Abstract
Objective:
The main objective of this review was to map the literature on the characteristics of patient navigation programs for people with dementia, their caregivers, and members of the care team across all settings. The secondary objective was to map the literature on the barriers and facilitators for implementing and delivering such patient navigation programs.
Introduction:
People with dementia have individualized needs that change according to the stage of their condition. They often face fragmented and uncoordinated care when seeking support to address these needs. Patient navigation may be one way to help people with dementia access better care. Patient navigation is a model of care that aims to guide people through the health care system, matching their unmet needs to appropriate resources, services, and programs. Organizing the available information on this topic will present a clearer picture of how patient navigation programs work.
Inclusion criteria:
This review focused on the characteristics of patient navigation programs for people living with dementia, their caregivers, and the members of the care team. It excluded programs not explicitly focused on dementia. It included patient navigation across all settings, delivered in all formats, and administered by all types of navigators if the programs aligned with this review’s definition of patient navigation. This review excluded case management programs.
Methods:
This review was conducted in accordance with JBI methodology for scoping reviews. MEDLINE, CINAHL, APA PsycINFO, Embase, and ProQuest Nursing and Allied Health databases were searched for published full-text articles. A gray literature search was also conducted. Two independent reviewers screened articles for relevance against the inclusion criteria. The results are presented in a Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram, and the extracted data are presented narratively and in tabular format.
Results:
Thirty-nine articles describing 20 programs were included in this review. The majority of these articles were published between 2015 and 2020, and based out of the United States. The types of sources included randomized controlled trials, quasi-experimental studies, and qualitative exploratory studies, among others. All programs provided some form of referral or linkage to other services or resources. Most dementia navigation programs included an interdisciplinary team, and most programs were community-based. There was no consistent patient navigator title or standard delivery method. Commonly reported barriers to implementing and delivering these programs were navigator burnout and a lack of coordination between stakeholders. Commonly reported facilitators were collaboration, communication, and formal partnerships between key stakeholders, as well as accessible and flexible program delivery models.
Conclusions:
This review demonstrates variety and flexibility in the types of services patient navigation programs provided, as well as in the modes of service delivery and in navigator title. This information may be useful for individuals and organizations looking to implement their own programs in the future. It also provides a framework for future systematic reviews that seek to evaluate the effectiveness or efficacy of dementia navigation programs.
Keywords: caregivers, dementia, health care delivery, patient navigation, scoping review
Introduction
Dementia is an umbrella term covering a collection of syndromes characterized by chronic cognitive impairment.1 Dementia commonly results in degenerative brain function, causing memory loss, communication difficulties, and declines in reasoning or other thinking skills that interfere with daily life.1,2 The most common type of dementia is Alzheimer’s disease.2 Other types include, but are not limited to, vascular dementia, Lewy body dementia, and mixed dementia.2 According to the World Health Organization, there are 50 million people living with dementia around the world, with nearly 10 million new cases diagnosed every year.3
Dementia is a progressive condition, and people with dementia often have individualized needs that change according to the different stages of their condition.4 As a result, they often require care from multiple health and social care services and providers across diverse settings; because of this, they experience transitions in care over the duration of their illness.4–6 Unfortunately, dementia care is often characterized as fragmented, uncoordinated, and difficult to navigate.4–6 People with dementia and their caregivers report a lack of knowledge and information about dementia and available support services, as well as limited access to relevant health and social care.1,4,7 As expected, these challenges can have negative repercussions for people with dementia, contributing to poor care transitions and extended hospital stays.6 These challenges can also have a negative impact on caregivers of people with dementia, who tend to report poor mental health, high rates of burnout and social isolation, and financial strain.1,8–10
Patient navigation is one way to address the care needs of people with dementia and their caregivers. Patient navigation is a model of care designed to guide and support people through health and social care systems to help them meet their care needs. It seeks to reduce the fragmentation of programs and services, improve access to care, and integrate care across settings and sectors.11–13 This process is facilitated by patient navigators. Patient navigators perform many tasks, such as providing tailored information and advice to patients and caregivers, assisting with goal-setting and decision-making, and connecting patients to social and health care providers and relevant support groups.6,11 Navigators may have backgrounds as health care professionals, laypersons, or persons with lived experience as either patients or caregivers. However, the term “patient navigator” is not used consistently in literature or practice.14,15 These individuals may also be referred to as care coordinators, system navigators, or peer navigators, among other titles. Patient navigators often work across a range of settings, including in the community, clinics, or hospitals.14,15
Implemented by Dr. Harold Freeman in New York City in the 1990s, the first patient navigation program was designed to support patients with cancer through the emotional, physical, and financial challenges associated with diagnosis and treatment.16 Patient navigation has since been adapted to assist people with other health issues and illnesses, such as diabetes,17,18 epilepsy,19 kidney disease,20 and mental health and addiction.21 There is some research to support patient navigation as a feasible model for people with dementia and their caregivers.22 Patient navigation can benefit this population because it operates across the continuum of care, can be adapted as dementia progresses, and is efficient and scalable.23 Moreover, patient navigators can be added to existing health systems without significant changes to the system or extensive care provider training. As more people develop dementia every year, patient navigation programs are one way to help meet the resulting challenges. However, there have been limited studies or reports related to the characteristics of patient navigation programs for this population.
This scoping review mapped the literature on the characteristics of patient navigation programs—a relatively new approach to care—for people with dementia, their caregivers, and members of the care team. We chose to conduct a scoping review to organize all available information on this topic, as well as to build a picture of how patient navigation programs work. A preliminary search of the PubMed database, JBI Evidence Synthesis, and PROSPERO confirmed that there were no current or ongoing reviews on this topic. An a priori scoping review protocol was registered and published.24
The main objective of this review was to map the literature on the characteristics of patient navigation programs for people with dementia, their caregivers, and members of the care team across all settings. The secondary objective was to map the literature on the barriers and facilitators for implementing and delivering these patient navigation programs.
Review question
What are the characteristics, barriers, and facilitators of patient navigation programs that have been reported in the literature to support people with dementia, their caregivers, and/or members of the care team?
Inclusion criteria
Participants
This scoping review focused on patient navigation programs for people with dementia, their caregivers, and/or members of the care team. People with dementia were defined as people who had received a dementia diagnosis. Types of dementia included, but were not limited to, Alzheimer’s disease, vascular dementia, Lewy body dementia, traumatic brain injury, untreated HIV infection, and Wernicke-Korsakoff syndrome. Programs for people with Huntington’s disease, cognitive dysfunction, or cognitive impairment were also considered for inclusion. Caregivers were defined as people who provide unpaid care or support for individuals but who may receive a pension or government allowance to help them in this caregiving role. Caregivers may or may not live with the person they are supporting and could be a family member, friend, or neighbor. Members of the care team were defined as those who work in the health or social care systems and provide services for people with dementia and/or their caregivers. These individuals can be either professionals or non-professionals.
Concept
The main concept covered in this review was the characteristics of patient navigation programs that support people living with dementia, their caregivers, and/or members of the care team. This review defined patient navigation programs as one or more interventions or services that target people with dementia, their caregivers, and/or members of the care team with the goal of improving navigation of services and resources for this population. A navigator, whether a professional or lay navigator, provided the services.15,25,26 Patient navigator support could be educational, emotional, or logistical. It could be used to navigate services, treatments, programs, or resources. To cast a wide net across potentially relevant sources, our search strategy used different terms related to patient navigators (eg, peer navigator, nurse navigator), as well as terms synonymous with patient navigation (eg, health navigation, care coordination, system navigation). The determination of what qualified as a patient navigation program was based on information such as program description, services provided, or program goals.
This review excluded patient navigation programs that do not explicitly focus on people with dementia, their caregivers, and/or members of their care team. This review also excluded case management programs. There is overlap between case management and patient navigation,27 as both types of programs employ health care workers to provide individualized assistance to patients and caregivers.26,27 However, case managers are typically individuals with professional experience (eg, nurses, social workers), whereas patient navigators can be individuals with or without professional experience (eg, knowledgeable peers). Moreover, patient navigators provide support rather than clinical care, and work to help patients navigate existing systems and services.26 Case managers, on the other hand, can provide clinical care (eg, psychosocial treatment) when confronted with gaps in services and programs. Finally, patient navigation programs are usually more accessible to patients and caregivers than case management programs, which often involve eligibility requirements.26
The secondary concept included in this review was barriers and facilitators for the implementation and delivery of patient navigation programs for people with dementia, their caregivers, and/or the care team. We widened the definition of our secondary concept to include delivery, which is a deviation from the protocol. We did this to more fully capture the barriers and facilitators patient navigation programs encounter when providing services and to avoid limiting the data we captured to implementation. Articles did not need to mention barriers or facilitators to be included. However, it was a requirement for articles to describe the characteristics of dementia navigation programs because it was the central concept of this review.
Context
This review included patient navigation in all settings, such as clinics, hospitals, long-term care centers, and community spaces, as well as services offered in person or remotely. There were no geographic limits placed on this review. The review was limited to publications published in or after 1990, because that was the year patient navigation was conceptualized.28
Types of sources
This scoping review included peer-reviewed published papers and gray literature. The peer-reviewed literature could include any type of study design (eg, qualitative studies, quasi-experimental studies, mixed methods studies). Descriptive reports and study protocols were also considered. We excluded all reviews, such as systematic and scoping reviews; however, the reference lists of relevant reviews were hand-searched for additional articles. Gray literature, such as unpublished papers or evaluation reports, were included.
Methods
This review was conducted using the JBI methodology for scoping reviews 29 and followed an a priori protocol.24
Search strategy
The search strategy aimed to locate both published and unpublished material. A multi-step approach was implemented by a JBI-trained librarian (AG) to develop the search strategies for this review. First, an exploratory search was performed in MEDLINE (Ovid) and CINAHL (EBSCOhost) and an analysis of the text words contained in the titles, abstracts, and subject descriptors was undertaken. Second, the search terms identified in step 1 were grouped into 2 concept blocks (patient navigation and dementia), and a search strategy was drafted in MEDLINE by testing these terms to ensure the results reflected the scope of research available on the topic. At this stage, the draft search strategy was reviewed by a second librarian (RW) using the Peer Review of Electronic Search Strategies (PRESS) guidelines30 and finalized. Third, the search strategy was adapted and implemented by AG in December 2020 across the following databases: MEDLINE (Ovid), CINAHL (EBSCOhost), APA PsycINFO (EBSCOhost), Embase (Elsevier), and ProQuest Nursing and Allied Health. Databases were searched from inception to December 2020. See Appendix I for the full search strategies. The reference lists of reviews were screened for additional papers, as were the reference lists of included articles.
Language and date limits were used as screening criteria and therefore were not applied to the search strategies. Only full-text articles published in English or French were included because those are the languages spoken fluently by the 2 independent reviewers.
The process of locating sources of unpublished studies and gray literature included searching ProQuest Dissertations and Theses, Google Scholar, and the Canadian Agency for Drugs and Technologies in Health (CADTH) database, as well as targeted searching in Google and websites of known patient navigation or dementia organizations and programs (eg, Alzheimer’s Association website). We added CADTH, a specialized health care database, after the publication of the protocol to expand our gray literature search. For each search, the first 100 results per source were examined. The search took place between May and June 2021.
Source of evidence selection
Following the search, all identified records were collated and uploaded into EndNote v.X8.2 (Clarivate Analytics, PA, USA) and duplicates were removed. The results were then transferred to Covidence (Veritas Health Innovation, Melbourne, Australia), where any duplicates missed by EndNote were removed. Two independent reviewers (GA and KJK) screened the titles and abstracts against the inclusion criteria. Any disagreements about the eligibility of a paper were resolved through discussion. Next, the 2 reviewers screened the full texts of the articles against the inclusion criteria. Once again, any disagreements about the eligibility of a paper were resolved through discussion. When agreement was not reached, the reviewers consulted a third reviewer (AL or SD). The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram (Figure 1) shows the search strategy and study inclusion process. The decisions for exclusion are reported according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews checklist (PRISMA-ScR).31 Full-text studies that did not meet the inclusion criteria were excluded, and reasons for their exclusion are provided in Supplemental Digital Content 1: http://links.lww.com/SRX/A3.
Figure 1.
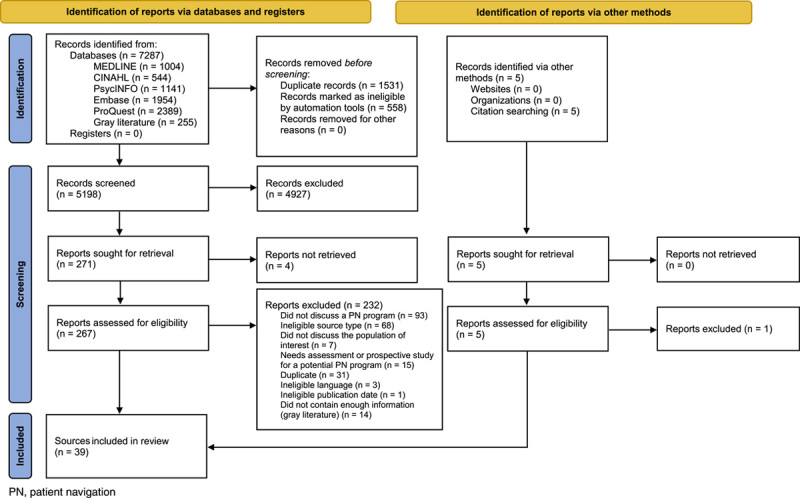
Search results and source selection and inclusion process31
Data extraction
Two independent reviewers (GA and KJK) used a data extraction tool developed for this review (see Appendix II) to extract data from papers included in the scoping review.24 The data extraction tool presented in the protocol was modified and revised during the process of data extraction. It was adapted to remove the row for program services because of the overlap with the column on program description.
Extracted data included i) author and year of publication; ii) type of source or study design (where applicable); iii) program characteristics (including geographic location, setting, delivery format, population and condition type), team composition, and navigator title; iv) barriers where applicable; and v) facilitators where applicable. The designation of what was a barrier or facilitator was based on the attributions by the authors of the included studies. The reviewers used Google Sheets to manage the extracted data. Any disagreements that arose between reviewers were resolved through discussion or with a third reviewer (AL).
Data analysis and presentation
A narrative summary describes how the results relate to the objectives of the scoping review. The full results of the search are reported in 2 tables that align with the objectives and question of this scoping review. The tables report specific details about patient navigation programs that serve people with dementia, their caregivers, and/or the care team. Appendix III includes author and year of publication; the type of source or study design; geographic location; setting; delivery format; population and condition type; team composition; and navigator title. Appendix IV contains the program description and services, barriers, and facilitators.
