Abstract
Background
Gastric-cancer is a heterogeneous type of neoplastic disease and it lacks appropriate therapeutic options. There is an urgent need for the development of innovative pharmacological strategies, particularly in consideration of the potential stratified/personalized treatment of this tumor. All-Trans Retinoic-acid (ATRA) is one of the active metabolites of vitamin-A. This natural compound is the first example of clinically approved cyto-differentiating agent, being used in the treatment of acute promyelocytic leukemia. ATRA may have significant therapeutic potential also in the context of solid tumors, including gastric-cancer. The present study provides pre-clinical evidence supporting the use of ATRA in the treatment of gastric-cancer using high-throughput approaches.
Methods
We evaluated the anti-proliferative action of ATRA in 27 gastric-cancer cell-lines and tissue-slice cultures from 13 gastric-cancer patients. We performed RNA-sequencing studies in 13 cell-lines exposed to ATRA. We used these and the gastric-cancer RNA-sequencing data of the TCGA/CCLE datasets to conduct multiple computational analyses.
Results
Profiling of our large panel of gastric-cancer cell-lines for their quantitative response to the anti-proliferative effects of ATRA indicate that approximately half of the cell-lines are characterized by sensitivity to the retinoid. The constitutive transcriptomic profiles of these cell-lines permitted the construction of a model consisting of 42 genes, whose expression correlates with ATRA-sensitivity. The model predicts that 45% of the TCGA gastric-cancers are sensitive to ATRA. RNA-sequencing studies performed in retinoid-treated gastric-cancer cell-lines provide insights into the gene-networks underlying ATRA anti-tumor activity. In addition, our data demonstrate that ATRA exerts significant immune-modulatory effects, which seem to be largely controlled by IRF1 up-regulation. Finally, we provide evidence of a feed-back loop between IRF1 and DHRS3, another gene which is up-regulated by ATRA.
Conclusions
ATRA is endowed with significant therapeutic potential in the stratified/personalized treatment gastric-cancer. Our data represent the fundaments for the design of clinical trials focusing on the use of ATRA in the personalized treatment of this heterogeneous tumor. Our gene-expression model will permit the development of a predictive tool for the selection of ATRA-sensitive gastric-cancer patients. The immune-regulatory responses activated by ATRA suggest that the retinoid and immune-checkpoint inhibitors constitute rational combinations for the management of gastric-cancer.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13046-023-02869-w.
Keywords: All-trans-retinoic-acid, Immune-responses, Gastric-cancer, IRF1, RNA-sequencing
Background
Gastric-cancer is a heterogeneous neoplasia and one of the leading causes of tumor mortality worldwide [1, 2]. The frequency of stomach tumors is higher in the male than the female population (2/3 of the cases). The traditional classification of gastric-cancer defines 3 sub-groups, “Intestinal”, “Diffuse” and “Mixed” [3]. In addition, this tumor classifies into different sub-types according to the clinical-stage, histo-pathological features and mutational/trascriptomic profiles [4–7]. A recently developed gene-expression fingerprint gathers gastric-cancers into the Genomic-intestinal (G-INT) and Genomic-diffuse (G-DIFF) sub-groups [8]. Gastric-cancer lacks significant treatment options and innovative pharmacological strategies are needed [9], particularly in the context of the stratified/personalized treatment of this neoplastic disease.
All-Trans Retinoic-acid (ATRA) is the active metabolite of vitamin-A and it is the first example of clinically approved cyto-differentiating agent, being used in Acute-Promyelocytic-Leukemia (APL) [10]. ATRA-based therapeutic strategies induce long-lasting remissions in approximately 80% of the APL cases [11, 12]. This has stirred enthusiasm on the use of ATRA for the treatment of solid tumors, including gastric-cancer. Indeed, recent studies indicate that ATRA exerts significant anti-tumor effects in breast-cancer [13–16].
Here, we provide pre-clinical evidence on the anti-tumor effects exerted by ATRA in gastric-cancer, using multiple cell-lines, short-term tumor-tissue cultures and mouse xenografts. In addition, we generate a gene-expression model based on 42 genes, which predicts gastric-cancer responsiveness to ATRA. The RNA-sequencing (RNA-seq) studies performed in ATRA-treated cell-lines provide insights into the gene-networks underlying the action of the retinoid. In particular, we demonstrate that ATRA up-regulates IRF1 and DHRS3, two genes whose silencing abrogates/reduces the anti-proliferative action of the retinoid. Finally, our data indicate that ATRA exerts a significant immune-modulatory action, resulting in increased antigen-presentation and interferon-dependent responses.
Methods
Chemicals, siRNAs and cell-lines
Chemicals: ATRA (Sigma-Aldrich, https://www.sigmaaldrich.com), AM580 (Tocris, http://www.tocris.com), BMS961 (Tocris), ER50891 (Tocris), CD2314 (Tocris), MM11253 (Tocris), ER50891 (Tocris) and CD2665 (Tocris). Stealth Interfering-RNAs (RNAi, Invitrogen-Thermo Fisher Scientific, Carlsbad, CA, USA): si-IRF1a = RNAi (HSS105500) and si-IRF1b = RNAi (HSS179960). RNAi Negative Control duplexes (high GC, cat. No. 12935-400) served as negative controls (si-CTRL). The characteristics/origin of the gastric-cancer cell-lines used is available in Table S1.
Silencing and over-expression studies
To silence IRF1 in a transient manner, HGC-27 or LMSU cells were transfected with the si-IRF1a, si-IRF1b and si-CTRL stealth RNAi oligonucleotides (60 nM), in OptiMem containing Lipofectamine-2000 (Invitrogen). To obtain the shRNA plasmid-constructs used for IRF1 (sh-IRF1a/sh-IRF1b) and DHRS3 (sh-DHRS3a/sh-DHRS3b) silencing and the non-targeted control-shRNA plasmid-constructs (sh-CTRL1/sh-CTRL-2), double-stranded DNA-oligonucleotides were designed by Biosettia Inc. (San Diego, CA) and synthesized by Metabion (Metabion international AG/metabion GmbH 2018). The shRNA-coding double-stranded DNAs were inserted into the pGreenPuro-plasmid (System Biosciences Inc, Palo Alto, CA), using the EcoRI/BamHI sites located downstream of the H1 gene promoter (double-stranded oligonucleotides structures: Table S2). The constructs were transfected in 293TN cells to generate lentiviral particles, which were concentrated with PEG-IT (System-Biosciences, Palo Alto, CA) and used to infect HGC-27 cells. Infected HGC-27 cells were selected in 5 µg/ml puromycin (Sigma-Aldrich). IRF1 over-expression studies in retinoid-resistant AGS cells: AGS cells were transiently transfected with a plasmid construct allowing the expression of the full-length IRF1 cDNA (RC203500; Origene) using a standard approach, as detailed in the legend to Fig. S8.
Western-blots, FACS analyses and cell-growth studies
Cell-lysates in RIPA buffer containing PMSF(1.0 mM)/1×protease-inhibitor were separated by SDS–PAGE, transferred to nitro-cellulose (Protran, Amersham) and incubated with primary-antibodies (1:1000) at 4 °C overnight. After staining with HRP-conjugated secondary-antibodies (1:10000 for anti-rabbit and 1:3000 for anti-mouse antibodies), signals were developed using the ECL-Star kit (Euroclone) and the BioRad-Chemidoc-TM imaging-system (Image LabTM touch software, BioRad). β2-actin served as the loading control. Western-blot experiments were conducted with anti-IRF1 (8478, Cell Signaling Technology; E-AB-12,522, Elabscience), anti-DHRS3 (FNab02372, FineTest, Wuhan, China) anti-β2-actin (SC-47,778, Santa Cruz) and anti-tubulin (T5168, Sigma-Aldrich) antibodies. In FACS (Fluorescence-Activated-Cell-Sorter) studies, samples were stained with Viakrome808 (Beckman Coulter, Miami, FL, USA) to exclude dead cells and then HLA-A/B/C monoclonal Ab (Biolegend, cat. 311,410) according to manufacturer’s instruction. Events were acquired with Cytoflex LX (Beckman Coulter, Miami, FL, USA). Flow cytometry data were analyzed using FlowJo™ v10.8 Software (BD Life Sciences). Cell growth studies were performed with the colorimetric MTS-assay kit (Abcam, ab197010), the Sulforhodamine assay [16] or an automatic counting of viable cells with the use of the Vi-cell Blu cell viability analyzer (Beckman-Coulter).
Short-term tissue-slice cultures
The gastric-cancer samples used for the short-term tissue-slice cultures were obtained from patients undergoing a Tru-cut diagnostic procedure and they were supplied by Academic-Hospital-of-Udine-ASUFC, Udine, and Fondazione-IRCCS-Istituto-Nazionale-Dei-Tumori, Milano. All the procedures were approved by the ethical committees of the two clinical centers and a signed informed consent for the donation of the samples was obtained from patients. We performed tissue-slice cultures of the tumor samples (Supplementary Methods), as described [16]. For the quantitative histochemical determination of the Ki67 protein, tumor slices were fixed, paraffin embedded, cut into 5 μm slices and stained for the Ki67 protein using a specific antibody (Abcam, Ab16667). The number of Ki67-positive cells was counted under the microscope using the generated slides. We examined 5 fields/slide, each containing at least 1,000 cells/field.
Studies involving experimental animals
Female athymic Nude mice (Charles River, Italy) were transplanted sub-cutaneously with the LMSU and NCI-N87 cell-lines. All the experiments involving mice (project: 685/2020-PR) were performed following approval of the internal Ethical Committee on Animal Experimentation of the Istituto-di-Ricerche-Farmacologiche-Mario-Negri-IRRCS. Project 685/2020-PR was approved by the Italian-Ministry-of-Health and it was conducted in compliance with the Italian legislation.
Calculation of the experimentally determined ATRA-score
Cell lines were exposed to increasing concentrations of ATRA (0.001–10.0 µM) for 3/6/9 days and cell-proliferation was determined with the colorimetric MTS-assay kit (Abcam, ab197010). To measure the sensitivity of each cell-line to ATRA anti-proliferative action, we calculated an experimental ATRA-score based on the Area-Under-the-Curve (AUC) determined for each cell-line exposed to ATRA for 6 days (Fig. S1). The calculated AUC values were re-scaled between the “1.00” and “0.00” reference-values.
RNA-sequencing
RNA-Seq was performed with an Illumina NextSeq500 instrument using paired-end, 121-base-pair-long reads. The quality of the sequencing reads was evaluated with the FastQC (v.0.11.9) protocol. Sequence alignment of total-RNA (stranded) to the reference human genome (GRCh38) was performed with STAR (v.2.7.9a) [17], using a two-pass mode. We quantified gene-expression with the comprehensive annotations of Gencode (v38 GTF File). We adjusted and normalized samples for library size using the cpm method in the R-statistical-environment. Differential analysis was conducted with the DESeq2 (v1.28.1) pipeline [18]. GSEA (Gene-Set-Enrichment-Analysis) was performed using the Limma (v. 3.52.2) package. Gene-set collections were retrieved from the Molecular-Signature-Database (MSigDB) [19]. We corrected the p-values for multiple testing using the False-Discovery-Rate (FDR) procedure, with the significance-threshold set at 0.1. The raw data are available in the EMBL-EBI Annotare database [20] (https://www.ebi.ac.uk/fg/annotare/) under the accession numbers: E-MTAB-12,387 (Cell-lines) and E-MTAB-12,385 (Patients). The processed RNA-seq data of our gastric-cancer cell-lines are available in Table S4. We utilized the processed/normalized RNA-Seq data to perform transcriptomic clustering of the cell-lines, using the R-programming language. We calculated the pairwise distances between samples using the Euclidean distance metric. To carry out hierarchical clustering, we used the above values as inputs for the hclust function to measure the distance between clusters with the Ward’s minimum variance method [21].
In-silico computation of the ATRA-score fingerprint
To obtain a signature predicting the response to ATRA treatment in gastric-cancer, we correlated the basal gene-expression levels and the ATRA-scores of each cell-line, using the Spearman’s approach. We retrieved the constitutive transcriptomic data of the cell-lines used for the correlation analysis from the CCLE (Cancer-Cell-Line-Encyclopedia) database. The correlation analysis resulted in an initial list of genes (p-value < 0.01; rho correlation coefficient > 0.4), whose number was reduced with a connectivity analysis [22] involving the STRING (Search-Tool-for-the-Retrieval-of-Interacting-Genes/Proteins) database [23]. Selection of the genes showing a degree of interconnectedness ≥ 2 resulted in the final gene-expression signature.
