentrations of sdLDL-C and sdLDL-C/LDL-C ratio was also observed. For this analysis, BS were divided into 3 subgroups by the frequency of consuming breakfast: rarely, once or twice a week, and 3-5 times a week.
Subjects who had three meals a day (breakfast-lunch-dinner) were extracted and divided into groups by dietary patterns: having meals with or without staple foods. Staple foods skippers (SS) had three meals a day, however, did not consume staple foods at every meal, while staple foods eaters (SE) consumed staple foods at every meal. Characteristics and laboratory data including lipid parameters in SS were compared with those in SE ( Fig.1 ) .
Fig.1.
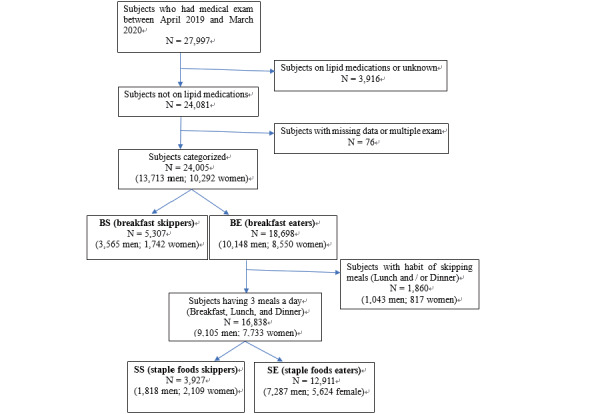
Flow diagram of subject selection and categorization
Since serum lipid levels change with age in both genders, and before and after menopause in women 5 , 22 , 24) , subjects were classified into two groups; younger group (<55 years old) and older group (≥ 55 years old) . Then data compared with BS and BE, SS and SE in younger group and in older group, separately.
Blood samples were collected from all subjects after an overnight fast. Serum creatinine, liver transaminases (ALT), total cholesterol (TC), triglycerides (TG), direct LDL-C, and high density lipoprotein cholesterol (HDL-C) were measured by automated standardized enzymatic analysis and sdLDL-C was measured using FDA cleared assay kit (Denka Co. Ltd) on TBX-FX8 instruments (Cannon Medical Systems, Japan) in the health evaluation centers 32 , 33) . All assays had within and between run coefficients of variation of <5.0%. Calculated LDL-C was derived using the Friedewald formula by subtracting the sum of HDL-C and TG/5 from TC 34) . Non HDL-C was calculated by subtracting HDL-C from TC.
Data are presented as median values with inter-quartile ranges (IQR) since some variables were not normally distributed. TG and sdLDL-C data were analyzed after log-transformation of values because these parameters are not normally distributed. Categorical variables are reported as frequencies and percentages. Analyses were performed by gender because of significant differences between men and women with regard to lipid and lipoprotein levels 28) . All statistical analyses were performed using SPSS software, version 23 (IBM, Armonk, NY). The t-test was used to compare continuous variables in two groups. One-way ANOVA was used for multiple comparisons. When a significant group effect was observed, the Turkey post-hoc analysis for equally distributed variables and the Games-Howell post-hoc analysis for non-equally distributed variables were performed. Chi-square test was used to compare categorical variables. Multivariate linear regression was performed to analyze the effect of lifestyle factors on serum levels of sdLDL-C and sdLDL-C/LDL-C ratio. P value <0.05 was considered to confer statistical significance.
Result
Since gender differences in lipid parameters have been noted, laboratory and clinical data are presented for men (n=13,713) and women (n=10,292), separately.
Breakfast Skippers versus Eaters
The percentages of BS were 26.0% in men and 16.9% in women. In both men and women, BS were younger than BE. In men, BS had significantly higher median levels of TG, direct LDL-C, and sdLDL-C than BE (103.0 versus 93.0 mg/dL, 124.0 versus 122.0 mg/dL, and 34.7 versus 32.0 mg/dL, respectively). The prevalence of diabetes in BS was significantly lower than BE. In women, BS had significantly higher median TG and sdLDL-C levels than BE (69.0 versus 66.0 mg/dL, 25.4 versus 24.9 mg/dL, respectively) ( Table 1 ) .
Table 1. Characteristics of subjects breakfast skippers or eaters.
| Male subjects | Female subjects | ||||||
|---|---|---|---|---|---|---|---|
|
BS n=3,565 |
BE n=10,148 |
P value |
BS n=1,742 |
BE n=8,550 |
P value | ||
| lipids | Age, year* | 47.0 (12.0) | 54.0 (16.0) | <0.001§ | 47.0 (13.0) | 52.0 (14.0) | <0.001§ |
| BMI, kg/m2* | 23.6 (4.0) | 23.3 (3.8) | <0.001§ | 21.3 (4.2) | 20.8 (3.8) | <0.001§ | |
| Waist circumference, cm* | 83.8 (11.0) | 83.3 (10.7) | 0.001§ | 76.0 (11.9) | 75.2 (11.5) | <0.001§ | |
| Albumin, g/dL* | 4.4 (0.3) | 4.3 (0.3) | <0.001§ | 4.2 (0.3) | 4.2 (0.3) | 0.382§ | |
| Creatinine, mg/dL* | 0.90 (0.16) | 0.92 (0.17) | <0.001§ | 0.67 (0.13) | 0.68 (0.13) | <0.001§ | |
| ALT, IU/L* | 22.0 (17.0) | 21.0 (13.0) | <0.001§ | 14.0 (8.0) | 15.0 (8.0) | 0.257§ | |
| Total cholesterol, mg/dl* | 200.0 (44.0) | 199.0 (41.0) | 0.016§ | 203.0 (46.0) | 207.0 (47.0) | 0.001§ | |
| Triglycerides, mg/dL*‡ | 103.0 (75.0) | 93.0 (67.0) | <0.001§ | 69.0 (44.0) | 66.0 (39.0) | <0.001§ | |
| Direct LDL-C, mg/dL* | 124.0 (42.0) | 122.0 (38.0) | <0.001§ | 117.0 (44.0) | 120.0 (40.3) | 0.060§ | |
| Calculated LDL-C, mg/dL* | 119.2 (41.2) | 119.6 (36.6) | 0.820§ | 118.0 (41.5) | 121.8 (41.0) | <0.001§ | |
| sdLDL-C, mg/dL*‡ | 34.7 (24.9) | 32.0 (21.9) | <0.001§ | 25.4 (13.9) | 24.9 (12.8) | 0.004§ | |
| sdLDL-C/LDL-C ratio *‡ | 0.276 (0.173) | 0.260 (0.148) | <0.001§ | 0.218 (0.084) | 0.209 (0.065) | <0.001§ | |
| nonHDL-C, mg/dL* | 144.0 (45.0) | 142.0 (41.0) | <0.001§ | 134.0 (46.0) | 137.0 (44.0) | 0.047§ | |
| HDL-C, mg/dL* | 54.0 (18.0) | 55.0 (18.0) | <0.001§ | 68.0 (20.0) | 69.0 (19.0) | <0.001§ | |
| Diabetes treatment, n (%)** | 97 (2.7%) | 465 (4.6%) | <0.001† | 9 (0.5%) | 66 (0.8%) | 0.254† | |
| Diabetes, n (%)** | 256 (7.2%) | 811 (8.0%) | 0.120† | 19 (1.1%) | 83 (1.0%) | 0.654† | |
| Hypertension treatment, n (%)** | 355 (10.0%) | 1701 (16.8%) | <0.001† | 81 (4.6%) | 627 (7.3%) | <0.001† | |
| Hypertension, n (%)** | 881 (24.7%) | 3012 (29.7%) | <0.001† | 211 (12.1%) | 1311 (15.3%) | 0.001† | |
| Smoker, n (%)** | 2,435 (68.3%) | 5,664 (55.8%) | <0.001† | 511 (29.3%) | 1,049 (12.3%) | <0.001† | |
| Drinker, n (%)** | 1,116 (31.3%) | 2,956 (29.1%) | 0.014† | 291 (16.7%) | 961 (11.2%) | <0.001† | |
| Snack eater, n (%)** | 453 (12.7%) | 2,019 (19.9%) | <0.001† | 719 (41.3%) | 4,543 (53.1%) | <0.001† | |
*Data are expressed as median (interquartile range). §Parameters were compared using T-test. P value <0.05 was considered statistically significant. ‡Variable was log-transformed prior to formal statistical analysis. **Data are expressed as number (percentage of) in cohort. † Parameters were compared using chi-square test. P value <0.05 was considered statistically significant.
