Abstract
Introduction
In Nepal, one-fourth of the adult population has hypertension. Despite provision of comprehensive hypertension services through the primary healthcare system, huge gaps in treatment and control of hypertension exist. Our study explored the individual, interpersonal, health system and community-level barriers and facilitators affecting hypertension management in urban Nepal.
Methods
We used a qualitative methodology informed by Kaufman’s socioecological model, conducting focus group discussions with hypertension patients and their family members. In-depth interviews with hypertension patients, healthcare providers and municipal officials were also conducted.
Results
We found that inadequate knowledge about hypertension and harmful cultural beliefs hindered effective treatment of hypertension. Interrupted medical supply and distrust in primary healthcare providers affected the poor’s access to hypertension services. Poor communication between family members and gender norms affected adaptation of treatment measures. This study emphasised the role of family members in supporting patients in adhering to treatment measures and rebuilding community trust in primary healthcare providers for better access to hypertension services. The findings guided the development of a manual to be used by community health workers during home visits to support patients to control high blood pressure.
Conclusion
The study highlights the importance of integrating various aspects of care to overcome the multiple barriers to hypertension management in urban settings in low-resource countries. Participatory home visits have the potential to empower individuals and families to develop and implement feasible and acceptable actions for home management of hypertension through improved adherence to antihypertensive medication, and behaviour change.
Keywords: hypertension, public health, global health
WHAT IS ALREADY KNOWN ON THIS TOPIC
Interplay of individual, interpersonal, health system and community factors determine effective management of hypertension.
WHAT THIS STUDY ADDS
Despite availability of hypertension services poor and elderly patients had poor access.
Inadequate counselling to address wrong beliefs and misconception regarding hypertension hindered effective control of blood pressure.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
To rebuild trust in primary healthcare facilities through improved counselling skills of healthcare providers and ensuring regular supply of hypertension medication.
To support individuals and family members in self-manage hypertension while encouraging routine physician follow-up for cost-effective management of hypertension without burdening the tertiary care.
Introduction
One-third of the world’s 30–79-year aged population have hypertension (1.28 billion), and two-thirds of them live in low and middle-income countries (LMICs).1 Huge gap exists in the management of hypertension, particularly in LMICs, including Nepal. A meta-analysis of surveys from 2005 onwards reported 30% of the patients with hypertension were on treatment and 10% were able to control hypertension in LMICs.2 In Nepal, a quarter of the adult population have hypertension and only 28% were aware of their diagnosis, 11% of those diagnosed were on treatment and 4% had their blood pressure under control.3
Medication adherence, self-monitoring of blood pressure and lifestyle interventions have been effective in controlling blood pressure and reducing the incidence of cardiovascular events.4 Despite evidences on the effectiveness of lifestyle measures and antihypertensive medication, hypertension management remains challenging.5–7 Understanding of the complexity in managing hypertension demands a holistic approach considering the individual, and structural factors and how their interaction affects patient pathways.
Individual’s beliefs or perceptions such as patients’ understanding of the causes, symptoms, course of illness and effect of treatment affect adherence to behaviours related to hypertension management.8 9 Additionally, exploring the social context is important to understand patient behaviourism. Literature on behaviour change theory10 indicates that individuals and families can implement new knowledge for behaviour change when education interventions are combined with improvement in contextual factors. Despite the crucial role family has in assisting hypertension patients adhere to healthy behaviours,11 12 medication and follow-up visits13 their perspective on perceived facilitators and barriers are not sufficiently explored in urban Nepal.
Literature shows individual-level barriers such as poor knowledge about hypertension and its complications, difficulty sustaining lifestyle changes and comorbidities hinder blood pressure control.14 15 However, positive relationships with healthcare providers and family encouragement for lifestyle changes facilitate hypertension management.15 Lack of community resources for lifestyle changes and self-monitoring of blood pressure are known community-level barriers.15 Inadequate infrastructure, unaffordable medication, inadequate time and incentive for counselling and poor adherence to guidelines contribute to poor management of hypertension.16 These challenges relate to the design and the responsiveness of the health system to patient’s needs in controlling hypertension. Also, there is insufficient contextual literature from urban Nepal on strategies to reach families in supporting patients adhere to proven treatment measures for hypertension.
Therefore, in this study, we explored facilitators and barriers affecting hypertension control in urban Nepal. The individual as well as community level facilitators and barriers that interact with the health system to affect hypertension control were explored and used to inform the design and implementation of a comprehensive approach to hypertension management intervention in urban Nepal.
Research design and methods
Study design
We applied an exploratory qualitative research design using focus group discussions (FGDs) and in-depth interviews (IDIs) for data collection. Kaufman’s socioecological model17 guided the study in understanding the facilitators and barriers to different aspects of hypertension control from the perspectives of different participants, including hypertension patients, their family members, primary healthcare providers, municipal official and ward representative. The socioecological approach has previously been used in understanding factors predicting cardiovascular risks in the USA18 and behaviourism promoting physical activity and healthy eating in the United Kingdom.19 It is acknowledged to provide a thorough understanding of complex health problems guiding development of interventions to promote health.20 The consolidated criteria for reporting qualitative research checklist were followed in reporting the study findings.21
Study setting
Budhanilkantha municipality is in Kathmandu valley, the capital of Nepal, and has a population of nearly 180 000.22 It is inhabited by the locals who have been living here for several generations and those who have moved and settled from other parts of the country. The adult literacy rate (82.1%) is higher than the national average (67.1%).23 Urban areas like Budhanilkantha have one of the highest prevalences of hypertension (28.4%) in Nepal.24
Budhanilakantha municipality runs four types of primary healthcare facilities, one municipal hospital, six health posts, two urban health centres and two basic health centres. There is a wide array of private pharmacies and hospitals within the municipality and several private and public specialised hospitals nearby. The basic and the urban health centres provide counselling, blood pressure measurement, primary treatment, including medication, referral and follow-up services for hypertension. In addition to these services, health posts provide basic pathology lab services.
