Abstract
Raynaud’s phenomenon (RP) is a common vasospastic disorder that causes severe pain and ulcers, but despite its high reported heritability, no causal genes have been robustly identified. We conducted a genome-wide association study including 5,147 RP cases and 439,294 controls, based on diagnoses from electronic health records, and identified three unreported genomic regions associated with the risk of RP (p < 5 × 10−8). We prioritized ADRA2A (rs7090046, odds ratio (OR) per allele: 1.26; 95%-CI: 1.20-1.31; p < 9.6 × 10−27) and IRX1 (rs12653958, OR: 1.17; 95%-CI: 1.12–1.22, p < 4.8 × 10−13) as candidate causal genes through integration of gene expression in disease relevant tissues. We further identified a likely causal detrimental effect of low fasting glucose levels on RP risk (rG = −0.21; p-value = 2.3 × 10−3), and systematically highlighted drug repurposing opportunities, like the antidepressant mirtazapine. Our results provide the first robust evidence for a strong genetic contribution to RP and highlight a so far underrated role of α2A-adrenoreceptor signalling, encoded at ADRA2A, as a possible mechanism for hypersensitivity to catecholamine-induced vasospasms.
Subject terms: Rheumatology, Genetics research, Translational research
Raynaud’s phenomenon is a common vasospastic disorder, but the genetic origins of the condition are not well understood. Here, the authors find common genetic variants associated with Raynaud’s phenomenon, and find genes putatively involved in the disorder.
Introduction
Raynaud’s phenomenon (RP) is a common episodic, vasospastic disorder that affects 2–5% of the population and can severely affect an individual’s quality of life by causing pain or even ulcers1–3. RP typically manifests with bi- or triphasic colour change in fingers and toes because of vasospasms in arteriovenous anastomoses responsible for thermoregulation, which can be triggered by cold or emotional stress4. The causes for the more common form of primary RP are largely unknown4,5, while secondary RP is diagnosed as a consequence of connective tissue diseases, like systemic lupus erythematosus (SLE) or systemic sclerosis (SSc), or triggered by the use of drugs such as beta-blockers. Management of RP is predominantly limited to the avoidance of triggers and evidence for medical treatment is generally weak. Repurposed vasodilators are the first line of treatment if pharmacological intervention is required due to progressive frequency of vasospastic attacks6, although only calcium channel blockers have so far been shown to lead to a significant and reproducible reduction in the frequency of vasospastic attacks7. However, the use of systemic drugs for localized symptoms puts patients at risk of generalized adverse effects, such as hypotension. While there are now trials investigating local application of botulinum toxin to mitigate vasospastic effects with early promising results8, a better understanding of the underlying mechanisms is needed to develop safe and effective treatments.
RP is highly heritable with estimates of 55–64% being reported9,10, but previous candidate gene studies11,12, like at serotonin receptors13, and an early, small (n = 640 cases) genome-wide association study (GWAS)14 failed to provide evidence for any robustly associated regions or genes. In-depth investigation and integration of detailed information from primary and secondary healthcare records with genetic array data now provide the opportunity to study under-investigated diseases with diagnostic specificity at an unprecedented scale.
Here, we present the so far largest GWAS for RP including 5147 cases in the UK Biobank cohort15 and report two robust and strong (p < 4.8 × 10−13) novel loci. We highlight two independent disease mechanisms supported by those loci that challenge and advance our current understanding of primary RP, with ADRA2A highlighting the role of α2A-adrenoreceptors and IRX1 as a putative regulator of vasodilation by altering prostaglandin and/or bradykinin responsiveness.
Results
We identified a total of 5147 RP cases and 439,294 controls of European descent included in the genetic analyses (Supplementary Table 1 and Supplementary Fig. 1) based on collation and evidence of absence or presence of diagnostic codes from electronic health records (ICD-10 codes: I73.0, I73.00, I73.01; CTV3/Read2: G730., G7300, G7301, G730z, XE0VQ), including 2185 prevalent cases and 2962 incident cases. We followed the recommendation by Wigley et al.4 to summarize all patients with a relevant code under the term Raynaud’s phenomenon (RP) rather than Raynaud’s syndrome.
Genome-wide association analysis
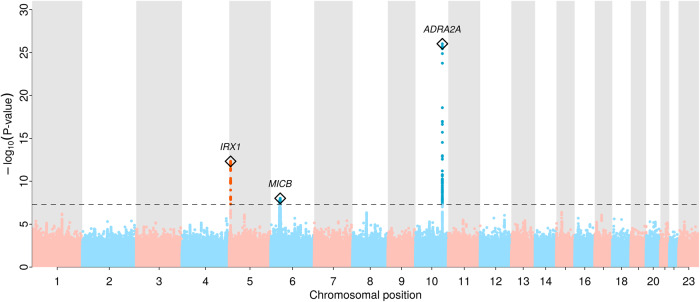
We identified a total of three genome-wide significant novel loci (p < 5.0 × 10−8, minor allele frequency (MAF) 14.3–31.1%) associated with RP (Fig. 1 and Table 1; regional association plots in Supplementary Fig. 2). Two of which met a more stringent significance threshold (p < 1.0 × 10−9; Table 1), which we consider as tier 1 findings of which one had previously been shown to increase the risk of myocardial infarction (rs12653958). All lead variants increased the risk for RP by ~20% per copy of the minor allele (Table 1) and resided in intergenic regions with no obvious functional variants in linkage disequilibrium (LD; r2 > 0.6) and were of low predicted impact (CADD score range: 0.36–3.41). Despite the established sex-difference of RP, we did not find evidence that the effects of any of the identified lead signals differed between men and women (all p-values for interaction > 0.05; Supplementary Table 2). We estimated a single nucleotide polymorphism (SNP)-based heritability on the liability scale of 7.7% (95% CI: 4.8–10.6%, p < 2.4 × 10−7) with little evidence of genomic inflation (LD-score intercept 1.01; Supplementary Fig. 3).
Fig. 1. Manhattan plot of genome-wide association results for Raynaud’s phenomenon (5147 RP cases and 439,294 controls).
Distribution of RP-associated single nucleotide polymorphisms across the genome, −log10(P-values) from logistic regression models are plotted for each variant. The grey dashed line indicates the genome-wide significant threshold at p = 5 × 10−8. Regional sentinel variants at significant loci are highlighted with a diamond and the closest gene, if any, is annotated.
Table 1.
Regional lead variants for the eight loci significantly associated with Raynaud’s phenomenon
| Tier | SNP | Chr | Position | Alleles | MAF | OR (95% CI) | P-value | Closest genea |
|---|---|---|---|---|---|---|---|---|
| 1 | rs7090046 | 10 | 112860930 | A/G | 0.31 | 1.26 (1.20, 1.31) | 9.58 × 10−27 | ADRA2A |
| 1 | rs12653958 | 5 | 4032849 | A/G | 0.30 | 1.16 (1.12, 1.22) | 4.76 × 10−13 | IRX1 |
| 2 | rs3094013 | 6 | 31434366 | G/A | 0.14 | 1.17 (1.11, 1.24) | 9.73 × 10−9 | MICB |
Tier = categorization whether genetic loci met a stringent Bonferroni threshold for significance (tier 1; p < 1.0 × 10−9) or the standard genome-wide significance threshold (tier 2; p < 5.0 × 10−8). N = 444,441, 5147 cases, and 439,294 controls. Alleles are given as effect allele/non-effect allele.
Chr chromosome, MAF minor allele frequency, OR odds ratio from logistic regression models.
aProtein coding gene in italics.
To evaluate whether genetic findings were specific to the development of RP or driven by associations with diseases leading to secondary RP, we performed sensitivity analyses based on a more stringent definition of primary RP (3505 cases, 68.1%) that excluded potential secondary cases (see the “Methods” section). Effect estimates for both tier 1 loci were highly consistent in size and direction (Supplementary Table 3) and remained genome-wide significant (p < 1.4 × 10−12 for both), indicating their potential role in the idiopathic origin of primary RP, whereas the association within the MHC region was attenuated.