“Diabetes” was defined as using anti-diabetic medication or having fasting blood glucose level >125 mg/dL. “Hypertension” was defined as using anti-hypertensive drugs or having systolic blood pressure >139 mmHg or diastolic blood pressure >89 mmHg. “Smoker” was defined as current
smokers and ex-smokers. “Drinker” was defined as consuming alcohol every day. “Snack eater” was defined as consuming snacks every day.
ALT, alanine aminotransferase; BMI, body mass index; BE, breakfast eaters; BS, breakfast skippers; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; sdLDL-C, small dense low-density lipoprotein cholesterol
Regarding the relationship between the frequency of having breakfast and median serum concentrations of sdLDL-C and sdLDL-C/LDL-C ratio, BE had significantly lower median levels of these parameters than any other group in male subjects. Median levels of these parameters were almost similar in the 3 BS subgroups. In female subjects, the difference of median serum levels of sdLDL-C was not significant among the 4 groups (BE and 3 BS subgroups), while BE had significantly lower median sdLDL-C/LDL-C ratio than any other group and the 3 BS subgroups had similar median values of this parameter ( Supplemental Table 1 and 2 ) .
Supplemental Table 1. The relationship between frequency of having breakfast and median serum concentrations of sdLDL-C in male subjects.
| Male Subjects | Frequency of having breakfast | P Value† | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
BE n=10,148 |
3-5/week n=1,228 |
1-2/week n=686 |
Rarely n=1,651 |
ANOVA P value§ |
BE vs 3-5/week | BE vs 1-2/week | BE vs Rarely | 3-5/week vs 1-2/ week | 3-5/week vs rarely | 1-2/week vs rarely | |
| sdLDL-C, mg/dL‡ |
32.0 (21.9) |
34.8 (24.4) |
34.1 (25.3) |
35.2 (25.4) |
<0.001 | <0.001 | 0.001 | <0.001 | 0.934 | 0.826 | 1.000 |
| sdLDL-C/LDL-C ratio‡ |
0.260 (0.148) |
0.275 (0.176) |
0.275 (0.170) |
0.277 (0.168) |
<0.001 | <0.001 | 0.007 | <0.001 | 1.000 | 1.000 | 1.000 |
Data are expressed as median (interquartile range).
§P value for comparison across the groups was determined by one-way analysis of variance. P value <0.05 was considered statistically significant.
†P value for comparison between individual groups, using Tukey post-hoc analysis for equally distributed variables and Games-Howell post-hoc analysis for non-equally distributed variables. P value <0.01 was considered statistically significant.
‡Variable was log-transformed prior to formal statistical analysis.
BE, breakfast eaters who consumed (had) breakfast almost every day; LDL-C, low-density lipoprotein cholesterol; Rarely, breakfast skippers who rarely consumed (had) breakfast; sdLDL-C, small dense low-density; lipoprotein cholesterol; 1-2/week, breakfast skippers who consumed (had) breakfast once or twice a week; 3-5/w, breakfast skippers who consumed (had) breakfast 3-5 times a week
Supplemental Table 2. The relationship between frequency of having breakfast and median serum concentrations of sdLDL-C in female subjects.
| Female Subjects | Frequency of having breakfast | P Value† | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
BE n=8,550 |
3-5/week n=797 |
1-2/week n=341 |
Rarely n=604 |
ANOVA P value§ |
BE vs 3-5/ week | BE vs 1-2/ week | BE vs Rarely | 3-5/week vs 1-2/ week | 3-5/week vs rarely | 1-2/week vs rarely | |
| sdLDL-C, mg/dL‡ |
24.9 (12.8) |
24.9 (14.2) |
26.8 (14.2) |
25.4 (13.7) |
0.010 | 0.097 | 0.056 | 0.816 | 0.361 | 0.652 | 0915 |
| sdLDL-C/LDL-C ratio‡ |
0.209 (0.065) |
0.215 (0.080) |
0.219 (0.083) |
0.220 (0.086) |
<0.001 | <0.001 | 0.034 | 0.001 | 0.996 | 0.732 | 0.932 |
Data are expressed as median (interquartile range).
§P value for comparison across the groups was determined by one-way analysis of variance. P value <0.05 was considered statistically significant.
†P value for comparison between individual groups, using Tukey post-hoc analysis for equally distributed variables and Games-Howell post-hoc analysis for non-equally distributed variables. P value <0.01 was considered statistically significant.
‡Variable was log-transformed prior to formal statistical analysis.
BE, breakfast eaters who consumed (had) breakfast almost every day; LDL-C, low-density lipoprotein cholesterol; Rarely, breakfast skippers who rarely consumed (had) breakfast; sdLDL-C, small dense low-density; lipoprotein cholesterol; 1-2/week, breakfast skippers who consumed (had) breakfast once or twice a week; 3-5/w, breakfast skippers who consumed (had) breakfast 3-5 times a week
Staple Foods Skippers versus Eaters
The percentages of SS were 20.0% in men and 27.3% in women. In both genders, SS had significantly higher median sdLDL-C than SE (34.1 versus 31.6 mg/dL in men, 25.8 versus 24.7 mg/dL in women, respectively). The prevalence of diabetes was significantly higher in SE than SS ( Table 2 ) .
Table 2. Characteristics of subjects staple foods skippers or eaters.
| Male subjects | Female subjects | ||||||
|---|---|---|---|---|---|---|---|
|
SS n=1,818 |
SE n=7,287 |
P value |
SS n=2,109 |
SE n=5,624 |
P value | ||
| lipids | Age, year* | 54.0 (14.0) | 54.0 (16.0) | 0.490§ | 53.0 (14.0) | 51.0 (15.0) | 0.001§ |
| BMI, kg/m2* | 23.4 (3.6) | 23.2 (3.7) | 0.006§ | 21.0 (3.6) | 20.7 (3.9) | 0.001§ | |
| Waist circumference, cm* | 83.7 (10.0) | 83.0 (10.7) | 0.007§ | 76.0 (11.1) | 75.0 (11.4) | 0.007§ | |
| Albumin, g/dL* | 4.3 (0.3) | 4.3 (0.3) | 0.161§ | 4.2 (0.3) | 4.2 (0.3) | 0.134§ | |
| Creatinine, mg/dL* | 0.92 (0.17) | 0.92 (0.17) | 0.097§ | 0.69 (0.13) | 0.68 (0.13) | 0.003§ | |
| ALT, IU/L* | 21.0 (12.0) | 21.0 (13.0) | 0.096§ | 15.0 (7.0) | 15.0 (8.0) | 0.634§ | |
| Total cholesterol, mg/dl* | 202.0 (40.0) | 198.0 (40.0) | <0.001§ | 209.0 (46.0) | 207.0 (46.0) | 0.004§ | |
| Triglycerides, mg/dL*‡ | 95.0 (71.0) | 93.0 (67.0) | 0.169§ | 66.0 (40.0) | 66.0 (39.0) | 0.757§ | |
| Direct LDL-C, mg/dL* | 122.0 (39.0) | 122.0 (37.0) | 0.810§ | 121.0 (42.0) | 120.0 (41.0) | 0.616§ | |
| Calculated LDL-C, mg/dL* | 120.0 (37.7) | 119.4 (36.0) | 0.589§ | 123.4 (39.6) | 121.8 (41.4) | 0.212§ | |
| sdLDL-C, mg/dL*‡ | 34.1 (22.7) | 31.6 (21.7) | <0.001§ | 25.8 (13.5) | 24.7 (12.6) | <0.001§ | |
| sdLDL-C/LDL-C ratio*‡ | 0.278 (0.158) | 0.256 (0.146) | <0.001§ | 0.215 (0.074) | 0.208 (0.064) | <0.001§ | |
| nonHDL-C, mg/dL* | 142.0 (40.0) | 141.0 (41.0) | 0.231§ | 138.0 (44.0) | 137.0 (45.8) | 0.185§ | |
| HDL-C, mg/dL* | 57.0 (18.0) | 55.0 (17.0) | <0.001§ | 70.0 (21.0) | 69.0 (19.0) | <0.001§ | |
| Diabetes treatment, n (%)** | 76 (4.2%) | 350 (4.8%) | 0.261† | 22 (1.0%) | 34 (0.6%) | 0.043† | |
| Diabetes, n (%)** | 153 (8.4%) | 576 (7.9%) | 0.472† | 28 (1.3%) | 48 (0.9%) | 0.060† | |
| Hypertension treatment, n (%)** | 347 (19.1%) | 1189 (16.3%) | 0.005† | 179 (8.5%) | 395 (7.0%) | 0.029† | |
| Hypertension, n (%)** | 611 (33.6%) | 2116 (29.0%) | <0.001† | 353 (16.7%) | 851 (15.1%) | 0.083† | |
| Smoker, n (%)** | 1,063 (58.5%) | 3,830 (52.6%) | <0.001† | 332 (15.7%) | 569 (10.1%) | <0.001† | |
| Drinker, n (%)** | 692 (38.1%) | 1,960 (26.9%) | <0.001† | 396 (18.8%) | 465 (8.3%) | <0.001† | |
| Snack eater, n (%)** | 301 (16.6%) | 1,550 (21.3%) | <0.001† | 1008 (47.8%) | 3,173 (56.4%) | <0.001† | |
*Data are expressed as median (interquartile range). §Parameters were compared using T-test. P value <0.05 was considered statistically significant. ‡Variable was log-transformed prior to formal statistical analysis. **Data are expressed as number (percentage of) in cohort. †Parameters were compared using chi-square test. P value <0.05 was considered statistically significant.
