Abstract
Objective:
The present study sought to characterize the temporal patterns of binge eating and theorized maintenance factors among individuals with binge-eating disorder (BED).
Method:
Ecological momentary assessment of 112 individuals and mixed-effects models were used to characterize the within- and between-day temporal patterns of eating behaviors (binge eating, loss of control only eating, and overeating only), positive and negative affect, emotion regulation difficulty, and food craving.
Results:
Risk for binge eating and overeating only was highest around 5:30 p.m., with additional binge-eating peaks around 12:30 p.m. and 11:00 p.m. In contrast, loss of control eating without overeating was more likely to occur before 2:00 p.m. Risk for binge eating, loss of control only eating, and overeating only did not vary across days in the week. There was no consistent pattern of change in negative affect throughout the day, but it decreased slightly on the weekend. Positive affect showed a decrease in the evenings and a smaller decrease on the weekend. The within-day patterns of food craving, and to some extent emotion regulation difficulty, resembled the pattern of binge eating, with peaks around meal times and at the end of the night.
Discussion:
Individuals with BED appear most susceptible to binge-eating around dinner time, with heightened risk also observed around lunch time and late evening, though the effects were generally small. These patterns appear to most strongly mimic fluctuations in craving and emotion dysregulation, although future research is needed to test the temporal relationships between these experiences directly.
Keywords: binge-eating disorder, affect, craving, emotion regulation, ecological momentary assessment, time of day, day of week, diurnal rhythm
Binge-eating disorder (BED) is characterized by recurrent episodes of objective overeating accompanied by a sense of having lost control over one’s eating, without the presence of inappropriate compensatory behaviors (American Psychiatric Association, 2013). BED impacts approximately 3.5% of women and 2.0% of men, and is associated with psychosocial impairment, as well as significant psychiatric and medical comorbidity (Hudson et al., 2007; Udo & Grilo, 2018). Current interventions for BED have demonstrated inadequate effectiveness, as 50% of patients do not achieve full remission of binge-eating symptoms (Linardon, 2018). Thus, improved understanding of the maintenance factors for BED is imperative, as this may significantly contribute to the enhancement of clinical interventions for the disorder.
Theoretical models of eating disorders identify several possible factors that may perpetuate binge-eating symptoms. For example, the affect regulation model (Heatherton & Baumeister, 1991) suggests that uncomfortable affective states (e.g., low positive affect, high negative affect) may increase risk for binge-eating episodes, which in turn may serve to regulate affect. Similarly, researchers have suggested that difficulties regulating emotions may increase risk for eating pathology (Lavender et al., 2015). Finally, models drawn from the substance use literature suggest that food craving may predict subsequent engagement in binge eating (Kober & Boswell, 2018; Verzijl et al., 2022). Several studies using ecological momentary assessment (EMA; a method that allows for repeated assessment of participants’ experiences in the natural environment) among individuals with binge-eating pathology provide support for these theories, indicating that worsening mood, emotion regulation difficulties, and heightened food craving all predict an increased likelihood of binge eating (Schaefer et al., 2020, 2023; Svaldi et al., 2019; J. A. Wonderlich et al., 2017; Zunker et al., 2011).
What is less clear, however, is how these experiences vary across time of day and across days in the week among individuals with BED. Understanding the temporal patterning of binge-eating episodes and their theorized maintenance factors is likely to have important implications for both clinical interventions and research. For example, clarifying the times of day or days in the week in which binge-eating episodes are most frequent may help orient clinicians and patients to the time periods during which patients are most at risk for binge eating. Further, clarifying the temporal patterns of affect, emotion regulation difficulties, and food craving may help clinicians and patients to better plan for and manage circumstances during which patients are more susceptible to binge eating. Finally, this information could be used to inform future studies using EMA or ecological momentary interventions (i.e., treatments that are provided to individuals in their natural environment, and are often sent at predetermined times via electronic devices), by allowing researchers to target their assessments and/or interventions during time periods of increased risk.
Prior work using EMA among individuals with bulimia nervosa (BN) (Smyth et al., 2009) and anorexia nervosa (AN) (Lavender et al., 2016) suggests both similarities and differences in the temporal patterning of affect and eating disorder symptoms across distinct eating disorder diagnoses. In general, individuals with BN displayed greater variability in affect and eating disorder behaviors across hours of the day and days in the week than individuals with AN. For example, while affect tended to worsen towards the later hours of the day in BN (i.e., positive affect declined and negative affect increased), affect did not vary across time of day in AN. However, both groups exhibited the greatest frequency of eating disorder behaviors (i.e., binge eating for the BN group, binge eating and vomiting for the AN group) during the late evening hours (i.e., 7:00 pm to 9:00 pm). In day of the week analyses, eating disorder behaviors were more common on weekends than weekdays for individuals with BN, but did not vary by day in the AN group. While positive affect was generally higher during the weekdays for those with BN, the opposite was true for those with AN. Negative affect tended to be lowest during the weekend (i.e., Friday, Saturday, and Sunday), across both diagnostic groups.
