Abstract
Background:
Social engagement technologies offer an opportunity to reduce social isolation. However, there are barriers to adoption among older adults with and without Mild Cognitive Impairment (MCI). Technology designed to meet the needs of those users may improve the acceptability, adoption, and benefits of social engagement technology.
Objective:
The goal was to assess older adults’ needs and preferences for using video chat systems. We used the Technology Acceptance Model as a framework for evaluating and optimizing usability of a web-based video chat system for older adults with and without MCI.
Methods:
Mixed methods (qualitative and quantitative) were used to achieve this objective. We developed questionnaires and interviews to identify experiences with video chat, and preferences and attitudes towards a web-based video chat system. We conducted heuristic analysis to evaluate and improve the usability of the system.
Results:
Participants reportedly used video chat less than other social network tools (e.g., Email). They were open to using a web-based video chat system to meet new people of all ages with shared interests. Their favorite topics of conversation were books, health, family, and exercise. Their ideal group size for a video chat session was 3 to 6 people. Overall, participants’ attitudes toward the system were positive and they perceived the system as easy to use and useful for social engagement. Their evaluations indicated high usability of the system. However, individuals with MCI might require additional assistance to use the system. Usability issues were identified, such as technical terminology, small font size, and potentially confusing icons that were addressed in the redesign.
Conclusion:
Older adults, with and without MCI, were interested in using a social engagement technology to interact with previously unfamiliar individuals with shared interests. They provided valuable insights for the design of the systems. Our findings provide guidance for the design of social engagement technologies. Our research approach serves as a case study for the assessment of other technology platforms.
Keywords: Social engagement technology, aging, mild cognitive impairment, perceived ease of use, perceived usefulness
Introduction
Social isolation is defined as a lack of social contact and can lead to feelings of loneliness (Hawkley & Capitanio, 2015; Zebhauser et al., 2014). People who live alone, without a partner, or have low quantity and quality of social relationships are at high risk of social isolation and loneliness (Hawkley, & Capitanio, 2015; Luhmann, & Hawkley, 2016). In the United States, 12 million older adults age 65 and older live alone and 19.5 million older adults are unmarried (Stepler, 2016; Vespa et al., 2013). Additionally, older adults are at increased risk of social isolation and loneliness due to significant life changes, including retirement, restricted mobility, sensory loss, and development of chronic health conditions (Child & Lawton, 2019; Tseng, et al., 2018).
The risk of social isolation is higher for 11.6% of older adults in the United States who have a diagnosis of Mild Cognitive Impairment (MCI; Petersen et al., 2014). Older adults with MCI experience cognitive decline beyond what is expected for their age and education level but are relatively high functioning. Given that intact cognitive function is essential to successfully maintain interpersonal social relationships, older adults with MCI often experience barriers to participating in social activities, and thus are at greater risk of social isolation (Garms-Homolova et al., 2017; Kotwal, Kim, Waite, & Dale, 2016). Social isolation and loneliness have a strong negative effect on health and well-being of older adults (Holt-Lunstad, Smith, Baker, Harris, & Stephenson, 2015; Klinenberg, 2016), including physical (e.g., high blood pressure, sleep disruptions), mental (e.g., depression, suicidality, low resilience, low life satisfaction), and cognitive health outcomes (Coyle & Dugan, 2012; Friedler, Crapser, & McCullough, 2015; Cacioppo & Cacioppo, 2014; Zebhauser et al., 2014).
The detrimental effects of social isolation can be reduced by promoting social engagement (Poscia, et al., 2018), which refers to the degree of participation in interpersonal activities and the maintenance of meaningful connections with other people (Bixter, Blocker, & Rogers, 2018). A growing body of literature has described the positive effects of social engagement on physical and mental health and quality of life in older adults (Huxhold, Fiori, & Windsor, 2013; Nyqvist, Forsman, Giuntoli, & Cattan, 2013; Yang et al., 2016). Higher levels of social engagement have been associated with higher cognitive functioning (Bourassa, Memel, Woolverton, & Sbarra, 2017; Haslam, Cruwys, Milne, Kan, & Haslam, 2016). Studies have shown positive relationships between social activities and executive function, speed of information processing, episodic memory, and semantic memory (de Frias & Dixon, 2014; Small, Dixon, McArdle, & Grimm, 2012). Moreover, social engagement interventions that target keeping individuals socially active and cognitively engaged have improved cognitive function. Mortimer et al. (2012) found that after 40 weeks of regular group meetings to discuss selected topics of interest, non-demented older people showed improvements in auditory verbal learning and speed of processing. Such research provides evidence for the benefits of social engagement interventions.
Social programs such as senior centers and congregate meals have been implemented (Morrow-Howell & Gehlert, 2012) to provide opportunities for social support and decrease the negative effects of social isolation among older adults (Christakis, 2004). These social engagement programs involve face-to-face interactions. Such programs require that people are co-located in space and time, which poses a major accessibility barrier. Social engagement technologies provide opportunities for social interaction without the requirement of being in the same location or time zone. Online platforms such as email and Facebook allow older adults to keep in contact with friends and family members in different geographic areas. Televideo applications (e.g., Skype, FaceTime) and devices allow users to see and hear others without having to leave their homes. The benefits of social engagement technology on social connectedness and health and cognitive function among older populations has been demonstrated in numerous studies (Chopik, 2016; Czaja, Boot, Charness, Rogers, & Sharit, 2018; Ihm, & Hsieh, 2015; Myhre et al., 2017). Higher social technology use has been associated with better self-rated health, fewer chronic illnesses, higher subjective well-being, and fewer depressive symptoms among older adults (Chopik, 2016). Information and communication technology system such as the Personal Reminder Information and Social Management (PRISM) system was found to be beneficial for social connectivity and loneliness reduction among older adults (Czaja, Boot, Charness, Rogers, & Sharit, 2018). Myhre et al. (2017) found that learning and using an online social networking site may provide specific benefits for complex working memory in a group of healthy older adults. However, most of the research has been conducted among cognitively normal older adults, so data are limited for individuals with MCI.
Despite the distinct benefits of social engagement technologies, older adults have lower access and usage of technology than younger adults (Gombault, 2013; Pew research center, 2015). Among older adults 65 years and older, only 35% of them report using social media (e.g., Facebook, Twitter, Instagram), compared with 90% of younger people (Pew research center, 2015). To understand this digital divide, it is important to consider factors that influence the adoption of technology among older adults. The Technology Acceptance Model (TAM; Davis, 1989) informs understanding of the adoption of technology through two core constructs: perceived usefulness and perceived ease of use. Perceived usefulness refers to the degree an individual believes using technology will enhance their performance. Perceived ease of use refers to the degree an individual believes using technology will be relatively free of effort. Both factors influence users’ preferences and intentions to use communication technologies. For example, Macedo (2017) demonstrated the importance of both performance expectancy (perceived usefulness) and effort expectancy (perceived ease of use) on the acceptance and use of information and communication technology by older adults.
In addition to usefulness and ease of use, other factors such as computer experience, computer self-efficacy, and interest related to technology acceptance. Mitzner et al. (2016) found that technology experience and attitudes (e.g., computer self-efficacy, interest) had significant positive correlations with both perceived usefulness and ease of use among older adults. More specifically, individuals with more technical experience and higher computer self-efficacy and interest were more likely to rate computers as useful and easy to use. Understanding users’ experiences, functional ability to use technology and preferences of social engagement technology is necessary to improve technologies to better suit the needs of older adults and increase social engagement technology acceptance.
