Abstract
Background and Objectives: The oral cavity is inhabited by pathogenic bacteria, whose growth can be inhibited by synthetic oral drugs, including antibiotics and other chemical compounds. Natural antimicrobial substances that elicit fewer negative side effects may serve as alternatives to synthetic agents for long-term use. Thus, the aim of this study was to evaluate the effects of edible mixed herbal extracts on the growth of oral pathogenic bacteria. Materials and Methods: The yield of each herbal extract was as follows: 5% Schizonepeta tenuifolia Briq (STB), 10.94% Mentha piperascens (MP), 5.47% Acanthopanax sessiliflorus Seem (AS), and 10.66% Glycyrrhiza uralensis (GU). The herbal extracts used included 0.5 mg/mL STB, 1.5 mg/mL MP, 1.5 mg/mL AS, and 2.0 mg/mL GU. Antimicrobial tests, morphological analyses (using scanning electron microscopy), microbial surface hydrophobicity measurements, and oral malodor reduction tests were performed using each extract. Statistical analyses were performed with IBM® SPSS® (version 24), using paired t-tests. Results: The mixed herbal extracts significantly inhibited the growth of Streptococcus mutans, Enterococcus faecalis, Candida albicans, and Porphyromonas gingivalis compared to the control (p < 0.001). Scanning electron microscopy results further revealed altered cellular morphology in the groups treated with the mixed herbal extracts. Additionally, the hydrophobicity assay results showed that the mixed herbal extracts reduced the oral adhesion capacities of bacteria (p < 0.001). Administration of the mixed herbal extracts also reduced the levels of volatile sulfur compounds, the main contributors to oral malodor (p < 0.001). Conclusions: Edible mixed herbal extracts can effectively eliminate oral pathogens and may be useful for improving oral health. The herbal extracts used were effective against all species of oral pathogens studied in this report.
Keywords: Acanthopanax sessiliflorus Seem, antimicrobial, Glycyrrhiza uralensis, Mentha piperascens, oral pathogens, Schizonepeta tenuifolia Briq
1. Introduction
The human oral cavity is inhabited by over 700 different bacterial species, some of which are disease-causing pathogens that can induce gastrointestinal dysfunction and tooth loss [1]. White spot lesions that develop due to Streptococcus mutans (S. mutans) retention in plaque can accumulate around orthodontic brackets and lead to enamel demineralization, based on studies using simulated cariogenic environments [2]. When streptococci accumulate in the mouth (via attachment to the initially acquired pellicle), plaques (comprising the bacterial cells, glycoproteins, and polysaccharides) can form. This then generates acids, which form a solid cluster and cause demineralization [3,4]. Furthermore, oral pathogens also induce dental pulp disease and fungal infections [5], and can cause both oral and systemic diseases [6]. Thus, substances that can selectively inhibit dental bacteria are necessary to prevent diseases caused by oral microorganisms.
To prevent and/or suppress the progression of bacterial oral diseases, the causal pathogen must be eliminated; this is typically achieved with mouthrinses or antibiotics. Chlorhexidine gluconate (CHX) is a widely utilized agent in mouthwashes that is effective in preventing plaque formation and oral microbial growth [7]. Octenidine (OCT) significantly inhibited plaque formation, gingivitis, and oral microbial growth, and was more effective than placebos and other common chemical agents used for plaque control [7]. However, currently used antimicrobial agents such as CHX and OCT can exert harmful effects on the body after long-term use, as well as having various side effects, including microbial drug resistance [8,9].
To overcome these limitations, natural herbal extracts with high pharmacological efficacy and low toxicity have recently been applied to inhibit the growth of oral pathogens and prevent oral diseases [10,11]. For instance, flavanone and flavanol (isolated from natural herbal extracts) can inhibit the glucosyltransferases that cause dental caries [12], while natural mulberry [13], green tea [14], and cardinal [15] extracts can inhibit oral pathogens.
STB is an annual plant in the Lamiaceae family; the whole plant, commonly known as catnip, is primarily used for medicinal purposes due to its antioxidant, anti-inflammatory, antiviral [16], hemostatic, and antimicrobial [17] effects. MP is a perennial herb in the Lamiaceae family with known anticancer [18], anti-allergic [19], antioxidant [20], and analgesic effects [21]. AS is a deciduous shrub in the Araliaceae family, and its roots and bark (as well as those of plants in the same genus) are used as medicinal herbs. Chiisanoside is among the main components of these extracts and has anti-inflammatory, anti-diabetic, and antiviral effects [22], with positive efficacies in diabetes, cancer, and rheumatoid arthritis [23]. Chiisanoside also exerts potent antioxidant effects by preventing DNA damage caused by oxidative stress or protein glycation [24]. GU is a perennial herb in the Fabaceae family; its roots and rhizomes are used as herbal medicines with various pharmacological effects including detoxification, antiulcer, anti-inflammation, antispasmodic, anti-hepatotoxic, and antitussive activities [25]. Moreover, GU contains licopyranocoumarin and licoarylcoumarin, which have antiviral effects, as well as glycyrol and glycycoumarin, which have antimicrobial effects [26]. The antibacterial effects of mixtures of STB, MP, AS, and GU against oral pathogens are currently unclear. We aimed to determine whether edible natural extracts can be used as alternatives to overcome the limitations of conventional chemical mouthwashes. In this study, we aimed to confirm the antimicrobial (bactericidal) effect of these natural herbal extracts, and also evaluate whether they can mitigate halitosis in vitro. The null hypothesis was that no difference in survival rates would be observed between bacteria treated with and without the mixed herbal extracts.
