Abstract
Bifidobacterium animalis subsp. lactis GCL2505 has been shown to have some positive effects on health, including improved defecation frequency and reduced visceral fat. These effects are thought to be due to GCL2505′s unique ability to reach the intestine in a viable form and proliferate after a single intake. This leads to an increased number of intestinal bifidobacteria. This randomized, double-blind, placebo-controlled, parallel-group study was conducted to confirm that intake of GCL2505 and inulin (a prebiotic) improve cognitive function (n = 80). Participants consumed test drinks containing 1 × 1010 colony-forming units of GCL2505 per 100 g and 2.0 g of inulin per 100 g for 12 weeks. The change in cognitive function assessment scores was set as the primary endpoint. There were significant improvements in scores in the neurocognitive index domain, which is an assessment of overall cognitive function, in addition to overall attention, cognitive flexibility, and executive function domains. The intervention significantly increased the number of fecal bifidobacteria and affected the levels of several inflammatory markers. These results suggest that intake of GCL2505 and inulin improves cognitive function by improving the intestinal environment and alleviating inflammation.
Keywords: Bifidobacterium animalis subsp. lactis, probiotics, visceral fat, metabolic syndrome, gut microbacteria, anti-inflammatory, mild cognitive impairment, aging
1. Introduction
It is estimated that more than 55 million people have dementia worldwide, and nearly 10 million new cases of the disease occur each year. Dementia is now the seventh leading cause of death and one of the leading causes of disability and dependency among the elderly. The global economic cost of dementia has reached USD 1.3 trillion, approximately half of which is attributed to care provided by informal caregivers (e.g., family members and close friends), who provide an average of 5 h of care and supervision per day [1]. Furthermore, it is estimated that the number of people with dementia will continue to rise, reaching 78 million by 2030 and 139 million by 2050 [2].
Alzheimer’s disease (AD), a disease of progressive cognitive decline, is the most common form of dementia, with a prevalence of more than 60%, and represents a serious threat to public health [1]. Although the pathogenesis of AD remains to be elucidated, a number of therapeutic approaches have been developed based on the “amyloid cascade hypothesis”, that neurofibrillary tangles are caused by the increase and accumulation of amyloid-β (Aβ) in the brain, followed by abnormal phosphorylation of tau protein [3,4]. AD is a chronic disease of the brain that progresses over decades, with Aβ accumulation in the brain beginning decades before clinical symptoms appear [5]. Once AD develops, it is difficult to improve its symptoms, and currently available AD drugs can only slow the progression of the disease; thus, there is no fundamental cure. For this reason, it is desirable to prevent the onset of AD. Mild cognitive impairment (MCI) is a pre-dementia condition characterized as a cognitive state between normal cognitive aging and dementia and is associated with an increased risk of developing AD [6]. Clinical studies have shown that patients with MCI progress to AD at a rate of 10% to 15% per year [7]. Meanwhile, it has been reported that it is possible to regress from MCI to a cognitively normal state [8,9]. Therefore, implementing appropriate intervention at the MCI stage is critical to reduce the number of patients with dementia. In addition, AD is not only caused by genetic factors and aging but also by environmental factors such as lifestyle habits, including sleep and diet. Accordingly, it is desirable for substances that contribute to the prevention of AD to be included in daily-use foods and used on a routine basis [10].
Various studies have investigated the triggers of AD, clarifying the relationship between obesity and cognitive function as well as the mechanisms of obesity-induced cognitive decline. An observational study reported that cognitive function was lower in participants with more visceral fat [11]. Another study reported that the insulin resistance that developed with obesity promoted the accumulation of Aβ and the formation of neurofibrillary tangles [12]. The association between inflammation and cognitive function has also received attention. Acute and chronic systemic inflammation associated with increased levels of tumor necrosis factor (TNF)-α, a typical inflammation-inducing cytokine, are associated with increased cognitive decline in AD [13]. Thus, management of environmental factors is now considered important for the prevention of AD, and lifestyle interventions aimed at preventing the onset and progression of AD as well as preventive measures in daily life with functional foods are necessary as one approach to solving the problem [14]. In addition, food ingredients such as chlorogenic acid [15], propolis extract [16], and astaxanthin [17] have been reported to improve cognitive function, while probiotics are expected to play a major role in future dementia countermeasures, based on the results of meta-analyses showing that probiotics improve cognitive function in patients with MCI [18]. The cognitive improvement effect of the probiotic bacterial strain Lactobacillus rhamnosus GG might be attributable to the improvement of signaling markers [19]. Meanwhile, intake of Bifidobacterium breve A1 might contribute to the modulation of brain immune response through the production of short-chain fatty acids (SCFAs), thereby contributing to the improvement of cognitive function [20,21]. It has also been reported that intake of Lactiplantibacillus plantarum OLL2712 protects against memory decline in the elderly due to its high IL-10 induction activity in immune cells [22].
Bifidobacterium animalis subsp. lactis GCL2505, a probiotic strain originally isolated from the feces of healthy adults [23,24,25], has been shown to reduce visceral fat [26]. Horiuchi et al. reported that GCL2505 affects host metabolic homeostasis (e.g., enhanced glucose tolerance, suppressed body fat accumulation) in a GPR43-dependent manner, due to enhanced SCFA production in the gut [27]. In clinical trials, daily consumption of fermented milk containing GCL2505 was shown to reduce abdominal visceral fat mass [28]. Furthermore, clinical studies have shown that GCL2505, when taken in combination with inulin [29], a typical prebiotic material, increases the total number of bifidobacteria in the gut more than GCL2505 alone [30].
In our study based on previous results, it was newly found that the combined intake of GCL2505 and inulin may reduce the risk of cognitive decline via visceral fat reduction. We also speculate that the anti-inflammatory effect of acetic acid produced by GCL2505 in the gut might improve cognitive function. SCFAs are known to exhibit anti-inflammatory effects by modulating immune cell chemotaxis as well as the release of reactive oxygen species (ROS) and cytokines [31]. However, it has not yet been demonstrated that the visceral-fat-reducing and anti-inflammatory effects of probiotics contribute directly to improving cognitive function. Therefore, in the present study, we conducted a randomized, double-blind, placebo-controlled, parallel-group study to test the hypothesis that the combined intake of GCL2505 and inulin improve cognitive function.
2. Materials and Methods
2.1. Participants
Participants were Japanese men and women between the ages of 50 and 80 years at the time of consent, who satisfied the inclusion criteria, did not satisfy any of the exclusion criteria, and were deemed eligible to participate by the study investigator. In this study, participants had to be selected from healthy people, not sick people, because the effects of food consumption—bifidobacteria and inulin—had to be confirmed. Young adults with documented cognitive decline were excluded from the study because they were more likely to have AD or other illnesses. Participants had to be drawn from healthy individuals with mild cognitive decline due to aging. The inclusion criteria were as follows: (1) score of 24 or higher on the Mini Mental State Examination—Japanese (MMSE-J), 17 or higher on the Japanese version of the Montreal Cognitive Assessment (MoCa-J), and 5 or less on the Geriatric Depression Scale—short version—Japanese (GDS-S-J); (2) subjective symptoms of memory loss or reported by close relatives or acquaintances to have other symptoms of memory loss; and (3) fully informed of the purpose and content of the study, deemed to have the capacity to consent, and volunteered of their own accord to participate in the study based on a thorough understanding of the purpose and content of the study, and provided written informed consent to participate in the study. Exclusion criteria were as follows: (1) current or past history of mental disorders (including depressive symptoms), cerebrovascular diseases, and sleep disorders; (2) serious liver, kidney, heart, respiratory, endocrine, or metabolic diseases; (3) smoker; (4) regular alcohol user (consuming ≥ 60 g pure alcohol equivalent daily) with an extremely irregular diet; (5) unable to follow the restrictions on foods or supplements that affect the intestinal environment during the study period; (6) use of antibiotics within 1 month prior to the start of the study; (7) have undergone digestive surgery (excluding appendicitis); (8) have experienced allergies to any of the study food ingredients; (9) currently taking medications that may affect cognitive function (e.g., antipsychotic, anxiolytic, antidepressant, antiparkinsonian, antisomatics, antiepileptic, and anticoagulant medications); (10) visual or hearing impairment that may interfere with cognitive function tests; (11) routinely consume foods or supplements that may affect cognitive function; (12) current or former drug or alcohol dependence; (13) participation in research involving the ingestion of other foods or the use of pharmaceuticals, the application of cosmetics or pharmaceuticals, or participation in other research while participating in this study; and (14) deemed ineligible by the principal investigator.
2.2. Test Foods
The test products were a dairy drink (active drink) containing inulin (Orafti GR; BENEO GmbH, Mannheim, Germany) and GCL2505 or placebo. The active drink contained 1 × 1010 colony-forming units of GCL2505 and 2.0 g of inulin per 100 g. The placebo was prepared using the same ingredients as the active drink, with the addition of food-grade acetic acid and lactic acid to adjust the flavor and pH; the basic ingredients were skim milk powder, fructose, dextrose, sucrose, yeast extract, acidifier, stabilizer, and flavoring. The nutritional details of the test products are shown in Table 1.
Table 1.
Nutritional details of the test drinks.
| Placebo | Active | |
|---|---|---|
| Energy, kcal/100 g | 48.0 | 52.0 |
| Moisture, g/100 g | 86.9 | 84.9 |
| Protein, g/100 g | 2.8 | 2.8 |
| Fat, g/100 g | 0.1 | 0.1 |
| Carbohydrate, g/100 g | 9.1 | 11.2 |
| Ash, g/100 g | 1.1 | 1.1 |
The active drink contained 2.0 g of inulin and 1.0 × 1010 colony-forming units of GCL2505.
