Abstract
BACKGROUND
Barrier surfaces composed of specialized epithelial cells separate the host body from the external environment, and are essential for maintaining proper intestinal physiologic and immune homeostasis.
AIM
To explore the development trends and research hotspots of intestinal barrier research in inflammatory bowel disease (IBD).
METHODS
The publications related to the intestinal barrier in IBD were obtained from the Web of Science Core Collection database. Bibliometric analysis and visualization were conducted using VOSviewer, CiteSpace and R software.
RESULTS
A total of 4482 articles published between 2002 and 2022 were identified. The United States is dominant in intestinal barrier research, whereas the University of Chicago is the most active institution. Jerrold from Harvard Medical School was the most productive authors with the most citations. The journals Inflammatory Bowel Disease and Gastroenterology have made significant contributions in this field. The keywords appearing at high frequency related to the intestinal barrier in IBD were detected, including nuclear factor kappa B, tumor necrosis factor-α, apoptosis, oxidative stress and probiotics. Among them, antioxidants, Akkermansia muciniphila, nanoparticles, short-chain fatty acids and extracellular vesicles have received growing interest in recent research.
CONCLUSION
The intestinal barrier field is developing rapidly with extensive cooperation. Targeting the gut microbiota and dietary metabolism to regulate the intestinal barrier has shown promising prospective applications and has generated broad interest. The importance of the intestinal barrier in IBD is gradually being fully recognized, providing a new therapeutic perspective for improving inflammation and prognosis.
Keywords: Intestinal barrier, Inflammatory bowel disease, Bibliometrics, Visualization, Hotspots
Core Tip: The complete composition and function of the intestinal mucosal barrier are essential for maintaining proper intestinal physiological and immune homeostasis. The study evaluated the developmental trends and research hotspots of intestinal barrier research in inflammatory bowel disease (IBD) using bibliometric methods. The results showed that Intestinal barrier field is developing rapidly with extensive cooperation. Targeting the gut microbiota and dietary metabolism to regulate intestinal barrier shown promising prospective applications. This may provide guidance and new insights for further research into improving IBD by modulating the intestinal barrier.
INTRODUCTION
Specialized epithelial cells constitute barrier surfaces that separate host body from the external environment. The complete composition and function of intestinal mucosal barrier is essential for maintaining proper intestinal physiologic and immune homeostasis[1]. There is growing evidence that a deficit of in the intestinal barrier contributes to inflammation activation, especially in inflammatory bowel disease (IBD).
The intestinal barrier is mainly composed of intestinal epithelial cells, tight junctions and mucous layers. Genetic predisposition and environmental influences generally lead to disruption of the intestinal barrier in IBD, including tight junction changes, mucous layer defects, reduced antimicrobial peptide expression, and autophagy dysregulation[2,3]. This imbalance in the intestinal barrier allows external antigens to invade the body through damaged intestinal barrier, causing inappropriate immune activation. A series of studies have shown that mucosal healing and reestablishment of barrier integrity are significantly associated with clinical remission and improved patient outcomes[4-6]. Knowledge of the research status and focus hotpots of the current field is helpful to further explore the pathogenesis of IBD and search for potential therapeutic targets.
Bibliometrics has become an important methodology for researchers to actively accumulate knowledge and collect evidence. The bibliographic and visual analysis provides new angles to identify development trends and predict research prospects of this field by mathematics and statistics[7-9]. Therefore, this study aimed to explore the knowledge landscape of the intestinal barrier in IBD, hoping to provide guidance and new insights for further research in the field of IBD.
MATERIALS AND METHODS
Search strategies
Bibliometric and visualization analyses were conducted through the Web of Science Core Collection (WoSCC) database, which is one of the most widely used source for academic and bibliometric analysis. The WoS database covers a broad spectrum of academic disciplines and offers precise citation data, facilitating in-depth evaluation of topic development and trend evolution[10-12]. The search strategy was as follows: TS (Topic) = (“inflammatory bowel disease” OR “ulcerative colitis” OR “crohn’s disease”) AND TS = (intestin* OR gut OR bowel) AND TS = (barrier OR integrity OR permeability). The publication period was between 2001 and 2021 with the publication type limited to original articles written in English (Figure 1).
Figure 1.
Flowchart of the literature screening.
Data collection
Bibliometric indicators were extracted from selected publications to quantitatively evaluate the characteristics of the literature and its trends, including titles, publication years, authors, affiliations, countries/regions, journals, abstracts, keywords, citations and references. The H-index of scholars, impact factor (IF) and Journal Citation Reports division of journals were also obtained from the Web of Science. Inappropriate formulations of elements were modified and multiple phrases with the same meaning were merged into a single element. The author's significant publications were obtained from the Reference Citation Analysis (RCA, https://referencecitationanalysis.com/) database. RCA is an open citation analysis database covering various fields and is owned by Baishideng Publishing Group Inc., situated in Pleasanton, CA 94566, United States[13-15]. Scientific data were searched and collected independently by two researchers to ensure the reliability of the results.
Bibliometric analysis
Bibliometric analysis is a quantitative research method that is widely employed to evaluate academic development in a specific field. VOSviewer, CiteSpace and R package were used for constructing the scientometric network and knowledge visualization. VOSviewer was adopted to conduct co-authorship analysis of authors and countries/regions, co-occurrence analysis of keywords and co-citation analysis of journals. Co-authorship and co-occurrence relationships were defined as the simultaneous occurrence of two items, while co-citation relationships referred to two items being cited simultaneously by a third item[16,17]. The network graph generated by VOSviewer displays the size of nodes based on the number of publications, and the connection represents the relationship between nodes. Closely related nodes were divided into clusters of the same color.
CiteSpace was used to calculate the node centrality and keyword burst trends. Centrality measures the quantity of all the shortest paths passing through a node in a network, with nodes having centrality greater than 0.1 identified as key nodes of significant importance. Burst detection was employed to identify keywords that experienced a sudden surge in their frequency of appearance during a specific time frame. The green line indicates the occurrence and development of keywords, while the red line represents the duration of the burst.
In addition, R software was used to develop the distribution of scientific productivity among authors and different countries/regions. Lotka’s Law demonstrates the relationship between the frequency of scientific paper authorship and the number of publications, revealing an unbalanced distribution of author productivity.