“Diabetes” was defined as using anti-diabetic medication or having fasting blood glucose level >125 mg/dL. “Hypertension” was defined as using anti-hypertensive drugs or having systolic blood pressure >139 mmHg or diastolic blood pressure >89 mmHg. “Smoker” was defined as current
smokers and ex-smokers. “Drinker” was defined as consuming alcohol every day. “Snack eater” was defined as consuming snacks every day.
ALT, alanine aminotransferase; BMI, body mass index; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; sdLDL-C, small dense low-density lipoprotein cholesterol; SE, staple foods eaters; SS, staple foods skippers
Daily nutrient intakes were estimated using data collected dietary record by the same method with the National Health and Nutrition Survey 6) , and they consumed 18-20% of energy from protein, 36-42% of energy from fat, and 38-46% of energy from carbohydrate.
Breakfast Skippers versus Eaters by Age Group
In men, the percentages of BS were 34.5% in the younger group (<55 y.o), and 13.5% in the older group. In both age groups, BS had significantly higher median TG than BE (103.0 versus 94.0 mg/dL in the younger group, 102.0 versus 93.0 mg/dL in the older group, respectively), and the same was true for sdLDL-C (34.1 versus 31.7 mg/dL in the younger group, 36.9 versus 32.1 mg/dL in the older group, respectively). In the younger group, BS had significantly higher median direct LDL-C than BE (123.0 versus 122.0 mg/dL, respectively) ( Table 3(A) ) .
Table 3. Characteristics of subjects breakfast skippers or eaters by age group.
| (A) Male Subjects | Younger <55 y.o | Older ≥ 55 y.o | |||||
|---|---|---|---|---|---|---|---|
|
BS n=2,812 |
BE n=5,328 |
P value |
BS n=753 |
BE n=4,820 |
P value | ||
| lipids | Age, year* | 45.0 (9.0) | 46.0 (9.0) | <0.001§ | 59.0 (6.5) | 62.0 (11.0) | <0.001§ |
| BMI, kg/m2* | 23.5 (4.0) | 23.4 (3.9) | 0.065§ | 23.7 (4.0) | 23.2 (3.6) | <0.001§ | |
| Waist circumference, cm* | 83.4 (11.1) | 82.9 (10.6) | 0.001§ | 85.1 (10.8) | 83.8 (10.1) | <0.001§ | |
| Albumin, g/dL* | 4.4 (0.3) | 4.4 (0.3) | 0.270§ | 4.3 (0.3) | 4.2 (0.3) | 0.648§ | |
| Creatinine, mg/dL* | 0.90 (0.16) | 0.92 (0.16) | 0.004§ | 0.90 (0.17) | 0.92 (0.18) | 0.009§ | |
| ALT, IU/L* | 23.0 (18.0) | 22.0 (15.0) | 0.001§ | 21.0 (14.0) | 20.0 (11.0) | <0.001§ | |
| Total cholesterol, mg/dl* | 199.0 (44.0) | 198.0 (41.0) | 0.003§ | 202.0 (42.0) | 200.0 (40.0) | 0.213§ | |
| Triglycerides, mg/dL*‡ | 103.0 (76.0) | 94.0 (73.0) | <0.001§ | 102.0 (73.0) | 93.0 (64.0) | <0.001§ | |
| Direct LDL-C, mg/dL* | 123.0 (43.0) | 122.0 (38.0) | 0.007§ | 124.0 (42.0) | 121.0 (37.0) | 0.173§ | |
| Calculated LDL-C, mg/dL* | 118.4 (41.0) | 118.6 (36.4) | 0.324§ | 121.2 (40.5) | 120.8 (36.4) | 0.728§ | |
| sdLDL-C, mg/dL* ‡ | 34.1 (24.9) | 31.7 (22.7) | <0.001§ | 36.9 (24.8) | 32.1 (21.2) | <0.001§ | |
| sdLDL-C/LDL-C ratio*‡ | 0.269 (0.169) | 0.255 (0.150) | <0.001§ | 0.301 (0.188) | 0.263 (0.145) | <0.001§ | |
| nonHDL-C, mg/dL* | 143.0 (45.0) | 141.0 (42.0) | <0.001§ | 145.0 (44.0) | 142.0 (40.0) | 0.100§ | |
| HDL-C, mg/dL* | 53.0 (17.0) | 54.0 (16.0) | 0.030§ | 55.0 (18.5) | 56.0 (18.0) | 0.370§ | |
| Diabetes treatment, n (%)** | 52 (1.8%) | 124 (2.3%) | 0.158† | 45 (6.0%) | 341 (7.1%) | 0.270† | |
| Diabetes, n (%)** | 145 (5.2%) | 238 (4.5%) | 0.162† | 111 (14.7%) | 573 (11.9%) | 0.026† | |
| Hypertension treatment, n (%)** | 171 (6.1%) | 393 (7.4%) | 0.029† | 184 (24.4%) | 1308 (27.1%) | 0.119† | |
| Hypertension, n (%)** | 550 (19.6%) | 966 (18.1%) | 0.115† | 331 (44.0%) | 2046 (42.4%) | 0.436† | |
| Smoker, n (%)** | 1,791 (63.7%) | 2,563 (48.1%) | <0.001† | 542 (72.0%) | 2,947 (61.1%) | <0.001† | |
| Drinker, n (%)** | 811 (28.8%) | 1,216 (22.8%) | <0.001† | 305 (40.5%) | 1,740 (36.1%) | 0.020† | |
| Snack eater, n (%)** | 355 (12.6%) | 1,001 (18.8%) | <0.001† | 98 (13.0%) | 1,018 (21.1%) | <0.001† | |
| (B) Female Subjects | Younger <55 y.o | Older ≥ 55 y.o | |||||
|
BS n=1,350 |
BE n=5,106 |
P value |
BS n=392 |
BE n=3,444 |
P value | ||
| lipids | Age, year* | 45.0 (9.0) | 46.0 (9.0) | <0.001§ | 59.0 (7.0) | 62.0 (10.0) | <0.001§ |
| BMI, kg/m2* | 21.2 (4.1) | 20.7 (3.7) | <0.001§ | 21.6 (4.6) | 21.0 (4.0) | <0.001§ | |
| Waist circumference, cm* | 75.4 (11.6) | 74.0 (10.8) | <0.001§ | 79.0 (12.8) | 77.0 (11.5) | <0.001§ | |
| Albumin, g/dL* | 4.3 (0.3) | 4.3 (0.3) | 0.931§ | 4.2 (0.3) | 4.2 (0.3) | 0.952§ | |
| Creatinine, mg/dL* | 0.67 (0.13) | 0.68 (0.12) | 0.001§ | 0.69 (0.12) | 0.70 (0.14) | 0.103§ | |
| ALT, IU/L* | 13.0 (7.0) | 14.0 (7.0) | 0.060§ | 17.0 (7.0) | 16.0 (8.0) | 0.441§ | |
| Total cholesterol, mg/dl* | 196.5 (43.0) | 196.0 (43.0) | 0.104§ | 224.0 (40.0) | 223.0 (40.0) | 0.405§ | |
| Triglycerides, mg/dL*‡ | 65.0 (42.0) | 61.0 (35.0) | <0.001§ | 81.0 (54.0) | 74.0 (42.0) | 0.002§ | |
| Direct LDL-C, mg/dL* | 113.0 (41.0) | 111.0 (40.0) | 0.083§ | 132.5 (39.0) | 131.0 (36.0) | 0.258§ | |
| Calculated LDL-C, mg/dL* | 112.9 (37.9) | 112.2 (38.4) | 0.417§ | 134.8 (40.1) | 135.0 (35.8) | 0.442§ | |
| sdLDL-C, mg/dL*‡ | 24.0 (12.7) | 22.7 (11.6) | <0.001§ | 30.7 (16.6) | 28.2 (13.3) | <0.001§ | |
| sdLDL-C/LDL-C ratio*‡ | 0.214 (0.080) | 0.204 (0.062) | <0.001§ | 0.228 (0.082) | 0.217 (0.068) | <0.001§ | |
| nonHDL-C, mg/dL* | 128.0 (43.0) | 126.0 (42.0) | 0.015§ | 153.5 (42.8) | 151.0 (39.0) | 0.078§ | |
| HDL-C, mg/dL* | 67.0 (20.0) | 68.0 (19.0) | 0.105§ | 69.5 (19.0) | 71.0 (20.0) | 0.037§ | |
| Diabetes treatment, n (%)** | 4 (0.3%) | 20 (0.4%) | 0.608† | 5 (1.3%) | 46 (1.3%) | 0.922† | |
| Diabetes, n (%)** | 11 (0.8%) | 28 (0.5%) | 0.261† | 8 (2.0%) | 55 (1.6%) | 0.512† | |
| Hypertension treatment, n (%)** | 34 (2.5%) | 142 (2.8%) | 0.598† | 56 (14.3%) | 472 (13.7%) | 0.326† | |
| Hypertension, n (%)** | 117 (8.7%) | 406 (8.0%) | 0.392† | 94 (24.0%) | 905 (26.3%) | 0.586† | |
| Smoker, n (%)** | 405 (30.0%) | 703 (13.8%) | <0.001† | 106 (27.0%) | 346 (10.0%) | <0.001† | |
| Drinker, n (%)** | 219 (16.2%) | 519 (10.2%) | <0.001† | 72 (18.4%) | 442 (12.8%) | 0.002† | |
| Snack eater, n (%)** | 584 (43.3%) | 2,861 (56.0%) | <0.001† | 135 (34.4%) | 1,682 (48.8%) | <0.001† | |
*Data are expressed as median (interquartile range). §Parameters were compared using T-test. P value <0.05 was considered statistically significant. ‡Variable was log-transformed prior to formal statistical analysis. **Data are expressed as number (percentage of) in cohort. † Parameters were compared using chi-square test. P value <0.05 was considered statistically significant.