Participant recruitment
Hypertension patients (n=36) and family members (n=33) were purposively recruited with aims to explore facilitators and barriers to hypertension management from the individual, family and social level. Healthcare providers from government (n=8) and private (n=4) health facilities, municipal official (n=1), ward representative (n=1) were conveniently sampled for interviews to explore facilitators and barriers to hypertension management from health system perspective. To explore heterogeneity in patient and family members’ experience young and old (patients 42–89 years; family members 20–90 years), of both genders as well as individuals from different ethnicities were recruited.
We contacted and scheduled a visit to all public health facilities. During the visit, healthcare providers primarily responsible for providing hypertension care were interviewed. There are a limited number of healthcare providers in primary healthcare setting, and interviewing one from each facility was sufficient to gain understanding of healthcare delivery from that facility. We took appointments with municipal health official, and ward representative before visiting their office for interview. The healthcare providers and ward representatives were requested to link us with hypertension patients and family members. They gave us contact information of the community volunteers who helped us recruit hypertensive patients and family members from the community. The private healthcare providers were recruited from health facilities frequently mentioned by patient and family members during interviews. None of those approached refused participation. A signed informed consent was taken from the participants. The information sheet was read to the illiterate participants before taking a thumbprint.
Data collection
Two female researchers (SaB and SwB), with more than a decade, experience in qualitative research conducted the interviews and focus groups. Recruiting participants with support from healthcare providers might have encouraged participants to expect the researchers to be care providers or higher level authorities coming to monitor hypertension care provision. However, it was explained to the participants that none of the researchers was care providers or was in a position to influence health service delivery.
Data were collected between January 2022 and June 2022, using FGD and IDI guides with different groups of study participants as shown in table 1. Data were collected on a time and place chosen by the respondent.
Table 1.
Data collection techniques and participants
| Respondent type | Focus group discussions | In-depth interviews |
| Hypertension patients, n | 3 | 8 |
| Family members, n | 4 | |
| Public healthcare providers | ||
| Physician, n | 2 | |
| Paramedic, n | 4 | |
| Nurses, n | 2 | |
| Private healthcare providers | ||
| Physician, n | 1 | |
| Paramedic, n | 1 | |
| Pharmacist, n | 2 | |
| Municipal official, n | 1 | |
| Ward representative, n | 1 | |
| Total | 7 | 22 |
FGD: we planned for four FGDs with hypertension patients and family members, which are considered sufficient to achieve code saturation gaining a comprehensive understanding of a range of new issues.25 We were only able to conduct three FGDs for hypertension patients as it was challenging to collect them to one place due to distance and work priorities. For the FGDs, the participants were either invited to the health facilities or other community spaces.
IDIs: we conducted eight individual interviews with hypertension patients to supplement FGD data. Interviews with hypertension patients were conducted in their home and healthcare providers, municipal official and ward representative in their workplaces.
Kaufman socioecological model guided development of the tool and discussion with participants.17 The model held that patients’ behaviour is influenced by individual, and environmental factors and their interaction.17 FGDs and interview guides were developed by SBW with feedback on the draft from all the authors. SwB pretested the guide in a nearby municipality. Interviews and FGDs were conducted in Nepali language, lasted between 30 min and 45 min and were audio-recorded. After each FGD and interview, SaB and SwB discussed the findings noting new emerging themes and gaps in information and adjusted the guide accordingly. Examples of open-ended questions used for patients and family members: ‘What do you understand about hypertension?’, ‘What went through your mind when you/your family member—were told you had hypertension?’, ‘What factors affected in management of hypertension?’ ‘What would help you to better manage hypertension?, What support do you receive/How do you support—in controlling blood pressure?
Example questions for healthcare providers, municipal official and ward representative were: ‘How successfully is hypertension managed in the community?’, ‘What measures are taken to improve quality of hypertension services?’, ‘What community resources are available for patient to control blood pressure?’ and ‘What problem have you run into ensuring access to hypertension services?’
Data management and analysis
The audio recordings of the interviews and FGDs were transcribed verbatim. SaW and SwB both knowledgeable of the socioecological model inductively coded four transcripts (two healthcare providers’ interviews and two hypertension patients FGDs) and compared codes achieving an intercoder reliability of 82.8%. Intercoder reliability was assessed for better reflexiveness and dialogue within the research team and to ensure quality of results.26 Coding 10% of transcripts of different respondent types and an intercoder reliability higher than 80% is considered reasonable.26 The disagreement in coding was discussed and mutually agreed before finalising the codebook. Then, SwB used the final codebook to code the remaining transcripts using dedoose qualitative data analysis software. When new codes emerged during coding, they were discussed before adding them to the codebook. New codes were added four times, and every time a new code was added, previously coded transcripts were reviewed. The emerging codes were summarised into categories in relation to the (1) individual (2) interpersonal (3) health system and (4) community-level factors affecting hypertension management. Descriptive write up and main interpretations were done by SaB and shared with all the team members for discussion, validation and adjustment.
Results
The characteristics of the study participants are shown in table 2. Patients with hypertension were on average 56 years old and family members were on average 42 years old. Majority of the participants were women (64% patients and 88% family members), Newar ethnicity (28% patients and 48% family members) and homemakers (53% patients and 73% family member). Most of the patients had no formal education (56%) and 39% of family members had secondary education. Most of the patients had a family history of hypertension (47%), were currently taking antihypertensive medication (69%) and sought hypertension care from private pharmacies (64%). Most of the interviewed family members were spouses (37%) or mother-in-law (33%). Most healthcare providers were women (58%) and paramedics (42%) (data not shown). Both the municipal official and ward representative were men (data not shown).
Table 2.