Despite the importance of understanding user needs, few studies have investigated these needs in the context of social engagement technologies or evaluated the usability of available products to guide technology design. To the best of our knowledge, there is only one previous study that has used qualitative methods to get insight into the user interface and user experience of social engagement technologies. Bixter et al. (2019) used semi-structured group interviews to identify problems of adoption of social communication technologies (e.g., Facebook, Instagram), such as computer experiences, performance expectancy, and effort expectancy. This study provided insights into facilitators and barriers to adoption of technologies. However, while it investigated older adults’ perspectives on these technologies, it did not identify usability issues that, if removed, would improve the systems’ design. Additionally, Bixter et al. (2019) only included cognitively healthy older adults; individuals with MCI might have different attitudes or usability challenges that must be assessed for broader uptake of social engagement technologies.
OneClick.chat video chat system
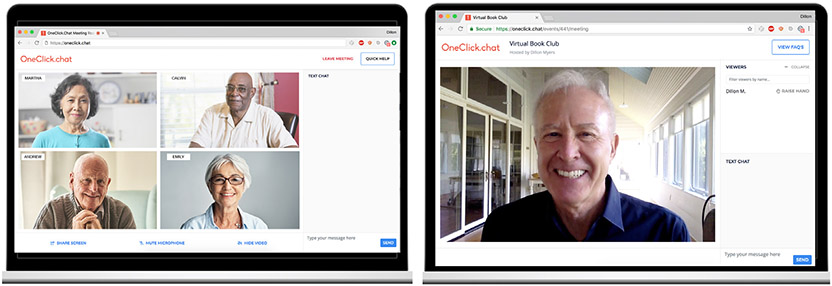
In this study, we used OneClick.chat’s video chat system to investigate older adults’ needs and preferences for using video chat and evaluate the usability of this specific system. OneClick. chat (referred to as ‘OneClick’ henceforth) is a web-based video chat system created by Potluck, LLC (Philadelphia, PA). OneClick is an Internet browser-based system and thus does not require an application download. Instead, users only need a computer, webcam, and Internet connection to participate in either OneClick video-based meetings or OneClick video-based events. Users can join other people in a group video conversation or an event by clicking a link that is typically provided via email. In a One Click video-based meeting room, people can interact with a small group (up to nine) of individuals by both video chat and text chat. In a OneClick video-based event, a host initiates the event, during which the audience can see and hear the host, but the host cannot see or hear the audience. The host can then send the audience to small breakout groups for discussion, which act similarly to the video-based meetings. Once the group discussion is completed, the host can bring the audience back to the event (Figure 1).
Figure 1.
Screenshots of OneClick video meeting room (left) and video event (right)
Overview of this study
The main objectives of this research were to (1) investigate experiences, attitudes, and preferences of video chat systems, particularly the OneClick video chat platform, among older adults with and without MCI; and (2) evaluate and optimize the OneClick system to accommodate the interests, abilities, and usability concerns. These objectives were accomplished in three phases Phase 1 (Demonstration Study) examined older adults’ experiences with well-known video chat systems (e.g. Skype, Facetime), their attitudes toward video chat in general, and to OneClick specifically, and their preferences on how they would like to use OneClick. In Phase 2 (Heuristic Evaluation), potential usability problems with the OneClick system were identified through heuristic evaluations conducted by experts with knowledge of human factors, aging, and MCI. The OneClick platform was then optimized based on Phase 1 and Phase 2 findings. In Phase 3 (Interaction Study), participants interacted with the optimized OneClick system and gave feedback on their attitudes toward the improved system and their opinions about using the system for real conversations. Importantly, these three studies provide insights not only for the design of OneClick, but more generally for the design of technology-based social engagement platforms for older adults with and without MCI.
Phase 1: Demonstration study
Participants completed questionnaires and structured interviews that investigated their experiences using video chat systems in general (e.g. Skype, Facetime), including frequency of use; the people they spoke with; the topics and activities they discussed; and their perceptions of ease-of-use and usefulness of these video chat systems. Participants then watched a demonstration video of the OneClick video chat system and had an opportunity to ask questions about the system. They were interviewed about their perceived ease of use (facilitators and barriers) and the usefulness of OneClick. Their preferences on how they would like to use OneClick, including who they would like to talk to, the topics they would like to discuss, and the group size for discussion were identified from their interview responses.
Method
Participants
Cognitively normal older adults (n=10) and older adults with MCI (n=5) provided written informed consent in accordance with the University of Illinois Urbana-Champaign Institutional Review Board. Participants met the following inclusion criteria: aged between 65 and 85 years old; live independently; fluent in English; adequate visual and auditory acuity; Geriatric Depression Scale (GDS) score of 4 or below; Instrumental Activities of Daily Living Scale (IADL) score of 6 or above; and Computer Proficiency Questionnaire (CPQ) score more than 18. Cognitively normal older adults were required to have a Montreal Cognitive Assessment (MoCA) score between 26 and 30. Participants were excluded if they had a history of other neurologic diseases, medical illnesses, major psychiatric disturbance, or currently taking psychoactive medications.
Older adults with MCI met the following additional eligibility criteria: subjective memory concern reported by participant, informant, or clinician; objective memory loss measured by education-adjusted scores on delayed recall of paragraph A from the Wechsler Memory Scale IV Logical Memory subtest; Clinical Dementia Rating of 0.5; essentially preserved activities of daily living determined by IADL scores, and an absence of dementia (no evidence of significant impairment in social or occupational functioning). Those who were on cholinesterase inhibitors and other medications (e.g., estrogen/estrogen-like compound) were included if on a stable dose for 12 weeks prior to the initial screening.
Questionnaires
Participants completed questionnaires (Table 1) to collect demographic information, computer proficiency, baseline level social engagement (loneliness and friendship), experiences with using social network systems, perceptions of video chat, and system usability evaluation.
Table 1.
