Version Changes
Revised. Amendments from Version 1
We have amended the text throughout to improve consistency and readability.
We have amended figure 2 for clarity and added figure 3 (logic model) and appendix 1 (sample exercise session template).
We have added co-author Professor Charles Abraham, School of Psychology, Deakin University, Melbourne, Australia. Conceptualization, funding acquisition, editing and review
Abstract
Background
Up to half of people hospitalised with COVID-19 report diverse and persistent symptoms affecting quality of life for months and sometimes years after discharge (long-COVID). We describe the development of an online group exercise and behavioural support intervention for people who continue to experience such physical and/or emotional health problems more than three months after hospital discharge.
Methods
Intervention development was informed by the Medical Research Council framework for complex interventions. Our multidisciplinary team of academics, clinicians, and people with long-COVID, had collective expertise in the development and testing of complex interventions. We integrated a bio-psycho-social model of care drawing on rehabilitation literature for long-term health conditions and experiences from our pre-pilot study. Multiple stakeholder meetings were held to refine the intervention which was designed to be deliverable within the UK National Health Service. We adhere to TIDieR guidance for transparent and explicit reporting of telehealth interventions.
Results
The final REGAIN online exercise and behavioural support intervention consisted of an initial 1:1 consultation with a trained practitioner, followed by eight online group exercise, and six group support, sessions delivered over eight weeks. Participants could also access an online library of on-demand exercise and support videos.
Conclusions
The final REGAIN intervention, combining exercise and behavioural support, is fully manualised with clear pathways to delivery and implementation. It is currently being tested in a randomised controlled trial. The intervention, developed with extensive patient and stakeholder engagement, could be incorporated into existing NHS rehabilitation programmes, should it prove to be clinically and cost-effective for people with long-COVID.
Trial registration
International Standard Randomised Controlled Trial Number (ISRCTN) 11466448: Rehabilitation exercise and psychological support after COVID-19 infection: REGAIN.
Keywords: rehabilitation, long-COVID, physical activity, online support, intervention development, physical activity
Plain English summary
Long-COVID has many debilitating symptoms, such as breathlessness, muscle weakness and fatigue, which significantly affect peoples’ physical and mental health and quality of life. Rehabilitation programmes can help people improve their quality of life in other medical conditions with similar symptoms. We developed a programme of physical and mental health rehabilitation, delivered online, specifically to support people with ongoing long-COVID symptoms more than three months after hospital discharge. The programme was developed by people with long-COVID along with clinicians and researchers. The programme described in this article is now being tested in a large research trial to see if it can help people with long-COVID.
Introduction
‘Long-COVID’ is the term commonly used to describe symptoms which continue or develop after the initial acute infection with COVID-19 has resolved. It includes ongoing symptomatic COVID-19 (from 4 to 12 weeks) and post-COVID-19 syndrome (12 weeks or more), where symptoms cannot be explained by an alternative diagnosis 1 . As of January 2023, there were approximately 2.1 million people (3.3% of the population) self-reporting long-COVID in the UK 1 . Of those, 57% reported symptoms lasting at least one year, and 76% reported symptoms that adversely affected their daily activities 1 . The most common symptoms were fatigue (71%), difficulty concentrating (‘brain fog’) (49%), breathlessness (47%), and muscle aches (46%) 1 . Symptoms vary in severity within and between individuals, and commonly remit and relapse over time leading to considerable distress and a negative impact on mental wellbeing 2 . People often feel dismissed by medical professionals, and abandoned after hospital discharge, and commonly seek validation and support elsewhere via peer behavioural support groups and social media 3, 4 . Long-COVID can have devastating psychological, physical and cognitive consequences that disrupt lives and livelihoods 5 .
To address long-COVID, an NIHR review 6 suggested the need for a holistic, integrated treatment approach rather than symptom by symptom management. This was supported by UK COVID-19 guidelines which recommended pragmatic treatment for psychological, emotional, and physical health 7 . However, for people with long-COVID, direct face-to-face contact with medical professionals in general, and specifically specialist post-COVID-19 clinics, has been difficult to access, and provision is highly variable. One method of countering these problems is to provide resources online.
The primary digital resource for people living with long-COVID in the UK is ‘Your COVID Recovery’ 8 produced by the National Health Service (NHS). ‘Your COVID Recovery’ is a comprehensive NHS online resource providing self-management symptom advice and support. However, this resource lacks the social connection that patients often desire, is necessarily generic, and may not be versatile enough to meet the needs of everyone with long-COVID. Furthermore, awareness of the website is not widespread, and evaluation of patient experience of the intervention has not yet been published.
Currently, few studies have examined rehabilitation for people with long-COVID, particularly in an online setting, although there are reports that multidisciplinary rehabilitation can improve symptoms in long-COVID 9 and enhance quality of life for people living with other long-term health conditions with similar symptom profiles, such as Chronic Obstructive Pulmonary Disease (COPD) 10 and Severe Acute Respiratory Syndrome (SARS) 11 . Therefore, a large-scale trial to test such an intervention suitable for online, remote delivery, is required.
This manuscript describes the design and development of an online exercise and behavioural support intervention for people with long-COVID. The REGAIN randomised controlled trial (RCT) was funded by the National Institute of Health Research COVID-19 Recovery and Learning Programme (NIHR132046) to evaluate the clinical and cost-effectiveness of an online exercise and psychological support intervention for people hospitalised with COVID-19 who still reported symptoms more than three months after hospital discharge 12 .
Methods
Ethical approval
Ethical approval was received from the East of England-Cambridge South Research Ethics Committee (REC: 20/EE/0235).
Written informed consent for publication of the participants details and/or their images was obtained from the participants.