Results
Study inclusion
A total of 7287 records were retrieved through the search strategy (7032 from the database searches and 255 from the gray literature search). From the 7032 database records, EndNote identified and removed 1531 duplicates. A total of 5501 database sources were then uploaded to Covidence, where an additional 496 duplicates were identified and removed. When the 255 records from the gray literature search were uploaded to Covidence, 62 duplicates were removed. The reviewers thus screened a total of 5198 titles and abstracts against the inclusion criteria. Of the potentially relevant reports, we sought 271 full-text citations, but were unable to retrieve 4. We assessed 267 reports in detail against the inclusion criteria. Reasons for excluding 232 full-text papers are presented in Supplemental Digital Content 1: http://links.lww.com/SRX/A3. The majority of reports excluded at full-text screening did not describe a patient navigation program or were ineligible source types (eg, conference abstracts). Hand-searches of relevant reviews and the reference lists of included sources produced an additional 4 articles. A total of 39 sources were included in this scoping review. Figure 1 shows the search strategy and source selection and inclusion process.31
Characteristics of included sources
A majority of the sources (n=28) were published between 2015 and 2020. Notably, 7 sources were published in 2020, and 8 sources were published in 2019. These sources included randomized controlled trials (n=9), quasi-experimental studies (n=3), qualitative exploratory studies (n=8), cross-sectional research studies (n=2), editorials (n=2), descriptive studies (n=2), mixed methods studies (n=4), cost analyses (n=2), protocols (n=3), reports (n=2), a brochure (n=1), and an information sheet (n=1).
Review findings
Across the 39 articles, there were 20 different patient navigation programs. Seven articles reported on the program Maximizing Independence (MIND) at Home, based out of Maryland, United States.32–38 Seven articles reported on Care Ecosystem, a program based in California, Nevada, and Iowa in the United States.22,39–44 Six articles reported on the Partners in Dementia Care program organized by US Department of Veterans Affairs and the Alzheimer’s Association.45–50 Two reports discussed the Dementia Navigator Service in Islington, a borough in London, United Kingdom.51,52 Two articles described LIVE@Home.Path, a program based in three municipalities in Norway.53,54 The remainder of the 15 programs were the subject of a single article each.
Programs were based in the United States (n=12), the United Kingdom (n=2), Australia (n=2), Canada (n=2), Norway (n=1), and New Zealand (n=1). In the United States, programs were based in California, the District of Columbia, Florida, Iowa, Maryland, Massachusetts, Michigan, Missouri, Nebraska, Nevada, New Hampshire, New York, Ohio, Oklahoma, Rhode Island, South Carolina, and Virginia.22,32–50,55–59 Programs in the United States were either statewide initiatives22,39–50,56,58 or concentrated in specific cities, such as Miami, Cleveland, or Baltimore.32–38,55,57,59 In Canada, programs were based in the provinces of Ontario and Saskatchewan.60,61 In the United Kingdom, programs were based out of Gateshead, Halton, and the Islington borough of London.51,52,62 In Australia, one program was based in Adelaide, South Australia, while the other was in Melbourne, Victoria.63,64
Program descriptions and services
All the patient navigation programs provided some form of referral and/or linkage to other services, resources, or care. They linked clients to community resources and services according to their region and/or socioeconomic background, assisted clients on how best to use these services to meet their needs, and sometimes contacted service agencies for clients or caregivers. Resources included information on dementia, behavior management, or respite (eg, adult day programs). Most of the programs (n=12) included the provision of education for people with dementia and their caregivers, either in the form of courses or tailored educational and informational resources.32,33,37,39,40,48,53–59,64–67 Ten programs involved assessments to evaluate and respond to clients’ needs during intake.32,35,41,45,47,48,56,59–61,64,68 Four programs used protocols to assess clients and their needs.37,40,42,47,59 Two other programs included resource libraries to benefit clients.55,62
Some programs (n=7) reported providing and supporting individualized care planning.22,32,54,59,61,63,66 Care coordination and liaising with primary care was another common service (n=9).33,37,40,41,47,48,56–58,61,64,65,68 Three programs provided emotional support or coaching to clients.40,42,45,48,54,57 Four programs assisted with needs related to legal issues or providing tools or resources to navigate legal issues.22,32,56 Three programs helped clients to develop coping and communication skills,39,56,61 and another provided behavioral management skills training.32
Team composition
Among the articles that reported on team composition, most (n=13) were delivered by an interdisciplinary team, such as nurses, pharmacists, or lay navigators.22,32,33,45,49–52,55–57,61,64,66–69 Three programs were delivered exclusively by clinicians, which were made up of either a mix of clinicians (ie, nurses, physicians) or only nurses.53,62,63 There were 2 teams made up of trained, nonclinical lay workers (ie, unlicensed coordinators).59,60 Notably, even programs that did not have clinical or licensed workers as team or staff members (eg, the First Link program) provided navigational support to individuals who had been referred to them by physicians.60 As such, all programs had some involvement of care providers.
Program setting
A majority (n=19) of programs were community-based.22,32,36,38,40,42,45,48,49,51,53,54,56–68 Community settings included municipal resource centers, memory clinics, and urban academic health centers based in the community. One program did not specify where it was based.55
Mode of delivery
There was no standard or universal mode of delivery for patient navigation programs. Modes of delivery included in person, telephone-based, web-based, or a combination. The most common approach was a combination of service delivery by phone and in person (n=9).51,53,54,56,62,63,65,66,68 Two programs delivered services by telephone, email, mail, and in person.40,42,46,47 Three programs were delivered only by telephone,57,59,60 and 2 programs were delivered only in person.58,61 One program provided services in person, by telephone, and by email.33 Within each program, communication methods were not uniform to all clients, but were adapted according to client needs. For example, a care team navigator from the Care Ecosystem program initially met the family in person, but follow-up services were typically delivered by telephone, email, mail, or a combination of these.40,41
Patient navigator titles
There was no standard professional title for individuals providing patient navigation services across programs. The most commonly used title was “care coordinator,” which 4 programs used,46,47,55,57,64 while 2 programs used “care consultant”58,59 and 2 programs used “dementia navigator.”52,68 Many of the titles were variations on the term “coordinator.” These included clinic coordinator,61 First Link Coordinator,60 memory care coordinator,36 support coordinator,66 Project Learn MORE coordinator,56 dementia care coordinator,67 service coordinator,65 or simply coordinator.53 Other titles incorporated the term “navigator,” such as care team navigator,22 Alzheimer’s patient navigator,69 and primary care navigator.62 One program was operated by specialist dementia nurses.63 There was no apparent relationship between the title of the navigators and the settings; coordinator and navigator titles were both used in community and clinical settings.
Target population
Most programs (n=16) served only people with dementia,40,42,45,50,52,57–59,64–67,69 whereas 4 programs served patients with dementia and people with cognitive impairment or a cognitive disorder.33,37,61,63,68 Five programs had age requirements, which varied from program to program.22,36,45,57,59 Age requirements included 45 years and older,39 50 years and older,45 60 years and older,57 and 70 years and older.34 Five programs required that clients be living at home and in the community to be eligible to receive services, because the goal of those programs was to help people to stay in the community longer.34,53,57,59,64 Seven programs required a diagnosis of dementia to be eligible for the program.37,42,45,53,54,56,57,60,66 Six programs required that clients, in this case people with dementia and their caregivers, be served together as dyads.34,42,47,48,53,57,64 One program was only for caregivers.67 The Partners in Dementia Care, Telephone-Linked Care, and Veterans Affairs Dementia Care Coordinator programs had the additional requirement that people with dementia also be veterans.46,57,67 No programs reported targeting the care team.
Barriers
Two articles that described the same program listed burnout and stress among patient navigators as barriers.22,41 Four articles describing 4 programs reported initial and ongoing difficulties coordinating with primary care providers or with key partners and partnering organizations, showing a lack of coordination across team members or stakeholders.32,48,56,61 Two articles describing 2 programs reported difficulty using referrals to recruit clients.56,60 This represented a barrier because it demonstrated the referring physicians’ lack of understanding of the program’s services. Organizations that operated exclusively or mainly through referrals to the program (First Link and MIND at Home) faced difficulties with recruitment.34,60 One of these programs also required a diagnosis,60 which can act as a barrier because dementia is often underdiagnosed.70,71 One article described identifying resources for people who are on a low income, do not speak English, or live in rural areas as barriers.39 Initial barriers to implementation included an absence of clear communication between all team members,61 and coordination between primary care providers and other team members.32,39
Facilitators
Twelve articles describing 7 programs listed collaboration and communication between key stakeholders, as well as formal partnerships between health care and community organizations, as facilitators for the development and implementation of patient navigation programs.22,32,34,38,45–48,57,59–61 These facilitators included linkages between organizations and key players,47,48,61 such as embedding representatives of the local Alzheimer Society chapters into memory clinics.61 It is also beneficial if program organizers, caregivers, and program site partners demonstrate an equal willingness to actively support and participate in the programs.48
Another commonly reported facilitator was a flexible and adaptable delivery model, which encouraged frequent and flexible communication with clients. Ten articles describing 7 programs listed this facilitator.32,39,40,42,44,45,48,56,60,68 Four articles describing 2 programs identified working closely with caregivers and coaching caregivers as facilitators for implementing program activities.22,39,47,48 Four sources describing 3 programs identified navigators’ listening skills and ability to form positive relationships with clients as facilitators.22,44,51,63
Several articles discussed logistical and administrative tools that facilitated program implementation. For example, 4 articles describing 3 programs reported a shared computer system or a specialized database for providing coordination, access to information, and information-sharing between key players. These key players included the navigator and members of the care team, sometimes across multiple organizations such as the Alzheimer’s Association chapters and Veterans Affairs.47,48,56,57 Six articles describing 4 programs reported tools and protocols for security of data and personal information, as well as program implementation (eg, implementation handbook, needs assessment).36,37,48,56,63,64 One article discussed the need for adequate space and necessary administrative support for documentation and records systems.61
An additional facilitator of program implementation that was identified in multiple articles was funding and the affordability of navigation programs. For example, 5 articles describing 3 programs listed affordability of programs and cost-effectiveness as facilitators.37,38,41,45,48 One article reported cost to be an initial barrier to implementation, although the patient navigation program may save money in the long term.33 For one program, a factor that helped ensure the program’s affordability was the employment of lay navigators. Opting not to employ specialized health professionals ensured these programs were more affordable.41 One article reported that costs decreased substantially during the implementation period and depended on caseload.43
Discussion
The results of this review provide considerable insight into the characteristics, barriers, and facilitators of patient navigation programs for people with dementia and their caregivers. Although characteristics varied across the 20 programs, most programs were located in the community, had interdisciplinary care teams, and delivered a variety of services, mainly through a combination of telephone and in-person mechanisms. Barriers and facilitators also varied across programs. The most reported barriers were navigator burnout and stress, as well as a lack of coordination between internal and external stakeholders. Conversely, the most reported facilitator was coordination between internal and external stakeholders.