RESULTS
Growth trend of publications
A total of 4482 publications related to the intestinal barrier in IBD were published between 2002-2022. There were only a small number of studies in the early stage, with less than 100 articles each year (Figure 2). During the middle period from 2006 to 2014, the number of publications showed a slow increase. Subsequently, annual publications have grown rapidly, with 53.8% of all publications occurring in the past two decades. Increasing attention to the intestinal barrier in IBD from researchers has driven further development of this field.
Figure 2.
Annual and cumulative growth trends of publications.
Countries/regions and institutions
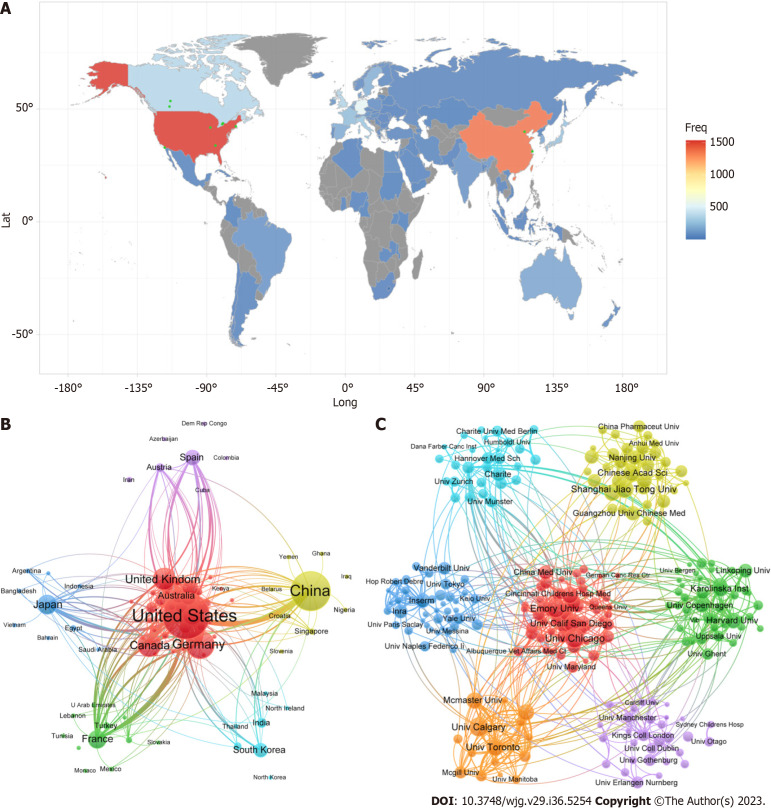
Intestinal barrier research in IBD has been carried out at 4650 institutions from 89 countries/regions (Figure 3A). The United States is dominant in this field with the highest number of publications (n = 1426) and citations (n = 89615). The next most productive countries/regions were China and Germany (Table 1). In addition, Germany achieved the highest citations per publication at 73.2. These countries were divided into seven clusters to show the extensive cooperation between nodes (Figure 3B). Multiple nodes played a strong bridging role in the collaboration, most notably for the United States, the United Kingdom and China.
Figure 3.
Network visualization map of countries/regions and institutions. A: Geographic distribution map based on the total publications; B: Cooperation map of countries/regions; C: Cooperation map of institutions. The nodes in the network map represent countries/regions, and the node size is proportional to the number of publications. The thickness of the connecting line between nodes indicates the strength of the co-authorship relationships.
Table 1.
The top 10 countries/regions and institutions in the intestinal barrier field relevant to inflammatory bowel disease
|
Country
|
Centrality
|
Count
|
Citation
|
CPR
|
Institution
|
Centrality
|
Count
|
Citation
|
CPR
|
| United States | 0.30 | 1534 | 90667 | 59.1 | University of Chicago | 0.08 | 87 | 8288 | 95.3 |
| China | 0.26 | 1383 | 25867 | 18.7 | University of Calgary | 0.06 | 84 | 4051 | 48.2 |
| Germany | 0.18 | 533 | 37129 | 69.7 | Emory University | 0.09 | 83 | 6183 | 74.5 |
| Canada | 0.09 | 352 | 17335 | 49.2 | Shanghai Jiao Tong University | 0.07 | 74 | 2323 | 31.4 |
| United Kingdom | 0.28 | 336 | 23096 | 68.7 | University of Toronto | 0.05 | 68 | 3125 | 46.0 |
| Italy | 0.12 | 266 | 12121 | 45.6 | Harvard Medical School | 0.07 | 62 | 1883 | 30.4 |
| Japan | 0.10 | 244 | 8467 | 34.7 | Chinese Academy of Sciences | 0.04 | 62 | 1600 | 25.8 |
| France | 0.16 | 226 | 11080 | 49.0 | University of California San Diego | 0.07 | 59 | 6034 | 102.3 |
| Sweden | 0.02 | 178 | 11089 | 62.3 | University of Alberta | 0.06 | 58 | 3310 | 57.1 |
| Netherlands | 0.03 | 168 | 7693 | 45.8 | McMaster University | 0.05 | 58 | 4047 | 69.8 |
CPR: Citations per publication.
The University of Chicago conducted the largest number of studies (n = 8236), followed by Emory University (n = 6437) and the University of Calgary (n = 4064). Among them, the University of California San Diego exhibited the highest average citations of 102.3. Cooperation between institutions is more evident than that between countries, which enables further exploration and collaboration on the subject (Figure 3C).
Authors and cited authors
A total of 26245 authors have participated in the field of intestinal barrier research in IBD. Seventy-six percent of the authors contributed one article, whereas only 6.0% contributed more than 3 articles (Figure 4A). Turner[18] (n = 35), Söderholm et al[19-21] (n = 32) and Keshavarzian et al[22-25] (n = 28) were the most productive authors (Table 2). Although Turner[18] from Harvard Medical School also has the most citations (n = 3399), the nodes of these scholars were more dispersed across different clusters rather than being aggregated (Figure 4B). Close communication and similar research directions exist in the nodes of the same cluster. In addition, the clusters displaying different colors are not entirely independent and exhibit a relatively low level of connections.
Figure 4.
