Abstract
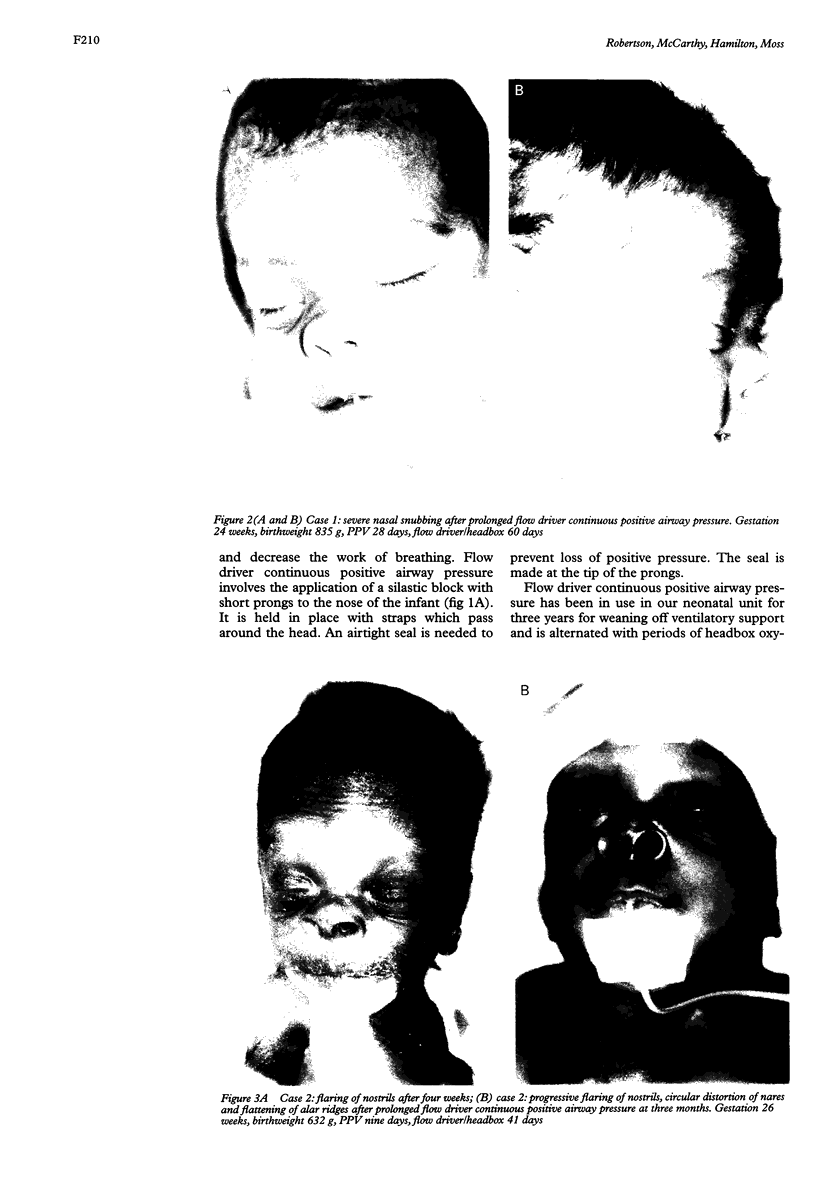
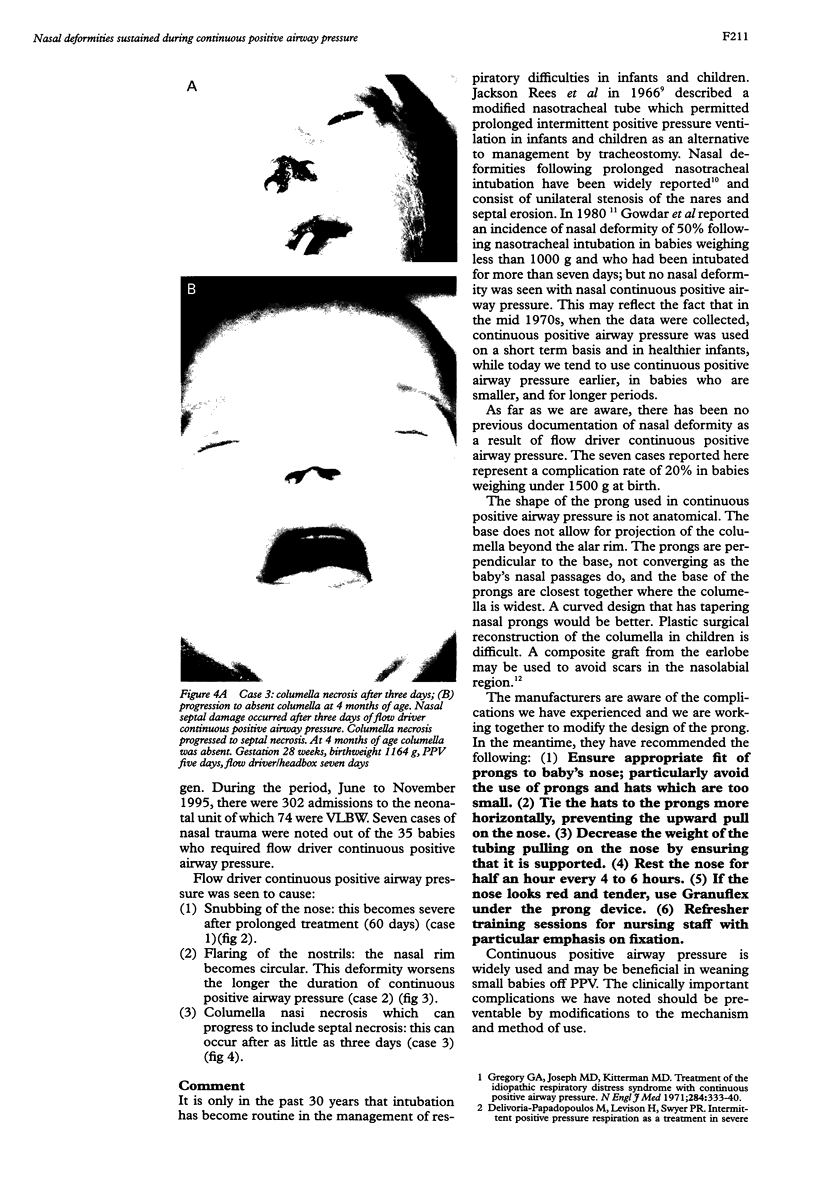
Over a period of six months, seven cases were documented of trauma to the nose as a result of flow driver continuous positive airway pressure in babies of very low birthweight (VLBW). There was a complication rate of 20% in the babies who required it. Deformities consisted of columella nasi necrosis which can occur within three days, flaring of nostrils which worsens with duration of continuous positive airway pressure, and snubbing of the nose which persists after prolonged continuous positive airway pressure. These complications should be preventable by modifications to the mechanism and method of use.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Avery M. E., Tooley W. H., Keller J. B., Hurd S. S., Bryan M. H., Cotton R. B., Epstein M. F., Fitzhardinge P. M., Hansen C. B., Hansen T. N. Is chronic lung disease in low birth weight infants preventable? A survey of eight centers. Pediatrics. 1987 Jan;79(1):26–30. [PubMed] [Google Scholar]
- Baxter R. J., Johnson J. D., Goetzman B. W., Hackel A. Cosmetic nasal deformities complicating prolonged nasotracheal intubation in critically ill newborn infants. Pediatrics. 1975 Jun;55(6):884–887. [PubMed] [Google Scholar]
