This cross-sectional study evaluates a relatively simple, noninvasive measurement method for exophthalmos using a smartphone.
Key Points
Question
What is the performance of a smartphone measurement of exophthalmos?
Findings
In this cross-sectional study of 23 patients and 16 healthy volunteers, smartphone measurements appeared accurate and precise compared with Hertel exophthalmometry or a high-resolution scanner.
Meaning
These data support the use of a smartphone in place of a Hertel exophthalmometer for measuring exophthalmos in the future.
Abstract
Importance
The current clinical criterion standard for measuring abnormal eyeball protrusion is still the historic Hertel exophthalmometer, which is prone to reading errors. Therefore, a smartphone application has been developed to measure exophthalmos.
Objective
To evaluate a relatively simple noninvasive measurement method for exophthalmos using a smartphone.
Design, Setting, and Participants
This cross-sectional study compared smartphone exophthalmometry with the existing reference standard, the Hertel exophthalmometer, or a professional high-resolution 3-dimensional scanner. Participants were patients with exophthalmos due to Graves orbitopathy and other intraorbital conditions and healthy volunteers who were recruited between June 2019 and January 2022 from the Department of Ophthalmology, University Hospital Zurich.
Interventions
All participants were examined twice by 3 different operators using 3 different methods (smartphone, high-resolution scanner, or Hertel exophthalmometer) at an interval of a minimum of 2 weeks or after exophthalmos-changing treatment.
Main Outcome Measures
Accuracy and precision, test-retest reliability, and interoperator reliability of eyeball protrusion measurements obtained with the smartphone compared to the Hertel exophthalmometer and the high-resolution face scanner.
Results
Of 39 participants, 23 patients (median [IQR] age, 54 [44-59] years; 15 [65%] female and 8 [35%] male) showed a mean difference in eyeball protrusion of 3.3 mm and 16 healthy volunteers (median [IQR] age, 32 [30-37] years; 11 [69%] female and 5 [31%] male) of 0.8 mm without any significant difference between the 3 methods. Accuracy and precision agreement between exophthalmos measures with the smartphone and the Hertel exophthalmometer showed an intraclass correlation coefficient (ICC) of 0.89 (95% CI, 0.80-0.94) and 0.93 (95% CI, 0.83-0.97) for the high-resolution scanner. Interoperator agreement was highest for the high-resolution scanner (ICC, 0.99 [95% CI, 0.98-0.99]), followed by the smartphone (ICC, 0.95 [95% CI, 0.92-0.97]) and the Hertel exophthalmometer (ICC, 0.91 [95% CI, 0.85-0.95]). Test retest reliability was similarly high for the smartphone (ICC, 0.93 [95% CI, 0.82-0.95]), the Hertel exophthalmometer (ICC, 0.92 [95% CI, 0.83-0.96]), and the high-resolution scanner (ICC, 0.95 [95% CI, 0.89-0.97]).
Conclusions and Relevance
The findings of this study demonstrate relatively high accuracy and precision, interoperator reliability, and test-retest reliability for smartphone exophthalmometry. These data support the use of a smartphone in place of a Hertel exophthalmometer for measuring exophthalmos in the future.
Introduction
Measurements of exophthalmos are essential for diagnosis and follow-up of patients with Graves disease and other intraorbital conditions that may lead to the protrusion of the eyeball. Graves orbitopathy (thyroid eye disease) is the most common cause of exophthalmos in adults, affecting female individuals more than male individuals. It is an inflammatory condition of the orbit and the surrounding tissue due to an autoimmune process. In addition to inflammatory conditions, the different etiologies of exophthalmos can be grouped under intraorbital and extraorbital tumors (eg, nerve sheath meningioma), vascular etiologies, and infectious conditions.1
A method for measuring exophthalmos should be easy to perform for both the patient and the examiner, repeatable under the same conditions, and the results of successive examinations should be comparable to each other objectively. The current criterion standard for measuring exophthalmos is the Hertel exophthalmometer, which was invented more than 100 years ago.2 It uses prism mirrors to determine the distance of the lateral orbital rim to the front of the cornea. From today’s point of view, it is rather inconvenient to use, prone to reading errors, and the proper use depends on the examiner’s experience.3
Recent developments in 3-dimensional (3-D) scanning methods have made building 3-D object models readily available. The Artec Space Spider is a 3-D scanner based on blue light technology (Artec3D). It is suitable for capturing small objects or intricate details of large objects because of the high resolution and high accuracy. The scanner has already been applied in the field of medicine, especially for obtaining 3-D models for orthopedic, prosthetic, and plastic surgery.4,5,6,7
The smartphone used in our study (iPhone 11; Apple Inc) includes a special camera that captures accurate face data by projecting and analyzing over 30 000 infrared light dots to create a depth map of the face (TrueDepth; Apple Inc). The infrared image is transformed into a mathematical representation of the face using the neural engine of the smartphone and can be obtained and exported as a geometry definition file (OBJ) for further analysis.
The aim of our study was to assess the accuracy and precision, interoperator reliability, and test-retest reliability of the 3-D scanning methods in comparison to the Hertel exophthalmometer. Our goal was to develop and validate an easy-to-use smartphone application to measure exophthalmos using the 3-D scanning feature of a smartphone.
