Abstract
Coupled with aging, chronic stress experienced by dementia caregivers often leads to deteriorating health. Comparing caregivers and non-caregivers, we tested whether depression and loneliness mediate the relationship between caregiver status and a measure of chronic stress, the Perceived Stress Scale. Seventy-six cognitively normal older adults (mean age 72.7) were identified as caregivers or non-caregivers based on the functional independence of a paired family member. Caregivers reported more perceived stress, depression, and loneliness than non-caregivers. Using multiple mediation analyses, we found that loneliness and depression mediated the relationship of caregiver status with perceived stress. The loneliness effect on perceived stress was both direct and via its relationship with depressive symptoms. The findings suggest loneliness as a likely point of intervention to reduce caregiver stress. Initiatives to enable caregivers to maintain or develop social relationships apart from caregiver responsibilities may mitigate stress and its negative impact on mental and physical health.
Keywords: caregivers, aging, dementia, depression, loneliness
Significance Statement
Chronic stress has a significant effect on the physical and cognitive health of caregivers of individuals with Alzheimer’s disease (AD). Our finding that loneliness is a pivotal mediator of caregiver stress suggests that reducing loneliness for dementia caregivers will improve quality of life and prolong healthy functioning essential to the public health mandate to care for the rapidly increasing numbers of patients living with AD.
Introduction
There is growing public concern about the welfare of dementia caregivers (CGs) in light of 1) the significant impact of sustained effects of stress on CG health, 2) greater personal, financial, and societal interest in caring for patients at home, and 3) the realization that the health care system is not prepared for the predicted increase in numbers of individuals with Alzheimer’s disease (AD) carrying with it a comparable increase in the need for caregiving. While caregiving can have positive aspects, most unpaid CGs experience chronic stress from caregiving that includes unrelenting daily hassles as well as uncertainty about the future. As is often seen in spousal caregivers, chronic stress is likely to have a greater effect on health when coupled with changes associated with aging. In addition to negative interactive effects of aging and caregiving, it is expected that highly stressful events and difficulties that often accompany aging (e.g., medical comorbidities and death of family members or friends) will be similar for both caregivers and non-caregivers (non-CGs). Since the additive effect of these multiple ongoing stressors can be devastating, 1 measuring those stressors associated with caregiving, as well as chronic stress resulting from recent events and difficulties, may help to identify factors that influence perceived stress and consequences of chronic stress in CGs. For older CGs, responsibilities of caregiving and concurrent stressful events are likely to significantly increase risk for negative health outcomes and challenge caregiving abilities.
The complexities of measuring stress in a given individual are considerable. Attempts to understand its effects are enhanced by a framework such as that proposed by Cohen and colleagues. 2 While stressors can often be objectively defined (e.g., death of a spouse), Cohen et al maintain that it is not the event that causes responses to stress, but “the cognitively mediated emotional response to the objective event.” They emphasize that the cognitive appraisal of an event is central in understanding responses to stress, noting that understanding the event’s objective properties is insufficient. They developed a widely used self-report questionnaire, the Perceived Stress Scale (PSS). 2 This instrument requires a self-appraisal of experienced perceived stress over the last month and is intended to measure the degree to which someone feels life is “unpredictable, uncontrollable, and overwhelming.” 3 In older adults without dementia, higher Perceived Stress Scale scores have been associated with increasing age,4,5 anxiety, depression, 4 and sleep disturbance, 6 as well as stress associated with caregiving. 6
Obtaining subjective responses to simple checklists of specific events and difficulties (e.g., death of spouse and chronic pain) is a common method used to measure chronic stress. However, these checklists often do not consider context, threat severity, event duration, and multiple instances of these events. Previous findings are mixed with respect to the association of stressful events and difficulties with outcomes that may be related (e.g., cognitive decline and depression7–11). In addition to the PSS, we included in the current study a brief checklist of recent events and difficulties (Chronic–Stressful Life Events and Difficulties; C-SLED), (see Additional Measures) commonly experienced by older adults. Importantly, the C-SLED provides not only the identification of recent experiences, but also subjective ratings of threat severity for each item.
Symptoms of depression and anxiety are among the most commonly addressed emotional responses associated with psychological stress. Animal studies, despite the absence of a cognitive appraisal of a stressful event, have the advantage of carefully monitoring past history and the stress type (e.g., immobilization, isolation, and social defeat), duration (e.g., acute vs chronic) and context, as well as specific neuroanatomical and behavioral consequences. A number of these studies (primarily with rats) have found relationships between objectively defined chronic stress and behavioral changes that suggest anxiety (e.g., reduced maze exploration)12,13 and depressed mood (e.g., reduced novelty seeking; social avoidance; freezing behavior; and weight loss).14–16 Studies measuring the effects of stressful events in humans often lack rigor in precisely characterizing the stressor(s). Caregiving is one of a vast number of life events that can cause stress. However, there is ample evidence that identifying caregiver status as a source of chronic stress can be useful in understanding its effects.