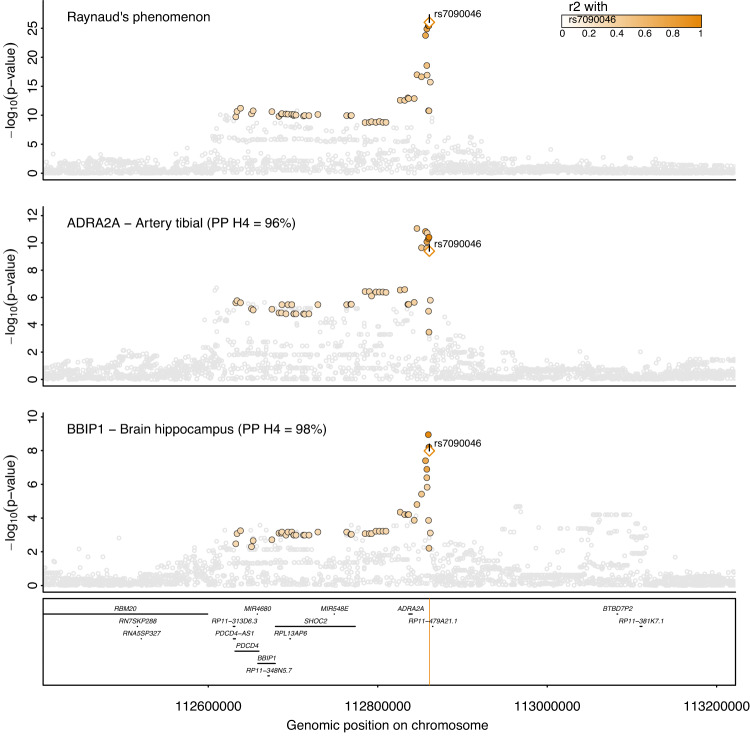
ADRA2A and BBIP1 are likely effector genes at 10q25.2
The lead variant at this strongest locus, rs7090046, is located 24.1k bp downstream to ADRA2A and 181.9k bases downstream from BBIP1 (Fig. 2) and Bayesian fine-mapping identified a 95%-credible set of only four variants (see the “Methods” section), comprising rs7090046, rs1343449, rs1343451, and rs7084501 with posterior inclusion probabilities (PIP) of 48.6%, 23.6%, 12.5% and 12.6% of the GWAS signal, respectively. Variant rs1343449 is a reported gene expression quantitative trait locus (cis-eQTL) for ADRA2A in artery tissue and statistical colocalization confirmed a shared genetic signal with RP with high confidence (tibial artery, posterior probability (PP) > 96%; Fig. 2), with the RP risk-increasing A-allele of rs7090046 being associated with higher ADRA2A expression (beta = 0.28, p = 1.0 × 10−9). We also observed evidence of colocalization with BBIP1 expression in the brain hippocampus and colon (PP > 98%; Fig. 2 and Supplementary Data 1), with the A-allele being associated with lower BBIP1 expression in brain hippocampus (beta = −0.37, p = 9.1 × 10−9), raising the possibility that variants in the credible set have pleiotropic, tissue-dependent effects in different directions.
Fig. 2. Regional association plot at ADRA2A/BBIP1.
Regional association plot for Raynaud’s phenomenon (top), gene expression of ADRA2A in a tibial artery (middle), and gene expression of BBIP1 in the hippocampus (bottom). ADRA2A and BBIP1 have been prioritized as candidate causal genes based on statistical colocalization. Summary statistics from logistic regression models for RP are from the present study whereas summary statistics from linear regression models were obtained from GTEx v822. Colouring of SNPs is based on linkage disequilibrium with the lead RP variant (rs7090046) at this locus. Numbers in brackets indicate posterior probabilities (PP) for a shared genetic signal with RP based on statistical colocalization.
ADRA2A encodes α2A-adrenoreceptors, responsible for mediating response to stress in the central and peripheral autonomous nervous system16, and vasoconstriction in response to catecholamine release in the small arteries and arterioles17. Our finding may imply that overstimulation or increased expression of α2A-adrenergic receptors contributes to the vasospastic effects characteristic of RP and its symptoms, also in line with RP being an adverse effect of α2-adrenergic agonists such as clonidine4,18,19. A possible role of BBIP1, in contrast, is less obvious. BBIP1 encodes for a protein in the BBSome complex, which is involved in the signalling from and to cilia.
Investigating thousands of other outcomes from the GWAS catalogue20 and the Open Targets platform21 in addition to phenome-wide analyses of UK Biobank (p < 10−6, see the “Methods” section), we observed no other significant associations for rs7090046 or its proxies (r2 > 0.6), except for “specified peripheral vascular disease” in UK Biobank (OR 1.18, p-value 4.5 × 10−11), a non-specific code that comprises, among other diseases, RP. These results suggest the specificity of the mechanism underlying the genetic signal at 10q25.2 on RP.
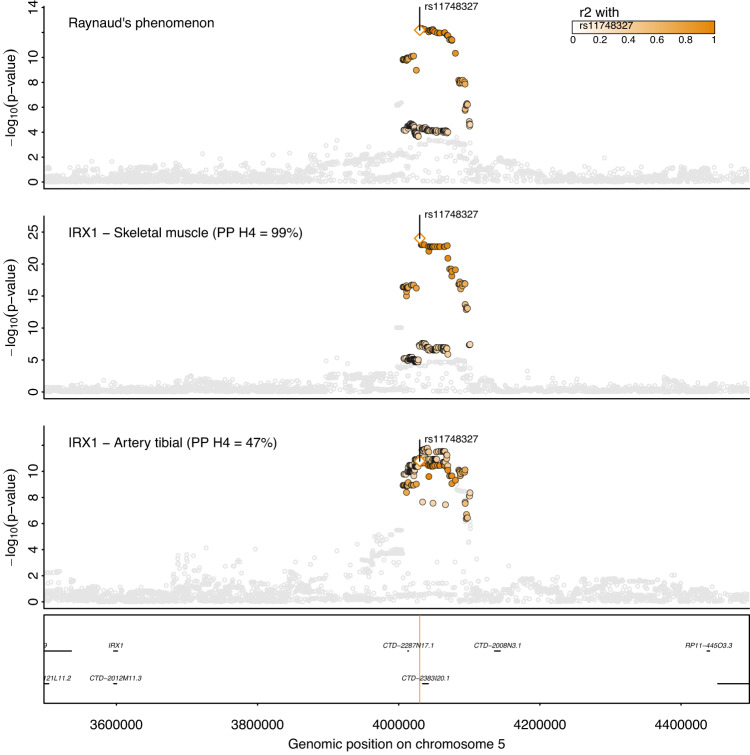
IRX1 is the likely effector gene at 5p15.33 and links to cardiovascular outcomes
We fine-mapped the second strongest signal at 5p15.33 to 24 variants with rs12653958 as the lead SNP with a PIP of 6.4%. The credible set also covered rs11748327 (PIP = 4.7%) which has been reported as a cis-eQTL for IRX1 in skeletal muscle22. Statistical colocalization further confirmed a shared genetic signal between RP and IRX1 expression in skeletal muscle and tibial artery with high (PP = 99%) and moderate (PP = 47%) confidence, respectively (Fig. 3). The RP-increasing effect-allele of rs11748327 was associated with higher expression of IRX1 in skeletal muscle (beta = 0.57, p = 1.1 × 10−22) and tibial artery (beta = 0.42, p = 5.7 × 10−11), suggesting that higher gene expression confers a higher risk for RP. IRX1 encodes for members of the homeobox-containing genes that have been shown to be involved in embryonic development and cellular differentiation23. The lead variant, rs12653958, at this locus, tags a cluster of variants (r2 = 0.7–1.0) that has previously been reported to be associated with myocardial infarction (MI)24,25 and coronary artery disease (CAD)26 among East Asian populations and is further a cross-ancestral signal for red blood cell phenotypes27,28. In detail, the RP risk-increasing G-allele was also associated with an increased risk for coronary artery disease (beta = −0.06; p < 1.8 × 10−8) in data from BioBank Japan26. The fact that this common variant (MAFEUR = 30.0%; MAFEAS = 22.3%) has not yet been identified for MI or CAD in Europeans (p = 1.61 × 10−7) despite much larger sample sizes (n = 181,522)29, might point to the possibility of a yet to be identified gene–environment interaction or other characteristics distinct to the East Asian cohorts that account for this observation.