Methods
Ethics
The study was approved by the ethics committee of the canton Zurich (2019-00233) and by Swissmedic (10000520), and written informed consent was obtained from all participants. The study device was registered in the European database of medical devices (EUDAMED CIV-19-08-029404). A patent was issued for the invention.8 Participants did not receive any compensation or other incentive. The results were reported as recommended by the Standards for Reporting of Diagnostic Accuracy (STARD) reporting guideline.9
Participants
Participants were recruited between June 2019 and January 2022 from the neuro-ophthalmology outpatient clinic at University Hospital Zurich. Adult patients with exophthalmos and healthy volunteers were included. Excluded were patients unable to cooperate with the exophthalmos measurements. One patient was lost to follow-up and therefore excluded. Morphological ethnicity was determined from the 3-D scans of the faces and consisted of Asian and White individuals. Because of the distribution and the relatively small sample size, no findings about race and ethnicity could be made.
Examination Procedure
All participants underwent standard exophthalmos measurements with a Hertel exophthalmometer (Oculus). Additionally, the face was scanned with a smartphone and a high-resolution 3-D scanner. Exophthalmos measurements were done by 3 different examiners (T.P., F.C.F., and K.P.W.) and repeated after 2 weeks or after an exophthalmos changing procedure (eFigure 1 in Supplement 1). To ensure reproducibility, all tests were performed by the same examiners and done under the same light conditions.
Smartphone Face Scanning
Face scanning was performed with a smartphone (iPhone 11; Apple Inc). The TrueDepth camera of the smartphone and a scanning application from the App store (Bellus3D FaceApp) were used to obtain 3-D models of the face. The smartphone was positioned on a tripod at eye level, and the distance was adjusted according to the application feedback. Patients were instructed to keep their eyelids wide open and to follow the voice commands of the smartphone application to turn the head to the left, to the middle, to the right, and back to the middle. The 3-D scan was exported in a geometry definition file (OBJ) and processed with self-developed MATLAB software version 2019b (MathWorks) to determine the exophthalmos in millimeters.
Hertel Exophthalmometry
Participants were seated opposite to the examiner at eye level. The legs of the exophthalmometer were positioned at the lateral orbital rims. The distance between the legs of the exophthalmometer was noted for each examiner and used again during follow-up measurements. Then the participant was asked to look straight ahead with eyelids wide open. The examiner looked through each prism mirror separately and moved their head horizontally until the red line was aligned to the gap in the ruler. The protrusion on the pupillary and corneal level was read in millimeters from the ruler.
Face Scanning With the High-Resolution 3-D Scanner
Face scanning was performed with an Artec Space Spider scanner (Artec3D). The examiner held the scanner at the appropriate distance and turned around the participant’s face from ear to ear. The participant was asked to look straight ahead without blinking and eyelids wide open. Two of the examiners (T.P. and F.C.F.) processed the raw scans by creating a watertight model, deleting unnecessary data points, and applying the texture of the face back onto the watertight model. The 3-D face model was then saved as an OBJ file. To determine the eyeball protrusion from the OBJ file, we used the same self-developed MATLAB software as for the smartphone.
Determining Exophthalmos From the 3-D Face Models
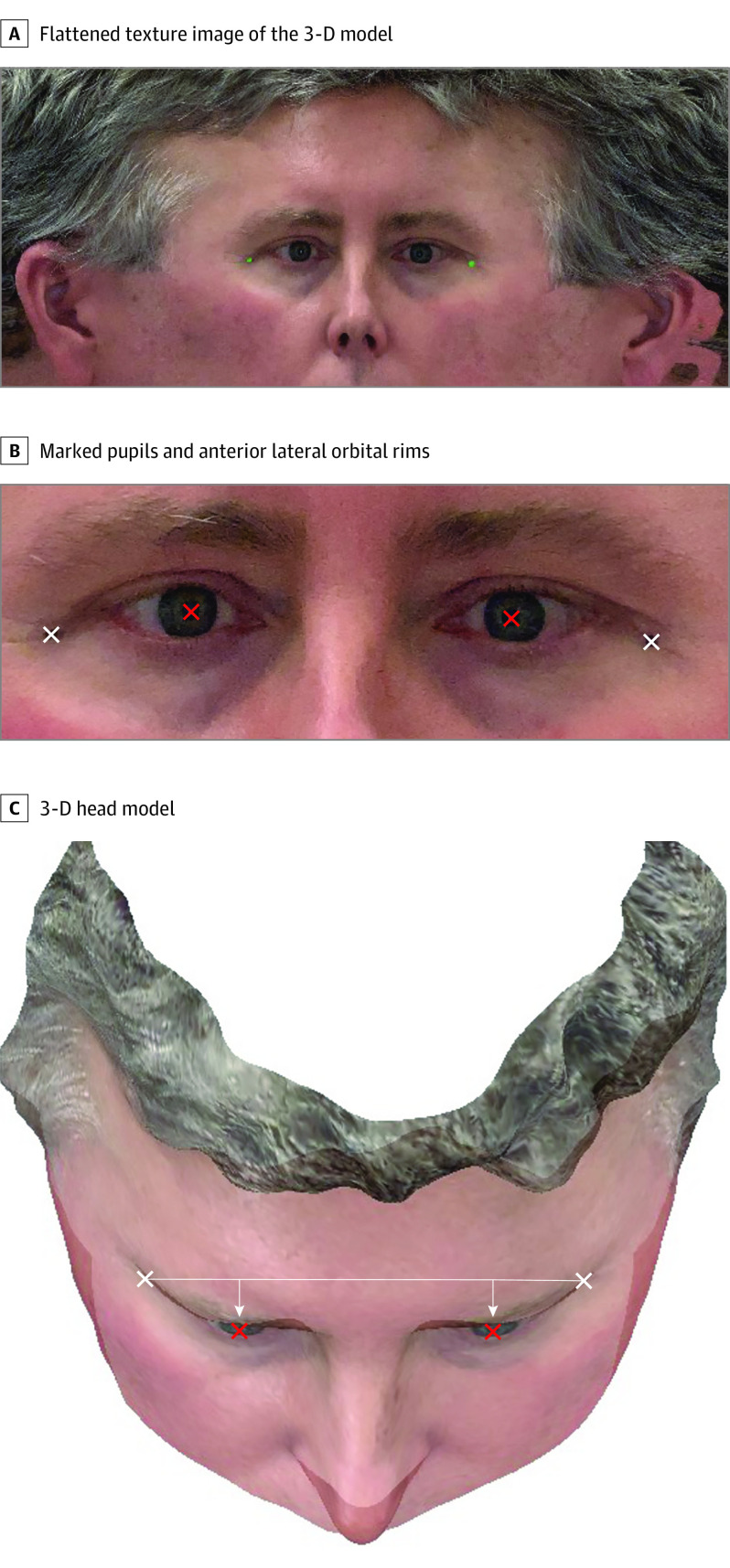
MATLAB software was used to analyze the OBJ files. The OBJ files contain the 3-D measurements of the participant’s head, which represents the face as a collection of polygon faces and an associated texture map with an image of the head (Figure 1). Texture data were used to detect the location of the pupils and the anterior lateral orbital rims. The rims were marked with a pen making them recognizable on the 3-D face model. Figure 1B shows a close-up with the marked locations. To measure eyeball protrusion, a line was drawn between the orbital rims, and the shortest distance of each pupil to this line was determined (Figure 1C).