In sum, evidence indicates that the frequency of eating disorder behaviors and associated psychological vulnerabilities may vary across the hours of the day and days of the week. Further, the temporal patterns of these experiences may vary across eating disorder diagnoses (i.e., AN and BN). However, to our knowledge, no study has yet examined these temporal patterns in BED. Therefore, the aim of the present study was to characterize the within- and between-day patterns of eating disorder behaviors and theorized maintenance factors among individuals with BED. Specifically, positive and negative affect, emotion regulation difficulties, food craving, and problematic eating episodes were tracked over the course of seven days using EMA in a BED sample. Binge eating (i.e., perceived overeating with loss of control), overeating only (i.e., perceived overeating without loss of control), and loss of control only eating (i.e., loss of control without perceived overeating) were each examined separately, as these types of eating episodes are commonly reported by individuals with BED and are associated with different patterns of psychological vulnerabilities (Berg et al., 2014). Explicit hypotheses regarding temporal patterns were not formulated, given the exploratory nature of this study. However, it was anticipated that binge eating would occur most frequently during the evening hours, given the consistency of this finding across both BN and AN samples (Lavender et al., 2016; Smyth et al., 2009).
Method
Participants
The data for this study were obtained from 112 individuals (93 female) who met criteria for BED based on the 5th edition of the Diagnostic Statistical Manual (DSM–5) (American Psychiatric Association, 2013) and were enrolled in, but had not yet begun, a randomized controlled trial for BED treatment (Peterson et al., 2020). Participants were between the ages of 18 and 65 and did not meet any of the following exclusion criteria: (a) unable to read English, (b) body mass index less than 21, (c) lifetime history of psychotic symptoms or bipolar disorder, (d) substance use disorder within 6 months of enrollment, (e) medical instability, (f) acute suicidality, (g) purging behavior (e.g., self-induced vomiting, misuse of laxatives or diuretics) more than once per month for the previous 3 months, (h) current diagnosis of DSM-5 BN, (i) medical condition impacting eating or weight (e.g., thyroid condition), (j) history of gastric bypass surgery, (k) currently pregnant or lactating, (l) currently receiving weight loss or eating disorder treatment, (m) use of medication impacting eating or weight (e.g., stimulants), and (n) psychotropic medication changes in the 6 weeks prior to enrollment. For participant demographic information, see Table 1. IRB approval for this study was obtained at both data collection sites and informed consent of all participants was obtained.
Table 1.
Participant Demographic Characteristics
| Characteristic | Statistics (total N=112) |
|---|---|
| Age (years), mean (SD) | 39.7 (13.4) |
| Female, n (%) | 92 (82.1%) |
| Caucasian, n (%) | 102 (91.1%) |
| Never married, n (%) | 58 (51.8%) |
| College degree, n (%) | 77 (68.8%) |
| Current SCID diagnosis, n (%) | |
| Mood | 13 (11.6%) |
| Anxiety | 22 (19.6%) |
| Lifetime SCID diagnosis, n (%) | |
| Mood | 64 (57.1%) |
| Anxiety | 42 (37.5%) |
| Substance abuse/ dependence | 44 (39.3%) |
| BMI (kg/ m2), mean (SD) | 35.1 (8.7) |
Notes. BMI = body mass index; SCID = Structured Clinical Interview for the Diagnostic and Statistical Manual, 5th edition.
Procedure
Participants were recruited from eating disorder clinics, community advertisements, and social media postings at two sites in the midwestern United States. After completing a brief eligibility screen, participants completed a baseline study visit where they completed structured clinical interviews to assess for eating disorder symptoms and comorbid psychopathology before completing a seven-day EMA protocol. The EMA surveys were obtained via smartphone using ReTAINE (Real-Time Assessment in the Natural Environment; see ReTAINE.org), and included signal-contingent and interval-contingent recordings. For signal-contingent surveys, five prompts were sent to participants each day, which were randomly distributed around five anchor points occurring between 8:00 a.m. and 10:00 p.m. For interval-contingent recordings, participants were asked to complete a self-initiated survey at the end of each day, before going to bed.
Structured Interviews
To establish a diagnosis of DSM-5 BED, the Eating Disorder Examination (EDE) version 16.0 (Fairburn et al., 2008) was administered by trained assessors. The Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Version (First et al., 1995) was also administered to evaluate comorbid DSM-IV diagnoses.
EMA Measures
Positive and Negative Affect
For the present analyses, we used the 10 items from the PANAS-Short Form (Thompson, 2007), which includes five items to measure positive affect – (a) determined, (b) attentive, (c) alert, (d) inspired, and (e) active – and five items to measure negative affect – (a) afraid, (b) nervous, (c) upset, (d) ashamed, and (e) hostile. The items were adapted to assess momentary affective experiences by asking participants to rate the degree to which they were currently experiencing each affective state (e.g., “How upset are you feeling right now?”) on a 1 (not at all) to 5 (extremely) Likert-type scale (Engel et al., 2013; Smyth et al., 2007). To create composite measures of positive and negative affect, we took the mean rating across positive and negative items, respectively. Based on a confirmatory factor analysis, we found that all five items significantly (all p-values < .001) loaded onto a single factor for both positive affect (within-person loadings: .58a, .70b, .65c, .51d, .53e; between-person loadings: .61a, .78b, .70c, .56d, .48e) and negative affect (within-person loadings: .29a, .35b, .57c, .41d, .27e; between-person loadings: .57a, .66b, .48c, .59d, .29e). Further, we found that measurement reliability was acceptable for positive affect (ω within-person = .86; ω between-person = .95) and negative affect (ω within-person = .80; ω between-person = .93) (Geldhof et al., 2014).
