Abstract
Introduction:
Spinal tuberculosis (STB) accounts for 1% of all tuberculosis (TB) cases and 50% of skeletal TB. The classic presentation is a paradiscal involvement leading to the destruction of bodies, progressive kyphosis that can end with neurological weakness. The advent of magnetic resonance imaging (MRI) has made detection early but at the same time, we find multilevel involvement which can be continuous/noncontinuous.
Case Report:
A 26-year-old male, non-alcoholic, non-smoker presented with complete paraplegia involving the bladder and bowel. His clinical examination did not show any gibbus. He was started on empirical antitubercular therapy and then referred to us as he failed to show improvement. An MRI of the spine showed extensive long-segment continuous spinal involvement with epidural abscess. The patient was taken for surgery with posterior decompression and instrumentation which was proven to be TB. He received complete treatment of 1 year and had complete recovery of his sensory and incomplete recovery of motor of lower limbs (became a wheelchair ambulator) with regain of bowel and bladder control at the end of treatment.
Conclusion:
This case report revealed that long-segment continuous STB without extensive destruction is atypical presentation. The clinical findings of paraplegia helped us to evaluate and clinch the diagnosis on MRI. However, the prognosis of rapid paraplegia remains guarded and patient had partial recovery of motor so he could become wheel chair ambulator only.
Keywords: Spinal tuberculosis, long segment, continuous, magnetic resonance imaging
Learning Point of the Article:
Long-segment tuberculosis of spine with involvement of nearly ten spinal segments without much deformity but paraplegia has not been reported previously.
Introduction
Spinal tuberculosis (STB) or the Pott’s disease is one of the most frequent extrapulmonary forms of tuberculosis (TB) accounting for about 1% of all TB cases and 50% of skeletal TB cases [1]. The classic radiological finding is a paradisical involvement (i.e., disk space and the two adjacent vertebral bodies) leading to the destruction of bodies and progressive kyphosis that can end with neurological weakness [2]. STB is common in an endemic area and nowadays with the advent of better imaging modalities such as magnetic resonance imaging (MRI), multiple-level involvement is seen [3, 4]. Long-segment multilevel continuous involvement such as ten vertebral bodies has not been reported.
Case Report
A 26-year-old male, non-alcoholic, non-smoker presented to our outpatient department with paraplegia in both legs for the past month. There was also complete loss of sensation below xiphisternum with loss of bladder and bowel control and paresthesia of both legs for the past 2 months. The onset of neurological weakness was sudden which had progressed to a present state in about 3–5 days’ time. He gave a history of intermittent episodes of low-grade fever; with typical evening rise of temperature and also associated with purulent cough, there was no deformity of the spine. He was started empirical anti-tubercular treatment (ATT) at peripheral hospital for the past 3 weeks. On examination, he was complete paraplegia (ASIA A) with Grade 1 bed sore in the sacral area.
The patients’ blood parameters included testing revealed a raised ESR of 90 mm/h, C-reactive protein of 35.62 mg/L, and interleuikin-6 of 40.2 pg/mL with lymphocytosis. The serology for human immunodeficiency virus (HIV) and other viral markers was negative. An initial X-ray was unremarkable, and hence, an urgent screening MRI of whole spine was done (Fig. 1a). The MRI showed a large segment spinal involvement of ten continuous vertebral bodies with anterior prevertebral, paravertebral, and epidural abscess extending from D3-12 (Fig. 1b-d) and involvement of bilateral lung parenchyma (Fig. 1e and f). The patient was counseled for emergency decompression. Long posterior instrumentation was from D3 to L1. Long midline decompression was done (D4-11) (Fig. 2). The upper dorsal cord was seen to be completely engulfed with granulation tissue which was carefully excised piecemeal and sent for culture, GeneXpert testing, and biopsy. About 20 mL of pus was also drained. The tissue came positive Mycobacterium tuberculosis (MTB) and rifampicin resistance was not detected. The culture also showed growth of MTB. The patient continued to receive ATT for complete 1 year. At the end of a year, he was ambulatory on wheel chair with a power 3/5 (MRC grade) in lower limbs with complete sensory recovery and recovery of bladder/bowel. His blood parameters had come to normal but he refused for a repeat MRI for documentation of radiological healing. The ATT was stopped.
