Abstract
Background
Sarcopenia is common in chronic advanced liver disease and is associated with poor prognosis. There is paucity of Indian data regarding sarcopenia in chronic advanced liver disease & its impact on prognosis. The aim of this study was to study the prevalence of sarcopenia in Indian patients with chronic advanced liver disease and its impact on morbidity and short-term mortality.
Methods
Patients with chronic advanced liver disease were prospectively evaluated for the presence of sarcopenia using computerized tomography (CT) abdomen. The cross-sectional area of the right psoas muscle was measured at the third lumbar vertebra (L3) and the Psoas muscle index (PMI) was calculated. Sarcopenia was defined as PMI <295 mm2/m2 for females and <356 mm2/m2 for males. The normative values of PMI were obtained from patients undergoing CT scan for non-specific abdominal pain who had no confounding factor which could result in sarcopenia. All patients were followed up for 6 months or until death, whichever was earlier. The impact of sarcopenia on mortality and rate of readmission has been assessed at the end of 6 months.
Results
Of the 156 patients with chronic advanced liver disease, 74 (47.4%) patients had sarcopenia. Sarcopenia was more commonly seen in males (M: F = 61:13) and in patients with alcohol-related liver disease. There was a linear correlation (negative) between the PMI and severity of liver disease as assessed by Child–Pugh and model for end-stage liver disease (MELD) scores (r = −0.591 and −0.465, respectively). Patients with encephalopathy, ascites, and coagulopathy had higher prevalence of sarcopenia. On six months follow-up, sarcopenic patients had higher readmission rates (74.3% vs. 22%; P = 0.0001) and higher mortality (24.3% vs. 3.7%; P = 0.002). MELD score and PMI were independent predictors of mortality. The cut-off value of PMI 305.9 mm2/m2 predicted mortality with a sensitivity of 76.2% and a false positivity of 22.2% (area under curve was 0.805; 95% confidence interval: 0.69–0.91, P = 0.001).
Conclusion
Sarcopenia is seen in about half of the patients with chronic advanced liver disease. It is commoner in males, patients with alcoholic liver disease, and those with advanced liver disease. Patients with sarcopenia have worse prognosis, require more frequent hospitalization and it negatively impacts short-term survival.
keywords: cirrhosis of liver, sarcopenia, muscle weakness
Sarcopenia has been defined as decline in muscle mass and muscle function (muscle strength or physical performance).1 Sarcopenia has been reported in 30–70% patients with liver cirrhosis, depending on the diagnostic tools utilized and the severity of the underlying liver disease.2 The prevalence of sarcopenia or malnutrition increases with severity of liver disease and sarcopenia or malnutrition is seen more frequently in males.3 Sarcopenia in cirrhotic patients is driven by multiple factors including impaired nutritional intake, improper absorption of food, altered metabolism, hormonal changes, hyperammonemia, and augmented muscle damage.4 The presence of sarcopenia leads to advanced rate of complications, such as infections, hepatic encephalopathy (HE), and ascites.5, 6, 7 Sarcopenia is also an independent predictor of mortality in patients with liver cirrhosis.8 Malnutrition and sarcopenia are associated with increased risk of decompensation, infections, and increased wait-list mortality in patients with cirrhosis.3 The diagnosis of sarcopenia is challenging in patients with cirrhosis who have fluid retention as fluid gains hide muscle and adipose tissue losses.9,10 The skeletal muscle index (SMI) at the level of the 3rd lumbar vertebra using computerized tomography (CT) or magnetic resonance imaging (MRI) is the most used and validated modality to evaluate muscle mass. It is the only modality that has validated sex-specific cut-offs (<50 cm2/m2 in men and <39 cm2/m2 in women).11 When normalized for stature, it is referred as L3 skeletal muscle index. Alternatively, psoas muscle index (PMI) defined as psoas muscle area measured at L3 level is used to diagnose sarcopenia and when normalized for stature it is referred as L3 PMI.
There is scant information on prevalence of sarcopenia and its prognostic significance in Indian patients with cirrhosis. The diagnostic criteria in Indian patients, who are often malnourished and already have a lower muscle mass comparative to western population, may be different. The aim of this study was to determine prevalence of sarcopenia in decompensated chronic liver disease and relation of encephalopathy and short-term survival with sarcopenia.
Methods
Patients
This study was carried out at the Institute of Liver, Gastroenterology and Pancreatico-Biliary Sciences of Sir Ganga Ram Hospital, New Delhi, India from May 2016 to December 2018. In this prospective study, we have included all adult patients with chronic advanced liver disease (18–75 years) who were admitted in our department for diagnostic work up or with complications of cirrhosis like HE, variceal bleeding, ascites, infection, or sepsis and had undergone CT scan of abdomen as well as evaluation for sarcopenia. Chronic advanced liver disease was diagnosed on imaging, elastographic and histological criteria. Patients with hepatocellular carcinoma, chronic kidney disease (renal damage for ≥3 months, as defined by structural or functional abnormalities of the kidney and/or serum creatinine value > 1.5 mg/dl)12 or those on maintenance hemodialysis, pregnant, or lactating females, those with spine and hip joint deformities or past history of spine surgery, patients on steroids, those with active alcohol intake (all the patients of alcoholic liver disease who were not on abstinence for ≥ 6 months) and those who did not give consent were excluded. The study was approved by the institutional ethics committee and the study conformed to the Helsinki declaration of 1975 as revised in 1983.
Evaluation
All patients underwent etiological evaluation of cirrhosis (viral markers, autoimmune markers, ceruloplasmin), ultrasound abdomen, transient elastography using fibroscans, upper gastrointestinal endoscopy, ultrasonography abdomen, and CT scan abdomen were done in all patients. Severity of the liver disease was assessed according to the Child–Turcotte–Pugh score (CTP) and model for end-stage liver disease (MELD) score. Patients were treated as per standard treatment guidelines and treating physician's discretion.
