Abstract
Antibiotics are recognized widely for their benefits when used appropriately. However, they are often used inappropriately despite the importance of responsible use within good clinical practice. Effective antibiotic treatment is an essential component of universal healthcare, and it is a global responsibility to ensure appropriate use. Currently, pharmaceutical companies have little incentive to develop new antibiotics due to scientific, regulatory, and financial barriers, further emphasizing the importance of appropriate antibiotic use. To address this issue, the Global Alliance for Infections in Surgery established an international multidisciplinary task force of 295 experts from 115 countries with different backgrounds. The task force developed a position statement called WARNING (Worldwide Antimicrobial Resistance National/International Network Group) aimed at raising awareness of antimicrobial resistance and improving antibiotic prescribing practices worldwide. The statement outlined is 10 axioms, or “golden rules,” for the appropriate use of antibiotics that all healthcare workers should consistently adhere in clinical practice.
Keywords: Antibiotic therapy, Antimicrobial resistance, Antimicrobial stewardship programs, Hospital-acquired infections, Infection prevention and control, Systemic antibiotic prophylaxis, Surgical site infections
Introduction
Antibiotics are essential and life-saving medicines. However, improper use is pervasive. Ensuring appropriate antibiotic prescribing is a fundamental aspect of good clinical practice [1]. Since Sir Alexander Fleming's discovery of penicillin in 1928, antibiotics have revolutionized medicine and been instrumental in saving countless lives [2].
There are also substantial disparities in antibiotic usage worldwide. Whereas some regions face the challenge of excessive antibiotic use, other areas suffer from limited access to essential antibiotics [3]. This concerning disparity creates a gap that jeopardizes the sustainability and safety of global antibiotic supplies, ultimately compromising access to effective treatments and leading to suboptimal prescription practices [4].
Effective antibiotic treatment is an essential component of universal healthcare. There is a global collective responsibility to use antibiotics appropriately to maintain their effectiveness. Pharmaceutical companies have few incentives to develop new antibiotics due to numerous scientific, regulatory, and financial barriers [5–8]. Thus, it is questionable whether industry will replace ineffective antibiotics in time.
Antibiotics are used commonly in acute care hospitals for the treatment of both community- and hospital-acquired infections (HAIs), as well as for surgical prophylaxis [9]. However, when prescribed incorrectly, antibiotics offer little benefit to patients while exposing them to risks of adverse effects [10]. Studies have demonstrated that adverse events are associated with antibiotic therapy in up to 20% of patients receiving systemic treatment [11, 12]. These events, in turn, can prolong hospitalizations, cause additional clinic or emergency department visits and hospital re-admissions, and result in a need for additional hospital services [13] that increase hospital cost [14].
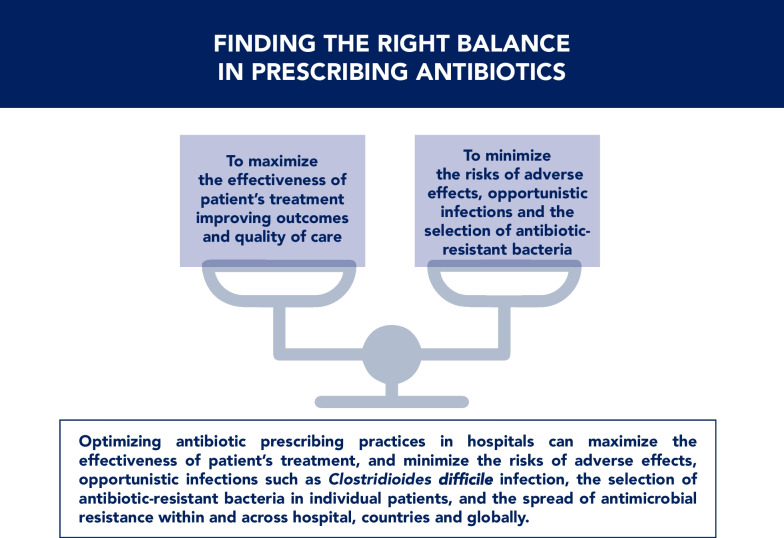
Optimizing inpatient antibiotic prescribing results in improved treatment effectiveness and patient safety, minimizes the risk of antibiotic-associated infections (e.g., Clostridioides difficile infection: [CDI]) and the selection and transmission of antimicrobial-resistant bacteria in individual patients within and across hospitals, countries, and globally [15].
We propose that clinical leaders drive antimicrobial stewardship and education programs to help standardize and improve prescribing behaviors. Furthermore, we argue that guidance on the appropriate use of antibiotics from clinical leaders within a specialty is vital to address the global threat of antimicrobial resistance (AMR).
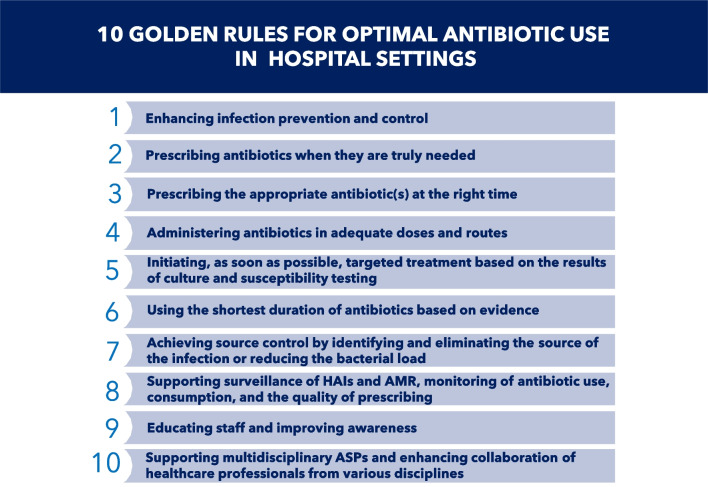
We present 10 core principles for the appropriate use of antibiotics, which clinicians should always follow in their clinical practice (Fig. 1).
Fig. 1.
The 10 “golden rules” for optimal antibiotic use in hospital settings, which clinicians should always follow in their clinical practice
Methods
In January 2023, the Global Alliance for Infections in Surgery [16] established an international multidisciplinary task force with the aim of developing a shared vision regarding the need for appropriate antibiotic use in hospital settings to address the threat of AMR in particular antibacterial resistance. Two hundred and ninety-five experts from 115 countries on six continents participated, including specialists in anesthesiology, clinical pharmacology, critical care medicine, emergency medicine, epidemiology, global health, health policy and management, hospital pharmacy, infection prevention and control, infectious diseases, internal medicine, microbiology, nursing, public health, and emergency and general surgery.
Supporting documentation was identified through comprehensive searches conducted using PubMed and Google Scholar. The search identified articles published in English between January 2000 and February 2023. Two experts, who collaborated in drafting the initial manuscript, reviewed the selected articles. Subsequently, the first version was shared with the experts’ group and was revised with the incorporation of additional references. The final document was reviewed thoroughly by each task force member to ensure accuracy, timeliness, and consensus. The project has been named WARNING (Worldwide Antimicrobial Resistance National/International Network Group) (Fig. 2).
Fig. 2.
Worldwide Antibiotic Resistance National/International Network Group (WARNING)
By adhering to the 10 core principles described, healthcare professionals in hospital (and community) settings can support responsible and effective antibiotic use, mitigate the risks of adverse effects and AMR, and promote better patient outcomes in their clinical practices. To enhance awareness and promote best practices, we developed impactful iconography that conveys salient messaging, facilitates implementation, and enhances the retention and application of recommended principles and practices.
The global burden of antimicrobial resistance (AMR)
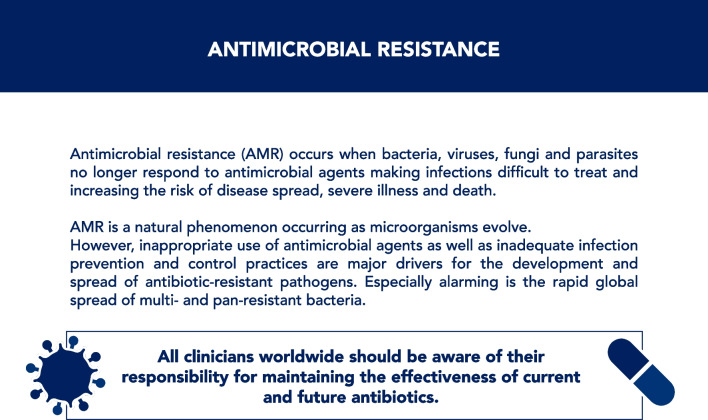
AMR occurs as bacteria, viruses, fungi, and parasites evolve antimicrobial defense mechanisms that reduce treatment efficacy and increase the risk of treatment failure, disease progression, severe illness, or death. However, misuse and overuse of antimicrobial agents, combined with ineffective infection prevention and control (IPC) practices, are recognized as major drivers of the increasing prevalence of AMR [1] (Fig. 3).
Fig. 3.
Antimicrobial resistance
Although antibiotic-resistant infections are a recognized public health threat, and this call to action addresses the appropriate use of antibacterial agents, less is known about the burden of AMR fungal infections [1]. Fungal infections are increasing in frequency, largely because of the increasing size of the population at risk, which includes persons with cancer, those requiring transplants, persons living with human immunodeficiency virus infection or who are immunosuppressed due to disease or therapy, and critically ill patients. Invasive fungal infections are associated with considerable morbidity and death.
Recently, Candida auris has emerged worldwide as a multidrug-resistant (MDR) pathogen [17–19] whose high transmissibility, broad-spectrum clinical manifestations, and potentially high mortality have led the US Centers for Disease Control and Prevention (CDC) to classify it as one of five pathogens in its Urgent Threats category [20]. Data published recently by the CDC highlight that C. auris is spreading at an alarming rate [21] since it was first described in 2009 [22] as an invasive infection [23]. Infections due to C. auris have increased to the point of higher prevalence than the common fungal pathogen, C. albicans, at some centers [24]. Candida auris is uniquely challenging due to five factors: high transmissibility leading to widespread outbreaks in numerous hospitals worldwide [25, 26]; a broad spectrum of clinical manifestations associated with a mortality rate as high as 70% [26, 27]; environmental hardiness, including persistence for weeks on dry surfaces [28, 29]; difficulty identifying C. auris by microbiology laboratories [29]; and a high rate of MDR and therapeutic failure [28, 30–32]. The environmental fitness of C. auris is associated with biofilm formation and production of proteinases and phospholipases [27, 33], in addition to environmental stress resistance and antifungal drug resistance.
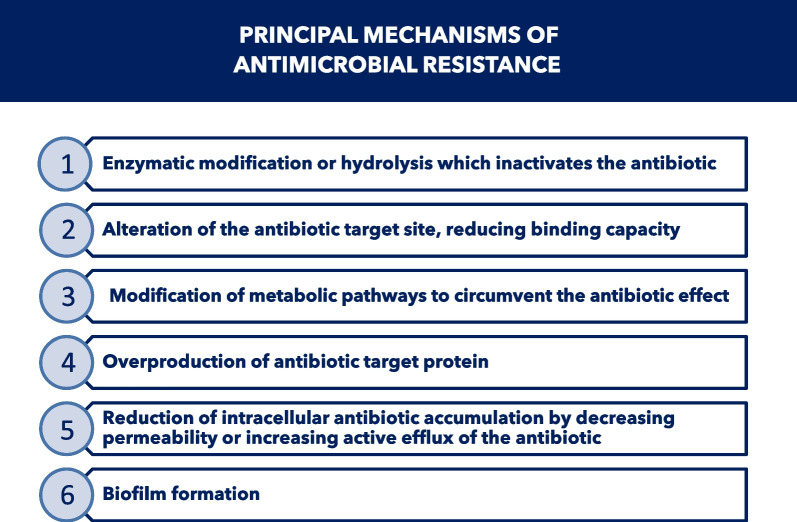
Bacteria may be intrinsically resistant to one or more classes of antibiotics or may acquire such resistance. Bacteria have developed different resistance mechanisms to avoid antibiotic action (Fig. 4). In addition to intrinsic resistance mechanisms, bacterial pathogens can acquire resistance to antibiotics through either mutation of existing genes [34], or by acquiring new genes from other strains or species through horizontal gene transfer [34].
Fig. 4.
Principal mechanisms of antimicrobial resistance
“Heteroresistance” describes the presence of subpopulations of bacterial cells with higher levels of antibiotic resistance than those of the rest of the population in the same culture [35]. Recent work indicates that heteroresistance is very common for several different bacterial species and antibiotic classes. The resistance phenotype is often unstable, and in the absence of antibiotic pressure, it can rapidly revert to susceptibility [36]. Heteroresistance occurs in both Gram-positive and Gram-negative bacteria. Its clinical relevance may be considerable, since more resistant subpopulations may be selected during antibiotic therapy. However, the use of nonstandard methods to define heteroresistance, which are costly and involve considerable labor and resources, precludes evaluating the clinical magnitude and severity of this phenomenon [35]. Since heteroresistance may have serious implications in antibiotic therapy, the development of standardized criteria and protocols for detecting and measuring heteroresistance is essential.
Infections caused by AMR bacteria pose a global challenge [37]. In 2008, the “ESKAPE” acronym was coined to name those bacteria that may “escape” the effects of antibiotics including Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii-calcoaceticus complex, Pseudomonas aeruginosa, and Enterobacter spp. [38]. The list of AMR bacteria is no longer up-to-date, as Escherichia coli, Mycobacterium tuberculosis and Neisseria gonorrhoeae are currently among the most prevalent bacterial pathogens affected by AMR issues.
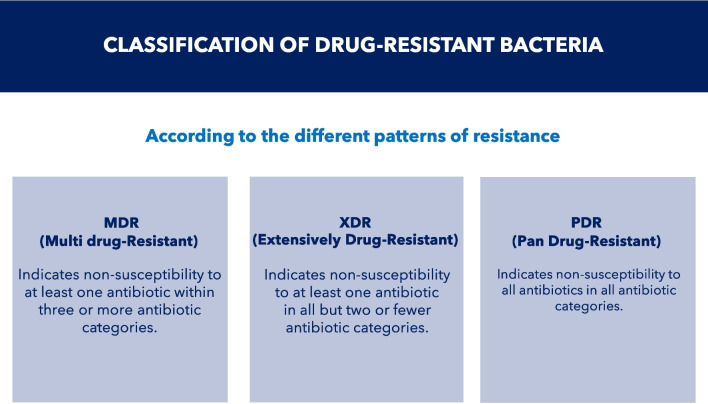
In 2012, the European Centre for Disease Prevention and Control (ECDC) and the CDC developed standardized nomenclature to describe acquired resistance profiles in bacteria [39]. MDR was defined as acquired non-susceptibility to at least one antibiotic in three or more antibiotic classes (e.g., cephalosporins, fluoroquinolones, tetracyclines). Extensively drug-resistant (XDR) bacteria were defined as non-susceptibility to at least one antibiotic in all but two or fewer antibiotic classes (bacterial isolates remain susceptible to only one or two classes). Pandrug-resistant (PDR) bacteria were defined as non-susceptibility to all antibiotics in all antibiotic classes (Fig. 5). These classifications provide a standardized nomenclature for categorizing and communicating resistance patterns of bacteria, aiding in surveillance, research, and the development of appropriate tactics to combat AMR [40]. Kadri et al. [41] proposed a new category of Gram-negative bacteremia, that is difficult-to-treat, based on non-susceptibility to “first-line” antibiotics, generally beta-lactams or fluoroquinolones, that necessitates the use of second-line, often more toxic, agents.
Fig. 5.
Classification of drug-resistant bacteria
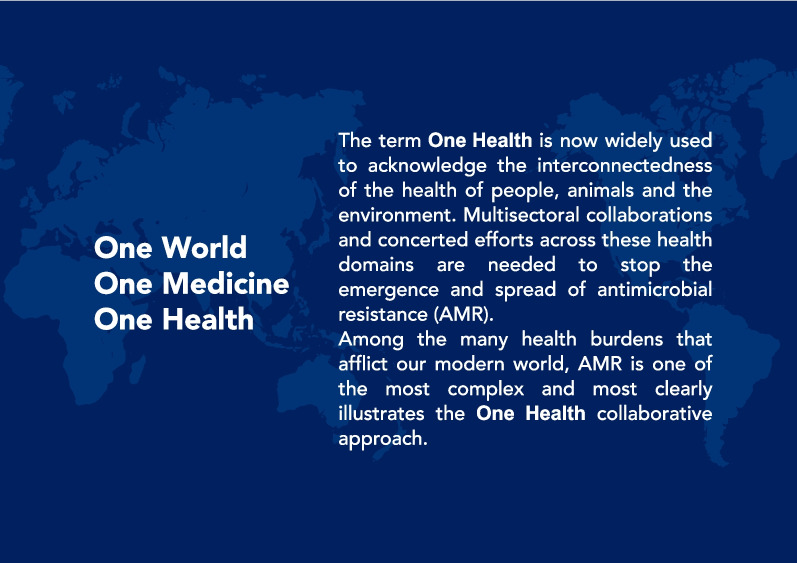
AMR is a complex and multifaceted issue that involves not only humans, but also animals and the environment [42, 43]. On March 17, 2022, four international agencies, the Food and Agriculture Organization of the United Nations (FAO), the World Organization for Animal Health (WOAH), the UN Environment Programme (UNEP), and the World Health Organization (WHO), signed a groundbreaking agreement to strengthen cooperation and promote sustainable practices that balance and optimize the health of humans, animals, plants and the environment. The concept of "One Health" recognizes the interconnectedness of the health of people, domestic animals, and the environment [44]. Multisectoral collaborations and concerted global efforts across multiple health domains are needed to tackle AMR [45–48] (Fig. 6).
Fig. 6.
One Health
In 2015, the WHO published the Global Action Plan on Antimicrobial Resistance [49]. Its five goals include: Improving awareness and understanding of AMR through effective communication, education, and training; strengthening knowledge through surveillance and research; preventing infection through effective sanitation, hygiene, and IPC measures; optimizing the use of antibiotics in human and animal health; and increasing investment in new drugs, diagnostic tools, vaccines, and other interventions. Member states committed to develop national action plans (NAPs) on AMR, which should be comprehensive, funded, and implemented with monitoring so that lessons learned can reshape priorities. Inter-country variability in economic and political resilience, and resource constraints, constitute a considerable barrier to implementation of the NAPs [50, 51]. Despite the strong commitment to addressing AMR, endorsement and implementation of NAPs have also been impeded by the prioritization of issues related to the coronavirus disease-2019 (COVID-19) pandemic [52].
There is increasing evidence that the pandemic accelerated the emergence and spread of AMR at least in hospital settings [53] particularly Acientobacter spp. Langford et al. reported that more than 60% of patients with COVID-19 who had a bacterial infection harbored a highly resistant organism [54]. However, multiple limitations intrinsic to the interpretation of COVID-19 data prevent accurate quantification of its impact on the global epidemiology of AMR [55, 56].
Alarming levels of AMR have been reported in all countries, regardless of their average income level [57]. The 2019 pre-pandemic analysis, published in 2022 by Murray et al. [57], revealed AMR as a leading cause of death worldwide (204 countries and territories) with 4.95 million estimated deaths associated with bacterial AMR, including 1.27 million deaths attributable directly to bacterial AMR. Among the 23 bacteria studied, six (E. coli, S. aureus, K. pneumoniae, S. pneumoniae, A. baumannii, and P. aeruginosa) were found to be responsible for 929,000 deaths due to AMR and 3.57 million deaths total. Notably, methicillin-resistant S. aureus (MRSA) alone caused more than 100,000 deaths in 2019. AMR bacterial infections were associated with the highest infection-related mortality rates in sub-Saharan Africa, with 99 deaths/100,000 people. By comparison, in high-income countries, AMR was associated with 56 deaths/100,000 individuals. However, Murray et al. may have underestimated the true burden of AMR [58]. Modern medical therapies, including trauma care, oncologic surgical interventions and chemotherapy, organ transplantation, and other invasive procedures, require effective antibiotics to prevent and treat infection. Untreatable infections reduce the value of these medical interventions by impacting efficacy adversely, although this is difficult to quantify [58].
The true burden of AMR in low- and middle-income countries (LMICs) would remain unknown unless surveillance is resourced adequately [59]. In particular, bacterial identification and susceptibility testing are not performed routinely in LMICs, owing to a lack of personnel, equipment, and supplies; moreover, testing may represent an out-of-pocket expense for patients in some healthcare systems [60]. As a result, antibiotic therapy is mostly empiric and broad-spectrum antibiotics may be misdirected. The resultant suboptimal care of infections can lead to clinical failure, higher mortality, and increased AMR. Some progress has been made in LMICs over the last decade regarding data collection to inform AMR, and monitoring of antibiotic use. However, more must be done.
The COVID-19 pandemic has demonstrated that morbidity and mortality from infectious diseases disproportionately impact upon certain populations [61]. The measures recommended to control the spread of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), including social distancing and frequent hand washing, pose challenges for those living in densely populated communities with inadequate housing, poor sanitation, and limited access to clean water. The poorest people are particularly vulnerable to the threat of AMR, as poverty increases the risk of contracting infectious diseases and being exposed to antibiotics. A 2018 systematic review by Alividza et al. [62] highlighted the complex relationship between AMR and various dimensions of poverty, including education level, income, and housing and water quality. Addressing these disparities will be crucial for reducing the burden of AMR and improving public health outcomes in vulnerable communities.
An important report from India (the ‘Chennai Declaration’) was published in November 2012, representing a major national step forward as a landmark commitment to antibiotic stewardship, with international importance and global implications [63]. Although there has been a national antibiotic policy in India since 2011, the recommendations were difficult to implement owing to a lack of a clear plan of action. The lack of impact of such a well-intentioned but difficult-to-implement policy gave rise in August 2012 to a meeting of Indian medical societies and national authorities to develop a ‘roadmap’ outlining the urgent actions required. The final declaration was released in November 2012. The effort represents an extraordinary example of national consensus and commitment that recognizes the clinical and public health issues of AMR.
Recognizing the gravity of AMR, the United Kingdom commissioned in 2014 a comprehensive analysis of this global problem [64]. The stunning finding of this report was that, provided no action was taken, AMR would result in as many as 10 million deaths by 2050. Separately, the World Bank warned that "in the high AMR-impact scenario, an additional 24 million people could be pushed into extreme poverty by 2030" [65]. Although there is undoubtedly a large clinical and public health burden associated with AMR, it is challenging to quantify the associated excess morbidity and mortality. Detailed, reliable data, preferably based on comprehensive, population-based surveillance from LMICs and high-income countries [66] will be needed to enhance AMR control measures.
In 2022, the Group of Seven (G7; Canada, France, Germany, Italy, Japan, UK, USA) issued the G7 Health Ministers’ Declaration [67]. Their communiqué covered a range of topics but focused on four priority areas: (1) overcoming COVID-19; (2) future pandemic preparedness; (3) AMR; (4) and health risks from climate change [67]. In a subsequent communiqué, the G7 health ministers called AMR an "urgent public health and socio-economic problem" that may have global effects but could have a greater impact on LMICs. Acknowledging AMR as a shared responsibility, they committed together to "taking further urgent and tangible action" to address the issue. Among the actions, they pledged to establish new or improved national integrated surveillance systems on AMR and antibiotic use in human beings, animal husbandry, farming, and environmental sectors; promotion of appropriate antimicrobial use through stewardship; strengthening implementation of IPC programs across the One Health spectrum; and strengthening the research and development pipeline for new antibiotics. This approach aims to achieve optimal health outcomes for people, animals, and the environment, while considering the diverse socioeconomic, political, and cultural contexts affecting AMR [68], including limited technical expertise, insufficient clinical and research laboratory infrastructure, other financial constraints, and necessary political commitment [69]. As effective antibiotics are a global public good on the verge of scarcity, AMR is rightly considered a serious threat [70]. Preserving antibiotics is a collective responsibility [8, 71].
On 13 June 2023, the European Council adopted a resolution calling for stronger EU action to combat AMR in human and animal health and the environment, employing a 'One Health' approach to AMR. The resolution encourages the prudent use of antimicrobial agents in human and animal health through a series of voluntary measures, with the aim of reducing AMR [72].
Antibiotic use in the hospital and community setting
Healthcare workers (HCWs) play a crucial role in combatting AMR [1]. Unfortunately, antibiotics are often prescribed inappropriately in human and animal health settings [73]. When prescribing antibiotics, understanding the differences among prophylactic, empiric, and targeted therapy can help ensure appropriate use and help prevent the development of AMR. Antibiotic prophylaxis refers to the antibiotic administration to patients without signs of infection, in order to prevent its occurrence. Empiric antibiotic therapy is prescribed to treat known or suspected infections based on the patient's symptoms and likely causative pathogens before definitive diagnostic test results, including antibiotic susceptibility testing, are available. Targeted antibiotic therapy is initiated based on microbial identification and susceptibility test results to identify the specific pathogen and ensure that the most effective (ideally, also the most cost-effective), least toxic, and narrowest spectrum antibiotic is used as therapy. Optimal targeted therapy requires early identification and characterization of bacteria. However, despite advancements in rapid microbial diagnostics, the turnaround time for microbiologic testing and reporting can still take up to 72 h, if it is available at all. As a result, clinicians often initiate empiric antibiotic therapies that can have negative consequences for patients' health and exacerbate the risk of AMR [74].
Although antibiotic decision-making is reported to be driven by different determinants in medical versus surgical settings [75], hospital antibiotic prescribing practices are often inadequate worldwide [76]. A point-prevalence survey of 33 hospitals in five Latin American countries (Cuba, El Salvador, Mexico, Paraguay and Peru) documented adherence to prescribing guidelines in 68.6% of cases. Third-generation cephalosporins were the most frequently prescribed antibiotic class (26.8%), followed by carbapenems (10.3%) and fluoroquinolones (8%). Targeted therapy was achieved in only 17.3% of cases [77].
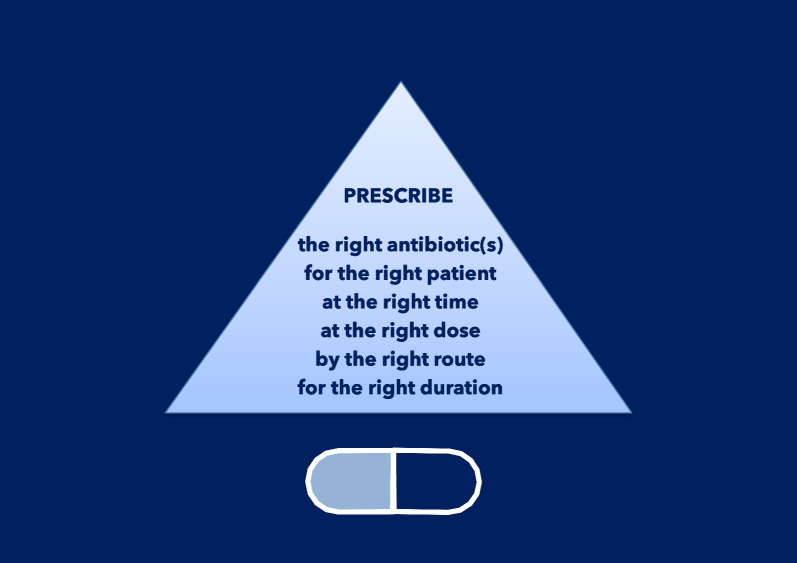
All clinicians must strive for improvement by incorporating antibiotic stewardship principles into daily practice [78]. Antimicrobial stewardship programs (ASPs) [79–81] should be integrated into all hospitals’ quality improvement programs worldwide. ASPs promote responsible antibiotic use by improving the diagnostic decision-making process (now called diagnostic stewardship); emphasizing the importance of prescribing antibiotics only when needed; to the right patient and clinical situation, at the right time, in the right dose and interval, and for the correct duration [82–84]. ASPs also play a vital role in increasing awareness of HCWs and community members regarding AMR [85, 86]. Diagnostic stewardship is an integral part of ASPs and emphasizes the importance of selecting the right diagnostic tests for the right patient at the right time [87], encouraging the use of rapid molecular diagnostics to initiate targeted antibiotic therapy as soon as possible while avoiding excessive use of broad-spectrum antibiotics when not (or no longer) needed. However, equally important is accurate interpretation of test results to prevent overdiagnosis and unnecessary cost [88], and improving the diagnostic decision-making process overall, integrating all needed information (clinical, biologic, imaging).
