Key Points
Question
What are the treatment rates for mental disorders among children and adolescents?
Findings
In this meta-analysis of 40 studies including 310 584 children and adolescents, the combined treatment rate was 38% (95% CI, 30%-45%) for any mental disorder, 36% (95% CI, 29%-43%) for depressive disorders, 31% (95% CI, 21%-42%) for anxiety disorders, 58% (95% CI, 42%-73%) for attention-deficit/hyperactivity disorder, and 49% for behavior disorders (95% CI, 35%-64%). Age, income level, and region were significantly associated with treatment rates for mental disorders among youths.
Meaning
This study suggests that the treatment rates of mental disorders among children and adolescents were generally low, especially for depression and anxiety; targeted interventions are needed to improve this situation.
Abstract
Importance
Mental disorders among children and adolescents are global health concerns. Published studies have provided discordant results regarding treatment rates for mental disorders among youths.
Objective
To estimate combined treatment rates for several common psychiatric disorders among children and adolescents.
Data Sources
PubMed, Web of Science, PsycINFO, Scopus, and Embase were searched from database inception until September 23, 2022, and supplemented with hand-searching of reference lists.
Study Selection
Included studies were those that used validated methods to report treatment rates for any mental disorder, depressive disorders, anxiety disorders, attention-deficit/hyperactivity disorder (ADHD), and behavior disorders among children and adolescents.
Data Extraction and Synthesis
This study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guideline. Two reviewers independently assessed study eligibility, extracted data, and scored quality. Studies with a Joanna Briggs Institute score of 5 or more were included in the meta-analysis. Treatment rates were pooled using random-effects models. Subgroup analyses were performed to investigate the association with treatment rates of factors, such as year of data collection, World Health Organization region, age, income level, timeframe of diagnosis, informant source, service type, sample origin, and internalizing or externalizing disorder.
Main Outcomes and Measures
Treatment rates for mental disorders among children and adolescents were the main outcomes, measured as percentage estimates.
Results
Forty studies were included in the analysis, comprising 310 584 children and adolescents, with boys accounting for 39% of participants (sex was not reported in 10 studies). The pooled treatment rate was 38% (95% CI, 30%-45%) for any mental disorder, 36% (95% CI, 29%-43%) for depressive disorders, 31% (95% CI, 21%-42%) for anxiety disorders, 58% (95% CI, 42%-73%) for ADHD, and 49% (95% CI, 35%-64%) for behavior disorders. Age, income level, and region were significantly associated with the combined treatment rates of mental disorders in children and adolescents. The treatment rate for depressive disorders was higher among adolescents than children (36% [95% CI, 25%-46%] vs 11% [95% CI, 0%-25%]), whereas the treatment rate for anxiety disorders was higher among children than adolescents (64% [95% CI, 52%-75%] vs 20% [95% CI, 9%-30%]). The treatment rate for any mental disorder in lower-middle income countries was 6% (95% CI, 2%-14%), in upper-middle income countries was 24% (95% CI, 2%-47%), and in high-income countries was 43% (95% CI, 35%-52%). For depressive disorders, treatment rates were higher in the Americas (40% [95% CI, 30%-51%]) than in Europe (28% [95% CI, 13%-43%]) and the Western Pacific region (6% [95% CI, 1%-16%]).
Conclusions and Relevance
This study suggests that, in general, the treatment rates for mental disorders among children and adolescents were low, especially for depression and anxiety. Targeted intervention policies and effective measures should be designed and implemented to improve treatment rates of psychiatric disorders among youths.
This meta-analysis of 40 studies estimates combined treatment rates for several common psychiatric disorders among children and adolescents.
Introduction
Over the past several decades, the prevalence of mental disorders among children and adolescents has been increasing substantially, which has caused a heavy burden on the public.1 Anxiety, depression, attention-deficit/hyperactivity disorder (ADHD), and behavior disorders, such as oppositional-defiant disorder and conduct disorders, are the most common mental disorders among children and adolescents: a meta-analysis showed that the worldwide pooled prevalence reached 7% for anxiety disorders, 3% for depressive disorders, 3% for ADHD, and 6% for behavior disorders.2 The prevalence of mental disorders varies considerably in different regions: 20% in North America, 12% in Europe and Asia, and 8% in Africa. Sex and age differences are also apparent: for instance, boys are more likely than girls to receive a diagnosis of ADHD and adolescents are more susceptible than children to affective disorders and behavior disorders.3
Among children and adolescents, mental disorders are associated with a variety of negative outcomes, such as absenteeism, substance abuse, and suicidal behaviors.4,5,6 Moreover, the detrimental effect of early initiated mental disorders can extend into adulthood: longitudinal studies found that approximately 75% of psychiatric diseases diagnosed among adults had roots in childhood or adolescence.7 Timely and effective treatment of mental disorders significantly reduces the risk of subsequent negative outcomes and saves related health costs.8 Currently, evidence-based pharmacologic and nonpharmacologic treatments have been used in managing mental disorders among children and adolescents. However, owing to concerns regarding safety and adverse effects, the use of medication among children and adolescents is still controversial.9 Nonpharmacologic methods have been more widely used in this age group. For example, abundant studies have proven that family-centered psychotherapies that require the involvement of parents are critical in the therapeutic success of mental disorders among children and adolescents.10,11,12
However, among children and adolescents with mental disorders, only a small fraction have received treatment.13 In the US, approximately half of all children with mental health problems have received mental health services14; in the Netherlands, the treatment rate was 21%.15 Data on treatment rates in low- and middle-income countries (LMICs) are still limited, but available evidence suggests an overall treatment rate of less than 20% in upper-middle income countries (UMICs).16,17 However, published studies have reported highly variant treatment rates for mental disorders among children and adolescents, which causes confusion in understanding the true severity of the problem. For instance, the treatment rate for depressive disorders was reported as less than 10% in a study from China,18 while the rate was reported as 64% in a US study.19 In this meta-analysis, we aim to synthesize currently available evidence of high quality to estimate treatment rates for several commonly seen mental disorders among children and adolescents.
Methods
This study was registered in PROSPERO (CRD42023398984) and performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guideline.
Retrieval Strategy and Eligibility Criteria
A systematic review of the literature was conducted using PubMed, Web of Science, PsycINFO, Scopus, and Embase from database inception to September 23, 2022, and the reference search was conducted for the included literature simultaneously. The search process and terms used are listed in eMethods 1 and the eAppendix in Supplement 1. Study inclusion criteria were (1) the upper limit of the age range was 18 years (to avoid missing pertinent studies, articles that did not specify the age range but instead reported a mean age of <18 years were also included); (2) treatment rates for mental disorders were reported; (3) diagnosis of mental disorder was based on well-accepted diagnostic methods; and (4) the article was published in English. There were no restrictions on study design.
Data Extraction
A standard information extraction table was designed. Two of us (S.W. and Q.L.) independently extracted relevant information from all included studies, and the results were compared carefully; if any inconsistencies in extracted data were found, the 2 authors checked the full text of the relevant studies together, to see whether consensus could be reached after discussion. If they failed to reach a consensus, a senior researcher (Y.X.) performed the data extraction again.
Exposure and Outcome
Exposure included the following commonly seen mental disorders among children and adolescents: any mental disorder, depressive disorders, anxiety disorders, ADHD, and behavior disorders. We included only studies that conducted diagnostic interviews based on the third, fourth, and fifth editions of the Diagnostic and Statistical Manual of Mental Disorders or the International Classification of Diseases, Ninth Revision or the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision. Depressive disorders included major depressive disorder, destructive mood disorder, and dysthymia. Anxiety disorders included the full spectrum of diagnoses, such as generalized anxiety disorder, panic disorder, and posttraumatic stress disorder. Behavior disorders included oppositional defiant disorder and conduct disorder. Details of definitions and diagnostic tools for included mental disorders are in eMethods 2 in Supplement 1.
The major outcome was the proportion of diagnosed patients who received treatment or medical services. Treatment seeking was defined as use of treatment services for a mental health problem. Services included general medical services delivered by health care clinicians or health professionals, specialist mental health services delivered by mental health professionals, and school-based psychological counseling or treatment services. Seeking help from informal channels was excluded.