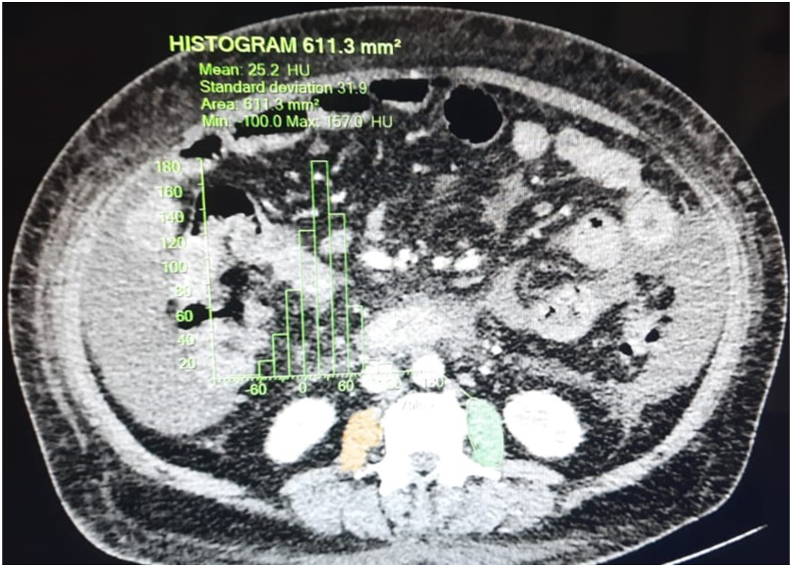
Technique of Assessment of Sarcopenia
Sarcopenia was diagnosed by calculating PMI at the level of third lumbar vertebra on axial CT scan images (Figure 1). The psoas muscle area was measured manually on the right side without using dedicated software by a CT scan technician. The cross-sectional area of the psoas muscle was normalized to stature (height in m2) to calculate PMI (mm2/m2). Normative values of PMI were obtained from a control group of non-cirrhotic patients who had undergone CT scan for non-specific abdominal pain and had no confounding factors which could result in sarcopenia like aging (>65 years), prolonged inactivity, known malignancy and spine and hip deformities. Forty patients were included in the control group (20 males and 20 females) with median age of 39 years (range 18–55 years). Mean PMI for males and females in control group were 430 ± 37.10 mm2/m2 and 357.96 ± 31.28 mm2/m2, respectively. The cut-off value of PMI for sarcopenia was defined as less than two standard deviations (SDs) below the mean PMI for males and females in the control group (less than 356 mm2/m2 and 295 mm2/m2 for males and females, respectively).
Figure 1.
CT abdomen image showing the methodology of calculation of psoas muscle index. CT, computerized tomography.
Follow-up of Patients
All patients were followed up physically on monthly basis for 6 months or until death, whichever was earlier. The clinical and laboratory data used for the analysis and to calculate MELD and Child–Pugh scores were obtained within 1 week from the index CT used to determine the PMI. All adverse clinical outcomes (hospital admissions/death/liver transplantation) during the follow-up period were recorded. Factors influencing the short-term mortality (6 months) and readmissions were analyzed.
Statistical Analysis
Statistical analysis was done using the SPSS 22.0 software (SPSS IBM Inc, Chicago). Continuous variables were expressed as mean ± SD while categorical variables were expressed as frequencies and percentages. The association of nominal categorical data between various variables and sarcopenia were compared using the Chi-square test or Fisher's exact test as appropriate. For comparisons of continuous variables between the two groups, Mann Whitney U test was used. Receiver operating characteristics (ROC) was used to determine the cut-off for predicting mortality and area under curve (AUC) was determined. Comparison of readmission and survival between the groups was done by Kaplan–Meier curve and log-rank test. A P value less than 0.05 was taken to indicate a significant difference for all statistical tests. Previous reported prevalence of 30%–70% of sarcopenia in patients with cirrhosis was used to calculate the sample size.2 Assuming the prevalence (P) of 40% at 5% level of significance with 10% margin of error, minimum required sample size calculated was 93 patients.
Results
Patients
A total of 156 patients with cirrhosis of liver who fulfilled the inclusion and exclusion criteria were enrolled for the study (Figure 1). The baseline characteristics of these patients are summarized in Table 1. The mean age of the cohort was 52.6 ± 10.5 years and majority (74.4%) were males. The commonest etiology for chronic advanced liver disease was alcohol-related liver disease (ALD) in 53 (34%) followed by non-alcoholic fatty liver disease (NAFLD) in 45 (28.8%). Of 156 patients, 25 (16%), 92 (59%), and 39 (25%) of the patients had CTP class A, CTP class B and CTP class C cirrhosis, respectively, and the mean MELD score was 15.89 ± 6.85. Forty patients were included in the control group (20 males and 20 females) with median age of 39 years (range 18–55 years).
Table 1.