Figure 1. Method for Determining the Eyeball Protrusion Using 3-Dimensional (3-D) Scanners.
A, Flattened texture image of the 3-D model. B, The location of the pupils (red) and anterior lateral orbital rims (white) are marked. C, The 3-D head model, seen from above. Lines are drawn connecting the anterior lateral orbital rims (long horizontal line) and perpendicular lines from the pupils to this line (shorter vertical lines) are shown.
a = LAOR – RAOR
b = PUP – RAOR
 |
where × is the cross product. LAOR indicates left anterior orbital rim position; RAOR, right anterior orbital rim position; and PUP, pupil position. This was for each marked pupil.
Statistical Analysis
Data analysis was done with R version 4.2.0 (R Foundation). The primary measure was the difference in eyeball protrusion. We first compared the methods with repeated measures analysis of variance with method (Hertel exophthalmometer, scanner, and smartphone), participant type (healthy volunteer, patient), and examiner as factors. To compare the 3 testing methods, we computed intraclass correlation coefficients (ICCs) to assess accuracy and precision on each examiner separately and reported the mean ICCs and 95% CIs. Thus, for each examiner, we calculated 3 ICCs (Hertel exophthalmometer vs smartphone, Hertel exophthalmometer vs scanner, and smartphone vs Hertel exophthalmometer). Test-retest reliability was computed with ICCs separately for each examiner and test and reported as a mean. To measure interoperator reliability, we computed ICCs for each test with all 3 examiners. Comparisons between ICCs were made with permutation tests with 5000 samples,10,11 with P values adjusted for multiple comparisons using Holm method.12 Two-sided P values were statistically significant at .05.
Results
Of 39 participants, 23 patients (median [IQR] age, 54 [44-59] years; 15 [65%] female and 8 [35%] male) showed a mean difference in eyeball protrusion of 3.3 mm and 16 healthy volunteers (median [IQR] age, 32 [30-37] years; 11 [69%] female and 5 [31%] male) of 0.8 mm without any significant difference between the 3 methods. Participants were aged 27 to 85 years (median [IQR] age, 44 [32-58] years). Seven patients had Graves disease, 10 had orbital tumors (sphenoid wing meningioma [n = 4], intraorbital meningioma [n = 5], lymphoma [n = 1]), 3 had cavernous hemangioma, and 2 had severe myopia. One patient had a microphthalmos and a relative exophthalmos of the other eye. Nine patients received treatment, and exophthalmos measurements were performed pretreatment and posttreatment.
Exophthalmos Measurements
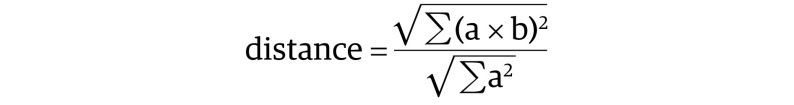
All participants were measured by 3 different examiners using all 3 methods, and the measurements were repeated after a minimum of 2 weeks or after an exophthalmos changing procedure. The Video illustrates the exophthalmos measurement procedure on a healthy participant using the 3-D front camera of a smartphone. Figure 2 illustrates an example of a patient with bilateral exophthalmos due to orbital B-cell lymphoma pretreatment and posttreatment.
Figure 2. Smartphone Exophthalmos Measurement in a Patient With Bilateral Exophthalmos Due to Orbital B-Cell Lymphoma Before and After Treatment.
A, A line connecting the anterior lateral orbital rims (long horizontal line) and perpendicular lines from the pupils to this line (shorter vertical lines) are shown. B, The distance between the lateral orbital rim and the pupil, representing the protrusion of the left and right eye, are illustrated in red. C, Posttreatment image illustrating marked reduction of the exophthalmos.
Video. Smartphone Exophthalmometer.
Visualization of the setup and functionality of exophthalmos measurements with a smartphone scanner. On the left side of the video, the setup is shown, and on the right side, the smartphone app. As the test person follows the commands of the app, a 3-dimensional model of the head is created. At the end, results of the measurement are displayed in the app.