- Chan V., Greenough A. Randomised trial of methods of extubation in acute and chronic respiratory distress. Arch Dis Child. 1993 May;68(5 Spec No):570–572. doi: 10.1136/adc.68.5_spec_no.570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delivoria-Papadopoulos M., Levison H., Swyer P. R. Intermittent positive pressure respiration as a treatment in severe respiratory distress syndrome. Arch Dis Child. 1965 Oct;40(213):474–479. doi: 10.1136/adc.40.213.474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin S. R., Graves S. A., Haberkern C. M. Aspiration in intubated premature infants. Pediatrics. 1985 Jan;75(1):85–88. [PubMed] [Google Scholar]
- Gowdar K., Bull M. J., Schreiner R. L., Lemons J. A., Gresham E. L. Nasal deformities in neonates. Their occurrence in those treated with nasal continuous positive airway pressure and nasal endotracheal tubes. Am J Dis Child. 1980 Oct;134(10):954–957. [PubMed] [Google Scholar]
- Higgins R. D., Richter S. E., Davis J. M. Nasal continuous positive airway pressure facilitates extubation of very low birth weight neonates. Pediatrics. 1991 Nov;88(5):999–1003. [PubMed] [Google Scholar]
- Rees G. J., Owen-Thomas J. B. A technique of pulmonary ventilation with a nasotracheal tube. Br J Anaesth. 1966 Nov;38(11):901–906. doi: 10.1093/bja/38.11.901. [DOI] [PubMed] [Google Scholar]
- So B. H., Tamura M., Mishina J., Watanabe T., Kamoshita S. Application of nasal continuous positive airway pressure to early extubation in very low birthweight infants. Arch Dis Child Fetal Neonatal Ed. 1995 May;72(3):F191–F193. doi: 10.1136/fn.72.3.f191. [DOI] [PMC free article] [PubMed] [Google Scholar]