Fig. 3. Regional association plot at IRX1.
Regional association plot for Raynaud’s phenomenon (top), gene expression of IRX1 in skeletal muscle (middle), and gene expression of IRX1 in tibial artery (bottom). Summary statistics from logistic regression models for RP are from the present study whereas summary statistics from linear regression models were obtained from GTEx v822. Colouring of SNPs is based on linkage disequilibrium with the lead RP variant (rs12653958) at this locus. Numbers in brackets indicate posterior probabilities (PP) for a shared genetic signal with RP based on statistical colocalization.
RP in individuals of South Asian ancestry
We aimed to test for replication and transferability of our European-centric results in 401 RP cases of British Bangladeshi and Pakistani ancestry from the Genes & Health cohort30 (n = 40,532), and observed directionally concordant results (rs11748327; OR = 1.16, 95%-CI = 0.99–1.37, p-value = 0.06; IRX1) for one of the two strongest loci, while for the second one, rs7090046 (ADRA2A), the lead variant or suitable genetic proxies were not available. However, further studies with comparable numbers of RP cases are needed to establish trans-ethnic and ethnic-specific risk variants for RP.
Genetic correlation between RP and other traits
We next tested for a shared genetic architecture (genetic correlation: rG) between RP and known or suspected risk factors and comorbidities with a vascular or immune origin/component like peripheral artery disease (PAD) or COVID-19 (Supplementary Data 2). We observed that possible causes or related disorders for RP, like migraine (rG = 0.21, p = 9.0 × 10−3), PAD (rG = 0.38, p = 2.1 × 10−3), or SLE (rG = 0.33 p = 1.0 × 10−3) significantly (false discovery rate < 5%) correlated when considering all RP patients, but were strongly attenuated once we computed genetic correlations restricted to patients with primary RP (Supplementary Fig. 5, Supplementary Data 3). In contrast, other significant correlations persisted (p < 0.05) when we restricted genetic correlation analysis to results based on patients with primary RP (to which we refer to as robust in the following). This included significant inverse correlations with type 2 diabetes (rG = −0.14, p = 2.7 × 10−3), fasting glucose (rG = −0.21, p = 0, p = 2.3 × 10−3), and a positive correlation with HDL-cholesterol levels (rG = 0.13, p = 9.2 × 10−4) (Supplementary Fig. 5).
To distinguish whether genetic correlations represent causal directions from versus towards RP or are due to shared risk factors that likely act independently on RP and correlated traits, we performed latent causal variable analysis31 (see the “Methods” section). Out of a total of six phenotypes with evidence for significant genetic correlations, only SLE (genetic causality proportion (GCP) = 0.75; p < 1.7 × 10−4) and fasting glucose (GCP = 0.77; p < 5.21 × 10−15) showed strong evidence for a causal genetic effect on RP risk, of which fasting glucose but not SLE persisted in analyses considering only patients with primary RP (GCP = 0.80; p < 1.3 × 10−16). These results indicate that low fasting glucose levels may causally increase the risk for RP, while frequent comorbidities of RP, like migraine, are likely explained by shared risk factors.
We then extended the targeted analysis by computing genetic correlations with 185 medical concepts—‘phecodes’, to gain a more comprehensive view of possible diseases that share a genetic architecture with RP (see the “Methods” section; Supplementary Data 4). We observed 8 phecodes with significant, although moderate, genetic correlations with RP (Supplementary Data 4), of which only the significant genetic correlation with osteoporosis persisted when we restricted the analysis to patients with primary RP (rG = 0.35, p < 8.7 × 10−5). However, none of the phenotypes showed evidence of a direct causal link towards or from RP in latent causal variant analysis (see the “Methods” section; Supplementary Table 4).
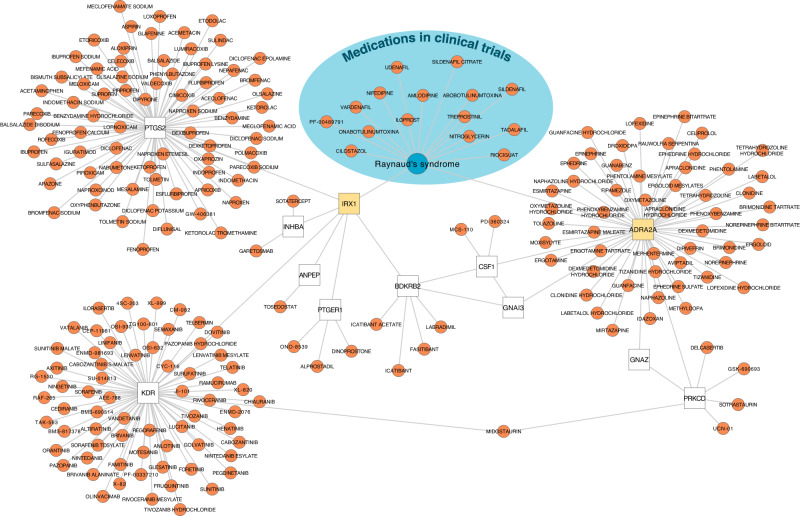
From genes to druggable targets
We finally searched for putative druggable targets for RP based on the identified loci by cross-referencing high-confidence gene assignments and functional interaction partners thereof32 in the Open Targets database21 (see the “Methods” section). While we identified no link for drugs with known (genetic) targets currently or previously in clinical trials for RP (e.g., phosphodiesterase inhibitors), we identified a total of 211 drugs that target either directly (e.g., ADRA2A) or indirectly (e.g., PTGS2) gene products identified in our study (Fig. 4 and Supplementary Data 5). More than 50 drugs had at least some affinity to α2A-adrenergic receptors, although none did so specifically. Since we identified increased expression of α2A-adrenergic receptors as a possible disease-causing mechanism, partially selective antagonists, such as the widely used antidepressant mirtazapine, might be promising candidates for repurposing. Among the drugs indirectly linked to RP-associated gene products, those counteracting vasoconstriction or promoting vasodilation have the greatest repurposing potential. For example, drugs promoting prostaglandin (via PTGER1 but not PTGS2) or bradykinin signalling (via BDKRB2) such as dinoprostone or labradimil, respectively, might exert beneficial effects. However, the indirect nature of the gene-drug–disease link for the latter (via altered IRX1 expression) requires further functional follow-up to establish the precise underlying mechanism and effect directions.
Fig. 4. Gene–Drug–Disease network for Raynaud’s phenomenon.
The network displays drug target information obtained from Open Targets21 for (1) Raynaud’s Phenomenon (RP; blueish area), (2) genes associated with RP in the present study (yellow), and (3) interacting genes (white) based on functional work32.
Discussion
RP is a common but understudied disease with a high heritable component and identifying responsible genes can advance our understanding of the aetiology and eventually guide the development of treatment strategies. We identified, for the first time, two robust susceptibility loci. Through integration with gene expression data, we demonstrated that the strongest locus likely acts via increased expression of α2A-adrenoreceptors in arterial tissue, augmenting the current concept of predominantly α2C-adrenoreceptors mediating the vasospasms seen in RP patients4. Increased expression of the transcription factor IRX1 in muscle, and possibly arterial tissue, may further alter genes involved in prostaglandin and/or bradykinin sensing and production, providing a putative second novel mechanism identified in our genetic study. We lastly observed no strong evidence for a shared genetic architecture with suspected cardiovascular comorbidities for primary RP but did observe a novel detrimental effect of low fasting plasma glucose that might help to guide primary RP management.
