Abstract
Social learning through friendships is important in child development. Autistic children often initiate and engage in social interactions differently than neurotypical peers. LEGO® based therapy is a group intervention which facilitates social interactions with peers using collaborative LEGO® play. A 1:1 cluster randomised controlled trial with autistic children aged 7–15 comparing 12 weeks’ LEGO® based therapy and usual support to usual support alone in 98 mainstream schools (2017–2019) was carried out. The primary outcome was social skills (Social Skills Improvement System) completed by unblinded teachers (not intervention deliverers) at 20 weeks. Analysis used intention-to-treat. Fifty intervention schools (127 participants) and 48 control schools (123 participants) were allocated. Primary analysis included 45 intervention schools (116 participants) and 42 control schools (101 participants). The between-arms difference was 3.74 (p = 0.06, 95% confidence interval: −0.16, 7.63) and 1.68 (p = 0.43, 95% confidence interval: −2.51, 5.87) at 20 and 52 weeks (0.18 and 0.08 standardised effect sizes). Twenty-week outcomes for those receiving per protocol intervention were 4.23 (95% confidence interval 0.27, 8.19) with a standardised effect size of 0.21. Sensitivity estimates were between 3.10 and 4.37 (0.15–0.21 standardised effect sizes). Three unrelated serious adverse events were reported. LEGO® based therapy has a small positive non-significant benefit for social skills at 20 weeks but not 52 weeks.
Lay abstract
Autism is characterised by keen interests and differences in social interactions and communication. Activities that help autistic children and young people with social skills are commonly used in UK schools. LEGO® based therapy is a new activity that provides interesting and fun social opportunities for children and young people and involves building LEGO® models together. This study looked at LEGO® based therapy for the social skills of autistic children and young people in schools. It was a randomised controlled trial, meaning each school was randomly chosen (like flipping a coin) to either run LEGO® based therapy groups in school over 12 weeks and have usual support from school or other professionals, or only have usual support from school or other professionals. The effect of the LEGO® based therapy groups was measured by asking children and young people, their parents/guardians, and a teacher at school in both arms of the study to complete some questionnaires. The main objective was to see if the teacher’s questionnaire answers about the children and young people’s social skills changed between their first and second completions. The social skills of participants in the LEGO® based therapy groups were found to have improved in a small way when compared to usual support only. The study also found that LEGO® based therapy was not very costly for schools to run and parents/guardians and teachers said they thought it was good for their children and young people. We suggest further research into different potential benefits of LEGO® based therapy.
Keywords: ASD, autism, child mental health, LEGO® based therapy, school-based
Many autistic children and young people (Keating et al., 2022) experience social isolation and loneliness, feel anxious in social situations, are at greater risk of being bullied and have smaller friend groups than the general population (Bauminger & Kasari, 2000; Carrington and Graham, 2001; Rowley et al., 2012). Autistic children and young people commonly attend mainstream education environments but may struggle to pick up on social rules or norms encountered in everyday life (Travis et al., 2001). This can adversely impact their opportunities to develop social and emotional competence (Bagwell et al., 1998), lead to difficulties in creating and maintaining peer relationships, inadvertently widen developmental differences with the general population and in turn increase feelings of isolation and perceived exclusion (Bellini et al., 2007; Department for Education and Skills, 2002; Ochs et al., 2001). Indeed, perceived exclusion from friendship groups can negatively affect autistic and non-autistic children and young people’s mental health and emotional wellbeing as well as their quality of life and educational success (Sansoni et al., 2010; Killen et al., 2013).
Interventions to promote development of social and emotional skills are a commonly used school-based approach both generally (Durlak et al., 2011) and for autistic pupils (Dean & Chang, 2021; Gates et al., 2017; Hirvikoski et al., 2015; Hughes et al., 2012; M. Schmidt et al., 2020; Sutton et al., 2019; Wong et al., 2015). Other programmes involve both parent/guardian and teacher assistance (e.g. Paediatric Autism Communication Therapy-Generalised [PACT-G] (Green et al., 2022), Programme for the Enrichment of Relational Skills [PEERS] (Laugeson et al., 2012), Autism Spectrum Conditions – enhancing Nurture and Development [ASCEND] (Pillay et al., 2011). A Cochrane review (Reichow et al., 2012) of five studies showed some improvement in social competence following a range of different types of interventions for autistic young people of varying ages and demographics. Most of these interventions, however, employed a skills-deficit model and relied on adult or expert-led learning, which may affect acceptability and generalisability. A systematic review by Chang and Locke (2016) investigated peer-mediated interventions for this population specifically using group designs. Five studies were found: four randomised controlled trials (RCTs) and one pre- and post-design. Although all studies reported improvements in participant social skills following the intervention, the review concludes that more work is needed around study designs, standardised assessment tools and assessment of additional objectives (e.g. implementation fidelity). The review also suggests some areas for further research including different age groups or symptom severities. More recently, a review of school-based interventions which target the social communication skills of autistic pupils found a further 22 studies, though only three of these reported effect sizes or significance (Sutton et al., 2019).
Focus on delivery of non-specialist school-based interventions, which can often be administered at a fraction of the cost of specialist services, is increasing. Naveed and colleagues (2019) conducted a meta-analysis which assessed the effectiveness of 33 RCTs in multiple domains including communication, joint engagement and social skills of autistic pupils. Results demonstrated the effectiveness of these non-specialist interventions for social skill and communication outcomes.
One such non-specialist school-based intervention is LEGO® based therapy (LeGoff et al., 2014), a group social interaction and play-based programme gaining increasing popularity in UK schools. Despite its rapid roll out, there have been no large, fully powered RCTs to date. The intervention focuses on collaborative LEGO® play in small groups facilitated by a trained adult who promotes child-led decision making and group problem solving.
Lindsay and colleagues (2017) carried out a scoping review of 15 studies investigating LEGO® based therapy. It was found to have the potential to improve multiple social skills; however, reported sample sizes were consistently low and study designs and outcome measures were inconsistent. The review concludes that more rigorously designed trials of LEGO® based therapy with larger sample sizes are needed.
A more recent systematic review of LEGO® based therapy reported similar findings, highlighting poor methodologies and small sample sizes (Narzisi et al., 2021). This review too calls for more rigorously designed trials with standardised outcome measures and larger sample sizes to ensure relevant and generalisable study findings.
Methods
Study design
The I-SOCIALISE trial used a pragmatic assessor-unblinded two-arm cluster RCT design to examine the clinical effectiveness of LEGO® based therapy groups in addition to usual support on the social and emotional competence (specifically the perceived social skills) of autistic children and young people within the school setting, when compared with usual support alone (primary objective). The pre-published trial protocol included an internal pilot study assessing recruitment feasibility during the first 10 months of recruitment (Varley et al., 2019).
Given the high rates of co-occurring emotional and behavioural difficulties reported for most autistic children and young people, and the importance of investigating the potential impact of LEGO® based therapy on other aspects of everyday functioning, a range of standardised measures were used to assess secondary objectives including perceived isolation, academic competence, assertion, social control, externalising and internalising, and emotional and behavioural symptoms. Intervention cost-effectiveness, fidelity and acceptability were also investigated and are reported elsewhere (Barr et al., 2022; Wang et al., 2022a; Wright et al., in press).
