Abstract
Purpose
The transition from pediatric to adult care can be complex and difficult to navigate for adolescents with cerebral palsy (CP). We aimed to assess the current state of transitional care for young persons with CP and delineate guidelines for best practice with opportunities for intervention.
Methods
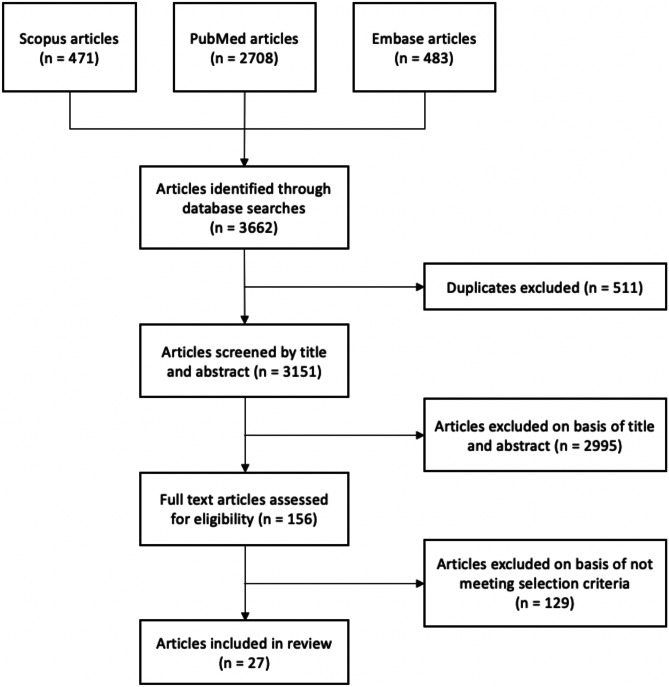
A systematic review was conducted using PRISMA guidelines to search PubMed, Embase, and Scopus databases. Articles were screened for relevance via title and abstract prior to full-text review.
Results
Of 3151 resultant articles, 27 observational studies were included. Fourteen (52%) studies assessed clinical outcomes of patients with CP during and post-transition. Transition-associated poor outcomes included housing instability, unemployment, difficulty forming relationships, increased hospital admission rates, and decreased use of rehabilitation services. Factors associated with improved outcomes included family participation, promotion of self-efficacy, and meeting the adult team before transition. Nine (33%) studies conducted interviews with transition-age persons with CP. Key themes were a lack of transition preparedness, difficulty navigating the adult system, gaps in seamless care, and limited accessibility to specialists and environments suitable for patients with complex care needs. Four (15%) studies examined features of current transition services. Perceived barriers included poor communication within health service teams, limited adult providers accepting CP patients, and the lack of financial resources for specialized care. There was no standardized transition tool or approach.
Conclusion
These findings underscore the importance of a planned transition process in optimizing long-term medical and psychosocial outcomes for persons with CP. Further research, including translational, team-based, and community-engaged research, are needed.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00381-023-06080-2.
Keywords: Cerebral palsy, Transitional care, Transition, Pediatric, Adulthood, Complex care
Introduction
Cerebral palsy (CP) is the most common childhood cause of mobility disability, with a prevalence of 2 to 2.5 per 1000 live births [1, 2]. Medical advancements have resulted in 40–90% of children with CP reaching adulthood, depending on disease severity, at which point care models historically limited to childhood may become inadequate [1, 3]. As a result, the number of young people with CP requiring transition to adult healthcare and developmental services has increased [4].
Young adults with CP require a broad period of transition from pediatric to adult care services. Additionally, transitional care is often complicated by a wide range of complex care needs, including neurodevelopmental and functional limitations [5–7]. Disease severity and associated impairments vary, requiring deeply personalized care throughout the individual’s lifespan [8, 9]. As a result, transition-associated goals must be curated to the patient’s capabilities and functional status. Unsuccessful transition to adult care is associated with the development of secondary disabilities [5], increased risk of treatment failure [10] or nonadherence [11], failure to establish care with adult providers [12], and increased rates of hospitalization [13, 14].
Despite the critical nature of effective transitional care and the serious negative health outcomes associated with inadequate transition, there is limited data characterizing the current state and development of transitional care paradigms for young persons with CP. A recent systematic review [15] examined gaps in transitional care interventions for young adults with childhood-onset neurologic disabilities but did not focus on disease-specific populations. Similarly, guidelines [16] for transitioning youth with complex care needs from pediatric to adult care have been established but are non-specific to young adults with CP. We conducted a systematic review to analyze the current state of transitional care for young persons with CP, including (1) healthcare-related, functional, and social outcomes of transition-aged patients; (2) patient, caregiver, and provider perspectives; and (3) structure and efficacy of existing transition-based interventions.
Methods
Search strategy
A systematic review was conducted using PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [17] to investigate the current state of transitional care for young persons with CP and current healthcare attitudes. Three databases were searched in December 2020: PubMed MEDLINE (National Library of Medicine), Embase (Elsevier), and Scopus (Elsevier). Search strategies for Embase and Scopus were adapted from the PubMed search strategy shown in Supplementary Table 1. Date, study type, and language limits were not applied. Searches were conducted using controlled vocabulary (MeSH), keywords, and keyword synonyms.
Screening
Duplicates were removed after search completion using the automated deduplication feature in Endnote X9 (Clarivate, London, UK). The remaining eligible studies were screened by title and abstract for relevance. Those selected for full-text review were screened using predetermined inclusion and exclusion criteria. Two authors, DLM and EW, completed both stages of screening. Conflicts were reconciled by discussion to achieve consensus.
Inclusion and exclusion criteria
Inclusion criteria were publications in or translated into English, with full text and abstract available, studying a transition-age patient population (between 16 and 24 years old) with the diagnosis of cerebral palsy and assessing healthcare use, functional or social outcomes, perspectives on transitional care, or current implementations of transitional care practices. Studies reporting data on adult and pediatric patients or for cerebral palsy and additional pathologies were included if definite outcomes for transition-age patients with cerebral palsy could be identified. Exclusion criteria were as follows: abstracts only, secondary literature, not assessing transition-age patients with cerebral palsy, and not reporting on specified outcomes.
Data extraction
Articles selected for final inclusion were assessed for bibliographic data, study design, participants, intervention where applicable, and outcome data. Outcome measures were specified a priori. The first primary outcome measure was transition readiness, which was assessed qualitatively via healthcare utilization metrics, social and functional outcomes, and patient, caregiver, and provider interviews and surveys. Healthcare utilization metrics included rates of primary care visits, hospital stays, specialist referrals and visits, and use of rehabilitation services. Social outcomes were assessed via level of social or community engagement, participation in support groups and activities, and relationship development. Functional outcomes were assessed via employment status, housing, and capacity to live independently, with consideration of Gross Motor Function Classification System (GMFCS) level. Key themes of interviews were summarized. Surveys ranged in structure and content, using various validated questionnaires, scales, or both. The second primary outcome measure was efficacy of existing transitional care interventions, which was assessed qualitatively via survey responses from program administrators, providers, patients, and caregivers.