Overview of the development process
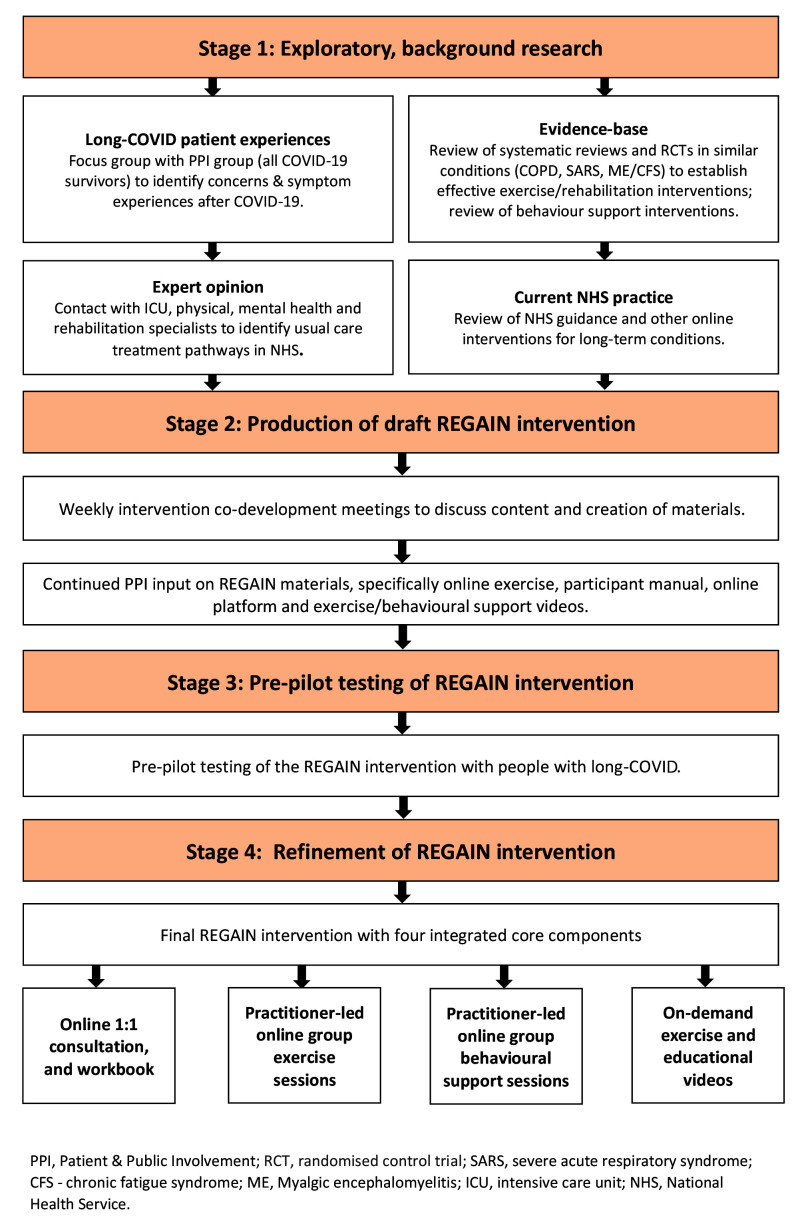
We followed the Medical Research Council framework 13 for design of complex interventions ( Figure 1). Our manuscript adheres to the recent Template for Intervention Development and Replication (TIDieR) for ‘telehealth’ complex interventions 14 . Work was conducted between August 2020 and January 2021.
Figure 1. Intervention development process.
Stage 1: Exploratory, background research (patient experience, evidence base, expert opinion, current practice)
A search of bibliographic databases (MEDLINE, PsycInfo and CINAHL) identified literature relating to behavioural or self-management needs for people living with long-COVID. Due to the relative paucity of long-COVID research, we also searched for literature on chronic fatigue syndrome (CFS), chronic obstructive pulmonary disease (COPD), and the 2002–2004 SARS epidemic. Collectively these conditions exhibit several of the most common and debilitating symptoms of long-COVID (e.g. fatigue, lethargy, breathlessness, muscle weakness, brain fog).
Titles and abstracts of papers were assessed for relevance, prioritising recent systematic reviews of needs and interventions in long-COVID, CFS, COPD and SARS. Articles were examined to ensure that the needs identified by our stakeholder groups were addressed by research evidence where possible. Reports of interventions for conditions with similar symptoms helped to identify core components that may be effective for people living with long-COVID.
The literature review revealed limited evidence regarding the efficacy of rehabilitation interventions for COVID-19 survivors 9 . One RCT (n=72) of respiratory rehabilitation reported improved respiratory function, quality of life (QoL) and anxiety in elderly people with COVID-19 15 , but there was little other data available. In other similar conditions, a meta-analysis of 65 RCTs involving 3822 participants reported that pulmonary rehabilitation programmes, combining exercise with various psychological support and education components, were beneficial in improving health-related quality of life (HR-QoL) and exercise capacity in people with COPD 10 . Similarly, a meta-analysis of eight RCTs (n=1518) concluded that people with CFS may generally benefit and feel less fatigued following exercise therapy, comparable to the effectiveness of cognitive behavioural therapy (CBT), with no evidence to suggest that exercise therapy may worsen outcomes 16 . Exercise training was also reported to be effective in improving cardiorespiratory and musculoskeletal fitness in people recovering from SARS, although there was no reported effect on HR-QoL 11 . Other studies highlighted the persistent mental and physical abnormalities in SARS survivors up to two years post-infection 17 . Exercise therapy alone, therefore, is likely insufficient to optimise recovery for people with long-COVID.
We concluded that to combat the multiple long-term physical and mental health consequences of COVID-19, a combined physical and psychological rehabilitation intervention was required. In order to make the programme as widely accessible as possible during COVID-19 ‘lock-downs’ and reduced access to healthcare, the intervention was developed to be deliverable online.
Stage 2: Production of draft REGAIN intervention
To holistically appraise the needs of people with long-term COVID-19 symptoms following hospitalisation, a core intervention development team was formed. The team (n=22) had specialism and extensive experience in clinical academia, physiotherapy, psychiatry, health psychology, clinical exercise physiology, critical care medicine, complex intervention development and implementation, and online rehabilitation and behavioural support. Six people (male n=3, female n=3; age 33–62 years) with symptoms of long-COVID (3–9 months duration) were also involved throughout every stage of the development of the REGAIN intervention (patient and public involvement (PPI) group). Online meetings facilitated discussions informed by evidence from Stage 1 development. The team met frequently with the objective of identifying and formulating the key components of a complex intervention.
The research team identified key themes and priorities from the literature to form the outline for a series of online discussions held between August and October 2020 ( Table 1). Consensus responses relating to core components for inclusion in the exercise and behavioural support intervention were collated into the following categories: online group exercise classes (frequency, intensity, time and type principles), concerns about post exertional malaise/chronic fatigue, exercise programme progression, behavioural support materials, and the feasibility of delivering the intervention online in a NHS setting to participants with diverse symptomology and varying degrees of information technology (IT) literacy. Findings from the stakeholder meetings are summarised in Table 1. A framework of a draft intervention was finalised for pre-pilot testing.