Participants
Participants were aged 7–15 years attending mainstream schools in Northern England with a clinical diagnosis of autism as reported by parents/guardians based on the current UK diagnostic process (NICE cg128, National Institute for Health and Care Excellence (NICE), 2011) including a full developmental history and validated autism assessment. Eligible children scored ⩾ 15 on the Social Communication Questionnaire (SCQ) (Rutter et al., 2003), could understand simple instructions and had no serious impairments which would prevent participation. For each participant recruited, a parent/guardian, facilitator teacher/teaching assistant (TA) (to run the intervention in schools randomly allocated to this arm) and separate associated teacher/TA (to complete outcome measures for each participant but not participate in intervention training or delivery) were also recruited.
Important changes to methods
In March 2018, the 16-week post-randomisation follow-up timepoint was changed to 20 weeks to adapt to school need for more time to complete the 12 sessions of LEGO® based therapy.
In July 2020, the health economics analysis method was amended, altering the perspective from NHS and education to NHS and personal social services (PSS) with the education perspective included in a sensitivity analysis.
Sample size calculation
The sample size was calculated using Cochrane review results of the effects of social skills groups on social competence (Reichow et al., 2012). The authors reported that when group intervention was compared to usual support, a weighted mean standardised difference in social competence of 0.47 standard deviations (95% confidence interval from 0.16 to 0.78) was found. It was suggested that this defined a clinically significant change. Equal-sized clusters (schools) were assumed with 4 participants in each. The intra-cluster correlation (ICC) was assumed to be 0.01 based on a previous school-based intervention study undertaken in the same locality (Wright et al., 2016). Detecting a standardised effect size of 0.47 with 90% power and 5% two-sided significance requires 194 participants (97 per treatment arm). Allowing for attrition of 16% (the highest found in the Cochrane review), this number was increased to 232 participants (116 per treatment arm). Accounting for within-cluster correlation in both arms further inflates the sample size to 240 participants (30 school clusters, 120 participants per treatment arm).
Informed consent
Informed consent was gained from parents/guardians and associated and facilitator teachers/TAs, and assent from children or young people.
Procedures
Participants were recruited from mainstream primary (ages 5–11 years) and secondary (ages 11–16 years) schools in Northern England. Schools were contacted by the research team via telephone and email to discuss the study and potentially eligible participants. Interested schools were given information packs (containing participant information sheets and a contact information reply slip) to pass to parents/guardians. Interested families contacted the research team who provided detailed study information. Interested schools also passed on study information to the eligible pupil’s teacher/TA.
Informed consent was gained from adult participants and assent from children and young people. Following completion of baseline measures (collected face-to-face or by post), schools were randomised using remote randomisation stratified by education stage (primary or secondary) and number of eligible participants in the school (⩽6 or >6). Allocation was implemented using randomisation software provided by epiGenesys, a University of Sheffield company. EpiGenesys created a user interface to specifications provided by the trial’s randomisation statistician. Following recruitment, the trial manager entered school details and was provided with allocation results without seeing the randomisation lists or knowing any algorithm details that might allow them to predict the allocation of the next school recruited.
Research assistants (RA) collecting data were blind to treatment allocation to limit potential bias. Where RA unblinding was reported, any subsequent follow-ups were completed by a different blinded study team member. No participants were blind to treatment allocation, but trial statisticians were blind to this throughout.
Measures
Multiple outcome measures were completed by each type of participant at each timepoint either face-to-face or via email link (Table 1). Measures were selected to enable comparison with prior literature using standardised measures and to meet the demands of funding body reviewers. The primary outcome measure, the social skills improvement system (SSIS), has been shown to have good internal consistency, test–retest and inter-rater reliability and has been widely used to measure social skills changes in school settings (Crosby, 2011; Gresham et al., 2018; McLeod & McCrimmon, 2022).
Table 1.
Outcome measures.
| Participant type | Measure – PRIMARY | Timepoint (baseline, 20, and 52 weeks) |
|---|---|---|
| Associated teacher/TA | Social Skills Improvement System (SSIS) (Gresham & Elliott, 2008) scales: Social skills scale (PRIMARY OUTCOME MEASURE). 46 items, higher scores indicate greater social competence. Social skills including social communication, co-operation, social engagement, empathy, assertion, responsibility and self-control are measured. |
20 weeks |
| Participant type | Measure – SECONDARY | Timepoint (baseline, 20, and 52 weeks) |
| Associated teacher/TA | Social Skills Improvement System (SSIS) (Gresham & Elliott, 2008) scales: 1. Social skills scale. 46 items, higher scores indicate greater social competence. Social skills including social communication, co-operation, social engagement, empathy, assertion, responsibility and self-control are measured. 2. Problem behaviours scale. 30 items, higher scores indicate fewer problem behaviours. Academic competence scale. 7 items, higher scores indicate higher academic competence. |
All (social skills scale at 20 weeks is primary outcome) |
| Strengths and Difficulties Questionnaire (SDQ) (Goodman, 1997). 25 items, higher scores indicate a higher chance of developing a mental health disorder. | All | |
| Bespoke resource use questionnaires capturing resource implications of ‘usual support’ received by ACYP in both arms of the study. *Specific questions were included at 20 weeks to assess any adverse events | All *20 weeks only |
|
|
Facilitator teacher/TA (intervention arm only) |
Bespoke demographic information form collecting demographic information and training and experience of the facilitator teacher/TA. | Baseline only |
| Bespoke resource use questionnaire capturing resource implications of running the LEGO® based therapy sessions at school. *Specific questions were included in the session resource use questionnaire to assess any adverse events potentially attributable to the intervention. | After each session | |
| A fidelity checklist based on the existing treatment manual (LeGoff et al., 2014). 17 items, higher scores indicate higher treatment fidelity. | After each session | |
| A bespoke questionnaire to assess acceptability of the intervention structured around the Theoretical Framework of Acceptability (Sekhon et al., 2017). 11 items, higher scores indicate greater acceptability. | 20 weeks only | |
| Autistic child/young person | Multidimensional Scale of Perceived Social Support (Zimet et al., 1988). 12 items, higher scores indicate a higher degree of perceived social support. | All |
| Asher Loneliness Scale (Asher et al., 1984). 24 items, higher scores indicate lower levels of loneliness and social dissatisfaction. | All | |
| Child Health Utility 9D (CHU-9D) (Stevens, 2011). 9 items, higher scores indicate higher health utility. | All | |
| Parent/guardian | The Social Communication Questionnaire (SCQ) (Rutter et al., 2003). 40 items, higher scores indicate more social communication difficulties. | Baseline only |
| SSIS (Gresham & Elliott, 2008) scales: 1. Social skills scale. 46 items, higher scores indicate greater social competence. Problem behaviours scale. 33 items, higher scores indicate fewer problem behaviours. |
All | |
| SDQ (Goodman, 1997). 25 items, higher scores indicate a higher chance of developing a mental health disorder. | All | |
| EQ-5D-Y (3 L proxy version) (The EuroQol Group, 1990). 5 items, higher scores indicate higher health utility. | All | |
| Bespoke resource use questionnaires to capture healthcare and non-health resource implications attributable to the ACYP’s autism. *Specific questions were included in resource use form at 20 weeks to assess any adverse events – 20 weeks only. |
All *20 weeks only |
|
| Bespoke questionnaire to assess acceptability of the intervention structured around the Theoretical Framework of Acceptability (Sekhon et al., 2017). 11 items, higher scores indicate greater acceptability. | Intervention arm and 20 weeks only. | |
| Bespoke demographic information form collecting demographic information pertaining to the ACYP and the parent/guardian. | Baseline only |
SSIS: social skills improvement system; SDQ: Strengths and Difficulties Questionnaire; CHU-9D: Child health utility 9D; SCQ: Social Communication Questionnaire; ACYP: Autistic children and young people.