Characteristics of study participants
| Characteristics | Hypertension patients | Family members | ||
| Focus group discussion (N=28) | In-depth interview (N=8) | Total (N=36) | Focus group discussion (N=33) | |
| Age mean years (±SD) | 57.8 (14.9) | 50.5 (17.0) | 56.4 (15.4) | 41.5 (12.8) |
| Age group | ||||
| <45, n (%) | 6 (21) | 4 (50) | 10 (28) | 22 (67) |
| 45–55, n (%) | 6 (21) | 2 (25) | 8 (22) | 5 (15) |
| >55, n (%) | 16 (58) | 2 (25) | 18 (50) | 6 (18) |
| Sex | ||||
| Male, n (%) | 10 (36) | 3 (37) | 13 (36) | 4 (12) |
| Female, n (%) | 18 (64) | 5 (63) | 23 (64) | 29 (88) |
| Ethnicity | ||||
| Advantaged group Brahmin/Chettri, n (%) | 6 (21) | 3 (37) | 9 (25) | 4 (12) |
| Newar (traditionally engaged in trading), n (%) | 9 (32) | 1 (13) | 10 (28) | 12 (37) |
| Indigenous (Tamang/ Magar/Gurung), n (%) | 8 (29) | 4 (50) | 12 (33) | 16 (48) |
| Disadvantages group (Dalits), n (%) | 5 (18) | 0 (0) | 5 (14) | 1 (3) |
| Education | ||||
| No education, n (%) | 19 (68) | 1 (13) | 20 (56) | 5 (15) |
| Primary, n (%) | 2 (7) | 1 (13) | 3 (8) | 7 (21) |
| Secondary, n (%) | 3 (11) | 2 (26) | 5 (14) | 13 (39) |
| High school and above, n (%) | 4 (14) | 4 (52) | 8 (22) | 8 (24) |
| Occupation | ||||
| Farming, n (%) | 1 (4) | 1 (13) | 2 (6) | 1 (3) |
| Formal employment, n (%) | 2 (7) | 1 (13) | 3 (8) | 1 (3) |
| Homemaker, n (%) | 15 (53) | 4 (52) | 19 (53) | 23 (73) |
| Business, n (%) | 3 (10) | 1 (13) | 4 (11) | 2 (6) |
| Retired, n (%) | 1 (4) | 1 (13) | 2 (6) | 2 (6) |
| Unemployed, n (%) | 5 (18) | 0 (0) | 5 (13) | 2 (6) |
| Unskilled labour (physical labour), n (%) | 1 (4) | 0 (0) | 1 (3) | 1 (3) |
| Place for seeking hypertension care | ||||
| Government health facility, n (%) | 4 (14) | 0 (0) | 4 (11) | |
| Private pharmacy, n (%) | 17 (60) | 6 (75) | 23 (64) | |
| Private hospital, n (%) | 7 (26) | 2 (25) | 9 (25) | |
| Family history of hypertension | ||||
| Yes, n (%) | 17 (60) | 0 (0) | 17 (47) | |
| No, n (%) | 11 (40) | 8 (100) | 19 (53) | |
| Currently taking medication | ||||
| Yes, n (%) | 19 (68) | 6 (75) | 25 (69) | |
| No, n (%) | 9 (32) | 2 (25) | 11 (31) | |
| Relationship with patients | ||||
| Spouse, n (%) | 12 (37) | |||
| Father, n (%) | 2 (6) | |||
| Mother, n (%) | 4 (12) | |||
| Father-in-law, n (%) | 2 (6) | |||
| Mother -in-law, n (%) | 11 (33) | |||
| Others, n (%) | 2 (6) | |||
Facilitators and barriers to hypertension management
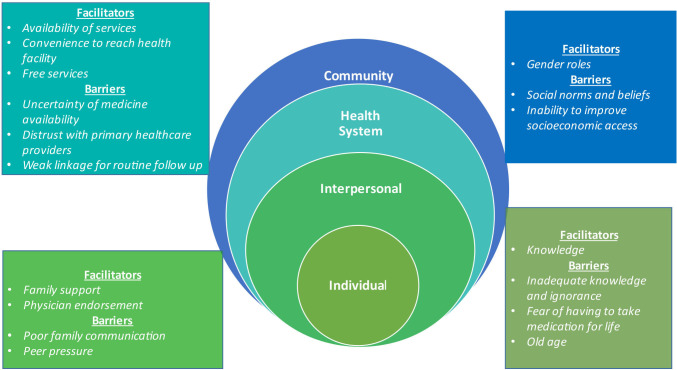
The barriers and facilitators to hypertension management were synthesised triangulating the perspectives of the hypertension patients, their family members, healthcare providers and municipal representatives. Figure 1 summarises the facilitators and barriers at individual, interpersonal, health system and the community level that emerged from the data. Knowledge was both a facilitator and a barrier, patients having knowledge adopted healthy behaviour, whereas patients with inadequate knowledge had poor adherence to antihypertensive medication. Inadequate knowledge also augmented social norms and beliefs regarding treatment measures affecting blood pressure control. Family support facilitated hypertension management, but its facilitating role varied with the level of interactions between family members.
Figure 1.
Multi-level facilitators and barriers to hypertension control.
Facilitators to hypertension management
Individual-level facilitator
Knowledge
When patients and family members were aware of the risk factors and hypertension control measures, they reported to adopt healthy behaviours. Drinking alcohol and eating a lot of oily food affects our blood pressure… we should limit what we eat—an 89-year-old male patient.
My mum (hypertension patient) preferred home remedies…eating bitter gourd to control blood pressure, but when she learned taking one medicine does good … she has been taking medication regularly for four years—an FGD family members
Interpersonal-level facilitators
Family support
Patients who had family support had better adaptation of blood pressure reduction measures. For example, families encouraged healthy diet and modified cooking practices to adapt with the necessary dietary modification required for the hypertension patients. They (family members) keep telling me you shouldn’t eat this and that,…. don’t eat oily and fried food—a 43 years male patient.
We have reduced the amount of salt when cooking food—an FGD family member
Physician endorsement
Primary healthcare providers expressed hypertension patients came for follow-up care when their competence is validated by physicians in tertiary hospitals. Sometimes they (patients) come back (for follow up) and tell us doctors in hospital told them we (primary healthcare provider) saved their life by referring them on time to hospital—a public healthcare provider.
Health system-level facilitators
Availability of services
Availability of multiple services including physician consultant, medication titering and laboratory facilities in the same health facility was a major facilitator as it saved patients and family members time in seeking hypertension care.
