Abstract
Background:
Epidemiological studies on children and adults have linked toxicants from plastics and personal care products to metabolic disruption. Yet, the impact of endocrine-disrupting chemicals (EDCs) on adolescent metabolic syndrome (MetS) risk during early and mid-adolescence is unclear.
Methods:
To examine the links between exposure to EDCs and MetS risk and its components, cross-sectional data from 344 Mexican youth in early-to-mid adolescence (10–17 years) were analyzed. Urinary biomarker concentrations of phthalates, phenol, and paraben analytes were measured from a single spot urine sample collected in 2015; study personnel obtained anthropometric and metabolic measures. We examined associations between summary phthalates and metabolites, phenol, and paraben analytes with MetS risk z-scores using linear regression, adjusted for specific gravity, sex, age, pubertal status, smoking, alcohol intake, physical activity level, and screen time. As a secondary aim, mediation analysis was conducted to evaluate the role of hormones in the association between summary phthalates with lipids and MetS risk z-scores.
Results:
The mean (SD) age was 13.2 (1.9) years, and 50.9% were female. Sex-stratified analyses revealed associations between summary phthalates and lipids ratio z-scores, including Σ DEHP [β = 0.21 (95% CI: 0.04, 0.37; p < 0.01)], phthalates from plastic sources (Σ Plastic) [β = 0.22 (95% CI: 0.05, 0.39; p < 0.01)], anti-androgenic phthalates (Σ AA) [β = 0.22 (95% CI: 0.05, 0.39; p < 0.01)], and individual phthalate metabolites (MEHHP, MEOHP, and MECPP) among males. Among females, BPA [β = 0.24 (95% CI: 0.03, 0.44; p < 0.05)] was positively associated with lipids ratio z-score and one phenol (2,5 DCP) [β = 0.09 (95% CI: 0.01, 0.18); p < 0.05)] was associated with increased waist circumference z-score. Results showed no evidence of mediation by hormone concentrations in the association between summary phthalates with lipids ratio or MetS risk z-scores.
Conclusion:
Higher EDC exposure was positively associated with serum lipids during adolescence, particularly among males.
Keywords: Adolescence, Birth cohort, Endocrine-disrupting chemicals, Lipids, Metabolic syndrome, Sex-differences
1. Introduction
Adolescence is a period of rapid physical, emotional, and cognitive maturation (Tarokh et al., 2019), during which significant body composition changes occurring during puberty can have implications on metabolic health (Rodríguez et al., 2004; Siervogel et al., 2003). Prevalence of overweight and obesity have increased markedly among adolescents from developed countries, with approximately 23% of males and females classified as overweight or obese in 2013 compared to <17% in 1980 (Ng et al., 2014). A robust body of literature has documented the complex relationship between biological, psychosocial, and behavioral risk factors with adolescent cardiovascular disease risk. In addition to biological processes that may influence metabolic health during adolescence (e.g., puberty), emerging research among children and older youth has demonstrated the role of environmental toxicants, particularly exposure to endocrine-disrupting chemicals (EDCs), may have on metabolism (Gaston and Tulve, 2019; Golestanzadeh et al., 2019; Trasande et al., 2013).
As EDCs (e.g., phthalates, phenols, and parabens) mimic endocrine hormones, exposure to these toxicants may promote weight gain, obesity, and other metabolic changes via disruption of lipid metabolism and adipogenesis, among other pathways (Janesick and Blumberg, 2011; Diamanti-Kandarakis et al., 2009; Grün and Blumberg, 2006). Reports from human epidemiologic studies have linked exposure to EDCs to poor metabolic health. Most studies report associations between early life or concurrent exposure to phthalates and phenols, namely bisphenol A (BPA), on outcomes among child (Russ and Howard, 2016; Silva et al., 2021) and adult populations (Wang et al., 2015; Shankar and Teppala, 2012; Urbina et al., 2013). However, studies of early (ages 10 to 13) to mid-adolescence (ages 14 to 17) (Stages of Adolescence, 2023) are needed as this is the time that coincides with the mid-to-late pubertal transition, which is characterized by fluctuating levels of hormones, and therefore could be especially sensitive to exogenous exposures that disrupt hormones. Most studies linking phthalates and BPA to metabolic change have measured individual components of cardiometabolic risk markers (e.g., lipids, adiposity) in children (Heindel et al., 2017; Grandjean et al., 2015) and adults (Wu et al., 2020a; Moon et al., 2021), as opposed to using comprehensive measures, such as the MetS risk score. In addition, a recent literature review provided evidence of sex-specific differences in the association between phthalates, phenols, and other classes of EDCs with metabolic changes among children, with most studies measuring exposure in early life (Perng et al., 2021). However, adolescents may be at significant risk of exposure given that phthalates, phenols, and parabens are found in household, personal care, and beauty products heavily consumed by adolescents (Buttke et al., 2012), with female adolescents at an even greater risk of exposure through these routes (Harley et al., 2016).
Given the possibility of sex-specific associations, sex hormones could mediate relationships between EDC exposure and metabolic health. Studies have revealed that a decrease in progesterone and a rise in estrogen in females can result in weight gain and other metabolic changes (Carlson et al., 2012). Existing literature has also provided evidence of the acute effects of endogenous progesterone on carbohydrate, lipid, and protein metabolism (Kalkhoff, 1982). Moreover, testosterone has been implicated in the homeostasis of metabolism; for example, a recent study that followed a sample of 1130 males from birth to age 20 found a strong association between obesity and low testosterone levels during crucial development periods, such as puberty (Mancini et al., 2021). Furthermore, EDCs have been shown to impact progesterone and testosterone levels, although the relationship during adolescence remains poorly understood.
One additional caveat to the literature is that current studies conducted among adolescent populations have centered on cohorts from the United States (US),European or Asian countries (Gaston and Tulve, 2019; Trasande et al., 2013; Urbina et al., 2013; Hashemi et al., 2021; Ding et al., 2021; Lin et al., 2016). The scarcity of studies examining linkages between EDCs and metabolic health among Latin American adolescent populations is a significant limitation given that adolescents from Latin America may be at greater risk of cardiometabolic disruption due to multifaceted social and environmental changes (Rivera et al., 2004; Popkin et al., 2012), such as the nutrition transition.
Given the high prevalence of overweight and obesity among Mexican adolescents, as well as the profound links between EDCs and metabolic health, the present cross-sectional study aimed to examine unstratified and sex-stratified associations between exposure to summary phthalate, phthalate metabolites, phenol, and paraben analytes with MetS risk in a cohort of Mexican youth during early-to-mid adolescence. A secondary exploratory aim was to evaluate the role of progesterone and testosterone in the association between summary phthalate measures, DEHP and DBP metabolites with lipids ratio and MetS risk z-scores, as well as sex-stratified informal mediation analysis to examine whether progesterone concentration in female adolescents and testosterone concentration in male adolescents mediated these associations.
2. Methods
2.1. Study population
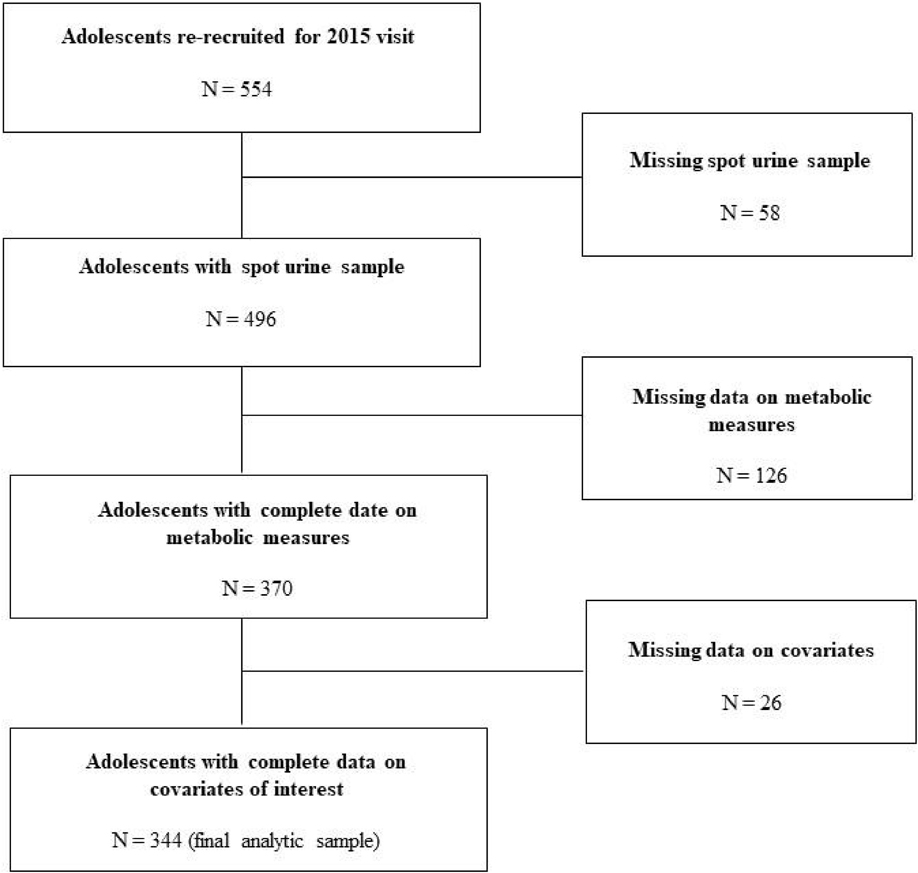
The study included adolescents from two of three sequentially enrolled cohorts of the Early Life Exposure in Mexico to Environmental Toxicants (ELEMENT) study (Perng et al., 2019). From 1997 to 2003, 1012 mother-offspring dyads were recruited from the Mexican Social Security Institute’s public maternity clinics, which serve a low-to-moderate income population in Mexico City. In 2015, a follow-up study was conducted among 554 adolescent offspring from the original birth cohorts two and three, ages 10 to 18. During the follow-up study, information was gathered on sociodemographic and lifestyle characteristics, and pubertal measurements for the 554 adolescents participating in the follow-up study, while only 496 adolescents (89.5%) provided a spot urine sample for EDC biomarker assessment. Compared to the overall sample of 496 adolescents, the sample of 554 adolescents was slightly older but did not differ in other sociodemographic characteristics (data not shown). Further, among the 496 adolescents with complete data on the aforementioned measures, 344 adolescents (69.4%) had complete data on previously mentioned covariates and ascertainment of metabolic outcomes (See Fig. 1 for study flow chart). Compared with the larger cohort sample of 496 adolescents, adolescents in the analytic sample (N=344) did not differ significantly across sociodemographic characteristics (Supplemental Table 1), except that adolescents in the larger cohort sample were slightly older than adolescents in the analytic sample [13.8 (2.1) vs. 13.2 (1.9) years; p < 0.0001], a greater proportion reported having consumed an alcoholic drink in the past year [83.9% vs. 70.6%; p = 0.03)], and reported slightly more screen time [19.6 (10.9) vs. 19.3 (10.6) h/wk; p = 0.0001] (Supplemental Table 1).
Fig. 1.
Study flow chart.
The National Institute of Public Health of Mexico (INSP) and the University of Michigan Human Subjects Committee approved all research protocols and procedures, and all participants provided informed consent.
2.2. Urinary EDC biomarkers
Spot urine samples were collected from adolescent participants. Samples were frozen, kept at −80 °C, and transported to the University of Michigan for analysis at NSF International (Ann Arbor, MI, USA). We measured 14 phthalate metabolites: metabolites of Σ dibutyl phthalate [Σ DBP] – monobutyl phthalate (MBP), mono-isobutyl phthalate (MiBP), metabolites of Σ Di(2-ethylhexyl)phthalate [Σ DEHP] - Mono-2-ethylhexyl phthalate (MEHP), mono(2-ethyl-5-hydroxyhexyl) phthalate (MEHHP), mono-(2-ethyl-5-oxohexyl) phthalate (MEOHP), mono (2-ethyl-5-carboxypentyl) phthalate (MECPP), monobenzyl phthalate (MBzP), monocarboxy-isononly phthalate (MCNP), monocarboxyoctyl phthalate (MCOP), mono-(3-carboxypropyl) phthalate (MCPP), monoethyl phthalate (MEP), ono-isononyl phthalate (MNP), cyclohexane-1,2-dicarboxylic mono carboxyisononyl ester (cx-MINCH), and cyclohexane-1,2-dicarboxylic mono hydroxyisononyl ester (OH-MINCH); 8 phenols - 2,4-Dichlorophenol (2,4 DCP), 2,5-Dichlorophenol (2,5 DCP), bisphenol A (BPA), bisphenol F (BPF), bisphenol S (BPS), benzophenone-3 (BP3), triclocarban, triclosan; and four paraben analytes - butyl paraben, ethyl paraben, methyl paraben, and propyl paraben–using isotope dilution–liquid chromatography-tandem mass spectrometry (ID–LC-MS/MS), as described elsewhere (Lewis et al., 2013). This method was developed and evaluated against acceptance criteria based on the Centers for Disease Control and Prevention (CDC) methods for measuring phenols, phthalates, and parabens from urinary samples (Silva et al., 2004). A summary measure of di-(2-ethyhexyl) phthalate (Σ DEHP) exposure was calculated by dividing the concentrations of each metabolite by their molar mass and then summing the results; a summary measure of dibutyl phthalate (Σ DBP) exposure was calculated by dividing the concentrations of each metabolite by their molar mass and then summing the total concentration. The following summary phthalate mixtures were calculated from urinary phthalate metabolites as previously described (Hatcher et al., 2020; Ziv-Gal et al., 2016): phthalate metabolites from plastic sources (Σ Plastic), phthalate metabolites from personal care products (Σ PCP), and anti-androgenic phthalate metabolites (Σ AA). To correct for urinary dilution, specific gravity was measured using a handheld digital refractometer (Atago Co., Ltd., Tokyo, Japan). All concentrations measured below the limit of detection (LOD) were replaced by the metabolite-specific LOD/√2.