ATRA sensitivity predictions in gastric-cancer patients
We predicted the ATRA-score values of the TCGA (The-Cancer-Genome-Atlas) and our 13 gastric-cancer cases (ATRA-scores and tumor histological characteristics in Supplementary Methods), using a Similarity-score algorithm (GSVA: Gene-Set-Variation-Analysis) based on the gene-expression signature described above and a Single-Sample-Gene-Set-Enrichment-Analysis (ssGSEA) approach [24]. The GSVA algorithm [25] permitted the calculation of a Similarity-score value reflecting the enrichment of the gene-set under study, using the GSVA-R-package.
Clustering of the samples into the G-DIFF and G-INT sub-groups
With the use of the signature template of 171 genes classifying gastric-cancers into the G-DIFF and G-INT sub-groups [8] and the NTP (Nearest Template Prediction) classification system [26], we clustered the 375 TCGA samples and our set of patients. We applied the NTP algorithm to the pre-processed data using the “NTP” R-package, which calculates the Euclidean distance between the expression profile of each sample and the centroid vector of each template, assigning the sample to the template characterized by the smallest distance. We evaluated the classification accuracy of the NTP method using a cross-validation approach (number of permutations = 100). With this approach, we split the data into a training- as well as a test-set in a random fashion and we assessed the performance according to the proportion of correctly classified samples in the test-set.
Results
A significant proportion of gastric-cancers are sensitive to ATRA
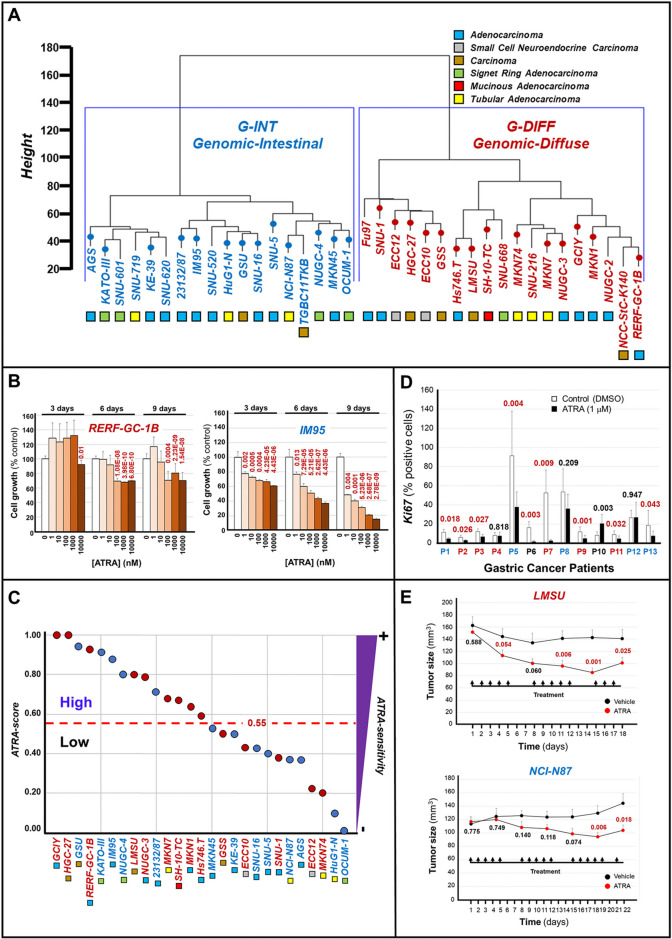
The heterogeneity of gastric-cancer [7, 27] is recapitulated by cell-lines whose constitutive gene-expression profiles are available in the CCLE (Cancer-Cell-Lines-Encyclopedia) database. This database contains RNA-sequencing (RNA-seq) data from 37 gastric-cancer cell-lines (Fig. 1A). According to their gene-expression profiles, these cell-lines classify into the G-INT and G-DIFF subgroups [8].
Fig. 1.
ATRA-dependent anti-tumor activity in gastric-cancer cell-lines, tissue-slice cultures of gastric-cancer specimens and LMSU/NCI-N87 mouse xenografts. A Unsupervised-hierarchical-clustering of the indicated gastric-cancer cell-lines based on the gene-expression profiles determined with the RNA-seq results (TCGA-dataset): cell-lines are classified according to transcriptomic-profile (G-DIFF=red; G-INT=blue) and histochemical-characteristics (colored-boxes). B ATRA growth-inhibitory effects in RERF-GC-1B (G-DIFF, red) and IM95 (G-INT, blue) cell-lines: the values are normalized for the vehicle-treated controls, which are taken as 100%. Each point is the mean±SD of 10 cultures. When the cell-growth results observed in ATRA-treated specimens are significantly lower than those of the vehicle-treated counterparts, p-values (two-tailed Student’s t-test) are shown in red. C Gastric-cancer cell-lines are ranked according to the ATRA-score values: the bimodal and arbitrary threshold-value of 0.55 separates the cell-lines characterized by high ATRA-sensitivity (ATRA-score >0.55) from the cell-lines showing low ATRA-sensitivity (ATRA-score <0.55). Each calculated value is representative of at least 2 independent experiments. D Surgical specimens of 13 patients (P1-P13) were challenged with vehicle (DMSO) or ATRA (1.0 μM) for 48 hours: P3-P6-P9=female-patients; P1-P2-P4-P5-P7-P8-P10-P11-P12-P13= male-patients; G-INT-cases=blue; G-DIFF-cases=red; not-determined=black. Each value = Mean ± SE of 5 histological-fields/experimental-sample. The p-values (two-tailed Student's t-test) of the comparisons between the ATRA and corresponding vehicle-treated samples are shown. When the Ki67 amounts observed in ATRA-treated specimens are lower than those of the vehicle-treated counterparts, the p-values are marked in red. E Mice were xenografted subcutaneously with 1×107 LMSU or NCI-N87 cells on both flanks. One week after transplantation, 10 animals/experimental group were treated with vehicle (DMSO) or ATRA (15.0 mg/kg) intra-peritoneally once/day, 5-days/week, as indicated (arrows). The calculated volumes of the tumors are plotted. As for LMSU, each point is the Mean ± SE of 15 and 19 tumors in the case of DMSO- and ATRA-treated animals, respectively. As for NCI-N87, each point is the Mean ± SE of 19 and 22 tumors. We compared the vehicle and ATRA-treated values at each time-point and the p-values (two-tailed Student’s t-test) of each comparison are shown
To define the sensitivity of gastric-cancer cells to ATRA growth-inhibitory action, we selected 27 cell-lines and exposed them to increasing concentrations of the retinoid (0.001-10µM). Subsequently, we evaluated the anti-proliferative effects of ATRA at day-3, day-6 and day-9, as exemplified in the case of the RERF-GC and IM95 cells (Fig. 1B). Cell-lines were ranked for their sensitivity to the retinoid (Fig. 1C) using a modified version of the quantitative ATRA-score index [14, 16]. This new version of the ATRA-score is based on the AUCs determined for each retinoid-treated cell-line and it ranges from a minimal “0.00” value to a maximal “1.00” value. We calculated the ATRA-scores using the growth-curves at day-6 (Fig. S1). To obtain a bimodal distribution of the 27 gastric-cancer cell-lines based on their level of sensitivity to the retinoid, we used an arbitrary ATRA-score threshold value of 0.55, which falls above the median number of cell-lines. Indeed, this threshold value allows separation of the cell-lines into 2 unbiased groups, consisting of 14 and 13 cell-lines, which are characterized by high (ATRA-score > 0.55) and low (ATRA-score < 0.55) ATRA-sensitivity (Fig. 1C). The 2 most sensitive (GCIY/HGC-27) and the 2 least sensitive (HuG1-N/OCUM-1) cell-lines have a G-DIFF and a G-INT phenotype, respectively. This reflects the trend observed in our panel of cell-lines, which shows a respective enrichment of the G-DIFF and G-INT phenotypes in the high ATRA-sensitivity (9/14) and the low ATRA-sensitivity (8/13) groups.
To validate the results obtained with cell-lines, we evaluated the anti-proliferative effects exerted by ATRA in gastric-cancer tissue-slice cultures [16, 28] from 13 patients (Table S4, patients-characteristics). Five and 6 of these tumors classify as G-INT and G-DIFF, respectively, according to the constitutive gene-expression profiles determined by the RNA-seq analyses performed on 11 cases. We challenged tissue-slices with vehicle or ATRA for 48 h and the growth-inhibitory action of the retinoid was determined by quantitative immune-histochemical measurement of the Ki-67 proliferation-marker, as exemplified for patient-1 (G-INT) and patient-2 (G-DIFF) (Fig. S2). The results demonstrate that ATRA causes a decrease of the Ki-67 levels in 9 cases (G-DIFF = 5 cases; G-INT = 3 cases; NotDefined = 1 case) (Fig. 1D).
To support the therapeutic potential of ATRA in gastric-cancer, we performed in-vivo studies with xenografts of a G-DIFF (LMSU/ATRA-score = 0.80) and a G-INT (NCI-N87/ATRA-score = 0.37) cell-line. Mice were administered vehicle (DMSO) or ATRA intra-peritoneally for 2/3 weeks and the tumor-size was determined at different time-points (Fig. 1E). As for LMSU, an ATRA-dependent reduction of the tumor-mass is already evident following 5 days of treatment and the decrease is maximal at day-15 (Fig. 1E, upper). In NCI-N87 xenografts, the maximal effect of ATRA is of lower magnitude and it is delayed, being observed only at day-19 (Fig. 1E, lower). In these conditions, ATRA is devoid of systemic toxicity, as it exerts no significant effect on the body-weight of LMSU- and NCI-N87-transplanted mice (Fig. S3).
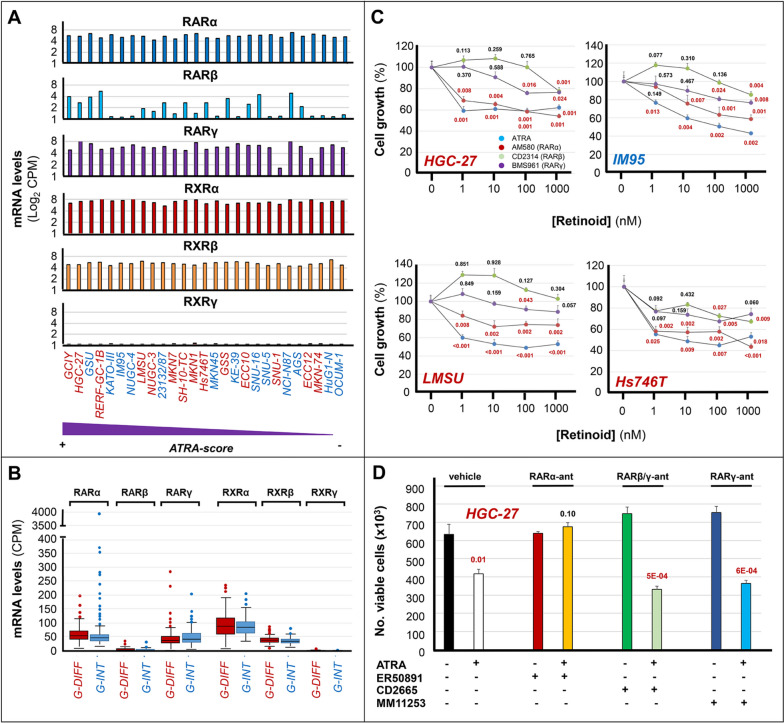
Involvement of RARα in the anti-proliferative action of ATRA
Six retinoid-receptors (RARα/RARβ/RARγ/RXRα/RXRβ/RXRγ) are known and the active forms of these transcription-factors consist of RAR/RXR heterodimers, in which RAR acts as the ligand-binding component [29, 30]. ATRA is a pan-RAR agonist, binding/trans-activating RARα/RARβ/RARγ with equal affinity/efficiency.
To identify the RAR isoform(s) underlying the anti-proliferative action of the retinoid, initially, we evaluated the constitutive expression of RARα, RARβ, RARγ, RXRα, RXRβ and RXRγ mRNAs in our gastric-cancer cell-lines (Fig. 2A). The CCLE RNA-seq data indicate that all the cell-lines express similar levels of RARα, RARγ, RXRα and RXRβ mRNAs. In contrast, the levels of RARβ mRNA are variable, although the majority of cell-lines expresses barely detectable amounts of the transcript. No correlation between RARβ mRNA levels and ATRA-sensitivity or G-DIFF/G-INT phenotype is evident. Moreover, no cell-line expresses detectable amounts of the RXRγ mRNA. Noticeably, the RAR/RXR expression profiles of the cell-lines recapitulate the situation of primary gastric-cancers, as indicated by the RNA-seq data of the TCGA database (Fig. 2B).