Study Quality Assessment
We used the 9-item Joanna Briggs Institute (JBI) Checklist for Prevalence Studies to evaluate the quality of the included studies.20 Each item in the JBI Checklist was assigned 1 point for meeting the criterion, with a maximum score of 9 points. An overall score of 5 or more indicates satisfactory quality.21
Statistical Analysis
Analyses were conducted using the “meta” and “forestplot” packages in R, version 4.2.2 (R Group for Statistical Computing). Forest plots were used to display the results graphically. A random-effects meta-analysis model was used to combine treatment rates. Heterogeneity was assessed using the Cochran Q test and the I2 index.22 The risk of publication bias was evaluated by visual inspection of a funnel plot, and further checked by the Egger test and a nonparametric trim-and-fill method.23 A series of stratified analyses were done to explore the origins of heterogeneity, in which the following factors were considered: year of data collection, region, age, income level, timeframe of diagnosis, informant sources, health service type, sample source, and internalizing or externalizing disorders. Statistical significance was set as P < .05, 2-tailed. The P value for all secondary subgroup analyses was adjusted using the Bonferroni correction. Sensitivity analyses were further performed to check the robustness of combined estimations.
Results
Study Selection
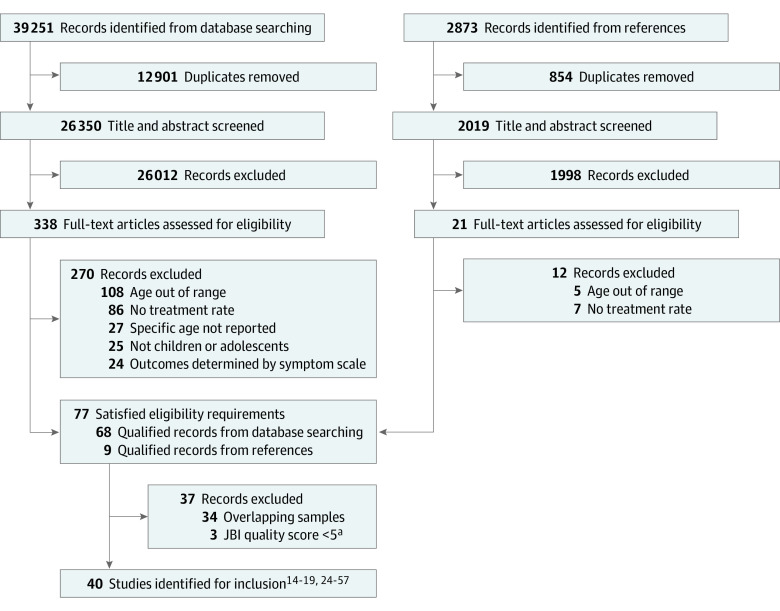
The procedure of literature screening is shown in a PRISMA flowchart (Figure 1).14,15,16,17,18,19,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57 In total, 39 251 records were found through literature searching, and 40 studies14,15,16,17,18,19,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57 were included after being screened by the researchers. Refer to the eResults in Supplement 1 for the detailed retrieval steps.
Figure 1. PRISMA Flow Diagram.
aThe Joanna Briggs Institute (JBI) quality score was evaluated by the JBI checklist for prevalence studies.
Study Characteristics
Table 1 shows the characteristics of all studies.14,15,16,17,18,19,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57 The 40 included articles were published between 1988 and 2021, and the data for the included studies were collected between 1984 and 2017 (5 studies19,24,25,30,38 did not specify when the data were collected). A total of 310 584 participants were included, with boys accounting for 39% (sex was not reported in 10 studies16,17,24,25,26,32,37,40,44,51). Seventeen studies reported treatment rates for any mental disorder,14,15,16,17,24,26,29,32,34,37,38,41,44,47,51,54,55 20 for depressive disorders,14,17,18,19,26,30,31,33,35,36,39,42,45,46,47,52,53,55,56,57 9 for anxiety disorders,14,17,26,30,35,47,48,49,55 10 for ADHD,14,25,27,28,30,31,40,43,47,50 and 7 for behavior disorders.26,31,37,40,47,55,56
Table 1. Study Characteristics.
| Source and country | WHO region | Income | Year of data collection | Sample origin | Sample size, No. | Age, mean (SD) or range, y, or grade | Male, % | Timeframe | Informant source | Outcomes | Tools |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Angold et al,24 2002; US | AMR | HIC | NR | School | 920 | 9-17 | NR | Last 3 mo | Parent and child | AMD | CAPA |
| Bird et al,25 2008; US | AMR | HIC | NR | Community | 2491 | 5-13 | NR | Last year | Child | ADHD | DISC-IV |
| Borges et al,17 2008; Mexico | AMR | UMIC | 2005 | Community | 3005 | 12-17 | NR | Last year | Child | AMD, DD, and AD | CIDI |
| Buckner and Bassuk,26 1997; US | AMR | HIC | 1992-1995 | Health care institution | 94 | 9-17 | NR | Last 6 mo or lifetime | Parent | DD, AD, AMD, and BD | DISC 2.3 |
| Bussing et al,27 2003; US | AMR | HIC | 1998-2000 | School | 1615 | 7.8 (1.8) | 52 | Current | Parent | ADHD | DISC-IV |
| Bussing et al,28 2011; US | AMR | HIC | 2004-2005 | School | 168 | 6.8 (0.5) | 47 | Last year or lifetime | Parent | ADHD | DISC-IV |
| Canino et al,29 2004; US | AMR | HIC | 1999-2000 | Community | 1879 | 4-17 | 53 | Last year | Parent and child | AMD | DISC-IV |
| Chavira et al,30 2004; US | AMR | HIC | NR | Health care institution | 190 | 8-17 | 50 | Lifetime | Parent | AD, DD, and ADHD | ADIS-C/P |
| Coker et al,31 2009; US | AMR | HIC | 2004-2006 | School | 5121 | Fifth grade | 51 | Lifetime | Parent | ADHD, BD, and DD | DISC |
| Cuffe et al,32 2001; US | AMR | HIC | 1987-1989 | School | 579 | 12.83 | NR | Lifetime | Parent and child | AMD | K-SADS |
| Cummings and Druss,33 2011; US | AMR | HIC | 2004-2008 | Community | 90 855 | 15.1 (0.02); 12-17 | 28 | Last year | Child | DD | CIDI-SF |
| Daeem et al,34 2019; Israel | EMR | HIC | 2012-2013 | School | 1639 | Ninth grade | 48 | Lifetime | Parent | AMD | DAWBA |
| Essau et al,35 2005; Germany | EMR | HIC | 1996-1997 | School | 1035 | 12-17 | 41 | Lifetime | Child | AD and DD | CIDI |
| Fatori et al,16 2019; Brazil | AMR | UMIC | 2010-2011 | Community | 2511 | 6-12 | NR | Lifetime | Parent | AMD | DAWBA |
| Flament et al,36 2001; France | EUR | HIC | 1988-1990 | School | 3287 | 17.6 (1.6) | 47 | Lifetime | Child | DD | K-SADS |
| Georgiades et al,37 2019; Canada | AMR | HIC | 2014-2015 | Community | 6537 | 4-17 | NR | Last 6 mo | Parent and child | AMD and BD | MINI-KID |
| Gómez-Beneyto et al,38 1994; Spain | EUR | HIC | NR | Community | 1127 | 8-15 | 50 | Lifetime | Child | AMD | K-SADS |