Studies have demonstrated that chronic stress experienced by caregivers of persons with dementia is associated with symptoms of anxiety and depression.17–23 In a systematic review and meta-analysis, Del-Pino-Casado and colleagues 24 found a large, positive association between subjective caregiver burden and symptoms of depression. Interestingly, in their study, there was a greater association between burden and depressive symptomatology for those caring for people with dementia than for those caring for frail older people and stroke survivors.
Studying loneliness in older adults has gained interest given increasing evidence of its association with physical and cognitive health.25–27 A meta-analysis revealed that older adults reporting loneliness had a higher risk of mortality (odds ratio: 1.45) than those not experiencing loneliness. 28 Loneliness has also been associated with increased risk of developing dementia,29–31 including evidence of risk due to AD neuropathology in cognitively normal adults. 32 Studies focusing on older adults who are unpaid CGs of a person with dementia reveal greater loneliness and negative affect in CGs than in non-CGs 33 and a significant relationship between loneliness and depression in CGs. 34
In the current study, we measured perceived stress (Perceived Stress Scale), 2 stress based on recent events and difficulties (C-SLED), depressed mood (Short Form of the Geriatric Depression Scale), 35 trait anxiety (State-Trait Anxiety Inventory-Form Y-2), 36 and loneliness (de Jong Gierveld Loneliness Scale). 37 We focused primarily on differences in these measures between CGs and non-CGs. We compared cognitively intact older adults caring for a spouse or another family member with dementia to those with no caregiving responsibilities and examined depressed mood, trait anxiety, and loneliness as potential mediators of the relationship between caregiver status and self-reported perceived stress. We hypothesized the following:
1) CGs will express significantly more perceived stress, depressive symptoms, anxiety, and loneliness than non-CGs.
2) Depressive symptoms, anxiety, and loneliness will each mediate the relationship between CG status and the total score on the perceived stress scale.
Methods
Participants
Seventy-six cognitively normal CGs (n=36) and non-CGs (n=40) over the age of 50 years (mean age = 73.4) participated in the study. Each of the 76 participants was considered a CG if he/she served as the primary unpaid CG for the co-participant who had a diagnosis of dementia (primarily AD) or a non-CG, if the co-participant was well known to the participant, cognitively normal, and functionally independent. The cohort included 25 Latino participants (33%); 10 (28%) were CGs and 15 were non-CGs (38%). The majority (86%) of CGs and non-CGs lived with their spouse.
Participants were recruited primarily from the Shiley-Marcos Alzheimer’s Disease Research Center (ADRC) at the University of California, San Diego (UCSD) and from several local, non-profit neighborhood-based facilities. Individuals with a history of severe head injury, alcoholism, or other serious or prolonged psychiatric illness were excluded. The Mini-Mental State Examination (MMSE) 38 was administered to CGs, non-CGs, and partners identified as co-participants (i.e., spouse or other family member) at initial screening along with a scale of instrumental activities of daily living (Functional Activities Questionnaire; FAQ) 39 to establish level of cognition and functioning. Enrolled CGs and non-CGs were asked to review and sign a written informed consent describing the procedures and outlining risks and benefits. Care recipients were asked to sign a separate consent describing their role in the project. Both consents were approved by the UCSD Human Research Protections Program. If the co-participant of the CG lacked capacity to consent due to severity of cognitive impairment, surrogate consent (usually the caregiver) was obtained.
Trained psychometrists administered neuropsychological tests and questionnaires to the CGs and non-CGs at the UCSD ADRC or in their homes. While a wide array of neuropsychological tests was administered, only baseline scores from 2 widely used screening measures of global cognition, the MMSE 38 and the Montreal Cognitive Assessment (MoCA) 40 are reported in this study to support the assumption that CGs and non-CGs were cognitively normal. Using the FAQ, 39 the CG and non-CG participants provided information about their own activities of daily living (ADLs), as well as the ADLs of their co-participants. The FAQ includes ten items (e.g., finances, shopping) reflecting level of independence in instrumental daily activities.
Additional Measures
The 10-item Perceived Stress Scale (PSS-10) 2 is a self-report measure of an individual’s appraisal of their level of chronic stress over the previous month, with items using specific or implied feeling terms, some positive and some negative (e.g., upset, nervous, confident, and angered). Several items are reverse-scored, and a total score is calculated with higher total scores indicative of greater perceived stress.
From a second measure of stress (in addition to the PSS), we obtained scores on a brief checklist (Chronic–Stressful Life Events and Difficulties; C-SLED) of recent (i.e., within the past year) events and difficulties rated as highly stressful in a previous study of cognitive change in 100 older adults 9 using the Life Events and Difficulties Schedule. 41 To avoid overlap with stressors associated with caregiving, we removed from the analyses 5 of the 16 items on the C-SLED expected to be acknowledged by a person in a caregiver role (e.g., serving as a caregiver and having a spouse with a serious chronic illness) to avoid multicollinearity. This resulted in an adapted 11-item scale (C-SLED-11). For each item reported as present within the last year, the participant rated the level of stress on a scale of 1 (none/very little) to 10 (major/significant), with these summed for a total score. The C-SLED-11 included the death of a spouse, parent, or sibling, death of a pet, chronic poor health, chronic pain in participant, spouse, or close friend/family member, finding out about a life threatening illness in the participant, conflict with a child or grandchild, and problems with money.
