Key Points
Question
Across US neighborhoods, is there an association between cumulative environmental burden and cardiovascular health?
Findings
In this cross-sectional study of 71 659 US Census tracts, neighborhoods in the top quartile of environmental burden experienced significantly higher rates of cardiovascular risk factors (hypertension, diabetes, and obesity) and diseases (coronary heart disease and stroke) compared with those in the bottom quartile. The association between environmental burden and cardiovascular health was more pronounced in socially vulnerable neighborhoods.
Meaning
The findings of an association between neighborhood environmental burden and worse cardiovascular health, especially in socially vulnerable communities that are also disproportionately exposed to these conditions, indicate that future studies should investigate the impact of addressing environmental hazards on cardiovascular health.
This cross-sectional study evaluates associations between environmental burden and cardiovascular risk factors and diseases at the neighborhood level and by levels of social vulnerability.
Abstract
Importance
Cardiovascular disease is the leading cause of death in the US. However, little is known about the association between cumulative environmental burden and cardiovascular health across US neighborhoods.
Objective
To evaluate the association of neighborhood-level environmental burden with prevalence of cardiovascular risk factors and diseases, overall and by levels of social vulnerability.
Design, Settings, and Participants
This was a national cross-sectional study of 71 659 US Census tracts. Environmental burden (EBI) and social vulnerability indices from the US Centers for Disease Control and Prevention (CDC) and Agency for Toxic Substances and Disease Registry were linked to the 2020 CDC PLACES data set. Data were analyzed from March to October 2023.
Exposures
The EBI, a measure of cumulative environmental burden encompassing 5 domains (air pollution, hazardous or toxic sites, built environment, transportation infrastructure, and water pollution).
Main Outcomes and Measures
Neighborhood-level prevalence of cardiovascular risk factors (hypertension, diabetes, and obesity) and cardiovascular diseases (coronary heart disease and stroke).
Results
Across the US, neighborhoods with the highest environmental burden (top EBI quartile) were more likely than those with the lowest environmental burden (bottom EBI quartile) to be urban (16 626 [92.7%] vs 13 414 [75.4%]), in the Midwest (5191 [28.9%] vs 2782 [15.6%]), have greater median (IQR) social vulnerability scores (0.64 [0.36-0.85] vs 0.42 [0.20-0.65]), and have higher proportions of adults in racial or ethnic minority groups (median [IQR], 34% [12-73] vs 12% [5-30]). After adjustment, neighborhoods with the highest environmental burden had significantly higher rates of cardiovascular risk factors than those with the lowest burden, including hypertension (mean [SD], 32.83% [7.99] vs 32.14% [6.99]; adjusted difference, 0.84%; 95% CI, 0.71-0.98), diabetes (mean [SD], 12.19% [4.33] vs 10.68% [3.27]; adjusted difference, 0.62%; 95% CI, 0.53-0.70), and obesity (mean [SD], 33.57% [7.62] vs 30.86% [6.15]; adjusted difference, 0.77%; 95% CI, 0.60-0.94). Similarly, neighborhoods with the highest environmental burden had significantly higher rates of coronary heart disease (mean [SD], 6.66% [2.15] vs 6.82% [2.41]; adjusted difference, 0.28%; 95% CI, 0.22-0.33) and stroke (mean [SD], 3.65% [1.47] vs 3.31% [1.12]; adjusted difference, 0.19%; 95% CI, 0.15-0.22). Results were consistent after matching highest and lowest environmentally burdened neighborhoods geospatially and based on other covariates. The associations between environmental burden quartiles and cardiovascular risk factors and diseases were most pronounced among socially vulnerable neighborhoods.
Conclusions and Relevance
In this cross-sectional study of US neighborhoods, cumulative environmental burden was associated with higher rates of cardiovascular risk factors and diseases, although absolute differences were small. The strongest associations were observed in socially vulnerable neighborhoods. Whether initiatives that address poor environmental conditions will improve cardiovascular health requires additional prospective investigations.
Introduction
Cardiovascular disease remains the leading cause of death in the US.1 Socially vulnerable communities experience a disproportionately higher burden of cardiovascular risk factors and diseases, driven in part by social determinants of health, such as poor access to care, inadequate housing, and food insecurity.2,3,4,5 In addition to these social risk factors, there is growing concern around the influence of environmental risk factors on cardiovascular health.6,7
Previous studies have focused on the contributions of individual environmental exposures on health outcomes. For example, several large-scale epidemiologic studies have demonstrated that exposure to gaseous pollutants (eg, ozone) and fine particulate matter (PM2.5) increase the risk of all-cause and cardiovascular mortality.8,9,10,11 Other environmental burdens, such as exposure to toxic metals and industrial waste, transportation noise pollution, and lack of recreational facilities and green spaces for regular exercise, have each been associated with worse health outcomes.12,13,14,15 However, little is currently known about the cumulative and collective impact of these environmental burdens on the neighborhood-level prevalence of cardiovascular risk factors and diseases. In addition, despite evidence that certain environmental factors, such as air pollution exposure, disproportionately affect low-income and high-proportion racial and ethnic minority communities,16,17,18 it is unclear if there are significant interactions between environmental burden and social vulnerability. Understanding the collective influence of neighborhood environmental burdens on cardiovascular health and how these associations vary by social vulnerability could inform targeted efforts by health systems, public health leaders, and other sectors to address these hazards and improve cardiovascular health outcomes.
Therefore, in this national study, we evaluated the association between neighborhood-level environmental burden and the prevalence of cardiovascular risk factors (hypertension, diabetes, and obesity) and diseases (coronary heart disease and stroke). We also assessed whether the association between environmental burden and cardiovascular health varied across different levels of neighborhood-level social vulnerability.
Methods
This cross-sectional study of 71 659 US neighborhoods used US Census tract–level data on environmental burden from the US Centers for Disease Control and Prevention (CDC).19 The study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for cross-sectional studies. Institutional review board approval from the Beth Israel Deaconess Medical Center was not required because of the use of publicly available and deidentified data, as per institutional policy.
The prevalence of cardiovascular risk factors and diseases within each Census tract (hereafter, neighborhood) among adults 18 years and older was extracted from the 2020 CDC PLACES data set, which is based on the 2017-2018 Behavioral Risk Factor Surveillance System and obtained through a validated multilevel regression and poststratification approach for small-area estimation (additional details provided in the eMethods in Supplement 1).20,21
Environmental Burden Index
In 2022, the CDC and the Agency for Toxic Substances and Disease Registry released the environmental burden index (EBI), the first national, granular, and comprehensive measure of exposure to environmental factors influencing human health.22 Data were collected by the CDC, US Census Bureau, US Environmental Protection Agency, and the US Mine Safety and Health Administration. Indicators were identified through a scoping review of the environmental burden literature and were evaluated for inclusion based on a set of criteria, including accuracy, reliability, validity, and availability at scale. Further details about the development and validation of the EBI have been detailed elsewhere.19 The EBI is calculated at the individual neighborhood level, and encompasses 17 indicators reflecting data from 2014 to 2021 and spanning 5 separate domains, including (1) air pollution, (2) hazardous and toxic sites (eg, coal and lead mines), (3) the built environment (eg, recreational parks and neighborhood walkability), (4) transportation infrastructure (eg, high-volume roads and airports), and (5) water pollution. Each indicator is a percentile rank. All EBI domains are computed by summing corresponding indicators and converting the summated score into an overall percentile score. The overall EBI is similarly calculated using all indicators. Each neighborhood receives an EBI score ranging from 0 to 1, with 0 representing the lowest environmental burden and 1 representing the highest environmental burden. Detailed descriptions of all indicators included in the EBI are provided in eTable 1 in Supplement 1.