2. Materials and Methods
2.1. Herbal Extracts
STB, MP, AS, and GU were purchased from Jecheon Herbal Medicine (Jecheon, Korea) and their antimicrobial efficacies were evaluated using antimicrobial tests. The herbs were dried and sectioned at the time of purchase. Each herbal material was finely ground, and 100 g of the ground material was mixed with 10× 70% ethanol (Sigma-Aldrich, St. Louis, MO, USA). The mixture was shaken at 60 °C for 12 h. The supernatants were isolated via filtration through filter paper and then concentrated using a vacuum evaporator (R-114; BÜUCHI, Flawil, Switzerland). The concentrate of each herbal extract was dehydrated using a freeze-dryer (FD, Ilshin Lab, Yangju, Korea) at −92 °C and then dissolved in dimethyl sulfoxide (Sigma-Aldrich, St. Louis, MO, USA) for subsequent use. The yield of each herbal extract was as follows: 5% STB, 10.94% MP, 5.47% ASS, and 10.66% GU [27]. Table 1 shows the concentration of each herbal extract, based on which combinations of STB, MP, ASS, and GU extracts were prepared.
Table 1.
Composition of mixed herbal extracts used in the experiments.
| Scientific Name | Plant Part | Concentration (mg/mL) |
|---|---|---|
| Schizonepeta tenuifolia | Above-ground | 0.5 |
| Mentha piperascens | Leaf | 1.5 |
| Acanthopanax sessiliflorus Seem | Bark | 1.5 |
| Glycyrrhiza uralensis | Root | 2 |
2.2. Test Strains and Culture Conditions
Table 2 shows the microbial strains studied and their respective culture conditions. All strains were obtained from the Korean Collection for Type Cultures of the Korea Research Institute of Bioscience and Biotechnology (Daejeon, Korea). The strains were sub-cultured at least three times prior to use. The growth media were purchased from Sigma (Sigma-Aldrich, St. Louis, MO, USA).
Table 2.
Studied microorganisms and culture requirements.
| Strains | Straining Property | Culture Requirement | Media |
|---|---|---|---|
| S. mutans a (KCTC b3065) | Gram-positive | Facultative anaerobic | Brain heart infusion/agar |
| E. faecalis c (KCTC2011) | Gram-positive | Facultative anaerobic | Brain heart infusion/agar |
| C. albicans d (KCTC7965) | Gram-positive | Aerobic | YM broth/agar |
| P. gingivalis e (KCTC5352) | Gram-negative | Anaerobic | Tryptic soy broth/agar |
a Streptococcus mutans (S. mutans); b Korean Collection for Type Cultures (KCTC); c Enterococcus faecalis (E. faecalis); d Candida albicans (C. albicans); e Porphyromonas gingivalis (P. gingivalis).
2.3. Antimicrobial Efficacy of Mixed Herbal Extracts
To determine the viable cell count of the oral microbial strains, each test strain was cultured at 5 × 104 colony-forming units (CFU)/mL; a mixture of 100 μL of bacteria and 900 μL of the mixed herbal extracts was prepared and cultured for 6 h. The cultured bacteria were spread on an agar dish (SPL Life Sciences, Pocheon, Korea) and cultured for 24 h in a 37 °C incubator (SPL Life Sciences, Pocheon, Korea), after which the viable cells were counted [28]. To improve the statistical validity, each measurement was performed in triplicate. The rate of microbial growth inhibition was calculated using the following equation:
2.4. Morphological Examination of Oral Pathogens via Scanning Electron Microscopy
Bacteria in the control and experimental groups were inoculated in liquid media at 5 × 105 CFU/mL. In the experimental group, the mixed herbal extracts were diluted to 5.5 mg/mL and added to the liquid media. The control and experimental groups were cultured at 37 °C for 24 h, after which the bacteria were transferred to a 1.5 mL tube for centrifugation at 3000 revolutions per minute (rpm) for 5 min. The supernatant was removed, and the pellet was washed with distilled water and centrifuged again at 5000 rpm for 5 min. The supernatant was removed, and the pellet was fixed in 2.5% glutaraldehyde solution (0.1 M sodium cacodylate buffer, pH 7.2, 4 °C) for 1 h, before being centrifuged again. Subsequently, 300 μL of 1% osmium tetroxide was added to the supernatant; a drop of the mixture was then placed on a cover slide for fixation for 1 h. The fixed bacteria were dehydrated by successively increasing the ethanol concentration to 50%, 70%, 80%, 95%, and 100%. After freeze-drying and gold-coating, images of each sample were acquired using scanning electron microscopy (Hitachi, Tokyo, Japan) [29].
2.5. Microbial Surface Hydrophobicity
The effects of the mixed herbal extracts on the surface hydrophobicity of each microbial strain were measured. The absorbance of each strain was set to 0.3 for optical density (OD)550 analysis. A total of 2 mL of the microbial suspension was added to a 15 mL round tube along with an equal amount of n-hexadecane (Sigma-Aldrich, St. Louis, MO, USA), and the sample was mixed for 1 min with a vortex mixer. The mixed herbal extracts were left to stand at room temperature for 30 min, after which the supernatant was removed and the absorbance at OD550 was measured using a spectrophotometer (Multiskan Go, Thermo Fisher Scientific, Waltham, MA, USA). Cell surface hydrophobicity was calculated using the following equation: %HP (hydrophobic) = [OD (initial) − OD (expt)] × 100/OD (initial). All measurements were performed in triplicate for statistical analysis [30].
2.6. Oral Malodor Reduction
Oral chroma (CHM-1, Nissha FIS, Inc., Osaka, Japan) was used to measure reductions in oral malodor. For the control group, liquid medium was placed in a 15 mL tube and inoculated with 5 × 105 CFU/mL bacteria. The experimental group was prepared in the same manner as the control group; however, 5.5 mg/mL of mixed herbal extracts was also added. The control and experimental groups were cultured for 6 h. A syringe was then inserted into the tube to collect the gas from the cultured bacteria. The gas was applied to the oral chroma, and the volatile sulfur compound (VSC) concentrations were measured. All measurements were performed in triplicate [31].