Some of the defining characteristics of patient navigation are the combination of care coordination interventions, such as facilitating access to services and resources, and building and developing a relationship between the navigator and client.72,73 In line with this understanding of patient navigation, all of the programs included in this review connected people with dementia and their caregivers to appropriate services and resources within the health care system and/or the community. While the specific services and supports provided by patient navigation programs varied, these programs all focused on improving the coordination of care and access to services across providers and settings. More specifically, programs offered logistical and care coordination support, such as providing individualized care planning, needs assessments, educational training or resources, and referrals and/or linkages to other services, resources, or care. This range of services across programs demonstrates a more general trend of how patient navigation programs can adapt based on context and client needs, which is often cited as an advantage of patient navigation programs.74,75 This flexibility in the provision of services benefits both the clients, who have specific and individualized needs, as well as the institutions and organizations that administer the programs, which can tailor the program to their own needs and goals as well.74
Although there is flexibility in where patient navigators can be based, a majority of the patient navigation programs in this review were based in the community. These programs were accessed via clinics, referrals from primary care providers, referrals from service organizations with staff trained in dementia case-finding, letters from service providers to their clients, and general community outreach. Community-based programs can benefit people with dementia by filling social needs, as well as by reducing stigma associated with dementia.76 For people with mild or moderate dementia, these community-based programs can have positive effects on cognitive functioning and improve communication and quality of life.77,78 Moreover, community-based programs can also decrease depression, stress, social isolation, and burden among caregivers,79–81 while increasing their quality of life.79,82 Community-based programs can also help support aging in place, a common desire among older persons.83 This review showed that there is an absence of patient navigation programs for people with dementia in hospital settings in the literature. Because people with dementia often have other comorbidities and difficulties with their health, hospital-based programs can still be beneficial.84,85
While eligibility requirements varied, most programs targeted people with dementia and their caregivers, but none targeted the care team. Many programs had broad eligibility requirements, whereas others had requirements around age, diagnosis, living in the community, and enrolling with a caregiver. Considering that patient navigation started as a way to facilitate care for people who face significant barriers related to factors such as poverty, broad eligibility requirements are in line with the principles of patient navigation. Programs with specific requirements, such as a diagnosis of dementia, can be challenging to access, because it can be difficult to get a timely appointment with a doctor to receive a dementia diagnosis or to obtain a diagnosis once the initial contact with a doctor is made.86–89 This is one of the reasons why dementia is often underdiagnosed.90
There are also cases of people with dementia (or their caregivers) mistaking symptoms for normal aging or experiencing stigma, which may also delay their attempts to seek support.91,92 Furthermore, there are inequalities to receiving a dementia diagnosis, and many groups face significant delays, particularly in immigrant communities (eg, African, Asian, and Anglo-European Americans; British South-Asian communities).93 Therefore, populations that face increased barriers can benefit from patient navigation programs with broad eligibility criteria. In our review, the programs with the most requirements (eg, age requirements, inclusion of caregivers as dyads, diagnosis requirements) were funded as research studies and thus had stricter inclusion criteria.32,40 Similarly, the programs requiring clients to be veterans were organized by the US Department of Veterans Affairs.42,57
For patient navigation programs in general, regardless of conditions and populations, navigators can work independently or within a team.14 This scoping review found that the majority of teams were interdisciplinary and included clinical and nonclinical staff. According to the core principles of patient navigation, the integration of navigators into health care teams optimizes patient care.12 Indeed, the programs captured by this review were all connected to care providers, either as team members or through program referrals from care providers. Generally speaking, patient navigation programs administered by health care professionals or interdisciplinary teams tend to focus on patient populations with complex health and social care needs.14,94 Programs that are integrated into the health care system may be most appropriate for people with dementia, as they often present with complex care needs and comorbidities.95,96 Notably, not everyone has access to care providers or an interdisciplinary care team. Patient navigators could help people with dementia gain access to a care team so that they can receive a diagnosis and postdiagnostic supports. Moreover, patient navigation programs can help patients and caregivers better understand the diagnostic process. Research has shown that interdisciplinary care teams can benefit older patients with complex care needs because they provide specialized knowledge and expertise from multiple disciplines.97 Interdisciplinary care can benefit people with dementia specifically by improving care and well-being, improving care outcomes, and decreasing the risk of hospital readmission.98,99
Not surprisingly, there was a lack of consistency in the professional titles of individuals implementing patient navigator programs. However, most programs used variations of the terms “coordinator” and “navigator.” This variation in titles is consistent with findings from other studies and reviews that have examined patient navigation programs.14,26,100 Despite the inconsistent terminology, the recurrence of “navigator” and “coordinator” represents the main purposes of patient navigators; that is, the assistance with coordination and navigation of available care, services, and resources. These professional titles also demonstrate one of patient navigation’s core functions: eliminating barriers to ensure that patients receive timely care.12 Our review found that the services provided across all position titles overlapped. Coordinators and navigators alike provided referrals and linkages, education, emotional support, and care coordination.22,46,55,57,69
This review found no standard mode of delivery for patient navigation programs presented in the literature. Patient navigation programs were delivered in person, using telephone-based or web-based communication, or some combination. The range of contact methods for patient navigation programs for people with dementia and their caregivers is consistent with patient navigation programs for other populations and other conditions, such as cancer and diabetes. For example, clients with other conditions contact patient navigators by telephone,11,18,26,27,101 by email,26 in person,26,101 or a combination.102 The lack of standard mode of delivery across programs and, in some cases, even within programs, suggests that communication is personalized according to client needs. This flexibility in communication for people with dementia reflects another strength of patient navigation: flexibility based on the context of the program and client needs.74,75 Indeed, a successful relationship between a client and a patient navigator requires flexibility on the part of the navigator.72 This flexibility also ensures that patient navigation remains a patient-centric approach, which is central to this model of care.12
Barriers to developing patient navigation programs for people with dementia are consistent with the difficulties encountered during the development of other types of patient navigation programs. For example, programs in the current review noted difficulty locating resources for individuals who were low-income, did not speak English, or lived in rural areas, which fits with previous studies in other areas.21,103,104 This finding also reflects dementia care more generally, as there are limited dementia-related support and education services in rural communities.105,106 Our review found that burnout was the primary barrier associated with the delivery of patient navigation programs for people with dementia. Navigator burnout is a commonly cited barrier to patient navigation programs serving other populations as well.107,108 Due to the frequently adaptable nature of patient navigation, navigators may not have clearly defined roles and tasks. As such, in responding to client needs, they often take on tasks beyond their role.107,109 According to research in other areas, setting boundaries and fostering social support by creating support networks with other patient navigators, either within the organization or across multiple organizations, can be one solution to burnout.107,109 Support from supervisors or managers can also be useful for establishing boundaries.107 Standardized training and skill development is another way to help navigators set boundaries in their professional lives and build resilience to avoid burnout.109
The most common facilitators for the development and implementation of patient navigation programs for people with dementia were collaboration and communication between key stakeholders. This included formal partnerships between health care and community organizations. This finding is consistent with patient navigation programs for other populations and conditions, such as mental health and vulnerable populations.21,75,110–112 It is also consistent with literature showing that collaboration facilitates the successful integration of dementia care more generally.6
The availability of specialized computer systems was another common facilitator for patient navigation programs identified in this review. This is also a facilitator for programs serving other populations.75,110,113–115 Although we found that cost was presented as a facilitator, this was not always reflected in the literature. This review, as well as research on patient navigation in general, found that it mainly depended on the availability of funding for the patient navigation program. Programs serving other populations have listed “maintaining funding for navigators” as a challenge.21,75,116 Notably, many of the programs included in this scoping review secured funding through a research grant, through the Department of Veterans Affairs, or through a community partnership, such as with the local or provincial Alzheimer Society chapter. A recommendation repeated across articles on navigation programs for other conditions was partnering with agencies or community partners.21,75,110 Community-based programs can also reduce costs because they can help people live at home longer, which costs less than long-term care in either a nursing home or a hospital. Community-based programs can also support caregivers by precluding their need to retire early or change working hours.79,117 This fits with one of the primary principles of patient navigation; namely, that it should be cost-effective.12
Strengths and limitations
This scoping review provides important knowledge on the characteristics, the barriers, and facilitators of patient navigation programs for people with dementia and their caregivers. The strengths of this scoping review include the comprehensiveness of the search strategy and the strict inclusion criteria that allowed the selection of sources. Notably, this scoping review did not locate any programs from South America, Asia, or Africa. The evidence related to those countries and continents may have been missed due to the language limits of the reviewers, who only spoke English and French. It is also possible that patient navigation programs may be less common in these regions. Furthermore, the literature search was limited to 1990 and beyond, 5 databases, and a gray literature search. It is possible that the search strategies may not have identified some relevant publications. Finally, this review did not report on outcomes of patient navigation programs. Although reporting on outcomes was not our purpose, it would have provided insight into the effectiveness of the patient navigation programs.
Conclusions
In recent years, rates of dementia around the world have increased, resulting in a greater need for dementia care. People with dementia and their caregivers continue to face many barriers to care. Initiatives such as patient navigation programs, which provide individualized and flexible support to people with dementia, their caregivers, and members of the care team, are one way to overcome barriers to care within health and social care systems. The purpose of this scoping review was to learn about the patient navigation programs and map the literature on their characteristics, barriers, and facilitators. Results showed that most programs are intended for people with dementia and their caregivers rather than care team members, are based in the community, involve interdisciplinary teams, and have variety and flexibility in terms of their characteristics. This was reflected in the range of services the programs provided, the modes of service delivery, navigator titles, and eligibility requirements. Barriers and facilitators for program development and implementation also varied. Program barriers included navigator burnout and locating resources to address specific needs. Common facilitators were collaboration between health care and community organizations, flexible delivery models, program affordability, and logistical and administrative tools.
Implications for research
This information may be useful for individuals and organizations looking to implement their own dementia navigation programs. It will also provide a framework for future systematic reviews that seek to evaluate the effectiveness of dementia navigation programs.
Supplementary Material
Acknowledgments
Richelle Witherspoon reviewed the search strategy. Katherine J. Kelly contributed to data collection by acting as an independent reviewer for the search of published materials. Hannah Trites and Matt Douglas contributed to data collection by acting as an independent reviewer for the gray literature review.
Funding
This project is supported by Healthcare Excellence Canada (formerly the Canadian Foundation for Healthcare Improvement) and the New Brunswick Innovation Foundation. Neither funder had any input into this review.
Author Contributions
All authors contributed to designing the methodology for this review and approved the final manuscript. GA wrote and edited the manuscript. AL, ALM, LM, and SD contributed to the writing and editing. AG created the search strategy, co-wrote and edited a section of this review, and edited the appendices. SD and AL are also co-leading the larger research study.
Appendix I: Search strategy
| Ovid MEDLINE(R) and Epub Ahead of Print, in Process & Other Non-Indexed Citations, Daily and Versions(R) 1946 to December 15, 2020 – Searched December 17, 2020 | ||
|---|---|---|
| # | Search string | Records retrieved |
| 1 | exp Patient Navigation/ | 790 |
| 2 | "Navigat*".ab,ti,kf,kw. | 42,982 |
| 3 | (coordinat* adj2 care).ab,kf,kw,ti. | 9594 |
| 4 | 1 OR 2 OR 3 | 52,361 |
| 5 | exp Dementia/ | 169,851 |
| 6 | exp Cognitive Dysfunction/ | 19,764 |
| 7 | "Dement*".ab,ti,kf,kw. | 120,702 |
| 8 | "Alzheimer*".ab,ti,kf,kw. | 154,083 |
| 9 | cognitive impairment.ab,kf,kw,ti. | 61,781 |
| 10 | Cognitive dysfunction.ab,kf,kw,ti. | 14,842 |
| 11 | "Huntington*".ab,kf,kw,ti. | 18,414 |
| 12 | "cognitive decline".ab,kf,kw,ti. | 23,756 |
| 13 | 5 or 6 or 7 or 8 or 9 or 10 or 11 OR 12 | 322,350 |
| 14 | 4 and 13 | 1004 |
| CINAHL Full-Text (EBSCOhost) – Searched December 17, 2020 | ||
|---|---|---|
| # | Search string | Records retrieved |
| 1 | (MH "Patient Navigation") | 1419 |
| 2 | Navigat* | 16,723 |
| 3 | coordinat* N2 care | 8400 |
| 4 | S1 OR S2 OR S3 | 24,738 |
| 5 | (MH "Dementia+") | 74,546 |
| 6 | Dement* | 66,578 |
| 7 | Alzheimer* | 43,816 |
| 8 | cognitive impairment | 43,533 |
| 9 | Cognitive dysfunction | 26,303 |
| 10 | cognitive decline | 12,746 |
| 11 | Huntington* | 2511 |
| 12 | S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 | 132,997 |
| 13 | S4 AND S12 | 544 |
| APA PsycINFO (EBSCOhost) – Searched December 17, 2020 | ||
|---|---|---|
| # | Search string | Records retrieved |
| 1 | Navigat* | 23,672 |
| 2 | coordinat* N2 care | 3292 |
| 3 | S1 OR S2 | 26,832 |
| 4 | DE "Dementia" OR DE "AIDS Dementia Complex" OR DE "Dementia with Lewy Bodies" OR DE "Presenile Dementia" OR DE "Pseudodementia" OR DE "Semantic Dementia" OR DE "Senile Dementia" OR DE "Vascular Dementia" | 46,821 |
| 5 | DE "Alzheimer's Disease" | 47,661 |
| 6 | DE "Cognitive Impairment" | 37,902 |
| 7 | DE "Huntingtons Disease" | 3273 |
| 8 | DE "Presenile Dementia" OR DE "Alzheimer's Disease" OR DE "Creutzfeldt Jakob Syndrome" OR DE "Picks Disease" | 48,711 |
| 9 | DE "Memory Disorders" | 13,602 |
| 10 | dement* | 81,645 |
| 11 | alzheimer* | 70,975 |
| 12 | cognitive impairment | 83,458 |
| 13 | Cognitive dysfunction | 49,360 |
| 14 | cognitive decline | 24,402 |
| 15 | Huntington* | 6079 |
| 16 | S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 | 199,248 |
| 17 | S3 OR S16 | 1141 |
| Embase – Searched December 17, 2020 | ||
|---|---|---|
| # | Search string | Records retrieved |
| 1 | 'patient navigator'/exp | 15 |
| 2 | 'patient navigator program'/exp | 11 |
| 3 | 'care coordinator'/exp | 274 |
| 4 | 'care coordination'/exp | 53 |
| 5 | navigat*:ti,ab,kw | 57,100 |
| 6 | (coordinat* NEAR/2 care):ti,ab,kw | 14,172 |
| 7 | #1 OR #2 OR #3 OR #4 OR #5 OR #6 | 70,636 |
| 8 | 'dementia'/exp | 372,932 |
| 9 | 'cognitive defect'/de | 173,185 |
| 10 | dement*:ti,ab,kw | 177,834 |
| 11 | alzheimer*:ti,ab,kw | 214,737 |
| 12 | 'cognitive impairment':ti,ab,kw | 97,617 |
| 14 | 'cognitive decline':ti,ab,kw | 37,140 |
| 15 | 'cognitive dysfunction':ti,ab,kw | 22,488 |
| 16 | huntington*:ti,ab,kw | 25,183 |
| 17 | #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 | 580,809 |
| 18 | #7 AND #17 | 1954 |
| ProQuest Nursing & Allied Health – Searched December 18, 2020 | ||
|---|---|---|
| # | Search string | Records retrieved |
| 1 | MESH.EXACT.EXPLODE("Patient Navigation") | 34 |
| 2 | navigat* | 92,030 |
| 3 | coordinat* NEAR/2 care | 42,338 |
| 4 | 1 OR 2 OR 3 | 128,739 |
| 5 | MESH.EXACT.EXPLODE("Dementia”) | 9314 |
| 6 | ((ab(dementia) OR ti(dementia)) | 32,807 |
| 7 | ((ab(Alzheimer*) OR ti(Alzheimer*)) | 27,572 |
| 8 | ((ab(cognitive NEAR/1 (impairment OR dysfunction OR decline)) OR ti(cognitive NEAR/1 (impairment OR dysfunction OR decline))) | 21,164 |
| 9 | ((ab(Huntington*) OR ti(Huntington*)) | 3197 |
| 10 | 5 OR 6 OR 7 OR 8 OR 9 | 66,767 |
| 11 | 4 AND 10 | 2389 |
Gray literature search
We searched keywords based on those found in our database search strategies. The searches were iterative, which is typical for gray literature searching. We limited the searches to the English language. For each search, we examined the first 100 results per source (some searches had fewer than 100 results). The gray literature review was conducted between May and June 2021.
https://www.google.com/ terms searched
Navigation Programs Dementia
Dementia Navigator
Patient Navigation Dementia
Patient Coordinator Dementia
Cognitive Dysfunction Patient Navigation
Cognitive Impairment Patient Navigation
Dementia Navigation
Dementia Coordination
Alzheimer’s Patient Navigation
Alzheimer’s Patient Coordination
Dementia Care Coordinator Programs
Dementia UK
Patient Navigators UK
Dementia Australia
Health Navigator Australia
Dementia Navigators Australia
Dementia Navigators United States
Dementia Europe
Dementia Navigators Europe
Dementia Navigators Africa
https://scholar.google.com/ terms searched
Navigation Programs Dementia
Dementia Navigator
Patient Navigation Dementia
Patient Coordinator Dementia
Cognitive Dysfunction Patient Navigation
Cognitive Impairment Patient Navigation
Dementia Navigation
Dementia Coordination
Alzheimer’s Patient Navigation
Alzheimer’s Patient Coordination
Dementia Care Coordinator Programs
ProQuest Dissertations and Theses terms searched
Navigation Programs Dementia
Dementia Navigator
Patient Navigation Dementia
Patient Coordinator Dementia
Cognitive Dysfunction Patient Navigation
Cognitive Impairment Patient Navigation
Dementia Navigation
Dementia Coordination
Alzheimer’s Patient Navigation
Alzheimer’s Patient Coordination
Dementia Care Coordinator Programs
https://www.cadth.ca/ terms searched
Navigation Programs Dementia
Dementia Navigator
Patient Navigation Dementia
Patient Coordinator Dementia
Cognitive Dysfunction Patient Navigation
Cognitive Impairment Patient Navigation
Dementia Navigation
Dementia Coordination
Alzheimer’s Patient Navigation
Alzheimer’s Patient Coordination
Dementia Care Coordinator Programs
For dementia-specific organizations, we hand-searched websites using key terms. We examined the first 100 results per site (some searches had fewer than 100 results). These terms were: Navigation Programs, Dementia Navigator, Patient Navigation, Patient Coordinator Dementia, Cognitive Dysfunction Patient Navigation, Cognitive Impairment Patient Navigation, Dementia Navigation, Dementia Coordination, Alzheimer’s Patient Navigation, Alzheimer’s Patient Coordination, Dementia Care Coordinator Programs.