Although 15 years have passed since the CDC, the Society for Healthcare Epidemiology of America (SHEA), and the Infectious Diseases Society of America (IDSA) published joint guidelines for the development of institutional ASPs, best practices for ASPs are still being defined and are likely to vary based on local practice patterns, policy, and available resources [89]. The preferred means of improving antimicrobial stewardship include a comprehensive program that incorporates collaboration among specialists and support staff within an institution. In this context, the direct involvement of all prescribers in ASPs can be highly impactful [90].
Thus, we present the following 10 principles for the appropriate use of antibiotics. These principles should be adhered to by all HCWs in their clinical practices, and they should be considered as core components of activity within ASPs.
Enhancing infection prevention and control (IPC)
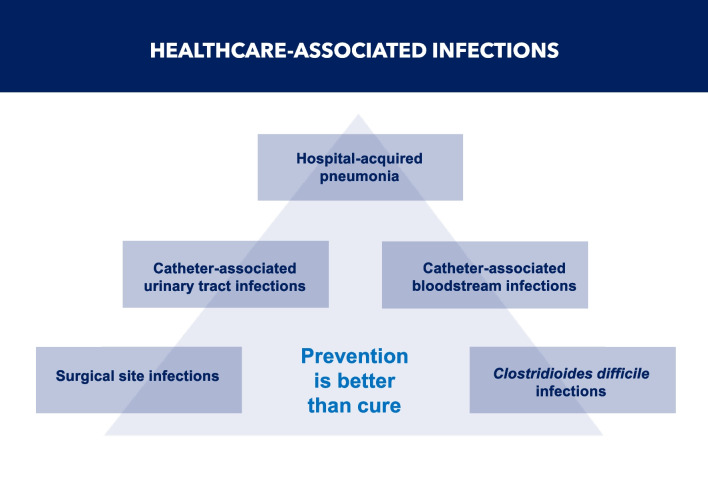
It is crucial for all HCWs to adhere to evidence-based measures of IPC to prevent the occurrence of HAIs. Effective IPC education and training significantly reduce HAIs [91–94], the most common of which are surgical site infections (SSIs), catheter-associated urinary tract infections, central line-associated blood stream infections, hospital- and ventilator-associated pneumonia (VAP), and CDI [95] (Fig. 7).
Fig. 7.
Healthcare-associated infections
Patients with HAIs require additional diagnostic and therapeutic procedures, have prolonged hospital stays, incur additional costs, and may have high morbidity and mortality. Moreover, many HAIs are caused by MDR bacteria [96, 97]. In the contexts of quality care and mitigation of AMR, preventing HAIs becomes increasingly important. These infections are associated with worse outcomes and often require broad-spectrum antibiotics [98]. According to the ECDC, the burden of the six major types of HAIs in the European Union/European Economic Area, expressed in disability-adjusted life years, was higher than the combined burden of all 32 other communicable diseases surveilled by the ECDC based on data from 2011 to 2012 [99].
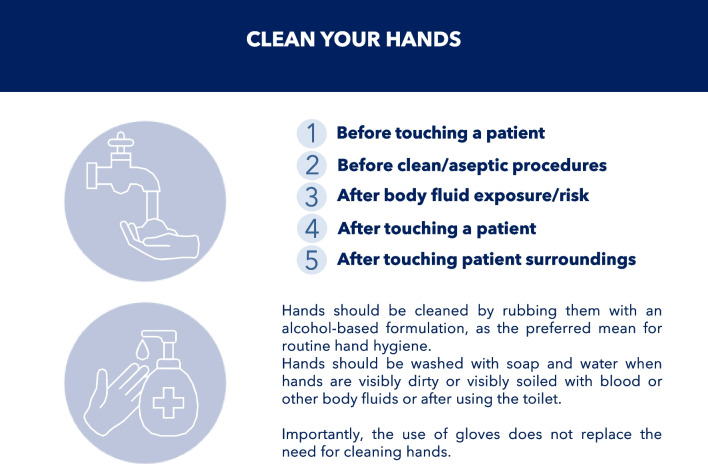
Many HAIs are preventable. A reduction in HAI rates of 35–55% has been documented by implementing multimodal prevention and developing a safety-oriented approach, regardless of the countries’ income levels [100]. Despite this, HCWs adhere poorly to evidence-based IPC measures [95]. A prominent example is hand hygiene, considered an indicator of patient safety and quality of care and the cornerstone of IPC in all healthcare settings. Numerous organizations, including WHO [101] and CDC [102], have published guidelines providing HCWs with specific recommendations to improve hand hygiene practices. Recently, SHEA, IDSA, and the Association for Professionals in Infection Control and Epidemiology (APIC) published practice recommendations for the prevention of HAIs through hand hygiene [103]. The Five Moments for Hand Hygiene were promulgated by WHO to encourage HCW adherence to hand hygiene recommendations and minimize the risk of infection and transmission [104] (Fig. 8).
Fig. 8.
The five moments for hand hygiene
Although hand hygiene is accepted universally as a cost-effective IPC measure, compliance remains unacceptably low. In a systematic review [105], reported compliance was ~ 40% (compared with the WHO benchmark rate of > 80%) and was variable across hospital units/wards and HCWs, calling for multifaceted mitigation activities to foster concordance. All HCWs involved in direct or indirect patient care should recognize the importance of hand hygiene and the need to perform it without fail. Hand hygiene at the point of care is recognized as a best practice for promoting compliance at the moments when hand hygiene is most crucial. According to current best practice, hand hygiene products should be available at the point of care. This requires that a hand hygiene product be easily accessible and as close as possible—ideally within arm’s reach of where patient care or treatment is taking place [106].
SSIs remain the most common HAIs among surgical patients. They represent a major clinical problem in terms of morbidity, mortality, length of hospital stay, and overall direct and indirect costs worldwide. It is obviously important to improve patient safety by acting before, during, and after surgery to reduce the occurrence of SSIs [107–109].
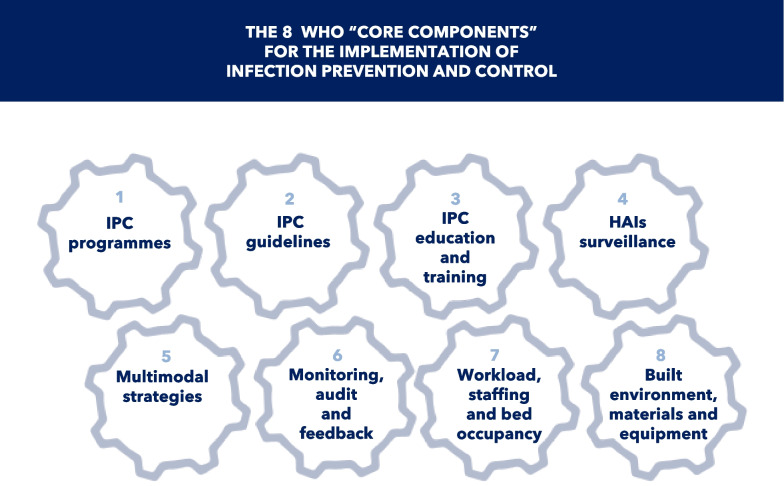
In 2016, WHO published evidence-based guidelines on the core components of effective IPC programs, to be implemented both at the national and hospital levels [110, 111]. IPC measures were summarized in eight “core components” (Fig. 9). Since the landmark Study on the Efficacy of Nosocomial Infection Control (SENIC) program in the 1970s [112] revealed the effectiveness of an IPC program in reducing HAIs, a dedicated IPC program is considered of paramount importance in every hospital. It should be led by experts in IPC, in close collaboration with HCWs in all relevant areas [113].
Fig. 9.
The 8 WHO “core components” for the implementation of infection prevention and control
Results of a WHO global survey designed to assess implementation of these programs in healthcare facilities worldwide have been published. This survey provides an important overview of IPC program implementation in 4440 healthcare facilities (81 countries) across all six WHO regions and income levels. The findings identify strengths, gaps in IPC implementation, and key opportunities for improvement to inform ongoing global IPC improvement efforts, particularly in LMICs, which showed significantly lower IPC implementation [114].
With the common goal of reducing AMR, IPC programs and ASPs should be partners in reducing HAIs. Support from institutional leadership is crucial for the success of each program and both together, including an effective microbiology laboratory (capacity, funding, and infrastructure) to enable rapid diagnosis, effective communication tools, and appropriate use of technology, including electronic health records. IPC and ASP programs are based on similar models of interdisciplinary work and activities such as education, monitoring, and feedback. Integrating these interventions may reduce redundancy and align forces for maximal influence on HCWs. ASPs, when implemented in concert with IPC interventions in hospitals, particularly hand hygiene, are significantly more effective in reducing the development and spread of MDR bacteria than ASPs alone [115].
Containing the spread of antibiotic-resistant bacteria is challenging because of their propensity for human-to-human transmission [116]. Carbapenem-resistant Enterobacterales (CRE), A. baumannii (CRAB), and P. aeruginosa (CRPA) are among the most difficult-to-treat bacteria due to a high prevalence of AMR. In 2017, the WHO published guidelines for the prevention and control of these bacteria in acute healthcare facilities [117]. The supporting systematic literature review was published in 2019 [118]. The most frequent interventions reported were contact precautions (90%); active surveillance cultures (80%); monitoring, audit, and feedback of measures (80%); patient isolation or cohorting (70%); hand hygiene (50%); and environmental cleaning (40%).
Vaccination deserves mention as one of the most impactful and cost-effective prevention measures. Vaccines are mostly used prophylactically, including post-exposure prophylaxis, to decrease the number of infectious disease cases, and thus antibiotic use and the propagation of AMR. Vaccines are also being developed against resistant bacterial pathogens that cause a substantial disease burden [119] such as MRSA and P. aeruginosa [120, 121]. Vaccines are commonly considered to impact AMR, either directly by preventing infection, thereby reducing the prevalence of the resistant pathogen and also antibiotic use, or indirectly by preventing non-bacterial primary infections (e.g., viral), which are often treated incorrectly with antibiotics [119]. Haemophilus influenzae serotype B (HiB), influenza, and pneumococcal conjugate vaccines are examples demonstrating the effectiveness of vaccines in reducing antibiotic use and reducing AMR [122–124]. Specific to surgery, vaccination against S. pneumoniae (which is increasingly resistant to penicillin), HiB, and Neisseria meningitidis following splenectomy is effective in preventing overwhelming post-splenectomy infection that is usually caused by encapsulated organisms [125]. Moreover, immunization against measles prevents measles virus infection, which infection reduces preexisting antibodies offering protection from other pathogens [126]. New vaccines are under development and evaluation, offering possibilities to address life-threatening diseases and help further curb antibiotic use and mitigate AMR [127].
Prescribing antibiotics when they are truly needed
Clinicians prescribing antibiotics are faced with conflicting priorities. On the one hand, they must provide patients with the best possible treatment. On the other hand, they must preserve the efficacy of antibiotics, minimize opportunistic infections such as CDI, reduce the selection of resistant pathogens in individual patients, and prevent the continued global increase of AMR. These conflicts should be evaluated and balanced before prescribing antibiotics [34] (Fig. 10).
Fig. 10.
Finding the right balance in prescribing antibiotics
The intestinal microbiota has an important role in human health and can protect the patient against colonizing enteric bacteria [128], a phenomenon known as colonization resistance. The indigenous bacteria of the microbiome provide an important host defense mechanism by inhibiting colonization by potentially pathogenic bacteria. However, in certain circumstances, a patient’s microbiota can be compromised, no longer protecting against colonization by opportunists.
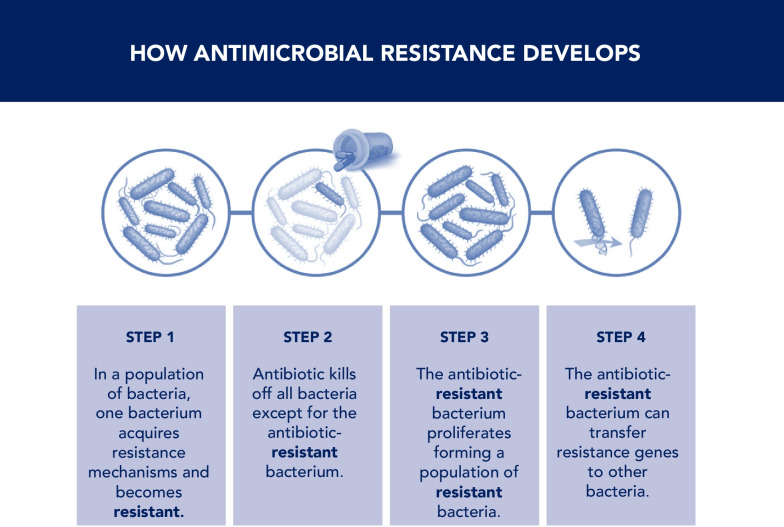
Antibiotics exert selection pressure on the human microbiome, predisposing to AMR. Antibiotic use can have unintended consequences on commensal intestinal microbiota. Whereas susceptible bacteria are destroyed, the resultant ecologic vacuum promotes the overgrowth of pathogenic bacteria that may already be antibiotic-resistant [129, 130]. Moreover, antibiotics facilitate the transmission of resistance genes conferring resistance to other bacteria [131, 132] (Fig. 11), thereby increasing the risks of cross-transmission between patients [133, 134] and outbreaks of infections caused by MDR bacteria.
Fig. 11.
How antimicrobial resistance develops
Many studies have evaluated the long‐term effect on gut microbiota following a course of antibiotics [135–137]. To demonstrate the long-term effects of antibiotics on the healthy microbiome, the effects of amoxicillin (500 mg) thrice daily for 5 days [138], ciprofloxacin (500 mg) twice daily for 5 days [139], and (second-generation cephalosporin) cefprozil (500 mg) twice daily for 7 days [140] were evaluated in healthy individuals. Changes in the microbiota persisted for up to 12 weeks after the end of the treatment, characterized by the incomplete restoration of microbial equilibrium and the emergence of MDR strains. Moreover, compared with parenteral antibiotics, oral agents result in higher concentrations of antibiotics in the intestine and larger numbers of MDR bacteria in the intestinal microbiota [141]. A study of ciprofloxacin (500 mg twice daily for 10 days) or clindamycin (150 mg four times daily for 10 days) on the fecal microbiota of healthy human beings for 1 year showed a profound impact on the diversity of the microbiome [141]. Changes in microbial equilibrium were most pronounced in the first month after treatment, but persisted until month 20.
The commensal intestinal microbiota plays a pivotal role in protection against CDI [142]. Candida difficile is rarely present in the gut of healthy adults (~ 3%) [143]. The correlation between antibiotic exposure and CDI has been demonstrated [144]. Disruption of normal intestinal flora consequential to antibiotic use provides an opportunity for C. difficile to proliferate 'and produce toxins [145]. Animal and clinical studies have shown that normal intestinal microbiota inhibits the expansion and persistence of C. difficile [146]. These alterations can be evident during administration and for several days after the discontinuation of an antibiotic [147], depending on the administered antibiotic and the person’s microbiota. The risk of CDI is estimated to increase up to sixfold during and in the subsequent month after antibacterial therapy [34]. Although most antibiotics have been associated with CDI, clindamycin, amoxicillin-clavulanic acid, third- and fourth-generation cephalosporins, fluoroquinolones, and carbapenems pose the greatest risk [34].
Surgical antibiotic prophylaxis (SAP) is a crucial component of perioperative infection prevention [148, 149], particularly in clean-contaminated and contaminated surgical procedures with a high infection risk. SAP may also be indicated in certain clean procedures where SSI, even if unlikely, may have devastating consequences, such as procedures with prosthetic implants. Patients with medical conditions associated with a higher risk of SSI, including immunocompromised individuals (e.g., neutropenia), patients with American Society of Anesthesiologists (ASA) score ≥ 3, and obese patients. Despite SAP not being required before all surgical procedures, over-administration is frequent, contributing substantially to overall antibiotic consumption in surgical services. Elective laparoscopic cholecystectomy carries a low risk of SSI. Use of prophylactic antibiotics is not justified in patients undergoing elective, uncomplicated laparoscopic cholecystectomy. The role of SAP in patients undergoing open-groin herniorrhaphy or hernioplasty remains uncertain owing to conflicting results of generally low evidence quality [150–155]. International guidelines [156] recommend SAP in open-groin mesh repair in any patient in a high-risk environment.
Antibiotic therapy should be prescribed after a bacterial infection has been confirmed. Colonization by potential pathogens without associated signs of infection occurs frequently in certain patients (e.g., those with indwelling urinary catheters, endotracheal tubes for mechanical ventilation, chronic wounds). Appropriate evaluation requires obtaining a culture from these sites only when indicated, without contamination by the collection protocol itself (superficial swab cultures and cultures of drains [157] and sinus tracts are inappropriate), and avoiding antibiotic treatment of a “positive” culture result without symptoms and signs of active infection [158]. Asymptomatic bacteriuria is a common scenario for which antibiotics are not recommended, yet it is often treated regardless. Patients with a urinary drainage catheter may have “positive” urine culture results owing to inevitable biofilm formation on the device. Numerous studies show that antibiotic treatment of patients with asymptomatic bacteriuria is not indicated except in specific circumstances, such as pregnancy or transurethral instrumentation, because it can increase the likelihood of subsequent urinary tract infections that can become resistant to common antibiotics [159, 160].
The use of antibiotics in the treatment of mild uncomplicated diverticulitis has been common, but is now being questioned. Mounting evidence suggests that mild uncomplicated diverticulitis is more likely to be an inflammatory rather than an infectious condition, questioning the appropriateness of antibiotic use [161]. Three randomized trials each showed that antibiotic treatment neither prevents complications or recurrences nor reduces symptoms or length of hospital stay [161–163], as did two prospective cohort studies [164, 165]. The results of these studies have led some experts to advocate against the routine use of antibiotics [166, 167].
Prescribing the appropriate antibiotic(s) at the right time
Once the treatment decision has been made, it is crucial to select the most appropriate antibiotic(s) for that specific patient (Fig. 12). The antibiotic selected for SAP should be active against the common bacteria causing SSIs in the specific procedure. SSIs in clean procedures are usually due to skin flora, including S. aureus or coagulase-negative staphylococci. Clean-contaminated and contaminated procedures can involve other bacteria, such as E. coli, other Enterobacterales, or anaerobes, depending on the flora of the mucous membranes incised.
Fig. 12.
Selecting the most appropriate antibiotic(s) for a specific patient
The most common antibiotics used for SAP have been first- and second-generation cephalosporins (e.g., cefazolin, cefuroxime) [148, 149]. Cefazolin is the drug of choice for SAP before most procedures. It has proven efficacy, a suitable duration of action, activity against the bacteria commonly encountered in SSI, a reasonable safety profile, and low cost. Routine use of vancomycin in SAP is not recommended. Vancomycin may be considered for SAP in patients with known MRSA colonization or those at high risk therefor, such as in institutions with a high incidence of MRSA infections, patients after a recent hospitalization, dialysis patients, and patients admitted from skilled nursing facilities, based on national recommendations and local epidemiology.
The administration is determined according to the antibiotic half-life. For most frequently used antibiotics, such as cefazolin or cefoxitin, intravenous administration 30–60 min before incision ensures effective tissue concentrations at the time of incision [168]. Redosing during surgery is required when the operative procedure lasts for more than 4 h or there is > 1.5 L blood loss [149, 169]. Vancomycin should be administered within 120 min before the incision, and given over 1 h for a 1 g dose (longer, if the dose is higher). Redosing is generally not required for antibiotics with a long half-life (e.g., fluoroquinolones, metronidazole, vancomycin).
Regarding empiric therapy before causative bacteria and susceptibilities are known, the optimal antibiotic choice should be based on the infection source, expected pathogens, the patient’s clinical condition, local epidemiology, and individual patient risk factors for MDR bacteria. Knowledge of patients’ risk factors for MDR bacteria is essential [1]. Treatment guidelines informed by local epidemiology and resistance patterns should be developed and implemented consistently according to ASP principles. Identifying the correct antibiotic(s) for a particular patient can be complex. Although the susceptibility of bacteria involved in community-acquired infections is usually substantially higher and broader than those involved in HAIs, clinicians often recommend broad-spectrum antibiotics for severe community-acquired infections to avoid “missing anything”. Whereas the spectrum of activity may be appropriate in doing so, the likelihood is over-treatment because narrow-spectrum antibiotics are equally effective in most cases. By contrast, for HAIs, the best course of action is empiric broad-spectrum therapy, including an antifungal agent in some circumstances [170, 171], with later de-escalation to tailored therapy once microbiology data are available [172, 173].
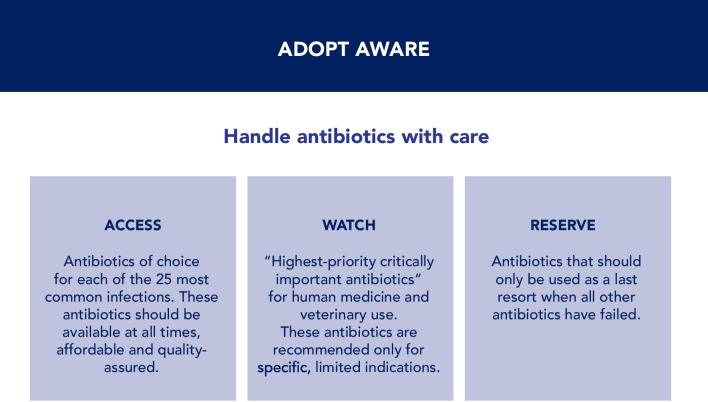
In 2017, the WHO Expert Committee on Selection and Use of Essential Medicines established the AWaRe (Access, Watch, Reserve) classification of antibiotics to aid antibiotic stewardship efforts globally at all levels of care. This classification system groups antibiotics into the aforementioned three categories, based on treatment of common bacterial infections and their impact on AMR, focusing on the need for appropriate use. The AWaRe classification [174] was updated in 2021 to include an additional 78 antibiotics that were not previously classified, bringing the total number of classified antibiotics to 258 (Fig. 13).
Fig. 13.
AWaRe classification
The “Access” category refers to the antibiotic of choice for each of the 25 most common infections. These antibiotics should be available at all times and places and should be acceptable and affordable. The “Watch” category includes most of the “highest-priority critically important antibiotics”, which are recommended only for specific indications. The “Reserve” category includes antibiotics that should only be used as a last resort (i.e., to treat MDR bacteria) and only when all other antibiotics have failed. WHO recommends reducing the use of antibiotics in the “Watch” and in the “Reserve” groups, and increasing the access and use of antibiotics in the “Access” group, expecting 60% of all antibiotic use in hospitals should come from this group [174]. As a practical matter, this would reduce the global utilization of piperacillin-tazobactam, an antipseudomonal ureidopenicillin that is overused to treat community-acquired infections.
Assessing the severity of infection is a crucial step in evaluating patients for antimicrobial therapy. Early implementation of appropriate empiric antibiotic therapy has a significant favorable impact on outcomes of septic shock, independent of infection site [175]. Whereas critically ill patients benefit from early antibiotic therapy, clinicians managing less severely ill patients may have time to consider carefully and determine the appropriate antibiotic treatment before initiating therapy [175]. Delayed antibiotic prescription, using a wait-and-see approach with reevaluation of the patient, has been reported as a useful tactic to help reduce antibiotic use, particularly for respiratory tract infections [176]. However, some data suggest that hasty antibiotic therapy may be harmful for critically ill surgical patients, where the adequacy of source control is the crucial determinant of survival. A before-after trial [177] compared universal early antibiotic therapy (aggressive approach) to a second period where immediate antibiotic therapy was given only in hypotensive patients. At the same time, other patients underwent therapy only after microbiological confirmation of infection (conservative approach). The aggressive approach was associated with a lower time interval from fever onset and blood culture collection to the start of treatment. The conservative approach was associated with more likely initial appropriate therapy, a shorter duration of therapy, and lower mortality. This differentiation of infection from inflammation can be challenging, especially in critically ill patients, wherein only about one-half of suspected infections are proven. Delaying antibiotics to investigate the cause of sepsis may be of benefit to patients without shock.
Delayed antibiotic prescription is especially useful to help reduce antibiotic use, especially for community-acquired respiratory tract infections [178], many of which have a viral etiology. In a meta-analysis, delayed prescription compared with no antibiotics was associated with similar symptom duration; withholding antibiotics pending pathogen identification and susceptibility testing may be acceptable to reduce unnecessary antibiotic use for viral respiratory tract infections.
By contrast, for patients (both adults and children) with sepsis-related shock and organ dysfunction, delay of appropriate empiric antibiotic therapy can be deleterious [179, 180]; early initiation of antibiotics is crucial for good outcomes. There is a strong correlation between each hour of delay in antibiotic initiation and mortality rates for patients with septic shock [181, 182]. The 2021 Surviving Sepsis Campaign guidelines recommend that adults with possible septic shock or probable sepsis should receive antibiotics as soon as possible, ideally within 1 h from symptom onset [183]. For adults with possible sepsis without shock, a rapid assessment for the likelihood of infectious vs. non-infectious causes of acute illness should be conducted, and antimicrobial agents should be administered within 3 h from the time sepsis was first recognized [183].
The involvement of MDR pathogens in HAIs is a risk factor for inappropriate empiric therapy and, as such, for adverse outcomes. Prior knowledge of colonization caused by MDR bacteria via surveillance cultures improves the likelihood of appropriate initial antibiotic therapy for subsequent HAIs in critically ill patients with blood stream infections or VAP [184, 185]. Additionally, as surveillance cultures have a high negative predictive value for MDR bacteria, early appropriate antibiotic therapy can have antibiotic-sparing potential by reducing use of carbapenems and other antipseudomonal agents compared with a hypothetical guideline-based prescription [185–188]. As such, antibiotic selection pressure on the local ecology may be reduced. A meta-analysis of diagnostic test accuracy revealed that a twice-weekly sampling frequency is the most efficient and that recent surveillance cultures have a higher positive predictive value for bacterial pathogens in VAP [185].