2.7. Data Analysis
All experiments were repeated three times, and the results were analyzed using SPSS Statistics 24.0 software (SPSS, Inc., Chicago, IL, USA) [32]. The normality of the data was assessed using the Shapiro–Wilk test. The significance of differences between the control and experimental groups was determined using paired t-tests. p < 0.05 was considered statistically significant.
3. Results
3.1. Inhibitory Effects of Mixed Herbal Extracts on Oral Pathogens
We aimed to determine the antimicrobial effects of the mixed herbal extracts (containing STB, MP, AS, and GU) on each oral pathogen strain. Treatment with the mixed herbal extracts significantly decreased the colony-forming ability of S. mutans, Enterococcus faecalis (E. faecalis), Candida albicans (C. albicans), and Porphyromonas gingivalis (Figure 1; p < 0.001). When treated with the mixed herbal extracts, S. mutans decreased from 5.90 ± 0.01 to 1.48 ± 0.03**, E. faecalis decreased from 5.95 ± 0.01 to 1.49 ± 0.05**, C. albicans decreased from 5.85 ± 0.02 to 0.90 ± 0.03**, and P. gingivalis decreased from 5.74 ± 0.01 to 0.95 ± 0.03**. The counts of S. mutans, E. faecalis, C. albicans, and P. gingivalis were reduced by 3.94 logarithm (log), 4.01 log, 4.94 log, and 4.79 log, respectively, when treated with the mixed herbal extracts (Table 3).
Figure 1.
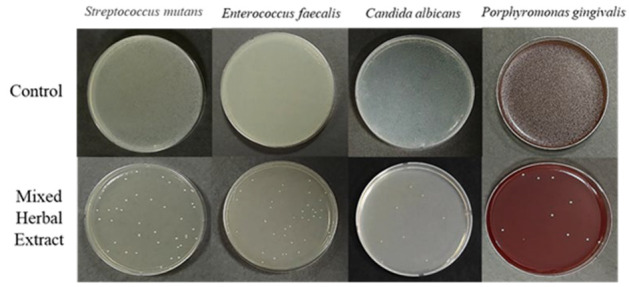
Colony-forming units (CFU) of oral pathogens following treatment with mixed herbal extracts (containing Schizonepeta tenuifolia, Mentha piperascens, Acanthopanax sessiliflorus, and Glycyrrhiza uralensis). Each white dot on the plates indicates an oral pathogen colony.
Table 3.
Growth inhibition of four microorganisms treated with mixed herbal extracts.
| Group | S. mutans a | E. faecalis b | C. albicans c | P. gingivalis d |
|---|---|---|---|---|
| Control | 5.90 ± 0.01 | 5.95 ± 0.01 | 5.85 ± 0.02 | 5.74 ± 0.01 |
| Mixed herbal extracts | 1.48 ± 0.03 ** | 1.49 ± 0.05 ** | 0.90 ± 0.03 ** | 0.95 ± 0.03 ** |
** p < 0.001; a Streptococcus mutans (S. mutans); b Enterococcus faecalis (E. faecalis); c Candida albicans (C. albicans); d Porphyromonas gingivalis (P. gingivalis).
3.2. Morphological Examination of Oral Pathogens
The cell surfaces of each bacterial test strain were examined using scanning electron microscopy after being treated with or without the mixed herbal extracts (Figure 2). All strains cultured with the mixed herbal extracts exhibited visible damage, with altered cellular morphologies due to the destruction of cell walls and membranes. Non-treated strains displayed normal cellular morphologies.
Figure 2.
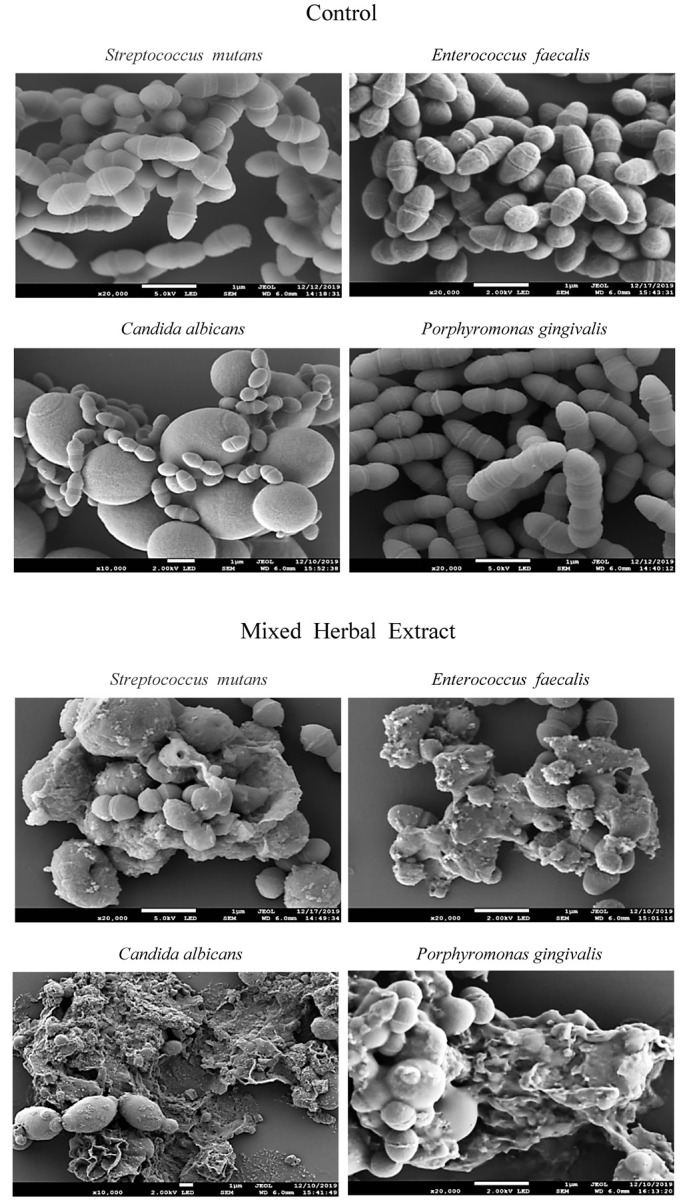
Scanning electron microscope images of studied microorganisms.