2.3. Experimental Design
This was a randomized, placebo-controlled, double-blind, parallel-group study. Participants were stratified by age at screening and sex, and Cognitrax (short), MMSE-J, and MoCa-J scores served as stratification factors for randomizing in block sizes of four by computer-generated randomization to two groups (1:1). The controller (allocation manager) assigned the two groups to the test drink intake group and the control food intake group. For sample size, the final target number of subjects was set at 80, referring to previous reports on probiotic-induced cognitive function [21,22]. Participants in the active and placebo groups consumed 100 g of dairy beverage once daily for 12 weeks. Both the participants and observers were blinded to the group allocation for the duration of the study. Double blinding was accomplished by labeling the test drink with only an identification number. The change in Cognitrax (long) scores between weeks 0 and 12 was set as the primary endpoint. The secondary endpoints were Cognitrax (long) scores between weeks 0 and 8, fecal bifidobacteria, SF-36v2® scores, blood inflammation markers (Olink Target 96 Inflammation), blood high-sensitivity C-reactive protein (hs-CRP), blood interleukin (IL)-1β, and serum brain-derived neurotrophic factor (BDNF). The study was conducted at Nihonbashi Cardiology Clinic (Tokyo, Japan) from September to December 2022 by K.S.O. Corporation (Tokyo, Japan), a contract research organization, and was registered with the University Hospital Medical Information Network Clinical Trials Registry (UMIN-CTR) “http://www.umin.ac.jp/ctr/index.htm (accessed on 15 July 2022)” as UMIN000048386. This article conforms to the Consolidated Standards of Reporting Trials (CONSORT) 2010 guidelines (Supplementary Materials, Table S1).
2.4. Cognitrax Test
Participants’ cognitive function was measured using Cognitrax, a computer-based battery of cognitive function tests that was developed as a Japanese version of CNS Vital Signs [32]. Based on a previous study [33], the cognitive function tests were administered in the following order: verbal memory test, visual memory test, finger tapping test, symbol digit coding test, Stroop test, shift attention test, continuous performance test, perception of emotion test, nonverbal reasoning test, and four-part continuous performance test.
2.5. Quality of Life Test
The SF-36v2®, a widely used quality of life rating scale, consists of the following eight scales: “physical functioning”, “role physical”, “bodily pain”, “general health perceptions”, “vitality”, “social functioning”, “role emotional”, and “mental health”. The score for each scale was estimated based on national norms (norm-based scoring) and calculated as a standard score (mean, 50) [34].
2.6. Mental Health Status
The Japanese version of the World Health Organization Five Well-Being Index (WHO-5-J) survey was conducted at weeks 0, 8, and 12 [35] to confirm that participants had no abnormal mental health status during the study period.
2.7. Biochemical Parameters
Blood pressure, pulse rate, and body weight were measured at weeks 0, 8, and 12. The concentrations of biochemical parameters were also measured at weeks 0 and 12. Blood samples were drawn from each participant after 4 h of no food or drink except water (fasting) prior to testing. Biochemical parameters included hematological tests (white blood cell count, red blood cell count, hemoglobin, hematocrit, mean corpuscular volume, mean corpuscular hemoglobin, mean corpuscular hemoglobin concentration, platelet count, leukogram), biochemical tests (total protein, albumin, total bilirubin, aspartate aminotransferase, alanine aminotransferase, lactate dehydrogenase (IFCC), alkaline phosphatase (IFCC), gamma-glutamyltransferase, urea nitrogen, creatinine, uric acid, sodium, chlorine, potassium, calcium, total cholesterol, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, triglycerides, phospholipids, glucose, HbA1c (NGSP), insulin), and urinalysis (protein, sugar, bilirubin, urinary ketone bodies, occult blood reaction, urobilinogen, pH, and specific gravity). In addition, serum BDNF was quantified. All of these tests were performed at LSI Medience Corporation (Tokyo, Japan).
2.8. Inflammatory Protein Profile
Blood inflammation markers in frozen serum were determined using Olink® Target 96 Inflammation Panels (Olink Proteomics AB, Uppsala, Sweden) with proximity expansion technology, a high-throughput multiplex proteomic immunoassay [36]. The panel contains 92 immune-related proteins, mostly cytokines and chemokines. The assay involves epitope-specific binding and hybridization of a set of paired oligonucleotide antibody probes, followed by amplification using quantitative PCR, normalized on a log base 2 to Olink’s own relative abundance units (normalized protein expression values). Quality control was performed on samples (using spiked internal controls) and external controls for each sample plate. This inspection was performed by Pharma Foods Corporation (Tokyo, Japan). In addition, blood hs-CRP (LSI Medience Corporation) and blood IL-1β (Filgen, Inc., Aichi, Japan) were quantified.
2.9. Fecal Samples
Fecal samples were submitted at weeks 0 and 12. Fecal samples were collected at home between 7 and 2 days before the specified visit. The submitted samples were promptly transported to the laboratory by refrigerated transport.
2.10. Fecal DNA Extraction
Bacterial DNA was extracted from fecal samples using the ISOSPIN Fecal DNA Kit (Nippon Gene Co., Ltd., Tokyo, Japan), following the procedure of Tourlousse et al. [37]. Specifically, a sample (here, 0.2 g fecal sample), 700 μL of FE1 buffer, and 10 μL of RNase were added to a tube with attached beads. A bead-beating homogenizer (FastPrep-24; MP Biomedicals, Irvine, CA) was used at a rate of 6 m/s for 1 min to crush the cells. The process was repeated three times, during which the sample was kept at room temperature for 5 min. Then, 90 µL of FE2 buffer was added and the samples were centrifuged at 12,000× g for 15 min. The supernatant (up to 500 µL) was collected and mixed with FB buffer and isopropanol, each at 0.4× the volume of the supernatant obtained. Finally, the sample was loaded onto a spin column and washed according to the manufacturer’s instructions. Purified DNA was eluted with 50 µL of Tris-EDTA buffer (pH 8.0).
2.11. Fecal Bifidobacteria
Following Tanaka et al. [38], real-time polymerase chain reaction (PCR) was performed using genus-specific primers capable of detecting Bifidobacterium spp., including GCL2505. The primer sequences were as follows: Bifidobacterium spp. sense primer, 5′-GATTCTGGCTCAGGATGAACGC-3′; Bifidobacterium spp. antisense primer, 5′-CTGATAGGACGCGACCCCAT-3′. Each PCR reaction mixture consisted of 20 pmol of each primer in a total volume of 10 µL; 5 µL of SYBR® premix Ex taq (Takara Bio, Shiga, Japan); and 1 µL of DNA solution [38]. This inspection was performed by the Kyoto Institute of Nutrition and Pathology (Kyoto, Japan).
2.12. Statistical Analysis
All measurements were expressed as mean and standard deviation (SD). All statistical analyses were performed using IBM® SPSS® Statistics 27 (IBM Corp., Armonk, NY, USA). A p-value < 0.05 was used as the threshold for determining significance. As basic statistics, means and SDs are expressed to the nearest significant digit, percentages are expressed to one decimal place, and finally digits were adjusted by rounding. Missing data were treated as missing values and no surrogate values were used; Cognitrax (Long) statistical analyses were performed with paired t-tests in order to compare the test results at the start date of the intake (week 0) with those at 8 and 12 weeks after intake. For the other items, Dunnett’s test (two-tailed) was used to compare the test results at the start of intake (week 0) with those at 8 and 12 weeks after the start of intake, and the Wilcoxon signed rank test was used for qualitative items. Comparisons between the active and placebo groups at each examination time were statistically analyzed with an unpaired t-test (two-tailed), and a Wilcoxon’s rank-sum test was used to compare the qualitative endpoints.
3. Results
3.1. Analysis of the Participant Population
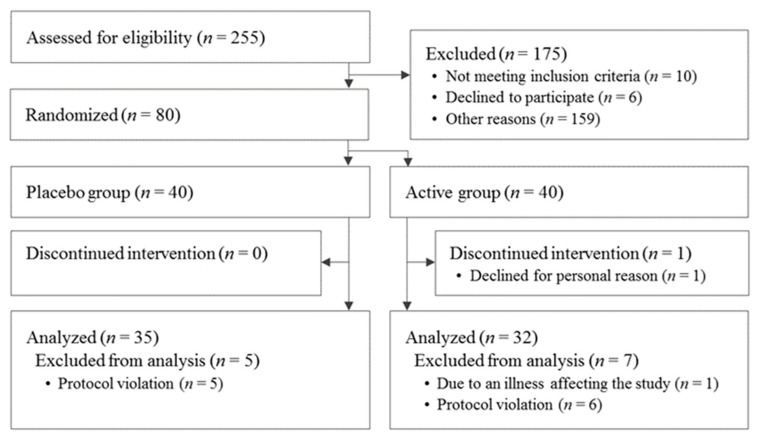
The participant selection process is shown in Figure 1. A total of 255 participants were screened for this study. After screening, 80 participants were eligible: 40 were assigned to the active group and 40 were assigned to the placebo. A significant difference in alkaline phosphatase levels between the active and placebo groups was observed at the beginning of the study but was deemed acceptable because it was within the reference range. For the other items, there were no differences in the baseline characteristics of the participants’ data (Table 2). By the end of the study, one participant from the active group withdrew for personal reasons. After the completion of the entire study, one participant from the placebo group was dropped due to an extremely irregular lifestyle. One participant from the active group was dropped due to a confirmed illness unrelated to the study that may have affected the results. In addition, nine participants were also excluded because they were found to have consumed drugs or foods during the study period that might have affected the results (n = 5 from the active group and n = 4 from the placebo group). Another participant in the active group was dropped due to partial missing primary-endpoint data. Thus, a total of 67 patients (32 in the active group and 35 in the placebo group) were included in the analysis. Moreover, four participants with reduced WHO-5-J scores were also excluded for Cognitrax analysis (n = 1 from the active group and n = 3 from the placebo group) because they had a score of ≤50, which is used as the cut-off for assigning a ‘screening diagnosis’ of depression in the global version of WHO-5 [39]; reduced WHO-5-J scores might indicate the possibility of earlier depression caused by isolation due to the COVID-19 pandemic, and thus Cognitrax tests may not have been performed properly in these participants. There were no reported harms or unintended effects in each group.