Intervention
LEGO® based therapy is a group social interaction and play-based intervention designed to offer playful opportunities for meaningful social interactions with peers. Through collaborative LEGO® play facilitated by a trained adult, autistic children and young people can experience supported opportunities to practise skills and have positive social experiences. Sessions involve building LEGO® models collaboratively, for example, with instructions in different roles (the engineer; shows everyone the picture and describes the instructions; the supplier finds the pieces indicated by the engineer and the builder puts the pieces together). Participants work together, swap roles frequently and take part in group decision making and team collaboration to help each other build the model. They can also build their own creations and designs together and decide as a team what LEGO® building activities to engage in. A trained adult carefully and playfully guides the group when needed, promoting collaborative working and problem solving, using experiential learning, and avoiding didactic teaching and instruction-giving. As a child-led activity, the types of models built differ according to the participant interests, building abilities and age. Deciding which model to build together as a team is part of the social problem solving in which children and young people engage during the sessions.
Potential mechanisms of change for this intervention are hypothetical. Autistic young people are often socially isolated and excluded. Attending a safe, playful group offers children meaningful social opportunities where they can develop social skills and build relationships. This could have a positive effect on self-esteem, reduce social isolation and improve emotional wellbeing, potentially leading to more confidence and appraisal of ability to cope in other social situations and increased likelihood of practising social skills. This in turn may help reduce social anxiety and improve social skills. More information can be found in the published trial protocol (Varley et al., 2019).
For the I-SOCIALISE study, LEGO® based therapy groups were held face-to-face in schools. Members of staff (‘facilitators’) with experience of autism ran 12 weekly hour-long intervention sessions. Facilitators were given a standard set of wide-ranging LEGO® models from which the children and young people in their group could choose, along with a set of freestyle LEGO® bricks for their own designs. Facilitators attended 3-h training in intervention delivery run by local authority staff and study team members. They also received training materials, an intervention manual (available via www.comic.org.uk) and editable versions of the resources from the manual. Training enabled facilitators to adapt elements of the intervention to suit participants in their group including LEGO® sets used, rules and rewards. Schools were provided with all materials needed to run the sessions.
Participants in schools allocated to the intervention arm also received ‘usual support’ (see below).
Usual support
A range of usual support was provided by school, primary care and/or community services in both arms. This included 1:1 support from teaching staff, educational interventions such as Social Stories™ (Wright et al., 2016) and Social-Communication Emotional Regulation and Transactional Support (SCERTS) (Rubin et al., 2013). Primary care and community services also provided a range of therapeutic and/or clinical services. Comparison between groups is reported elsewhere (Wang et al., 2022a).
Effectiveness analysis
The planned primary analysis used the intention-to-treat (ITT) principle. Alongside this, pre-planned per-protocol (PP) analysis was conducted defined as participants receiving at least half the planned sessions (n = 6) based on pre-specified clinical expert agreement. Robustness of the PP analysis was investigated by complier average causal effect analysis using treatment as an instrument for per-protocol compliance in a two-stage least-squares regression. Multiple imputation was used to assess robustness of the primary analysis to missing values at baseline and follow-up. Imputation used chained equation and all model parameters including treatment arm in the imputation equation. An as-treated analysis was undertaken to account for the school randomised to the control arm, which mistakenly delivered the intervention. In this analysis, the school was included in the intervention arm. A final sensitivity analysis used the subset of participants for whom baseline and outcome data were provided by the same associated teacher/TA. Intervention sustainability was investigated using the primary outcome at 52 weeks.
All analyses used a linear mixed model with treatment arm, age, sex, baseline score and stratification variables as fixed effects with a school random effect and robust standard errors to account for clustering. The stratification variables were number of autistic children and young people in the school (⩽ six or > six) and school level (primary or secondary).
Mixed methods substudy
A mixed methods substudy was conducted to assess fidelity and acceptability of the intervention. Intervention fidelity was assessed using a fidelity checklist and video recordings and acceptability was measured via an acceptability questionnaire and qualitative interviews.
Health economics substudy
An economic evaluation was conducted to assess the cost-effectiveness of LEGO® based therapy and usual support versus usual support alone from the NHS and PSS perspective and the societal perspective.
Community involvement statement
The I-SOCIALISE research team worked with several patient and public involvement (PPI) representatives throughout the study. The Young Dynamos research advisory group and the National Autistic Society (NAS) were involved in the overall design of the study and provided feedback on participant facing documents, intervention delivery and other key elements (e.g. planning for schools with fewer than three participants). A parent of an autistic young person was a member of the trial steering committee (TSC) and provided insight into lived experience of autism throughout the trial. PPI representatives were also involved in the write-up of the study report to the funder in the form of feeding back on the lay summary and discussing the best use of terminology for research outputs.
Results
Effectiveness analysis results
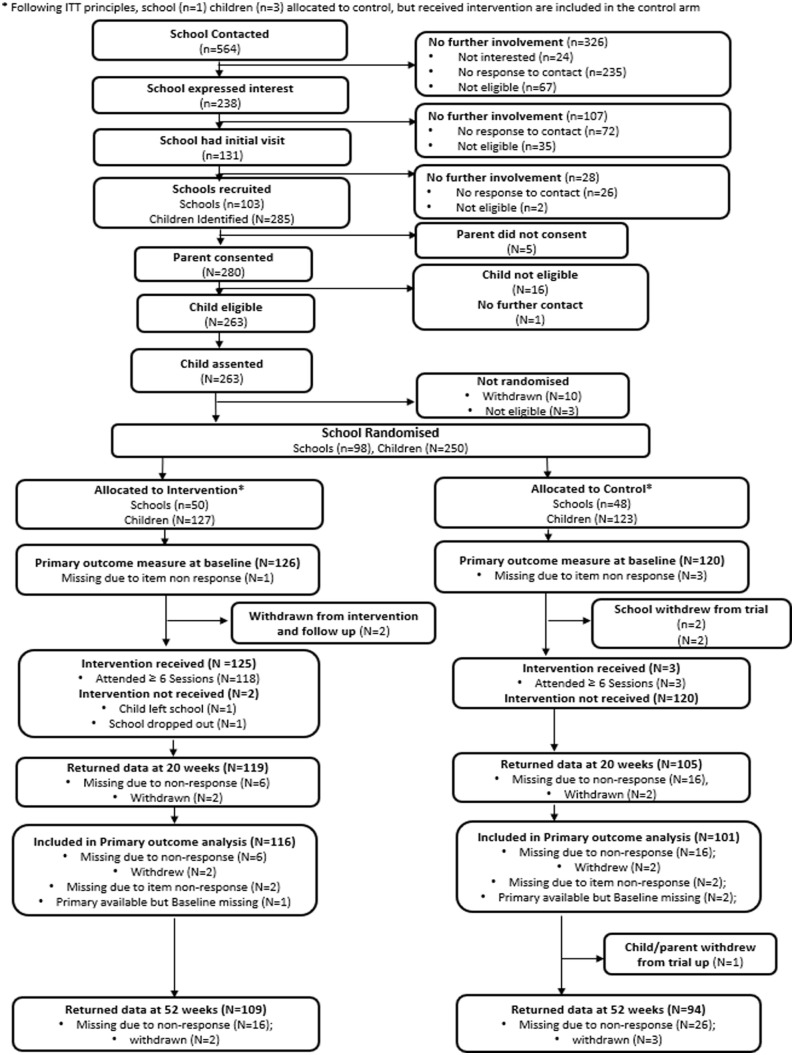
Ninety-eight schools with 250 autistic participants were recruited between October 2017 and March 2019, with 20-week and 52-week follow-ups conducted between March 2018 and June 2020. Fifty schools (127 participants) were randomised to the intervention arm and 48 schools (123 participants) to the control arm. One school randomised to the control arm (3 participants) was allocated to the intervention arm in error. ITT analysis included this misallocated school in the intended control arm. Per protocol analysis excluded this misallocated school. Figure 1 shows the flow of participants through the trial and follow-up. Participant withdrawal or loss to follow-up was 10% between randomisation and 20 weeks (n = 26), rising to 19% at 52 weeks (n = 48). No participants were excluded.