“Diabetes” was defined as using anti-diabetic medication or having fasting blood glucose level >125 mg/dL. “Hypertension” was defined as using anti-hypertensive drugs or having systolic blood pressure >139 mmHg or diastolic blood pressure >89 mmHg. “Smoker” was defined as current
smokers and ex-smokers. “Drinker” was defined as consuming alcohol every day. “Snack eater” was defined as consuming snacks every day.
ALT, alanine aminotransferase; BMI, body mass index; BE, breakfast eaters; BS, breakfast skippers; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; sdLDL-C, small dense low-density lipoprotein cholesterol
In women, the percentages of BS were 20.9% in the younger group and 10.2% in the older group. BS had significantly higher median TG than BE (65.0 versus 61.0 mg/dL in the younger group, 81.0 versus 74.0 mg/dL in the older group, respectively), and the same went for sdLDL-C (24.0 versus 22.7 mg/dL in the younger group, 30.7 versus 28.2 mg/dL in the older group, respectively) ( Table 3(B) ) .
Staple Foods Skipper versus Eaters by Age Group
In men, the percentages of SS were 19.4% in the younger group, and 20.6% in the older group. In both age groups, SS had significantly higher median sdLDL-C than SE (33.7 versus 31.6 mg/dL in the younger group, 34.4 versus 31.5 mg/dL in the older group, respectively) ( Table 4(A) ) . In women, the percentages of SS were 25.9% in the younger group, 29.3% in the older group. In the older group, SS had significantly higher sdLDL-C than SE (29.4 versus 28.1 mg/dL, respectively) ( Table 4(B) ) .
Table 4. Characteristics of subjects staple foods skippers or eaters by age group.
| (A) Male Subjects | Younger <55 y.o | Older ≥ 55 y.o | |||||
|---|---|---|---|---|---|---|---|
|
SS n=912 |
SE n=3,793 |
P value |
SS n=906 |
SE n=3,494 |
P value | ||
| lipids | Age, year* | 47.0 (9.0) | 46.0 (9.0) | 0.004§ | 61.0 (10.0) | 63.0 (11.0) | <0.001§ |
| BMI, kg/m2* | 23.5 (3.7) | 23.4 (3.9) | 0.344§ | 23.4 (3.3) | 23.1 (3.5) | 0.001§ | |
| Waist circumference, cm* | 83.0 (11.0) | 82.8 (10.9) | 0.492§ | 84.0 (9.6) | 83.5 (10.3) | 0.002§ | |
| Albumin, g/dL* | 4.4 (0.3) | 4.4 (0.3) | 0.154§ | 4.3 (0.3) | 4.2 (0.3) | 0.145§ | |
| Creatinine, mg/dL* | 0.92 (0.16) | 0.92 (0.16) | 0.378§ | 0.92 (0.17) | 0.92 (0.18) | 0.144§ | |
| ALT, IU/L* | 22.0 (14.0) | 22.0 (15.0) | 0.024§ | 20.0 (10.0) | 19.0 (11.0) | 0.473§ | |
| Total cholesterol, mg/dl* | 199.0 (41.0) | 197.0 (40.0) | 0.006§ | 204.0 (39.3) | 199.0 (40.0) | 0.001§ | |
| Triglycerides, mg/dL*‡ | 93.0 (72.0) | 94.0 (74.0) | 0.829§ | 96.5 (68.3) | 92.0 (62.0) | 0.018§ | |
| Direct LDL-C, mg/dL* | 121.0 (40.0) | 122.0 (38.0) | 0.740§ | 122.0 (37.0) | 121.0 (37.0) | 0.962§ | |
| Calculated LDL-C, mg/dL* | 118.9 (38.4) | 118.4 (35.8) | 0.587§ | 121.5 (37.3) | 120.6 (35.8) | 0.880§ | |
| sdLDL-C, mg/dL* ‡ | 33.7 (23.4) | 31.6 (22.7) | 0.007§ | 34.4 (22.3) | 31.5 (20.6) | <0.001§ | |
| sdLDL-C/LDL-C ratio*‡ | 0.274 (0.158) | 0.253 (0.151) | <0.001§ | 0.283 (0.158) | 0.258 (0.141) | <0.001§ | |
| nonHDL-C, mg/dL* | 140.0 (42.3) | 141.0 (42.0) | 0.679§ | 144.0 (37.0) | 142.0 (41.0) | 0.188§ | |
| HDL-C, mg/dL* | 56.0 (17.0) | 54.0 (17.0) | <0.001§ | 58.0 (18.0) | 56.0 (18.0) | <0.001§ | |
| Diabetes treatment, n (%)** | 22 (2.4%) | 93 (2.5%) | 0.945† | 54 (6.0%) | 257 (7.4%) | 0.144† | |
| Diabetes, n (%)** | 50 (5.5%) | 161 (4.2%) | 0.105† | 103 (11.4%) | 415 (11.9%) | 0.672† | |
| Hypertension treatment, n (%)** | 78 (8.6%) | 268 (7.1%) | 0.122† | 269 (29.7%) | 921 (26.4%) | 0.044† | |
| Hypertension, n (%)** | 199 (21.8%) | 661 (17.4%) | 0.002† | 412 (45.5%) | 1455 (41.6%) | 0.038† | |
| Smoker, n (%)** | 465 (51.0%) | 1,761 (46.4%) | 0.013† | 598 (66.0%) | 2,069 (59.2%) | <0.001† | |
| Drinker, n (%)** | 290 (31.8%) | 778 (20.5%) | <0.001 | 402 (44.4%) | 1,182 (33.8%) | <0.001 | |
| Snack eater, n (%)** | 140 (15.4%) | 764 (20.1%) | 0.001 | 161 (17.8%) | 786 (22.5%) | 0.002 | |
| (B) Female Subjects | Younger <55 y.o | Older ≥ 55 y.o | |||||
|
SS n=1,188 |
SE n=3,404 |
P value |
SS n=921 |
SE n=2,220 |
P value | ||
| lipids | Age, year* | 47.0 (9.0) | 46.0 (9.0) | <0.001§ | 61.0 (10.0) | 62.0 (10.0) | <0.001§ |
| BMI, kg/m2* | 20.9 (3.6) | 20.6 (3.7) | 0.016§ | 21.2 (3.8) | 21.0 (4.0) | 0.043§ | |
| Waist circumference, cm* | 74.5 (10.6) | 74.0 (10.7) | 0.159§ | 77.2 (11.1) | 76.8 (11.9) | 0.061§ | |
| Albumin, g/dL* | 4.2 (0.3) | 4.3 (0.3) | 0.254§ | 4.2 (0.3) | 4.2 (0.3) | 0.487§ | |
| Creatinine, mg/dL* | 0.68 (0.13) | 0.67 (0.12) | <0.001§ | 0.70 (0.14) | 0.70 (0.14) | 0.964§ | |
| ALT, IU/L* | 14.0 (8.0) | 14.0 (8.0) | 0.275§ | 16.0 (7.0) | 17.0 (9.0) | 0.249§ | |
| Total cholesterol, mg/dl* | 197.5 (45.0) | 195.0 (44.0) | 0.065§ | 224.0 (42.0) | 223.5 (40.0) | 0.603§ | |
| Triglycerides, mg/dL*‡ | 61.0 (34.0) | 62.0 (35.0) | 0.322§ | 73.0 (44.0) | 75.0 (41.0) | 0.667§ | |
| Direct LDL-C, mg/dL* | 112.0 (41.0) | 111.0 (39.0) | 0.967§ | 131.0 (39.5) | 132.0 (36.0) | 0.375§ | |
| Calculated LDL-C, mg/dL* | 113.0 (38.4) | 112.0 (38.8) | 0.479§ | 134.2 (37.4) | 135.6 (35.6) | 0.486§ | |
| sdLDL-C, mg/dL*‡ | 23.3 (11.7) | 22.6 (11.5) | 0.053§ | 29.4 (15.1) | 28.1 (13.0) | 0.007§ | |