The mean (SD) difference of eyeball protrusion was about 3.3 (0.57) mm in patients and about 0.8 (0.17) mm in healthy participants (eFigure 2 in Supplement 1). No significant difference between the 3 methods and examiners was noted (Hertel exophthalmometer vs scanner: 0.65 [95% CI, −0.2 to 1.5] mm; Hertel exophthalmometer vs smartphone: 0.12 [95% CI, −0.69 to 0.94] mm; scanner vs smartphone: −0.52 [95% CI, −1.33 to 0.28] mm). Repeated-measures analysis of variance with participant type, test method, and examiner as factors found a significant main association of participant type (F1,37 = 15.6; P < .001) with outcomes, and the main association of method was marginally significant (F2,296 = 2.7; P = .07). The interaction of participant type and method was also significant (F2,296 = 5.6; P < .001), apparently because the patient measurements for the Hertel exophthalmometer were slightly higher than the other methods, while the Hertel exophthalmometer measurements for healthy participants were slightly lower. No other differences were identified.
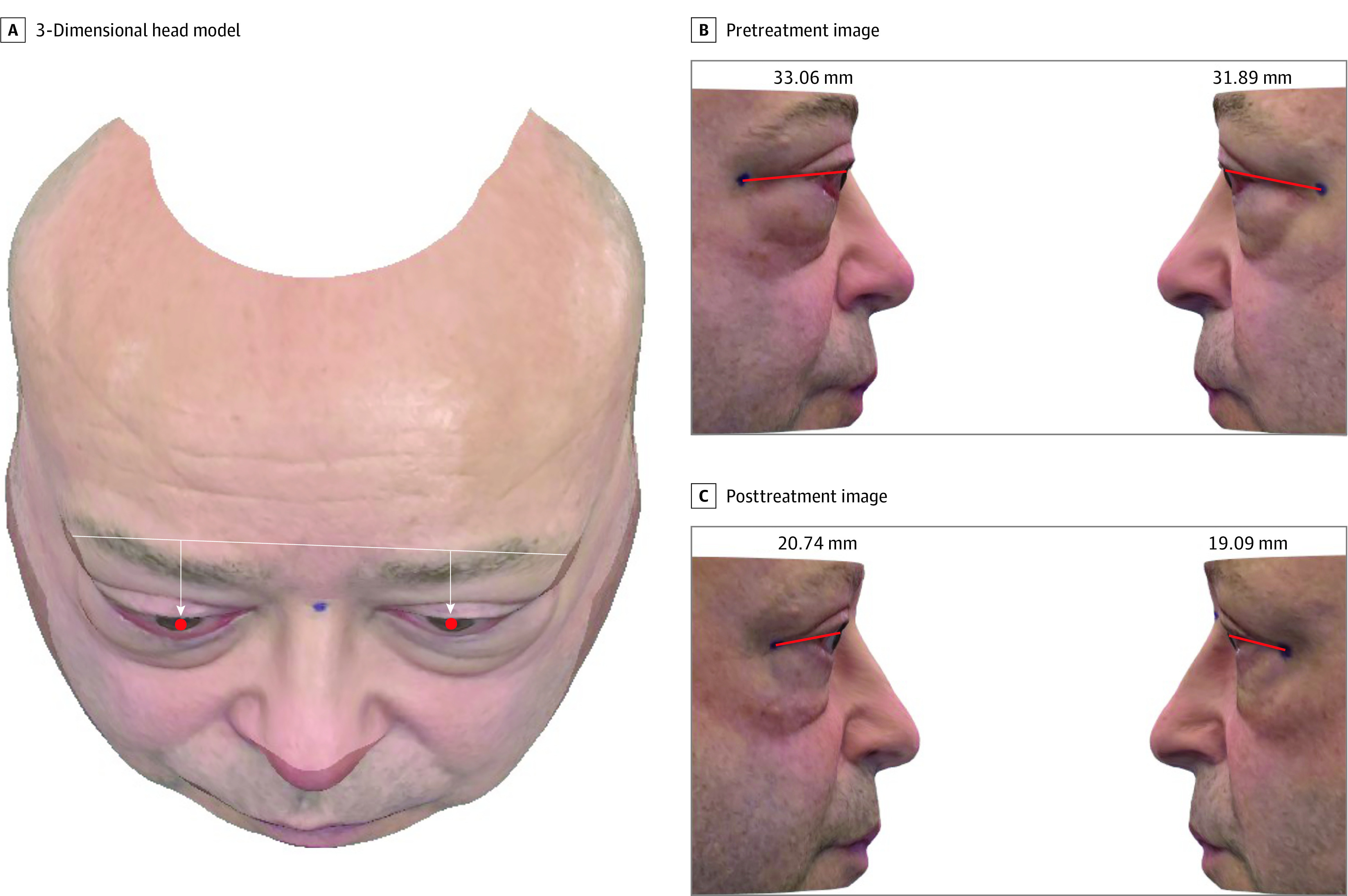
Accuracy and Precision
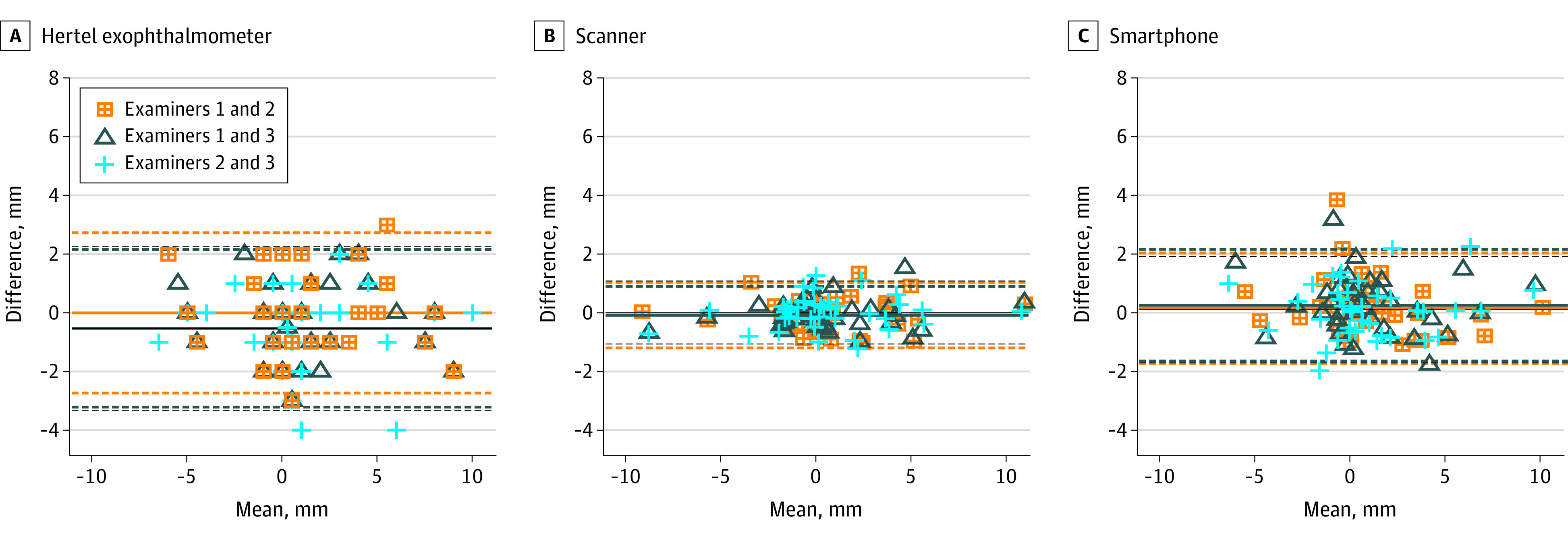
Figure 3 and eFigure 3 in Supplement 1 visualize the correlation between the 3 different methods regarding accuracy and precision using correlation graphs and Bland-Altman plots. There were strong and similar correlations in the difference of eyeball protrusion for all tests. The ICCs comparing Hertel exophthalmometer and smartphone for the 3 examiners had a mean of 0.89 (95% CI, 0.80-0.94) (ICCs of 0.88, 0.92, and 0.87); the mean ICC for the Hertel exophthalmometer compared with the scanner was 0.89 (95% CI, 0.74-0.94) (ICCs of 0.80, 0.91, and 0.88); and the mean ICC for the smartphone compared to the scanner was 0.93 (95% CI, 0.83-0.97) (ICCs of 0.92, 0.94, and 0.94).