Statistical analysis
Data was analyzed descriptively. Means were calculated as weighted means and reported with range when available. As data was heterogenous by study design and execution, data were not pooled, and a meta-analysis was not conducted.
Quality assessment
The income status for countries of study origin was determined using the World Bank designation [18]. Quality and risk of bias were assessed using the GRADE framework [19] and Cochrane ROBINS-I (Risk of Bias in Non-Randomized Studies of Interventions) tool [20] for each of the included studies. Overall risk of bias for this systematic review was inferred based on risk of bias of each included study.
Results
Search results
The search identified 3151 articles, of which 27 were included (Fig. 1, Tables 1, 2, and 3) [21–47]. Study designs included longitudinal cohort (3, 11.1%), cross-sectional survey (10, 37.0%), qualitative interview (10, 37.0%), retrospective analysis (3, 11.1%), and retrospective cohort (1, 3.7%). All included studies originated from high-income countries, including the USA (9, 33.3%), the UK (7, 25.9%), Canada (4, 14.8%), Sweden (3, 11.1%), Scotland (1, 3.7%), Denmark (1, 3.7%), France (1, 3.7%), and the Netherlands (1, 3.7%). Twenty-three of the included studies [21–25, 27–29, 31–38, 40–44, 46, 47] (85.2%) assessed transition-aged persons with CP and four studies [26, 30, 39, 45] (14.8%) assessed transitional care interventions. The quality of most studies was moderate (12, 44.4%). Most studies had a moderate risk of bias (12, 44.4%), resulting in this review having a moderate risk of bias as well.
Fig. 1.
PRISMA flowchart outlining the search and review process used to identify and select articles for inclusion in the systematic review
Table 1.
Studies with transition-associated metrics as outcome measures included in the review
| Reference | Country | H/L/MIC | Study design | Quality | Bias risk | Patients, N | Mean Age, yrs (range) | GMFCS level, N | Cohort | Key findings |
|---|---|---|---|---|---|---|---|---|---|---|
| Alriksson et al. (2014) [21] | Sweden | High | Longitudinal cohort | High | Low | 102 | 20.6 median (18.3–23.7) | I, 38; II, 21; III, 13; IV, 10; V, 20 | Participants of a CP follow-up program | Living arrangements differed significantly among GMFCS levels. 70% of participants with severe disabilities lived with their parents. 90% of employed participants had a GMFCS level of I–II |
| Colver et al. (2018) [29] | UK | High | Longitudinal cohort | High | Low | 74 | 19.1 (16.1–22.0) | Not provided | Young persons with CP | Parent involvement was significantly associated with wellbeing. Satisfaction with services was significantly associated with promotion of health self-efficacy. Meeting the adult team before transfer was significantly associated with participation in arranging personal care |
| Donkervoort et al. (2009) [32] | Netherlands | High | Cross-sectional survey | High | Low | 81 | 20.4 (18.0–22.0) | I, 63; II, 7; III, 5; IV, 5; V, 1 | Young persons with CP with normal intelligence (IQ > 70) | Young adults with CP significantly lagged peers in development of housing, employment, and intimate relationships. 50% of participants did not visit a rehab physician in the previous year and only 33% visited a rehab physician in adult care |
| Goodman et al. (2011) [33] | USA | High | Cross-sectional survey | High | Low | 1300 | (18.0–21.0) | Not provided | Young persons with CP | Hospital utilization increased significantly among transitional age patients with CP in terms of number of annual discharges, inpatient days, and charges |
| Ko et al. (2004) [34] | UK | High | Qualitative interview | Moderate | Moderate | 11 | (15.0–17.0) | Not provided | Young persons with CP on school leave with physical disabilities | 49 potential referrals to adult specialist services were identified, but 17 were not made as such services did not exist. Adult physiotherapy and OT services were under-provided |
| Liljenquist et al. (2018) [36] | USA | High | Retrospective analysis | Moderate | Moderate | 35,290 | (13.0–18.0 at wave 1, 21.0–26.0 at wave 5) | Not provided | Young persons with CP in school (wave 1) and out of school (wave 5) | 59.4% of the youth utilized PT services; only 33.7% of them reported using PT since leaving secondary school. Female sex and use of a mobility device were significantly associated with PT use post-high school |
| McDowell et al. (2015) [37] | UK | High | Cross-sectional survey | Moderate | Moderate | 123 | 16.2 (4.0–27.0) | IV, 55; V, 68 | Young persons with CP and their parents | There was a significant decrease in access to specialists between the adolescent age group and the young adult age group |
| Merrick et al. (2015) [38] | UK | High | Cross-sectional survey | Moderate | Moderate | 106 | 16.5 (14.0–18.9) | I, 25; II, 42; III, 16; IV, 11; V, 2; unclassified, 10 | Young persons with CP | The median “gap” score between ideal and current care for physical environment and care processes was 1.0 when rated by young persons with CP. Parents’ satisfaction was significantly lower than their children’s |
| Blackman et al. (2013) [25] | USA | High | Cross-sectional survey | High | Low | 80 | (15.0–18.0) | Not provided | Parents of young persons with CP | 29% reported that their doctors discussed their child eventually seeing adult providers. 42% reported their doctors have discussed changing healthcare needs as the child ages |
| Roquet et al. (2018) [41] | France | High | Retrospective analysis | Moderate | Moderate | 512 | (2.0–40.0 +) | I–III, 277; IV/V, 235 | Family members and individuals with CP | Use of medication increased, while physical types of healthcare decreased with age, independent of GMFCS status |
| Solanke et al. (2018) [42] | UK | High | Cross-sectional survey | Moderate | Moderate | 106 | 16.4 (14.0–18.9) | I, 53; II, 20; III, 15; IV/V, 18 | Family members and individuals with CP | Highest areas of unmet needs were for management of pain, bone or joint problems, and speech, and were associated with increased severity of motor impairment and attending non-specialist education |
| Warschausky et al. (2017) [44] | USA | High | Cross-sectional survey | Moderate | Moderate | 43 | 18.63 | I, 19; II, 11; III, 4; IV, 9; V, 0 | Parents and young persons with CP | TRAQ scores in the CP population indicated poor transition readiness for self-management but sufficient readiness in self-advocacy |
| Young et al. (2007) [46] | Canada | High | Retrospective cohort | High | Low | 1064 total; youth 587, adults 477 | Youth 15.4 (13.0–17.0); adults 26.3 (23.0–32.0) | Not specified for most of the sample | Youth and adults with CP | Adults had a significantly higher rate of GP visits and annual physicals compared to youth and a lower rate of specialist and pediatrician visits. Specialists provided 28.4% of youth visits but only 18.8% of adult visits |
| Young et al. (2010) [47] | Canada | High | Cross-sectional survey | High | Low | 199 total; youth 129, adults 70 | Youth 15.5 (13.0–17.0); adults 26.6 (23.0–33.0) | Youth: I–III, 68; IV/V, 61; adults: I–III, 39; IV/V, 31 | Youth and adults with CP | SRH was reported to be excellent or very good by 57% of youth and 46% of adults |
N refers to the number of patients in each study, H/L/MIC high/low/middle income country, SRH self-rated health, CP cerebral palsy, GP general practitioner, TRAQ Transition Readiness Assessment Questionnaire, GMFCS Gross Motor Function Classification System, PT physical therapy, IQ intelligence quotient, OT occupational therapy
Table 2.