Administering antibiotics in adequate doses and appropriate routes
Administering antibiotics in adequate doses should be based on the intrinsic pharmacokinetic (PK) and pharmacodynamic (PD) characteristics of each antibiotic class and the specific agent, and on the specific pathophysiologic characteristics of the patient. Antibiotic PD refers to the relationship between the concentration of the drug and its ability to inhibit bacterial growth. The minimal inhibitory concentration (MIC) is the primary in vitro parameter used to assess the effectiveness of an antibiotic against its target bacteria. In order to obtain a therapeutic effect, the concentration at the site of infection should exceed the MIC against the target bacteria for at least 40% of the dosing interval, and ideally longer (if killing is time-dependent) or by > tenfold (if killing is concentration-dependent) [189]. Antibiotic PK describes how antibiotics are absorbed, distributed, metabolized, and eliminated from the body, which in turn determines the time course and concentration of antibiotics in serum and tissues and at the site of infection. Suboptimal concentrations at the target site may have important clinical consequences such as therapeutic failure and promotion of AMR development, especially when clinical isolates have borderline in vitro susceptibility [190].
Clinical- and antibiotic-related factors can contribute to a differential distribution of antibiotics at the target site [191]. Knowledge of PK/PD of each antibiotic may provide a more appropriate definition of optimal dosing regimens in terms of both dose and administration interval [192]. The concentration gradient between plasma and the site of action may be of high relevance in cases of MDR bacterial infection. For example, data suggest that increased doses of ceftazidime, meropenem, and imipenem-cilastatin are required to reach target attainment in patients with severe intra-abdominal infections [193–195].
Critically ill patients are at high risk of infections, risking life-threatening sepsis and multiple organ dysfunction syndrome. The pathophysiology of sepsis and septic shock can have a major effect on PK parameters. Knowledge of pathophysiologic effects on PK/PD is essential for optimizing antibiotic treatment in critically ill patients with sepsis or septic shock [196, 197]. Hepatic or especially renal dysfunction are conditions where PK changes and dosage reduction may be needed.
The dosing frequency of an antibiotic is determined by the concepts of time-dependent vs. concentration-dependent activity. For example, beta-lactam antibiotics exhibit time-dependent activity, whereby optimal bactericidal activity is achieved when antibiotic concentrations are maintained above the MIC over prolonged periods of time. For this reason, the serum concentration of the antibiotics should exceed the MIC for at least 40% (optimally 70%) of the dosing interval [196]. Higher dosing frequency, prolonged infusions, and continuous infusions achieve this effect and optimize beta-lactam activity [196]. By contrast, antibiotics having concentration-dependent activity are ideally administered to achieve a high peak plasma concentration. For these antibiotics, the peak serum concentration:MIC, not the time above the MIC (fT > MIC), is more closely associated with efficacy [196]. Despite the ideal method of administration and the preferred dosing schemes of aminoglycosides being once-daily dosing for most therapeutic indications, especially in critically ill patients [198], aminoglycoside nephrotoxicity is due to their uptake saturation and a direct vasoconstrictive effect on the renal cortical microcirculation. Thus, limiting aminoglycoside exposure to the renal cortex, by limiting administration to once-daily, reduces the risk of nephrotoxicity [34, 199].
In patients with septic shock, administering a first “loading” dose is probably as fundamental as the timing of administration, depending on the antimicrobial agent [34]. The volume of distribution (VD) of hydrophilic agents (such as beta-lactams, aminoglycosides, and glycopeptides) in septic shock patients may be increased due to increased microvascular endothelial permeability, expanding the extracellular fluid compartment. Loading doses of beta-lactams, aminoglycosides (especially with once-daily dosing) or glycopeptides are recommended to maximize the therapeutic effect [196].
Once initiated, the antibiotic regimen should be reassessed at least daily, given that fluctuating organ function, common in critically ill patients, may substantially affect antibiotic exposure. For example, lower doses of antibiotics excreted in urine should be administered in the presence of impaired renal function, whereas higher than standard doses should be administered in patients with augmented renal clearance (e.g., burn patients, obesity) [34]. Antibiotic therapy represents a challenge for obese patients because of altered PK/PD [200]. Obesity increases VD, especially for lipophilic antibiotics, which can lead to lower-than-expected plasma antibiotic concentrations. Augmented renal clearance is frequent. In addition, fatty infiltration of the liver may impair hepatic function. In general, regardless of body mass, the dosing of lipophilic antibiotics should be based on total body weight, or adjusted body weight for hydrophilic antibiotics. Individualized dosing, supported by laboratory testing, is essential owing to patient heterogeneity and clinical fluctuation.
Recently, a revised consensus guideline and review on therapeutic monitoring of vancomycin for serious MRSA infections was published by the American Society of Health-System Pharmacists, the IDSA, the Pediatric Infectious Diseases Society, and the Society of Infectious Diseases Pharmacists. This consensus revision evaluates the current scientific data and controversies associated with vancomycin dosing and serum concentration monitoring for serious MRSA infections (including but not limited to bacteremia, sepsis, infective endocarditis, pneumonia, osteomyelitis, and meningitis) and provides new recommendations based on recent available evidence [201].
Oral antibiotic administration has been shown to decrease the cost and length of hospitalization [202, 203]. The general guidance for the timing of intravenous-to-oral switching of antibiotics provided the gastrointestinal tract is functional, includes defervescence and clinical improvement with or without improvement in laboratory markers [204]. Numerous antibiotics with high oral bioavailability can be considered for switching, and the switch need not be to the same agent. Many serious infections can now be treated successfully with partial oral antibiotic therapy [205]. However, the switch to oral antibiotics should not lead to an antibiotic therapy which is longer than that used for parenteral therapy. Actually, it is increasingly evident that prescribing oral antibiotics could influence gut microbiome dynamics, promoting more strongly AMR [206].
Initiating, as soon as possible, targeted treatment based on the results of culture and susceptibility testing
Microbiologic tests play a crucial role in selecting targeted antibiotic therapy. This testing allows clinicians to tailor the spectrum of the antibiotic, broadening if the initial choice was too narrow, but more commonly narrowing an empiric regimen spectrum that was too broad, known as de-escalation. Antibiotic therapy reassessment based on microbiologic culture and susceptibility testing supports ASP and is associated with improved outcomes in severe infections [34].
The de-escalation tactic involves transitioning from a broad-spectrum empiric antibiotic regimen to a narrower-spectrum regimen, or reducing the number of antibiotics used in combination therapy [207], or to monotherapy. The rationale of de-escalation is to avoid broad-spectrum antibiotics whenever possible, diminishing selection pressure and ultimately the prevalence of MDR bacteria, but the practice is controversial as data are scant [208]. The data are strongest for patients with VAP, with higher survival rates reported in several studies [209, 210], obtaining sputum samples before antibiotic administration is a crucial facet to make de-escalation possible. De-escalation has been embraced as part of ASP.
The MIC, the lowest antimicrobial agent concentration that inhibits microbial growth, can be determined by different methods, such as broth or agar dilution, and disk or gradient diffusion. The MIC value, expressed as mcg/mL, is often translated by clinical microbiology laboratories as “susceptible,” “intermediate,” or “resistant” according to defined “breakpoints” established by the Clinical and Laboratory Standards Institute (CLSI, Wayne, PA, USA) or “susceptible,” “susceptible, increased exposure,” or “resistant” according to the criteria of the European Committee on Antimicrobial Susceptibility Testing (EUCAST, Vaxjo, Sweden) [34].
Rapid diagnostics may contribute in furtherance by limiting unnecessary initiation of broad-spectrum therapy, thus decreasing the need for subsequent de-escalation [211, 212]. Most of the commercially available rapid detection methods for MDR bacteria include genotyping that relies on the detection of resistance genes [213] based on DNA sequencing. Genotypic methods may be used in conjunction with phenotyping [214], but genotypic methods in current clinical use should be regarded as supplemental to traditional phenotypic antimicrobial susceptibility testing owing to several limitations. Genotyping can effectively predict AMR, but does not inform susceptibility testing. In addition, the panel of resistance determinants is small, so other resistance determinants may not be detected. Moreover, with genotypic methods there is also the possibility of overestimating AMR, because the presence of a resistance gene is not necessarily associated with the phenotypic expression of resistance (the gene could be inactivated or not expressed).
The greatest advantage of genotyping is undoubtedly speed, with turnaround times of 1–4 h. Employment of comparative genomics, probes, microarrays, nucleic acid amplification techniques, and deoxyribonucleic acid sequencing should allow for the detection of multiple resistance genes or variants simultaneously. However, a logistic challenge in practice is that when new antibiotics are marketed, there may be a lag before methods to measure in vitro susceptibility are validated for clinical use, which may limit the initial clinical use of new agents [215].
Rapid diagnostic testing for possible pathogens is considered indispensable for ASPs. Coupled with prompt, appropriate therapy, antibiotic use is decreased, mortality is reduced, hospital stays are shortened, and cost is lowered [216–218]. The lack of availability of modern diagnostic tests represents an important barrier in low-resource settings [219].
Using the shortest duration of antibiotics based on evidence
The duration of antibiotic therapy prescribed in daily practice is often longer than recommended by guidelines [220]. WHO [220] recommends against prolonging the administration of SAP after surgical intervention to prevent SSIs, based on a meta-analysis [220] of 69 randomized controlled trials (RCTs) investigating the optimal duration of SAP. For clean and clean-contaminated procedures, CDC guidelines recommend not to give additional doses of prophylactic antibiotics after the surgical incision has been closed in the operating room, even in the presence of a drain [109]. Updated guidelines of IDSA and SHEA recommend stopping all SAP at incision closure, regardless of procedure type or duration [221].
de Jonge et al. examined the effect of continued SAP on the rate of SSI [222]. Eighty-three RCTs were evaluated; 52 (19,273 participants) were included in the primary meta-analysis. No conclusive evidence for the benefit of the post-operative continuation of antibiotic prophylaxis (vs. discontinuation) was identified. When combined with a comprehensive approach to best practices in SSI prevention, post-operative continuation of SAP produced no additional benefit in reducing the incidence of SSI in any surgical setting. In a 2019 multicenter retrospective cohort study [223], increased duration of antibiotic prophylaxis was associated with a higher risk of acute kidney injury and CDI, but no reduction in SSIs.
A study of 34 urban and rural South African hospitals demonstrated that implementation of process improvement initiatives and principles targeted to institutional needs, utilizing pharmacists, effectively improved SAP guideline compliance and sustainable patient outcomes [224]. Efforts to shorten antibiotic therapy duration in hospital practice are a growing area of focus for ASPs [225]. However, Langford et al. showed that ASP advice to stop antibiotics or reduce their duration was accepted less often than advice to start or increase antibiotic exposure [226].
Shortening the duration of antibiotic therapy is a crucial tactic for reducing unnecessary inpatient antibiotic use, where antibiotic pressure is intense [227]. Although there are circumstances that may require prolonged antibiotic therapy (e.g., endocarditis, osteomyelitis), the duration of antibiotic therapy should always be as brief as possible. Regarding intra-abdominal infections, the STOP-IT trial [228] demonstrated that, in the setting of adequate source control, 4 days of antibiotic therapy was non-inferior to 8 days of therapy. In the DURAPOP randomized clinical trial [229], critically ill patients with post-operative intra-abdominal infections treated with a short course of antibiotics (8 days) showed similar outcomes compared with those treated for 15 days.
Antibiotic therapy of up to 21 days for VAP and hospital-acquired pneumonia (HAP) was used historically until several prospective studies demonstrated the effectiveness of shorter (7–8 days) therapy with no differences in mortality, intensive care unit (ICU) stay, mechanical ventilation-free days or organ failure-free days [230, 231]. The 2017 European Society of Clinical Microbiology and Infectious Diseases (ESCMID) guidelines and the 2016 IDSA guidelines [232] both recommend 7 days of therapy for HAP/VAP. Ongoing studies [233] are determining if therapy duration could be reduced further.
Bacteremia caused by Enterobacterales has been treated traditionally with 2 weeks of antibiotics. Recent RCTs and meta-analyses investigating shorter (7–8 days) versus longer antibiotic courses (14–15 days) in patients with gram-negative bacteremia (mostly of urinary tract origin) demonstrate non-inferiority [234–239]. Regarding acute uncomplicated cellulitis, evidence also suggests that prolonged courses may be unnecessary and that 5 days of treatment may be sufficient [240]. IDSA guidelines recommend a 5-day antibiotic therapy duration for uncomplicated cellulitis, but may be extended if the infection has not improved within that time frame [241].
Generally, in critically ill patients, decisions about antibiotic therapy duration should be individualized, taking into account patient parameters such as severity of illness, the site and type of infection, whether source control has been achieved, whether PK has been optimized, and clinical response [242]. Procalcitonin (PCT) may be useful to guide antibiotic therapy in the ICU. PCT-guided treatment can reduce the duration of therapy and length of hospital stay in adult critically ill patients with sepsis [243, 244]. Based on apparent benefit and no obvious undesirable effects, the 2021 Surviving Sepsis Campaign guidelines suggest using PCT along with a clinical evaluation to decide when to discontinue antibiotics in adults with an initial diagnosis of sepsis or septic shock and adequate source control, if the optimal duration of therapy is unclear and if PCT is available [183].
Achieving source control by identifying and eliminating the source of the infection or reducing the bacterial load
Source control aims to eliminate the source of infection, reduce the bacterial inoculum, and correct anatomic derangements to restore physiologic homeostasis. Additionally, it involves draining abscesses or infected fluid collections, debriding necrotic tissue, or removing contaminated medical devices, all being situations where antibiotics alone have limited efficacy.
Source control is crucial in the management of surgical infections, particularly intra-abdominal and soft tissue infections. Adequate source control achieved by the index operation allows for a shorter course of antibiotic therapy, thereby improving patients’ outcomes, including lower risk of organ dysfunction [245, 246]. In the setting of uncomplicated intra-abdominal infections, such as uncomplicated appendicitis or cholecystitis, post-operative antibiotic therapy is not necessary if source control is adequate [246]. In the setting of complicated intra-abdominal infections, a short course of antibiotic therapy is always suggested even if source control is adequate [228, 229].
In some circumstances, organizational determinants may influence the excessive use of antibiotics. For example, acute cholecystitis should be managed by early cholecystectomy [247]. Nevertheless, because operating room availability is at a premium in many centers, acute cholecystitis cases are sometimes managed by percutaneous drainage or a delayed cholecystectomy, requiring a longer duration of antibiotic therapy.
The urgency (but not the need, ultimately) for source control is determined by the affected organ(s) and the rapidity at which underlying physiological stability deteriorates. Prompt source control may also be important for indolent infections (e.g., infected medical devices). A challenging management problem is central venous catheters associated with catheter-related blood stream infections. In these cases, removal of the catheter (required if the pathogen is Pseudomonas spp., S. aureus or fungal) constitutes source control. There is little reason to delay source control, even for a few hours, in patients with sepsis [248–250]. The 2021 Surviving Sepsis Campaign guidelines [183] recommend identifying the anatomic source of infection and implementing source control (if amenable) as soon as possible. Delays of as little as 6 h in the setting of sepsis or septic shock have been associated with increased mortality. A multicenter cohort study (2013–2017) of hospitalized adults with community-acquired sepsis (according to SEPSIS-3 definitions) undergoing source control procedures [251] showed that source control within 6 h was associated with a reduced risk of 90-day mortality. In a post hoc analysis of a multicenter observational study (Abdominal Sepsis Study, AbSeS) [252], urgent, successful source control was associated with improved survival, whereas appropriateness of empiric antibiotic treatment was not, suggesting that source control is determinative of outcome for patients with sepsis of abdominal origin. Prompt source control may also be important for other infections [253]. A prospective international cohort study of adult patients (≥ 18 years old) with hospital-acquired blood stream infections treated in ICUs (June 2019–February 2021) reported mortality of 37%. Failure to achieve source control, if required, was associated with death in a multivariable logistic regression model.
Some patients are prone to persistent or recurrent sepsis, despite initial attempts at source control [254]. Index source control procedures may fail up to 25% of the time in abdominal sepsis with shock [255]. Timely surgical re-intervention provides the only option that significantly improves outcomes. Failure of source control may be caused by incomplete initial source control, particularly if contamination is ongoing [256]. Failure of source control can be difficult to diagnose. Therefore, monitoring the success of source control is crucial, with a high index of suspicion if a patient does not improve. Most often, diagnosis is based on a lack of clinical improvement (persistent signs and symptoms of inflammation) and confirmed by imaging.
Supporting surveillance of HAIs and AMR, monitoring of antibiotic use, consumption, and the quality of prescribing
Surveillance and prevalence studies to determine the frequency of HAIs are crucial tactics of a strategy to reduce HAIs and contain AMR. Data on HAI prevalence allow hospitals to measure the effectiveness of IPC activities; audits and feedback are used to drive change, improving quality and safety. The European Healthcare-Associated Infections Surveillance Network (HAI-Net) [257], coordinated by the ECDC, provides surveillance of HAIs. The main priorities of HAI-Net are the coordination of European point prevalence surveys of HAIs and antimicrobial use in acute care hospitals and long-term care facilities, surveillance of SSIs, and surveillance of HAIs in ICUs. In the USA, the CDC National Healthcare Safety Network (NHSN) [258] is the most widely used HAI tracking system. NHSN provides facilities and governmental entities with data needed to identify problem areas, measure progress of prevention efforts, and ultimately eliminate HAIs. In addition, NHSN allows tracking of blood transfusion safety errors and important healthcare process measures such as personnel influenza vaccination status, and IPC adherence rates. Surveillance of MDR bacteria provides a basis for taking action to control AMR. Consistent data on the incidence and prevalence of MDR bacteria and geographic patterns related to AMR guide patient treatment and monitor the effectiveness of interventions.
A recent joint publication by ECDC and the WHO Regional Office for Europe reported AMR rates in Europe, using data from invasive bacterial isolates [259]. Carbapenem resistance in K. pneumoniae and vancomycin resistance in E. faecium increased during 2016–2020. Moreover, high rates of resistance to third-generation cephalosporins and high rates of carbapenem-resistant Acinetobacter spp. and P. aeruginosa in several European Region countries were identified.
In 2015, WHO launched the Global Antimicrobial Resistance and Use Surveillance System (GLASS), a collaborative effort to standardize AMR surveillance worldwide. Since its launch, GLASS has expanded its coverage and as of 2021, 109 countries and territories worldwide have contributed data to GLASS [260]. High rates of AMR to first-line antibiotics were reported by most countries and in some countries even to last-resort antibiotics. GLASS data demonstrate that globally, carbapenem-resistant bacteria are a serious concern. High rates of carbapenem-resistant Acinetobacter spp. and K. pneumoniae, resistance to third-generation cephalosporins in Enterobacterales, MDR and XDR tuberculosis, and MRSA will require ongoing close monitoring.
Inappropriate antibiotic use is a main driver of AMR [261]. Data on antibiotic utilization (volume and appropriateness) are essential to evaluate the impact of ASPs. Antibiotic consumption and appropriateness of use can be measured at different levels from nationally down to the prescriber level, allowing informed, focused efforts to reduce unnecessary or inappropriate use [262]. The most common metric to monitor antibiotic consumption is based on the concept of the defined daily dose (DDD). The DDD is the average maintenance dose per day of an antibiotic used in adults for its primary indication. Expressing antibiotic consumption in DDD/1000 patient-days allows comparison regardless of differences in individual antibiotic choices, measuring changes over time to assess the impact of ASP interventions. Between 2000 and 2015, antibiotic consumption expressed in DDD increased by 65% from 21.1 to 34.8 billion DDDs, while the antibiotic consumption rate increased by 39%, from 11.3 to 15.7 DDD/1,000 inhabitants/day) in 76 countries worldwide [263]. Of particular concern was the rapid increase in the use of last-resort compounds, both in high-income countries and LMICs, such as glycylcyclines, oxazolidinones, carbapenems, and polymyxins.
Educating staff and improving awareness
One of the goals of the WHO Global Action Plan on Antimicrobial Resistance [49] is to improve awareness and understanding of AMR through effective communication, education, and training. To address AMR, all prescribers must become stewards of antibiotics by prescribing appropriately and educating colleagues and patients on their proper use. The goal of raising awareness is to change behaviors that fuel AMR. Not only can behaviors, beliefs, and practices regarding antibiotic use be inappropriate, there are misconceptions about the concept of AMR itself and its emergence, dissemination, and impact. Clinical leaders should promote awareness by encouraging an institutional culture of patient safety and responsible use where clinicians are persuaded, rather than constrained, to be compliant with antibiotic prescribing measures. Strong patient safety cultures promote education, collaboration, and engagement. Patients must also be engaged with information about the social cost of AMR and the individual benefits of targeted therapy.
The ultimate goal of any stewardship program should be to stimulate a behavioral change in prescribing practices [264]. It is important to incorporate fundamental antimicrobial stewardship, diagnostic stewardship, and IPC principles in under- and post-graduate training and education in order to provide confidence, skills, and expertise in the field of infection management [265]. The education of prescribers is pivotal to convince clinicians to use antibiotics appropriately [1], by respecting correct prescribing practices and following IPC recommendations. There is an urgent call for the integration of antimicrobial stewardship teaching at the undergraduate level of medical education to train future prescribers on this critical aspect of public health. Proper undergraduate education on rational antibiotics use would enable health professional graduates to enter clinical practice with adequate competencies to become rational prescribers [266]. However, although education to intensify AMR prevention is fundamental, without concurrent interventions education alone is of little value. Diagnostic uncertainty, fear of clinical failure or potential litigation, time pressure, or organizational contexts can complicate antibiotic prescribing decisions.
A cross-sectional study of perceptions and practices of physicians and pharmacists regarding antibiotic misuse at primary care centers in the Middle East reported a number of misconceptions and inappropriate practices relating to antibiotic use in Qatar by patients and healthcare providers [267].
Interestingly, the study found that about a third (29.2%) of physicians felt they were often under pressure by patients to prescribe antibiotics. Physicians who are overworked, underinformed, or pressured tend to overprescribe antibiotics and thereby contribute to the spread of AMR. Patients often expect to be prescribed antibiotics, and this pressure can be difficult for physicians to ignore. However, physicians' communication with patients influences their satisfaction more than the actual receipt of antibiotics, especially when patients are asked by their physician to contact them if symptoms do not improve [268]. Therefore, these findings suggest that educating patients about their diagnosis and course of treatment may result in reduced demand for unwarranted antibiotics [267].
Supporting multidisciplinary ASPs and enhancing collaboration of healthcare professionals from various disciplines
The promotion of ASPs is pivotal to ensure more standardized and responsible antibiotic use within a healthcare facility [269]. ASPs promulgate and implement best practices to prescribe, administer, monitor, and dispose of antibiotics. However, practices for implementing ASPs may vary based on local culture, policies, and resources. Some hospitals still lack formal ASPs, but even established programs can struggle with sufficient resources and gaining acceptance [270]. The effectiveness of measures to reduce excessive antibiotic prescribing to hospital inpatients and the impact of these measures on reducing the incidence of AMR or CDI have been evaluated [271]. Analyzed measures were able to reduce AMR and HAIs and improve clinical outcomes. Restrictive interventions were recommended when the need to intervene is considered urgent, but over the long term (6 months or more), persuasive measures are equally effective [271].
Promoting ASPs across clinical specialties is crucial to ensuring standardized, rational antibiotic use within a facility as well as a healthcare system [272]. Collaboration allows sharing of knowledge and widespread diffusion of best practices. Timely and accurate reporting of susceptibility test results allows the selection of appropriate targeted therapy and may help reduce broad-spectrum antimicrobial use. ASPs can provide periodic reports on AMR and identify the local microbiological epidemiology for both phenotypic and genotypic analyses [273]. This can impact greatly the choice of empiric therapy. When involved in an ASP, clinical prescribers with knowledge of infectious diseases may help refine antibiotic policy based on local data, audit antibiotic prescribing, provide feedback, integrate best practices of antibiotic use, and act as “champions” among colleagues. Such a champion model has been applied previously to surgical safety implementations in general, such as surgical checklists, and plays a key role in successful quality improvement at the hospital level [274].
Surgeons are responsible for many of the processes that impact the risk for SSIs and play a key role in their prevention. Surgeons are also at the forefront in managing patients with infections, often providing prompt source control and appropriate antibiotic therapy, and are directly responsible for their outcomes. In this context, the direct involvement of surgeons is of utmost importance [270].
Infections are the main factor contributing to ICU mortality. Intensivists have a crucial role in preventing and treating AMR in critically ill patients. Intensivists prescribe antimicrobial agents to challenging patients and thus are at the forefront of successful ASPs [275]. Emergency Departments (EDs) represent a particularly important setting for addressing inappropriate antimicrobial prescribing practices, given the frequent use of antibiotics in this interface between the community and the hospital. Therefore, ED practitioners should also be involved in ASPs [276, 277]. An essential participant in ASPs, often unrecognized and underutilized, is the staff nurse. Nurses are first-responders, crucial communicators, and 24-h guardians of patient status [278]. Their role is becoming formalized in implementing and operating ASPs [278], performing numerous functions that are integral to success. Without adequate support and resources from healthcare administrators, the ASP will not function optimally, in that these programs do not generate revenue. The engagement of healthcare administrators has been confirmed as a key factor for both developing and sustaining an ASP [270].
Successful ASPs can reduce the incidence of infections and colonization with MDR bacteria, including CDI among inpatients [15]. The best means to improve ASP programs is to create a collaborative environment, including all prescribing practitioners [86, 270], to exchange knowledge on best practices and diagnostic capacity.
Due to the challenges posed by the development of new antibiotics, the emergence of MDR bacteria is likely to outpace the introduction of new drugs to combat them. Thus, it may be important to focus on alternative non-antibiotic measures to address AMR [279]. Health information technology is a novel approach to optimize antibiotic use in the healthcare setting, although computerized decision support for hospital antibiotic use may not work in all settings [280]. Curtis et al. demonstrated the utility of computerized decision support of antibiotic usage and even in reduction of mortality in hospital settings [281].
Whereas clinical research should work toward developing new management techniques and therapies to address AMR, physicians should continue to preserve the use of antibiotics as much as possible. Additionally, public health campaigns aimed at promoting awareness about the responsible use of antibiotics and IPC measures can also be crucial in reducing the spread of MDR bacteria.
This document confirms the mission of the Global Alliance for Infections in Surgery, promoting standards of care in managing surgical infections through a cohesive and multidisciplinary approach. The axiom “if you want to go fast, go alone; if you want to go far, go together” reminds us that we need global solidarity not only to reduce health inequalities, but also to be united against all global health challenges, including AMR (Fig. 14).
Fig. 14.
Supporting a cohesive and multidisciplinary approach
Conclusions
Appropriate use of antibiotics should be integral to good clinical practice and standards of care. Inappropriate antibiotic use as well as poor IPC practices are contributing to the development and spread of AMR. Antibiotics should be treated as a global public good on the verge of scarcity; there is a global collective responsibility to preserve them in order to avoid countless future victims of MDR infections. Infections, especially those with MDR bacteria, compromise the success of all medical practitioners, including surgeons. A technically proficient surgery will be unsuccessful if the patient succumbs to a HAI that cannot be treated. Through collaborative initiatives and a united front, a future of effective antimicrobial therapy can be envisioned for generations to come.