Fig. 2.
RAR and RXR mRNAs expression and RAR agonists anti-proliferative effects in gastric-cancer. A The panel shows the constitutive expression levels of the mRNAs coding for the indicated RAR and RXR isoforms in our panel of 27 gastric-cancer cell-lines. The cell-lines are ranked according to their decreasing sensitivity to the anti-proliferative effects of ATRA from left to right, as indicated. The expression values of the RAR and RXR mRNAs in gastric-cancer cell-lines are calculated using the RNA-seq results of the CCLE database. The values are expressed as Log 2 [CPM (Counts Per Million)]. G-DIFF and G-INT cell-lines are marked in red and blue, respectively. B The box plots indicate the constitutive expression levels of the mRNAs coding for the indicated RAR and RXR isoforms in gastric-cancer tissues characterized by a G-DIFF (red) or a G-INT (blue) phenotype. The values are calculated with the RNA-seq results of the TCGA database. The results are expressed as the Median [CPM] values ± SD. C The indicated G-DIFF (HGC-27; LMSU; Hs746T) and G-INT (IM95) cell-lines were exposed to vehicle (DMSO; [Retinoid] = 0 nM) or the indicated concentrations of the pan-RAR agonist, ATRA, the RARα agonist, AM580, the RARβ agonist, CD2314, and the RARγ agonist, BMS961, for 6 days. At the end of the treatment, the growth of each cell line was evaluated with the MTS assay. Each value is the Mean ± SD of 5 independent cultures and the data are normalized for the growth value of vehicle-treated cells (100%). We compare each compound-treated sample with the corresponding vehicle-treated counterparts at the different concentrations of the compounds. In case of statistical significance (two-tailed Student’s t-test), the p-values are shown in red. When the p-values lack statistical significance, they are marked in black. D Three independent cultures of HGC-27 cells were exposed to vehicle (DMSO) the RARα antagonist, ER50891 (0.1 µM), the RARβ /γ antagonist, CD2665 (0.1 µM), or the RARγ antagonist, MM11253 (0.1 µM), in the absence and presence of ATRA (0.01 µM) for 9 days. At the end of the treatment, the number of viable cells was counted automatically. In all samples, cell viability was always ≥ 85%. The values indicated by the columns are the Mean ± SD of the 3 independent cultures considered. We compare each ATRA, ATRA + ER50891, ATRA + CD2665 and ATRA + MM11253 treated sample with the corresponding vehicle, ER50891, CD2665 and MM11253 treated counterparts. In case of statistical significance (two-tailed Student’s t-test), the p-values shown above the corresponding columns are marked in red
Subsequently, we took a pharmacological approach involving the use of RARα/RARβ/RARγ agonists. With this approach, we determined the growth of the HGC-27 (ATRA-score = 1.00), IM95 (ATRA-score = 0.88), LMSU (ATRA-score = 0.80) and Hs747T (ATRA-score = 0.59) cell-lines, which belong to the high ATRA-sensitivity group. To this purpose, we exposed the 4 cell-lines to increasing concentrations of ATRA, AM580 (RARα agonist) [31], CD2314 (RARβ agonist) [32] and BMS961 (RARγ agonist) [16] for 6 days (Fig. 2C). In all the cell-lines, AM580 is the sole RAR agonist causing a concentration-dependent growth-inhibitory action of the same order of magnitude as the one observed with ATRA. Indeed, CD2314 and BMS961 exert only marginal effects on the growth of HGC-27, LMSU, IM95 and Hs747T cells and these effects are observed only with the highest concentration(s) of the two compounds. The data obtained with the RAR agonists support the idea that RARα is the primary retinoid receptor involved in the anti-proliferative action exerted by ATRA in gastric cells.
Finally, we performed experiments aimed at validating the hypothesized role of RARα in the growth inhibitory action exerted by ATRA, with the use of a specific RARα antagonist (ER50891), a RARβ/γ antagonist (CD2665) and a selective RARγ antagonist (MM11253) (Fig. 2D). To conduct these studies, we exposed HGC-27 cells to ATRA, ER50891, CD2665 and MM11253 as well as the combinations of ATRA + ER50891, ATRA + CD2665 and ATRA + MM11253 for 9 days. In these experimental conditions, ATRA causes the expected growth inhibitory effect, while ER50891, CD2665 and MM11253 are devoid of any anti-proliferative action on HGC-27 cells. Remarkably, the RARα antagonist, ER50891, is the sole compound suppressing the growth inhibitory action of ATRA. Indeed, exposure of HGC-27 cells to ATRA + CD2665 and ATRA + MM11253 results in the same level of growth inhibition observed with ATRA alone.
In conclusion, the data obtained in HGC-27 cells with a pharmacological approach based on the use of RAR agonists and antagonists are consistent with the idea that activation of RARα is necessary and sufficient to mediate the anti-proliferative activity of ATRA in sensitive gastric-cancer cells.
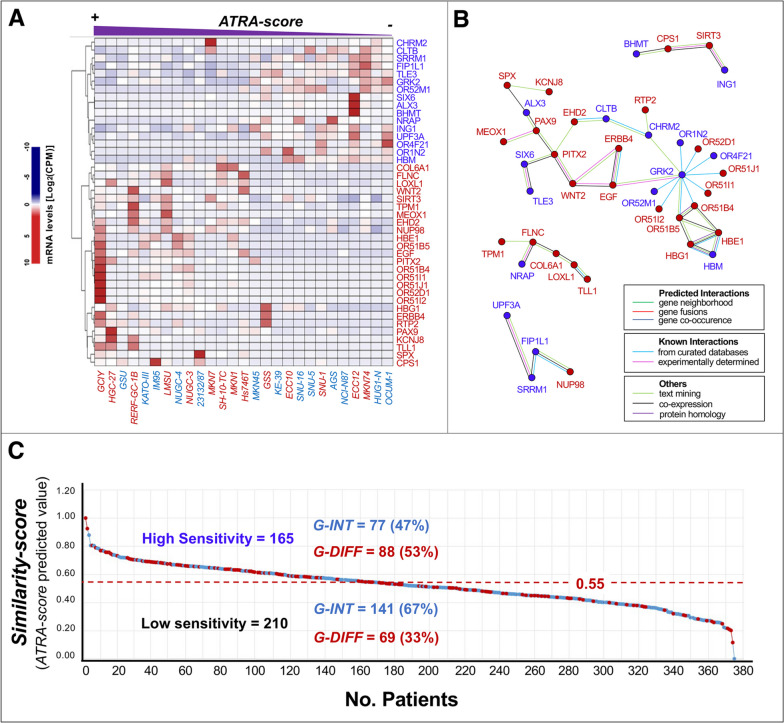
Networks of genes whose constitutive expression is associated with ATRA-sensitivity
As a first step towards the generation of a predictive tool for the selection of ATRA-sensitive gastric-cancer patients, we defined the constitutive gene-expression profiles of our panel of 27 cell-lines, employing the CCLE/RNA-seq data. The computational approach used identifies a limited number of transcripts whose basal expression levels correlate directly or inversely with the experimentally determined ATRA-score values in a quantitative manner (Fig. 3A). Indeed, 26 and 16 protein-coding mRNAs correlate with ATRA-sensitivity directly (high-Basal-Expression-Levels/high-ATRA-scores) and inversely (low-Basal-Expression-Levels/high-ATRA-scores). According to an analysis performed with the STRING database [23], the products of these 42 genes converge into 4 distinct networks of interacting proteins (Fig. 3B). The largest network (28 elements) contains proteins involved in tissue-development (PITX2/PAX9/ALX3/MEOX1/SIX6/TLE3) and the WNT pathway (WNT2/TLE3/EGF/ERBB3). The second network (6 elements) encloses proteins playing a role in myogenesis and collagen-homeostasis (TPM1/FLNC/NRAP/COL6A1/LOXL1/TLL1). The third and fourth networks consist of factors controlling pre-mRNA-processing (UPF3A/SRRM1/FIP1L1/NUP98) and metabolic-/mitochondrial-homeostasis (CPS1/BHMT/SIRT3/ING1).
Fig. 3.
Transcriptomic model based on genes whose basal expression is associated with gastric-cancer cell-lines ATRA-scores. A The panel shows a heat-map illustrating the levels of the 42 genes whose constitutive expression is quantitatively associated with the ATRA-score values of the gastric-cancer cell-lines profiled for their sensitivity to ATRA. The mRNAs directly (high-Basal-Expression-Levels/high-ATRA-scores) and inversely (low-Basal-Expression-Levels/high-ATRA-scores) correlated with ATRA-sensitivity are marked in red and blue respectively. The expression values of the 42 mRNAs in gastric-cancer cell-lines are calculated with the use of the RNA-seq results available in the CCLE (Cancer Cell Line Encyclopedia) database. The values are expressed as Log 2 [CPM (Counts Per Million)]. The G-DIFF and G-INT cell-lines are marked in red and light-blue, respectively. B The panel illustrates the results of a STRING (Search-Tool-for-the-Retrieval-of-Interacting-Genes/Proteins) analysis performed on the 42 gene-products directly or inversely associated with ATRA-sensitivity. The genes directly and inversely associated with ATRA-sensitivity are marked by red and blue dots, respectively. C The panel shows the level of ATRA-sensitivity predicted in the 375 gastric-cancer samples of the TCGA dataset for which RNA-seq results are available. The predictions rest on the 42-gene model shown in panels (A) and (B) and they were generated with the use of a quantitative Similarity-score applied to the RNA-seq data. The ATRA-score threshold value of 0.55 is used to separate the cases predicted to be characterized by high ATRA-sensitivity (≥ 0.55) and low ATRA-sensitivity (< 0.55). The G-DIFF and G-INT cases are marked in red and blue, respectively. The number and percentage of G-DIFF and G-INT cases observed in the high ATRA-sensitivity and low ATRA-sensitivity groups are indicated
We used the combined expression levels of the 42 transcripts to calculate Similarity-score values from the RNA-seq of the 375 gastric-cancer cases available in the TCGA-dataset. These Similarity-scores were utilized to predict the corresponding ATRA-score values (Fig. 3C). Indeed, we predict an ATRA-score ≥ 0.55 in 165 cases (high ATRA-sensitivity) and an ATRA-score < 0.55 in the remaining 210 cases (low ATRA-sensitivity). Thus, consistent with the proportion of gastric-cancer cell-lines experimentally responsive to ATRA (52%; Fig. 1C), 44% of gastric-cancers are predicted to be characterized by high ATRA-sensitivity. As expected from the cell-lines data, the G-INT phenotype is prevailing in patients characterized by predicted low ATRA-sensitivity (67%; Fig. 3C).
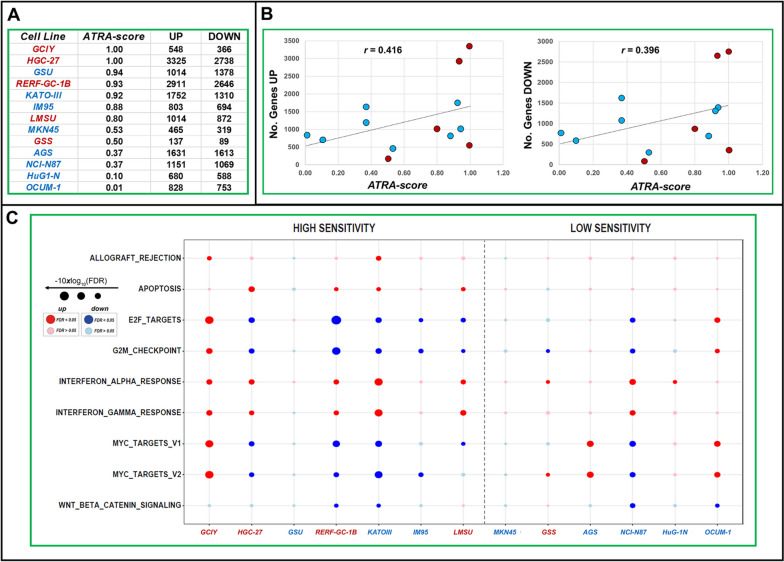
Effects of ATRA on gene-expression in gastric-cancer cell-lines
To obtain insights into the gene-networks mediating the action of ATRA in gastric-cancer, we performed RNA-seq studies in 13 of our cell-lines (Table S4). Seven and 6 cell-lines are characterized by high (ATRA-score > 0.55) and low (ATRA-score < 0.55) sensitivity to the retinoid, respectively (Fig. 4A). To perform these RNA-seq studies, we exposed each cell-line to vehicle or ATRA (1.0 µM) for 48 h, a time-interval preceding any sign of growth-inhibition. The number of transcripts up- and down-regulated by ATRA in each cell-line (Fig. 4A) shows a direct correlation with the ATRA-scores, as indicated by the linear-regression r-values (Fig. 4B). Indeed, the higher is the ATRA-score determined in each cell-line, the higher is the number of mRNAs up-/down-regulated by ATRA.