Comparison of Baseline Parameters.
| Characteristics | N = 156 | No sarcopenia (N = 82) | Sarcopenia(N = 74) | P value | |
|---|---|---|---|---|---|
| Age (years) (±SD) | 52 (±10.5) | 53.4 (31–72) | 51.7 (28–74) | 0.489 | |
| Sex (Male/Female) (%) | 116/40 (74.4/25.6) | 55/27 (67.1/32.9) | 61/13 (82.4/17.6) | 0.043 | |
| Etiology | Ethanol (%) | 53 (33.9) | 16 (19.5) | 37 (50) | 0.001 |
| NASH (%) | 45 (28.8) | 28 (34.1) | 17 (23) | ||
| HBV (%) | 8 (5.1) | 5 (6.1) | 3 (4.1) | ||
| HCV (%) | 16 (10.2) | 9 (10.9) | 7 (9.5) | ||
| Autoimmune (%) | 12 (7.6) | 9 (10.9) | 3 (4.1) | ||
| Cryptogenic (%) | 22 (14.1)) | 15 (18.3) | 7 (9.5) | ||
| Albumin (g/dL) (±SD) | 2.7 (±0.56) | 3.01 (±0.53) | 2.51 (±0.47) | 0.001 | |
| Bilirubin (mg/dL) (±SD) | 4.8 (±6.78) | 2.7 (±4.19) | 7.12 (±8.2) | 0.001 | |
| Creatinine (mg/dL) (±SD) | 1.1 (±0.38) | 0.87 (±0.25) | 1.16 (±0.43) | 0.06 | |
| Sodium (mEq/L) (±SD) | 134 (±11.86) | 136 (±4.52) | 132 (±5.1) | 0.71 | |
| INR (±SD) | 1.58 (±0.50) | 1.34 (±0.23) | 1.84 (±0.58) | 0.001 | |
| MELD score (±SD) | 15.89 (±6.85) | 12.36 (±4.2) | 19.7 (±7.6) | 0.0001 | |
| CTP score (±SD) | 8.5 (±1.9) | 7.28 (±1.23) | 9.87 (±1.76) | 0.001 | |
| Ascites | Absent (%) | 43 (27.5) | 33 (40.2) | 10 (13.5) | 0.003 |
| Mild-Mod (%) | 95 (60.9) | 46 (56.1) | 49 (66.2) | ||
| Gross (%) | 18 (11.5) | 3 (3.7) | 15 (20.3) | ||
| CTP Class | A (%) | 25 (16) | 22 (26.85) | 3 (4) | 0.0001 |
| B (%) | 92 (59) | 58 (70.7) | 34 (46) | ||
| C (%) | 39 (25) | 2 (2.4) | 37 (50) | ||
| Hepatic Encephalopathy (%) | 33 (21.2) | 5 (6.1) | 28 (37.8) | 0.0001 | |
| Psoas Muscle Index (mm2/m2) (±SD) | 344.10 (±58.7) | 385.49 (±41.1) | 298.2 (±37.3) | 0.001 | |
CTP, Child–Turcotte–Pugh; MELD, Model for End-stage Liver Disease; HBV, Hepatitis B Virus; HCV, Hepatitis C Virus; INR, International Normalized Ratio; NASH, Non-alcoholic Steohepatitis; SD, Standard Deviation.
Prevalence of Sarcopenia
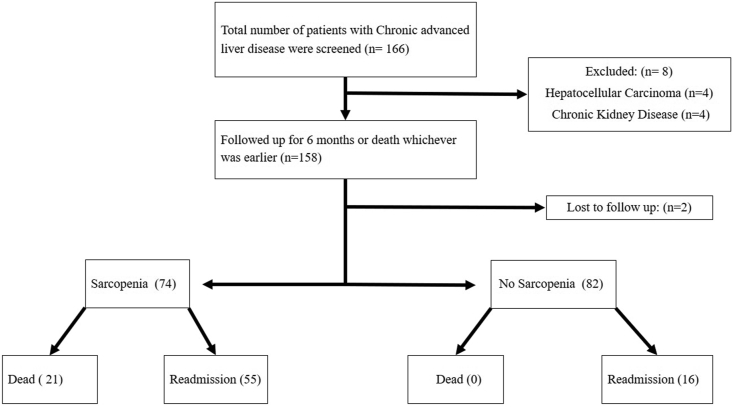
Sarcopenia was present in 74 (47.4%) patients with liver cirrhosis and was more common in men. Sarcopenia was more common in cirrhotic males (61/116; 52.5%) than females (13/40; 32%). PMI in control group was 385.49 (±41.1) mm2/mm2, while in patients who had sarcopenia, PMI was 298.2 (±37) mm2/m2 (P = 0.001). Sarcopenia was seen in 70% (37/53) patients with alcohol-related chronic advanced liver disease, 37.8% (17/45) of non-alcoholic steatohepatitis-related cirrhosis, 41% (10/24) of viral disease (Hepatitis B&C), and 25% autoimmune liver disease (3/12) (Figure 2).
Figure 2.
Flowchart depicting the outcome of the patients enrolled in the study.
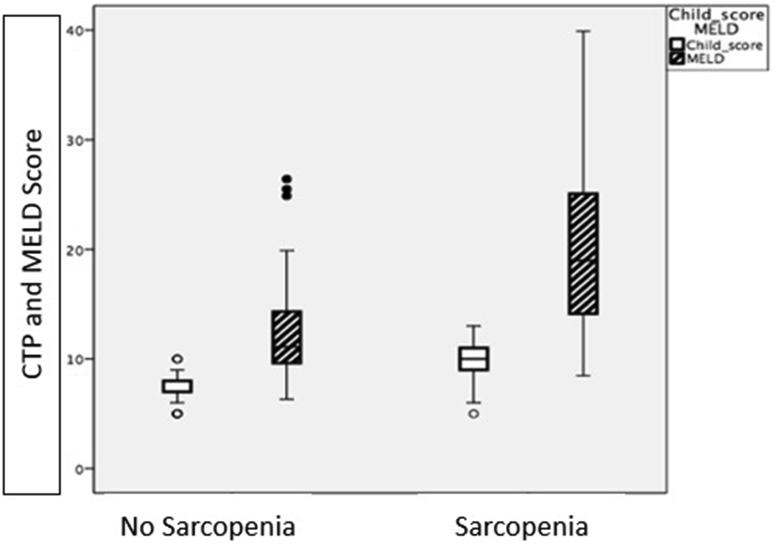
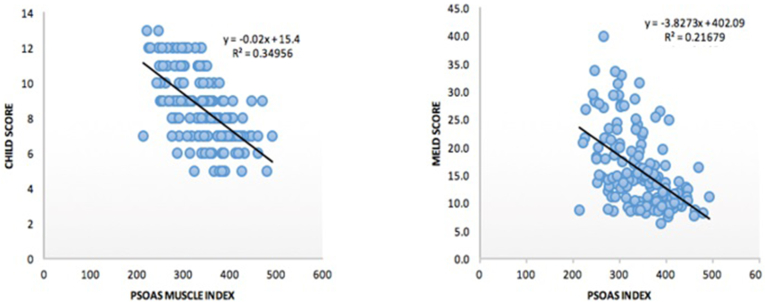
Sarcopenic patients had lower albumin levels (P = 0.001), higher bilirubin levels (P = 0.001), higher MELD and CTP scores (P = 0.0001 and 0.001, respectively) than those without sarcopenia (Figure 3). Patients with CTP class C had higher prevalence of sarcopenia. There was an inverse linear correlation between the PMI and severity of liver disease as assessed by CTP and MELD scores (r = − 0.591 and −0.465, respectively) (Figure 4). Patients with HE (P = 0.0001), ascites (P = 0.003), and coagulopathy (P = 0.001) had higher prevalence of sarcopenia.