Emotion Regulation Difficulty
Emotion regulation difficulty was assessed using five items from the Modulate subscale of the state-based (Lavender et al., 2017) Difficulties in Emotion Regulation Scale (DERS) (Gratz & Roemer, 2004), which reflect current or recent difficulties modulating emotional and behavioral responses. On a 1 (not at all) to 5 (completely) Likert-type scale, participants indicated how the following statements applied to them in the moment: (a) “My emotions feel out of control”, (b) “I feel out of control”, (c) “My emotions feel overwhelming”, (d) “Difficulty controlling behaviors”, and (e) “Difficulty doing the things I need to do”. The mean rating across the five items was used to quantify Emotion Regulation Difficulty. Confirmatory factor analysis indicated that all five items significantly (all p-values < .001) loaded onto a single factor (within-person loadings: .71a, .57b, .72c, .43d, .45e; between-person loadings: .81a, .72 b, .81c, .61d, .67e) and that measurement reliability was acceptable (ω within-person = .86; ω between-person = .95) (Geldhof et al., 2014).
Craving
Craving was assessed using a single item (“I am craving food”) on a Likert-type scale ranging from 1 (not at all) to 5 (completely).
Binge Eating, Loss of Control Only, and Overeating Only Behaviors
Whenever participants reported an eating episode, they were asked to indicate how much time had passed between the current (automatically recorded) time and the time that the eating episode occurred. This allowed us to locate the eating episode in time, relative to the timing of the signal. They were also asked to indicate the degree to which the episode was characterized by loss of control and perceived overeating. Loss of control was assessed with four items: (a) “While you were eating, to what extent did you feel a sense of loss of control?”, (b) “While you were eating, to what extent did you feel that you could not resist eating?”, (c) “While you were eating, to what extent did you feel that you could not stop eating once you had started?”, and (d) “While you were eating, to what extent did you feel driven or compelled to eat?”. Perceived overeating was assessed with two items: (a) “To what extent to do you feel that you overate?” and (b) “To what extent do you feel that you ate an excessive amount of food?”. Each item was rated on a Likert-type scale from 1 (not at all) to 5 (extremely). When an eating episode was rated as a 4 or higher on at least one loss of control item and at least one overeating item, it was categorized as a “Binge Eating” episode. When an eating episode was rated as a 4 or higher on at least one loss of control item, but rated as less than a 4 on both overeating items, the eating episode was categorized as a “Loss of Control Only Eating” episode. When an eating episode was rated as a 4 or higher on at least one overeating item, but rated as less than a 4 on each loss of control item, the eating episode was categorized as an episode of “Overeating Only”. This approach has been supported in previous EMA research conducted among individuals with binge-eating pathology (Berg et al., 2015; Goldschmidt et al., 2014; Schaefer et al., 2020; Wonderlich et al., 2015). The cutoff of 4 on loss of control and overeating items was selected because it represents one increment higher than the mid-point of the scale (i.e., 3) and was reasoned to represent significantly elevated levels of both perceived loss of control and overeating. Note that to confirm that dichotomizing loss of control and overeating scores (i.e., present or absent) did not obscure temporal patterns in continuous loss of control and overeating scores, we also conducted the time-of-day and day-of-week analyses on continuous measures of loss of control and overeating separately. Results from this analysis matched the results obtained in the primary, categorical analysis, and thus are not further reported in the manuscript.
Statistical Analysis
Mixed-effects models were used to test for linear, quadratic, and cubic effects of time-of-day and day-of-week. For all models, time-of-day was nested within day-of-week, and day-of-week was nested within individuals. Thus, for within-day analyses, random intercepts were included for individuals and day-of-week, while time-of-day was treated as a fixed effect (without a random slope). For the between-day analyses, random intercepts were included for individuals and time-of-day, while day-of-week was treated as a fixed effect (without a random slope). In addition, because participants had variable start days for the EMA protocol (e.g., starting on Monday or another day of the week), we included linear, quadratic, and cubic effects of “day-in-protocol” as control variables (fixed effects without a random slope) for the between-day analyses. Only EMA responses provided between 7:00 a.m. and 11:59 p.m., which accounted for 98.9% of all responses, were used for the analyses. For the day-of-week analyses, Monday was treated as the first day of the week (i.e., day-of-week 0). Similarly, the first day of the EMA protocol was treated as day-in-protocol 0 for the control variable.