Figure 1.
Flowchart of participant selection.
Table 2.
Baseline characteristics of the participants (placebo group: n = 40; active group: n = 40).
| Placebo Group | Active Group | p-Value | |
|---|---|---|---|
| Age, years | 62.7 (6.9) | 64.6 (7.1) | 0.229 |
| MMSE-J | 28.0 (1.6) | 28.0 (1.3) | 0.878 |
| Corrected MOCA-J | 22.9 (1.8) | 22.9 (2.1) | 0.955 |
| GDS-S-J | 2.1 (1.6) | 1.8 (1.7) | 0.372 |
| Height, cm | 161.5 (9.0) | 161.8 (8.0) | 0.907 |
| Body weight, kg | 59.0 (11.3) | 59.5 (12.1) | 0.842 |
| Body mass index, kg/m2 | 22.4 (2.8) | 22.6 (3.1) | 0.861 |
| Systolic blood pressure, mmHg | 129.5 (17.0) | 128.3 (16.3) | 0.733 |
| Diastolic blood pressure, mmHg | 77.8 (12.8) | 75.7 (10.7) | 0.439 |
| Heartbeat, bpm | 70.6 (10.7) | 71.1 (12.0) | 0.830 |
| White blood cell count, /µL | 5817.5 (1731.7) | 5685.0 (1543.8) | 0.719 |
| Red blood cell count, ×10⁴/µL | 446 (40.9) | 445.5 (41.1) | 0.957 |
| Hemoglobin, g/dL | 13.7 (1.3) | 13.7 (1.1) | 0.978 |
| Hematocrit, % | 43.3 (3.7) | 43.4 (3.3) | 0.914 |
| Platelet count, ×10⁴/μL | 24.6 (5.1) | 23.5 (5.1) | 0.354 |
| Mean corpuscular volume, fL | 97.3 (4.3) | 97.6 (3.8) | 0.764 |
| Mean corpuscular hemoglobin, pg | 30.9 (1.8) | 30.9 (1.3) | 0.966 |
| Mean corpuscular hemoglobin concentration, % | 31.7 (1.1) | 31.7 (0.9) | 0.711 |
| Neutrophil ratio, % | 54.9 (7.7) | 55.4 (8.8) | 0.777 |
| Lymphocyte ratio, % | 35.1 (6.7) | 34.2 (7.7) | 0.573 |
| Monocyte ratio, % | 6.3 (1.8) | 6.0 (1.5) | 0.501 |
| Eosinophil ratio, % | 2.9 (2.0) | 3.6 (2.5) | 0.173 |
| Basophil ratio, % | 0.8 (0.3) | 0.8 (0.3) | 0.461 |
| Total serum protein, g/dL | 7.1 (0.4) | 7.1 (0.4) | 0.358 |
| Albumin, g/dL | 4.4 (0.2) | 4.4 (0.2) | 0.718 |
| Aspartate aminotransferase, U/L | 22.0 (6.2) | 22.2 (9.6) | 0.923 |
| Alanine aminotransferase, U/L | 18.1 (9.0) | 17.5 (9.1) | 0.777 |
| Lactate dehydrogenase, U/L | 185.1 (23.8) | 187.5 (23.5) | 0.655 |
| Total bilirubin, mg/dL | 1.0 (0.4) | 0.9 (0.3) | 0.175 |
| Alkaline phosphatase, U/L | 59.8 (14.6) | 66.1 (13.0) | 0.045 |
| γ-Glutamyl transpeptidase, U/L | 26.3 (13.7) | 30.4 (32.7) | 0.467 |
| Blood urea nitrogen, mg/dL | 14.8 (2.5) | 14.4 (3.4) | 0.594 |
| Creatinine, mg/dL | 0.8 (0.2) | 0.8 (0.1) | 0.788 |
| Uric acid, mg/dL | 5.6 (1.6) | 5.1 (1.3) | 0.181 |
| Sodium (Na), mEq/L | 141.5 (1.7) | 141.2 (1.9) | 0.392 |
| Chlorine (Cl), mEq/L | 104.3 (2.0) | 104.1 (2.1) | 0.664 |
| Potassium (K), mEq/L | 4.3 (0.4) | 4.3 (0.3) | 0.667 |
| Calcium (Ca), mg/dL | 9.3 (0.3) | 9.3 (0.3) | 0.966 |
| Total cholesterol, mg/dL | 216.3 (35.0) | 212.7 (36.0) | 0.649 |
| LDL cholesterol, mg/dL | 125.0 (30.8) | 118.9 (25.6) | 0.338 |
| HDL cholesterol, mg/dL | 71.3 (17.0) | 73.1 (24.1) | 0.705 |
| Triglycerides, mg/dL | 98.8 (49.1) | 103.0 (52.6) | 0.711 |
| Phospholipid, mg/dL | 233.9 (31.5) | 233.9 (37.9) | 0.995 |
| Glucose, mg/dL | 88.6 (8.4) | 87.5 (9.8) | 0.601 |
| HbA1c (NGSP), % | 5.5 (0.3) | 5.5 (0.3) | 0.778 |
| Urine pH | 6.2 (0.7) | 6.2 (0.8) | 0.759 |
All data are presented as mean (standard deviation). Comparisons between the placebo and active groups were tested by analysis of variance.
3.2. Cognitrax Test
The change in neurocognitive index domain score from week 0 to week 12 in the active group (5.5 ± 7.1) was greater than that in the placebo group (2.3 ± 4.0), and there was a statistically significant difference between them (p = 0.027 by the unpaired t-test). Furthermore, the changes in complex attention domain score (8.3 ± 11.8 vs. 3.2 ± 6.9, p = 0.041 by the unpaired t-test), cognitive flexibility domain score (9.8 ± 11.5 vs. 4.8 ± 6.7, p = 0.038 by the unpaired t-test), and executive function domain score (9.5 ± 11.8 vs. 4.5 ± 6.9, p = 0.044 by the unpaired t-test) in the active group from week 0 to 12 were significantly higher than those in the placebo group (Table 3). The results of the Cognitrax task to calculate scores for each domain are presented in Supplementary Materials, Table S2.
Table 3.
Post-intervention changes in each cognitive function parameter (placebo group: n = 32; active group: n = 31).
| Week 0 | Week 8 | Week 12 | ||||
|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | p-Value | Mean (SD) | p-Value | ||
| Neurocognitive index | Placebo | 103.5 (5.7) | 104.8 (4.9) | 0.090 | 105.7 (5.9) | 0.003 |
| Active | 101.6 (6.8) | 104.5 (8.2) | 0.045 | 107.2 (5.1) | <0.001 | |
| ∆ Neurocognitive index | Placebo | 1.4 (4.4) | 0.345 | 2.3 (4.0) | 0.027 | |
| Active | 2.9 (7.6) | 5.5 (7.1) | ||||
| Composite memory | Placebo | 105.3 (13.6) | 102.7 (15.9) | 0.264 | 102.6 (12.3) | 0.231 |
| Active | 104.4 (14.8) | 107.6 (13.6) | 0.147 | 107.2 (13.3) | 0.297 | |
| ∆ Composite memory | Placebo | −2.7 (13.2) | 0.070 | −2.8 (12.7) | 0.114 | |
| Active | 3.2 (12.1) | 2.8 (14.7) | ||||
| Verbal memory | Placebo | 105.3 (13.6) | 106.1 (15.0) | 0.746 | 105.1 (13.2) | 0.926 |
| Active | 104.6 (14.3) | 107.9 (13.6) | 0.129 | 108.5 (14.6) | 0.142 | |
| ∆ Verbal memory | Placebo | 0.8 (14.1) | 0.452 | −0.2 (13.3) | 0.241 | |
| Active | 3.3 (11.7) | 3.9 (14.5) | ||||
| Visual memory | Placebo | 103.7 (14.8) | 98.3 (15.7) | 0.035 | 99.2 (14.8) | 0.124 |
| Active | 103.3 (12.8) | 105.1 (11.8) | 0.495 | 103.7 (11.0) | 0.861 | |
| ∆ Visual memory | Placebo | −5.4 (14.0) | 0.047 | −4.5 (16.1) | 0.202 | |
| Active | 1.8 (14.3) | 3.9 (14.5) | ||||
| Psychomotor speed | Placebo | 106.3 (8.8) | 108.5 (9.3) | 0.045 | 108.3 (10.1) | 0.073 |
| Active | 106.2 (8.3) | 108.9 (8.4) | 0.016 | 108.6 (7.6) | 0.054 | |
| ∆ Psychomotor speed | Placebo | 2.1 (5.7) | 0.664 | 1.9 (5.8) | 0.720 | |
| Active | 2.8 (6.1) | 2.5 (6.9) | ||||
| Reaction time | Placebo | 94.7 (11.3) | 94.8 (11.8) | 0.906 | 98.8 (11.1) | <0.001 |
| Active | 96.6 (9.1) | 98.8 (10.6) | 0.112 | 100.8 (9.5) | 0.003 | |
| ∆ Reaction time | Placebo | 0.1 (6.0) | 0.230 | 4.2 (4.8) | 0.981 | |
| Active | 2.2 (7.3) | 4.2 (7.1) | ||||
| Complex attention | Placebo | 108.3 (8.9) | 111.9 (6.2) | 0.028 | 111.5 (6.4) | 0.015 |