Network visualization map of authors. A: Scientific productivity of authors based on Lotka’s Law; B: Cooperation map of authors. Each node represents a different author, and the connections between the nodes reflect the co-authorship relationships.
Table 2.
The top 10 productive authors and cited authors in the intestinal barrier field relevant to inflammatory bowel disease
|
Ref.
|
Count
|
H-index
|
Ref.
|
Count
|
H-index
|
| Turner[18] | 35 | 78 | Turner[18] | 3399 | 78 |
| Söderholm et al[19-21] | 32 | 46 | Neurath[35] | 3257 | 87 |
| Keshavarzian et al[22-25] | 28 | 77 | Ma et al[40] | 2811 | 26 |
| Rogler[59] | 26 | 66 | Hansson[60] | 2785 | 71 |
| Neurath[35] | 25 | 87 | Johansson et al[61] | 2725 | 47 |
| Schulzke et al[62] | 23 | 58 | Al-Sadi et al[63] | 2489 | 21 |
| Merlin et al[64] | 23 | 62 | Danese and Fiocchi[46] | 2440 | 96 |
| Ma et al[40] | 22 | 26 | Becker et al[44] | 2319 | 61 |
| Fromm et al[34] | 21 | 66 | Schulzke et al[62] | 1852 | 58 |
| Vermeire et al[51] | 21 | 122 | Nusrat et al[33] | 1838 | 47 |
Journals and cited academic journals
There were 1045 journals involved in the publication of intestinal barrier research in IBD. IBDs contributed the most articles (n = 258), while Gastroenterology received the most citations (Table 3). The next most productive journals were PLoS One (n = 145) and the American Journal of Physiology-Gastrointestinal and Liver Physiology (n = 119). Articles published in established journals exhibit a higher average citation count, which is consistent with the IF of the journal.
Table 3.
The top 10 journals and co-cited journals in the intestinal barrier field relevant to inflammatory bowel disease
|
Journal
|
Count
|
IF (2022)
|
JCR (2022)
|
Cited journal
|
Citation
|
IF (2022)
|
JCR (2022)
|
| Inflammatory Bowel Diseases | 258 | 7.290 | Q1 | Gastroenterology | 14345 | 33.883 | Q1 |
| PLos One | 145 | 3.752 | Q2 | Gut | 12840 | 31.793 | Q1 |
| American Journal of Physiology-Gastrointestinal and Liver Physiology | 119 | 4.871 | Q1/Q2 | Inflammatory Bowel Diseases | 10188 | 69.504 | Q1 |
| Gastroenterology | 118 | 33.883 | Q1 | American Journal of Physiology-Gastrointestinal and Liver Physiology | 8962 | 4.871 | Q1/Q2 |
| World Journal of Gastroenterology | 107 | 5.374 | Q2 | Plos One | 6557 | 3.752 | Q2 |
| Gut | 94 | 31.793 | Q1 | Proceedings of the National Academy of Sciences of the United States of America | 6250 | 12.779 | Q1 |
| Frontiers in Immunology | 86 | 8.786 | Q1 | Nature | 4978 | 69.504 | Q1 |
| Food & Function | 83 | 6.317 | Q1 | World Journal of Gastroenterology | 4509 | 5.374 | Q2 |
| Digestive Diseases and Sciences | 78 | 3.487 | Q3 | Journal of Immunology | 4142 | 5.426 | Q2 |
| Scientific Reports | 74 | 4.996 | Q2 | Journal of Clinical Investigation | 3390 | 19.456 | Q1 |
IF: Impact factor; JCR: Journal Citation Reports.
Among them, the majority of journals had an early initiation into this field (Figure 5A). Despite being relatively new to the field, Frontiers in Immunology, Food & Function and Scientific Reports demonstrated rapid development. As shown in Figure 5B, these journals were divided into five clusters based on the similarity of their themes. The higher the number of co-citations between two journals, the stronger is the link between the two nodes.
Figure 5.
Network visualization map of authors. A: Annual number of publications for the top 10 journals; B: Cooperation map of Journals. The nodes in the graph represented journals, and the connections between the nodes reflect the co-authorship relationships.
Keywords co-occurrence, clusters and bursts
Keywords were extracted for multidimensional analysis to determine the research hotspot and exploration direction in the specific field. The keywords appearing at high frequency related with intestinal barrier in IBD were identified, including molecules, pathological processes and treatments (Table 4). Nuclear factor kappa B (NF-κB) (n = 418), tumor necrosis factor-α (TNF-α) (n = 329) and interferon (IFN)-γ (n = 173) were the most commonly implicated molecules. Apoptosis (n = 292), oxidative stress (n = 232) and metabolism (n = 88) were widely involved in research on the intestinal barrier. Regarding treatments, probiotics (n = 237), nanoparticles (n = 77) and antioxidant (n = 73) have attracted extensive attention.
Table 4.
The top 10 molecules, pathological processes and disease in the intestinal barrier field relevant to inflammatory bowel disease
|
Molecule
|
Count
|
Pathological process
|
Count
|
Treatment
|
Count
|
| NF-kB | 418 | Apoptosis | 292 | Probiotic | 237 |
| TNF-α | 329 | Oxidative stress | 232 | Nanoparticles | 77 |
| IFN-gamma | 173 | Metabolism | 88 | Antioxidant | 73 |
| Mucin | 100 | Dysbiosis | 83 | Butyrate | 70 |
| Occludin | 90 | Autophagy | 82 | Infliximab | 66 |
| Nitric oxide | 87 | Infection | 80 | Polysaccharide | 48 |
| ZO-1 | 55 | Bacterial translocation | 68 | Prebiotic | 40 |
| Claudin-2 | 54 | Endoplasmic reticulum stress | 65 | Fecal microbiota transplantation | 37 |
| E-cadherin | 51 | Transport | 59 | Lactobacillus | 32 |
| Antimicrobial peptide | 50 | Absorption | 50 | Vitamin D | 26 |
NF-kB: Nuclear factor kappa B; TNF-α: Tumor necrosis factor-α; IFN: Interferon.