Fig. 4.
Effects of ATRA on the gene-expression profiles of gastric cancer cells: RNA-seq pathway analysis. Exponentially growing triplicate cultures of the indicated cell lines were exposed to ATRA (1.0 µM) for 48 hours. At the end of the treatment cells were subjected to RNA-seq analysis (processed data in Table S4). A The panel shows the ATRA-sensitivity scores (ATRA-scores) of the 13 gastric cell-lines considered along with the number of genes significantly (FDR<0.1) up-regulated (UP) and down-regulated (DOWN) by ATRA (1.0µM) following 48 hours of exposure. B The diagram illustrates the correlations between the ATRA-score values and the number of genes up-regulated by the retinoid in our experimental conditions. The r-correlation values are indicated. C The RNA-seq data were subjected to pathway analysis using the HALLMARK data set. The Figure illustrates a Dot-Plot of the most significant HALLMARK pathways which are up-regulated (red dots) and down-regulated (blue dots) by ATRA in the indicated cell-lines. The size of the dots is inversely proportional to the FDR (False-Discovery-Rate) values calculated. When the FDR values are <0.1, they are considered to be statistically significant. The dots shown in dark color are statistically significant, while those shown in light color lack significance. Only the most relevant up- (red) or downregulated (blue) pathways are illustrated. The full results of the analysis are available in Fig. S4
To gather further information regarding the pathways regulated by ATRA in the responsive cell-lines, we performed GSEA on the RNA-seq data, using the HALLMARK platform (Figs. 4C and S4). The ATRA-dependent anti-proliferative effects are associated with a decrease in the expression of genes involved in the control of the G2M checkpoint and genes regulated by the E2F transcription-factor. In the retinoid-sensitive cell-lines, the growth-inhibitory action of ATRA seems to involve a specific down-regulation of c-myc target-genes (Figs. 4C and S4). In the majority of the cell-lines, regardless of their sensitivity to the retinoid, ATRA increases the expression of genes controlled by interferon-α (IFNα) and interferon-γ (IFNγ) (Figs. 4C and S4). These data indicate that the retinoid activates a series of IFN-dependent immune-responses, which may be necessary but insufficient for the anti-proliferative effects of ATRA in gastric-cancer cells. As for the potential metabolic pathways involved in the growth-inhibitory action of ATRA, the KEGG-Metabolism platform indicates that ATRA tends to up-regulate genes controlling glycerophospholids and retinol metabolism in all cell-lines (Fig. S5).
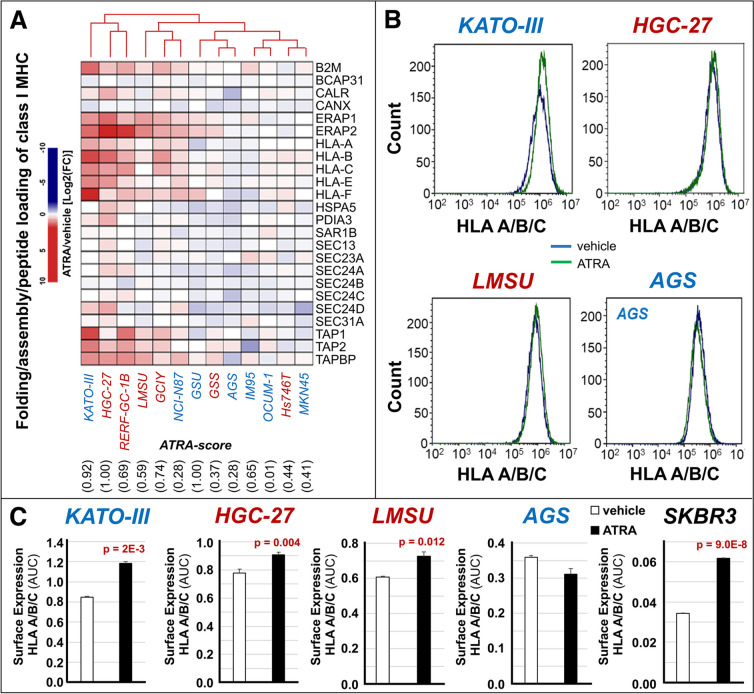
ATRA-dependent up-regulation of the genes involved in IFN-dependent immune-responses is accompanied by an increase in the HALLMARK “Allograft-Rejection” gene-set (Figs. 4C and S4). This HALLMARK network contains genes involved in antigen-presentation and T-cell dependent suppression of tumor-growth/metastatic-spread, which suggests that ATRA increases the immunogenicity of gastric-cancer cells. Thus, we took into consideration the REACTOME “Folding-Assembly-and-Peptide-Loading-of-Class-I-MHC” gene-set, which consists of 24 genes playing key roles in antigen-presentation. ATRA up-regulates this gene-network in the majority of our gastric-cancer cell-lines, regardless of retinoid-sensitivity and G-DIFF/G-INT phenotype (Fig. 5A). In particular, ATRA stimulates the expression of the HLA-A/B/C and the B2M genes whose products are components of the Major-Histocompatibility-Complex (MHC). To evaluate whether these ATRA-dependent transcriptomic effects translate into an increase of the HLA-A/B/C surface-antigens, we performed FACS (Fluorescence-Activated-Cell-Sorter) analyses in the gastric-cancer HGC-27, LMSU, KATO-III, AGS and the breast-cancer SKBR3 (positive control) cell-lines, using an anti-HLA-A/B/C antibody (Fig. 5B and C). Consistent with the general up-regulation of the REACTOME gene-network, HGC-27, LMSU and KATO-III cells show an ATRA-dependent increase in HLA-A/B/C surface-expression. Significantly, ATRA does not alter HLA-A/B/C surface-expression in AGS, the only cell-line showing a slight down-regulation of the REACTOME gene-network.
Fig. 5.
Effects of ATRA on the process of antigen-presentation in gastric-cancer cell-lines. The indicated cell-lines were exposed to vehicle (DMSO) or ATRA (1µM) for 48 hours. At the end of the treatment, each cell-line was subjected to RNA-seq analysis. A The panel shows a heat-map illustrating the effects of ATRA on the expression levels of the 24 genes constituting the “Folding-Assembly-and-Peptide-Loading-of-Class-I-MHC” REACTOME gene-network in the indicated gastric-cancer cell-lines. The results are expressed as the ATRA-vehicle ratio [Log2FC (Fold-Change)]. The G-INT cell-lines are marked in blue and the G-DIFF cell-lines are marked in red. The cell-lines ATRA-score values are shown below the heat-map, as indicated. B and C The indicated gastric-cancer and the control SKBR3 breast cancer cell-lines were exposed to vehicle (DMSO) or ATRA (1µM) for 48 hours. At the end of the treatment, the cell-lines were subjected to FACS (Fluorescence-Activated-Cell-Sorter) analysis with an anti-HLA/B/C antibody. Panel B shows representative FACS graphs obtained with the indicated gastric-cancer cell-lines. Panel C shows the calculated FACS quantitative data. The data are expressed as the Mean+SD (N=3) of the AUC (Area Under the Curve) values determined from the FACS graphs. The surface expression of HLA/B/C was compared in each of the indicated vehicle-treated and ATRA-treated cell-lines. In case of significance (two-tailed Student’s t-test), the p-values of the comparisons are shown
Genes commonly modulated by ATRA in both G-INT and G-DIFF cell-lines
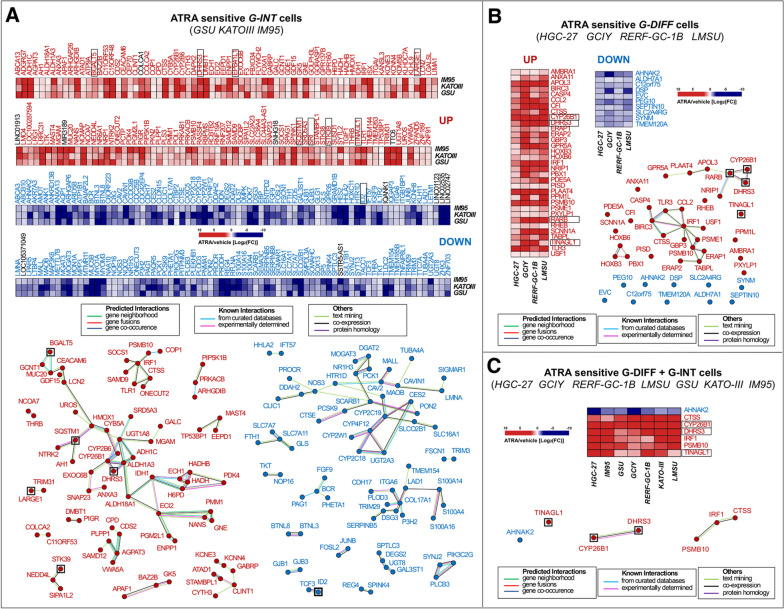
To identify genes potentially involved in the anti-tumor action of ATRA in G-INT tumors, we performed RNA-seq studies with 8 G-INT cell-lines exposed to ATRA for 48 h. In a first set of experiments, we focused on the G-INT cell-lines, GSU, KATO-III and IM95 (ATRA-score > 0.55) characterized by high ATRA-sensitivity. In these cell-lines, ATRA modulates the expression of a few thousands transcripts (Fig. S6, left). However, only 143 and 154 common mRNAs are up-regulated and down-regulated by ATRA, respectively, in all these cell-lines (Fig. 6A).
Fig. 6.
Gene-networks modulated by ATRA in retinoid-sensitive G-INT and G-DIFF gastric-cancer cell-lines. The G-INT/ATRA-sensitive GSU/KATO-III/IM95 and the G-DIFF/ATRA-sensitive HGC-27/GCIY/RERF-GC-1B/LMSU cell-lines were exposed to vehicle (DMSO) or ATRA (1µM) for 48 hours and subjected to RNA-seq analysis. A Upper: heat-maps illustrating the effects of ATRA on the expression of the 297 genes commonly up-regulated (143 genes; UP) and down-regulated (154 genes; DOWN) in the 3 G-INT cell-lines (FDR < 0.1). The results (Mean of 3 independent vehicle-treated and ATRA-treated cultures) are expressed as the ATRA-vehicle ratio [Log2 FC (Fold Change)]. Up-regulated/genes=red; Down-regulated/genes=blue; Non-protein-coding/genes=black. Lower: STRING (Search-Tool-for-the-Retrieval-of-Interacting-Genes/Proteins) analysis of the 143 up-regulated gene-products (left diagram; red dots) and the 154 down-regulated gene-products (right diagram; blue dots). The proteins in black squares are encoded by genes up-regulated and down-regulated in the retinoid-resistant G-DIFF cell-lines, AGS, NCI-N87, HuG1-N, MKN45, OCUM-1. B Upper: 2 heat-maps illustrating the effects of ATRA on the expression levels of the 43 genes commonly (FDR < 0.1) up-regulated (33 genes; UP) and down-regulated (10 genes; DOWN) in the in the 4 G-DIFF gastric-cancer cell-lines. The results are expressed as the ATRA-vehicle ratio [Log2 FC (Fold Change)] and they represent the mean of 3 independent vehicle-treated and ATRA-treated cultures. Lower: STRING-analysis of the 33 up-regulated gene-products (red-dots) and the 10 down-regulated gene products (blue-dots). The proteins in black squares are encoded by genes up-regulated in the retinoid-resistant G-DIFF cell-line, GSS. C Upper: heat-map illustrating the effects of ATRA on the expression of the genes commonly up-regulated (6 genes; UP) and down-regulated (1 gene; DOWN) in ATRA-sensitive G-INT/G-DIFF cell-lines (FDR < 0.1). The results (mean of 3 vehicle-treated and ATRA-treated cultures) are expressed as the ATRA-vehicle ratio [Log2 FC (Fold Change)]. Lower: STRING-analysis of the 6 up-regulated gene products (upper diagram; red dots) and the single down-regulated gene product (lower diagram; blue dots) which are common to the 7 ATRA-sensitive G-DIFF and G-INT cell-lines shown in panels A and B. The type of protein interactions available in the literature are shown in the rectangular boxes
As for the commonly up-regulated mRNAs, a STRING analysis of the data demonstrates that some of the corresponding translated products are part of 12 separate interactomes (Fig. 6A, lower-left). The largest interactome (37 elements) contains proteins involved in lipid-metabolism (HADHB/HADH/ECH1/ECI2/ALDH1A3/ADH1C/DHRS3/CYP26B1/CYP2B6/UGT1A8/SRD5A3/GALC/BGALT5), with particular reference to the retinol metabolic pathway (ALDH1A3/ADH1C/DHRS3/CYP26B1/CYP2B6/UGT1A8). This is consistent with the GSEA results obtained with the KEGG-Metabolism platform (Fig. S5). The second-largest interactome (8 elements) is centered on IRF1 (Interferon-Responsive-Factor-1) and it contains proteins involved in inflammation and antigen-presentation (IRF1/SOCS1/SAMD9/TLR1/PSMB10/CTSS). In this case too, up-regulation of the network is in line with the GSEA results (Fig. S4). The third-largest interactome (7 elements) contains proteins controlling ion-channels (KCNE3/KCNN4) and epithelial-polarization (CYTH3). The fourth-largest network includes the tumor-suppressor VWA5A [33] and 5 other proteins (SAMD12/PLPP1/AGPAT3/CDS2/CPD) regulating membrane phospholipids. Finally, one of the commonly up-regulated genes is DMBT1, a tumor-suppressive demethylase [34], which interacts with PGR.
