Abstract
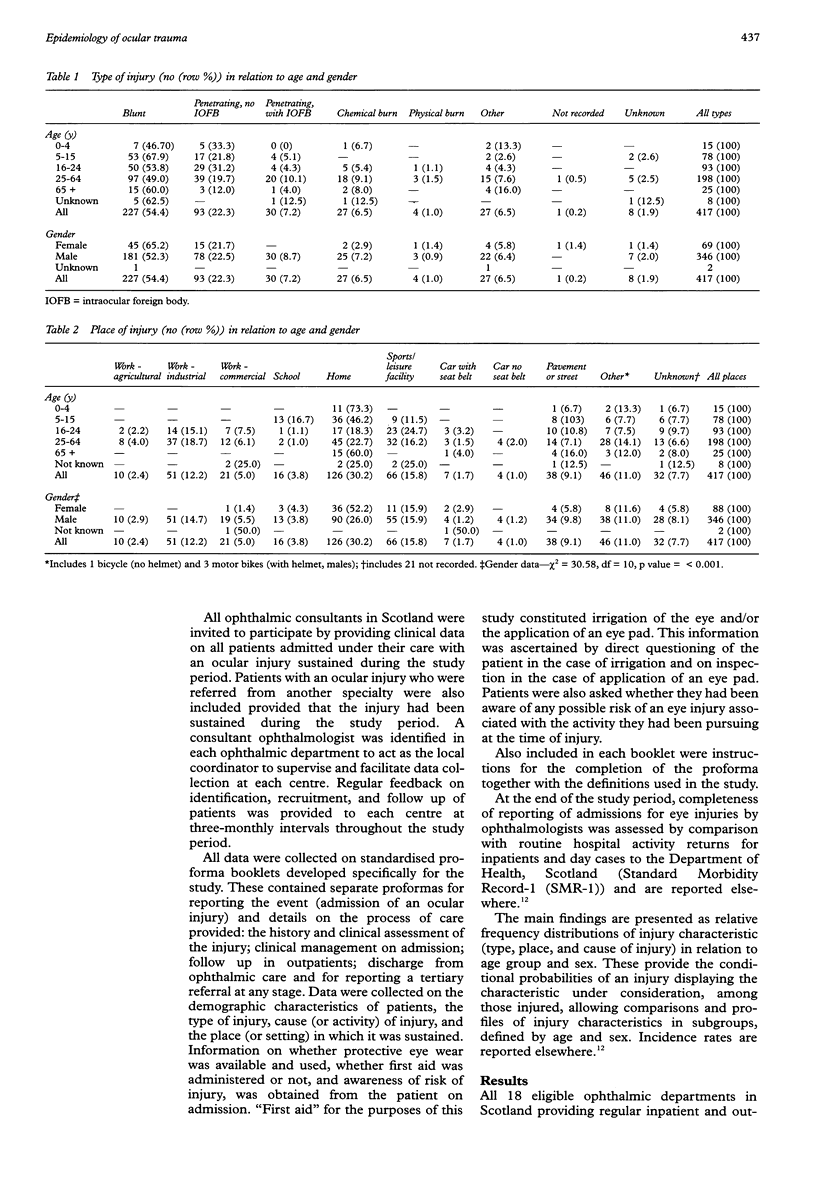
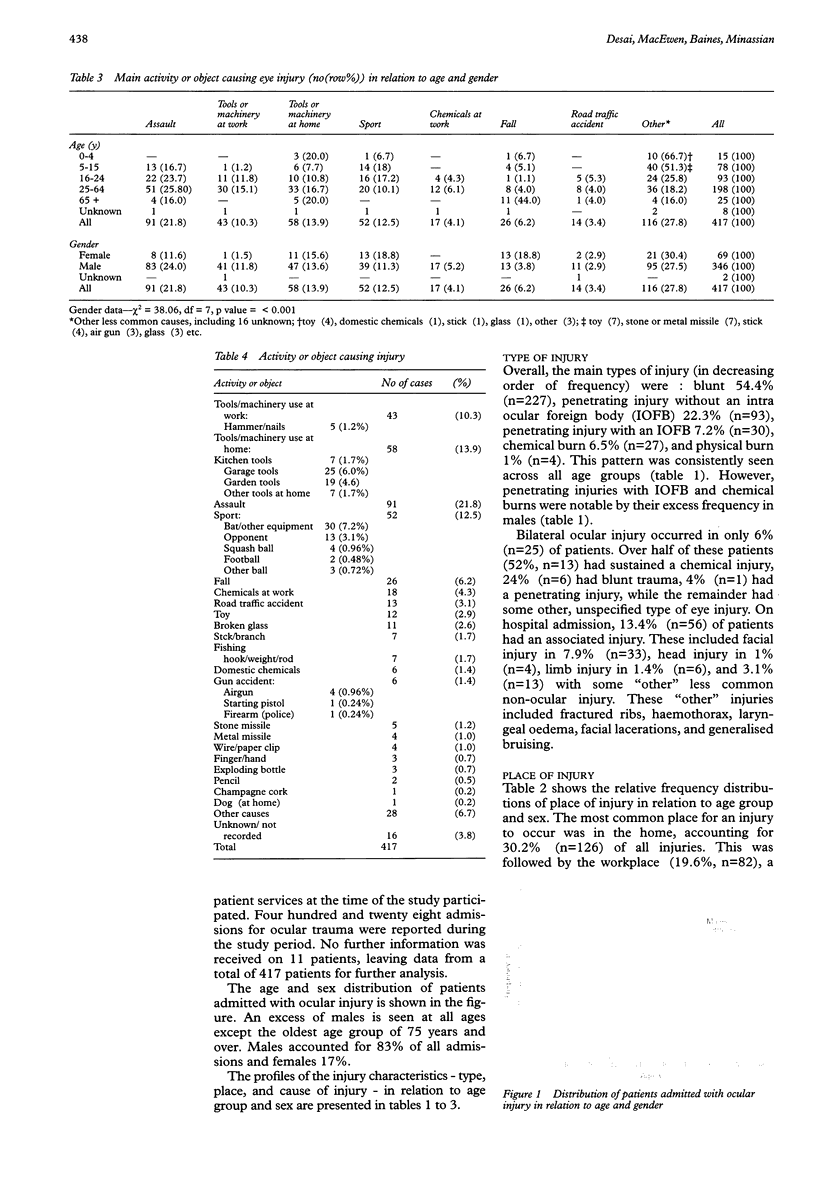
OBJECTIVES: To describe the current epidemiology of serious ocular trauma which necessitates admission to hospital so that health and safety strategies for the prevention of ocular injuries and their role within the national health strategy, The Health of the Nation, can be better informed. DESIGN: A prospective observational study of all patients with ocular trauma admitted to hospital under the care of a consultant ophthalmologist between 1 November 1991 and 31 October 1992. SETTING: All ophthalmic department in Scotland. SUBJECTS: All patients with ocular trauma admitted to hospital in Scotland. The population of Scotland represented the population at risk of injury. MEASURES AND MAIN RESULTS: Measures included the type and cause of injury, the place where it occurred, and awareness of risk and safety. All ophthalmic departments in Scotland participated and 428 admissions were reported. The home was the most common place for a serious injury to occur (30.2%), followed by the workplace (19.6%) and a sports or leisure facility (15.8%). The home was the single most frequent place of injury for the 0-15 year and 65 year and over age groups. Tools or machinery, either at home (13.9%) or at work (10.3%), were collectively (24.2%) the most frequent cause of injury, followed by assault (21.8%) and sports-related activities (12.5%). The most frequent type of injury was a blunt injury (54.4%). Six per cent (n = 25) of all injuries were bilateral. Only 13.2% of patients were aware of any risk of injury, with 5.6% aware of any risk at home. When applicable, protective eye wear was only available to 48.6% of patients and only 19.4% of these used it. CONCLUSION: Serious ocular trauma frequently occurs at home and the young and the elderly are particularly at risk. This represents a significant change in the epidemiology of serious ocular trauma and has important implications for prevention. Health and safety strategies specifically aimed at preventing eye injury should now include the home as a high risk environment in addition to the work-place and sports/leisure facilities. The target groups for accident prevention in The Health of the Nation strategy include those at risk of serious ocular trauma with potentially sight threatening sequelae. Those involved in implementing the national accident prevention strategy should be aware of this, for in this process it is possible that some serious eye injuries may also be prevented.