Figure 1.
CONSORT flow diagram.
The study was in its final stages of follow-up data collection when the COVID-19 pandemic began. There was no impact on the primary outcome timepoint (20 weeks). Between 1 and 3 participants did not complete their 52-week follow-ups between March and June 2020, potentially due to impacts of the pandemic (e.g. social distancing). Participants may have also reported higher levels of anxiety in their outcome measures due to the pandemic; however, it is unclear if this occurred.
Primary outcome measure (social skills scale of the SSIS) and complete baseline data were available for 217 (87%) participants: 116 intervention participants (91%) and 101 control participants (82%). The primary outcome ITT analysis included 45 (90%) intervention schools and 42 (88%) control schools. The average number of children and young people in schools (i.e. average cluster sizes) were 2.6 and 2.4 in intervention and control schools, respectively. Table 2 shows balanced baseline demographic characteristics across arms. Specific data on socioeconomic status were not recorded.
Table 2.
Autistic child/young person baseline demographic characteristics, ITT.
| Intervention | Control | ||
|---|---|---|---|
| (n = 127) | (n = 123) | ||
| Categorical Variables | |||
| Gender | Male | 102 (80%) | 92 (75%) |
| Female | 25 (20%) | 31 (25%) | |
| Age group at start of school year | 6–10 | 89 (70%) | 86 (70%) |
| 11–14 | 38 (30%) | 37 (30%) | |
| Ethnicity | White | 105 (83%) | 108 (88%) |
| Asian/Asian British | 9 (7%) | 4 (3%) | |
| Mixed/Multiple ethnic groups | 4 (3%) | 7 (6%) | |
| Black/African/Caribbean/Black British | 5 (4%) | 1 (1%) | |
| Other ethnic groups | 3 (2%) | 1 (1%) | |
| Prefer not to say | 1 (1%) | 2 (2%) | |
| Continuous variables | |||
| Age | N (%) | 127 (100%) | 123 (100%) |
| Mean (SD) | 9.6 (2.3) | 9.7 (2.1) | |
| Median (IQR) | 9 (8, 11) | 9 (8, 11) | |
| Min., Max. | 7, 15 | 7, 15 | |
| SCQ score | N (%) | 127 (100%) | 123 (100%) |
| Mean (SD) | 25.1 (5.2) | 24.2 (5.2) | |
| Median (IQR) | 25 (22, 29) | 24 (21, 28) | |
| Min., Max. | 15, 37 | 15, 36 | |
| SSIS social skills (teacher) | N (%) | 126 (99%) | 120 (98%) |
| Mean (SD) | 66.1 (19.3) | 64.9 (21.4) | |
| Median (IQR) | 64 (50, 79) | 66 (48, 77) | |
| Min., Max. | 29, 117 | 26, 129 | |
SD: standard deviation; IQR: inter-quartile range; SCQ: Social Communication Questionnaire; SSIS: social skills improvement system.
Table 3 shows the difference in primary outcome between arms at baseline and 20 weeks and the difference at 20 weeks after adjusting for baseline score and other covariates. Table 4 summarises the differences between arms estimated by primary and planned sensitivity analysis.
Table 3.
Teacher SSIS social skills subscale at 20 weeks ITT difference between arms and intra-cluster correlation coefficient.
| Descriptive statistics | Model estimates | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Treatment | Control | Differences | |||||||
| (n = 127) | (n = 123) | ||||||||
| n (%) | Mean | SD | n (%) | Mean | SD | Mean diff (95% CI) | Adjusted mean diff (95% CI) | p-value | |
| Baseline | 126 (99%) | 66.12 | 19.32 | 120 (98%) | 64.90 | 21.45 | 1.22 (−3.88, 6.32) | ||
| 20 weeks | 117 (92%) | 72.93 | 18.81 | 103 (84%) | 69.78 | 20.21 | 3.15 (−2.01, 8.31) | ||
| Overall | 3.74 (−0.16, 7.63) | 0.06 | |||||||
| ICC | ICC controlling for covariates | 0.00 | |||||||
| ICC (unconditional) | 0.10 | ||||||||
SD: standard deviation; CI: confidence interval; ICC: intra-cluster correlation.
Table 4.
Summary of sensitivity analysis for teacher SSIS social skills subscale at 20 weeks.
| n | Adjusted mean diff (95% CI) | p-value | Standardised effect size | |
|---|---|---|---|---|
| Misallocated school a | 217 | 4.37 (0.53, 8.20) | 0.026 | 0.21 |
| Teacher providing score b | 184 | 3.92 (0.02, 7.81) | 0.049 | 0.19 |
| Per protocol c | 207 | 4.23 (0.27, 8.19) | 0.036 | 0.21 |
| Complier average causal effect d | 217 | 3.97 (−0.11, 8.06) | 0.056 | 0.19 |
| Multiple imputation e | 250 | 3.10 (−0.74, 6.95) | 0.110 | 0.15 |
CI: confidence interval.
The school allocated to control and receiving treatment is included in the treatment arm. Same model as primary analysis.
Excludes participants for whom a different teacher provided the scores at baseline and 20 weeks. Same model as primary analysis.
As described in efficacy analysis below. Same model as primary analysis.
As described in efficacy analysis below
As described in efficacy analysis below.
The effect of LEGO® based therapy on the social skills scale of the teacher/TA-rated SSIS in the ITT analysis was 3.74 at 20 weeks (p = 0.06, 95% CI: −0.16, 7.63) and 1.68 at 52 weeks (p = 0.43, 95% CI: −2.51, 5.87). The standardised ITT treatment effect sizes at 20 and 52 weeks were 0.18 and 0.08, where standardised effect sizes are calculated by rescaling the estimated mean difference by pooled standard deviation at baseline (20.4). Twenty-week mean main outcome difference for those receiving per protocol intervention of six sessions or more was 4.23 (95% CI 0.27, 8.19) with a standardised effect size of 0.21. The treatment effect at 20 weeks using planned sensitivity analysis ranged between 3.10 and 4.37 or between 0.15 and 0.21 (p-values between 0.026 and 0.11) Although the primary analysis was not statistically significant at the 5% level, the p-values in the sensitivity analysis span the 5% threshold and the ITT and sensitivity analysis provides consistent evidence that LEGO® based therapy groups seemed to have a small positive effect on participant social and emotional skills at 20 weeks.