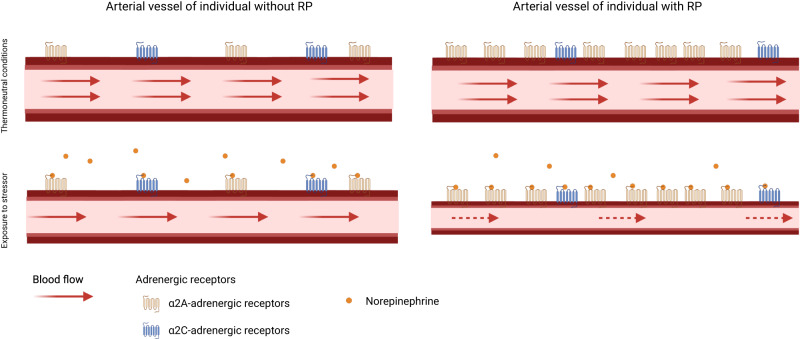
Vasospastic attacks in RP have been repeatedly attributed to cold-induced activation of α2C-adrenoreceptors4,18,33,34, but attacks also occur under thermoneutral conditions and selective, pharmacological blocking of α2C-adrenoreceptors did not mitigate symptoms in clinical trials35. An observation that aligns with the absence of an effect of a strong cis-eQTL for ADRA2C (rs35729104), encoding for α2C-adrenoreceptors, on RP risk (OR = 1.02, p = 0.29) in our study. We, in contrast, provide genetically anchored evidence that α2A-adrenoreceptors play an underrated role further supported by adverse drug reactions seen with α2A-adrenoreceptor agonists (Fig. 5). More specifically, α2A-adrenoreceptors mediate arterial vasoconstriction, thrombus stabilization, and hypothermic effects on body temperature36,37. Our results are in line with a vasoconstrictive role of α2A-adrenoreceptors under thermoneutral conditions17 and subsequent RP risk and further support findings of a quantitively stronger role of α2-adrenoreceptors compared to α1-adrenoreceptors during cold stress in RP patients38,39. However, it might still be conceivable that both α2-adrenoreceptors act in a context-specific manner to induce vasospastic effects19 or another mechanism partakes in cold-induced RP attacks since pharmacological inhibition of α2-adrenergic receptors did blunt but not eliminate cold-induced vasoconstriction38.
Fig. 5. Scheme of the key finding.
In people without Raynaud’s phenomenon (RP) stimulation of α2A- and α2C-adrenoreceptors contributes to vasoconstriction and lower blood flow. In patients with RP, blood flow is further reduced due to overexpression of α2A-adrenoreceptors creating a state of hypersensitivity to catecholamine-release. Created with BioRender.com.
Currently, RP is treated depending on its severity. For mild cases, avoidance of triggers like cold or emotional stress might be sufficient, but severe vasospastic attacks require pharmacological interventions with calcium channel blockers as first-line response6. However, the overall effectiveness of calcium channel blockers5 or alternative vasodilatory medications such as angiotensin receptor blockers, selective serotonin reuptake inhibitors, or phosphodiesterase-5 inhibitors is limited6,7. Negative findings that overall align well with the absence of genetic evidence for those targets in our study. A staggering characteristic of the ADRA2A locus was the specificity in phenome-wide screens and comprehensive database lookups, which indicated an RP-specific effect. Such a characteristic may make the inhibition of the gene product, α2A-adrenoreceptors, an interesting pharmacological target. This does not rule out that systemically administered antagonists might exert adverse effects, but inhibiting α2A-adrenoreceptor activity in disease-relevant tissue, for example using topical solutions, might provide a safe and effective treatment option. There are already approved medications that target α2-adrenoreceptor antagonistically like the widely prescribed antidepressant mirtazapine, but they lack specificity for α2A-adrenoreceptor36 and case reports described the occurrence or worsening of RP in two male patients under yohimbine treatment, another α2-adrenoreceptor antagonist, for erectile dysfunction40,41. Clinical trials are needed to test whether treatment with mirtazapine, or topical solutions thereof, can indeed mitigate vasospastic attacks in patients with primary RP, also because an early study described relieved symptoms under methyldopa, an α2-adrenergic agonist42.
In addition to hypersensitivity to vasoconstrictive stimuli, missing vasodilation is the primary cause of persistent vasospasms in RP. We identified overexpression of IRX1, the second strongest signal for RP, in muscle cells and possibly the tibial artery as a putative RP risk-increasing mechanism. While little is known about IRX1 in general, a transfection study in gastric cancer cell lines identified several putative target genes of IRX1 with a role in vasoconstriction and vasolidation43. This included the downregulation of PTGER1, encoding the prostaglandin E2 receptor 1 (EP1) and upregulation of PTGS2, encoding prostaglandin G/H synthase 2, as well as downregulation of BDKRB2, encoding bradykinin receptor B2. Prostaglandin E2 (PGE2) can induce both vasodilation and vasoconstriction depending on receptor binding, with binding to EP1 inducing vasoconstriction in smooth muscle cells44,45. Downregulation of BDKRB2 in endothelial and smooth muscle cells, in turn, may blunt the vasodilative function of bradykinin46, in line with observations in RP patients treated with bradykinin47,48. A putative role of the IRX1 locus in vasodilation/vasoconstriction might also explain its association with cardiovascular disease as described among people of East Asian descent24–26. Further experimental work will help clarify this, and might also help to refine the application of prostaglandin or bradykinin analogues, as vasodilators in RP4.
Little is known about the causes of primary RP, and we provided evidence that genetic liability towards low fasting glucose levels increases RP risk. A putative mechanism, however, remains elusive and we did not observe evidence that other metabolic risk factors were causally associated with RP risk, including BMI (Supplementary Data 3). Overexpression of α2A-adrenoreceptors in pancreatic islet cells has been postulated as a mechanism for diminished insulin secretion and postprandial hyperglycaemia among carriers of risk alleles in ADRA2A49. However, the reported risk allele, rs553668, is only weakly correlated (r2 = 0.15) with our RP lead signal at the same locus and the same applies to the more recently identified genome-wide significant finding50. Although likely via distinct genetic variants, both diseases seem to share overexpression of ADRA2A as a common, but tissue-specific, disease mechanism, and it is unclear whether overexpression of ADRA2A in pancreatic beta-cells also contributes to fasting glucose levels. Conversely, hypoglycaemia exerts profound changes on the vasculature, including vasoconstriction via increased adrenal catecholamine release to maintain blood flow to the brain51, which may, in turn, exaggerate hypersensitivity to catecholamines of arteriovenous anastomoses in fingers and toes. However, a drop in body temperature following hypoglycaemia is caused by cutaneous vasodilation, which might itself be a trigger for vasospastic effects in RP patients. Even a role of β-adrenergic receptors might be conceivable since beta-blockers can cause both, hypoglycaemia52 and RP4. A pragmatic consequence for people at RP risk, or even RP patients, might be to avoid episodes of low plasma glucose levels.
While we identified eight loci robustly associated with RP, we did not find support for genes highlighted by previous smaller-scale and candidate gene studies. This included subthreshold findings from an earlier GWAS14 (NOS1, smallest p-value in NOS1 region ± 500 kb (pmin) = 2.6 × 10−3) as well as candidate gene studies for serotonin 1B (HTR1B; pmin = 6.8 × 10−4) and 1E (HTR1E; pmin = 1.2 × 10−5) receptors and the beta subunit of the muscle acetylcholine receptor (CHRNB1; pmin = 1.3 × 10−3)13. Our results therefore highlight the need for large sample sizes, which are only now possible with the increased availability of electronic health record linkage.
Our study has limitations that need to be considered in the interpretation of the results. Firstly, we defined patients with RP based on billing codes from medical records of various sources which might have missed patients with milder presentations and suffer from potential misclassification if patient symptoms have been wrongly assigned to RP, in particular in the presence of disease that causes RP as a secondary phenomenon. However, our conservative sensitivity analysis, excluding all patients with potential known causes of RP revealed congruent findings and the associated loci have a clear biological link towards RP pathology. Secondly, our study was exclusively comprised of participants of European descent and low case numbers and poor imputation quality of the main locus did not permit robust analysis in other ancestries, which is needed to achieve fair representation of different ancestries in genomic studies and may reveal additional findings. Thirdly, while we were able to replicate the association between ADRA2A expression in tibial artery and risk of RP in a small, independent cohort (n = 124 RP patients; OR = 1.27; p = 0.0039) from the BioVU study53, additional efforts in large biobanks with linked primary care data are needed to further consolidate our findings. Finally, while we assign putative candidate genes at two loci, more work is needed to improve gene assignment pipelines to elucidate possible mechanisms at other loci including rare variants with strong effect sizes.