Description of questionnaires
| Category | Questionnaires | Description |
|---|---|---|
| Demographics and health status | Demographic and health questionnaire (Czaja et al., 2006) | Self-report demographic information (e.g., sex, age, education, marital status, race/ethnicity, type of housing), and health status |
| Social networking and technology use experiences | Social Networking Questionnaire | Self-report on frequency of use of video chat (e.g. Skype, FaceTime), response options 0= Never heard of this, 1 = Never, 2 = Once or twice a year, 3= A few times a month, 4 = At least once a week, 5 = Daily; who they connected with on video chat |
| Adapted Perceived Ease of Use and Perceived Usefulness Questionnaire | Adapted the Perceived Ease of Use and Perceived Usefulness scales from the TAM (Davis, 1989; e.g., “video chat is easy to use”; “video chat increases communication”), with response options 1 = Strongly disagree, 2 = Disagree, 3 = Neutral, 4 = Agree, 5 = Strongly agree. | |
| Computer Proficiency Questionnaire-12 (Boot et al., 2015) | Assessed participants’ computer proficiency using six subscales: a) computer basics, b) printing, c) communication, d) Internet, e) scheduling software, f) multimedia use. Each subscale has two questions. To evaluate users’ proficiency in using video chat, we added three additional items: camera, external camera, and microphone. Participants rated their ability on a 5-point scale (1 = Never tried, 2 = Not at all, 3 = Not very easily, 4 = Somewhat easily, 5 = Very easily). | |
| Usability evaluation | System Usability Scale (Brooke, 1996) | Quantifies the usability of user-machine interfaces, consisting of 10 standard questions ((e.g., 1 found the system unnecessarily complex; 1 felt very confident using the system), with response options 1 = Strongly disagree, 2 = Disagree, 3 = Neutral, 4 = Agree, 5 = Strongly agree. Higher scores indicating greater usability. |
| Conversation topics of interest | Conversation Topic Questionnaire | Measures interest in 21 conversation topics, with response options 1 = not at all interested, 5 = extremely interested. Topics include aging, art, books, college experience, cooking, education, exercise, family, fashion, gardening, health, hobbies, holidays, movies, music, pets, sports, technology, television shows, travel, and volunteering. |
| Social engagement | UCLA Loneliness scale (Version 3; Russell, 1996) | Measures the feeling of loneliness, using ratings of 20 items on a 4-point scale (1= Never, 2= Rarely, 3= Sometimes, 4= Always). Higher scores indicate greater degrees of loneliness (maximum score 80). |
| Friendship scale (Hawthorne, 2006) | Measures social isolation and social connection, consisting of six items, with response options, 0= Not at all, 1=Occasionally, 2= About half the time, 3= Most of the time, 4= Almost always. Score range is 0-24, with 0-11 very socially isolated; 12-15 isolated or low-level social support; 16-18 some social support; 19-21 socially connected; and 22-24 very socially connected. |
Procedure
There were four parts of the demonstration study. First was the pre-demonstration interview, where-in participants completed the Social Networking Questionnaire, Perceived Ease of Use and Usefulness Questionnaire, Computer Proficiency Questionnaire, and were asked to elaborate on the answers they provided in these questionnaires in an interview format. Next, participants were presented a demonstration video of the purpose and functionality of the OneClick system. During the demonstration interview, participants were asked about their general opinions and initial reactions to the system and their specific opinions for each step and interface of the system. In the postdemonstration interview, participants answered open-ended questions related to the ease-of-use, usefulness, recommendations for modifications, and their preferences towards conversation topics, group size, and characteristics of potential conversational partners (e.g., age, familiarity with the partners; see Table 2 for details of the interview questions). Finally, participants completed System Usability Scale, demographic and health questionnaires, Loneliness Scale, and Friendship Scale. The entire procedure took approximately two hours to complete and all interviews were audio-recorded.
Table 2.
Overview of interview questions
| General opinions |
|
| Preferences of using OneClick |
Group size
|
People
|
Topics
|
| Usability testing (Phase 1 and 3) |
Ease of use
|
Usefulness
|
| Concerns (Phase 1 and 3) |
|
Data and statistical analysis
A theoretically driven approach (Mason, 2006) based on the TAM was used for analysis to capture participants’ opinions, preferences, perceived ease of use, perceived usefulness, and concerns. The analysis was completed by two trained graduate students, with backgrounds in dementia, aging, and human factors research. Audio files were first professionally transcribed verbatim. Qualitative data from transcripts and field notes taken during the interview were reviewed to develop a coding system. The unit of analysis was defined as the completion of one thought. The units were entered into Microsoft Excel and were coded based on TAM constructs (e.g., user intent, usefulness, ease of use) to capture participants’ perceptions of the OneClick system. Codes with similar content were grouped into thematic categories to identify participants’ responses related to experiences, preferences, ease of use, and perceived usefulness.
Following a mixed-method approach, data from the Social Networking Questionnaire, Perceived Ease of Use and Usefulness Questionnaire, Computer Proficiency Questionnaire, and System Usability Scale were analyzed in SPSS 24.0. System Usability Scale scores were averaged for each participant and transformed into a usability score out of 100, where a score of 68 or above is considered to be above average (Bangor, Kortum, Miller, 2008).
Results
Participants
Table 3 provides summary information about the participants. Participants had some social support (Friendship Scale) and low levels of loneliness (Loneliness Scale). All participants had basic computer skills and were able to complete simple tasks, such as using a computer keyboard and mouse, and opening and sending emails (Computer Proficiency).
Table 3.
Description of participants
| Characteristics | Phase 1 (n=15) | Phase 3 (n=4) |
|---|---|---|
| Mean (SD) | Mean (SD) | |
| Age | 76.7 (5.6) | 74.5 (6.6) |
| Friendship scale | 15.67 (1.18) | 21.25 (2.22) |
| Loneliness scale | 34.87 (7.67) | 32.00 (7.44) |
| Computer proficiency questionnaire | ||
| Computer basic | 4.73 (0.37) | 4.50 (0.58) |
| Communication | 4.90 (0.28) | 5.00 (0.00) |
| Characteristics | n (%) | n (%) |
| Gender | ||
| Male | 9 (60) | 1 (25) |
| Female | 6 (40) | 3 (75) |
| Education | ||
| High school | 1 (25) | |
| Some college | 1 (7) | 1 (25) |
| Bachelor’s degree | 2 (13) | |
| Master’s degree | 9 (60) | 1 (25) |
| PhD | 3 (20) | 1 (25) |
| Race (White) | 15 (100) | 4 (100) |
| Health status | ||
| Fair | 1 (7) | |
| Good | 2 (13) | 2 (50) |
| Very good | 9 (60) | 2 (50) |
| Excellent | 3 (20) |
Experiences with using video chat (compared with other social network systems)
The overall pattern of results was similar for older adults with MCI and those cognitively normal older adults; thus, combined data are presented. We compared participants’ experiences using video chat with four other popular social networking systems (Email, text messaging, Facebook, and hobby-related forums). Video chat systems (e.g., Skype, Facetime) were used less (“less than once or twice a year”) than other social networking systems: Email (“more than once a week”), text messaging (“more than a few times a month”), Facebook (“more than a few times a month”), and hobby-related forums (“nearly once or twice a year”). Eight participants (53.3%) reported they never used video chat, four (26.7%) used video chat once or twice a year, and three (20.0%) used video chat a few times a month. The people they spoke with via video chat were mostly family and friends. Only one participant (6.6%) reported talking to people they had never met before. The interviews revealed that all participants with the experience of using video chat used it to contact family who lived far away to discuss general family affairs or to set up events (e.g., holiday gatherings). In sum, participants used video chat less frequently than other social networking systems and they largely used it in ways that were more family- and friends-focused.
Attitudes toward video chat and original OneClick system
We assessed participants’ attitudes toward video chat, in general, using Perceived Ease of Use and Usefulness Questionnaire. The result of t-test indicates that the mean score (M=3.50, SD=.67) was significantly higher than neutral (p=.01), suggesting that participants perceived video chat would be easy to use and useful to them.
Participants’ attitudes toward OneClick specifically were investigated by the System Usability Scale (SUS) and interview questions about their perceived ease of use and usefulness of OneClick after they watched the demonstration video of OneClick. The average SUS score was 78.17 ±13.41 across all participants. Although the scores were higher for the cognitively normal group, the difference was not significant (p>.05); cognitively normal older adults (82.25 ± 12.99) and older adults with MCI (70.00 ± 11.18). These scores represent good usability (i.e., above-average score of 68) after participants viewed the demonstration of the OneClick system.