The network map was classified into four clusters by co-occurrence analysis, which portrayed the fundamental knowledge structure of related research fields (Figure 6). Based on the closeness between nodes, the largest blue cluster contains keywords associated with clinical characteristics, such as risk, children and therapy. The red cluster was mainly composed of tight junctions, permeability and transport, which drew attention to barrier function in IBD. The yellow cluster mainly focused on the gut microbiota, including probiotics, metabolism and dysbiosis. The green cluster was involved in the regulation of inflammation, with keywords such as apoptosis, NF-κB and oxidative stress.
Figure 6.
The network map of keywords in the intestinal barrier field relevant to inflammatory bowel disease. The network map displays the size of nodes based on the number of publications, and the connection represents the co-occurrence relationships between nodes. Closely related nodes were divided into clusters of the same color.
The visual keyword burst trend was constructed to show the major research interests in the intestinal barrier field (Figure 7). Early keyword bursts were mainly concentrated on intestinal barrier function and related inflammatory molecules, where intestinal permeability showed strong bursts. During the middle period, only a limited number of keywords exhibited an outbreak trend, such as autophagy, matrix metalloproteinase, and vitamin D. In contrast, targeted intestinal barrier therapy has been receiving growing interest from researchers, with a particular focus on antioxidants, Akkermansia muciniphila, nanoparticles, short-chain fatty acids, and extracellular vesicles as recent areas of research attention.
Figure 7.
The top 50 keywords with the strongest citation bursts in the intestinal barrier field relevant to inflammatory bowel disease. The green line indicates the occurrence and development of keywords, while the red line represents the duration of the burst.
DISCUSSION
The intestinal barrier refers to the physiological barrier composed of intestinal epithelial cells and mucous layers, which plays a crucial role in the onset and progression of IBD[26-28]. The disruption of the intestinal barrier in IBD patients is closely related to the severity of intestinal inflammation and immune response. The significant increase in the number of annual publications indicates a rapidly growing interest and recognition of the intestinal barrier field.
The United States occupied the dominant places in the intestinal barrier field with the highest number of publications and citations. Although China is developing rapidly in this field, it exhibits lower average citation rates. Other countries such as Germany and the United Kingdom have conducted more in-depth research and have the highest average citation rates. It is necessary to increase the depth and influence of research to address the imbalance between the number of publications and citations. Extensive collaboration is observed in countries such as the United States and the United Kingdom, however, institutional collaboration tends to show a trend of geographic alignment in terms of its distribution.
The author’s productivity is consistent with Lotka’s Law. Turner[18] from Harvard Medical School has made significant contributions to intestinal barrier research. He and His group found that MLCK-dependent tight junction dysfunction can cause immune system activation and experimental colitis induction[18,29]. Söderholm et al[19-21] mainly investigated how chronic stress triggers intestinal inflammation, which is closely associated with mast cells. In contrast, Keshavarzian et al[22-25] focused on the connections between colitis and other systemic diseases, such as Alzheimer's disease. These findings demonstrate the feasibility of improving IBD through barrier repair, which could become a strong candidate for nonimmune suppressive methods to achieve or maintain disease remission.
Intestinal barrier research was initially published in gastroenterology journals, particularly in IBD. The exploration of the intestinal barrier has revealed extensive relationships between this field and several other research areas, such as physiology, biochemistry and immunology. As a result, there has been an increase in the number of interdisciplinary journals to better cater to the needs of this rapidly expanding field. Comprehensive journals have a wide readership and are more conducive to interdisciplinary collaboration.
The integrity of the intestinal barrier has been found to be closely associated with host defense and regulates the progression of IBD. Keywords in the field of the intestinal barrier mainly revolve around four aspects, encompassing clinical characteristics, barrier function, the gut microbiota, and inflammation regulation. Studies have reported that disruptions in the intestinal barrier lead to persistent intestinal symptoms and poor prognosis in IBD patients[30,31]. The increase in intestinal permeability is a marker of intestinal barrier dysfunction. The tight junction between intestinal epithelial cells are dynamic structures capable of swift adjustments, which determine the mucosal permeability[32-34]. The active transcellular transport of ions and water relies on the presence of intact tight junction barriers. Damage to epithelial cells triggers the release of inflammatory cytokines such as TNF and IFN-γ[35-37]. Stimulation of TNF downregulates the expression of tight junction proteins and changes their localization in colonic epithelial cells[38-40]. Insufficiency of interleukin (IL)-10, excessive production of nitric oxide, and impaired autophagy can also induce an overactive immune system and enhance barrier loss[41-44], which in turn causes further leakage of luminal substances and amplifies local inflammation. The homeostasis of intestinal barrier can be affected either directly by inducing intracellular signaling pathways, or indirectly by the gut microbiota as an interacting partner to a greater extent[45,46]. Reduced intestinal community richness in patients with IBD leads to loss of intestinal homeostasis and inappropriate immune activation, which is characterized by a decrease in Firmicutes and proliferation of facultative anaerobic Enterobacteriaceae and adherent invasive Escherichia coli[47-49].
Recently, there has been widespread research interest in improving the intestinal barrier by targeting gut microbiota and dietary metabolism. Exogenous administration of probiotics can influence the composition and characteristics of the intestinal microbiota to exert intervention effects, typically in combination with prebiotics. The colonization of the beneficial bacterium Akkermansia muciniphila increased the number of goblet cells and upregulated the expression of genes encoding mucin[50]. Although fecal microbiota transplantation (FMT) has been shown to induce clinical remission of ulcerative colitis, the long-term effects of FMT as maintenance therapy have not been validated in IBD[51,52]. Microbial and dietary metabolites also demonstrate a regulatory influence on the intestinal barrier. Short-chain fatty acids produced by dietary fiber fermentation are the main energy source of colon cells, promoting the integrity of epithelial tight junctions and mucus secretion, which may be related to the activation of AMPK and STAT3[53,54]. The observed abnormality in bile acid metabolism may contribute to an enhanced epithelial inflammatory response. The reduction in secondary bile acids weakens the inhibition of IL-8 secretion[55] and the activation of TGR5 receptors in intestinal stem cells[56]. In addition, extracellular vesicles produced by host cells and microorganisms are also involved in cellular communication. Immune cells such as mast cells can secrete extracellular vesicles containing miR-223 to regulate intestinal permeability with downregulation of tight junction proteins[57]. Notably, extracellular vesicles themselves also represent a natural nanomaterial for drug delivery, that can improve the therapeutic effect and reduce systemic exposure in healthy tissues to promote remission of IBD[58].