| Active | 104.0 (11.2) | 105.2 (23.4) | 0.762 | 112.3 (4.7) | <0.001 | |
| ∆ Complex attention | Placebo | 3.6 (8.8) | 0.580 | 3.2 (6.9) | 0.041 | |
| Active | 1.2 (22.4) | 8.3 (11.8) | ||||
| Cognitive flexibility | Placebo | 102.8 (9.3) | 106.1 (7.3) | 0.004 | 107.5 (8.4) | <0.001 |
| Active | 96.7 (10.9) | 102.2 (9.8) | 0.014 | 106.5 (6.4) | <0.001 | |
| ∆ Cognitive flexibility | Placebo | 3.3 (6.0) | 0.359 | 4.8 (6.7) | 0.038 | |
| Active | 5.5 (11.6) | 9.8 (11.5) | ||||
| Processing speed | Placebo | 114.4 (9.3) | 115.9 (9.9) | 0.312 | 116.8 (10.2) | 0.100 |
| Active | 114 (9.3) | 117.2 (11.1) | 0.058 | 118.4 (9.3) | 0.004 | |
| ∆ Processing speed | Placebo | 1.4 (7.9) | 0.403 | 2.3 (7.7) | 0.291 | |
| Active | 3.3 (9.2) | 4.4 (7.8) | ||||
| Executive function | Placebo | 102.8 (9.3) | 105.3 (7.5) | 0.016 | 107.2 (9) | 0.001 |
| Active | 96.8 (11.1) | 102.0 (9.9) | 0.022 | 106.3 (6.4) | <0.001 | |
| ∆ Executive function | Placebo | 2.5 (5.5) | 0.265 | 4.5 (6.9) | 0.044 | |
| Active | 5.2 (11.9) | 9.5 (11.8) | ||||
| Social acuity | Placebo | 86.2 (14.7) | 92.0 (14.5) | 0.052 | 94.0 (18.0) | 0.013 |
| Active | 90.0 (17.6) | 94.5 (17.2) | 0.213 | 98.1 (14.9) | 0.018 | |
| ∆ Social acuity | Placebo | 5.8 (16.3) | 0.790 | 7.8 (16.8) | 0.937 | |
| Active | 4.6 (20.1) | 8.2 (18.1) | ||||
| Reasoning | Placebo | 94.7 (16.5) | 91.3 (18.3) | 0.264 | 95.0 (17.5) | 0.929 |
| Active | 92.8 (15.9) | 96.6 (14.5) | 0.166 | 93.9 (14.2) | 0.706 | |
| ∆ Reasoning | Placebo | −3.4 (16.9) | 0.078 | 0.3 (15.8) | 0.837 | |
| Active | 3.8 (14.9) | 1.1 (15.6) | ||||
| Working memory | Placebo | 105.7 (12.1) | 105.0 (14.1) | 0.779 | 105.6 (11.0) | 0.952 |
| Active | 103.5 (13.7) | 109.2 (9.3) | 0.010 | 107.7 (10.6) | 0.095 | |
| ∆ Working memory | Placebo | −0.7 (14.3) | 0.056 | −0.1 (11.6) | 0.180 | |
| Active | 5.7 (11.6) | 4.2 (13.5) | ||||
| Sustained attention | Placebo | 108.3 (10.0) | 108.8 (9.0) | 0.767 | 109.0 (10.3) | 0.737 |
| Active | 106.7 (9.9) | 110.6 (9.1) | 0.020 | 111.7 (7.2) | 0.013 | |
| ∆ Sustained attention | Placebo | 0.6 (10.6) | 0.184 | 0.7 (11.5) | 0.126 | |
| Active | 3.9 (8.8) | 5.0 (10.6) | ||||
| Simple attention | Placebo | 102.5 (11.6) | 103.0 (14.1) | 0.892 | 103.8 (9.8) | 0.528 |
| Active | 105.6 (7.3) | 81.4 (136.6) | 0.337 | 105.7 (6.8) | 0.948 | |
| ∆ Simple attention | Placebo | 0.5 (19.3) | 0.320 | 1.3 (11.3) | 0.683 | |
| Active | −24.2 (137.7) | 0.1 (10.9) | ||||
| Motor speed | Placebo | 99.7 (10.7) | 101.4 (10.0) | 0.101 | 100.5 (11.4) | 0.523 |
| Active | 99.2 (11.7) | 100.8 (10.4) | 0.129 | 99.8 (10.2) | 0.673 | |
| ∆ Motor speed | Placebo | 1.8 (5.9) | 0.926 | 0.8 (7.1) | 0.901 | |
| Active | 1.6 (5.8) | 0.6 (7.6) | ||||
All data are presented as mean (SD) of Cognitrax scores. Data at week 8 and week 12 were compared with those at week 0 using the paired t-test. Comparisons between the placebo and active groups were calculated as changes from week 0, indicated by the “Δ” symbol, and tested using the unpaired t-test.
3.3. Quality of Life Test
Changes in quality of life during the study period were assessed by the SF-36v2®. No statistically significant differences were found between the active and placebo groups in terms of change in score (Table 4).
Table 4.
Post-intervention changes in each quality-of-life parameter (placebo group: n = 35; active group: n = 32).
| Week 0 | Week 8 | Week 12 | ||||
|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | p-Value | Mean (SD) | p-Value | ||
| Physical functioning | Placebo | 52.2 (5.4) | 51.7 (6.0) | 0.682 | 52.8 (4.8) | 0.633 |
| Active | 53.2 (5.0) | 53.6 (4.0) | 0.660 | 53.7 (5.1) | 0.556 | |
| ∆ Physical functioning | Placebo | −0.6 (5.4) | 0.115 | 0.6 (4.0) | 0.473 | |
| Active | 0.4 (3.0) | 0.5 (3.1) | ||||
| Role physical | Placebo | 52.8 (5.6) | 53.6 (5.1) | 0.534 | 53.6 (5.5) | 0.471 |
| Active | 53.3 (6.8) | 53.7 (4.7) | 0.873 | 54 (4.4) | 0.710 | |
| ∆ Role physical | Placebo | 0.8 (4.3) | 0.895 | 0.9 (6.0) | 0.777 | |
| Active | 0.4 (7.2) | 0.7 (6.0) | ||||
| Bodily pain | Placebo | 49.9 (8.8) | 48.6 (7.9) | 0.472 | 49.3 (10.1) | 0.825 |
| Active | 50.9 (10.3) | 50.9 (9.2) | 1.000 | 51.8 (9.4) | 0.648 | |
| ∆ Bodily pain | Placebo | −1.4 (6.8) | 0.273 | −0.7 (9.6) | 0.296 | |
| Active | 0.0 (6.2) | 0.9 (7.7) | ||||
| General health perceptions | Placebo | 58.2 (6.9) | 57.2 (6.9) | 0.256 | 58.2 (6.8) | 1.000 |
| Active | 57.1 (6.8) | 57.5 (7.1) | 0.846 | 57.2 (8.0) | 0.981 | |
| ∆ General health perceptions | Placebo | −1.0 (4.3) | 0.877 | 0.0 (4.7) | 0.575 | |
| Active | 0.4 (3.9) | 0.1 (5.2) | ||||
| Vitality | Placebo | 55.5 (7.0) | 55.8 (7.7) | 0.930 | 56.0 (6.2) | 0.854 |
| Active | 56.8 (6.7) | 57.2 (6.2) | 0.862 | 57.0 (6.4) | 0.963 | |
| ∆ Vitality | Placebo | 0.3 (6.6) | 0.443 | 0.5 (6.5) | 0.535 | |
| Active | 0.4 (5.0) | 0.2 (5.6) | ||||
| Social functioning | Placebo | 54.2 (6.6) | 55.3 (6.3) | 0.423 | 55.0 (6.3) | 0.632 |
| Active | 53.5 (7.0) | 55.1 (5.7) | 0.183 | 55.2 (5.2) | 0.128 | |
| ∆ Social functioning | Placebo | 1.1 (5.1) | 0.877 | 0.8 (7.0) | 0.850 | |
| Active | 1.6 (6.7) | 1.8 (5.6) | ||||
| Role emotional | Placebo | 52.8 (6.3) | 54.9 (4.5) | 0.041 | 54.6 (4.3) | 0.093 |
| Active | 54.4 (5.1) | 53.8 (4.8) | 0.779 | 54.9 (4.2) | 0.783 | |
| ∆ Role emotional | Placebo | 2.1 (6.1) | 0.332 | 1.8 (6.3) | 0.720 | |
| Active | −0.6 (7.2) | 0.6 (3.2) | ||||
| Mental health | Placebo | 56.9 (4.4) | 57.6 (5.5) | 0.663 | 57.6 (6.9) | 0.718 |
| Active | 57.1 (6.7) | 57.1 (6.5) | 0.993 | 57.5 (5.4) | 0.775 | |
| ∆ Mental health | Placebo | 0.7 (6.1) | 0.732 | 0.7 (5.2) | 0.982 | |
| Active | 0.1 (5.1) | 0.5 (4.4) | ||||
All data are presented as mean (SD) of SF-36v2® scores. Data at week 8 and week 12 were compared with those at week 0 using Dunnett’s test. Comparisons between the placebo and active groups were calculated as changes from week 0, indicated by the “Δ” symbol, and tested using the unpaired t-test.