Figure 3. Accuracy and Precision of Eyeball Protrusion Measurements With the Smartphone Compared With the Hertel Exophthalmometer and High-Resolution Scanner.
Bland-Altman plots for comparison of the difference in eyeball protrusion between the Hertel exophthalmometer and professional high-resolution scanner (A), between the Hertel exophthalmometer and smartphone (B), and between the scanner and smartphone (C). Solid lines represent the means, and dashed lines indicate 95% CIs. Data of patients and healthy participants are pooled together.
We also computed ICCs for eyeball protrusion (as opposed to the difference between the eyes). For the left eyes (results for right eyes were similar), we found a mean ICC across examiners for the Hertel exophthalmometer compared to the smartphone of 0.63 (95% CI, 0.11-0.84), for the Hertel exophthalmometer compared to the scanner of 0.62 (95% CI, −0.04 to 0.86), and for the smartphone compared to the scanner of 0.94 (95% CI, 0.88-0.97). Note that the ICCs including the Hertel exophthalmometer were both lower and the CIs much larger than the ICC not involving the Hertel exophthalmometer. Part of the reason for the drop in correlations is probably due to the Hertel exophthalmometer measuring a larger eyeball protrusion than the smartphone and the scanner (mean left eye protrusion was 20.3 mm for the Hertel exophthalmometer, 17.5 mm for the smartphone, and 16.9 mm for the scanner). This result is expected since the Hertel exophthalmometer measures up to the cornea, while the imaging methods measure to the pupillary plane and the typical distance from the corneal surface to the pupillary plane is about 3.0 mm.13 This offset is removed when looking at the difference between eyeball protrusion, which also removes some of the variability between examiners in how they identify the cornea and orbital rims (see the higher ICCs in the previous paragraph).