Figure 1.

The X-ray of spine shows no extensive damage/kyphosis (a); magnetic resonance imaging of the spine shows extensive involvement of the vertebral bodies in T2-weighted (b); T1-weighted (c); and fat-suppressed T2-weighted images with compression of cord due to epidural abscess (d); the computed topographic scan (done post-optatively) also shows involvement of bilateral lung parenchyma (e and f).
Figure 2.
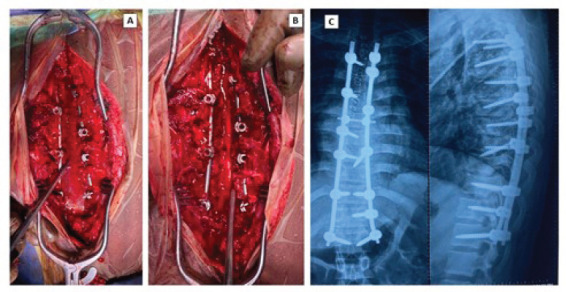
Intraoperative images showing long-segment midline decompression (a), showing a free thoracic spinal cord (b); final radiological imaging showing multilevel fixation with pedicle screw rod construct.
Discussion
STB is endemic in certain parts of the world but there is resurgence even in the developed world due to infection with HIV. This makes awareness about STB mandatory, especially with multi-level presentation. Typically, there is continuous involvement and authors have reported up to 5 segments involvement. Jain et al. have reported a mean number of vertebrae involved of 3.29 ± 0.86 [4]. Shen et al. also have reported multilevel STB and found that most are 3–4 level involvement with only one case of six-level infection [5]. Atypical presentation includes non-contagious multilevel involvement of STB [6]. Authors have reported this to be rate of 17–71% in their series [6, 7], a lot can be attributed to early detection and especially a whole spine screening algorithm of spine with an MRI [3, 7]. Long-segment multilevel continuous involvement such as ten vertebral bodies has not been reported.
However, most multilevel STBs are not multidrug-resistant TB as was our case. Multiple vertebrae involvement causes collapse of vertebrae [8]. Jain reported that the development of kyphosis in TB spine is a rule rather than exception [9]. Our patient had ten vertebral body involvement with paraspinal and epidural abscess that caused rapid onset paraplegia. The other uniqueness of our case has been that patient had no immunosuppression (negative for HIV) but still had multiorgan involvement (concomitant pulmonary TB and STB) and the body destruction was minimal even with such a severe involvement. Dharmalingam had earlier reported that 2/3rd STB patients have coexistent pulmonary TB [10]. This also has anesthetic implication if patient is planned for surgery and especially in prone position. Rapid molecular techniques such as GeneXpert MTB/ Rif assay have made the detection of MTB in STB easy, fast, and simple [11]. However, the main diagnostic dilemma in STB remains is sample collection from deeper sites, and paucibacillary nature of disease [12]. Chemotherapy is treatment for STB and surgery is indicated in selective cases [4] Nevertheless, recovery after rapid-onset paraplegia remains guarded [13]. Garg et al. studied the prognostic factors in patients treated for STB [14]. The authors concluded that the three most important factors responsible for poor prognosis are duration of illness (>6 months 0, extensive involvement (>3 segments) and cord compression. Dunn et al. have noted that rapid paraplegia due to vascular involvement (tubercular endarteritis casing infraction of spinal cord) also carries a poor prognosis [15].
Conclusion
Long-segment STB without clinical deformities is difficult to diagnose clinically. MRI is helpful for early diagnosis. Management of paraplegia needs early decompression as in our case. However, the prognosis is guarded.
Clinical Message.
Multi-level STB is atypical presentation of STB. With early use of MRI in the diagnosis of STB, there is an increased incidence of multi-level STB which can be contiguous or non-contagious. Deformity in STB is a rule but here, we presented a case of long-segment continuous STB without much deformity but extensive neurological deficit.