Continuous outcomes (i.e., Positive Affect, Negative Affect, Emotion Control Difficulty, and Craving) were modeled using linear mixed effects models with first-order autoregressive covariance structures, and categorical outcomes (i.e., Binge Eating, Loss of Control Only Eating, Overeating Only) were modeled using generalized linear mixed effects models and binomial distributions. Time-of-day and day-of-week were treated as continuous predictors for the primary statistical analyses. For descriptive purposes, parallel models treated time-of-day and day-of-week categorically, providing estimated marginal means for all outcomes per hour and per day. To obtain the categorical measure of time-of-day, we binned measurements into 17 one-hour bins (7:00 a.m. - 7:59 a.m., 8:00 a.m. - 8:59 a.m., …, 11:00 p.m. - 11:59 p.m.). All analyses were conducted using the lme4 (Bates et al., 2015), lmerTest (Kuznetsova et al., 2017), and nlme (Pinheiro et al., 2022) packages in R version 4.2.1(R Core Team, 2022). Given the large number of tests being conducted, we set α = .005 for significance testing, in order to reduce the Type I error rate. Finally, within-person effect sizes were estimated using change in R2, comparing model R2 for a given effect (and any lower order effects) to a model with random intercepts only for within-day analyses, and comparing to a model with random intercepts and the control variable effects of day-in-protocol for between-day analyses (Rights & Sterba, 2020). For interpretation of these effect size estimates, an R2 of .02 is considered small, .13 medium, and .26 large (Cohen, 1988).
Results
On average, participants completed 76% of signal-contingent surveys and 52% of end-of-day surveys. A total of 3,096 surveys within the time frame used for the statistical analyses (7:00 a.m. – 11:59 p.m.) were obtained. Within this time frame, participants reported an average of 4.84 Binge Eating episodes (SD = 4.74), 3.75 Loss of Control Only Eating episodes (SD = 3.73), and 0.81 Overeating Only episodes (SD = 1.47) across the seven-day EMA protocol. The average per participant ratings for the remaining outcomes were: Positive Affect = 2.32 (SD = 0.68), Negative Affect = 1.56 (SD = 0.55), Emotion Regulation Difficulty = 1.80 (SD = 0.76), and Craving = 2.37 (SD = 0.77). See Tables 1 and 2 in the Supplementary Material for all model effects.
Temporal Patterns of Affect, Emotion Regulation Difficulty, and Craving
For the within-day analysis (see Figure 1), there were small to medium sized significant linear, t(2374) = −18.15, p < .001, R2 =.10, and quadratic, t(2374) = −12.83, p < .001, R2 = .15, effects on Positive Affect, reflecting that Positive Affect increased slightly across the morning and then declined relatively steeply beginning at around 2:00 p.m. There were no significant time-of-day effects on Negative Affect. There was a small but significant quadratic effect of time-of-day on Emotion Regulation Difficulty, t(2374) = −2.88, p = .004, R2 < .01, reflecting that difficulty in emotion regulation was highest between approximately 12:00 p.m. and 8:00 p.m. Finally, there were small but significant linear, t(2374) = −3.17, p = .002, R2 < .01, and quadratic, t(2374) = −6.61, p < .001, R2 = .02, effects on Craving, reflecting that Craving was highest between approximately 11:00 a.m. and 7:00 p.m., and then declined thereafter.
Figure 1. Significant Within-Day and Between-Day Temporal Patterns.
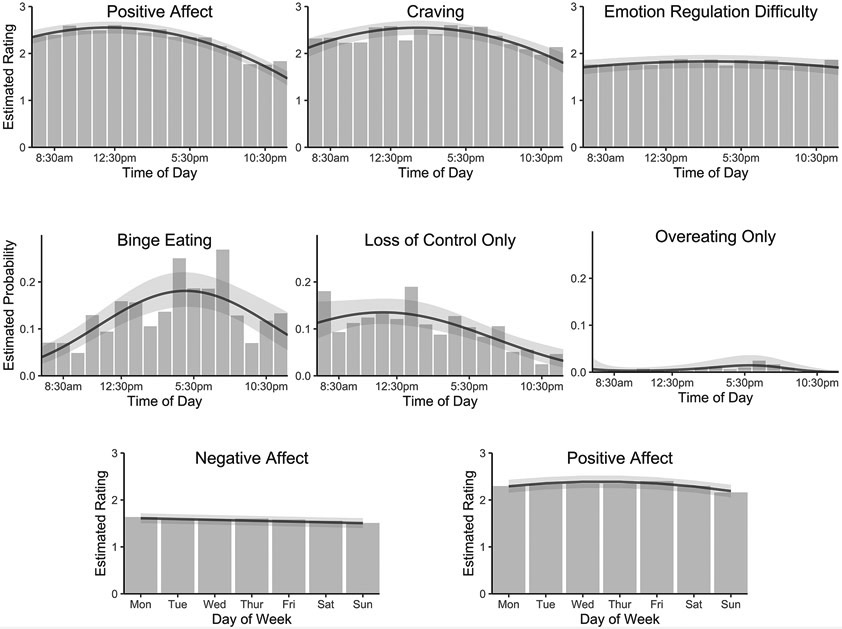
Note. The black line in each panel represents the model predictions based on statistically significant polynomial (linear, quadratic, cubic) effects of time-of-day or day-of-week. The shaded area around the line represents the 95% confidence interval. For the within-day plots, the vertical gray bars represent the estimated marginal means for each hour of the day when binning time into one-hour categories. For the between-day plots, the vertical gray bars represent the marginal means for each day of the week when the days are treated as categories.