We searched the following organization websites:
Dementia UK: https://www.dementiauk.org/
Dementia Australia: https://www.dementia.org.au/
Alzheimer Society of Canada: https://alzheimer.ca/en
Alzheimer’s Association (United States): https://www.alz.org/
Appendix II: Data extraction instrument
| Author/year | |||
|---|---|---|---|
| Type of source/study design where applicable | |||
| Geographic location | |||
| Setting | |||
| Delivery format | |||
| Population/condition type | |||
| Team composition | |||
| Navigator title | |||
| Program description and services | |||
| Program barriers (where applicable) | |||
| Program facilitators (where applicable) |
Appendix III: Characteristics of included studies
| Author, year | Title | Type of source/study design (where applicable) | Geographic location | Setting | Delivery format | Population/condition | Team composition | Navigator title |
|---|---|---|---|---|---|---|---|---|
| Amjad et al.,32 2018 | Health services utilization in older adults with dementia receiving care coordination: the MIND at Home trial | Randomized controlled trial | Baltimore, Maryland, US | Home and community | Phone and in person | 70 years and older, English-speaking, community residing in northwest Baltimore (28 postal codes), with a reliable study partner (ie, dyad); met Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) criteria for dementia or cognitive disorder not otherwise specified, and had one or more unmet care needs on the Johns Hopkins Dementia Care Needs Assessment | Interdisciplinary team of nonclinical memory care coordinators linked to a registered nurse and a geriatric psychiatrist | Care coordinator |
| Bass et al.,59 2003 | The Cleveland Alzheimer’s managed care demonstration: outcomes after 12 months of implementation | Randomized controlled trial | Cleveland, Ohio, US | Home and community | Phone | People with memory problems and people with dementia (pre-diagnosis); 55 years and older; living in the community | Lay team of care consultants and trained volunteers | Care consultant |
| Bass et al.,45 2013 | Caregiver outcomes of Partners in Dementia Care: effect of a care coordination program for veterans with dementia and their family members and friends | Quasi-experimental study (participants were not randomized to intervention or control) | US (Boston, Massachusetts; Providence, Rhode Island; Houston, Texas; Oklahoma City, Oklahoma; and Beaumont, Texas) | Home and community (based out of a Veterans Affairs center) | Phone, email, and mail | Veterans with dementia (aged 50 years and older) and their caregivers | Interdisciplinary team of care coordinators from Veterans Affairs and Alzheimer’s Association | Care coordinator |
| Bass et al.,46 2014 | A controlled trial of Partners in Dementia Care: veteran outcomes after six and twelve months | Randomized controlled trial | 5 regions in the US | Home and community (based out of a Veterans Affairs center) | Phone, email, mail, and in person | Veterans with dementia and their caregivers | Interdisciplinary team of care coordinators from Veterans Affairs and Alzheimer’s Association with administrative support | Care coordinator |
| Bass et al.,47 2015 | Impact of the care coordination program “Partners in Dementia Care” on veterans’ hospital admissions and emergency department visits | Randomized controlled trial | US (Boston, Massachusetts; Providence, Rhode Island; Houston, Texas; Oklahoma City, Oklahoma; and Beaumont, Texas) | Home and community | Phone, email, and mail | Veterans with dementia and their caregivers | Interdisciplinary team of care coordinators from Veterans Affairs and Alzheimer’s Association | Care coordinator |
| Bernstein et al.,22 2019 | The role of care navigators working with people with dementia and their caregivers | Qualitative exploratory study | California, Nebraska, and Iowa, US | Home and community | Phone and web-based | Dyads made up of people with dementia and their caregivers; with a diagnosis, speaking English, Spanish, or Cantonese | Interdisciplinary team of care team navigators, advanced practice clinical nurse, a social worker, and a pharmacist | Care team navigator |
| Bernstein et al.,39 2020 | Using care navigation to address caregiver burden in dementia: a qualitative case study analysis | Qualitative exploratory study | California and Nebraska, US | Home and community (based out of urban academic health centers) | Phone and web-based | Dyads made up of people with dementia and their caregivers; with a diagnosis, speaking English, Spanish, or Cantonese | Interdisciplinary team of care team navigators, advanced practice clinical nurse, a social worker, and a pharmacist | Care team navigator |
| Chen et al.,55 2020 | Effect of care coordination on patients with Alzheimer disease and their caregivers | Quasi-experimental study | Greenville, South Carolina, US | N/A | N/A | People with dementia and their caregivers | Interdisciplinary team included care coordinator and licensed social worker | Care coordinator |
| Dang et al.,57 2008 | Care coordination assisted by technology for multiethnic caregivers of persons with dementia: a pilot clinical demonstration project on caregiver burden and depression | Qualitative study | Miami, Florida, US | Home and community | Phone | Home-dwelling veterans over the age of 60 years, with a diagnosis of dementia or related disorders; caregivers were required to live with the veteran | Interdisciplinary team of nurse care coordinator and a support person, who also communicated with the care recipients’ providers | Care coordinator |
| Dementia Waikato,66 2017 | Dementia navigator service | Brochure | Waikato, New Zealand | Home and community | Phone and in person | People with dementia and caregivers, residing in the Waikato District Health Board area, dementia diagnosis required, must be eligible for public health services | Interdisciplinary team of registered nurses, occupational therapists, social workers, and dementia navigator | Support coordinator |
| Department of Veterans Affairs,67 2020 | Rural Interdisciplinary Team Training (RITT) dementia care coordinator program | Information sheet | US | Home and community | Phone and email | Caregivers of veterans with dementia | Interdisciplinary team of licensed clinical social workers and volunteers | Dementia care coordinator |
| Fæø et al.,53 2020 | The compound role of a coordinator for home-dwelling persons with dementia and their informal caregivers: qualitative study | Qualitative study | Norway | Home and community | Phone and in person | Dyads made up of people with dementia and their care partners, who lived at home | Clinical team of 2 specialist nurses acting as coordinators | Coordinator |
| Fortinsky et al.,65 2002 | Helping family caregivers by linking primary care physicians with community-based dementia care services: the Alzheimer’s Service Coordination Program | Mixed methods | Cleveland, Ohio, US | Home and community | Phone and in person | People with dementia and their caregivers | N/A | Service coordinator |
| Galik and Stefanacci,69 2019 | Improving care for patients with dementia: what to do before, during, and after a transition | Editorial | US | Home and community | N/A | People with dementia and their caregivers | Interdisciplinary team | Alzheimer’s patient navigation |
| Galvin et al.,56 2014 | Public–private partnerships improve health outcomes in individuals with early-stage Alzheimer’s disease | Cross-sectional, non-randomized research study | Missouri, US | Home and community | Phone and in person | People with dementia and their caregivers, diagnosis required | Interdisciplinary team of New York University researchers, the Missouri Department of Health and Senior Services, Area Agencies on Aging, and local Alzheimer’s Association Chapters | Project Learn MORE (Missouri Outreach and Referral Expanded) coordinator |
| Goeman et al.,63 2016 | Development of a model of dementia support and pathway for culturally and linguistically diverse communities using co-creation and participatory action research | Qualitative study using a co-creation and participatory action research approach | Australia | Home and community | Phone and in person | Culturally and linguistically diverse community members with cognitive impairment living in the community and their family or caregiver | Clinical team of nurses | Specialist dementia nurse |
| Husebo et al.,54 2020 | LIVE@Home.Path—innovating the clinical pathway for home-dwelling people with dementia and their caregivers: study protocol for a mixed methods, stepped-wedge, randomized controlled trial | Study protocol | 3 municipalities in Norway | Home and community | Phone and in person | Dyads made up of people with dementia and their care partners, who lived at home | Clinical team of 2 specialist nurses, acting as coordinators | Coordinator |
| Joels and van Pol,51 2014 | How to manage follow-up patients: Dementia Navigators | Report/presentation slides | Islington borough of London, UK | Home and community | Phone and in person | People with dementia and their informal caregivers | Interdisciplinary team of a full-time team leader with clinical and managerial responsibilities and 3 dementia navigators | Dementia navigator |
| Judge et al.,48 2011 | Partners in Dementia Care: a care coordination intervention for individuals with dementia and their family caregivers | Qualitative descriptive analysis | Huston, Texas and Boston, Massachusetts, US | Home and community | Phone | Veterans with dementia and their primary caregivers | Interdisciplinary team included the VA Dementia Care Coordinator who worked in the Veterans Affairs, and the Alzheimer’s Association Care Consultant who worked in the Alzheimer’s Association chapter | Care coordinator |
| Lee et al.,61 2014 | Integrating community services into primary care: improving the quality of dementia care | Qualitative exploratory study | Ontario, Canada | Community (based out of primary care clinic) | In person | People with mild cognitive impairment or dementia and their caregivers | Interdisciplinary team included a physician, nurse practitioner, registered nurse, social worker, occupational therapist, and pharmacist | Clinic coordinator |
| Liu et al.,68 2019 | Patient and caregiver outcomes and experiences with team-based memory care: a mixed methods study | Mixed methods | Southeastern US | Community (based out of memory clinic) | Phone and in person | People with dementia and other memory issues and their caregivers | Interdisciplinary team made up of a geriatric physician, nurse, nurse practitioner, and social worker who functioned as the dementia navigator | Dementia navigator |
| McAiney et al.,60 2012 | ‘Throwing a lifeline’: the role of First Link™ in enhancing support for individuals with dementia and their caregivers | Mixed methods | Ontario and Saskatchewan, Canada | Home and community | Phone | People with dementia and their caregiver | Lay team made up of First Link Coordinator who worked with Alzheimer Society and the family | First Link coordinator |
| Merrilees et al.,40 2020 | The Care Ecosystem: promoting self-efficacy among dementia family caregivers | Qualitative exploratory study | California, Nebraska, and Iowa, US | Home and community | Phone, email, mail, and in person | Dyads made up of people with dementia and caregivers | Interdisciplinary team made up of care team navigators, advanced practice nurse, social worker, and pharmacist | Care team navigator |
| Morgan et al.,49 2015 | A break-even analysis for dementia care collaboration: Partners in Dementia Care | Cost analysis | US | Home and community | Phone and email | Veterans with dementia and their caregivers | Interdisciplinary team made up of Veterans Health Administration Coordinator and Alzheimer’s Association coordinator | Alzheimer’s Association care coordinator |
| Morgan et al.,50 2019 | Does care consultation affect use of VHA versus non-VHA care? | Cross-sectional research study | 5 regions in the US | Home and community | Phone | Veterans with dementia and their primary caregivers | Interdisciplinary team made up of half-time Veterans Health Administration dementia care coordinator and a half-time Alzheimer’s Association care consultant | Alzheimer’s Association care coordinator |
| Possin et al.,41 2017 | Development of an adaptive, personalized, and scalable dementia care program: early findings from the Care Ecosystem | Pragmatic randomized controlled trial | US | Home and community | Phone, email, and in person | People diagnosed with dementia of any type by any medical provider; 45 years and older; Medicare- or Medicaid-enrolled or pending; residing in California, Nebraska, or Iowa; a caregiver who may or may not reside with the patient; and fluency in English, Spanish, or Cantonese | Interdisciplinary team made up of care team navigators, dementia specialist nurse, social worker, and pharmacist | Care team navigator |
| Possin et al.,42 2019 | Effect of collaborative dementia care via telephone and internet on quality of life, caregiver well-being, and health care use: the Care Ecosystem randomized clinical trial | Randomized controlled trial | California, Nebraska, and Iowa, US | Home and community (based out of urban academic health centers) | Phone, email, and mail | Dyads made up of people with dementia and their caregiver; diagnosis required; speaking either English, Spanish, or Cantonese, residing in Iowa, California, or Nebraska | Interdisciplinary team consisting of a care team navigator, advanced practice nurse, social worker, and pharmacist | Care team navigators |
| Rosa et al.,43 2019 | Variations in costs of a collaborative care model for dementia | Cost analysis | California, Nebraska, and Iowa, US | Home and community (based out of urban academic health centers) | Phone, email, and in person | Dyads of persons with dementia and their caregiver; diagnosis required; speaking either English, Spanish, or Cantonese, residing in Iowa, California, or Nebraska | Interdisciplinary team consisting of a care team navigator, advanced practice clinical nurse, social worker, and pharmacist | Care team navigators |
| Samus et al.,33 2014 | A multidimensional home-based care coordination intervention for elders with memory disorders: the Maximizing Independence at Home (MIND) pilot randomized trial | Randomized controlled trial | Baltimore, Maryland, US | Home and community | Phone, email, and in person | People with cognitive disorder, 70 years and older, English-speaking, living in the community, had a reliable study partner (dyad) | Interdisciplinary team made up of community workers (coordinators), registered nurse, and geriatric psychiatrist | Memory care coordinator |
| Samus et al.,34 2015 | A multipronged, adaptive approach for the recruitment of diverse community-residing elders with memory impairment: The MIND at Home experience | Descriptive analysis | Baltimore, Maryland, US | Home and community | Phone and in person | Community-residing people in northwest Baltimore (28 postal codes), 70 years and older, English-speaking, met criteria for dementia or cognitive disorder, and had a reliable study partner (dyad) | Interdisciplinary team made up of trained nonclinical community workers (ie, memory care coordinator), nurses, physicians (ie, geriatric psychiatrists), and occupational therapists | Memory care coordinator |
| Samus et al.,35 2017 | Comprehensive home-based care coordination for vulnerable elders with dementia: Maximizing Independence at Home-Plus—study protocol | Protocol for randomized controlled trial | US | Home and community | Phone and in person | People with dementia and their caregivers | Interdisciplinary made up of geriatric psychiatrist, registered nurse, occupational therapist, memory care coordinator | Memory care coordinator |
| Samus et al.,36 2018 | MIND at Home-streamlined: study protocol for a randomized trial of home-based care coordination for persons with dementia and their caregivers | Protocol for randomized controlled trial | Baltimore, Maryland, US | Home and community | Phone and in person | Community-residing people in northwest Baltimore (28 postal codes), 70 years and older, English-speaking, met criteria for dementia or cognitive disorder, and had a reliable study partner (dyad) | Interdisciplinary team made up of geriatric psychiatrist, registered nurse, occupational therapist, memory care coordinator | Memory care coordinator |
| Silverstein et al.,58 2015 | The Alzheimer’s Association Dementia Care Coordination program: a process evaluation, executive summary | Mixed methods | Massachusetts and New Hampshire, US | Community | In person | People with dementia and their families | N/A | Care consultant |
| Tanner et al.,37 2015 | A randomized controlled trial of a community-based dementia care coordination intervention: effects of MIND at Home on caregiver outcome | Randomized controlled trial | Baltimore, Maryland, US | Home and community | Phone and in person | Community-residing people in northwest Baltimore (28 postal codes), 70 years and older, English-speaking, met criteria for dementia or cognitive disorder, and had a reliable study partner (dyad) | Interdisciplinary team made up of geriatric psychiatrist, registered nurse, occupational therapist, memory care coordinator | Memory care coordinator |
| Taylor et al.,62 2015 | The Primary Care Navigator programme for dementia: benefits of alternative working models | Report using qualitative assessment | Gateshead and Halton, UK | Community (based out of a general practitioner practice and a well-being enterprises community interest company) | Phone and in person | People with dementia, pre- and post-diagnosis | Clinical; each site organized differently. At Gateshead, 2 people shared the primary care navigator role, switching roles as health care assistant and primary care navigator weekly. They worked with a clinical team, which included doctors, a registrar, nurse practitioners, and a nursing team. At Halton, 10 community well-being officers acted as primary care navigators. They had clinical backgrounds. They partnered with 17 practices. | Primary care navigator |
| Tjia,44 2019 | A telephone-based dementia care management intervention-finding the time to listen | Editorial/ invited commentary | California, Nebraska, and Iowa, US | Home and community (based out of urban academic health centers) | Phone and email | Dyads made up of people with dementia and their caregivers; diagnosis required, speaking English, Spanish or Cantonese, and residing in Iowa, California, or Nebraska | Interdisciplinary team made up of a care team navigator, dementia specialist nurse, social worker, and pharmacist | Care team navigators |
| Willink et al.,38 2020 | Cost-effective care coordination for people with dementia at home | Prospective, quasi-experimental intervention trial design | Baltimore and Maryland suburban District of Columbia, US | Home and community | Phone and in person | Community-residing people in northwest Baltimore (28 postal codes), 70 years and older, English-speaking, met criteria for dementia or cognitive disorder, and had a reliable study partner (dyad) | Interdisciplinary team made up of geriatric psychiatrist, registered nurse, occupational therapist, memory care coordinator | Memory care coordinator |
| Wood et al.,52 2017 | A holistic service for everyone with a dementia diagnosis (innovative practice) | Report | Islington borough of London, UK | Home and community | Phone, mail, and in person | People with dementia and their caregivers | Interdisciplinary team made up of dementia navigators, 3 full-time assistant practitioners, and specialist practitioner as team leader | Dementia navigators |
| Xiao et al.,64 2016 | The effect of a personalized dementia care intervention for caregivers from Australian minority groups | Randomized controlled trial | Adelaide, South Australia | Home and community | Phone and in person | Dyads made up of people with dementia and their caregivers; caregivers were from a minority group, living at home | Interdisciplinary team made up of 8 care coordinators, which included a registered nurse, a social worker, and 6 Community Home Care Certificate holders | Care coordinator |
N/A, not applicable.