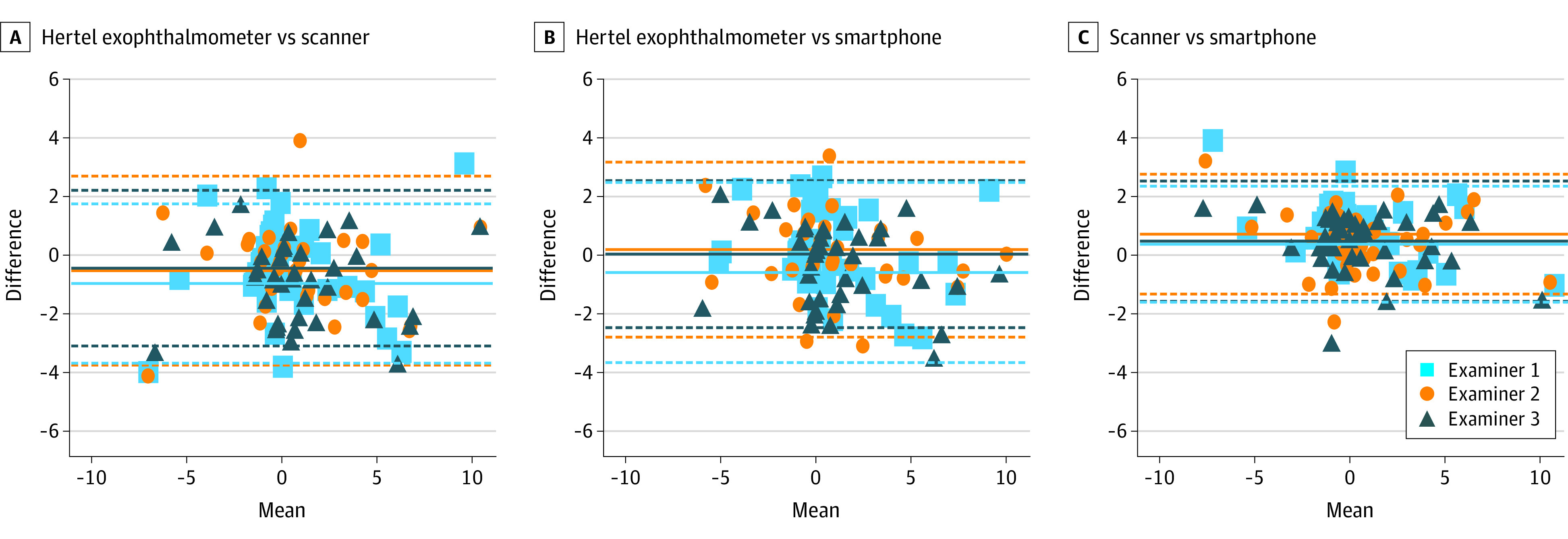
Interoperator Reliability
Figure 4 illustrates the interoperator reliability of the exophthalmos measurements between the 3 different examiners, using all 3 methods on healthy participants and patients with exophthalmos. We observed the narrowest limit of agreement and, thus, the highest interoperator reliability for the high-resolution scanner (ICC, 0.99 [95% CI, 0.98-0.99]). The smartphone measurements demonstrated a slightly wider limit of agreement and, thus, a slightly lower interoperator reliability (ICC, 0.95 [95% CI, 0.92-0.97]). Both methods showed almost no bias (systematic error). The Hertel exophthalmometer measurements as the current criterion standard showed the largest limit of agreement and the highest measurement error, resulting in the lowest interoperator reliability of all 3 methods (ICC, 0.91 [95% CI, 0.85-0.95]). Comparisons of these ICCs found that the ICCs were different from each other (permutation tests, all P < .05, adjusted for multiple comparisons with Holm method). ICC differences for Hertel exophthalmometer vs scanner was 0.08 (95% CI, 0.04-0.16; P < .05); for Hertel exophthalmometer vs smartphone was 0.04 (95% CI, 0.001-0.11; P < .05); and for scanner vs smartphone was 0.04 (95% CI, 0.02-0.09; P < .05).
Figure 4. Interoperator Reliability of Eyeball Protrusion Measurements With the Smartphone Compared to the Hertel Exophthalmometer and High-Resolution Scanner.
In these Bland-Altman plots, solid lines represent the means, and dashed lines indicate 95% CIs.
Test-Retest Reliability
Figure 5 compares the first and the second measurement of each method to assess test-retest reliability. All methods showed similar limits of agreement and, thus, similar test-retest reliabilities. Mean ICC of all 3 examiners was 0.95 (95% CI, 0.89-0.97) for the high-resolution scanner, 0.90 (95% CI, 0.82-0.95) for the smartphone, and 0.92 (95% CI, 0.83-0.96) for the Hertel exophthalmometer. The systematic errors (differences) between tests and retests were negligible for all three methods. When we compared the test-retest ICCs within examiners, we did not find a consistent pattern of significant differences. Each comparison (scanner vs Hertel exophthalmometer, smartphone vs Hertel exophthalmometer, and scanner vs smartphone) was different for 2 of the 3 examiners (permutations tests, P < .05, adjusted for multiple comparisons with Holm method), but each examiner had a different pattern of results.
Figure 5. Test-Retest Reliability of Eyeball Protrusion Measurements With the Smartphone Compared to the Hertel Exophthalmometer and High-Resolution Scanner.
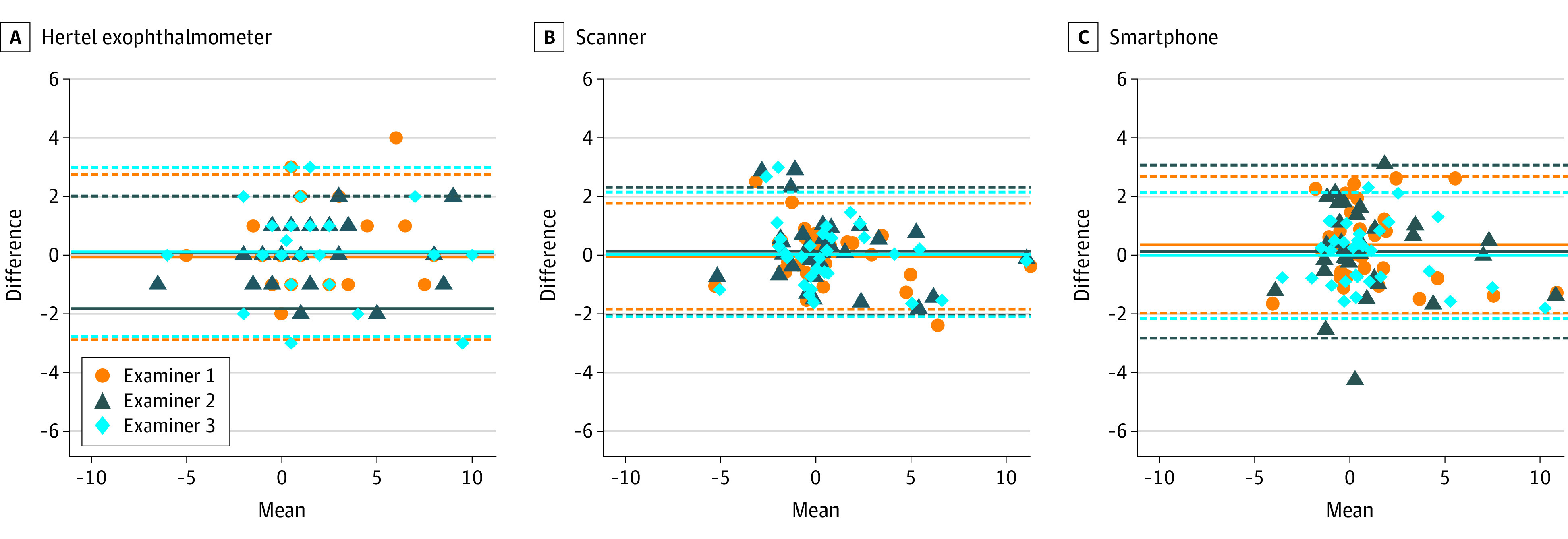
In these Bland-Altman plots, solid lines represent the means, and dashed lines indicate 95% CIs.