The bibliometric analysis offers novel and objective insights into evolving intestinal barrier research hotspots and trends across multiple dimensions. Inevitably, there were several limitations to this study. The data were extracted from the WoSCC database, potentially omitting some information from other sources. Furthermore, while bibliometric methods based on natural language processing are susceptible to biases from subject categorization and citation behavior, a sufficient sample size helps ensure the accuracy of research findings to some extent.
CONCLUSION
In conclusion, the intestinal barrier field is developing rapidly with extensive cooperation. Targeting the gut microbiota and dietary metabolism to regulate the intestinal barrier shown promising prospective applications and has generated broad interest. The importance of the intestinal barrier in IBD is gradually being fully recognized, providing a new therapeutic perspective for improving inflammation.
ARTICLE HIGHLIGHTS
Research background
Barrier surfaces composed of specialized epithelial cells separate the host body from the external environment, and are essential for maintaining proper intestinal physiologic and immune homeostasis. There is growing evidence that the mucosal healing and reestablishment of barrier integrity are significantly associated with clinical remission and improved patient outcomes.
Research motivation
With the rapid expansion of research topics, it has become challenging for researchers to accumulate knowledge and actively collect evidence in specific field. The bibliographic and visual analysis provides new angles to identify development trends and predict research prospects of this field by mathematics and statistics.
Research objectives
The purpose of this study was to provide a comprehensive overview of the knowledge structure and research hotspots of intestinal barrier in inflammatory bowel disease (IBD).
Research methods
The publications related to intestinal barrier in IBD were obtained from the Web of Science Core Collection database. Bibliometric analysis and visualization were conducted using VOSviewer, CiteSpace and R software.
Research results
A comprehensive analysis of 4482 articles published between 2002 and 2022 has revealed significant insights in the realm of intestinal barrier research. Intestinal barrier research mainly focuses on four aspects, including clinical characteristics, barrier function, gut microbiota, and inflammation regulation. The keywords appearing at high frequency related with intestinal barrier in IBD were detected, including nuclear factor kappa B, tumor necrosis factor-α, apoptosis, oxidative stress and probiotics. Among them, antioxidants, Akkermansia muciniphila, nanoparticles, short-chain fatty acids and extracellular vesicles have received extensive interest in current research.
Research conclusions
The intestinal barrier field is developing rapidly with extensive cooperation. Targeting the gut microbiota and dietary metabolism to regulate intestinal barrier shown promising applied prospective and has generated broad interest.
Research perspectives
The importance of the intestinal barrier in IBD is gradually being fully recognized, providing a new therapeutic perspective for improving inflammation.
Footnotes
Conflict-of-interest statement: None of the authors have any conflicts of interest or financial ties to disclose.
PRISMA 2009 Checklist statement: The authors have read the PRISMA 2009 Checklist, and the manuscript was prepared and revised according to the PRISMA 2009 Checklist.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: July 20, 2023
First decision: August 5, 2023
Article in press: September 8, 2023
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Iizuka M, Japan; Wu H, United States S-Editor: Fan JR L-Editor: A P-Editor: Zhao S
Contributor Information
Feng Zhou, Department of Gastroenterology, The First Affiliated Hospital of Nanchang University, Nanchang 330000, Jiangxi Province, China.
Nan-Zhen Wu, Department of Gastrointestinal Surgery, Fengcheng People's Hospital, Fengcheng 331100, Jiangxi Province, China.
Yong Xie, Department of Gastroenterology, The First Affiliated Hospital of Nanchang University, Nanchang 330000, Jiangxi Province, China.
Xiao-Jiang Zhou, Department of Gastroenterology, The First Affiliated Hospital of Nanchang University, Nanchang 330000, Jiangxi Province, China. yfyzxj1970@163.com.
References
- 1.Villablanca EJ, Selin K, Hedin CRH. Mechanisms of mucosal healing: treating inflammatory bowel disease without immunosuppression? Nat Rev Gastroenterol Hepatol. 2022;19:493–507. doi: 10.1038/s41575-022-00604-y. [DOI] [PubMed] [Google Scholar]
- 2.Ramos GP, Papadakis KA. Mechanisms of Disease: Inflammatory Bowel Diseases. Mayo Clin Proc. 2019;94:155–165. doi: 10.1016/j.mayocp.2018.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen Y, Cui W, Li X, Yang H. Interaction Between Commensal Bacteria, Immune Response and the Intestinal Barrier in Inflammatory Bowel Disease. Front Immunol. 2021;12:761981. doi: 10.3389/fimmu.2021.761981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schoultz I, Keita ÅV. Cellular and Molecular Therapeutic Targets in Inflammatory Bowel Disease-Focusing on Intestinal Barrier Function. Cells. 2019;8 doi: 10.3390/cells8020193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Michaels M, Madsen KL. Immunometabolism and microbial metabolites at the gut barrier: Lessons for therapeutic intervention in inflammatory bowel disease. Mucosal Immunol. 2023;16:72–85. doi: 10.1016/j.mucimm.2022.11.001. [DOI] [PubMed] [Google Scholar]