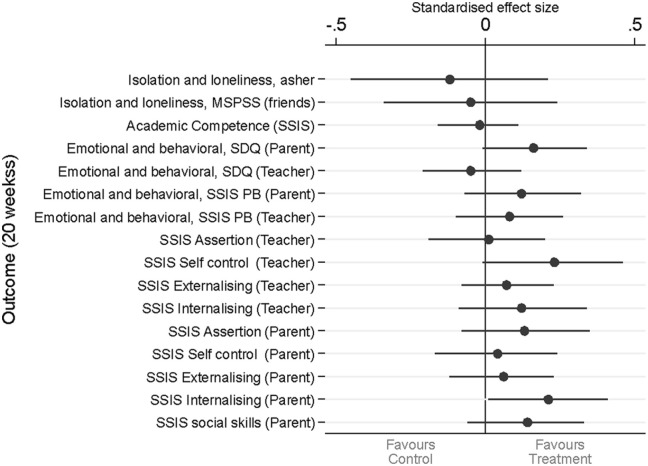
Figure 2 shows a Forest plot of the secondary outcomes at 20 weeks. Most secondary outcomes favour the treatment arm, but the effects are generally small and statistically non-significant. Table 5 shows there was no evidence of sustainability of effect on social skills at 52 weeks.
Figure 2.
Forest plot of secondary outcomes at 20 weeks.
Adjusted difference between arms (and confidence limits) divided by pooled standard deviation at baseline and multiplied by −1 if lower scores are associated with an improvement.
Table 5.
Secondary outcomes – sustainability of effect on social skills.
| Adjusted mean diff (95% CI) | p-value | ||
|---|---|---|---|
| Sustainability of effect on Social Skills | SSIS Social Skills subscale (Teacher) | ||
| 52 weeks | 1.68 (−2.51, 5.87) | 0.43 |
CI: confidence interval; SSIS: social skills improvement system.
Planned and unplanned moderator analysis was undertaken but was not conclusive. The moderator analysis investigated treatment moderation by autism severity, school level and number of autistic pupils in schools. Baseline SCQ scores were a proxy for autism severity and the analysis was pre-planned. Other moderators were randomisation stratification variables and not planned. Separate models for each subgroup were fitted and a treatment–subgroup interaction was separately added to the main model. Results suggest effectiveness may be greater in secondary schools, schools with > six autistic pupils and pupils with less severe symptomatology (Table 6). Further investigation, exploring moderation by these subgroups for six secondary outcomes, found further support for moderation by school level only. Results are available on request. We were, however, not powered for subgroup analysis and three subgroups increase the risk of false positives.
Table 6.
Moderation by subgroup.
| Subgroup | Category | n | Adjusted mean diff (95% CI) | p | Interaction p-value |
|---|---|---|---|---|---|
| Autism severity (SCQ score) | Low (< 22) | 78 | 8.32 (2.56, 14.09) | 0.005 | 0.08 |
| Medium (23–27) | 73 | 3.65 (−2.50, 9.80) | 0.245 | ||
| High (> 28) | 66 | −2.64 (−9.71, 4.43) | 0.465 | ||
| Autistic pupils in school | < 6 | 156 | 2.30 (−2.10, 6.70) | 0.306 | 0.11 |
| >= 6 | 61 | 8.23 (1.79, 14.68) | 0.012 | ||
| School level | Primary | 153 | 1.86 (−2.08, 5.80) | 0.355 | 0.20 |
| Secondary | 64 | 7.45 (−0.93, 15.83) | 0.081 |
CI: confidence interval; SCQ: Social Communication Questionnaire.
Two serious adverse events were reported for the treatment arm and one for the control arm. None were related to the intervention. Details are available on request.
Mixed methods substudy results
Analysis of intervention fidelity was positive with good self-reported (91%) and independent reviewer-reported (77%) fidelity to the intervention. Further details of this and intervention acceptability are reported elsewhere (Barr et al., 2022; Wright et al., in press).
Health economics substudy results
Health economics analysis results indicate that, compared to usual support only, LEGO® based therapy and usual support produced marginal but robust reduction in costs and improvement in quality-adjusted life years from both perspectives, suggesting it is likely to be cost-effective. Details and results are reported elsewhere (Wang et al., 2022a).
Discussion
Main findings
Primary and sensitivity analyses suggest LEGO® based therapy groups had a small positive effect on social and emotional skills at 20 weeks. This was non-significant on ITT analysis and significant on PP, but with small effect sizes (0.21). The forest plot of outcomes shows that small benefits are supported by secondary outcomes, which can be seen mainly in positive directions (Figure 2). Although ¾ of these favour the intervention, the CIs cross 0 for most, suggesting caution in interpretation. LeGoff and colleagues (2014) maintain that effects continue to accrue when the intervention goes on for longer (e.g. after school clubs); however, we were not able to test this. Mixed methods substudy findings (Barr et al., 2022) that the intervention is received positively by those involved would support further research. It was also indicated that the effect could be larger in secondary school autistic children and young people. Explanations for this difference may include secondary school children and young people being developmentally more able to make use of the intervention. Pragmatic community-based trials often result in lower effect sizes compared with university-based clinical trials (Nahmias, 2019). This may explain why LEGO® based therapy groups in this real-world setting showed lower effect sizes.
In summary, the results show limited effect with 6–12 sessions of therapy. To contextualise this, the mean 3- to 4-point changes found on the SSIS may represent, for example, improvements in social problem skills and/or social interactional skills such as greeting and co-operation. We believe that the intervention remains worthy of further research.
The team found strong willingness of schools to be involved despite research demands. This is positive and perhaps reflects how the study addressed school needs raised by previous researchers including manualisation, good fit for school environments and availability of more school-based interventions for this population (Kasari & Smith, 2013).
Strengths of the trial
This is the first large-scale RCT investigating the clinical and cost-effectiveness of LEGO® based therapy delivered in schools by school staff. It addressed the limitations of previous studies by using a larger sample size, achieving successful recruitment to target and employing standardised outcome measures focusing on social skill development (primary outcome), academic attainment and emotional and behavioural skills and difficulties (secondary outcomes).
This study benefitted from a high level of PPI from the Young Dynamos group, NAS and a parent of an autistic young person. They advised on overall study design and materials used including participant facing documents and communications.
Limitations
The primary outcome was rated by associated teachers/TAs not blind to treatment allocation. Although these teachers/TAs were not directly involved in intervention delivery, they may have held pre-existing views about its efficacy, potentially introducing bias into their assessments. However, if such bias exists, there is no evidence about whether it would positively or negatively affect the estimated treatment effect.
There was minor differential attrition in the treated group (10% schools, 9% participants) compared to the control group (12% schools, 18% participants) for the primary outcome. However, when multiple imputation was used to account for attrition, the between-group difference reduced to 3.1.