Convenience to reach health facility
Proximity and convenient opening hours facilitated patients to go for routine blood pressure monitoring. I would go to a private pharmacy nearby, the public health facility opens late and closes early—43-year old male patient. Convenience was particularly important for older patients with mobility problems. … as long as mum (patient) is able to walk, we go to the pharmacy nearby—an FGD family member.
Free services
Most healthcare providers reported that provision of free blood pressure monitoring, counselling and antihypertensive medication encourages patients to use service from public primary healthcare, particularly among poor and elderly patients. Those from low socioeconomic status… elderly who have no children to take them to hospitals, and those who don’t have money to buy medicine come here (pubic primary healthcare facility)—a public healthcare provider.
Community-level facilitator
Gender roles
Incorporating healthy behaviour into their daily routine was easier for men than women because men in Nepali society have lower responsibility for household chores and hence have more time for leisure. Furthermore, it is also more culturally acceptable for men to do physical activity. Our father gets up in the morning, he is careful about what he eats… he goes for walks—an FGD family member. Particularly, the men who are retired followed healthy behaviour because not having a daily job provides them time to focus on their health. I have reached a certain age now, so I go for a walk in the morning, do not take much stress and eat less oily and salty food to balance the pressure—a male FGD patient. In contrast Nepali women have responsibilities of household chores, resulting in less or no time and have social restriction for mobility. I don’t exercise… I don’t have time…. I am busy… go there, do that, just like that—a female FGD patient.
Barriers for hypertension management
Individual-level barriers
Inadequate knowledge and ignorance
Ignorance about hypertension and its management can delay seeking care and adopting control measures. Many admitted that they do not regularly check their blood pressure because of not having symptoms. When I have headaches, feel dizzy and have breathing difficulty… I go to a private pharmacy to check my blood pressure—45 years female patient. Some patients who are on antihypertensive medication thought that they could stop medication after following a healthy lifestyle. I used to take antihypertensive medication when I had headaches. After one year I discontinued and began doing exercise—an FGD patien. While patients had the perception that antihypertensive medication alone was sufficient to control high blood pressure. Hypertension patients drink alcohol, eat oily food alongside medicine. They believe nothing is needed when you are taking medicines—an FGD patient. Some healthcare providers expressed that their patients ignored high blood pressure because they do not understand its consequences. It is very difficult to make them understand……we ask them to go to see a doctor they ignore—a private healthcare provider. Some patients reported that they delayed treatment believing high blood pressure to be fleeting and can be reduced easily through dietary adjustment. I didn’t take medicine, because I thought that I could just stop drinking coffee and salty packaged food…—42-year female patient.
Fear of having to take medication for life
Most patients and family members delayed initiating antihypertensive medication fearing having to take medication for life. When the doctor told us to start medication and that it must be taken every day (for life), we were scared…—an FGD family member. Patients considered medicines to be harmful and taking it everyday a nuisance. We don’t want to take medicine, after all medicines are chemicals … I feel our body should not be exposed to harmful chemicals ….also I forget taking medicine because…. I don’t want to take it, but I guess I need to start taking it as there is no other way—a 44-year female patient. Also, patients with low knowledge on benefits of taking medication had interrupted medication adherence. I didn’t want medication,…but started again after three years and left once more …. I didn’t think medication is necessary—an FGD patient. Even after multiple encounters with healthcare providers fear of medication remained affecting optimal medication adherence. She (hypertension patient) has high blood pressure for many years … she usually maintains her diet…. but takes hypertension medicine when she has headaches that are intolerable—an FGD family member
Old age
Some older patients refrained physical exercise fearing it to be too arduous. he sometimes goes for walk ……but he fears his body and knees will not cope excercise—an FGD family member
Interpersonal-level barriers
Poor family communication
Poor communication within family regarding hypertension and adherence status negatively affected medication adherence because family members would not know medicine ran out or reminded patients to take medication. It has been 3 weeks since I stopped taking medication but no one in my family knows, if they know they will scold me—44 years female patient. Poor communication also made it difficult to do the necessary dietary adjustments. I have high (blood pressure), my wife has low, it is difficult to balance (diet) so we don’t bring it up…—an FGD patient.
Peer pressure
Peer pressure to drink alcohol and unhealthy food during gatherings often demotivated hypertension patients to follow healthier lifestyle. Drinking and eating happens,…. when friends coax us. They say if you drink a little or eat just for one day…. nothing will happen—an FGD patient.
Health system-level barriers
Uncertainty of medicine availability
Gaps in antihypertensive medication at the primary healthcare facilities delayed treatment of hypertension patients. Many patients did not go to public facilities because they think that antihypertensive medication is not available. do they (public health facilities) give hypertension medication?….if we had known we would definitely go there—an FGD family member. Some patients do not go for refill because of their previous experience of not being able to receive medication.
Distrust with primary healthcare providers
Primary healthcare providers expressed that the services were underutilised because patients and family members’ do not trust on their competency. People in the community think we know nothing,… they want to consult with a heart specialist—a public healthcare provider. Lack of trust often arise because of irregular supply of antihypertensive medication at the health facility when they come for refill. Patients reported the lack of trust due to poor behaviour of primary healthcare providers and through that they compromise with the quality of hypertension services. They (public primary healthcare providers) were not keen on providing services…. ignored my mother (patient) I got angry and shouted at them—an FGD family member.
Weak linkage for routine follow-up
The ward representative expressed that patients were lost to follow-up at the primary level care because they did not receive proper counselling in hospitals. Patients don’t come to health centres…due to the high volume of patients, doctors in hospitals do not have sufficient time to explain treatment options and follow up care—the ward representative. Only on rare occasions, hypertension patients with ongoing relationships with primary healthcare providers returned for counselling, follow-up care and medication.