Appendix IV: Barriers, facilitators, and descriptions of included studies
| Author, year | Title | Program description and services | Program barriers (barriers to implementation or delivery) | Program facilitators |
|---|---|---|---|---|
| Amjad et al.,32 2018 | Health services utilization in older adults with dementia receiving care coordination: the MIND at Home trial | Maximizing Independence (MIND) at Home’s primary goals were to delay transition from the home and to reduce unmet care needs. The secondary goals included improving quality of life, decreasing neuropsychiatric symptoms, and reducing depression. The program provided services to clients, such as resource referrals, identifying and addressing potential environmental safety hazards, dementia care education, behavior management skills training, informal counseling, and problem-solving. They handled care needs, such as evaluation/diagnosis (primary care provider or specialist referral for dementia evaluation), treatment of cognitive symptoms and behavior management, referral to Alzheimer’s Association, medication administration, general medical/health care and safety, assistance with daily activities, legal issues/advance care planning, caregiver education, caregiver referrals, caregiver mental health care, and caregiver general medical/health care. | MIND care coordinators had difficulties establishing contacts with the respective health providers on behalf of intervention participants. | Integration, communication, and collaboration between the MIND care team and clients’ health providers. |
| Bass et al.,59 2003 | The Cleveland Alzheimer’s managed care demonstration: outcomes after 12 months of implementation | Care consultants worked with families to help identify personal strengths and resources within the family system, health plan, and community to make an individual care plan. Often this included using other association services, such as education and training programs, support groups, a respite reimbursement program, and a nationwide program to return wanderers safely home. The program’s goal was to provide tools to enhance patients’ and caregivers’ competence and self-efficacy. Consultants also provided information about available community services, facilitated decisions about how to best utilize and apply for these services, and contacted service agencies on behalf of patients and caregivers. Standardized protocol for service delivery included conducting a structured initial assessment, identifying problems or challenges, and developing strategies for using personal, family, and community resources. | — | Collaboration and partnership with Alzheimer’s Association. |
| Bass et al.,45 2013 | Caregiver outcomes of Partners in Dementia Care: effect of a care coordination program for veterans with dementia and their family members and friends | The Partners in Dementia Care care-coordination program was focused on integrating and improving access to medical and nonmedical services, while strengthening clients’ informal care network and providing information, coaching, and emotional support. There were two coordinators. The VA care coordinator also focused on helping families use VA services and benefits effectively, whereas the Alzheimer’s Association care coordinator focused on helping families use community services effectively. Standardized protocol included assessment and reassessment, action planning, and ongoing monitoring. | — | Shared electronic Care Coordination Information System; regularly scheduled planning and case-conference meetings; frequent contact with clients; and the low cost to deliver the navigation service. |
| Bass et al.,46 2014 | A controlled trial of Partners in Dementia Care: veteran outcomes after six and twelve months | Partners in Dementia Care was a formal partnership between Veterans Affairs medical centers (a health care organization) and Alzheimer’s Association chapters (a community service organization). The care coordinator gave equal attention to veterans with dementia and their primary informal caregivers. The program was designed to facilitate holistic care; improve fragmentation and lack of coordination between medical care and community services; increase health care providers’ awareness about nonmedical needs of patients and caregivers; increase information and educational resources on dementia, its care, and illness-related strain; reduce difficulties accessing and monitoring services; and improve management of dementia with coexisting medical conditions. | — | Partnership between medical and community organizations. |
| Bass et al.,47 2015 | Impact of the care coordination program “Partners in Dementia Care” on veterans’ hospital admissions and emergency department visits | Partners in Dementia Care was designed to coordinate health care and community services. This partnership promoted holistic, less fragmented care for the medical and nonmedical needs of individuals with dementia and their caregivers; increased attention to informal caregivers as fundamental to long-term care; increased access to information and educational resources; and improved management of coexisting medical conditions. The program had a standardized protocol and followed a coaching model. | — | Formal partnership between a health care organization and community service organization; increased attention to informal caregivers as the lynchpin of long-term care. |
| Bernstein et al.,22 2019 | The role of care navigators working with people with dementia and their caregivers | The Care Ecosystem was a dementia-capable model that provides personalized and proactive care for people with dementia and their caregivers. People with dementia were assigned to a care team navigator, who identified needs and concerns; provided education and curated information about community-based resources; provided linkages to resources; provided care coordination; and provided emotional support by phone and email. Care team navigators also shared care planning and legal and decision-making tools, and provided tailored behavioral interventions. Behavioral interventions included providing, as needed, educational information about behaviors and instrumental help identifying resources, such as day programs or caregiver support programs. | Patient navigator burnout; the progressive nature of dementia; coordinating with primary care providers; and identifying resources for dyads who are low-income, do not speak English, and/or live in rural areas. | Working closely with caregivers; tailoring education and resources; and coordinating with a clinical team around issues ranging from clinical questions to financial and legal decision-making as facilitators. |
| Bernstein et al.,39 2020 | Using care navigation to address caregiver burden in dementia: a qualitative case study analysis | Care team navigators, who were dementia specialists without medical degrees but received training, implemented the Care Ecosystem program’s care model. They worked directly with caregivers and patients, enrolled as dyads. Care team navigators identified needs and concerns. They provided education and information, linkages to resources, care coordination, and emotional support. They also coordinated with the clinical support team and other providers as needed. | — | Care team navigators had continuous contact with dyads by providing support and information; and the flexible delivery model enabled the Care Ecosystem to be more accessible and sustainable, with a broader reach. |
| Chen et al.,55 2020 | Effect of care coordination on patients with Alzheimer disease and their caregivers | The Memory Program prioritized meeting both caregiver and patient needs by assisting with communication with their primary care physicians; providing licensed social worker services and other health care professionals for support, coaching, education, and referrals; creating a Caregiver Resource Library, an information source to learn about caregiving, managing stress, giving care, and topics related to memory health and self-care; and disseminating educational and supportive events led by experts in memory and geriatric care. | — | — |
| Dang et al.,57 2008 | Care coordination assisted by technology for multiethnic caregivers of persons with dementia: a pilot clinical demonstration project on caregiver burden and depression | The Telephone-Linked Care for dementia program was modeled on the REACH program. Telephone-Linked Care offered access to resources and provided communication, support, education, and monitoring of caregivers, supplemented by access to the care coordinator and to a wide variety of community and Veterans Health Administration resources. | — | Veteran Affairs computerized patient record system, which provided access to medical information about the clients and facilitated care coordination and communication with the clients’ providers. |
| Dementia Waikato,66 2017 | Dementia navigator service | Dementia Navigator Service provided initial information and education following a diagnosis of dementia, and then provided ongoing support, advice, and assistance to live well with dementia at home. It provided education about dementia symptoms and how to manage them; referral for professional assessment of any additional funded services; information and support about planning for the future; navigation through health system services; and ongoing contact by phone or visits as necessary, with a support coordinator. | — | — |
| Department of Veterans Affairs,67 2020 | Rural Interdisciplinary Team Training (RITT) dementia care coordinator program | The dementia care coordinator provided one-on-on counseling, support, and education for caregivers of veterans with dementia. They helped caregivers connect to needed resources, apply for benefits, and navigate the health care systems. The program’s goal was to help caregivers reduce stress, improve problem-solving skills, and connect them to helpful resources. VA medical centers and VA community-based outpatient clinics referred caregivers to the program. Caregivers received 4-5 individual sessions based around assessment, instruction in stress-reduction techniques, and help with problem-solving. | — | — |
| Fæø et al.,53 2020 | The compound role of a coordinator for home-dwelling persons with dementia and their informal caregivers: qualitative study | LIVE@Home.Path was a multicomponent, multidisciplinary intervention aiming to support dyads of people with dementia and their informal caregivers to live safely and independently at home. The program’s core components are learning, innovation, volunteers, and empowerment (LIVE). The education component included an optional educational course. The empowerment component involved the dementia coordinator coordinating the LIVE components and ensuring that the individual with dementia is empowered throughout the LIVE intervention process. The coordinator aimed to provide participants with care and support that was in line with their own perceived needs and wishes. The coordinator was a safety net, a pathfinder, and a source for emotional care and support. This function was flexible and ranged from giving basic information on available care and support to more or less taking over coordination of the many health and care services involved. | — | Flexibility and accessibility of delivery model allowed navigators to meet participants’ needs. |
| Fortinsky et al.,65 2002 | Helping family caregivers by linking primary care physicians with community-based dementia care services: the Alzheimer’s Service Coordination Program | The Alzheimer’s Service Coordination Program was established to link primary care physicians in a partnership arrangement with a local branch of the Alzheimer’s Association that specialized in dementia care education and support services. The purposes of the program were to educate family caregivers about dementia symptom management; how to access community resources to enhance their own care; and to raise awareness among primary care physicians about community resources for people with dementia and their families. Physicians referred family caregivers to a service coordinator, who provided individualized consultation to family caregivers and people with dementia regarding all nonmedical aspects of dementia care and available resources in the community. | — | — |
| Galik and Stefanacci,69 2019 | Improving care for patients with dementia: what to do before, during, and after a transition | The Alzheimer’s patient navigator helped people with dementia and their families plan to better manage the necessary medical care and social services. The navigators functioned across the continuum of care. They provided proactive care planning; caregiver support and education; and minimized unnecessary patient transitions. The program helped build communication skills with respect to cultural sensitivity and person-centered plans. The program also provided the necessary skills to help differentiate and navigate among the multiple systems and organizations involved in care. | — | — |
| Galvin et al.,56 2014 | Public–private partnerships improve health outcomes in individuals with early-stage Alzheimer’s disease | Project Learn MORE (Missouri Outreach and Referral Expanded) was a multisite intervention consisting of comprehensive care consultations to improve coping skills. The program operated through referrals. Area Agencies on Aging care coordinators visited participants’ homes and conducted an assessment to determine eligibility for services such as nutrition and dining programs, care transitions, and case management services. Care consultations were an individualized 2-hour consultation with the care recipient and caregiver, conducted in a convenient location. The consultation included a comprehensive assessment and an individualized action plan to address client needs regarding coping skills, education, supportive services, planning for the future, and referrals to services (eg, legal advice, driving assessments). Social workers, physicians, or direct telephone calls from older adults initiated the referrals. | Difficulty coordinating efforts between community service partners to refer eligible clients for additional services. | Area Agencies on Aging computer database and AD8 dementia screening tool to identify older Missourians with dementia. |
| Goeman et al.,63 2016 | Development of a model of dementia support and pathway for culturally and linguistically diverse communities using co-creation and participatory action research | The specialist dementia nurse navigated clients through health care service systems. They provided culturally appropriate information to assist people with dementia and their caring unit to adjust to living with memory loss by educating them about dementia and the need for forward care planning; identified unmet needs; provided in-home strategies to manage changes in behavior to improve the quality of life of people with dementia and reduce caregiver strain; obtained culturally appropriate assessment and diagnosis; and acted as an advocate when necessary. Interventions included brochures translated into clients’ language, information on forward planning, accessing local council home care and personal hygiene services, incontinence advice, referral to consumer and caregiver advocacy groups, community assessment services, behavioral management services, music therapy, assistance in accessing financial reimbursements, and aids and assistive technology. | In some cases, available services and activities were not always compatible with participants’ needs. | The navigator’s ability to build trusting professional relationships, excellent assessment abilities, an in-depth knowledge of dementia, excellent interpersonal, listening, and advocacy skills. Tools such as the culturally and linguistically diverse dementia care pathway quick reference cards to guide engagement with the client. |
| Husebo et al.,54 2020 | LIVE@Home.Path—innovating the clinical pathway for home-dwelling people with dementia and their caregivers: study protocol for a mixed methods, stepped-wedge, randomized controlled trial | LIVE@Home.Path was a multicomponent, multidisciplinary intervention aiming to support dyads of people with dementia and their informal caregivers to live safely and independently at home. The program’s coordinator facilitated learning, innovation, volunteers, and empowerment (LIVE). The coordinator facilitated participation in local educational programs. The innovation component consisted of the coordinator assessing and evaluating the usefulness of information and communication technology solutions that were already in use for the dyads and informing them about other relevant welfare technology available in the municipality. The coordinator also informed participants about new communication platforms that could meet needs of families organizing dementia care. For volunteering, the coordinator contacted and facilitated linkages between the dyads and volunteer organizations that can help them. For the empowerment component, the coordinator scheduled a meeting with the general practitioner to promote an empowered approach to advanced care planning. The coordinator conducted a minimum of 2 home visits and monthly phone calls. | — | — |
| Joels and van Pol,51 2014 | How to manage follow-up patients: dementia navigators | This navigator model provided information about diagnosis; proactive referral to a range of resources (eg, health and social care, day service, third-sector support, benefits check, taxi-cards, well-being and housing, will-writing services); follow-up calls to confirm referral efficacy; and ongoing contact with services. They also scheduled reviews for those in need and wrote care plans, which were cc’d to general practitioners. | — | Program used a risk stratification tool to help determine intervention frequency and format. |
| Judge et al.,48 2011 | Partners in Dementia Care: a care coordination intervention for individuals with dementia and their family caregivers | Partners in Dementia Care was a formal partnership between VA medical centers and Alzheimer’s Association chapters. It included a multidimensional assessment and treatment approach; ongoing monitoring and long-term relationships with families; and a computerized information system that guided service delivery and fidelity monitoring. The 4 main ways to assist patients and families were providing disease-related education and information; offering emotional support and coaching; linking/connecting families to medical and nonmedical services and resources; and mobilizing and organizing the informal care network. The program used an intervention protocol, assessment of care needs, development of care goals, development of action steps, and ongoing monitoring of action steps. | Perceptions of problems with the quality of Alzheimer’s Association services; quality of VA services; lack of knowledge of the Alzheimer’s Association services; lack of knowledge of VA services; and organizational financial problems limiting the success of Partners in Dementia Care, ability to share patient/family information between partner organizations, and overall challenges in collaboration between organizations. | The computer system; involvement of caregivers; initial and ongoing support from key leaders and site champions at both organizations; flexible communication model enabled maintenance of long-term relationships in a time- and cost-efficient way with clients; and scalable to rural areas. |