No subgroup interactions were significant. As such, separate estimates for each subgroup should be treated with caution and are presented to inform possible future research and meta-analysis.
Despite recruiting from a relatively large geographical area, the sample was not representative of the cultural diversity across the UK, though the gender balance does reflect current literature (Lai et al., 2015). In keeping with published findings, the SDQ and other measures of social functioning and isolation confirmed that this sample of autistic participants likely had additional social, behavioural, and mental health comorbidities. However, the school-based study design used here did not include any opportunities for either individual assessments or obtaining additional in-depth information about co-occurring health conditions.
It is possible that the COVID-19 pandemic may have impacted follow-up assessments through, for example, the processes of school closures, teacher/TA changes and reduced available education and health resources locally (Wang et al., 2022b).
The longer-term 52-week follow-up timepoint is a strength compared to shorter follow-up periods of many intervention studies in this area. However, this longer-term follow-up often meant that the children or young people had moved to a new class or school with a new associated teacher/TA, potentially impacting upon reliability. It is also possible that, in keeping with well-established theories about supporting and enhancing developmental progress over time (Cantor et al., 2019), the effect of this 6- to 12-week intervention might not extend without additional input to build on progress as previously suggested by LeGoff and colleagues (2014).
Implications for practice and policy
Establishing the delivery of timely and effective school-based interventions is one potential way of addressing inequities in health care outcomes (Knopf et al., 2016). Autistic pupils in both mainstream and specialist schools can receive a wide range of interventions, from whole-school approaches to targeted interventions (Dean & Chang, 2021; Gates et al., 2017; MacKenzie & Williams, 2018). Many of these approaches have limited or no research evidence of clinical or cost-effectiveness and often involve external professionals with specialist expertise (e.g. speech and language therapists). Though there are several interventions that can be delivered by teachers/TAs in an individual and/or group setting (e.g. visual schedules, Social Stories™), many have had limited evaluation, typically without an RCT design. As far as the research team are aware, LEGO® based therapy delivered by school staff with specific training is the first intervention evaluated using an adequately powered RCT design.
Based on overall findings, we suggest that implementation of LEGO® based therapy in schools does no apparent harm and is well received by participating children and young people, teachers/TAs and parents/guardians. It may make a small contribution to social skills development for autistic children and young people alongside other support, particularly given the limited resources currently available for specialist interventions in the UK. Furthermore, substudy findings (Barr et al., 2022; Wang et al., 2022a) have identified that LEGO® based therapy is an acceptable and enjoyable intervention for autistic pupils attending mainstream schools, which can reduce the need for access to CAMHS and specialist services. Results also show that this intervention can be integrated into everyday school provision and can be implemented without the need for additional resources following diagnosis.
Conclusion
Previous systematic reviews of school-based social skills interventions have suggested promise, though more research is needed (Dean & Chang, 2021). To date, we have not explored the specific mechanisms of action of LEGO® based therapy, although these might be investigated in future research. Mechanisms may include social problem-solving skill development and self-esteem building in the context of positive social interactions, establishment of successful communicative partnerships and social identity (LeGoff & Sherman, 2006). Peer support, feeling connected to and spending time with autistic peers may also be an important component of intervention (Crompton et al., 2022). Further, it would be helpful to evaluate whether outcomes are improved with a longer intervention duration (e.g. full school year), or more frequent sessions (e.g. twice weekly).
The length and depth of training received, and the skills of trained facilitators, could be explored regarding impact on outcomes and optimal delivery, as could the influence of ongoing support and supervision for those delivering the intervention.
Future research to investigate whether subgroups of autistic children and young people (and/or groups with other social communication difficulties) may benefit in different ways at different developmental stages from LEGO® based therapy may be helpful. For example, whether those with more severe symptomatology benefit as much as those with milder symptoms.
Overall, this study shows that LEGO® based therapy is worthy of further research as it may have a small positive effect leading to improved social interactions for autistic children and young people in the short term.
Acknowledgments
We gratefully acknowledge the hard work, support and advice from the following:
PPI representatives: The Young Dynamos research advisory group, the National Autistic Society, Karen Watson (PPI TSC member), the York Youth Council and several individuals including Tina Hardman and Ann McLaren. Participant screening and data collection: Jules Beresford-Dent, Sarah Jacob-Eshtan, Lisa Hackney, Rebecca Joy, Sam Bennett, Emma Sellers, Holly Taylor, Alix Smith, Katie Sutherland, Richard Campbell, Rachel Hodkinson, Megan Garside, Jane Blackwell, Pavithra Kumar, Jennifer Lomas. Administrative and clerical support: Sharon Bird, Rita Lynch, Daniel Gottschalk, Katy Harmston, Thasamia Akhtar, Louise Turner, Heather Dakin. Sponsor Study monitoring: Tahir Idrees. LEGO® based therapy expertise: Elinor Brett, Abigail Dodson. Support on data management concerns: Emily Turton, Richard Campbell. Support on ethical and governance issues: Sinead Audsley and Stephen Holland.
Footnotes
Authors’ note: LEGO® is a registered trademark with a fair use policy which will be adhered to throughout the duration of the trial. Discussions with the LEGO® Foundation have led to agreement of the use of this term solely for this project and its outputs. With patient and public involvement input, the term LEGO® based therapy has been paired with the new term Play Brick Therapy, which we suggest is used henceforth.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship and/or publication of this article: Co-applicant Gina Gomez de la Cuesta co-authored the LEGO® based therapy manual which formed the basis of the delivered intervention. The co-authors of the manual have given full permission to use it without licence and to develop an abridged version to become available. Co-applicant Gomez de la Cuesta has also agreed for the team to adapt the fidelity checklist used in her previous study. Co-applicant Gomez de la Cuesta is a Director of Play Included, a community interest company that offers training and resources for interventions involving play bricks for children. Play included CIC is a partner of the LEGO® Foundation.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: The trial was funded by the National Institute for Health Research’s Public Health Research programme (PHR15/49/32; ISRCTN64852382 http://isrctn.org).
Ethical approval: The study received positive ethical opinion from the Health Research Authority (18/HRA/0101) and the University of York Department of Health Sciences Research Ethics Committee.
ORCID iDs: Barry Wright  https://orcid.org/0000-0002-8692-6001
https://orcid.org/0000-0002-8692-6001
Ellen Kingsley  https://orcid.org/0000-0002-0964-4588
https://orcid.org/0000-0002-0964-4588
David Marshall  https://orcid.org/0000-0001-5969-9539
https://orcid.org/0000-0001-5969-9539
Data sharing: We support the principle of Open Science and access to methods, data and code. Requests for patient-level data and statistical code should be made to the corresponding author and will be considered by members of the original trial management group, including the chief investigator and members of CTRU, who will release data on a case-by-case basis. The data will not contain any direct identifiers, and indirect identifiers will be minimised. Free text data will be removed to minimise the risk of identification.