Acknowledgements
Worldwide Antimicrobial Resistance National/International Network Group (WARNING) Collaborators:
Massimo Sartelli1, Philip S. Barie2, Federico Coccolini3, Mohamed Abbas4, Lilian M. Abbo5,6, Gulnora K. Abdukhalilova7, Yishak Abraham8, Salisu Abubakar9, Fikri M. Abu-Zidan10, Yusuff Adebayo Adebisi11,12, Harissou Adamou13, Gulara Afandiyeva14, Ervis Agastra15, Wadha A. Alfouzan16,17, Majdi N. Al-Hasan18, Sajjad Ali19, Syed Muhammad Ali20,21, Fatima Allaw22, Gbemisola Allwell-Brown23, Afreenish Amir24, Obed Kwabena Offe Amponsah25, Abdelkarim Al Omari26, Luca Ansaloni27, Shamshul Ansari28, Ana Belen Arauz29, Goran Augustin30,31, Bih Awazi32, Mohammad Azfar33, Mamadou Saliou Bailo Bah34, Miklosh Bala35, Anura S.K. Banagala36, Suman Baral37, Matteo Bassetti38,39, Luis Bavestrello40, Gregory Beilman41, Kebebe Bekele42, Moussa Benboubker43, Bojana Beović44,45, Maria Daniela Bergamasco46, Silvia Bertagnolio47, Walter L. Biffl48, Stijn Blot49,50, Marja A. Boermeester51, Robert A. Bonomo52,53, Adrian Brink54, Silvio Brusaferro55, Jonathan Butemba56, Miguel A. Caínzos57, Adrian Camacho-Ortiz58, Rafael Canton59-60, Antonio Cascio61,62, Alessandro Cassini63,64, Enrique Cástro-Sanchez65-67, Marco Catarci68, Rodolfo Catena69, Leili Chamani-Tabriz70, Sujith J. Chandy71, Esmita Charani72, William G. Cheadle73, Diana Chebet74, Ibrahim Chikowe75, Francesca Chiara76, Vincent Chi-Chung Cheng77,78, Anna Chioti79, Maria Elena Cocuz80,81, Raul Coimbra82, Francesco Cortese83, Yunfeng Cui84, Jacek Czepiel85,86, Mira Dasic87, Nataliya de Francisco Serpa88, Stijn W. de Jonge52, Samir Delibegovic89, E. Patchen Dellinger90, Zaza Demetrashvili91, Alessandra De Palma92, Danushka De Silva93, Belinda De Simone94, Jan De Waele95, Sameer Dhingra96, Jose J. Diaz97, Claudia Dima98, Natalia Dirani99, Cornelius C. Dodoo100, Gereltuya Dorj101,102, Therese M. Duane103, Christian Eckmann104, Beverly Egyir105, Mutasim M. Elmangory106, Mushira A. Enani107, Onder Ergonul108,09, Juan Pablo Escalera-Antezana110, Kevin Escandon111, Abdul-Wahab Omo-ope Ettu112,113, Joseph O. Fadare114, Massimo Fantoni115, Mohammad Farahbakhsh116, Mario Paulo Faro117, Alberto Ferreres118, Gianina Flocco119, Esteban Foianini120, Donald E. Fry121, Alberto Federico Garcia122,123, Chiara Gerardi124, Wagih Ghannam125, Helen Giamarellou126, Natalya Glushkova127, George Gkiokas128, Debra A. Goff129, Harumi Gomi130, Magnus Gottfredsson131,132, Ewen A. Griffiths133, Rosio Isabel Guerra Gronerth134,135, Xavier Guirao136, Yogesh K. Gupta137, Gregory Halle-Ekane138, Sonja Hansen139, Mainul Haque140, Timothy C. Hardcastle141, David T.S. Hayman142, Andreas Hecker143, Markus Hell144, Vanessa P. Ho145,146, Adrien M. Hodonou147, Arda Isik148, Salequl Islam149,150, Kamal M.F. Itani151, Nadia Jaidane152, Ib Jammer153, David R. Jenkins154, Ibrahim Franklyn Kamara155, Souha S. Kanj21, Desmond Jumbam156, Masoud Keikha157, Ashish K, Khanna158,159, Sahil Khanna160, Gaetanjali Kapoor161, Garima Kapoor162, Samuel Kariuki163, Faryal Khamis164, Vladimir Khokha165, Reuben Kiggundu166, Ronald Kiguba167, Hong Bin Kim168, Peter K. Kim169, Andrew W Kirkpatrick170, Yoram Kluger171, Wen-Chien Ko172,173, Kenneth Y.Y. Kok174, Vihar Kotecha175, Ibrahima Kouma176, Bojan Kovacevic177, Jehona Krasniqi178, Marcela Krutova179, Igor Kryvoruchko180, Ravina Kullar181, Kwaku A. Labi182, Francesco M. Labricciosa183, Sulaiman Lakoh184, Botond Lakatos185,186, Mary Ann D. Lansang187, Ramanan Laxminarayan161, Young Ran Lee188, Marc Leone189, Ari Leppaniemi190, Gabriel Levy Hara191, Andrey Litvin192, Varut Lohsiriwat193, Gustavo M. Machain194, Fawzi Mahomoodally195, Ronald V. Maier196, Md Anwarul Azim Majumder197, Sydney Malama198, Justen Manasa199, Vikas Manchanda200, Ramiro Manzano-Nunez201, Luis Martínez-Martínez202,203, Ignacio Martin-Loeches204-207, Sanjay Marwah208, Emilio Maseda209, Maleda Mathewos210, Ryan C. Maves211, Deborah McNamara212,213, Ziad Memish214-216, Dominik Mertz217,218, Shyam Kumar Mishra219,220, Philippe Montravers221, Maria Luisa Moro222, Elias Mossialos223, Fabrizio Motta224, Steward Mudenda225, Patrick Mugabi56, Mc Juan Muco Mugisha226, Eleftherios Mylonakis227,228, Lena M. Napolitano229, Dilip Nathwani230, Leontine Nkamba231, Emmanuel Fru Nsutebu232, Donal B. O'Connor233, Sade Ogunsola234, Peter Østrup Jensen235,236, Juliana Maria Ordoñez122, Carlos A. Ordoñez122,123, Pablo Ottolino237, Abdoul-Salam Ouedraogo238,239, José Artur Paiva240,241, Miriam Palmieri242, Angelo Pan243, Narayan Pant244,245, Arpád Panyko246, Ciro Paolillo247, Jay Patel248,249, Federico Pea250,251, Patrizio Petrone252, Nicola Petrosillo253, Tadeja Pintar254, Haralds Plaudis255,256, Mauro Podda257, Alfredo Ponce-de-Leon258, Susan L. Powell259, Adrián Puello-Guerrero260, Celine Pulcini261, Kemal Rasa262, Jean-Marc Regimbeau263, Jordi Rello264,265, Manuel Renato Retamozo-Palacios266, Glendee Reynolds-Campbell267, Julival Ribeiro268, Jennifer Rickard269, Nuno Rocha-Pereira,270, Victor D. Rosenthal271, Gian Maria Rossolini272,273, Godfrey M. Rwegerera274, Megan Rwigamba275, Michela Sabbatucci276,277, Žilvinas Saladžinskas278, Rasha E. Salama279, Tondore Sali280, Samson Sahile Salile281,282, Ibrahima Sall283, Hossein Samadi Kafil284, Boris E. Sakakushev285, Robert G. Sawyer286, Marco Scatizzi287, Jeremiah Seni288, Edward J. Septimus289,290, Gabriele Sganga291, Daniel Mønsted Shabanzadeh292, Vishal G. Shelat293,294, Agumas Shibabaw295, Francis Somville296,297, Selma Souf298, Stefania Stefani299, Evelina Tacconelli300, Buon Kim Tan301, Pierre Tattevin302, Carlos Rodriguez-Taveras303, João Paulo Telles304, Orlando Téllez-Almenares305, Jeffrey Tessier306, Nguyen Toan Thang307, Cristian Timmermann308, Jean-François Timsit309,310, Joel Noutakdie Tochie311, Matti Tolonen190, Gabriel Trueba312, Constantinos Tsioutis313, Fabio Tumietto314, Felipe Francisco Tuon315, Jan Ulrych316, Selman Uranues317, Maarten van Dongen318, Harry van Goor319, George C. Velmahos320, Andras Vereczkei321, Bruno Viaggi322, Pierluigi Viale323,324, Jordi Vila325-327, Andreas Voss328, Jasmina Vraneš329,330, Richard R. Watkins331, Nyambura Wanjiru-Korir332, Olivia Waworuntu333, Agnes Wechsler-Fördös334, Klara Yadgarova335, Mohammed Yahaya336, Ali I Yahya337, Yonghong Xiao338, Andee Dzulkarnaen Zakaria339, Tanya L. Zakrison340, Victor Zamora Mesia341, Walter Siquini1, Ara Darzi342, Leonardo Pagani343, Fausto Catena344.
1Department of Surgery, Macerata Hospital, Macerata, Italy. 2Department of Surgery, Weill Cornell Medicine, New York, New York, USA. 3General, Emergency and Trauma Surgery Unit, Pisa University Hospital, Pisa, Italy. 4Infection Control Program, University of Geneva Hospitals and Faculty of Medicine, Geneva, Switzerland. 5Antimicrobial Stewardship Program, Department of Pharmacy, Jackson Health System, Miami, Florida, USA. 6Division of Infectious Diseases and Miami Transplant Institute, Department of Medicine, University of Miami Miller School of Medicine, Miami, Florida, USA. 7Research Institute of Epidemiology, Microbiology and Infectious Diseases, Tashkent, Republic of Uzbekistan. 8Addis Ababa University, College of Health Sciences, Center for Innovative Drug Development and Therapeutic Trials for Africa (CDT-Africa), Addis Ababa, Ethiopia. 9School of Health Sciences, University of Dundee, Dundee, UK. 10The Research Office, College of Medicine and Health Sciences, United Arab Emirates University, Al-Ain, United Arab Emirates. 11Nuffield Department of Population Health, University of Oxford, Oxford, UK. 12Global Health Focus, Kigali, Rwanda. 13Department of Surgery and Surgical Specialties, Zinder National Hospital, Faculty of Health Sciences, University of Zinder, Niger. 14Enhancing Primary Health Care Services Project, Representative Office of the Swiss Tropical and Public Health Institute, Dushanbe, Tajikistan. 15General Surgery Department, Regional Hospital of Korce, Albania. 16Department of Microbiology, Faculty of Medicine, Kuwait University, Kuwait. 17Microbiology Unit, Department of Laboratories, Farwania Hospital, Farwania, Kuwait. 18Department of Internal Medicine, University of South Carolina School of Medicine, Columbia, South Carolina, USA. 19Department of Internal Medicine, Rehman Medical Institute, Peshawar, Pakistan. 20Department of Surgery, Weill Cornell Medical College, Doha, Qatar. 21Acute Care Surgery, Hamad General Hospital, Doha, Qatar. 22Infectious Diseases Division, Internal Medicine Department, American University of Beirut Medical Center, Beirut, Lebanon. 23Department of Infectious Diseases, University of Gothenburg, Gothenburg, Sweden. 24Department of Microbiology, National Institute of Health, Islamabad, Pakistan. 25Department of Pharmacy Practice, Faculty of Pharmacy and Pharmaceutical Sciences, College of Health Sciences, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana. 26Department of General Surgery, Faculty of Medicine, Jordan University of Science and Technology, Irbid, Jordan. 27Department of General and Emergency Surgery, Fondazione IRCCS San Matteo, Pavia, Italy. 28Faculty of Health Sciences, Abu Dhabi Women’s College, Higher Colleges of Technology, Abu Dhabi, United Arab Emirates. 29Infectious Diseases Department, Hospital Santo Tomas, Avenida Balboa, Panama City, Panama. 30School of Medicine, University of Zagreb, Zagreb, Croatia. 31Department of Surgery, University Hospital Centre Zagreb, Zagreb, Croatia. 32Medical Laboratory, Ekomdoum Baptist Hospital Yaounde, Yaounde, Cameroon. 33Department of Surgery, Yas Clinic Hospital, Khalifa City, Abu Dhabi, United Arab Emirates. 34Universitè Gamal Abdel Nasser, Conakry, Guinea. 35Acute Care Surgery and Trauma Unit, Department of General Surgery, Hadassah Medical Center and Faculty of Medicine, Hebrew University of Jerusalem Kiriat Hadassah, Jerusalem, Israel. 36Department of Surgery, National Hospital of Sri Lanka, Colombo, Sri Lanka. 37Department of Surgery, Dirghayu Pokhara Hospital, Pokhara, Nepal. 38Department of Health Sciences (DISSAL), University of Genoa, Genoa, Italy. 39Unit of infectious diseases, IRCCS Ospedale Policlinico San Martino, Genoa, Italy. 40Clinica Reñaca, Viña Del Mar, Chile. 41Department of Surgery, University of Minnesota, Minneapolis, Minnesota, USA. 42Department of Surgery, Madda Walabu University Goba Referral Hospital, Bala-Robe, Ethiopia. 43Human Pathology Biomedicine and Environment Laboratory, Faculty of Medicine and Pharmacy, Sidi Mohammed Ben Abdellah University, Fez, Morocco. 44Department of Infectious Diseases, University Medical Centre Ljubljana, Ljubljana, Slovenia. 45Faculty of Medicine, University of Ljubljana, Ljubljana, Slovenia. 46Hospital do Coração, Sao Paulo, Brazil. 47Department of Control, Surveillance and Prevention of Antimicrobial Resistance, World Health Organization, Geneva, Switzerland. 48Division of Trauma and Acute Care Surgery, Scripps Clinic Medical Group, La Jolla, California, USA. 49Department of Internal Medicine and Pediatrics, Faculty of Medicine and Health Sciences, Ghent University, Ghent, Belgium. 50UQ Centre for Clinical Research, The University of Queensland, Brisbane, Australia. 51Department of Surgery, Amsterdam Gastroenterology and Metabolism, Amsterdam UMC, University of Amsterdam, Amsterdam, The Netherlands. 52Research Service, VA Northeast Ohio Healthcare System, Cleveland, Ohio, USA. 53Case Western Reserve University-Cleveland VA Medical Center for Antimicrobial Resistance and Epidemiology (Case VA CARES), Cleveland, Ohio, USA. 54Division of Medical Microbiology, Department of Pathology, Institute of Infectious Disease and Molecular Medicine, Faculty of Health Sciences, University of Cape Town, Cape Town, South Africa. 55Department of Medicine, University of Udine, Udine, Italy 56Gulu University, Faculty of Medicine, Global Surgery Unit, Laroo, Uganda. 57Department of Surgery, Hospital Clinico Universitario, IDIS, University of Santiago de Compostela, Spain. 58Department of Infectious Diseases, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán (INCMyNSZ), Mexico City, Mexico. 59Servicio de Microbiología, Hospital Universitario Ramón y Cajal, Instituto Ramón y Cajal de Investigación Sanitaria (IRYCIS), Madrid, Spain. 60CIBER en Enfermedades Infecciosas (CIBERINFEC), Instituto de Salud Carlos III, Madrid, Spain. 61Infectious and Tropical Disease Unit, AOU Policlinico "P. Giaccone", Palermo, Italy. 62Department of Health Promotion, Mother and Child Care, Internal Medicine and Medical Specialties "G. D'Alessandro", University of Palermo, Palermo, Italy. 63Cantonal Doctor Office, Public Health Department, Canton of Vaud, Lausanne, Switzerland 64Infection Prevention and Control Unit, Infectious Diseases Service, Lausanne University Hospital, Lausanne, Switzerland. 65NIHR Health Protection Research Unit in Healthcare Associated Infections and Antimicrobial Resistance, Imperial College London, London, UK. 66College of Business, Arts, and Social Sciences, Brunel University, London, UK. 67Global Health Group, University of Balearic Islands, Palma, Spain. 68General Surgery Unit, Sandro Pertini Hospital, ASL Roma 2, Roma, Italy. 69UCL Global Business School for Health, London, UK. 70Infectious Diseases Unit, Clemenceau Medical Center Hospital, Dubai, United Arab Emirates. 71Department of Pharmacology & Clinical Pharmacology, Christian Medical College, Vellore, India. 72National Institute for Health Research Health Protection Research Unit in Healthcare Associated Infections and Antimicrobial Resistance, Imperial College London, London, UK. 73Department of Surgery, School of Medicine, University of Louisville, Louisville, KY, USA. 74Kenyatta National Hospital, Nairobi, Kenya. 75Pharmacy Department, Kamuzu University of Health Sciences (KUHES), Blantyre, Malawi. 76Center for Infectious Disease Research and Policy, Antimicrobial Stewardship Project. University of Minnesota. Minneapolis, Minnesota, USA. 77Department of Microbiology, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong Semi-Autonomous Republic, China. 78Department of Microbiology, Queen Mary Hospital, Hong Kong SAR, China. 79Division of Pharmacy and Medicines, Luxembourg Health Directorate-Direction de la santé, Luxembourg, Grand Duchy of Luxembourg. 80Clinical Hospital of Pneumophthisiology and Infectious Diseases, Brasov, Romania. 81Faculty of Medicine, Transylvania University of Brasov, Brasov, Romania. 82Department of Surgery, Riverside University Health System Medical Center, Loma Linda University, Loma Linda, California, USA. 83Emergency Surgery Unit, San Filippo Neri Hospital, Roma, Italy. 84Department of Surgery, Tianjin Nankai Hospital, Nankai Clinical School of Medicine, Tianjin Medical University, Tianjin, China. 85Department of Infectious Diseases, University Hospital in Krakow, Krakow, Poland. 86Department of Infectious and Tropical Diseases, Jagiellonian University Medical College, Krakow, Poland. 87South-Eastern Europe Health Network (SEEHN), Skopje, North Macedonia. 88The World Bank, Washington, District of Columbia, USA. 89Clinic for Surgery, University Clinical Centre of Tuzla, Bosnia and Herzegovina. 90Department of Surgery, University of Washington, Seattle, Washington, USA. 91Department of Surgery, Tbilisi State Medical University, Tblisi, Georgia. 92Forensic Medicine and Integrated Risk Management Unit, Azienda Ospedaliero-Universitaria di Bologna, Bologna, Italy. 93Directorate of Healthcare Quality and Safety, Ministry of Health, Sri Jayawardenapura Kotte, Sri Lanka. 94Digestive and Metabolic Minimally Invasive Surgery Unit, Clinique Saint Louis, Poissy, Poissy, Ile de France, France. 95Department of Intensive Care Medicine, Ghent University Hospital, Ghent, Belgium. 96Department of Pharmacy Practice, National Institute of Pharmaceutical Education and Research (NIPER), Hajipur, India. 97Division of Acute Care Surgery, University of South Florida/Tampa General Hospitall, Tampa, Florida, USA. 98National Institute of Public Health, Bucharest, Romania. 99Research Institute, McGill University Health Centre, Montreal, Canada. 100School of Pharmacy, University of Health and Allied Sciences, Ho, Ghana. 101Quality Use of Medicines and Pharmacy Research Centre, Clinical and Health Sciences, University of South Australia, Adelaide, Australia. 102Mongolian National University of Medical Sciences, Ulaanbaatar, Mongolia. 103Department of Surgery, Medical City Plano, Plano, Texas, USA. 104Department of General, Visceral and Thoracic Surgery, Klinikum Hann. Munden Academic Hospital of Goettingen University, Hann. Munden, Germany. 105Department of Bacteriology, Noguchi Memorial Institute for Medical Research, College of Health Sciences, University of Ghana, Legon, Ghana. 106National Public Health Laboratory, Khartoum, Sudan. 107Infectious Diseases Section, King Fahad Medical City, Riyadh, Saudi Arabia. 108Department of Infectious Diseases and Clinical Microbiology, School of Medicine, Koç University, Istanbul, Turkiye. 109Koç University İşbank Center for Infectious Diseases, Koç University, Istanbul, Turkiye. 110Direction of First Level, Municipal Secretary of Health, Municipal Autonomous Government of Cochabamba, Cochabamba, Bolivia. 111Division of Infectious Diseases and International Medicine, University of Minnesota Medical School, Minneapolis, Minnesota, USA. 112Lagos State Health Service Commission, Lagos, Nigeria. 113Department of Pathology, General Hospital Odan, Lagos, Nigeria. 114Department of Pharmacology and Therapeutics, College of Medicine, Ekiti State University, Ado-Ekiti, Nigeria. 115Dipartimento di Scienze di Laboratorio e Infettivologiche, Fondazione Policlinico Universitario Agostino Gemelli IRCSS, Rome, Italy. 116Infectious Diseases and Tropical Medicine Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran. 117General and Trauma Surgery Division, Hospital das Clínicas, School of Medicine, São Paulo State University, Brazil. 118Department of Surgery, University of Buenos Aires, Buenos Aires, Argentina. 119Department of Gastroenterology and Hepatology, Cleveland Clinic, Cleveland, Ohio, USA. 120Clínica Foianini, Santa Cruz de la Sierra, Santa Cruz, Bolivia. 121Department of Surgery, Northwestern University Feinberg School of Medicine, Chicago, Illinois, USA. 122Division of Trauma and Acute Care Surgery, Department of Surgery, Department of Intensive Care, Fundación Valle del Lili, Cali, Colombia. 123Division of Trauma and Acute Care Surgery, Department of Surgery, Universidad del Valle, Cali, Colombia. 124Istituto di Ricerche Farmacologiche "Mario Negri" IRCCS, 20156 Milan, Italy. 125Department of Surgery, Mansoura Faculty of Medicine, Mansoura University, Mansoura, Egypt. 126First Department of Internal Medicine-Infectious Diseases, Hygeia General Hospital, Athens, Greece. 127Faculty of Medicine and Health Care, Al-Farabi Kazakh National University, Almaty, Kazakhstan. 128Department of Surgery, Medical School, National and Kapodistrian University of Athens, "Aretaieio" Hospital, Athens, Greece. 129Department of Pharmacy, The Ohio State University Wexner Medical Center, Ohio State University College of Pharmacy, Columbus, Ohio, USA. 130Office of Medical Education and Center for Infectious Diseases, International University of Health and Welfare School of Medicine, Narita, Chiba, Japan. 131Department of Infectious Diseases, Landspitali University Hospital, Reykjavik, Iceland. 132Faculty of Medicine, School of Health Sciences, University of Iceland, Reykjavik, Iceland. 133Department of Upper Gastrointestinal Surgery, Queen Elizabeth Hospital Birmingham, University Hospitals Birmingham NHS Trust, Birmingham, UK. 134Centro Médico Naval Cirujano Mayor Santiago Tavara, Callao, Peru. 135School of Medicine, Universidad Científica del Sur, Lima, Peru. 136Unit of Endocrine, Head, and Neck Surgery and Unit of Surgical Infections Support, Department of General Surgery, Parc Taulí Hospital Universitari, Sabadell, Spain. 137Rukamni Birla hospital, Jaipur, India. 138Faculty of Health Sciences, University of Buea, Buea, Cameroon. 139Institute of Hygiene and Environmental Medicine, Charité–Universitätsmedizin Berlin, Freie Universität Berlin, Humboldt‑Universitat zu Berlin, and Berlin Institute of Health, Berlin, Germany. 140Unit of Pharmacology, Faculty of Medicine and Defence Health, Universiti Pertahanan Nasional Malaysia, Kuala Lumpur, Malaysia. 141Department of Surgical Sciences, Nelson R Mandela School of Clinical Medicine, University of KwaZulu-Natal, and Inkosi Albert Luthuli Central Hospital, Durban, South Africa.. 142Molecular Epidemiology and Public Health Laboratory, Hopkirk Research Institute, Massey University, Palmerston North, New Zealand. 143Department of General and Thoracic Surgery, University Hospital of Giessen, Giessen, Germany. 144Department of Clinical Microbiology and Hygiene, Medilab, Academic Teaching Laboratories of the Paracelsus Medical University, Salzburg, Austria. 145Division of Trauma Surgery, Acute Care Surgery, Critical Care, and Burns, Department of Surgery, MetroHealth Medical Center, Cleveland, Ohio; Case Western Reserve University School of Medicine, Cleveland, Ohio, USA. 146Case Western Reserve University, Department of Population and Quantitative Health Sciences, Cleveland, Ohio, USA. 147Department of Surgery, Faculty of Medicine, University of Parakou, Parakou, Benin. 148Department of Surgery, Istanbul Medeniyet University, Turkiye. 149School of Optometry and Vision Science, University of New South Wales, Sydney, Australia. 150Department of Microbiology, Jahangirnagar University, Savar, Dhaka, Bangladesh. 151Department of Surgery, Veterans Affairs Boston Health Care System, Boston University Chobianian and Avedisian School of Medicine, and Harvard Medical School, Boston, Massachusetts, USA. 152Research Unit, Emergent Bacterial Resistance and Safety of Care UR12SP37, Laboratory of Microbiology, University Hospital Sahloul, Sousse, Tunisia. 153Department of Anesthesia and Intensive Care, Haukeland University Hospital, Bergen, Norway. 154Department of Clinical Microbiology, University Hospitals of Leicester NHS Trust, Leicester, UK. 155World Health Organization Country Office, Freetown, Sierra Leone. 156Department of Health Policy and Advocacy, Operation Smile, Virginia Beach, Virginia, USA. 157Department of Microbiology and Virology, School of Medicine, Iranshahr University of Medical Sciences, Iranshahr, Iran. 158Department of Anesthesiology, Section on Critical Care Medicine, Wake Forest Center for Biomedical Informatics, Perioperative Outcomes and Informatics Collaborative, Wake Forest University School of Medicine, Winston-Salem, North Carolina, USA. 159Outcomes Research Consortium, Cleveland, Ohio, USA. 160Division of Gastroenterology and Hepatology, Mayo Clinic, Rochester, Minnesota, USA. 161One Health Trust, Washington, District of Colombia, USA. 162Department of Microbiology, Gandhi Medical College, Bhopal, India. 163Centre for Microbiology Research, Kenya Medical Research Institute, Nairobi, Kenya. 164Adult Infectious Diseases, Department of Medicine, Royal Hospital, Muscat, Oman. 165Department of Emergency Surgery, City Hospital, Mozyr, Belarus. 166USAID Medicines, Technologies, and Pharmaceutical Services Program, Management Sciences for Health, Kampala, Uganda. 167Department of Pharmacology and Therapeutics, College of Health Sciences, Makerere University, Kampala, Uganda. 168Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. 169Department of Surgery, Jacobi Medical Center, Albert Einstein College of Medicine, New York, New York, USA. 170Departments of Surgery and Critical Care Medicine, University of Calgary, Foothills Medical Centre, Calgary, AB, Canada. 171Department of General Surgery, Rambam Medical Center, Haifa, Israel. 172Department of Internal Medicine, National Cheng Kung University Hospital, College of Medicine, National Cheng Kung University, Tainan, Taiwan. 173Department of Medicine, College of Medicine, National Cheng Kung University, Tainan, Taiwan. 174Pengiran Anak Puteri Rashidah Sa'adatul Bolkiah Institute of Health Sciences, Universiti Brunei Darussalam, Bandar Seri Begawan, Brunei. 175Department of General Surgery, Catholic University of Health and Allied Sciences, Bugando, Mwanza, Tanzania. 176One Health in Action Initiative, Bouaké, Ivory Coast. 177Department of Surgery, UMC Zvezdara, Belgrade, Serbia. 178Clinic of Infectious Diseases, University Clinical Center of Kosova, Prishtina, Kosovo. 