| Gould et al,39 2009; US | AMR | HIC | 2002-2006 | School | 2342 | 15 (1.0); 13-19 | 42 | Last year | Child | DD | DISC-IV |
| Heiervang et al,40 2007; Norway | EUR | HIC | 2002-2003 | School | 6297 | 7-9 | NR | Lifetime | Parent | ADHD and BD | DAWBA |
| Leaf et al,41 1996; US | AMR | HIC | 1991-1992 | NR | 1285 | 12.9 (2.6); 9-17 | 53 | Last year or lifetime | Parent and child | AMD | DISC 2.3 |
| Lewinsohn et al,42 1998; US | AMR | HIC | 1987-1989 | School | 1507 | 13.4 | 52 | Lifetime | Child | DD | K-SADS |
| Locke et al,43 2017; US | AMR | HIC | 2008-2009 | Health care institutions | 23 601 | 5-17 | 63 | Lifetime | Child | ADHD | ICD-9 |
| Maalouf et al,44 2016; Lebanon | EMR | LMIC | 2012 | Community | 510 | 11-17 | NR | Lifetime | Parent | AMD | DAWBA |
| Magklara et al,45 2015; Greece | EUR | HIC | 2007-2008 | School | 2427 | 16-18 | 41 | Last year | Child | DD | ICD-10 |
| Meredith et al,46 2009; US | AMR | HIC | 2005-2006 | Health care institution | 368 | 15.2 (1.4); 13-17 | 22 | Last 6 mo | Child | DD | DISC |
| Merikangas et al,14 2010; US | AMR | HIC | 2001-2004 | Community | 3042 | 8-15 | 49 | Last year | Child | AMD, ADHD, AD, and DD | DISC-IV |
| Merikangas et al,47 2011; US | AMR | HIC | 2002-2004 | Community | 6483 | 13-18 | 51 | Lifetime | Parent and child | AMD, DD, AD, ADHD, and BD | CIDI |
| Niermann et al,48 2021; Germany | EUR | HIC | 2015 | Community | 635 | 14-17 | 42 | Lifetime | Child | AD | CIDI |
| Reardon et al,49 2020; Great Britain | EUR | HIC | 2016-2017 | School | 222 | 9.6 (1.2); 7-11 | 52 | Lifetime | parent | AD | ADIS-P |
| Sawyer et al,50 2004; Australia | AMR | HIC | 1998 | Community | 398 | 6-17 | 69 | Last 6 mo | Parent | ADHD | DISC-IV |
| Sawyer et al,51 2018; Australia | AMR | HIC | 2013-2014 | Community | 6310 | 4-17 | NR | Last year | Parent | AMD | DISC-IV |
| Stiffman et al,52 1988; US | AMR | HIC | 1984-1985 | Health care institution | 2787 | 13-18 | 33 | Last year | Child | DD | DICA |
| Tanielian et al,53 2009; US | AMR | HIC | 2005-2006 | Health care institution | 4713 | 15.2 (1.3); 13-17 | 22 | Last 6 mo | Parent and child | DD | DISC |
| Vicente et al,54 2012; Chile | AMR | HIC | 2007-2009 | Community | 1558 | 4-18 | 51 | Last year | Parent and child | AMD | DISC-IV |
| Wagner et al,55 2017; Austria | EUR | HIC | 2013-2015 | School | 3477 | 10-18 | 45 | Lifetime | Child | DD, AD, BD, and AMD | CDI-MD |
| Wu et al,56 1999; US | AMR | HIC | 1991-1992 | Community | 1285 | 12.9 (2.6); 9-17 | 53 | Last year or lifetime | Parent and child | DD and BD | DISC 2.3 |
| Wu et al,19 2001; US | AMR | HIC | NR | Community | 206 | 9-17 | 44 | Last year | Parent and child | DD | DISC 2.3 |
| Zhang et al,57 2021; US | AMR | HIC | 2010-2016 | Community | 11 4250 | 12-17 | 51 | Last year | Child | DD | CIDI-SF |
| Zhong et al,18 2013; China | WPR | UMIC | 2009-2010 | Community | 3582 | 6-14 | 52 | Lifetime | Parent and child | DD | MINI-KID |
| Zwaanswijk et al,15 2005; Netherlands | EUR | HIC | 2000-2002 | Health care institution | 246 | 4-11 | 56 | Last year | Parent | AMD | DISC-IV |
Abbreviations: AD, anxiety disorders; ADHD, attention-deficit/hyperactivity disorder; ADIS-C/P, Anxiety Disorders Interview, Children-Parent Version; ADIS-P, Anxiety Disorder Interview Schedule, Parent Version; AMD, any mental disorder; AMR, region of the Americas; BD, behavior disorders; CAPA, Child and Adolescent Psychiatric Assessment; CDI-MD, Children’s Diagnostic Interview for Mental Disorders; CIDI, World Mental Health Composite International Diagnostic Interview; CIDI-SF, World Composite International Diagnostic Interview–Short Form; DAWBA, Development and Well-Being Assessment; DICA, Diagnostic Interview for Children and Adolescents; DISC, Diagnostic Interview for Children; DISC-IV, Diagnostic Interview for Children, Version IV; DISC 2.3, NIMH Diagnostic Interview Schedule for Children, Version 2.3; DD, depressive disorders; EMR, Eastern Mediterranean region; EUR, European region; HIC, high-income country; ICD-9, International Classification of Diseases, Ninth Revision; ICD-10, International Statistical Classification of Diseases and Related Health Problems, Tenth Revision; K-SADS, Present Episode Version of the Schedule for Affective Disorders and Schizophrenia for School-Aged Children; LMIC, lower-middle income country; MINI-KID, Mini International Neuropsychiatric Interview for Children and Adolescents; NR, information not reported in the article; UMIC, upper-middle income country; WHO, World Health Organization; WPR, Western Pacific region.
Quality Assessment
For the risk of bias assessment, 34 (85%) included articles were of medium quality (JBI score 5-7) and 6 (15%) articles were of high quality (JBI score ≥8). The details of the quality assessment are shown in the eTable in Supplement 1.
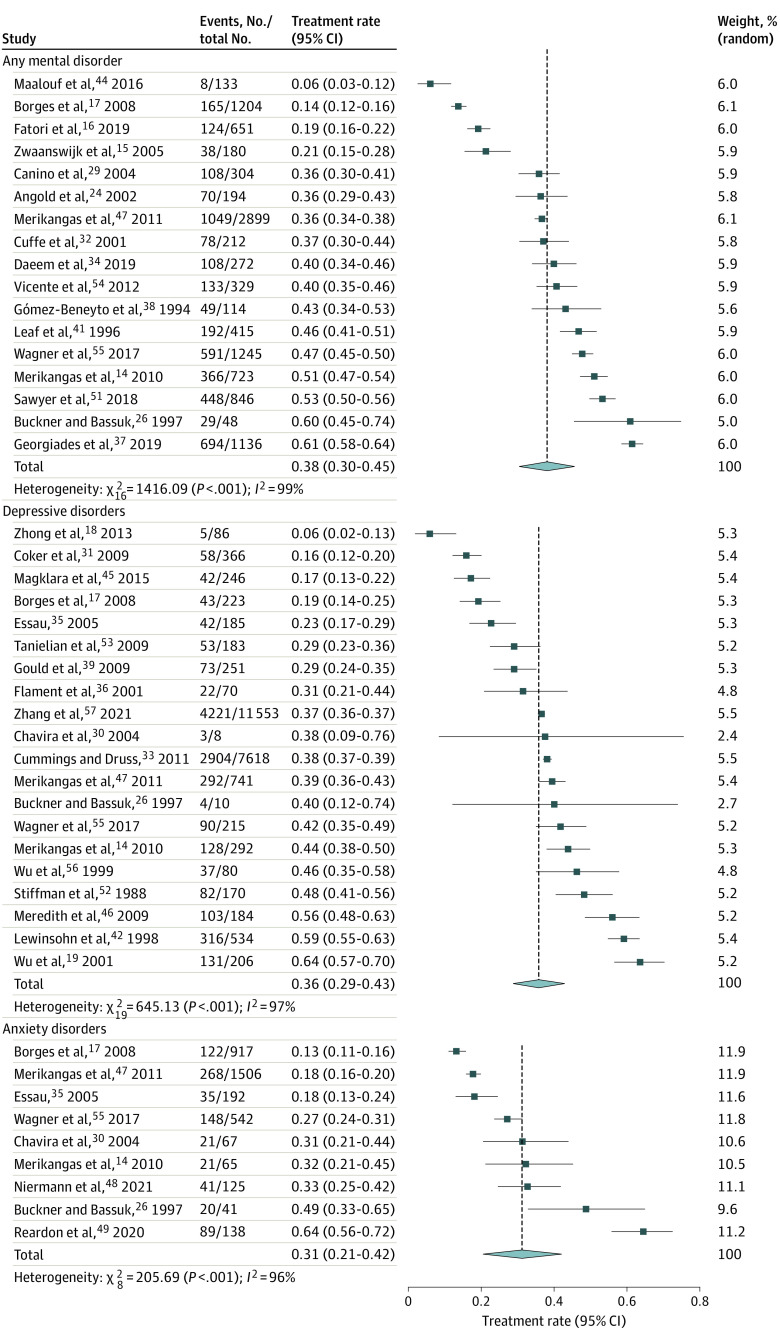
Treatment Rates for Mental Disorders
The pooled treatment rate of any mental disorder from the random-effects meta-analysis was 38% (95% CI, 30%-45%) (Figure 2), which was highly heterogeneous (I2 = 99%; P < .001). The combined treatment rate was 36% (95% CI, 29%-43%; I2 = 97%; P < .001) (Figure 2) for depressive disorders, 31% (95% CI, 21%-42%; I2 = 96%; P < .001) (Figure 2) for anxiety disorders, 58% (95% CI, 42%-73%; I2 = 100%; P < .001) (eFigure 52 in Supplement 1) for ADHD, and 49% (95% CI, 35%-64%; I2 = 99%; P < .001) (eFigure 53 in Supplement 1) for behavior disorders, all of which were highly heterogeneous.