The Short Form of the Geriatric Depression Scale (GDS-15) 42 is a 15-item screening test for depression, found to be valid in cognitively intact older adults. The State-Trait Anxiety Inventory (STAI), specifically, Form Y-2,36 is a 20-item self-report measure of how the participant generally feels (i.e., trait anxiety) designed to measure relatively stable individual differences in the tendency to perceive stressful situations as dangerous or threatening. The modified version of the de Jong Gierveld Loneliness Scale 37 assesses loneliness using a brief self-report measure of 11 items (e.g., I miss having a really close friend). Three response scale categories include “yes,” “more or less,” and “no.” A total score is calculated ranging from 0 (“no loneliness”) to 11 (“extreme loneliness”). 37 Measures of reliability (Cronbach’s alpha) range from .80 to .90. In terms of validity, the scale correlates moderately with the UCLA-Loneliness scale. 43
Statistical Analyses
With a sample size of 36 caregivers and 40 non-caregivers, we had 80% power to detect a .65 standard deviation or larger shift in means between the 2 groups. Although the cohort included 25 (33%) Latino participants, sample sizes when divided by CG status did not support statistical analyses to explore differences between CGs and non-CGs for this subset of participants.
We used independent sample t-tests to compare groups on continuous variables and the non-parametric Fisher’s exact test to compare groups on categorical variables. The non-parametric Spearman rho correlation coefficient was used to describe the association between perceived stress scores and ordinal variables. Assumptions of all parametric tests (symmetry, approximate normality, and absence of outlier values) were assessed by visual inspection of histograms and relevant bivariate scatterplots.
Scores derived from the C-SLED-11 were categorized as indicating high or low stress based on a median split for the full cohort. These groups were compared on the distribution of depression, loneliness, anxiety, and perceived stress using t-tests within CG and non-CG participants.
Mediation models (structural equation models) were fit using the lavaan package 44 written in the statistical programming language R. 45 Model fit was evaluated by standard criteria, 46 as follows: that the maximum likelihood (ML)-based standardized root mean squared residual (SRMR) was less than .08, the Comparative Fit Index (CFI) was greater than .95, and the root mean squared error of approximation (RMSEA) was less than or equal to .06. Product-of-coefficients statistics 47 were used to formally test mediation effects. All mediation models covaried for the effects of demographic variables (age, education, and sex) on perceived stress.
Results
With all participants included, mean age was 72.7 years (SD=8.3; range 54-91). CGs and non-CGs did not differ significantly in age, education, total scores on tests of global cognition (i.e., MMSE, MoCA), or independence in daily activities (i.e., FAQ) (see Table 1). For CGs and non-CGs, scores on measures of global cognition and functional independence indicated that they were functioning normally with respect to cognition and daily activities. There was a greater percentage of females in the CG group than the non-CG group, but the difference was not significant using Fisher’s Exact Test.
Table 1.
Demographic and cognitive variables for participants (n=76) divided by caregiver status.
| Caregivers n=36 | Non-caregivers n=40 | P-value | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | T-test | |
| Age (years) | 74.6 | 8.2 | 70.9 | 8.1 | .056 |
| Education (years) | 15.1 | 3.4 | 15.4 | 4.6 | .696 |
| MMSE/30 | 28.3 | 1.9 | 28.9 | 1.8 | .149 |
| MoCA/30 | 25.3 | 3.6 | 25.0 | 4.0 | .750 |
| FAQ/30 | .33 | .68 | .57 | 1.2 | .289 |
| % | % | Fisher’s exact | |||
| % female | 77.8 | 55.0 | .053 | ||
MMSE, Mini-Mental State Examination; MoCA, Montreal Cognitive Assessment; FAQ, Functional Activities Questionnaire.
CGs reported significantly more perceived stress and loneliness than non-CGs (see Table 2). Relative to published norms for the 10-item Perceived Stress Scale from a Scandinavian cohort 48 (mean=12.9; SD=6.0), 34% of CGs and 10% of non-CGs produced scores greater than 1 SD above the mean, with 3 participants in the CG group scoring greater than 2 SDs above the mean (i.e., greater perceived stress controlling for age). Characterizing loneliness as absent, moderate, severe, and very severe, 43 non-CGs reported scores suggesting no loneliness (65%) or moderate loneliness (35%), while CGs reported a more affected distribution of loneliness scores (33% no loneliness, 58% moderately lonely, 6% severely lonely, and 3% very severely lonely). Sixty-seven percent of CGs acknowledged at least moderate loneliness, while only 35% of non-CGs reported moderate loneliness and no non-CGs reported a more severe level.