179Department of Medical Microbiology, Second Faculty of Medicine, Charles University and Motol University Hospital, Prague, Czech Republic. 180Department of Surgery No.2, Kharkiv National Medical University, Kharkiv, Ukraine. 181Expert Stewardship, Inc., Newport Beach, California, USA. 182Department of Medical Microbiology, University of Ghana Medical School, , Accra, Ghana. 183Global Alliance for Infections in Surgery, Macerata, Italy. 184Department of Internal Medicine, College of Medicine and Allied Health Sciences, University of Sierra Leone, Freetown, Sierra Leone. 185South Pest Central Hospital, National Institute of Hematology and Infectious Diseases, Budapest, Hungary. 186Department of Internal Medicine and Hematology, Division of Infectology, Semmelweis University, Budapest, Hungary. 187Department of Clinical Epidemiology, University of the Philippines, Manila, Philippines. 188Department of Clinical Sciences, Ben and Maytee Fisch College of Pharmacy, University of Texas at Tyler, TX, USA. 189Department of Anaesthesia and Intensive Care Unit, Aix-Marseille University, AP-HM, North Hospital, Marseille, France. 190Department of Abdominal Surgery, Helsinki University Hospital and University of Helsinki, Helsinki, Finland. 191Unit of Infectious Diseases, Hospital Carlos G. Durand, Buenos Aires, Argentina. 192Department of Surgery, Immanuel Kant Baltic Federal University, Kaliningrad, Russia. 193Department of Surgery, Faculty of Medicine, Siriraj Hospital, Mahidol University, Bangkok, Thailand. 194Department of Surgery, Universidad Nacional de Asuncion, Asuncion, Paraguay. 195Department of Health Sciences, Faculty of Medicine and Health Sciences, University of Mauritius, Réduit, Mauritius. 196Department of Surgery, Harborview Medical Center, University of Washington, Seattle, Washington, USA. 197Faculty of Medical Sciences, The University of the West Indies, Cave Hill Campus, Bridgetown, Barbados. 198Department of Biological Sciences, School of Natural Sciences, University of Zambia, Lusaka, Zambia. 199Microbiology Unit, Faculty of Medicine and Health Sciences, University of Zimbabwe, Harare, Zimbabwe. 200Department of Microbiology, Maulana Azad Medical College, New Delhi, India. 201Clinical Research Unit, Hospital del Mar Medical Research Institute, Barcelona, Spain. 202Unit of Microbiology, University Hospital Reina Sofía, Córdoba, Spain. 203Department of Agricultural Chemistry, Edaphology and Microbiology, Maimonides Biomedical Research Institute of Cordoba, Córdoba, Spain. 204Department of Intensive Care Medicine, Multidisciplinary Intensive Care Research Organisation, St James's Hospital, Dublin, Ireland. 205Trinity College Dublin, Dublin, Ireland. 206Centro de Investigacion Biomedica En Red Entermedades Respiratorias, Institute of Health Carlos III, Madrid, Spain. 207Pulmonary Department, Hospital Clinic, Universitat de Barcelona, Barcelona, Spain. 208Pandit Bhagwat Dayal Sharma Postgraduate Institute of Medical Sciences, Rohtak, India. 209Department of Anesthesiology and Surgical Critical Care, Hospital Universitario La Paz, Madrid, Spain. 210Department of Surgery, Wolaita Sodo University, Sodo, Ethiopia. 211Section of Infectious Diseases, Department of Internal Medicine, Wake Forest University School of Medicine, Winston-Salem, North Carolina, USA. 212Department of Colorectal Surgery, Beaumont Hospital, Dublin, Ireland. 213Royal College of Surgeons, St. Stephen's Green, Dublin, Ireland. 214Al-Faisal University, Riyadh, Saudi Arabia. 215Ministry of Health, King Saud Medical City, Riyadh, Saudi Arabia. 216Hubert Department of Global Health, Rollins School of Public Health, Emory University, Atlanta, Georgia, USA. 217Department of Health Research Methods, Evidence, and Impact, McMaster University, Hamilton, Ontario, Canada. 218Department of Medicine, McMaster University, Hamilton, Ontario, Canada. 219Department of Microbiology, Tribhuvan University Teaching Hospital, Institute of Medicine, Kathmandu, Nepal. 220School of Optometry and Vision Science, Faculty of Medicine and Health, University of New South Wales, Sydney, Australia. 221Département d'anesthésie-réanimation, université de Paris, CHU Bichat-Claude Bernard, APHP, Paris, France. 222Italian Multidisciplinary Society for the Prevention of Healthcare-associated infections, Milan, Italy. 223Department of Health Policy, London School of Economics and Political Science, London, UK. 224Hospital da Criança Santo Antônio, Porto Alegre, Brazil. 225Department of Pharmacy, School of Health Sciences, University of Zambia, Lusaka, Zambia. 226Rinda Ubuzima Clinical Research Center, Kigali, Rwanda. 227Department of Medicine, Houston Methodist Hospital and Academic Institute, Houston, Texas, USA. 228Weill Cornell Medicine, New York, NY, USA 229Department of Surgery, University of Michigan Health System, Ann Arbor, Michigan, USA. 230Global Antimicrobial Stewardship Partnership Hub. British Society for Antimicrobial Chemotherapy, Birmingham, UK. 231Higher Teacher Training College, University of Bertoua, Cameroon 232Tropical and Infectious Diseases Division, Sheikh Shakhbout Medical City, Abu Dhabi, United Arab Emirates. 233Department of Surgery, School of Medicine, Trinity College, Dublin, Ireland. 234Centre for Integrated Health Programs, Lagos University Teaching Hospital, Lagos, Nigeria. 235Department of Clinical Microbiology, Rigshospitalet, University of Copenhagen, Copenhagen, Denmark. 236Costerton Biofilm Center, Department of Immunology and Microbiology, University of Copenhagen, Copenhagen, Denmark. 237Department of Surgery, Hospital Sotero Del Rio, Universidad Católica, Santiago, Chile. 238Emerging and Re-emerging Pathogens Laboratory, Sourô Sanou University Hospital Center, Bobo-Dioulasso, Burkina Faso. 239Bacteriology-Virology Department, Sourô Sanou University Hospital, Bobo-Dioulasso, Burkina Faso. 240Intensive Care Department, Centro Hospitalar Universitário São João, Porto, Portugal 241Department of Medicine, Faculty of Medicine, University of Porto, Portugal. 242Department of General and Emergency Surgery, Polytechnic University of Marche, Ancona, Italy. 243Unit of Infectious Diseases, ASST Cremona, Cremona, Italy. 244College of Medicine and Dentistry, James Cook University, Townsville, Australia. 245Australian Institute of Tropical Health and Medicine, Townsville, Australia. 246Fourth Department of Surgery, Faculty of Medicine, Comenius University Bratislava and University Hospital Bratislava, Slovakia. 247Emergency Department, University of Verona, Verona, Italy. 248Global Health Governance Program, Usher Institute, University of Edinburgh, Edinburgh, UK. 249School of Dentistry, Faculty of Medicine and Health, University of Leeds, Leeds, UK. 250Department of Medical and Surgical Sciences, Alma Mater Studiorum, University of Bologna, Bologna, Italy. 251Clinical Pharmacology Unit, Department for Integrated Infectious Risk Management, Azienda Ospedaliero-University di Bologna, Bologna, Italy. 252Department of Surgery, NYU Long Island School of Medicine, NYU Langone Hospital-Long Island, Mineola, New York, USA. 253Infection Prevention and Control, Infectious Disease Service, Fondazione Policlinico Universitario Campus Bio-Medico, Rome, Italy. 254Department of Abdominal Surgery, University Medical Center Ljubljana, Ljubljana, Slovenia. 255Faculty of Medicine, Riga Stradins University, Riga, Latvia. 256Department of General and Emergency Surgery, Riga East Clinical University Hospital, Latvia. 257Department of Surgical Science, Emergency Surgery Unit, University of Cagliari, Cagliari, Italy. 258Infectious Diseases Department, Instituto Nacional de Ciencias Médicas y Nutrición "Salvador Zubirán", Vasco de Quiroga 15, Mexico City, Mexico. 259Department of Geriatric Medicine, Worcestershire Acute Hospitals NHS Foundation Trust, Worcestershire, UK. 260Universidad Autónoma de Santo Domingo, Instituto Nacional del Cáncer, Santo Domingo, Dominican Republic. 261Laboratoire APEMAC, Centre Hospitalier Régional Universitaire de Nancy, and Centre regional en antibiothérapie du Grand Est, Université de Lorraine, Nancy, France. 262Department of General Surgery, Anadolu Medical Center Hospital, Kocaeli, Turkiye. 263Department of Digestive Surgery, CHU Amiens Picardie and University of Picardie Jules Verne, Amiens, France. 264Global Health eCore, Vall d’Hebron Institute of Research (VHIR), Ps. Vall d’Hebron 129, AMI-14, 08035, Barcelona, Spain. 265Unité de Recherche FOREVA, Réanimation Douleur Urgences, Centre Hospitalier Universitaire de Nîmes, Nîmes, France. 266Infectious Diseases Section, Hospital Regional de Taguatinga, Taguatinga, Brasília, Brazil. 267Department of Microbiology, The University of the West Indies, Mona, Jamaica. 268Infection Control, Hospital de Base, Brasília, Distrito Federal, Brazil. 269Department of Surgery, University of Minnesota, Minneapolis, Minnesota, USA. 270Infection and Antimicrobial Resistance Prevention and Control Unit, Centro Hospitalar Universitário São João, Porto, Portugal. 271International Nosocomial Infection Control Consortium (INICC) Foundation, Miami, FL, USA. 272Department of Microbiology and Virology, University of Florence, Florence, Italy. 273Microbiology and Virology Unit, Careggi University Hospital, Florence, Italy. 274Department of Internal Medicine, University of Botswana, Gaborone, Botswana. 275Wits School of Public Health, University of the Witwatersrand, Johannesburg, South Africa 276Ministry of Health, Directorate-General for Health Prevention, Rome, Italy. 277Department of Infectious Diseases, Italian National Institute of Health, Rome, Italy. 278Clinic of Surgery, Lithuanian University of Health Sciences, Kaunas, Lithuania. 279Department of Community Medicine and Public Health, Suez Canal University, Ismailia, Egypt. 280Hôpital DOGTA-LAFIE, Lomé, Togo. 281Pharmacology Department, School of Pharmacy, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia. 282 Pharmacy Department, College of Medicine and Health Sciences, Arba Minch University, Arba Minch, Ethiopia. 283General Surgery Department, Military Teaching Hospital, Dakar, Senegal. 284Drug Applied Research Center, Tabriz University of Medical Sciences, Tabriz, Iran. 285Research Institute at Medical University Plovdiv/University Hospital St George, Plovdiv, Bulgaria. 286Department of Surgery, Western Michigan University School of Medicine, Kalamazoo, Michigan, USA. 287General Surgery Unit, Santa Maria Annunziata & Serristori Hospital, Firenze, Italy. 288Department of Microbiology and Immunology, Weill Bugando School of Medicine, Catholic University of Health and Allied Sciences, Mwanza, Tanzania. 289Department of Population Medicine, Harvard Medical School/Harvard Pilgrim Health Care Institute, Boston, Masachusetts, USA. 290Department of Internal Medicine, Texas A&M University, Houston, Texas, USA. 291Emergency Surgery and Trauma-Fondazione Policlinico Universitario "A. Gemelli," Catholic University of Sacred Heart, Rome, Italy. 292Department of Surgery, Nordsjaellands University Hospital, Hilleroed, Denmark. 293Lee Kong Chian School of Medicine, Nanyang Technological University, Novena, Singapore. 294Department of General Surgery, Tan Tock Seng Hospital, Novena, Singapore. 295Department of Medical Laboratory Sciences, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia. 296Department of Emergency Medicine, Ziekenhuis Geel, Geel, Belgium; Faculty of Medicine and Health Sciences, University of Antwerp, Wilrijk, Belgium. 297Faculty of Medicine, University of Leuven, Leuven, Belgium; Center for Research and Education in Emergency Care, University of Leuven, Leuven, Belgium. 298Institut Pasteur of Algeria, Algiers, Algeria. 299Department of Biomedical and Biotechnological Sciences, University of Catania, Catania, Italy. 300Division of Infectious Diseases, Department of Diagnostics and Public Health, University of Verona, Verona, Italy. 301Intensive Care Unit, Saint Joseph-Saint Luc Hospital, Lyon, France. 302Infectious Diseases and Intensive Care Unit, Pontchaillou University Hospital, Rennes, France. 303Hospital Central de Las Fuerzas Armadas, Santo Domingo, Dominican Republic. 304Infectious Diseases Department, AC Camargo Cancer Center, São Paulo, Brazil 305Departemnt of Surgery, Saturnino Oral Provincial Hospital, Santiago de Cuba, Cuba. 306Division of Infectious Diseases and Geographic Medicine, University of Texas Southwestern Medical Center, Dallas, Texas, USA. 307Department of Anesthesia, Bachmai University Hospital, Hanoi, Vietnam. 308Division of Ethics of Medicine, Medical Faculty, University of Augsburg, Augsburg, Germany. 309Medical and Infectious Diseases ICU, APHP Bichat Hospital F, Paris, France. 310Infection, Antimicrobials, Modelling, Evolution. French Institute for Medical Research, University of Paris, Paris, France. 311Anesthesiology and Critical Care Units, Douala Laquintinie Hospital, Douala, Cameroon. 312Institute of Microbiology, Biological and Environmental Sciences College, University San Francisco de Quito, Quito, Ecuador. 313School of Medicine, European University Cyprus, Nicosia, Cyprus. 314Unit of Antimicrobial Stewardship, Local Health Authority, City of Bologna, Bologna, Italy. 315Laboratory of Emerging Infectious Diseases, School of Medicine, Pontifícia Universidade Católica do Paraná, Curitiba, Paraná, Brazil. 316First Department of Surgery, First Faculty of Medicine, Charles University in Prague and General University Hospital in Prague, Prague, Czech Republic. 317Section for Surgical Research, Department of Surgery, Medical University of Graz, Graz, Austria. 318AMR Insights, Amsterdam, The Netherlands. 319Department of Surgery, Radboud University Medical Center, Nijmegen, The Netherlands. 320Division of Trauma, Emergency Surgery, and Surgical Critical Care, Department of Surgery, Massachusetts General Hospital, Boston, Massachusetts, USA. 321Department of Surgery, Medical School, University of Pecs, Pecs, Hungary. 322Department of Anesthesiology, Neuro-Intensive Care Unit, Careggi University Hospital, Florence, Italy. 323Department of Medical and Surgical Sciences, University of Bologna, S. Orsola-Malpighi Hospital, Bologna, Italy. 324Infectious Diseases Unit, Department for Integrated Infectious Risk Management, Istituto di Ricovero e Cura a Carattere Scientifico, Azienda Ospedaliero-Universitaria di Bologna, Bologna, Italy. 325Department of Clinical Microbiology, Center for Biomedical Diagnosis, Hospital Clinic-Universitat de Barcelona, Barcelona, Spain. 326Department of Basic Clinical Practice, School of Medicine, University of Barcelona, Barcelona, Spain. 327Barcelona Institute for Global Health, Barcelona, Spain. 328Department of Medical Microbiology and Infection Prevention, University Medical Center, Groningen, The Netherlands. 329Clinical Microbiology Department, Dr. Andrija Štampar Teaching Institute of Public Health, Zagreb, Croatia. 330Medical Microbiology Department, School of Medicine, University of Zagreb, Zagreb, Croatia 331Division of Infectious Diseases, Department of Medicine, Northeast Ohio Medical University, Rootstown, Ohio, USA. 332Coast General Teaching and Referral Hospital, Mombasa, Kenya. 333Antimicrobial Stewardship Committee, Prof. Dr. R.D. Kandou Central General Hospital, Manado, Indonesia. 334Division of Infectious Diseases, Hospital Rudolfstiftung, Wien, Austria. 335The National Chamber of Innovative Healthcare of the Republic of Uzbekistan, Tashkent, Uzbekistan. 336Department of Medical Microbiology and Parasitology, Faculty of Basic Clinical Sciences, College of Health Sciences, Usmanu Danfodiyo University, Sokoto, Nigeria. 337General Surgery Department, Zliten Medical Center, Zliten, Libya. 338State Key Laboratory for Diagnosis and Treatment of Infectious Diseases, National Clinical Research Center for Infectious Diseases, Collaborative Innovation Center for Diagnosis and Treatment of Infectious Diseases, The First Affiliated Hospital, School of Medicine, Zhejiang University, Hangzhou, China. 339Department of Surgery, School of Medical Sciences, Universiti Sains Malaysia, Health Campus, Kota Bharu, Malaysia. 340Section of Trauma and Acute Care Surgery, Department of Surgery, University of Chicago, Chicago, Illinois, USA. 341Universidad Peruana Cayetano Heredia, Facultad de Salud Pública y Administración, Lima, Peru. 342Institute of Global Health Innovation, St. Mary's Hospital, Imperial College London, London, UK. 343Antimicrobial Stewardship Project, Provincial Hospital of Bolzano, Bolzano, Italy. 344Department of Surgery, “Bufalini” Hospital, Cesena, Italy.
Abbreviations
- AMR
Antimicrobial resistance
- ASPs
Antimicrobial Stewardship Programs
- CDC
Centers for Disease Control and Prevention
- CDI
Clostridioides difficile infection
- COVID-19
Coronavirus disease 2019
- CRAB
Carbapenem-resistant Acinetobacter baumannii
- CRE
Carbapenem-resistant enterobacterales
- CRPA
Carbapenem-resistant Pseudomonas aeruginosa
- DDD
Defined daily doses
- ECDC
European Centre for Disease Prevention and Control
- EDs
Emergency departments
- GLASS
Global antimicrobial resistance and use surveillance system
- HAIs
Hospital-acquired infections
- HAP
Hospital-acquired pneumonia
- HCWs
Healthcare workers
- Hib
Haemophilus influenzae type B
- ICU
Intensive care unit
- IDSA
Infectious Diseases Society of America
- IPC
Infection prevention and control
- LMICs
Low- and middle-income countries
- MDR
Multidrug-resistant
- MIC
Minimal inhibitory concentration
- MRSA
Methicillin-resistant Staphylococcus. aureus
- NAPs
National action plans
- PCT
Procalcitonin
- PD
Pharmacodynamics
- PDR
Pan-drug-resistant
- PK
Pharmacokinetics
- RCTs
Randomized controlled trials
- SAP
Surgical antibiotic prophylaxis
- SARS-CoV-2
Severe acute respiratory syndrome coronavirus-2
- SHEA
Society for Healthcare Epidemiology of America
- SSIs
Surgical site infections
- VAP
Ventilator-associated pneumonia
- WHO
World Health Organization
- XDR
Extensively drug-resistant
Author contributions
MS wrote the original draft. PSB provided English-language editing. All authors were contributors in reviewing and editing the manuscript. All authors read and approved the final manuscript.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Worldwide Antimicrobial Resistance National/International Network Group (WARNING) Collaborators:
Massimo Sartelli, Philip S. Barie, Federico Coccolini, Mohamed Abbas, Lilian M. Abbo, Gulnora K. Abdukhalilova, Yishak Abraham, Salisu Abubakar, Fikri M. Abu-Zidan, Yusuff Adebayo Adebisi, Harissou Adamou, Gulara Afandiyeva, Ervis Agastra, Wadha A. Alfouzan, Majdi N. Al-Hasan, Sajjad Ali, Syed Muhammad Ali, Fatima Allaw, Gbemisola Allwell-Brown, Afreenish Amir, Obed Kwabena Offe Amponsah, Abdelkarim Al Omari, Luca Ansaloni, Shamshul Ansari, Ana Belen Arauz, Goran Augustin, Bih Awazi, Mohammad Azfar, Mamadou Saliou Bailo Bah, Miklosh Bala, Anura S. K. Banagala, Suman Baral, Matteo Bassetti, Luis Bavestrello, Gregory Beilman, Kebebe Bekele, Moussa Benboubker, Bojana Beović, Maria Daniela Bergamasco, Silvia Bertagnolio, Walter L. Biffl, Stijn Blot, Marja A. Boermeester, Robert A. Bonomo, Adrian Brink, Silvio Brusaferro, Jonathan Butemba, Miguel A. Caínzos, Adrian Camacho-Ortiz, Rafael Canton, Antonio Cascio, Alessandro Cassini, Enrique Cástro-Sanchez, Marco Catarci, Rodolfo Catena, Leili Chamani-Tabriz, Sujith J. Chandy, Esmita Charani, William G. Cheadle, Diana Chebet, Ibrahim Chikowe, Francesca Chiara, Vincent Chi-Chung Cheng, Anna Chioti, Maria Elena Cocuz, Raul Coimbra, Francesco Cortese, Yunfeng Cui, Jacek Czepiel, Mira Dasic, Nataliya de Francisco Serpa, Stijn W. de Jonge, Samir Delibegovic, E. Patchen Dellinger, Zaza Demetrashvili, Alessandra De Palma, Danushka De Silva, Belinda De Simone, Jan De Waele, Sameer Dhingra, Jose J. Diaz, Claudia Dima, Natalia Dirani, Cornelius C. Dodoo, Gereltuya Dorj, Therese M. Duane, Christian Eckmann, Beverly Egyir, Mutasim M. Elmangory, Mushira A. Enani, Onder Ergonul, Juan Pablo Escalera-Antezana, Kevin Escandon, Abdul-Wahab Omo-ope Ettu, Joseph O. Fadare, Massimo Fantoni, Mohammad Farahbakhsh, Mario Paulo Faro, Alberto Ferreres, Gianina Flocco, Esteban Foianini, Donald E. Fry, Alberto Federico Garcia, Chiara Gerardi, Wagih Ghannam, Helen Giamarellou, Natalya Glushkova, George Gkiokas, Debra A. Goff, Harumi Gomi, Magnus Gottfredsson, Ewen A. Griffiths, Rosio Isabel Guerra Gronerth, Xavier Guirao, Yogesh K. Gupta, Gregory Halle-Ekane, Sonja Hansen, Mainul Haque, Timothy C. Hardcastle, David T. S. Hayman, Andreas Hecker, Markus Hell, Vanessa P. Ho, Adrien M. Hodonou, Arda Isik, Salequl Islam, Kamal M. F. Itani, Nadia Jaidane, Ib Jammer, David R. Jenkins, Ibrahim Franklyn Kamara, Souha S. Kanj, Desmond Jumbam, Masoud Keikha, Ashish K. Khanna, Sahil Khanna, Gaetanjali Kapoor, Garima Kapoor, Samuel Kariuki, Faryal Khamis, Vladimir Khokha, Reuben Kiggundu, Ronald Kiguba, Hong Bin Kim, Peter K. Kim, Andrew W. Kirkpatrick, Yoram Kluger, Wen-Chien Ko, Kenneth Y. Y. Kok, Vihar Kotecha, Ibrahima Kouma, Bojan Kovacevic, Jehona Krasniqi, Marcela Krutova, Igor Kryvoruchko, Ravina Kullar, Kwaku A. Labi, Francesco M. Labricciosa, Sulaiman Lakoh, Botond Lakatos, Mary Ann D. Lansang, Ramanan Laxminarayan, Young Ran Lee, Marc Leone, Ari Leppaniemi, Gabriel Levy Hara, Andrey Litvin, Varut Lohsiriwat, Gustavo M. Machain, Fawzi Mahomoodally, Ronald V. Maier, Md Anwarul Azim Majumder, Sydney Malama, Justen Manasa, Vikas Manchanda, Ramiro Manzano-Nunez, Luis Martínez-Martínez, Ignacio Martin-Loeches, Sanjay Marwah, Emilio Maseda, Maleda Mathewos, Ryan C. Maves, Deborah McNamara, Ziad Memish, Dominik Mertz, Shyam Kumar Mishra, Philippe Montravers, Maria Luisa Moro, Elias Mossialos, Fabrizio Motta, Steward Mudenda, Patrick Mugabi, Mc Juan Muco Mugisha, Eleftherios Mylonakis, Lena M. Napolitano, Dilip Nathwani, Leontine Nkamba, Emmanuel Fru Nsutebu, Donal B. O’Connor, Sade Ogunsola, Peter Østrup Jensen, Juliana Maria Ordoñez, Carlos A. Ordoñez, Pablo Ottolino, Abdoul-Salam Ouedraogo, José Artur Paiva, Miriam Palmieri, Angelo Pan, Narayan Pant, Arpád Panyko, Ciro Paolillo, Jay Patel, Federico Pea, Patrizio Petrone, Nicola Petrosillo, Tadeja Pintar, Haralds Plaudis, Mauro Podda, Alfredo Ponce-de-Leon, Susan L. Powell, Adrián Puello-Guerrero, Celine Pulcini, Kemal Rasa, Jean-Marc Regimbeau, Jordi Rello, Manuel Renato Retamozo-Palacios, Glendee Reynolds-Campbell, Julival Ribeiro, Jennifer Rickard, Nuno Rocha-Pereira, Victor D. Rosenthal, Gian Maria Rossolini, Godfrey M. Rwegerera, Megan Rwigamba, Michela Sabbatucci, Žilvinas Saladžinskas, Rasha E. Salama, Tondore Sali, Samson Sahile Salile, Ibrahima Sall, Hossein Samadi Kafil, Boris E. Sakakushev, Robert G. Sawyer, Marco Scatizzi, Jeremiah Seni, Edward J. Septimus, Gabriele Sganga, Daniel Mønsted Shabanzadeh, Vishal G. Shelat, Agumas Shibabaw, Francis Somville, Selma Souf, Stefania Stefani, Evelina Tacconelli, Buon Kim Tan, Pierre Tattevin, Carlos Rodriguez-Taveras, João Paulo Telles, Orlando Téllez-Almenares, Jeffrey Tessier, Nguyen Toan Thang, Cristian Timmermann, Jean-François Timsit, Joel Noutakdie Tochie, Matti Tolonen, Gabriel Trueba, Constantinos Tsioutis, Fabio Tumietto, Felipe Francisco Tuon, Jan Ulrych, Selman Uranues, Maarten van Dongen, Harry van Goor, George C. Velmahos, Andras Vereczkei, Bruno Viaggi, Pierluigi Viale, Jordi Vila, Andreas Voss, Jasmina Vraneš, Richard R. Watkins, Nyambura Wanjiru-Korir, Olivia Waworuntu, Agnes Wechsler-Fördös, Klara Yadgarova, Mohammed Yahaya, Ali I. Yahya, Yonghong Xiao, Andee Dzulkarnaen Zakaria, Tanya L. Zakrison, Victor Zamora Mesia, Walter Siquini, Ara Darzi, Leonardo Pagani, and Fausto Catena
References
- 1.Anonymous A global declaration on appropriate use of antimicrobial agents across the surgical pathway. Surg Infect (Larchmt) 2017;18(8):846–853. doi: 10.1089/sur.2017.219. [DOI] [PubMed] [Google Scholar]
- 2.Charani E, McKee M, Ahmad R, Balasegaram M, Bonaconsa C, Merrett GB, et al. Optimising antimicrobial use in humans-review of current evidence and an interdisciplinary consensus on key priorities for research. Lancet Reg Health Eur. 2021;7:100161. doi: 10.1016/j.lanepe.2021.100161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.International Pharmaceutical Federation (FIP). 2009 FIP global pharmacy workforce report. 2009. https://www.fip.org/files/fip/publications/2009_FIP_Global_Pharmacy_Workforce_Report.pdf. Accessed 12 July 2023.