Participants’ perceptions of ease of use of OneClick were captured by their interview responses about their general impression and opinions of the system. Overall, participants found the OneClick system easy to use. Fourteen participants (93.3%) expressed that the system was simple and required little effort to use, such as easy access, clear design and layout, and the functions of icons were easy to understand. For example, one participant mentioned that it was much easier than Skype, and said:
“I like that I can text and talk, people might have an idea that they didn’t wanna interrupt the conversation”
[Male, 74 years old].
However, there was one participant who reported that the video meeting room was:
“way more trouble than it’s worth, it might take some time to get used to that”, and she preferred video events because video events “would have a purpose, an announcement or something”
[Female, 76 years old].
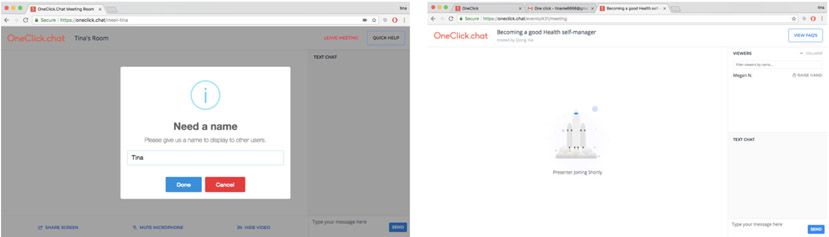
Some participants identified design problems related to terminology of buttons, visibility of system status, font size, and layout of the interface. For example, one participant mentioned that the meanings of “mute microphone” and “hide video” were not clear and instead suggested using “turn off” (Figure 1). Two participants reported that the “done” button did not make sense and advised changing it to a “join” button (Figure 2 left). Three participants said that the meaning of the “raise hand” button was not clear or a little childish and suggested changing it to “post a question” or “ask a question” (Figure 2 right). One participant suggested showing a clock before events began to tell them how long they had to wait until the event started. Two participants reported that the buttons below the video area were hardly visible due to the font. Another participant reported that the buttons under the video chat area were too scattered (Figure 1).
Figure 2.
Screenshots of the interface before entering OneClick meeting room (left) and OneClick video event starts (right)
In addition to some design issues, participants noted potential points of frustration with using the system. Five participants mentioned possible problems with the conversation itself, such as someone dominating the conversation. For example, one participant reported the potential difficulty in coordinating the conversation:
“Conversation could be frustrating, whenever you get people in there, there’s gonna be some different ideas”
[Male, 79 years old, MCI].
Four participants reported that their memory issues might influence using the system, including one participant with MCI. For example, one participant shared her own frustration of remembering things:
“Many times, I think I know how to use it, it turns out I always miss a step”
[Female, 86 years old].
Participants also mentioned their strategies for overcoming memory issues, such as printed instructions or repetition:
“I would probably have it written down on a piece of paper. You know, the steps…”
[Female, 86 years old];
“Getting into the system could be frustrating if one were beginning to have some cognitive issues or lack of basic computer knowledge. A printout of steps might help because we are print-oriented”
[Female, 84 years old];
“I might get confused about what I [was] supposed to click on, but once I did, I would know”
[Female, 86 years old];
“If you show me where. I’ll not remember it, but that’s okay, if I see it a couple of times, I will get it”
[Male, 70 years old, MCI];
“I got confused at some point, but my own learning style is with repetition”
[Female, 85 years old].
A few participants reported concerns about privacy (n=2), price (n=1), quality of video (n=1), busy schedule (n=1), and problems of interacting with other people due to shyness (n=1). The two participants concerned about privacy preferred to use a pseudonym instead of their real name when they did not know the people in the group.
Regarding the perceived usefulness of the system, participants described benefits and drawbacks of it. It appeared that all participants could see the value of the OneClick system, both in general and for very specific features. Participants expressed that OneClick was useful in providing another opportunity for social interaction with diverse individuals, sharing interests and ideas, and expanding their horizons. For example, one participant expressed what he liked about communication via video chat:
“I like the concept of video chat, so you can actually see people that you are speaking with, and communicating with and they can communicate back with You....The basic thing that would attract me is you can sense another person’s emotions both through hearing and seeing”
[Male, 70 years old, MCI].
More than half of the participants also pointed out the specific potential benefits of using the system. They mentioned that it might be beneficial for people who have mobility or health issues, lonely people, new residents of locations such as continuing care retirement communities, those who live far away from friends and/or family, and during bad weather. Participants also mentioned that it could be used for committee meetings, book clubs, educational purposes, talking about medical problems, catching up with friends or family members, playing online games, and learning and keeping up with new technology. With regard to the drawbacks of the system, participants stated their preference for in-person communication rather than video chat and potential problems of the conversation. Ten participants (66.7%) reported that they would prefer to be socially engaged with others in face-to-face conversation, such as going out to eat, going to a movie with close friends, or going to other service groups (e.g., church), rather than online via OneClick video chat. Moreover, two participants indicated they might become bored easily if the conversation is uninteresting or at a slow pace. Another two participants mentioned that there might be more enjoyment after real interaction with the system, as opposed to just watching the demonstration video.
Preference for video chat using OneClick
We investigated participants’ preferences on how they would like to use OneClick, including the topics they would like to discuss, who they would like to talk to, and the group size for discussion. To investigate participants’ interest for conversation topics, we listed 21 topics (e.g., aging, art, books) on a 5-point Likert scale (1= not at all interested, 5= extremely interested). Participants identified ten topics that they were interested in: Books (M=3.89, SD=0.93), health (M=3.70, SD=0.95), family (M=3.67, SD=1.41), exercise (M=3.40, SD=1.43), hobbies (M=3.33, SD=1.50), technology (M=3.10, SD=1.10), music (M=3.10, SD=1.10), aging (M=3.00, SD=0.94), movies (M=3.00, SD=1.41), and travel (M=3.00, SD=0.94).
Their preference for people and group size were identified from the interview responses. All participants reported that the age of the group members did not matter, but three participants mentioned that it could depend on the type of person or the topic of the conversation. More specifically, participants reported that they preferred to talk about health, cooking, and travel with people who were of a similar age.
“It [is] ok to talk to people who are similar in age to me, they have similar experiences.”
“It is good to talk to people who are older. I have a good friend, who is 100… I just admire her so much. It depends on the person.”
[Female, 86 years old]
One participant expressed her preference for talking with younger people stating:
“I like to have friends quite a bit younger too.”
[Female, 86 years old]
Two participants with MCI did express concern about talking with younger people, even though they reported that overall they did not have a problem talking with them:
“I don’t have problem to talk with younger people, as long as they don’t try to overwhelm my knowledge.”
[Male, 79 years old, MCI]
“We probably wouldn’t be on the same page with younger people, we might have different opinions, but we’d be okay with kind of expressing that with it”
[Male, 70 years old, MCI]
Regarding meeting new people via video chat, five participants reported that they had no problem meeting new people and two participants reported enjoyment in talking with new people. However, seven participants expressed concern, stating that they needed a topic or preliminary conversation, extra effort, or good manners to get used to new people. One participant stated:
“I think I’d probably be a little uncomfortable at first. When you meet someone new, you kind of get a sense of the direction or what they like and what they don’t like and how they think, so it’s just getting used to it.”