Discussion
We assessed eyeball protrusion in patients and healthy participants by comparing measurements with a smartphone to a high-resolution, high-precision 3-D scanner and the Hertel exophthalmometer as the current criterion standard. All measurement methods showed relatively high accuracy and precision, interoperator reliability, and test-retest reliability. Measurements with the smartphone appeared better than measurements with the Hertel exophthalmometer but slightly inferior to the scanner in terms of interoperator reliability.
The Hertel exophthalmometer may be difficult to operate by an inexperienced examiner, prone to reading errors, and may have poor interoperator reliability and test-retest reliability in clinical practice.3 The lower interoperator reliability of the Hertel exophthalmometer could be shown in our study; however, we observed almost no difference in test-retest reliability. This could be explained by the study-specific training of our examiners and the standardized measurements.
As expected, the high-resolution scanner showed the best accuracy and precision, higher interoperator reliability (significant), and test-retest reliability (not significant) in comparison to the other methods. However, it required the longest examination and analysis time, the greatest cooperation of the patient, and was very susceptible to involuntary movements of the patient’s eyes or eyelids. Training and a steady hand of the examiner are required for accurate measurements. Further disadvantages are the high costs, the intricate setup and use, as well as the tedious and time-consuming postprocessing of the raw data (approximately 30 minutes per patient), which makes measurements impractical in everyday clinical care.
In contrast, the smartphone may be more convenient for clinical use. It is readily available for everyone everywhere and requires little skill from the examiner. Both 3-D face scanners have the advantage that the measurements are contactless. For the same reasons, Magazin et al14 took an even simpler approach by taking sagittal smartphone photographs of the face including a reference for the absolute distances to emulate the Hertel exophthalmometer. Smartphone measurements could even be taken by the patients themselves and may be useful for telemedicine.
A disadvantage of both scanners is the need to mark the bony rims of the lateral orbit with a pen to detect their exact location on the 3-D scans. Asymmetries of skin texture and surface due to wrinkles or periorbital swelling may therefore compromise the measurement accuracy. To avoid this problem, we plan to establish new reliable surface reference points for measuring exophthalmos, such as the bridge of the nose and the tragi of the ears. Although this disadvantage was apparent from the beginning of the study, we chose to perform the measurements with exactly the same reference points as the current criterion standard to ensure the best comparison. One difference remains, though, that the Hertel exophthalmometer determines the surface of the cornea relative to the lateral orbital rim, whereas the 3-D scanners measure from the pupillary plane instead. This is inevitable because the cornea is invisible to the scanners. Since there are no absolute normal values for eyeball protrusion, we chose to compare the differences between the protrusion of each eye in addition to the absolute values of eyeball protrusion.
Smartphones use LiDAR scanners (light detection and ranging) for face recognition to unlock smartphones or create special effects in calls, videos, or photos. In addition, smartphones can also record a texture map of 3-D objects with their photo cameras. This image allowed us to identify the precise locations of the pupils and orbital rims to calculate eyeball protrusion. The scanning procedure was very well tolerated by the patients and showed no adverse effects.
The high-precision scanner uses blue light technology to create a 3-D model of all kinds of objects. We used this technology to obtain a high-resolution 3-D model of the face. In comparison to the smartphone, there was no dedicated application for face scanning available. Our method based on the generic scanning software was also safe, but in our experience, the flickering of the blue light at 7.5 Hz was rather disturbing for the patients and led to an increase of eye blinking artifacts. Accordingly, the scans required tedious, manual postprocessing to obtain useful face scans. The postprocessing of the scans was done by 2 different examiners to reduce any possible bias.
The resolution of the 3-D models captured with the smartphone was slightly lower compared to those taken with the high-resolution scanner. This is probably the reason why the results with the high-resolution scanner were slightly better than with the smartphone. However, with further development of LiDAR technology, smartphone scans will be even more precise in the future to measure eyeball protrusion.
The Hertel exophthalmometer is not the only tool for measuring exophthalmos, but it is the only one so far practical to use in clinical practice.15 Magnetic resonance imaging and computed tomography scans have also been shown to measure eyeball protrusion accurately, and the results correlated well with the Hertel exophthalmometer.16 These imaging techniques are also very useful for determining the underlying disease. However, magnetic resonance imaging scans are time consuming, and computed tomography scans require radiation. For these reasons, repeated examinations with these diagnostic modalities are barely practical.