3.4. Fecal Bifidobacteria
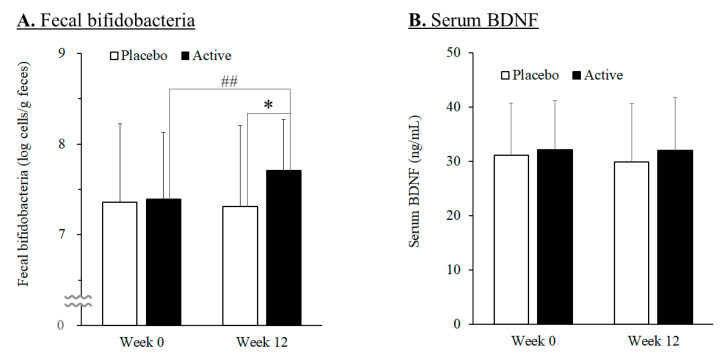
Quantification of the bifidobacteria in the feces (Figure 2A) revealed that the total number of bifidobacteria in the active group at week 12 increased significantly compared to week 0, while that of the placebo group did not change much. And the total number of bifidobacteria was significantly increased in the active group (7.71 ± 0.56 log cells/g feces) compared with the placebo group (7.31 ± 0.90 log cells/g feces) at week 12 (p = 0.031 using the unpaired t-test).
Figure 2.
Changes in fecal bifidobacteria (A) and in serum BDNF (B) in the placebo (n = 35) and active (n = 32) groups during the study period. Values are means, with error bars as standard deviation. Double number signs (##) indicate p-value < 0.01 as a result of intra-group difference (week 0 vs. week 12; paired t-test). Asterisk (*) indicates p-value < 0.05 as a result of inter-group difference (the placebo group vs. the active group; unpaired t-test).
3.5. Serum BDNF
Serum BDNF levels were quantified. The results showed no statistically significant difference between the active and placebo groups during the study period (Figure 2B).
3.6. Blood Inflammation Markers
The expression levels of 92 inflammatory markers were examined at weeks 0 and 12 using Olink® Target 96 Inflammation Panels; 75 inflammatory markers that were determined to be quantifiable were analyzed (Supplementary Materials, Table S3). The results showed that there were statistically significant differences between the change in scores from week 0 to week 12 for leukemia inhibitory factor receptor, sulfotransferase 1A1, C-C motif hemokine (CCL)23, and TNF (ligand) superfamily member 12 (TWEAK) in the active and the placebo groups (using the unpaired t-test) (Table 5). In addition, there were no statistically significant differences between the change in scores from week 0 to week 12 of adenosine deaminase, osteoprotegerin, eotaxin, glial cell line-derived neurotrophic factor, fractalkine, interleukin-8 (IL-8), CCL28, IL-18, IL-10, CCL19, and T-cell surface glycoprotein CD5 in the active and placebo groups, but the trends were considered significant because the p-value was <0.1 (Table 5). Blood hs-CRP and blood IL-1β were also measured at weeks 0 and 12, but neither showed a statistically significant difference between the active and placebo groups (Supplementary Materials, Table S4).
Table 5.
Post-intervention changes in each cognitive function parameter (placebo group: n = 32; active group: n = 31).
| Parameter | Week 0 | Week 12 | Change | |||
|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | p-Value | Mean (SD) | p-Value | ||
| LIF-R, NPX | Placebo | 3.36 (0.27) | 3.39 (0.23) | 0.459 | 0.02 (0.19) | 0.012 |
| Active | 3.49 (0.30) | 3.40 (0.20) | 0.008 | −0.10 (0.19) | ||
| ST1A1, NPX | Placebo | 2.19 (1.16) | 1.75 (0.83) | 0.111 | −0.36 (1.10) | 0.020 |
| Active | 1.82 (0.82) | 2.10 (1.00) | 0.079 | 0.33 (0.86) | ||
| CCL23, NPX | Placebo | 10.86 (0.35) | 10.88 (0.25) | 0.718 | 0.02 (0.25) | 0.021 |
| Active | 11.09 (0.46) | 10.90 (0.40) | 0.012 | −0.15 (0.32) | ||
| TWEAK, NPX | Placebo | 9.10 (0.34) | 9.08 (0.33) | 0.658 | −0.01 (0.18) | 0.033 |
| Active | 9.22 (0.26) | 9.10 (0.20) | 0.002 | −0.12 (0.19) | ||
| ADA, NPX | Placebo | 5.39 (0.41) | 5.46 (0.39) | 0.068 | 0.08 (0.23) | 0.052 |
| Active | 5.53 (0.37) | 5.50 (0.30) | 0.345 | −0.04 (0.24) | ||
| OPG, NPX | Placebo | 10.49 (0.4) | 10.58 (0.41) | 0.134 | 0.09 (0.34) | 0.052 |
| Active | 10.60 (0.30) | 10.60 (0.20) | 0.188 | −0.04 (0.17) | ||
| CCL11, NPX | Placebo | 8.66 (0.43) | 8.76 (0.36) | 0.029 | 0.09 (0.24) | 0.054 |
| Active | 8.72 (0.29) | 8.70 (0.20) | 0.649 | −0.02 (0.21) | ||
| GDNF, NPX | Placebo | 1.98 (0.47) | 2.19 (0.44) | 0.003 | 0.20 (0.33) | 0.055 |
| Active | 2.15 (0.33) | 2.10 (0.30) | 0.447 | 0.04 (0.28) | ||
| CX3CL1, NPX | Placebo | 3.66 (0.48) | 3.82 (0.51) | 0.059 | 0.17 (0.48) | 0.058 |
| Active | 3.86 (0.41) | 3.80 (0.40) | 0.520 | −0.04 (0.34) | ||
| IL-8, NPX | Placebo | 5.97 (0.41) | 6.22 (0.49) | 0.012 | 0.24 (0.53) | 0.063 |
| Active | 6.15 (0.75) | 6.20 (0.70) | 0.733 | 0.02 (0.37) | ||
| CCL28, NPX | Placebo | 2.62 (0.50) | 2.64 (0.49) | 0.711 | 0.02 (0.27) | 0.063 |
| Active | 2.73 (0.46) | 2.60 (0.50) | 0.009 | −0.09 (0.18) | ||
| IL-18, NPX | Placebo | 9.10 (0.67) | 9.28 (0.68) | 0.002 | 0.18 (0.30) | 0.064 |
| Active | 9.14 (0.63) | 9.20 (0.50) | 0.912 | 0.01 (0.41) | ||
| IL-10, NPX | Placebo | 3.22 (0.52) | 3.44 (0.78) | 0.035 | 0.22 (0.56) | 0.064 |
| Active | 3.47 (0.44) | 3.50 (0.40) | 0.975 | 0.00 (0.28) | ||
| CCL19, NPX | Placebo | 8.73 (0.77) | 8.88 (0.90) | 0.163 | 0.15 (0.60) | 0.081 |
| Active | 8.72 (0.49) | 8.70 (0.60) | 0.278 | −0.06 (0.31) | ||
| CD5, NPX | Placebo | 5.92 (0.40) | 5.91 (0.37) | 0.864 | −0.01 (0.19) | 0.092 |
| Active | 6.02 (0.39) | 5.90 (0.30) | 0.017 | −0.09 (0.20) | ||
All data were obtained using Olink® Target 96 Inflammation Panels and are presented as the mean (SD) of log base 2-normalized protein expression values (NPX). Data at week 12 were compared with those at week 0 using the paired t-test. Comparisons between the placebo and active groups were evaluated by calculating the change in measurements at week 0 and 12 in both groups using unpaired t-tests. LIF-R, leukemia inhibitory factor receptor; ST1A1, sulfotransferase 1A1; CCL23, C-C motif hemokine 23; TWEAK, tumor necrosis factor (ligand) superfamily, member 12; ADA, adenosine deaminase; OPG, osteoprotegerin; CCL11, eotaxin; GDNF, glial cell line-derived neurotrophic factor; CX3CL1, fractalkine; IL-8, interleukin 8; CCL28, C-C motif chemokine 28; IL-18, interleukin 18; IL-10, interleukin 10; CCL19, C-C motif chemokine 19; CD5, T-cell surface glycoprotein CD5.
4. Discussion
We investigated the effects of consuming a dairy beverage containing Bifidobacterium animalis subsp. lactis GCL2505 and inulin on cognitive function in healthy adults. The results showed that the test drink had a positive effect on cognitive function.
Cognitive function was assessed using Cognitrax, a computerized battery of neurocognitive tests developed for routine clinical screening applications. Cognitrax has been reported to have very similar characteristics to traditional psychological tests. It can measure a wide range of cognitive functions and is suitable for accurate assessment of scored cognitive functions because of its high sensitivity to discriminating between individuals with MCI and healthy individuals [32]. A similar test, CNS Vital Signs, is reported to adequately discriminate between healthy individuals, patients with MCI, and patients with dementia [40]. Cognitrax has also been used to assess cognitive function in clinical trials [15,16,17]. Therefore, Cognitrax was considered a suitable tool for testing cognitive function in this study.
The change in neurocognitive index domain scores from week 0 to week 12 was significantly higher in the active group than in the placebo group. The Neurocognitive Index domain score is calculated by averaging the scores from the total memory, cognitive functioning speed, reaction time, total attention, and cognitive flexibility domains, and is, therefore, used to assess a person’s overall neurocognitive status. Furthermore, intake of GCL2505 and inulin was associated with statistically significant improvements in scores in the complex attention, cognitive flexibility, and executive function domains. Total attention refers to the ability to process things accurately while maintaining attention. Cognitive flexibility refers to the ability to understand and process changes in instructions. Executive function refers to the ability to make decisions based on an understanding of background rules and concepts. Thus, it is considered that intake of GCL2505 and inulin may contribute to improved activities of daily living by improving these functions.