3.3. Bacterial Surface Hydrophobicity
The surface hydrophobicities of each test strain are shown in Table 4. When compared to the control, bacteria treated with the mixed herbal extracts exhibited significantly decreased hydrophobicity with increasing treatment time (p < 0.05). Similar results were observed for E. faecalis, C. albicans, and P. gingivalis. The relative hydrophobicity of S. mutans (assuming 100 in the untreated group) decreased to 61.20 ± 3.20**, 60.37 ± 0.73*, 59.23 ± 1.73*, and 57.35 ± 1.47%* after being treated with the mixed herbal extract for 1, 3, 5, and 10 min, respectively. The relative hydrophobicity of E. faecalis decreased to 85.63 ± 3.70*, 83.10 ± 1.46*, 74.34 ± 2.67*, and 72.06 ± 1.10%*, respectively. The relative hydrophobicity of C. albicans decreased to 80.89 ± 1.17*, 38.75 ± 2.89*, 27.91 ± 6.52*, and 19.91 ± 2.73%*, respectively. The relative hydrophobicity of P. gingivalis decreased to 44.11 ± 2.10*, 30.78 ± 2.13*, 26.96 ± 1.39**, and 22.14 ± 1.50%*, respectively.
Table 4.
Effects of mixed herbal extracts on the hydrophobic properties of the studied microorganisms.
| Group | S. mutans a | E. faecalis b | C. albicans c | P. gingivalis d |
|---|---|---|---|---|
| Control | 100 | 100 | 100 | 100 |
| 1 min e | 61.20 ± 3.20 ** | 85.63 ± 3.70 * | 80.89 ±1.17 * | 44.11 ± 2.10 * |
| 3 min e | 60.37 ± 0.73 * | 83.10 ± 1.46 * | 38.75 ± 2.89 * | 30.78 ± 2.13 * |
| 5 min e | 59.23 ± 1.73 * | 74.34 ± 2.67 * | 27.91 ± 6.52 * | 26.96 ± 1.39 ** |
| 10 min e | 57.35 ± 1.47 * | 72.06 ± 1.10 * | 19.91 ± 2.73 ** | 22.14 ± 1.50 ** |
* p < 0.05, ** p < 0.001; a Streptococcus mutans (S. mutans); b Enterococcus faecalis (E. faecalis); c Candida albicans (C. albicans); d Porphyromonas gingivalis (P. gingivalis); e minute (min).
After 10 min of treatment with the mixed herbal extracts, the surface hydrophobicity decreased by 42.65% in S. mutans, 27.94% in E. faecalis, 80.08% in C. albicans, and 77.86% in P. gingivalis.
3.4. Measurement of VSCs
The effects of the mixed herbal extracts on oral malodor were determined by measuring the generated VSCs, which are the main components of oral malodor (Table 5). Treatment with the mixed herbal extracts led to significant decreases in the relative production of VSCs; VSC production decreased by 91.25% in S. mutans, 97.03% in E. faecalis, 88.99% in C. albicans, and 100% in P. gingivalis when compared with the control group (p < 0.001).
Table 5.
Effects of mixed herbal extracts on the production of volatile sulfur compounds.
| Group | S. mutans a | E. faecalis b | C. albicans c | P. gingivalis d |
|---|---|---|---|---|
| Control | 1244.33 ± 22.24 | 109.00 ± 20.60 ** | 644.00 ± 28.00 | 47.00 ± 13.01 |
| Mixed herbal extracts | 109.00 ± 20.60 ** | 38.33 ± 10.80 ** | 71.00 ± 12.53 ** | 0.00 ± 0.00 ** |
** p < 0.001; a Streptococcus mutans (S. mutans); b Enterococcus faecalis (E. faecalis); c Candida albicans (C. albicans); d Porphyromonas gingivalis (P. gingivalis).
4. Discussion
Various microbial species inhabit the oral cavity, and the growth of pathogenic bacteria can cause oral diseases. Frequent consumption of refined carbohydrates accelerates the demineralization of tooth enamel due to dental caries, causing imbalances in remineralization and demineralization [33].
S. mutans refers to a group of seven closely related species that are collectively known as mutans Streptococci. S. mutans are commonly found in the mouth, pharynx, and intestines. The etiology of dental caries is heavily influenced by S. mutans and Streptococcus sobrinus [34]. Oral diseases such as caries, endodontic infections, periodontitis, and peri-implantitis have also been linked to E. faecalis, the predominant human Enterococcus. E. faecalis has been observed to comprise 3.7–35% of the oral microbiota in periodontitis patients [35]. Candida albicans is a commensal fungal species that commonly colonizes human mucosal surfaces. C. albicans has been observed in carious dentin/dentine tubules [36]. P. gingivalis is the major causative agent of periodontitis, a chronic inflammatory disease that causes tooth loss and degeneration of the gingiva, alveolar bones, and periodontal ligaments [37].