References
- Asher S. R., Hymel S., Renshaw P. D. (1984). Loneliness in children. Child Development, 1, 1456–1464. [Google Scholar]
- Bagwell C. L., Newcomb A. F., Bukowski W. M. (1998). Preadolescent friendship and peer rejection as predictors of adult adjustment. Child Development, 69(1), 140–153. [PubMed] [Google Scholar]
- Barr A., Coates E., Kingsley E., Biggs K., Le Couteur A., Wright B. (2022). A mixed methods evaluation of the acceptability of therapy using LEGO® bricks (LEGO® based therapy) in mainstream primary and secondary education. Autism Research, 15, 1237–1248. 10.1002/aur.2725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauminger N., Kasari C. (2000). Loneliness and friendship in high-functioning children with autism. Child Development, 71(2), 447–456. [DOI] [PubMed] [Google Scholar]
- Bellini S., Peters J. K., Benner L., Hopf A. (2007). A meta-analysis of school-based social skills interventions for children with autism spectrum disorders. Remedial and Special Education, 28(3), 153–162. [Google Scholar]
- Cantor P., Osher D., Berg J., Steyer L., Rose T. (2019). Malleability, plasticity, and individuality: How children learn and develop in context. Applied Developmental Science, 23(4), 307–337. [Google Scholar]
- Carrington S., Graham L. (2001). Perceptions of school by two teenage boys with Asperger syndrome and their mothers: A qualitative study. Autism, 5(1), 37–48. [DOI] [PubMed] [Google Scholar]
- Chang Y. C., Locke J. A. (2016). A systematic review of peer-mediated interventions for children with autism spectrum disorder. Research in Autism Spectrum Disorders, 27, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crompton C. J., Hallett S., Axbey H., McAuliffe C., Cebula K. (2022). ‘Someone like-minded in a big place’: Autistic young adults’ attitudes towards autistic peer support in mainstream education. Autism, 27, 76–91. 10.1177/13623613221081189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crosby J. W. (2011). Test review: F.M. Gresham & S. N. Elliott Social Skills Improvement System Rating Scales. Minneapolis, MN: NCS Pearson, 2008. Journal of Psychoeducational Assessment, 29(3), 292–296. 10.1177/0734282910385806 [DOI] [Google Scholar]
- Dean M., Chang Y.-C. (2021). A systematic review of school-based social skills interventions and observed social outcomes for students with autism spectrum disorder in inclusive settings. Autism, 25, 1828–1843. [DOI] [PubMed] [Google Scholar]
- Department for Education and Skills. (2002). Autistic spectrum disorders: Good practice guidance. [Google Scholar]
- Durlak J. A., Weissberg R. P., Dymnicki A. B., Taylor R. D., Schellinger K. B. (2011). The impact of enhancing students’ social and emotional learning: A meta-analysis of school-based universal interventions. Child Development, 82(1), 405–432. [DOI] [PubMed] [Google Scholar]
- The EuroQol Group. (1990). EuroQol – a new facility for the measurement of health-related quality of life. Health Policy (New York), 16(3), 199–208. [DOI] [PubMed] [Google Scholar]
- Gates J. A., Kang E., Lerner M. D. (2017). Efficacy of group social skills interventions for youth with autism spectrum disorder: A systematic review and meta-analysis. Clinical Psychology Review, 52, 164–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman R. (1997). The Strengths and Difficulties Questionnaire: A research note. Journal of Child Psychology and Psychiatry, 38(5), 581–586. [DOI] [PubMed] [Google Scholar]
- Green J., Leadbitter K., Ellis C., Taylor L., Moore H. L., Carruthers S., James K., Taylor C., Balabanovska M., Langhorne S., Aldred C., Slonims V., Grahame V., Parr J., Humphrey N., Howlin P., McConachie H., Le Couteur A., Charman T., Emsley R., Pickles A. (2022). Combined social communication therapy at home and in education for young autistic children in England (PACT-G): A parallel, single-blind, randomised controlled trial. The Lancet Psychiatry, 9(4), 307–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gresham A. F., Elliott S. N. (2008). Social Skills Improvement System (SSIS) Rating Scales. Pearson Assessments. [Google Scholar]
- Gresham A. F., Elliott S. N., Metallo S., Byrd S., Wilson E., Erickson M., Cassidy K., Altman R. (2020). Psychometric fundamentals of the social skills improvement system: Social-emotional learning edition rating forms. Assessment for Effective Intervention, 45(3), 194–209. [Google Scholar]
- Hirvikoski T., Jonsson U., Halldner L., Lundequist A., de Schipper E., Nordin V., Bölte S. (2015). A systematic review of social communication and interaction interventions for patients with autism spectrum disorder. Scandinavian Journal of Child and Adolescent Psychiatry and Psychology, 3(3), 147–168. [Google Scholar]
- Hughes C., Kaplan L., Bernstein R., Boykin M., Reilly C., Brigham N., Cosgriff J., Heilingoetter J., Harvey M. (2012). Increasing social interaction skills of secondary school students with autism and/or intellectual disability: A review of interventions. Research and Practice for Persons with Severe Disabilities, 37(4), 288–307. [Google Scholar]
- Kasari C., Smith T. (2013). Interventions in schools for children with autism spectrum disorder: Methods and recommendations. Autism, 173(3), 254–267. [DOI] [PubMed] [Google Scholar]
- Keating C. T., Hickman L., Leung J., Monk R., Montgomery A., Heath H., Sowden S. (2022). Autism-related language preferences of English-speaking individuals across the globe: A mixed methods investigation. Autism Research, 16, 406–428. 10.1002/aur.2864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killen M., Mulvey K. L., Hitti A. (2013). Social exclusion in childhood: A developmental intergroup perspective. Child Development, 84(3), 772–790. [DOI] [PubMed] [Google Scholar]
- Knopf J. A., Finnie R. K., Peng Y., Hahn R. A., Truman B. I., Vernon-Smiley M., Johnson V. C., Johnson R. L., Fielding J. E., Muntaner C., Hunt P. C. (2016). School-based health centers to advance health equity: A community guide systematic review. American Journal of Preventive Medicine, 51(1), 114–126. 10.1016/j.amepre.2016.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai M. C., Lombardo M. V., Auyeung B., Chakrabarti B., Baron-Cohen S. (2015). Sex/gender differences and autism: Setting the scene for future research. Journal of the American Academy of Child and Adolescent Psychiatry, 54(1), 11–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laugeson E. A., Frankel F., Gantman A., Dillon A. R., Mogil C. (2012). Evidence- based social skills training for adolescents with autism spectrum disorders: The UCLA PEERS program. Journal of Autism and Developmental Disorders, 42(6), 1025–1036. [DOI] [PubMed] [Google Scholar]
- LeGoff D. B., Gomez De, La Cuesta G., Krauss G. W., Baron-Cohen S. (2014). LEGO®- based therapy: How to build social competence through Lego®-based clubs for children with autism and related conditions. Jessica Kingsley Publishers. [Google Scholar]
- LeGoff D. B., Sherman M. (2006). Long-term outcome of social skills intervention based on interactive LEGO© play. Autism, 10(4), 317–329. 10.1177/1362361306064403 [DOI] [PubMed] [Google Scholar]
- Lindsay S., Hounsell K. G., Cassiani C. (2017). A scoping review of the role of LEGO® therapy for improving inclusion and social skills among children and youth with autism. Disability and Health Journal, 10(2), 173–182. [DOI] [PubMed] [Google Scholar]
