Abstract
Pulmonary function tests (FVC, FEV1, FEV1/FVC%, TLCO, single breath CO diffusion), chest x ray film, renal function (serum creatinine and blood urea nitrogen), liver function (serum alanine aminotransferase, aspartate transferase, and alkaline phosphatase, bilirubin, total protein, and albumin), a haematological screen (haemoglobin and packed cell volume), and a general clinical examination were performed on 85 paraquat spraymen (mean spraying time 12 years) and on two control groups (76 factory workers and 79 general workers) frequency matched for age and years of occupational service. All the subjects were men. There were no clinically important differences in any of the measurements made between the study group and the two control groups. In particular the results of the lung function tests, appropriate for paraquat toxicity of the study group, were similar to those of the control groups. The same was true of blood tests for liver and kidney function. The incidence of skin damage, nose bleeds, and nail damage in the study group was slightly higher than in the control groups but lower than the incidence reported for paraquat workers in previous studies. The results of this study confirmed that long term spraying of paraquat, at the concentrations used, produced no adverse health effects, in particular no lung damage, attributable to the occupational use of the herbicide.
Full text
PDF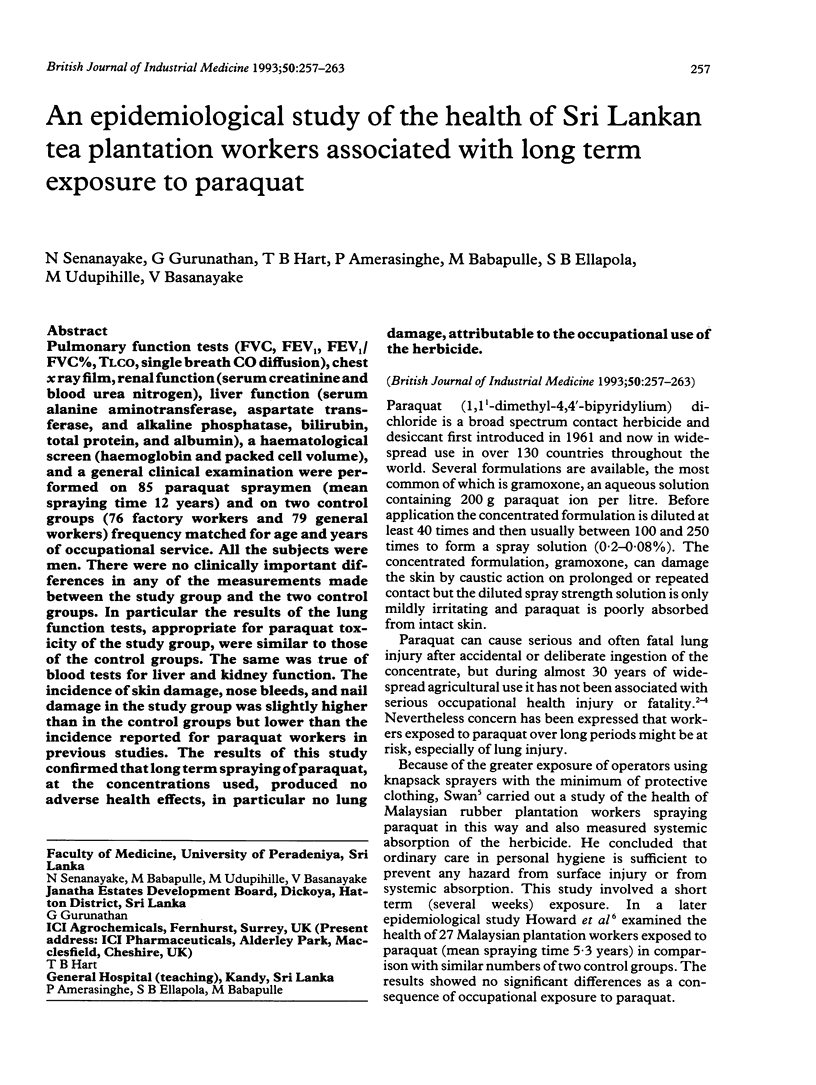

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Hart T. B. Paraquat--a review of safety in agricultural and horticultural use. Hum Toxicol. 1987 Jan;6(1):13–18. doi: 10.1177/096032718700600103. [DOI] [PubMed] [Google Scholar]
- Hearn C. E., Keir W. Nail damage in spray operators exposed to paraquat. Br J Ind Med. 1971 Oct;28(4):399–403. doi: 10.1136/oem.28.4.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard J. K. Paraquat: a review of worker exposure in normal usage. J Soc Occup Med. 1980 Jan;30(1):6–11. doi: 10.1093/occmed/30.1.6. [DOI] [PubMed] [Google Scholar]
- Howard J. K., Sabapathy N. N., Whitehead P. A. A study of the health of Malaysian plantation workers with particular reference to paraquat spraymen. Br J Ind Med. 1981 May;38(2):110–116. doi: 10.1136/oem.38.2.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewin R. Parkinson's disease: an environmental cause? Science. 1985 Jul 19;229(4710):257–258. doi: 10.1126/science.3925554. [DOI] [PubMed] [Google Scholar]
- Rose M. S., Lock E. A., Smith L. L., Wyatt I. Paraquat accumulation: tissue and species specificity. Biochem Pharmacol. 1976 Feb 15;25(4):419–423. doi: 10.1016/0006-2952(76)90344-0. [DOI] [PubMed] [Google Scholar]
- Rose M. S., Smith L. L., Wyatt I. Evidence for energy-dependent accumulation of paraquat into rat lung. Nature. 1974 Nov 22;252(5481):314–315. doi: 10.1038/252314b0. [DOI] [PubMed] [Google Scholar]
- Smith L. L., Wright A., Wyatt I., Rose M. S. Effective treatment for paraquat poisoning in rats and its relevance to treatment of paraquat poisoning in man. Br Med J. 1974 Dec 7;4(5944):569–571. doi: 10.1136/bmj.4.5944.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swan A. A. Exposure of spray operators to paraquat. Br J Ind Med. 1969 Oct;26(4):322–329. doi: 10.1136/oem.26.4.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vale J. A., Meredith T. J., Buckley B. M. Paraquat poisoning: clinical features and immediate general management. Hum Toxicol. 1987 Jan;6(1):41–47. doi: 10.1177/096032718700600107. [DOI] [PubMed] [Google Scholar]
- Wester R. C., Maibach H. I., Bucks D. A., Aufrere M. B. In vivo percutaneous absorption of paraquat from hand, leg, and forearm of humans. J Toxicol Environ Health. 1984;14(5-6):759–762. doi: 10.1080/15287398409530624. [DOI] [PubMed] [Google Scholar]