Covariates
Neighborhood-level social vulnerability index (SVI) was obtained from the CDC and Agency for Toxic Substances and Disease Registry. The SVI is a composite measure of demographic and socioeconomic factors that influence how communities respond to external stresses on human health.2,23 It encompasses 14 indicators reflecting data from 2015 to 2019 and spanning 4 separate domains, including (1) racial or ethnic minority status, (2) socioeconomic status (eg, poverty and unemployment), (3) household characteristics (eg, disability status and limited English-speaking ability), and (4) housing type (eg, group quarters). Each indicator is a percentile rank. Similar to the EBI, the SVI is calculated by summing indicators and converting the summated score into an overall percentile score. Each neighborhood receives an SVI score ranging from 0 to 1, with 0 representing the least social vulnerability and 1 representing the most social vulnerability. Detailed descriptions of all indicators included in the SVI are provided in eTable 2 in Supplement 1.
Data on neighborhood age and sex composition were obtained from the 2018 American Community Survey. Neighborhood-level rates of current smoking and routine checkup in the past year among adults were obtained from CDC PLACES. The number of nonfederal primary care physicians and physicians specializing in cardiovascular disease per 100 000 population at the county level were extracted from the 2018 Area Health Resources File. Neighborhoods were designated as urban (1-3) or rural (4-9) based on 2013 Rural-Urban Continuum Codes from the US Department of Agriculture.
Outcomes
We evaluated the prevalence of 3 cardiovascular risk factors: hypertension, diabetes, and obesity. Hypertension and diabetes were defined based on self-report of a clinical diagnosis by a health care professional. Obesity was defined as a body mass index of 30 or greater (calculated from self-reported weight and height as weight in kilograms divided by height in meters squared). We also evaluated the prevalence of 2 cardiovascular diseases: coronary heart disease and stroke. Coronary heart disease was defined based on self-report of a clinical diagnosis of angina or coronary heart disease by a health care professional. Stroke was also defined as a self-reported clinical diagnosis by a health care professional.
Statistical Analysis
Neighborhoods were divided into quartiles of environmental burden using the EBI. Neighborhoods in quartile 4 were designated as the most environmentally burdened and those in quartile 1 were designated as the least environmentally burdened. Neighborhood characteristics and covariates were summarized descriptively and compared across EBI quartiles using χ2 and Kruskal-Wallis tests.
For the main analysis, we fit mixed-effects linear regression models weighted for population size to evaluate differences in the prevalence of cardiovascular risk factors and diseases across quartiles of environmental burden at the neighborhood level. Random effects terms were included in models to account for clustering of neighborhoods within counties. Models were adjusted for neighborhood age and sex composition, SVI quartile, rurality, region (Midwest, Northeast, South, or West), and measures of health care access (number of physicians specializing in cardiovascular disease per 100 000 population, number of primary care physicians per 100 000 population, and percent of adults who received a routine checkup in the last year). We also repeated this main analysis after including the continuous SVI, rather than SVI quartiles, as a covariate in our models. As a sensitivity analysis, we adjusted models for neighborhood-level rates of current smoking because cigarette use could be considered either a confounder or mediator in this analysis.24,25 We then conducted a falsification test for our main analysis by evaluating the association between neighborhood environmental burden and the prevalence of arthritis, a non-cardiovascular health outcome that has not been strongly linked to environmental hazards.26,27
Next, to assess whether associations between environmental burden and cardiovascular health varied across different levels of neighborhood social vulnerability, EBI × SVI interaction terms were included in our models. Environmental burden was treated as a continuous exposure in these models to improve visualization of potential effect modification across different levels of neighborhood social vulnerability. The adjusted prevalence of cardiovascular risk factors and diseases based on environmental burden and stratified by neighborhood social vulnerability were estimated using marginal standardization of regression coefficients. To explore potential contributions of distinct environmental burden domains at different levels of neighborhood social vulnerability, we also fit multivariate mixed-effects linear regression models to evaluate associations between all 5 EBI domains and cardiovascular health stratified across SVI quartiles.
Finally, we performed an additional analysis to address the possibility that unmeasured factors contributed to observed associations between environmental burden and cardiovascular health. We first used matching to identify neighborhoods that were geospatially close to one another but had very different levels of environmental burden (Q4 vs Q1). Two matching methods were used.28 The first set of neighborhood pairs were generated through simple matching based on geospatial proximity within 50 miles. Geographic distance was calculated using longitude and latitude coordinates of the geometric centroid of neighborhoods obtained from the US Census Bureau. The second set of neighborhood pairs were generated using stricter criteria through exact matching for SVI quartile, rurality, and region and caliper matching for geospatial proximity (within 50 miles), sex composition (within 5% of percentage female), age composition (within 5% of percentage 65 years and older), per capita rate of cardiovascular disease physicians (within 5 per 100 000 population), per capita rate of primary care physicians (within 10 per 100 000 population), and percentage of adults who received a routine checkup in the last year (within 5%). We then used weighted and multivariate mixed-effects linear regression models with neighborhood pair random effects to determine associations between environmental burden and cardiovascular risk factors and diseases.
All statistical tests were 2-sided, and P < .05 was considered statistically significant. Analyses were conducted between March and October 2023 using STATA version 18.0 (StataCorp) and MATLAB 2022b (MathWorks).
Results
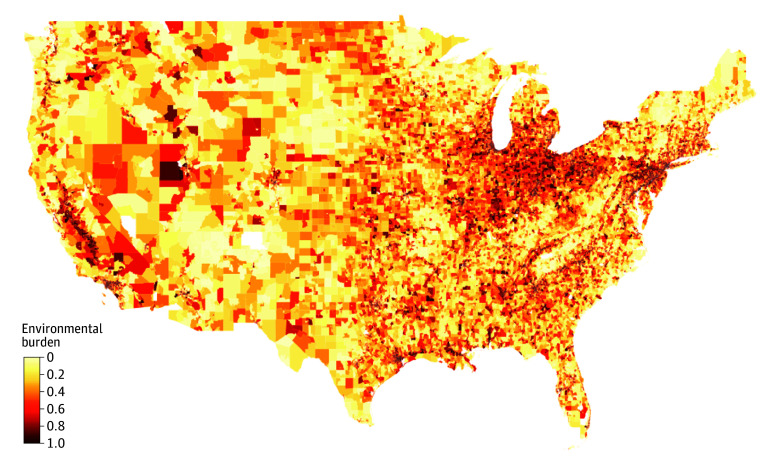
Our study sample included 71 659 neighborhoods across the US. The geographic distribution of neighborhood environmental burden is illustrated in Figure 1. Compared to those with the lowest environmental burden, neighborhoods with the highest environmental burden were more likely to be located in the Midwest (5191 [28.9%] vs 2782 [15.6%]) or Northeast (4782 [26.7%] vs 2004 [11.3%]), to be urban (16 626 [92.7%] vs 13 414 [75.4%]), and to have higher median (IQR) SVI scores (0.64 [0.36-0.85] vs 0.42 [0.20-0.65]) (Table 1). In addition, median (IQR) rates of poverty (16% [9-27] vs 10% [6-16]), uninsurance (15% [11-22] vs 12% [9-17]), and the proportion of adults in racial and ethnic minority groups (34% [12-73] vs 12% [5-30]) were higher in the most compared with the least environmentally burdened neighborhoods.
Figure 1. Neighborhood-Level Environmental Burden in the US.