2.3. Serum sex hormones
We measured serum progesterone and testosterone concentrations in adolescent females and males collected during the 2015 visit. Serum sex hormones were selected based on a priori knowledge demonstrating independent associations between respective sex hormones with EDCs (Drake et al., 2009; Chang et al., 2015; Sheikh et al., 2016; Chou and Tzeng, 2021) and metabolic health (Gaston and Tulve, 2019; Golestanzadeh et al., 2019). Briefly, serum aliquots were separated and frozen at −80 °C and then sent to the Clinical Ligand Assay Service Satellite (CLASS) Laboratory at the University of Michigan (Ann Arbor, MI) for hormone analysis (Ashrap et al., 2019). Total testosterone and progesterone were measured using competitive chemiluminescence immunoassays (Bayer Diagnostics Corp, Tarrytown, NY); a complete description of the serum analysis procedures has been described elsewhere (Cathey et al., 2020). Undetectable levels were replaced with the LOD/√2 (Hornung and Reed, 1990). Progesterone and testosterone concentrations were evaluated for non-normality and log-transformed to provide the best fit and modeled as continuous variables. We calculated the geometric mean (GM) and standard deviation (SD) for all samples to account for individual variability.
2.4. Metabolic syndrome risk markers
Given the disagreement in using dichotomous measures for MetS among young populations (Kassi et al., 2011) and in line with recent recommendations, the authors calculated a continuous MetS score instead of a definition based on a dichotomous diagnosis. The validated adolescent MetS risk score (MetS risk z-score) was computed using sex-specific z-scores based on the current sample. The MetS risk z-score was calculated by summing sex-specific z-scores for the following metabolic variables: waist circumference, fasting glucose, insulin, average blood pressure ((SBP + DBP)/2)(Viitasalo et al., 2014) and fasting lipids ratio (TG/HDL-c), with a larger lipids ratio indicating insulin resistance (IR), cardiometabolic risk, and cardiovascular disease (Urbina et al., 2013; Salazar et al., 2014) in adolescents.
Waist circumference was measured to the nearest 1 mm in a consistent location with a non-stretchable tape, guided by sex-specific diagrams of tape placement. All anthropometric data were obtained after the adolescents had removed their clothing and shoes, remaining in their undergarments and a hospital gown. Seated blood pressure measurements were performed in duplicate, and the average systolic blood pressure (SBP) and diastolic blood pressure (DBP) levels were used for analyses. Fasting glucose, triglyceride (TG), and high-density lipoprotein cholesterol (HDL-c) levels were measured using a biochemical analyzer (Cobas Mira Plus, Roche Diagnostics, Basel, Switzerland) on-site in Mexico City.
2.5. Covariates
Potential confounding covariates of interest included sex, age, household socioeconomic status (SES), pubertal status, smoking behavior, alcohol intake, physical activity, and weekly screen time. Household socioeconomic status (SES) was self-reported and assessed using a 10-item region-specific household-based survey that was developed and index standardized (i.e., AMAI 8 × 7) by the Mexican Association of Marketing Research and Public Opinion Agencies (Spanish acronym AMAI) to classify the SES of the Mexican population (Asociación Mexicana de Agencias de Inteligencia de Mercado and Opinión (AMAI), 2018; Lopez Romo, 2009). The survey included household-based assets for the following items: computer and colored television ownership, type of floor, number of rooms, functioning shower, exclusive bathroom, number of lights, type of stove, number of automobiles, and the education level of the highest income earners in the household. Points were assigned to each item in the home and summed to create an overall measure of SES. The overall measure was then categorized into seven categories ranging from A to E based on the sum of the total points. We further categorized the variable into two groups: higher or middle SES (A/B, C+, C, and C−) and lower SES (D+ and D); no participants in the cohort were in the E category.
Trained physicians implemented standard methods for Tanner staging during the in-person visit to assess sexual maturation status (Chavarro et al., 2017). The questionnaire encompassed Tanner stages for pubic hair and breast or genital development. Participants were divided into two pubertal groups: transitioning (Tanner Stage 1 through Tanner Stage 4 in pubic hair and gonadal development) and mature (Tanner Stage 5 in pubic hair and gonadal development). We also obtained information on smoking behavior and alcohol intake behavior. We separately classified smoking behavior and alcohol intake behavior into dichotomous variables: for smoking whether they self-reported ever having smoked (yes or no), and for alcohol intake, whether they had ever consumed an alcoholic drink in the past year (yes or no).
Physical activity information wasobtained from the actigraph, details previously described elsewhere (Wu et al., 2020b), using Chandler’s vector magnitude cutoffs (Chandler et al., 2016), and classified as moderate/vigorous physical activity (MVPA) hours per week (h/wk). Screen time was self-reported and measured using a questionnaire validated in Mexican youth (Hernández et al., 2000). Briefly, screen time was estimated based on the total number of hours per day that the participant reported watching TV (not counting time playing video games or watching movies on the VCR), hours per day watching movies or videos on a VCR or DVD player, and the hours per day playing video games and using the internet for entertainment purposes only. We summed the total number of screen time hours reported and categorized screen time into tertiles of the average screen time hours per week (h/wk).
2.6. Statistical analyses
The distribution of the exposures were explored, and summary statistics (GM, geometric standard errors (GSE), and percentiles) were calculated to measure exposure distribution in the unstratified sample and stratified by adolescent sex. The normality of all variables was investigated via Q-Q plots of residuals; right-skewed variables were ln-transformed, including urinary phthalates, phenol, and paraben analytes. Only analytes detected in ≥70% of the analytic sample were included in regression analysis.
Mean and SD were examined to evaluate the crude associations between adolescent sociodemographic and lifestyle characteristics by the concentration of five summary phthalate measures. Next, crude associations between sociodemographic and lifestyle characteristics by adolescent sex-specific z-scores for each of the five MetS risk components, and the overall measure of MetS risk were evaluated.
Beta (β) coefficients and 95% confidence intervals (CIs) were computed from unstratified and sex-stratified linear regression models to examine the association between ln-transformed urinary exposure and MetS risk Z-score and its components (waist circumference, fasting lipids ratio, fasting glucose, average blood pressure, and insulin). The first model was adjusted for specific gravity only (Model 1); the second was adjusted for specific gravity, sex, age group, pubertal status, smoking behavior, alcohol intake behavior, physical activity level, and screen time (Model 2). In addition, to investigate potential nonlinear associations within the unstratified sample, multivariate linear regression models were used to examine the relations between urinary EDC concentration tertiles and adolescent components of MetS risk z-scores, and overall MetS risk z-scores, adjusting for urinary specific gravity, sex, age group, puberty status, smoking behavior, alcohol intake behavior, physical activity level, screen time. To examine potential nonlinear associations stratified by adolescent sex, we ran similar multivariate linear regression models adjusted for all covariates, except for sex.
We conducted the Baron and Kenny test (i.e., informal mediation analyses) (Baron and Kenny, 1986) to determine the potential mediating role of progesterone and testosterone hormones in the associations between EDCs (i.e., summary phthalate measures, DEHP, and DBP metabolites) and select metabolic markers (i.e., lipids ratio z-score and MetS risk z-score). Unadjusted (adjusted for specific gravity only) informal mediation analyses were conducted by adjusting for progesterone and testosterone concentration and evaluating differences in beta estimates. Finally, we conducted sex-stratified mediation analyses to evaluate the role of progesterone in the associations between EDCs (i.e., summary phthalate measures, DEHP, and DBP metabolites) with the aforementioned metabolic markers among female adolescents and separate informal mediation analyses to evaluate the role of testosterone in the associations between EDCs (i.e., summary phthalate measures, DEHP and DBP metabolites) with the aforementioned metabolic markers among male adolescents. In post-hoc analyses, we conducted the previously mentioned informal mediation models, adjusting for specific gravity, sex, age group, puberty status, smoking behavior, alcohol intake behavior, physical activity level, and screen time (data not shown). Finally, to adjust for multiple comparisons (Benjamini and Hochberg, 1995), we conducted post-hoc analyses for the unstratified sample using a false discovery rate (FDR) with the statistical significant set at p < 0.05.
All statistical analyses were performed using SAS 9.4 software (Cary, NC, USA). The results were considered statistically significant at p < 0.05.
3. Results
At the early to-mid adolescent study visit, participants’ mean (SD) age was 13.2 (1.9) with a range of 10–17 years; 50.9% were female.
