Abstract
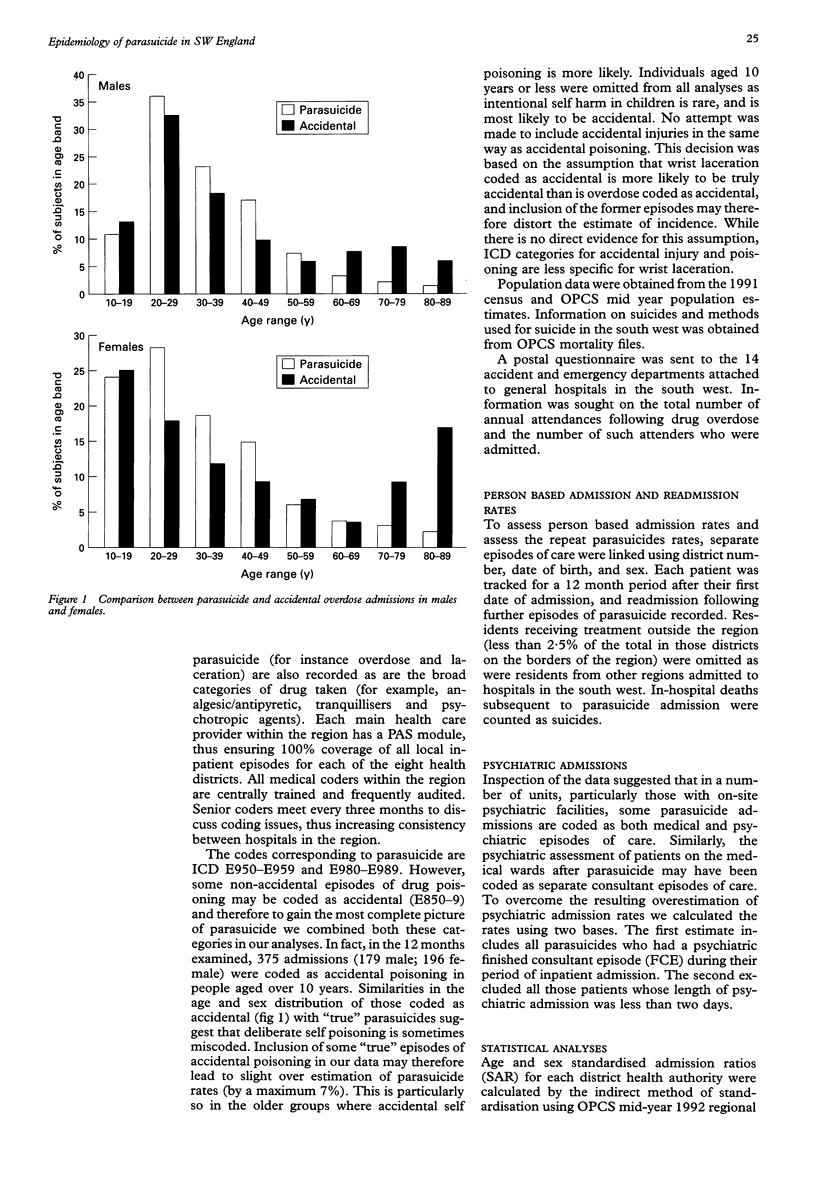
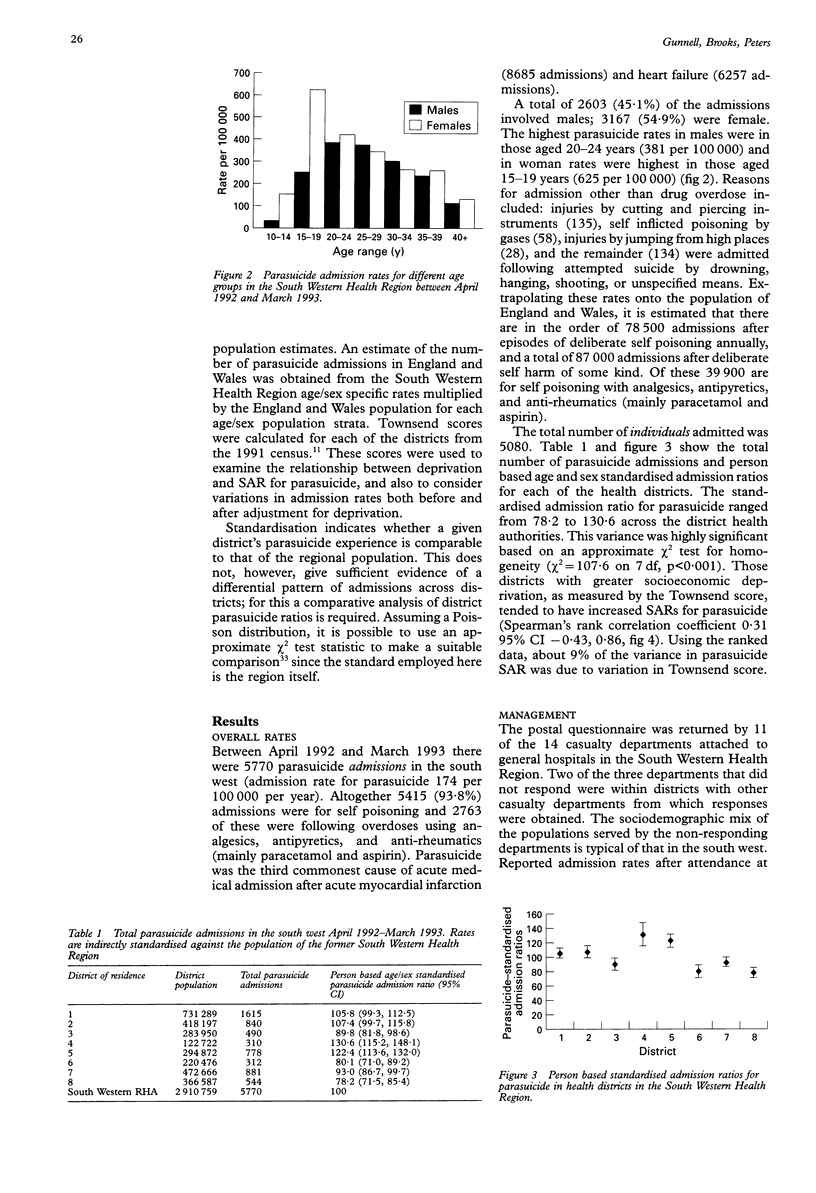
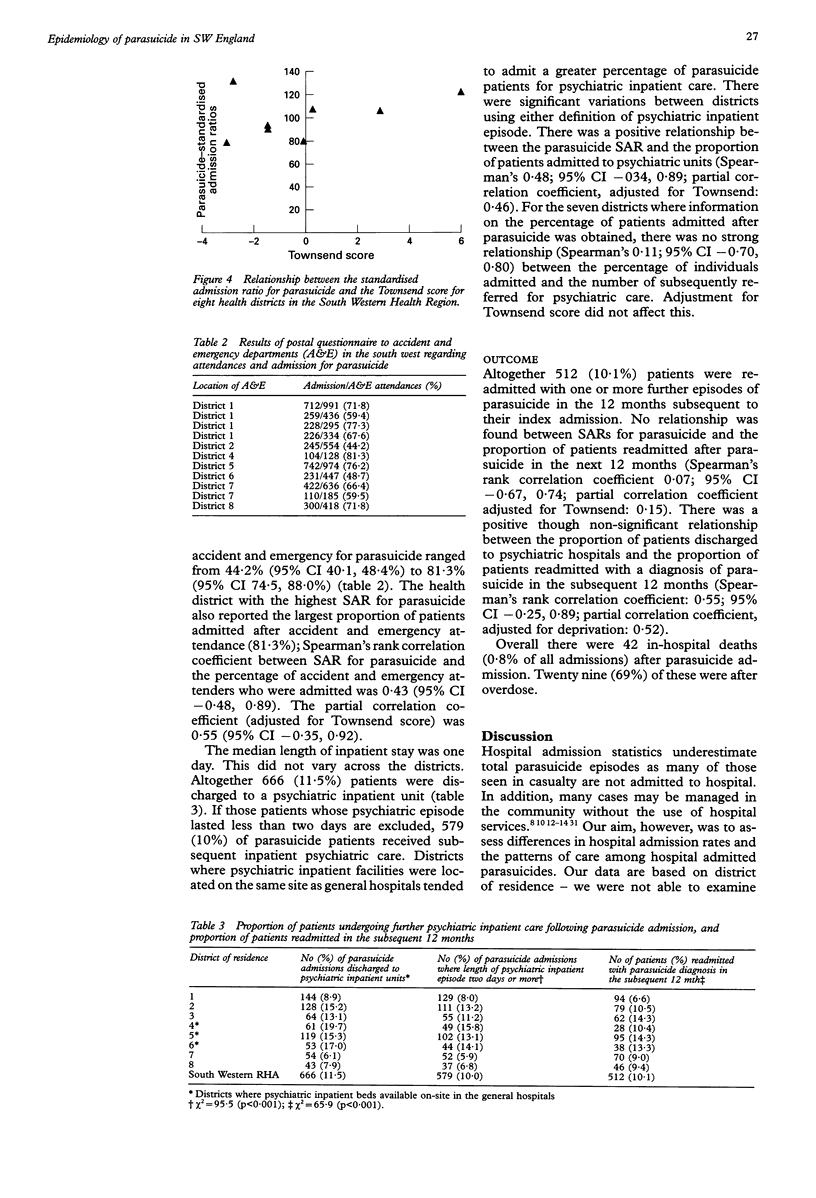
OBJECTIVE: To describe the epidemiology, management, and outcome of parasuicide in the south west of England. DESIGN: Descriptive analysis using routine information systems. SETTING: The former South Western Regional Health Authority, population aged 10 and over: 2.9 million. SUBJECTS: These comprised 5080 residents of the South Western Health Region, admitted on 5770 occasions for parasuicide between April 1992 and March 1993 to hospitals in the south west. MAIN OUTCOME MEASURES: Person based age and sex standardised admission ratios for parasuicide; readmission for parasuicide in the subsequent 12 months; admission to psychiatric hospital after parasuicide; in-hospital mortality for those admitted after attempted suicide. RESULTS: The overall rate of parasuicide admission was 174 per 100,000 per year. Rates were highest in males aged 20-24 (381 per 100,000) and in females aged 15-19 (625 per 100,000). Parasuicide is the third most frequent cause of acute medical admission in the south west. A total of 10.0% of admissions received psychiatric inpatient care as a direct result of their parasuicide admission and 10.1% were readmitted in the following 12 months with a repeat episode of parasuicide. Significant variations in standardised admission ratios for parasuicide were observed between the districts. Some of this variation is related to socioeconomic differences between districts, the rest is probably due to differences in practice between districts. There is no clear evidence that these variations result in differences in readmission rates. Districts where psychiatric inpatient facilities were located on the same site as the general hospital tended to admit a greater percentage of parasuicide patients for psychiatric inpatient care. A quarter of all suicide deaths from overdose occurred in hospital. It is estimated that there are 87,000 parasuicide admissions in England and Wales annually. CONCLUSIONS: Parasuicide is a common cause of acute hospital admission and there is evidence that hospital admission practices for parasuicide vary across the south west. Randomised controlled trials are needed to evaluate the most appropriate form of management for those patients who do not require admission on medical grounds.