Community-level barriers
Social norms and beliefs
Family members believed that inclination towards socially accepted norms and beliefs regarding home remedies (eg, eating bitter gourd) to control blood pressure interfered with hypertension treatment. He (hypertension patient) ate boiled bitter gourd, or anything bitter, …bitter food to reduce blood pressure level at first …it didn’t work so started medication—an FGD family member. An elderly patient expressed that the lifestyle modification required unattainable self-discipline. If people are … religious and spiritual like ‘saints’,…. having a lot of self-control… then blood pressure would be under control—89-year-old male patient. Such fatalistic notion deter patients from even initiating behaviour change.
Inability to improve socioeconomic access
As expected, poor and elderly patients with comorbid conditions had poorer access to medication. When you have both diabetes and hypertension, it is very difficult, medicines are so expensive most of us can’t afford to buy them—FGD family members. Though government provides some funds to underprivileged, healthcare providers have difficulty recommending patients due to absence of a well-defined process to identify the poor (eligible). We are unable to support them (poor) because we are not from this community; we don't know whose economic condition is what—a public healthcare provider.
Discussion
Several barriers and facilitators affecting hypertension management in urban Nepal were explored to inform the implementation of comprehensive approaches to hypertension management intervention. The major facilitators were, knowledge about risk factors and control measures motivating patients to adopt healthy lifestyle at individual level, family support at interpersonal level, availability of hypertension services at health system level and gender role enabling men to adopt healthy lifestyles at community level. Several important barriers were identified such as inadequate knowledge affecting medication adherence at individual level, peer pressure and poor family communication at interpersonal level, distrust in primary healthcare providers at the health system level and misconceptions regarding treatment at the community level. These findings have implications for future community interventions seeking to engage patients and families for hypertension control in Nepal and in similar LMICs, and we discuss these below.
We found that the individuals with adequate knowledge on hypertension were motivated to adopt healthy lifestyles and adhere to medication, which is also reported by previous studies from Nepal27 28 and LMICs.29–33 Consistent with findings from previous studies, motivation to adopt healthy lifestyles waned after starting medication in part due to insufficient knowledge about treatment measures.27 30 31 34 Patients and families could benefit from understanding the value of antihypertensive medication, and medication in tandem with lifestyle measures giving the best health benefit. Receiving information is insufficient to adopt healthy behaviours for blood pressure control.35 36 Paulo Freire’s empowering education approach37 engaging families over a period of time to critically analyse problems and its causes to develop and implement prioritised behavioural actions have been successful in managing chronic conditions.38
Intersections of age, gender and income affect patients’ ability to manage hypertension.39 We found that elderly patients refrained from physical activity equating it to vigorous exercise, while female patients were unable to allocate time. In Nepal, women are primarily responsible for unpaid housework (cooking, cleaning, washing, shopping) spending on average 268 min per day in comparison to 56 min per day spent by men.40 Tailoring physical activity to patient capacity may boost confidence in incorporating physical activity to control blood pressure.41
Adherence to antihypertensive medication is one of the keys to effective management of hypertension.42–44 Non-adherence to antihypertensive medication increases the risk of complications such as cardiovascular diseases (heart failure, myocardial infarction and stroke), which are increasing in Nepal.45 The cultural belief that medicines are mainly for curing severe diseases and not for reducing high blood pressure, an asymptomatic condition46 has created delays in initiation and discontinuation among those who initiated in our study.
A strong belief in home remedies such as eating bitter food to reduce blood pressure delayed or caused discontinuation of medication. Previous studies have also reported preference for home remedies to manage hypertension and other chronic conditions in Nepal27 28 and LMIC.31 32 47 Preference for home remedies is due to their easy availability, perceived safety and endorsement from family and friends.27 Misconception found in our study may be due to the high proportion of illiterate patient participants. Illiterates usually have poor access to information and knowledge,48 impending timely treatment and control of hypertension and its complications.29 Increased knowledge on the benefits of medication could counteract the negative consequences of misconception.
Our study found patients receiving family support were able to adopt healthy lifestyles. Family support in ensuring recommended diet was also reported in a previous study from India.49 It is an important factor for patients’ blood pressure control.32 Improved interaction and providing authentic information to patients and family could enhance hypertension control. For example, family reminding patients to take medicine is known to improve adherence in South Asian countries.34 However, the changing attitudes towards elderly and declining intergenerational support in Nepal50 highlight further research on family’s role in providing hypertension care. Also, families may be forced to prioritise the needs of breadwinners as opposed to elderly.51 The adult children and spouses as caregivers can be key stakeholders in the intervention, and they can play an active role in helping patients in monitoring blood pressure and adhering to medication and healthy behaviours.
The health system’s inability to identify poor obstructed socioeconomic access to hypertension care. Poor patients may not have the financial resources to seek care and medicines.52 53 Reliable estimates of poverty are the basis for inclusive healthcare. Also consistent with previous studies from LMIC,34 54 55 patients distrusted the competency of primary healthcare providers. When patients doubt the quality of healthcare, they self-refer overcrowding the tertiary care.56 The cost of travel and high fees at the tertiary care burden patients from low socioeconomic status.56 Studies from Nepal have shown patient discontinue treatment due to high cost of medicine and diagnostic tests.27 Hypertension services in the public primary healthcare facilities are free, therefore ensuring uninterrupted supply of antihypertensive medication, and training healthcare providers on treatment protocols can improve access. Trained primary healthcare providers can personalise counselling based on patients’ blood pressure measurements,43 and regular positive interaction can help instate trust in the primary-level care.
Positive patient–provider interactions are important for hypertension management.57 Our study identified poor patient counselling negatively affected patient follow-up. The high volume of patients in LMIC health centres is not conducive for positive patient–provider interaction35 in lack of healthcare provider time and space. Patients not receiving counselling are likely to be non-adherent to treatment and routine follow-up.28 29 35 36 In Nepal, the female community health volunteers have traditionally channelled health information to the community.58 Female community health volunteers may find participatory discussion difficult to implement,59 but there is a possibility to leverage on the existing approach to bridge patient–provider communication gap by recruiting trained nurses for a comprehensive approach to hypertension management. Flexible and tailored approaches considering individuals’ and family context are important when developing and implementing hypertension intervention.