The distribution of summary phthalate measures, individual phthalate metabolites, phenol, and paraben analyte concentrations are presented in Table 1. The detection rate for toxicants varied, with most toxicants being detected in the analytic sample. All GM and geometric standard errors (GSE) are listed in Table 1. Of note, Σ AA GM (GSE) for males was slightly higher in males than females [233.5 (16.7) ng/mL vs. 208.2 (12.9) ng/mL]. Similar patterns were observed for all summary phthalate measures and phthalate metabolites. However, females had higher GM (SE) concentrations of most phenol metabolites (Table 1).
Table 1.
Summary statistics for urinary exposure biomarkers (ng/mL) measured from spot urine (N = 344).
| LOD | % < LOD | Entire Sample (N = 344) |
Males (N = 169) |
Females (N = 175) |
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GM | SE | Min | Q1 | Q3 | Max | GM | SE | Min | Q1 | Q3 | Max | GM | SE | Min | Q1 | Q3 | Max | |||
|
| ||||||||||||||||||||
| Σ PCP | – | – | 251.8 | 14.3 | 2.4 | 131.1 | 468.7 | 9114.1 | 259.1 | 21.7 | 14.6 | 124.9 | 483.7 | 8498.2 | 245.1 | 18.9 | 2.4 | 136.3 | 463.8 | 9114.1 |
| Σ AA | – | – | 220.3 | 10.4 | 5.2 | 129.4 | 374.1 | 7067.4 | 233.5 | 16.7 | 22.0 | 130.5 | 400.1 | 7067.4 | 208.2 | 12.9 | 5.2 | 128.5 | 332.6 | 2023.5 |
| Σ Plastic | – | – | 66.4 | 3.3 | 2.9 | 38.6 | 113.1 | 6030.9 | 69.7 | 5.1 | 6.3 | 40.5 | 113.6 | 6030.9 | 63.3 | 4.2 | 2.9 | 35.3 | 109.8 | 855.4 |
| Σ DEHP | – | – | 83.9 | 4.3 | 3.7 | 49.3 | 145.7 | 8529.0 | 88.2 | 6.7 | 7.9 | 51.4 | 144.6 | 8529.0 | 80.0 | 5.5 | 3.7 | 45.6 | 146.0 | 1193.4 |
| Σ DBP | – | – | 132.2 | 6.6 | 2.2 | 77.0 | 230.3 | 4280.3 | 137.6 | 10.1 | 8.0 | 76.2 | 255.9 | 4280.3 | 127.3 | 8.5 | 2.2 | 78.0 | 222.4 | 1068.6 |
| MCPP | 0.2 | 1.2 | 1.8 | 0.1 | 0.1 | 1.0 | 2.9 | 51.2 | 1.8 | 0.1 | 0.1 | 1.0 | 3.0 | 36.2 | 1.7 | 0.1 | 0.1 | 1.0 | 2.7 | 51.2 |
| MEP | 1 | 0.0 | 103.4 | 7.5 | 0.8 | 42.8 | 231.0 | 8990.0 | 104.0 | 10.7 | 6.6 | 39.8 | 219.5 | 8440.0 | 102.9 | 10.5 | 0.8 | 44.9 | 235.4 | 8990.0 |
| MECPP | 0.2 | 0.0 | 43.6 | 2.2 | 2.0 | 24.8 | 78.4 | 3512.3 | 45.8 | 3.5 | 3.7 | 25.1 | 77.6 | 3512.3 | 41.6 | 2.9 | 2.0 | 24.1 | 78.5 | 580.0 |
| MEHHP | 0.1 | 0.0 | 28.1 | 1.5 | 0.8 | 16.2 | 47.2 | 3569.8 | 29.8 | 2.3 | 2.6 | 17.1 | 46.4 | 3569.8 | 26.6 | 2.0 | 0.8 | 14.8 | 48.4 | 459.0 |
| MIBP | 0.1 | 0.0 | 10.0 | 0.5 | 0.4 | 5.9 | 17.9 | 155.5 | 10.2 | 0.7 | 1.3 | 5.8 | 16.3 | 155.5 | 9.8 | 0.7 | 0.4 | 6.0 | 18.5 | 115.0 |
| MEOHP | 0.1 | 0.0 | 13.6 | 0.7 | 0.5 | 7.6 | 23.1 | 1869.0 | 14.3 | 1.1 | 1.4 | 7.8 | 22.8 | 1869.0 | 12.9 | 0.9 | 0.5 | 7.3 | 23.0 | 180.0 |
| MBP | 0.5 | 0.0 | 118.9 | 6.1 | 1.9 | 70.8 | 210.2 | 4264.0 | 123.4 | 9.5 | 3.1 | 69.0 | 221.6 | 4264.0 | 114.6 | 7.8 | 1.9 | 71.0 | 202.6 | 1050.0 |
| MBzP | 0.2 | 0.3 | 3.8 | 0.2 | 0.1 | 2.1 | 6.5 | 161.3 | 3.8 | 0.3 | 0.5 | 2.0 | 7.0 | 70.9 | 3.7 | 0.3 | 0.1 | 2.3 | 6.1 | 161.3 |
| MEHP | 1.0 | 4.9 | 4.0 | 0.2 | 0.2 | 2.4 | 7.0 | 243.3 | 4.0 | 0.3 | 0.2 | 2.4 | 7.1 | 243.3 | 4.0 | 0.3 | 0.2 | 2.4 | 6.8 | 71.0 |
| MNP | 0.5 | 99.7 | 0.3 | 0.0 | 0.0 | 0.2 | 0.3 | 0.4 | 0.3 | 0.0 | 0.0 | 0.2 | 0.3 | 0.4 | 0.3 | 0.0 | 0.0 | 0.2 | 0.3 | 0.4 |
| MCOP | 0.2 | 0.0 | 4.1 | 0.2 | 0.3 | 2.1 | 7.3 | 143.4 | 4.4 | 0.3 | 0.6 | 2.4 | 7.5 | 104.9 | 3.8 | 0.3 | 0.3 | 1.9 | 6.8 | 143.4 |
| MCNP | 0.2 | 0.9 | 0.8 | 0.0 | 0.1 | 0.5 | 1.2 | 8.8 | 0.8 | 0.0 | 0.0 | 0.1 | 0.5 | 8.3 | 0.7 | 0.0 | 0.1 | 0.5 | 1.1 | 8.8 |
| cx-MINCH | 0.2 | 36.0 | 0.3 | 0.0 | 0.0 | 0.1 | 0.5 | 5.1 | 0.2 | 0.0 | 0.0 | 0.1 | 0.5 | 5.1 | 0.3 | 0.0 | 0.0 | 0.2 | 0.5 | 5.0 |
| OH-MINCH | 0.2 | 31.3 | 0.3 | 0.0 | 0.0 | 0.1 | 0.5 | 8.3 | 0.3 | 0.0 | 0.2 | 0.6 | 1.3 | 8.2 | 0.3 | 0.0 | 0.0 | 0.1 | 0.5 | 6.0 |
| 2,4 DCP | 0.2 | 0.3 | 3.8 | 0.3 | 0.1 | 1.5 | 6.9 | 601.0 | 3.9 | 0.4 | 0.3 | 1.6 | 6.4 | 536.0 | 3.7 | 0.4 | 0.1 | 1.3 | 7.1 | 601.0 |
| 2,5 DCP | 0.2 | 0.0 | 32.0 | 3.1 | 1.6 | 9.5 | 72.7 | 6740.0 | 30.1 | 4.1 | 1.9 | 9.1 | 59.4 | 6740.0 | 33.9 | 4.6 | 1.6 | 9.7 | 85.1 | 5590.0 |
| BP3 | 0.4 | 0.3 | 24.7 | 2.2 | 0.3 | 7.7 | 61.9 | 8500.0 | 17.4 | 2.2 | 0.8 | 6.1 | 38.3 | 8500.0 | 34.6 | 4.4 | 0.3 | 11.4 | 85.1 | 3620.0 |
| BPA | 0.4 | 5.8 | 1.2 | 0.1 | 0.3 | 0.7 | 1.9 | 70.1 | 1.2 | 0.1 | 0.3 | 0.7 | 1.8 | 70.1 | 1.3 | 0.1 | 0.3 | 0.7 | 2.0 | 12.2 |
| BPS | 0.2 | 80.2 | 0.4 | 0.0 | 0.3 | 0.3 | 0.3 | 21.1 | 0.4 | 0.0 | 0.3 | 0.3 | 0.3 | 11.4 | 0.4 | 0.0 | 0.3 | 0.3 | 0.3 | 21.1 |
| triclocarban | 2.0 | 84.6 | 1.7 | 0.1 | 1.4 | 1.4 | 1.4 | 47.5 | 1.8 | 0.1 | 1.4 | 1.4 | 1.4 | 40.4 | 1.7 | 0.1 | 1.4 | 1.4 | 1.4 | 47.5 |
| triclosan | 2.0 | 26.2 | 10.4 | 1.1 | 1.4 | 1.4 | 38.7 | 1956.1 | 10.2 | 1.6 | 1.4 | 1.4 | 44.0 | 1105.3 | 10.6 | 1.6 | 1.4 | 2.1 | 35.4 | 1956.1 |
| butyl paraben | 0.2 | 80.2 | 0.2 | 0.0 | 0.1 | 0.1 | 0.1 | 103.0 | 0.2 | 0.0 | 0.1 | 0.1 | 0.1 | 21.5 | 0.2 | 0.0 | 0.1 | 0.1 | 0.1 | 103.0 |
| ethyl paraben | 1.0 | 80.2 | 3.1 | 0.3 | 0.7 | 0.7 | 8.6 | 967.0 | 3.0 | 0.4 | 0.7 | 0.7 | 7.7 | 447.2 | 3.3 | 0.4 | 0.7 | 0.7 | 8.7 | 967.0 |
| methyl paraben | 1.0 | 0.0 | 47.8 | 4.7 | 1.2 | 10.1 | 199.0 | 3740.0 | 39.3 | 5.4 | 1.2 | 8.7 | 188.0 | 2330.0 | 57.8 | 7.9 | 1.3 | 15.0 | 217.4 | 3740.0 |
| propyl paraben | 0.2 | 2.0 | 4.7 | 0.6 | 0.1 | 0.7 | 31.2 | 839.0 | 2.9 | 0.5 | 0.1 | 0.6 | 8.3 | 592.0 | 7.4 | 1.3 | 0.1 | 1.0 | 50.0 | 839.0 |
ABBR: EDCs: endocrine-disrupting chemicals; N = Sample size; LOD: limit of detection; Q1: Lower Quartile; Q3: Upper Quartile; DBP: dibutyl phthalate metabolites; DEHP: di-2-ethylhexyl phthalate metabolites; MECPP: mono-2-ethyl-5-carboxypentyl phthalate; MEHHP: mono-2-ethyl-5-hydroxyhexyl phthalate; MEHP: mono-2-ethylhexyl phthalate; MEOH: mono-2-ethyl-5-oxohexyl phthalate; MECPTP: Mono-2-ethyl-5-carboxypentyl Terephthalate-d4; MEHHTP: mono-2-ethyl-5-hydroxyhexyl terephthalate; MBzP: monobenzyl phthalate; MBP: Mono-n-butyl phthalate; MCNP: Monocarboxy-isononly phthalate; MCOP: Monocarboxyoctyl phthalate; MCPP: mono-3-carboxypropyl phthalate; MEP: monoethyl phthalate; MNP: Mono-isononyl phthalate; MiBP: mono-isobutyl phthalate; cxMINCH: cyclohexane-1,2-dicarboxylic mono carboxyisooctyl ester; OH-MINCH: cyclohexane-1,2-dicarboxylic mono hydroxyisononyl ester; 2,4 DCP: 2,4-Dichlorophenol; 2,5 DCP:2,5-Dichlorophenol; BP3: Benzophenone-3; BPA: Bisphenol A; BPS: Bisphenol S.
In Supplemental Table 2, we present the distribution of serum sex hormone concentrations in the unstratified sample and stratified by sex.
Table 2 presents the crude associations between sociodemographic characteristics and urinary phthalate summary measures. Adolescents belonging to the lower SES group had a significantly lower concentration of Σ DBP [169.3 (153.8) vs. 237.2 (388.2); p = 0.04) and Σ PCP [169.3 (153.8) vs. 237.2 (388.2); p = 0.01] than their counterparts with higher SES. No other differences were observed in the concentrations of urinary EDCs according to the demographics. Table 3 presents differences in the crude associations between demographics, MetS risk z-scores, and components. Females had higher waist circumference, and fasting glucose, than males. Older adolescents had higher blood pressure, and waist circumference z-scores than younger adolescents; similar trends were observed for adolescents of mature (vs. transitioning) pubertal status.
Table 2.
Baseline demographics according to urinary phthalate summary variables (N = 344).
| N | Σ DEHP | Σ DBP | Σ Plastic | Σ AA | Σ PCP | |
|---|---|---|---|---|---|---|
| Mean (SD) (ng/mL) | Mean (SD) (ng/mL) | Mean (SD) (ng/mL) | Mean (SD) (ng/mL) | Mean (SD) (ng/mL) | ||
|
| ||||||
| Sex | ||||||
| Male | 169 | 211.5 (777.9) | 229.2 (390.0) | 156.8 (550.2) | 403.2 (752.4) | 500.7 (901.9) |
| Female | 175 | 121.2 (145.2) | 177.5 (154.7) | 93.3 (105.1) | 279.8 (235.5) | 444.7 (885.0) |
| P | 0.53 | 0.71 | 0.55 | 0.56 | 0.72 | |
| Age group, (years) | ||||||
| 10–12 | 146 | 152.8 (295.2) | 191.3 (205.5) | 115.0 (209.3) | 318.4 (324.9) | 422.9 (656.9) |
| 13–15 | 139 | 163.8 (719.0) | 184.5 (190.9) | 123.3 (508.3) | 321.1 (618.8) | 484.8 (944.6) |
| 16–17 | 59 | 201.3 (615.1) | 274.7 (563.7) | 151.0 (436.8) | 440.5 (801.0) | 564.4 (1222.12) |
| P | 0.67 | 0.61 | 0.67 | 0.88 | 0.98 | |
| SES | ||||||
| Lower | 174 | 195.9 (692.8) | 169.3 (153.8) | 145.3 (489.9) | 330.8 (595.8) | 428.0 (917.0) |
| Middle/Higher | 170 | 134.5 (366.3) | 237.2 (388.2) | 103.3 (260.3) | 350.3 (513.8) | 517.4 (867.1) |
| P | 0.21 | 0.04 | 0.38 | 0.31 | 0.01 | |
| Pubertal status | ||||||
| Transitioning | 306 | 158.6 (528.8) | 206.3 (308.3) | 119.5 (374.0) | 338.2 (537.5) | 489.0 (937.5) |
| Mature | 38 | 221.7 (746.3) | 175.2 (158.4) | 164.7 (529.8) | 358.5 (696.6) | 336.8 (344.1) |
| P | 0.46 | 0.58 | 0.53 | 0.48 | 0.78 | |
| Smoking behavior | ||||||
| Ever Smoker | 51 | 123.9 (106.0) | 191.8 (129.8) | 97.5 (81.1) | 297.7 (191.8) | 490.4 (660.3) |
| Never Smoker | 293 | 172.8 (600.7) | 204.8 (315.7) | 129.2 (425.0) | 347.9 (597.1) | 469.0 (927.9) |
| P | 0.39 | 0.13 | 0.41 | 0.22 | 0.29 | |
| Alcohol intake | ||||||
| Consumed drink in past year | 243 | 131.5 (317.6) | 185.1 (177.3) | 100.3 (226.1) | 295.4 (353.9) | 489.0 (971.8) |
| Did not consume drink in past year | 101 | 247.4 (898.1) | 245.7 (469.9) | 182.8 (634.6) | 448.7 (860.7) | 431.7 (666.7) |
| P | 0.30 | 0.78 | 0.26 | 0.37 | 0.47 | |
| MVPA tertiles, (h/wk) | ||||||
| 15.5–66.4 | 103 | 202.4 (839.5) | 224.1 (445.1) | 151.0 (593.3) | 391.3 (812.0) | 605.3 (1362.3) |
| 66.5–90.4 | 117 | 202.5 (529.6) | 177.6 (145.8) | 150.8 (375.7) | 345.4 (501.7) | 411.3 (637.4) |
| 90.6–216.3 | 124 | 100.2 (79.7) | 209.1 (241.2) | 77.7 (59.0) | 293.5 (271.6) | 419.1 (598.3) |
| P | 0.44 | 0.92 | 0.39 | 0.69 | 0.91 | |
| Screen time tertiles, (h/wk) | ||||||
| 0.5–14.0 | 111 | 234.3 (865.1) | 209.4 (427.9) | 172.4 (611.4) | 400.9 (862.90 | 351.9 (458.4) |
| 14.5–21.0 | 121 | 119.9 (110.0) | 205.1 (229.6) | 93.3 (81.5) | 307.3 (266.7) | 451.9 (675.9) |
| 21.5–72.0 | 112 | 146.8 (439.5) | 194.0 (176.8) | 110.7 (312.1) | 316.4 (442.3) | 613.4 (1313.1) |
| P | 0.27 | 0.29 | 0.31 | 0.41 | 0.23 | |
ABBR: Σ DBP: molar sum of dibutyl phthalate metabolites; Σ DEHP: molar sum of di-2-ethylhexyl phthalate metabolites; Σ Plastic: molar sum of phthalate metabolites from plastic sources.
Σ AA: molar sum of anti-androgenic phthalate metabolites; Σ PCP: molar sum of personal care product phthalate metabolites; h/wk: hours per week; N = sample size; MVPA: moderate-vigorous; physical activity; SES: socioeconomic status; SE: standard deviation.
Table 3.