[Female, 70 years old, MCI].
The results suggest that older adults are interested in getting to know new people and broadening their social networks, but their concerns about conversation arrangement and social techniques should be addressed when organizing social activities for them.
With regard to participants’ preference for group size for video chat via OneClick, eleven participants (73.3%) reported that they would prefer a group size between three to six people, but it ultimately depended on the conversation. If the conversation were brainstorming or developing ideas, then more people would be better, but if it were a more casual discussion then fewer people would be better. Four participants reported they preferred one-on-one conversations.
Phase 1: Study summary
The demonstration study revealed that participants used video chat less than other popular social networks, such as Email, text messaging, and Facebook. Family and friends were the main people they spoke with via video chat. The topics and activities they discussed were mainly related to family affairs, event set-ups, etc. However, such family- and friends-focused activities might limit the variety of their social activities. The OneClick video chat system was perceived as providing opportunities for older adults to get to know new people and talk about different topics, thus connecting and engaging them in broader social activities. Participants’ attitudes toward video chat were positive. The usability testing showed that participants perceived OneClick to be easy to use and useful after they viewed the demonstration video. As we expected, specific system design issues for older adults with and without MCI were identified, and the system was updated based on participants’ feedback. To identify more potential issues of the system, we next conducted expert heuristic evaluations.
Phase 2: Heuristic evaluations
Two separate heuristic evaluations were completed to identify usability problems with the OneClick system. We followed the basic protocol and the ten heuristics described by Nielsen (Nielsen and Molich, 1990) and available on NN/g Nielson Norman Group website (https://www.nngroup.com/articles/ten-usability-heuris-tics/). One heuristic evaluation was conducted by two human factors experts with specific consideration for motor, perceptual, and cognitive limitations of older adults. The other heuristic evaluation was conducted by three experts with a background in MCI and dementia by taking the perspective of older adults with MCI to focus on particular use challenges for this target user group. Evaluations by these two groups were conducted independently and employed standard usability metrics, focusing on learnability (how easy it is to learn to use); efficiency (can users achieve their intended objectives within a reasonable amount of time); memorability (how easy it is to remember how to use the device following periods of nonuse); and errors (user’s desired goal not being accomplished).
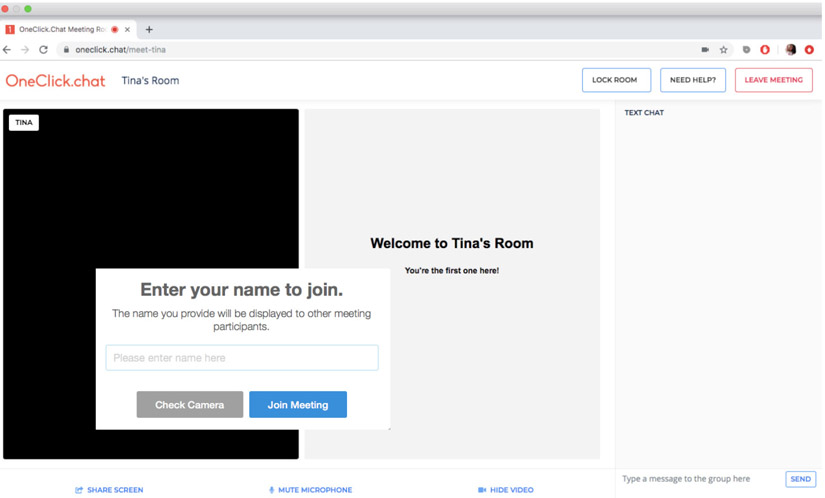
A total of 54 problems were identified by the experts. The heuristic most frequently violated was Match Between System and the Real World (e.g., speaking users’ language) accounting for 28% (15 issues). Consistency and Standard (e.g., buttons with different colors should not have same functions) were second contributing to 19% (10 issues) of the total errors, followed by Visibility of System Status (e.g., appropriate feedback from the system; 11%; 6 issues) and Recognition rather than Recall (e.g., minimizing users’ memory load by visible options; 11%; 6 issues), and lastly Aesthetic and Minimalist Design (e.g., simple information) (7%; 4 issues). Together, the feedback from participants in Phase 1 and the two expert heuristic evaluations guided the OneClick redesign, such as changes related to making technical terminology more user-friendly language (e.g., change “done” button to “join meeting” button) and showing the users the status of the system (e.g., after entering the meeting room, provide feedback “you are the first one here!”; Figure 3).
Figure 3.
Updated OneClick system
Phase 3: Interaction study
Based on the learnings from Phases 1 and 2, we updated and refined the OneClick system for use by older adults with and without MCI. In Phase 3, we used the redesigned OneClick system to move beyond a demonstration of the system and enabled participants to have hands-on experience with using OneClick through actual video chat conversations. We examined participants’ attitudes toward OneClick and the preferences for conversation topics, group size, and characteristics of potential conversation partners after they viewed a presentation about the system. Subsequently, participants interacted with the updated OneClick system after which they were interviewed and asked to complete the same questionnaires as in Phase 1 (Table 1) to obtain post-interaction data. The data were analyzed using the same methodology as Phase 1
Method
Four individuals (n=2 cognitively normal older adults; n=2 older adults with MCI) completed testing. Two of the four participants had also participated in Phase 1. The inclusion and exclusion criteria were the same as Phase 1. Participants first viewed a presentation on the purpose and functionality of the updated OneClick system. To address potential memory issues reported by participants in Phase 1, we provided printed guidance to show participants different steps and review demonstration slides with participants after the presentation. As participants in Phase 1 reported that they were comfortable speaking with different ages and new people, younger trained research assistants acted as conversation partners when participants interacted with the OneClick system. During the interaction, participants performed a series of tasks, including joining an event, initiating a conversation during breakout group discussions, participating in a two-person conversation on the topic of hometown, and participating in a four-person discussion on the topic of favorite restaurants in the local community. After the interaction, participants were asked questions about their perceived ease of use and usefulness of the system (Table 2). Following the interviews, participants completed questionnaires. The whole process took approximately two hours to finish and the interviews were audio-recorded.
Results
Participants
Table 3 provides summary information about the participants. The Friendship Scale score indicated that participants were socially connected on average. The Loneliness Scale score indicated that participants had low levels of loneliness. Scores for the computer proficiency questionnaire showed that all participants had basic computer skills and were able to complete simple tasks, such as using a computer keyboard and mouse, and opening and sending emails. Three out of four participants had experience using video chat, such as using Skype or FaceTime to connect with their children or grandchildren.
Attitudes toward the updated OneClick system
After interacting with the updated system, the average score on the SUS was 70.63 (SD=7.18) across all participants. The average score on the SUS was 75.00 (SD=7.07) among cognitively normal older adults and 66.25 (SD=5.30) among older adults with MCI. The difference in scores was largely due to (i) cognitively normal older adults perceiving the system as easier to use without help than older adults with MCI, (ii) cognitively normal older adults feeling more confident using the system than older adults with MCI, and (iii) older adults with MCI being concerned that they needed to learn a lot of things before using the system. However, participants reported the ease of use of the system in the interview, such as clear instructions, easy accessibility, and good video quality. No one reported challenges or difficulties related to using the new system. One participant stated:
“I liked it; it was clear both auditorily and visually. What I like [about] seeing someone is the added cues of seeing obviously over hearing....I thought it was fun, and it was easy, and it was like being with them. It didn’t seem that the technology was even there.”