As for the commonly down-regulated genes, the corresponding products aggregate into 14 interactomes (Fig. 6A, lower-right). The largest interactome (28 elements) contains factors involved in lipid metabolism (MOGAT3/DGAT2/PCK1/NR1H3/SCARB1/PCSK9/PON2/CES2/CYP2C19/CYP4F12/CYP2C18/CYP2W1/SLC16A1). Interestingly, other proteins controlling lipid metabolism (SPTLC3/DEGS2/UGT8/GAL3ST1) cluster inside a smaller network. This supports the idea that the anti-proliferative effects of ATRA in the G-INT neoplastic cells are associated with lipid-homeostasis modulation. The second-largest interactome of down-regulated gene-products (CDH17/ITGA6/COL17A1/DSG3/TRIM29/SERPINB5/PLOD3/LAD1/P3H2/TMEM154/S100A14/S100A16/S100A4) contains proteins involved in cell-adhesion and motility. Down-regulation of this last group of gene-products may relate to a potential increase in the process of epithelial-polarization mentioned in the case of the up-regulated CYTH3 gene.
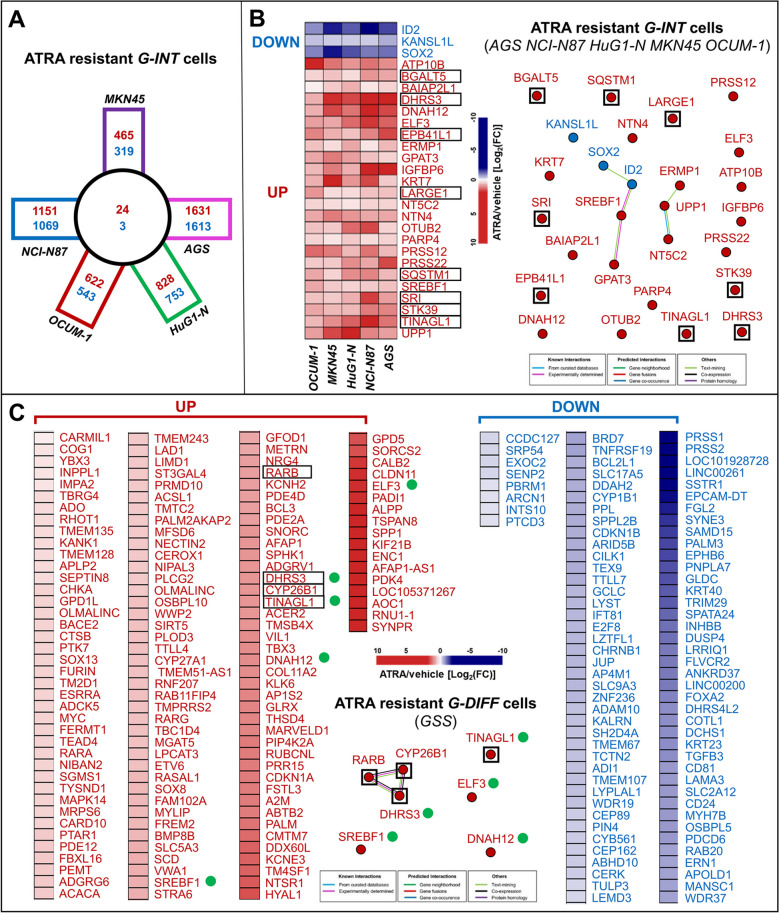
To evaluate possible associations with ATRA-sensitivity, we conducted similar studies in 5 G-INT cell-lines (MKN45, AGS, NCI-N87, HuG1-N and OCUM-1) characterized by low ATRA-sensitivity (ATRA-score < 0.55). The 5 cell-lines respond to ATRA with the up-/down-regulation of several hundred genes (Fig. 7A). Nevertheless, the number of commonly up-/down-regulated genes is limited to 24 and 3, respectively (Fig. 7A and B). Interestingly, 8 genes (BGALT5/SRI/EPB41L1/TINAGL1/LARGE1/SQSTM1/STK39/DHRS3), are up-regulated in both G-INT cells showing low and high ATRA-sensitivity (Figs. 6A and 7B, black-squares). A similar situation is observed in the case of the down-regulated ID2 gene.
Fig. 7.
Gene-networks modulated by ATRA in retinoid-resistant G-INT and G-DIFF gastric cancer cell-lines. The G-INT/retinoid-resistant MKN45/NCI-N87/AGS/OCUM-1/HuG1-N cell-lines and the G-DIFF/retinoid-resistant GSS cell-line were exposed to vehicle (DMSO) or ATRA (1.0 µM) for 48 hours and subjected to RNA-seq analysis. A The panel illustrates the number of genes selectively up-regulated (red) or down-regulated (blue) in each G-INT cell-line (squares) and commonly up-regulated (red) or down-regulated (blue) in the 5 cell-lines (circle). B The left side of the panel shows a heat-map illustrating the effects of ATRA on the expression levels of the 27 genes commonly and significantly (FDR < 0.1) up-regulated (24 genes; UP) and down-regulated (3 genes; DOWN) in the 5 retinoid-resistant G-INT gastric-cancer cell-lines. The results are expressed as the ATRA-vehicle ratio [Log2 FC (Fold-Change)] and they represent the mean of 3 independent vehicle-treated and ATRA-treated cultures. The right side of the panel illustrates the results of a STRING (Search-Tool-for-the-Retrieval-of-Interacting-Genes/Proteins) analysis performed on the 24 up-regulated gene-products (red dots) and the 3 down-regulated gene products (blue dots). The proteins included in black squares are encoded by genes which are commonly up-regulated or down-regulated also in the 3 retinoid-sensitive G-INT cell-lines, GSU, KATO-III and IM95. C The panel shows two heat-maps illustrating the effects of ATRA on the expression levels of the 225 genes significantly (FDR < 0.1) up-regulated (137 genes; UP) and down-regulated (88 genes; DOWN) in the retinoid-resistant G-DIFF cell-line, GSS. In addition, the panel illustrates the results of a STRING analysis performed on the 7 gene products which are commonly up-regulated by ATRA in the GSS and the retinoid-sensitive G-DIFF cell-lines, HGC-27, LMSU, GCIY and RERF-GC-1B (black squares) or the retinoid-resistant G-INT cell-lines, MKN45, NCI-N87, AGS, OCUM-1 and HuG1-N (green dots). The results are expressed as the ATRA-vehicle ratio [Log2 FC (Fold-Change)] and they represent the mean of 3 independent vehicle-treated and ATRA-treated cultures.
We extended our analyses to the G-DIFF context, performing studies in the G-DIFF cell-lines, HGC-27, RERF-GC-1B, LMSU and GCIY (ATRA-score > 0.55), showing high ATRA-sensitivity, as well as GSS cells, the only G-DIFF cell-line characterized by low ATRA-sensitivity (ATRA-score = 0.50). In HGC-27 and RERF-GC-1B cells, ATRA modulates the expression of 6,063 and 5,557 genes, respectively, while a lower number of genes is up- and down-regulated in LMSU (1,886 genes) and GCIY (914 genes) cells (Fig. S6, right). In these retinoid-sensitive cell-lines, ATRA up- and down-regulates 33 and 10 common genes, respectively (Fig. 6B). The STRING analysis performed on the 33 up-regulated genes demonstrates that the corresponding proteins cluster into 3 networks. The largest network (13 elements) centers on IRF1 and it contains factors regulating inflammation (BIRC3/TLR3/USF1/CCL2) and antigen-presentation (PSME1/PSMB10/TAPBPL2/ERAP1/ERAP2/CTSS). The second-largest network consists of 7 proteins (CYP26B1/DHRS3/NRIP1/RARB/GPRC5A/RARRES3/APOL3) controlling retinoid-metabolism and epithelial-differentiation. As for the 10 down-regulated genes, they do not code for any interacting protein. In retinoid-resistant GSS cells, ATRA causes a significant up- and down-regulation of 137 and 89 genes, respectively (Fig. 7C). Noticeably, 4 of these genes (CYP26B1/RARB/DHRS3/TINAGL1) are equally up-regulated in the retinoid-sensitive G-DIFF cell-lines, GCIY, HGC-27, RERF-GC-1B and LMSU (Fig. 7C, black-squares).
In a last set of studies, we looked for genes up- or down-regulated by ATRA in G-INT and G-DIFF cell-lines characterized by high ATRA-sensitivity (Fig. 6C). In all the G-DIFF and G-INT cell-lines ATRA increases the expression of 6 common genes, i.e. IRF1, DHRS3, CTSS, PSMB10, CYP26B1 and TINAGL1. In contrast, only AHNAK2 is down-regulated by ATRA in the entire set of G-INT/G-DIFF cell-lines. As already observed, the CTSS and PSMB10 gene-products interact with IRF1 and are part of the interactome centered on IRF1 itself (Fig. 6A and B). Furthermore, the CYP26B1 gene-product binds DHRS3 and the 2 proteins are part of a network involved in retinoid metabolism and epithelial-differentiation (Fig. 6A and B).
Role of IRF1 and DHRS3 in the growth inhibitory action of ATRA
Given the potential role played by IRF1 in inflammatory/immunological/IFN-dependent responses [35, 36] and by DHRS3 (Short-Chain-Dehydrogenase/Reductase-Family-16 C-Member-1 or Retinol-Dehydrogenase-17) in retinoid metabolism, we conducted functional studies on the 2 factors in HGC-27 cells.
In a first set of experiments, we transiently transfected HGC-27 cells with 2 IRF1-targeting siRNAs (siIRF1a and siIRF1b) and a control siRNA (siCTRL). We exposed the transfected cells to vehicle or ATRA for 48 h. In accordance with the up-regulation of the corresponding mRNA, ATRA increases the basal levels of the IRF1 protein in mock transfected (no siRNA) and siCTRL transfected HGC-27 cells, as indicated by the Western-blot analyses performed (Fig. 8A). By converse, the IRF1 protein is undetectable in siIRF1a and siIRF1b transfected cells regardless of vehicle or ATRA treatment. As ATRA co-regulates IRF1 and DHRS3 mRNAs, we determined the levels of the DHRS3 protein as well. In native and siCTRL-transfected cells, ATRA induces the DHRS3 protein (Fig. 8A). The two siRNAs, siIRF1a and siIRF1b reduce the basal levels of the DHRS3 protein. More importantly, the retinoid-dependent DHRS3 induction is abolished in siIRF1a- and siIRF1b-transfected cells. Thus, IRF1 up-regulation may be responsible for the increase in DHRS3 that ATRA triggers in gastric-cancer cells. As for the functional role played by IRF1, siIRF1a and siIRF1b reduce the anti-proliferative effects exerted by ATRA in native and siCTRL-transfected HGC-27 cells (Fig. 8B). These data indicate that IRF1 up-regulation takes part in the growth-inhibitory action exerted by ATRA in HGC-27 cells. To confirm the role played by IRF1 in ATRA-dependent growth inhibition of retinoid-sensitive gastric cancer cells, we performed similar silencing experiments in the LMSU cell line (Fig. S7). As expected, siIRF1a/siIRF1b transfection abolishes the constitutive levels of IRF1 protein and suppresses the ATRA-dependent IRF1 induction observed in mock transfected (no siRNA) and siCTRL transfected LMSU cells. In addition, IRF1 silencing abrogates the growth inhibitory action exerted by ATRA in the cultures of the two control LMSU cell lines (Fig. S7). This is consistent with the results generated in the HGC-27 line and it supports the idea that IRF1 up-regulation is involved in the anti-proliferative action exerted by ATRA in retinoid-sensitive gastric cancer cells.