Baseline demographics according to metabolic measures (N = 344).
| N | Waist circumference z-score | Insulin z-score | Average blood pressure (Tarokh et al., 2019) z-score | Lipids ratio (Rodríguez et al., 2004) z-score | Fasting glucose z-score | MetS Risk z-score | |
|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||
|
| |||||||
| Sex | |||||||
| Male | 169 | −0.17 (1.1) | −0.14 (0.80) | 0.05 (1.0) | −0.08 (0.91) | 0.16 (1.0) | −0.06 (1.0) |
| Female | 175 | 0.12 (1.0) | 0.12 (1.2) | −0.24 (0.90) | 0.04 (1.1) | −0.15 (1.0) | 0.04 (1.0) |
| P | 0.0075 | 0.0028 | 0.0083 | 0.08 | 0.0040 | 0.26 | |
| Age groups, (years) | |||||||
| 10–12 | 146 | −0.10 (1.1) | 0.07 (1.2) | −0.34 (0.94) | 0.08 (1.2) | 0.08 (0.96) | 0.03 (1.1) |
| 13–15 | 139 | −0.09 (0.92) | −0.08 (0.72) | −0.04 (0.96) | −0.13 (0.74) | 0.00 (1.0) | −0.10 (0.88) |
| 16–17 | 59 | 0.35 (1.1) | −0.04 (1.0) | 0.38 (0.93) | 0.00 (0.94) | −0.14 (1.1) | 0.11 (1.0) |
| P | 0.02 | 0.51 | <.0001 | 0.57 | 0.61 | 0.39 | |
| SES | |||||||
| Lower | 174 | 0.08 (1.0) | 0.06 (1.2) | −0.10 (1.0) | 0.07 (1.1) | 0.01 (1.1) | 0.08 (1.1) |
| Middle/Higher | 170 | −0.11 (1.0) | −0.08 (0.8) | −0.08 (1.0) | −0.11 (0.90) | 0.00 (0.91) | −0.11 (0.88) |
| P | 0.05 | 0.29 | 0.81 | 0.04 | 0.94 | 0.21 | |
| Pubertal status | |||||||
| Transitioning | 306 | −0.05 (1.0) | 0.00 (1.0) | −0.16 (0.96) | −0.02 (1.0) | 0.01 (1.0) | −0.02 (1.0) |
| Mature | 38 | 0.24 (0.87) | −0.08 (0.77) | 0.45 (1.0) | −0.03 (1.0) | −0.02 (1.0) | 0.10 (0.91) |
| P | 0.04 | 0.80 | 0.0010 | 0.83 | 0.89 | 0.26 | |
| Smoker | |||||||
| Ever Smoker | 51 | 0.16 (1.1) | −0.12 (0.89) | 0.15 (0.96) | −0.26 (0.55) | −0.10 (1.2) | −0.09 (0.89) |
| Never Smoker | 293 | −0.05 (1.1) | 0.01 (1.0) | −0.13 (0.98) | 0.02 (1.0) | 0.02 (1.0) | 0.00 (1.0) |
| P | 0.30 | 0.20 | 0.12 | 0.14 | 0.59 | 0.72 | |
| Alcohol intake | |||||||
| Consumed drink in past year | 243 | 0.02 (1.0) | −0.05 (0.79) | −0.06 (0.90) | −0.05 (1.0) | 0.02 (1.0) | −0.01 (0.95) |
| Did not consume drink in past year | 101 | −0.12 (1.1) | 0.09 (1.4) | −0.18 (1.1) | 0.06 (1.0) | −0.04 (0.95) | −0.01 (1.1) |
| P | 0.17 | 0.95 | 0.28 | 0.52 | 0.52 | 0.49 | |
| MVPA tertiles, (h/wk) | |||||||
| 15.5–66.4 | 103 | 0.08 (1.1) | 0.02 (0.90) | 0.05 (1.1) | 0.04 (0.88) | −0.15 (1.1) | 0.01 (1.0) |
| 66.5–90.4 | 117 | −0.09 (0.97) | −0.06 (0.83) | −0.12 (0.93) | 0.00 (1.1) | 0.01 (0.93) | −0.05 (1.0) |
| 90.6–216.3 | 124 | −0.04 (0.98) | 0.02 (1.2) | −0.18 (0.93) | −0.08 (1.0) | 0.13 (1.0) | 0.01 (1.1) |
| P | 0.86 | 0.93 | 0.27 | 0.18 | 0.01 | 0.82 | |
| Screen time tertiles, (h/wk) | |||||||
| 0.5–14.0 | 111 | 0.06 (1.1) | −0.05 (0.80) | −0.26 (1.0) | −0.12 (0.79) | 0.00 (1.0) | −0.05 (0.91) |
| 14.5–21.0 | 121 | −0.16 (0.99) | −0.01 (1.2) | −0.05 (0.94) | 0.02 (1.0) | −0.04 (1.0) | −0.06 (1.0) |
| 21.5–72.0 | 112 | 0.05 (1.0) | 0.04 (0.93) | 0.02 (1.0) | 0.04 (1.2) | 0.05 (1.0) | 0.08 (1.1) |
| P | 0.20 | 0.71 | 0.07 | 0.65 | 0.87 | 0.51 | |
Average blood pressure: (SBP + DBP/2)
Lipids ratio: TG/HDL-c
ABBR: h/wk: hours per week; N = sample size; MVPA: moderate-vigorous physical activity; SES: socioeconomic status; SD: standard deviation.
Table 4 presents the unadjusted and fully adjusted associations between every 1-unit log increase in summary phthalate measures or EDC analytes with sex-specific z-scores for MetS risk components and overall MetS risk z-score in the unstratified sample. Table 5 presents sex-stratified findings from the multivariate linear models between each toxicant and metabolic syndrome risk and individual component z-scores adjusted for specific gravity, age group, puberty status, smoking behavior, alcohol intake behavior, physical activity level, and screen time. In the following sections we present the statistically significant results from Tables 4 and 5 according to each MetS risk component.
Table 4.
Unadjusted and adjusted linear regression of associations between ln-transformed urinary EDCs by metabolic outcomes (N = 344).
| Waist circumference z-score β (95% CI) | Insulin z-score β (95% CI) | Average blood pressure (Tarokh et al., 2019) z-score β (95% CI) | Lipids ratio (Rodriguez et al., 2004) z-score β (95% CI) | Fasting glucose z-score β (95% CI) | MetS risk z-score β (95% CI) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | |
| Σ DEHP | 0.06 (−0.06, 0.18) | 0.08 (−0.04, 0.20) | 0.09 (−0.03, 0.20) | 0.10 (−0.02, 0.21) | 0.07 (−0.04, 0.18) | 0.07 (−0.04, 0.18) | 0.13 (0.01, 0.24)* | 0.12 (0.01, 0.24)* | 0.07 (−0.05, 0.19) | 0.07 (−0.04, 0.19) | 0.13 (0.01, 0.25)* | 0.14 (0.03, 0.26)* |
| MEHP | 0.00 (−0.12, 0.12) | 0.00 (−0.13, 0.11) | 0.04 (−0.08, 0.16) | 0.04 (−0.08, 0.16) | 0.04 (−0.07, 0.16) | 0.03 (−0.08, 0.15) | 0.09 (−0.03, 0.20) | 0.11 (−0.01, 0.22) | 0.04 (−0.08, 0.16) | 0.06 (−0.06, 0.17) | 0.06 (−0.06, 0.18) | 0.07 (−0.05, 0.19) |
| MEHHP | 0.06 (−0.05, 0.17) | 0.08 (−0.03, 0.19) | 0.08 (−0.03, 0.19) | 0.09 (−0.02, 0.20) | 0.07 (−0.04, 0.18) | 0.07 (−0.04, 0.17) | 0.12 (0.01, 0.23)* | 0.13 (0.01, 0.25)* | 0.06 (−0.06, 0.17) | 0.06 (−0.05, 0.17) | 0.12 (0.01, 0.23)* | 0.13 (0.02, 0.25)* |
| MECPP | 0.06 (−0.06, 0.18) | 0.09 (−0.03, 0.21) | 0.10 (−0.02, 0.21) | 0.10 (−0.01, 0.22) | 0.07 (−0.04, 0.18) | 0.08 (−0.04, 0.19) | 0.13 (−0.01, 0.24)* | 0.14 (0.01, 0.26)* | 0.09 (−0.03, 0.21) | 0.09 (−0.02, 0.21) | 0.14 (0.03, 0.26)* | 0.15 (0.04, 0.27)* |
| MEOHP | 0.04 (−0.07, 0.16) | 0.06 (−0.06, 0.17) | 0.07 (−0.04, 0.18) | 0.08 (−0.03, 0.19) | 0.06 (−0.04, 0.17) | 0.05 (−0.05, 0.16) | 0.10 (−0.01, 0.21) | −0.02 (−0.08, 0.03) | 0.04 (−0.07, 0.16) | −0.05 (−0.6, 0.17) | 0.10 (−0.11, 0.21) | 0.11 (−0.01, 0.22) |
| Σ DBP | 0.00 (−0.13, 0.12) | 0.00 (−0.12, 0.13) | 0.02 (−0.11, 0.14) | 0.03 (−0.10, 0.15) | 0.09 (−0.03, 0.20) | 0.06 (−0.05, 0.18) | 0.07 (−0.05, 0.20) | 0.08 (−0.04, 0.20) | −0.04 (−0.17, 0.08) | −0.04 (−0.16, 0.08) | 0.02 (−0.10, 0.15) | 0.03 (−0.10, 0.16) |
| MBP | 0.00 (−0.13, 0.12) | 0.00 (−0.12, 0.12) | 0.02 (−0.10, 0.14) | 0.03 (−0.09, 0.15) | 0.09 (−003, 0.20) | 0.06 (−0.05, 0.17) | 0.07 (−0.04, 019) | 0.08 (−0.04, 0.20) | −0.05 (−0.16, 0.07) | −0.04 (−0.16, 0.08) | 0.02 (−0.09, 0.14) | 0.03 (−0.09, 0.15) |
| MiBP | 0.01 (−0.11, 0.13) | 0.01 (−0.11, 0.13) | −0.03 (−0.15, 0.09) | −0.03 (−0.16, 0.09) | 0.00 (−0.11, 0.11) | −0.02 (−0.13, 0.10) | 0.03 (−0.09, 0.15) | 0.03 (−0.09, 0.15) | −0.05 (0.17, 0.07) | −0.04 (−0.16, 0.08) | −0.02 (−0.14, 0.11) | −0.01 (−0.14, 0.11) |
| MBzP | −0.02 (−0.14, 0.10) | 0.01 (−0.11, 0.13) | −0.02 (−0.14, 0.10) | −0.02 (−0.14, 0.10) | 0.00 (−0.11, 0.11) | 0.01 (−0.10, 0.12) | 0.06 (−0.05, 0.18) | 0.05 (−0.06, 0.17) | −0.04 (−0.16, 0.08) | −0.05 (−0.16, 0.07) | −0.01 (−0.12, 0.10) | 0.00 (−0.12, 0.12) |
| MCNP | 0.14 (−0.03, 0.30) | 0.14 (−0.02, 0.31) | 0.03 (−0.14, 0.19) | 0.07 (−0.10, 0.24) | 0.19 (0.03, 0.35)* | 0.12 (−0.04, 0.28) | 0.15 (−0.01, 0.31) | 0.18 (0.01, 0.34)* | 0.11 (−0.05, 0.28) | 0.12 (−0.04, 0.30) | 0.17 (0.01, 0.34)* | 0.20 (0.03, 0.37)* |
| MCOP | 0.12 (0.01, 0.24)* | 0.11 (−0.01, 0.23) | 0.05 (−0.06, 0.17) | 0.08 (−0.04, 0.20) | 0.12 (0.00, 0.23)* | 0.07 (−0.04, 0.19) | 0.07 (−0.04, 0.19) | 0.10 (−0.02, 0.22) | 0.06 (−0.06, 0.17) | 0.07 (−0.05, 0.19) | 0.12 (0.00, 0.24)* | 0.14 (0.02, 0.26)* |
| MCPP | −0.03 (−0.16, 0.09) | −0.03 (−0.016, 0.09) | −0.06 (−0.18, 0.06) | −0.06 (−0.18, 0.07) | 0.02 (−0.10, 0.14) | 0.00 (−0.12, 0.11) | −0.04 (−0.16, 0.09) | −0.03 (−0.15, 0.09) | 0.00 (−0.13, 0.11) | 0.00 (−0.13, 0.12) | −0.05 (−0.17, 0.07) | −0.05 (−0.17, 0.08) |
| MEP | 0.01 (−0.07, 0.10) | 0.02 (−0.06, 0.10) | 0.00 (−0.08, 0.08) | 0.01 (−0.08, 0.09) | 0.05 (−0.03, 0.12) | 0.04 (−0.03, 0.12) | 0.03 (−0.05, 0.12) | 0.04 (0.04, 0.12) | −0.02 (−0.10, 0.06) | −0.02 (−0.10, 0.07) | 0.02 (−0.07, 0.10) | 0.02 (−0.06, 0.10) |
| Σ Plastic | 0.06 (−0.07, 0.18) | 0.08 (−0.04, 0.20) | 0.08 (−0.03, 0.20) | 0.09 (−0.03, 0.22) | 0.08 (−0.04, 0.19) | 0.08 (−0.04, 0.19) | 0.13 (0.01, 0.25)* | 0.12 (0.01, 0.25)* | 0.07 (−0.05, 0.19) | 0.07 (−0.05, 0.19) | 0.13 (0.01, 025)* | 0.14 (0.02, 0.26)* |
| Σ AA | 0.03 (−0.10, 0.16) | 0.04 (−0.09, 0.18) | 0.07 (−0.06, 0.20) | 0.08 (−0.06, 0.21) | 0.01 (−0.01, 0.23) | 0.10 (−0.02, 0.22) | 0.13 (0.00, 0.26)* | 0.13 (0.01, 0.26)* | 0.01 (−0.012, 0.14) | 0.01 (−0.12, 0.14) | 0.10 (−0.03, 0.23) | 0.11 (−0.03, 0.24) |
| Σ PCP | 0.01 (−0.10, 0.12) | 0.01 (−0.10, 0.12) | 0.02 (−0.10, 0.12) | 0.02 (−0.09, 0.13) | 0.09 (−0.02, 0.19) | 0.07 (−0.03, 0.17) | 0.07 (−0.03, 0.18) | 0.07 (−0.03, 0.18) | −0.03 (−0.13, 0.08) | −0.02 (−0.13, 0.08) | 0.03 (−0.07, 0.14) | 0.04 (−0.07, 0.15) |
| 2,4 DCP | 0.06 (−0.02, 0.13) | 0.05 (−0.02, 0.13) | −0.02 (−0.10, 0.05) | −0.02 (−0.10, 0.05) | 0.06 (−0.01, 0.14) | 0.05 (−0.02, 0.12) | 0.04 (−0.03, 0.12) | 0.04 (0.03, 0.12) | 0.03 (−0.04, 0.11) | 0.03 (−0.04, 0.11) | 0.05 (−0.03, 0.12) | 0.04 (−0.03, 0.12) |
| 2,5 DCP | 0.08 (0.02, 0.14)* | 0.07 (0.00, 0.13)* | 0.00 (−0.06, 0.06) | 0.00 (−0.06, 0.07) | 0.07 (0.01, 0.13)* | 0.06 (0.00, 0.12)* | 0.04 (−0.02, 010) | 0.04 (−0.02, 0.10) | 0.02 (−0.04, 0.08) | 0.03 (−0.03, 0.09) | 0.06 (−0.01, 0.12) | 0.06 (0.00, 0.12) |
| BP3 | 0.05 (−0.02, 0.11) | 0.03 (−0.04, 0.09) | 0.03 (−0.04, 0.09) | 0.01 (−0.06, 0.07) | 0.00 (−0.06, 0.06) | 0.01 (−0.05, 0.07) | 0.05 (−0.01, 0.12) | 0.04 (−0.02, 0.11) | −0.03 (−0.10, 0.03) | −0.01 (−0.08, 0.06) | 0.04 (−0.03, 0.10) | 0.02 (−0.04, 0.09) |
| BPA | 0.03 (−0.11, 0.18) | 0.00 (−0.14, 0.14) | 0.12 (−0.01, 0.26) | 0.11 (−0.02, 0.26) | 0.09 (−0.04, 0.23) | 0.07 (−0.06, 0.20) | 0.16 (0.02, 0.29)* | 0.16 (0.02, 0.30)* | −0.07 (−0.21, 0.07) | −0.03 (−0.17, 0.11) | 0.10 (−0.04, 0.24) | 0.10 (−0.05, 0.24) |
| triclosan | 0.02 (−0.03, 0.78) | 0.01 (−0.04, 0.07) | −0.01 (−0.07, 0.04) | −0.01 (−0.07, 0.04) | 0.00 (−0.05, 0.06) | 0.00 (−0.05, 0.05) | −0.02 (−0.07, 0.03) | −0.02 (0.08, 0.03) | 0.01 (−0.04, 0.06) | 0.01 (−0.04, 0.07) | 0.00 (0.05, 0.06) | 0.00 (−0.06, 0.05) |
| ethyl paraben | 0.05 (−0.01, 0.12) | 0.03 (−0.04, 0.10) | 0.02 (−0.05, 0.08) | 0.01 (−0.05, 0.08) | 0.05 (−0.10, 0.11) | 0.02 (−0.04, 0.09) | 0.07 (0.00, 0.13)* | 0.07 (0.01, 0.13)* | −0.04 (−0.10, 0.03) | −0.03 (−0.09, 0.04) | 0.04 (−0.02, 0.11) | 0.03 (−0.03, 0.10) |
| methyl paraben | 0.01 (−0.05, 0.07) | 0.00 (−0.06, 0.05) | −0.02 (−0.09, 0.04) | −0.03 (−0.09, 0.03) | 0.06 (0.00, 0.12) | 0.05 (−0.01, 0.11) | 0.00 (−0.05, 0.06) | 0.01 (−0.05, 0.07) | −0.03 (−0.09, 0.03) | −0.02 (−0.08, 0.04) | 0.00 (−0.07, 0.05) | −0.01 (−0.07, 0.05) |
| propyl paraben | 0.03 (−0.02, 0.08) | 0.00 (−0.05, 0.05) | −0.02 (−0.07, 0.03) | −0.03 (−0.08, 0.02) | 0.00 (−0.04, 0.05) | 0.01 (−0.04, 0.06) | −0.01 (−0.06, 0.04) | 0.00 (0.05, 0.04) | −0.03 (−0.07, 0.02) | −0.02 (−0.07, 0.03) | −0.01 (−0.06, 0.04) | −0.02 (−0.07, 0.04) |
Average blood pressure: (SBP + DBP/2)
Lipids ratio: TG/HDL-c
Model 1: adjusted for specific gravity only; Model 2: adjusted for specific gravity, sex, age group, puberty status, smoking behavior, alcohol intake behavior, physical activity level, screen time
P < 0.05
P < 0.01.