[Male, 74 years old]
However, some participants identified design problems related to control of action and visibility of the system status. One participant reported that they could not contact the host during the four-person discussion group and advised providing a way to text the host or add a “help” button to connect with the host. One participant reported that they did not know how much time was left for the group discussion and advised showing a clock to warn people about the time. Another participant reported that there was no auditory alert when the host sent a text message to the breakout group, making it easy to miss the message:
“I wasn’t paying attention when you gave a cue, maybe there should be a little ‘ding’ every time when a cue appears.”
[Male, 74 years old]
Two participants reported concerns about the video event invitation and the length of the conversation. One participant reported that it might be better to provide text reminders about up-coming events because they might miss or not see an email reminder in time. Another participant expressed that it was important to balance the length of the conversation so that it was not too long or too short.
In this interaction study, participants reported similar perceptions of the usefulness of OneClick system as compared to Phase 1. All four participants could imagine the benefits of OneClick events for themselves or others, such as facilitating communication, connecting with friends and family members who lived far away, meeting with people they had never met before, and participating in events (e.g., book club). One participant even expressed their preference for video chat over the telephone:
“I hate telephone, seeing someone and talking to them is easier for me.”
[Male, 74 years old]
However, two out of four participants stated their preference for face-to-face conversation rather than video chat.
Preference of video chat with OneClick
After their interaction using OneClick, all participants reported that they had no problem interacting with new people and felt comfortable interacting with one other or three other people. Three out of four participants reported no preference between the two types of conversation. However, one participant reported that they preferred two-person conversation because they could just concentrate on that one person. All participants reported their enjoyment of both hometown and restaurant topics.
Phase 3 study summary
In Phase 3, all participants reported no problems with the topics, group size, and people who were part of the conversation. All participants perceived the new system easy to use after having real interaction with it, but their perceptions of the usability of the system were more focused on the process of using the system, such as accessibility and instruction. The reported concerns and problems were also about the interaction process, such as feedback from the system and visibility of the system status, and length about the conversation. Overall, all participants perceived the new system as useful for social engagement.
Discussion
Main findings
In this work, we investigated the experiences and preferences of using a video chat system, received feedback on usability, and identified facilitators and barriers of perceived ease of use and usefulness from older adults with and without MCI.
Participants revealed that most of their previous experiences using social network systems were with email, messaging, and video chat to keep in touch with family members and friends, and with Facebook and hobby-related forums to look through information and updates from different people. This echoes two previous studies that older people use different communication channels with different social relationships for different social support (Bixter et al., 2018; Quan-Haase, Mo, & Wellman, 2017). Older people generally use (i) email, messaging, phone and video chat (e.g. Skype) with friends or family members for coordination or connection-strengthening; and (ii) Facebook or hobby-related forums with other older adults or family members for gathering and sharing information (information-sharing) and/or forming new connections (connection-forming) or maintaining social ties. As such, these experiences provide older adults benefits of accessing information, building and maintaining connections, and reinforces their behavior of using social network systems.
The current study also found that older adults with and without MCI mostly connect with family and friends. This is consistent with previous findings of the age-related changes in the size and composition of social networking. Chang et al. (2015) found that network size was negatively associated with age, and the proportion of meaningful ties was positively associated with age. This has been explained by the socioemotional selectivity theory by Carstensen, Isaacowitz, and Charles (1999) and the idea that older adults assign greater importance to have small social networks that are comprised of family members and longtime friends. Family and friends are strong ties in the social networks of older adults, as they are important sources of social support for older people to maintain their health and well-being. However, other findings indicate that diverse network and friend-focused network types are more beneficial to older adults’ health than family-focused networks and restricted network types (Li & Zhang, 2015). Therefore, participating in various social activities is important for older adults’ health and well-being (Fankhauser, Maercker, & Forstmeier, 2017). Social engagement technology such as OneClick provides an opportunity for older people to interact with a diverse group of social contacts and increase the variety of their social relationships.
After viewing and interacting with the video chat system in Phase 1 and Phase 3, respectively, the system was perceived as easy to use by participants. They reported little effort to access and understand the system, and their high SUS scores indicated acceptable usability levels of the system. Research shows that once older people are engaged in a technology they tend to be high utilizers (Wildenbos, Peute, & Jaspers, 2017). Therefore, promoting the design of easy-to-use features may foster participant satisfaction and further use of additional features.
However, through iterative usability testing, we identified issues to be addressed for designing such technologies for older adults with and without MCI. First, the terminology used in the system should be easily understood by users and technical jargon should be avoided. Second, both visual and auditory feedback should be provided to inform users what they have done and what they need to do next. Third, large font size is important to help older adults see and read information and decrease their frustration with using the system. Fourth, the system should give users the autonomy to control their actions and not force users to execute unknown steps. Additionally, memory issues are common among older people, so clear and consistent instruction should be provided, such as hard copy instructions. Training is also necessary to address memory issues, such as teaching them the required steps in their first several times of using technology and allowing users more time to repeat. Following these lessons may help develop a highly usable social engagement system for older adults with and without MCI.
Although we found that some participants prefer face-to-face conversations over video chat conversations, generally, participants were open to meeting new people of all ages with OneClick. They perceived the system to be useful, such as the benefits of connecting with family, friends and participating in social events. These data suggest that social engagement technology has the potential to broaden older adults’ social networks and enhance their social interactions. However, the arrangement of conversations is important and should take older people’s preferences into account. To facilitate conversation via the system, it is necessary to facilitate a respectful environment to ease the process of knowing new group members. Our participants reported their favorite topics to be books, health, family, exercise, hobbies, technology, music, movies, and travel. They suggested that certain topics (e.g., health, hobbies, travel) might be better to discuss with similarly aged people. Their ideal group size was 3 to 6 people. Additionally, they described possible problem situations, such as someone dominating the conversation, which should be considered early and prepared for in advance. These preferences and concerns arising from our findings should be considered by designers of video chat systems.
In our study, we did not find differences in experiences or preferences for the video chat system between older adults with and without MCI. This is consistent with the work of Eghdam and colleagues (2018), who found that the communication of individuals with mild acquired cognitive impairment is similar to the healthy population, including the content, frequency, and types of interactions. We also did not find a significant difference in usability scores between the groups. This might be due to the small sample of this study or the use of the SUS measure. One study suggests that the SUS was not reliable for individuals with dementia, as it relies on reflection and short-term memory (Gibson et al., 2016); a similar issue might affect individuals with MCI. Individuals with MCI might require additional assistance and effort to use a video chat system. We did have to make some accommodations for the individuals with MCI in terms of reiteration of training materials and provision of reminders.