- MacKenzie K., Williams C. (2018). Universal, school-based interventions to promote mental and emotional well-being: What is being done in the UK and does it work? A systematic review. British Medical Journal Open, 8(9), Article e022560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeod J., McCrimmon A. W. (2022). Variables associated with successful treatment outcomes of autistic youth enrolled in PEERS. Frontiers in Psychiatry, 13, Article 834801. 10.3389/fpsyt.2022.834801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahmias A.S., Pellecchia M., Stahmer A.C., Mandell D.S. (2019), Effectiveness of community-based early intervention for children with autism spectrum disorder: a meta-analysis. Journal of Child Psychology and Psychiatry, 60, 1200–1209. [DOI] [PubMed] [Google Scholar]
- Narzisi A., Sesso G., Berloffa S., Fantozzi P., Muccio R., Valente E., Viglione V., Villafranca A., Milone A., Masi G. (2021). Could you give me the blue brick? LEGO®-based therapy as a social development program for children with autism spectrum disorder: A systematic review. Brain Sciences, 11(6), Article 702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence. (2011). Autism spectrum disorder in under 19s: Recognition, referral and diagnosis [Clinical guideline CG128]. https://www.nice.org.uk/guidance/cg128 [PubMed]
- Naveed S., Waqas A., Amray A. N., Memon R. I., Javed N., Tahir M. A., Ghozy S., Jahan N., Khan A. S., Rahman A. (2019). Implementation and effectiveness of non-specialist mediated interventions for children with autism spectrum disorder: A systematic review and meta-analysis. PLOS ONE, 14(11), Article e0224362. 10.1371/journal.pone.0224362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ochs E., Kremer-Sadlik T., Solomon O., Sirota K. G. (2001). Inclusion as social practice: Views of children with autism. Social Development, 10(3), 399–419. [Google Scholar]
- Pillay M., Alderson-Day B., Wright B., Williams C., Urwin B. (2011). Autism spectrum conditions-enhancing nurture and development (ASCEND): An evaluation of intervention support groups for parents. Clinical Child Psychology and Psychiatry, 16(1), 5–20. [DOI] [PubMed] [Google Scholar]
- Reichow B., Steiner A. M., Volkmar F. (2012). Social skills groups for people aged 6 to 21 with autism spectrum disorders (ASD). Campbell Systematic Reviews, 8(1), 1–76:. https://www.cochranelibrary.com/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowley E., Chandler S., Baird G., Simonoff E., Pickles A., Loucas T., Charman T. (2012). The experience of friendship, victimization and bullying in children with an autism spectrum disorder: Associations with child characteristics and school placement. Research In Autism Spectrum Disorders, 6(3), 1126–1134. [Google Scholar]
- Rubin E., Prizant B. M., Laurent A. C., Wetherby A. M. (2013). Social communication, emotional regulation, and transactional support (SCERTS). In Goldstein S., Naglieri J. (Eds.), Interventions for autism spectrum disorders (pp. 107–127). Springer. [Google Scholar]
- Rutter M., Bailey A., Lord C. (2003). The social communication questionnaire: Manual. Western Psychological Services. [Google Scholar]
- Sansoni J., Marosszeky N., Sansoni E., Fleming G. (2010). Effective assessment of social isolation. Centre for Health Service Development, University of Wollongong. [Google Scholar]
- Schmidt M., Werbrouck A., Verhaeghe N., Putman K., Simoens S., Annemans L. (2020). Universal mental health interventions for children and adolescents: A systematic review of health economic evaluations. Applied Health Economics and Health Policy, 18(2), 155–175. [DOI] [PubMed] [Google Scholar]
- Sekhon M., Cartwright M., Francis J. J. (2017). Acceptability of healthcare interventions: An overview of reviews and development of a theoretical framework. BMC Health Services, 17(1), Article 88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens K. (2011). Assessing the performance of a new generic measure of health-related quality of life for children and refining it for use in health state valuation. Applied Health Economics and Health Policy, 9(3), 157–169. [DOI] [PubMed] [Google Scholar]
- Sutton B. M., Webster A. A., Westerveld M. F. (2019). A systematic review of school-based interventions targeting social communication behaviors for students with autism. Autism, 23(2), 274–286. [DOI] [PubMed] [Google Scholar]
- Travis L., Sigman M., Ruskin E. (2001). Links between social understanding and social behavior in verbally able children with autism. Journal of Autism and Developmental Disorders, 31(2), 119–130. [DOI] [PubMed] [Google Scholar]
- Varley D., Wright B., Cooper C., Marshall D., Biggs K., Ali S., Chater T., Coates E., Gilbody S., de la Cuesta G. G., Kingsley E., Le Couteur A., McKelvey A., Shephard N., Teare D. (2019). Investigating SOcial Competence and Isolation in children with Autism taking part in LEGO-based therapy clubs In School Environments (I-SOCIALISE): Study protocol. British Medical Journal Open, 9, Article e030471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H.-I., Wright B., Bursnall M., Cooper C., Kingsley E., Le Couteur A., Biggs K., McKendrick K., Gomez de, la Cuesta G., Chater T., Barr A., Solaiman K., Packham A., Marshall D., Varley D., Nekooi R., Gilbody S., Parrott S. (2022. a). Cost-utility analysis of LEGO® based therapy for school children and young people with autism spectrum disorder: Results from a randomised controlled trial. British Medical Journal Open, 12, Article e056347. 10.1136/bmjopen-2021-056347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H.-I., Wright B., Tindall L., Cooper C., Biggs K., Lee E., Teare M. D., Gega L., Scott A. J., Hayward E., Solaiman K. (2022. b). Cost and effectiveness of one session treatment (OST) for children and young people with specific phobias compared to multi-session cognitive behavioural therapy (CBT): Results from a randomised controlled trial. BMC Psychiatry, 22, Article 547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong C., Odom S. L., Hume K. A., Cox A. W., Fettig A., Kucharczyk S., Brock M. E., Plavnick J. B., Fleury V. P., Schultz T. R. (2015). Evidence-based practices for children, youth, and young adults with autism spectrum disorder: A comprehensive review. Journal of Autism and Developmental Disorders, 45(7), 1951–1966. [DOI] [PubMed] [Google Scholar]
- Wright B., Kingsley E., Cooper C., Biggs K., Bursnall M., Wang H.-I., Chater T., Coates E., Teare M. D., McKendrick K., Gomez de, la Cuesta G., Barr A., Solaiman K., Packham A., Marshall D., Varley D., Nekooi R., Parrott S., Ali S., Couteur A. (in press). I-SOCIALISE: A cluster randomised controlled trial investigating the social competence and isolation of children with autism taking part in LEGO®-based therapy clubs in school environments. NIHR Public Health Research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright B., Marshall D., Adamson J., Ainsworth H., Ali S., Allgar V., Moore D. C., Cook E., Dempster P., Hackney L., McMillan D. (2016). Social Stories™ to alleviate challenging behaviour and social difficulties exhibited by children with autism spectrum disorder in mainstream schools: Design of a manualised training toolkit and feasibility study for a cluster randomised controlled trial with nested qualitative and cost-effectiveness components. Health Technology Assessment (Winchester, England), 20(6), 1–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimet G. D., Dahlem N. W., Zimet S. G., Farley G. K. (1988). The multidimensional scale of perceived social support. Journal of Personality Assessment, 52(1), 30–41. [DOI] [PubMed] [Google Scholar]