Table 1. Key findings from intervention co-development meetings.
| Component | Outcome/consensus |
|---|---|
|
Online group
exercise classes |
All agreed that one supervised exercise session per week of 20-60 minutes duration, dependent on
fitness level, should be tested for acceptability during the pre-pilot phase. Additional pre-recorded exercise classes planned to provide “on- demand” video material for participants to follow unsupervised at home, up to 2-3 per week. Videos would include a variety of exercises to appeal to all, including: Yoga, Pilates, chair-based and breathing exercise videos. Concerns were expressed by patients that some exercises may not be tolerated by more debilitated patients. The need for robust safety/emergency procedures was also highlighted. People with long-COVID symptoms expressed a loss of confidence about being physically active and anxiety about relapse; also concern about over-exertion. An emphasis on fun over intensity was agreed for first few weeks to promote confidence and adherence. All agreed that light-moderate aerobic exercise (40-70% Heart Rate Reserve (HRR), rating of perceived exertion (RPE) - 11–14) was realistic for most participants after familiarisation. Gentle mobility, coordination, and balance exercises would be needed after long sedentary periods for some participants. Clinical exercise physiologists should test acceptability during the pre-pilot phase. All Long Covid patients agreed that IT literacy might be an obstacle to accessing sessions for older participants. |
|
Concern about
post-exertional malaise (PEM) |
Members of trial team met with ME groups to discuss the dangers of post-exertional malaise (PEM) in
the long-COVID population. The word exercise seemed to have negative connotations, assumed to only mean high intensity/exertion levels which could be detrimental to recovery. Use of term physical activity would be better received. Groups were reassured that (a) intensity would be low-moderate and at the comfort level of the individual and (b) that the risk of PEM would be minimised by closely monitoring participants before, during, and after each session, as well as assessing risk of PEM during the initial 1:1 consultation (c) a pre-determined ‘graded’ approach adopted in previous trials would not be applied to this population. Specific information was provided to participating clinicians during the training sessions highlighting the need to be aware of PEM and how to address it, and a section on PEM was incorporated into the Practitioner Manual provided to all clinicians taking part in REGAIN. |
|
Exercise
progression |
It was agreed that exercise physiologists should produce 8-12 exercise session templates of different
levels of intensity for standardised delivery across the trial. Classes would follow a circuit format with active recovery between exercises. A point was made that quite conceivably a group containing very low and very high ability participants was likely as practitioners would not always be able to arrange groups based on ability level. Therefore, a great degree of versatility was needed with exercise class design and delivery. People with long-COVID symptoms requested ample rest periods and water breaks. Following warm-up and mobility, duration of exercise should be progressed primarily as tolerated, for maximal therapeutic benefit. Researchers requested that exercise physiologists collect ratings of perceived exertion (RPE) to assess intervention fidelity. |
|
Behavioural
support materials |
Mind-body disconnect was mentioned by people with long-COVID symptoms, so they felt it would be
really useful to have an integrated intervention. They felt strongly that long Covid wasn’t simply physical symptoms of fatigue and breathlessness, but also how this affected their thoughts and feelings. Many topics were deemed useful by patients, especially ‘challenging unhelpful thoughts’ and ‘anxiety management’. Pacing of activities was considered crucial. Talking to the trained practitioner before and after group exercise sessions in a supportive environment was thought to be important to ensure continued adherence and group cohesion. This would also promote peer support. Breathing was difficult for some and so being able to stop, take a breath and relax was important. Reinfection was also major source of anxiety/worry. The participant workbook was thought by patients to be a long document, but all content was relevant as this could be read in their own time. The written targets were welcomed (e.g. writing down goals), and making notes during the session was deemed useful. Patients preferred a paper copy to an online PDF. Patients suggested colour-coded sections of the workbook to make it less daunting, and tabs to make easy to find sections for each weekly session. Suggested workbook format included adding the aims of behavioural support, with short clear statements at the beginning of each section of the workbook. |
|
Feasibility of
delivery within NHS setting |
Exercise physiologists and health psychologists highlighted potential obstacles to online delivery. These
included: the need for a second practitioner, or ‘co-pilot’, for safety reasons, IT connectivity , participant retention, risk of busy classes, accurate intensity monitoring, and adequate behavioural intervention training for practitioners less experienced with these techniques. Actions were agreed to mitigate these issues: (1) deliver appropriate training for practitioners led by health psychologist and an experienced clinical research fellow; (2) provide comprehensive reference manuals for participants and practitioners to follow; and (3) ensure sufficient time was spent with each participant during the 1:1 consultation to familiarise them with the online platform and IT requirements. |
Post exertional malaise
During the development phase, the trial team were contacted by several organisations representing the Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) community with concerns relating to the potential harms of unsupervised vigorous exercise for people with long-COVID, in particular the risk of post-exertional malaise 18 . We recognised the lived experience and expertise within these groups and sought to ensure that REGAIN practitioners were appropriately trained in risks relating to post-exertional malaise. Furthermore, early identification screening measures for post-exertional malaise were incorporated into the intervention protocols, particularly during the initial one-to-one consultation and every subsequent exercise session. Practitioners were encouraged to monitor the progress of participants during and after exercise sessions in order to ensure that exercise intensity and volume were within individuals’ capabilities and did not cause undue persistent fatigue or other problems.
Stage 3: Pre-pilot testing of the REGAIN intervention
To test acceptability and deliverability, the draft REGAIN intervention was feasibility tested in a pre-pilot study with eight people living with long-COVID. The online exercise and behavioural support sessions were delivered from a community NHS exercise rehabilitation facility (Atrium Health, Centre for Exercise and Health, Coventry). Feedback was gathered on the acceptability and practicality of the intervention from eight participants as well as the healthcare practitioners delivering the intervention. This included comments on the written and online trial materials (e.g. practitioner/participant manuals) and the online platforms used to deliver the intervention. This helped the trial team further refine and develop the intervention before proceeding to the main trial. The key findings from the pre-pilot stage are described in Table 2.