Figure 2. Forest Plots for Treatment Rates of Mental Disorders in Children and Adolescents.
Subgroup Analysis
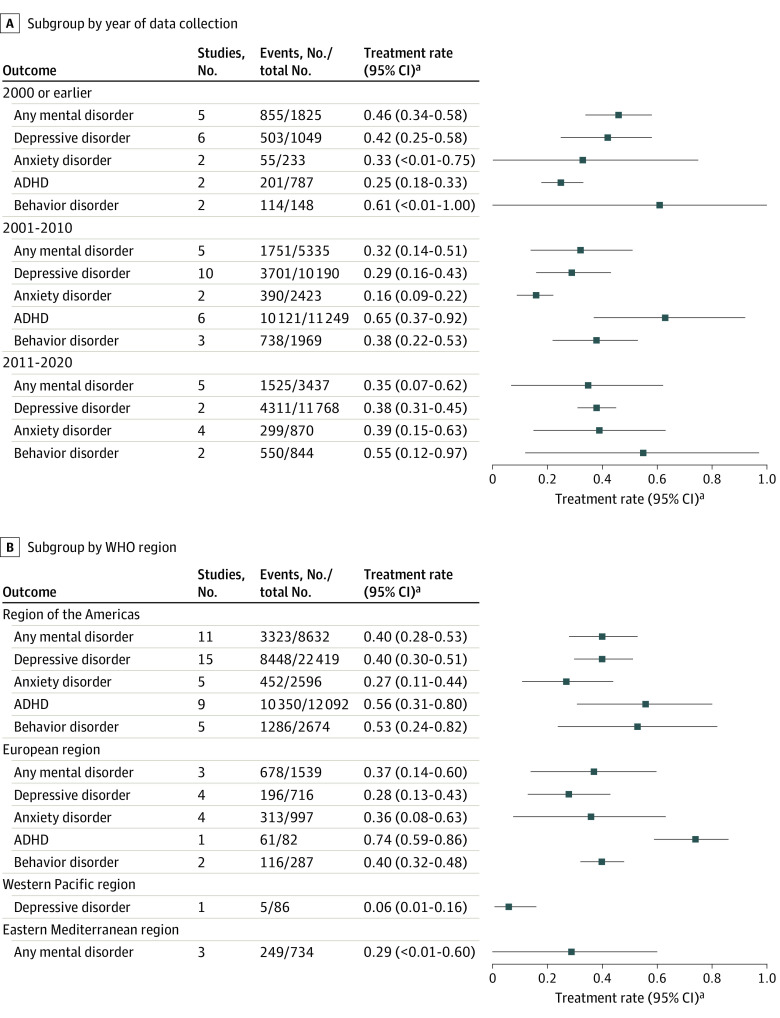
Treatment Rates by Year of Data Collection
Figure 3A shows treatment rates by year of data collection. There were no significant differences in treatment rates for any mental disorder, depressive disorders, anxiety disorders, or behavior disorders (eFigures 1-3, and 5 in Supplement 1). Subgroup differences were statistically significant only for ADHD (eFigure 4 in Supplement 1).
Figure 3. Forest Plots for Subgroup Analyses by Different Factors.
A, Subgroup by year of data collection. B, Subgroup by World Health Organization (WHO) region. ADHD indicates attention-deficit/hyperactivity disorder.
a95% CIs adjusted by Bonferroni correction.
Treatment Rates by Region
Figure 3B shows treatment rates by region. For any mental disorder, anxiety disorders, ADHD, and behavior disorders, treatment rates were not statistically different among all regions (eFigures 6 and 8-10 in Supplement 1). For depressive disorders, treatment rates were higher in the Americas (40%; 95% CI, 30%-51%) than in Europe (28%; 95% CI, 13%-43%) and the Western Pacific region (6%; 95% CI, 1%-16%) (P < .001; eFigure 7 in Supplement 1).
Treatment Rates by Age
eFigure 54 in Supplement 1 shows treatment rates by age. There were no significant differences between children (≤12 years of age) and adolescents (13-17 years of age) in treatment rates of any mental disorder, ADHD, and behavior disorders (eFigures 11, 14, and 15 in Supplement 1). The treatment rate for depressive disorders was higher among adolescents (36%; 95% CI, 25%-46%) than children (11%; 95% CI, 0%-25%) (P < .001; eFigure 12 in Supplement 1), whereas the treatment rate for anxiety disorders was higher among children (64%; 95% CI, 52%-75%) than adolescents (20%; 95% CI, 9%-30%) (P < .001; eFigure 13 in Supplement 1).
Treatment Rates by Income Level
eFigure 55 in Supplement 1 shows treatment rates by income level. The treatment rate for any mental disorder in lower-middle income countries was 6% (95% CI, 2%-14%), in upper-middle income countries was 24% (95% CI, 2%-47%), and in high-income countries (HICs) was 43% (95% CI, 35%-52%). The treatment rate for depressive disorders was 13% (95% CI, 0%-31%) in UMICs and 39% (95% CI, 29%-48%) in HICs (eFigure 17 in Supplement 1); the treatment rate for anxiety disorders was 31% (95% CI, 16%-46%) in UMICs and 34% (95% CI, 18%-49%) in HICs (eFigure 18 in Supplement 1). There were significant differences among income groups in the treatment rates of any mental disorder, depressive disorders, and anxiety disorders (eFigures 16-18 in Supplement 1). Studies reporting ADHD and behavior disorders were all from HICs.
Treatment Rates by Other Important Characteristics
Subgroup analyses were also performed using other important characteristics, such as timeframe of diagnosis, informant source, health service type, sample source population, and internalizing or externalizing disorder (eFigures 19-43 in Supplement 1). Incongruity was observed in treatment rates of anxiety reported by different informant sources: parents reported higher treatment rates (48% [95% CI, 21%-76%]) than children themselves (24% [95% CI, 13%-35%]) (eFigure 28 in Supplement 1). The combined treatment rate for internalizing disorders was 34% (95% CI, 26%-43%), significantly lower than the rate for externalizing disorders (54%; 95% CI, 39%-70%) (eFigure 43 in Supplement 1).
Sensitivity Analysis and Publication Bias
Leave-one-out sensitivity analysis of any mental disorder, depressive disorders, anxiety disorders, ADHD, and behavior disorders showed acceptable stability of the pooled results (Table 2; eFigures 44-48 in Supplement 1). Outlier analysis was performed by excluding studies in which the 95% CIs were outside the aggregated 95% CI of all studies, and the combined results showed insignificant change (eFigure 49 in Supplement 1). Another round of sensitivity analysis, including only studies (n = 32) with the upper limit of participant age range of 18 years, showed that the combined estimates were comparable to those based on all 40 included studies (eFigure 50 in Supplement 1). Funnel plots, together with the Egger test and the trim-and-fill method suggested significant publication bias for anxiety disorders and ADHD (eFigure 51 in Supplement 1).
Table 2. Summary of Leave-One-Out Sensitivity Analysis Results.
| Outcome | Combined treatment rate (95% CI) | ||
|---|---|---|---|
| Minimum | Maximum | Overall | |
| Any mental disorder | 0.36 (0.29-0.44) | 0.40 (0.33-0.46) | 0.38 (0.30-0.45) |
| Depressive disorders | 0.34 (0.28-0.41) | 0.37 (0.31-0.44) | 0.36 (0.29-0.43) |
| Anxiety disorders | 0.26 (0.19-0.33) | 0.34 (0.23-0.45) | 0.31 (0.21-0.42) |
| ADHD | 0.52 (0.38-0.65) | 0.60 (0.46-0.75) | 0.58 (0.42-0.73) |
| Behavior disorders | 0.44 (0.32-0.56) | 0.53 (0.38-0.69) | 0.49 (0.35-0.64) |
Abbreviation: ADHD, attention-deficit/hyperactivity disorder.
Discussion
This meta-analysis included 40 studies, comprising 310 584 children and adolescents, that reported treatment rates for mental disorders among children and adolescents. After synthesis, the combined treatment rate was 38% for any mental disorder, 36% for depressive disorders, 31% for anxiety disorders, 58% for ADHD, and 49% for behavior disorders. Moreover, treatment rates for mental disorders among children and adolescents varied significantly across different regions and income levels. Other characteristics, such as age, also showed a nonnegligible association with treatment rates. Our findings provide important evidence for constructing evidence-based, targeted intervention policies and measures that aim to improve treatment rates for mental disorders among children and adolescents.