Data on neighborhood level environmental burden index (EBI) were obtained from the US Centers for Disease Control and Prevention and the Agency for Toxic Substances and Disease Registry. The EBI encompasses the following 17 variables: (1) ozone; (2) fine particulate matter; (3) diesel particulate matter; (4) air toxics cancer risk; (5) national priority list sites; (6) toxic release inventory sites; (7) treatment, storage, and disposal sites; (8) risk management plan sites; (9) coal mines; (10) lead mines; (11) recreational parks; (12) houses built before 1980; (13) walkability; (14) high-volume roads; (15) railways; (16) airports, and (17) impaired surface water.
Table 1. Characteristics of Neighborhoods by Environmental Burden Quartile.
| Characteristic | All neighborhoods (N = 71 659) | Environmental burden quartile | P value | |||
|---|---|---|---|---|---|---|
| First (lowest) (n = 17 794) | Second (n = 17 967) | Third (n = 17 960) | Fourth (highest) (n = 17 938) | |||
| Total population, No. |
306 156 446 | 76 318 546 | 79 210 373 | 77 172 158 | 73 455 369 | |
| Age, median (IQR), y | 39 (34-44) | 42 (36-47) | 40 (35-45) | 39 (34-43) | 37 (32-42) | <.001 |
| Female, median % (IQR) | 51 (49-53) | 51 (49-53) | 51 (49-53) | 51 (49-53) | 51 (49-53) | <.001 |
| Census region, No. (%) | ||||||
| Midwest | 16 930 (23.6) | 2782 (15.6) | 4125 (23.0) | 4832 (26.9) | 5191 (28.9) | <.001 |
| Northeast | 13 343 (18.6) | 2004 (11.3) | 2731 (15.2) | 3826 (21.3) | 4782 (26.7) | |
| South | 25 951 (36.2) | 7356 (41.3) | 7339 (40.8) | 6290 (35.0) | 4966 (27.7) | |
| West | 15 435 (21.5) | 5652 (31.8) | 3772 (21.0) | 3012 (16.8) | 2999 (16.7) | |
| Rurality, No. (%)a | ||||||
| Rural | 11 864 (16.6) | 4380 (24.6) | 3690 (20.5) | 2482 (13.8) | 1312 (7.3) | <.001 |
| Urban | 59 795 (83.4) | 13 414 (75.4) | 14 277 (79.5) | 15 478 (86.2) | 16 626 (92.7) | |
| Health care access | ||||||
| Rate of annual physician visit, median % (IQR)b | 76 (73-79) | 75 (72-78) | 76 (73-79) | 77 (73-79) | 77 (73-80) | <.001 |
| Cardiologists per 100 000 population, median (IQR)c | 6 (3-9) | 5 (2-8) | 6 (2-9) | 7 (3-10) | 7 (5-11) | <.001 |
| Primary care physicians per 100 000 population, median (IQR)d | 73 (55-93) | 70 (49-86) | 72 (51-92) | 73 (55-95) | 74 (59-95) | <.001 |
| Social vulnerability index | ||||||
| Social vulnerability index score, median (IQR)e | 0.50 (0.25-0.75) | 0.42 (0.20-0.65) | 0.45 (0.22-0.70) | 0.51 (0.26-0.76) | 0.64 (0.36-0.85) | <.001 |
| Racial and ethnic minority population, median % (IQR)f | 19 (7-47) | 12 (5-30) | 15 (6-37) | 21 (7-50) | 34 (12-73) | <.001 |
| Poverty rate, median % (IQR)g | 12 (7-21) | 10 (6-16) | 11 (6-18) | 12 (7-21) | 16 (9-27) | <.001 |
| Uninsurance rate, median % (IQR)h | 13 (10-19) | 12 (9-17) | 13 (9-18) | 13 (10-19) | 15 (11-22) | <.001 |
| Population without high school diploma, median % (IQR)i | 10 (5-18) | 8 (4-14) | 9 (5-16) | 10 (6-18) | 14 (8-23) | <.001 |
Derived from 2013 Rural-Urban Continuum Codes from the US Department of Agriculture.
Neighborhood-level measure from the US Centers for Disease Control and Prevention’s PLACES data set of the percent of adults aged 18 years and older who report having been to a doctor for a routine checkup (eg, a general physical examination, not an examination for a specific injury, illness, or condition) in the previous year.
County-level number of physicians specializing in cardiovascular disease per 100 000 population from the Area Health Resources File.
County-level number of nonfederal primary care physicians per 100 000 population from the Area Health Resources File.
Neighborhood-level percentile ranked sum of social vulnerability indicators, ranging from 0 to 1, with 0 representing the least social vulnerability and 1 representing the most social vulnerability.
Percentage of neighborhood composed of racial and ethnic minority individuals (all persons except non-Hispanic White individuals).
Percentage of neighborhood population with incomes below 200% of the federal poverty level.
Percentage of civilian and noninstitutionalized population in the neighborhood with no health insurance.
Percentage of neighborhood population with no high school diploma among those 25 years and older.
Neighborhood Environmental Burden and Cardiovascular Health
Neighborhood environmental burden was significantly associated with a higher prevalence of cardiovascular risk factors and diseases in a dose-dependent manner (Figure 2). After adjustment for age, sex, SVI quartile, rurality, region, and health care access, the most environmentally burdened neighborhoods (quartile 4) had significantly higher rates of cardiovascular risk factors than the least environmentally burdened neighborhoods (quartile 1), including hypertension (mean [SD], 32.83% [7.99] vs 32.4% [6.99]; adjusted difference, 95% CI, 0.84%; 95% CI, 0.71-0.98), diabetes (mean [SD], 12.19% [4.33] vs 10.68% [3.27]; adjusted difference, 0.62%; 95% CI, 0.53-0.70), and obesity (mean [SD], 33.57% [7.62] vs 30.86% [6.15]; adjusted difference, 0.77%; 95% CI, 0.60-0.94). Similar patterns were observed across cardiovascular diseases, with significantly higher rates of coronary heart disease (mean [SD], 6.66% [2.15] vs 6.82% [2.41]; adjusted difference, 0.28%; 95% CI, 0.22-0.33) and stroke (mean [SD], 3.65% [1.47] vs 3.31% [1.12]; adjusted difference: 0.19%; 95% CI: 0.15-0.22) in the most vs least environmentally burdened neighborhoods. Notably, falsification testing revealed no significant associations between neighborhood environmental burden and prevalence of arthritis (eFigure 1 in Supplement 1).
Figure 2. Neighborhood Environmental Burden and Cardiovascular Risk Factor and Disease Prevalencea,b,c.