Limitations
One overarching limitation of the present research was the relatively small sample sizes. The Phase 1 sample size was 15 participants, perhaps not providing enough power to detect a statistically significant difference between healthy individuals and ones with MCI. The sample size of phase 3 was relatively small. Nonetheless, Nielson (2012) argued that around five participants are sufficient for identifying usability problems. Two participants in Phase 3 had participated in Phase 1. They might have adopted the system more easily, although they only saw a demonstration in Phase 1 but did not get to interact with the system. Furthermore, the SUS scale might be an invalid instrument for individuals with MCI due to memory demands and the need for self-reflection (Gibson et al., 2016). However, further research is needed to investigate the validity of the SUS scale for different severe levels of dementia.
Future research should consider how social engagement technology may benefit more diverse groups of older adults (ethnically and educationally), with different levels of cognitive impairment. Intervention studies are needed to test the effectiveness of social engagement technology to increase both quality and quantity of social interactions among the older population.
Design considerations
Our findings point to both general and specific ways to make social engagement technologies more easily usable and palatable to older adults with and without MCI. First, to optimize the design of social communication technologies for these groups, it is important to follow the basic principles and processes, such as identify the needs, preferences, experiences, and capacities of them, iterative usability testing, follow good human factors principles from the perspectives of them, and involve them in the design process.
Moreover, we found that the method of combining user-centered testing and expert evaluation was effective to identify problems with the system, including for older adults with MCI. Empirical measurement using questionnaires as well as quantitative or qualitative usability testing data are essential for successful social communication technology design.
In addition, our findings add specific design considerations to basic guidance. We found that older adults lacked experience using social communication technology (e.g. only half of the participants had even minimal experience using video chat systems). Providing users training could help them get access to the system. To decrease barriers to use for older adults, the lessons we learned from the user testing should be followed by the designer of social engagement technologies. To accommodate the needs of older adults with MCI to use social engagement system, besides providing refresher training and instructional support to address their memory challenges, designers should highlight the ease of use of the system and make the instructions and help system accessible and clear to increase their confidence of using the system.
Conclusions
We gained many valuable and novel insights from our participants about their experiences and preferences for using video chat systems, which was important for understanding what influences users’ perceived ease of use and usefulness and technology acceptance. Overall, participants found the OneClick video chat system to be useful and easy to use. We also tested and improved the OneClick system to enhance social interaction among older adults with and without MCI, and provided guidelines for key considerations promoting usefulness and ease of use. Older adults are unlikely to adopt burdensome technologies. Our processes showcased how technology for older adults can be developed, illustrating how to engage older adults with and without MCI in the iterative design process. In addition, our results provide general guidance for the development of social engagement technologies. Social engagement technology designers should obtain ongoing user interface and user experience feedback from older adults when developing or improving new technologies.
Acknowledgements
This research was supported in part by the National Institutes of Health (National Institute on Aging) Small Business Innovation Research Grant (R43 AG059450-01).
Presented meetings:
The Gerontological Society of America, Boston, Massachusetts, USA. November 14-18, 2018.
Human Factors and Ergonomics Society Health Care Symposium, Chicago, Illinois, USA. March 24-27, 2019
References
- Bangor A, Kortum PT, & Miller JT (2008). An empirical evaluation of the system usability scale. Intl. Journal of Human–Computer Interaction, 24(6), 574–594. [Google Scholar]
- Bixter MT, Blocker KA, & Rogers WA (2018). Enhancing social engagement of older adults through technology. In Aging, Technology and Health (pp. 179–214). Academic Press. 10.1016/B978-0-12-811272-4.00008-7 [DOI] [Google Scholar]
- Bourassa KJ, Memel M, Woolverton C, & Sbarra DA (2017). Social participation predicts cognitive functioning in aging adults over time: comparisons with physical health, depression, and physical activity. Aging & mental health, 21(2), 133–146. [DOI] [PubMed] [Google Scholar]
- Brooke J (1996). SUS-A quick and dirty usability scale. Usability evaluation in industry, 189(194), 4–7. [Google Scholar]
- Cacioppo JT, & Cacioppo S (2014). Social relationships and health: The toxic effects of perceived social isolation. Social and personality psychology compass, 8(2), 58–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carstensen LL, Isaacowitz DM, & Charles ST (1999). Taking time seriously: A theory of socioemotional selectivity. American psychologist, 54(3), 165. [DOI] [PubMed] [Google Scholar]
- Chang PF, Choi YH, Bazarova NN, & Löckenhoff CE (2015). Age differences in online social networking: Extending socioemotional selectivity theory to social network sites. Journal of Broadcasting & Electronic Media, 59(2), 221–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Child ST, & Lawton L (2019). Loneliness and social isolation among young and late middle-age adults: Associations with personal networks and social participation. Aging & mental health, 23(2), 196–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chopik WJ (2016). The benefits of social technology use among older adults are mediated by reduced loneliness. Cyberpsychology, Behavior, and Social Networking, 19(9), 551–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christakis N (2004). Social networks and collateral health effects: Have been ignored in medical care and clinical trials, but need to be studied. British Medical Journal, 329(7459), Article 184. doi: 10.1136/bmj.329.7459.184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyle CE, & Dugan E (2012). Social isolation, loneliness and health among older adults. Journal of aging and health, 24(8), 1346–1363. [DOI] [PubMed] [Google Scholar]
- Czaja SJ, Boot WR, Charness N, Rogers WA, & Sharit J (2018). Improving social support for older adults through technology: Findings from the PRISM randomized controlled trial. The Gerontologist, 58(3), 467–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czaja SJ, Charness N, Fisk AD, Hertzog C, Nair SN, Rogers WA, & Sharit J (2006). Factors predicting the use of technology: findings from the Center for Research and Education on Aging and Technology Enhancement (CREATE). Psychology and aging, 21(2), 333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis FD (1989). Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS quarterly, 319–340. [Google Scholar]
- de Frias CM, & Dixon RA (2013). Lifestyle engagement affects cognitive status differences and trajectories on executive functions in older adults. Archives of Clinical Neuropsychology, 29(1), 16–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eghdam A, Hamidi U, Bartfai A, & Koch S (2018). Facebook as communication support for persons with potential mild acquired cognitive impairment: A content and social network analysis study. PloS one, 13(1), e0191878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fankhauser S, Maercker A, & Forstmeier S (2017). Social network and cognitive functioning in old age. Zeitschrift für Gerontologie und Geriatrie, 50(2), 123–131. [DOI] [PubMed] [Google Scholar]