The generally low treatment rates for children and adolescents with mental disorders could be associated with multiple determinants. Despite the consensus on the more hazardous effect of mental disorders on youths, compared with adults, the coverage of mental health services is inadequate.54,58 Fewer approved drug therapies for treating mental disorders among children and adolescents limit possible treatment options.59 Moreover, lack of knowledge about mental health and available help, perceived social stigma and embarrassment, therapeutic relationships with professionals, financial costs associated with mental health services, and logistical concerns were also frequently cited barriers.60 Compared with ADHD and behavior disorders, even lower treatment rates were found for depressive disorders and anxiety disorders, probably because children and adolescents are reluctant to disclose their emotional difficulties to other people for support, owing to fears of negative social consequences.61 Low public acceptance of the use of antidepressants and cognitive behavioral therapy for young people may also hinder their self-rescue behaviors.62 In addition, parents may perceive anxiety or depression in children and adolescents as typical for their age group, and think that it can be improved without professional help.49
Income levels are closely associated with medical investment, which will undoubtedly influence treatment rates of mental disorders to a certain extent, as demonstrated by the pooled estimates of our study. For example, the treatment rate for any mental disorder was 24% in UMICs and 43% in HICs, the treatment rate for depressive disorders was 13% in UMICs and 39% in HICs, and the treatment rate for anxiety disorders was 31% in UMICs and 34% in HICs. Compared with HICs, mental health services are severely underfunded in LMICs: according to the World Health Organization 2020 Mental Health Atlas, government annual mental health expenditure per capita was $52.73 in HICs, compared with $3.29 in UMICs and $0.08 in low-income countries.63 Moreover, for LMICs, there is an overreliance on out-of-pocket payments to support mental health, which further obstructs development of health care systems.64 In addition, the mental health workforce is very underrepresented.63 Therefore, at the governmental level, the utmost priority for LMICs is to increase allocation of mental health expenditures.65 Public education to increase knowledge of mental disorders is also vital to foster mental health service–seeking behaviors.66
This study also found that, even for regions with the same income level, significant differences in treatment rates were observed. A previous study showed marked disparities in the use of child mental health services across developed countries.67 The studies from Europe and the Americas that were included in this meta-analysis were largely from HICs, but we found that the treatment rate for depressive disorders in the Americas was 40%, significantly higher than the 28% in Europe. This discrepancy may be caused by social norms and the stigma associated with psychological disorders, for negative biases against people with mental illnesses have been found to be common in Western European countries68; compared with US adults (23%), a much higher proportion of European adults (41%-45%) reported unwillingness to see a professional when experiencing emotional distress.69 These findings accentuate the necessity of incorporating cultural factors when devising domestic intervention policies for improving treatment rates of mental disorders among children and adolescents in different countries.
Although treatment rates for any mental disorder, ADHD, and behavior disorders were comparable between children and adolescents in this study, age was associated with treatment rates of depressive and anxiety disorders. Specifically, compared with children, adolescents were more than 3 times as likely to be treated for diagnosed depressive disorders (36% vs 11%). The onset of childhood depression can be subtle: children may express irritability and frustration through tantrums and behavioral problems rather than verbally expressing their feelings.70 Meanwhile, compared with adolescents, children with a diagnosis of depressive disorder are less prone to exhibit suicidal behavior,70 which may account for their lower treatment rates. Only 2 original studies regarding childhood depressive disorders satisfied the inclusion criteria of the current meta-analysis, which raises concerns about the representativeness of treatment rates for this age group. The treatment rate of anxiety disorders among adolescents was lower than among children, probably because, compared with adolescents, children with anxiety disorders are more prone to experiencing physical symptoms such as shortness of breath, headaches, stomach pain, and heart palpitations,71 which may prompt parents to seek assistance.
Limitations
This meta-analysis provides a comprehensive and systematic summary of treatment rates for mental disorders in children and adolescents. Nevertheless, some limitations should be noted. First, owing to the limited number of published studies, we were able to combine treatment rates only for several of the most prevalent mental disorders among children and adolescents; other less commonly seen but equally important psychiatric problems in this age group, such as bipolar disorder, borderline personality disorder, and autism spectrum disorder, could not be investigated. Second, as a high level of heterogeneity has been discerned among the included studies, although we performed elaborate subgroup analyses to investigate potential sources of heterogeneity, because we were restricted by the design of the original studies, other meaningful sources could not be analyzed. Third, a small number of the included studies in some subgroups may compromise the representativeness and statistical power of the pooled estimates; therefore, the generalization of the study results should be pursued with caution. Future studies with large and representative samples, focusing on less commonly seen mental disorders, and providing more exhaustive analytical results, are needed, especially from less-developed countries or regions, to better understand the treatment rates of psychiatric problems among young people.
Conclusions
In this systematic review and meta-analysis of high-quality evidence, we found that, in general, treatment rates for mental disorders among children and adolescents are unsatisfactorily low, especially for depression and anxiety. Individual characteristics such as age and environmental factors such as region and income level were associated with treatment rates of mental disorders among this age group. Targeted intervention policies and measures should be designed and implemented to improve treatment rates of psychiatric disorders among youths. Some promising methods have already been highlighted in newly published evidence. For instance, telemedicine was found to be effective in reducing treatment barriers for psychiatric patients, and skills training in mental health assessment and treatment for primary care professionals could also be considered.72
eTable. JBI Quality Scores of Included Studies (N=40)
eFigure 1. Treatment Rates for Any Mental Disorder by Year of Data Collection
eFigure 2. Treatment Rates for Depressive Disorders by Year of Data Collection
eFigure 3. Treatment Rates for Anxiety Disorders by Year of Data Collection
eFigure 4. Treatment Rates for ADHD by Year of Data Collection
eFigure 5. Treatment Rates for Behavior Disorders by Year of Data Collection
eFigure 6. Treatment Rates for Any Mental Disorder by Region
eFigure 7. Treatment Rates for Depressive Disorders by Regions
eFigure 8. Treatment Rates for Anxiety Disorders by Regions
eFigure 9. Treatment Rates for ADHD by Regions
eFigure 10. Treatment Rates for Behavior Disorders by Regions
eFigure 11. Treatment Rates for Any Mental Disorder by Age Groups
eFigure 12. Treatment Rates for Depressive Disorders by Age Groups
eFigure 13. Treatment Rates for Anxiety Disorders by Age Groups
eFigure 14. Treatment Rates for ADHD by Age Groups
eFigure 15. Treatment Rates for Behavior Disorders by Age Groups
eFigure 16. Treatment Rates for Any Mental Disorder by Income Groups
eFigure 17. Treatment Rates for Depressive Disorders by Income Groups
eFigure 18. Treatment Rates for Anxiety Disorders by Income Groups
eFigure 19. Subgroup by Timeframe
eFigure 20. Treatment Rates for Any Mental Disorder by Timeframes
eFigure 21. Treatment Rates for Depressive Disorders by Timeframes
eFigure 22. Treatment Rates for Anxiety Disorders by Timeframes
eFigure 23. Treatment Rates for ADHD by Timeframes
eFigure 24. Treatment Rates for Behavior Disorders by Timeframes
eFigure 25. Subgroup by Informant Source
eFigure 26. Treatment Rates for Any Mental Disorder by Informant Sources
eFigure 27. Treatment Rates for Depressive Disorders by Informant Sources
eFigure 28. Treatment Rates for Anxiety Disorders by Informant Sources
eFigure 29. Treatment Rates for ADHD by Informant Sources
eFigure 30. Treatment Rates for Behavior Disorders by Informant Sources
eFigure 31. Subgroup by Health Service Type
eFigure 32. Treatment Rates for Any Mental Disorder by Health Service Types
eFigure 33. Treatment Rates for Depressive Disorders by Health Service Types
eFigure 34. Treatment Rates for Anxiety Disorders by Health Service Types
eFigure 35. Treatment Rates for ADHD by Health Service Types
eFigure 36. Treatment Rates for Behavior Disorders by Health Service Types
eFigure 37. Subgroup by Sample Origin Population
eFigure 38. Treatment Rates for Any Mental Disorder by the Sample Origin Population
eFigure 39. Treatment Rates for Depressive Disorders by the Sample Origin Population
eFigure 40. Treatment Rates for Anxiety Disorders by the Sample Origin Population
eFigure 41. Treatment Rates for ADHD by the Sample Origin Population
eFigure 42. Treatment Rates for Behavior Disorders by the Sample Origin Population
eFigure 43. Treatment Rates for Internalizing and Externalizing Disorders
eFigure 44. Sensitivity Analysis Forest Plots for Any Mental Disorder
eFigure 45. Sensitivity Analysis Forest Plots for Depressive Disorders
eFigure 46. Sensitivity Analysis Forest Plots for Anxiety Disorders
eFigure 47. Sensitivity Analysis Forest Plots for ADHD
eFigure 48. Sensitivity Analysis Forest Plots for Behavior Disorders
eFigure 49. Sensitivity Analysis by Excluding Studies in Which the 95% CI Was Outside the Aggregated 95% CI of All Studies
eFigure 50. Sensitivity Analysis by Excluding Studies Not Reported Age Ranges
eFigure 51. Funnel Plot (Left) and Trim-and-Fill Funnel Plot (Right)
eFigure 52. Treatment Rates for ADHD
eFigure 53. Treatment Rates for Behavior Disorders
eFigure 54. Subgroup Analysis by Age Group
eFigure 55. Subgroup Analysis by Income Level
eMethods 1. Retrieval Strategy
eMethods 2. Exposure
eResults. Study Selection
eAppendix. Explicit Search Entry
eReferences.