Table 2.
Means (Standard Deviations) comparing Caregivers and Non-caregivers on clinical and behavioral variables.
| Caregivers N=36 |
Non-caregivers N=40 |
P-value | |
|---|---|---|---|
| Perceived Stress Scale total | 15.4 (7.4) | 10.2 (6.9) | .002 |
| Depression a | 3.2 (2.5) | 1.1 (1.4) | .000 |
| Trait anxiety | 34.2 (9.2) | 31.7 (9.2) | .237 |
| Loneliness | 4.0 (3.0) | 2.3 (2.7) | .012 |
aUnequal variance, greater for Caregivers than Non-Caregivers P=.000.
The CG and non-CG groups did not differ significantly on the measure of trait anxiety. Using the original norms for older adults, 36 15% of non-CGs produced scores greater than 1 standard deviation (SD) above the mean, with only 3% (1 participant) greater than 2 SDs. For CGs, 25% produced scores greater than 1 SD above the mean, with 8% (3 participants) greater than 2 SDs.
While neither of the group means on the measure of depression fell within the range of clinical depression based on data suggesting cut-off scores (i.e., score greater than 4 raises question of depression), 49 the groups were significantly different, with the CG group scoring higher than the non-CG group. For the GDS, 28% of CGs (25% mild, 3% moderate) and 3% of non-CGs (mild) reported scores in the mild to moderate range of depression. Also, the significant difference in the variance of the GDS scores between the groups (Levene’s test for equality of variances: F=14.9; P=.000) was of note. Only one participant in the non-CG group (2.5%) received a score above 4, while 10 participants in the CG group (27.8%) received a score above 4.
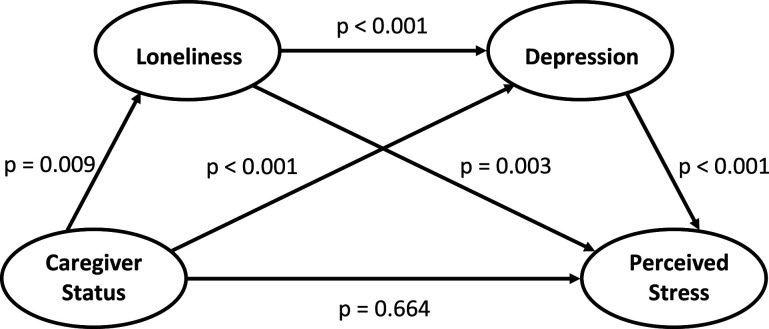
Independent preliminary mediation analyses were run to assess the effects of depressive symptomatology, anxiety, and loneliness, on the relationship between CG status and responses to the perceived stress questionnaire. In these preliminary analyses, depressive symptomatology and loneliness were significant mediators of the relationship between CG status and perceived stress, while anxiety had no mediation effect (P = .20). Based on these results, a multiple mediation model was fit including depressive symptomatology and loneliness as mediators. Loneliness effects were also assumed to be fully or partially mediated by depression in our model (Table 3, Figure 1) based on prior literature. 34 Structural equation model (SEM) fit indexes (CFI = .988; RSMEA = .051; SRMR = .074) confirm this model well represents the data. In the multiple mediation model, depressive symptomatology (P = .002) and loneliness (P = .047) were significant mediators, and moreover the loneliness effect was statistically significantly (P = .001) mediated by depression (Table 3). CG status effects were completely mediated by loneliness and depression (CG direct effect P value = .66 after controlling for the mediating effects of loneliness and depression).
Table 3.
Multiple mediation model of caregiver (CG) status on perceived stress (PSS) including the Geriatric Depression Scale score (GDS) and loneliness score as mediators.
| Estimate | Standard error | z-value | P-value | |
|---|---|---|---|---|
| Direct effects | ||||
| CG status | −.607 | 1.395 | −.435 | .664 |
| GDS | 1.758 | .321 | 5.474 | 2.33 × 10−6 |
| Loneliness | .682 | .226 | 3.022 | .003 |
| Defined parameters | ||||
| Estimate | Standard error | z-value | P-value | |
| Mediation effects | ||||
| CG -> GDS -> PSS | 2.913 | .925 | 3.148 | .002 |
| CG -> loneliness -> PSS | 1.159 | .584 | 1.984 | .047 |
| Loneliness -> GDS -> PSS | .517 | .16 | 3.225 | .001 |
Figure 1.
Multiple mediation model of caregiver status effects (P values for strength of association between components of the multiple mediation model).
CGs and non-CGs did not differ on the number of recent stressful events and difficulties or on the total score on the C-SLED-11. CGs with a relatively high total score (indicating greater chronic stress) acknowledged more symptoms of depression (t=−2.1; P=.04) (see Table 4) than those CGs with a relatively low score, but the high and low CG groups did not differ significantly on reports of perceived stress or anxiety. Non-CGs with higher scores on the C-SLED-11 acknowledged more symptoms not only of depression (t=−2.8; P=.01), but also perceived stress (t=−3.1; P=.004) and anxiety (t=−2.7; P=.01) compared to those non-CGs with lower scores. These high and low C-SLED-11 groups did not differ on loneliness for either the CGs or the non-CGs.