Full text
PDF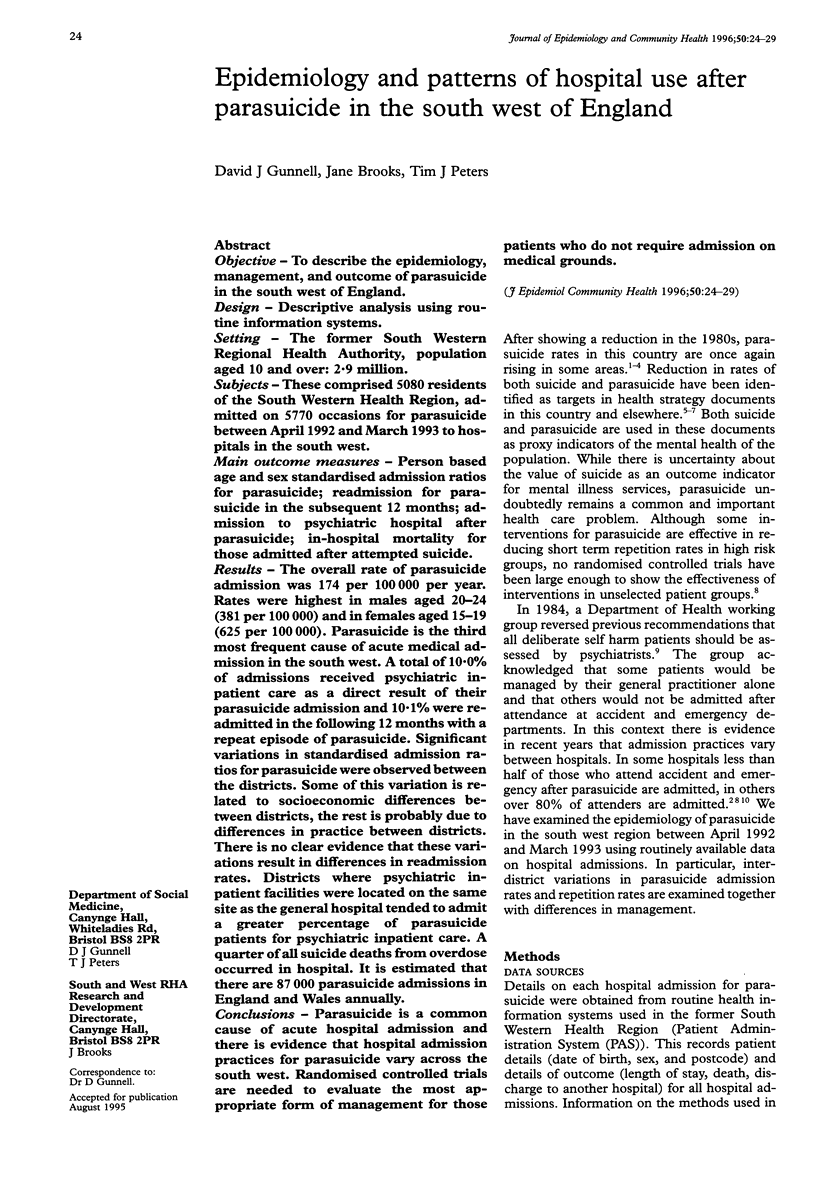
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alderson M. R. National trends in self-poisoning in women. Lancet. 1985 Apr 27;1(8435):974–975. doi: 10.1016/s0140-6736(85)91738-6. [DOI] [PubMed] [Google Scholar]
- Barraclough B., Bunch J., Nelson B., Sainsbury P. A hundred cases of suicide: clinical aspects. Br J Psychiatry. 1974 Oct;125(0):355–373. doi: 10.1192/bjp.125.4.355. [DOI] [PubMed] [Google Scholar]
- Beck P., Lazarus J., Scorer R., Smith P., Routledge P. Increasing rate of deliberate self poisoning. BMJ. 1994 Mar 19;308(6931):789–789. doi: 10.1136/bmj.308.6931.789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron I., Renvoize E., Garside G. Deliberate self-poisoning: the need for a new approach. Health Trends. 1990;22(3):126–128. [PubMed] [Google Scholar]
- Dennis M., Owens D., Jones S. Epidemiology of deliberate self-poisoning: trends in hospital attendances. Health Trends. 1990;22(3):125–126. [PubMed] [Google Scholar]
- Deykin E. Y., Hsieh C. C., Joshi N., McNamarra J. J. Adolescent suicidal and self-destructive behavior. Results of an intervention study. J Adolesc Health Care. 1986 Mar;7(2):88–95. doi: 10.1016/s0197-0070(86)80002-x. [DOI] [PubMed] [Google Scholar]
- Ettlinger R. Evaluation of suicide prevention after attempted suicide. Acta Psychiatr Scand Suppl. 1975;260:1–135. [PubMed] [Google Scholar]
- Gibbons J. S., Butler J., Urwin P., Gibbons J. L. Evaluation of a social work service for self-poisoning patients. Br J Psychiatry. 1978 Aug;133:111–118. doi: 10.1192/bjp.133.2.111. [DOI] [PubMed] [Google Scholar]
- Gunnell D. J., Peters T. J., Kammerling R. M., Brooks J. Relation between parasuicide, suicide, psychiatric admissions, and socioeconomic deprivation. BMJ. 1995 Jul 22;311(6999):226–230. doi: 10.1136/bmj.311.6999.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnell D., Frankel S. Prevention of suicide: aspirations and evidence. BMJ. 1994 May 7;308(6938):1227–1233. doi: 10.1136/bmj.308.6938.1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawton K., Fagg J. Suicide, and other causes of death, following attempted suicide. Br J Psychiatry. 1988 Mar;152:359–366. doi: 10.1192/bjp.152.3.359. [DOI] [PubMed] [Google Scholar]
- Hawton K., Fagg J. Trends in deliberate self poisoning and self injury in Oxford, 1976-90. BMJ. 1992 May 30;304(6839):1409–1411. doi: 10.1136/bmj.304.6839.1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawton K., McKeown S., Day A., Martin P., O'Connor M., Yule J. Evaluation of out-patient counselling compared with general practitioner care following overdoses. Psychol Med. 1987 Aug;17(3):751–761. doi: 10.1017/s0033291700025988. [DOI] [PubMed] [Google Scholar]