Data Sharing Statement
References
- 1.Piao J, Huang Y, Han C, et al. Alarming changes in the global burden of mental disorders in children and adolescents from 1990 to 2019: a systematic analysis for the Global Burden of Disease study. Eur Child Adolesc Psychiatry. 2022;31(11):1827-1845. doi: 10.1007/s00787-022-02040-4 [DOI] [PubMed] [Google Scholar]
- 2.Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. 2015;56(3):345-365. doi: 10.1111/jcpp.12381 [DOI] [PubMed] [Google Scholar]
- 3.Park JH, Bang YR, Kim CK. Sex and age differences in psychiatric disorders among children and adolescents: high-risk students study. Psychiatry Investig. 2014;11(3):251-257. doi: 10.4306/pi.2014.11.3.251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Green H, McGinnity A, Meltzer H, Ford T, Goodman R. Mental Health of Children and Young People in Great Britain, 2004: A Survey Carried Out by the Office for National Statistics on Behalf of the Department of Health and the Scottish Executive. Palgrave Macmillan; 2005. doi: 10.1037/e557702010-001 [DOI] [Google Scholar]
- 5.Barnes AJ, Eisenberg ME, Resnick MD. Suicide and self-injury among children and youth with chronic health conditions. Pediatrics. 2010;125(5):889-895. doi: 10.1542/peds.2009-1814 [DOI] [PubMed] [Google Scholar]
- 6.Clayborne ZM, Varin M, Colman I. Systematic review and meta-analysis: adolescent depression and long-term psychosocial outcomes. J Am Acad Child Adolesc Psychiatry. 2019;58(1):72-79. doi: 10.1016/j.jaac.2018.07.896 [DOI] [PubMed] [Google Scholar]
- 7.Dunedin Multidisciplinary Health & Development Research Unit . Welcome to the Dunedin Multidisciplinary Health and Development Research Unit (DMHDRU). Accessed April 15, 2023. https://dunedinstudy.otago.ac.nz/
- 8.GOV.UK. Chief Medical Officer annual report 2012: children and young people’s health. Accessed April 15, 2023. https://www.gov.uk/government/publications/chief-medical-officers-annual-report-2012-our-children-deserve-better-prevention-pays
- 9.Dubicka B, Brent D. Editorial: pharmacotherapy and adolescent depression—an important treatment option. Child Adolesc Ment Health. 2017;22(2):59-60. doi: 10.1111/camh.12223 [DOI] [PubMed] [Google Scholar]
- 10.Fabiano GA, Pelham WE Jr. Evidence-based treatment for mental disorders in children and adolescents. Curr Psychiatry Rep. 2002;4(2):93-100. doi: 10.1007/s11920-002-0041-6 [DOI] [PubMed] [Google Scholar]
- 11.Dietz LJ. Family-based interpersonal psychotherapy: an intervention for preadolescent depression. Am J Psychother. 2020;73(1):22-28. doi: 10.1176/appi.psychotherapy.20190028 [DOI] [PubMed] [Google Scholar]
- 12.Lebowitz ER, Marin C, Martino A, Shimshoni Y, Silverman WK. Parent-based treatment as efficacious as cognitive-behavioral therapy for childhood anxiety: a randomized noninferiority study of supportive parenting for anxious childhood emotions. J Am Acad Child Adolesc Psychiatry. 2020;59(3):362-372. doi: 10.1016/j.jaac.2019.02.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry. 2010;10:113. doi: 10.1186/1471-244X-10-113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Merikangas KR, He JP, Brody D, Fisher PW, Bourdon K, Koretz DS. Prevalence and treatment of mental disorders among US children in the 2001-2004 NHANES. Pediatrics. 2010;125(1):75-81. doi: 10.1542/peds.2008-2598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zwaanswijk M, van der Ende J, Verhaak PF, Bensing JM, Verhulst FC. Help-seeking for child psychopathology: pathways to informal and professional services in the Netherlands. J Am Acad Child Adolesc Psychiatry. 2005;44(12):1292-1300. doi: 10.1097/01.chi.0000181038.98712.c6 [DOI] [PubMed] [Google Scholar]
- 16.Fatori D, Salum GA, Rohde LA, et al. Use of mental health services by children with mental disorders in two major cities in Brazil. Psychiatr Serv. 2019;70(4):337-341. doi: 10.1176/appi.ps.201800389 [DOI] [PubMed] [Google Scholar]
- 17.Borges G, Benjet C, Medina-Mora M, Orozco R, Wang P. Treatment of mental disorders for adolescents in Mexico City. Bull World Health Organ. 2008;86(10):757-764. doi: 10.2471/BLT.07.047696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhong BL, Ding J, Chen HH, et al. Depressive disorders among children in the transforming China: an epidemiological survey of prevalence, correlates, and service use. Depress Anxiety. 2013;30(9):881-892. doi: 10.1002/da.22109 [DOI] [PubMed] [Google Scholar]
- 19.Wu P, Hoven CW, Cohen P, et al. Factors associated with use of mental health services for depression by children and adolescents. Psychiatr Serv. 2001;52(2):189-195. doi: 10.1176/appi.ps.52.2.189 [DOI] [PubMed] [Google Scholar]
- 20.JBI . Critical appraisal tools. Accessed November 20, 2022. https://jbi.global/critical-appraisal-tools
- 21.Cénat JM, Blais-Rochette C, Morse C, et al. Prevalence and risk factors associated with attention-deficit/hyperactivity disorder among US Black individuals: a systematic review and meta-analysis. JAMA Psychiatry. 2021;78(1):21-28. doi: 10.1001/jamapsychiatry.2020.2788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods. 2006;11(2):193-206. doi: 10.1037/1082-989X.11.2.193 [DOI] [PubMed] [Google Scholar]
- 23.Mavridis D, Salanti G. Exploring and accounting for publication bias in mental health: a brief overview of methods. Evid Based Ment Health. 2014;17(1):11-15. doi: 10.1136/eb-2013-101700 [DOI] [PubMed] [Google Scholar]
- 24.Angold A, Erkanli A, Farmer EM, et al. Psychiatric disorder, impairment, and service use in rural African American and white youth. Arch Gen Psychiatry. 2002;59(10):893-901. doi: 10.1001/archpsyc.59.10.893 [DOI] [PubMed] [Google Scholar]
- 25.Bird HR, Shrout PE, Duarte CS, Shen S, Bauermeister JJ, Canino G. Longitudinal mental health service and medication use for ADHD among Puerto Rican youth in two contexts. J Am Acad Child Adolesc Psychiatry. 2008;47(8):879-889. doi: 10.1097/CHI.0b013e318179963c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Buckner JC, Bassuk EL. Mental disorders and service utilization among youths from homeless and low-income housed families. J Am Acad Child Adolesc Psychiatry. 1997;36(7):890-900. doi: 10.1097/00004583-199707000-00010 [DOI] [PubMed] [Google Scholar]
- 27.Bussing R, Zima BT, Gary FA, Garvan CW. Barriers to detection, help-seeking, and service use for children with ADHD symptoms. J Behav Health Serv Res. 2003;30(2):176-189. doi: 10.1007/BF02289806 [DOI] [PubMed] [Google Scholar]
- 28.Bussing R, Zima BT, Mason DM, Porter PC, Garvan CW. Receiving treatment for attention-deficit hyperactivity disorder: do the perspectives of adolescents matter? J Adolesc Health. 2011;49(1):7-14. doi: 10.1016/j.jadohealth.2010.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Canino G, Shrout PE, Rubio-Stipec M, et al. The DSM-IV rates of child and adolescent disorders in Puerto Rico: prevalence, correlates, service use, and the effects of impairment. Arch Gen Psychiatry. 2004;61(1):85-93. doi: 10.1001/archpsyc.61.1.85 [DOI] [PubMed] [Google Scholar]
- 30.Chavira DA, Stein MB, Bailey K, Stein MT. Child anxiety in primary care: prevalent but untreated. Depress Anxiety. 2004;20(4):155-164. doi: 10.1002/da.20039 [DOI] [PubMed] [Google Scholar]