Table 2. Main findings from pre-pilot study testing REGAIN intervention delivery.
| Component | Finding(s) | Implications for REGAIN Intervention |
|---|---|---|
|
IT/online
issues |
Participants not placing device in adequate
position for practitioner to view during exercises. Some older participants had difficulty navigating Zoom/MS Teams, enabling microphone/camera, and accessing link to session. Some participants accessed the session through their Smartphone which limited functionality (couldn’t see the rest of group). One person held smartphone throughout, so very jerky & too close; it was not possible for the practitioner to safely monitor exertion levels or technique. |
During 1:1 consultation there is a need to go through
set up - test the device and where the camera will be set up. etc. Log in to zoom and do test session. Practitioners and ‘co-pilot’ to log in early to group sessions as considerable time needed to let everyone into session. Amend workbook/telephone screening calls to indicate that a smartphone not good enough unless it can be ‘cast’ to a TV. Laptops & tablets preferred. |
| Progression | Participants found the progression more
acceptable once they had gained confidence in the sessions and felt included in short ’debrief’ post exercise with rest of group. |
Class templates amended so that Practitioners could
alter the duration of exercises and recovery periods to suit each group. Participants to be asked how they felt the day after each session, as well as post session, to guard against post exertional fatigue. |
| Safety | Participants would frequently talk or make
noise throughout, inadvertently interrupting practitioners’ instructions. Occasionally participants would disappear from view- going to toilet/answering door- practitioners were unsure if the patient was unwell. |
All participants should be instructed to mute during
exercise. Hand signals required to indicate whether easy, ok, too hard and another to say I am unwell/need to stop/etc. Set ground rules and instructions at start of each class requesting participants to signal before they leave the screen. |
|
Very
debilitated participants |
One participant was chair bound in the same
session as another with a relatively high level of fitness. Practitioners needed assistance from ‘co- pilots’ (via chat function) to adequately monitor all participants. |
Need alternative chair-based option for all exercises
in the session templates. Priority should be given to enjoyment while participants gain confidence. Frequent water breaks should be provided and the emphasis placed on the participant to take responsibility for their own exertion level |
|
One to one
consultation |
Several participants were identified as having case
level mental health disorder on anxiety/depression questionnaire. More discussion during the consultations revealed a higher level of emotional support needed than initially planned. Some participants spent longer overcoming IT issues than they did talking about their long- COVID. |
Consultations should be at least an hour in order
to introduce website and sign-up process, triage participant for exercise classes, and go through IT accessibility/optimal camera position etc. Regular meetings with psychologist planned throughout trial for ongoing advice/support for practitioners during trial. |
|
Behavioural
education |
Participants required more support coping with
anxiety/avoidance around social interaction and not just physical activity. Goal setting session was difficult as most participants experienced frequent setbacks and had unknown timescale of recovery. Some participants dominated the support sessions and others barely spoke. Practitioners were unsure how long to ‘let it go’ before interrupting. Practitioners were also unsure about PTSD issues that some participants may be facing, and giving advice outside of their competences. |
Additional material included in the participant workbook
relating to negative thought patterns. Practitioners should approach long COVID differently to traditional rehabilitation for long term conditions with no expectation of linear improvement each week Health psychologists to do additional training with practitioners regarding managing groups. |
Stage 4: Refinement of the REGAIN intervention
On-demand exercise and educational videos. The intervention team, with the support of our patient partners, developed 14 ‘on-demand’ exercise videos which used a similar format to the live online exercise sessions and were designed to account for all abilities. Lower intensity videos with postural stability and balance exercises were included for people with more pronounced levels of fatigue or disability. Some videos were themed (e.g., shopping, housework) to reintroduce activities of daily living and to add some additional context for those unaccustomed to exercise videos. We also included videos of other exercise modalities (e.g., Yoga, Pilates, and high intensity interval training (HIIT)), which had already been produced by the online physical activity provider (BeamFeelGood) used to deliver the intervention. Finally, five videos providing advice and education on lung function and care, including breathing techniques/exercises (Fit for Surgery team, University Hospital Birmingham) and six ‘mindfulness’ videos (Dr Gail Davies) were produced to give participants additional online resources. All videos were hosted on the online platform via a trial-specific protected user area. Participants were encouraged to access these exercise videos, unsupervised, between weekly group sessions and to progress to performing up to two additional exercise sessions per week as tolerated.
Practitioner-led online group exercise sessions
A series of 12 templates were designed for the online group exercise sessions. They ranged in modality from low intensity chair-based activity to higher intensity whole body exercise. These formed the basis of all online group exercise sessions and ensured a level of exercise programme standardisation throughout the trial. All the exercises within each template required little or no equipment and were easily modifiable to account for different ability levels within the group. Depending on the group, different exercises were swapped in or out of the session template to cater for the specific needs. Generally, the templates included 7–8 exercises to be completed 2–3 times (i.e., 2-3 circuits). The warm-up and cool down lasted 5–10 minutes each.
Results
Overview of REGAIN intervention
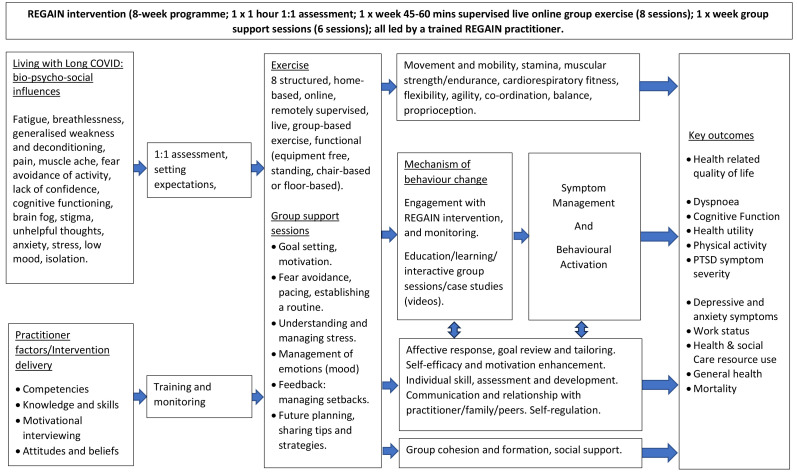
The final REGAIN exercise and behavioural support intervention consisted of four main components delivered by clinical exercise physiologists or physiotherapists (REGAIN practitioners). The final intervention structure and accompanying logic model are presented in Figure 2) and Figure 3 respectively.
Figure 2. Final format and components of the ‘Rehabilitation Exercise and psycholoGical support After covid-19 InfectioN’ (REGAIN) intervention.