Our results advance the understanding of RP pathology by shifting the focus from a merely cold-induced phenomenon to a clinical entity in its own right with a distinct genetic architecture. The identification of ADRA2A and IRX1 as candidate causal genes will further inform the development and refinement of treatment strategies although more experimental work is needed.
Methods
United Kingdom Biobank (UKBB)
UK Biobank is a prospective cohort study from the UK that contains more than 500,000 volunteers between 40 and 69 years of age at inclusion. The study design, sample characteristics, and genome-wide genotype data have been described in Sudow et al. and Bycroft et al.15,54. The UKBB was approved by the National Research Ethics Service Committee North West Multi-Centre Haydock and all study procedures were performed in accordance with the World Medical Association Declaration of Helsinki ethical principles for medical research. We included 444,441 individuals in the GWAS for whom inclusion criteria (given consent to further usage of the data, availability of genetic data, and passed quality control of genetic data) applied. Data from the UKBB were linked to death registries, hospital episode statistics (HES), and primary care data.
RP case ascertainment
We used all available electronic health records, including primary (~45% of the population) and secondary care, death certificates as well as participant’s self-report to define RP cases. We manually curated relevant codes for RP based on the different coding systems used (ICD-10 codes: I73.0, I73.00, I73.01; CTV3/Read2: G730., G7300, G7301, G730z, XE0VQ) and flagged the first occurrence of a related code in the records of a participant as the incidence date. We compared the date of the very first record related to RP with the date of the baseline examination of the same participant to distinguish between prevalent and incident RP. We followed the criteria from Wigley et al.4 to differentiate between primary and secondary RP. In detail, we classified each RP case as ‘secondary’ when patients were either under beta-blocker treatment or had been diagnosed with one of the following diseases prior or at the same time of their RP diagnosis: arteriosclerosis, carpal tunnel syndrome, systemic lupus erythematosus, systemic sclerosis, polymyositis, dermatomyositis, Sjögren syndrome, hypothyroidism, cryoglobulinemia, frostbite or other connective tissues diseases (Supplementary Data 6).
UKBB medication classification/ beta-blocker usage
During the baseline assessment self-reported regular medication use was recorded. Medication data were categorized into 6745 groups (Data field: 20,003). 38 categories of the medication data were identified manually to represent medication containing beta-blocker substances.
Demographic analysis
We performed χ2-tests and analysis of variance to test for statistically significant differences in demographic characteristics between controls and RP cases using standard implementations in R (v4.1.2).
Genotyping, quality control and participant selection
Details on genotyping for UKBB have been reported in detail by Bycroft et al.15. Briefly, we used data from the ‘v3’ release of UKBB containing the full set of Haplotype Reference Consortium (HRC) and 1000 Genomes imputed variants. We applied recommended sample exclusions by UKBB including low-quality control values, sex mismatch, and heterozygosity outliers. We defined a subset of ‘white European’ ancestry by clustering participants based on the first four genetic principal components derived from the genotyped data using a k-means clustering approach with k = 5. We classified all participants who belonged to the largest cluster and self-identified as of being ‘white,’ ‘British’, ‘Any other white background’, or ‘Irish’ as ‘white European’. After the application of quality control criteria and dropping participants who had withdrawn their consent, a total of 444,441 UKBB participants were available for analysis with genotype and phenotype data.
We used only called or imputed genotypes and short insertions/deletions (here commonly referred to as SNPs for simplicity) with a minor allele frequency (MAF) > 0.001%, imputation score > 0.4 for common (MAF ≥ 0.5%) and >0.9 for rare (MAF < 0.5%), within Hardy–Weinberg equilibrium (pHWE > 10−15), and minor allele count (MAC) > 10. This left us with 15,519,342 autosomal and X-chromosomal variants for statistical analysis. GRCh37 was used as reference genome assembly.
Genome-wide association study
We performed genome-wide association studies for RP and primary RP using REGENIE v2.2.4 via a two-step procedure to account for population structure as described in detail elsewhere55. We used a set of high-quality genotyped variants (MAF > 1%, MAC > 100, missingness < 10%, pHWE > 10−15) in the first step for individual trait predictions using the leave one chromosome out (LOCO) scheme. These predictions were used in the second step as offset to run logistic regression models with saddle point approximation to account for case/control imbalance and rare variant associations. Models were adjusted for age, sex, genotyping batch, assessment centre, and the first ten genetic principal components. We used a tier system to classify genome-wide significant loci. Given the absence of a substantial replication cohort, we consider loci meeting a stringent p-value threshold of p < 1.0 × 10−9 as robust findings (tier 1) and further considered loci meeting the standard genome-wide significance threshold of p < 5.0 × 10−8 as strongly suggestive loci (tier 2).
LD score regression and genetic correlation to other common diseases
We tested for genomic inflation and calculated the SNP-based heritability using LD-score regression (LDSC v1.0.1)56. We further used LDSC to compute the genetic correlation between RP as well as primary RP and a set of 20 preselected traits and diseases (Supplementary Data 2). P-values were corrected for multiple testing by controlling the false-discovery rate at 5% according to the Benjamini–Hochberg procedure. To explore genetic correlation with other common diseases, we computed genetic correlation to a set of 185 phecodes (see below; Supplementary Data 4) with at least 1% SNP-based heritability derived from the UKBB.
Signal selection and fine-mapping
We used regional clumping (±500 kb) to select independent genomic regions associated with RP treating the extended MHC region as a whole (chr6:25.5-34.0 Mb) and collapsed neighbouring regions using BEDtools v1.5.
Within each region, apart from the MHC region, we performed statistical fine-mapping using “Sum of single effects” model (SuSiE)57 as implemented in the R package susieR (v.0.11.92). Briefly, SuSiE employs a Bayesian framework for variable selection in a multiple regression problem with the aim to identify sets of independent variants each of which likely contains the true causally underlying genetic variant. We implemented the workflow using default prior and parameter settings, apart from the minimum absolute correlation, which we set to 0.1. Since SuSiE is implemented in a linear regression framework, we used the GWAS summary statistics with a matching correlation matrix of dosage genotypes instead of individual-level data to implement fine-mapping (susie_rss()) as recommended by the authors57. We computed the correlation matrix with LDstore v1.0.
Sex-specific SNP effect
We tested for a potential modulating effect of sex on SNP–RP association using an additional interaction term in logistic regression models with the same adjustment set as described above. We implemented this analysis in R v.4.1.2 using a set of 361,781 unrelated white European individuals.
Replication in East London Genes & Health
We performed a genome-wide association analysis of RP in the Genes & Health cohort of British individuals of South Asian ancestry. We defined RP status using electronic health records and using the same code list as for the European-ancestry cohort. We identified 401 RP cases and 40,131 controls with complete covariate and genetic data passing quality control30 (mean age at recruitment: 41.2 yr [s.d.D:14.2], 55.6% females).
Genotyping and quality control for Genes & Health is described in Supplemental File 1. Briefly, genotyping was done using the Illumina Infinium Global Screening Array v3 with additional multi-disease variants and imputed to TopMed version 3 using the Michigan Imputation Server. We used REGENIE55 for association testing with age, sex, age2, and the first twenty genetic principal components as covariates. We included only autosomal genetic variants with an MAF > 1% (in this cohort), INFO score > 0.7 for imputed variants, pHWE > 10−10, and missingness < 10%. To allow for comparison with the results from the UK Biobank, we used the liftOver tool (v.2.0) to map between hg19 and hg38.
eQTL mapping to tissues/functional annotation
We systematically tested for a shared genetic signal between RP loci and gene expression levels (eQTL) in 49 tissues from the GTEx project (v8)22. Briefly, we considered all protein-coding genes or processed transcripts encoded in a 1 Mb window around RP loci and performed statistical colocalization58 to test for a shared genetic signal between RP and gene expression, as implemented in the R coloc package (v.2.0). We only report RP loci–gene–tissue triplets with a posterior probability >80% for a shared genetic signal as candidate causal genes. We adopted a recently recommended prior setting59 with p12 = 5 × 10−6. All GTEx variant-gene cis-eQTL associations from each tissue were downloaded in January 2020 from https://console.cloud.google.com/storage/browser/gtex-resources.