Figure 3.
Baseline CTP and MELD scores in sarcopenic and non-sarcopenic patients with chronic advanced liver disease. CTP, Child–Turcotte–Pugh; MELD, model for end-stage liver disease.
Figure 4.
Correlation between CTP score and MELD score with psoas muscle index (PMI). CTP, Child–Turcotte–Pugh; MELD, model for end-stage liver disease.
Short-term Clinical Outcome
Readmission
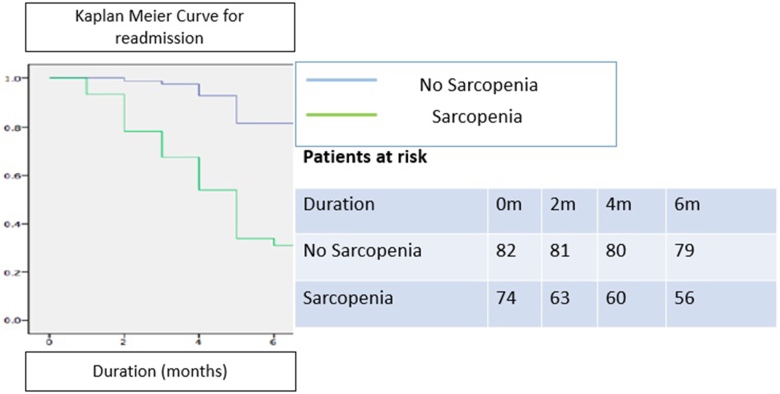
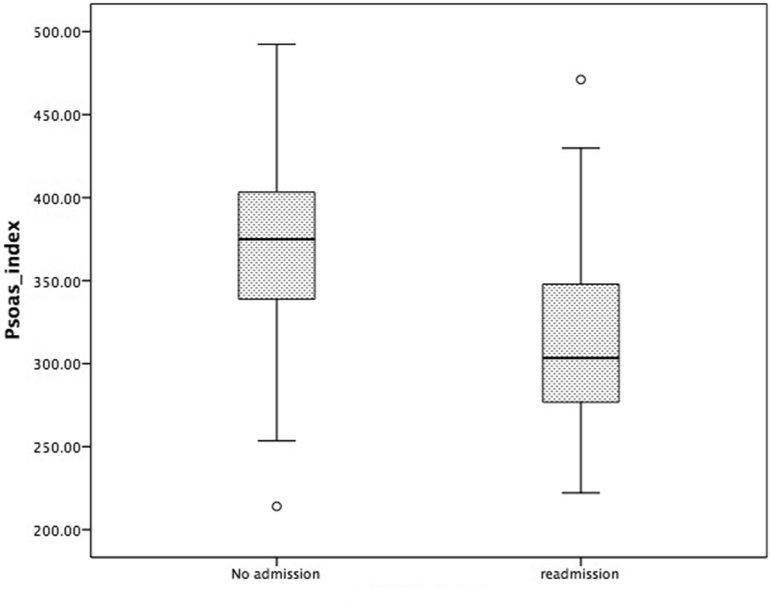
During follow-up period of 6 months, 71 (46%) patients were readmitted. Fifty-five out of 71 patents requiring readmission had sarcopenia (Figure 2). The reasons for readmission in sarcopenic patients was ascites in 23 patients, jaundice in 14 patients, HE in 13 patients, upper gastrointestinal bleed in 4 patients, and infection/sepsis in 13 patients and non-hepatic causes in 8 patients (Table 2). Rehospitalization within 6 months was significantly higher in patients who had sarcopenia than those who did not have sarcopenia [55/74 (74.3%) vs. 16/82 (20%); P = 0.0001; Log-rank test], represented by Kaplan–Meier curve (Figure 5). PMI was significantly lower in patients who were rehospitalized (284.2 (±41.3) mm2/m2) than those who did not require rehospitalization (374.68 (±47.7) mm2/m2)(P value-0.0001) (Figure 6).
Table 2.
Indications for Readmission in Both Sarcopenic and Non-sarcopenic Groups (During Readmission Few Patients had More Than One Indication or Overlapping Features of Hepatic Decompensation).
| No sarcopenia (N = 16) | Sarcopenia (N = 55) | |
|---|---|---|
| Ascites | 8 (50%) | 23 (42%) |
| Jaundice | 2 (13%) | 14 (25%) |
| Hepatic encephalopathy | 1 (6%) | 13 (24%) |
| Upper gastrointestinal bleed | 2 (13%) | 4 (7%) |
| Infection/sepsis | 1 (6%) | 13 (24%) |
| Non-hepatic cause | 3 (19%) | 8 (14%) |
Figure 5.