For the between-day analysis (see Figure 1), there was a small but significant quadratic, t(89) = −3.21, p < .001, R2 = .02, effect on Positive Affect, reflecting that Positive Affect increased from Monday through Friday, and then decreased on the weekend. There was a small but significant linear effect of day-of-week on Negative Affect, t(89) = −3.68, p < .001, R2 = .01, reflecting that Negative Affect decreased slightly across the week. There were no significant day-of-week effects on Emotion Regulation Difficulty or Craving.
Temporal Patterns of Binge Eating, Loss of Control Only, and Overeating Only Behaviors
For the within-day analysis (see Figure 1), there were small but significant linear, z = 4.71, p < .001, R2 = .02, and quadratic, z = −5.01, p < .001, R2 = .05, effects of time-of-day on Binge Eating, reflecting that Binge Eating increased until peaking between 4:00 p.m. and 8:00 p.m., before again declining. There were small but significant linear, z = −5.00, p < .001, R2 = .02, and quadratic, z = −3.16, p = .002, R2 = .04, effects of time-of-day on Loss of Control Only Eating, reflecting that Loss of Control Only Eating generally increased throughout the morning until peaking between 1:00 p.m. and 2:00 p.m., and then declined across the rest of the day. Finally, there was a small but significant cubic effect, z = −2.94, p = .003, R2 = .10, of time-of-day on Overeating Only, reflecting that Overeating Only started low but dipped slightly across the first few hours of the day, before beginning to increase slightly at approximately 2:00 p.m., peaking between approximately 6:00 p.m. and 8:00 p.m., and then declining thereafter. To test if patterns of compliance might have influenced the temporal effects observed in the eating behavior variables, we conducted a pattern-mixture analysis (Hedeker & Gibbons, 1997), separating individuals into groups based on whether they responded to more signals in the first half of the day (before 2:00 p.m.) or in the second half of the day. The temporal effects did not significantly interact with this grouping variable, suggesting that the observed patterns did not depend on patterns of compliance.
For the between-day analysis (see Figure 1), there were no significant effects of day-of-week on Binge Eating, Loss of Control Only Eating, or Overeating Only.
Discussion
Previous research on individuals with AN and BN suggests that eating disorder behaviors and associated psychological vulnerabilities vary across the time of day and day of week (Lavender et al., 2016; Smyth et al., 2009). The present study is the first to examine these temporal patterns among a large sample of treatment-seeking individuals with BED using naturalistic assessment methods.
Although the effects were small, participants in the current sample were most likely to report loss of control only eating episodes in the morning and early afternoon (i.e., before 2:00 p.m.), while binge-eating episodes were most commonly reported during the afternoon and evening. The predominance of loss of control only episodes earlier in the day may reflect the fact that many individuals with BED attempt to restrict their intake during this time period (often due to reduced appetite and a desire to limit caloric intake) (de Young & Bottera, 2022). It is therefore possible that this increased dietary restraint contributes to individuals with BED feeling out of control, even when consuming small or “normal” amounts of food. Over the course of the day, binge-eating episodes became more common, with risk for binge-eating highest around dinner time (5:30 p.m.), and additional peaks occurring around lunch time (12:30 p.m.) and in the late evening (11:00 p.m.). Overeating only episodes were relatively uncommon (averaging around only one episode per week), perhaps because consuming larger amounts of food is typically linked with a sense of having lost control among individuals with BED (Telch et al., 1998). However, when simple overeating did occur, it was more likely to take place around 6:00 p.m. In contrast to these within-day patterns, none of the eating behaviors significantly varied across the week. Notably, the observation that risk for binge eating increased later in the day, but did not vary across the week, is consistent with previous research in AN and BN samples (Lavender et al., 2016; Smyth et al., 2009).
The most prominent temporal patterns in relevant psychological vulnerabilities were for positive affect and craving. Positive affect exhibited a small to moderate decrease in the late evening hours, and a small decrease on the weekends, consistent with patterns observed in BN. Food craving most closely resembled patterns of binge eating, exhibiting a small peak around mealtimes (i.e., 12:30 p.m. and 5:30 p.m.), with a slight increase at the end of the day (i.e., 11:00 p.m.). This pattern was also observed for emotion regulation difficulty, though the effect was smaller.
The current findings seem to provide mixed support for affect regulation models. For example, although positive affect declined in the late evening hours, when binge-eating episodes were relatively common, similar declines were not observed over the lunch hour and dinner time, when binge-eating episodes were also common. Further, despite clear changes in the likelihood of binge eating throughout the day, there was no consistent pattern of change in negative affect over this same timeframe. However, prior examination of the within-person temporal relationships between affect and binge-eating episodes within this sample indicated that increasing negative affect and decreasing positive affect predicted subsequent binge-eating episodes (Schaefer et al., 2020), providing strong support for affect regulation models and highlighting the importance of research examining these within-person temporal relationships at the momentary level.