We further used the PrediXcan software60 to associate genetically predicted expression levels of ADRA2A with the risk of RP in 124 RP cases and 16,965 controls of the BioVU cohort53.
Phenome-wide association studies and variant look-up
We performed phenome-wide association studies for each RP locus identified using the comprehensive electronic health record linkage to generate a set of 1448 ‘phecodes’, from which we used 1155 ‘phecodes’ with a case number of more than 200. To generate phecode-based outcome variables, we mapped ICD-10, ICD-9, Read version 2, Clinical Terms Version 3 (CTV3) terms codes from self-report or medical health records, including cancer registry, death registry, hospitalization (e.g., Hospital Episode Statistics for England), and primary care, to a set of summarized clinical entities called phecodes61,62. For example, more than 90 ICD-10 codes can indicate participants with type 1 diabetes that are here collectively summarized under the phecode ‘type 1 diabetes’63. We used any code that was recorded, irrespective if it contributed to the primary cause of death or hospital admission, to define phecodes. We adjusted all analyses for the test centre to account for regional differences in coding systems and case ascertainment. For each participant and phecode, we kept only the first entry irrespective of the original data set, generating a first occurrence data set. We dropped codes that were before or in the participants’ birth year to minimize coding errors from electronic health records. We implemented the same logistic regression framework used for sex-interaction testing among unrelated individuals of White European ancestry. We applied a stringent Bonferroni correction to account for multiple testing (p < 3.7 × 10−5).
We further performed look-ups for all independent lead variants and proxies (r2 > 0.6) associated with RP in the OpenTargets database21 and the GWAS catalogue20 (download: 27/04/2022) to search for possibly previously reported traits and to establish novelty.
LCV analysis
To assess the evidence for a causal relationship between RP and each of the genetically correlated phenotypes (Supplementary Data 3 and 4) we implemented a latent causal variable (LCV) model31. The LCV model estimates a parameter termed genetic causality proportion (GCP). The values of GCP range from −1 to 1, quantifying both the magnitude and direction of genetic causality between two traits. Briefly, the LCV model fits an unobserved latent variable, L, which mediates the genetic correlation between two traits and compares the correlation of each trait with L to estimate the GCP. A|GCP| value of one indicates full genetic causality (suggestive of vertical pleiotropy) whereas a GCP value of zero implies no evidence for genetic causality (suggesting that the genetic correlation between two traits is likely to be mediated by horizontal pleiotropy or shared risk factors) and |GCP| < 1 indicates partial genetic causality between two traits. Negative values of the GCP estimate suggest that RP lies downstream of the other trait and interventions on the other trait are likely to affect RP, while positive GCP values indicate that the other trait lies downstream of RP. We implemented LCV analysis using standard parameters with version 1.0. We used the same LD-scores as in the genetic correlation analysis and excluded the extended MHC regions from any calculations. We considered the number of significant genetic correlations as a testing burden for LCV results.
Drug target annotation
To identify putative druggable targets for RP and test for evidence for drugs already in clinical trials, we queried the Open Target database21 for all genes likely linked to GWAS loci (i.e., evidence from eQTL annotation or intronic). We augmented this gene list by functionally validated interaction partners from the SIGNOR network32 and retained all matching drugs for further investigation. We lastly manually screened all prioritized drugs to match mechanisms to signs and symptoms of RP.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Supplementary information
Description of Additional Supplementary Files
Acknowledgements
All research related to UK Biobank has been done under the application number 44448. Mu. P. wishes to thank the MRC (MR/L006758/1, MR/V033867/1) and NIHR (NIHR202349) for their support. This collaboration is part of the National Institute For Health Barts Biomedical Research Centre portfolio. B.M.J. is funded by a Medical Research Council (MRC) Clinical Research Training Fellowship (CRTF) jointly supported by the UK MS Society (B.M.J.; grant reference MR/V028766/1), and by Barts Charity. The authors acknowledge the Scientific Computing of the IT Division at the Charité—Universitätsmedizin Berlin for providing computational resources that have contributed to the research results reported in this paper (https://www.charite.de/en/research/research_support_services/research_infrastructure/science_it/#c30646061). Genes & Health is/has recently been core-funded by Wellcome (WT102627, WT210561), the Medical Research Council (UK) (M009017, MR/X009777/1), Higher Education Funding Council for England Catalyst, Barts Charity (845/1796), Health Data Research UK (for London substantive site), and research delivery support from the NHS National Institute for Health Research Clinical Research Network (North Thames). Genes & Health is/has recently been funded by Alnylam Pharmaceuticals, Genomics PLC; and a Life Sciences Industry Consortium of Astra Zeneca PLC, Bristol-Myers Squibb Company, GlaxoSmithKline Research and Development Limited, Maze Therapeutics Inc, Merck Sharp & Dohme LLC, Novo Nordisk A/S, Pfizer Inc, Takeda Development Centre Americas Inc. We thank Social Action for Health, Centre of The Cell, members of our Community Advisory Group, and staff who have recruited and collected data from volunteers. We thank the NIHR National Biosample Centre (UK Biocentre), the Social Genetic & Developmental Psychiatry Centre (King’s College London), Wellcome Sanger Institute, and Broad Institute for sample processing, genotyping, sequencing and variant annotation. We thank: Barts Health NHS Trust, NHS Clinical Commissioning Groups (City and Hackney, Waltham Forest, Tower Hamlets, Newham, Redbridge, Havering, Barking and Dagenham), East London NHS Foundation Trust, Bradford Teaching Hospitals NHS Foundation Trust, Public Health England (especially David Wyllie), Discovery Data Service/Endeavour Health Charitable Trust (especially David Stables), NHS Digital—for GDPR-compliant data sharing backed by individual written informed consent. Most of all we thank all of the volunteers participating in Genes & Health.
Author contributions
Conceptualization: Ma. P. and C.L. Data curation/Software: S.H., S.Y., B.M.J., S.D. and Ma. P. Formal analysis: S.H., S.Y., B.M.J., E.G. and Ma. P. Methodology: S.D. and Ma. P. Visualization: S.H., S.Y. and Ma. P. Funding acquisition: C.L. and H.H. Project administration: C.L. and H.H. Supervision: Ma. P. and C.L. Writing—original draft: S.H., Ma. P. and C.L. Writing—review & editing: S.Y., B.M.J., S.D., H.H., Mu. P. and M.C.
Peer review
Peer review information
Nature Communications thanks Biqing Chen and Dominic Furniss for their contribution to the peer review of this work. A peer review file is available.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Data availability
All individual-level data is publicly available to bona fide researchers from the UK Biobank (https://www.ukbiobank.ac.uk/) or Genes & Health study (https://www.genesandhealth.org/). GWAS summary statistics have been deposited in the GWAS Catalogue (accession codes: GCST90271713 and GCST90271714). Lookups and druggable targets were derived from the GWAS Catalogue https://www.ebi.ac.uk/gwas/ and the OpenTargets Genetics data base (https://genetics.opentargets.org/).
Code availability
Associated code and scripts for the analysis are available on Github64 (https://github.com/pietznerm/gwas_rp).
Competing interests
Mu. P. has received partnership funding for the following: MRC Clinical Pharmacology Training Scheme (co-funded by MRC and Roche, UCB, Eli Lilly, and Novartis); and a Ph.D. studentship jointly funded by EPSRC and Astra Zeneca. Mu. P. also has unrestricted educational grant support for the UK Pharmacogenetics and Stratified Medicine Network from Bristol-Myers Squibb. Mu. P. has developed an HLA genotyping panel with MC Diagnostics, but does not benefit financially from this. He is part of the IMI Consortium ARDAT (www.ardat.org). None of the funding outlined above is related to the current paper. None of the other authors have competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors jointly supervised this work: Maik Pietzner, Claudia Langenberg.
A list of authors and their affiliations appears at the end of the paper.
Contributor Information
Maik Pietzner, Email: maik.pietzner@bih-charite.de.
Claudia Langenberg, Email: claudia.langenberg@bih-charite.de.
Supplementary information
The online version contains supplementary material available at 10.1038/s41467-023-41876-5.