Limitations
A limitation of the study is the relatively small number of individuals evaluated for this proof-of-concept study. In addition, the application is not yet available for clinical use.
Conclusions
Our smartphone scanning method may be readily available with little experience or special training needed for the examiner and likely takes less than a minute to record a patient. In addition, no adverse events were identified, and the measurements can be repeated as often as needed. This may make it suitable to assess patients with exophthalmos and follow their clinical course, for example, after surgery, radiation, or drug treatment. We could successfully validate the smartphone against the Hertel exophthalmometer and a high-resolution 3-D scanner in patients with exophthalmos and healthy volunteers. Hopefully, with further refinement, the application will be approved for distribution on smartphones for future use in clinical practice. Finally, its application will need to prove useful in future clinical trials.
eFigure 1. Study flowchart
eFigure 2. Difference between exophthalmos in patients and healthy participants measured with the smartphone, Hertel exophthalmometer, and high-resolution scanner
eFigure 3. Accuracy and precision of eyeball protrusion measurements with the smartphone compared to the Hertel exophthalmometer and the high-resolution scanner
Data sharing statement
References
- 1.Topilow NJ, Tran AQ, Koo EB, Alabiad CR. Etiologies of proptosis: a review. Intern Med Rev (Wash D C). 2020;6(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hertel E. Ein einfaches exophthalmometer. Albrecht von Graefes Archiv für Ophthalmologie. 1905;60:171-174. doi: 10.1007/BF01885286 [DOI] [Google Scholar]
- 3.Musch DC, Frueh BR, Landis JR. The reliability of Hertel exophthalmometry: observer variation between physician and lay readers. Ophthalmology. 1985;92(9):1177-1180. doi: 10.1016/S0161-6420(85)33880-0 [DOI] [PubMed] [Google Scholar]
- 4.Cammarata MJ, Wake N, Kantar RS, et al. Three-dimensional analysis of donor masks for facial transplantation. Plast Reconstr Surg. 2019;143(6):1290e-1297e. doi: 10.1097/PRS.0000000000005671 [DOI] [PubMed] [Google Scholar]
- 5.Franco de Sá Gomes C, Libdy MR, Normando D. Scan time, reliability and accuracy of craniofacial measurements using a 3D light scanner. J Oral Biol Craniofac Res. 2019;9(4):331-335. doi: 10.1016/j.jobcr.2019.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grant CA, Johnston M, Adam CJ, Little JP. Accuracy of 3D surface scanners for clinical torso and spinal deformity assessment. Med Eng Phys. 2019;63:63-71. doi: 10.1016/j.medengphy.2018.11.004 [DOI] [PubMed] [Google Scholar]
- 7.Seminati E, Canepa Talamas D, Young M, Twiste M, Dhokia V, Bilzon JLJ. Validity and reliability of a novel 3D scanner for assessment of the shape and volume of amputees’ residual limb models. PLoS One. 2017;12(9):e0184498. doi: 10.1371/journal.pone.0184498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WO2022018271 - method for determining a coronal position of an eye relative to the HEADWIPO. Accessed August 10, 2023. https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2022018271
- 9.Bossuyt PM, Reitsma JB, Bruns DE, et al. ; Standards for Reporting of Diagnostic Accuracy . Towards complete and accurate reporting of studies of diagnostic accuracy: the STARD initiative: standards for reporting of diagnostic accuracy. Clin Chem. 2003;49(1):1-6. doi: 10.1373/49.1.1 [DOI] [PubMed] [Google Scholar]
- 10.Maris E, Oostenveld R. Nonparametric statistical testing of EEG- and MEG-data. J Neurosci Methods. 2007;164(1):177-190. doi: 10.1016/j.jneumeth.2007.03.024 [DOI] [PubMed] [Google Scholar]
- 11.Moore DS, McCabe G, Duckworth WM, Alwan L. The Practice of Business Statistics: Using Data for Decisions. 2nd ed. W.H. Freeman and Co;2009. [Google Scholar]
- 12.Holm S. A simple sequentially rejective multiple test procedure. Scand J Stat. 1979;6:65-70. [Google Scholar]
- 13.Goldsmith JA, Li Y, Chalita MR, et al. Anterior chamber width measurement by high-speed optical coherence tomography. Ophthalmology. 2005;112(2):238-244. doi: 10.1016/j.ophtha.2004.09.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Magazin M, Tran AQ, Tooley AA. Utilizing a mobile platform to obtain quantitative measurements of exophthalmos. Orbit. 2022;41(5):591-597. doi: 10.1080/01676830.2021.1980894 [DOI] [PubMed] [Google Scholar]
- 15.Gushchina MB, Afanasyeva DS, Borzenok SA. Exophthalmometry with computed tomography [article in Russian]. Vestn Oftalmol. 2018;134(2):48-52. doi: 10.17116/oftalma2018134248-52 [DOI] [PubMed] [Google Scholar]
- 16.Ramli N, Kala S, Samsudin A, Rahmat K, Abidin ZZ. Proptosis–correlation and agreement between Hertel exophthalmometry and computed tomography. Orbit. 2015;34(5):257-262. doi: 10.3109/01676830.2015.1057291 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Study flowchart
eFigure 2. Difference between exophthalmos in patients and healthy participants measured with the smartphone, Hertel exophthalmometer, and high-resolution scanner
eFigure 3. Accuracy and precision of eyeball protrusion measurements with the smartphone compared to the Hertel exophthalmometer and the high-resolution scanner
Data sharing statement