It is hypothesized that intake of GCL2505 and inulin improves cognitive function through a mechanism involving the following three steps. Step 1: Intake of GCL2505 and inulin improves the intestinal environment. In this study, the number of fecal bifidobacteria was significantly increased in the active group compared with the placebo group. It was reported that intake of GCL2505 increases the number of bifidobacteria in the feces and the concentration of acetic acid in the feces and blood [23,25,26,27]. Clinical studies have shown the effects of inulin [41] as well as the enhanced effect of GCL2505 in combination with inulin in terms of increased total bifidobacteria count in the intestine [30]. Thus, participants in the active group who consumed a test drink containing GCL2505 and inulin in the present study had an improved intestinal environment via increasing the number of bifidobacteria in the gut. This change may possibly have increased the level of acetic acid, an SCFA, in the gut of the active group. Step 2: Improvement in the intestinal environment leads to alleviation of inflammation. Increased SCFA levels in the gut alleviate inflammation in the body. It was reported that administration of dietary fiber or acetic acid to mice reduced blood levels of IL-1, a known inflammatory cytokine [42]. SCFAs are also known to have positive effects on inflammation by reducing visceral fat and improving glucose metabolism. Experiments with mice showed that GCL2505 played a role in reducing visceral fat area by increasing the number of bifidobacteria in the intestine, as evidenced by the increased numbers in the feces as well as the higher acetic acid levels in feces and blood [26]. Daily consumption of yogurt containing GCL2505 has been shown in clinical studies to reduce visceral fat mass in the abdomen of humans [28]. Inulin consumption has also been proven to reduce visceral fat area [43], and Lauridsen et al. found that obese individuals have decreased expression of IL-10, which contributes to reducing inflammation, and increased expression of nitric oxide synthase 2, which triggers inflammation, in the brain [44]. A correlation between high-fat diet intake and hypothalamic inflammatory status has been reported [45,46], and Mao et al. reported that administration of a high-fat diet in combination with (-)-epigallocatechin gallate in mice suppressed the increased expression of IL-6, TNF-α, and IL-1β in the hypothalamus by inhibiting body weight gain [47]. Step 3: Alleviating inflammation improves cognitive function. It has recently been shown that inflammatory conditions and cognitive function are closely linked. Studies on patients with AD have reported a correlation between attenuated cognitive function and acute and chronic systemic inflammation associated with increased TNF-α levels [13], and that reduced levels of NLRP3 (nucleotide-binding oligomerization domain-like receptor family, pyrin domain-containing 3) inflammasome-derived inflammatory cytokines alleviate the progression of AD pathology [48]. TNF-α is a typical pro-inflammatory cytokine [49], and Habbas et al. suggested a link between increased TNF-α levels in the brain and cognitive impairment [50]. Increasing the number of SCFA-producing bacteria by fecal transplantation in rats resulted in increased SCFA levels in the gut and a reduction in cognitive decline [51]. The hypothesis thus far indicates that the effects of GCL2505 and inulin on cognitive function may be realized by increasing intestinal SCFA levels and alleviating inflammatory conditions.
In this study, the changes in expression of 75 inflammation markers from week 0 to 12 were analyzed by principal component analysis and tested by permutational multivariate analysis of variance, but there were no statistically significant differences between the active and placebo groups (p = 0.109) (Supplementary Materials, Figure S1). However, some reductions in pro-inflammatory cytokine levels were observed. For example, TWEAK is expressed in animals with chronic intestinal inflammation [52] and induces secretion of the pro-inflammatory cytokine IL-8 [53]. CCL23 is also secreted by neutrophils stimulated by lipopolysaccharides and TNF-α [54]. These results suggest that the chronic inflammatory state of the intestinal tract may be somehow affected by GCL2505 and inulin and that the inhibitory effect of Bifidobacterium breve A1 on brain atrophy may be related to the suppression of inflammation [55]. The effect of Lactiplantibacillus plantarum OLL2712, which has been shown to strongly induce IL-10 production and have an effect on chronic inflammation, was confirmed to improve cognitive function, suggesting that the suppressive effect of OLL2712 on gut and nerve inflammation may be the reason for the improvement [22]. Intake of Bifidobacterium longum BB68S led to a decrease in the numbers of the inflammation-inducing bacteria Solobacterium and Oribacterium, indicating that improved cognitive function might be due to reduced inflammation [56]. Akbari et al. reported that administration of multiple probiotics had a favorable effect on hs-CRP as well as MMSE scores, malondialdehyde, insulin metabolic markers, and triglyceride levels in patients with AD [57]. An intervention involving the intake of Bifidobacterium bifidum BGN4 and Bifidobacterium longum BORI decreased intestinal levels of inflammatory bacteria and increased BDNF levels, suggesting that these bifidobacteria might have an anti-inflammatory effect [58]. The effects of probiotics on cognitive function have also been verified by multiple clinical trials. Many of these effects are presumed to be due to the alleviation of inflammation, but in many cases, the results from indirectly assessing inflammatory conditions have been used. In contrast, in the present study, multiple inflammation markers were measured for the first time in a study in which probiotics were ingested, thereby directly demonstrating the relationship between inflammation and the effect of probiotics on cognitive function. Although further research is needed to understand the inflammatory state, it is believed that the effects of GCL2505 and inulin on cognitive function are strongly related to the inflammatory state in the gut.
The results of the SF-36v2® health-related quality of life assessment in the present study did not reveal any differences between the active and placebo groups. All scores at week 0 were above 50 except for the bodily pain scale. It is possible that the participants in this study did not originally have low SF-36v2® scores, so the improvement effect was not apparent. The selection criteria “subjective or other symptoms of forgetfulness” established in this study suggested that the person’s quality of life was not significantly impaired. Also, we did not confirm the effect of GCL2505 and inulin on BDNF, which is a neurotrophic factor that is essential for synaptogenesis, plasticity, and neuroimmune responses and plays an important role in learning, memory formation, and affective disorders [59,60]. Although BDNF levels have been reported to be associated with gut microbiota [61,62], meta-analyses have shown no correlation between probiotic intake and BDNF levels. [63]. Given the inconsistent relationship between BDNF and the gut microbiota observed here, further research is warranted.
Just to be sure, no serious health problems have been reported as a result of the consumption of foods containing GCL2505. In addition, foods using Bifidobacterium animalis subsp. lactis have been sold all over the world, and no health hazard has been reported to be caused by these bifidobacteria. So the safety of GCL2505 is assured, but in some cases, intake of GCL2505 may cause slightly increased farting or softer stools in some people.
5. Conclusions
This is the first randomized controlled trial to demonstrate the efficacy of GCL2505 and inulin in improving memory function in the elderly. Elderly patients with early memory loss who consumed GCL2505 and inulin for 12 weeks showed significant improvements in scores in the neurocognitive index domain, which is an assessment of overall cognitive function, in addition to the complex attention, cognitive flexibility, and executive function domains, and the number of bifidobacteria in feces increased significantly. Because there is currently no effective pharmacological therapy to prevent the onset and progression of cognitive decline in the pre-dementia stage, the findings of this study suggest that continuous intake of GCL2505 and inulin may be an effective approach to protect memory function in the elderly.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu15194175/s1, Table S1: CONSORT 2010 checklist of information to include when reporting a randomized trial. Table S2: Post-intervention changes in Cognitrax scores (placebo group: n = 32; active group: n = 31), Table S3: Post-intervention changes in each inflammatory marker (all data), Table S4: Post-intervention changes in IL-1β and hs-CRP scores, Figure S1: Principal coordinate analysis with t-distribution ellipses between the active and the placebo groups.
Author Contributions
Conceptualization, N.A., T.M. and Y.S.; methodology, T.M. and Y.S.; validation, T.M. and Y.S.; formal analysis, T.M. and M.S.; investigation, N.A., T.M. and M.T.; writing—original draft preparation, N.A. and Y.S.; writing—review and editing, T.M., Y.S., M.T. and Y.I.; visualization, N.A., M.T. and M.S.; supervision, Y.I.; funding acquisition, Y.S. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethical Committee of Kobuna Orthopedics Clinic (approval date: 12 March 2022; approval number: MK-2205-01).
Informed Consent Statement
Informed consent was obtained from all participants involved in the study.
Data Availability Statement
Datasets generated during the current study and/or analyzed during the current study are available from the responsible author upon reasonable request.
Conflicts of Interest
N.A., T.M., Y.S., M.T., and M.S. are employees of Ezaki Glico Co., Ltd. The other author, Y.I., reports no conflict of interest in this work.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.World Health Organization Dementia. [(accessed on 15 March 2023)]. Available online: https://www.who.int/news-room/fact-sheets/detail/dementia.