References
- 1.Hughes M, et al. Prediction and impact of attacks of Raynaud’s phenomenon, as judged by patient perception. Rheumatology. 2015;54:1443–1447. doi: 10.1093/rheumatology/kev002. [DOI] [PubMed] [Google Scholar]
- 2.De Angelis R, Salaffi F, Grassi W. Health-related quality of life in primary Raynaud phenomenon. J. Clin. Rheumatol. 2008;14:206–210. doi: 10.1097/RHU.0b013e31817a2485. [DOI] [PubMed] [Google Scholar]
- 3.Fábián B, Csiki Z, Bugán A. Raynaud–szindrómás betegek életminőségének jellemzői. Orv. Hetil. 2018;159:636–641. doi: 10.1556/650.2018.31034. [DOI] [PubMed] [Google Scholar]
- 4.Wigley FM, Flavahan NA. Raynaud’s phenomenon. N. Engl. J. Med. 2016;375:556–565. doi: 10.1056/NEJMra1507638. [DOI] [PubMed] [Google Scholar]
- 5.Rirash, F. et al. Calcium channel blockers for primary and secondary Raynaud’s phenomenon. Cochrane Database Syst. Rev. 2017, (2017). [DOI] [PMC free article] [PubMed]
- 6.Belch J, et al. ESVM guidelines—the diagnosis and management of Raynaud’s phenomenon. Vasa. 2017;46:413–423. doi: 10.1024/0301-1526/a000661. [DOI] [PubMed] [Google Scholar]
- 7.Su, K. Y. C. et al. Vasodilators for primary Raynaud’s phenomenon. Cochrane Database Syst. Rev. 2021, (2021). [DOI] [PMC free article] [PubMed]
- 8.Ennis D, Ahmad Z, Anderson MA, Johnson SR. Botulinum toxin in the management of primary and secondary Raynaud’s phenomenon. Best Pract. Res. Clin. Rheumatol. 2021;35:101684. doi: 10.1016/j.berh.2021.101684. [DOI] [PubMed] [Google Scholar]
- 9.Cherkas LF, et al. Heritability of Raynaud’s phenomenon and vascular responsiveness to cold: a study of adult female twins. Arthritis Care Res. 2007;57:524–528. doi: 10.1002/art.22626. [DOI] [PubMed] [Google Scholar]
- 10.Hur YM, et al. Feeling of cold hands and feet is a highly heritable phenotype. Twin Res. Hum. Genet. 2012;15:166–169. doi: 10.1375/twin.15.2.166. [DOI] [PubMed] [Google Scholar]
- 11.Smyth AE, Hughes AE, Bruce IN, Bell AL. A case-control study of candidate vasoactive mediator genes in primary Raynaud’s phenomenon. Rheumatology. 1999;38:1094–1098. doi: 10.1093/rheumatology/38.11.1094. [DOI] [PubMed] [Google Scholar]
- 12.Shemirani AH, et al. Polymorphism of clotting factors in Hungarian patients with Raynaud’s. Blood Coagul. Fibrinolysis. 2011;22:56–59. doi: 10.1097/MBC.0b013e32834234fe. [DOI] [PubMed] [Google Scholar]
- 13.Susol E, et al. A two-stage, genome-wide screen for susceptibility loci in primary Raynaud’s phenomenon. Arthritis Rheum. 2000;43:1641–1646. doi: 10.1002/1529-0131(200007)43:7<1641::AID-ANR30>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 14.Munir S, Freidin MB, Brain S, Williams FMK. Association of Raynaud’s phenomenon with a polymorphism in the NOS1 gene. PLoS ONE. 2018;13:1–8. doi: 10.1371/journal.pone.0196279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bycroft C, et al. The UK Biobank resource with deep phenotyping and genomic data. Nature. 2018;562:203–209. doi: 10.1038/s41586-018-0579-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang, X. & Sun, Y. The predictive role of adra2a rs1800544 and htr3b rs3758987 polymorphisms in motion sickness susceptibility. Int. J. Environ. Res. Public Health18, 1–51 (2021). [DOI] [PMC free article] [PubMed]
- 17.Chotani MA, Flavahan S, Mitra S, Daunt D, Flavahan NA. Silent α(2C)-adrenergic receptors enable cold-induced vasoconstriction in cutaneous arteries. Am. J. Physiol.—Hear. Circ. Physiol. 2000;278:1075–1083. doi: 10.1152/ajpheart.2000.278.4.H1075. [DOI] [PubMed] [Google Scholar]
- 18.Freedman RR, Sabharwal SC, Desai N, Wenig P, Mayes M. Increased α‐adrenergic responsiveness in idiopathic Raynaud’s disease. Arthritis Rheum. 1989;32:61–65. doi: 10.1002/anr.1780320110. [DOI] [PubMed] [Google Scholar]
- 19.Freedman RR, Moten M, Migaly P, Mayes M. Cold‐induced potentiation of α2‐adrenergic vasoconstriction in primary Raynaud’s disease. Arthritis Rheum. 1993;36:685–690. doi: 10.1002/art.1780360517. [DOI] [PubMed] [Google Scholar]
- 20.Buniello A, et al. The NHGRI-EBI GWAS catalog of published genome-wide association studies, targeted arrays and summary statistics 2019. Nucleic Acids Res. 2019;47:D1005–D1012. doi: 10.1093/nar/gky1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ochoa D, et al. Open Targets Platform: supporting systematic drug-target identification and prioritisation. Nucleic Acids Res. 2021;49:D1302–D1310. doi: 10.1093/nar/gkaa1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.GTEx Consortium. The GTEx Consortium atlas of genetic regulatory effects across human tissues. Science369, 1318–1330 (2020). [DOI] [PMC free article] [PubMed]
- 23.Küster MM, et al. Epigenetic inactivation of the tumor suppressor IRX1 occurs frequently in lung adenocarcinoma and its silencing is associated with impaired prognosis. Cancers (Basel). 2020;12:1–20. doi: 10.3390/cancers12123528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aoki A, et al. SNPs on chromosome 5p15.3 associated with myocardial infarction in Japanese population. J. Hum. Genet. 2011;56:47–51. doi: 10.1038/jhg.2010.141. [DOI] [PubMed] [Google Scholar]
- 25.Sakaue S, et al. A cross-population atlas of genetic associations for 220 human phenotypes. Nat. Genet. 2021;53:1415–1424. doi: 10.1038/s41588-021-00931-x. [DOI] [PubMed] [Google Scholar]
- 26.Koyama S, et al. Population-specific and trans-ancestry genome-wide analyses identify distinct and shared genetic risk loci for coronary artery disease. Nat. Genet. 2020;52:1169–1177. doi: 10.1038/s41588-020-0705-3. [DOI] [PubMed] [Google Scholar]
- 27.Vuckovic D, et al. The Polygenic and Monogenic Basis of Blood Traits and Diseases. Cell. 2020;182:1214–1231.e11. doi: 10.1016/j.cell.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen, M. H. et al. Trans-ethnic and ancestry-specific blood-cell genetics in 746,667 individuals from 5 global populations. Cell182, 1198–1213.e14 (2020). [DOI] [PMC free article] [PubMed]
- 29.Aragam, K. G. et al. Discovery and systematic characterization of risk variants and genes for coronary artery disease in over a million participants. medRxiv10.1101/2021.05.24.21257377 (2021). [DOI] [PMC free article] [PubMed]
- 30.Finer S, et al. Cohort Profile: East London Genes & Health (ELGH), a community-based population genomics and health study in British Bangladeshi and British Pakistani people. Int. J. Epidemiol. 2020;49:20–21i. doi: 10.1093/ije/dyz174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.O’Connor LJ, Price AL. Distinguishing genetic correlation from causation across 52 diseases and complex traits. Nat. Genet. 2018;50:1728–1734. doi: 10.1038/s41588-018-0255-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Licata L, et al. SIGNOR 2.0, the SIGnaling Network Open Resource 2.0: 2019 update. Nucleic Acids Res. 2020;48:D504–D510. doi: 10.1093/nar/gkz949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Edwards JM, Phinney ES, Taylor LM, Keenan EJ, Porter JM. α2-Adrenergic receptor levels in obstructive and spastic Raynaud’s syndrome. J. Vasc. Surg. 1987;5:38–45. [PubMed] [Google Scholar]
- 34.Flavahan NA. A vascular mechanistic approach to understanding Raynaud phenomenon. Nat. Rev. Rheumatol. 2015;11:146–158. doi: 10.1038/nrrheum.2014.195. [DOI] [PubMed] [Google Scholar]