Risk of readmission in sarcopenic and non-sarcopenic patients.
Figure 6.
Psoas muscle index in patients readmitted and those without readmission.
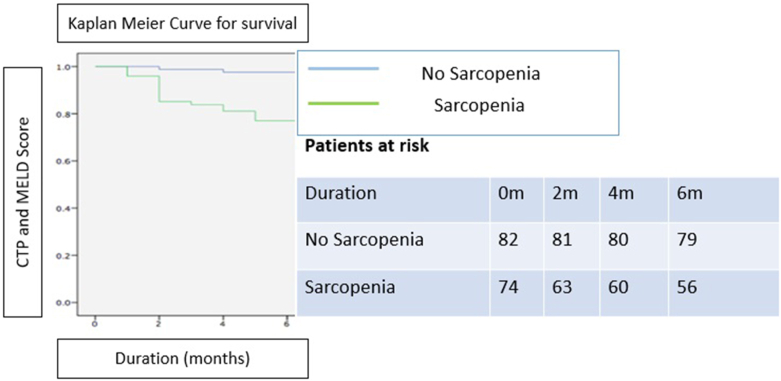
Mortality
Mortality was higher among the patients who had sarcopenia than those without sarcopenia (18/74 (24.3%) vs. 3/82 (3.7%); P = 0.0002) (Figure 7). On univariate analysis, albumin, bilirubin, INR, presence of HE, CTP score, MELD score, and PMI were associated with mortality (Table 3).
Figure 7.
Difference of survival between sarcopenic and non-sarcopenic patients.
Table 3.
Univariate Analysis of Baseline Parameters Predicting Death.
| Variables | Survivors N = 135 | Death N = 21 | P value | |
|---|---|---|---|---|
| Body mass index (kg/m2) (±SD) | 26.9 ± 3.86 | 26.45 ± 4.41 | 0.606 | |
| Albumin (g/dL) (±SD) | 2.81 ± 0.57 | 2.51 ± 0.45 | 0.023 | |
| Bilirubin (mg/dL) (±SD) | 3.1 ± 3.76 | 15.71 ± 10.82 | 0.0001 | |
| Creatinine (mg/dL) (±SD) | 0.98 ± 0.36 | 1.18 ± 0.43 | 0.2 | |
| International normalized ratio (±SD) | 1.47 ± 0.62 | 2.23 ± 0.83 | 0.01 | |
| MELD score (±SD) | 14.33 ± 5.3 | 25.94 ± 7.27 | 0.0001 | |
| Child–Pugh score (±SD) | 8.14 ± 1.75 | 10.8 ± 1.82 | 0.0001 | |
| Psoas Muscle index (mm2/m2) (±SD) | 352 ± 55 | 288 ± 51 | 0.0001 | |
| Hepatic encephalopathy | 9 | 24 | 0.009 | |
| Ascites | Absent | 41 | 2 | 0.09 |
| Mild – Mod | 79 | 16 | ||
| Gross | 15 | 3 | ||
MELD, Model for End-stage Liver Disease; SD, Standard Deviation.
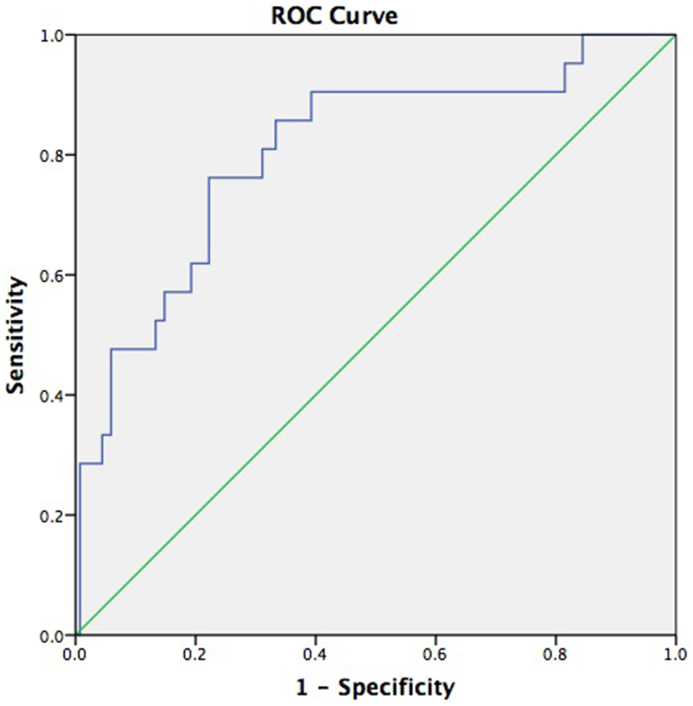
PMI cut-off for predicting mortality
Based on the PMI values of patients, receiver operating curve (ROC) was calculated. The cut-off value of 305.9 mm2/m2 predicted mortality with a sensitivity of 76.2%, specificity of 77.7%, false positivity of 22.2%, and false negativity of 23.8%. AUC was 0.805 (95% confidence interval: 0.69–0.91, P = 0.001) (Figure 8).
Figure 8.
ROC curve for PMI (psoas muscle index) predicting mortality of patients with cirrhosis.
A flowchart of results of this study is shown in Figure 2.
Discussion
In this prospective study, sarcopenia was seen in 74/156 (47.4%) patients with chronic advanced liver disease. Sarcopenia was more commonly seen in males (M: F = 61:13) and in patients with ALD. Two studies from India have reported prevalence of sarcopenia in patients with cirrhosis up to 13% and 56%, respectively, based on CT assessment.13,14 Other Asian countries like Japan and Korea have reported prevalence of sarcopenia in cirrhosis ranging from 42 to 68%.15 CT-based studies from the west have reported prevalence of sarcopenia in cirrhosis in range of 35–45% (16, 17, 18) (Table 4).