Table 5.
Sex-stratified adjusted linear regression of associations between ln-transformed urinary EDCs by metabolic outcomes (N = 344).
| Waist circumference z-score β (95% CI) | Insulin z-score β (95% CI) | Average blood pressure (Tarokh et al., 2019) z-score β (95% CI) | Lipids ratio (Rodriguez et al., 2004) z-score β (95% CI) | Fasting glucose z-score β (95% CI) | MetS risk z-score β (95% CI) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Males | Females | Males | Females | Males | Females | Males | Females | Males | Females | Males | Females | |
| Σ DEHP | 0.03 (−0.16, 0.21) | 0.15 (−0.02, 0.33) | 0.09 (−0.05, 0.23) | 0.07 (−0.14, 0.27) | 0.01 (−0.17, 0.17) | 0.09 (−0.06, 0.25) | 0.21 (0.04, 0.37)* | 0.04 (−0.15, 0.22) | 0.10 (−0.09, 0.29) | 0.04 (−0.13, 0.21) | 0.16 (−0.02, 0.33) | 0.11 (−0.06, 0.30) |
| MEHP | −0.14 (−0.31, 0.04) | 0.12 (−0.06, 0.31) | 0.03 (−0.10, 0.17) | 0.02 (−0.19, 0.24) | −0.07 (−0.23, 0.10) | 0.08 (−0.09, 0.25) | 0.12 (−0.04, 0.27) | 0.03 (−0.16, 0.23) | 0.03 (−0.15, 0.21) | 0.08 (−0.10, 0.26) | 0.01 (−0.16, 0.18) | 0.10 (−0.09, 0.29) |
| MEHHP | 0.03 (−0.15, 0.21) | 0.14 (−0.02, 0.31) | 0.08 (−0.06, 0.21) | 0.08 (−0.11, 0.27) | 0.01 (−0.16, 0.18) | 0.07 (−0.08, 0.22) | 0.20 (0.05, 0.36)* | 0.04 (−0.14, 0.21) | 0.11 (−0.07, 0.29) | 0.01 (−0.15, 0.16) | 0.15 (−0.02, 0.32) | 0.10 (−0.07, 0.27) |
| MECPP | 0.04 (−0.14, 0.22) | 0.16 (−0.01, 0.33) | 0.11 (−0.03, 0.25) | 0.06 (−0.15, 0.26) | 0.00 (−0.17, 0.17) | 0.11 (−0.04, 0.27) | 0.20 (0.04, 0.36)** | 0.04 (−0.15, 0.22) | 0.11 (−0.08, 0.30) | 0.06 (−0.11, 0.23) | 0.17 (−0.01, 0.34) | 0.13 (−0.05, 0.31) |
| MEOHP | 0.02 (−0.16, 0.20) | 0.10 (−0.06, 0.27) | 0.07 (−0.07, 0.21) | 0.06 (−0.13, 0.25) | 0.00 (−0.17, 0.17) | 0.06 (−0.09, 0.21) | 0.20 (0.04, 0.35)** | 0.01 (−0.16, 0.19) | 0.08 (−0.10, 0.26) | 0.02 (−0.14, 0.18) | 0.13 (−0.04, 0.30) | 0.08 (−0.09, 0.25) |
| Σ DBP | 0.00 (−0.22, 0.22) | −0.04 (−0.22, 0.14) | 0.05 (−0.12, 0.22) | −0.02 (−0.24, 0.19) | 0.11 (−0.10, 0.32) | −0.06 (−0.23, 0.10) | 0.16 (−0.04, 0.35) | −0.01 (−0.20, 0.20) | −0.07 (−0.30, 0.15) | −0.04 (−0.22, 0.14) | 0.06 (−0.16, 0.27) | −0.04 (−0.23, 0.14) |
| MBP | 0.00 (−0.21, 0.21) | −0.05 (−0.23, 0.13) | 0.04 (−0.12, 0.20) | −0.01 (−0.22, 0.20) | 0.11 (−0.09, 0.30) | −0.06 (−0.22, 0.10) | 0.15 (−0.04, 0.33) | 0.00 (−0.19, 0.19) | −0.07 (−0.28, 0.14) | −0.05 (−0.22, 0.13) | 0.05 (−0.15, 0.25) | −0.04 (−0.23, 0.14) |
| MiBP | −0.06 (−0.29, 0.17) | 0.02 (−0.14, 0.18) | −0.04 (−0.21, 0.14) | −0.04 (−0.23, 0.15) | −0.08 (−0.29, 0.13) | −0.06 (−0.20, 0.09) | 0.03 (−0.17, 0.24) | 0.00 (−0.18, 0.17) | −0.08 (−0.31, 0.15) | −0.03 (−0.19, 0.13) | −0.06 (−0.28, 0.16) | −0.02 (−0.19, 0.14) |
| MBzP | −0.04 (−0.23, 0.15) | 0.02 (−0.15, 0.18) | 0.03 (−0.12, 0.19) | −0.08 (−0.27, 0.10) | 0.02 (−0.16, 0.20) | −0.04 (−0.19, 0.10) | 0.04 (−0.13, 0.21) | 0.06 (−0.11, 0.23) | 0.00 (−0.20, 0.19) | −0.08 (−0.23, 0.08) | 0.01 (−0.18, 0.20) | −0.04 (−0.20, 0.13) |
| MCNP | −0.11 (−0.19, 0.42) | 0.16 (−0.08, 0.39) | 0.07 (−0.17, 0.32) | 0.05 (−0.23, 0.33) | 0.15 (−0.15, 0.43) | 0.00 (−0.22, 0.20) | 0.19 (−0.08, 0.46) | 0.14 (−0.10, 0.40) | 0.13 (−0.18, 0.43) | 0.17 (−0.06, 0.40) | 0.20 (−0.10, 0.49) | 0.19 (−0.06, 0.43) |
| MCOP | −0.04 (−0.18, 0.25) | 0.15 (−0.01, 0.31) | 0.08 (−0.09, 0.25) | 0.05 (−0.14, 0.24) | 0.02 (−0.18, 0.22) | 0.06 (−0.08, 0.21) | 0.09 (−0.10, 0.28) | 0.09 (−0.08, 0.26) | 0.17 (−0.04, 0.39) | 0.02 (−0.14, 0.18) | 0.14 (−0.07, 0.35) | 0.12 (−0.05, 0.29) |
| MCPP | −0.09 (−0.32, 0.14) | −0.05 (−0.21, 0.12) | −0.01 (−0.19, 0.17) | −0.15 (−0.36, 0.05) | −0.07 (−0.29, 0.14) | −0.05 (−0.21, 0.09) | −0.09 (−0.30, 0.11) | −0.05 (−0.23, 0.13) | −0.02 (−0.25, 0.22) | 0.00 (−0.17, 0.16) | −0.09 (−0.31, 0.14) | −0.10 (−0.27, 0.08) |
| MEP | −0.05 (−0.17, 0.08) | 0.08 (−0.04, 0.19) | −0.02 (−0.11, 0.08) | 0.02 (−0.11, 0.16) | 0.03 (−0.08, 0.15) | 0.04 (−0.07, 0.14) | −0.03 (−0.14, 0.09) | 0.09 (−0.03, 0.21) | −0.01 (−0.14, 0.11) | −0.02 (−0.13, 0.09) | −0.04 (−0.16, 0.09) | 0.06 (−0.05, 0.18) |
| Σ Plastic | 0.02 (−0.17, 0.21) | 0.15 (−0.03, 0.33) | 00.09 (−0.06, 0.24) | 0.05 (−0.16, 0.26) | 0.01 (−0.17, 0.19) | 0.09 (−0.07, 0.25) | 0.22 (−0.05, 0.39)** | 0.04 (−0.15, 0.23) | 0.11 (−0.08, 0.30) | 0.03 (−0.15, 0.20) | 0.16 (−0.02, 0.35) | 0.11 (−0.08, 0.29) |
| Σ AA | −0.01 (−0.23, 0.21) | 0.08 (−0.12, 0.27) | 0.11 (−0.06, 0.28) | 0.02 (−0.21, 0.25) | 0.10 (−0.10, 0.31) | 0.02 (−0.16, 0.20) | 0.27 (0.07, 0.46)** | 0.02 (−0.19, 0.23) | 0.04 (−0.19, 0.26) | −0.02 (−0.21, 0.17) | 0.16 (−0.06, 0.37) | 0.04 (−0.17, 0.24) |
| Σ PCP | −0.06 (−0.23, 0.10) | 0.06 (−0.10, 0.22) | 0.01 (−0.12, 0.14) | 0.01 (−0.17, 0.20) | 0.08 (−0.08, 0.24) | 0.02 (−0.12, 0.16) | 0.11 (−0.12, 0.17) | 0.09 (−0.07, 0.26) | −0.05 (−0.21, 0.12) | 0.00 (−0.15, 0.14) | 0.02 (−0.18, 0.15) | 0.06 (−0.10, 0.22) |
| 2,4 DCP | 0.05 (−0.07, 0.17) | 0.07 (−0.04, 0.17) | −0.02 (−0.12, 0.07) | −0.02 (−0.15, 0.10) | 0.04 (−0.08, 0.15) | 0.04 (−0.05, 0.14) | 0.06 (−0.05, 0.17) | 0.01 (−0.11, 0.12) | 0.03 (−0.09, 0.15) | 0.03 (−0.07, 0.13) | 0.05 (−0.07, 0.16) | 0.03 (−0.07, 0.14) |
| 2,5 DCP | 0.05 (−0.05, 0.14) | 0.09 (0.01, 0.18)* | 0.00 (−0.07, 0.08) | 0.01 (−0.09, 0.11) | 0.04 (−0.04, 0.13) | 0.06 (−0.01, 0.14) | 0.07 (−0.02, 0.15) | 0.00 (−0.09, 0.09) | 0.03 (−0.06, 0.13) | 0.03 (−0.06, 0.11) | 0.06 (−0.03, 0.15) | 0.05 (−0.04, 0.14) |
| BP3 | 0.04 (−0.06, 0.14) | 0.02 (−0.08, 0.11) | −0.04 (−0.12, 0.04) | 0.04 (−0.07, 0.14) | 0.03 (−0.07, 0.13) | −0.03 (−0.11, 0.05) | 0.03 (−0.06, 0.12) | 0.04 (−0.05, 0.14) | −0.02 (−012, 0.09) | −0.02 (−0.10, 0.07) | 0.01 (−0.09, 0.11) | 0.03 (−0.07, 0.12) |
| BPA | −0.05 (−0.27, 0.18) | 0.02 (−0.17, 0.22) | 0.07 (−0.10, 0.25) | 0.15 (−0.08, 0.38) | 0.04 (−0.17, 0.25) | 0.04 (−0.14, 0.22) | 0.03 (−0.17, 0.23) | 0.24 (0.03, 0.44)* | −0.12 (−0.35, 0.11) | 0.01 (−0.18, 0.20) | −0.02 (−0.24, 0.20) | 0.16 (−0.05, 0.36) |
| triclosan | −0.02 (−0.10, 0.07) | 0.04 (−0.04, 0.11) | −0.05 (−0.12, 0.02) | 0.02 (−0.06, 0.11) | −0.03 (−0.11, 0.05) | 0.00 (−0.06, 0.07) | 0.08 (−0.15, 0.01) | 0.04 (−0.05, 0.12) | 0.00 (−0.08, 0.08) | 0.02 (−0.06, 0.09) | −0.06 (−0.14, 0.03) | 0.04 (−0.04, 0.12) |
| ethyl paraben | 0.02 (−0.07, 0.12) | 0.02 (−0.08, 0.12) | 0.02 (−0.06, 0.09) | 0.01 (−0.11, 0.13) | 0.03 (−0.06, 0.12) | 0.00 (−0.09, 0.09) | 0.07 (−0.01, 0.16) | 0.05 (−0.05, 0.16) | 0.03 (−0.07, 0.13) | −0.08 (−0.17, 0.02) | 0.06 (−0.04, 0.15) | 0.00 (−0.10, 0.10) |
| methyl paraben | −0.02 (−0.11, 0.07) | 0.00 (−0.08, 0.09) | −0.03 (−0.10, 0.04) | −0.03 (−0.14, 0.07) | 0.07 (−0.02, 0.15) | 0.03 (−0.05, 0.11) | 0.00 (−0.08, 0.08) | 0.03 (−0.06, 0.13) | 0.02 (−0.07, 0.11) | −0.05 (−0.13, 0.04) | 0.00 (−0.10, 0.08) | −0.01 (−0.10, 0.08) |
| propyl paraben | 0.00 (−0.08, 0.07) | 0.02 (−0.06, 0.09) | 0.00 (−0.06, 0.06) | −0.05 (−0.13, 0.04) | 0.05 (−0.03, 0.12) | −0.02 (−0.08, 0.05) | 0.02 (−0.04, 0.09) | −0.03 (−0.10, 0.05) | −0.03 (−0.11, 0.05) | 0.00 (0.07, 0.08) | 0.00 (−0.08, 0.08) | −0.02 (−0.09, 0.05) |
Average blood pressure: (SBP + DBP/2)
Lipids ratio: TG/HDL-c
All effect estimates from models adjusted for specific gravity, age group, puberty status, smoking behavior, alcohol intake behavior, physical activity level, screen time
P < 0.05
P < 0.01.