- 2.World Health Organization . Global Status Report on the Public Health Response to Dementia. World Health Organization; Geneva, Switzerland: 2021. [Google Scholar]
- 3.Hosaka A., Araki W., Oda A., Tomidokoro Y., Tamaoka A. Statins reduce amyloid β-peptide production by modulating amyloid precursor protein maturation and phosphorylation through a cholesterol-independent mechanism in cultured neurons. Neurochem. Res. 2013;3:589–600. doi: 10.1007/s11064-012-0956-1. [DOI] [PubMed] [Google Scholar]
- 4.Soeda Y., Yoshikawa M., Almeida O.F.X., Sumioka A., Maeda S., Osada H., Kondoh Y., Saito A., Miyasaka T., Kimura T., et al. Toxic tau oligomer formation blocked by capping of cysteine residues with 1,2-dihydroxybenzene groups. Nat. Commun. 2015;6:10216. doi: 10.1038/ncomms10216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jack C.R., Jr., Knopman D.S., Jagust W.J., Shaw L.M., Aisen P.S., Weiner M.W., Petersen R.C., Trojanowski J.Q. Hypothetical model of dynamic biomarkers of the Alzheimer’s pathological cascade. Lancet Neurol. 2010;9:119–128. doi: 10.1016/S1474-4422(09)70299-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Petersen R.C., Smith G.E., Waring S.C., Ivnik R.J., Tangalos E.G., Kokmen E. Mild cognitive impairment: Clinical characterization and outcome. Arch. Neurol. 1999;56:303–308. doi: 10.1001/archneur.56.3.303. [DOI] [PubMed] [Google Scholar]
- 7.Plassman B.L., Langa K.M., Fisher G.G., Heeringa S.G., Weir D.R., Ofstedal M.B., Burke J.R., Hurd M.D., Potter G.G., Rodgers W.L., et al. Prevalence of cognitive impairment without dementia in the United States. Ann. Intern. Med. 2008;148:427–434. doi: 10.7326/0003-4819-148-6-200803180-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ganguli M., Jia Y., Hughes T.F., Snitz B.E., Chang C.-C.H., Berman S.B., Sullivan K.J., Kamboh M.I. Mild cognitive impairment that does not progress to dementia: A population-based study. J. Am. Geriatr. Soc. 2019;67:232–238. doi: 10.1111/jgs.15642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shimada H., Makizako H., Park H., Doi T., Lee S. Validity of the national center for geriatrics and gerontology-functional assessment tool and mini-mental state examination for detecting the incidence of dementia in older Japanese adults. Geriatr. Gerontol. Int. 2017;17:2383–2388. doi: 10.1111/ggi.13079. [DOI] [PubMed] [Google Scholar]
- 10.Yusufov M., Weyandt L.L., Piryatinsky I. Alzheimer’s disease and diet: A systematic review. Int. J. Neurosci. 2017;127:161–175. doi: 10.3109/00207454.2016.1155572. [DOI] [PubMed] [Google Scholar]
- 11.Ozato N., Saitou S., Yamaguchi T., Katashima M., Misawa M., Jung S., Mori K., Kawada H., Katsuragi Y., Mikami T., et al. Association between visceral fat and brain structural changes or cognitive function. Brain Sci. 2021;11:1036. doi: 10.3390/brainsci11081036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Toppala S., Ekblad L.L., Lötjönen J., Helin S., Hurme S., Johansson J., Jula A., Karrasch M., Koikkalainen J., Laine H., et al. Midlife insulin resistance as a predictor for late-life cognitive function and cerebrovascular lesions. J. Alzheimers Dis. 2019;72:215–228. doi: 10.3233/JAD-190691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holmes C., Cunningham C., Zotova E., Woolford J., Dean C., Kerr S., Culliford D., Perry V.H. Systemic inflammation and disease progression in Alzheimer disease. Neurology. 2009;73:768–774. doi: 10.1212/WNL.0b013e3181b6bb95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pistollato F., Cano S.S., Elio I., Vergara M.M., Giampieri F., Battino M. Role of gut microbiota and nutrients in amyloid formation and pathogenesis of Alzheimer disease. Nutr. Rev. 2016;74:624–634. doi: 10.1093/nutrit/nuw023. [DOI] [PubMed] [Google Scholar]
- 15.Saitou K., Ochiai R., Kozuma K., Sato H., Koikeda T., Osaki N., Katsuragi Y. Effect of chlorogenic acids on cognitive function: A randomized, double-blind, placebo-controlled trial. Nutrients. 2018;10:1337. doi: 10.3390/nu10101337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Asama T., Hiraoka T., Ohkuma A., Okumura N., Yamaki A., Urakami K. Cognitive improvement and safety assessment of a dietary supplement containing propolis extract in elderly Japanese: A placebo-controlled, randomized, parallel-group, double-blind human clinical study. Evid. Based Complement. Alternat. Med. 2021;2021:6664217. doi: 10.1155/2021/6664217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sekikawa T., Kizawa Y., Li Y., Takara T. Cognitive function improvement with astaxanthin and tocotrienol intake: A randomized, double-blind, placebo-controlled study. J. Clin. Biochem. Nutr. 2020;67:307–316. doi: 10.3164/jcbn.19-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhu G., Zhao J., Zhang H., Chen W., Wang G. Probiotics for mild cognitive impairment and Alzheimer’s disease: A systematic review and meta-analysis. Foods. 2021;10:1672. doi: 10.3390/foods10071672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sanborn V., Azcarate-Peril M.A., Updegraff J., Manderino L., Gunstad J. Randomized clinical trial examining the impact of Lactobacillus rhamnosus GG probiotic supplementation on cognitive functioning in middle-aged and older adults. Neuropsychiatr. Dis. Treat. 2020;16:2765–2777. doi: 10.2147/NDT.S270035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kobayashi Y., Sugahara H., Shimada K., Mitsuyama E., Kuhara T., Yasuoka A., Kondo T., Abe K., Xiao J.-Z. Therapeutic potential of Bifidobacterium breve strain A1 for preventing cognitive impairment in Alzheimer’s disease. Sci. Rep. 2017;7:13510. doi: 10.1038/s41598-017-13368-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xiao J., Katsumata N., Bernier F., Ohno K., Yamauchi Y., Odamaki T., Yoshikawa K., Ito K., Kaneko T. Probiotic Bifidobacterium breve in improving cognitive functions of older adults with suspected mild cognitive impairment: A randomized, double-blind, placebo-controlled trial. J. Alzheimers Dis. 2020;77:139–147. doi: 10.3233/JAD-200488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sakurai K., Toshimitsu T., Okada E., Anzai S., Shiraishi I., Inamura N., Kobayashi S., Sashihara T., Hisatsune T. Effects of Lactiplantibacillus plantarum OLL2712 on memory function in older adults with declining memory: A randomized placebo-controlled trial. Nutrients. 2022;14:4300. doi: 10.3390/nu14204300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ishizuka A., Tomizuka K., Aoki R., Nishijima T., Saito Y., Inoue R., Ushida K., Mawatari T., Ikeda T. Effects of administration of Bifidobacterium animalis subsp. lactis GCL2505 on defecation frequency and bifidobacterial microbiota composition in humans. J. Biosci. Bioeng. 2012;113:587–591. doi: 10.1016/j.jbiosc.2011.12.016. [DOI] [PubMed] [Google Scholar]
- 24.Tanaka Y., Takami K., Nishijima T., Aoki R., Mawatari T., Ikeda T. Short- and long-term dynamics in the intestinal microbiota following ingestion of Bifidobacterium animalis subsp. lactis GCL2505. Biosci. Microbiota Food Health. 2015;34:77–85. doi: 10.12938/bmfh.2015-001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aoki R., Tsuchida S., Arai Y., Ohno K., Nishijima T., Mawatari T., Mikami Y., Ushida K. Effect of Bifidobacterium animalis subsp. lactis GCL2505 on the physiological function of intestine in a rat model. Food Sci. Nutr. 2016;4:782–790. doi: 10.1002/fsn3.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aoki R., Kamikado K., Suda W., Takii H., Mikami Y., Suganuma N., Hattori M., Koga Y. A proliferative probiotic Bifidobacterium strain in the gut ameliorates progression of metabolic disorders via microbiota modulation and acetate elevation. Sci. Rep. 2017;7:43522. doi: 10.1038/srep43522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Horiuchi H., Kamikado K., Aoki R., Suganuma N., Nishijima T., Nakatani A., Kimura I. Bifidobacterium animalis subsp. lactis GCL2505 modulates host energy metabolism via the short-chain fatty acid receptor GPR43. Sci. Rep. 2020;10:4158. doi: 10.1038/s41598-020-60984-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Takahashi S., Anzawa D., Takami K., Ishizuka A., Mawatari T., Kamikado K., Sugimura H., Nishijima T. Effect of Bifidobacterium animalis ssp. lactis GCL2505 on visceral fat accumulation in healthy Japanese adults: A randomized controlled trial. Biosci. Microbiota Food Health. 2016;35:163–171. doi: 10.12938/bmfh.2016-002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mensink M.A., Frijlink H.W., van der Voort Maarschalk K., Hinrichs W.L.J. Inulin, a flexible oligosaccharide I: Review of its physicochemical characteristics. Carbohydr. Polym. 2015;130:405–419. doi: 10.1016/j.carbpol.2015.05.026. [DOI] [PubMed] [Google Scholar]
- 30.Anzawa D., Mawatari T., Tanaka Y., Yamamoto M., Genda T., Takahashi S., Nishijima T., Kamasaka H., Suzuki S., Kuriki T. Effects of synbiotics containing Bifidobacterium animalis subsp. lactis GCL2505 and inulin on intestinal bifidobacteria: A randomized, placebo-controlled, crossover study. Food Sci. Nutr. 2019;7:1828–1837. doi: 10.1002/fsn3.1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wu W., Sun M., Chen F., Cao A.T., Liu H., Zhao Y., Huang X., Xiao Y., Yao S., Zhao Q., et al. Microbiota metabolite short-chain fatty acid acetate promotes intestinal IgA response to microbiota which is mediated by GPR43. Mucosal Immunol. 2017;10:946–956. doi: 10.1038/mi.2016.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gualtieri C.T., Johnson L.G. Reliability and validity of a computerized neurocognitive test battery, CNS Vital Signs. Arch. Clin. Neuropsychol. 2006;21:623–643. doi: 10.1016/j.acn.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 33.Baba Y., Inagaki S., Nakagawa S., Kaneko T., Kobayashi M., Takihara T. Effect of daily intake of green tea catechins on cognitive function in middle-aged and older subjects: A randomized, placebo-controlled study. Molecules. 2020;25:4265. doi: 10.3390/molecules25184265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ware J.E., Jr., Sherbourne C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care. 1992;30:473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 35.Awata S., Bech P., Yoshida S., Hirai M., Suzuki S., Yamashita M., Ohara A., Hinokio Y., Matsuoka H., Oka Y. Reliability and validity of the Japanese version of the World Health Organization-Five Well-Being Index in the context of detecting depression in diabetic patients. Psychiatry Clin. Neurosci. 2007;61:112–119. doi: 10.1111/j.1440-1819.2007.01619.x. [DOI] [PubMed] [Google Scholar]