Table 4.
Recent Studies Highlighting the Importance of Sarcopenia in Patients with Chronic Advanced Liver Disease.
| Author | Number of patients | Site of PMI/SMI measurement | Prevalence of Sarcopenia | Comments |
|---|---|---|---|---|
| Montano-Loza (2012)27 | 112 | L3 | 40% | Sarcopenia proved to be an independent factor associated with mortality in cirrhotic patients waiting for transplant. |
| Tandon (2012)28 | 142 | L3 | 41% | The prediction of sarcopenia was done by subjective nutritional assessment tools such as BMI, subjective global assessment, and the presence of sarcopenia is associated with high waiting list mortality. |
| DiMartini (2013)20 | 338 | L3 | 68% | Sarcopenia is associated with high waiting list mortality and aggressive strategies to combat sarcopenia may lead to better outcome post-operatively. |
| Hanai (2015)15 | 130 | L3 | 68% | Sarcopenia is significantly associated with mortality in patients with liver cirrhosis. |
| Gu (2018)29 | 653 | L3 | 36.90% | The inter relationship between the Psoas muscle thickness per height (PMTH) and skeletal muscle index in cirrhotic patients was well correlated in this study and was established as a predictor of mortality. |
| Paternostro (2019)30 | 109 | L3 | 57.8–63.3% | Multiple indices were measured and compared including gender specific SMI, transversal psoas muscle thickness (TPMT), total psoas volume and para-spinal muscle index were measured. Only, TPMT turned out to be an independent risk factor for mortality in patients with liver cirrhosis. |
| Kumar (2020)14 | 115 | L3 | 47.80% | Sarcopenia is associated with higher post-operative septic complications, increased ventilatory support and higher neurological complications in LT recipients. |
| Ebadi (2020)31 | 603 | L3 | 31.10% | Sarcopenia is associated with higher morbidity and mortality in cirrhotic patients. Decline of SMI on follow up may indicate worsening disease. |
PMTH, Psoas Muscle Thickness Per Height; PMI, Psoas Muscle Index; SMI, Skeletal Muscle Index; TPMT, Transversal Psoas Muscle Thickness; LT, Liver Transplant.
These differences in prevalence of sarcopenia in patients of Asian and Western population may be due to two factors.
-
(i)
Differences in racial characteristics, body size and dietary differences between the Asian and the Western individuals.
-
(ii)
Different methods and cut-offs used to assess the sarcopenia.
Cross-sectional imaging either by MRI or CT is considered gold standard for assessment of sarcopenia. However, there is no uniformity in the definition of sarcopenia due to variability in the method of assessment. In our study, we have defined sarcopenia based on PMI value obtained by CT abdomen. We have defined cut-offs of sarcopenia for males and females as less than 356 mm2/m2 and 295 mm2/m2, respectively (less than two SDs of the mean PMI values of the control group). In an Indian study conducted by Sidhu et al. which included 3087 healthy (non-cirrhotic) individuals showed that the mean SMI at third lumbar vertebra (L3) for Indian men and women was 443.3 ± 65.6 mm2/m2 and 412.5 ± 44.2 mm2/m2, respectively, which was significantly lesser than the L3 SMI obtained from a healthy Caucasian population (609 ± 78 mm2/m2 in men and 475 ± 66 mm2/m2 in women).19 Either the entire muscle area or the thickness of the psoas muscle or area of only the psoas muscle can be used to assess sarcopenia. There is an established close relationship between the total muscle area and the psoas muscle area at the level of L3 for the assessment of sarcopenia.20 Measurement of only the psoas muscle area compared to the total muscle area is less cumbersome and does not require any additional software.
In our study, patients with ALD had higher prevalence of sarcopenia (70%) comparative to other etiologies of liver cirrhosis. Likewise, DiMartini et al. have reported sarcopenia in 80% patients with alcoholic liver disease.20 In our study, patients with sarcopenia had lower serum albumin, higher bilirubin, higher MELD (18.8 ± 7.6 vs. 11.45 ± 4.2) and CTP score (9.8 ± 1.7 vs. 7.2 ± 1.2) than those without sarcopenia. There was a negative linear correlation between the PMI and severity of liver disease as assessed by CTP and MELD scores (r = −0.591 and −0.465 respectively). Sarcopenic patients had higher mean MELD and CTP scores than those who did not have sarcopenia (19.7 vs. 12.36 for MELD, 9.87 vs. 7.28 for CTP score). Similar results have been reported by Durand et al.21 In our study, prevalence of sarcopenia was 4%, 46%, and 50% for CTP class A, B, and C class, respectively. In a study conducted by Hanai et al.,15 sarcopenia was more frequently seen in CTP class C (94%), while sarcopenia was seen in only 12% patients of CTP class A. We can infer that prevalence of sarcopenia increases with degree of liver dysfunction.