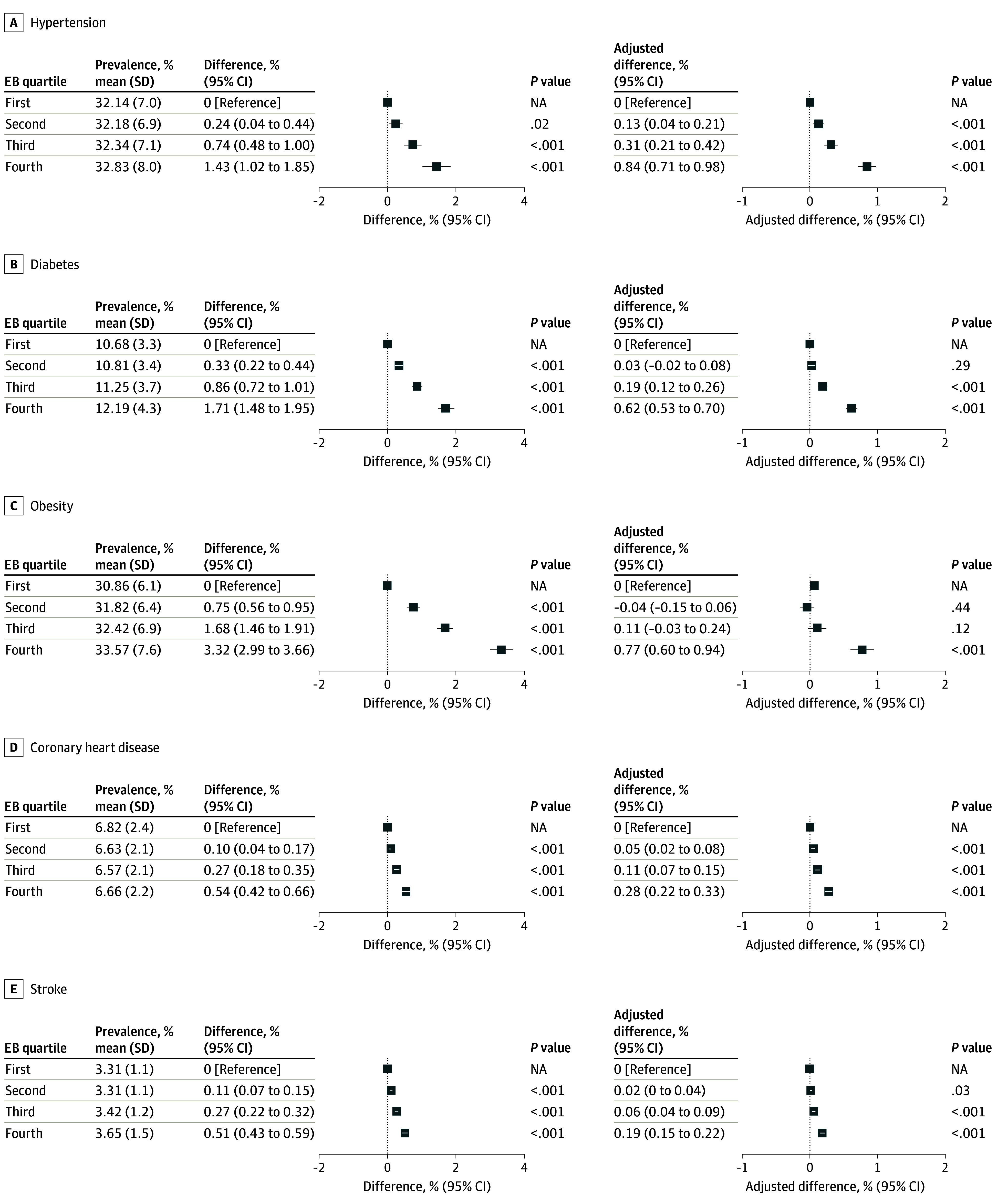
EB indicates environmental burden; NA, not applicable.
aDifferences between neighborhoods by environmental burden quartile were estimated using mixed-effects linear regression models weighted for population size and including county-level random effects.
bAdjusted differences were obtained from models that adjusted for social vulnerability index quartile, age (percentage 18-29, 30-44, 40-64, and ≥65 years), sex (percentage female), rurality, region (Midwest, Northeast, South, or West), and health care access (number of cardiovascular disease physicians per 100 000 population, number of primary care physicians per 100 000 population, and percentage of adults having received a routine checkup in the last year).
cError bars represent 95% CIs.
Neighborhood Environmental Burden and Cardiovascular Health by Social Vulnerability
The adjusted prevalence of each cardiovascular risk factor and disease by EBI is shown across neighborhood SVI quartiles in Figure 3. Neighborhoods with the highest level of social vulnerability had the largest estimated regression slopes for all outcomes, indicating a stronger association between environmental burden and cardiovascular risk factor and disease prevalence at higher levels of social vulnerability. The adjusted differences in cardiovascular risk factor prevalence across EBI quartiles were significantly more pronounced among highest SVI quartile neighborhoods vs lowest SVI quartile neighborhoods for hypertension (0.49%; 95% CI, 0.40-0.57 vs 0.13%; 95% CI, 0.08-0.18; P < .001 for interaction between EBI quartile and SVI quartile), diabetes (0.44%; 95% CI, 0.37-0.50 vs 0.05%; 95% CI, 0.02-0.07; P < .001 for interaction), and obesity (0.52%; 95% CI, 0.42-0.62 vs 0.05%; 95% CI, 0.00-0.11; P < .001 for interaction) (eTable 3 in Supplement 1). Associations between environmental burden and cardiovascular diseases were also stronger at higher levels of social vulnerability, including for coronary heart disease (0.16%; 95% CI, 0.13-0.20 vs 0.05%; 95% CI, 0.03-0.07; P < .001 for interaction) and stroke (0.13%; 95% CI, 0.10-0.15; vs 0.02%; 95% CI, 0.01-0.03; P < .001 for interaction).
Figure 3. Neighborhood Prevalence of Cardiovascular Risk Factor and Disease by Environmental Burden and Social Vulnerability.
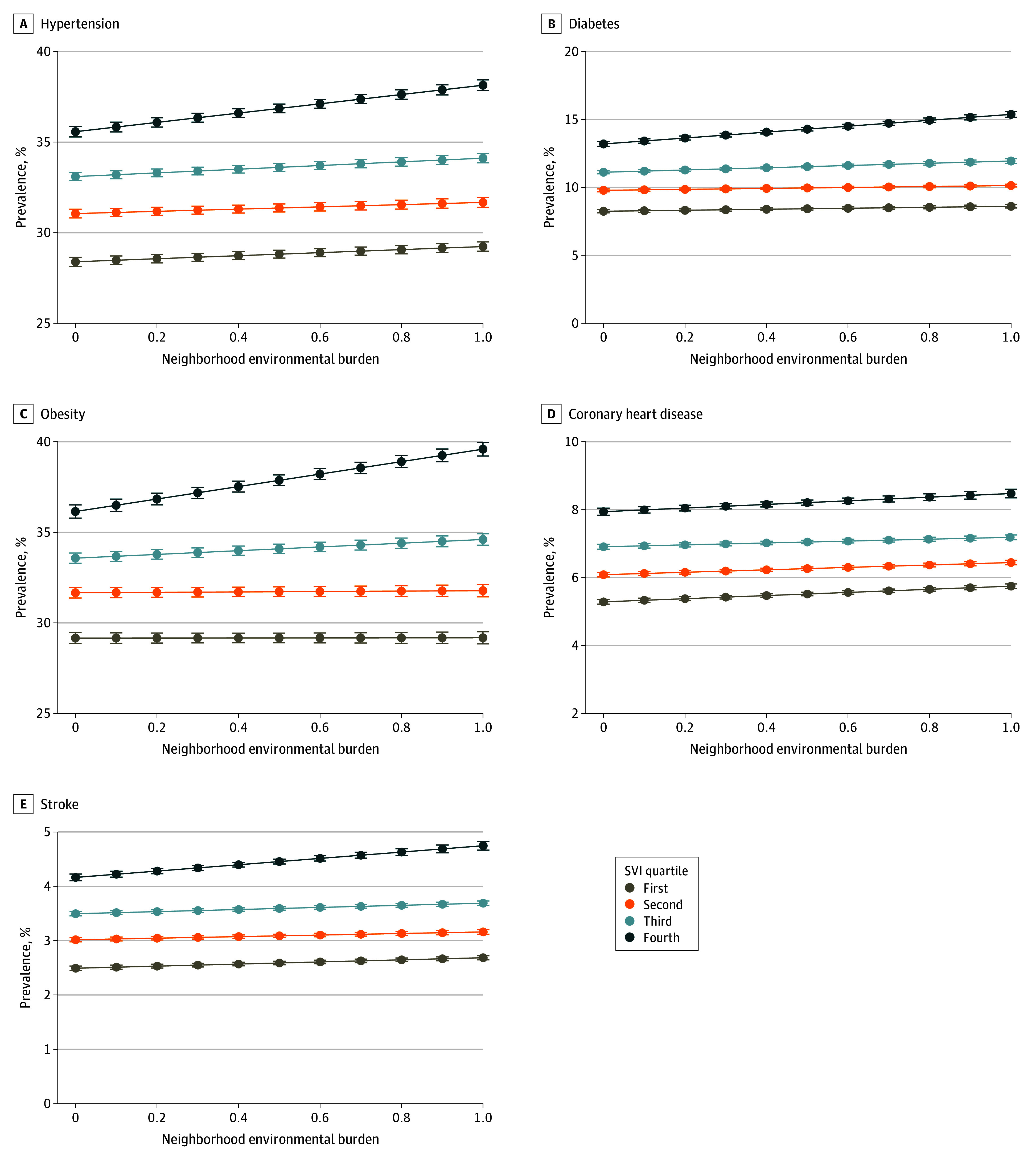
Adjusted prevalence rates were derived from marginal means extracted from mixed-effects linear regression models weighted for population size and including county-level random effects. Models included neighborhood environmental burden, social vulnerability index (SVI) quartile, an environmental burden index × SVI quartile interaction term, age (percentage 18-29, 30-44, 40-64, and ≥65 years), sex (percentage female), rurality, region (Midwest, Northeast, South, or West), and health care access (number of cardiovascular disease physicians per 100 000 population, number of primary care physicians per 100 000 population, and percentage of adults having received a routine checkup in the last year). Error bars represent 95% CIs.