- 4.Dhingra S, Rahman NAA, Peile E, Rahman M, Sartelli M, Hassali MA, et al. Microbial resistance movements: an overview of global public health threats posed by antimicrobial resistance, and how best to counter. Front Public Health. 2020;8:535668. doi: 10.3389/fpubh.2020.535668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dutescu IA, Hillier SA. Encouraging the development of new antibiotics: Are financial incentives the right way forward? A systematic review and case study. Infect Drug Resist. 2021;14:415–434. doi: 10.2147/IDR.S287792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Renwick M, Mossialos E. What are the economic barriers of antibiotic R&D and how can we overcome them? Expert Opin Drug Discov. 2018;13(10):889–892. doi: 10.1080/17460441.2018.1515908. [DOI] [PubMed] [Google Scholar]
- 7.Renwick MJ, Brogan DM, Mossialos E. A systematic review and critical assessment of incentive strategies for discovery and development of novel antibiotics. J Antibiot (Tokyo) 2016;69(2):73–88. doi: 10.1038/ja.2015.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jamrozik E, Selgelid M, editors. Ethics and drug resistance: collective responsibility for global public health. Heidelberg: Springer; 2020. [Google Scholar]
- 9.Plachouras D, Kärki T, Hansen S, Hopkins S, Lyytikäinen O, Moro ML, Point Prevalence Survey Study Group et al. Antimicrobial use in European acute care hospitals: Results from the second point prevalence survey (PPS) of healthcare-associated infections and antimicrobial use, 2016 to 2017. Euro Surveill. 2018;23(46):1800393. doi: 10.2807/1560-7917.ES.23.46.1800393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fridkin S, Baggs J, Fagan R, Magill S, Pollack LA, Malpiedi P, Centers for Disease Control and Prevention (CDC) et al. Vital signs: improving antibiotic use among hospitalized patients. MMWR Morb Mortal Wkly Rep. 2014;63(9):194–200. [PMC free article] [PubMed] [Google Scholar]
- 11.Geller AI, Lovegrove MC, Shehab N, Hicks LA, Sapiano MRP, Budnitz DS. National estimates of emergency department visits for antibiotic adverse events among adults-United States, 2011–2015. J Gen Intern Med. 2018;33(7):1060–1068. doi: 10.1007/s11606-018-4430-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bauer KA, Kullar R, Gilchrist M, File TM., Jr Antibiotics and adverse events: the role of antimicrobial stewardship programs in 'doing no harm'. Curr Opin Infect Dis. 2019;32(6):553–558. doi: 10.1097/QCO.0000000000000604. [DOI] [PubMed] [Google Scholar]
- 13.Tamma PD, Avdic E, Li DX, Dzintars K, Cosgrove SE. Association of adverse events with antibiotic use in hospitalized patients. JAMA Intern Med. 2017;177(9):1308–1315. doi: 10.1001/jamainternmed.2018.6226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Silva ML, Cargnello C, Aulois-Griot M, Dumartin C. Antibiotic misuse: How to evaluate the costs? Med Mal Infect. 2019;49(7):485–494. doi: 10.1016/j.medmal.2019.03.012. [DOI] [PubMed] [Google Scholar]
- 15.Baur D, Gladstone BP, Burkert F, Carrara E, Foschi F, Döbele S, et al. Effect of antibiotic stewardship on the incidence of infection and colonisation with antibiotic-resistant bacteria and Clostridium difficile infection: a systematic review and meta-analysis. Lancet Infect Dis. 2017;17(9):990–1001. doi: 10.1016/S1473-3099(17)30325-0. [DOI] [PubMed] [Google Scholar]
- 16.Global Alliance for Infections in Surgery. https://www.infectionsinsurgery.org. Accessed 12 July 2023.
- 17.Dahiya S, Chhillar AK, Sharma N, Choudhary P, Punia A, Balhara M, et al. Candida auris and nosocomial infection. Curr Drug Targets. 2020;21(4):365–373. doi: 10.2174/1389450120666190924155631. [DOI] [PubMed] [Google Scholar]
- 18.Dubey AK, Singla RK. Perspectives on anti-Candida drug development. Curr Top Med Chem. 2019;19:2375–2376. doi: 10.2174/156802661928191206162925. [DOI] [PubMed] [Google Scholar]
- 19.Vassilopoulos S, Mylonakis E. Avenues for antifungal drug discovery and development: Where to now? Expert Opin Drug Discov. 2022;17:667–672. doi: 10.1080/17460441.2022.2098950. [DOI] [PubMed] [Google Scholar]
- 20.CDC. Antibiotic resistance threats in the United States, 2019. Atlanta: U.S. Department of Health and Human Services, CDC; 2019. www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-report-508.pdf. Accessed 12 July 2023.
- 21.Lyman M, Forsberg K, Sexton DJ, Chow NA, Lockhart SR, Jackson BR, et al. Worsening spread of Candida auris in the United States, 2019 to 2021. Ann Intern Med. 2023;176(4):489–495. doi: 10.7326/M22-3469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Satoh K, Makimura K, Hasumi Y, Nishiyama Y, Uchida K, Yamaguchi H. Candida auris sp. Nov., a novel ascomycetous yeast isolated from the external ear canal of an inpatient in a Japanese hospital. Microbiol Immunol. 2009;53:41–44. doi: 10.1111/j.1348-0421.2008.00083.x. [DOI] [PubMed] [Google Scholar]
- 23.Kim MN, Shin JH, Sung H, Lee K, Kim EC, Ryoo N, et al. Candida haemulonii and closely related species at 5 university hospitals in Korea: identification, antifungal susceptibility, and clinical features. Clin Infect Dis. 2009;48:e57–e61. doi: 10.1086/597108. [DOI] [PubMed] [Google Scholar]
- 24.van Schalkwyk E, Mpembe RS, Thomas J, Shuping L, Ismail H, Lowman W, GERMS-SA et al. Epidemiologic shift in candidemia driven by Candida auris, South Africa, 2016–2017. Emerg Infect Dis. 2019;25:1698–1707. doi: 10.3201/eid2509.190040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vallabhaneni S, Kallen A, Tsay S, Chow N, Welsh R, Kerins J, et al. Investigation of the first seven reported cases of Candida auris, a globally emerging invasive, multidrug-resistant fungus-United States, May 2013-August 2016. Am J Transplant. 2017;17:296–299. doi: 10.1111/ajt.14121. [DOI] [PubMed] [Google Scholar]
- 26.Borman AM, Szekely A, Johnson EM. Comparative pathogenicity of United Kingdom isolates of the emerging pathogen Candida auris and other key pathogenic Candida species. mSphere. 2016;1(4):e00189–e216. doi: 10.1128/mSphere.00189-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cortegiani A, Misseri G, Fasciana T, Giammanco A, Giarratano A, Chowdhary A. Epidemiology, clinical characteristics, resistance, and treatment of infections by Candida auris. J Intensive Care. 2018;6:69. doi: 10.1186/s40560-018-0342-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spivak ES, Hanson KE. Candida auris: an emerging fungal pathogen. J Clin Microbiol. 2018;56(2):e01588–e1617. doi: 10.1128/JCM.01588-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kean R, Brown J, Gulmez D, Ware A, Ramage G. Candida auris: a decade of understanding of an enigmatic pathogenic yeast. J Fungi (Basel) 2020;6(1):30. doi: 10.3390/jof6010030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee WG, Shin JH, Uh Y, Kang MG, Kim SH, Park KH, et al. First three reported cases of nosocomial fungemia caused by Candida auris. J Clin Microbiol. 2011;49(9):3139–3142. doi: 10.1128/JCM.00319-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rossato L, Colombo AL. Candida auris: What have we learned about its mechanisms of pathogenicity? Front Microbiol. 2018;9:3081. doi: 10.3389/fmicb.2018.03081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yue H, Bing J, Zheng Q, Zhang Y, Hu T, Du H, et al. Filamentation in Candida auris, an emerging fungal pathogen of humans: passage through the mammalian body induces a heritable phenotypic switch. Emerg Microbes Infect. 2018;7(1):188. doi: 10.1038/s41426-018-0187-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mayer FL, Wilson D, Hube B. Candida albicans pathogenicity mechanisms. Virulence. 2013;4(2):119–128. doi: 10.4161/viru.22913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sartelli M, Weber DG, Ruppé E, Bassetti M, Wright BJ, Ansaloni L, et al. Antimicrobials: a global alliance for optimizing their rational use in intra-abdominal infections (AGORA) World J Emerg Surg. 2016;11:33. doi: 10.1186/s13017-016-0089-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.El-Halfawy OM, Valvano MA. Antimicrobial heteroresistance: an emerging field in need of clarity. Clin Microbiol Rev. 2015;28(1):191–207. doi: 10.1128/CMR.00058-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Andersson DI, Nicoloff H, Hjort K. Mechanisms and clinical relevance of bacterial heteroresistance. Nat Rev Microbiol. 2019;17(8):479–496. doi: 10.1038/s41579-019-0218-1. [DOI] [PubMed] [Google Scholar]
- 37.Roca I, Akova M, Baquero F, Carlet J, Cavaleri M, Coenen S, et al. The global threat of antimicrobial resistance: science for intervention. New Microbes New Infect. 2015;6:22–29. doi: 10.1016/j.nmni.2015.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rice LB. Federal funding for the study of antimicrobial resistance in nosocomial pathogens: No ESKAPE. J Infect Dis. 2008;197(8):1079–1081. doi: 10.1086/533452. [DOI] [PubMed] [Google Scholar]
- 39.Boucher HW, Talbot GH, Bradley JS, Edwards JE, Gilbert D, Rice LB, et al. Bad bugs, no drugs: No ESKAPE! An update from the Infectious Diseases Society of America. Clin Infect Dis. 2009;48:1–12. doi: 10.1086/595011. [DOI] [PubMed] [Google Scholar]
- 40.Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268–281. doi: 10.1111/j.1469-0691.2011.03570.x. [DOI] [PubMed] [Google Scholar]
- 41.Kadri SS, Adjemian J, Lai YL, Spaulding AB, Ricotta E, Prevots DR, National Institutes of Health Antimicrobial Resistance Outcomes Research Initiative (NIH–ARORI) et al. Difficult-to-treat resistance in gram-negative bacteremia at 173 US hospitals: Retrospective cohort analysis of prevalence, predictors, and outcome of resistance to all first-line agents. Clin Infect Dis. 2018;67(12):1803–1814. doi: 10.1093/cid/ciy378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Iskandar K, Molinier L, Hallit S, Sartelli M, Catena F, Coccolini F, et al. Drivers of antibiotic resistance transmission in low- and middle-income countries from a "one health" perspective-a review. Antibiotics (Basel) 2020;9(7):372. doi: 10.3390/antibiotics9070372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hollis A, Maybarduk P. Antibiotic resistance is a tragedy of the commons that necessitates global cooperation. J Law Med Ethics. 2015;43(Suppl 3):33–37. doi: 10.1111/jlme.12272. [DOI] [PubMed] [Google Scholar]
- 44.One Health High-Level Expert Panel (OHHLEP) Adisasmito WB, Almuhairi S, Behravesh CB, Bilivogui P, Bukachi SA, et al. One Health: A new definition for a sustainable and healthy future. PLoS Pathog. 2022;18(6):e1010537. doi: 10.1371/journal.ppat.1010537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Venter H, Henningsen ML, Begg SL. Antimicrobial resistance in healthcare, agriculture and the environment: the biochemistry behind the headlines. Essays Biochem. 2017;61(1):1–10. doi: 10.1042/EBC20160053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Crisci E. From open access to circular health: Ilaria Capua's journey through science and politics. Viruses. 2022;14(6):1296. doi: 10.3390/v14061296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Boudreau LeBlanc A, Williams-Jones B, Aenishaenslin C. Bioethics and one health: a case study approach to building reflexive governance. Front Public Health. 2022;18:311. doi: 10.3389/fpubh.2022.648593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Laxminarayan R, Duse A, Wattal C, Zaidi AK, Wertheim HF, Sumpradit N, et al. Antibiotic resistance-the need for global solutions. Lancet Infect Dis. 2013;13(12):1057–1098. doi: 10.1016/s1473-3099(13)70318-9. [DOI] [PubMed] [Google Scholar]
- 49.WHO. World Health Organization global action plan on antimicrobial resistance. 2015. https://www.who.int/publications/i/item/9789241509763. Accessed 12 July 2023. [DOI] [PubMed]
- 50.Charani E, Mendelson M, Pallett SJC, Ahmad R, Mpundu M, Mbamalu O, et al. An analysis of existing national action plans for antimicrobial resistance-gaps and opportunities in strategies optimising antibiotic use in human populations. Lancet Glob Health. 2023;11(3):e466–e474. doi: 10.1016/S2214-109X(23)00019-0. [DOI] [PubMed] [Google Scholar]
- 51.Patel J, Harant A, Fernandes G, Mwamelo AJ, Hein W, Dekker D, et al. Measuring the global response to antimicrobial resistance, 2020–21: a systematic governance analysis of 114 countries. Lancet Infect Dis. 2023;3(6):706–718. doi: 10.1016/S1473-3099(22)00796-4. [DOI] [PubMed] [Google Scholar]
- 52.Patel J, Sridhar D. The pandemic legacy of antimicrobial resistance in the USA. Lancet Microbe. 2022;3(10):e726–e727. doi: 10.1016/S2666-5247(22)00227-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nandi A, Pecetta S, Bloom DE. Global antibiotic use during the COVID-19 pandemic: analysis of pharmaceutical sales data from 71 countries, 2020–2022. EClinicalMedicine. 2023;57:101848. doi: 10.1016/j.eclinm.2023.101848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Langford BJ, So M, Simeonova M, Leung V, Lo J, Kan T, et al. Antimicrobial resistance in patients with COVID-19: a systematic review and meta-analysis. Lancet Microbe. 2023;4(3):e179–e191. doi: 10.1016/S2666-5247(22)00355-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Brink AJ, Richards G, Tootla H, Prentice E. Epidemiology of Gram-negative bacteria during coronavirus disease 2019. What is the real pandemic? Curr Opin Infect Dis. 2022;35(6):595–604. doi: 10.1097/QCO.0000000000000864. [DOI] [PubMed] [Google Scholar]
- 56.Langford BJ, Soucy JR, Leung V, So M, Kwan ATH, Portnoff JS, et al. Antibiotic resistance associated with the COVID-19 pandemic: a systematic review and meta-analysis. Clin Microbiol Infect. 2022 doi: 10.1016/j.cmi.2022.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Antimicrobial Resistance Collaborators Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022;399(10325):629–655. doi: 10.1016/S0140-6736(21)02724-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Laxminarayan R. The overlooked pandemic of antimicrobial resistance. Lancet. 2022;399(10325):606–607. doi: 10.1016/S0140-6736(22)00087-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Makoka MH, Miller WC, Hoffman IF, Cholera R, Gilligan PH, Kamwendo D, et al. Bacterial infections in Lilongwe, Malawi: Aetiology and antibiotic resistance. BMC Infect Dis. 2012;12:67. doi: 10.1186/1471-2334-12-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ouedraogo AS, Jean Pierre H, Bañuls AL, Ouédraogo R, Godreuil S. Emergence and spread of antibiotic resistance in West Africa: contributing factors and threat assessment. Med Sante Trop. 2017;27(2):147–154. doi: 10.1684/mst.2017.0678. [DOI] [PubMed] [Google Scholar]
- 61.Lancet T. Redefining vulnerability in the era of COVID-19. Lancet. 2020;395(10230):1089. doi: 10.1016/S0140-6736(20)30757-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Alividza V, Mariano V, Ahmad R, Charani E, Rawson TM, Holmes AH, et al. Investigating the impact of poverty on colonization and infection with drug-resistant organisms in humans: a systematic review. Infect Dis Poverty. 2018;7(1):76. doi: 10.1186/s40249-018-0459-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Holmes AH, Sharland M. The Chennai Declaration: India's landmark national commitment to antibiotic stewardship demonstrates that 'truth alone triumphs'. J Antimicrob Chemother. 2013;68(7):1453–1454. doi: 10.1093/jac/dkt062. [DOI] [PubMed] [Google Scholar]
- 64.O’Neill J. Tackling drug-resistant infections globally: final report and recommendations. The review on antimicrobial resistance. 2016. https://amr-review.org/sites/default/files/160525_Final%20paper_with%20cover.pdf. Accessed 12 July 2023.
- 65.Jonas O, Irwin A, Berthe FCJ, Le Gall FG, Marquez PV. Drug-resistant infections: a threat to our economic future (vol 2): final report (English). HNP/Agriculture Global Antimicrobial Resistance Initiative Washington, D.C.: World Bank Group. http://documents.worldbank.org/curated/en/323311493396993758/final-report. Accessed 12 July 2023.
- 66.de Kraker ME, Stewardson AJ, Harbarth S. Will 10 million people die a year due to antimicrobial resistance by 2050? PLoS Med. 2016;13(11):e1002184. doi: 10.1371/journal.pmed.1002184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Global Health Hub Germany. Results of the G7 health ministers’ meeting in Berlin, 19–20 May 2022. https://www.globalhealthhub.de/de/news/detail/g7-health-ministers-unite-to-secure-a-healthy-future-results-of-the-g7-health-ministers-meeting-in-berlin-may-19-20-2022. Accessed 12 July 2023
- 68.Anderson M, Schulze K, Cassini A, Plachouras D, Mossialos E. A governance framework for development and assessment of national action plans on antimicrobial resistance. Lancet Infect Dis. 2019;19(11):e371–e384. doi: 10.1016/S1473-3099(19)30415-3. [DOI] [PubMed] [Google Scholar]
- 69.Kiggundu R, Lusaya E, Seni J, Waswa JP, Kakooza F, Tjipura D, et al. Identifying and addressing challenges to antimicrobial use surveillance in the human health sector in low- and middle-income countries: experiences and lessons learned from Tanzania and Uganda. Antimicrob Resist Infect Control. 2023;12(1):9. doi: 10.1186/s13756-023-01213-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ren M, So AD, Chandy SJ, Mpundu M, Peralta AQ, Åkerfeldt K, et al. Equitable access to antibiotics: a core element and shared global responsibility for pandemic preparedness and response. J Law Med Ethics. 2022;50(S2):34–39. doi: 10.1017/jme.2022.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Broom A, Kenny K, Prainsack B, Broom J. Antimicrobial resistance as a problem of values? Views from three continents. Crit Public Health. 2021;31(4):451–463. doi: 10.1080/09581596.2020.1725444. [DOI] [Google Scholar]
- 72.Council of the EU and the European Council. Tackling antimicrobial resistance: council adopts recommendation. https://www.consilium.europa.eu/en/press/press-releases/2023/06/13/tackling-antimicrobial-resistance-council-adopts-recommendation/. Accessed 12 July 2023.
- 73.Ndaki PM, Mushi MF, Mwanga JR, Konje ET, Ntinginya NE, Mmbaga BT, et al. Dispensing antibiotics without prescription at community pharmacies and accredited drug dispensing outlets in Tanzania: a cross-sectional study. Antibiotics (Basel) 2021;10(8):1025. doi: 10.3390/antibiotics10081025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kaprou GD, Bergšpica I, Alexa EA, Alvarez-Ordóñez A, Prieto M. Rapid methods for antimicrobial resistance diagnostics. Antibiotics (Basel) 2021;10(2):209. doi: 10.3390/antibiotics10020209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Charani E, Ahmad R, Rawson TM, Castro-Sanchèz E, Tarrant C, Holmes AH. The differences in antibiotic decision-making between acute surgical and acute medical teams: an ethnographic study of culture and team dynamics. Clin Infect Dis. 2019;69(1):12–20. doi: 10.1093/cid/ciy844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cantón R, Horcajada JP, Oliver A, Garbajosa PR, Vila J. Inappropriate use of antibiotics in hospitals: the complex relationship between antibiotic use and antimicrobial resistance. Enferm Infecc Microbiol Clin. 2013;31(Suppl 4):3–11. doi: 10.1016/S0213-005X(13)70126-5. [DOI] [PubMed] [Google Scholar]
- 77.Levy Hara G, Rojas-Cortés R, Molina León HF, Dreser Mansilla A, Alfonso Orta I, Rizo-Amezquita JN, et al. Point prevalence survey of antibiotic use in hospitals in Latin American countries. J Antimicrob Chemother. 2022;77(3):807–815. doi: 10.1093/jac/dkab459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sartelli M, Duane TM, Catena F, Tessier JM, Coccolini F, Kao LS, et al. Antimicrobial stewardship: a call to action for surgeons. Surg Infect (Larchmt) 2016;17(6):625–631. doi: 10.1089/sur.2016.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Goff DA, Kullar R, Goldstein EJC, Gilchrist M, Nathwani D, Cheng AC, et al. A global call from five countries to collaborate in antibiotic stewardship: United we succeed, divided we might fail. Lancet Infect Dis. 2017;17(2):e56–e63. doi: 10.1016/S1473-3099(16)30386-3. [DOI] [PubMed] [Google Scholar]
- 80.Doron S, Davidson LE. Antimicrobial stewardship. Mayo Clin Proc. 2011;86(11):1113–1123. doi: 10.4065/mcp.2011.0358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Dyar OJ, Huttner B, Schouten J, Pulcini C, ESGAP (ESCMID Study Group for Antimicrobial stewardshiP) What is antimicrobial stewardship? Clin Microbiol Infect. 2017;23(11):793–798. doi: 10.1016/j.cmi.2017.08.026. [DOI] [PubMed] [Google Scholar]
- 82.Kpokiri EE, Ladva M, Dodoo CC, Orman E, Aku TA, Mensah A, et al. Knowledge, awareness and practice with antimicrobial stewardship programmes among healthcare providers in a Ghanaian tertiary hospital. Antibiotics (Basel) 2021;11(1):6. doi: 10.3390/antibiotics11010006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Retamar P, Rodríguez-Baño J. A step forward in the definition of antimicrobial stewardship indicators: better measurements, better work. Farm Hosp. 2019;43(3):77–78. doi: 10.7399/fh.11238. [DOI] [PubMed] [Google Scholar]
- 84.Dryden M, Johnson AP, Ashiru-Oredope D, Sharland M. Using antibiotics responsibly: right drug, right time, right dose, right duration. J Antimicrob Chemother. 2011;66(11):2441–2443. doi: 10.1093/jac/dkr370. [DOI] [PubMed] [Google Scholar]
- 85.Kakkar AK, Shafiq N, Singh G, Ray P, Gautam V, Agarwal R, et al. Antimicrobial stewardship programs in resource constrained environments: understanding and addressing the need of the systems. Front Public Health. 2020;8:140. doi: 10.3389/fpubh.2020.00140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Godman B, Egwuenu A, Haque M, Malande OO, Schellack N, Kumar S, et al. Strategies to improve antimicrobial utilization with a special focus on developing countries. Life (Basel) 2021;11(6):528. doi: 10.3390/life11060528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Dyar OJ, Moran-Gilad J, Greub G, Pulcini C, ESGMD Executive Committee and the ESGAP Executive Committee Diagnostic stewardship: Are we using the right term? Clin Microbiol Infect. 2019;25(3):272–273. doi: 10.1016/j.cmi.2018.12.011. [DOI] [PubMed] [Google Scholar]
- 88.Patel R, Fang FC. Diagnostic stewardship: opportunity for a laboratory-infectious diseases partnership. Clin Infect Dis. 2018;67(5):799–801. doi: 10.1093/cid/ciy077.\. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Dellit TH, Owens RC, McGowan JE, Jr, Gerding DN, Weinstein RA, Burke JP, et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis. 2007;44(2):159–177. doi: 10.1086/510393. [DOI] [PubMed] [Google Scholar]
- 90.Vieceli T, Rello J. Optimization of antimicrobial prescription in the hospital. Eur J Intern Med. 2022;106:39–44. doi: 10.1016/j.ejim.2022.08.035. [DOI] [PubMed] [Google Scholar]
- 91.Safdar N, Abad C. Educational interventions for prevention of healthcare-associated infection: a systematic review. Crit Care Med. 2008;36(3):933–940. doi: 10.1097/CCM.0B013E318165FAF3. [DOI] [PubMed] [Google Scholar]
- 92.Ward DJ. The role of education in the prevention and control of infection: a review of the literature. Nurse Educ Today. 2011;31(1):9–17. doi: 10.1016/j.nedt.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 93.Carlet J, Astagneau P, Brun-Buisson C, Coignard B, Salomon V, Tran B, French National Program for Prevention of Healthcare-Associated Infections and Antimicrobial Resistance et al. French national program for prevention of healthcare-associated infections and antimicrobial resistance, 1992–2008: positive trends, but perseverance needed. Infect Control Hosp Epidemiol. 2009;30(8):737–745. doi: 10.1086/598682. [DOI] [PubMed] [Google Scholar]
- 94.Alhumaid S, Al Mutair A, Al Alawi Z, Alsuliman M, Ahmed GY, Rabaan AA, et al. Knowledge of infection prevention and control among healthcare workers and factors influencing compliance: a systematic review. Antimicrob Resist Infect Control. 2021;10(1):86. doi: 10.1186/s13756-021-00957-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sartelli M, Pagani L, Iannazzo S, Moro ML, Viale P, Pan A, et al. A proposal for a comprehensive approach to infections across the surgical pathway. World J Emerg Surg. 2020;15(1):13. doi: 10.1186/s13017-020-00295-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sartelli M, Labricciosa FM, Coccolini F, Coimbra R, Abu-Zidan FM, Ansaloni L, et al. It is time to define an organizational model for the prevention and management of infections along the surgical pathway: a worldwide cross-sectional survey. World J Emerg Surg. 2022;17(1):17. doi: 10.1186/s13017-020-00295-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Cassini A, Högberg LD, Plachouras D, Quattrocchi A, Hoxha A, Simonsen GS, Burden of AMR Collaborative Group et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: A population-level modelling analysis. Lancet Infect Dis. 2019;19(1):56–66. doi: 10.1016/S1473-3099(18)30605-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Suetens C, Latour K, Kärki T, Ricchizzi E, Kinross P, Moro ML, et al. Prevalence of healthcare-associated infections, estimated incidence and composite antimicrobial resistance index in acute care hospitals and long-term care facilities: results from two European point prevalence surveys, 2016 to 2017. Euro Surveill. 2018;23(46):1800516. doi: 10.2807/1560-7917.ES.2018.23.46.1800516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Cassini A, Plachouras D, Eckmanns T, Abu Sin M, Blank HP, Ducomble T, et al. Burden of six healthcare-associated infections on European population health: estimating incidence-based disability-adjusted life years through a population prevalence-based modelling study. PLoS Med. 2016;13(10):e1002150. doi: 10.1371/journal.pmed.1002150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Schreiber PW, Sax H, Wolfensberger A, Clack L, Kuster SP, Swissnoso The preventable proportion of healthcare-associated infections 2005–2016: systematic review and meta-analysis. Infect Control Hosp Epidemiol. 2018;39:1277–1295. doi: 10.1017/ice.2018.183. [DOI] [PubMed] [Google Scholar]
- 101.World Health Organization. WHO guidelines on hand hygiene in health care. Geneva: World Health Organization; 2009. https://www.who.int/publications/i/item/9789241597906. Accessed 12 July 2023.