Oral diseases such as dental caries, periodontal disease, periapical lesions, and oral candidiasis are the main causes of tooth loss and oral malodor, for which effective management methods are urgently needed. Mouthwashes containing chemical agents are commonly used to eliminate bacteria and/or inhibit microbial activity. In a previous study, the use of mouthwash containing antimicrobial and anticaries agents decreased dental plaque formation by approximately 61% [38]. In other studies, mouthwashes containing eucalyptol and thymol or cetylpyridinium chloride were able to inhibit dental plaque formation and gingivitis, and both exhibited excellent antimicrobial activity against oral pathogens [39,40]. However, long-term use of mouthwash can also cause discoloration of the teeth and/or soft tissues and affect taste sensation [41]. In addition, the chemical agents in mouthwash can affect the normal microbial flora along with pathogens in the oral cavity. Furthermore, ethanol-containing mouthwashes may increase the risk of oral cancer and thus should only be used for limited periods [42]. Recent studies have focused on identifying natural substances as alternatives for synthetic chemical agents to selectively eliminate pathogenic bacteria.
In this study, the effects of a natural herbal extract mixture (containing STB, MP, AS, and GU) on oral bacteria were determined to help develop a natural-substance-based mouthwash. All herbal extracts used in the experiment are edible; thus, the proposed product can be gargled or can be safely consumed. In particular, STB [43] and GU [44] have been reported to inhibit the growth of Helicobacter pylori, a major cause of gastric cancer and gastritis. The herbs used in our proposed mixture exhibit anti-inflammatory and antimicrobial effects; however, excessive doses of GU can elicit negative effects such as severe hypertension, hypokalemia, and hypermetabolism. Hence, GU must be used with caution [45]. Approximately 20% of GU is comprised of glycyrrhizin [46], which possesses mineralocorticoid activity to degrade nicotine and alcohol, thereby acting as a detoxifying agent [45]. The recommended daily dose of GU for adults is 0.7 g, although a dose of ≥0.1 g/mL can have negative effects in patients with neurological disease [47]. Accordingly, when preparing the mixed herbal extracts, only a small amount of the raw GU material was added to minimize the risks of side effects.
Our experimental results showed that S. mutans, which causes dental caries, and E. faecalis, which is a causative agent of dental pulp disease, were reduced by ≥3 log CFU/mL under treatment with the mixed herbal extracts. Additionally, the numbers of C. albicans, a fungal strain that infects the oral mucosa, and P. gingivalis, which causes periodontal disease, were reduced by ≥4 log CFU/mL; thus, our proposed mixture has significant efficacy in inhibiting oral pathogens. Based on these findings, the null hypothesis was rejected. These results indicate that the mixed herbal extracts had stronger effects on Gram-positive fungi and Gram-negative bacteria than on Gram-positive bacteria. This disagrees with the findings of a previous study (Koohsari et al.), which found that the extract was more effective against Gram-positive bacteria than Gram-negative bacteria [48].
Morphological examination of each microbial strain showed that the oral microorganisms exhibited disorganized damage after treatment with the mixed herbal extracts. Particularly, C. albicans showed an overall damaged morphology. Similarly, Sangetha et al. [49] treated C. albicans with Cassia spectabilis leaf extract for 24 h and found that the extract damaged the microbial surface. We obtained identical results after 24 h of treatment with the mixed herbal extracts, which further validates that this herbal extract mixture possesses antimicrobial activity and can induce morphological damage in oral pathogens.
The hydrophobicity of cells is closely associated with microbial adhesion, and microbial strains with a high level of hydrophobicity can form biofilms. Many studies have reported that chlorohexidine, which is widely used as a component of mouthwashes, induces microbial adhesion. However, in one study, treatment of S. mutans with a high concentration of chlorohexidine decreased microbial adhesion, whereas in another study, biofilm formation was increased [50,51]. We found that treatment with the mixed herbal extracts reduced microbial adhesion, indicating that these extracts reduced the surface hydrophobicity of oral pathogens. Further studies are needed to investigate the mechanisms underlying the effects of these mixed herbal extracts on microbial cell hydrophobicity.
Oral malodor, also known as halitosis, is a disease that can significantly impact quality of life. It can be caused by oral, physiological, and/or pathological factors, with oral factors considered to be the main cause [52]. The main compounds contributing to bacteria-induced oral malodor are VSCs such as hydrogen sulfide, methyl mercaptan, and dimethyl sulfide. Indeed, VSC levels increase in patients with oral diseases such as dental caries [53]. Several studies have reported that reducing the levels of anaerobic oral bacteria resulted in decreases in VSC levels [54,55]. We demonstrated that the mixed herbal extracts reduced oral malodor by suppressing VSC formation. Treatment with the mixed herbal extracts inhibited the growth of P. gingivalis (the causal bacteria of periodontal disease) by 100%, indicating that the extracts have the potential to reduce oral malodor. We verified the antimicrobial effects of the mixed herbal extracts on oral disease-causing strains.
Based on these results and the mitigation of oral malodor, edible mixed herbal extracts may represent an effective antimicrobial agent against oral disease pathogens with minimal side effects since they are naturally derived. Thus, edible mixed herbal extracts are expected to have a strong antibacterial effect that can replace the activities of CHX and OCT in existing mouthwash and have a high potential for practical use.
However, as mixed extracts were used, the specific component(s) responsible for the observed antimicrobial effects remains unclear. Thus, further studies are needed to isolate and examine the individual effects of the edible mixed herbal extracts’ components. Therefore, it is necessary to conduct further research to confirm the antibacterial effects of each component of the extract against oral bacteria. Finally, our findings on the efficacy of edible mixed herbal extracts will provide guidance for clinical decision making in the future, as these compounds are tested via clinical trials.