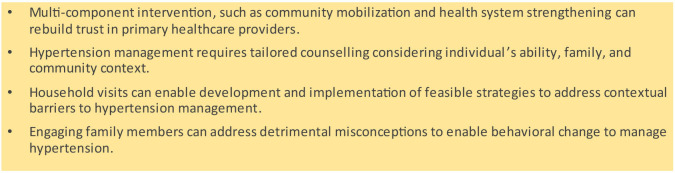
Our results provide insights which can be applied globally. Research from other LMICs also show that adequate knowledge on hypertension services motivates patients to adopt treatment measures,30–33 and that addressing misconceptions29 46 and continued family support34 49 contribute to sustained behavioural changes. Rebuilding trust in primary healthcare providers34 49 55 is critical to ensure access to services for marginalised communities.56 Figure 2 highlights the recommendations drawn from our findings to guide future implementation of similar interventions in LMICs.
Figure 2.
Overcoming barriers to hypertension control—future perspective.
Strengths and limitations
The study’s main strength was collecting the perspectives of different stakeholders: hypertension patients, family members, private and public healthcare providers and municipal and ward officials to gain a comprehensive understanding of hypertension management in the community. Mixing different methods of data collection provided opportunities for clarification and triangulation of findings. The iterative process in data collection to achieve code saturation to gain comprehensive understanding of a range of new issues is expected to provide better internal validity. All focus groups and interviews were conducted by the authors (SaB and SwB) from similar cultural backgrounds as the participants. There were some limitations too. The heterogeneous (various socioeconomic background) sampling prevented us from understanding the intersection between evolving family roles, social class, gender, ethnicity, but we expect the participatory discussion during the intervention will allow further exploration. The findings are from a sample within one municipality and may not be generalisable to rural Nepal. Nevertheless, findings can be relevant for urban municipalities in similar low resource settings hoping to successfully manage hypertension.
Conclusion
Our study revealed the complexity of managing hypertension in urban Nepal. Inadequate knowledge and misconception on hypertension and medication affected adherence to treatment measures. Empowering families with knowledge on hypertension and its management was vital to optimise family support in home management of hypertension. The findings were and can be used in designing and implementing interventions to overcome the individual, interpersonal, health system and community barriers in managing hypertension.
Patient and public involvement
Participating hypertension patients, their family members, healthcare providers and municipal representatives were informed about the objective of the study and its implication. However, they were not directly involved in developing research questions and study design. The results of this study were discussed with the municipal representatives when developing the home visit manual.
Footnotes
Contributors: SwB developed the tools, collected and analysed data and drafted the manuscript. SB supported in data collection and analysis. ArS, AbS and BPM reviewed and provided feedback to the preliminary findings and structure of the manuscript. AS, BPM, BOÅ, ES and AbS provided feedback on the tools and the draft manuscript. All authors approved the final manuscript. SwB is the guarantor.
Funding: This work was supported by Norwegian University of Science and Technology, Trondheim, Norway (Project number 981023100).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request. Data cannot be shared publicly for ethical reasons but are available on reasonable request to Sanju Bhattarai and Dr. Sen.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The study was approved by the Nepal Health Research Council (682/2021) and the Regional Committee for Medical and Health Research Ethics, Norwegian University of Science and Technology (Approval number: 3999476). Participants gave informed consent to participate in the study before taking part.
References
- 1. Zhou B, Carrillo-Larco RM, Danaei G, et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 2021;398:957–80. 10.1016/S0140-6736(21)01330-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Geldsetzer P, Manne-Goehler J, Marcus M-E, et al. The state of hypertension care in 44 low-income and middle-income countries: a cross-sectional study of nationally representative individual-level data from 1·1 million adults. Lancet 2019;394:652–62. 10.1016/S0140-6736(19)30955-9 [DOI] [PubMed] [Google Scholar]
- 3. Dhimal M, Bista B, Bhattarai S, et al. Report of non communicable disease risk factors: STEPS survey Nepal 2019. Nepal Health Research Council, Kathmandu 2020. Available: https://nhrc.gov.np/wp-content/uploads/2020/04/NEPAL%E2%80%93Noncommunicable-disease-risk-factors-STEPS-Survey-2019-%E2%80%93-Tobacco-Factsheet.pdf [Google Scholar]
- 4. Carey RM, Wright JT, Taler SJ, et al. Taler SJ et al guideline-driven management of hypertension: an evidence-based update. Circ Res 2021;128:827–46. 10.1161/CIRCRESAHA.121.318083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Weingarten SR, Henning JM, Badamgarav E, et al. Interventions used in disease management programmes for patients with chronic illness---which ones work? meta-analysis of published reports. BMJ 2002;325:925. 10.1136/bmj.325.7370.925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Svetkey LP, Pollak KI, Yancy WS, et al. Hypertension improvement project: randomized trial of quality improvement for physicians and lifestyle modification for patients. Hypertension 2009;54:1226–33. 10.1161/HYPERTENSIONAHA.109.134874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. World Health Organization . Global action plan for the prevention and control of Noncommunicable diseases 2013-2020. WHO 2013. Available: https://www.who.int/publications/i/item/9789241506236 [Google Scholar]
- 8. Bosworth HB, Olsen MK, Neary A, et al. Take control of your blood pressure (TCYB) study: a multifactorial tailored behavioral and educational intervention for achieving blood pressure control. Patient Educ Couns 2008;70:338–47. 10.1016/j.pec.2007.11.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kressin NR, Wang F, Long J, et al. Hypertensive patients’ race, health beliefs, process of care, and medication adherence. J Gen Intern Med 2007;22:768–74. 10.1007/s11606-007-0165-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Briscoe C, Aboud F. Behaviour change communication targeting four health behaviours in developing countries: a review of change techniques. Social Science & Medicine 2012;75:612–21. 10.1016/j.socscimed.2012.03.016 [DOI] [PubMed] [Google Scholar]
