Abstract
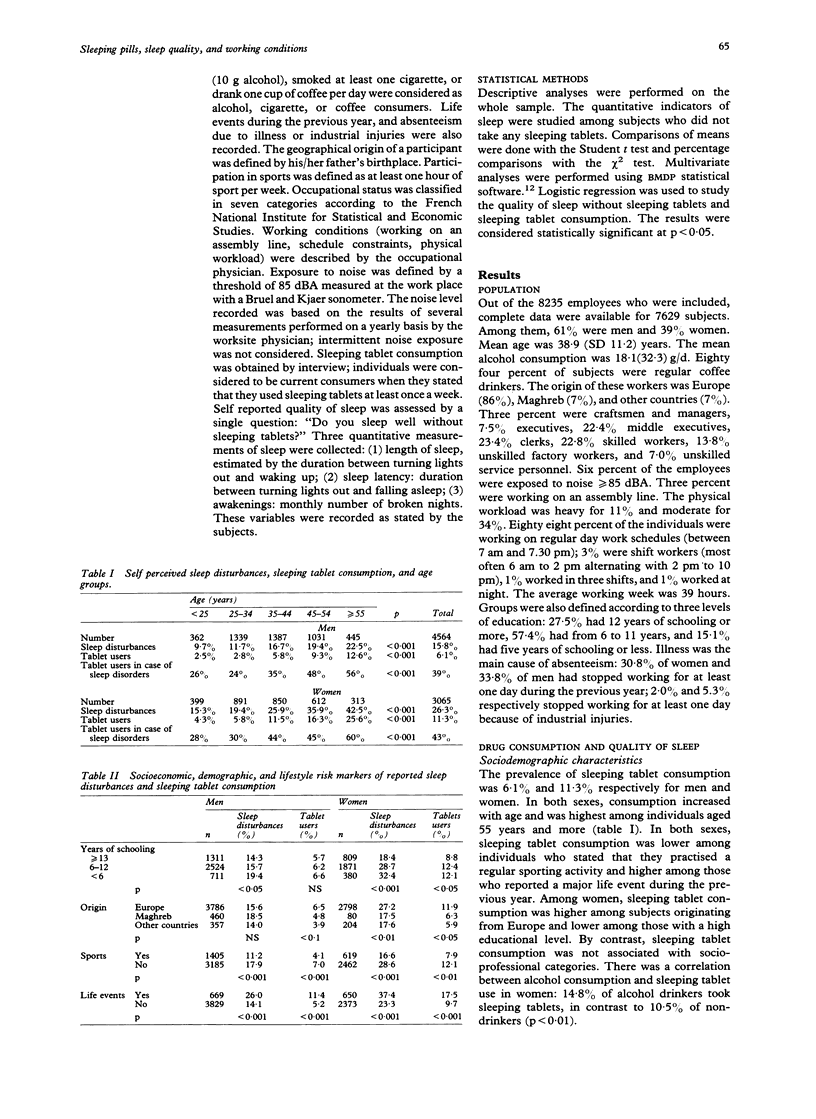
STUDY OBJECTIVE--The aim was to assess the frequency of sleep disorders in relation to working conditions. DESIGN--This was a cross sectional study. Data were collected prospectively, on a standardised form, by 13 occupational physicians. The quality of sleep was assessed by self perceived sleep disturbances and consumption of sleeping tablets. Working conditions were described by the worksite physician as well as by the participants. SETTING--2769 small or medium sized firms in the Paris area. PARTICIPANTS--A random sample of 7629 wage earners was studied. Among the participants, 61% were men and 39% women; 44% were blue collar workers. MAIN RESULTS--The prevalence of sleeping tablet consumption was 6.1% and 11.3% respectively for men and women. Sixteen percent of men and 26% of women stated that they had sleep disturbances (p < 0.001). In both sexes, drug consumption and sleep disturbances increased with age and were highest among individuals aged 55 years and more. No association between working conditions (exposure to noise, assembly line working, or physical workload) and sleep disturbances or drug consumption was found. Sleeping tablet consumption was higher among subjects reporting a bad atmosphere at work; the same was true for men with little interest in their job and for women working under time pressure. For both sexes, subjects reporting any of these conditions were more likely to report sleep disturbances. CONCLUSIONS--A high prevalence of self reported sleep problems and related drug consumption was observed. Physical working conditions were not related to the quality of sleep in contrast to perceived job conditions. The results suggest that sleep quality might be a useful health indicator for the occupational physician.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bixler E. O., Kales A., Soldatos C. R., Kales J. D., Healey S. Prevalence of sleep disorders in the Los Angeles metropolitan area. Am J Psychiatry. 1979 Oct;136(10):1257–1262. doi: 10.1176/ajp.136.10.1257. [DOI] [PubMed] [Google Scholar]
- Bourbonnais R., Vinet A. L'absence du travail comme indicateur de santé: signification, mesures et conditions d'utilisation. Rev Epidemiol Sante Publique. 1989;37(2):173–182. [PubMed] [Google Scholar]