5. Conclusions
We examined the antimicrobial effects of mixed herbal extracts on oral pathogens and found that the abundances of the four evaluated strains of oral pathogens were reduced after treatment. Additionally, treatment with the mixed herbal extracts altered the morphologies of S. mutans, E. faecalis, C. albicans, and P. gingivalis cells based on scanning electron microscopy observations. All the studied oral pathogen strains also showed decreased hydrophobicity after treatment, and C. albicans exhibited the greatest decrease. Treatment with the mixed herbal extracts also reduced malodor caused by these pathogens. In particular, the levels of P. gingivalis-related VSCs were reduced by 100%. Based on our results, it can be concluded that the proposed natural mixed herbal extracts (containing STB, MP, AS, and GU) may demonstrate efficacies in inhibiting and/or limiting bacterial and fungal growth and preventing halitosis. However, further toxicity tests using human oral cavity cells are needed to confirm their safety.
Author Contributions
Conceptualization, S.-E.Y. and B.-B.r.C.; methodology, S.-E.Y. and S.-H.N.; formal analysis, S.-E.Y. and S.-H.N.; writing—original draft preparation, S.-E.Y. and B.-B.r.C.; writing—review and editing, B.-B.r.C. and G.-C.K.; visualization, S.-E.Y. and B.-B.r.C.; supervision, G.-C.K. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available upon request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (No. 2021R1A2C2008215).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Bumm C.V., Folwaczny M., Stokes L.N., Olsen I., Dewhirst F.E. Infective endocarditis and oral health—A Narrative Review. Cardivasc. Diagn. Ther. 2021;11:1403–1415. doi: 10.21037/cdt-20-908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Toz Ertop M., Cicek O., Erener H., Ozkalayci N., Demir Cicek B., Comert F. Evaluation of the Demineralization Development around Different Types of Orthodontic Brackets. Materials. 2023;16:984. doi: 10.3390/ma16030984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang R., Li M., Gregory R.L. Bacterial interactions in dental biofilm. Virulence. 2011;2:435–444. doi: 10.4161/viru.2.5.16140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen X., Daliri E.B., Tyagi A., Oh D.H. Cariogenic Biofilm: Pathology-Related Phenotypes and Targeted Therapy. Microorganisms. 2021;9:1311. doi: 10.3390/microorganisms9061311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rajendra Santosh A.B., Muddana K., Bakki S.R. Fungal Infections of Oral Cavity: Diagnosis, Management, and Association with COVID-19. SN Compr. Clin. Med. 2021;3:1373–1384. doi: 10.1007/s42399-021-00873-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bui F.Q., Almeida-da-Silva C.L.C., Huynh B., Trinh A., Liu J., Woodward J., Asadi H., Ojcius D.M. Association between periodontal pathogens and systemic disease. Biomed. J. 2019;42:27–35. doi: 10.1016/j.bj.2018.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grover V., Mahendra J., Gopalakrishnan D., Jain A. Effect of octenidine mouthwash on plaque, gingivitis, and oral microbial growth: A systematic review. Clin. Exp. Dent. Res. 2021;7:450–464. doi: 10.1002/cre2.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Katsura H., Tsukiyama R.I., Suzuki A., Kobayashi M. In vitro antimicrobial activities of bakuchiol against oral microorganism. Antimicrob. Agents Chemother. 2001;45:3009–3013. doi: 10.1128/AAC.45.11.3009-3013.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Inhartová L., Michalíková K., Šrédlová K., Cajthaml T. Biodegradability of Dental Care Antimicrobial Agents Chlorhexidine and Octenidine by Ligninolytic Fungi. Molecules. 2020;25:400. doi: 10.3390/molecules25020400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pytko-Polończyk J., Stawarz-Janeczek M., Kryczyk-Poprawa A., Muszyńska B. Antioxidant-Rich Natural Raw Materials in the Prevention and Treatment of Selected Oral Cavity and Periodontal Diseases. Antioxidants. 2021;10:1848. doi: 10.3390/antiox10111848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schönknecht K., Surdacka A., Rudenko L., Scherer W. Effectiveness of composed herbal extract in the treatment of gingivitis and oral and pharyngeal mucosa—Review of studies. Wiad. Lek. 2021;74:1737–1749. doi: 10.36740/WLek202107131. [DOI] [PubMed] [Google Scholar]
- 12.Kováč J., Slobodníková L., Trajčíková E., Rendeková K., Mučaji P., Sychrová A., Bittner Fialová S. Therapeutic Potential of Flavonoids and Tannins in Management of Oral Infectious Diseases–A Review. Molecules. 2022;28:158. doi: 10.3390/molecules28010158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lin Z., Gan T., Huang Y., Bao L., Liu S., Cui X., Wang H., Jiao F., Zhang M., Su C., et al. Anti-Inflammatory Activity of Mulberry Leaf Flavonoids In Vitro and In Vivo. Int. J. Mol. Sci. 2022;23:7694. doi: 10.3390/ijms23147694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vyas T., Nagi R., Bhatia A., Bains S.K. Therapeutic effects of green tea as an antioxidant on oral health—A review. J. Fam. Med. Prim. Care. 2021;10:3998–4001. doi: 10.4103/jfmpc.jfmpc_943_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Takasago K. Addition of cariogenic pathogens to complex oral microflora drives significant changes in biofilm compositions and functionalities. Microbiome. 