- 11. Park E-W, Tudiver F, Schultz JK, et al. Does enhancing partner support and interaction improve smoking cessation? A meta-analysis. Ann Fam Med 2004;2:170–4. 10.1370/afm.64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chandola T, Head J, Bartley M. Socio-demographic predictors of quitting smoking: how important are household factors Addiction 2004;99:770–7. 10.1111/j.1360-0443.2004.00756.x [DOI] [PubMed] [Google Scholar]
- 13. DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol 2004;23:207–18. 10.1037/0278-6133.23.2.207 [DOI] [PubMed] [Google Scholar]
- 14. Shrestha S, Shrestha A, Koju RP, et al. Barriers and facilitators to treatment among patients with newly diagnosed hypertension in Nepal. Heart Asia 2018;10:e011047. 10.1136/heartasia-2018-011047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Flynn SJ, Ameling JM, Hill-Briggs F, et al. Facilitators and barriers to hypertension self-management in urban African Americans: perspectives of patients and family members. Patient Prefer Adherence 2013;7:741–9. 10.2147/PPA.S46517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rawal LB, Kharel C, Yadav UN, et al. Community health workers for non-communicable disease prevention and control in Nepal: a qualitative study.BMJ open. BMJ Open 2020;10:e040350. 10.1136/bmjopen-2020-040350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kaufman MR, Cornish F, Zimmerman RS, et al. Health behavior change models for HIV prevention and AIDS care. JAIDS 2014;66:S250–8. 10.1097/QAI.0000000000000236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Balcázar H, Wise S, Rosenthal EL, et al. An ecological model using Promotores de Salud to prevent cardiovascular disease on the US-Mexico border: the HEART project. Prev Chronic Dis 2012;9:E35. 10.5888/pcd9.110100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cochrane T, Davey RC. Increasing uptake of physical activity: a social ecological approach. J R Soc Promot Health 2008;128:31–40. 10.1177/1466424007085223 [DOI] [PubMed] [Google Scholar]
- 20. Richard L, Gauvin L, Raine K. Ecological models revisited: their uses and evolution in health promotion over two decades. Annu Rev Public Health 2011;32:307–26. 10.1146/annurev-publhealth-031210-101141 [DOI] [PubMed] [Google Scholar]
- 21. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349–57. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 22. Central Bureau of Statistics . Preliminary Report of National Population 2021, Central Bureau of Statistics, Government of Nepal, Kathmandu Nepal. 2021. Available: https://censusnepal.cbs.gov.np/Home/Details?tpid=5&dcid=3479c092-7749-4ba6-9369-%2045486cd67f30&tfsid=17
- 23. Karki M. Budhanilakantha municipality profile. 2019. Available: https://www.nepalarchives.com/content/budhanilkantha-municipality-kathmandu-profile/#:~:text=Top%20five%20castes%20of%20people,of%20107%2C918%20in%20Budhanilkantha%20Municipality
- 24. Huang Y, Guo P, Karmacharya BM, et al. Prevalence of hypertension and prehypertension in Nepal: a systematic review and meta-analysis. Glob Health Res Policy 2019;4:11. 10.1186/s41256-019-0102-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hennink MM, Kaiser BN, Weber MB. What influences saturation? estimating sample sizes in focus group research. Qual Health Res 2019;29:1483–96. 10.1177/1049732318821692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. O’Connor C, Joffe H. Intercoder reliability in qualitative research: debates and practical guidelines. Int J Qualit Method 2020;19:160940691989922. 10.1177/1609406919899220 [DOI] [Google Scholar]
- 27. Bhandari B, Narasimhan P, Vaidya A, et al. Barriers and facilitators for treatment and control of high blood pressure among hypertensive patients in Kathmandu, Nepal: a qualitative study informed by com-B model of behavior change. BMC Public Health 2021;21:1524. 10.1186/s12889-021-11548-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Devkota S, Dhungana RR, Pandey AR, et al. Barriers to treatment and control of hypertension among hypertensive participants: a community-based cross-sectional mixed method study in municipalities of Kathmandu. Front Cardiovasc Med 2016;3:26. 10.3389/fcvm.2016.00026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Khatib R, Schwalm J-D, Yusuf S, et al. Patient and healthcare provider barriers to hypertension awareness, treatment and follow up: a systematic review and meta-analysis of qualitative and quantitative studies. PLoS One 2014;9:e84238. 10.1371/journal.pone.0084238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ukoha-Kalu BO, Adibe MO, Ukwe CV. A qualitative study of patients’ and Carers’ perspectives on factors influencing access to hypertension care and compliance with treatment in Nigeria. J Hypertens 2023;41:845–51. 10.1097/HJH.0000000000003409 [DOI] [PubMed] [Google Scholar]
- 31. Gebrezgi MT, Trepka MJ, Kidane EA. Barriers to and facilitators of hypertension management in Asmara, Eritrea: patients' perspectives. J Health Popul Nutr 2017;36:11. 10.1186/s41043-017-0090-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Legido-Quigley H, Camacho Lopez PA, Balabanova D, et al. Patients’ knowledge, attitudes, behaviour and health care experiences on the prevention, detection, management and control of hypertension in Colombia: a qualitative study. PLOS ONE 2015;10:e0122112. 10.1371/journal.pone.0122112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Abaynew Y, Hussien M. A qualitative study on barriers to treatment and control of hypertension among patients at Dessie referral hospital, northeast Ethiopia, Ethiopia: healthcare workers’ perspective. Integr Blood Press Control 2021;14:173–8. 10.2147/IBPC.S339773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Legido-Quigley H, Naheed A, de Silva HA, et al. Patients' experiences on accessing health care services for management of hypertension in rural Bangladesh, Pakistan and Sri Lanka: a qualitative study. PLoS One 2019;14:e0211100. 10.1371/journal.pone.0211100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Perera M, de Silva CK, Tavajoh S, et al. Patient perspectives on hypertension management in health system of Sri Lanka: a qualitative study. BMJ Open 2019;9:e031773. 10.1136/bmjopen-2019-031773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kebede T, Taddese Z, Girma A. Knowledge, attitude and practices of lifestyle modification and associated factors among hypertensive patients on-treatment follow up at Yekatit 12 general hospital in the largest city of East Africa: a prospective cross-sectional study. PLoS One 2022;17:e0262780. 10.1371/journal.pone.0262780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Wallerstein N. Empowerment and health: the theory and practice of community change. Community Dev J 1993;28:218–27. 10.1093/cdj/28.3.218 [DOI] [Google Scholar]