- Cafferata G. L., Meyers S. M. Pathways to psychotropic drugs. Understanding the basis of gender differences. Med Care. 1990 Apr;28(4):285–300. doi: 10.1097/00005650-199004000-00001. [DOI] [PubMed] [Google Scholar]
- D'Hoore W., D'Hoore K. Analyse des relations entre les données polysomnographiques et l'évaluation subjective du sommeil dans un groupe de sujets normaux. Encephale. 1990 Sep-Oct;16(5):383–388. [PubMed] [Google Scholar]
- Folkard S. Shift work--a growing occupational hazard. Occup Health (Lond) 1989 Jul;41(7):182-4, 186. [PubMed] [Google Scholar]
- Ford D. E., Kamerow D. B. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989 Sep 15;262(11):1479–1484. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- Frese M., Harwich C. Shiftwork and the length and quality of sleep. J Occup Med. 1984 Aug;26(8):561–566. doi: 10.1097/00043764-198408000-00008. [DOI] [PubMed] [Google Scholar]
- Habte-Gabr E., Wallace R. B., Colsher P. L., Hulbert J. R., White L. R., Smith I. M. Sleep patterns in rural elders: demographic, health, and psychobehavioral correlates. J Clin Epidemiol. 1991;44(1):5–13. doi: 10.1016/0895-4356(91)90195-f. [DOI] [PubMed] [Google Scholar]
- Hedouin M., Lagrange T., Leroy C. Relation entre l'étude objective des éveils à l'EEG et l'auto-observation du sujet au réveil. Rev Electroencephalogr Neurophysiol Clin. 1981 Sep;11(1):110–115. doi: 10.1016/s0370-4475(81)80041-x. [DOI] [PubMed] [Google Scholar]
- Jenkins R. Minor psychiatric morbidity in employed young men and women and its contribution to sickness absence. Br J Ind Med. 1985 Mar;42(3):147–154. doi: 10.1136/oem.42.3.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karacan I., Thornby J. I., Anch M., Holzer C. E., Warheit G. J., Schwab J. J., Williams R. L. Prevalence of sleep disturbance in a primarily urban Florida County. Soc Sci Med. 1976 May;10(5):239–244. doi: 10.1016/0037-7856(76)90006-8. [DOI] [PubMed] [Google Scholar]
- Mellinger G. D., Balter M. B., Uhlenhuth E. H. Insomnia and its treatment. Prevalence and correlates. Arch Gen Psychiatry. 1985 Mar;42(3):225–232. doi: 10.1001/archpsyc.1985.01790260019002. [DOI] [PubMed] [Google Scholar]
- Rahman A. Workers' sleep quality as determined by shift system and demographic factors. Int Arch Occup Environ Health. 1988;60(6):425–429. doi: 10.1007/BF00381390. [DOI] [PubMed] [Google Scholar]