Fig. 8.
IRF1 and DHRS3 involvement in the anti-proliferative effects exerted by ATRA in HGC-27 cells. HGC-27 cells were transfected with two IRF1-targeting (si-IRF1a/si-IRF1b) and a control siRNA (si-CTRL). Twenty-four hours later, cells were treated with vehicle (DMSO) or ATRA (1µM) for 48 hours. A Western-blot analysis using anti-IRF1, anti-DHRS3 and anti-βactin antibodies: the lanes marked as “no-siRNA” indicate parental HGC-27 cells. B Cell-growth of transfected HGC-27 cells (MTS-assay): Mean+SD of 3 replicate cultures; values normalized for vehicle-treated cells (100%). The p-values (two-tailed Student's t-test) of the comparisons between ATRA-treated and vehicle-treated cells and the comparisons between the indicated groups are shown above each red column and above the diagram, respectively. C HGC-27 cells were infected with lentiviral particles containing 2 IRF1-targeting-shRNAs (sh-IRF1a/sh-IRF1b), one control-shRNA (sh-CTRL1) or the pGreenPuro-vector (pGR). Following puromycin-selection, we isolated 4 green-fluorescent cell-populations characterized by pGR-, sh-CTRL-, sh-IRF1a- and sh-IRF1b-integration. The cell-populations were treated with vehicle or ATRA (1µM) for 48 hours and subjected to Western-blot analysis using anti-IRF1, anti-DHRS3 and anti-βactin antibodies as in (A). D The pGR-, sh-CTRL-, sh-IRF1a- and sh-IRF1b-infected cell-populations were treated with vehicle or ATRA (0.1µM/1.0µM) for 3/6/9 days: “no-sh”=parental-HGC-27 cells. Cell-growth (MTS-assay): each value is the Mean+SD of 3 cultures; values are normalized as in (B). The p-values (two-tailed-Student's-t-test) of the comparisons between ATRA-treated and corresponding vehicle-treated cells are shown above each column. E HGC-27 cells were infected with lentiviral-particles containing two DHRS3-targeting pGreenPuro-constructs (sh-DHRS3a/sh-DHRS3b), the pGreenPuro-vector (pGR) and a control shRNA (sh-CTRL2). Following infection/puromycin-selection, we isolated 4 populations of green-fluorescent HGC-27 cells characterized by stable pGR/sh-CTRL/sh-DHRS3a/sh-DHRS3b-integration. The cell-populations were treated with vehicle or ATRA (1.0µM) for 48 hours and subjected to Western-blot analysis using anti-IRF1/anti-DHRS3/anti-βactin antibodies as in (A). F pGR/sh-CTRL/sh-DHRS3a/sh-DHRS3b-infected cell-populations were treated with vehicle or ATRA as in (D). Cell-growth (MTS-assay): Mean+SD of 3 cultures; values normalized as in (D). The p-values (two-tailed-Student’s-t-test) of the ATRA-treated/vehicle-treated cells comparison are shown above each column
To validate the siRNA results we took a complementary approach based on the use of IRF1-targeting shRNAs. To this purpose, we infected HGC-27 cells with lentiviral particles containing two distinct IRF1-targeting shRNAs (shIRF1a and shIRF1b), an untargeted control shRNA (shCTRL1) or the void vector (pGR). This resulted in the generation of 4 distinct and puromycin-resistant cell-populations characterized by stable integration of the pGR, shCTRL1, shIRF1a and shIRF1b constructs. Consistent with a silencing effect of the shIRF1a and shIRF1b constructs, the basal levels of the IRF1 protein are measurable only in pGR- and shCTRL1-infected cells (Fig. 8C). As expected, ATRA causes a significant induction of the IRF1 protein in both pGR- and shCTRL1-infected cells. This ATRA-dependent increase of the IRF1 protein is abolished in shIRF1a- and shIRF1b-infected cells. As for DHRS3, vehicle-treated pGR- and shCTRL1-infected cells express measurable amounts of the corresponding protein. Upon exposure to ATRA, the two cell-populations show the expected induction of DHRS3. By converse, shIRF1a- and shIRF1b-infected cells do not express detectable levels of the DHRS3 protein, in either basal conditions or following exposure to ATRA. To define the functional consequences of the IRF1 knock-down, we exposed native as well as pGR-, shCTRL1-, shIRF1a- and shIRF1b-infected cells to vehicle and ATRA (0.1µM/1.0µM) for 3, 6 and 9 days. At day-6 and day-9, both concentrations of ATRA cause the expected reduction in the growth of native and pGR/shCTRL1 infected cells, while the observed ATRA-dependent anti-proliferative effects are absent/reduced in shIRF1a- and shIRF1b-infected cells (Fig. 8D). Overall, the data obtained in these cellular models confirm the siRNA results.
In a second set of experiments, we studied the involvement of DHRS3 in ATRA growth-inhibitory action, using the same shRNA approach described for IRF1. We infected HGC-27 cells with lentiviral particles containing DHRS3-targeting shRNA constructs (shDHRS3a and shDHRS3b) and the pGR/shCTRL2 controls. This resulted in the generation of distinct and puromycin-resistant cell-populations, which we treated with vehicle or ATRA for 48 h. Vehicle-treated pGR and shCTRL2 cells synthesize significant amounts of DHRS3, whereas the protein is undetectable in shDHRS3a and shDHRS3b cells (Fig. 8E). As expected, ATRA increases the amounts of DHRS3 in pGR- and shCTRL2-infected cells, while the protein remains undetectable in retinoid-treated shDHRS3a- and shDHRS3b-infected cells. Surprisingly, DHRS3-silencing blocks the ATRA-dependent induction of IRF1, which suggests a positive feed-back loop. To define the consequences of DHRS3-silencing, we treated pGR- shCTRL2-, shDHRS3a- and shDHRS3b-infected cells with vehicle or ATRA (0.1µM/1.0µM) for 3, 6 and 9 days. At all these time-points, both concentrations of ATRA reduce the growth of pGR-/shCTRL-infected cells (Fig. 8F). At day-9, the ATRA-dependent anti-proliferative effect observed in pGR-/shCTRL-infected cells is diminished in the shDHRS3a-/shDHRS3b-infected counterparts. These last data indicate that also DHRS3 up-regulation may be involved, at least partially, in the growth-inhibitory effects exerted by ATRA in gastric-cancer cells. However, it must be pointed out that the RNA-sequencing data indicate that ATRA induces DHRS3 expression in all the gastric cancer cell-lines considered, regardless of their relative sensitivity/resistance to the retinoid. This suggests that DHRS3 is likely to require other gene-products/factors or pathways, which are selectively stimulated/repressed by the retinoid only in sensitive gastric cancer cells, to play a role in the anti-proliferative action of ATRA.
In a last set of studies, we evaluated whether ATRA-dependent up-regulation of the IRF1 protein is dependent or independent of retinoid sensitivity. To address the point we determined the amounts of the protein in four representative lines characterized by a high level of resistance to the anti-proliferative effects of ATRA, i.e. MKN74 (G-DIFF), AGS (G-INT), HuG1-N (G-INT) and OCUM-1 (G-INT) cells. As in the case of the retinoid-sensitive HGC-27 and LMSU cells, we exposed the four cell-lines to ATRA (1µM) for 48 h and we determined the levels of the IRF1 protein by Western blot analysis (Fig. S8A). In basal conditions, MKN74 cells express higher levels of the IRF1 protein than the AGS, HuG1-N and OCUM-1 counterparts. ATRA exerts no effect on the amounts of the IRF1 protein determined in the 4 retinoid resistant cell-lines. This supports the idea that ATRA-dependent up-regulation of the IRF1 protein is a characteristic of the retinoid sensitive gastric cancer cell-lines. The results described above prompted us to evaluate the effects of IRF1 over-expression on the growth of one cell-line characterized by low sensitivity to the anti-proliferative effects of ATRA. We conducted these studies in the retinoid-resistant AGS cell-line, by stable transfection of a plasmid construct allowing expression of a functionally active IRF1 protein (Fig. S8B). In our experimental conditions, IRF1 over-expression does not alter the growth of AGS cells exposed to either vehicle or ATRA (Fig. S8C).
Overall, the data obtained with the knock-down and over-expression approaches considered suggest that IRF1 up-regulation is a necessary but insufficient determinant of the anti-proliferative action exerted by ATRA in gastric cancer cells.
Discussion
The results obtained in this pre-clinical study indicate that ATRA has significant potential in the treatment of patients affected by gastric-cancer. Indeed, our experimental data and predictions support the idea that at least one-half of the gastric-cancer cases may benefit from ATRA-based therapeutic strategies. Interestingly, ATRA-sensitive tumors are not enriched for any of the gastric-cancer sub-types defined according to the Lauren’s classification, histological characteristics or gene-expression profiles. The platform of 42 genes whose basal expression is directly or inversely associated to ATRA-sensitivity provides indications as to the characteristics of the gastric-cancers which respond to the retinoid. Among the genes directly associated with ATRA-sensitivity, WNT2 stands out. In fact, high expression of WNT2 is a negative prognostic factor, which associates with the invasive/metastatic behavior of gastric-cancer cells [37, 38], via stimulation of the EMT (Epithelial-to-Mesenchimal-Transition) process [39]. Thus, WNT2 and EMT activation may be factors involved in the sensitivity of gastric-cancer cells to ATRA. With respect to this, the direct correlation of LOXL1 (Lysyl-Oxidase-Like-1) levels with ATRA-sensitivity is consistent with the idea that EMT represents a determinant of this sensitivity. Indeed, the enzyme is over-expressed in gastric-cancer cells and it favors their EMT-dependent dissemination in the peritoneum [40].
Another important result of our studies is the observation that ATRA stimulates IFN-dependent immune-responses and increases antigen presentation in gastric-cancer cell-lines. This is similar to what we observed in the context of breast-cancer [13]. In breast cancer, the immune-modulatory effects activated by ATRA are associated with a “viral-mimicry” response resulting from an increase in the RNAs produced by endogenous retroviruses. In contrast, the ATRA-dependent immune-modulation observed in gastric-cancer cells is not accompanied by a “viral-mimicry” response, as we observe no alteration in the expression of the numerous endogenous retroviral mRNAs detected (Table S5). The data suggest that the molecular mechanisms underlying the immune-modulatory action of ATRA in gastric- and breast-cancers are different. From a translational and therapeutic prospective, the immune responses activated by ATRA in gastric-cancer are of great relevance, as they indicate that the retinoid is likely to increase the sensitivity of this tumor to immune-modulatory agents, such as immune-checkpoint inhibitors [41, 42].