Table 4.
Means (Standard Deviations) comparing participants divided on caregiver status and high vs low scores (median split) on the 11-item Chronic–Stressful Life Events and Difficulties scale (C-SLED-11) a .
|
N=76 |
C-SLED-11 Groups | |||||
|---|---|---|---|---|---|---|
| Caregiver | Non-caregiver | |||||
| Low N=16 |
High N=20 |
P-value | Low N=24 |
High N=16 |
P-value | |
| Perceived stress | 13.5 (6.8) | 16.8 (7.7) | NS | 7.7 (5.8) | 13.9 (6.9) | .004 |
| Depression | 2.3 (2.0) | 4.0 (2.6) | .04 | .58 (.72) | 1.9 (1.7) | .01 |
| Trait anxiety | 31.1 (8.3) | 36.7 (9.4) | NS | 28.8 (7.4) | 36.1 (10.0) | .01 |
| Loneliness | 3.8 (3.4) | 4.1 (2.6) | NS | 2.0 (2.9) | 2.8 (2.4) | NS |
aLow vs High scores on C-SLED-11 based on median split: High = >6.
For CGs, depressive symptomatology, trait anxiety, and loneliness had no mediation effect on the relationship between total recent chronic stress total scores based on the C-SLED-11 scores and perceived stress. For non-CGs, only trait anxiety was a significant mediator of this relationship (data not shown).
Discussion
In the current study older caregivers of individuals with dementia reported significantly more perceived stress, depressive symptomatology, and loneliness than non-caregivers who were similar in age, education, global cognition, and functional independence. These results were expected and largely consistent with findings from previous studies. However, the 2 groups did not differ on a measure of trait anxiety.
Our findings highlight a significant relationship between caregiving and an increase in perceived stress. Of interest, however, are factors that may underlie this relationship. The total effect of CG status on perceived stress was mediated by self-reported scores on measures of loneliness and depression. In the mediation model, the loneliness effect was both direct and via its relationship with depression. Anxiety was a predictor of perceived stress but was not associated with CG status and had no mediation effect on the CG status relationship with perceived stress. These results suggest that for understanding effects of chronic stress experienced by older adults in general, symptoms associated with loneliness and depression are the best predictors of perceived stress. These results also suggest loneliness as a target for interventions to mitigate CG stress. Loneliness was common (endorsed by 67% of our CG sample), a precedent to depression, 34 and an integral mediator of CG effects on stress (Figure 1).
As noted, the anxiety scale used in the study (STAI-Y-2) is a measure of trait anxiety designed to assess anxiety as a persisting personal characteristic or, in other words, a consistent reaction to typical day to day challenges. As a measure that is related more to responses associated with personality than those based on specific events and difficulties including caregiving, it makes sense that there were no differences in means on the trait anxiety scale between the CG and non-CG groups, and that level of trait anxiety did not mediate the relationship between CG status and perceived stress.
CGs with a relatively high score on the C-SLED-11 acknowledged more symptoms of depression than CGs with a relatively low score, but these CG groups did not differ on perceived stress or anxiety. Non-CGs with higher scores on the C-SLED-11 acknowledged more symptoms, not only of depression, but also perceived stress and anxiety compared to those with lower scores. For non-CGs, trait anxiety was a significant mediator of the relationship between the C-SLED-11 scores and perceived stress, but there were no significant mediators of the relationship between the C-SLED-11 scores and perceived stress for the CGs. These results support the view that recent events and difficulties unrelated to caregiving may affect CGs and non-CGs in different ways. For the non-CGs, in the absence of CG duties, trait anxiety was found to be an important factor associated with the Perceived Stress Scale total score, that is, with the expectation that life is “unpredictable, uncontrollable, and overwhelming." 3
The study has several limitations. Convenience sampling was used to identify participants and the sample size of the cohort was relatively small. While trying to understand contributions to perceived stress reported by CGs, we did not consider duration of caregiving, availability of CG help, coping strategies, and ethnicity. Also, we did not include difficulties associated with the care recipient that may affect the caregiver’s distress such as disinhibited behavior, degree of cognitive impairment, and level of functional decline. The temporal order of association implied by our mediation model was technically not assessed in our study. While CG status was a long-standing exposure prior to assessing loneliness and depression, the mediators and the perceived stress outcome were assessed at a single point in time. However, these measures reflect the cumulative experiences of the CGs to the date of assessment, and the direction of temporal association (loneliness predicting depression) is consistent with a well-established literature on the interrelationship of these factors. 34
While many of the participants in the current cohort did report perceived stress, symptoms associated with depression, loneliness, and anxiety, and differences between CGs and non-CGs were detected, most participants, regardless of group membership, reported relatively mild stress and symptoms of depression, anxiety, and loneliness. This may reflect some selection bias favoring participants who, despite caregiving responsibilities and other sources of stress, have resources (e.g., time, energy, and transportation) that mitigate demands associated with research participation.