- 6.Otte ML, Lama Tamang R, Papapanagiotou J, Ahmad R, Dhawan P, Singh AB. Mucosal healing and inflammatory bowel disease: Therapeutic implications and new targets. World J Gastroenterol. 2023;29:1157–1172. doi: 10.3748/wjg.v29.i7.1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agarwal A, Durairajanayagam D, Tatagari S, Esteves SC, Harlev A, Henkel R, Roychoudhury S, Homa S, Puchalt NG, Ramasamy R, Majzoub A, Ly KD, Tvrda E, Assidi M, Kesari K, Sharma R, Banihani S, Ko E, Abu-Elmagd M, Gosalvez J, Bashiri A. Bibliometrics: tracking research impact by selecting the appropriate metrics. Asian J Androl. 2016;18:296–309. doi: 10.4103/1008-682X.171582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen C, Song M. Visualizing a field of research: A methodology of systematic scientometric reviews. PLoS One. 2019;14:e0223994. doi: 10.1371/journal.pone.0223994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen C. Searching for intellectual turning points: progressive knowledge domain visualization. Proc Natl Acad Sci U S A. 2004;101 Suppl 1:5303–5310. doi: 10.1073/pnas.0307513100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheng K, Guo Q, Shen Z, Yang W, Wang Y, Sun Z, Wu H. Bibliometric Analysis of Global Research on Cancer Photodynamic Therapy: Focus on Nano-Related Research. Front Pharmacol. 2022;13:927219. doi: 10.3389/fphar.2022.927219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheng K, Zhang H, Guo Q, Zhai P, Zhou Y, Yang W, Wang Y, Lu Y, Shen Z, Wu H. Emerging trends and research foci of oncolytic virotherapy for central nervous system tumors: A bibliometric study. Front Immunol. 2022;13:975695. doi: 10.3389/fimmu.2022.975695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yeung AWK. Web of Science, PubMed and publishers for mislabelled review papers. Curr Sci. 2019;116:1909–1914. [Google Scholar]
- 13.Wang JL, Ma YJ, Ma L, Ma N, Guo DM, Ma LS. Baishideng's Reference Citation Analysis database announces the first Journal Article Influence Index of 101 core journals and a list of high-quality academic journals in gastroenterology and hepatology. World J Gastroenterol. 2022;28:5383–5394. doi: 10.3748/wjg.v28.i37.5383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang JL, Ma YJ, Ma L, Ma N, Guo DM, Ma LS. Baishideng's Reference Citation Analysis database announces the first Journal Article Influence Index of 104 core journals and a list of high-quality academic journals in orthopedics. World J Orthop. 2022;13:891–902. doi: 10.5312/wjo.v13.i10.891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang JL, Ma YJ, Ma L, Ma N, Guo DM, Ma LS. Baishideng's Reference Citation Analysis database announces the first Article Influence Index of multidisciplinary scholars. World J Clin Cases. 2022;10:10391–10398. doi: 10.12998/wjcc.v10.i29.10391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu Z, Cheng K, Shen Z, Lu Y, Wang H, Wang G, Wang Y, Yang W, Sun Z, Guo Q, Wu H. Mapping knowledge landscapes and emerging trends of sonodynamic therapy: A bibliometric and visualized study. Front Pharmacol. 2022;13:1048211. doi: 10.3389/fphar.2022.1048211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu H, Cheng K, Tong L, Wang Y, Yang W, Sun Z. Knowledge structure and emerging trends on osteonecrosis of the femoral head: a bibliometric and visualized study. J Orthop Surg Res. 2022;17:194. doi: 10.1186/s13018-022-03068-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Turner JR. Molecular basis of epithelial barrier regulation: from basic mechanisms to clinical application. Am J Pathol. 2006;169:1901–1909. doi: 10.2353/ajpath.2006.060681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Söderholm JD, Yang PC, Ceponis P, Vohra A, Riddell R, Sherman PM, Perdue MH. Chronic stress induces mast cell-dependent bacterial adherence and initiates mucosal inflammation in rat intestine. Gastroenterology. 2002;123:1099–1108. doi: 10.1053/gast.2002.36019. [DOI] [PubMed] [Google Scholar]
- 20.Söderholm JD, Yates DA, Gareau MG, Yang PC, MacQueen G, Perdue MH. Neonatal maternal separation predisposes adult rats to colonic barrier dysfunction in response to mild stress. Am J Physiol Gastrointest Liver Physiol. 2002;283:G1257–G1263. doi: 10.1152/ajpgi.00314.2002. [DOI] [PubMed] [Google Scholar]
- 21.Söderholm JD. Mast cells and mastocytosis. Dig Dis. 2009;27 Suppl 1:129–136. doi: 10.1159/000268133. [DOI] [PubMed] [Google Scholar]
- 22.Keshavarzian A, Farhadi A, Forsyth CB, Rangan J, Jakate S, Shaikh M, Banan A, Fields JZ. Evidence that chronic alcohol exposure promotes intestinal oxidative stress, intestinal hyperpermeability and endotoxemia prior to development of alcoholic steatohepatitis in rats. J Hepatol. 2009;50:538–547. doi: 10.1016/j.jhep.2008.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Keshavarzian A, Green SJ, Engen PA, Voigt RM, Naqib A, Forsyth CB, Mutlu E, Shannon KM. Colonic bacterial composition in Parkinson's disease. Mov Disord. 2015;30:1351–1360. doi: 10.1002/mds.26307. [DOI] [PubMed] [Google Scholar]
- 24.Keshavarzian A, Mutlu E, Guzman JP, Forsyth C, Banan A. Phosphodiesterase 4 inhibitors and inflammatory bowel disease: emerging therapies in inflammatory bowel disease. Expert Opin Investig Drugs. 2007;16:1489–1506. doi: 10.1517/13543784.16.9.1489. [DOI] [PubMed] [Google Scholar]
- 25.Keshavarzian A, Engen P, Bonvegna S, Cilia R. The gut microbiome in Parkinson's disease: A culprit or a bystander? Prog Brain Res. 2020;252:357–450. doi: 10.1016/bs.pbr.2020.01.004. [DOI] [PubMed] [Google Scholar]