The associations between separate EBI domains and cardiovascular risk factors and diseases varied across different levels of neighborhood social vulnerability (eTable 4 in Supplement 1). Associations were strongest for air pollution and hazardous and toxic sites among most socially vulnerable neighborhoods, whereas associations were strongest for the built environment among least socially vulnerable neighborhoods.
Sensitivity Analyses
The associations between environmental burden and cardiovascular health were similar after adjusting for SVI as a continuous variable (rather than SVI quartiles) in our models (eFigure 2 in Supplement 1). The inclusion of smoking prevalence as a covariate in models also yielded similar results (eFigure 3 in Supplement 1). The additional analysis that used geospatial-based and geospatial- and covariate-based matching of neighborhoods with very different levels of environmental burden (quartile 4 vs quartile 1) demonstrated findings consistent with the main analysis (Table 2). Geospatial-based matching identified 17 889 neighborhood pairs while both geospatial- and covariate-based matching identified 3497 neighborhood pairs. Adjusted differences in cardiovascular risk factor prevalence between the most and least environmentally burdened neighborhoods after geospatial-based and covariate-based matching were 0.62% (95% CI, 0.50-0.73) for hypertension, 0.56% (95% CI, 0.49-0.64) for diabetes, and 0.57% for obesity (95% CI, 0.44-0.70). Similar patterns were observed for cardiovascular diseases, with adjusted differences of 0.20% (95% CI, 0.16-0.25) for coronary heart disease and 0.14% (95% CI, 0.12-0.17) for stroke.
Table 2. Environmental Burden and Cardiovascular Risk Factor and Disease Prevalence Among Matched Neighborhoodsa.
| Outcome | Mean disease prevalence, % (SD) | |||||||
|---|---|---|---|---|---|---|---|---|
| Geospatially matched neighborhoods (n = 35 778)b | Geospatially and covariate-matched neighborhoods (n = 6994)c | |||||||
| Highest environmental burdend | Lowest environmental burdene | Adjusted risk difference, % (95% CI) | P value | Highest environmental burdend | Lowest environmental burdene | Adjusted risk difference, % (95% CI) | P value | |
| Cardiovascular risk factors | ||||||||
| Hypertension | 32.82 (8.00) | 30.99 (6.13) | 0.63 (0.56-0.70) | <.001 | 31.00 (6.78) | 30.93 (5.99) | 0.62 (0.50-0.73) | <.001 |
| Diabetes | 12.18 (4.33) | 9.87 (2.69) | 0.64 (0.60-0.68) | <.001 | 10.68 (3.62) | 10.31 (3.04) | 0.56 (0.49-0.64) | <.001 |
| Obesity | 33.56 (7.62) | 30.29 (5.68) | 0.54 (0.45-0.63) | <.001 | 31.23 (6.62) | 30.89 (5.96) | 0.57 (0.44-0.70) | <.001 |
| Cardiovascular diseases | ||||||||
| Coronary heart disease | 6.66 (2.15) | 6.14 (1.96) | 0.21 (0.19-0.23) | <.001 | 6.22 (1.98) | 6.16 (1.85) | 0.20 (0.16-0.25) | <.001 |
| Stroke | 3.65 (1.47) | 2.97 (0.93) | 0.17 (0.15-0.18) | <.001 | 3.20 (1.17) | 3.11 (0.98) | 0.14 (0.12-0.17) | <.001 |
Estimates were derived from mixed-effects linear regression models weighted for population size, including neighborhood pair random effects, and adjusting for social vulnerability index (SVI) quartile, age (percentage 18-29, 30-44, 40-64, and ≥65 years), sex (percentage female), rurality, region (Midwest, Northeast, South, or West), and health care access (number of cardiovascular disease physicians per 100 000 population, number of primary care physicians per 100 000 population, and percentage of adults having received a routine checkup in the last year). Estimates indicate adjusted risk difference in cardiovascular risk factor and disease prevalence between top environmental burden quartile and bottom environmental burden quartile neighborhoods.
Top and bottom environmental burden quartile neighborhoods were matched based on geospatial proximity (within 50 miles).
Top and bottom environmental burden quartile neighborhoods were exact matched on SVI quartile, rurality, and region, and caliper matched on geospatial proximity (within 50 miles), sex composition (within 5% of percentage female), age composition (within 5% of percent aged ≥65 years), per capita rate of cardiovascular disease physicians (within 5 per 100 000 population), per capita rate of primary care physicians (within 10 per 100 000 population), and percent of adults having received a routine checkup in the last year (within 5%).
Neighborhoods in the top environmental burden quartile.
Neighborhoods in the bottom environmental burden quartile.
Discussion
In this cross-sectional study, we found that greater cumulative environmental burden was associated with a higher prevalence of cardiovascular risk factors and diseases across US neighborhoods, even after controlling for neighborhood age and sex composition, social vulnerability, geography, and health care access. Although differences in the prevalence of hypertension, diabetes, obesity, coronary heart disease, and stroke between the most vs least environmentally burdened neighborhoods were modest, they translate to a substantial number of excess cases at a population level.29 In addition, associations between environmental burden and cardiovascular risk factor and disease prevalence were stronger at higher levels of neighborhood social vulnerability, indicating that environmental burden disproportionately influences cardiovascular health in socioeconomically disadvantaged and racial and ethnic minority communities across the US.