| sdLDL-C/LDL-C ratio* | 0.207 (0.066) | 0.204 (0.062) | 0.002§ | 0.224 (0.077) | 0.215 (0.064) | <0.001§ | |
| nonHDL-C, mg/dL* | 127.0 (42.0) | 126.0 (42.0) | 0.647§ | 151.0 (41.0) | 152.0 (38.0) | 0.729§ | |
| HDL-C, mg/dL* | 69.0 (19.0) | 68.0 (18.0) | 0.002§ | 72.0 (21.0) | 71.0 (20.0) | 0.082§ | |
| Diabetes treatment, n (%)** | 7 (0.6%) | 11 (0.3%) | 0.206 | 15 (1.6%) | 23 (1.0%) | 0.167 | |
| Diabetes, n (%)** | 11 (0.9%) | 13 (0.4%) | 0.025 | 17 (1.8%) | 35 (1.6%) | 0.590 | |
| Hypertension treatment, n (%)** | 39 (3.3%) | 89 (2.6%) | 0.228 | 140 (15.2%) | 306 (13.8%) | 0.300 | |
| Hypertension, n (%)** | 95 (8.0%) | 270 (7.9%) | 0.943 | 258 (28.0%) | 581 (26.2%) | 0.288 | |
| Smoker, n (%)** | 203 (17.1%) | 394 (11.6%) | <0.001 | 129 (14.0%) | 175 (7.9%) | <0.001 | |
| Drinker, n (%)** | 201 (16.9%) | 255 (7.5%) | <0.001 | 195 (21.2%) | 210 (9.5%) | <0.001 | |
| Snack eater, n (%)** | 614 (51.7%) | 2,013 (59.1%) | <0.001 | 394 (42.8%) | 1,160 (52.3%) | <0.001 | |
*Data are expressed as median (interquartile range). §Parameters were compared using T-test. P value <0.05 was considered statistically significant. Variable was log-transformed prior to formal statistical analysis. **Data are expressed as number (percentage of) in cohort. Parameters were compared using chi-square test. P value <0.05 was considered statistically significant.
“Diabetes” was defined as using anti-diabetic medication or having fasting blood glucose level >125 mg/dL. “Hypertension” was defined as using anti-hypertensive drugs or having systolic blood pressure >139 mmHg or diastolic blood pressure >89 mmHg. “Smoker” was defined as current
smokers and ex-smokers. “Drinker” was defined as consuming alcohol every day. “Snack eater” was defined as consuming snacks every day.
ALT, alanine aminotransferase; BMI, body mass index; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; sdLDL-C, small dense low-density lipoprotein cholesterol; SE, staple foods eaters; SS, staple foods skippers
Breakfast Skippers versus Eaters by Lifestyle
In men, BS had significantly higher median levels of sdLDL-C than BE, regardless of their lifestyle. In women, the same was true for only non-smokers, drinkers and non-snack eaters ( Table 5 ) . In female non-drinkers, BS were significantly younger than BE (mean age 47.4 versus 52.3 years, p<0.001)
Table 5. SdLDL-C levels and sdLDL-C/LDL-C ratio of subjects breakfast skippers or eaters by lifestyle.
| Male subjects | Female subjects | ||||||
|---|---|---|---|---|---|---|---|
| BS | BE | P value | BS | BE | P value | ||
| sdLDL-C, mg/dL*‡ | All | 34.7 (24.9) | 32.0 (21.9) | <0.001§ | 25.4 (13.9) | 24.9 (12.8) | 0.004§ |
| Smoker | 35.2 (25.4) | 33.5 (23.3) | <0.001§ | 25.3 (14.6) | 25.3 (13.8) | 0.455§ | |
| Non-smoker | 33.5 (24.7) | 30.4 (20.5) | <0.001§ | 25.5 (13.6) | 24.9 (12.6) | 0.016§ | |
| Drinker | 39.1 (26.3) | 35.6 (24.0) | <0.001§ | 30.3 (17.6) | 27.9 (14.9) | 0.001§ | |
| Non-drinker | 32.6 (23.6) | 30.6 (20.6) | <0.001§ | 24.4 (12.8) | 24.7 (12.4) | 0.158§ | |
| Snack eater | 31.0 (22.5) | 29.5 (19.3) | 0.025§ | 24.2 (12.3) | 24.5 (12.4) | 0.721§ | |
| Non-snack eater | 35.2 (25.2) | 32.6 (22.6) | <0.001§ | 26.4 (15.2) | 25.5 (13.2) | 0.001§ | |
| sdLDL-C/LDL-C ratio*‡ | All | 0.276 (0.173) | 0.260 (0.148) | <0.001§ | 0.218 (0.084) | 0.209 (0.065) | <0.001§ |
| Smoker | 0.284 (0.182) | 0.272 (0.161) | <0.001§ | 0.223 (0.102) | 0.218 (0.092) | 0.143§ | |
| Non-smoker | 0.262 (0.143) | 0.244 (0.130) | <0.001§ | 0.216 (0.077) | 0.2084 (0.063) | <0.001§ | |
| Drinker | 0.326 (0.197) | 0.304 (0.176) | <0.001§ | 0.284 (0.116) | 0.249 (0.095) | <0.001§ | |
| Non-drinker | 0.253 (0.151) | 0.244 (0.129) | <0.001§ | 0.208 (0.068) | 0.205 (0.061) | 0.010§ | |
| Snack eater | 0.237 (0.146) | 0.237 (0.121) | 0.115§ | 0.206 (0.066) | 0.205 (0.059) | 0.382§ | |
| Non-snack eater | 0.281 (0.176) | 0.266 (0.153) | <0.001§ | 0.227 (0.097) | 0.215 (0.073) | <0.001§ | |
*Data are expressed as median (interquartile range). §Parameters were compared using T-test. P value <0.05 was considered statistically significant. ‡Variable was log-transformed prior to formal statistical analysis.
BE, breakfast eaters; BS, breakfast skippers; LDL-C, low-density lipoprotein cholesterol; sdLDL-C, small dense low-density lipoprotein cholesterol
The multivariate analysis was performed, and data were adjusted for lifestyle factors such as smoking, drinking and snacking. In male subjects, median sdLDL-C levels and sdLDL-C/LDL-C ratio in BS were still significantly higher than those in BE. In contrast, in female subjects, BS had significantly higher median sdLDL-C/LDL-C ratio than BE, however, median sdLDL-C levels were not significantly different between BS and BE after being adjusted for the lifestyle factors (p=0.071).
Staple Foods Skippers versus Eaters by Lifestyle
In men, SS had significantly higher median levels of sdLDL-C than SE except for snack eaters. In women, SS in non-smokers, drinkers and non-snack eaters also has higher median levels of sdLDL-C than SE ( Table 6 ) . In female non-drinkers, SS and SE were similar age and their BMI levels were also similar.