It is important to acknowledge that although the current study is the first to examine the naturalistic temporal patterns of eating disorder behaviors and associated psychological vulnerabilities among a large sample of individuals with BED, it contains several notable limitations. First, the size of the effects were generally quite small and many effects were not statistically significant. This suggests that – on average – risk for problematic eating episodes (and experiences of worsening affect, craving, and emotion regulation ability) may not greatly vary across the course of the day or days in the week among individuals with BED. Importantly, aggregating data across all participants in the sample may obscure individual variability in patterns of risk across time. Therefore, clinicians are still encouraged to collaboratively explore an individual patient’s pattern of eating, craving, and affective experiences to identify possible idiosyncratic patterns of risk. Second, temporal relationships between variables (e.g., food craving and binge eating) were not tested directly in this study. Thus, observed similarities and differences in temporal patterns between variables are merely descriptive. Third, although this study utilized previously validated EMA methods (Goldschmidt et al., 2014; J. A. Wonderlich et al., 2015) of identifying binge-eating and overeating episodes that incorporated an assessment of the participant’s perception of overeating and loss of control, the actual amount of food consumed was not assessed. Therefore, it is possible that high levels of perceived overeating may not perfectly reflect actual objective overeating. Further, although loss of control eating is commonly defined by feeling unable to control one’s intake, regardless of the amount of food consumed (Tanofsky-Kraff et al., 2011; 2020) or when the amount of food consumed is either subjectively or objectively large (Fairburn & Wilson 1993; Hilbert et al., 2013), Loss of Control Only eating episodes in the current manuscript were characterized by high levels of feeling out of control without the perception of having overeaten. While this approach allowed us to more clearly distinguish between three different types of eating episodes reported by individuals with BED (Binge Eating, Overeating Only, Loss of Control Eating Only), care must be taken when integrating the current findings alongside previous research on “loss of control eating.” Fourth, the PANAS positive affect scale did not include items capturing joviality or excitement, which may be important precipitants of binge eating (Boggiano et al., 2014), and craving was measured using a single item, which may introduce measurement error. Fifth, we did not allow for random variation in the slopes of the temporal effects between individuals, the EMA protocol was relatively brief in duration (i.e., one week) and utilized only five daily signal-contingent ratings to reduce participant burden, and compliance during the EMA protocol was somewhat low, potentially limiting the reliability and generalizability of the findings. Finally, the sample was primarily comprised of White, treatment seeking individuals from the United States, which further limits the generalizability of the findings. Future studies should seek to address these limitations.
In sum, risk for binge eating was found to be greatest in the early evening (i.e., 5:30 p.m.), with additional peaks around lunch time (i.e., 12:30 p.m.) and at the end of the night (i.e., 11:00 p.m.). Thus, although the size of the effects were small, use of strategies to ameliorate binge-eating risk may be most needed at these times. Notably, patterns of binge eating appeared to most closely mimic patterns of food craving and, to a somewhat lesser extent, emotion regulation difficulty. Although several existing treatment approaches for eating disorders directly address affect and/or emotion regulation difficulties (Safer et al., 2009; S. A. Wonderlich et al., 2015), fewer treatments have been developed to address food craving, and their efficacy in BED remains underexplored (Boutelle et al., 2015; Sun & Kober, 2020). If future research supports a temporal relationship between craving and binge eating, intervention approaches that target craving may hold value as potential treatment adjuncts for BED. Further, the robust diurnal patterns of binge eating observed across AN, BN, and BED support research suggesting that disrupted circadian rhythms may contribute to the onset and maintenance of binge-eating behavior. Therefore, it is possible that supplementing traditional treatments with intervention techniques specifically designed to regulate diurnal rhythms may support enhanced treatment efficacy, though additional research is needed to evaluate this possibility (de Young & Bottera, 2022).
Supplementary Material
Public Significance Statement:
It is unknown which times of the day and days of the week individuals with binge-eating disorder are most at risk for binge eating. By assessing binge eating behaviors in the natural environment across the week, we found that individuals are most likely to binge in the evening, which corresponds to the times when they experience the strongest food craving and difficulty with regulating emotions.