- 31.Coker TR, Elliott MN, Kataoka S, et al. Racial/ethnic disparities in the mental health care utilization of fifth grade children. Acad Pediatr. 2009;9(2):89-96. doi: 10.1016/j.acap.2008.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cuffe SP, Waller JL, Addy CL, et al. A longitudinal study of adolescent mental health service use. J Behav Health Serv Res. 2001;28(1):1-11. doi: 10.1007/BF02287230 [DOI] [PubMed] [Google Scholar]
- 33.Cummings JR, Druss BG. Racial/ethnic differences in mental health service use among adolescents with major depression. J Am Acad Child Adolesc Psychiatry. 2011;50(2):160-170. doi: 10.1016/j.jaac.2010.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Daeem R, Mansbach-Kleinfeld I, Farbstein I, et al. Barriers to help-seeking in Israeli Arab minority adolescents with mental health problems: results from the Galilee Study. Isr J Health Policy Res. 2019;8(1):45. doi: 10.1186/s13584-019-0315-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Essau CA. Frequency and patterns of mental health services utilization among adolescents with anxiety and depressive disorders. Depress Anxiety. 2005;22(3):130-137. doi: 10.1002/da.20115 [DOI] [PubMed] [Google Scholar]
- 36.Flament MF, Cohen D, Choquet M, Jeammet P, Ledoux S. Phenomenology, psychosocial correlates, and treatment seeking in major depression and dysthymia of adolescence. J Am Acad Child Adolesc Psychiatry. 2001;40(9):1070-1078. doi: 10.1097/00004583-200109000-00016 [DOI] [PubMed] [Google Scholar]
- 37.Georgiades K, Duncan L, Wang L, Comeau J, Boyle MH; 2014 Ontario Child Health Study Team . Six-month prevalence of mental disorders and service contacts among children and youth in Ontario: evidence from the 2014 Ontario Child Health Study. Can J Psychiatry. 2019;64(4):246-255. doi: 10.1177/0706743719830024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gómez-Beneyto M, Bonet A, Catalá MA, Puche E, Vila V. Prevalence of mental disorders among children in Valencia, Spain. Acta Psychiatr Scand. 1994;89(5):352-357. doi: 10.1111/j.1600-0447.1994.tb01528.x [DOI] [PubMed] [Google Scholar]
- 39.Gould MS, Marrocco FA, Hoagwood K, Kleinman M, Amakawa L, Altschuler E. Service use by at-risk youths after school-based suicide screening. J Am Acad Child Adolesc Psychiatry. 2009;48(12):1193-1201. doi: 10.1097/CHI.0b013e3181bef6d5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Heiervang E, Stormark KM, Lundervold AJ, et al. Psychiatric disorders in Norwegian 8- to 10-year-olds: an epidemiological survey of prevalence, risk factors, and service use. J Am Acad Child Adolesc Psychiatry. 2007;46(4):438-447. doi: 10.1097/chi.0b013e31803062bf [DOI] [PubMed] [Google Scholar]
- 41.Leaf PJ, Alegria M, Cohen P, et al. Mental health service use in the community and schools: results from the four-community MECA Study: Methods for the Epidemiology of Child and Adolescent Mental Disorders Study. J Am Acad Child Adolesc Psychiatry. 1996;35(7):889-897. doi: 10.1097/00004583-199607000-00014 [DOI] [PubMed] [Google Scholar]
- 42.Lewinsohn PM, Rohde P, Seeley JR. Treatment of adolescent depression: frequency of services and impact on functioning in young adulthood. Depress Anxiety. 1998;7(1):47-52. doi: [DOI] [PubMed] [Google Scholar]
- 43.Locke J, Kang-Yi CD, Pellecchia M, Marcus S, Hadley T, Mandell DS. Ethnic disparities in school-based behavioral health service use for children with psychiatric disorders. J Sch Health. 2017;87(1):47-54. doi: 10.1111/josh.12469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Maalouf FT, Ghandour LA, Halabi F, Zeinoun P, Shehab AA, Tavitian L. Psychiatric disorders among adolescents from Lebanon: prevalence, correlates, and treatment gap. Soc Psychiatry Psychiatr Epidemiol. 2016;51(8):1105-1116. doi: 10.1007/s00127-016-1241-4 [DOI] [PubMed] [Google Scholar]
- 45.Magklara K, Bellos S, Niakas D, et al. Depression in late adolescence: a cross-sectional study in senior high schools in Greece. BMC Psychiatry. 2015;15:199. doi: 10.1186/s12888-015-0584-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Meredith LS, Stein BD, Paddock SM, et al. Perceived barriers to treatment for adolescent depression. Med Care. 2009;47(6):677-685. doi: 10.1097/MLR.0b013e318190d46b [DOI] [PubMed] [Google Scholar]
- 47.Merikangas KR, He JP, Burstein M, et al. Service utilization for lifetime mental disorders in U.S. adolescents: results of the National Comorbidity Survey–Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 2011;50(1):32-45. doi: 10.1016/j.jaac.2010.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Niermann HCM, Voss C, Pieper L, Venz J, Ollmann TM, Beesdo-Baum K. Anxiety disorders among adolescents and young adults: prevalence and mental health care service utilization in a regional epidemiological study in Germany. J Anxiety Disord. 2021;83:102453. doi: 10.1016/j.janxdis.2021.102453 [DOI] [PubMed] [Google Scholar]
- 49.Reardon T, Harvey K, Creswell C. Seeking and accessing professional support for child anxiety in a community sample. Eur Child Adolesc Psychiatry. 2020;29(5):649-664. doi: 10.1007/s00787-019-01388-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sawyer MG, Rey JM, Arney FM, Whitham JN, Clark JJ, Baghurst PA. Use of health and school-based services in Australia by young people with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2004;43(11):1355-1363. doi: 10.1097/01.chi.0000138354.90981.5b [DOI] [PubMed] [Google Scholar]
- 51.Sawyer MG, Reece CE, Sawyer AC, Johnson SE, Hiscock H, Lawrence D. Access to health professionals by children and adolescents with mental disorders: are we meeting their needs? Aust N Z J Psychiatry. 2018;52(10):972-982. doi: 10.1177/0004867418760713 [DOI] [PubMed] [Google Scholar]
- 52.Stiffman AR, Earls F, Robins LN, Jung KG. Problems and help seeking in high-risk adolescent patients of health clinics. J Adolesc Health Care. 1988;9(4):305-309. doi: 10.1016/0197-0070(88)90255-0 [DOI] [PubMed] [Google Scholar]
- 53.Tanielian T, Jaycox LH, Paddock SM, Chandra A, Meredith LS, Burnam MA. Improving treatment seeking among adolescents with depression: understanding readiness for treatment. J Adolesc Health. 2009;45(5):490-498. doi: 10.1016/j.jadohealth.2009.03.005 [DOI] [PubMed] [Google Scholar]
- 54.Vicente B, Saldivia S, de la Barra F, et al. Prevalence of child and adolescent mental disorders in Chile: a community epidemiological study. J Child Psychol Psychiatry. 2012;53(10):1026-1035. doi: 10.1111/j.1469-7610.2012.02566.x [DOI] [PubMed] [Google Scholar]
- 55.Wagner G, Zeiler M, Waldherr K, et al. Mental health problems in Austrian adolescents: a nationwide, two-stage epidemiological study applying DSM-5 criteria. Eur Child Adolesc Psychiatry. 2017;26(12):1483-1499. doi: 10.1007/s00787-017-0999-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wu P, Hoven CW, Bird HR, et al. Depressive and disruptive disorders and mental health service utilization in children and adolescents. J Am Acad Child Adolesc Psychiatry. 1999;38(9):1081-1090. doi: 10.1097/00004583-199909000-00010 [DOI] [PubMed] [Google Scholar]
- 57.Zhang S, Cain DS, Liao M. Racial/ethnic disparities in the decision points of mental health service use and psychotropic medication receipt among depressed youth. Youth Soc. 2021;53(4):610-635. doi: 10.1177/0044118X19871853 [DOI] [Google Scholar]
- 58.Rocha TB, Graeff-Martins AS, Kieling C, Rohde LA. Provision of mental healthcare for children and adolescents: a worldwide view. Curr Opin Psychiatry. 2015;28(4):330-335. doi: 10.1097/YCO.0000000000000169 [DOI] [PubMed] [Google Scholar]