Table 6. SdLDL-C levels and sdLDL-C/LDL-C ratio of subjects staple foods skippers or eaters by lifestyle.
| Male subjects | Female subjects | ||||||
|---|---|---|---|---|---|---|---|
| SS | SE | P value | SS | SE | P value | ||
| sdLDL-C, mg/dL*‡ | All | 34.1 (22.7) | 31.6 (21.7) | <0.001§ | 25.8 (13.5) | 24.7 (12.6) | <0.001§ |
| Smoker | 35.6 (24.7) | 33.0 (22.6) | <0.001§ | 25.8 (15.0) | 25.0 (13.8) | 0.137§ | |
| Non-smoker | 31.8 (20.4) | 30.2 (20.3) | 0.026§ | 25.8 (13.4) | 24.7 (12.5) | <0.001§ | |
| Drinker | 38.5 (24.9) | 34.5 (23.6) | <0.001§ | 28.6 (17.1) | 26.8 (13.9) | 0.002§ | |
| Non-drinker | 31.6 (20.9) | 30.4 (20.7) | 0.008§ | 25.3 (12.7) | 24.6 (12.5) | 0.092§ | |
| Snack eater | 29.6 (21.8) | 29.3 (18.5) | 0.108§ | 24.9 (12.3) | 24.4 (12.6) | 0.089§ | |
| Non-snack eater | 34.7 (22.8) | 32.2 (22.3) | <0.001§ | 26.5 (14.8) | 25.2 (12.8) | 0.001§ | |
| sdLDL-C/LDL-C ratio*‡ | All | 0.278 (0.158) | 0.256 (0.146) | <0.001§ | 0.215 (0.074) | 0.208 (0.064) | <0.001§ |
| Smoker | 0.294 (0.178) | 0.269 (0.157) | <0.001§ | 0.234 (0.102) | 0.214 (0.082) | 0.006§ | |
| Non-smoker | 0.261 (0.136) | 0.241 (0.129) | 0.001§ | 0.213 (0.067) | 0.208 (0.062) | <0.001§ | |
| Drinker | 0.329 (0.181) | 0.299 (0.171) | <0.001§ | 0.256 (0.097) | 0.246 (0.094) | 0.004§ | |
| Non-drinker | 0.253 (0.132) | 0.243 (0.130) | 0.014§ | 0.206 (0.063) | 0.206 (0.060) | 0.129§ | |
| Snack eater | 0.244 (0.125) | 0.236 (0.118) | 0.094§ | 0.205 (0.058) | 0.205 (0.059) | 0.214§ | |
| Non-snack eater | 0.286 (0.162) | 0.262 (0.151) | <0.001§ | 0.225 (0.084) | 0.213 (0.069) | <0.001§ | |
*Data are expressed as median (interquartile range). §Parameters were compared using T-test. P value <0.05 was considered statistically significant. ‡Variable was log-transformed prior to formal statistical analysis.
“Smoker” was defined as current smokers and ex-smokers. “Drinker” was defined as consuming alcohol every day. “Snack eater” was defined as consuming snacks every day.
LDL-C, low-density lipoprotein cholesterol; sdLDL-C, small dense low-density lipoprotein cholesterol; SE, staple foods eaters; SS, staple foods skippers
The multivariate analysis was performed, and data were adjusted for the lifestyle factors. In both male and female subjects, median sdLDL-C levels and sdLDL-C/LDL-C ratio in SS were still significantly higher than those in SE even after being adjusted for the lifestyle factors.
Discussion
The current study provided the first data regarding the association between sdLDL-C levels and eating patterns and dietary patterns. Overall our data confirmed that breakfast skippers had higher sdLDL-C levels than breakfast eaters, and staple foods skippers also had higher sdLDL-C levels than staple foods eaters.
Our study showed that BS had higher levels of TG and sdLDL-C, and sdLDL-C/LDL-C ratio than BE in both men and women. And in only male subjects, BS had significantly higher LDL-C levels than BE. Some previous studies also reported on the association between breakfast skipping and serum lipid levels, however, they were small size, single gender or limited age of the subjects 7 - 9) . A report from South Korea showed that low frequency of having breakfast lead to increases in TC, LDL-C, and TG levels in men, but no statistically significant difference in any lipid parameter was observed in women 35) . Our current large-scale study clearly showed that BS had unfavorable lipid parameters including higher sdLDL-C levels in both gender and all ages in Japanese population. Moreover, our data showed that BE had more favorable sdLDL-C levels and sdLDL-C/LDL-C ratio than BS, and these values were identical among BS subgroups, regardless of frequency of having breakfast. These data may suggest that having breakfast almost every day is important to keep lipid parameters favorable and prevent CVD.
Previous studies reported that breakfast skipping lead to weight gain and decreased muscle weight due to circadian disorders, relatively unfavorable nutritional balance, decreasing physical activity, and poor quality of sleep 36 - 39) . Another previous study showed that poor sleep quality associated with higher sdLDL-C 40) . These data explains the mechanistic link between breakfast skipping and unfavorable lipid profiles. In addition to these data, the current study provided valuable data explaining how breakfast skipping promote CVD, that is, via developing atherogenic lipid profiles.
In our study, the prevalence of BS was 26.0% in men and 16.9% in women, that was clearly higher than data in the National Health and Nutrition Survey. Since definition of breakfast skipping was different between the studies, these data cannot be simply compared.
According to some previous reports, younger people tend to have irregular eating patterns 3 , 6 , 41) . A Japanese survey reported that half of breakfast skippers continued breakfast skipping since their young age (~ 20s) 41 , 42) . Since previous studies showed that improvement of eating pattern from a young age can prevent future morbidity, everyone should keep good eating pattern from childhood 43 , 44) .
SS had higher levels of sdLDL-C and sdLDL-C/LDL-C ratio than SE, in men and postmenopausal women. In recent years, skipping staple foods diet has been prevalent. SS tends to replace staple foods with other foods such as meat, fish, or soy products in Japan. Using the dairy nutrient intake estimation, our data showed that SS consumed 38-46% of energy from carbohydrate, and 36-42% of energy from fat. These dietary patterns resulted in low-carbohydrate and high-fat diet 6 , 15) . Some reports showed that consuming low-carbohydrate diets is a dietary method that leads to weight loss in a short period 45 , 46) . However, most of the subjects in these reports were obese 14 , 15 , 45) . In contrast, some studies reported that a high-fat diet changes gut microbiota, increases appetite, cause insulin resistance and unfavorable lipid profiles, and then promote CVD 47 - 49) .
The traditional Japanese diet is three meals a day, breakfast-lunch-dinner pattern, and every meal consists of staple foods, main dishes and side dishes. It is known as the nutritionally balanced diet. According to the results of the National Health and Nutrition Survey, the average energy intake of Japanese adults was 1915 kcal/day and their protein % of energy was 16%, fat % of energy was 30%, and carbohydrate % of energy was 54% 6) . Those who had the traditional Japanese diet had lower rates of obesity, hyperlipidemia (high LDL-C), heart disease, and all-cause mortality 11 - 13) . In contrast, a large long-term cohort study in the US reported that low (<45%) percentage of energy from carbohydrates was associated with increased mortality 50) . And they described that 50-55% of energy from carbohydrate associated with the minimum risk for mortality. Overall these data suggested that the traditional Japanese diet and Japanese dietary pattern contribute to the prevention of CVD and lowering risk for mortality.
One of the strengths of our study was quite large number of subjects approximately 28,000. In addition, no previous reports exist on the relationship between sdLDL-C and eating and dietary patterns in worldwide. Since all subjects were Japanese, a single ethnic group, the data were not influenced by race.
In contrast, our study had several limitations. First, this study was the cross-sectional study design. Although long-term intervention studies of 10 years or longer are desirable to confirm the effects of dietary changes on lipid parameters, such intervention is not realistic. Second, the dietary pattern, staple foods, main dishes, and side dishes, is common only in Asian regions including Japan. Therefore, staple foods skipping may be recognized as a local problem. However the dietary pattern of staple foods skipping resulted in a low-carbohydrate and high-fat diet. Therefore, our data on staple foods skipping can be generalized as the risk of low-carbohydrate diets for CVD. Third, since the data were collected only in Japan. The result might be different in other ethnic group. In addition, our data were based on self-reported questionnaires at a yearly medical examination, and limited data were available on lifestyle factors. We used available information as much as we could. However, some of our findings could not be fully explained because of lack of enough information. For example, in female non-drinkers, median levels of sdLDL-C and sdLDL-C/LDL-C ratio in BS and BE were similar, that was unexpected. One of the possible explanations is the fact that BS were significantly younger than BE. Similarly, median levels of sdLDL-C and sdLDL-C/LDL-C ratio in SS and SE were identical in female non-drinkers, that was also unexpected. In this comparison, their age and BMI levels were also similar, and no appropriate data were available for explaining the reasons and/or mechanisms. More information and further analysis are needed to clarify these issues. Other lifestyle factors such like exercise habits may be confounders.
Overall, our data confirmed that 1) lipid parameters are more favorable in breakfast eaters than those in breakfast skippers, and 2) lipid parameters are more favorable in staple foods eaters than those in staple foods skippers. Our findings clarified the importance and benefit of consuming three meals a day and having a set of staple foods, main dishes and side dishes, the Japanese traditional diet.