Interestingly, noting the oversimplification of event-based measures, Cohen 2 defends the use of the Perceived Stress Scale to measure cognitively mediated emotions in response to events as opposed to measuring the events themselves. Also, the Perceived Stress Scale has enjoyed wide use in research in part due to features of self-report and brevity that contribute to ease of administration. Others, however, consider the Perceived Stress Scale to measure only one type of stress 50 and have proposed sources of stress that may or may not overlap with Cohen’s. These are based primarily on factors described by McEwen and Akil 51 that include chronic social and environmental stress (e.g., poverty), physiological stressors (e.g., inflammation), major life events and trauma (e.g., divorce), and individual differences in stress vulnerability (e.g., genetic status). McEwen and Akil 51 identify the brain as “a primary organ that perceives and responds to what is stressful to an individual.” For health-related studies, these definitions of stress are useful to the extent that they can signal impending progression to disease.
Conclusions
Older adults caring for persons with dementia are particularly vulnerable to negative effects of chronic stress on emotional and physical health. Persisting events and difficulties (including caregiving) that are sufficiently severe often lead to a number of distressing symptoms, many of which are treatable. Understanding ways in which these symptoms act and interact to cause stress and compromise mental and physical health can provide useful information to lessen their negative impact. Identifying barriers to obtaining treatment to reduce stress is equally important. Since factors that affect caregiver responses to stress may differ among culturally diverse groups, their representation in sufficient numbers to detect differences in responses and vulnerability to stress is essential. Future studies should test interventions in larger samples representative of the general population while evaluating factors that may prevent access of older adults to resources. Our finding that loneliness is common and a pivotal mediator of caregiver stress suggests that this is a likely locus for interventions. Dementia CGs experience both reduced social engagement with their care recipient, often a life partner, as well as reduced access to outside relationships because of the time burden of caregiving. CG support groups and other initiatives to encourage or enable CGs to maintain or develop new social relationships outside their caregiver responsibilities may mitigate CG stress and loneliness and their associated negative impact on mental and physical health.
Acknowledgments
This work was supported by the State of California, Department of Public Health, Alzheimer’s Disease Program (Alzheimer’s Disease Research Award, #16-10054) and the National Institute on Aging at the National Institutes of Health (grants P-30 AG062429, R01 AG049810). We thank Dr. Christina Gigliotti and Emily Little for their help and flexibility in leveraging the resources of the Shiley-Marcos Alzheimer’s Disease Research Center to complete data collection. Finally, we are most grateful to the research participants who generously gave their time and effort to volunteer for this study.
Appendix A
Abbreviations
- AD
Alzheimer’s disease
- ADRC
Alzheimer’s Disease Research Center
- CG
Caregiver
- C-SLED
Chronic Stressful Life Events and Difficulties
- C-SLED-11
11-Item Chronic Stressful Life Events and Difficulties
- FAQ
Functional Activities Questionnaire
- MMSE
Mini-Mental State Examination
- MoCA
Montreal Cognitive Assessment
- Non-CG
Non-caregiver
- PSS-10
10-Item Perceived Stress Scale
- GDS-15
Short Form of the Geriatric Depression Scale
- STAI-Y-2
Spielberger State-Trait Anxiety Inventory, form Y-2
- UCSD
University of California, San Diego
Footnotes
The authors report no conflicts of interests.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Guerry Peavy https://orcid.org/0000-0001-7785-7916
References
- 1.Mandavia AD, Bonanno GA. When natural disaster follows economic downturn: The incremental impact of multiple stressor events on trajectories of depression and posttraumatic stress disorder. Disaster Med Public Health Prep. 2019;13(2):173-182. [DOI] [PubMed] [Google Scholar]
- 2.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385-396. [PubMed] [Google Scholar]
- 3.Cohen S, Tyrrell DAJ, Smith AP. Psychological stress and susceptibility to the common cold. N Engl J Med. 1991;325(9):606-612. [DOI] [PubMed] [Google Scholar]
- 4.Ezzati A, Jiang J, Katz MJ, Sliwinski MJ, Zimmerman ME, Lipton RB. Validation of the Perceived Stress Scale in a community sample of older adults. Int J Geriatr Psychiatr. 2014;29(6):645-652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Osmanovic-Thunström A, Mossello E, Åkerstedt T, Fratiglioni L, Wang HX. Do levels of perceived stress increase with increasing age after age 65? A population-based study. Age Ageing. 2015;44(5):828-834. [DOI] [PubMed] [Google Scholar]