A final and significant outcome of our study is the identification of a restricted number of genes which are up-regulated (IRF1, CTSS, PSMB10, CYP26B1, DHRS3 and TINAGL1) and down-regulated (AHNAK2) by ATRA in all the retinoid-sensitive gastric-cancer cell-lines considered. Interestingly, IRF1, CTSS and PSMB10 are direct or indirect transcriptional targets of ATRA [43–45] and code for interacting proteins involved in the regulation of immunity [35, 46, 47]. In particular, the IRF1 gene is likely to play a key role in the IFN-dependent and immunological responses activated by ATRA in gastric-cancer. Moreover, CYP26B1 and DHRS3 up-regulation indicates that ATRA causes significant effects on the metabolism of endogenous vitamin-A in gastric-cancer cells. In fact, CYP26B1 codes for a protein catalyzing the oxidation of ATRA into an inactive oxo-derivative [48], while DHRS3 codes for an NADPH-dependent enzyme which reduces retinaldehyde into retinol [49] [50] [51]. From a functional point of view, TINAGL1 is one of the most interesting up-regulated genes, since the corresponding protein-product suppresses the progression and diffusion of triple-negative breast-cancer via inhibition of the FAK and EGFR signaling pathways [52]. Finally, AHNAK2 is the only gene, which is down-regulated by ATRA in sensitive gastric-cancer cells. AHNAK2 codes for an oncogenic nucleoprotein [53], which may play a role in calcium signaling [54]. In gastric-cancer, AHNAK2 expression is involved in the resistance to chemotherapeutics [55]. Thus, AHNAK2 down-regulation suggests that ATRA may boost the efficacy of certain chemotherapeutics in the clinics. Although functional studies need to be performed for all the above genes, we focused our initial attention on IRF1 and DHRS3. Our results indicate that IRF1 and to a lesser extent DHRS3 modulate the growth-inhibitory action of ATRA in retinoid-sensitive gastric-cancer cells. In fact, knock-down of the two corresponding proteins suppresses and reduces ATRA anti-proliferative action in representative cell-lines. The modulatory effect exerted by IRF1 in gastric cancer cells seems to be limited to ATRA-sensitive cell-lines, as indicated by the results obtained in G-INT and ATRA-resistant AGS cells which were engineered to over-express IRF1 (Fig. S8).
Overall, the data obtained in this study suggest that pharmacological agents targeting the two proteins may be used for the design of innovative therapeutic strategies in retinoid-sensitive gastric-cancers.
Conclusion
The present study provides data supporting the therapeutic potential of ATRA in the stratified/personalized treatment of gastric-cancer. In this context, the gene-expression model that we generated will permit the development of a predictive clinical tool for the selection of patients who may benefit from ATRA-based therapeutic strategies. Overall, our data represent the fundaments for the design/organization of clinical trials focusing on the use of ATRA in the treatment of this heterogeneous type of tumor. In particular, the strong immune-regulatory responses activated by the retinoid suggest that ATRA and immune checkpoint inhibitors constitute rational combinations in the management of gastric-cancer.
Supplementary Information
Additional file 1: Supplementary Methods. Supplementary Table S1. Characteristics and source of the gastric-cancer cell-lines. Supplementary Table S2. Structure of the double stranded DNAs used for the construction of the shRNA plasmid constructs. Figure S1. Growth curves of the gastric cancer cell-lines exposed to increasing concentrations of ATRA. Figure S2. Ki67 immune-histochemistry in tissue-slice cultures of representative primary gastric-cancers exposed to ATRA. Figure S3. Effects of ATRA on the body weight of SCID mice transplanted with LMSU and NCI-N87 cells. Figure S4. HALLMARK pathway analysis of the RNA-seq results obtained following treatment of the indicated gastric cell lines with ATRA. Figure S5. KEGG pathway analysis of the RNA-seq results obtained following treatment of the indicated gastric cell lines with ATRA. Figure S6. Number of genes modulated by ATRA in retinoid-sensitive G-INT and G-DIFF gastric cancer cell-lines.Figure S7. Effects of ATRA on IRF1 protein levels and cell-growth in the retinoid-sensitive LMSU cell-line.Figure S8. Effects of ATRA on IRF1 protein expression in retinoid resistant gastric cancer cells and IRF1 over-expression in AGS cells. Original Western blots.
Additional file 2: Table S3. Characteristics of the gastric-cancer patients used for the studies involving tissue-slice cultures. The table summarizes the clinical characteristics of the 13 patients considered.
Additional file 3: Table S4. RNA-sequencing data. The table contains the processed RNA-seq data obtained with our panel of gastric cancer cell-lines exposed to vehicle and ATRA.
Additional file 4: Table S5. Effects of ATRA on the expression of the RNAs derived from endogenous retroviruses. The table contains the levels of endogenous retroviral RNAs determined by RNA-seq data obtained from the indicated cell lines exposed to vehicle and ATRA.
Acknowledgements
We would like to thank Dr. Antonio Santangelo (Department of General Surgery, Academic Hospital of Udine ASUFC, Piazzale Santa Maria della Misericordia 15, Udine, UD 33100 Italy) and Dr. Federica Majer (Department of Oncology, Academic Hospital of Udine ASUFC, Piazzale Santa Maria della Misericordia 15, Udine, UD 33100 Italy) for the work performed on the preparation of the gastric-cancer tissue samples. We would like to thank the Associazione Italiana per la Ricerca contro il Cancro (AIRC) for the funding to Enrico Garattini (Project Code: 22963) which permitted the completion of the present study. We would also like to thank the ONLUS “Ricerchiamo”-Brescia, for the financial support provided. We acknowledge the CINECA award under the ISCRA and ELIXIR-IV initiative, for the availability of high-performance computing resources and support.
Abbreviations
- ATRA
All-Trans Retinoic-acid
- APL
Acute-Promyelocytic-Leukemia
- RNA-seq
RNA-sequencing
- AUC
Area Under the Curve
- GSEA
Gene Set Enrichment Analysis
- CCLE
Cancer Cell Line Encyclopedia
- TCGA
The Cancer Genome Atlas
- GSVA
Gene Set Variation Analysis
Authors’ contributions
GL: Conceptualization; data curation; formal analysis; validation; investigation; writing – original draft. KM: investigation; methodology; experimental work in-vivo. GSK: Conceptualization; management of the patients primary tumor samples; formal analysis; writing – original draft. FG: management and provision of the patients primary tumor samples. RL: management and provision of the patients primary tumor samples. PM: management and provision of the patients primary tumor samples. DBM: management and provision of the patients primary tumor samples. BM: management of the RNA-sequencing data and analyses. RP: investigation; methodology; experimental work in-vitro. NC: Conduction of the experiments involving the use of FACS; FM: investigation; methodology; RNA-sequencing. ZA: investigation; methodology; experimental work in-vitro. PG: investigation; methodology; experimental work in-vitro. GM: investigation; methodology; experimental work in-vitro. TM: Conceptualization; data curation; formal analysis; validation; investigation; writing – original draft. GE: Conceptualization; supervision; funding acquisition; visualization; methodology; writing – original draft; project administration; writing – review and editing.
Funding
We would like to thank the Associazione Italiana per la Ricerca contro il Cancro (AIRC) for the funding to Enrico Garattini (Project Code: 22963) which permitted the completion of the present study. The research leading to these results has also received funding from MUR under PNRR M4C2I1.3 Heal Italia project PE00000019 CUP B43D22000710006 to Enrico Garattini.
Availability of data and materials
All the cell-lines used in the study are available upon request. The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request. All data generated or analysed during this study are included in this published article and its supplementary information files. The raw data of the RNA-sequencing studies are also available in the EMBL-EBI Annotare database (https://www.ebi.ac.uk/fg/annotare/) under the accession numbers: E-MTAB-12,387 (Cell-lines), E-MTAB-12,385 (Patients). The processed RNA-seq data of our gastric-cancer cell-lines are available in Table S4.
Declarations
Ethics approval and consent to participate
The gastric-cancer samples used for the short-term tissue-slice cultures were obtained from patients undergoing a Tru-cut diagnostic procedure and they were supplied by Academic-Hospital-of-Udine-ASUFC, Udine, and Fondazione-IRCCS-Istituto-Nazionale-Dei-Tumori, Milano. All the procedures were approved by the ethical committees of the two clinical centers and a signed informed consent for the donation of the samples was obtained from patients. All the experiments involving mice (project: 685/2020-PR) were performed following approval of the internal Ethical Committee on Animal Experimentation of the Istituto-di-Ricerche-Farmacologiche-Mario-Negri-IRRCS. Project 685/2020-PR was approved by the Italian-Ministry-of-Health and it was conducted in compliance with the Italian legislation.
Consent for publication
Not applicable.
Competing interests
All the authors declare that they have no conflict of interest as to the content of the present manuscript.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Luca Guarrera, Mami Kurosaki and Silvio-Ken Garattini share the first-authorship.
References
- 1.Hartgrink HH, Jansen EP, van Grieken NC, van de Velde CJ. Gastric cancer. Lancet. 2009;374(9688):477–490. doi: 10.1016/S0140-6736(09)60617-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kamangar F, Dores GM, Anderson WF. Patterns of Cancer Incidence, Mortality, and Prevalence Across Five Continents: defining priorities to reduce Cancer disparities in different Geographic regions of the World. JCO. 2006;24(14):2137–50. doi: 10.1200/JCO.2005.05.2308. [DOI] [PubMed] [Google Scholar]
- 3.Laurén P. The two histological main types of gastric carcinoma: diffuse and so-called intestinal-type carcinoma: an attempt at a histo-clinical classification. Acta Pathol Microbiol Scand. 1965;64(1):31–49. doi: 10.1111/apm.1965.64.1.31. [DOI] [PubMed] [Google Scholar]
- 4.Lim HJ, Zhuang L, Fitzgerald RC. Current advances in understanding the molecular profile of hereditary diffuse gastric cancer and its clinical implications. J Exp Clin Cancer Res. 2023;42(1):57. doi: 10.1186/s13046-023-02622-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hu B, El Hajj N, Sittler S, Lammert N, Barnes R, Meloni-Ehrig A. Gastric cancer: classification, histology and application of molecular pathology. J Gastrointest Oncol. 2012;3(3):251–261. doi: 10.3978/j.issn.2078-6891.2012.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yeoh KG, Tan P. Mapping the genomic diaspora of gastric cancer. Nat Rev Cancer. 2022;22(2):71–84. doi: 10.1038/s41568-021-00412-7. [DOI] [PubMed] [Google Scholar]
- 7.Wang Q, Liu G, Hu C. Molecular classification of gastric adenocarcinoma. Gastroenterol Res. 2019;12(6):275–282. doi: 10.14740/gr1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tan IB, Ivanova T, Lim KH, Ong CW, Deng N, Lee J, et al. Intrinsic subtypes of gastric cancer, based on gene expression pattern, predict survival and respond differently to chemotherapy. Gastroenterology. 2011;141(2):476–485e11. doi: 10.1053/j.gastro.2011.04.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xu W, Yang Z, Lu N. Molecular targeted therapy for the treatment of gastric cancer. J Exp Clin Cancer Res. 2016;35:1. doi: 10.1186/s13046-015-0276-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang ZY, Chen Z. Differentiation and apoptosis induction therapy in acute promyelocytic Leukaemia. Lancet Oncol. 2000;1:101–106. doi: 10.1016/S1470-2045(00)00017-6. [DOI] [PubMed] [Google Scholar]
- 11.Sanz MA, Fenaux P, Tallman MS, Estey EH, Löwenberg B, Naoe T, et al. Management of acute promyelocytic leukemia: updated recommendations from an expert panel of the European LeukemiaNet. Blood. 2019;133(15):1630–1643. doi: 10.1182/blood-2019-01-894980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cicconi L, Fenaux P, Kantarjian H, Tallman M, Sanz MA, Lo-Coco F. Molecular remission as a therapeutic objective in acute promyelocytic leukemia. Leukemia. 2018;32(8):1671–1678. doi: 10.1038/s41375-018-0219-5. [DOI] [PubMed] [Google Scholar]