Full text
PDF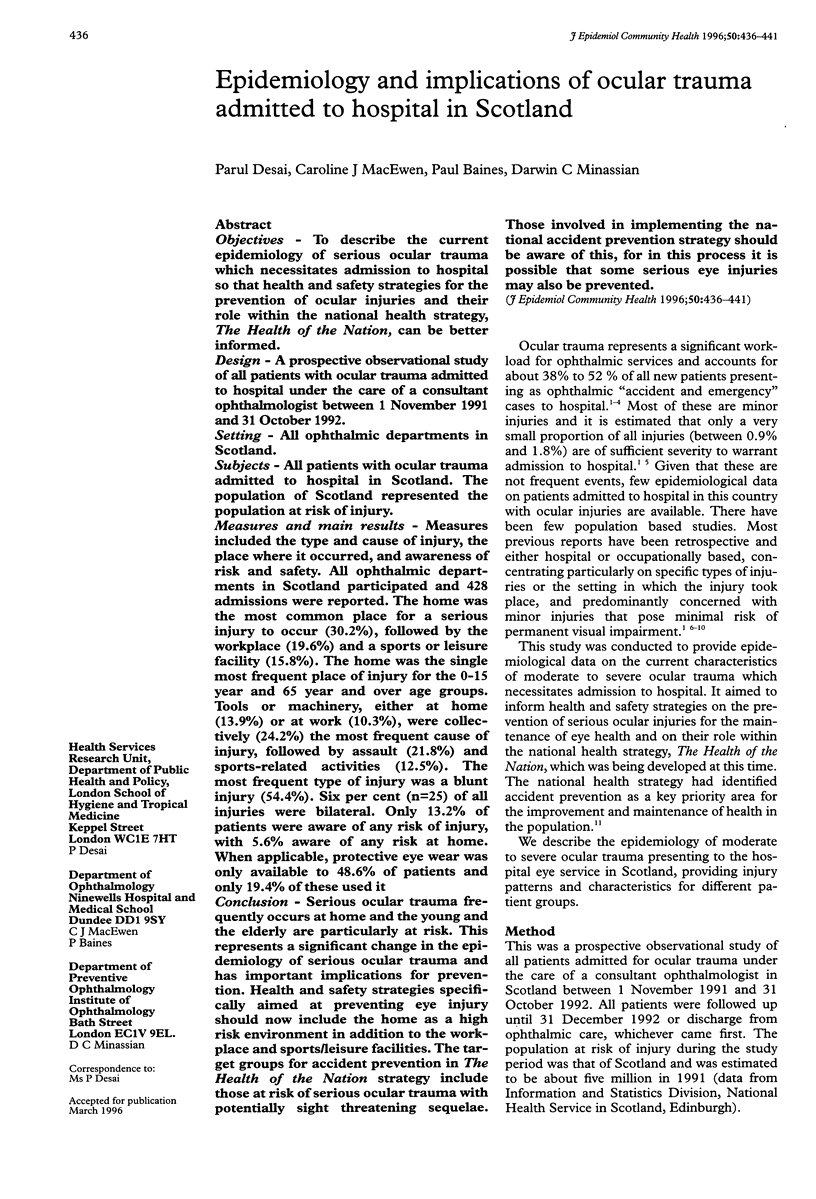
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bhopal R. S., Parkin D. W., Gillie R. F., Han K. H. Pattern of ophthalmological accidents and emergencies presenting to hospitals. J Epidemiol Community Health. 1993 Oct;47(5):382–387. doi: 10.1136/jech.47.5.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canavan Y. M., O'Flaherty M. J., Archer D. B., Elwood J. H. A 10-year survey of eye injuries in Northern Ireland, 1967-76. Br J Ophthalmol. 1980 Aug;64(8):618–625. doi: 10.1136/bjo.64.8.618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiapella A. P., Rosenthal A. R. One year in an eye casualty clinic. Br J Ophthalmol. 1985 Nov;69(11):865–870. doi: 10.1136/bjo.69.11.865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole M. D., Clearkin L., Dabbs T., Smerdon D. The seat belt law and after. Br J Ophthalmol. 1987 Jun;71(6):436–440. doi: 10.1136/bjo.71.6.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dannenberg A. L., Parver L. M., Brechner R. J., Khoo L. Penetration eye injuries in the workplace. The National Eye Trauma System Registry. Arch Ophthalmol. 1992 Jun;110(6):843–848. doi: 10.1001/archopht.1992.01080180115038. [DOI] [PubMed] [Google Scholar]
- Dannenberg A. L., Parver L. M., Fowler C. J. Penetrating eye injuries related to assault. The National Eye Trauma System Registry. Arch Ophthalmol. 1992 Jun;110(6):849–852. doi: 10.1001/archopht.1992.01080180121039. [DOI] [PubMed] [Google Scholar]
- Hall N. F., Denning A. M., Elkington A. R., Cooper P. J. The eye and the seatbelt in Wessex. Br J Ophthalmol. 1985 May;69(5):317–319. doi: 10.1136/bjo.69.5.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilsar M., Chirambo M., Belkin M. Ocular injuries in Malawi. Br J Ophthalmol. 1982 Feb;66(2):145–148. doi: 10.1136/bjo.66.2.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones N. P., Griffith G. A. Eye injuries at work: a prospective population-based survey within the chemical industry. Eye (Lond) 1992;6(Pt 4):381–385. doi: 10.1038/eye.1992.78. [DOI] [PubMed] [Google Scholar]