The association between cumulative environmental burden and cardiovascular health has important clinical and public health implications. The World Health Organization estimates that 35% and 42% of global disability adjusted life years due to ischemic heart disease and stroke are attributable to modifiable environmental risks, respectively.26 Our findings reveal significant variation in cumulative environmental burden (air pollution, hazardous and toxic sites, poor built environment, transportation infrastructure, and water pollution) across US neighborhoods and underscore the role these hazards collectively play as determinants of cardiovascular health. Prior research of animal models and humans have identified that environmental exposures, such as air and noise pollution, erode cardiovascular health through the induction of chronic inflammation, oxidative stress, endothelial dysfunction, and autonomic imbalance.6,30,31 These mechanisms underlying cardiovascular disease pathogenesis overlap with those of traditional risk factors, such as cigarette smoking, unhealthy diets, and physical inactivity.32 However, the impact of environmental burdens on cardiovascular health, such as the causal role of PM2.5 exposure,9 has largely been absent from major clinical and cardiovascular practice guidelines.33,34,35 Our study highlights the need for health systems, policymakers, and leaders from other sectors to intensify efforts to implement multifaceted initiatives that both identify and address environmental burdens and their negative effects on cardiovascular health.36,37
We also found that the most socially vulnerable neighborhoods were more likely to experience greater levels of environmental burden. This environmental injustice—rooted in factors such as economic inequality and systemic racism (eg, historical redlining)—has resulted in the concentration of low income and people of racial and ethnic minority groups in regions in close proximity to polluting facilities, major roadways, landfills, and other hazardous environmental exposures.38,39,40 The most-impacted neighborhoods often lack the political power and resources to influence decision-making processes and advocate against policies that exacerbate environmental burdens.
The stronger associations between environmental burden and poor cardiovascular health observed at higher levels of social vulnerability illustrate the greater environmental susceptibility of disadvantaged neighborhoods. These areas may lack the resources and opportunities to mitigate the harms of environmental burdens. For example, individuals living in lower socioeconomic status neighborhoods may be unable to afford high-quality air purification systems,41,42 depend on occupational roles that increase direct exposure to surrounding environmental hazards,43 or could be discouraged from using nearby recreational facilities and green spaces due to safety concerns.44 The detrimental pathophysiological pathways induced by environmental burdens may also accentuate and magnify stress-related responses known to be associated with social disadvantage.45 Multilevel interventions that improve environmental conditions in the most socially vulnerable neighborhoods, which are disproportionately exposed to and uniquely susceptible to the health-harming effects of environmental burdens, could help reduce inequities in cardiovascular health outcomes.46
Our study highlights the importance of ongoing and future initiatives to address environmental burdens, especially in the context of the current climate crisis worsened by continued emission of greenhouse gases, deforestation, and urbanization.47,48 Most health care spending in the US has historically been allocated to the treatment of individuals and less so on the protection of population health, as laid bare by the COVID-19 pandemic.49,50 Recent federal legislation such as the 2021 Infrastructure Investment and Jobs Act and 2022 Inflation Reduction Act include important provisions focused on environmental remediation. Policy makers should continue to expand evidence-based interventions to improve local environmental conditions, including source-specific emission standards, vehicle electrification, and toxic site cleanup programs.51,52 Collaborations between health professionals, local governments, and other sectors could also enable heart-healthy and sustainable built environments, such as higher-density compact cities that reduce private car usage, promote active transportation, and encourage physical activity.6,53 Concerted efforts to reduce inequities in environmental burden will also be critical. One recent example is the enactment of the Justice40 Initiative, which requires that 40% of benefits from federal investments in areas such as climate change, clean energy, transit, sustainable housing, and remediation of legacy pollution are directed to marginalized and disadvantaged communities.54,55
Limitations
Our study has several limitations. First, although this cross-sectional analysis adjusted for demographic characteristics, social vulnerability, health care access, and other geographic features, it is possible that we were not able to account for other important covariates not captured by study data sets. However, our findings were highly consistent even after performing geospatial-matching analyses to address the potential for unobserved confounders related to geography. Furthermore, falsification testing revealed no evidence of residual confounding given lack of observed association between environmental burden and a negative control outcome. Second, neighborhood-level outcome data were derived from a multilevel regression and poststratification approach conducted by the CDC. Several validation studies have reported concordance between model-based and direct estimates for health outcomes.56,57 Third, the prevalence of cardiovascular risk factors and diseases were based on self-report of clinical diagnoses and were therefore subject to recall and social desirability bias. However, previous studies have reported that prevalence estimates for study outcomes from the Behavioral Risk Factor Surveillance System are reliable, valid, and concordant with results from face-to-face interviews, such as the National Health and Nutrition Examination Survey and National Health Interview Survey.58,59 In addition, receiving a clinical diagnosis is conditional on access to a health care professional; the most environmentally burdened neighborhoods (which tend to have lower average socioeconomic status) experience worse access to care, which would bias observed associations to the null. Fourth, the measure of environmental burden in this study does not capture all possible environmental hazards, including extreme heat and weather events that have been exacerbated by climate change.60,61 Nonetheless, the EBI has been sequentially developed and validated by the CDC and is uniquely positioned to identify cumulative environmental burden across the contiguous US with available data and at a highly granular level.19 Fifth, these ecological findings are important for understanding population-level associations between cumulative environmental burden and cardiovascular health but should not be generalized to individual-level exposures and outcomes.
Conclusions
The findings in this study indicate that across US neighborhoods, cumulative environmental burden was associated with small but statistically significantly higher rates of cardiovascular risk factors and diseases. These associations were most pronounced in socially vulnerable neighborhoods that are also disproportionately exposed to environmental hazards. Future prospective investigations are needed to evaluate whether addressing poor environmental conditions, particularly in the most socially vulnerable neighborhoods, improves cardiovascular health outcomes and equity.