| Lee et al.,61 2014 | Integrating community services into primary care: improving the quality of dementia care | Primary care collaborative memory clinics provided patients with comprehensive multidisciplinary assessments and a shared care and evidence-based approach to support timely access to quality dementia care. This included a needs assessment; referrals to other care providers; facilitation of linkages to other community services, such as Alzheimer Society of Ontario; and coordination of access to resources and services. Clinics had a partnership with the Alzheimer Society. | Concerns related to privacy and confidentiality issues associated with sharing patient information with an external service (these were resolved with the development of formal confidentiality agreements). Clinics faced some challenges establishing efficient strategies for maintaining effective communication between all team members; and initial struggles with the stigma associated with introducing someone from the Alzheimer Society before a diagnosis. | Training course provided to the clinics to improve the detection and management of dementia. |
| Liu et al.,68 2019 | Patient and caregiver outcomes and experiences with team-based memory care: a mixed methods study | This single hospital-based memory clinic provided specialized memory care services using a team-based approach to diagnose and treat Alzheimer’s disease, related dementias, and other memory issues in older adults. The program focused on counseling patients and caregivers about diagnosis and disease progression; helping them work through economic and social concerns while navigating the medical system; and ensuring that providers receive information necessary for seamless care coordination. Each visit included a detailed interview with the patient and caregiver(s), medication reconciliation and review, comprehensive geriatric physical examination, functional assessment, goals of care discussion, social support and health literacy assessments, and depression/cognitive testing. | Patients and caregivers did not indicate they would reach out to the clinic as the first line of care for perceived unrelated medical conditions, so enhancing this program to include a memory care medical home could improve appropriate utilization of health care services in this population. | Incorporation of a navigator into the care team is a useful way to involve caregivers while providing protected space for both parties to express their concerns. |
| McAiney et al.,60 2012 | ‘Throwing a lifeline’: the role of First Link(TM) in enhancing support for individuals with dementia and their caregivers | The First Link initiative of the Alzheimer Society aimed to support individuals with dementia through a partnership between the Alzheimer Society and physicians, who referred people with dementia and their caregivers to the program. First Link referred them to community resources, education material, and support and coordination services. It encouraged health professionals to refer individuals to First Link at the time of diagnosis and accepted self-referrals as well. Individuals with dementia (or family members) who agreed to have their name shared with the Alzheimer Society were contacted by phone by the First Link coordinator. | In Saskatchewan, despite the ease with which referrals were made, the requirement for signed consent for the referral was identified as a significant barrier to referrals. | Linkages and partnerships with primary care physicians; and community resources and support helped increased clients’ access. |
| Merrilees et al.,40 2020 | The Care Ecosystem: promoting self-efficacy among dementia family caregivers | The Care Ecosystem was a dementia-capable model providing personalized and proactive care for people with dementia and their caregivers. They were assigned to a care team navigator who identified needs and concerns. The care team navigator provided education and information, linkages to resources, care coordination, and emotional support and active listening. The proactive care protocols focused on issues critical to quality dementia care such as caregiver support and education, strategies for dealing with dementia-related behaviors, safety counseling, medication review, advance care planning, and links to community resources. | — | Adaptability of the program, which emphasized a multicomponent array of strategies and suggestions that could be personalized for each dyad, with flexible communication depending on dyad needs. |
| Morgan et al.,49 2015 | A break-even analysis for dementia care collaboration: Partners in Dementia Care | Partners in Dementia Care was a telephone-based care coordination and support service for veterans with dementia and their caregivers. It was designed to be a feasible and practical intervention integrating health, community, and support services to address the unmet care needs of patients and their caregivers across all dementia stages. The service assisted families by providing disease-related education and information; offering emotional support and coaching; linking families to medical and nonmedical services and resources; and mobilizing and organizing the informal care network. | — | — |
| Morgan et al.,50 2019 | Does care consultation affect use of VHA versus non-VHA care? | Partners in Dementia Care was a telephone-based care coordination and support service intervention for veterans with dementia and their caregivers. It was delivered through partnerships between VHA medical centers and local Alzheimer’s Association chapters. It was designed to integrate health, community, and support services to address the unmet care needs of patients and caregivers across all dementia stages. | — | — |
| Possin et al.,41 2017 | Development of an adaptive, personalized, and scalable dementia care program: early findings from the Care Ecosystem | The Care Ecosystem was a scalable model of dementia specialty care that complemented primary care with additional caregiver support and education, medication consultation, and support in planning for future medical, financial, and legal decisions consistent with patient values. The role of the care team navigator was limited to include identifying gaps in planning (eg, identifying a health care agent); making legal referrals; preparing the family for a billable advance care planning appointment with their primary care provider; providing education and screening monthly for acute health changes; and providing emotional support/active listening. | Navigator burnout and stress; unclear triage protocols and the limits of using a non-licensed staff member as the first point of contact in delivering specialty care. | The navigators not being specialists/licensed health providers made them affordable. |
| Possin et al.,42 2019 | Effect of collaborative dementia care via telephone and internet on quality of life, caregiver well-being, and health care use: the Care Ecosystem randomized clinical trial | The Care Ecosystem was a dementia-capable model, which provided personalized and proactive care for people with dementia and their caregivers. People with dementia were assigned to a care team navigator who identified needs and concerns. Care team navigators also provided education and information, linkages to resources, care coordination, and emotional support by phone and email. | — | Patient navigators’ flexible communication with clients, which makes the program scalable and accessible in rural areas; the program can be delivered from a centralized hub to clients either affiliated with multiple health systems or integrated within a single health system. |
| Rosa et al.,43 2019 | Variations in costs of a collaborative care model for dementia | The Care Ecosystem used care protocols that guided navigators through caregiver support and education, medications, advance care planning, and behavior symptom management. | — | The cost of program implementation decreased substantially during the implementation periods and depended on caseload (minimum of 50). |
| Samus et al.,33 2014 | A multidimensional home-based care coordination intervention for elders with memory disorders: the Maximizing Independence at Home (MIND) pilot randomized trial | MIND at Home was an 18-month care coordination intervention to systematically identify and address dementia-related care needs through individualized care planning, referral and linkage to services, provision of dementia education and skill-building strategies, and care monitoring by an interdisciplinary team. Coordinators reviewed the assessment, conducted an in-home visit with the participant and study partner to review and prioritize needs, and developed the care plan. A menu of care options/strategies was available for each unmet need and consisted of referrals and linkages to resources/services; caregiver memory disorder education and skill-building; and informal counseling and problem-solving. There were 2 in-home visits and monthly contacts. The intervention was designed to be deliverable through community-based aging service providers or service networks and link community-based care with a medical team. | — | Affordability of program. |
| Samus et al.,34 2015 | A multipronged, adaptive approach for the recruitment of diverse community-residing elders with memory impairment: the MIND at Home experience | MIND at Home’s intervention components included in-home dementia-related needs assessments, individualized care planning, implementation of standardized evidence-based care strategy protocols, and ongoing monitoring and reassessment. | Access to eligible clients, underdiagnosis, misinformation about dementia, stigma, isolation, cultural insensitivity. | Targeted outreach to potential clients, partnerships with nontraditional, nonmedical, and cultural-specific organizations; providing dementia education in local forums and use of proactive strategies to counteract underdiagnosis and raise awareness; aligning study objectives with unmet community needs and seeking input to obtain community stakeholder buy-in. To improve referrals: expand eligibility criteria, increase reminders about the study and eligibility criteria, and improve case identification knowledge. |
| Samus et al.,35 2017 | Comprehensive home-based care coordination for vulnerable elders with dementia: Maximizing Independence at Home-Plus—study protocol | Maximizing Independence at Home-Plus (MIND at Home) was a new model of comprehensive home-based dementia care coordination tested in the United States. The program aimed to address delivery gaps, improve outcomes, and lower costs. MIND at Home-Plus systematically assessed and addressed a broad range of unmet dementia-related care needs that placed elders at risk of health disparities, unwanted long-term care placement, poor quality of life, and caregiver burden. MIND at Home-Plus services were delivered to participants for up to 24 months, with the primary end point for evaluation of impact on outcomes assessed at 18 months. | — | A set of tools that support the implementation and delivery of MIND-S, such as MIND at Home Intervention Handbook and Johns Hopkins Dementia Care Needs Assessment 2.0. |
| Samus et al.,36 2018 | MIND at Home-streamlined: study protocol for a randomized trial of home-based care coordination for persons with dementia and their caregivers | The Maximizing Independence at Home dementia care coordination program was a comprehensive, home-based care coordination intervention for people with dementia who lived in the community and for their caregivers. Intervention components included in-home dementia-related needs assessments, individualized care planning, implementation of standardized evidence-based care strategy protocols, and ongoing monitoring and reassessment. | — | A set of tools that support the implementation and delivery of MIND-S, such as MIND at Home Intervention Handbook and Johns Hopkins Dementia Care Needs Assessment 2.0. |
| Silverstein et al.,58 2015 | The Alzheimer’s Association Dementia Care Coordination Program: a process evaluation, executive summary | In the Dementia Care Coordination program, care consultants connected directly with people with dementia and their caregivers who were referred to the Massachusetts/New Hampshire Alzheimer’s Association chapter by health care providers. The care consultant provided disease-specific education, symptom management strategies, emotional support, and referrals and linkages to community resources. They also encouraged the caregiver to utilize other Alzheimer’s Association services, including support groups, education programs, and advocacy opportunities. Consultants collaborated with other staff members and volunteers to provide ongoing information and support to families. Consultants provided written feedback to health care providers and nurse case managers on client needs and recommendations to meet those needs. | Consultants experienced issues in communicating with physicians, who work with different electronic medical record systems that have varying degrees of security and have differing preferences regarding their preferred communication methods – fax, phone, or email. | One way to manage the workload was to utilize dedicated volunteers, trained in the 24/7 Helpline and care consultation, to support the care consultants. |
| Tanner et al.,37 2015 | A randomized controlled trial of a community-based dementia care coordination intervention: effects of MIND at Home on caregiver outcome | Maximizing Independence at Home, a community-based, multicomponent care coordination intervention, reduced unmet caregiving needs and burden in informal caregivers of persons with memory disorders. | While intended to empower caregivers, the intervention asked caregivers to take a larger role in the care of the person with dementia, which may have added additional stresses. It was possible that dyads and coordinators prioritized intervening on care recipient needs before caregivers needs. | — |
| Taylor et al.,62 2015 | The Primary Care Navigator programme for dementia: benefits of alternative working models | The Primary Care Navigator for dementia role provided support for people with dementia who were both pre- and post-diagnosis. The primary care navigator was trained to listen and guide people to the support and resources they needed from local and national services. Organizations developed the roles according to the needs of each site. They created care plans and supported physicians and nurses. At the Gateshead site, the primary care navigator developed a directory of services. | — | Full engagement from the outset, together with continued leadership from the practice; a collaborative approach; agreeing individual care plans and assigning general practitioners. |
| Tjia,44 2019 | A telephone-based dementia care management intervention-finding the time to listen | The Care Ecosystem was a dementia-capable model that provided personalized and proactive care for people with dementia and their caregivers. People with dementia were assigned to a care team navigator who identified needs and concerns, provided education and information, supported linkages to resources, provided care coordination, and provided emotional support by phone and email. | — | Navigators’ strong communication and listening skills, responding to caregivers’ immediate needs and then screening for common problems and providing personalized support; telephone provided flexible and accessible communication; program was scalable across economic, and health system boundaries. |
| Willink et al.,38 2020 | Cost-effective care coordination for people with dementia at home | Maximizing Independence at Home was a home-based dementia care coordination program administered by trained, nonclinical community workers as the primary contact between people with dementia and their caregivers, supported by a multidisciplinary clinical team with expertise in dementia care. It systematically assessed and addressed a broad range of unmet dementia-related care needs for people with dementia and caregivers that place older adults at risk of health disparities, high health care costs, poor clinical outcomes, poor quality of life, and caregiver burden. | — | Cost-effective; scalable; collaboration between medical organizations, community resources, patients, and families. |
| Wood et al.,52 2017 | A holistic service for everyone with a dementia diagnosis (innovative practice) | The Dementia Navigator Service was built on the existing Dementia Advisors Model operated by the Alzheimer’s Society to provide signposting to services and assistance to navigate the health and social care systems. This service aimed to reduce social isolation; monitor and manage risk; promote effective communication and partnerships by working between health and social care and third-sector providers; provide a person-centered responsive service to everyone in the borough with dementia living in the community; and enable people living with dementia and those who care for them to access the services they need to avoid crisis. Most referrals to the Dementia Navigator Service were received following diagnosis by the Memory Assessment and Treatment Service. | — | Liaising with general practitioners, social workers, and those working in the nonprofit sector facilitates access to appropriate health and social care services in a timely manner to prevent crises. |
| Xiao et al.,64 2016 | The effect of a personalized dementia care intervention for caregivers from Australian minority groups | A community care coordinator-led personalized dementia care intervention for caregivers from 10 minority groups. “The Inventory of Carer’s Needs” listed 5 areas of caregiver support: information needs, educational and skill needs, environmental safety needs, social-cultural care needs, and self-care needs that reflect the current research evidence in dementia caregiver support. The coordinators used a Personalized Caregiving Support Plan to assess caregivers’ needs. They provided regular and frequent visits to assess needs. They referred caregivers to new services and education programs based on this needs assessment. When necessary, they organized conferences with caregivers and care staff to discuss ongoing challenges. The usual caregiver support included activities such as monthly caregiver support group meetings and information sessions that were funded by the National Respite for Carers Program. | — | Two instruments, the Personalized Caregiving Support Plan and a “caregiving diary”: the use of the caregiving diary allowed care staff to identify care needs of care recipients and provide face-to-face coaching with caregivers and evaluate the effectiveness of care staff’s actions. |
VA, Veterans Affairs.