Qualitative interview or survey-type studies on patient, caregiver, or provider perceptions of their experiences with transitional care
| Reference | Country | H/L/MIC | Study design | Quality | Bias risk | Patients, N | Mean age, yrs (range) | GMFCS | Cohort | Key themes |
|---|---|---|---|---|---|---|---|---|---|---|
| Bagatell et al. (2016) [22] | USA | High | Qualitative interview | Moderate | Moderate | 9 | 26.2 (19.0–33.0) | I, 4; II, 1; III, 0; IV, 2; V, 2 | Young adults with CP who graduated from high school | Being thrust into adulthood, difficulty with navigating systems and services, understanding and managing my body, and dealing with stereotypes and prejudice |
| Bjorquist et al. (2015) [23] | Sweden | High | Qualitative interview | Low | High | 12 | (17.0–18.0) | Not provided | Young adults with CP | Looking forward to being an adult, but not feeling ready yet; belonging to a family means security but may be “too much”; socializing and love are necessary but not always possible; ADL are manageable but challenging; surrounded by support but don’t know what’s going on; hopes for the future but a desire for steppingstones |
| Bjorquist et al. (2016) [24] | Sweden | High | Qualitative interview | Low | High | 10 | (17.0–18.0) | I, 8; II, 3; III, 1; IV, 1; V, 2 | Parents of young adults with CP | “Friction blisters chafing and healing during transition.” Five subthemes: concern and sorrow, stress and suffering in daily life, worries about what was to come, desire for help, strategies for coping and cohesion |
| Brandon et al. (2019) [27] | Canada | High | Qualitative interview | Moderate | Moderate | 7 | 20.0 (18.0–30.0) | IV, 5; V, 2 | Young adults with CP, parents of young adults with CP, pediatricians and PCPs | All participant groups reported transition challenges with respect to accessibility, the suitability of some primary care environments for caring for individuals with complex care needs, gaps in seamless care, and limited time and funding when receiving or providing primary care services to young adults with CP |
| Carroll et al. (2015) [28] | USA | High | Qualitative interview | Moderate | Moderate | 9 | (19.0–25.0) | Not provided | Young adults with CP | Expert novices, evidence/experience-based expectations, negotiating new systems, interdependence, and accepting less than was expected |
| Difazio et al. (2014) [31] | USA | High | Qualitative interview | Low | High | 13 | 32.0 (24.0–44.0) | Not provided | Young adults with CP, parents of young adults with CP | Lost in Transition, Roadmap to Care, List of None, and One Stop Shopping |
| Lariviere et al. (2013) [35] | Canada | High | Qualitative interview | Low | High | 14 | 20.9 (18.0–25.0) | Not provided | Young adults with CP | Transition envisaged with fear and apprehension, lack of cooperation between providers in the pediatric and adult healthcare systems, lack of support during transition, improper management of medical records, and feelings of abandonment |
| Normann et al. (2020) [40] | Denmark | High | Qualitative interview | Low | High | 6 | 25.8 (21.0–31.0) | I, 2; II, 1; III, 1; IV, 2 | Young adults with CP | Being a young adult, development in physical disability and new challenges in adulthood, and navigating the healthcare system |
| Stevenson et al. (1997) [43] | UK | High | Cross-sectional survey | Moderate | Moderate | 74 | Young (15.0–18.0), older (20.0–22.0) | Not provided | Young adults with CP, parents of young adults with CP | Carers expressed anxieties about the provision of services, and frustration in obtaining information about help |
N refers to the number of patients in each study, H/L/MIC high/low/middle income country, CP cerebral palsy, GMFCS Gross Motor Function Classification System, ADL activities of daily living
Table 3.
Studies assessing current implementations of transitional care or structured transition programs for young persons with cerebral palsy included in this review
| Reference | Country | H/L/MIC | Study design | Quality | Bias risk | Participants, N (type) | Key findings |
|---|---|---|---|---|---|---|---|
| Bolger et al. (2016) [26] | USA | High | Cross-sectional survey | Moderate | Moderate | 11 (clinics) | Top 3 perceived barriers to successful TOC were limited adult providers willing to accept CP patients, concern about the level of care in the adult healthcare system, and lack of financial resources. 55% of clinics had structured transition programs, but only one transitioned 100% of their patients to adult providers by age 22. 40% of clinics had transitioned < 25% of their patients with CP to adult providers by age 22. Only one clinic had an absolute upper age limit for seeing patients, and 36% of clinics accepted new patients older than 21. No respondents were “completely satisfied” with their transition process and only one was “moderately satisfied.” |
| Colver et al. (2018) [30] | UK | High | Longitudinal cohort | High | Low | 85 (patients) | The nine proposed beneficial features of transition services were poorly provided. Fewer than half of services stated they provided an age-banded clinic, written transition plan, transition manager for clinical team, a protocol for promotion of health self-efficacy, or holistic life-skills training. Young people reported that they had not experienced the features which services said they provided. Agreement for written transition plan, holistic life-skills training and key worker was 30, 43, and 49%, respectively. Agreement was better for appropriate parent involvement, age-banded clinic, promotion of health self-efficacy, and coordinated team at 77, 77, 80, and 69% respectively |
| Morton et al. (2021) [39] | USA | High | Retrospective analysis | High | Low | 1 (clinic) | More than 2/3 of families received services in seven categories: support primary care, specialty care, school, legal, community inclusion, healthcare financing, and providing medical care. Workplace, direct service providers and healthcare financing case workers received the least attention |
| Wright et al. (2015) [45] | Scotland | High | Qualitative interview | High | Low | 13 (clinics) | Key areas in need of improvement were coordination and communication within health services and between health services and educational, social services and adult health services to which young people were transitioning |
N refers to the number of participants in each study, H/L/MIC high/low/middle income country, CP cerebral palsy, TOC transition of care
Patient demographics
The 23 included studies (85.2%) assessing transition-aged persons with CP consisted of 39,245 adolescent and young adult patients with cerebral palsy (Tables 1 and 2). The mean age of study participants at time of assessment ranged from 2 to 44 years old, with a weighted mean of 19.6 years. Nine studies [23–25, 28, 33, 34, 36, 41, 43] (39.1%) did not report a mean age. Six studies [32, 34, 37, 41, 43, 44] (26.1%) classified participants by cerebral palsy subtype, of which 72.7% (614/844) were spastic, 10.5% (89/844) were dyskinetic, 3.5% (29/844) were ataxic, 9.8% (83/844) were classified as “other,” and 3.5% (29/844) were unclassifiable. Additionally, 12 studies [21, 22, 24, 27, 32, 37, 38, 40–42, 44, 47] (52.2%) classified participants according to GMFCS level, of which 58.1% (757/1304) were levels I–III (mild/moderate impairment, ambulatory), 41.2% (537/1304) were level IV/V (severe impairment, non-ambulatory), and 0.8% (10/1304) were unclassifiable.