- 26.Mehandru S, Colombel JF. The intestinal barrier, an arbitrator turned provocateur in IBD. Nat Rev Gastroenterol Hepatol. 2021;18:83–84. doi: 10.1038/s41575-020-00399-w. [DOI] [PubMed] [Google Scholar]
- 27.Odenwald MA, Turner JR. The intestinal epithelial barrier: a therapeutic target? Nat Rev Gastroenterol Hepatol. 2017;14:9–21. doi: 10.1038/nrgastro.2016.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yu LC. Microbiota dysbiosis and barrier dysfunction in inflammatory bowel disease and colorectal cancers: exploring a common ground hypothesis. J Biomed Sci. 2018;25:79. doi: 10.1186/s12929-018-0483-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Graham WV, He W, Marchiando AM, Zha J, Singh G, Li HS, Biswas A, Ong MLDM, Jiang ZH, Choi W, Zuccola H, Wang Y, Griffith J, Wu J, Rosenberg HJ, Snapper SB, Ostrov D, Meredith SC, Miller LW, Turner JR. Intracellular MLCK1 diversion reverses barrier loss to restore mucosal homeostasis. Nat Med. 2019;25:690–700. doi: 10.1038/s41591-019-0393-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chang J, Leong RW, Wasinger VC, Ip M, Yang M, Phan TG. Impaired Intestinal Permeability Contributes to Ongoing Bowel Symptoms in Patients With Inflammatory Bowel Disease and Mucosal Healing. Gastroenterology. 2017;153:723–731.e1. doi: 10.1053/j.gastro.2017.05.056. [DOI] [PubMed] [Google Scholar]
- 31.Turpin W, Lee SH, Raygoza Garay JA, Madsen KL, Meddings JB, Bedrani L, Power N, Espin-Garcia O, Xu W, Smith MI, Griffiths AM, Moayyedi P, Turner D, Seidman EG, Steinhart AH, Marshall JK, Jacobson K, Mack D, Huynh H, Bernstein CN, Paterson AD Crohn’s and Colitis Canada Genetic Environmental Microbial Project Research Consortium; CCC GEM Project recruitment site directors include Maria Abreu, Croitoru K. Increased Intestinal Permeability Is Associated With Later Development of Crohn's Disease. Gastroenterology. 2020;159:2092–2100.e5. doi: 10.1053/j.gastro.2020.08.005. [DOI] [PubMed] [Google Scholar]
- 32.Slifer ZM, Blikslager AT. The Integral Role of Tight Junction Proteins in the Repair of Injured Intestinal Epithelium. Int J Mol Sci. 2020;21 doi: 10.3390/ijms21030972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nusrat A, Turner JR, Madara JL. Molecular physiology and pathophysiology of tight junctions. IV. Regulation of tight junctions by extracellular stimuli: nutrients, cytokines, and immune cells. Am J Physiol Gastrointest Liver Physiol. 2000;279:G851–G857. doi: 10.1152/ajpgi.2000.279.5.G851. [DOI] [PubMed] [Google Scholar]
- 34.Fromm M, Krug SM, Zeissig S, Richter JF, Rosenthal R, Schulzke JD, Günzel D. High-resolution analysis of barrier function. Ann N Y Acad Sci. 2009;1165:74–81. doi: 10.1111/j.1749-6632.2009.04047.x. [DOI] [PubMed] [Google Scholar]
- 35.Neurath MF. Targeting cytokines in inflammatory bowel disease. Sci Transl Med. 2022;14:eabq4473. doi: 10.1126/scitranslmed.abq4473. [DOI] [PubMed] [Google Scholar]
- 36.Abraham C, Abreu MT, Turner JR. Pattern Recognition Receptor Signaling and Cytokine Networks in Microbial Defenses and Regulation of Intestinal Barriers: Implications for Inflammatory Bowel Disease. Gastroenterology. 2022;162:1602–1616.e6. doi: 10.1053/j.gastro.2021.12.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Luissint AC, Parkos CA, Nusrat A. Inflammation and the Intestinal Barrier: Leukocyte-Epithelial Cell Interactions, Cell Junction Remodeling, and Mucosal Repair. Gastroenterology. 2016;151:616–632. doi: 10.1053/j.gastro.2016.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Al-Sadi R, Guo S, Ye D, Rawat M, Ma TY. TNF-α Modulation of Intestinal Tight Junction Permeability Is Mediated by NIK/IKK-α Axis Activation of the Canonical NF-κB Pathway. Am J Pathol. 2016;186:1151–1165. doi: 10.1016/j.ajpath.2015.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yu M, Wang Q, Ma Y, Li L, Yu K, Zhang Z, Chen G, Li X, Xiao W, Xu P, Yang H. Aryl Hydrocarbon Receptor Activation Modulates Intestinal Epithelial Barrier Function by Maintaining Tight Junction Integrity. Int J Biol Sci. 2018;14:69–77. doi: 10.7150/ijbs.22259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ma TY, Iwamoto GK, Hoa NT, Akotia V, Pedram A, Boivin MA, Said HM. TNF-alpha-induced increase in intestinal epithelial tight junction permeability requires NF-kappa B activation. Am J Physiol Gastrointest Liver Physiol. 2004;286:G367–G376. doi: 10.1152/ajpgi.00173.2003. [DOI] [PubMed] [Google Scholar]
- 41.Koelink PJ, Bloemendaal FM, Li B, Westera L, Vogels EWM, van Roest M, Gloudemans AK, van 't Wout AB, Korf H, Vermeire S, Te Velde AA, Ponsioen CY, D'Haens GR, Verbeek JS, Geiger TL, Wildenberg ME, van den Brink GR. Anti-TNF therapy in IBD exerts its therapeutic effect through macrophage IL-10 signalling. Gut. 2020;69:1053–1063. doi: 10.1136/gutjnl-2019-318264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cross RK, Wilson KT. Nitric oxide in inflammatory bowel disease. Inflamm Bowel Dis. 2003;9:179–189. doi: 10.1097/00054725-200305000-00006. [DOI] [PubMed] [Google Scholar]
- 43.Larabi A, Barnich N, Nguyen HTT. New insights into the interplay between autophagy, gut microbiota and inflammatory responses in IBD. Autophagy. 2020;16:38–51. doi: 10.1080/15548627.2019.1635384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Becker C, Dornhoff H, Neufert C, Fantini MC, Wirtz S, Huebner S, Nikolaev A, Lehr HA, Murphy AJ, Valenzuela DM, Yancopoulos GD, Galle PR, Karow M, Neurath MF. Cutting edge: IL-23 cross-regulates IL-12 production in T cell-dependent experimental colitis. J Immunol. 2006;177:2760–2764. doi: 10.4049/jimmunol.177.5.2760. [DOI] [PubMed] [Google Scholar]