- 38. Pires M, Shaha S, King C, et al. Equity impact of participatory learning and action community mobilisation and mHealth interventions to prevent and control type 2 diabetes and intermediate hyperglycaemia in rural Bangladesh: analysis of a cluster randomised controlled trial. J Epidemiol Community Health 2022;76:586–94. 10.1136/jech-2021-217293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Liew SJ, Lee JT, Tan CS, et al. Sociodemographic factors in relation to hypertension prevalence, awareness, treatment and control in a multi-ethnic Asian population: a cross-sectional study. BMJ Open 2019;9:e025869. 10.1136/bmjopen-2018-025869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Budlender D, Moussie R. Making care visible: women’s unpaid care work in Nepal, Nigeria, Uganda and Kenya. 2013. Available: https://actionaid.ie/wp-content/uploads/2016/10/Making-Care-Visible.pdf
- 41. Bytyci Katanolli A, Probst-Hensch N, Ann Obas K, et al. Perceived barriers to physical activity behaviour among patients with diabetes and hypertension in Kosovo: a qualitative study. BMC Prim Care 2022;23:257. 10.1186/s12875-022-01866-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. van der Laan DM, Elders PJM, Boons CCLM, et al. Factors associated with antihypertensive medication non-adherence: a systematic review. J Hum Hypertens 2017;31:687–94. 10.1038/jhh.2017.48 [DOI] [PubMed] [Google Scholar]
- 43. Asgedom SW, Atey TM, Desse TA. Antihypertensive medication adherence and associated factors among adult hypertensive patients at Jimma University specialized hospital, Southwest Ethiopia. BMC Res Notes 2018;11:27. 10.1186/s13104-018-3139-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Nielsen JØ, Shrestha AD, Neupane D, et al. Non-adherence to anti-hypertensive medication in Low- and middle-income countries: a systematic review and meta-analysis of 92443 subjects. J Hum Hypertens 2017;31:14–21. 10.1038/jhh.2016.31 [DOI] [PubMed] [Google Scholar]
- 45. Kibria GMA, Swasey K, Kc A, et al. Estimated change in prevalence of hypertension in Nepal following application of the 2017 ACC/AHA guideline. JAMA Netw Open 2018;1:e180606. 10.1001/jamanetworkopen.2018.0606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Rahman ARA, Wang J-G, Kwong GMY, et al. Perception of hypertension management by patients and doctors in Asia: potential to improve blood pressure control. Asia Pac Fam Med 2015;14:2. 10.1186/s12930-015-0018-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hill MN, Sutton BS. Barriers to hypertension care and control. Curr Hypertens Rep 2000;2:445–50. 10.1007/s11906-000-0026-y [DOI] [PubMed] [Google Scholar]
- 48. Mohd Isa D, Shahar S, He FJ, et al. Associations of health literacy with blood pressure and dietary salt intake among adults: a systematic review. Nutrients 2021;13:4534. 10.3390/nu13124534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Chacko S, Jeemon P. Role of family support and self-care practices in blood pressure control in individuals with hypertension: results from a cross-sectional study in Kollam district, Kerala. Wellcome Open Res 2020;5:180. 10.12688/wellcomeopenres.16146.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Speck S, Müller-Böker U. Population ageing and family change: older people’s perceptions of current changes in family composition in rural Nepal. Ebhr 2020:7–37. 10.4000/ebhr.234 [DOI] [Google Scholar]
- 51. Schulz R, Beach SR, Czaja SJ, et al. Family caregiving for older adults. Annu Rev Psychol 2020;71:635–59. 10.1146/annurev-psych-010419-050754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Harrison MA, Marfo AFA, Opare-Addo MNA, et al. Anti-hypertensive medication access and affordability and their association with blood pressure control at a teaching hospital in Ghana. Pan Afr Med J 2021;39:184. 10.11604/pamj.2021.39.184.27977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Zack RM, Irema K, Kazonda P, et al. Determinants of high blood pressure and barriers to diagnosis and treatment in Dar es Salaam, Tanzania. J Hypertens (Los Angel) 2016;34:2353–64. 10.1097/HJH.0000000000001117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Kabir A, Karim MN, Billah B. Health system challenges and opportunities in organizing non-communicable diseases services delivery at primary Healthcare level in Bangladesh: a qualitative study. Front Public Health 2022;10:1015245. 10.3389/fpubh.2022.1015245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Hort K, Gilbert K, Basnayaka P, et al. POLICY BRIEF strategies to strengthen referral from primary care to secondary care in low-and middle-income countries. World Health Organization Regional Office for South-East Asia 2019. Available: http://apps.who.int/iris/ [Google Scholar]
- 56. Chakraborty S, Rai RK, Biswas AK, et al. Health care seeking behaviour and financial protection of patients with hypertension: a cross-sectional study in rural West Bengal, India. PLoS One 2022;17:e0264314. 10.1371/journal.pone.0264314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Tavakoly Sany SB, Behzhad F, Ferns G, et al. Communication skills training for physicians improves health literacy and medical outcomes among patients with hypertension: a randomized controlled trial. BMC Health Serv Res 2020;20:60. 10.1186/s12913-020-4901-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Neupane D, McLachlan CS, Christensen B, et al. Community-based intervention for blood pressure reduction in Nepal (COBIN trial): study protocol for a cluster-randomized controlled trial. Trials 2016;17:292. 10.1186/s13063-016-1412-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Morrison J, Tumbahangphe K, Sen A, et al. Health management committee strengthening and community mobilisation through women’s groups to improve trained health worker attendance at birth in rural Nepal: a cluster randomised controlled trial. BMC Pregnancy Childbirth 2020;20:268. 10.1186/s12884-020-02960-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request. Data cannot be shared publicly for ethical reasons but are available on reasonable request to Sanju Bhattarai and Dr. Sen.