- 36.Assarsson E., Lundberg M., Holmquist G., Björkesten J., Thorsen S.B., Ekman D., Eriksson A., Dickens E.R., Ohlsson S., Edfeldt G., et al. Homogenous 96-plex PEA immunoassay exhibiting high sensitivity, specificity, and excellent scalability. PLoS ONE. 2014;9:e95192. doi: 10.1371/journal.pone.0095192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tourlousse D.M., Narita K., Miura T., Sakamoto M., Ohashi A., Shiina K., Matsuda M., Miura D., Shimamura M., Ohyama Y., et al. Validation and standardization of DNA extraction and library construction methods for metagenomics-based human fecal microbiome measurements. Microbiome. 2021;9:95. doi: 10.1186/s40168-021-01048-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tanaka K., Nakamura Y., Terahara M., Yanagi T., Nakahara S., Furukawa O., Tsutsui H., Inoue R., Tsukahara T., Koshida S. Poor bifidobacterial colonization is associated with late provision of colostrum and improved with probiotic supplementation in low birth weight infants. Nutrients. 2019;11:839. doi: 10.3390/nu11040839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Topp C.H., Østergaard S.D., Søndergaard S., Bech P. The WHO-5 Well-Being Index: A systematic review of the literature. Psychother. Psychosom. 2015;84:167–176. doi: 10.1159/000376585. [DOI] [PubMed] [Google Scholar]
- 40.Gualtieri C.T., Johnson L.G. Neurocognitive testing supports a broader concept of mild cognitive impairment. Am. J. Alzheimers Dis. Other Demen. 2005;20:359–366. doi: 10.1177/153331750502000607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Birkeland E., Gharagozlian S., Birkeland K.I., Valeur J., Måge I., Rud I., Aas A.-M. Prebiotic effect of inulin-type fructans on faecal microbiota and short-chain fatty acids in type 2 diabetes: A randomised controlled trial. Eur. J. Nutr. 2020;59:3325–3338. doi: 10.1007/s00394-020-02282-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Marques F.Z., Nelson E., Chu P.-Y., Horlock D., Fiedler A., Ziemann M., Tan J.K., Kuruppu S., Rajapakse N.W., El-Osta A., et al. High-fiber diet and acetate supplementation change the gut microbiota and prevent the development of hypertension and heart failure in hypertensive mice. Circulation. 2017;135:964–977. doi: 10.1161/CIRCULATIONAHA.116.024545. [DOI] [PubMed] [Google Scholar]
- 43.Nakajima H., Nakanishi N., Miyoshi T., Okamura T., Hashimoto Y., Senmaru T., Majima S., Ushigome E., Asano M., Yamaguchi M., et al. Inulin reduces visceral adipose tissue mass and improves glucose tolerance through altering gut metabolites. Nutr. Metab. 2022;19:50. doi: 10.1186/s12986-022-00685-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lauridsen J.K., Olesen R.H., Vendelbo J., Hyde T.M., Kleinman J.E., Bibby B.M., Brock B., Rungby J., Larsen A. High BMI levels associate with reduced mRNA expression of IL10 and increased mRNA expression of iNOS (NOS2) in human frontal cortex. Transl. Psychiatry. 2017;7:e1044. doi: 10.1038/tp.2016.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Waise T.M.Z., Toshinai K., Naznin F., NamKoong C., Moin A.S.M., Sakoda H., Nakazato M. One-day high-fat diet induces inflammation in the nodose ganglion and hypothalamus of mice. Biochem. Biophys. Res. Commun. 2015;464:1157–1162. doi: 10.1016/j.bbrc.2015.07.097. [DOI] [PubMed] [Google Scholar]
- 46.Thaler J.P., Yi C.-X., Schur E.A., Guyenet S.J., Hwang B.H., Dietrich M.O., Zhao X., Sarruf D.A., Izgur V., Maravilla K.R., et al. Obesity is associated with hypothalamic injury in rodents and humans. J. Clin. Investig. 2012;122:153–162. doi: 10.1172/JCI59660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mao L., Hochstetter D., Yao L., Zhao Y., Zhou J., Wang Y., Xu P. Green tea polyphenol (-)-epigallocatechin gallate (EGCG) attenuates neuroinflammation in palmitic acid-stimulated BV-2 microglia and high-fat diet-induced obese mice. Int. J. Mol. Sci. 2019;20:5081. doi: 10.3390/ijms20205081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Heneka M.T., Kummer M.P., Stutz A., Delekate A., Schwartz S., Vieira-Saecker A., Griep A., Axt D., Remus A., Tzeng T.-C., et al. NLRP3 is activated in Alzheimer’s disease and contributes to pathology in APP/PS1 mice. Nature. 2013;493:674–678. doi: 10.1038/nature11729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tzanavari T., Giannogonas P., Karalis K.P. TNF-alpha and obesity. Curr. Dir. Autoimmun. 2010;11:145–156. doi: 10.1159/000289203. [DOI] [PubMed] [Google Scholar]
- 50.Habbas S., Santello M., Becker D., Stubbe H., Zappia G., Liaudet N., Klaus F.R., Kollias G., Fontana A., Pryce C.R., et al. neuroinflammatory TNFα impairs memory via astrocyte signaling. Cell. 2015;163:1730–1741. doi: 10.1016/j.cell.2015.11.023. [DOI] [PubMed] [Google Scholar]
- 51.Xiao W., Su J., Gao X., Yang H., Weng R., Ni W., Gu Y. The microbiota-gut-brain axis participates in chronic cerebral hypoperfusion by disrupting the metabolism of short-chain fatty acids. Microbiome. 2022;10:62. doi: 10.1186/s40168-022-01255-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dohi T., Burkly L.C. The TWEAK/Fn14 pathway as an aggravating and perpetuating factor in inflammatory diseases: Focus on inflammatory bowel diseases. J. Leukoc. Biol. 2012;92:265–279. doi: 10.1189/jlb.0112042. [DOI] [PubMed] [Google Scholar]
- 53.Lee S.J., Kim J., Ko J., Lee E.J., Koh H.J., Yoon J.S. Tumor necrosis factor-like weak inducer of apoptosis induces inflammation in Graves’ orbital fibroblasts. PLoS ONE. 2018;13:e0209583. doi: 10.1371/journal.pone.0209583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Arruda-Silva F., Bianchetto-Aguilera F., Gasperini S., Polletti S., Cosentino E., Tamassia N., Cassatella M.A. Human neutrophils produce CCL23 in response to various TLR-agonists and TNFα. Front. Cell. Infect. Microbiol. 2017;7:176. doi: 10.3389/fcimb.2017.00176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Asaoka D., Xiao J., Takeda T., Yanagisawa N., Yamazaki T., Matsubara Y., Sugiyama H., Endo N., Higa M., Kasanuki K., et al. Effect of probiotic Bifidobacterium breve in improving cognitive function and preventing brain atrophy in older patients with suspected mild cognitive impairment: Results of a 24-week randomized, double-blind, placebo-controlled trial. J. Alzheimers Dis. 2022;88:75–95. doi: 10.3233/JAD-220148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shi S., Zhang Q., Sang Y., Ge S., Wang Q., Wang R., He J. Probiotic Bifidobacterium longum BB68S improves cognitive functions in healthy older adults: A randomized, double-blind, placebo-controlled trial. Nutrients. 2022;15:51. doi: 10.3390/nu15010051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Akbari E., Asemi Z., Kakhaki R.D., Bahmani F., Kouchaki E., Tamtaji O.R., Hamidi G.A., Salami M. Effect of probiotic supplementation on cognitive function and metabolic status in Alzheimer’s disease: A randomized, double-blind and controlled trial. Front. Aging Neurosci. 2016;8:256. doi: 10.3389/fnagi.2016.00256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kim C.-S., Cha L., Sim M., Jung S., Chun W.Y., Baik H.W., Shin D.-M. Probiotic supplementation improves cognitive function and mood with changes in gut microbiota in community-dwelling older adults: A randomized, double-blind, placebo-controlled, multicenter trial. J. Gerontol. A Biol. Sci. Med. Sci. 2021;76:32–40. doi: 10.1093/gerona/glaa090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Melzack R. The McGill Pain Questionnaire: Major properties and scoring methods. Pain. 1975;1:277–299. doi: 10.1016/0304-3959(75)90044-5. [DOI] [PubMed] [Google Scholar]
- 60.Schulz K.F., Altman D.G., Moher D. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. BMC Med. 2010;8:18. doi: 10.1186/1741-7015-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bercik P., Denou E., Collins J., Jackson W., Lu J., Jury J., Deng Y., Blennerhassett P., Macri J., McCoy K.D., et al. The intestinal microbiota affect central levels of brain-derived neurotropic factor and behavior in mice. Gastroenterology. 2011;141:599–609. doi: 10.1053/j.gastro.2011.04.052. [DOI] [PubMed] [Google Scholar]
- 62.Rahimlou M., Hosseini S.A., Majdinasab N., Haghighizadeh M.H., Husain D. Effects of long-term administration of multi-strain probiotic on circulating levels of BDNF, NGF, IL-6 and mental health in patients with multiple sclerosis: A randomized, double-blind, placebo-controlled trial. Nutr. Neurosci. 2022;25:411–422. doi: 10.1080/1028415X.2020.1758887. [DOI] [PubMed] [Google Scholar]
- 63.Dehghani F., Abdollahi S., Shidfar F., Clark C.C.T., Soltani S. Probiotics supplementation and brain-derived neurotrophic factor (BDNF): A systematic review and meta-analysis of randomized controlled trials. Nutr. Neurosci. 2023;26:942–952. doi: 10.1080/1028415X.2022.2110664. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Datasets generated during the current study and/or analyzed during the current study are available from the responsible author upon reasonable request.