3.1. Waist circumference z-score
After adjusting for confounding variables, we observed an association between 2,5 DCP and waist circumference z-score [β = 0.07 (95% CI: 0.00, 0.13; p < 0.05)] among the unstratified sample (Table 4). However, when we stratified by sex, 2,5 DCP was positively associated with a higher female waist circumference z-score [β = 0.09 (95% CI: 0.01, 0.18); p < 0.05)] (Table 5). Although not statistically significant, we observed a positive association between DEHP and DEHP metabolites with waist circumference z-scores. For example, each log unit increase in the sum DEHP was associated with a 0.15 (95% CI: 0.02, 0.33) higher female waist circumference z-score, while associations between waist circumference with MEHP [β = 0.12 (95% CI: 0.06, 0.31)], MEHHP [β = 0.14 (95% CI: 0.02, 0.31)], MECPP [β = 0.16 (95% CI: 0.01, 0.33)] and MEOHP [β = 0.10 (95% CI: 0.06, 0.27)] was also associated in the same direction for female adolescents. No statistically significant associations were observed among male adolescents.
3.2. Insulin z-score
Among the unstratified sample, no significant associations were observed between exposure to EDCs and insulin z-scores before or after adjustment for confounders (Table 4), nor were any significant associations observed between toxicants and insulin z-scores after sex stratification (Table 5).
3.3. Average blood pressure z-score
After adjusting for confounding variables, we observed a significant association between 2,5 DCP and blood pressure z-score [β = 0.06 (95% CI:0.00, 0.12; p < 0.05)] among the unstratified sample (Table 4). No significant associations were observed between toxicants and blood pressure z-scores after sex stratification (Table 5).
3.4. Lipids ratio z-score
Among the unstratified sample, several positive associations were observed between EDCs and lipid z-scores before and after adjusting for confounders. Notably, we found that multiple phthalates (Σ DEHP, MEHHP, MECPP, MCNP, Σ Plastic, and Σ AA), one phenol (BPA), and one paraben (methyl paraben) were associated with the lipid z-scores. To illustrate, for each 1-unit increase in log Σ DEHP, MEHHP, and MECPP, there was a 0.12 unit [β = 0.12 (95% CI: 0.01, 0.24; p < 0.05)], 0.13 unit [β = 0.13 (95% CI: 0.01, 0.25; p < 0.05)] and 0.14 unit [β = 0.14 (95% CI: 0.01, 0.26; p < 0.05)] increase in the lipids ratio z-score (Table 4). We observed several differences when we stratified by sex (Table 5). To illustrate, among males, Σ DEHP was positively associated with the lipids ratio z-score [β = 0.21 (95% CI: 0.04, 0.37; p < 0.01)]. DEHP metabolites, including MEHHP [β = 0.20 (95% CI: 0.05, 0.36; p < 0.01)], MECPP [β = 0.20 (95% CI: 0.04 0.36, p < 0.01)], and MEOHP [β = 0.20 (95% CI: 0.05, 0.35; p < 0.01)], were positively associated with increased lipids ratio z-scores of male adolescents. For other summary phthalate measures, the findings also revealed positive associations between each 1-unit log increase in Σ Plastic [β = 0.22 (95% CI: 0.05, 0.39; p < 0.01)] and Σ AA [β = 0.27 (95% CI: 0.07, 0.46; p < 0.01)] with male lipids ratio z-scores. BPA was positively associated with female lipids ratio z-scores [β = 0.24 (95% CI: 0.03, 0.44; p < 0.05)] (Table 5).
3.5. Fasting glucose z-score
Among the unstratified sample, no significant associations were observed between exposure to EDCs and fasting glucose z-scores before or after adjustment for confounders (Table 4). No significant associations were observed between toxicants and fasting glucose z-scores after sex stratification (Table 5).
3.6. MetS risk z-score
Results among the unstratified sample revealed multiple significant positive associations between summary phthalate measures and phthalate metabolites with MetS risk z-scores before and after adjustment for confounding variables. Σ DEHP and its metabolites MEHHP and MECPP were associated with MetS risk z-scores ranging from 0.13 to 0.15. Finally, one summary phthalate and two phthalate metabolites were positively associated with the MetS risk z-score, including Σ Plastic [β = 0.14 (95% CI: 0.02, 0.26; p < 0.05)], MCNP [β = 0.20 (95% CI: 0.03, 0.37; p < 0.05)], and MCOP [β = 0.14 (95% CI: 0.02, 0.26; p < 0.05)] (Table 4). Although various EDCs were positively associated with MetS risk z-score in the unstratified sample, none of the associations were statistically significant after stratification by adolescent sex (Table 5).
3.7. Adjustment for multiple comparisons
After adjusting for multiple comparisons using the FDR test, results revealed that none of the associations met the FDR correction p-value for statistical significance (Supplemental Table 3).
3.8. Nonlinear regression results
Results from post-hoc analyses of adjusted nonlinear regression analyses among the unstratified sample revealed several nonmonotonic associations for select EDCs. For example, the second tertile (β = 0.27; 95% CI: 0.01, 0.53; p = 0.0474) of adolescent MEHP urinary concentration was significantly associated with lipids ratio z-score compared to the first (reference group), while the third tertile showed no difference [β = 0.07 (95% CI: 0.20, 0.34)] (p, trend = 0.0445) (Supplemental Table 4). We also found that for BP3, the third tertile [β = 0.27 (95% CI: 0.01, 0.54; p = 0.0432)] was associated with higher lipids ratio z-score compared to the first tertile (p, trend = 0.0158). For insulin z-scores, we observed nonmonotonic associations between the second tertile [β = 0.32 (95% CI: 0.05, 0.60; p = 0.0224)] of 2,5 DCP compared to the first tertile, while the third tertile showed no difference. In addition, nonmonotonic associations were observed between the second tertile [β = 0.34 (95% CI: 0.07, 0.60; p = 0.0120)] of BPA with insulin z-score compared to the first tertile (p, trend = 0.0408).
Results from sex-stratified models among male adolescents did not provide evidence of nonmonotonic associations (Supplemental Table 5). However, among female adolescents, we observed U-shaped curve associations between Σ DEHP with average blood pressure and fasting glucose z-scores (Supplemental Table 6). We observed a similar U-shaped association between MEHHP with average blood pressure z-score and MECPP and fasting glucose z-score (p, trend = 0.0079). We also observed a few inverted U-shape associations among female adolescents, for example, between 2,5 DCP with lipids ratio and MetS risk z-scores and between 2,4 DCP with lipids ratio z-score.
3.9. Informal mediation analysis results
Results from the unstratified informal mediation revealed that when progesterone and testosterone hormone was added as a covariate to the unadjusted regression models for the unstratified sample, there was no evidence of mediation by progesterone or testosterone for 1) the association between summary phthalate measures, DEHP metabolites and DBP metabolites and lipids ratio z-score nor evidence of progesterone or testosterone mediation for 2) the association between summary phthalate measures, DEHP metabolites and DBP metabolites with MetS risk z-score (Supplemental Table 7). In addition, results from sex-stratified informal mediation analysis demonstrated that progesterone (for females) and testosterone (for males) did not mediate associations between EDCs withlipids ratio or MetS risk z-scores (Supplemental Table 8). Models adjusted for potential confounders revealed no significant associations (data not shown).
4. Discussion
The main objectives of the present study were to investigate cross-sectional relationships between urinary summary phthalate measures, phthalate metabolites, phenols, and paraben analytes with MetS risk among Mexican youth in early-to-mid-adolescence. From linear regression models, unstratified results demonstrated positive associations between higher exposure to phthalates and phenols with lipids, waist circumference, blood pressure, and overall MetS risk z-scores among Mexican youth. Moreover, sex-stratified results revealed that some associations differed by sex. Among males, we found positive associations between higher exposures to mixtures of phthalates, as well as individual phthalate metabolites, with lipid z-scores, while for female adolescents, we observed positive associations between phenol metabolites and waist circumference and lipids ratio z-scores. No significant associations were observed between parabens and MetS risk components in either sex group. Nonlinear models demonstrated mostly dose-response associations between EDCs and metabolic markers in the unstratified and sex-stratified samples. Albeit a few toxicants were nonmonotonically associated (i.e., U-shaped or inverted U-shaped curve) with select metabolic markers, such as average blood pressure, glucose, and lipids ratio z-scores among adolescent females.
The present study found associations between EDCs and overall MetS risk as well as with individual MetS risk components in the unstratified sample. Considering overall MetS risk, multiple phthalates were positively associated with MetS risk z-score in the unstratified adolescent sample. These findings align with studies that have demonstrated positive associations between phthalate exposure and metabolic syndrome risk among adult populations (Radke et al., 2019; James-Todd et al., 2016; Zamora et al., 2021). Previous studies have also offered potential explanations for the effects of phthalate, phenol, and paraben exposure on metabolic health by elucidating the mechanisms by which these toxicants interfere with hormone homeostasis (Diamanti-Kandarakis et al., 2009). For example, EDCs compete with endogenous steroid hormones that bind to receptors and hormone transport proteins or alter the metabolism or synthesis of endogenous hormones (Casals-Casas and Desvergne, 2011).
The examination of the individual MetS risk components provides more specificity on how the EDCs may alter MetS risk. Notably, we found that Σ DEHP, MEHHP, MECPP, MCNP, Σ Plastic, and Σ AA were positively associated with higher lipids ratio z-scores in the unstratified sample. Moreover, when we stratified by sex, we found that the associations between phthalates and lipids that remained statistically significant were among male adolescents, including for Σ DEHP, MEHHP, MECPP, MEOHP, Σ Plastic, and Σ AA, whereas one phenol metabolite (BPA) was positively associated with the female lipids ratio z-score. To our knowledge, no other studies have examined the relationship between concurrent phthalate exposure with the lipids ratio – which is a validated marker for IR, cardiometabolic risk, and cardiovascular disease in adolescent (Urbina et al., 2013; Salazar et al., 2014). However, various studies have examined other lipid biomarkers in relation to phthalate exposure. For example, a recent cross-sectional study among a sample of 16–19-year-old Chinese adolescents found that multiple phthalate metabolites (MECPP and Σ DEHP) were negatively associated with HDL-c levels and positively associated with TG levels (association not statistically significant) (Ding et al., 2021). This finding aligns with our results since they indicated that higher exposure to phthalate metabolites might affect lipid levels during adolescence. However, we caution against comparison due to cohort differences, including exposure levels between the two populations.
Moreover, a previous cross-sectional study conducted among a subsample of 248 ELEMENT adolescents showed that higher exposure to MCPP, MEP, and DBP was associated with lower total cholesterol and low-density lipoprotein cholesterol (LDL-c) levels, with sex-stratified findings showing that associations between Σ DEHP and lower LDL-c levels were significant among females only (Perng et al., 2017). These findings contradict our results, indicating that higher exposure to phthalates during early-to-mid-adolescence is associated with worse lipid profiles among males but not females. Our findings may differ for various reasons. For example, although we adjusted for pubertal status, studies have shown that during puberty, circulating lipid levels decrease (Mascarenhas et al., 2015; Eissa et al., 2016). Thus, differences in findings between the present study and the comparison study by Perng et al. (2017) could have been driven by pubertal status. This theory may also explain why the findings were sex-specific, with female adolescents at greater risk at a younger age, while male adolescents seemed to be at a greater risk at an older age (i.e., likely post-puberty). The present sexually dimorphic results indicate that phthalate exposure may affect lipid metabolism in male adolescents by increasing serum TGs and reducing HDL-c levels.