2023;11:123. doi: 10.1186/s40168-023-01561-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen S.G., Cheng M.L., Chen K.H., Horng J.T., Liu C.C., Wang S.M., Sakurai H., Leu Y.L., Wang S.D., Ho H.Y. Antiviral activities of Schizonepeta tenuifolia Briq. against enterovirus 71 in vitro and in vivo. Sci. Rep. 2017;7:935. doi: 10.1038/s41598-017-01110-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nadeem A., Shahzad H., Ahmed B., Muntean T., Waseem M., Tabassum A. Phytochemical profiling of antimicrobial and potential antioxidant plant: Nepeta cataria. Front. Plant Sci. 2022;13:969316. doi: 10.3389/fpls.2022.969316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dolghi A., Coricovac D., Dinu S., Pinzaru I., Dehelean C.A., Grosu C., Chioran D., Merghes P.E., Sarau C.A. Essential Oils and In Vitro Potential Cytotoxic Effect in Human Colorectal Carcinoma Cells. Molecules. 2022;27:6106. doi: 10.3390/molecules27186106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sim L.Y., Abd Rani N.Z., Husain K. Lamiaceae: An Insight on Their Anti-Allergic Potential and Its Mechanisms of Action. Front. Pharmacol. 2019;10:677. doi: 10.3389/fphar.2019.00677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aebisher D., Cichonski J., Szpyrka E., Masjonis S., Chrzanowski G. Essential Oils of Seven Lamiaceae Plants and Their Antioxidant Capacity. Molecules. 2021;26:3793. doi: 10.3390/molecules26133793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Uritu C.M., Mihai C.T., Stanciu G.D., Dodi G., Alexa-Stratulat T., Luca A., Leon-Constantin M.M., Stefanescu R., Bild V., Melnic S., et al. Medicinal Plants of the Family Lamiaceae in Pain Therapy: A Review. Pain Res. Manag. 2018;2018:7801543. doi: 10.1155/2018/7801543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bae E.A., Yook C.S., Oh O.J., Chang S.Y., Nohara T., Kim D.H. Metabolism of chiisanoside from Acanthopanax divaricatus var. albeofructus by human intestinal bacteria and its relation to some biological activities. Biol. Pharm. Bull. 2001;24:582–585. doi: 10.1248/bpb.24.582. [DOI] [PubMed] [Google Scholar]
- 23.Bian X., Zhao Y., Guo X., Zhang L., Li P., Fu T., Wang W., Yin Y., Chen G., Liu J. Chiisanoside, a triterpenoid saponin, exhibits anti-tumor activity by promoting apoptosis and inhibiting angiogenesis. RSC Adv. 1996;19:41640–41650. doi: 10.1039/C7RA08041G. [DOI] [Google Scholar]
- 24.Bian X., Liu X., Liu J., Zhao Y., Li H., Zhang L., Li P., Gao Y. Hepatoprotective effect of chiisanoside from Acanthopanax sessiliflorus against LPS/D-GalN-induced acute liver injury by inhibiting NF-κB and activating Nrf2/HO-1 signaling pathways. J. Sci. Food Agric. 2019;99:3283–3290. doi: 10.1002/jsfa.9541. [DOI] [PubMed] [Google Scholar]
- 25.Hu C., Liu H., Du J., Mo B., Qi H., Wang X., Ye S., Li Z. Estrogenic activities of extracts of Chinese licorice (Glycyrrhiza uralensis) root in MCF-7 breast cancer cells. J. Steroid Biochem. Mol. Biol. 2009;113:209–216. doi: 10.1016/j.jsbmb.2008.12.019. [DOI] [PubMed] [Google Scholar]
- 26.Tanaka Y., Kikuzaki H., Fukuda S., Nakatani N. Antimicrobial compounds of licorice against upper airway respiratory tract pathogens. J. Nutr. Sci. Vitaminol. 2001;47:270–273. doi: 10.3177/jnsv.47.270. [DOI] [PubMed] [Google Scholar]
- 27.Choi B.B., Choi J.H., Park S.R., Kim J.Y., Hong J.W., Kim G.C. Scutellariae radix induces apoptosis in chemoresistant SCC-25 human tongue squamous carcinoma cells. Am. J. Chin. Med. 2015;43:167–181. doi: 10.1142/S0192415X15500111. [DOI] [PubMed] [Google Scholar]
- 28.Park N.S., Yun S.E., Lee H.Y., Lee H.J., Choi J.H., Kim G.C. No-ozone cold plasma can kill oral pathogenic microbes in H2O2-dependent and independent manner. Sci. Rep. 2022;12:7597. doi: 10.1038/s41598-022-11665-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Golding C.G., Lamboo L.L., Beniac D.R., Booth T.F. The scanning electron microscope in microbiology and diagnosis of infectious disease. Sci. Rep. 2016;23:26516. doi: 10.1038/srep26516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lather P., Mohanty A.K., Jha P., Garsa A.K. Contribution of Cell Surface Hydrophobicity in the Resistance of Staphylococcus aureus against Antimicrobial Agents. Biochem. Res. Int. 2016;2016:1091290. doi: 10.1155/2016/1091290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li F., Wang C., Xu J., Wang X., Cao M., Wang S., Zhang T., Xu Y., Wang J., Pan S., et al. Evaluation of the antibacterial activity of Elsholtzia ciliate essential oil against halitosis-related Fusobacterium nucleatum and Porphyromonas gingivalis. Front. Microbiol. 2023;14:1219004. doi: 10.3389/fmicb.2023.1219004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.IBM Corp . IBM SPSS Statistics for Windows, Version 24.0. IBM Corp.; Armonk, NY, USA: 2016. [Google Scholar]
- 33.Demircioglu R.M., Cicek O., Comert F., Erener H. Do Different Types of Adhesive Agents Effect Enamel Demineralization for Orthodontic Bonding? An In Vitro Study. Coatings. 2023;13:401. doi: 10.3390/coatings13020401. [DOI] [Google Scholar]