- 6.Luchesi BM, Souza ÉN, Gratão ACM, Gomes GADO, Inouye K, Alexandre TDS, et al. The evaluation of perceived stress and associated factors in elderly caregivers. Arch Gerontol Geriatr. 2016;67:7-13. [DOI] [PubMed] [Google Scholar]
- 7.Peavy GM, Lange KL, Salmon DP, Patterson TL, Goldman S, Gamst AC, et al. The effects of prolonged stress and APOE genotype on memory and cortisol in older adults. Biol Psychiatr. 2007;62(5):472-478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peavy GM, Salmon DP, Jacobson MW, Hervey A, Gamst AC, Wolfson T, et al. Effects of chronic stress on memory decline in cognitively normal and mildly impaired older adults. Am J Psychiatr. 2009;166(12):1384-1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peavy GM, Jacobson MW, Salmon DP, Gamst AC, Patterson TL, Goldman S, et al. The influence of chronic stress on dementia-related diagnostic change in older adults. Alzheimer Dis Assoc Disord. 2012;26(3):260-266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gershon A, Johnson SL, Miller I. Chronic stressors and trauma: prospective influences on the course of bipolar disorder. Psychol Med. 2013;43(12):2583-2592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dong GC, Li M. Stressful Life Events and Late-Life Cognitive Function in Community-Dwelling Chinese Older Adults: Findings from a Population-Based Cohort Study in the Greater Chicago Area. Journal of Ageing and Longevity. 2021;1:24-35. [Google Scholar]
- 12.Mitra R, Jadhav S, McEwen BS, Vyas A, Chattarji S. Stress duration modulates the spatiotemporal patterns of spine formation in the basolateral amygdala. Proc Natl Acad Sci Unit States Am. 2005;102(26):9371-9376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jacinto LR, Mata R, Novais A, Marques F, Sousa N. The habenula as a critical node in chronic stress-related anxiety. Exp Neurol. 2017;289:46-54. [DOI] [PubMed] [Google Scholar]
- 14.Das SK, Baitharu I, Barhwal K, Hota SK, Singh SB. Early mood behavioral changes following exposure to monotonous environment during isolation stress is associated with altered hippocampal synaptic plasticity in male rats. Neurosci Lett. 2016;612:231-237. [DOI] [PubMed] [Google Scholar]
- 15.Duclot F, Hollis F, Darcy MJ, Kabbaj M. Individual differences in novelty-seeking behavior in rats as a model for psychosocial stress-related mood disorders. Physiol Behav. 2011;104(2):296-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iñiguez SD, Flores-Ramirez FJ, Riggs LM, Alipio JB, Garcia-Carachure I, Hernandez MA, et al. Vicarious social defeat stress induces depression-related outcomes in female mice. Biol Psychiatr. 2018;83(1):9-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cooper C, Balamurali TB, Livingston G. A systematic review of the prevalence and covariates of anxiety in caregivers of people with dementia. Int Psychogeriatr. 2007;19(2):175-195. [DOI] [PubMed] [Google Scholar]
- 18.Monteiro AMF, Santos RL, Kimura N, Baptista MAT, Dourado MCN. Coping strategies among caregivers of people with Alzheimer disease: a systematic review. Trends in Psychiatry and Psychotherapy. 2018;40(3):258-268. [DOI] [PubMed] [Google Scholar]
- 19.Mahoney R, Regan C, Katona C, Livingston G. Anxiety and depression in family caregivers of people with Alzheimer disease: the LASER-AD study. Am J Geriatr Psychiatr. 2005;13(9):795-801. [DOI] [PubMed] [Google Scholar]
- 20.Mausbach BT, Chattillion EA, Roepke SK, Patterson TL, Grant I. A comparison of psychosocial outcomes in elderly Alzheimer caregivers and noncaregivers. Am J Geriatr Psychiatr. 2013;21(1):5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mohamed S, Rosenheck R, Lyketsos CG, Schneider LS. Caregiver burden in Alzheimer disease: cross-sectional and longitudinal patient correlates. Am J Geriatr Psychiatr. 2010;18(10):917-927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Manzini CSS, do Vale FAC. Emotional disorders evidenced by family caregivers of older people with Alzheimer’s disease. Dementia Neuropsychologia. 2020;14(1):56-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mayo AM, Siegle K, Savell E, Bullock B, Preston GJ, Peavy GM. Lay caregivers' experiences with caring for persons with dementia: A phenomenological study. J Gerontol Nurs. 2020;46(8):17-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Del-Pino-Casado R, Rodríguez Cardosa M, López-Martínez C, Orgeta V. The association between subjective caregiver burden and depressive symptoms in carers of older relatives: A systematic review and meta-analysis. PLoS One. 2019;14(5):e0217648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cacioppo S, Capitanio JP, Cacioppo JT. Toward a neurology of loneliness. Psychol Bull. 2014;140(6):1464-1504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee EE, Depp C, Palmer BW, Glorioso D, Daly R, Liu J, et al. High prevalence and adverse health effects of loneliness in community-dwelling adults across the lifespan: role of wisdom as a protective factor. Int Psychogeriatr. 2019;31(10):1447-1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Quadt L, Esposito G, Critchley HD, Garfinkel SN. Brain-body interactions underlying the association of loneliness with mental and physical health. Neurosci Biobehav Rev. 2020;116:283-300. [DOI] [PubMed] [Google Scholar]