Biography




Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that informed consent was obtained from the patient for publication of this case report
References
- 1.Wang LN, Wang L, Liu LM, Song YM, Li Y, Liu H. Atypical spinal tuberculosis involved noncontiguous multiple segments:Case series report with literature review. Medicine (Baltimore) 2017;96:e6559. doi: 10.1097/MD.0000000000006559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Turgut M. Spinal tuberculosis (Pott's disease):Its clinical presentation, surgical management, and outcome. A survey study on 694 patients. Neurosurg Rev. 2001;24:8–13. doi: 10.1007/pl00011973. [DOI] [PubMed] [Google Scholar]
- 3.Garg RK, Somvanshi DS. Spinal tuberculosis:A review. J Spinal Cord Med. 2011;34:440–54. doi: 10.1179/2045772311Y.0000000023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jain M, Sahu RN, Behera S, Rana R, Tripathy SK, Pattnaik A. Standalone instrumented posterior approach used as universal approach for tuberculosis spondylodiscitis. J Neurosci Rural Pract. 2019;10:225–33. doi: 10.4103/jnrp.jnrp_294_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shen X, Huang X, Xiao S, Liu H, Zhang Y, Xiang T, et al. Surgical treatment of selected patients with multilevel contiguous thoracolumbar spinal tuberculosis by only posterior instrumentation without any bone fusion. Int J Clin Exp Med. 2015;8:18611–9. [PMC free article] [PubMed] [Google Scholar]
- 6.Kaila R, Malhi AM, Mahmood B, Saifuddin A. The incidence of multiple level noncontiguous vertebral tuberculosis detected using whole spine MRI. J Spinal Disord Tech. 2007;20:78–81. doi: 10.1097/01.bsd.0000211250.82823.0f. [DOI] [PubMed] [Google Scholar]
- 7.Polley P, Dunn R. Noncontiguous spinal tuberculosis:Incidence and management. Eur Spine J. 2009;18:1096–101. doi: 10.1007/s00586-009-0966-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pawar UM, Kundnani V, Agashe V, Nene A, Nene A. Multidrug-resistant tuberculosis of the spine--is it the beginning of the end?A study of twenty-five culture proven multidrug-resistant tuberculosis spine patients. Spine (Phila Pa 1976) 2009;34:E806–10. doi: 10.1097/BRS.0b013e3181af7797. [DOI] [PubMed] [Google Scholar]
- 9.Jain AK. Tuberculosis of the spine:A fresh look at an old disease. J Bone Jt Surg Br. 2010;92-B:905–13. doi: 10.1302/0301-620X.92B7.24668. [DOI] [PubMed] [Google Scholar]
- 10.Dharmalingam M. Tuberculosis of the spine-the Sabah experience. Epidemiology, treatment and results. Tuberculosis (Edinb) 2004;84:24–8. doi: 10.1016/j.tube.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 11.Karthek V, Bhilare P, Hadgaonkar S, Kothari A, Shyam A, Sancheti P, et al. Gene Xpert/MTB RIF assay for spinal tuberculosis- sensitivity, specificity and clinical utility. J Clin Orthop Trauma. 2021;16:233–8. doi: 10.1016/j.jcot.2021.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mohanty M, Mishra B, Jain M, Puthiyapura LK. Diagnostic role of Xpert-MTB RIF assay in osteoarticular tuberculosis:A retrospective study. World J Orthop. 2022;13:289–96. doi: 10.5312/wjo.v13.i3.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jain AK, Kumar J. Tuberculosis of spine:Neurological deficit. Eur Spine J. 2013;22(Suppl 4):624–33. doi: 10.1007/s00586-012-2335-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garg RK, Raut T, Malhotra HS, Parihar A, Goel M, Jain A, et al. Evaluation of prognostic factors in medically treated patients of spinal tuberculosis. Rheumatol Int. 2013;33:3009–15. doi: 10.1007/s00296-013-2841-x. [DOI] [PubMed] [Google Scholar]
- 15.Dunn R, Zondagh I, Candy S. Spinal tuberculosis:Magnetic resonance imaging and neurological impairment. Spine (Phila Pa 1976) 2010;36:469–73. doi: 10.1097/brs.0b013e3181d265c0. [DOI] [PubMed] [Google Scholar]