- Friedler B, Crapser J, & McCullough L (2015). One is the deadliest number: the detrimental effects of social isolation on cerebrovascular diseases and cognition. Acta neuropathologica, 129(4), 493–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garms-Homolová V, Notthoff N, Declercq A, van der Roest HG, Onder G, Jónsson P, & van Hout H (2017). Social and functional health of home care clients with different levels of cognitive impairments. Aging & mental health, 21(1), 18–23. [DOI] [PubMed] [Google Scholar]
- Gibson A, McCauley C, Mulvenna MD, Ryan A, Laird EA, Curran K, & Bond R (2016, October). How Usable Are Usability Tests? Examining the Suitability of Standard Usability Testing Methods for the Assessment of Apps for People Living with Dementia. In International Workshop on ICTs for Improving Patients Rehabilitation Research Techniques (pp. 126–143). Springer, Cham. 10.1007/978-3-030-16785-1_10 [DOI] [Google Scholar]
- Gombault V (2013). L’internet de plus en plus prisé, l’internaute de plus en plus mobile. INSEE première, 1452, 1–4. [Google Scholar]
- Haslam C, Cruwys T, Milne M, Kan CH, & Haslam SA (2016). Group ties protect cognitive health by promoting social identification and social support. Journal of aging and health, 28(2), 244–266. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, & Capitanio JP (2015). Perceived social isolation, evolutionary fitness and health outcomes: a lifespan approach. Philosophical Transactions of the Royal Society B: Biological Sciences, 370(1669), 20140114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawthorne G (2006). Measuring Social Isolation in Older Adults: Development and Initial Validation of the Friendship Scale. Social Indicators Research, 77(3), 521–548. Retrieved from http://www.jstor.org/stable/27522594 [Google Scholar]
- Hughes TF, Flatt JD, Fu B, Chang CCH, & Ganguli M (2013). Engagement in social activities and progression from mild to severe cognitive impairment: the MYHAT study. International psychogeriatrics, 25(4), 587–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huxhold O, Fiori KL, & Windsor TD (2013). The dynamic interplay of social network characteristics, subjective well-being, and health: The costs and benefits of socio-emotional selectivity. Psychology and Aging, 28(1), 3. [DOI] [PubMed] [Google Scholar]
- Ihm J, & Hsieh YP (2015). The implications of information and communication technology use for the social well-being of older adults. Information, Communication & Society, 18(10), 1123–1138. [Google Scholar]
- Klinenberg E (2016). Social isolation, loneliness, and living alone: identifying the risks for public health. American journal of public health, 106(5), 786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotwal AA, Kim J, Waite L, & Dale W (2016). Social function and cognitive status: results from a US nationally representative survey of older adults. Journal of general internal medicine, 31(8), 854–862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li T, & Zhang Y (2015). Social network types and the health of older adults: Exploring reciprocal associations. Social Science & Medicine, 130, 59–68. [DOI] [PubMed] [Google Scholar]
- Luhmann M, & Hawkley LC (2016). Age differences in loneliness from late adolescence to oldest old age. Developmental Psychology, 52(6), 943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bixter MT, Blocker KA, Mitzner TL, Prakash A, Rogers WA (2019). Understanding the use and non-use of social communication technologies by older adults: A qualitative test and extension of the UTAUT model. Gerontechnology,18(2), 70–88. 10.4017/gt.2019.18.2.002.00 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macedo IM (2017). Predicting the acceptance and use of information and communication technology by older adults: An empirical examination of the revised UTAUT2. Computers in Human Behavior, 75, 935–948. [Google Scholar]
- Mason J (2006). Mixing methods in a qualitatively driven way. Qualitative research, 6(1), 9–25. [Google Scholar]
- Mitzner TL, Boron JB, Fausset C, Adams AE, Charness N, Czaja SJ, Sharit J (2010). Older adults talk technology: Technology use and attitudes. Computers in Human Behavior, 26(6), 1710–1721. 10.1016/j.chb.2010.06.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitzner TL, Rogers WA, Fisk AD, Boot WR, Charness N, Czaja SJ, & Sharit J (2016). Predicting older adults’ perceptions about a computer system designed for seniors. Universal Access in the Information Society, 15(2), 271–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrow-Howell N, & Gehlert S (2012). Social engagement and a healthy aging society. Public health for an aging society, 205. [Google Scholar]
- Mortimer JA, Ding D, Borenstein AR, DeCarli C, Guo Q, Wu Y, & Chu S (2012). Changes in brain volume and cognition in a randomized trial of exercise and social interaction in a community-based sample of non-demented Chinese elders. Journal of Alzheimer's Disease, 30(4), 757–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myhre JW, Mehl MR, & Glisky EL (2017). Cognitive benefits of online social networking for healthy older adults. The Journals of Gerontology: Series B, 72(5), 752–760. [DOI] [PubMed] [Google Scholar]
- Nielsen J, and Molich R (1990). Heuristic evaluation of user interfaces. In Proceedings of the SIGCHI conference on Human factors in computing systems (pp. 249–256). New York: ACM. 10.1145/97243.97281 [DOI] [Google Scholar]
- Nielsen J (2012). How many test users in a usability study. Nielsen Norman Group, 4(06). [Google Scholar]
- Nygård L, & Kottorp A (2014). Engagement in instrumental activities of daily living, social activities, and use of everyday technology in older adults with and without cognitive impairment. British Journal of Occupational Therapy, 77(11), 565–573. [Google Scholar]
- Nyqvist F, Forsman AK, Giuntoli G, & Cattan M (2013). Social capital as a resource for mental well-being in older people: A systematic review. Aging & Mental Health, 17(4), 394–410. [DOI] [PubMed] [Google Scholar]
- Poscia A, Stojanovic J, La Milia DI, Duplaga M, Grysztar M, Moscato U, & Magnavita N (2018). Interventions targeting loneliness and social isolation among the older people: an update systematic review. Experimental gerontology, 102, 133–144. 10.1016/j.exger.2017.11.017 [DOI] [PubMed] [Google Scholar]
- Quan-Haase A, Mo GY, & Wellman B (2017). Connected seniors: How older adults in East York exchange social support online and offline. Information, Communication & Society, 20(7), 967–983. [Google Scholar]
- Russell DW (1996). UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. Journal of personality assessment, 66(1), 20–40. [DOI] [PubMed] [Google Scholar]
- Small BJ, Dixon RA, McArdle JJ, & Grimm KJ (2012). Do changes in lifestyle engagement moderate cognitive decline in normal aging? Evidence from the Victoria Longitudinal Study. Neuropsychology, 26(2), 144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stepler R (2016. February). Smaller share of women ages 65 and older are living alone: More are living with spouse or children. Washington, DC: Pew Research Center. [Google Scholar]
- The Pew Research Center Reports on Technology Device Ownership and Social Media Usage Levels. (2015). Digital Publishing Report, 4(8), 2. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=edb&AN=111887070&site=eds-live&scope=site [Google Scholar]
- Tseng YC, Liu SHY, Lou MF, & Huang GS (2018). Quality of life in older adults with sensory impairments: a systematic review. Quality of Life Research, 27(8), 1957–1971. [DOI] [PubMed] [Google Scholar]
- Vespa J, Lewis JM, & Kreider RM (2013). America’s families and living arrangements: 2012. Current Population Reports, 20(2013), P570. Retrieved from https://www.census.gov/data/tables/2016/demo/families/cps-2016.html (updated in 2018). [Google Scholar]
- Wildenbos GA, Peute L, & Jaspers M (2017). Facilitators and barriers of electronic health record patient portal adoption by older adults: a literature study. Stud Health Technol Inform, 235, 308–312. [PubMed] [Google Scholar]
- Yang YC, Boen C, Gerken K, Li T, Schorpp K, & Harris KM (2016). Social relationships and physiological determinants of longevity across the human life span. Proceedings of the National Academy of Sciences, 113(3), 578–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zebhauser A, Hofmann-Xu L, Baumert J, Häfner S, Lacruz ME, Emeny RT, & Ladwig KH (2014). How much does it hurt to be lonely? Mental and physical differences between older men and women in the KORA-Age Study. International journal of geriatric psychiatry, 29(3), 245–252. [DOI] [PubMed] [Google Scholar]