eMethods. CDC PLACES Multi-Level Regression and Poststratification Approach
eTable 1. Detailed Description of the Environmental Burden Index
eTable 2. Detailed Description of the Social Vulnerability Index
eTable 3. Cardiovascular Risk Factor and Disease Prevalence by Neighborhood Environmental Burden and Social Vulnerability
eTable 4. Domains of Environmental Burden and Cardiovascular Risk Factor and Disease Prevalence by Neighborhood Social Vulnerability
eFigure 1. Neighborhood Environmental Burden and Arthritis Prevalence
eFigure 2. Neighborhood Environmental Burden and Cardiovascular Risk Factor and Disease Prevalence Adjusting for Continuous Social Vulnerability Index
eFigure 3. Neighborhood Environmental Burden and Cardiovascular Risk Factor and Disease Prevalence Adjusting for Current Smoking Rate
eReferences
Data sharing statement
References
- 1.Ahmad FB, Anderson RN. The leading causes of death in the US for 2020. JAMA. 2021;325(18):1829-1830. doi: 10.1001/jama.2021.5469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khan SU, Javed Z, Lone AN, et al. Social vulnerability and premature cardiovascular mortality among US counties, 2014 to 2018. Circulation. 2021;144(16):1272-1279. doi: 10.1161/CIRCULATIONAHA.121.054516 [DOI] [PubMed] [Google Scholar]
- 3.Shah NS, Ning H, Petito LC, et al. Associations of clinical and social risk factors with racial differences in premature cardiovascular disease. Circulation. 2022;146(3):201-210. doi: 10.1161/CIRCULATIONAHA.121.058311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beckman AL, Herrin J, Nasir K, Desai NR, Spatz ES. Trends in cardiovascular health of US adults by income, 2005-2014. JAMA Cardiol. 2017;2(7):814-816. doi: 10.1001/jamacardio.2017.1654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schultz WM, Kelli HM, Lisko JC, et al. Socioeconomic status and cardiovascular outcomes: challenges and interventions. Circulation. 2018;137(20):2166-2178. doi: 10.1161/CIRCULATIONAHA.117.029652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Münzel T, Hahad O, Sørensen M, et al. Environmental risk factors and cardiovascular diseases: a comprehensive expert review. Cardiovasc Res. 2022;118(14):2880-2902. doi: 10.1093/cvr/cvab316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rajagopalan S, Landrigan PJ. Pollution and the heart. N Engl J Med. 2021;385(20):1881-1892. doi: 10.1056/NEJMra2030281 [DOI] [PubMed] [Google Scholar]
- 8.Di Q, Wang Y, Zanobetti A, et al. Air pollution and mortality in the Medicare population. N Engl J Med. 2017;376(26):2513-2522. doi: 10.1056/NEJMoa1702747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brook RD, Franklin B, Cascio W, et al. ; Expert Panel on Population and Prevention Science of the American Heart Association . Air pollution and cardiovascular disease: a statement for healthcare professionals from the Expert Panel on Population and Prevention Science of the American Heart Association. Circulation. 2004;109(21):2655-2671. doi: 10.1161/01.CIR.0000128587.30041.C8 [DOI] [PubMed] [Google Scholar]
- 10.Miller KA, Siscovick DS, Sheppard L, et al. Long-term exposure to air pollution and incidence of cardiovascular events in women. N Engl J Med. 2007;356(5):447-458. doi: 10.1056/NEJMoa054409 [DOI] [PubMed] [Google Scholar]
- 11.Thurston GD, Burnett RT, Turner MC, et al. Ischemic heart disease mortality and long-term exposure to source-related components of U.S. fine particle air pollution. Environ Health Perspect. 2016;124(6):785-794. doi: 10.1289/ehp.1509777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chowdhury R, Ramond A, O’Keeffe LM, et al. Environmental toxic metal contaminants and risk of cardiovascular disease: systematic review and meta-analysis. BMJ. 2018;362:k3310. doi: 10.1136/bmj.k3310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Münzel T, Sørensen M, Daiber A. Transportation noise pollution and cardiovascular disease. Nat Rev Cardiol. 2021;18(9):619-636. doi: 10.1038/s41569-021-00532-5 [DOI] [PubMed] [Google Scholar]
- 14.Münzel T, Gori T, Babisch W, Basner M. Cardiovascular effects of environmental noise exposure. Eur Heart J. 2014;35(13):829-836. doi: 10.1093/eurheartj/ehu030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sallis JF, Floyd MF, Rodríguez DA, Saelens BE. Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation. 2012;125(5):729-737. doi: 10.1161/CIRCULATIONAHA.110.969022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tessum CW, Paolella DA, Chambliss SE, Apte JS, Hill JD, Marshall JD. PM2.5 polluters disproportionately and systemically affect people of color in the United States. Sci Adv. 2021;7(18):eabf4491. doi: 10.1126/sciadv.abf4491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Josey KP, Delaney SW, Wu X, et al. Air pollution and mortality at the intersection of race and social class. N Engl J Med. 2023;388(15):1396-1404. doi: 10.1056/NEJMsa2300523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jbaily A, Zhou X, Liu J, et al. Air pollution exposure disparities across US population and income groups. Nature. 2022;601(7892):228-233. doi: 10.1038/s41586-021-04190-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Owusu C, Flanagan B, Lavery AM, et al. Developing a granular scale environmental burden index (EBI) for diverse land cover types across the contiguous United States. Sci Total Environ. 2022;838(pt 1):155908. doi: 10.1016/j.scitotenv.2022.155908 [DOI] [PubMed] [Google Scholar]
- 20.Zhang X, Holt JB, Yun S, Lu H, Greenlund KJ, Croft JB. Validation of multilevel regression and poststratification methodology for small area estimation of health indicators from the behavioral risk factor surveillance system. Am J Epidemiol. 2015;182(2):127-137. doi: 10.1093/aje/kwv002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Greenlund KJ, Lu H, Wang Y, et al. PLACES: local data for better health. Prev Chronic Dis. 2022;19:E31. doi: 10.5888/pcd19.210459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stephenson J. Federal agencies launch tool to measure health effects of environmental hazards for communities. JAMA Health Forum. 2022;3(8):e223527. doi: 10.1001/jamahealthforum.2022.3527 [DOI] [PubMed] [Google Scholar]
- 23.Jain V, Al Rifai M, Khan SU, et al. Association between social vulnerability index and cardiovascular disease: a behavioral risk factor surveillance system study. J Am Heart Assoc. 2022;11(15):e024414. doi: 10.1161/JAHA.121.024414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peris E, Fenech B. Associations and effect modification between transportation noise, self-reported response to noise and the wider determinants of health: A narrative synthesis of the literature. Sci Total Environ. 2020;748:141040. doi: 10.1016/j.scitotenv.2020.141040 [DOI] [PubMed] [Google Scholar]
- 25.Martin L, White MP, Pahl S, May J, Wheeler BW. Neighbourhood greenspace and smoking prevalence: Results from a nationally representative survey in England. Soc Sci Med. 2020;265:113448. doi: 10.1016/j.socscimed.2020.113448 [DOI] [PubMed] [Google Scholar]
- 26.Prüss-Ustün A, Wolf J, Corvalán C, Neville T, Bos R, Neira M. Diseases due to unhealthy environments: an updated estimate of the global burden of disease attributable to environmental determinants of health. J Public Health (Oxf). 2017;39(3):464-475. doi: 10.1093/pubmed/fdw085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Murray CJL, Aravkin AY, Zheng P, et al. ; GBD 2019 Risk Factors Collaborators . Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223-1249. doi: 10.1016/S0140-6736(20)30752-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stuart EA. Matching methods for causal inference: a review and a look forward. Stat Sci. 2010;25(1):1-21. doi: 10.1214/09-STS313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rose G. Sick individuals and sick populations. Int J Epidemiol. 2001;30(3):427-432. doi: 10.1093/ije/30.3.427 [DOI] [PubMed] [Google Scholar]
- 30.Münzel T, Sørensen M, Gori T, et al. Environmental stressors and cardio-metabolic disease: part II-mechanistic insights. Eur Heart J. 2017;38(8):557-564. doi: 10.1093/eurheartj/ehw294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cosselman KE, Navas-Acien A, Kaufman JD. Environmental factors in cardiovascular disease. Nat Rev Cardiol. 2015;12(11):627-642. doi: 10.1038/nrcardio.2015.152 [DOI] [PubMed] [Google Scholar]