Transition-associated healthcare metrics
Forty-two percent of parents of transition-age youth with CP reported their doctors having discussed the changing healthcare needs of their child as they aged [25]. However, only 28–29% reported that their doctors had discussed the eventual need to see adult providers or had provided help in coordinating transitional care [25]. Nonetheless, 64% of participants were able to formulate their care demands themselves [32]. Higher level of motor functioning, higher level of education, participation in activities, parent involvement, satisfaction with services, and meeting the adult team before transfer were associated with increased participation and independence in formulating personal care plans [29, 32].
Adults with CP had a significantly higher rate of both GP visits and annual physicals compared to pre-transition young persons, but the total rate of physician visits was not significantly different between age groups [46]. Hospital utilization increased significantly among transitional age patients with CP in terms of number of annual discharges, inpatient days, and charges [33].
Comparatively, there was a significant decrease in both access and number of visits to specialists by young adults compared to pre-transition youth [37, 41, 46]. Specialists provided 28.4% of youth visits but only 18.8% of adult visits [46]. 34.7% of specialist referrals were unable to be made as such services did not exist for adult patients [34]. Adult physiotherapy and occupational therapy services were particularly under-provided [34]. Use of rehabilitation services decreased with age, independently of GMFCS status, while use of psychotropic and analgesic medication increased with age [32, 34, 36, 41, 43]. The highest areas of unmet needs in specialty care were for management of pain, bone or joint problems, and speech [42].
Transition-associated social and functional outcomes
Young adults with CP significantly lagged non-CP peers in their development of housing, employment, and intimate relationships [32]. Use of formal respite services, support groups, and youth clubs was also relatively poor [37]. Social engagement decreased with age [43]. Living arrangements differed significantly among GMFCS levels, with 70% of participants with severe disability living with their parents [21]. Nonetheless, 55.9% of young adults with CP lived with their parents overall [21, 22]. Unmet needs in daily living healthcare and personal assistance were associated with increased severity of motor impairment (GMFCS) and attending non-specialist education [21, 42]. Unmet needs tended to increase over time but were not significantly related to whether the young person had transferred from child services [42]. One representative cohort of young adults with CP was 34.3% students, 19.6% employed, 35.2% participating in daily activities, and 8.8% unemployed, with 90% of employed participants having a GMFCS level of I–II [21].
Qualitative interview key themes
Five studies [22, 23, 28, 35, 40] assessed attitudes of young adults with CP regarding their lived transition experiences. Shared themes included a lack of transition readiness and support, becoming a young adult and associated challenges, progression of physical disability, struggling to navigate the healthcare system, and feelings of isolation and abandonment.
Four studies [24, 31, 38, 43] assessed parents and caregiver attitudes towards their child’s transition from pediatric to adult healthcare services. Overarching themes included anxiety about service provisions, difficulty obtaining help and informational resources, poor communication and transparency from healthcare providers, the lack of coping skills, and a desire for community support. Parents also reported significantly lower satisfaction with current transition care processes than their children [38].
One study [27] included the provider perspective on transition challenges for young adults with CP. Themes included problems with accessibility, the suitability of primary care environments for caring for individuals with complex needs, gaps in seamless care, and limited time and funding when receiving or providing primary care services to young adults with CP.
Outcomes of current transition programs
Four studies [26, 30, 39, 45] assessed current implementations of transitional care practice (Table 3). The top three perceived barriers to successful transition of care included limited adult providers willing to accept CP patients, concern about the level of care in the adult healthcare system, and the lack of financial resources [26]. One survey [26] of 11 clinics across the USA found that 55% of clinics had structured transition programs, but only one program successfully transitioned 100% of their patients to adult providers by age 22. Forty percent of the clinics had transitioned < 25% of their patients with CP to adult providers by age 22 [26]. Only one clinic had an absolute upper age limit for seeing patients, and 36% of clinics accepted new patients older than 21 [26]. None of the responding providers were “completely satisfied” with their transition process [26].
Significant gaps existed between the advertised services and the experiences of young people utilizing them [30]. Proposed beneficial features of transition services included a written transition plan, holistic life-skills training, and having a key worker, which only 30, 43, and 49% of young people agreed were available to them, respectively [30]. Agreement was better for appropriate parent involvement, age-banded clinic, promotion of health self-efficacy, and coordinated team at 77, 77, 80, and 69%, respectively [30]. Comparatively, a retrospective evaluation [39] of another transition clinic demonstrated that more than 2/3 of families reported receiving services across seven categories: support primary care, specialty care, school, legal, community inclusion, healthcare financing, and providing medical care. Key areas identified for improvement included coordination and communication between and within health services [45].
Discussion
We present a systematic review of the state of transitional care for young persons with CP. To the best of our knowledge, this is the first systematic review on the topic. We emphasize three primary findings. First, the current state of transitional care for young adults with CP is inadequate, a perception shared by patients, caregivers, and providers. Second, key barriers to successful transition include poor communication between pediatric and adult provider teams, the lack of resources for coordinating and navigating care or for creating space for accommodating physical needs, and few providers for patients with CP or education on caring for adults with CP. Third, critical interventions to improve transitional care include early discussion and transition planning with pediatricians, community engagement and training, assigning a patient navigator or case worker to transition-age patients, and establishment of best practice guidelines to standardize existing transition programs.
Current state of transitional care
Consistently, young adults with CP have expressed not feeling ready for the transition to adulthood [22–24, 27, 28, 31, 35, 40, 43, 44], as well as a desire for a comprehensive transition approach that prioritizes capacity building and personal empowerment [22–24, 28, 29, 31, 35]. However, the results of this review demonstrate that the current state of transitional care is insufficient to meet the complex needs of young adults with CP. While many transition-age persons with CP and their caregivers are actively seeking both primary and specialty care, there is poor access [25–27, 30–38, 40–43]. Medical providers with the expertise, office and financial resources, and capacity or willingness to see young adults with CP are limited in quantity and location [25–27, 30–38, 40–43]. Furthermore, such providers may be difficult to identify, have long waiting lists, or be financially inaccessible. As a result, these patients are frequently being seen in the emergency room instead of by trained specialists equipped to manage their complex care needs [33]. While hospital staff may be able to manage short-term, emergent care in these patients, long-term goals of care and management are rarely addressed in this setting [48].
The impact of opportunities for improvement in transitional care is further illustrated by the social and functional outcomes of study participants after aging out of the pediatric system. A lack of early intervention to promote social and career development leaves many young adults with CP unable to manage independent living, build careers, form intimate relationships, or engage socially [21, 22, 24, 32, 37, 40, 43]. These findings were magnified in those with more severe disabilities [21, 32]. However, current literature suggests that many adults with CP can live independently and have a high quality of life, especially if they have a strong support system and continuous specialty care [49]. As such, transitional care for young adults with CP should include means to address their social, emotional, and financial needs as they navigate adulthood.