In the present study, we found evidence supporting a positive association between a phenol metabolite (2,5 DCP) and waist circumference that was specific to females. A recently published study by Gajjar et al. found inverse associations between exposure to BPA during childhood and childhood body fat, as well as an inverse association between childhood exposure and adolescent body fat levels (prospective), while urinary BPS concentrations were positively associated with percent body fat at age eight years, but not at 12 years; Gajjar et al. did not find evidence of sex-differences (Gajjar et al., 2021). We posit that discrepancies are due to various factors, including the fact that 2,5 DCP and bisphenols are different chemicals. Importantly, the comparative study did not examine associations with 2,5 DCP, a metabolite that remains pervasive in the environment.
Study results also demonstrated that one phenol metabolite (2,5 DCP) was associated with an increased blood pressure z-score in the unstratified sample. The link between increased exposure to phenols and blood pressure has been documented in adult human epidemiological (Bae et al., 2012; Jiang et al., 1987) and animal (Al Mansi et al., 2020), and mechanistic studies (Han and Hong, 2016). However, a study conducted among 12–15-year-old Turkish youth found no association between free and total BPA and blood pressure profiles (Yalçin et al., 2022). Differences between our study and the Turkish study are likely because 2,5 DCP is a phenol chemical structurally different from BPA or BPS. This finding may still indicate that 2,5 DCP is an emerging health threat, although it remains understudied. Although we found no significant associations between phthalates and blood pressure, a recent study conducted among Chinese children and youth found that urinary phthalates were dose-responsively related to elevated blood pressure and risk of hypertension, particularly for MEP, MECPP, and MEHHP (Liu et al., 2022). It is possible that the present study was underpowered to detect associations between phthalates and blood pressure. Moreover, the underlying mechanism by which exposure to EDCs, such as phthalates and phenols, may result in elevated blood pressure has been posited to be related to inflammation. For example, experimental studies have shown that in-vitro DEHP is associated with increased inflammatory cytokine levels within endothelial cells (Wang and Dong, 2012) and vascular smooth muscle cells (Shih et al., 2018), known to elevate blood pressure.
The present study found no evidence of a significant associations between exposure biomarkers with insulin and fasting glucose z-scores. Our findings are inconsistent with most of the existing literature on the relationship between EDCs and insulin levels (Trasande et al., 2013; Dong et al., 2018). For example, a study using NHANES 2009–2012 data examined the correlation between LMW and high-molecular-weight (HMW) phthalates and Σ DEHP, di-isodecyl phthalate (DIDP), and diisononyl phthalate (DINP), and IR in adolescents (Attina and Trasande, 2015). Adolescents classified as insulin-resistant had significantly higher concentrations of HMW, DEHP, and DINP metabolites (Attina and Trasande, 2015). In addition, a cross-sectional study among Iranian children and adolescents found a significant relationship between fasting blood glucose and MEHHP in the overall sample (Hashemi et al., 2021). However, this study did not stratify participants by developmental age group.
Although mostly dose-response associations were detected, a few U-shaped and inverted U-shaped relationships were observed between several metabolites and z-scores for metabolic markers (i.e., blood pressure, fasting glucose, and lipids ratio), in particular among female adolescents. Similar nonlinear relationships have been shown between toxicants, such as DEHP and blood pressure in Chinese children (Yao et al., 2020) and mice models (Mariana et al., 2018). Nonlinear relationships may be attributed to various biological factors. One plausible explanation is the saturation of the metabolic system at higher doses of the substance which may lead to an opposing effect compared to low concentrations (Lagarde et al., 2015).
We did not find evidence of informal mediation by progesterone or testosterone concentration in the unstratified and sex-stratified associations between summary phthalate measures, DBP and DEHP metabolites with lipids ratio, and MetS risk z-score. In contrast, previous studies have shown that hormones mediate associations between phthalates and metabolic health markers. For example, a recent study found that free T4 (i.e., thyroid hormone) levels mediate the effects of exposure to phthalates on insulin resistance in adults (Huang et al., 2021). Other studies have shown that phthalates are associated with hormones such as testosterone (Drake et al., 2009) and progesterone (Sheikh et al., 2016). Our findings may not align due to study design; in this report, we measured exposures, outcomes, and sex hormones at one-time point.
We utilized urinary biomarkers of toxicant exposure rather than relying on self-reported EDC exposure. Another strength was the larger sample size compared to many previous epidemiologic studies. In addition, this study is among the few to use an epidemiologic framework to examine sex-differences during a sensitive period for metabolic programming. This study also has some limitations. First, a causal relationship between exposure and outcomes could not be established because of the cross-sectional study design. The temporality of the associations could not be assessed using predictors and outcomes of interest simultaneously collected. Urinary phthalate metabolites were estimated from a single spot urine sample, and metabolic parameters were measured simultaneously. This may have resulted in random error and imprecise or biased study findings (Hutcheon et al., 2010). Multiple urine samples are required to estimate chronic exposure to EDCs. As with any epidemiological study, some unmeasured confounders, such as diet, may bias effect estimates obtained from regression models. Finally, other than running models for select summary phthalate measures, we did not apply other statistical approaches for multipollutant exposure, such as principal component analysis (PCA), which allows for the examination of cumulative effects for correlated groups of exposures.
5. Conclusions
Study findings revealed multiple positive links between phthalate and phenol exposure, lipids ratio, and MetS risk z-scores among Mexican adolescents. Given that none of the present study effect estimates met statistical significance after correcting for multiple comparisons, future studies with larger sample sizes are required to confirm study findings. In addition, future studies should examine the present questions using large-scale studies with a longitudinal design and repeated measures at multiple time points to test for underlying biological mechanisms.
Supplementary Material
Acknowledgments
We gratefully acknowledge the mothers and children who participated in the Early Life Exposure in Mexico to Environmental Toxicants (ELEMENT) and the American British Cowdray Medical Center (ABC) for providing facilities for this research.
Funding
This work was supported by the US Environmental Protection Agency [grant RD 83543601], National Institute of Environmental Health Sciences [grants: P01 ES02284401, P30 ES017885, R24 ES028502, and R24 ES028502 Supplement], and the National Heart, Lung, and Blood Institute [grant K01 HL151673]. This study was also supported and partially funded by the National Institute of Public Health/Ministry of Health of Mexico. The funding sources were not involved in the study design; collection, analysis, or interpretation of the data; writing of the report; or decision to submit the article for publication.
Footnotes
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
CRediT authorship contribution statement
Astrid N. Zamora: Conceptualization, Methodology, Software, Data curation, Formal analysis, Visualization, Writing – original draft, Writing – review & editing. Erica C. Jansen: Supervision, Methodology, Project administration, Resources, Funding acquisition, Writing – review & editing. Jaclyn M. Goodrich: Methodology, Writing – review & editing. Martha M. Téllez-Rojo: Methodology, Resources, Project administration, Funding acquisition, Writing – review & editing. Peter X.K. Song: Methodology, Writing – review & editing. John D. Meeker: Methodology, Writing – review & editing. Dana C. Dolinoy: Methodology, Writing – review & editing. Libni A.Torres-Olascoaga: Investigation, Project administration, Writing – review & editing. Alejandra Cantoral: Investigation, Resources, Writing – review & editing. Karen E. Peterson: Supervision, Methodology, Project administration, Resources, Funding acquisition, Writing – review & editing.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envres.2023.116706.
Data availability
Data will be made available on request.
References
- Al Mansi MH, Chuang Y, MohanKumar PS, MohanKumar SMJ, 2020. SAT-719 prenatal exposure to bisphenol A, S and F increases blood pressure in female rats. J Endocr Soc 4 (Suppl. ment_1). 10.1210/jendso/bvaa046.1864. SAT–719. [DOI] [Google Scholar]
- Ashrap P, Sánchez BN, Téllez-Rojo MM, et al. , 2019. In utero and peripubertal metals exposure in relation to reproductive hormones and sexual maturation and progression among girls in Mexico City. Environ. Res. 177, 108630 10.1016/j.envres.2019.108630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asociación Mexicana de Agencias de Inteligencia de Mercado Opinión (AMAI), y, 2018. Avances del Comité de Niveles Socioeconómicos. Comité de Niveles Socioeconómicos. http://www.amai.org/nse/wp-content/uploads/2018/04/Nota-Metodolo%CC%81gico-NSE-2018-v3.pdf. [Google Scholar]
- Attina TM, Trasande L, 2015. Association of exposure to di-2-ethylhexylphthalate replacements with increased insulin resistance in adolescents from NHANES 2009–2012. J. Clin. Endocrinol. Metab. 100 (7), 2640–2650. 10.1210/jc.2015-1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bae S, Kim JH, Lim YH, Park HY, Hong YC, 2012. Associations of bisphenol A exposure with Heart rate variability and blood pressure. Hypertension 60 (3), 786–793. 10.1161/HYPERTENSIONAHA.112.197715. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA, 1986. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 51 (6), 1173–1182. 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Benjamini Y, Hochberg Y, 1995. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B Methodol 57 (1), 289–300. 10.1111/j.2517-6161.1995.tb02031.x. [DOI] [Google Scholar]
- Buttke DE, Sircar K, Martin C, 2012. Exposures to endocrine-disrupting chemicals and age of menarche in adolescent girls in NHANES (2003–2008). Environ. Health Perspect. 120 (11), 1613–1618. 10.1289/ehp.1104748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson MJ, Thiel KW, Yang S, Leslie KK, 2012. Catch it before it kills: progesterone, obesity, and the prevention of endometrial cancer. Discov. Med. 14 (76), 215–222. [PMC free article] [PubMed] [Google Scholar]
- Casals-Casas C, Desvergne B, 2011. Endocrine disruptors: from endocrine to metabolic disruption. Annu. Rev. Physiol. 73 (1), 135–162. 10.1146/annurev-physiol-012110-142200. [DOI] [PubMed] [Google Scholar]
- Cathey AL, Watkins DJ, Sanchez BN, et al. , 2020. Onset and tempo of sexual maturation is differentially associated with gestational phthalated exposure between boys and girls in a Mexico City birth cohort. Environ. Int. 136, 105469 10.1016/j.envint.2020.105469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandler JL, Brazendale K, Beets MW, Mealing BA, 2016. Classification of physical activity intensities using a wrist-worn accelerometer in 8–12-year-old children. Pediatr. Obes. 11 (2), 120–127. 10.1111/ijpo.12033. [DOI] [PubMed] [Google Scholar]
- Chang WH, Li SS, Wu MH, Pan HA, Lee CC, 2015. Phthalates might interfere with testicular function by reducing testosterone and insulin-like factor 3 levels. Hum. Reprod. 30 (11), 2658–2670. 10.1093/humrep/dev225. [DOI] [PubMed] [Google Scholar]
- Chavarro JE, Watkins DJ, Afeiche MC, et al. , 2017. Validity of self-assessed sexual maturation against physician assessments and hormone levels. J. Pediatr. 186, 172–178.e3. 10.1016/j.jpeds.2017.03.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou YC, Tzeng CR, 2021. The impact of phthalate on reproductive function in women with endometriosis. Reprod. Med. Biol. 20 (2), 159–168. 10.1002/rmb2.12364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamanti-Kandarakis E, Bourguignon JP, Giudice LC, et al. , 2009. Endocrine-disrupting chemicals: an endocrine society scientific statement. Endocr. Rev. 30 (4), 293–342. 10.1210/er.2009-0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding S, Qi W, Xu Q, et al. , 2021. Relationships between di-(2-ethylhexyl) phthalate exposure and lipid metabolism in adolescents: human data and experimental rat model analyses. Environ. Pollut. 286, 117570 10.1016/j.envpol.2021.117570. [DOI] [PubMed] [Google Scholar]
- Dong R, Chen J, Zheng J, et al. , 2018. The role of oxidative stress in cardiometabolic risk related to phthalate exposure in elderly diabetic patients from Shanghai. Environ. Int. 121, 340–348. 10.1016/j.envint.2018.09.028. [DOI] [PubMed] [Google Scholar]
- Drake AJ, van den Driesche S, Scott HM, Hutchison GR, Seckl JR, Sharpe RM, 2009. Glucocorticoids amplify dibutyl phthalate-induced disruption of testosterone production and male reproductive development. Endocrinology 150 (11), 5055–5064. 10.1210/en.2009-0700. [DOI] [PubMed] [Google Scholar]