- 102.Boyce JM, Pittet D, Healthcare Infection Control Practices Advisory Committee. HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force Guideline for hand hygiene in health-care settings. Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Society for Healthcare Epidemiology of America/Association for Professionals in Infection Control/Infectious Diseases Society of America. MMWR Recomm Rep. 2002;51(16):1–45. [PubMed] [Google Scholar]
- 103.Glowicz JB, Landon E, Sickbert-Bennett EE, Aiello AE, deKay K, Hoffmann KK, et al. SHEA/IDSA/APIC practice recommendation: strategies to prevent healthcare-associated infections through hand hygiene: 2022 Update. Infect Control Hosp Epidemiol. 2023;44(3):355–376. doi: 10.1017/ice.2022.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Sax H, Allegranzi B, Uçkay I, Larson E, Boyce J, Pittet D. 'My five moments for hand hygiene': a user-centred design approach to understand, train, monitor and report hand hygiene. J Hosp Infect. 2007;67(1):9–21. doi: 10.1016/j.jhin.2015.04.011. [DOI] [PubMed] [Google Scholar]
- 105.Erasmus V, Daha TJ, Brug H, Richardus JH, Behrendt MD, Vos MC, et al. Systematic review of studies on compliance with hand hygiene guidelines in hospital care. Infect Control Hosp Epidemiol. 2010;31(3):283–294. doi: 10.1086/650451. [DOI] [PubMed] [Google Scholar]
- 106.Kirk J, Kendall A, Marx JF, Pincock T, Young E, Hughes JM, Landers T. Point of care hand hygiene-where's the rub? A survey of US and Canadian health care workers' knowledge, attitudes, and practices. Am J Infect Control. 2016;44(10):1095–1101. doi: 10.1016/j.ajic.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 107.Allegranzi B, Zayed B, Bischoff P, Kubilay NZ, de Jonge S, de Vries F, et al. New WHO recommendations on intraoperative and postoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis. 2016;16:e288–303. doi: 10.1016/S1473-3099(16)30402-9. [DOI] [PubMed] [Google Scholar]
- 108.Allegranzi B, Bischoff P, de Jonge S, Kubilay NZ, Zayed B, Gomes SM, et al. New WHO recommendations on preoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis. 2016;16:e276–287. doi: 10.1016/S1473-3099(16)30398-X. [DOI] [PubMed] [Google Scholar]
- 109.Berríos-Torres SI, Umscheid CA, Bratzler DW, Leas B, Stone EC, Kelz RR, et al. Centers for Disease Control and Prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg. 2017;152:784–791. doi: 10.1001/jamasurg.2017.0904. [DOI] [PubMed] [Google Scholar]
- 110.World Health Organization. Guidelines on core components of infection prevention and control programmes at the national and acute health care facility level. Geneva: World Health Organization; 2016. https://apps.who.int/iris/handle/10665/251730. Accessed 12 July 2023. [PubMed]
- 111.Storr J, Twyman A, Zingg W, Damani N, Kilpatrick C, Reilly J, et al. Core components for effective infection prevention and control programmes: new WHO evidence-based recommendations. Antimicrob Resist Infect Control. 2017;6:6. doi: 10.1186/s13756-016-0149-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Sydnor ER, Perl TM. Hospital epidemiology and infection control in acute-care settings. Clin Microbiol Rev. 2011;24(1):141–173. doi: 10.1128/CMR.00027-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Zingg W, Holmes A, Dettenkofer M, Goetting T, Secci F, Clack L, et al. Hospital organisation, management, and structure for prevention of health-care-associated infection: a systematic review and expert consensus. Lancet Infect Dis. 2015;15(2):212–224. doi: 10.1016/S1473-3099(14)70854-0. [DOI] [PubMed] [Google Scholar]
- 114.Tomczyk S, Twyman A, de Kraker MEA, Coutinho Rehse AP, Tartari E, Toledo JP, et al. The first WHO global survey on infection prevention and control in health-care facilities. Lancet Infect Dis. 2022;22(6):845–856. doi: 10.1016/S1473-3099(21)00809-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Brink AJ, Richards GA. Antimicrobial stewardship: leveraging the "butterfly effect" of hand hygiene. Antibiotics (Basel) 2022;11(10):1348. doi: 10.3390/antibiotics11101348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Mills JP, Marchaim D. Multidrug-resistant gram-negative bacteria: infection prevention and control update. Infect Dis Clin N Am. 2021;35(4):969–994. doi: 10.1016/j.idc.2021.08.001. [DOI] [PubMed] [Google Scholar]
- 117.Guidelines for the prevention and control of carbapenem-resistant Enterobacteriaceae, Acinetobacter baumannii and Pseudomonas aeruginosa in health care facilities. Geneva: World Health Organization; 2017. https://www.ncbi.nlm.nih.gov/books/NBK493061/. Accessed 12 July 2023. [PubMed]
- 118.Tomczyk S, Zanichelli V, Grayson ML, Twyman A, Abbas M, Pires D, et al. Control of carbapenem-resistant Enterobacteriaceae, Acinetobacter baumannii, and Pseudomonas aeruginosa in healthcare facilities: a systematic review and reanalysis of quasi-experimental studies. Clin Infect Dis. 2019;68(5):873–884. doi: 10.1093/cid/ciy752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Micoli F, Bagnoli F, Rappuoli R, Serruto D. The role of vaccines in combatting antimicrobial resistance. Nat Rev Microbiol. 2021;19(5):287–302. doi: 10.1038/s41579-020-00506-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Merakou C, Schaefers MM, Priebe GP. Progress toward the elusive Pseudomonas aeruginosa vaccine. Surg Infect (Larchmt) 2018;19(8):757–768. doi: 10.1089/sur.2018.233. [DOI] [PubMed] [Google Scholar]
- 121.Barie PS, Narayan M, Sawyer RG. Immunization against Staphylococcus aureus infections. Surg Infect (Larchmt) 2018;19(8):750–756. doi: 10.1089/sur.2018.263. [DOI] [PubMed] [Google Scholar]
- 122.Sihvonen R, Siira L, Toropainen M, Kuusela P, Patari-Sampo A. Streptococcus pneumoniae antimicrobial resistance decreased in the Helsinki metropolitan area after routine 10-valent pneumococcal conjugate vaccination of infants in Finland. Eur J Clin Microbiol Infect Dis. 2017;36:2109–2116. doi: 10.1007/s10096-017-3033-5. [DOI] [PubMed] [Google Scholar]
- 123.Jansen KU, Anderson AS. The role of vaccines in fighting antimicrobial resistance (AMR) Hum Vaccin Immunother. 2018;14(9):2142–2149. doi: 10.1080/21645515.2018.1476814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Tekle YI, Nielsen KM, Liu J, Pettigrew MM, Meyers LA, Galvani AP, et al. Controlling antimicrobial resistance through targeted, vaccine-induced replacement of strains. PLoS ONE. 2012;7:e50688. doi: 10.1371/journal.pone.0050688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Mina MJ, Kula T, Leng Y, Li M, de Vries RD, Knip M, et al. Measles virus infection diminishes preexisting antibodies that offer protection from other pathogens. Science. 2019;366(6465):599–606. doi: 10.1126/science.aay6485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Dionne B, Dehority W, Brett M, Howdieshell TR. The asplenic patient: post-insult immunocompetence, infection, and vaccination. Surg Infect (Larchmt) 2017;18(5):536–544. doi: 10.1089/sur.2016.267. [DOI] [PubMed] [Google Scholar]
- 127.Gabutti G. Available evidence and potential for vaccines for reduction in antibiotic prescriptions. Hum Vaccin Immunother. 2022;18(7):2151291. doi: 10.1080/21645515.2022.2151291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Kim S, Covington A, Pamer EG. The intestinal microbiota: antibiotics, colonization resistance, and enteric pathogens. Immunol Rev. 2017;279(1):90–105. doi: 10.1111/imr.12563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Donskey CJ. Antibiotic regimens and intestinal colonization with antibiotic-resistant gram-negative bacilli. Clin Infect Dis. 2006;43(Suppl 2):S62–S69. doi: 10.1086/504481. [DOI] [PubMed] [Google Scholar]
- 130.Salyers AA, Gupta A, Wang Y. Human intestinal bacteria as reservoirs for antibiotic resistance genes. Trends Microbiol. 2004;12:412–416. doi: 10.1016/j.tim.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 131.Bhalla A, Pultz NJ, Ray AJ, Hoyen CK, Eckstein EC, Donskey CJ. Antianaerobic antibiotic therapy promotes overgrowth of antibiotic-resistant, gram-negative bacilli and vancomycin-resistant enterococci in the stool of colonized patients. Infect Control Hosp Epidemiol. 2003;24(9):644–649. doi: 10.1086/502267. [DOI] [PubMed] [Google Scholar]
- 132.Donskey CJ, Chowdhry TK, Hecker MT, Hoyen CK, Hanrahan JA, Hujer AM, et al. Effect of antibiotic therapy on the density of vancomycin-resistant enterococci in the stool of colonized patients. N Engl J Med. 2000;343(26):1925–1932. doi: 10.1056/NEJM200012283432604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Taur Y, Xavier JB, Lipuma L, Ubeda C, Goldberg J, Gobourne A, et al. Intestinal domination and the risk of bacteremia in patients undergoing allogeneic hematopoietic stem cell transplantation. Clin Infect Dis. 2012;55(7):905–914. doi: 10.1093/cid/cis580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Ruppé E, Lixandru B, Cojocaru R, Büke C, Paramythiotou E, Angebault C, et al. Relative fecal abundance of extended-spectrum-β-lactamase-producing Escherichia coli strains and their occurrence in urinary tract infections in women. Antimicrob Agents Chemother. 2013;57(9):4512–4517. doi: 10.1128/AAC.00238-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Rashid MU, Zaura E, Buijs MJ, Keijser BJ, Crielaard W, Nord CE, et al. Determining the long-term effect of antibiotic administration on the human normal intestinal microbiota using culture and pyrosequencing methods. Clin Infect Dis. 2015;60(Suppl 2):S77–S84. doi: 10.1093/cid/civ137. [DOI] [PubMed] [Google Scholar]
- 136.Lindgren M, Lofmark S, Edlund C, Huovinen P, Jalava J. Prolonged impact of a one-week course of clindamycin on Enterococcus spp. in human normal microbiota. Scand J Infect Dis. 2009;41(3):215–219. doi: 10.1080/00365540802651897. [DOI] [PubMed] [Google Scholar]
- 137.Patangia DV, Anthony Ryan C, Dempsey E, Paul Ross R, Stanton C. Impact of antibiotics on the human microbiome and consequences for host health. Microbiol Open. 2022;11(1):e1260. doi: 10.1002/mbo3.1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.De La Cochetière MF, Durand T, Lepage P, Bourreille A, Galmiche JP, Doré J. Resilience of the dominant human fecal microbiota upon short-course antibiotic challenge. J Clin Microbiol. 2005;43(11):5588–5592. doi: 10.1128/JCM.43.11.5588-5592.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Dethlefsen L, Huse S, Sogin ML, Relman DA. The pervasive effects of an antibiotic on the human gut microbiota, as revealed by deep 16S rRNA sequencing. PLoS Biol. 2008;6(11):e280. doi: 10.1371/journal.pbio.0060280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Raymond F, Ouameur AA, Déraspe M, Iqbal N, Gingras H, Dridi B, et al. The initial state of the human gut microbiome determines its reshaping by antibiotics. ISME J. 2016;10(3):707–720. doi: 10.1038/ismej.2015.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Zhang L, Huang Y, Zhou Y, Buckley T, Wang HH. Antibiotic administration routes significantly influence the levels of antibiotic resistance in gut microbiota. Antimicrob Agents Chemother. 2013;57(8):3659–3666. doi: 10.1128/AAC.00670-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Solbach P, Chhatwal P, Woltemate S, Tacconelli E, Buhl M, Autenrieth IB, et al. Microbiota-associated risk factors for Clostridioides difficile acquisition in hospitalized patients: a prospective, multicentric study. Clin Infect Dis. 2021;73(9):e2625–e2634. doi: 10.1093/cid/ciaa871. [DOI] [PubMed] [Google Scholar]
- 143.Aguilar RC, Salmanton-García J, Carney J, Böll B, Kochanek M, Jazmati N, et al. Clostridioides difficile infections in the intensive care unit: a monocentric cohort study. Infection. 2020;48(3):421–427. doi: 10.1007/s15010-020-01413-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Sartelli M, Di Bella S, McFarland LV, Khanna S, Furuya-Kanamori L, Abuzeid N, et al. 2019 update of the WSES guidelines for management of Clostridioides (Clostridium) difficile infection in surgical patients. World J Emerg Surg. 2019;14:8. doi: 10.1186/s13017-015-0033-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Farrell RJ, LaMont JT. Pathogenesis and clinical manifestations of Clostridium difficile diarrhea and colitis. Curr Top Microbiol Immunol. 2000;250:109–125. doi: 10.1007/978-3-662-06272-2_6. [DOI] [PubMed] [Google Scholar]
- 146.Britton RA, Young VB. Role of the intestinal microbiota in resistance to colonization by Clostridium difficile. Gastroenterology. 2014;146(6):1547–1553. doi: 10.1053/j.gastro.2014.01.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Kachrimanidou M, Tsintarakis E. Insights into the role of human gut microbiota in Clostridioides difficile infection. Microorganisms. 2020;8(2):200. doi: 10.3390/microorganisms8020200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter PG, Bolon MK, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Surg Infect (Larchmt) 2013;14(1):73–156. doi: 10.1089/sur.2013.9999. [DOI] [PubMed] [Google Scholar]
- 149.Sartelli M, Boermeester MA, Cainzos M, Coccolini F, de Jonge SW, Rasa K, et al. Six long-standing questions about antibiotic prophylaxis in surgery. Antibiotics (Basel) 2023;12(5):908. doi: 10.3390/antibiotics12050908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Yin Y, Song T, Liao B, Luo Q, Zhou Z. Antibiotic prophylaxis in patients undergoing open mesh repair of inguinal hernia: a meta-analysis. Am Surg. 2012;78:359–365. doi: 10.1177/000313481207800348. [DOI] [PubMed] [Google Scholar]
- 151.Al Riyees L, Al Madani W, Firwana N, Balkhy HH, Ferwana M, Alkhudhayri A. Antibiotic prophylaxis against surgical site infection after open hernia surgery: a systematic review and meta-analysis. Eur Surg Res. 2021;62:121–133. doi: 10.1159/000517404. [DOI] [PubMed] [Google Scholar]
- 152.Erdas E, Medas F, Pisano G, Nicolosi A, Calò PG. Antibiotic prophylaxis for open mesh repair of groin hernia: systematic review and meta-analysis. Hernia. 2016;20:765–776. doi: 10.1007/s10029-016-1536-0. [DOI] [PubMed] [Google Scholar]
- 153.Orelio CC, van Hessen C, Sanchez-Manuel FJ, Aufenacker TJ, Scholten RJ. Antibiotic prophylaxis for prevention of postoperative wound infection in adults undergoing open elective inguinal or femoral hernia repair. Cochrane Database Syst Rev. 2020;4:CD003769. doi: 10.1002/14651858.CD003769.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Mazaki T, Mado K, Masuda H, Shiono M. Antibiotic prophylaxis for the prevention of surgical site infection after tension-free hernia repair: a Bayesian and frequentist meta-analysis. J Am Coll Surg. 2013;217(788–801):e1–e4. doi: 10.1016/j.jamcollsurg.2013.07.386. [DOI] [PubMed] [Google Scholar]
- 155.Boonchan T, Wilasrusmee C, McEvoy M, Attia J, Thakkinstian A. Network meta-analysis of antibiotic prophylaxis for prevention of surgical-site infection after groin hernia surgery. Br J Surg. 2017;104(2):e106–e117. doi: 10.1002/bjs.10441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.HerniaSurge Group International guidelines for groin hernia management. Hernia. 2018;22:1–165. doi: 10.1007/s10029-017-1668-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Reiffel AJ, Barie PS, Spector JA. A multi-disciplinary review of the potential association between closed-suction drains and surgical site infection. Surg Infect (Larchmt) 2013;14(3):244–269. doi: 10.1089/sur.2011.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Leekha S, Terrell CL, Edson RS. General principles of antimicrobial therapy. Mayo Clin Proc. 2011;86(2):156–167. doi: 10.4065/mcp.2010.0639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Cai T, Nesi G, Mazzoli S, Meacci F, Lanzafame P, Caciagli P, et al. Asymptomatic bacteriuria treatment is associated with a higher prevalence of antibiotic resistant strains in women with urinary tract infections. Clin Infect Dis. 2015;61(11):1655–1661. doi: 10.1093/cid/civ696. [DOI] [PubMed] [Google Scholar]
- 160.Cash MC, Hile G, Johnson J, Stone T, Smith J, Ohl C, et al. Sustained impact of an antibiotic stewardship initiative targeting asymptomatic bacteriuria and pyuria in the emergency department. Antimicrob Steward Healthc Epidemiol. 2022;2(1):e148. doi: 10.1017/ash.2022.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Chabok A, Påhlman L, Hjern F, Haapaniemi S, Smedh K, AVOD Study Group Randomized clinical trial of antibiotics in acute uncomplicated diverticulitis. Br J Surg. 2012;99(4):532–539. doi: 10.1002/bjs.8688. [DOI] [PubMed] [Google Scholar]
- 162.Daniels L, Ünlü Ç, de Korte N, van Dieren S, Stockmann HB, Vrouenraets BC, et al. Randomized clinical trial of observational versus antibiotic treatment for a first episode of CT-proven uncomplicated acute diverticulitis. Br J Surg. 2017;104(1):52–61. doi: 10.1002/bjs.10309. [DOI] [PubMed] [Google Scholar]
- 163.Jaung R, Nisbet S, Gosselink MP, Di Re A, Keane C, Lin A, et al. Antibiotics do not reduce length of hospital stay for uncomplicated diverticulitis in a pragmatic double-blind randomized trial. Clin Gastroenterol Hepatol. 2021;19(3):503–510.e1. doi: 10.1016/j.cgh.2020.03.049. [DOI] [PubMed] [Google Scholar]
- 164.Mali JP, Mentula PJ, Leppäniemi AK, Sallinen VJ. Symptomatic treatment for uncomplicated acute diverticulitis: a prospective cohort study. Dis Colon Rectum. 2016;59(6):529–534. doi: 10.1097/DCR.0000000000000579. [DOI] [PubMed] [Google Scholar]
- 165.Estrada Ferrer O, Ruiz Edo N, Hidalgo Grau LA, Abadal Prades M, Del Bas Rubia M, Garcia Torralbo EM, et al. Selective non-antibiotic treatment in sigmoid diverticulitis: Is it time to change the traditional approach? Tech Coloproctol. 2016;20(5):309–315. doi: 10.1007/s10151-016-1464-0. [DOI] [PubMed] [Google Scholar]
- 166.Barie PS, Kao LS, Moody M, Sawyer RG. Infection or inflammation: Are uncomplicated acute appendicitis, acute cholecystitis, and acute diverticulitis infectious diseases? Surg Infect (Larchmt) 2023;24(2):99–111. doi: 10.1089/sur.2022.363. [DOI] [PubMed] [Google Scholar]
- 167.Chabok A, Thorisson A, Nikberg M, Schultz JK, Sallinen V. Changing paradigms in the management of acute uncomplicated diverticulitis. Scand J Surg. 2021;110(2):180–186. doi: 10.1177/14574969211011032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.de Jonge SW, Gans SL, Atema JJ, Solomkin JS, Dellinger PE, Boermeester MA. Timing of preoperative antibiotic prophylaxis in 54,552 patients and the risk of surgical site infection: a systematic review and meta-analysis. Medicine. 2017;96:e6903. doi: 10.1097/MD.0000000000006903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Wolfhagen N, Boldingh QJJ, de Lange M, Boermeester MA, de Jonge SW. Intraoperative redosing of surgical antibiotic prophylaxis in addition to preoperative prophylaxis versus single-dose prophylaxis for the prevention of surgical site infection: a meta-analysis and GRADE recommendation. Ann Surg. 2022;275:1050–1057. doi: 10.1097/SLA.0000000000005436. [DOI] [PubMed] [Google Scholar]
- 170.Mazuski JE, Tessier JM, May AK, Sawyer RG, Nadler EP, Rosengart MR, et al. The Surgical Infection Society revised guidelines on the management of intra-abdominal infection. Surg Infect (Larchmt) 2017;18(1):1–76. doi: 10.1089/sur.2016.261. [DOI] [PubMed] [Google Scholar]
- 171.McCarty TP, White CM, Pappas PG. Candidemia and invasive candidiasis. Infect Dis Clin N Am. 2021;35(2):389–413. doi: 10.1016/j.idc.2021.03.007. [DOI] [PubMed] [Google Scholar]
- 172.Kollef MH, Shorr AF, Bassetti M, Timsit JF, Micek ST, Michelson AP, et al. Timing of antibiotic therapy in the ICU. Crit Care. 2021;25(1):360. doi: 10.1186/s13054-021-03787-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Eachempati SR, Hydo LJ, Shou J, Barie PS. Does de-escalation of antibiotic therapy for ventilator-associated pneumonia affect the likelihood of recurrent pneumonia or mortality in critically ill surgical patients? J Trauma. 2009;66(5):1343–1348. doi: 10.1097/TA.0b013e31819dca4e. [DOI] [PubMed] [Google Scholar]
- 174.Zanichelli V, Sharland M, Cappello B, Moja L, Getahun H, Pessoa-Silva C, et al. The WHO AWaRe (Access, Watch, Reserve) antibiotic book and prevention of antimicrobial resistance. Bull World Health Organ. 2023;101(4):290–296. doi: 10.2471/BLT.22.288614. [DOI] [Google Scholar]
- 175.Kumar A, Ellis P, Arabi Y, Roberts D, Light B, Parrillo JE, Cooperative Antimicrobial Therapy of Septic Shock Database Research Group et al. Initiation of inappropriate antimicrobial therapy results in a fivefold reduction of survival in human septic shock. Chest. 2009;136(5):1237–1248. doi: 10.1378/chest.09-0087. [DOI] [PubMed] [Google Scholar]
- 176.Stuart B, Hounkpatin H, Becque T, Yao G, Zhu S, Alonso-Coello P, et al. Delayed antibiotic prescribing for respiratory tract infections: individual patient data meta-analysis. BMJ. 2021;373:n808. doi: 10.1136/bmj.n808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Hranjec T, Rosenberger LH, Swenson B, Metzger R, Flohr TR, Politano AD, et al. Aggressive versus conservative initiation of antimicrobial treatment in critically ill surgical patients with suspected intensive-care-unit-acquired infection: a quasi-experimental, before and after observational cohort study. Lancet Infect Dis. 2012;12(10):774–780. doi: 10.1016/S1473-3099(12)70151-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Paul M, Shani V, Muchtar E, Kariv G, Robenshtok E, Leibovici L. Systematic review and meta-analysis of the efficacy of appropriate empiric antibiotic therapy for sepsis. Antimicrob Agents Chemother. 2010;54(11):4851–4863. doi: 10.1128/AAC.00627-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Bassetti M, Rello J, Blasi F, Goossens H, Sotgiu G, Tavoschi L, et al. Systematic review of the impact of appropriate versus inappropriate initial antibiotic therapy on outcomes of patients with severe bacterial infections. Int J Antimicrob Agents. 2020;56(6):106184. doi: 10.1016/j.ijantimicag.2020.106184. [DOI] [PubMed] [Google Scholar]
- 180.Weinberger J, Rhee C, Klompas M. A critical analysis of the literature on time-to-antibiotics in suspected sepsis. J Infect Dis. 2020;222(Suppl 2):S110–S118. doi: 10.1093/infdis/jiaa146. [DOI] [PubMed] [Google Scholar]
- 181.Seymour CW, Gesten F, Prescott HC, Friedrich ME, Iwashyna TJ, Phillips GS, et al. Time to treatment and mortality during mandated emergency care for sepsis. N Engl J Med. 2017;376(23):2235–2244. doi: 10.1056/NEJMoa1703058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Liu VX, Fielding-Singh V, Greene JD, Baker JM, Iwashyna TJ, Bhattacharya J, et al. The timing of early antibiotics and hospital mortality in sepsis. Am J Respir Crit Care Med. 2017;196(7):856–863. doi: 10.1164/rccm.201609-1848OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Surviving Sepsis Campaign: International guidelines for management of sepsis and septic shock 2021. Crit Care Med. 2021;49(11):e1063–e1143. doi: 10.1097/CCM.0000000000005337. [DOI] [PubMed] [Google Scholar]
- 184.Blot S, Depuydt P, Vogelaers D, Decruyenaere J, De Waele J, Hoste E, et al. Colonization status and appropriate antibiotic therapy for nosocomial bacteremia caused by antibiotic-resistant gram-negative bacteria in an intensive care unit. Infect Control Hosp Epidemiol. 2005;26(6):575–579. doi: 10.1086/502575. [DOI] [PubMed] [Google Scholar]
- 185.Brusselaers N, Labeau S, Vogelaers D, Blot S. Value of lower respiratory tract surveillance cultures to predict bacterial pathogens in ventilator-associated pneumonia: systematic review and diagnostic test accuracy meta-analysis. Intensive Care Med. 2013;39(3):365–375. doi: 10.1007/s00134-012-2759-x. [DOI] [PubMed] [Google Scholar]
- 186.Michel F, Franceschini B, Berger P, Arnal JM, Gainnier M, Sainty JM, et al. Early antibiotic treatment for BAL-confirmed ventilator-associated pneumonia: a role for routine endotracheal aspirate cultures. Chest. 2005;127(2):589–597. doi: 10.1378/chest.127.2.589. [DOI] [PubMed] [Google Scholar]
- 187.Depuydt PO, Blot SI, Benoit DD, Claeys GW, Verschraegen GL, Vandewoude KH, et al. Antimicrobial resistance in nosocomial bloodstream infection associated with pneumonia and the value of systematic surveillance cultures in an adult intensive care unit. Crit Care Med. 2006;34(3):653–659. doi: 10.1097/01.CCM.0000201405.16525.34. [DOI] [PubMed] [Google Scholar]
- 188.Depuydt P, Benoit D, Vogelaers D, Decruyenaere J, Vandijck D, Claeys G, et al. Systematic surveillance cultures as a tool to predict involvement of multidrug antibiotic resistant bacteria in ventilator-associated pneumonia. Intensive Care Med. 2008;34(4):675–682. doi: 10.1007/s00134-007-0953-z. [DOI] [PubMed] [Google Scholar]
- 189.Müller M, Dela Peña A, Derendorf H. Issues in pharmacokinetics and pharmacodynamics of anti-infective agents: distribution in tissue. Antimicrob Agents Chemother. 2004;48:1441–1453. doi: 10.1128/AAC.48.5.1441-1453.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Pea F, Viale P, Furlanut M. Antimicrobial therapy in critically ill patients: a review of pathophysiological conditions responsible for altered disposition and pharmacokinetic variability. Clin Pharmacokinet. 2005;44(10):1009–1034. doi: 10.2165/00003088-200544100-00002. [DOI] [PubMed] [Google Scholar]
- 191.Gonzalez D, Schmidt S, Derendorf H. Importance of relating efficacy measures to unbound drug concentrations for anti-infective agents. Clin Microbiol Rev. 2013;26:274–288. doi: 10.1128/CMR.00092-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Levison ME. Pharmacodynamics of antimicrobial drugs. Infect Dis Clin N Am. 2004;18:451–465. doi: 10.1016/j.idc.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 193.Buijk SL, Gyssens IC, Mouton JW, Van Vliet A, Verbrugh HA, Bruining HA. Pharmacokinetics of ceftazidime in serum and peritoneal exudate during continuous versus intermittent administration to patients with severe intra-abdominal infections. J Antimicrob Chemother. 2002;49:121–128. doi: 10.1093/jac/49.1.121. [DOI] [PubMed] [Google Scholar]