Footnotes
The authors declare no conflicts of interest.
Supplemental Digital Content is available for this article. Direct URL citations appear in the text and are provided in the HTML version of this article on the journal's website, www.jbievidencesynthesis.com.
Contributor Information
Grailing Anthonisen, Email: grailing.anthonisen@mcgill.ca.
Alison Luke, Email: aluke1@unb.ca.
Lillian MacNeill, Email: lillian.macneill@unb.ca.
A. Luke MacNeill, Email: luke.MacNeill@unb.ca.
Alex Goudreau, Email: Alex.Goudreau@unb.ca.
Shelley Doucet, Email: sdoucet@unb.ca.
References
- 1.Singh P, Hussain R, Khan A, Irwin L, Foskey R. Dementia care: intersecting informal family care and formal care systems. J Aging Res 2014;2014:486521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alzheimer’s Association. Dementia vs. Alzheimer’s disease: what is the difference? [internet]. Alzheimer’s Disease and Dementia. [cited 2021 Jan 18]. Available from: https://alz.org/alzheimers-dementia/difference-between-dementia-and-alzheimer-s. [Google Scholar]
- 3.World Health Organization. Dementia factsheet [internet]. WHO; 2020 [cited 2021 Jan 21]. Available from: https://www.who.int/news-room/fact-sheets/detail/dementia.
- 4.Canadian Dementia Priority Setting Partnership. Canadian Dementia research priorities: report of the Canadian Dementia Priority Setting Partnership. Canadia Dementia; 2018; p. 22.
- 5.Moore A, Frank C, Chambers LW. Role of the family physician in dementia care. Can Fam Physician 2018;64(10):717–9. [PMC free article] [PubMed] [Google Scholar]
- 6.Smith R, Martin A, Wright T, Hulbert S, Hatzidimitriadou E. Integrated dementia care: a qualitative evidence synthesis of the experiences of people living with dementia, informal carers and healthcare professionals. Arch Gerontol Geriatr 2021;97:104471. [DOI] [PubMed] [Google Scholar]
- 7.Stephan A, Bieber A, Hopper L, Joyce R, Irving K, Zanetti O, et al. Barriers and facilitators to the access to and use of formal dementia care: findings of a focus group study with people with dementia, informal carers and health and social care professionals in eight European countries. BMC Geriatr 2018;18(1):131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee C. Health, stress and coping among women caregivers: a review. J Health Psychol 1999;4(1):27–40. [DOI] [PubMed] [Google Scholar]
- 9.Lee C, Gramotnev H. Transitions into and out of caregiving: health and social characteristics of mid-age Australian women. Psychol Health 2007;22(2):193–209. [Google Scholar]
- 10.Sinha M; Statistics Canada, Social and Aboriginal Statistics Division. Portrait of caregivers 2012 [internet]. 2014. [cited 2021 Apr 27]. Available from:http://www.deslibris.ca/ID/240440. [Google Scholar]
- 11.Fillion L, Cook S, Veillette AM, Aubin M, de Serres M, Rainville F, et al. Professional navigation framework: elaboration and validation in a Canadian context. Oncol Nurs Forum 2012;39(1):E58–69. [DOI] [PubMed] [Google Scholar]
- 12.Freeman HP, Rodriguez RL. History and principles of patient navigation. Cancer 2011;117(S15):3537–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McMullen L. Oncology nurse navigators and the continuum of cancer care. Semin Oncol Nurs 2013;29(2):105–117. [DOI] [PubMed] [Google Scholar]
- 14.Carter N, Valaitis RK, Lam A, Feather J, Nicholl J, Cleghorn L. Navigation delivery models and roles of navigators in primary care: a scoping literature review. BMC Health Serv Res 2018;18(1):96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reid AE, Doucet S, Luke A, Azar R, Horsman AR. The impact of patient navigation: a scoping review protocol. JBI Evid Synth 2019;17(6):1079–85. [DOI] [PubMed] [Google Scholar]
- 16.Freeman HP. The history, principles, and future of patient navigation: commentary. Semin Oncol Nurs 2013;29(2):72–5. [DOI] [PubMed] [Google Scholar]
- 17.Beverly EA, Hamel-Lambert J, Jensen LL, Meeks S, Rubin A. A qualitative process evaluation of a diabetes navigation program embedded in an endocrine specialty center in rural Appalachian Ohio. BMC Endocr Disord 2018;18(1):50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Loskutova NY, Tsai AG, Fisher EB, LaCruz DM, Cherrington AL, Harrington TM, et al. Patient navigators connecting patients to community resources to improve diabetes outcomes. J Am Board Fam Med 2016;29(1):78–89. [DOI] [PubMed] [Google Scholar]
- 19.Anand SK, Macki M, Culver LG, Wasade VS, Hendren S, Schwalb JM. Patient navigation in epilepsy care. Epilepsy Behav 2020;113:107530. [DOI] [PubMed] [Google Scholar]
- 20.Sullivan C, Leon JB, Sayre SS, Marbury M, Ivers M, Pencak JA, et al. Impact of navigators on completion of steps in the kidney transplant process: a randomized, controlled trial. Clin J Am Soc Nephrol 2012;7(10):1639–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anderson JE, Larke SC. Navigating the mental health and addictions maze: a community-based pilot project of a new role in primary mental health care. Ment Health Fam Med 2009;6(1):15–9. [PMC free article] [PubMed] [Google Scholar]
- 22.Bernstein A, Harrison KL, Dulaney S, Merrilees J, Bowhay A, Heunis J, et al. The role of care navigators working with people with dementia and their caregivers. J Alzheimers Dis 2019;71(1):45–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stefanacci RG, Freeman HP, Gay R, Michael M, Digby D. Community long-term care and the Alzheimer’s disease patient navigator. Ann Long Term Care 2016;24(5):19–21. [Google Scholar]
- 24.Doucet S, Luke A, Anthonisen G, Kelly KJ, Goudreau A, MacNeill AL, et al. Patient navigation programs for people with dementia, their caregivers, and members of their care team: a scoping review protocol. JBI Evid Synth 2022;20(1):270–6. [DOI] [PubMed] [Google Scholar]
- 25.Luke A, Doucet S, Azar R. Paediatric patient navigation models of care in Canada: an environmental scan. Paediatr Child Health 2018;23(3):e46–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kelly KJ, Doucet S, Luke A. Exploring the roles, functions, and background of patient navigators and case managers: a scoping review. Int J Nurs Stud 2019;98:27–47. [DOI] [PubMed] [Google Scholar]
- 27.Schutt RK, Siegfriedt J, Fawcett J. Who cares? Case management and patient navigation in a public health programme. Int J Care Caring 2017;1(3):367–87. [Google Scholar]
- 28.Freeman HP. Patient navigation: a community centered approach to reducing cancer mortality. J Cancer Educ Off J Am Assoc Cancer Educ 2006;21(1 Suppl):S11–4. [DOI] [PubMed] [Google Scholar]
- 29.Peters MDJ, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil H.Aromataris E, Munn Z. Chapter 11: Scoping reviews. JBI Manual for Evidence Synthesis [internet]. Adelaide: JBI; 2020. [cited 2021 Feb 4]. Available from:https://synthesismanual.jbi.global. [Google Scholar]
- 30.McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol 2016;75:40–6. [DOI] [PubMed] [Google Scholar]
- 31.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169(7):467–73. [DOI] [PubMed] [Google Scholar]
- 32.Amjad H, Wong SK, Roth DL, Huang J, Willink A, Black BS, et al. Health services utilization in older adults with dementia receiving care coordination: the MIND at Home Trial. Health Serv Res 2018;53(1):556–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Samus Q, Johnston D, Black B, Hess E, Lyman C, Vavilikolanu A, et al. A multidimensional home-based care coordination intervention for elders with memory disorders: the Maximizing Independence at Home (MIND) pilot randomized trial. Am J Geriatr Psychiatry 2014;22(4):398–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Samus QM, Amjad H, Johnston D, Black BS, Bartels SJ, Lyketsos CG. a multipronged, adaptive approach for the recruitment of diverse community-residing elders with memory impairment: The MIND at Home Experience. Am J Geriatr Psychiatry 2015;23(7):698–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Samus QM, Davis K, Willink A, Black BS, Reuland M, Leoutsakos J, et al. Comprehensive home-based care coordination for vulnerable elders with dementia: Maximizing Independence at Home-Plus—study protocol. Int J Care Coord 2017;20(4):123–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Samus QM, Black BS, Reuland M, Leoutsakos JMS, Pizzi L, Frick KD, et al. MIND at Home-Streamlined: study protocol for a randomized trial of home-based care coordination for persons with dementia and their caregivers. Contemp Clin Trials 2018;71:103–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tanner JA, Black BS, Johnston D, Hess E, Leoutsakos JM, Gitlin LN, et al. A randomized controlled trial of a community-based dementia care coordination intervention: effects of MIND at Home on caregiver outcomes. Am J Geriatr Psychiatry 2015;23(4):391–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Willink A, Davis K, Johnston DM, Black B, Reuland M, Stockwell I, et al. Cost-effective care coordination for people with dementia at home. Innov Aging 2020;4(2):igz051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bernstein A, Merrilees J, Dulaney S, Harrison KL, Chiong W, Ong P, et al. Using care navigation to address caregiver burden in dementia: a qualitative case study analysis. Alzheimers Dement 2020;6(1):e12010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Merrilees JJ, Bernstein A, Dulaney S, Heunis J, Walker R, Rah E, et al. The care ecosystem: promoting self-efficacy among dementia family caregivers. Dementia 2020;19(6):1955–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Possin KL, Merrilees J, Bonasera SJ, Bernstein A, Chiong W, Lee K, et al. Development of an adaptive, personalized, and scalable dementia care program: early findings from the Care Ecosystem. PLoS Med 2017;14(3):e1002260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Possin KL, Merrilees JJ, Dulaney S, Bonasera SJ, Chiong W, Lee K, et al. Effect of collaborative dementia care via telephone and internet on quality of life, caregiver well-being, and health care use: the care ecosystem randomized clinical trial. JAMA Intern Med 2019;179(12):1658–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rosa TD, Possin KL, Bernstein A, Merrilees J, Dulaney S, Matuoka J, et al. Variations in costs of a collaborative care model for dementia. J Am Geriatr Soc 2019;67(12):2628–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tjia J. A telephone-based dementia care management intervention—finding the time to listen. JAMA Intern Med 2019;179(12):1667. [DOI] [PubMed] [Google Scholar]
- 45.Bass DM, Judge KS, Snow AL, Wilson NL, Morgan R, Looman WJ, et al. Caregiver outcomes of partners in dementia care: effect of a care coordination program for veterans with dementia and their family members and friends. J Am Geriatr Soc 2013;61(8):1377–86. [DOI] [PubMed] [Google Scholar]
- 46.Bass DM, Judge KS, Snow AL, Wilson NL, Morgan RO, Maslow K, et al. A controlled trial of Partners in Dementia Care: veteran outcomes after six and twelve months. Alzheimers Res Ther 2014;6(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bass DM, Judge KS, Maslow K, Wilson NL, Morgan RO, McCarthy CA, et al. Impact of the care coordination program “Partners in Dementia Care” on veterans’ hospital admissions and emergency department visits. Alzheimers Dement 2015;1(1):13–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Judge KS, Bass DM, Snow AL, Wilson NL, Morgan R, Looman WJ, et al. Partners in dementia care: a care coordination intervention for individuals with dementia and their family caregivers. Gerontologist 2011;51(2):261–72. [DOI] [PubMed] [Google Scholar]
- 49.Morgan RO, Bass DM, Judge KS, Liu CF, Wilson N, Snow AL, et al. A break-even analysis for dementia care collaboration: Partners in Dementia Care. J Gen Intern Med 2015;30(6):804–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Morgan RO, Pathak S, Bass DM, Judge KS, Wilson NL, McCarthy C, et al. Does care consultation affect use of VHA versus non-VHA care? Am J Manag Care 2019;25(4):e119–25. [PubMed] [Google Scholar]
- 51.Joels DS, van de Pol E. How to manage follow- up patients. United Kingdom: National Health Service; 2014. [Epub ahead of print]. [Google Scholar]
- 52.Wood JH, Souris H, Weston-Clarke SM, Bristow S. A holistic service for everyone with a dementia diagnosis (innovative practice). Dementia 2020;19(4):1274–9. [DOI] [PubMed] [Google Scholar]
- 53.Fæø SE, Tranvåg O, Samdal R, Husebo BS, Bruvik FK. The compound role of a coordinator for home-dwelling persons with dementia and their informal caregivers: qualitative study. BMC Health Serv Res 2020;20(1):1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Husebo BS, Allore H, Achterberg W, Angeles RC, Ballard C, Bruvik FK, et al. LIVE@Home.Path—innovating the clinical pathway for home-dwelling people with dementia and their caregivers: study protocol for a mixed-method, stepped-wedge, randomized controlled trial. Trials 2020;21(1):510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chen B, Cheng X, Streetman-Loy B, Hudson MF, Jindal D, Hair N. Effect of care coordination on patients with Alzheimer disease and their caregivers. Am J Manag Care 2020;26(11):e369–75. [DOI] [PubMed] [Google Scholar]
- 56.Galvin JE, Tolea MI, George N, Wingbermuehle C. Public–private partnerships improve health outcomes in individuals with early stage Alzheimer’s disease. Clin Interv Aging 2014;9:621–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dang S, Remon N, Harris J, Malphurs J, Sandals L, Cabrera AL, et al. Care coordination assisted by technology for multiethnic caregivers of persons with dementia: a pilot clinical demonstration project on caregiver burden and depression. J Telemed Telecare 2008;14(8):443–7. [DOI] [PubMed] [Google Scholar]
- 58.Silverstein N, Porell F, Nadash P. The Alzheimer’s Association Dementia Care Coordination Program: a process evaluation, executive summary [internet]. Boston, Massachusetts: Gerontology Institute, McCormack Graduate School of Policy & Global Studies, University of Massachusetts; 2015. [cited 2021 June 17]. Available from: https://scholarworks.umb.edu/gerontologyinstitute_pubs/111. [Google Scholar]
- 59.Bass DM, Clark PA, Looman WJ, McCarthy CA, Eckert S. The Cleveland Alzheimer’s managed care demonstration: outcomes after 12 months of implementation. Gerontologist 2003;43(1):73–85. [DOI] [PubMed] [Google Scholar]
- 60.McAiney CA, Hillier LM, Stolee P, Harvey D, Michael J. ‘Throwing a lifeline’: the role of First LinkTM in enhancing support for individuals with dementia and their caregivers. Neurodegener Dis Manag 2012;2(6):623–38. [Google Scholar]
- 61.Lee L, Hillier LM, Harvey D. Integrating community services into primary care: improving the quality of dementia care. Neurodegener Dis Manag 2014;4(1):11–21. [DOI] [PubMed] [Google Scholar]
- 62.Taylor K, Norris C, Khan S. The Primary Care Navigator programme for dementia: benefits of alternative working models [internet]. United Kingdom: Deloitte Centre for Health Solutions; 2015. [cited 2021 Jun 18]. Available from:https://napc.co.uk/wp-content/uploads/2017/09/PCN_Case_Study_Report.pdf. [Google Scholar]
- 63.Goeman D, King J, Koch S. Development of a model of dementia support and pathway for culturally and linguistically diverse communities using co-creation and participatory action research. BMJ Open 2016;6(12):e013064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Xiao LD, De Bellis A, Kyriazopoulos H, Draper B, Ullah S. The effect of a personalized dementia care intervention for caregivers from Australian minority groups. Am J Alzheimers Dis Other Demen 2016;31(1):57–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fortinsky RH, Unson CG, Garcia RI. Helping family caregivers by linking primary care physicians with community-based dementia care services: the Alzheimer’s Service Coordination Program. Dementia 2002;1(2):227–40. [Google Scholar]
- 66.Dementia Waikato. Dementia Navigator Service [internet]. Waikato, New Zealand: Dementia Waikato; 2017 [cited 2022 Sep 5]. Available from:https://www.dementiawaikato.org.nz/wp-content/uploads/2020/09/Navigator-Service-Dementia-Waikato_20200724_112656-2.pdf. [Google Scholar]
- 67.Department of Veteran’s Affairs. Rural Interdisciplinary Team Training (RITT) Dementia Care Coordinator Program [internet]. Department of Veteran’s Affairs; 2017 [cited 2022 Sep 5]. Available from: https://www.gerischolars.org/pluginfile.php/6277/mod_page/content/95/Dementia%20Care%20Coordination%20Program%202020.pdf.