- Kennedy P., Kreitman N. An epidemiological survey of parasuicide ('attempted suicide') in general practice. Br J Psychiatry. 1973 Jul;123(572):23–34. doi: 10.1192/bjp.123.1.23. [DOI] [PubMed] [Google Scholar]
- Linehan M. M., Armstrong H. E., Suarez A., Allmon D., Heard H. L. Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Arch Gen Psychiatry. 1991 Dec;48(12):1060–1064. doi: 10.1001/archpsyc.1991.01810360024003. [DOI] [PubMed] [Google Scholar]
- Monk M. Epidemiology of suicide. Epidemiol Rev. 1987;9:51–69. doi: 10.1093/oxfordjournals.epirev.a036308. [DOI] [PubMed] [Google Scholar]
- Montgomery S. A., Montgomery D. Pharmacological prevention of suicidal behaviour. J Affect Disord. 1982 Dec;4(4):291–298. doi: 10.1016/0165-0327(82)90026-x. [DOI] [PubMed] [Google Scholar]
- Nordentoft M., Breum L., Munck L. K., Nordestgaard A. G., Hunding A., Laursen Bjaeldager P. A. High mortality by natural and unnatural causes: a 10 year follow up study of patients admitted to a poisoning treatment centre after suicide attempts. BMJ. 1993 Jun 19;306(6893):1637–1641. doi: 10.1136/bmj.306.6893.1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillimore P., Beattie A., Townsend P. Widening inequality of health in northern England, 1981-91. BMJ. 1994 Apr 30;308(6937):1125–1128. doi: 10.1136/bmj.308.6937.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Platt S., Hawton K., Kreitman N., Fagg J., Foster J. Recent clinical and epidemiological trends in parasuicide in Edinburgh and Oxford: a tale of two cities. Psychol Med. 1988 May;18(2):405–418. doi: 10.1017/s0033291700007959. [DOI] [PubMed] [Google Scholar]
- Salkovskis P. M., Atha C., Storer D. Cognitive-behavioural problem solving in the treatment of patients who repeatedly attempt suicide. A controlled trial. Br J Psychiatry. 1990 Dec;157:871–876. doi: 10.1192/bjp.157.6.871. [DOI] [PubMed] [Google Scholar]
- Sellar C., Goldacre M. J., Hawton K. Reliability of routine hospital data on poisoning as measures of deliberate self poisoning in adolescents. J Epidemiol Community Health. 1990 Dec;44(4):313–315. doi: 10.1136/jech.44.4.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stark C., Smith H., Hall D. Increase in parasuicide in Scotland. BMJ. 1994 Jun 11;308(6943):1569–1570. doi: 10.1136/bmj.308.6943.1569a. [DOI] [PMC free article] [PubMed] [Google Scholar]