Those few structured transition-programs that do exist are notable, and geographic location and financial resources restrict wider availability [26]. Many of these programs accept patients with a wide range of chronic illnesses, so management may be difficult to tailor to individuals’ disease-specific needs [50]. Most clinics in the USA are in major cities, affiliated with large, well-resourced, academic institutions, and thus primarily serve urban populations. These factors can create additional barriers to access, including physical distance or financial challenges for travel. Even those with access to these programs report low rates of satisfaction with the transition process and support services [26, 30, 45], a sentiment reflected by caregivers and providers alike [24, 26, 27, 30, 31, 39, 43]. There is a need for continued evaluation and reform in transitional healthcare.
Barriers to successful transition
Many young adults with CP are lost to follow-up upon graduating from the pediatric healthcare system. The level of care coordination and close monitoring provided during childhood is often not continued or available to adults or older age groups, even in countries with universal healthcare coverage [51]. Many patients and their families may struggle to leave pediatric providers and multidisciplinary care teams with longitudinal relationships they have been with for their entire life and establish trust with a new provider or ecosystem. Release of records may be delayed or forgotten altogether as the time interval between providers grows [35]. As a result, transition planning tools that may have been constructed with the patient’s pediatric team are not optimally utilized. In addition, frameworks for transition of care exist, so the application of transition planning is not prescriptive. For instance, GotTransition.org outlines 6 domains, without a specific detailed way of making it happen. The implementation is thus variable based on many factors, including individuals, providers, and health system factors, which leaves the outcome somewhat to chance.
Young adults with CP struggle to navigate the complex terrain of the adult healthcare system, which assigns, functions, and delivers healthcare in significantly different ways than the pediatric system. Cognitive delay and worsening physical disability can create additional challenges for patients in the domains of self-advocacy, scheduling appointments, and coordinating their own care [51]. Aging out of “dependent” status on parent or caregiver insurance plans leaves many young adults with CP on public aid, requiring them to adapt their healthcare needs to newly limited provider coverage and benefits [51]. There is also generally greater support from ancillary services in pediatric care, such as social work, nurse coordinators, and resources for caregivers. However, similar resources are largely limited in the adult healthcare system, leading to increased demands on caregivers, stress, burnout, and difficulty managing their adolescent’s changing needs [24, 27, 43].
Providers also face obstacles in providing care, emphasizing lack of time, resources, financial reimbursement, and training [27, 52, 53]. Providers may consider themselves ill-equipped to manage young persons with CP due to limited education on treating spasticity, dystonia, and complex orthopedic issues in this population [53–55]. Additionally, persons with CP often require wheelchair-accessible entrances, exam rooms, exam equipment, and office personnel trained in proper patient handling techniques. These patients may also require longer appointments or have public insurance, which some providers may struggle to accommodate [27, 52, 53]. While the Americans with Disabilities Act (ADA) requires medical service providers in the USA to make their services accessible [56], similar statutes do not exist in every country or may be upheld to varying degrees [57].
Opportunities for intervention
Adults with CP require the expertise of both pediatric and adult-trained providers who are familiar with the pediatric and adult manifestations of the condition. As such, collaboration between pediatric and adult providers is crucial to transition success [26, 33]. Pediatricians should begin the discussion and planning for transition to adult healthcare early in adolescence, so as to identify possible barriers to care early on [25]. Additionally, pediatric providers can actively seek out adult care providers in their communities with an interest in caring for patients with CP to start a dialogue focused on potential barriers to care and work towards building local networks of CP providers [26]. Such a network could assist in facilitating patients meeting their adult teams prior to transfer, which has been significantly associated with increased participation in organizing their own care [29]. Convening a national focus group of pediatric and adult care providers to discuss and publish optimal transition processes could also be valuable [26].
Adult-training programs should continue to implement teaching on adult manifestations of pediatric conditions to accurately reflect the needs of today’s patient population. Mandating transition training at both the student and resident level, either via direct incorporation into a national curriculum or creation of a specialty certification program, is needed [55]. Essential elements of such a curriculum would include patient-family involvement in teaching, addressing critical issues regarding financing, and discussion of medical decision making for adults with varying degrees of dependence on caregivers and illness progression [58, 59]. Community providers with experience transitioning young persons with CP should serve as instructors and faculty mentors across specialties [55]. Certification could also be accessible via the completion of online training modules [58]. As transitional care for this population requires a multidisciplinary healthcare team, students and residents should practice providing and coordinating care in multidisciplinary settings [54, 59]. Mentors should assist students and residents interested in advocacy projects to identify opportunities for greater involvement and funding. In doing so, we can ensure there are ample adult providers with the comfort and competence to treat young adults with CP [25, 54].
Furthermore, transition of care protocols should be usable across various clinics and geographic areas, and not merely successful in one clinic or hospital system [26]. Once best practice guidelines have been established, standardized transition clinics designed around the complex care needs of adolescents and young adults with CP can be established. A comprehensive clinic would ideally address the health, vocational, and daily living needs of young adults with CP, including counseling, therapy, legal, and financial support services [22]. The provision of a “navigator” for parents and adolescents during their transition to adult healthcare services could be immensely helpful in facilitating use of multiple services [22, 24]. This intervention has been effective in transitional care for young adults with other chronic diseases of childhood, resulting in decreased loss to follow-up and significant improvement in mean transition readiness scores, disease knowledge, and confidence in both disease and pain management [1, 60]. Further quantitative and qualitative research, including possible trials and implementation science collaborations, are needed to elucidate the most effective interventions and program structure.
Recommendations for transitional care practices, based on the findings of this review, are summarized in Table 4.
Table 4.