- 34.Forssten S.D., Björklund M., Ouwehand A.C. Streptococcus mutans, caries and simulation models. Nutrients. 2010;2:290–298. doi: 10.3390/nu2030290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Komiyama E.Y., Lepesqueur L.S., Yassuda C.G., Samaranayake L.P., Parahitiyawa N.B., Balducci I., Koga-Ito C.Y. Enterococcus Species in the Oral Cavity: Prevalence, Virulence Factors and Antimicrobial Susceptibility. PLoS ONE. 2016;11:e0163001. doi: 10.1371/journal.pone.0163001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Du Q., Ren B., He J., Peng X., Guo Q., Zheng L., Li J., Dai H., Chen V., Zhang L., et al. Candida albicans promotes tooth decay by inducing oral microbial dysbiosis. ISME J. 2021;15:894–908. doi: 10.1038/s41396-020-00823-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carrol D.H., Chassagne F., Dettweiler M., Quave C.L. Antibacterial activity of plant species used for oral health against Porphyromonas gingivalis. PLoS ONE. 2020;15:e0239316. doi: 10.1371/journal.pone.0239316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Baker P.J., Coburn R.A., Genco R.J., Evans R.T. The in vitro inhibition of microbial growth and plaque formation by surfactant drugs. J. Periodontal Res. 1978;13:474–485. doi: 10.1111/j.1600-0765.1978.tb00200.x. [DOI] [PubMed] [Google Scholar]
- 39.Vergara-Buenaventura A., Castro-Ruiz C. Use of mouthwashes against COVID-19 in dentistry. Br. J. Oral Maxillofac. Surg. 2020;58:924–927. doi: 10.1016/j.bjoms.2020.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Palombo E.A. Traditional Medicinal Plant Extracts and Natural Products with Activity against Oral Bacteria: Potential Application in the Prevention and Treatment of Oral Diseases. Evid. Based Complement. Altern. Med. 2011;2011:680354. doi: 10.1093/ecam/nep067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.James P., Worthington H.V., Parnell C., Harding M., Lamont T., Cheung A., Whelton H., Riley P. Chlorhexidine mouthrinse as an adjunctive treatment for gingival health. Cochrane Database Syst. Rev. 2017;3:CD008676. doi: 10.1002/14651858.CD008676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McCullough M.J., Farah C.S. The role of alcohol in oral carcinogenesis with particular reference to alcohol-containing mouthwashes. Aust. Dent. J. 2008;53:302–305. doi: 10.1111/j.1834-7819.2008.00070.x. [DOI] [PubMed] [Google Scholar]
- 43.Zhao X., Zhou M. Review on Chemical Constituents of Schizonepeta tenuifolia Briq. and Their Pharmacological Effects. Molecules. 2022;27:5249. doi: 10.3390/molecules27165249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fukai T., Marumo A., Kaitou K., Kanda T., Terada S., Nomura T. Anti-Helicobacter pylori flavonoids from licorice extract. Life Sci. 2002;2002:1449–1463. doi: 10.1016/S0024-3205(02)01864-7. [DOI] [PubMed] [Google Scholar]
- 45.Asl M.N., Hosseinzadeh H. Review of pharmacological effects of Glycyrrhiza sp. and its bioactive compounds. Phytother. Res. 2008;22:709–724. doi: 10.1002/ptr.2362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wen D., Liu Y., Li W., Liu H. Separation methods for antimicrobial and antirheumatism agents in plant medicines. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 2004;812:101–117. doi: 10.1016/S1570-0232(04)00550-1. [DOI] [PubMed] [Google Scholar]
- 47.Størmer F.C., Reistad R., Alexander J. Glycyrrhizic acid in liquorice—Evaluation of health hazard. Food Chem. Toxicol. 1993;31:303–312. doi: 10.1016/0278-6915(93)90080-I. [DOI] [PubMed] [Google Scholar]
- 48.Koohsari H., Ghaemi E.A., Sadegh Sheshpoli M., Jahedi M., Zahiri M. The investigation of antibacterial activity of selected native plants from North of Iran. J. Med. Life. 2015;8:38–42. [PMC free article] [PubMed] [Google Scholar]
- 49.Sangetha S., Zuraini Z., Sasidharan S., Suryani S. Fungicidal effect and oral acute toxicity of Cassia spectabilis leaf extract. Nihon Ishinkin Gakkai Zasshi. 2008;49:299–304. doi: 10.3314/jjmm.49.299. [DOI] [PubMed] [Google Scholar]
- 50.Meurman J.H. Ultrastructure, growth, and adherence of Streptococcus mutans after treatment with chlorhexidine and fluoride. Caries Res. 1988;22:283–287. doi: 10.1159/000261122. [DOI] [PubMed] [Google Scholar]
- 51.Dong L., Tong Z., Linghu D., Lin Y., Tao R., Liu J., Tian Y., Ni L. Effects of sub-minimum inhibitory concentrations of antimicrobial agents on Streptococcus mutans biofilm formation. Int. J. Antimicrob. Agents. 2012;39:390–395. doi: 10.1016/j.ijantimicag.2012.01.009. [DOI] [PubMed] [Google Scholar]
- 52.Izidoro C., Botelho J., Machado V., Reis A.M., Proença L., Alves R.C., Mendes J.J. Revisiting Standard and Novel Therapeutic Approaches in Halitosis: A Review. Int. J. Environ. Res. Public Health. 2022;19:11303. doi: 10.3390/ijerph191811303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Morita M., Wang H.L. Relationship of sulcular sulfide level and oral malodor in subjects with periodontal disease. J. Periodontol. 2001;72:79–84. doi: 10.1902/jop.2001.72.1.79. [DOI] [PubMed] [Google Scholar]
- 54.Yoo H.J., Jwa S.K., Kim D.H., Ji Y.J. Inhibitory effect of Streptococcus salivarius K12 and M18 on halitosis in vitro. Clin. Exp. Dent. Res. 2020;6:207–214. doi: 10.1002/cre2.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Suzuki N., Yoneda M., Takeshita T., Hirofuji T., Hanioka T. Induction and inhibition of oral malodor. Mol. Oral Microbiol. 2019;34:85–96. doi: 10.1111/omi.12259. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available upon request from the corresponding author.