- 35.Herrick AL, et al. A double-blind, randomized, placebo-controlled crossover trial of the α2c-adrenoceptor antagonist orm-12741 for prevention of cold-induced vasospasm in patients with systemic sclerosis. Rheumatology. 2014;53:948–952. doi: 10.1093/rheumatology/ket421. [DOI] [PubMed] [Google Scholar]
- 36.Gyires K, Zádori ZS, Török T, Mátyus P. α2-Adrenoceptor subtypes-mediated physiological, pharmacological actions. Neurochem. Int. 2009;55:447–453. doi: 10.1016/j.neuint.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 37.Hunter JC, et al. Assessment of the role of α2-adrenoceptor subtypes in the antinociceptive, sedative and hypothermic action of dexmedetomidine in transgenic mice. Br. J. Pharmacol. 1997;122:1339–1344. doi: 10.1038/sj.bjp.0701520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cooke JP, et al. Role of digital artery adrenoceptors in Raynaud’s disease. Vasc. Med. 1997;2:1–7. doi: 10.1177/1358863X9700200101. [DOI] [PubMed] [Google Scholar]
- 39.Freedman RR, Baer RP, Mayes MD. Blockade of vasospastic attacks by alpha 2-adrenergic but not alpha 1-adrenergic antagonists in idiopathic Raynaud’s disease. Circulation. 1995;92:1448–1451. doi: 10.1161/01.CIR.92.6.1448. [DOI] [PubMed] [Google Scholar]
- 40.Johnson S, Iazzetta J, Dewar C. Severe Raynaud’s phenomenon with Yohimbine therapy for erectile dysfunction. J. Rheumatol. 2003;30:2503–2505. [PubMed] [Google Scholar]
- 41.Sandler B, Aronson P. Yohimbine-induced cutaneous drug eruption, progressive renal failure, and lupus-like syndrome. Urology. 1993;41:343–345. doi: 10.1016/0090-4295(93)90592-X. [DOI] [PubMed] [Google Scholar]
- 42.Varadi DP, Lawrence AM. Suppression of Raynaud’s phenomenon by methyldopa. Arch. Intern. Med. 1969;124:13–18. doi: 10.1001/archinte.1969.00300170015003. [DOI] [PubMed] [Google Scholar]
- 43.Guo X, et al. Homeobox gene IRX1 is a tumor suppressor gene in gastric carcinoma. Oncogene. 2010;29:3908–3920. doi: 10.1038/onc.2010.143. [DOI] [PubMed] [Google Scholar]
- 44.Gomez I, Foudi N, Longrois D, Norel X. The role of prostaglandin E2 in human vascular inflammation. Prostaglandins Leukot. Essent. Fat. Acids. 2013;89:55–63. doi: 10.1016/j.plefa.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 45.Ren J, Karpinski E, Benishin CG. Prostaglandin E2 contracts vascular smooth muscle and inhibits potassium currents in vascular smooth muscle cells of rat tail artery. J. Pharmacol. Exp. Ther. 1995;275:710–719. [PubMed] [Google Scholar]
- 46.Marceau F, Regoli D. Bradykinin receptor ligands: therapeutic perspectives. Nat. Rev. Drug Discov. 2004;3:845–852. doi: 10.1038/nrd1522. [DOI] [PubMed] [Google Scholar]
- 47.Freedman RR, Girgis R, Mayes MD. Abnormal responses to endothelial agonists in Raynaud’s phenomenon and scleroderma. J. Rheumatol. 2001;28:119–121. [PubMed] [Google Scholar]
- 48.Bedarida G, Kim D, Blaschke TF, Hoffman BB. Venodilation in Raynaud’s disease. Lancet (Lond., Engl.) 1993;342:1451–1454. doi: 10.1016/0140-6736(93)92932-J. [DOI] [PubMed] [Google Scholar]
- 49.Rosengren AH, et al. Overexpression of alpha2A-adrenergic receptors contributes to type 2 diabetes. Science. 2010;327:217–220. doi: 10.1126/science.1176827. [DOI] [PubMed] [Google Scholar]
- 50.Vujkovic M, et al. Discovery of 318 new risk loci for type 2 diabetes and related vascular outcomes among 1.4 million participants in a multi-ancestry meta-analysis. Nat. Genet. 2020;52:680–691. doi: 10.1038/s41588-020-0637-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Morrison SF. Differential control of sympathetic outflow. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2001;281:R683–R698. doi: 10.1152/ajpregu.2001.281.3.R683. [DOI] [PubMed] [Google Scholar]
- 52.Carnovale C, et al. Beta-blocker-associated hypoglycaemia: new insights from a real-world pharmacovigilance study. Br. J. Clin. Pharmacol. 2021;87:3320–3331. doi: 10.1111/bcp.14754. [DOI] [PubMed] [Google Scholar]
- 53.Gamazon ER, et al. Using an atlas of gene regulation across 44 human tissues to inform complex disease- and trait-associated variation. Nat. Genet. 2018;50:956–967. doi: 10.1038/s41588-018-0154-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sudlow C, et al. UK Biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12:1–10. doi: 10.1371/journal.pmed.1001779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mbatchou J, et al. Computationally efficient whole-genome regression for quantitative and binary traits. Nat. Genet. 2021;53:1097–1103. doi: 10.1038/s41588-021-00870-7. [DOI] [PubMed] [Google Scholar]
- 56.Bulik-sullivan, B. K. et al. LD Score regression distinguishes confounding from polygenicity in genome-wide association studies. Nat. Publ. Gr. 47, 291–295 (2015). [DOI] [PMC free article] [PubMed]
- 57.Wang G, Sarkar A, Carbonetto P, Stephens M. A simple new approach to variable selection in regression, with application to genetic fine mapping. J. R. Stat. Soc. Ser. B Stat. Methodol. 2020;82:1273–1300. doi: 10.1111/rssb.12388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Giambartolomei, C. et al. Bayesian test for colocalisation between pairs of genetic association studies using summary statistics. PLoS Genet. 10, e1004383 (2014). [DOI] [PMC free article] [PubMed]
- 59.Wallace C. Eliciting priors and relaxing the single causal variant assumption in colocalisation analyses. PLoS Genet. 2020;16:1–20. doi: 10.1371/journal.pgen.1008720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gamazon, E. R. et al. A gene-based association method for mapping traits using reference transcriptome data. Nat. Genet.47, 1091–1098 (2015). [DOI] [PMC free article] [PubMed]
- 61.Denaxas S, et al. Mapping the Read2/CTV3 controlled clinical terminologies to Phecodes in UK Biobank primary care electronic health records: implementation and evaluation. AMIA Annu. Symp. Proc. AMIA Symp. 2021;2021:362–371. [PMC free article] [PubMed] [Google Scholar]
- 62.Wu P, et al. Mapping ICD-10 and ICD-10-CM Codes to phecodes: workflow development and initial evaluation. JMIR Med. Inform. 2019;7:1–13. doi: 10.2196/14325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bastarache L. Using phecodes for research with the electronic health record: from PheWAS to PheRS. Annu. Rev. Biomed. Data Sci. 2021;4:1–19. doi: 10.1146/annurev-biodatasci-122320-112352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hartmann, S. et al. ADRA2A and IRX1 are putative risk genes for Raynaud’s phenomenon. Zenodo10.5281/zenodo.8082736 (2023). [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Description of Additional Supplementary Files
Data Availability Statement
All individual-level data is publicly available to bona fide researchers from the UK Biobank (https://www.ukbiobank.ac.uk/) or Genes & Health study (https://www.genesandhealth.org/). GWAS summary statistics have been deposited in the GWAS Catalogue (accession codes: GCST90271713 and GCST90271714). Lookups and druggable targets were derived from the GWAS Catalogue https://www.ebi.ac.uk/gwas/ and the OpenTargets Genetics data base (https://genetics.opentargets.org/).
Associated code and scripts for the analysis are available on Github64 (https://github.com/pietznerm/gwas_rp).