Abstract
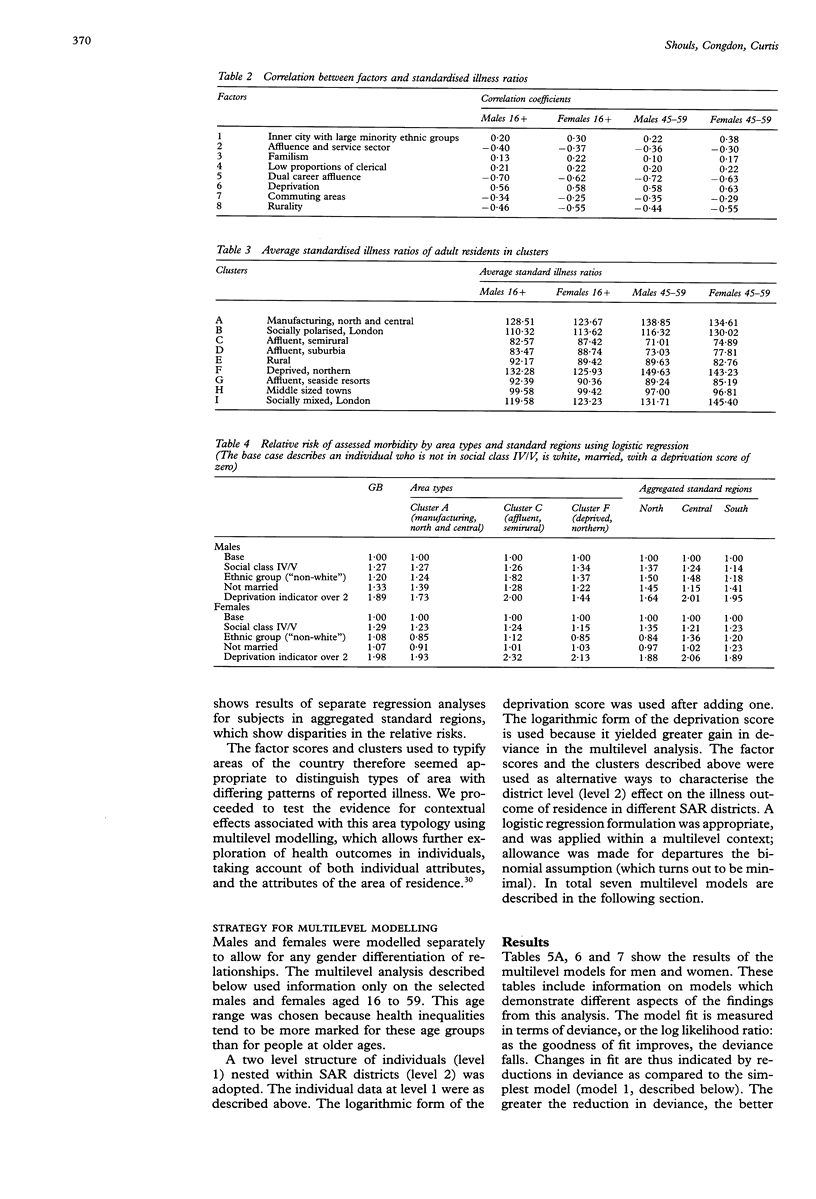
STUDY OBJECTIVE: To assess the nature of the relation between health and social factors at both the aggregated scale of geographical areas and the individual scale. DESIGN AND SETTING: The individual data are derived from the sample of anonymised records (SAR) from the census of 1991 in Great Britain, and are combined with area data from this census. The ecological setting (context) was defined using multivariate methods to classify the 278 districts of residence identifiable in the SAR. The outcome health variable is the 1991 census long-term limiting illness question. Health variations were analysed by multilevel logistic regression to examine the compositional variation (at the level of the individual) and the contextual variation (variability operating at the level of districts) in reported illness. PARTICIPANTS: 10 per cent randomised subsample of the SAR who are aged 16+ and are resident in households. MAIN RESULTS: The multi-level modelling revealed that area factors have a significant association with individual health outcome but their effect is smaller than that of individual attributes. The results show evidence for both compositional and contextual effects in the pattern of variation in propensity to report illness. CONCLUSIONS: The results suggest generally higher levels of ill health for individuals who are older, not married, in a semi/unskilled manual social class, and socioeconomically deprived (as measured by a composite deprivation score). All individuals living in areas with high levels of illness (which tend to be more deprived areas) show greater morbidity, even after allowing for their individual characteristics. However, within affluent areas, where morbidity was generally lower, the health inequality (health gradient) between rich and poor individuals was particularly strong. We consider the implications of these findings for health and resource allocation policy.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Duncan C., Jones K., Moon G. Do places matter? A multi-level analysis of regional variations in health-related behaviour in Britain. Soc Sci Med. 1993 Sep;37(6):725–733. doi: 10.1016/0277-9536(93)90366-c. [DOI] [PubMed] [Google Scholar]
- Eames M., Ben-Shlomo Y., Marmot M. G. Social deprivation and premature mortality: regional comparison across England. BMJ. 1993 Oct 30;307(6912):1097–1102. doi: 10.1136/bmj.307.6912.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox A. J., Jones D. R., Goldblatt P. O. Approaches to studying the effect of socio-economic circumstances on geographic differences in mortality in England and Wales. Br Med Bull. 1984 Oct;40(4):309–314. doi: 10.1093/oxfordjournals.bmb.a071996. [DOI] [PubMed] [Google Scholar]
- Humphreys K., Carr-Hill R. Area variations in health outcomes: artefact or ecology. Int J Epidemiol. 1991 Mar;20(1):251–258. doi: 10.1093/ije/20.1.251. [DOI] [PubMed] [Google Scholar]
- Ostlin P. Occupational history, self reported chronic illness, and mortality: a follow up of 25,586 Swedish men and women. J Epidemiol Community Health. 1990 Mar;44(1):12–16. doi: 10.1136/jech.44.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillimore P. R., Morris D. Discrepant legacies: premature mortality in two industrial towns. Soc Sci Med. 1991;33(2):139–152. doi: 10.1016/0277-9536(91)90174-b. [DOI] [PubMed] [Google Scholar]
- Phillimore P., Reading R. A rural advantage? Urban-rural health differences in northern England. J Public Health Med. 1992 Sep;14(3):290–299. [PubMed] [Google Scholar]
- Reading R., Openshaw S., Jarvis S. Are multidimensional social classifications of areas useful in UK health service research? J Epidemiol Community Health. 1994 Apr;48(2):192–200. doi: 10.1136/jech.48.2.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloggett A., Joshi H. Higher mortality in deprived areas: community or personal disadvantage? BMJ. 1994 Dec 3;309(6967):1470–1474. doi: 10.1136/bmj.309.6967.1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wannamethee G., Shaper A. G. Self-assessment of health status and mortality in middle-aged British men. Int J Epidemiol. 1991 Mar;20(1):239–245. doi: 10.1093/ije/20.1.239. [DOI] [PubMed] [Google Scholar]
- Watt I. S., Franks A. J., Sheldon T. A. Health and health care of rural populations in the UK: is it better or worse? J Epidemiol Community Health. 1994 Feb;48(1):16–21. doi: 10.1136/jech.48.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]