Themes with cross-study consensus, associated subthemes, and recommendations for successful healthcare transition in young persons with cerebral palsy
| Global themes and subthemes | |||
|---|---|---|---|
| Overarching theme | Subthemes | Recommendations | |
| Patients | Transition readiness |
Attachment to pediatric team Fear of abandonment Lack of external support Not knowing what happens next |
Transition should be timed based on clinical milestones and emotional readiness, jointly determined by provider, patient and caregiver assessment, as opposed to age. Meeting the adult team before transfer, improved communication between pediatric and adult providers, written transition planning, and patient education on personal disease management may aid in transition readiness. Establishment of a comprehensive, standardized transition readiness assessment could also be useful |
| Becoming a young adult |
Progression of physical disability Stereotypes and prejudice Locating support for post-secondary education and employment Living independently—exciting but intimidating |
Successful transition should be holistic with emphasis on functional, social, and emotional support, as well as teach financial and healthcare planning to empower young adults to be self-sufficient. As transition clinics and longitudinal programs for young adults with CP are developed, these elements should be incorporated into the care model | |
| Navigating the healthcare system |
Encouraging independence but with limited guidance Locating experienced providers Understanding insurance benefits |
Successful transition must account for the individual’s barriers to care, including access and availability of specialists, proximity to healthcare facilities, disparity in policy, insurance restrictions, stigma, and financial resources. Assigning a care coordinator or transition navigator to each patient could alleviate stress and confusion and lend to more successful transition | |
| Caregivers | Isolation and abandonment |
Identifying supportive resources Communication with providers Coping skills Community support |
Assigning care coordinators or transition navigators to patients and their families, forming parent support groups as part of transition clinics or as online communities, and improved provider education on caring for young adults with CP can help alleviate caregiver stress and burnout |
| Providers | Accessibility |
Care environment suitability Available time Funding |
Expansion of public insurance benefits, healthcare policy reform, and increased private and public funding sources are needed to support the financial burden of providing complex care |
| Training |
Provider education Network for seamless care |
Development of accessible educational resources, such as a free, online certification course, and incorporation of transitional care training into the teaching curriculum of residency programs is needed to expand the network of providers comfortable treating young adults with CP. Providers with this special certification are added to a searchable registry for patients seeking care | |
Limitations
There are several limitations to this review. As only published full-text studies were included, results are at risk for publication bias. Studies not written or translated into English were excluded from this review, potentially resulting in missed findings on the presence and efficacy of transition programs in other countries. Included studies had an overall moderate risk of bias given that the majority were descriptive or qualitative in nature. None of the included studies were randomized controlled trials, which are necessary to provide the highest-quality evidence on successful transition measures and associated outcome data. These elements limit our ability to detect potential differences in race, gender, or institution. Some of the included studies excluded children with varying degrees of cognitive impairment and/or functional status. Additionally, there was extensive variety in the measures and tools used to assess transition readiness across studies. Data from low- or middle-income countries were lacking. While many high-income countries have begun to implement healthcare transition-type programs, a notable worldwide gap still exists due to limited data from resource-limited areas [61, 62]. Despite these limitations, strict PRISMA guidelines were followed to systematically assess and provide a comprehensive analysis of the published literature. Future studies should develop and evaluate contextually appropriate, comprehensive, transitional readiness tools and care models [63–66].
Conclusions
Although people with CP may attain a high quality of life and a degree of independence, current transitional care paradigms are often insufficient. A flexible, individualized, transition period should be employed for each person with CP. Additionally, there is a need for evidence-based transition strategies, long-term care planning, and financial and educational resources.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contribution
All authors contributed to the study conception and design. Material preparation and data collection were performed by Devon L. Mitchell, Nathan A. Shlobin, and Emily Winterhalter. Analysis was performed by Devon L. Mitchell. The first draft of the manuscript was written by Devon L. Mitchell, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Data availability
Data regarding the systematic review can be available upon request.
Declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Footnotes
Previous presentations: No part of this work has been previously published.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hutton JL, Pharoah PO. Life expectancy in severe cerebral palsy. Arch Dis Child. 2006;91(3):254–258. doi: 10.1136/adc.2005.075002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rosenbaum P. Cerebral palsy: what parents and doctors want to know. BMJ. 2003;326(7396):970–974. doi: 10.1136/bmj.326.7396.970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Strauss DJ, Shavelle RM, Anderson TW. Life expectancy of children with cerebral palsy. Pediatr Neurol. 1998;18(2):143–149. doi: 10.1016/s0887-8994(97)00172-0. [DOI] [PubMed] [Google Scholar]
- 4.Steinbeck KS, Brodie L, Towns SJ. Transition in chronic illness: who is going where? J Paediatr Child Health. 2008;44(9):478–482. doi: 10.1111/j.1440-1754.2008.01321.x. [DOI] [PubMed] [Google Scholar]
- 5.Myers LL, Nerminathan A, Fitzgerald DA, et al. Transition to adult care for young people with cerebral palsy. Paediatr Respir Rev. 2020;33:16–23. doi: 10.1016/j.prrv.2019.12.002. [DOI] [PubMed] [Google Scholar]
- 6.Smith SE, Gannotti M, Hurvitz EA, et al. Adults with cerebral palsy require ongoing neurologic care: a systematic review. Ann Neurol. 2021;89(5):860–871. doi: 10.1002/ana.26040. [DOI] [PubMed] [Google Scholar]
- 7.Speyer R, Cordier R, Kim JH, Cocks N, Michou E, Wilkes-Gillan S. Prevalence of drooling, swallowing, and feeding problems in cerebral palsy across the lifespan: a systematic review and meta-analyses. Dev Med Child Neurol. 2019;61(11):1249–1258. doi: 10.1111/dmcn.14316. [DOI] [PubMed] [Google Scholar]