Patients with encephalopathy and ascites had higher prevalence of sarcopenia. There was higher prevalence of sarcopenia in patients presenting with HE than those without encephalopathy (P = 0.0001). In our study, 28/33 (85%) patients with HE had sarcopenia. In this study, HE was seen in 37.8% of the patients with sarcopenia, while only 6.4% of non-sarcopenic patients had HE. Skeletal muscle has a significant role in non-hepatic ammonia detoxification and cirrhotic patients with muscle depletion are at a higher risk of HE due to hyperammonemia.4 Ammonia uptake and disposal via glutamine synthesis in the muscle and transport into the circulation may be impaired in sarcopenia. The association between sarcopenia and HE was also described in a retrospective study including a group of 120 cirrhotic Japanese patients, presence of sarcopenia was associated with more chances of minimal HE and the presence of sarcopenia was an independent predictor of minimal HE by multivariate analysis.22 Another study displayed the importance of adductor pollicis muscle thickness and handgrip strength and lower values of both was associated with higher chances of HE in cirrhotic patient.23
In our study, patients with sarcopenia had lower albumin levels and higher grade of ascites than non-sarcopenic patients. Gross ascites was seen in 20.3% of the sarcopenic patients when compared to 3.7% in non-sarcopenic patients. Cirrhotic patients with refractory ascites are prone to develop malnutrition and sarcopenia.24 Dolz et al. have shown that ascites increases the resting energy expenditure. Food intake is decreased in patients with ascites due to raised abdominal pressure and early satiety. Associated hypoalbuminemia may also be an important contributing factor for the development of ascites, and this being a vicious cycle may further increase the muscle mass depletion leading to worsening of sarcopenia.24
Sarcopenia in cirrhosis of liver influences the clinical outcome of patients in terms of both morbidity and mortality. In our study, significant proportion of patients with sarcopenia (74.3%) was readmitted to the hospital at least once during the follow-up period of 6 months compared to 22% in the non-sarcopenic group. Mortality was also significantly higher in the sarcopenic patients (24.3% vs. 3.7%). MELD score and PMI were found to be independent factors associated with mortality by multivariate analysis. PMI cut-off value for predicting mortality obtained was 305.9 mm2/m2 with a sensitivity of 76.2% and a false positivity of 22.2% (AUC was 0.805; 95% confidence interval: 0.69–0.91, P = 0.001). Montano Loza et al. also reported that presence of sarcopenia was associated with mortality in cirrhosis of liver and they also reported that sarcopenia increases the risk of mortality by 1.5- to 2-fold compared with patients who do not have sarcopenia.25 Kang et al. have elegantly demonstrated that sarcopenia was an independent predictor of survival in compensated and early decompensated cirrhosis (MELD <15; CTP classes A and B; non-CSPH and CSPH). However, sarcopenia was not a prognostic factor in advanced decompensated cirrhosis [MELD ≥15; CTP class C; extremely severe portal hypertension (HVPG ≥20 mmHg)].26
This study has a few limitations:
-
1)
Majority of the patients included in the study had CTP class B or C cirrhosis who were admitted at a tertiary care center, the prevalence of sarcopenia may be lower in a population-based cohort of cirrhotic patients.
-
2)
In this study, follow-up duration was just six months. To assess the impact of sarcopenia on mortality and clinical outcome in cirrhotic patients, a follow-up period of longer duration may have been more appropriate
-
3)
In this study, the size of control cohort is limited as this study was conducted in a private setup and for a restricted time frame.
-
4)
There is inseparable distinction between critically ill hospitalized patients with advanced chronic liver disease and patients with acute on chronic liver disease (as per APASL criteria). Hence the prevalence of sarcopenia may be overestimated in the control group due to overlapping acute on chronic liver failure.
Sarcopenia is seen in about half of the patients with liver cirrhosis and measurement of PMI at L3 is simple, objective, and easily reproducible method for diagnosis. Prevalence of sarcopenia correlates with severity of liver disease as assessed by Child and MELD score. Patients with sarcopenia are more prone to develop complications of liver cirrhosis like HE. Sarcopenia is an independent prognostic marker of survival and rehospitalization. This can be concluded that in patients with chronic advanced liver disease, the presence of sarcopenia is associated with poor outcome compared to the patients who do not have sarcopenia.
Credit authorship contribution statement
Surakshith TK: Writing original draft, Formal analysis, Data Curation, Investigation.
Samarth Sharma: Writing original draft, Review and editing.
Mandhir Kumar: Formal analysis, validation, Project administration.
Anil Arora: Conceptualization, Supervision.
Samarjit Singh Ghumman: Resources, Validation, review.
Piyush Ranjan: Conceptualization, Methodology, Supervision, Review and editing.
Conflicts of interest
The authors have none to declare.
Funding
All the authors declare that we have not received any funding for this study.
References
- 1.Cruz-Jentoft A.J., Bahat G., Bauer J., et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48:16–31. doi: 10.1093/ageing/afy169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dasarathy S., Merli M. Sarcopenia from mechanism to diagnosis and treatment in liver disease. J Hepatol. 2016;65:1232–1244. doi: 10.1016/j.jhep.2016.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Puri P., Dhiman R.K., Taneja S., et al. Nutrition in chronic liver disease: consensus statement of the Indian national association for study of the liver. J Clin Exp Hepatol. 2021 Jan-Feb;11:97–143. doi: 10.1016/j.jceh.2020.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jindal A., Jagdish R.K. Sarcopenia: Ammonia metabolism and hepatic encephalopathy. Clin Mol Hepatol. 2019;25:270–279. doi: 10.3350/cmh.2019.0015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huisman E.J., Trip E.J., Siersema P.D., Van Hoek B., Van Erpecum K.J. Protein energy malnutrition predicts complications in liver cirrhosis. Eur J Gastroenterol Hepatol. 2011;23:982–989. doi: 10.1097/MEG.0b013e32834aa4bb. [DOI] [PubMed] [Google Scholar]