Conclusion
Our data indicate that both breakfast skipping and staple foods skipping increase serum sdLDL-C concentration and cause unfavorable lipid profiles. Our study reconfirmed that the importance of consuming three meals a day and having a good balanced diet for preventing CVD.
Acknowledgements and Notice of Grant Support
The contribution of all subjects in this study is gratefully appreciated.
We thank Mr. Tomoaki Yamada of Tokyo Medical and Dental University for his advice on statistical analysis.
This study was supported by the university research fund (No.32782) and the research grant (No.2A232) from Denka Co., Ltd., Tokyo, Japan to M.Ai.
Conflict of Interests
YI is an employee of Denka Co., Ltd, M.Ai is supported by a research grant from Denka Co., Ltd., Tokyo, Japan. All other authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions
M.Arimoto and M.Ai designed and conducted the study. Y.Y, W.I, T.K and R.T recruited study subjects and collected data. M.Arimoto and M.Ai wrote the manuscript and MN and YI revised it. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
References
- 1).WHO, Mortality and global health estimates https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates?msclkid=09ea8b83c21f11eca4ba955c74e0696f (accessed 18th Aplil 2022) [Google Scholar]
- 2).Alice H Lichtenstein, Lawrence J Appel, Maya Vadiveloo, Frank B Hu, Penny M Kris-Etherton, Casey M Rebholz, Frank M Sacks, Anne N Thorndike, Linda Van Horn, Judith Wylie-Rosett: 2021 Dietary Guidance to Improve Cardiovascular Health: A Scientific Statement From the American Heart Association. Circulation, 2021; 144: e472-e487 [DOI] [PubMed] [Google Scholar]
- 3).St-Onge MP, Ard J, Baskin ML, Chiuve SE, Johnson HM, Kris-Etherton P, Varady K; American Heart Association Obesity Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular Disease in the Young; Council on Clinical Cardiology; and Stroke Council: Meal Timing and Frequency: Implications for Cardiovascular Disease Prevention: A Scientific Statement From the American Heart Association. Circulation, 2017; 135: e96-e121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4).Fujioka Y: Diet therapy in Japan Atherosclerosis Society(JAS) Guidelines for Preventing Atherosclerotic Cardiovascular Disease 2017. J Jpn Coron Assoc, 2018; 24: 20-25 [Google Scholar]
- 5).Japan Atherosclerosis Society: Japan Atherosclerosis Society (JAS) Guidelines for prevention of Atherosclerosis Cardiovascular Diseases 2022, 2022 [Google Scholar]
- 6).Ministry of Health, Labour and Welfare: The National Health and Nutrition Survey reports 2019. https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/kenkou_iryou/kenkou/eiyou/r1-houkoku_00002.html (accessed 18th Aplil 2022) [Google Scholar]
- 7).Kaneko H, Itoh H, Kiriyama H, Kamon T, Fujiu K, Morita K, Michihata N, Jo T, Takeda N, Morita H, Yasunaga H, Komuro I: Possible association between eating behaviors and cardiovascular disease in the general population: Analysis of a nationwide epidemiological database. Atherosclerosis, 2021; 320: 79-85 [DOI] [PubMed] [Google Scholar]
- 8).Farshchi HR, Taylor MA, Macdonald IA: Deleterious effects of omitting breakfast on insulin sensitivity and fasting lipid profiles in healthy lean women. Am J Clin Nutr, 2005; 81: 388-396 [DOI] [PubMed] [Google Scholar]
- 9).Cahill LE, Chiuve SE, Mekary RA, Jensen MK, Flint AJ, Hu FB, Rimm EB: Prospective study of breakfast eating and incident coronary heart disease in a cohort of male US health professionals. Circulation, 2013; 128: 337-343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10).Kubota Y, Iso H, Sawada N, Tsugane S: Association of Breakfast Intake With Incident Stroke and Coronary Heart Disease: The Japan Public Health Center-Based Study. Stroke, 2016; 47: 477-481 [DOI] [PubMed] [Google Scholar]
- 11).Ministry of Agriculture, Forestry and Fisheries: Traditional Dietary Cultures of the Japanese. https://www.maff.go.jp/e/data/publish/attach/pdf/index-20.pdf (Access 11th April 2022) [Google Scholar]
- 12).Ueshima H, Okayama A, Saitoh S, Nakagawa H, Rodriguez B, Sakata K, Okuda N, Choudhury SR, Curb JD: Differences in cardiovascular disease risk factors between Japanese in Japan and Japanese-Americans in Hawaii: the INTERLIPID study. J Hum Hypertens, 2003; 17: 631-639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13).Kurotani K, Akter S, Kashino I, Goto A, Mizoue T, Noda M, Sasazuki S, Sawada N, Tsugane S: Quality of diet and mortality among Japanese men and women: Japan Public Health Center based prospective study. BMJ, 2016; 22; 352: i1209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14).Shai I, Schwarzfuchs D, Henkin Y, Shahar DR, Witkow S, Greenberg I, Golan R, Fraser D, Bolotin A, Vardi H, Tangi-Rozental O, Zuk-Ramot R, Sarusi B, Brickner D, Schwartz Z, Sheiner E, Marko R, Katorza E, Thiery J, Fiedler GM, Blüher M, Stumvoll M, Stampfer MJ: Dietary Intervention Randomized Controlled Trial (DIRECT) Group. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N Engl J Med, 2008; 359: 229-241 [DOI] [PubMed] [Google Scholar]
- 15).Stern L, Iqbal N, Seshadri P, Chicano KL, Daily DA, McGrory J, Williams M, Gracely EJ, Samaha FF: The effects of low-carbohydrate versus conventional weight loss diets in severely obese adults: one-year follow-up of a randomized trial. Ann Intern Med, 2004; 140: 778-785 [DOI] [PubMed] [Google Scholar]
- 16).Ajala O, English P, Pinkney J: Systematic review and meta-analysis of different dietary approaches to the management of type 2 diabetes. Am J Clin Nutr, 2013; 97: 505-516 [DOI] [PubMed] [Google Scholar]
- 17).Santos FL, Esteves SS, da Costa Pereira A, Yancy WS Jr, Nunes JP: Systematic review and meta-analysis of clinical trials of the effects of low carbohydrate diets on cardiovascular risk factors. Obes Rev, 2012; 13: 1048-1066 [DOI] [PubMed] [Google Scholar]
- 18).Leslie MA, Cohen DJ, Liddle DM, Robinson LE, Ma DW: A review of the effect of omega-3 polyunsaturated fatty acids on blood triacylglycerol levels in normolipidemic and borderline hyperlipidemic individuals. Lipids Health Dis, 2015; 14: 53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19).Eslick GD, Howe PR, Smith C, Priest R, Bensoussan A: Benefits of fish oil supplementation in hyperlipidemia: a systematic review and meta-analysis. Int J Cardiol, 2009; 136: 4-16 [DOI] [PubMed] [Google Scholar]
- 20).Balk EM, Lichtenstein AH, Chung M, Kupelnick B, Chew P, Lau J: Effects of omega-3 fatty acids on serum markers of cardiovascular disease risk: a systematic review. Atherosclerosis, 2006; 189: 19-30 [DOI] [PubMed] [Google Scholar]
- 21).Agren JJ, Hänninen O, Julkunen A, Fogelholm L, Vidgren H, Schwab U, Pynnönen O, Uusitupa M: Fish diet, fish oil and docosahexaenoic acid rich oil lower fasting and postprandial plasma lipid levels. Eur J Clin Nutr, 1996; 50: 765-771 [PubMed] [Google Scholar]
- 22).Nakamura Y, Okuda N, Turin TC, Fujiyoshi A, Okamura T, Hayakawa T, Yoshita K, Miura K, Ueshima H: Fatty acids intakes and serum lipid profiles: NIPPON DATA90 and the national nutrition monitoring. J Epidemiol, 2010; 20 Suppl 3: S544-S548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23).Bergeron N, Chiu S, Williams PT, M King S, Krauss RM: Effects of red meat, white meat, and nonmeat protein sources on atherogenic lipoprotein measures in the context of low compared with high saturated fat intake: a randomized controlled trial. Am J Clin Nutr, 2019; 110: 24-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24).Imamura T, Doi Y, Arima H, Yonemoto K, Hata J, Kubo M, Tanizaki Y, Ibayashi S, Iida M, Kiyohara Y: LDL cholesterol and the development of stroke subtypes and coronary heart disease in a general Japanese population: the Hisayama study. Stroke, 2009; 40: 382-388 [DOI] [PubMed] [Google Scholar]