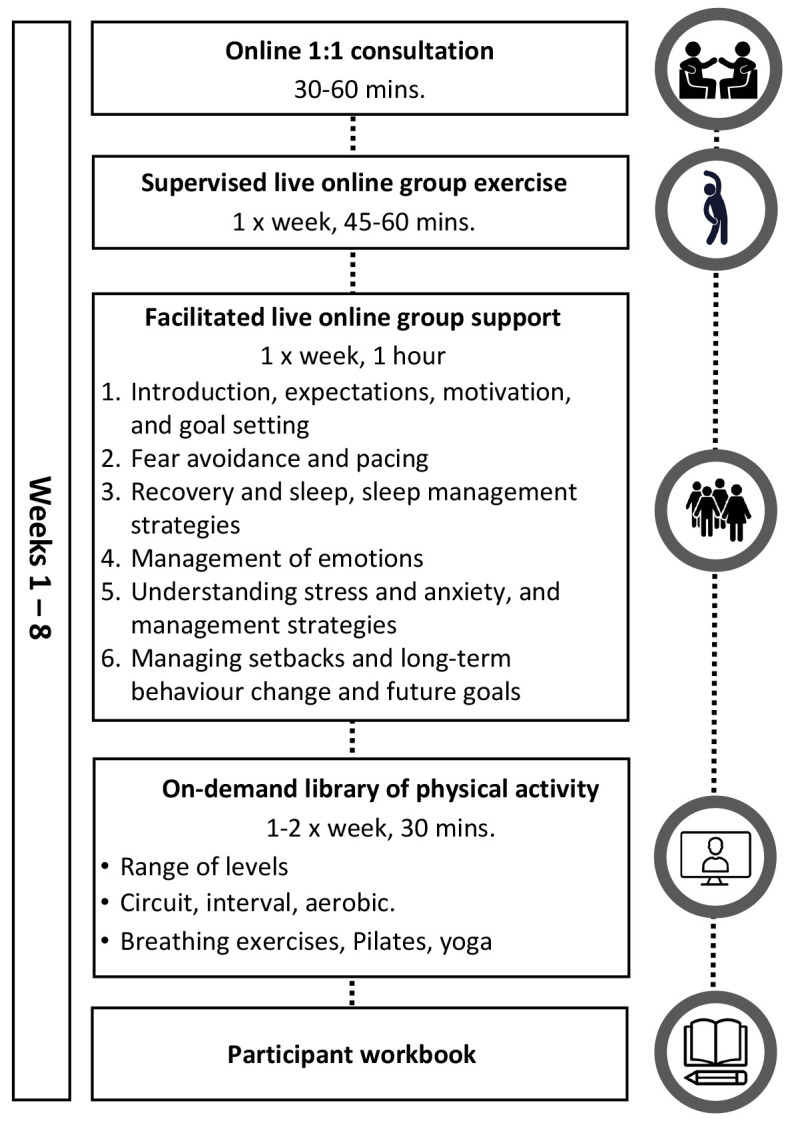
Figure 3. Logic model for the REGAIN intervention.
-
1.
Online one-to one video consultation and participant workbook
-
2.
Eight-week exercise programme: practitioner-led live online group sessions once per week
-
3.
Six practitioner-led live online group behavioural support sessions (during weeks 1–5 & week 8).
-
4.
On-demand exercise sessions.
Online one-to-one consultation
The one-to one consultation with a REGAIN practitioner included several components and was designed to triage the participant for safe exercise, and familiarise them with the IT requirements:
Clinical history including COVID-19 hospitalisation episode(s), resulting problems and other relevant medical history and co-morbidities
Potential barriers to participation
Demonstration of, and sign-up processes, for the online platform.
Discussion regarding home (e.g. space, lighting) and device set-up for live group exercise and support sessions
Eight-week exercise programme
The online exercise rehabilitation programme delivered by REGAIN practitioners consisted of up to 30 minutes of light to moderate intensity exercise two to three times per week for eight weeks. Practitioners individualised group sessions to accommodate varying abilities, with progressive multi-modality exercise at a manageable intensity, monitored with breathlessness and perceived exertion scales. Participants were encouraged to attend one live online group exercise session each week, and additionally access the online, pre-recorded exercise videos once or twice each week. This equipment-free exercise programme aimed to improve cardiovascular fitness, strength, balance, co-ordination, and confidence. Sessions were undertaken in discrete groups where participants remained in the same group over the eight-week programme. An example of an intermediate level exercise session is presented in Table 3.
Table 3. Example template for a live online REGAIN exercise session.
| Session Plan – REGAIN session 5 | Challenge: | Intermediate | Circuits: | 2 | |||
|---|---|---|---|---|---|---|---|
| Equipment: | chair (optional: weights of some kind e.g. water bottles, tins, dumbells etc) | ||||||
| Comments: | All exercises below are interspersed with active recovery (AR), e.g. marching, side-steps, heel digs etc | ||||||
| Exercise Name | Reps and/or
Time |
Teaching Points
(Key safety points) |
Progression | Alternatives
(where appropriate) |
|||
| 1 |
Squat + one
arm reach |
45s on/30s AR | □ Feet hip width apart
□ Back straight, head up, extend arm up as you stand up |
□ Increase ROM
□ Add weight |
□ Decrease ROM | ||
| 2 |
Lateral raise
super slow |
45s on/30s AR | □ Hold abdominals tight
□ Slow controlled movement □ Arms up to shoulders |
□ Add weight
□ Pause at top |
□ Front raise
□ Seated □ Alternate arms |
||
| 3 |
Side lunge
with super slow bicep curl |
45s on/30s AR | □ Toe down first to side
□ Slight bend in knee □ When in lunge squeeze arms into curl |
□ Deeper lunge
□ Add Weight □ Pause at top |
□ External support
□ Shallow lunge |
||
| 4 | High pull | 45s on/30s AR | Feet hip width apart
Slight bend in knees back straight Stand back up bringing hands from knees to chest in 1 movt |
Add weight
increase ROM |
Decrease ROM
upright row w/out legs |
||
| 5 |
Wide stance
knee to opp. toe touch |
45s on/30s AR | □ Feet flat on floor, shoulder width
apart □ Back straight, head up □ Knees soft □ Rotate to reach down to opposing knee |
□ Increase ROM to ankle
□ wider stance |
□ Decrease ROM
□ seated |
||
| 6 |
Standing
overhead press |
45s on/30s AR | □ Feet hip width apart
□ Slight pelvic tilt to protect back, Abdominals tight □ Extend both arms up to meet in arc overhead |
□ Add weight
□ Pause at top |
□ Alternate arms
□ Seated □ Frontal raise |
||
| 7 |
Seated leg lift
over object |
45s on/30s AR | □ Sit towards edge of chair
□ Lean back into chair □ Lift straight leg one at a time over water bottle |
□ both legs together | □ bent leg
□ hold chair for balance |
||
Online group support sessions
Emerging evidence highlighted the importance of the biopsychosocial model 19, 20 in understanding the interrelationships among risk factors and multidimensional clinical and psychosocial COVID-19 outcomes. The support sessions were based on behaviour change theory (Michie’s COM-B model: mapping key processes and functions to enhance Capability, Opportunity, and Motivation) 21 , self-efficacy 22 , motivational interviewing 23 , and group-based learning 24 . These theoretical principles were used to inform the psychosocial content, structure and delivery of the sessions in combination with the British Psychological Guidance for management of long-COVID which was available at the time 25 .