- Jones N. P., Hayward J. M., Khaw P. T., Claoué C. M., Elkington A. R. Function of an ophthalmic "accident and emergency" department: results of a six month survey. Br Med J (Clin Res Ed) 1986 Jan 18;292(6514):188–190. doi: 10.1136/bmj.292.6514.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlson T. A., Klein B. E. The incidence of acute hospital-treated eye injuries. Arch Ophthalmol. 1986 Oct;104(10):1473–1476. doi: 10.1001/archopht.1986.01050220067028. [DOI] [PubMed] [Google Scholar]
- Klopfer J., Tielsch J. M., Vitale S., See L. C., Canner J. K. Ocular trauma in the United States. Eye injuries resulting in hospitalization, 1984 through 1987. Arch Ophthalmol. 1992 Jun;110(6):838–842. doi: 10.1001/archopht.1992.01080180110037. [DOI] [PubMed] [Google Scholar]
- Koval R., Teller J., Belkin M., Romem M., Yanko L., Savir H. The Israeli Ocular Injuries Study. A nationwide collaborative study. Arch Ophthalmol. 1988 Jun;106(6):776–780. doi: 10.1001/archopht.1988.01060130846037. [DOI] [PubMed] [Google Scholar]
- Liggett P. E., Pince K. J., Barlow W., Ragen M., Ryan S. J. Ocular trauma in an urban population. Review of 1132 cases. Ophthalmology. 1990 May;97(5):581–584. doi: 10.1016/s0161-6420(90)32539-3. [DOI] [PubMed] [Google Scholar]
- Macewen C. J. Eye injuries: a prospective survey of 5671 cases. Br J Ophthalmol. 1989 Nov;73(11):888–894. doi: 10.1136/bjo.73.11.888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tielsch J. M., Parver L., Shankar B. Time trends in the incidence of hospitalized ocular trauma. Arch Ophthalmol. 1989 Apr;107(4):519–523. doi: 10.1001/archopht.1989.01070010533025. [DOI] [PubMed] [Google Scholar]
- Vernon S. A. Analysis of all new cases seen in a busy regional centre ophthalmic casualty department during 24-week period. J R Soc Med. 1983 Apr;76(4):279–282. doi: 10.1177/014107688307600408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood C. Metastases to the conjunctiva. Br J Ophthalmol. 1996 Jan;80(1):1–1. doi: 10.1136/bjo.80.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wykes W. N. A 10-year survey of penetrating eye injuries in Gwent, 1976-85. Br J Ophthalmol. 1988 Aug;72(8):607–611. doi: 10.1136/bjo.72.8.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zagelbaum B. M., Tostanoski J. R., Kerner D. J., Hersh P. S. Urban eye trauma. A one-year prospective study. Ophthalmology. 1993 Jun;100(6):851–856. doi: 10.1016/s0161-6420(93)31564-2. [DOI] [PubMed] [Google Scholar]