- 25).Imano H, Noda H, Kitamura A, Sato S, Kiyama M, Sankai T, Ohira T, Nakamura M, Yamagishi K, Ikeda A, Shimamoto T, Iso H: Low-density lipoprotein cholesterol and risk of coronary heart disease among Japanese men and women: the Circulatory Risk in Communities Study (CIRCS). Prev Med, 2011; 52: 381-386 [DOI] [PubMed] [Google Scholar]
- 26).Kaneko H, Itoh H, Kiriyama H, Kamon T, Fujiu K, Morita K, Michihata N, Jo T, Takeda N, Morita H, Yasunaga H, Komuro I: Lipid Profile and Subsequent Cardiovascular Disease among Young Adults Aged <50 Years. Am J Cardiol, 2021; 142: 59-65 [DOI] [PubMed] [Google Scholar]
- 27).Ito Y, Fujimura M, Ohta M, Hirano T: Development of a homogeneous assay for measurement of small dense LDL cholesterol. Clin Chem, 2011; 57: 57-65 [DOI] [PubMed] [Google Scholar]
- 28).Ai M, Otokozawa S, Asztalos BF, Ito Y, Nakajima K, White CC, Cupples LA, Wilson PW, Schaefer EJ: Small dense LDL cholesterol and coronary heart disease: results from the Framingham Offspring Study. Clin Chem, 2010; 56: 967-976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29).Koba S, Hirano T, Ito Y, Tsunoda F, Yokota Y, Ban Y, Iso Y, Suzuki H, Katagiri T: Significance of small dense low-density lipoprotein-cholesterol concentrations in relation to the severity of coronary heart diseases. Atherosclerosis, 2006; 189: 206-214 [DOI] [PubMed] [Google Scholar]
- 30).Hoogeveen RC, Gaubatz JW, Sun W, Dodge RC, Crosby JR, Jiang J, Couper D, Virani SS, Kathiresan S, Boerwinkle E, Ballantyne CM: Small dense low-density lipoprotein-cholesterol concentrations predict risk for coronary heart disease: the Atherosclerosis Risk In Communities (ARIC) study. Arterioscler Thromb Vasc Biol, 2014; 34: 1069-1077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31).Hirano T, Kodera R, Hirashima T, Suzuki N, Aoki E, Hosoya M, Oshima T, Hayashi T, Koba S, Ohta M, Satoh N, Ito Y: Metabolic Properties of Lowdensity Lipoprotein (LDL) Triglycerides in Patients with Type 2 Diabetes, Comparison with Small Dense LDL-Cholesterol. J Atheroscler Thromb, 2022; 29: 762-774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32).Nakamura M, Yamamoto Y, Imaoka W, Kuroshima T, Toragai R, Ito Y, Kanda E, Schaefer EJ, Ai M: Relationships between Smoking Status, Cardiovascular Risk Factors, and Lipoproteins in a Large Japanese Population. J Atheroscler Thromb, 2021; 28: 942-953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33).Nakamura M, Yamamoto Y, Imaoka W, Kuroshima T, Toragai R, Ito Y, Yoshida H, Ai M: Reference interval for serum concentration of small dense low-density lipoprotein cholesterol in the healthy Japanese population. Ann Clin Biochem, 2022; 59: 242-252 [DOI] [PubMed] [Google Scholar]
- 34).Friedewald WT, Levy RI, Fredrickson DS: Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem, 1972; 18: 499-502 [PubMed] [Google Scholar]
- 35).Lee DW, Choi DW, Ju YJ, Lee SA, Park EC: The association between low frequency of having breakfast and dyslipidemia in South Korean men and women. Eur J Clin Nutr, 2019; 73: 896-904 [DOI] [PubMed] [Google Scholar]
- 36).Kiriyama K, Yamamoto M, Kim D, Sun S, Yamamoto H, Oda H: Skipping breakfast regimen induces an increase in body weight and a decrease in muscle weight with a shifted circadian rhythm in peripheral tissues of mice. Br J Nutr, 2022; 128: 2308-2319 [DOI] [PubMed] [Google Scholar]
- 37).Otsuka Y, Kaneita Y, Tanaka K, Itani O, Matsumoto Y, Kuriyama K: Longitudinal assessment of lifestyle factors associated with nonrestorative sleep in Japan. Sleep Med, 2023; 101: 99-105 [DOI] [PubMed] [Google Scholar]
- 38).Min C, Noh H, Kang YS, Sim HJ, Baik HW, Song WO, Yoon J, Park YH, Joung H: Skipping breakfast is associated with diet quality and metabolic syndrome risk factors of adults. Nutr Res Pract, 2011; 5: 455-463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39).Sakurai M, Yoshita K, Nakamura K, Miura K, Takamura T, Nagasawa SY, Morikawa Y, Kido T, Naruse Y, Nogawa K, Suwazono Y, Sasaki S, Ishizaki M, Nakagawa H: Skipping breakfast and 5-year changes in body mass index and waist circumference in Japanese men and women. Obes Sci Pract, 2017; 3: 162-170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40).Yao CA, Chen IL, Chen CY, Torng PL, Su TC: Association between Wakeup Frequency at Night and Atherogenic Dyslipidemia: Evidence for Sex Differences. J Atheroscler Thromb, 2023; 30: 87-99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41).Ministry of Agriculture, Forestry and Fisheries: Policies for the Promotion of Shokuiku (White Paper on Shokuiku) 2019. https://www.maff.go.jp/j/syokuiku/wpaper/attach/pdf/r1_index-7.pdf (Access 11th April 2022) [Google Scholar]
- 42).Ministry of Health, Labour and Welfare: National Health and Nutrition Examination Survey 52: When Breakfast Missing Started, by Sex and Age Group. Ministry of Health, Labour and Welfare. Portal Site of Official Statistics of Japan website, https://www.e-stat.go.jp/(accessed 6th May 2022) [Google Scholar]
- 43).Kotani K, Nishida M, Yamashita S, Funahashi T, Fujioka S, Tokunaga K, Ishikawa K, Tarui S, Matsuzawa Y: Two decades of annual medical examinations in Japanese obese children: do obese children grow into obese adults? Int J Obes Relat Metab Disord, 1997; 21: 912-921 [DOI] [PubMed] [Google Scholar]
- 44).Ministry of Agriculture, Forestry and Fisheries: The Fourth Basic Plan for the Promotion of Shokuiku. https://www.maff.go.jp/e/policies/tech_res/attach/pdf/shokuiku-18.pdf (accessed 6th May 2022) [Google Scholar]
- 45).Nordmann AJ, Nordmann A, Briel M, Keller U, Yancy WS Jr, Brehm BJ, Bucher HC: Effects of low-carbohydrate vs low-fat diets on weight loss and cardiovascular risk factors: a meta-analysis of randomized controlled trials. Arch Intern Med, 2006; 166: 285-293 [DOI] [PubMed] [Google Scholar]
- 46).Naude CE, Schoonees A, Senekal M, Young T, Garner P, Volmink J: Low carbohydrate versus isoenergetic balanced diets for reducing weight and cardiovascular risk: a systematic review and meta-analysis. PLoS One, 2014; 9: e100652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47).Wan Y, Wang F, Yuan J, Li J, Jiang D, Zhang J, Li H, Wang R, Tang J, Huang T, Zheng J, Sinclair AJ, Mann J, Li D: Effects of dietary fat on gut microbiota and faecal metabolites, and their relationship with cardiometabolic risk factors: a 6-month randomised controlled-feeding trial. Gut, 2019; 68: 1417-1429 [DOI] [PubMed] [Google Scholar]
- 48).Anderson AS, Haynie KR, McMillan RP, Osterberg KL, Boutagy NE, Frisard MI, Davy BM, Davy KP, Hulver MW: Early skeletal muscle adaptations to short-term high-fat diet in humans before changes in insulin sensitivity. Obesity (Silver Spring), 2015; 23: 720-724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49).Thaler JP, Yi CX, Schur EA, Guyenet SJ, Hwang BH, Dietrich MO, Zhao X, Sarruf DA, Izgur V, Maravilla KR, Nguyen HT, Fischer JD, Matsen ME, Wisse BE, Morton GJ, Horvath TL, Baskin DG, Tschöp MH, Schwartz MW: Obesity is associated with hypothalamic injury in rodents and humans. J Clin Invest, 2012; 122: 153-162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50).Seidelmann SB, Claggett B, Cheng S, Henglin M, Shah A, Steffen LM, Folsom AR, Rimm EB, Willett WC, Solomon SD: Dietary carbohydrate intake and mortality: a prospective cohort study and meta-analysis. Lancet Public Health, 2018; 3: e419-e428 [DOI] [PMC free article] [PubMed] [Google Scholar]