To enhance the psychological capability of participants (as per the COM-B model), support sessions, delivered by REGAIN practitioners, were designed to increase knowledge and understanding about COVID-19 and its impact on daily living. Feedback from patient partners highlighted the need for practitioners to address misinformation from various sources (e.g., friends/relatives, news, social media etc.) which often caused more anxiety and distress. Reduced processing and retention of information due to brain fog and poor concentration also informed the design and content of the support sessions. Resources and activities could be paused at any time and revisited by participants via the provided study materials (PowerPoint presentations, written summaries of key topics, video clips and further reading). Motivation was incorporated into support sessions through exploration of self-identity and the meaning of COVID-19 to the participants and those around them (e.g., family). By discussing COVID-19 experiences in a group setting, participants could see that others were having the same issues and could share experiences and coping strategies. The aim was for participants to feel validated that their symptoms were not only real, but that they were not alone in experiencing them.
Opportunity was the third core principle incorporated into the support sessions: participants were permitted time to engage in sessions in a supportive environment. Group based support sessions were chosen because they can promote behaviour change through shared values and norms, influencing beliefs, and encouraging common motivations and behavioural patterning. We stressed the importance of engaging with all elements of the intervention. To help attenuate fatigue, group support sessions were no longer than 60 minutes. The six group support sessions below are further summarised in Table 4:
Table 4. Summary of REGAIN intervention components and theoretical underpinnings.
| Intervention
component |
Aims | Theoretical
Framework(s) |
Behaviour Change Taxonomy |
|---|---|---|---|
| One to one consultation | To gather relevant information (clinical
history) To assess motivations and potential barriers to engagement with the REGAIN Intervention To demonstrate and introduce the online platform To offer an opportunity to answer any questions related to the study or intervention and discuss home environment for engagement with the sessions |
COM-B
Self-efficacy Communication |
Goal setting (behaviour)
Restructuring the physical environment Instruction on how to perform a behaviour (online platform) Verbal persuasion about capability (if appropriate) |
| Support session 1
Introduction, expectations, motivation and goal setting |
To introduce and familiarise participant with
the programme Getting to know the group Explore personal and group expectations allowing time for planning, prioritising and setting achievable targets Explore motivation, understanding potential short term and long-term benefits of engagement in the programme |
COM-B
Social Learning Theory Bio-Psycho-Social |
Goal setting (behaviour)
Goal setting (outcome) Action planning |
| Group session 2 Fear
avoidance and pacing |
To introduce relationship between thoughts,
feelings, and emotions related to avoidance of behaviour (for example fear of aggravating COVID-19 symptoms such as breathlessness/ fatigue) Exploring reasons for fear avoidance and consequences on health outcomes Exploring strategies to overcome fear avoidance and introduce pacing of activities |
COM-B
Self-Efficacy Bio-Psycho-Social |
Information about
antecedents Problem solving |
| Group session 3
Recovery and sleep, sleep management strategies |
To explore how sleep patterns may have
changed since having COVID Understanding sleep Introduction of sleep management strategies |
COM-B
Bio-Psycho-Social |
Information about health
consequences Problem solving Re-attribution |
| Group session 4
Management of emotions (perceived stigma, mood/ unhelpful thoughts) |
To introduce and explore the impact of
COVID on mood, thoughts and behaviour including unhelpful thought patterns Introduce skills for reframing thoughts, encouraging engagement with all components of the programme |
COM-B
Cognitive Behavioural Principles |
Social support (emotional)
Information about emotional consequences Monitoring of emotional Consequences Framing/reframing |
| Group session 5
Understanding stress and anxiety and management strategies |
To understand and explore impact of stress
on symptom management (acute vs chronic stress) Understand own stress response to COVID and hospitalisation Introduce stress management strategies |
COM-B
Bio-Psycho-Social |
Information about social and
environmental consequences Reduce negative emotions |
| Group Session 6 Managing
setbacks and long-term behaviour change and future goals. |
To consolidate learning from previous
sessions and reinforce long term behaviour change To introduce management of setbacks and strategies of problem solving for long term change |
COM-B
Group Based Learning Self-management |
Problem solving
Review behaviour goal(s) Social support (emotional) Comparative imagining of future outcomes Self-talk Focus on past success |
| Practitioner handbook | To provide step-by-step guidance on
delivering the REGAIN intervention To provide facilitation skills and motivational interviewing prompts and questions for group sessions |
COM-B
Motivational Interviewing |
Feedback on behaviour (through
quality assessment and observations of sessions) Credible source |
| Participant workbook | Provide information on programme
structure, safety and contact information for further support if needed Provide information and content for each session, with clear aims, and tasks to complete to consolidate learning To allow a log of personal progress and reflection and point of reference during the programme and beyond |
COM-B
Self-Efficacy Bio-Psycho-Social |
Self-monitoring of outcome(s) of
behaviour Information about health consequences Behavioural practice/rehearsal |
| Live group exercise
sessions |
To increase ability to engage in physical
activity To increase strength, flexibility, balance and aerobic capacity. To increase confidence in ability to move and engage in physical activity To encourage physical activity outside of live sessions. To strengthen group dynamics |
COM-B
Self-Efficacy Group Based Learning Social Learning Theory |
Feedback on outcome(s) of
behaviour Instruction on how to perform a behaviour Demonstration of the behaviour Graded tasks Body changes |
| On demand exercise
Videos |
To increase ability to engage in physical
activity To increase strength, flexibility, balance and aerobic capacity. To increase confidence in ability to move and engage in physical activity To encourage physical activity outside of live sessions. |
COM-B
Self-Efficacy |
Demonstration of the Behaviour
Instruction on how to perform a behaviour Behavioural practice/rehearsal Body changes |
| Other on demand videos;
breathing technique, mindfulness |
To provide advice and education on relevant
topics. To provide associated skills/behaviours to promote engagement in physical activity To increase confidence in ability to move and engage in physical activity |
COM-B
Self-Efficacy |
Demonstration of the Behaviour
Instruction on how to perform a behaviour Behavioural practice/Rehearsal Distraction |
Session 1: Introduction, expectations, motivation and goal setting
Session 2: Fear avoidance and pacing
Session 3: Recovery and sleep, sleep management strategies
Session 4: Management of emotions (perceived stigma, mood/unhelpful thoughts)
Session 5: Understanding stress and anxiety, and management strategies
Session 6: Managing setbacks and long-term behaviour change and future goals.