- Eissa MA, Mihalopoulos NL, Holubkov R, Dai S, Labarthe DR, 2016. Changes in fasting lipids during puberty. J. Pediatr. 170, 199–205. 10.1016/j.jpeds.2015.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gajjar P, Liu Y, Li N, et al. , 2021. Associations of mid-childhood bisphenol A and bisphenol S exposure with mid-childhood and adolescent obesity. Environ. Epidemiol. 6 (1), e187. 10.1097/EE9.0000000000000187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaston SA, Tulve NS, 2019. Urinary phthalate metabolites and metabolic syndrome in U.S. adolescents: cross-sectional results from the National Health and Nutrition Examination Survey (2003–2014) data. Int. J. Hyg Environ. Health 222 (2), 195–204. 10.1016/j.ijheh.2018.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golestanzadeh M, Riahi R, Kelishadi R, 2019. Association of exposure to phthalates with cardiometabolic risk factors in children and adolescents: a systematic review and meta-analysis. Environ. Sci. Pollut. Res. 26 (35), 35670–35686. 10.1007/s11356-019-06589-7. [DOI] [PubMed] [Google Scholar]
- Grandjean P, Barouki R, Bellinger DC, et al. , 2015. Life-long implications of developmental exposure to environmental stressors: new perspectives. Endocrinology 156 (10), 3408–3415. 10.1210/en.2015-1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grün F, Blumberg B, 2006. Environmental obesogens: organotins and endocrine disruption via nuclear receptor signaling. Endocrinology 147 (6 Suppl. l), S50–S55. 10.1210/en.2005-1129. [DOI] [PubMed] [Google Scholar]
- Han C, Hong YC, 2016. Bisphenol A, hypertension, and cardiovascular diseases: epidemiological, laboratory, and clinical trial evidence. Curr. Hypertens. Rep. 18 (2), 11. 10.1007/s11906-015-0617-2. [DOI] [PubMed] [Google Scholar]
- Harley KG, Kogut K, Madrigal DS, et al. , 2016. Reducing phthalate, paraben, and phenol exposure from personal care products in adolescent girls: findings from the HERMOSA intervention study. Environ. Health Perspect. 124 (10), 1600–1607. 10.1289/ehp.1510514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hashemi M, Amin MM, Chavoshani A, Rafiei N, Ebrahimpour K, Kelishadi R, 2021. Relationship of urinary phthalate metabolites with cardiometabolic risk factors and oxidative stress markers in children and adolescents. J. Environ. Pub. Heal. 2021, e5514073 10.1155/2021/5514073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatcher KM, Smith RL, Chiang C, Li Z, Flaws JA, Mahoney MM, 2020. Associations of phthalate exposure and endogenous hormones with self-reported sleep disruptions: results from the Midlife Women’s Health Study. Menopause. 10.1097/GME.0000000000001614. Publish Ahead of Print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heindel JJ, Blumberg B, Cave M, et al. , 2017. Metabolism disrupting chemicals and metabolic disorders. Reprod. Toxicol. 68, 3–33. 10.1016/j.reprotox.2016.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernández B, Gortmaker SL, Parra-Cabrera S, 2000. Validez y reproducibilidad deun cuestionario de actividad e inactividad física para escolares de la ciudad de México. Salud Publica Mex 42 (4), 315–323. [PubMed] [Google Scholar]
- Hornung RW, Reed LD, 1990. Estimation of average concentration in the presence of nondetectable values. Appl. Occup. Environ. Hyg 5 (1), 46–51. 10.1080/1047322X.1990.10389587. [DOI] [Google Scholar]
- Huang HB, Siao CY, Lo YTC, Shih SF, Lu CH, Huang PC, 2021. Mediation effects of thyroid function in the associations between phthalate exposure and glucose metabolism in adults. Environ. Pollut. 278, 116799 10.1016/j.envpol.2021.116799. [DOI] [PubMed] [Google Scholar]
- Hutcheon JA, Chiolero A, Hanley JA, 2010. Random measurement error and regression dilution bias. BMJ 340, c2289. 10.1136/bmj.c2289. [DOI] [PubMed] [Google Scholar]
- James-Todd TM, Huang T, Seely EW, Saxena AR, 2016. The association between phthalates and metabolic syndrome: the national health and nutrition examination survey 2001–2010. Environ. Health 15 (1), 52. 10.1186/s12940-016-0136-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janesick A, Blumberg B, 2011. Endocrine disrupting chemicals and the developmental programming of adipogenesis and obesity. Birth Defects Res. Part C Embryo Today - Rev. 93 (1), 34–50. 10.1002/bdrc.20197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang S, Liu H, Zhou S, et al. , 1987. Association of bisphenol A and its alternatives bisphenol S and F exposure with hypertension and blood pressure: a cross-sectional study in China. Enviro.n Poll. Barking Essex. 257, 113639 10.1016/j.envpol.2019.113639, 2020. [DOI] [PubMed] [Google Scholar]
- Kalkhoff RK, 1982. Metabolic effects of progesterone. Am. J. Obstet. Gynecol. 142, 735–738. 10.1016/S0002-9378(16)32480-2, 6, Part 2. [DOI] [PubMed] [Google Scholar]
- Kassi E, Pervanidou P, Kaltsas G, Chrousos G, 2011. Metabolic syndrome: definitions and controversies. BMC Med. 9 (1), 48. 10.1186/1741-7015-9-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagarde F, Beausoleil C, Belcher SM, et al. , 2015. Non-monotonic dose-response relationships and endocrine disruptors: a qualitative method of assessment. Environ. Health 14 (1), 13. 10.1186/1476-069X-14-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis RC, Meeker JD, Peterson KE, et al. , 2013. Predictors of urinary bisphenol A and phthalate metabolite concentrations in Mexican children. Chemosphere 93 (10), 2390–2398. 10.1016/j.chemosphere.2013.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin CY, Hsieh CJ, Lo SC, et al. , 2016. Positive association between concentration of phthalate metabolites in urine and microparticles in adolescents and young adults. Environ. Int. 92–93, 157–164. 10.1016/j.envint.2016.04.006. [DOI] [PubMed] [Google Scholar]
- Liu M, Zhao L, Liu L, et al. , 2022. Phthalate mixture exposure is associated with elevated blood pressure in Chinese children: a panel study. Expo. Health. 10.1007/s12403-022-00471-7. [DOI] [Google Scholar]
- López Romo H, 2009. Nivel Socieconómico AMAI. AMAI. INEGI: Comparación de la distribución del nivel socioeconómico Índice AMAI con encuesta ingreso gasto INEG. http://intranet.iesmoda.edu.mx/docs/NivelSocioeconomicoAMAI.pdf.
- Mancini M, Pecori Giraldi F, Andreassi A, et al. , 2021. Obesity is strongly associated with low testosterone and reduced penis growth during development. J. Clin. Endocrinol. Metab. 106 (11), 3151–3159. 10.1210/clinem/dgab535. [DOI] [PubMed] [Google Scholar]
- Mariana M, Feiteiro J, Cairrao E, 2018. Cardiovascular response of rat aorta to di-(2-ethylhexyl) phthalate (DEHP) exposure. Cardiovasc. Toxicol. 18 (4), 356–364. 10.1007/s12012-017-9439-6. [DOI] [PubMed] [Google Scholar]
- Mascarenhas LPG, Leite N, Titski ACCK, Brito LMS, Boguszewski MCS, 2015. Variability of lipid and lipoprotein concentrations during puberty in Brazilian boys. J. Pediatr. Endocrinol. Metab. 28 (1–2), 125–131. 10.1515/jpem-2013-0450. [DOI] [PubMed] [Google Scholar]
- Moon S, Seo MY, Choi K, Chang Y seok, Kim SH, Park MJ, 2021. Urinary bisphenol A concentrations and the risk of obesity in Korean adults. Sci. Rep. 11 (1), 1603. 10.1038/s41598-021-80980-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng M, Fleming T, Robinson M, et al. , 2014. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384 (9945), 766–781. 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perng W, Watkins DJ, Cantoral A, et al. , 2017. Exposure to phthalates is associated with lipid profile in peripubertal Mexican youth. Environ. Res. 154, 311–317. 10.1016/j.envres.2017.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perng W, Tamayo-Ortiz M, Tang L, et al. , 2019. Early life exposure in Mexico to ENvironmental toxicants (ELEMENT) Project. BMJ Open 9 (8), e030427. 10.1136/bmjopen-2019-030427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perng W, Cantoral A, Soria-Contreras DC, et al. , 2021. Exposure to obesogenic endocrine disrupting chemicals and obesity among youth of Latino or Hispanic origin in the United States and Latin America: a lifecourse perspective. Obes. Rev. 22 (S3), e13245 10.1111/obr.13245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popkin BM, Adair LS, Ng SW, 2012. Global nutrition transition and the pandemic of obesity in developing countries. Nutr. Rev. 70 (1), 3–21. 10.1111/j.1753-4887.2011.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radke EG, Galizia A, Thayer KA, Cooper GS, 2019. Phthalate exposure and metabolic effects: a systematic review of the human epidemiological evidence. Environ. Int. 132, 104768 10.1016/j.envint.2019.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivera JA, Barquera S, González-Cossío T, Olaiz G, Sepúlveda J, 2004. Nutrition transition in Mexico and in other Latin American countries. Nutr. Rev. 62 (Suppl. l_ 2), S149–S157. 10.1111/j.1753-4887.2004.tb00086.x. [DOI] [PubMed] [Google Scholar]
- Rodríguez G, Moreno LA, Blay MG, et al. , 2004. Body composition in adolescents: measurements and metabolic aspects. Int. J. Obes. 28 (3), S54–S58. 10.1038/sj.ijo.0802805. [DOI] [PubMed] [Google Scholar]
- Russ K, Howard S, 2016. Developmental exposure to environmental chemicals and metabolic changes in children. Curr. Probl. Pediatr. Adolesc. Health Care 46 (8), 255–285. 10.1016/j.cppeds.2016.06.001. [DOI] [PubMed] [Google Scholar]
- Salazar MR, Carbajal HA, Espeche WG, Aizpurúa M, Maciel PM, Reaven GM, 2014. Identification of cardiometabolic risk: visceral adiposity index versus triglyceride/HDL cholesterol ratio. Am. J. Med. 127 (2), 152–157. 10.1016/j.amjmed.2013.10.012. [DOI] [PubMed] [Google Scholar]
- Shankar A, Teppala S, 2012. Urinary bisphenol A and hypertension in a multiethnic sample of US adults. J. Environ. Pub. Heal. 2012, 481641 10.1155/2012/481641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheikh IA, Abu-Elmagd M, Turki RF, Damanhouri GA, Beg MA, Al-Qahtani M, 2016. Endocrine disruption: in silico perspectives of interactions of di-(2-ethylhexyl) phthalate and its five major metabolites with progesterone receptor. BMC Struct. Biol. 16 (S1), 16. 10.1186/s12900-016-0066-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shih MF, Pan KH, Liu CC, Shen CR, Cherng JY, 2018. Treatment of β-thujaplicin counteracts di(2-ethylhexyl)phthalate (DEHP)-exposed vascular smooth muscle activation, inflammation and atherosclerosis progression. Regul. Toxicol. Pharmacol. 92, 333–337. 10.1016/j.yrtph.2017.12.021. [DOI] [PubMed] [Google Scholar]
- Siervogel RM, Demerath EW, Schubert C, et al. , 2003. Puberty and body composition. Horm. Res. Paediatr. 60 (Suppl. 1), 36–45. 10.1159/000071224. [DOI] [PubMed] [Google Scholar]
- Silva MJ, Slakman AR, Reidy JA, et al. , 2004. Analysis of human urine for fifteen phthalate metabolites using automated solid-phase extraction. J. Chromatogr. B 805 (1), 161–167. 10.1016/j.jchromb.2004.02.038. [DOI] [PubMed] [Google Scholar]
- Silva CCV, Jaddoe VWV, Sol CM, et al. , 2021. Phthalate and bisphenol urinary concentrations, body fat measures, and cardiovascular risk factors in Dutch school-age children. Obesity 29 (2), 409–417. 10.1002/oby.23082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stages of Adolescence. HealthyChildren.org. https://www.healthychildren.org/English/ages-stages/teen/Pages/Stages-of-Adolescence.aspx. (Accessed 19 January 2023).
- Tarokh L, Short M, Crowley SJ, Fontanellaz-Castiglione CEG, Carskadon MA, 2019. Sleep and circadian rhythms in adolescence. Curr. Sleep Med. Rep. 5 (4), 181–192. 10.1007/s40675-019-00155-w. [DOI] [Google Scholar]
- Trasande L, Spanier AJ, Sathyanarayana S, Attina TM, Blustein J, 2013. Urinary phthalates and increased insulin resistance in adolescents. Pediatrics 132 (3), e646–e655. 10.1542/peds.2012-4022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urbina EM, Khoury PR, McCoy CE, Dolan LM, Daniels SR, Kimball TR, 2013. Triglyceride to HDL-C ratio and increased arterial stiffness in children, adolescents, and young adults. Pediatrics 131 (4), e1082–e1090. 10.1542/peds.2012-1726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viitasalo A, Lakka TA, Laaksonen DE, et al. , 2014. Validation of metabolic syndrome score by confirmatory factor analysis in children and adults and prediction of cardiometabolic outcomes in adults. Diabetologia 57 (5), 940–949. 10.1007/s00125-014-3172-5. [DOI] [PubMed] [Google Scholar]
- Wang J, Dong S, 2012. ICAM-1 and IL-8 are expressed by DEHP and suppressed by curcumin through ERK and p38 MAPK in human umbilical vein endothelial cells. Inflammation 35 (3), 859–870. 10.1007/s10753-011-9387-4. [DOI] [PubMed] [Google Scholar]
- Wang T, Xu M, Xu Y, et al. , 2015. Association of bisphenol A exposure with hypertension and early macrovascular diseases in Chinese adults. Medicine (Baltim.) 94 (43), e1814. 10.1097/MD.0000000000001814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu W, Li M, Liu A, et al. , 2020a. Bisphenol A and the risk of obesity a systematic review with meta-analysis of the epidemiological evidence. Dose Response 18 (2), 1559325820916949. 10.1177/1559325820916949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y, Goodrich JM, Dolinoy DC, et al. , 2020b. Accelerometer-measured physical activity, reproductive hormones, and DNA methylation. Med. Sci. Sports Exerc. 52 (3), 598–607. 10.1249/MSS.0000000000002175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yalçin SS, Erdal I, Oğuz B, Duzova A, 2022. Association of urine phthalate metabolites, bisphenol A levels and serum electrolytes with 24-h blood pressure profile in adolescents. BMC Nephrol. 23 (1), 141. 10.1186/s12882-022-02774-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao Y, Chen DY, Yin JW, et al. , 2020. Phthalate exposure linked to high blood pressure in Chinese children. Environ. Int. 143, 105958 10.1016/j.envint.2020.105958. [DOI] [PubMed] [Google Scholar]
- Zamora AN, Jansen EC, Tamayo-Ortiz M, et al. , 2021. Exposure to phenols, phthalates and parabens and development of metabolic syndrome among Mexican women in midlife. Front. Public Health 9. 10.3389/fpubh.2021.620769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziv-Gal A, Gallicchio L, Chiang C, et al. , 2016. Phthalate metabolite levels and menopausal hot flashes in midlife women. Reprod. Toxicol. 60, 76–81. 10.1016/j.reprotox.2016.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.