Acknowledgments
This research was supported by funding from the National Institute of Mental Health (grant numbers R34 MH099040 and T32 MH082761) and National Institute of General Medical Science (grant number 1P20GM134969). The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washinton DC: Author. [Google Scholar]
- Bates D, Mächler M, Bolker BM, & Walker SC (2015). Fitting linear mixed-effects models using lme4. Journal of Statistical Software, 67(1), 1–48. 10.18637/JSS.V067.I01 [DOI] [Google Scholar]
- Berg KC, Crosby RD, Cao L, Crow SJ, Engel SG, Wonderlich SA, & Peterson CB (2015). Negative affect prior to and following overeating-only, loss of control eating-only, and binge eating episodes in obese adults. International Journal of Eating Disorders, 48(6), 641–653. 10.1002/EAT.22401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg KC, Peterson CB, Crosby RD, Cao L, Crow SJ, Engel SG, & Wonderlich SA (2014). Relationship between daily affect and overeating-only, loss of control eating-only, and binge eating episodes in obese adults. Psychiatry Research, 215(1), 185–191. 10.1016/J.PSYCHRES.2013.08.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boggiano MM, Burgess EE, Turan B, Soleymani T, Daniel S, Vinson LD, Lokken KL, Wingo BC, & Morse A (2014). Motives for eating tasty foods associated with binge-eating. Results from a student and a weight-loss seeking population. Appetite, 83, 160–166. 10.1016/J.APPET.2014.08.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boutelle KN, Liang J, Knatz S, Matheson B, Risbrough V, Strong D, Rhee KE, Craske MG, Zucker N, & Bouton ME (2015). Design and implementation of a study evaluating extinction processes to food cues in obese children: the Intervention for Regulations of Cues Trial (iROC). Contemporary Clinical Trials, 40, 95–104. 10.1016/J.CCT.2014.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- de Young KP, & Bottera AR (2022). A biobehavioral circadian model of restrictive eating and binge eating. International Journal of Eating Disorders, 55(10), 1291–1295. 10.1002/EAT.23758 [DOI] [PubMed] [Google Scholar]
- Engel SG, Wonderlich SA, Crosby RD, Mitchell JE, Crow S, Peterson CB, Le Grange D, Simonich HK, Cao L, Lavender JM, & Gordon KH (2013). The role of affect in the maintenance of anorexia nervosa: Evidence from a naturalistic assessment of momentary behaviors and emotion. Journal of Abnormal Psychology, 122(3), 709. 10.1037/A0034010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z, & O’Connor M (2008). Eating Disorder Examination. In Fairburn CG (Ed.), Cognitive behavior therapy and eating disorders (16.0D). Guilford Press. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JB (1995). Structured clinical interview for the DSM–IV axis I disorders—Patient edition (SCID–I/P, version 2). New York State Psychiatric Institute, Biometrics Research Department. [Google Scholar]
- Geldhof GJ, Preacher KJ, & Zyphur MJ (2014). Reliability estimation in a multilevel confirmatory factor analysis framework. Psychological Methods, 19(1), 72–91. 10.1037/A0032138 [DOI] [PubMed] [Google Scholar]
- Goldschmidt AB, Crosby RD, Cao L, Engel SG, Durkin N, Beach HM, Berg KC, Wonderlich SA, Crow SJ, & Peterson CB (2014). Ecological momentary assessment of eating episodes in obese adults. Psychosomatic Medicine, 76(9), 747–752. 10.1097/PSY.0000000000000108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, & Roemer L (2004). Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. 10.1023/B:JOBA.0000007455.08539.94 [DOI] [Google Scholar]
- Heatherton TF, & Baumeister RF (1991). Binge eating as escape from self-awareness. Psychological Bulletin, 110(1), 86–108. 10.1037/0033-2909.110.1.86 [DOI] [PubMed] [Google Scholar]
- Hedeker D, & Gibbons RD (1997). Application of random-effects pattern-mixture models for missing data in longitudinal studies. Psychological Methods, 2(1), 64–78. 10.1037/1082-989X.2.1.64 [DOI] [Google Scholar]
- Hilbert A, Hartmann AS, Czaja J, & Schoebi D (2013). Natural course of preadolescent loss of control eating. Journal of Abnormal Psychology, 122(3), 684–693. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, & Kessler RC (2007). The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry, 61(3), 348–358. 10.1016/J.BIOPSYCH.2006.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kober H, & Boswell RG (2018). Potential psychological & neural mechanisms in binge eating disorder: Implications for treatment. Clinical Psychology Review, 60, 32–44. 10.1016/J.CPR.2017.12.004 [DOI] [PubMed] [Google Scholar]
- Kuznetsova A, Brockhoff PB, & Christensen RHB (2017). lmerTest package: Tests in linear mixed effects models. Journal of Statistical Software, 82(13), 1–26. 10.18637/JSS.V082.I13 [DOI] [Google Scholar]
- Lavender JM, Tull MT, DiLillo D, Messman-Moore T, & Gratz KL (2017). Development and validation of a state-based measure of emotion dysregulation. Assessment, 24(2), 197–209. 10.1177/1073191115601218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavender JM, Utzinger LM, Crosby RD, Goldschmidt AB, Ellison J, Wonderlich SA, Engel SG, Mitchell JE, Crow SJ, Peterson CB, & Le Grange D (2016). A naturalistic examination of the temporal patterns of affect and eating disorder behaviors in anorexia nervosa. International Journal of Eating Disorders, 49(1), 77–83. 10.1002/EAT.22447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavender JM, Wonderlich SA, Engel SG, Gordon KH, Kaye WH, & Mitchell JE (2015). Dimensions of emotion dysregulation in anorexia nervosa and bulimia nervosa: A conceptual review of the empirical literature. Clinical Psychology Review, 40, 111–122. 10.1016/j.cpr.2015.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linardon J. (2018). Rates of abstinence following psychological or behavioral treatments for binge-eating disorder: Meta-analysis. International Journal of Eating Disorders, 51(8), 785–797. 10.1002/EAT.22897 [DOI] [PubMed] [Google Scholar]