Behavioural support videos
Feedback from our patient partners and intervention practitioners suggested potential benefit of having a short video or conversation where topics could be explored and viewed during the group sessions. We developed short introductory videos for each of the six group support topics. The videos featured discussions between the trial health psychologist and patient partners, filmed and edited by a professional production company. Practitioners played the relevant video at the start of each group support session with the intention that participants may recognise patterns of behaviour in themselves, thus stimulating support group discussion.
Intervention fidelity: practitioner training and quality control
To ensure standardisation of intervention delivery, all REGAIN practitioners completed a full day of training. This included practical and theoretical components, delivered by a clinical exercise research fellow and health psychologist. Guidance was provided on delivery of behavioural education sessions, motivational interviewing techniques, and group facilitation skills. All practitioners completed an assessment after training, to gauge readiness to deliver the intervention and/or the need for further training or support. Practitioners were provided with comprehensive written instruction manuals, and met monthly with a senior health psychologist and other members of the intervention delivery team for ongoing support, advice and troubleshooting. All intervention components were within the scope of normal practice for the clinicians involved. The REGAIN intervention was designed for delivery by NHS clinical exercise physiologists or physiotherapists. All practitioners were subject to regular quality control reviews conducted by an independent health psychologist, clinical exercise physiologist, and qualitative researcher using pre-determined checklist criteria. This ensured that exercise and behavioural support sessions were delivered in a standardised manner. All online sessions were recorded for independent review as part of a separate process evaluation.
Safety
Supervised sessions were led by practitioners experienced in the assessment, prescription, and delivery of exercise for multi-morbid clinical populations. Pre-exercise session online poll questions were completed by participants to capture any adverse events experienced since the previous supervised session. Practitioners also ended each session by inquiring about any symptoms or adverse events the participants may have experienced. Participants with any issues were asked to remain online after the session or were contacted by telephone or email to explore further. If a participant failed to attend an intervention appointment, the practitioner attempted to contact them via telephone or email to ascertain their welfare.
Exercise carries a very small theoretical risk of complications. All participants were assessed during the one-to-one consultation for any underlying health conditions or severe complications related to COVID-19. Participants were excluded from the study at the eligibility stage where exercise was clearly contraindicated, as assessed by a clinical member of the research team. A further assessment was undertaken by the REGAIN practitioner, through discussion with the patient about their current health, at the time of the initial online intervention assessment. During all group online exercise and support sessions, a second practitioner (‘co-pilot’) was immediately available online to assist with any emergencies, or if a participant became unresponsive or left the session without prior notification.
Regulatory compliance
To ensure compliance with appropriate confidentiality and data protection regulation, the proposed online intervention delivery platform and associated data storage facilities were rigorously reviewed and approved by organisational Information Governance committees, further to submission of a comprehensive Data Protection Impact Assessment.
Discussion
Regular physical activity can benefit people recovering from illness by increasing cardiorespiratory fitness and muscle strength, and reducing breathlessness. However, overly vigorous or prolonged activity without adaptation for ability or adequate rest periods can be detrimental to recovery and motivation, particularly for people with post-viral fatigue. It is important to mediate the psychosocial obstacles to activity and include intervention components designed to reduce anxiety and improve confidence, thus supporting people to regain physical strength, mobility, and independence. Provision of psychological support has become more challenging due to online delivery and differing levels of IT literacy. Hence, during development and pre-pilot testing, it was consistently demonstrated that our intervention would need to be as accessible and well supported as possible to avoid poor uptake and maintain adherence.
The introduction of an hour-long one-to-one consultation prior to the group sessions, a ‘co-pilot’ facilitator during the exercise sessions, and a comprehensive printed participant workbook aimed to address participants’ concerns about their condition and any additional fear of engaging with digital technology. During the pre-pilot phase, we discovered that not only did the support sessions enhance engagement with the exercise sessions, but equally, the exercise sessions enhanced engagement with the support sessions. that the opposite was also true. We found substantial unmet need for this patient group in being able to talk about their traumatic experiences in hospital with COVID-19, and their need to validate their ongoing problems since discharge. Our patient stakeholders expressed their desire to return to activities of normal living, (e.g., returning to work, walking to collect their children from school), or resume basic domestic chores at home. This required not only improved aerobic endurance and muscle strength, but also the knowledge, confidence and skills to cope with the inevitable peaks and troughs of recovery. Exercise practitioners also expressed their desire to improve their own group facilitation skills to best support the complex emotional needs of patients traumatised by COVID-19 and hospitalisation. The final fully manualised complex intervention for the REGAIN trial was co-produced with patients, lay people and healthcare professionals, and has been rolled out for testing in the REGAIN randomised controlled trial.
Conclusion
The REGAIN trial will be the largest study to-date to test whether online group exercise rehabilitation and psychological support delivered by NHS professionals is clinically and cost-effective for people with long-COVID symptoms more than three months after hospitalisation, when compared to best practice usual care. The REGAIN intervention, developed with extensive patient and stakeholder engagement, could be incorporated into existing NHS rehabilitation programmes, should it prove to be clinically and cost-effective for people with long-COVID.