- 8.Pizzighello S, Pellegri A, Vestri A et al (2019) Becoming a young adult with cerebral palsy. Res Dev Disabil. 92:103450. 10.1016/j.ridd.2019.103450 [DOI] [PubMed]
- 9.Shevell M (2018) Cerebral palsy to cerebral palsy spectrum disorder: time for a name change? [published online ahead of print, 19 Dec 2018]. Neur. 10.1212/WNL.0000000000006747
- 10.Wafa S, Nakhla M. Improving the transition from pediatric to adult diabetes healthcare: a literature review. Can J Diabetes. 2015;39(6):520–528. doi: 10.1016/j.jcjd.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 11.Campagna BR, Weatherley K, Shemesh E, Annunziato RA. Adherence to medication during transition to adult services. Paediatr Drugs. 2020;22(5):501–509. doi: 10.1007/s40272-020-00414-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.White PH, Cooley WC (2018) TRANSITIONS CLINICAL REPORT AUTHORING GROUP; AMERICAN ACADEMY OF PEDIATRICS; AMERICAN ACADEMY OF FAMILY PHYSICIANS; AMERICAN COLLEGE OF PHYSICIANS. Supporting the Health Care Transition From Adolescence to Adulthood in the Medical Home [published correction appears in Pediatrics. 2019 Feb;143(2):]. Pediatrics. 2018;142(5):e20182587. 10.1542/peds.2018-2587 [DOI] [PubMed]
- 13.Carter B, Bennett CV, Jones H, et al. Healthcare use by children and young adults with cerebral palsy. Dev Med Child Neurol. 2021;63(1):75–80. doi: 10.1111/dmcn.14536. [DOI] [PubMed] [Google Scholar]
- 14.Gill J, Morgan P, Enticott J. Emergency department usage by adults with cerebral palsy: a retrospective cohort study. Emerg Med Australas. 2022;34(2):169–175. doi: 10.1111/1742-6723.13832. [DOI] [PubMed] [Google Scholar]
- 15.Levy BB, Song JZ, Luong D et al (2020) Transitional care interventions for youth with disabilities: a systematic review. Pediatr 146(5):e20200187. 10.1542/peds.2020-0187 [DOI] [PubMed]
- 16.Kingsnorth S, Lindsay S, Maxwell J et al (2021) Bridging pediatric and adult rehabilitation services for young adults with childhood-onset disabilities: evaluation of the LIFEspan Model of Transitional Care. Front Pediatr 9:728640. Published 17 Sep 2021. 10.3389/fped.2021.728640 [DOI] [PMC free article] [PubMed]
- 17.Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. Published 29 Mar 2021. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed]
- 18.The world by income and region. WDI - the world by income and region. Accessed 5 Dec 2022. https://datatopics.worldbank.org/world-development-indicators/the-world-by-income-and-region.html
- 19.Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sterne JA, Hernán MA, Reeves BC et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:i4919. Published 12 Oct 2016. 10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed]
- 21.Alriksson-Schmidt A, Hägglund G, Rodby-Bousquet E, Westbom L. Follow-up of individuals with cerebral palsy through the transition years and description of adult life: the Swedish experience. J Pediatr Rehabil Med. 2014;7(1):53–61. doi: 10.3233/PRM-140273. [DOI] [PubMed] [Google Scholar]
- 22.Bagatell N, Chan D, Rauch KK, Thorpe D. “Thrust into adulthood”: transition experiences of young adults with cerebral palsy. Disabil Health J. 2017;10(1):80–86. doi: 10.1016/j.dhjo.2016.09.008. [DOI] [PubMed] [Google Scholar]
- 23.Björquist E, Nordmark E, Hallström I. Living in transition - experiences of health and well-being and the needs of adolescents with cerebral palsy. Child Care Health Dev. 2015;41(2):258–265. doi: 10.1111/cch.12151. [DOI] [PubMed] [Google Scholar]
- 24.Björquist E, Nordmark E, Hallström I. Parents’ experiences of health and needs when supporting their adolescents with cerebral palsy during transition to adulthood. Phys Occup Ther Pediatr. 2016;36(2):204–216. doi: 10.3109/01942638.2015.1101041. [DOI] [PubMed] [Google Scholar]
- 25.Blackman JA, Conaway MR. Adolescents with cerebral palsy: transitioning to adult health care services. Clin Pediatr (Phila) 2014;53(4):356–363. doi: 10.1177/0009922813510203. [DOI] [PubMed] [Google Scholar]
- 26.Bolger A, Vargus-Adams J, McMahon M. Transition of care in adolescents with cerebral palsy: a survey of current practices. PM R. 2017;9(3):258–264. doi: 10.1016/j.pmrj.2016.08.001. [DOI] [PubMed] [Google Scholar]
- 27.Brandon E, Ballantyne M, Penner M, Lauzon A, McCarvill E (2019) Accessing primary health care services for transition-aged young adults with cerebral palsy; perspectives of young adults, parents, and physicians. J Transit Med 1(1). 10.1515/jtm-2019-0004
- 28.Carroll EM. Health care transition experiences of young adults with cerebral palsy. J Pediatr Nurs. 2015;30(5):e157–e164. doi: 10.1016/j.pedn.2015.05.018. [DOI] [PubMed] [Google Scholar]
- 29.Colver A, McConachie H, Le Couteur A et al (2018) A longitudinal, observational study of the features of transitional healthcare associated with better outcomes for young people with long-term conditions. BMC Med 16(1):111. Published 23 Jul 2018. 10.1186/s12916-018-1102-y [DOI] [PMC free article] [PubMed]
- 30.Colver A, Pearse R, Watson RM et al (2018) How well do services for young people with long term conditions deliver features proposed to improve transition?. BMC Health Serv Res 18(1):337. Published 8 May 2018. 10.1186/s12913-018-3168-9 [DOI] [PMC free article] [PubMed]
- 31.DiFazio RL, Harris M, Vessey JA, Glader L, Shanske S. Opportunities lost and found: experiences of patients with cerebral palsy and their parents transitioning from pediatric to adult healthcare. J Pediatr Rehabil Med. 2014;7(1):17–31. doi: 10.3233/PRM-140276. [DOI] [PubMed] [Google Scholar]
- 32.Donkervoort M, Wiegerink DJ, van Meeteren J, Stam HJ, Roebroeck ME (2009) Transition Research Group South West Netherlands. Transition to adulthood: validation of the Rotterdam transition profile for young adults with cerebral palsy and normal intelligence. Dev Med Child Neurol 51(1):53–62. 10.1111/j.1469-8749.2008.03115.x [DOI] [PubMed]
- 33.Goodman DM, Hall M, Levin A, et al. Adults with chronic health conditions originating in childhood: inpatient experience in children’s hospitals. Pediatrics. 2011;128(1):5–13. doi: 10.1542/peds.2010-2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ko B, McEnery G. The needs of physically disabled young people during transition to adult services. Child Care Health Dev. 2004;30(4):317–323. doi: 10.1111/j.1365-2214.2004.00422.x. [DOI] [PubMed] [Google Scholar]
- 35.Larivière-Bastien D, Bell E, Majnemer A, Shevell M, Racine E. Perspectives of young adults with cerebral palsy on transitioning from pediatric to adult healthcare systems. Semin Pediatr Neurol. 2013;20(2):154–159. doi: 10.1016/j.spen.2013.06.009. [DOI] [PubMed] [Google Scholar]
- 36.Liljenquist K, O’Neil ME, Bjornson KF. Utilization of physical therapy services during transition for young people with cerebral palsy: a call for improved care into adulthood. Phys Ther. 2018;98(9):796–803. doi: 10.1093/ptj/pzy068. [DOI] [PubMed] [Google Scholar]
- 37.McDowell BC, Duffy C, Parkes J. Service use and family-centred care in young people with severe cerebral palsy: a population-based, cross-sectional clinical survey. Disabil Rehabil. 2015;37(25):2324–2329. doi: 10.3109/09638288.2015.1019649. [DOI] [PubMed] [Google Scholar]
- 38.Merrick H, McConachie H, Le Couteur A et al (2015) Characteristics of young people with long term conditions close to transfer to adult health services. BMC Health Serv Res 15:435. Published 30 Sep 2015. 10.1186/s12913-015-1095-6 [DOI] [PMC free article] [PubMed]