- 59.Cardwell GS, Findling RL, Robb AS. Psychiatric diseases in children and adolescents. Handb Exp Pharmacol. 2020;261:397-413. doi: 10.1007/164_2019_262 [DOI] [PubMed] [Google Scholar]
- 60.Radez J, Reardon T, Creswell C, Lawrence PJ, Evdoka-Burton G, Waite P. Why do children and adolescents (not) seek and access professional help for their mental health problems? a systematic review of quantitative and qualitative studies. Eur Child Adolesc Psychiatry. 2021;30(2):183-211. doi: 10.1007/s00787-019-01469-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Stapinski LA, Araya R, Heron J, Montgomery AA, Stallard P. Peer victimization during adolescence: concurrent and prospective impact on symptoms of depression and anxiety. Anxiety Stress Coping. 2015;28(1):105-120. doi: 10.1080/10615806.2014.962023 [DOI] [PubMed] [Google Scholar]
- 62.Jorm AF, Morgan AJ, Wright A. Interventions that are helpful for depression and anxiety in young people: a comparison of clinicians’ beliefs with those of youth and their parents. J Affect Disord. 2008;111(2-3):227-234. doi: 10.1016/j.jad.2008.02.021 [DOI] [PubMed] [Google Scholar]
- 63.World Health Organization. Mental Health Atlas 2020. Accessed May 12, 2023. https://apps.who.int/iris/handle/10665/345946
- 64.Belfer ML, Saxena S. WHO Child Atlas project. Lancet. 2006;367(9510):551-552. doi: 10.1016/S0140-6736(06)68199-3 [DOI] [PubMed] [Google Scholar]
- 65.Kieling C, Baker-Henningham H, Belfer M, et al. Child and adolescent mental health worldwide: evidence for action. Lancet. 2011;378(9801):1515-1525. doi: 10.1016/S0140-6736(11)60827-1 [DOI] [PubMed] [Google Scholar]
- 66.Richmond JB, Kotelchuck M. Political Influences: Rethinking National Health Policy: Handbook of Health Professions Education. Jossey-Bass; 1983:384-404. [Google Scholar]
- 67.Delamare C, Ibeziako P. A comparison of child mental health systems in France and the United States. Adolesc Psychiatry. 2013;3(1):5-10. doi: 10.2174/2210676611303010002 [DOI] [Google Scholar]
- 68.Mascayano F, Tapia T, Schilling S, et al. Stigma toward mental illness in Latin America and the Caribbean: a systematic review. Braz J Psychiatry. 2016;38(1):73-85. doi: 10.1590/1516-4446-2015-1652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tikkanen R, Fields K, Williams RD, Abrams MK. Mental health conditions and substance use: comparing US needs and treatment capacity with those in other high-income countries. Commonwealth Fund. 2020. Accessed May 22, 2023. https://www.commonwealthfund.org/publications/issue-briefs/2020/may/mental-health-conditions-substance-use-comparing-us-other-countries
- 70.Birmaher B, Brent D, Bernet W, et al. ; AACAP Work Group on Quality Issues . Practice parameter for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry. 2007;46(11):1503-1526. doi: 10.1097/chi.0b013e318145ae1c [DOI] [PubMed] [Google Scholar]
- 71.Connolly SD, Bernstein GA; Work Group on Quality Issues . Practice parameter for the assessment and treatment of children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry. 2007;46(2):267-283. doi: 10.1097/01.chi.0000246070.23695.06 [DOI] [PubMed] [Google Scholar]
- 72.Benton TD, Boyd RC, Njoroge WFM. Addressing the global crisis of child and adolescent mental health. JAMA Pediatr. 2021;175(11):1108-1110. doi: 10.1001/jamapediatrics.2021.2479 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. JBI Quality Scores of Included Studies (N=40)
eFigure 1. Treatment Rates for Any Mental Disorder by Year of Data Collection
eFigure 2. Treatment Rates for Depressive Disorders by Year of Data Collection
eFigure 3. Treatment Rates for Anxiety Disorders by Year of Data Collection
eFigure 4. Treatment Rates for ADHD by Year of Data Collection
eFigure 5. Treatment Rates for Behavior Disorders by Year of Data Collection
eFigure 6. Treatment Rates for Any Mental Disorder by Region
eFigure 7. Treatment Rates for Depressive Disorders by Regions
eFigure 8. Treatment Rates for Anxiety Disorders by Regions
eFigure 9. Treatment Rates for ADHD by Regions
eFigure 10. Treatment Rates for Behavior Disorders by Regions
eFigure 11. Treatment Rates for Any Mental Disorder by Age Groups
eFigure 12. Treatment Rates for Depressive Disorders by Age Groups
eFigure 13. Treatment Rates for Anxiety Disorders by Age Groups
eFigure 14. Treatment Rates for ADHD by Age Groups
eFigure 15. Treatment Rates for Behavior Disorders by Age Groups
eFigure 16. Treatment Rates for Any Mental Disorder by Income Groups
eFigure 17. Treatment Rates for Depressive Disorders by Income Groups
eFigure 18. Treatment Rates for Anxiety Disorders by Income Groups
eFigure 19. Subgroup by Timeframe
eFigure 20. Treatment Rates for Any Mental Disorder by Timeframes
eFigure 21. Treatment Rates for Depressive Disorders by Timeframes
eFigure 22. Treatment Rates for Anxiety Disorders by Timeframes
eFigure 23. Treatment Rates for ADHD by Timeframes
eFigure 24. Treatment Rates for Behavior Disorders by Timeframes
eFigure 25. Subgroup by Informant Source
eFigure 26. Treatment Rates for Any Mental Disorder by Informant Sources
eFigure 27. Treatment Rates for Depressive Disorders by Informant Sources
eFigure 28. Treatment Rates for Anxiety Disorders by Informant Sources
eFigure 29. Treatment Rates for ADHD by Informant Sources
eFigure 30. Treatment Rates for Behavior Disorders by Informant Sources
eFigure 31. Subgroup by Health Service Type
eFigure 32. Treatment Rates for Any Mental Disorder by Health Service Types
eFigure 33. Treatment Rates for Depressive Disorders by Health Service Types
eFigure 34. Treatment Rates for Anxiety Disorders by Health Service Types
eFigure 35. Treatment Rates for ADHD by Health Service Types
eFigure 36. Treatment Rates for Behavior Disorders by Health Service Types
eFigure 37. Subgroup by Sample Origin Population
eFigure 38. Treatment Rates for Any Mental Disorder by the Sample Origin Population
eFigure 39. Treatment Rates for Depressive Disorders by the Sample Origin Population
eFigure 40. Treatment Rates for Anxiety Disorders by the Sample Origin Population
eFigure 41. Treatment Rates for ADHD by the Sample Origin Population
eFigure 42. Treatment Rates for Behavior Disorders by the Sample Origin Population
eFigure 43. Treatment Rates for Internalizing and Externalizing Disorders
eFigure 44. Sensitivity Analysis Forest Plots for Any Mental Disorder
eFigure 45. Sensitivity Analysis Forest Plots for Depressive Disorders
eFigure 46. Sensitivity Analysis Forest Plots for Anxiety Disorders
eFigure 47. Sensitivity Analysis Forest Plots for ADHD
eFigure 48. Sensitivity Analysis Forest Plots for Behavior Disorders
eFigure 49. Sensitivity Analysis by Excluding Studies in Which the 95% CI Was Outside the Aggregated 95% CI of All Studies
eFigure 50. Sensitivity Analysis by Excluding Studies Not Reported Age Ranges
eFigure 51. Funnel Plot (Left) and Trim-and-Fill Funnel Plot (Right)
eFigure 52. Treatment Rates for ADHD
eFigure 53. Treatment Rates for Behavior Disorders
eFigure 54. Subgroup Analysis by Age Group
eFigure 55. Subgroup Analysis by Income Level
eMethods 1. Retrieval Strategy
eMethods 2. Exposure
eResults. Study Selection
eAppendix. Explicit Search Entry
eReferences.
Data Sharing Statement