Acknowledgements
We thank the wonderful group of people with long-COVID who participated fully in the development of the intervention at a time when their health and wellbeing was significantly impacted by COVID-19 – Elaine Fairbrother, Zoe Noakes, Bogdan Zutic, Helen Atherton, Lee Austin, Tom Forsyth, Anne Bush, Alan Bush, Patrick Sawdon. Also, our intervention team at Atrium Health – Jonathon Prosser, Lee Tompkins, Scott McGuire, Grace Lobley, Francesca Denton, David Montgomery.
Funding Statement
This research was funded by the National Institute for Health Research Health Technology Assessment Programme: COVID-19 Recovery & Learning (NIHR132046).
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
[version 2; peer review: 2 approved]
Data availability
Underlying data
Dryad: REGAIN trial intervention development process evaluation data, https://doi.org/10.5061/dryad.n8pk0p30r 26 .
This project contains the following underlying data:
REGAIN_PPI_feedback_on_behavioural_component_and_practitioner_manual.doc
Live_online_exercise_session.docx
Data are available under the terms of the Creative Commons Zero "No rights reserved" data waiver (CC0 1.0 Public domain dedication).
References
- 1. Office for National Statistics: Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK 5. 2023. Reference Source
- 2. Higgins V, Sohaei D, Diamandis EP, et al. : COVID-19: from an acute to chronic disease? Potential long-term health consequences. Crit Rev Clin Lab Sci. 2021;58(5):297–310. 10.1080/10408363.2020.1860895 [DOI] [PubMed] [Google Scholar]
- 3. Ladds E, Rushforth A, Wieringa S, et al. : Persistent symptoms after Covid-19: qualitative study of 114 "long Covid" patients and draft quality principles for services. BMC Health Serv Res. 2020;20(1): 1144. 10.1186/s12913-020-06001-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mahase E: Covid-19: What do we know about "long covid"? BMJ. 2020;370: m2815. 10.1136/bmj.m2815 [DOI] [PubMed] [Google Scholar]
- 5. Evans RA, McAuley H, Harrison EM, et al. : Physical, cognitive, and mental health impacts of COVID-19 after hospitalisation (PHOSP-COVID): a UK multicentre, prospective cohort study. Lancet Respir Med. 2021;9(11):1275–1287. 10.1016/S2213-2600(21)00383-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. NIHR: Themed Review: Living with Covid19 - Second review.NIHR;2021. Reference Source
- 7. National Institute for Health and Care Excellence (NICE) SIGNS, Royal College of General Practitioners (RCGP): COVID-19 rapid guideline: managing the long-term effects of COVID-19. [PubMed]
- 8. NHS England: Your COVID Recovery. Reference Source
- 9. Fugazzaro S, Contri A, Esseroukh O, et al. : Rehabilitation Interventions for Post-Acute COVID-19 Syndrome: A Systematic Review. Int J Environ Res Public Health. 2022;19(9): 5185. 10.3390/ijerph19095185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. McCarthy B, Casey D, Devane D, et al. : Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015;2015(2): CD003793. 10.1002/14651858.CD003793.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lau HMC, Ng GYF, Jones AYM, et al. : A randomised controlled trial of the effectiveness of an exercise training program in patients recovering from severe acute respiratory syndrome. Aust J Physiother. 2005;51(4):213–9. 10.1016/s0004-9514(05)70002-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. McGregor G, Sandhu H, Bruce J, et al. : Rehabilitation Exercise and psycholoGical support After covid-19 InfectioN' (REGAIN): a structured summary of a study protocol for a randomised controlled trial. Trials. 2021;22(1):8. 10.1186/s13063-020-04978-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Skivington K, Matthews L, Simpson SA, et al. : A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ. 2021;374: n2061. 10.1136/bmj.n2061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rhon DI, Fritz JM, Kerns RD, et al. : TIDieR-telehealth: precision in reporting of telehealth interventions used in clinical trials - unique considerations for the Template for the Intervention Description and Replication (TIDieR) checklist. BMC Med Res Methodol. 2022;22(1):161. 10.1186/s12874-022-01640-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Liu K, Zhang W, Yang Y, et al. : Respiratory rehabilitation in elderly patients with COVID-19: A randomized controlled study. Complement Ther Clin Pract. 2020;39: 101166. 10.1016/j.ctcp.2020.101166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Larun L, Brurberg KG, Odgaard-Jensen J, et al. : Exercise therapy for chronic fatigue syndrome. Cochrane Database Syst Rev. 2017;4(4): CD003200. 10.1002/14651858.CD003200.pub7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ngai JC, Ko FW, Ng SS, et al. : The long-term impact of severe acute respiratory syndrome on pulmonary function, exercise capacity and health status. Respirology. 2010;15(3):543–50. 10.1111/j.1440-1843.2010.01720.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Stussman B, Williams A, Snow J, et al. : Characterization of Post-exertional Malaise in Patients With Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Front Neurol. 2020;11: 1025. 10.3389/fneur.2020.01025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kop WJ: Biopsychosocial Processes of Health and Disease During the COVID-19 Pandemic. Psychosom Med. 2021;83(4):304–308. 10.1097/PSY.0000000000000954 [DOI] [PubMed] [Google Scholar]
- 20. Chakrawarty A, Ranjan P, Klanidhi KB, et al. : Psycho-social and behavioral impact of COVID-19 on middle-aged and elderly individuals: A qualitative study. J Educ Health Promot. 2021;10:269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Michie S, van Stralen MM, West R: The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. 10.1186/1748-5908-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bandura A: Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. 10.1037//0033-295x.84.2.191 [DOI] [PubMed] [Google Scholar]
- 23. Copeland L, McNamara R, Kelson M, et al. : Mechanisms of change within motivational interviewing in relation to health behaviors outcomes: A systematic review. Patient Educ Couns. 2015;98(4):401–11. 10.1016/j.pec.2014.11.022 [DOI] [PubMed] [Google Scholar]
- 24. Borek AJ, Abraham C: How do Small Groups Promote Behaviour Change? An Integrative Conceptual Review of Explanatory Mechanisms. Appl Psychol Health Well Being. 2018;10(1):30–61. 10.1111/aphw.12120 [DOI] [PubMed] [Google Scholar]
- 25. British Psychological Society: Guidance for the public on the mental health and wellbeing aspects of coronavirus (COVID-19).
- 26. McGregor G: REGAIN trial intervention development process evaluation data. Dryad. [Dataset],2023. 10.5061/dryad.n8pk0p30r [DOI]