- 68.Liu TL, Yates TD, Taylor YJ, Rossman W, Mangieri D, Black S, et al. Patient and caregiver outcomes and experiences with team-based memory care: a mixed methods study. J Appl Gerontol 2019:0733464819888838. [DOI] [PubMed] [Google Scholar]
- 69.Galik E, Stefanacci R. Improving care for patients with dementia: what to do before, during, and after a transition. Caring Ages 2019;20(8):4–5. [Google Scholar]
- 70.Lin PJ, Daly AT, Olchanski N, Cohen JT, Neumann PJ, Faul JD, et al. Dementia diagnosis disparities by race and ethnicity. Med Care 2021;59(8):679–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Connolly A, Gaehl E, Martin H, Morris J, Purandare N. Underdiagnosis of dementia in primary care: Variations in the observed prevalence and comparisons to the expected prevalence. Aging Ment Health 2011;15(8):978–84. [DOI] [PubMed] [Google Scholar]
- 72.Jean-Pierre P, Hendren S, Fiscella K, Loader S, Rousseau S, Schwartzbauer B, et al. Understanding the processes of patient navigation to reduce disparities in cancer care: perspectives of trained navigators from the field. J Cancer Educ 2011;26(1):111–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Paskett ED, Harrop JP, Wells KJ. Patient navigation: an update on the state of the science. CA Cancer J Clin 2011;61(4):237–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Riley S, Riley C. The role of patient navigation in improving the value of oncology care. J Clin Pathw 2016;2(1):41–7. [Google Scholar]
- 75.Valaitis RK, Carter N, Lam A, Nicholl J, Feather J, Cleghorn L. Implementation and maintenance of patient navigation programs linking primary care with community-based health and social services: a scoping literature review. BMC Health Serv Res 2017;17(1):116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Burgener SC, Buettner LL, Beattie E, Rose KM. Effectiveness of community-based, nonpharmacological interventions for early-stage dementia: conclusions and recommendations. J Gerontol Nurs 2009;35(3):50–7. [DOI] [PubMed] [Google Scholar]
- 77.Bartfay E, Bartfay W. The effects of adult day programs on the quality of life of individuals with Alzheimer’s disease: a pilot study. JMED Res 2014;2014:1–14. [Google Scholar]
- 78.Young R, Camic PM, Tischler V. The impact of community-based arts and health interventions on cognition in people with dementia: a systematic literature review. Aging Ment Health 2016;20(4):337–51. [DOI] [PubMed] [Google Scholar]
- 79.Bartfay E, Bartfay WJ. Quality-of-life outcomes among Alzheimer’s disease family caregivers following community-based intervention. West J Nurs Res 2013;35(1):98–116. [DOI] [PubMed] [Google Scholar]
- 80.Colvez A, Joël ME, Ponton-Sanchez A, Royer AC. Health status and work burden of Alzheimer patients’ informal caregivers. Health Policy 2002;60(3):219–33. [DOI] [PubMed] [Google Scholar]
- 81.Mittelman MS, Bartels SJ. Translating research into practice: case study of a community-based dementia caregiver intervention. Health Aff (Millwood) 2014;33(4):587–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Weir A, Fouche C. Community-based dementia day programmes: Common elements and outcome measures. Dementia 2017;16(3):297–314. [DOI] [PubMed] [Google Scholar]
- 83.Caldeira C, Bietz M, Vidauri M, Chen Y. Senior care for aging in place: balancing assistance and independence. In: Proceedings of the 2017 ACM Conference on Computer Supported Cooperative Work and Social Computing [internet]. Portland, Oregon: ACM; 2017 [cited 2021 Sep 9]. Available from: https://dl.acm.org/doi/10.1145/2998181.2998206.
- 84.Cowdell F. Care of older people with dementia in an acute hospital setting. Nurs Stand 2010;24(23):42–8. [DOI] [PubMed] [Google Scholar]
- 85.Digby R, Lee S, Williams A. Interviewing people with dementia in hospital: recommendations for researchers. J Clin Nurs 2016;25(7–8):1156–65. [DOI] [PubMed] [Google Scholar]
- 86.Garand L, Lingler JH, Conner KO, Dew MA. Diagnostic labels, stigma, and participation in research related to dementia and mild cognitive impairment. Res Gerontol Nurs 2009;2(2):112–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hansen EC, Hughes C, Routley G, Robinson AL. General practitioners’ experiences and understandings of diagnosing dementia: factors impacting on early diagnosis. Soc Sci Med 2008;67(11):1776–83. [DOI] [PubMed] [Google Scholar]
- 88.Pathak KP, Montgomery A. General practitioners’ knowledge, practices, and obstacles in the diagnosis and management of dementia. Aging Ment Health 2015;19(10):912–20. [DOI] [PubMed] [Google Scholar]
- 89.Teel CS. Rural practitioners’ experiences in dementia diagnosis and treatment. Aging Ment Health 2004;8(5):422–9. [DOI] [PubMed] [Google Scholar]
- 90.Iliffe S, Robinson L, Brayne C, Goodman C, Rait G, Manthorpe J, et al. Primary care and dementia: diagnosis, screening and disclosure. Int J Geriatr Psychiatry 2009;24(9):895–901. [DOI] [PubMed] [Google Scholar]
- 91.Burgener SC, Berger B. Measuring perceived stigma in persons with progressive neurological disease: Alzheimer’s dementia and Parkinson’s disease. Dementia 2008;7(1):31–53. [Google Scholar]
- 92.Devlin E, MacAskill S, Stead M. ‘We’re still the same people’: developing a mass media campaign to raise awareness and challenge the stigma of dementia. Int J Nonprofit Volunt Sect Mark 2007;12(1):47–58. [Google Scholar]
- 93.Mukadam N, Cooper C, Livingston G. A systematic review of ethnicity and pathways to care in dementia. Int J Geriatr Psychiatry 2011;26(1):12–20. [DOI] [PubMed] [Google Scholar]
- 94.Browne T, Darnell J, Estes Savage T, Brown A. Social workers as patient navigators: a review of the literature. Soc Work Res 2015;39(3):158–66. [Google Scholar]
- 95.Hancock GA, Woods B, Challis D, Orrell M. The needs of older people with dementia in residential care. Int J Geriatr Psychiatry 2006;21(1):43–9. [DOI] [PubMed] [Google Scholar]
- 96.Polacsek M, Goh A, Malta S, Hallam B, Gahan L, Cooper C, et al. ‘I know they are not trained in dementia’: addressing the need for specialist dementia training for home care workers. Health Soc Care Community 2020;28(2):475–84. [DOI] [PubMed] [Google Scholar]
- 97.Geriatrics Interdisciplinary Advisory Group. interdisciplinary care for older adults with complex needs: American Geriatrics Society Position Statement: special article. J Am Geriatr Soc 2006;54(5):849–52. [DOI] [PubMed] [Google Scholar]
- 98.Chapman DG, Toseland RW. Effectiveness of advanced illness care teams for nursing home residents with dementia. Soc Work 2007;52(4):321–9. [DOI] [PubMed] [Google Scholar]
- 99.Griffiths P, Bridges J, Sheldon H, Thompson R. The role of the dementia specialist nurse in acute care: a scoping review. J Clin Nurs 2015;24(9–10):1394–405. [DOI] [PubMed] [Google Scholar]
- 100.Reid AE, Doucet S, Luke A. Exploring the role of lay and professional patient navigators in Canada. J Health Serv Res Policy 2020;25(4):229–37. [DOI] [PubMed] [Google Scholar]
- 101.Pedersen AE, Hack TF. The British Columbia patient navigation model: a critical analysis. Oncol Nurs Forum 2011;38(2):200–6. [DOI] [PubMed] [Google Scholar]
- 102.Fillion L, Serres M, de, Lapointe-Goupil R, Bairati I, Gagnon P, Deschamps M, et al. Implementing the role of patient-navigator nurse at a university hospital centre. Can Oncol Nurs J 2006;16(1):11–7. [DOI] [PubMed] [Google Scholar]
- 103.Dohan D, Schrag D. Using navigators to improve care of underserved patients. Cancer 2005;104(4):848–55. [DOI] [PubMed] [Google Scholar]
- 104.Anderson J, Larke S. The Sooke Navigator project: using community resources and research to improve local service for mental health and addictions. Ment Health Fam Med 2009;6:21–8. [PMC free article] [PubMed] [Google Scholar]
- 105.Bayly M, Morgan D, Chow AF, Kosteniuk J, Elliot V. Dementia-related education and support service availability, accessibility, and use in rural areas: barriers and solutions. Can J Aging Rev Can Vieil 2020;39(4):545–85. [DOI] [PubMed] [Google Scholar]
- 106.Pierse T, Keogh F, O’Shea E, Cullinan J. Geographic availability and accessibility of day care services for people with dementia in Ireland. BMC Health Serv Res 2020;20(1):476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ferrante JM, Wu J, Dicicco-Bloom B. Strategies used and challenges faced by a breast cancer patient navigator in an urban underserved community. J Natl Med Assoc 2011;103(8):729–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hiestand S. A qualitative analysis of four Appalachian cervical cancer patient navigators interviews [internet]. Theses Diss--Public Health MPH DrPH; 2015. [cited 2021 Sep 7]. Available from: https://uknowledge.uky.edu/cph_etds/56. [Google Scholar]
- 109.Roland KB, Higa DH, Leighton CA, Mizuno Y, DeLuca JB, Koenig LJ. HIV patient navigation in the United States: a qualitative meta-synthesis of navigators’ experiences. Health Promot Pract 2022;23(1):74–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Spiro A, Oo SA, Marable D, Collins JP. A unique model of the community health worker: the MGH Chelsea Community Health Improvement Team. Fam Community Health 2012;35(2):147–60. [DOI] [PubMed] [Google Scholar]
- 111.McCann TV, Clark E. Adopting care provider–facilitator roles: community mental health nurses and young adults with an early episode of schizophrenia. Soc Theory Health 2005;3(1):39–60. [Google Scholar]
- 112.Mullins CD, Shaya FT, Blatt L, Saunders E. A qualitative evaluation of a citywide community health partnership program. J Natl Med Assoc 2012;104(1):53–60. [DOI] [PubMed] [Google Scholar]
- 113.Braun KL, Kagawa-Singer M, Holden AEC, Burhansstipanov L, Tran JH, Seals BF, et al. Cancer patient navigator tasks across the cancer care continuum. J Health Care Poor Underserved 2012;23(1):398–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Boyd CM, Boult C, Shadmi E, Leff B, Brager R, Dunbar L, et al. Guided care for multimorbid older adults. Gerontologist 2007;47(5):697–704. [DOI] [PubMed] [Google Scholar]
- 115.Giddens JF, Tanner E, Frey K, Reider L, Boult C. Expanding the gerontological nursing role in guided care. Geriatr Nur (Lond) 2009;30(5):358–64. [DOI] [PubMed] [Google Scholar]
- 116.Palinkas LA, Ell K, Hansen M, Cabassa L, Wells A. Sustainability of collaborative care interventions in primary care settings. J Soc Work 2011;11(1):99–117. [Google Scholar]
- 117.Black SE, Gauthier S, Dalziel W, Keren R, Correia J, Hew H, et al. Canadian Alzheimer’s disease caregiver survey: baby-boomer caregivers and burden of care. Int J Geriatr Psychiatry 2010;25(8):807–13. [DOI] [PubMed] [Google Scholar]