- 6.Merli M., Lucidi C., Giannelli V., et al. Cirrhotic patients are at risk for health care–associated bacterial infections. Clin Gastroenterol Hepatol. 2010;8:979–985.e1. doi: 10.1016/j.cgh.2010.06.024. [DOI] [PubMed] [Google Scholar]
- 7.Merli M., Giusto M., Lucidi C., et al. Muscle depletion increases the risk of overt and minimal hepatic encephalopathy: results of a prospective study. Metab Brain Dis. 2013;28:281–284. doi: 10.1007/s11011-012-9365-z. [DOI] [PubMed] [Google Scholar]
- 8.Khan S., Benjamin J., Maiwall R., et al. Sarcopenia is the independent predictor of mortality in critically ill patients with cirrhosis. J Clin Transl Res. 2022 May 25;8:200–208. [PMC free article] [PubMed] [Google Scholar]
- 9.Figueiredo F.A., De Mello Perez R., Kondo M. Effect of liver cirrhosis on body composition: evidence of significant depletion even in mild disease. J Gastroenterol Hepatol. 2005;20:209–216. doi: 10.1111/j.1440-1746.2004.03544.x. [DOI] [PubMed] [Google Scholar]
- 10.Peng S., Plank L.D., McCall J.L., Gillanders L.K., McIlroy K., Gane E.J. Body composition, muscle function, and energy expenditure in patients with liver cirrhosis: a comprehensive study. Am J Clin Nutr. 2007;85:1257–1266. doi: 10.1093/ajcn/85.5.1257. [DOI] [PubMed] [Google Scholar]
- 11.Carey E.J., Lai J.C., Sonnenday C., et al. A north American expert opinion statement on sarcopenia in liver transplantation. Hepatology. 2019 Nov;70:1816–1829. doi: 10.1002/hep.30828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Kidney Foundation KDOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002 Feb;39(2 suppl 1):S1–S266. 11904577 [PubMed] [Google Scholar]
- 13.Benjamin J., Shasthry V., Kaal C.R., et al. Characterization of body composition and definition of sarcopenia in patients with alcoholic cirrhosis: a computed tomography based study. Liver Int. 2017 Nov;37:1668–1674. doi: 10.1111/liv.13509. [DOI] [PubMed] [Google Scholar]
- 14.Kumar V., Benjamin J., Shasthry V., et al. Sarcopenia in cirrhosis: fallout on liver transplantation. J Clin Exp Hepatol. 2020 Sep-Oct;10:467–476. doi: 10.1016/j.jceh.2019.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hanai T., Shiraki M., Nishimura K., et al. Sarcopenia impairs prognosis of patients with liver cirrhosis. Nutrition. 2015;31:193–199. doi: 10.1016/j.nut.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 19.Sidhu S., Saggar K., Goyal O. Normative values of sarcopenia in the Indian population. Indian Society of Gastroenterology. Indian J Gastroenterol. 2018;37:1–137. [Google Scholar]
- 20.DiMartini A., Cruz R.J., Dew M.A., et al. Muscle mass predicts outcomes following liver transplantation. Liver Transplant. 2013;19:1172–1180. doi: 10.1002/lt.23724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Durand F., Buyse S., Francoz C. Prognostic value of muscle atrophy in cirrhosis using psoas muscle thickness oncomputed tomography. Hepatology. 2014;60:1151–1157. doi: 10.1016/j.jhep.2014.02.026. [DOI] [PubMed] [Google Scholar]
- 22.Hanai T., Shiraki M., Watanabe S., et al. Sarcopenia predictsminimal hepatic encephalopathy in patients with liver cirrhosis. Hepatol Res. 2017 Dec;47:1359–1367. doi: 10.1111/hepr.12873. [DOI] [PubMed] [Google Scholar]
- 23.Augusti L., Franzoni L.C., Santos L.A., et al. Lower values of handgrip strength and adductor pollicis muscle thickness are associated with hepatic encephalopathy manifestations in cirrhotic patients. Metab Brain Dis. 2016 Aug;31:909–915. doi: 10.1007/s11011-016-9828-8. [DOI] [PubMed] [Google Scholar]
- 24.Dolz C., Raurich J.M., Ibanez J., Obrador A., Marse P., Gaya J. Ascites increases the resting energy expenditure in liver cirrhosis. Gastroenterology. 1991;100:738–744. doi: 10.1016/0016-5085(91)80019-6. [DOI] [PubMed] [Google Scholar]
- 25.Montano-Loza A.J., Angulo P., Meza-Junco J., et al. Sarcopenic obesity and myosteatosis are associated with higher mortality in patients with cirrhosis. J Cachexia Sarcopenia Muscle. 2016;7:126–135. doi: 10.1002/jcsm.12039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kang S.H., Jeong W.K., Baik S.K., Cha S.H., Kim M.Y. Impact of sarcopenia on prognostic value of cirrhosis: going beyond the hepatic venous pressure gradient and MELD score. J Cachexia Sarcopenia Muscle. 2018 Oct;9:860–870. doi: 10.1002/jcsm.12333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Montano–Loza A.J., Meza–Junco J., Prado C.M., et al. Muscle wasting is associated with mortality in patients with cirrhosis. Clin Gastroenterol Hepatol. 2012;10:166–173.e1. doi: 10.1016/j.cgh.2011.08.028. [DOI] [PubMed] [Google Scholar]
- 28.Tandon P., Ney M., Irwin I., et al. Severe muscle depletion in patients on the liver transplant wait list: its prevalence and independent prognostic value. Liver Transplant. 2012;18:1209–1216. doi: 10.1002/lt.23495. [DOI] [PubMed] [Google Scholar]
- 29.Gu D.H., Kim M.Y., Seo Y.S., et al. Clinical usefulness of psoas muscle thickness for the diagnosis of sarcopenia in patients with liver cirrhosis. Clin Mol Hepatol. 2018;24:319–330. doi: 10.3350/cmh.2017.0077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Paternostro R., Lampichler K., Bardach C., et al. The value of different CT-based methods for diagnosing low muscle mass and predicting mortality in patients with cirrhosis. Liver Int. 2019;39:2374–2385. doi: 10.1111/liv.14217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ebadi M., Bhanji R.A., Dunichand-Hoedl A.R., Mazurak V.C., Baracos V.E., Montano-Loza A.J. Sarcopenia severity based on computed tomography image analysis in patients with cirrhosis. Nutrients. 2020;12:3463. doi: 10.3390/nu12113463. [DOI] [PMC free article] [PubMed] [Google Scholar]