- 32.Mozaffarian D, Wilson PWF, Kannel WB. Beyond established and novel risk factors: lifestyle risk factors for cardiovascular disease. Circulation. 2008;117(23):3031-3038. doi: 10.1161/CIRCULATIONAHA.107.738732 [DOI] [PubMed] [Google Scholar]
- 33.American Diabetes Association Professional Practice Committee . 1. Improving care and promoting health in populations: standards of medical care in diabetes—2022. Diabetes Care. 2022;45(suppl 1):S8-S16. doi: 10.2337/dc22-S001 [DOI] [PubMed] [Google Scholar]
- 34.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 2018;71(19):e127-e248. doi: 10.1016/j.jacc.2017.11.006 [DOI] [PubMed] [Google Scholar]
- 35.Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 2019;74(10):1376-1414. doi: 10.1016/j.jacc.2019.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Salas RN, Friend TH, Bernstein A, Jha AK. Adding a climate lens to health policy in the United States. Health Aff (Millwood). 2020;39(12):2063-2070. doi: 10.1377/hlthaff.2020.01352 [DOI] [PubMed] [Google Scholar]
- 37.Romanello M, Di Napoli C, Drummond P, et al. The 2022 report of the Lancet Countdown on health and climate change: health at the mercy of fossil fuels. Lancet. 2022;400(10363):1619-1654. doi: 10.1016/S0140-6736(22)01540-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chowkwanyun M. Environmental justice: where it has been, and where it might be going. Annu Rev Public Health. 2023;44:93-111. doi: 10.1146/annurev-publhealth-071621-064925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Salas RN. Environmental racism and climate change—missed diagnoses. N Engl J Med. 2021;385(11):967-969. doi: 10.1056/NEJMp2109160 [DOI] [PubMed] [Google Scholar]
- 40.Wadhera RK, Dahabreh IJ. The US health equity crisis—an economic case for a moral imperative? JAMA. 2023;329(19):1647-1649. doi: 10.1001/jama.2023.4018 [DOI] [PubMed] [Google Scholar]
- 41.Chen R, Zhao A, Chen H, et al. Cardiopulmonary benefits of reducing indoor particles of outdoor origin: a randomized, double-blind crossover trial of air purifiers. J Am Coll Cardiol. 2015;65(21):2279-2287. doi: 10.1016/j.jacc.2015.03.553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li H, Cai J, Chen R, et al. Particulate matter exposure and stress hormone levels: a randomized, double-blind, crossover trial of air purification. Circulation. 2017;136(7):618-627. doi: 10.1161/CIRCULATIONAHA.116.026796 [DOI] [PubMed] [Google Scholar]
- 43.Gochfeld M, Burger J. Disproportionate exposures in environmental justice and other populations: the importance of outliers. Am J Public Health. 2011;101(Suppl 1)(suppl 1):S53-S63. doi: 10.2105/AJPH.2011.300121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Weiss CC, Purciel M, Bader M, et al. Reconsidering access: park facilities and neighborhood disamenities in New York City. J Urban Health. 2011;88(2):297-310. doi: 10.1007/s11524-011-9551-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tawakol A, Osborne MT, Wang Y, et al. Stress-associated neurobiological pathway linking socioeconomic disparities to cardiovascular disease. J Am Coll Cardiol. 2019;73(25):3243-3255. doi: 10.1016/j.jacc.2019.04.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ward JB, Gartner DR, Keyes KM, Fliss MD, McClure ES, Robinson WR. How do we assess a racial disparity in health? distribution, interaction, and interpretation in epidemiological studies. Ann Epidemiol. 2019;29:1-7. doi: 10.1016/j.annepidem.2018.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Atwoli L, Baqui AH, Benfield T, et al. Call for emergency action to limit global temperature increases, restore biodiversity, and protect health. Lancet. 2021;398(10304):939-941. doi: 10.1016/S0140-6736(21)01915-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McMichael AJ. Globalization, climate change, and human health. N Engl J Med. 2013;368(14):1335-1343. doi: 10.1056/NEJMra1109341 [DOI] [PubMed] [Google Scholar]
- 49.Committee on Public Health Strategies to Improve Health, Institute of Medicine . For the Public’s Health: Investing in a Healthier Future. National Academies Press; 2012. https://www.ncbi.nlm.nih.gov/books/NBK201023/ [PubMed] [Google Scholar]
- 50.Maani N, Galea S. COVID-19 and underinvestment in the public health infrastructure of the United States. Milbank Q. 2020;98(2):250-259. doi: 10.1111/1468-0009.12463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Choma EF, Evans JS, Hammitt JK, Gómez-Ibáñez JA, Spengler JD. Assessing the health impacts of electric vehicles through air pollution in the United States. Environ Int. 2020;144:106015. doi: 10.1016/j.envint.2020.106015 [DOI] [PubMed] [Google Scholar]
- 52.Landrigan PJ, Fuller R, Acosta NJR, et al. The Lancet Commission on pollution and health. Lancet. 2018;391(10119):462-512. doi: 10.1016/S0140-6736(17)32345-0 [DOI] [PubMed] [Google Scholar]
- 53.Stevenson M, Thompson J, de Sá TH, et al. Land use, transport, and population health: estimating the health benefits of compact cities. Lancet. 2016;388(10062):2925-2935. doi: 10.1016/S0140-6736(16)30067-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Patel VR, Jella T, Gupta A, Nassel A, Ibrahim A, Hussaini SMQ. Association of neighborhood-level environmental injustice with health status in the US. JAMA Intern Med. 2023;183(10):1162-1163. doi: 10.1001/jamainternmed.2023.2835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Morello-Frosch R, Obasogie OK. The climate gap and the color line—racial health inequities and climate change. N Engl J Med. 2023;388(10):943-949. doi: 10.1056/NEJMsb2213250 [DOI] [PubMed] [Google Scholar]
- 56.Zhang X, Holt JB, Lu H, et al. Multilevel regression and poststratification for small-area estimation of population health outcomes: a case study of chronic obstructive pulmonary disease prevalence using the behavioral risk factor surveillance system. Am J Epidemiol. 2014;179(8):1025-1033. doi: 10.1093/aje/kwu018 [DOI] [PubMed] [Google Scholar]
- 57.Wang Y, Holt JB, Zhang X, et al. Comparison of methods for estimating prevalence of chronic diseases and health behaviors for small geographic areas: Boston Validation Study, 2013. Prev Chronic Dis. 2017;14:E99. doi: 10.5888/pcd14.170281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pierannunzi C, Hu SS, Balluz L. A systematic review of publications assessing reliability and validity of the Behavioral Risk Factor Surveillance System (BRFSS), 2004-2011. BMC Med Res Methodol. 2013;13(1):49. doi: 10.1186/1471-2288-13-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Li C, Balluz LS, Ford ES, Okoro CA, Zhao G, Pierannunzi C. A comparison of prevalence estimates for selected health indicators and chronic diseases or conditions from the Behavioral Risk Factor Surveillance System, the National Health Interview Survey, and the National Health and Nutrition Examination Survey, 2007-2008. Prev Med. 2012;54(6):381-387. doi: 10.1016/j.ypmed.2012.04.003 [DOI] [PubMed] [Google Scholar]
- 60.Khatana SAM, Werner RM, Groeneveld PW. Association of extreme heat and cardiovascular mortality in the United States: a county-level longitudinal analysis from 2008 to 2017. Circulation. 2022;146(3):249-261. Published online July 19, 2022. doi: 10.1161/CIRCULATIONAHA.122.060746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Babaie J, Pashaei Asl Y, Naghipour B, Faridaalaee G. Cardiovascular diseases in natural disasters; a systematic review. Arch Acad Emerg Med. 2021;9(1):e36. doi: 10.22037/aaem.v9i1.1208 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. CDC PLACES Multi-Level Regression and Poststratification Approach
eTable 1. Detailed Description of the Environmental Burden Index
eTable 2. Detailed Description of the Social Vulnerability Index
eTable 3. Cardiovascular Risk Factor and Disease Prevalence by Neighborhood Environmental Burden and Social Vulnerability
eTable 4. Domains of Environmental Burden and Cardiovascular Risk Factor and Disease Prevalence by Neighborhood Social Vulnerability
eFigure 1. Neighborhood Environmental Burden and Arthritis Prevalence
eFigure 2. Neighborhood Environmental Burden and Cardiovascular Risk Factor and Disease Prevalence Adjusting for Continuous Social Vulnerability Index
eFigure 3. Neighborhood Environmental Burden and Cardiovascular Risk Factor and Disease Prevalence Adjusting for Current Smoking Rate
eReferences
Data sharing statement