- 194.Dahyot-Fizelier C, Lefeuvre S, Laksiri L, Marchand S, Sawchuk RJ, Couet W, et al. Kinetics of imipenem distribution into the peritoneal fluid of patients with severe peritonitis studied by microdialysis. Clin Pharmacokinet. 2010;49:323–334. doi: 10.2165/11319370-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 195.Karjagin J, Lefeuvre S, Oselin K, Kipper K, Marchand S, Tikkerberi A, et al. Pharmacokinetics of meropenem determined by microdialysis in the peritoneal fluid of patients with severe peritonitis associated with septic shock. Clin Pharmacol Ther. 2008;83:452–459. doi: 10.1038/sj.clpt.6100312. [DOI] [PubMed] [Google Scholar]
- 196.Pea F, Viale P. Bench-to-bedside review: Appropriate antibiotic therapy in severe sepsis and septic shock-does the dose matter? Crit Care. 2009;13(3):214. doi: 10.1186/cc7774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Blot SI, Pea F, Lipman J. The effect of pathophysiology on pharmacokinetics in the critically ill patient-concepts appraised by the example of antimicrobial agents. Adv Drug Deliv Rev. 2014;77:3–11. doi: 10.1016/j.addr.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 198.Bland CM, Pai MP, Lodise TP. Reappraisal of contemporary pharmacokinetic and pharmacodynamic principles for informing aminoglycoside dosing. Pharmacotherapy. 2018;38(12):1229–1238. doi: 10.1002/phar.2193. [DOI] [PubMed] [Google Scholar]
- 199.Pagkalis S, Mantadakis E, Mavros MN, Ammari C, Falagas ME. Pharmacological considerations for the proper clinical use of aminoglycosides. Drugs. 2011;71(17):2277–2294. doi: 10.2165/11597020-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 200.Al-Dorzi HM, Al Harbi SA, Arabi YM. Antibiotic therapy of pneumonia in the obese patient: dosing and delivery. Curr Opin Infect Dis. 2014;27(2):165–173. doi: 10.1097/QCO.0000000000000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Rybak MJ, Le J, Lodise TP, Levine DP, Bradley JS, Liu C, Mueller BA, et al. Therapeutic monitoring of vancomycin for serious methicillin-resistant Staphylococcus aureus infections: a revised consensus guideline and review by the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, the Pediatric Infectious Diseases Society, and the Society of Infectious Diseases Pharmacists. Am J Health Syst Pharm. 2020;77(11):835–864. doi: 10.1093/ajhp/zxaa036. [DOI] [PubMed] [Google Scholar]
- 202.McMullan BJ, Andresen D, Blyth CC, Avent ML, Bowen AC, Britton PN, et al. Antibiotic duration and timing of the switch from intravenous to oral route for bacterial infections in children: systematic review and guidelines. Lancet Infect Dis. 2016;16:E139–E152. doi: 10.1016/S1473-3099(16)30024-X. [DOI] [PubMed] [Google Scholar]
- 203.Landersdorfer CB, Gwee A, Nation RL. Clinical pharmacological considerations in an early intravenous to oral antibiotic switch: Are barriers real or simply perceived? Clin Microbiol Infect. 2023 Apr 12:S1198–743X(23)00179–9. doi: 10.1016/j.cmi.2023.04.009. Online ahead of print. [DOI] [PubMed]
- 204.Quintiliani R, Grant E, Quintiliani R., Jr Transitional (intravenous to oral) antibiotic therapy. J Med Liban. 2000;48(4):233–240. [PubMed] [Google Scholar]
- 205.Al-Hasan MN, Rac H. Transition from intravenous to oral antimicrobial therapy in patients with uncomplicated and complicated bloodstream infections. Clin Microbiol Infect. 2020;26:299–306. doi: 10.1016/j.cmi.2019.05.012. [DOI] [PubMed] [Google Scholar]
- 206.Fishbein SRS, Mahmud B, Dantas G. Antibiotic perturbations to the gut microbiome. Nat Rev Microbiol. 2023 doi: 10.1038/s41579-023-00933-y. [DOI] [PubMed] [Google Scholar]
- 207.Tabah A, Bassetti M, Kollef MH, Zahar JR, Paiva JA, Timsit JF, et al. Antimicrobial de-escalation in critically ill patients: a position statement from a task force of the European Society of Intensive Care Medicine (ESICM) and European Society of Clinical Microbiology and Infectious Diseases (ESCMID) Critically Ill Patients Study Group (ESGCIP) Intensive Care Med. 2020;46(2):245–265. doi: 10.1007/s00134-019-05866-w. [DOI] [PubMed] [Google Scholar]
- 208.Silva BN, Andriolo RB, Atallah AN, Salomão R. De-escalation of antimicrobial treatment for adults with sepsis, severe sepsis or septic shock. Cochrane Database Syst Rev. 2013;2013(3):CD007934. doi: 10.1002/14651858.CD007934.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Niederman MS. De-escalation therapy in ventilator-associated pneumonia. Curr Opin Crit Care. 2006;12(5):452–457. doi: 10.1097/01.ccx.0000244126.84989.a2. [DOI] [PubMed] [Google Scholar]
- 210.Rello J, Vidaur L, Sandiumenge A, Rodríguez A, Gualis B, Boque C, et al. De-escalation therapy in ventilator-associated pneumonia. Crit Care Med. 2004;32(11):2183–2190. doi: 10.1097/01.ccm.0000145997.10438.28. [DOI] [PubMed] [Google Scholar]
- 211.De Waele JJ, Schouten J, Beovic B, Tabah A, Leone M. Antimicrobial de-escalation as part of antimicrobial stewardship in intensive care: no simple answers to simple questions-a viewpoint of experts. Intensive Care Med. 2020;46(2):236–244. doi: 10.1007/s00134-019-05871-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Lim C, Ashley EA, Hamers RL, Turner P, Kesteman T, Akech S, et al. Surveillance strategies using routine microbiology for antimicrobial resistance in low- and middle-income countries. Clin Microbiol Infect. 2021;27(10):1391–1399. doi: 10.1016/j.cmi.2021.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Cansizoglu MF, Tamer YT, Farid M, Koh AY, Toprak E. Rapid ultrasensitive detection platform for antimicrobial susceptibility testing. PLoS Biol. 2019;17(5):e3000291. doi: 10.1371/journal.pbio.3000291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Anjum MF, Zankari E, Hasman H. Molecular methods for detection of antimicrobial resistance. Microbiol Spectr. 2017 doi: 10.1128/microbiolspec.ARBA-0011-2017. [DOI] [PubMed] [Google Scholar]
- 215.Burnham CD, Leeds J, Nordmann P, O'Grady J, Patel J. Diagnosing antimicrobial resistance. Nat Rev Microbiol. 2017;15(11):697–703. doi: 10.1038/nrmicro.2017.103. [DOI] [PubMed] [Google Scholar]
- 216.Giordano C, Piccoli E, Brucculeri V, Barnini S. A prospective evaluation of two rapid phenotypical antimicrobial susceptibility technologies for the diagnostic stewardship of sepsis. Biomed Res Int. 2018;2018:6976923. doi: 10.1155/2018/6976923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Cals JW, Ament AJ, Hood K, Butler CC, Hopstaken RM, Wassink GF, et al. C-reactive protein point of care testing and physician communication skills training for lower respiratory tract infections in general practice: economic evaluation of a cluster randomized trial. J Eval Clin Pract. 2011;17(6):1059–1069. doi: 10.1111/j.1365-2753.2010.01472.x. [DOI] [PubMed] [Google Scholar]
- 218.Holmes EAF, Harris SD, Hughes A, Craine N, Hughes DA. Cost-effectiveness analysis of the use of point-of-care C-reactive protein testing to reduce antibiotic prescribing in primary care. Antibiotics (Basel) 2018;7(4):106. doi: 10.3390/antibiotics7040106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Hunter R. Cost-effectiveness of point-of-care C-reactive protein tests for respiratory tract infection in primary care in England. Adv Ther. 2015;32:69–85. doi: 10.1007/s12325-015-0180-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Global guidelines for the prevention of surgical site infection. Geneva: World Health Organization; 2018. Web Appendix 25. Summary of a systematic review on surgical antibiotic prophylaxis prolongation. https://www.ncbi.nlm.nih.gov/books/NBK536429/. Accessed 12 July 2023.
- 221.Calderwood MS, Anderson DJ, Bratzler DW, Dellinger EP, Garcia-Houchins S, Maragakis LL, et al. Strategies to prevent surgical site infections in acute-care hospitals: 2022 Update. Infect Control Hosp Epidemiol. 2023;44(5):695–720. doi: 10.1017/ice.2023.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.de Jonge SW, Boldingh QJJ, Solomkin JS, Dellinger EP, Egger M, Salanti G, et al. Effect of postoperative continuation of antibiotic prophylaxis on the incidence of surgical site infection: a systematic review and meta-analysis. Lancet Infect Dis. 2020;20(10):1182–1192. doi: 10.1016/S1473-3099(20)30084-0. [DOI] [PubMed] [Google Scholar]
- 223.Branch-Elliman W, O'Brien W, Strymish J, Itani K, Wyatt C, Gupta K. Association of duration and type of surgical prophylaxis with antimicrobial-associated adverse events. JAMA Surg. 2019;154:590–598. doi: 10.1001/jamasurg.2019.0569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Brink AJ, Messina AP, Feldman C, Richards GA, van den Bergh D, Netcare Antimicrobial Stewardship Study Alliance From guidelines to practice: a pharmacist-driven prospective audit and feedback improvement model for peri-operative antibiotic prophylaxis in 34 South African hospitals. J Antimicrob Chemother. 2017;72(4):1227–1234. doi: 10.1093/jac/dkw523. [DOI] [PubMed] [Google Scholar]
- 225.Spellberg B, Rice LB. Duration of antibiotic therapy: shorter is better. Ann Intern Med. 2019;171(3):210–211. doi: 10.7326/M19-1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Langford BJ, Nisenbaum R, Brown KA, Chan A, Downing M. Antibiotics: easier to start than to stop? Predictors of antimicrobial stewardship recommendation acceptance. Clin Microbiol Infect. 2020;26(12):1638–1643. doi: 10.1016/j.cmi.2020.07.048. [DOI] [PubMed] [Google Scholar]
- 227.Spellberg B. The new antibiotic mantra-“shorter Is better”. JAMA Intern Med. 2016;176(9):1254–1255. doi: 10.1001/jamainternmed.2016.3646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Sawyer RG, Claridge JA, Nathens AB, Rotstein OD, Duane TM, Evans HL, STOP-IT Trial Investigators et al. Trial of short-course antimicrobial therapy for intraabdominal infection. N Engl J Med. 2015;372(21):1996–2005. doi: 10.1056/NEJMoa1411162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Montravers P, Tubach F, Lescot T, Veber B, Esposito-Farèse M, Seguin P, et al. Short-course antibiotic therapy for critically ill patients treated for postoperative intra-abdominal infection: the DURAPOP randomised clinical trial. Intensive Care Med. 2018;44(3):300–310. doi: 10.1007/s00134-018-5088-x. [DOI] [PubMed] [Google Scholar]
- 230.Chastre J, Wolff M, Fagon JY, Chevret S, Thomas F, Wermert D, et al. Comparison of 8 vs 15 days of antibiotic therapy for ventilator-associated pneumonia in adults: a randomized trial. JAMA. 2003;290(19):2588–2598. doi: 10.1001/jama.290.19.2588. [DOI] [PubMed] [Google Scholar]
- 231.Dimopoulos G, Poulakou G, Pneumatikos IA, Armaganidis A, Kollef MH, Matthaiou DK. Short- vs long-duration antibiotic regimens for ventilator-associated pneumonia: a systematic review and meta-analysis. Chest. 2013;144(6):1759–1767. doi: 10.1378/chest.13-0076. [DOI] [PubMed] [Google Scholar]
- 232.Martin-Loeches I, Rodriguez AH, Torres A. New guidelines for hospital-acquired pneumonia/ventilator-associated pneumonia: USA vs. Europe. Curr Opin Crit Care. 2018;24(5):347–352. doi: 10.1097/MCC.0000000000000535. [DOI] [PubMed] [Google Scholar]
- 233.Mo Y, West TE, MacLaren G, Booraphun S, Li AY, Kayastha G, et al. Reducing antibiotic treatment duration for ventilator-associated pneumonia (REGARD-VAP): a trial protocol for a randomised clinical trial. BMJ Open. 2021;11(5):e050105. doi: 10.1136/bmjopen-2021-050105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Yahav D, Franceschini E, Koppel F, Turjeman A, Babich T, Bitterman R, et al. Seven versus 14 days of antibiotic therapy for uncomplicated gram-negative bacteremia: a noninferiority randomized controlled trial. Clin Infect Dis. 2019;69(7):1091–1098. doi: 10.1093/cid/ciy1054. [DOI] [PubMed] [Google Scholar]
- 235.Daneman N, Rishu AH, Pinto R, Aslanian P, Bagshaw SM, Carignan A, et al. 7 versus 14 days of antibiotic treatment for critically ill patients with bloodstream infection: a pilot randomized clinical trial. Trials. 2018;19(1):111. doi: 10.1186/s13063-019-4033-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Chotiprasitsakul D, Han JH, Cosgrove SE, Harris AD, Lautenbach E, Conley AT, et al. Comparing the outcomes of adults with Enterobacteriaceae bacteremia receiving short-course versus prolonged-course antibiotic therapy in a multicenter, propensity score-matched cohort. Clin Infect Dis. 2018;66(2):172–177. doi: 10.1093/cid/cix767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Tansarli GS, Andreatos N, Pliakos EE, Mylonakis E. A systematic review and meta-analysis of antibiotic treatment duration for bacteremia due to Enterobacteriaceae. Antimicrob Agents Chemother. 2019;63(5):e02495–e2518. doi: 10.1128/AAC.02495-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Fabre V, Amoah J, Cosgrove SE, Tamma PD. Antibiotic therapy for Pseudomonas aeruginosa bloodstream infections: How long is long enough? Clin Infect Dis. 2019;69(11):2011–2014. doi: 10.1093/cid/ciz223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.von Dach E, Albrich WC, Brunel AS, Prendki V, Cuvelier C, Flury D, et al. Effect of C-reactive protein-guided antibiotic treatment duration, 7-day treatment, or 14-day treatment on 30-day clinical failure rate in patients with uncomplicated gram-negative bacteremia: a randomized clinical trial. JAMA. 2020;323(21):2160–2169. doi: 10.1001/jama.2020.6348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Hepburn MJ, Dooley DP, Skidmore PJ, Ellis MW, Starnes WF, Hasewinkle WC. Comparison of short-course (5 days) and standard (10 days) treatment for uncomplicated cellulitis. Arch Intern Med. 2004;164(15):1669–1674. doi: 10.1001/archinte.164.15.1669. [DOI] [PubMed] [Google Scholar]
- 241.Stevens DL, Bisno AL, Chambers HF, Dellinger EP, Goldstein EJ, Gorbach SL, Infectious Diseases Society of America et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014;59(2):e10–52. doi: 10.1093/cid/ciu444. [DOI] [PubMed] [Google Scholar]
- 242.Brink AJ, Richards G. Best practice: antibiotic decision-making in ICUs. Curr Opin Crit Care. 2020;26(5):478–488. doi: 10.1097/MCC.0000000000000752. [DOI] [PubMed] [Google Scholar]
- 243.Khilnani GC, Tiwari P, Zirpe KG, Chaudhry D, Govil D, Dixit S, et al. Guidelines for the use of procalcitonin for rational use of antibiotics. Indian J Crit Care Med. 2022;26(Suppl 2):S77–S94. doi: 10.5005/jp-journals-10071-24326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Wirz Y, Meier MA, Bouadma L, Luyt CE, Wolff M, Chastre J, et al. Effect of procalcitonin-guided antibiotic treatment on clinical outcomes in intensive care unit patients with infection and sepsis patients: a patient-level meta-analysis of randomized trials. Crit Care. 2018;22(1):191. doi: 10.1186/s13054-018-2125-2127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Sartelli M, Coccolini F, Kluger Y, Agastra E, Abu-Zidan FM, Abbas AES, et al. WSES/GAIS/WSIS/SIS-E/AAST global clinical pathways for patients with skin and soft tissue infections. World J Emerg Surg. 2022;17(1):3. doi: 10.1186/s13017-022-00406-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Sartelli M, Coccolini F, Kluger Y, Agastra E, Abu-Zidan FM, Abbas AES, et al. WSES/GAIS/SIS-E/WSIS/AAST global clinical pathways for patients with intra-abdominal infections. World J Emerg Surg. 2021;16(1):49. doi: 10.1186/s13017-021-00387-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Kao LS, Ball CG, Chaudhury PK, for Members of the Evidence Based Reviews in Surgery Group Evidence-based reviews in surgery: Early cholecystectomy for cholecystitis. Ann Surg. 2018;268(6):940–942. doi: 10.1097/SLA.0000000000002867. [DOI] [PubMed] [Google Scholar]
- 248.De Waele JJ. Early source control in sepsis. Langenbecks Arch Surg. 2010;395:489–494. doi: 10.1007/s00423-010-0650-1. [DOI] [PubMed] [Google Scholar]
- 249.Martínez ML, Ferrer R, Torrents E, Guillamat-Prats R, Gomà G, Suárez D, et al. Impact of source control in patients with severe sepsis and septic shock. Crit Care Med. 2017;45(1):11–19. doi: 10.1097/CCM.0000000000002011. [DOI] [PubMed] [Google Scholar]
- 250.Bloos F, Rüddel H, Thomas-Rüddel D, Schwarzkopf D, Pausch C, Harbarth S, et al. Effect of a multifaceted educational intervention for anti-infectious measures on sepsis mortality: a cluster randomized trial. Intensive Care Med. 2017;43(11):1602–1612. doi: 10.1007/s00134-017-4782-4. [DOI] [PubMed] [Google Scholar]
- 251.Reitz KM, Kennedy J, Li SR, Handzel R, Tonetti DA, Neal MD, et al. association between time to source control in sepsis and 90-day mortality. JAMA Surg. 2022;157(9):817–826. doi: 10.1001/jamasurg.2022.2761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.De Pascale G, Antonelli M, Deschepper M, Arvaniti K, Blot K, Brown BC, et al. Poor timing and failure of source control are risk factors for mortality in critically ill patients with secondary peritonitis. Intensive Care Med. 2022;48(11):1593–1606. doi: 10.1007/s00134-022-06883-y. [DOI] [PubMed] [Google Scholar]
- 253.Tabah A, Buetti N, Staiquly Q, EUROBACT-2 Study Group. ESICM, ESCMID ESGCIP and the OUTCOMEREA Network et al. Epidemiology and outcomes of hospital-acquired bloodstream infections in intensive care unit patients: the EUROBACT-2 international cohort study. Intensive Care Med. 2023 doi: 10.1007/s00134-012-2695-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.De Waele JJ, Girardis M, Martin-Loeches I. Source control in the management of sepsis and septic shock. Intensive Care Med. 2023;48(12):1799–1802. doi: 10.1007/s00134-022-06852-5. [DOI] [PubMed] [Google Scholar]
- 255.Barie PS, Williams MD, McCollam JS, Bates BM, Qualy RL, Lowry SF, PROWESS Surgical Evaluation Committee et al. Benefit/risk profile of drotrecogin alfa (activated) in surgical patients with severe sepsis. Am J Surg. 2004;188(3):212–220. doi: 10.1016/j.amjsurg.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 256.van de Groep K, Verhoeff TL, Verboom DM, Bos LD, Schultz MJ, Bonten MJM, et al. Epidemiology and outcomes of source control procedures in critically ill patients with intra-abdominal infection. J Crit Care. 2019;52:258–264. doi: 10.1016/j.jcrc.2019.02.029. [DOI] [PubMed] [Google Scholar]
- 257.European Center for Disease Prevention and Control. Healthcare-associated infections surveillance network (HAI-Net). https://www.ecdc.europa.eu/en/about-us/partnerships-and-networks/disease-and-laboratory-networks/hai-net. Accessed 12 July 2023.
- 258.Centers for Disease Control and Prevention. National Healthcare Safety Network (NHSN). https://www.cdc.gov/nhsn/index.html. Accessed 12 July 2023.
- 259.European Center for Disease Prevention and Control. Antimicrobial resistance surveillance in Europe 2022–2020 data. www.ecdc.europa.eu/en/publications-data/antimicrobial-resistance-surveillance-europe-2022-2020-data. Accessed 12 July 2023.
- 260.Global antimicrobial resistance and use surveillance system (GLASS) report: 2022. Geneva: World Health Organization; 2022. www.who.int/publications/i/item/9789240062702. Accessed 12 July 2023.
- 261.Maugeri A, Barchitta M, Puglisi F, Agodi A. Socio-economic, governance and health indicators shaping antimicrobial resistance: an ecological analysis of 30 European countries. Glob Health. 2023;19(1):12. doi: 10.1186/s12992-023-00913-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Pallares C, Hernández-Gómez C, Appel TM, Escandón K, Reyes S, Salcedo S, et al. Impact of antimicrobial stewardship programs on antibiotic consumption and antimicrobial resistance in four Colombian healthcare institutions. BMC Infect Dis. 2022;22(1):420. doi: 10.1186/s12879-022-07410-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Klein EY, Van Boeckel TP, Martinez EM, Pant S, Gandra S, Levin SA, et al. Global increase and geographic convergence in antibiotic consumption between 2000 and 2015. Proc Natl Acad Sci USA. 2018;115(15):E3463–E3470. doi: 10.1073/pnas.1717295115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Rawson TM, Moore LS, Tivey AM, Tsao A, Gilchrist M, Charani E, et al. Behaviour change interventions to influence antimicrobial prescribing: a cross-sectional analysis of reports from UK state-of-the-art scientific conferences. Antimicrob Resist Infect Control. 2017;6(1):11. doi: 10.1186/s13756-019-0603-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Majumder MAA, Rahman S, Cohall D, Bharatha A, Singh K, Haque M, Gittens-St Hilaire M. Antimicrobial stewardship: fighting antimicrobial resistance and protecting global public health. Infect Drug Resist. 2020;13:4713–4738. doi: 10.2147/IDR.S290835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Majumder MAA, Singh K, Hilaire MG, Rahman S, Sa B, Haque M. Tackling antimicrobial resistance by promoting antimicrobial stewardship in medical and allied health professional curricula. Expert Rev Anti Infect Ther. 2020;18(12):1245–1258. doi: 10.1080/14787210.2020.1796638. [DOI] [PubMed] [Google Scholar]
- 267.Alkhuzaei AMJB, Salama RE, Eljak IEI, Chehab MA, Selim NA. Perceptions and practice of physicians and pharmacists regarding antibiotic misuse at primary health centres in Qatar: a cross-sectional study. J Taibah Univ Med Sci. 2017;13(1):77–82. doi: 10.1016/j.jtumed.2017.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Mangione SR, McGlynn E, Elliot M. Parent expectations for antibiotics, physician–parent communication, and satisfaction. Arch Pediatr Adolesc Med. 2001;7(155):800–806. doi: 10.1001/archpedi.155.7.800. [DOI] [PubMed] [Google Scholar]
- 269.Saleem Z, Godman B, Cook A, et al. Ongoing efforts to improve antimicrobial utilization in hospitals among African countries and implications for the future. Antibiotics (Basel) 2022;11(12):1824. doi: 10.3390/antibiotics11121824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Sartelli M, Labricciosa FM, Barbadoro P, Pagani L, Ansaloni L, Brink AJ, et al. The global alliance for infections in surgery: defining a model for antimicrobial stewardship-results from an international cross-sectional survey. World J Emerg Surg. 2017;12:34. doi: 10.1186/s13017-017-0145-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Davey P, Brown E, Charani E, Fenelon L, Gould IM, Holmes A, et al. Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database Syst Rev. 2013;4:CD003543. doi: 10.1002/14651858.CD003543.pub4. [DOI] [PubMed] [Google Scholar]
- 272.Rawson TM, Moore LS, Gilchrist MJ, Holmes AH. Antimicrobial stewardship: Are we failing in cross-specialty clinical engagement? J Antimicrob Chemother. 2016;71:554–559. doi: 10.1093/jac/dkv337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Howard P, Pulcini C, Levy Hara G, West RM, Gould IM, Harbarth S, et al. An international cross-sectional survey of antimicrobial stewardship programmes in hospitals. J Antimicrob Chemother. 2015;70(4):1245–1255. doi: 10.1093/jac/dku497. [DOI] [PubMed] [Google Scholar]
- 274.Raval MV, Bentrem DJ, Eskandari MK, Ingraham AM, Hall BL, Randolph B, et al. The role of surgical champions in the American College of Surgeons National Surgical Quality Improvement Program-a national survey. J Surg Res. 2011;166(1):e15–25. doi: 10.1016/j.jss.2010.10.036. [DOI] [PubMed] [Google Scholar]
- 275.Wunderink RG, Srinivasan A, Barie PS, Chastre J, Dela Cruz CS, Douglas IS, et al. Antibiotic stewardship in the intensive care unit. An official American Thoracic Society workshop report in collaboration with the AACN, CHEST, CDC, and SCCM. Ann Am Thorac Soc. 2020;17(5):531–540. doi: 10.1513/AnnalsATS.202003-188ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.May L, Martín Quirós A, Ten Oever J, Hoogerwerf J, Schoffelen T, Schouten J. Antimicrobial stewardship in the emergency department: characteristics and evidence for effectiveness of interventions. Clin Microbiol Infect. 2021;27(2):204–209. doi: 10.1016/j.cmi.2020.10.028. [DOI] [PubMed] [Google Scholar]
- 277.Paul M, Pulia M, Pulcini C. Antibiotic stewardship in the emergency department: not to be overlooked. Clin Microbiol Infect. 2021;27(2):172–174. doi: 10.1016/j.cmi.2020.11.015. [DOI] [PubMed] [Google Scholar]
- 278.Castro-Sánchez E, Gilchrist M, Ahmad R, Courtenay M, Bosanquet J, Holmes AH. Nurse roles in antimicrobial stewardship: lessons from public sectors models of acute care service delivery in the United Kingdom. Antimicrob Resist Infect Control. 2019;22(8):162. doi: 10.1186/s13756-019-0621-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Kumar M, Sarma DK, Shubham S, Kumawat M, Verma V, Nina PB, et al. Futuristic non-antibiotic therapies to combat antibiotic resistance: a review. Front Microbiol. 2021;12:609459. doi: 10.3389/fmicb.2021.609459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Catho G, Sauser J, Coray V, Da Silva S, Elzi L, Harbarth S, et al. Impact of interactive computerised decision support for hospital antibiotic use (COMPASS): an open-label, cluster-randomised trial in three Swiss hospitals. Lancet Infect Dis. 2022;22(10):1493–1502. doi: 10.1016/S1473-3099(22)00308-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Curtis CE, Al Bahar F, Marriott JF. The effectiveness of computerised decision support on antibiotic use in hospitals: a systematic review. PLoS ONE. 2017;12(8):e0183062. doi: 10.1371/journal.pone.0183062. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.