- 45.Iyer N, Corr SC. Gut Microbial Metabolite-Mediated Regulation of the Intestinal Barrier in the Pathogenesis of Inflammatory Bowel Disease. Nutrients. 2021;13 doi: 10.3390/nu13124259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Danese S, Fiocchi C. Etiopathogenesis of inflammatory bowel diseases. World J Gastroenterol. 2006;12:4807–4812. doi: 10.3748/wjg.v12.i30.4807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schirmer M, Garner A, Vlamakis H, Xavier RJ. Microbial genes and pathways in inflammatory bowel disease. Nat Rev Microbiol. 2019;17:497–511. doi: 10.1038/s41579-019-0213-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Palmela C, Chevarin C, Xu Z, Torres J, Sevrin G, Hirten R, Barnich N, Ng SC, Colombel JF. Adherent-invasive Escherichia coli in inflammatory bowel disease. Gut. 2018;67:574–587. doi: 10.1136/gutjnl-2017-314903. [DOI] [PubMed] [Google Scholar]
- 49.Glassner KL, Abraham BP, Quigley EMM. The microbiome and inflammatory bowel disease. J Allergy Clin Immunol. 2020;145:16–27. doi: 10.1016/j.jaci.2019.11.003. [DOI] [PubMed] [Google Scholar]
- 50.Everard A, Belzer C, Geurts L, Ouwerkerk JP, Druart C, Bindels LB, Guiot Y, Derrien M, Muccioli GG, Delzenne NM, de Vos WM, Cani PD. Cross-talk between Akkermansia muciniphila and intestinal epithelium controls diet-induced obesity. Proc Natl Acad Sci U S A. 2013;110:9066–9071. doi: 10.1073/pnas.1219451110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vermeire S, Joossens M, Verbeke K, Wang J, Machiels K, Sabino J, Ferrante M, Van Assche G, Rutgeerts P, Raes J. Donor Species Richness Determines Faecal Microbiota Transplantation Success in Inflammatory Bowel Disease. J Crohns Colitis. 2016;10:387–394. doi: 10.1093/ecco-jcc/jjv203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tan P, Li X, Shen J, Feng Q. Fecal Microbiota Transplantation for the Treatment of Inflammatory Bowel Disease: An Update. Front Pharmacol. 2020;11:574533. doi: 10.3389/fphar.2020.574533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Miao W, Wu X, Wang K, Wang W, Wang Y, Li Z, Liu J, Li L, Peng L. Sodium Butyrate Promotes Reassembly of Tight Junctions in Caco-2 Monolayers Involving Inhibition of MLCK/MLC2 Pathway and Phosphorylation of PKCβ2. Int J Mol Sci. 2016;17 doi: 10.3390/ijms17101696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zheng L, Kelly CJ, Battista KD, Schaefer R, Lanis JM, Alexeev EE, Wang RX, Onyiah JC, Kominsky DJ, Colgan SP. Microbial-Derived Butyrate Promotes Epithelial Barrier Function through IL-10 Receptor-Dependent Repression of Claudin-2. J Immunol. 2017;199:2976–2984. doi: 10.4049/jimmunol.1700105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Duboc H, Rajca S, Rainteau D, Benarous D, Maubert MA, Quervain E, Thomas G, Barbu V, Humbert L, Despras G, Bridonneau C, Dumetz F, Grill JP, Masliah J, Beaugerie L, Cosnes J, Chazouillères O, Poupon R, Wolf C, Mallet JM, Langella P, Trugnan G, Sokol H, Seksik P. Connecting dysbiosis, bile-acid dysmetabolism and gut inflammation in inflammatory bowel diseases. Gut. 2013;62:531–539. doi: 10.1136/gutjnl-2012-302578. [DOI] [PubMed] [Google Scholar]
- 56.Sorrentino G, Perino A, Yildiz E, El Alam G, Bou Sleiman M, Gioiello A, Pellicciari R, Schoonjans K. Bile Acids Signal via TGR5 to Activate Intestinal Stem Cells and Epithelial Regeneration. Gastroenterology. 2020;159:956–968.e8. doi: 10.1053/j.gastro.2020.05.067. [DOI] [PubMed] [Google Scholar]
- 57.Li M, Zhao J, Cao M, Liu R, Chen G, Li S, Xie Y, Xie J, Cheng Y, Huang L, Su M, Xu Y, Zheng M, Zou K, Geng L, Xu W, Gong S. Mast cells-derived MiR-223 destroys intestinal barrier function by inhibition of CLDN8 expression in intestinal epithelial cells. Biol Res. 2020;53:12. doi: 10.1186/s40659-020-00279-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Li DF, Yang MF, Xu J, Xu HM, Zhu MZ, Liang YJ, Zhang Y, Tian CM, Nie YQ, Shi RY, Wang LS, Yao J. Extracellular Vesicles: The Next Generation Theranostic Nanomedicine for Inflammatory Bowel Disease. Int J Nanomedicine. 2022;17:3893–3911. doi: 10.2147/IJN.S370784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rogler G. The effects of NOD2/CARD15 mutations on the function of the intestinal barrier. J Crohns Colitis. 2007;1:53–60. doi: 10.1016/j.crohns.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 60.Hansson GC. Mucins and the Microbiome. Annu Rev Biochem. 2020;89:769–793. doi: 10.1146/annurev-biochem-011520-105053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Johansson ME, Gustafsson JK, Holmén-Larsson J, Jabbar KS, Xia L, Xu H, Ghishan FK, Carvalho FA, Gewirtz AT, Sjövall H, Hansson GC. Bacteria penetrate the normally impenetrable inner colon mucus layer in both murine colitis models and patients with ulcerative colitis. Gut. 2014;63:281–291. doi: 10.1136/gutjnl-2012-303207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Schulzke JD, Siegmund B, Günzel D. New insights into intestinal secretion. Gut. 2014;63:1371–1372. doi: 10.1136/gutjnl-2013-305214. [DOI] [PubMed] [Google Scholar]
- 63.Al-Sadi R, Dharmaprakash V, Nighot P, Guo S, Nighot M, Do T, Ma TY. Bifidobacterium bifidum Enhances the Intestinal Epithelial Tight Junction Barrier and Protects against Intestinal Inflammation by Targeting the Toll-like Receptor-2 Pathway in an NF-κB-Independent Manner. Int J Mol Sci. 2021;22 doi: 10.3390/ijms22158070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Merlin D, Sitaraman S, Liu X, Eastburn K, Sun J, Kucharzik T, Lewis B, Madara JL. CD98-mediated links between amino acid transport and beta 1 integrin distribution in polarized columnar epithelia. J Biol Chem. 2001;276:39282–39289. doi: 10.1074/jbc.M105077200. [DOI] [PubMed] [Google Scholar]