- 28.Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality. Perspect Psychol Sci. 2015;10(2):227-237. [DOI] [PubMed] [Google Scholar]
- 29.Sundström A, Adolfsson AN, Nordin M, Adolfsson R. Loneliness increases the risk of all-cause dementia and alzheimer's disease. J Gerontol: Ser Bibliogr. 2020;75(5):919-926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rafnsson SB, Orrell M, d’Orsi E, Hogervorst E, Steptoe A. Loneliness, Social Integration, and Incident Dementia Over 6 Years: Prospective Findings From the English Longitudinal Study of Ageing. J Gerontol: Ser Bibliogr. 2020;75(1):114-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wilson RS, Krueger KR, Arnold SE, Schneider JA, Kelly JF, Barnes LL, et al. Loneliness and risk of Alzheimer disease. Arch Gen Psychiatr. 2007;64(2):234-240. [DOI] [PubMed] [Google Scholar]
- 32.Donovan NJ, Okereke OI, Vannini P, Amariglio RE, Rentz DM, Marshall GA, et al. Association of higher cortical amyloid burden with loneliness in cognitively normal older adults. JAMA Psychiatry. 2016;73(12):1230-1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Adams KB. Specific effects of caring for a spouse with dementia: differences in depressive symptoms between caregiver and non-caregiver spouses. Int Psychogeriatr. 2008;20(3):508-520. [DOI] [PubMed] [Google Scholar]
- 34.Beeson R, Horton-Deutsch S, Farran C, Neundorfer M. Loneliness and depression in caregivers of persons with Alzheimer's disease or related disorders. Issues Ment Health Nurs. 2000;21(8):779-806. [DOI] [PubMed] [Google Scholar]
- 35.Shin C, Park MH, Lee H, Ko YH, Kim YK, Han KM, et al. Usefulness of the 15-item geriatric depression scale (GDS-15) for classifying minor and major depressive disorders among community-dwelling elders. J Affect Disord. 2019;259:370-375. [DOI] [PubMed] [Google Scholar]
- 36.Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Consulting Psychologists Press; 1983. [Google Scholar]
- 37.de Jong-Gierveld J, Kamphuls F. The development of a Rasch-type loneliness scale. Appl Psychol Meas. 1985;9:289-299. [Google Scholar]
- 38.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. J Psychiatr Res. 1975;12(3):189-198. [DOI] [PubMed] [Google Scholar]
- 39.Pfeffer RI, Kurosaki TT, Harrah CH, Jr., Chance JM, Filos S. Measurement of functional activities in older adults in the community. J Gerontol. 1982;37(3):323-329. [DOI] [PubMed] [Google Scholar]
- 40.Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695-699. [DOI] [PubMed] [Google Scholar]
- 41.Brown GW, Harris TO. The Bedford College Life Events and Difficulty Schedule: Directory of Contextual Threat Ratings of Events. University of London; 1978. [Google Scholar]
- 42.Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS). Recent evidence and development of a shorter version. In: Brink TL, ed. Clinical Gerontology: A Guide to Assessment and Intervention. NY: The Haworth Press, Inc.; 1986:165-173. [Google Scholar]
- 43.van Tilburg TG, de Jong Gierveld J. [Reference standards for the loneliness scale]. Tijdschr Gerontol Geriatr. 1999;30(4):158-163. [PubMed] [Google Scholar]
- 44.Rosseel Y. lavaan: An R Package for Structural Equation Modeling. J Stat Software. 2012;48(2):1-36. [Google Scholar]
- 45.R_Core_Team . R: A language and environment for statistical computing. R Foundation for Statistical Computing. 2020; Available from: https://www.R-project.org/
- 46.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Model. 1999;6(1):1-55. [Google Scholar]
- 47.Sobel ME. Some New Results on Indirect Effects and Their Standard Errors in Covariance Structure Models. Socio Methodol. 1986;16:159-186. [Google Scholar]
- 48.Nordin M, Nordin S. Psychometric evaluation and normative data of the Swedish version of the 10-item perceived stress scale. Scand J Psychol. 2013;54(6):502-507. [DOI] [PubMed] [Google Scholar]
- 49.Greenberg SA. How to try this: the Geriatric Depression Scale: Short Form. American Journal of Nursing. 2007;107(10):60-69. [DOI] [PubMed] [Google Scholar]
- 50.Pearlin LI, Menaghan EG, Lieberman MA, Mullan JT. The stress process. J Health Soc Behav. 1981;22(4):337-356. [PubMed] [Google Scholar]
- 51.McEwen BS, Akil H. Revisiting the Stress Concept: Implications for Affective Disorders. J Neurosci. 2020;40(1):12-21. [DOI] [PMC free article] [PubMed] [Google Scholar]