- 39.Morton B, Damato EG, Ciccarelli MR, Currie J. Care coordination for children with special healthcare needs anticipating transition: a program evaluation. J Pediatr Nurs. 2021;61:7–14. doi: 10.1016/j.pedn.2021.02.024. [DOI] [PubMed] [Google Scholar]
- 40.Normann G, Arntz Boisen K, Uldall P, Brødsgaard A (2020) Navigating being a young adult with cerebral palsy: a qualitative study. Int J Adolesc Med Health 34(4):187–195. Published 4 Sep 2020. 10.1515/ijamh-2020-0039 [DOI] [PubMed]
- 41.Roquet M, Garlantezec R, Remy-Neris O, et al. From childhood to adulthood: health care use in individuals with cerebral palsy. Dev Med Child Neurol. 2018;60(12):1271–1277. doi: 10.1111/dmcn.14003. [DOI] [PubMed] [Google Scholar]
- 42.Solanke F, Colver A, McConachie H (2018) Transition collaborative group. Are the health needs of young people with cerebral palsy met during transition from child to adult health care?. Child Care Health Dev 44(3):355–363. 10.1111/cch.12549 [DOI] [PMC free article] [PubMed]
- 43.Stevenson CJ, Pharoah PO, Stevenson R. Cerebral palsy–the transition from youth to adulthood. Dev Med Child Neurol. 1997;39(5):336–342. doi: 10.1111/j.1469-8749.1997.tb07441.x. [DOI] [PubMed] [Google Scholar]
- 44.Warschausky S, Kaufman JN, Schutt W, Evitts M, Hurvitz EA. Health self-management, transition readiness and adaptive behavior in persons with cerebral palsy or myelomeningocele. Rehabil Psychol. 2017;62(3):268–275. doi: 10.1037/rep0000157. [DOI] [PubMed] [Google Scholar]
- 45.Wright AE, Robb J, Shearer MC. Transition from paediatric to adult health services in Scotland for young people with cerebral palsy. J Child Health Care. 2016;20(2):205–213. doi: 10.1177/1367493514564632. [DOI] [PubMed] [Google Scholar]
- 46.Young NL, Gilbert TK, McCormick A, et al. Youth and young adults with cerebral palsy: their use of physician and hospital services. Arch Phys Med Rehabil. 2007;88(6):696–702. doi: 10.1016/j.apmr.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 47.Young NL, Rochon TG, McCormick A, Law M, Wedge JH, Fehlings D. The health and quality of life outcomes among youth and young adults with cerebral palsy. Arch Phys Med Rehabil. 2010;91(1):143–148. doi: 10.1016/j.apmr.2009.08.152. [DOI] [PubMed] [Google Scholar]
- 48.Bowlyow JE. Acute and long-term care linkages: a literature review. Med Care Rev. 1990;47(1):75–103. doi: 10.1177/107755879004700105. [DOI] [PubMed] [Google Scholar]
- 49.Pettersson K, Rodby-Bousquet E (2021) Living conditions and social outcomes in adults with cerebral palsy. Front Neurol 12:749389. Published 21 Oct 2021 . 10.3389/fneur.2021.749389 [DOI] [PMC free article] [PubMed]
- 50.Scal P, Evans T, Blozis S, Okinow N, Blum R. Trends in transition from pediatric to adult health care services for young adults with chronic conditions. J Adolesc Health. 1999;24(4):259–264. doi: 10.1016/s1054-139x(98)00127-x. [DOI] [PubMed] [Google Scholar]
- 51.McManus MA, Pollack LR, Cooley WC, et al. Current status of transition preparation among youth with special needs in the United States. Pediatrics. 2013;131(6):1090–1097. doi: 10.1542/peds.2012-3050. [DOI] [PubMed] [Google Scholar]
- 52.Green Corkins K, Miller MA, Whitworth JR, McGinnis C. Graduation day: healthcare transition from pediatric to adult. Nutr Clin Pract. 2018;33(1):81–89. doi: 10.1002/ncp.10050. [DOI] [PubMed] [Google Scholar]
- 53.Szalda DE, Jimenez ME, Long JE, Ni A, Shea JA, Jan S. Healthcare system supports for young adult patients with pediatric onset chronic conditions: a qualitative study. J Pediatr Nurs. 2015;30(1):126–132. doi: 10.1016/j.pedn.2014.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hunt S, Sharma N. Pediatric to adult-care transitions in childhood-onset chronic disease: hospitalist perspectives. J Hosp Med. 2013;8(11):627–630. doi: 10.1002/jhm.2091. [DOI] [PubMed] [Google Scholar]
- 55.Patel MS, O'Hare K. Residency training in transition of youth with childhood-onset chronic disease. Pediatrics. 2010;126(Suppl 3):S190–S193. doi: 10.1542/peds.2010-1466P. [DOI] [PubMed] [Google Scholar]
- 56.Pharr JR (2013) Accommodations for patients with disabilities in primary care: a mixed methods study of practice administrators. Glob J Health Sci 6(1):23–32. Published 8 Oct 2013. 10.5539/gjhs.v6n1p23 [DOI] [PMC free article] [PubMed]
- 57.Adugna MB, Nabbouh F, Shehata S, Ghahari S (2020) Barriers and facilitators to healthcare access for children with disabilities in low and middle income sub-Saharan African countries: a scoping review. BMC Health Serv Res 20(1):15. Published 2020 Jan 6. 10.1186/s12913-019-4822-6 [DOI] [PMC free article] [PubMed]
- 58.Hagood JS, Lenker CV, Thrasher S. A course on the transition to adult care of patients with childhood-onset chronic illnesses. Acad Med. 2005;80(4):352–355. doi: 10.1097/00001888-200504000-00009. [DOI] [PubMed] [Google Scholar]
- 59.Hart LC, Mouw MS, Teal R, Jonas DE. What care models have generalists implemented to address transition from pediatric to adult care?: a qualitative study. J Gen Intern Med. 2019;34(10):2083–2090. doi: 10.1007/s11606-019-05226-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Manwani D, Doyle MH, Davidson L, et al. Transition navigator intervention improves transition readiness to adult care for youth with sickle cell disease. Acad Pediatr. 2022;22(3):422–430. doi: 10.1016/j.acap.2021.08.005. [DOI] [PubMed] [Google Scholar]
- 61.Lotstein DS, Kuo AA, Strickland B, Tait F. The transition to adult health care for youth with special health care needs: do racial and ethnic disparities exist? Pediatrics. 2010;126(Suppl 3):S129–S136. doi: 10.1542/peds.2010-1466F. [DOI] [PubMed] [Google Scholar]
- 62.Narla NP, Ratner L, Bastos FV, Owusu SA, Osei-Bonsu A, Russ CM (2021) Paediatric to adult healthcare transition in resource-limited settings: a narrative review. BMJ Paediatr Open 5(1):e001059. Published 19 Apr 2021. 10.1136/bmjpo-2021-001059 [DOI] [PMC free article] [PubMed]
- 63.Allemang B, Allan K, Johnson C et al (2019) Impact of a transition program with navigator on loss to follow-up, medication adherence, and appointment attendance in hemoglobinopathies. Pediatr Blood Cancer 66(8):e27781. 10.1002/pbc.27781 [DOI] [PubMed]
- 64.Hart LC, Díaz-González de Ferris M, Nazareth M et al (2021) Evaluation of the TRxANSITION index-parent version for assessment of readiness to transition to adult care among youth with chronic conditions. J Pediatr Nurs 58:1–8. 10.1016/j.pedn.2020.08.010 [DOI] [PubMed]
- 65.Schwartz LA, Daniel LC, Brumley LD, Barakat LP, Wesley KM, Tuchman LK. Measures of readiness to transition to adult health care for youth with chronic physical health conditions: a systematic review and recommendations for measurement testing and development. J Pediatr Psychol. 2014;39(6):588–601. doi: 10.1093/jpepsy/jsu028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wood DL, Sawicki GS, Miller MD, et al. The transition readiness assessment questionnaire (TRAQ): its factor structure, reliability, and validity. Acad Pediatr. 2014;14(4):415–422. doi: 10.1016/j.acap.2014.03.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data regarding the systematic review can be available upon request.