- Peterson CB, Engel SG, Crosby RD, Strauman T, Smith TL, Klein M, Crow SJ, Mitchell JE, Erickson A, Cao L, Bjorlie K, & Wonderlich SA (2020). Comparing integrative cognitive-affective therapy and guided self-help cognitive-behavioral therapy to treat binge-eating disorder using standard and naturalistic momentary outcome measures: A randomized controlled trial. International Journal of Eating Disorders, 53(9), 1418–1427. 10.1002/EAT.23324 [DOI] [PubMed] [Google Scholar]
- Pinheiro J, Bates D, & R Core Team. (2022). _nlme: Linear and Nonlinear Mixed Effects Models_. R package version 3.1-157. https://CRAN.R-project.org/package=nlme [Google Scholar]
- R Core Team. (2022). R: A language and environment for statistical computing. R Foundation for Statistical Computing. https://www.R-project.org/
- Rights JD, & Sterba SK (2020). New recommendations on the use of r-squared differences in multilevel model comparisons. Multivariate Behavioral Research, 55(4), 568–599. 10.1080/00273171.2019.1660605 [DOI] [PubMed] [Google Scholar]
- Safer DL, Teach CF, & Chen EF (2009). Dialectical behavior therapy for binge eating and bulimia. New York, NY: Guilford Press. [Google Scholar]
- Schaefer LM, Smith KE, Anderson LM, Cao L, Crosby RD, Engel SG, Crow SJ, Peterson CB, & Wonderlich SA (2020). The role of affect in the maintenance of binge-eating disorder: Evidence from an ecological momentary assessment study. Journal of Abnormal Psychology, 129(4), 387–396. 10.1037/ABN0000517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smyth JM, Wonderlich SA, Heron KE, Sliwinski MJ, Crosby RD, Mitchell JE, & Engel SG (2007). Daily and momentary mood and stress are associated with binge eating and vomiting in bulimia nervosa patients in the natural environment. Journal of Consulting and Clinical Psychology, 75(4), 629–638. 10.1037/0022-006X.75.4.629 [DOI] [PubMed] [Google Scholar]
- Smyth JM, Wonderlich SA, Sliwinski MJ, Crosby RD, Engel SG, Mitchell JE, & Calogero RM (2009). Ecological momentary assessment of affect, stress, and binge-purge behaviors: day of week and time of day effects in the natural environment. International Journal of Eating Disorders, 42(5), 429–436. 10.1002/EAT.20623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun W, & Kober H (2020). Regulating food craving: From mechanisms to interventions. Physiology & Behavior, 222, 112878. 10.1016/J.PHYSBEH.2020.112878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svaldi J, Werle D, Naumann E, Eichler E, & Berking M (2019). Prospective associations of negative mood and emotion regulation in the occurrence of binge eating in binge eating disorder. Journal of Psychiatric Research, 115, 61–68. 10.1016/J.JPSYCHIRES.2019.05.005 [DOI] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Schvey NA, & Grilo CM (2020). A developmental framework of binge-eating disorder based on pediatric loss of control eating. American Psychologist, 75(2), 189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky M, Yanovski SZ, & Yanovski JA (2011). Loss of control over eating in children and adolescents. In Striegel-Moore RH, Wonderlich SA, Walsh BT, & Mitchell JE (Eds.), Developing an evidence-based classification of eating disorders: Scientific findings for DSM-5 (pp. 221–236). New York, NY: American Psychiatric Association Press. [Google Scholar]
- Telch CF, Pratt EM, & Niego SH (1998). Obese women with binge eating disorder define the term binge. International Journal of Eating Disorders, 24(3), 313–317. [DOI] [PubMed] [Google Scholar]
- Thompson ER (2007). Development and validation of an internationally reliable short-form of the Positive and Negative Affect Schedule (PANAS). Journal of Cross-Cultural Psychology, 38(2), 227–242. 10.1177/0022022106297301 [DOI] [Google Scholar]
- Udo T, & Grilo CM (2018). Prevalence and correlates of dsm-5–defined eating disorders in a nationally representative sample of U.S. adults. Biological Psychiatry, 84(5), 345–354. 10.1016/j.biopsych.2018.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verzijl CL, Gius B, Schlauch R, & Rancourt D (2022). The transdiagnostic role of food craving: An application of substance use models. Appetite, 170, 105867. 10.1016/J.APPET.2021.105867 [DOI] [PubMed] [Google Scholar]
- Wonderlich JA, Breithaupt LE, Crosby RD, Thompson JC, Engel SG, & Fischer S (2017). The relation between craving and binge eating: Integrating neuroimaging and ecological momentary assessment. Appetite, 117, 294–302. 10.1016/J.APPET.2017.07.005 [DOI] [PubMed] [Google Scholar]
- Wonderlich JA, Lavender JM, Wonderlich SA, Peterson CB, Crow SJ, Engel SG, Le Grange D, Mitchell JE, & Crosby RD (2015). Examining convergence of retrospective and ecological momentary assessment measures of negative affect and eating disorder behaviors. International Journal of Eating Disorders, 48(3), 305–311. 10.1002/EAT.22352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wonderlich SA, Peterson CB, Leone Smith T, Klein MH, Mitchell JE, & Crow SJ (2015). Integrative Cognitive-Affective Therapy for bulimia nervosa. New York, NY: Guilford Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zunker C, Peterson CB, Crosby RD, Cao L, Engel SG, Mitchell JE, & Wonderlich SA (2011). Ecological momentary assessment of bulimia nervosa: does dietary restriction predict binge eating? Behaviour Research and Therapy, 49(10), 714–717. 10.1016/J.BRAT.2011.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