- 13.Bolis M, Paroni G, Fratelli M, Vallerga A, Guarrera L, Zanetti A, et al. All-trans retinoic acid stimulates viral mimicry, Interferon responses and antigen presentation in breast-cancer cells. Cancers. 2020;12(5):1169. doi: 10.3390/cancers12051169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bolis M, Garattini E, Paroni G, Zanetti A, Kurosaki M, Castrignanò T, et al. Network-guided modeling allows tumor-type independent prediction of sensitivity to all-trans-retinoic acid. Ann Oncol. 2017;28(3):611–621. doi: 10.1093/annonc/mdw660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Terao M, Goracci L, Celestini V, Kurosaki M, Bolis M, Di Veroli A, et al. Role of mitochondria and cardiolipins in growth inhibition of Breast cancer cells by retinoic acid. J Exp Clin Cancer Res. 2019;38(1):436. doi: 10.1186/s13046-019-1438-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centritto F, Paroni G, Bolis M, Garattini SK, Kurosaki M, Barzago MM, et al. Cellular and molecular determinants of all-trans retinoic acid sensitivity in breast cancer: luminal phenotype and RARα expression. EMBO Mol Med. 2015;7(7):950–972. doi: 10.15252/emmm.201404670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dobin A, Davis CA, Schlesinger F, Drenkow J, Zaleski C, Jha S, et al. STAR: ultrafast universal RNA-seq aligner. Bioinformatics. 2013;29(1):15–21. doi: 10.1093/bioinformatics/bts635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Love MI, Huber W, Anders S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 2014;15(12):550. doi: 10.1186/s13059-014-0550-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liberzon A, Subramanian A, Pinchback R, Thorvaldsdóttir H, Tamayo P, Mesirov JP. Molecular signatures database (MSigDB) 3.0. Bioinformatics. 2011;27(12):1739–1740. doi: 10.1093/bioinformatics/btr260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Athar A, Füllgrabe A, George N, Iqbal H, Huerta L, Ali A, et al. ArrayExpress update – from bulk to single-cell expression data. Nucleic Acids Res. 2019;47(D1):D711–715. doi: 10.1093/nar/gky964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Murtagh F, Legendre P. Ward’s hierarchical agglomerative clustering method: which Algorithms Implement Ward’s Criterion? J Classif. 2014;31:274–275. doi: 10.1007/s00357-014-9161-z. [DOI] [Google Scholar]
- 22.Shannon P, Markiel A, Ozier O, Baliga NS, Wang JT, Ramage D, et al. Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res. 2003;13(11):2498–2504. doi: 10.1101/gr.1239303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Szklarczyk D, Gable AL, Nastou KC, Lyon D, Kirsch R, Pyysalo S, et al. The STRING database in 2021: customizable protein–protein networks, and functional characterization of user-uploaded gene/measurement sets. Nucleic Acids Res. 2021;49(D1):D605–612. doi: 10.1093/nar/gkaa1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Subramanian A, Tamayo P, Mootha VK, Mukherjee S, Ebert BL, Gillette MA, et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc Natl Acad Sci USA. 2005;102(43):15545–15550. doi: 10.1073/pnas.0506580102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hänzelmann S, Castelo R, Guinney J. GSVA: gene set variation analysis for microarray and RNA-Seq data. BMC Bioinformatics. 2013;14(1):7. doi: 10.1186/1471-2105-14-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hoshida Y. Nearest template prediction: a single-sample-based flexible class prediction with confidence assessment. PLoS One. 2010;5(11):e15543. doi: 10.1371/journal.pone.0015543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Berlth F. Pathohistological classification systems in gastric cancer: diagnostic relevance and prognostic value. WJG. 2014;20(19):5679. doi: 10.3748/wjg.v20.i19.5679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van der Kuip H, Mürdter TE, Sonnenberg M, McClellan M, Gutzeit S, Gerteis A, et al. Short term culture of Breast cancer tissues to study the activity of the anticancer drug taxol in an intact tumor environment. BMC Cancer. 2006;6(1):86. doi: 10.1186/1471-2407-6-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Garattini E, Bolis M, Garattini SK, Fratelli M, Centritto F, Paroni G, et al. Retinoids and Breast cancer: from basic studies to the clinic and back again. Cancer Treat Rev. 2014;40(6):739–749. doi: 10.1016/j.ctrv.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 30.Petkovich M, Chambon P. Retinoic acid receptors at 35 years. J Mol Endocrinol. 2022;69(4):T13–24. doi: 10.1530/JME-22-0097. [DOI] [PubMed] [Google Scholar]
- 31.Delescluse C, Cavey MT, Martin B, Bernard BA, Reichert U, Maignan J, et al. Selective high affinity retinoic acid receptor alpha or beta-gamma ligands. Mol Pharmacol. 1991;40(4):556–562. [PubMed] [Google Scholar]
- 32.Sun SY, Yue P, Mao L, Dawson MI, Shroot B, Lamph WW, et al. Identification of receptor-selective retinoids that are potent inhibitors of the growth of human head and neck squamous cell carcinoma cells. Clin Cancer Res. 2000;6(4):1563–1573. [PubMed] [Google Scholar]
- 33.Zhou YQ, Chen SL, Ju JY, Shen L, Liu Y, Zhen S, et al. Tumor suppressor function of BCSC-1 in nasopharyngeal carcinoma. Cancer Sci. 2009;100(10):1817–1822. doi: 10.1111/j.1349-7006.2009.01261.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kang W, Nielsen O, Fenger C, Leslie G, Holmskov U, Reid KBM. Induction of DMBT1 expression by reduced ERK activity during a gastric mucosa differentiation-like process and its association with human gastric cancer. Carcinogenesis. 2005;26(6):1129–1137. doi: 10.1093/carcin/bgi045. [DOI] [PubMed] [Google Scholar]
- 35.Zhou H, Tang YD, Zheng C. Revisiting IRF1-mediated antiviral innate immunity. Cytokine Growth Factor Rev. 2022;64:1–6. doi: 10.1016/j.cytogfr.2022.01.004. [DOI] [PubMed] [Google Scholar]
- 36.Feng H, Zhang YB, Gui JF, Lemon SM, Yamane D. Interferon regulatory factor 1 (IRF1) and anti-pathogen innate immune responses. Blumenthal A, curatore. PLoS Pathog. 2021;17(1):e1009220. doi: 10.1371/journal.ppat.1009220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lin L, Li L, Ma G, Kang Y, Wang X, He J. Overexpression of IL-8 and Wnt2 is associated with prognosis of gastric cancer. Folia Histochem Cytobiol. 2022;60(1):66–73. doi: 10.5603/FHC.a2022.0002. [DOI] [PubMed] [Google Scholar]
- 38.Zhang Z, Wang J, Dong X. Wnt2 contributes to the progression of gastric cancer by promoting cell migration and invasion. Oncol Lett. 2018;16(3):2857–2864. doi: 10.3892/ol.2018.9050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Katoh M. Epithelial-mesenchymal transition in gastric cancer (review) Int J Oncol. 2005;27(6):1677–1683. [PubMed] [Google Scholar]
- 40.Hu Q, Masuda T, Kuramitsu S, Tobo T, Sato K, Kidogami S, et al. Potential association of LOXL1 with peritoneal dissemination in gastric cancer possibly via promotion of EMT. PLoS One. 2020;15(10):e0241140. doi: 10.1371/journal.pone.0241140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yoon J, Kim TY, Oh DY. Recent progress in Immunotherapy for gastric cancer. J Gastric Cancer. 2023;23(1):207. doi: 10.5230/jgc.2023.23.e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shen J, Wang Z. Recent advances in the progress of immune checkpoint inhibitors in the treatment of advanced gastric cancer: a review. Front Oncol. 2022;12:934249. doi: 10.3389/fonc.2022.934249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yang XW, Wang P, Liu JQ, Zhang H, Xi WD, Jia XH, et al. Coordinated regulation of the immunoproteasome subunits by PML/RARα and PU.1 in acute promyelocytic Leukemia. Oncogene. 2014;33(21):2700–2708. doi: 10.1038/onc.2013.224. [DOI] [PubMed] [Google Scholar]
- 44.Shen M, Bunaciu RP, Congleton J, Jensen HA, Sayam LG, Varner JD, et al. Interferon regulatory factor-1 binds c-Cbl, enhances mitogen activated protein kinase signaling and promotes retinoic acid-induced differentiation of HL-60 human myelo-monoblastic Leukemia cells. Leuk Lymphoma. 2011;52(12):2372–2379. doi: 10.3109/10428194.2011.603449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Coyle KM, Maxwell S, Thomas ML, Marcato P. Profiling of the transcriptional response to all-trans retinoic acid in Breast cancer cells reveals RARE-independent mechanisms of gene expression. Sci Rep. 2017;7(1):16684. doi: 10.1038/s41598-017-16687-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang Y, Yan K, Guo Y, Lu Y, Su H, Li H. IP-score correlated to endogenous tumour antigen peptide processing: a candidate clinical response score algorithm of immune checkpoint inhibitors therapy in multiple cohorts. Front Immunol. 2022;13:1085491. doi: 10.3389/fimmu.2022.1085491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.de Mingo Pulido Á, de Gregorio E, Chandra S, Colell A, Morales A, Kronenberg M, et al. Differential Role of Cathepsins S and B in hepatic APC-Mediated NKT Cell activation and cytokine secretion. Front Immunol. 2018;9:391. doi: 10.3389/fimmu.2018.00391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Isoherranen N, Zhong G. Biochemical and physiological importance of the CYP26 retinoic acid hydroxylases. Pharmacol Ther. 2019;204:107400. doi: 10.1016/j.pharmthera.2019.107400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gudas LJ. Retinoid metabolism: new insights. J Mol Endocrinol. 2022;69(4):T37–49. doi: 10.1530/JME-22-0082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Billings SE, Pierzchalski K, Tjaden NEB, Pang X, Trainor PA, Kane MA, et al. The retinaldehyde reductase DHRS3 is essential for preventing the formation of excess retinoic acid during embryonic development. FASEB J. 2013;27(12):4877–4889. doi: 10.1096/fj.13-227967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Adams MK, Belyaeva OV, Wu L, Kedishvili NY. The retinaldehyde reductase activity of DHRS3 is reciprocally activated by Retinol dehydrogenase 10 to Control Retinoid Homeostasis. J Biol Chem. 2014;289(21):14868–14880. doi: 10.1074/jbc.M114.552257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shen M, Jiang YZ, Wei Y, Ell B, Sheng X, Esposito M, et al. Tinagl1 suppresses triple-negative Breast Cancer Progression and Metastasis by simultaneously inhibiting Integrin/FAK and EGFR Signaling. Cancer Cell. 2019;35(1):64–80e7. doi: 10.1016/j.ccell.2018.11.016. [DOI] [PubMed] [Google Scholar]
- 53.Xu M, Cheng A, Yu L, Wei W, Li J, Cai C. AHNAK2 is a biomarker and a potential therapeutic target of adenocarcinomas. Acta Biochim Biophys Sin (Shanghai) 2022;54(11):1708–1719. doi: 10.3724/abbs.2022112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Komuro A, Masuda Y, Kobayashi K, Babbitt R, Gunel M, Flavell RA, et al. The AHNAKs are a class of giant propeller-like proteins that associate with calcium channel proteins of cardiomyocytes and other cells. Proc Natl Acad Sci U S A. 2004;101(12):4053–4058. doi: 10.1073/pnas.0308619101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ohmura H, Ito M, Uchino K, Okada C, Tanishima S, Yamada Y, et al. Methylation of drug resistance-related genes in chemotherapy-sensitive Epstein-Barr virus-associated gastric cancer. FEBS Open Bio. 2020;10(1):147–157. doi: 10.1002/2211-5463.12765. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplementary Methods. Supplementary Table S1. Characteristics and source of the gastric-cancer cell-lines. Supplementary Table S2. Structure of the double stranded DNAs used for the construction of the shRNA plasmid constructs. Figure S1. Growth curves of the gastric cancer cell-lines exposed to increasing concentrations of ATRA. Figure S2. Ki67 immune-histochemistry in tissue-slice cultures of representative primary gastric-cancers exposed to ATRA. Figure S3. Effects of ATRA on the body weight of SCID mice transplanted with LMSU and NCI-N87 cells. Figure S4. HALLMARK pathway analysis of the RNA-seq results obtained following treatment of the indicated gastric cell lines with ATRA. Figure S5. KEGG pathway analysis of the RNA-seq results obtained following treatment of the indicated gastric cell lines with ATRA. Figure S6. Number of genes modulated by ATRA in retinoid-sensitive G-INT and G-DIFF gastric cancer cell-lines.Figure S7. Effects of ATRA on IRF1 protein levels and cell-growth in the retinoid-sensitive LMSU cell-line.Figure S8. Effects of ATRA on IRF1 protein expression in retinoid resistant gastric cancer cells and IRF1 over-expression in AGS cells. Original Western blots.
Additional file 2: Table S3. Characteristics of the gastric-cancer patients used for the studies involving tissue-slice cultures. The table summarizes the clinical characteristics of the 13 patients considered.
Additional file 3: Table S4. RNA-sequencing data. The table contains the processed RNA-seq data obtained with our panel of gastric cancer cell-lines exposed to vehicle and ATRA.
Additional file 4: Table S5. Effects of ATRA on the expression of the RNAs derived from endogenous retroviruses. The table contains the levels of endogenous retroviral RNAs determined by RNA-seq data obtained from the indicated cell lines exposed to vehicle and ATRA.
Data Availability Statement
All the cell-lines used in the study are available upon request. The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request. All data generated or analysed during this study are included in this published article and its supplementary information files. The raw data of the RNA-sequencing studies are also available in the EMBL-EBI Annotare database (https://www.ebi.ac.uk/fg/annotare/) under the accession numbers: E-MTAB-12,387 (Cell-lines), E-MTAB-12,385 (Patients). The processed RNA-seq data of our gastric-cancer cell-lines are available in Table S4.