Abstract
Background
Otitis media with effusion (OME) is an accumulation of fluid in the middle ear cavity, common amongst young children. It may cause hearing loss which, when persistent, may lead to developmental delay, social difficulty and poor quality of life. Management includes watchful waiting, autoinflation, medical and surgical treatment. Insertion of ventilation tubes has often been used as the preferred treatment.
Objectives
To evaluate the effects (benefits and harms) of ventilation tubes (grommets) for OME in children.
Search methods
We searched the Cochrane ENT Register, CENTRAL, Ovid MEDLINE, Ovid Embase, Web of Science, ClinicalTrials.gov, ICTRP and additional sources for published and unpublished trials on 20 January 2023.
Selection criteria
We included randomised controlled trials (RCTs) and quasi‐RCTs in children (6 months to 12 years) with OME for ≥ 3 months. We included studies that compared ventilation tube (VT) insertion with five comparators: no treatment, watchful waiting (ventilation tubes inserted later, if required), myringotomy, hearing aids and other non‐surgical treatments.
Data collection and analysis
We used standard Cochrane methods. Our primary outcomes were determined following a multi‐stakeholder prioritisation exercise and were: 1) hearing; 2) OME‐specific quality of life; 3) persistent tympanic membrane perforation (as a severe adverse effect of the surgery). Secondary outcomes were: 1) persistence of OME; 2) other adverse effects (including tympanosclerosis, VT blockage and pain); 3) receptive language skills; 4) speech development; 5) cognitive development; 6) psychosocial skills; 7) listening skills; 8) generic health‐related quality of life; 9) parental stress; 10) vestibular function; 11) episodes of acute otitis media. We used GRADE to assess the certainty of evidence for key outcomes.
Although we included all measures of hearing assessment, the proportion of children who returned to normal hearing was our preferred method, due to challenges in interpreting the results of mean hearing thresholds.
Main results
We included 19 RCTs (2888 children). We considered most of the evidence to be very uncertain, due to wide confidence intervals for the effect estimates, few participants, and a risk of performance and detection bias. Here we report our key outcomes at the longest reported follow‐up. There were some limitations to the evidence. No studies investigated the comparison of ventilation tubes versus hearing aids. We did not identify any data on disease‐specific quality of life; however, many studies were conducted before the development of specific tools to assess this in otitis media. Short‐acting ventilation tubes were used in most studies and thus specific data on the use of long‐acting VTs is limited. Finally, we did not identify specific data on the effects of VTs in children at increased risk of OME (e.g. with craniofacial syndromes).
Ventilation tubes versus no treatment (four studies)
The odds ratio (OR) for a return to normal hearing after 12 months was 1.13 with VTs (95% confidence interval (CI) 0.46 to 2.74; 54% versus 51%; 1 study, 72 participants; very low‐certainty evidence).
At six months, VTs may lead to a large reduction in persistent OME (risk ratio (RR) 0.30, 95% CI 0.14 to 0.65; 20.4% versus 68.0%; 1 study, 54 participants; low‐certainty evidence).
The evidence is very uncertain about the chance of persistent tympanic membrane perforation with VTs at 12 months (OR 0.85, 95% CI 0.38 to 1.91; 8.3% versus 9.7%; 1 RCT, 144 participants).
Early ventilation tubes versus watchful waiting (six studies)
There was little to no difference in the proportion of children whose hearing returned to normal after 8 to 10 years (i.e. by the age of 9 to 13 years) (RR for VTs 0.98, 95% CI 0.94 to 1.03; 93% versus 95%; 1 study, 391 participants; very low‐certainty evidence).
VTs may also result in little to no difference in the risk of persistent OME after 18 months to 6 years (RR 1.21, 95% CI 0.84 to 1.74; 15% versus 12%; 3 studies, 584 participants; very low‐certainty evidence).
We were unable to pool data on persistent perforation. One study showed that VTs may increase the risk of perforation after a follow‐up duration of 3.75 years (RR 3.65, 95% CI 0.41 to 32.38; 1 study, 391 participants; very low‐certainty evidence) but the actual number of children who develop persistent perforation may be low, as demonstrated by another study (1.26%; 1 study, 635 ears; very low‐certainty evidence).
Ventilation tubes versus non‐surgical treatment (one study)
One study compared VTs to six months of antibiotics (sulphisoxazole). No data were available on return to normal hearing, but final hearing thresholds were reported. At four months, the mean difference was ‐5.98 dB HL lower (better) for those receiving VTs, but the evidence is very uncertain (95% CI ‐9.21 to ‐2.75; 1 study, 125 participants; very low‐certainty evidence).
No evidence was identified regarding persistent OME.
VTs may result in a low risk of persistent perforation at 18 months of follow‐up (no events reported; narrative synthesis of 1 study, 60 participants; low‐certainty evidence).
Ventilation tubes versus myringotomy (nine studies)
We are uncertain whether VTs may slightly increase the likelihood of returning to normal hearing at 6 to 12 months, since the confidence intervals were wide and included the possibility of no effect (RR 1.22, 95% CI 0.59 to 2.53; 74% versus 64%; 2 studies, 132 participants; very low‐certainty evidence).
After six months, persistent OME may be reduced for those who receive VTs compared to laser myringotomy, but the evidence is very uncertain (OR 0.27, 95% CI 0.19 to 0.38; 1 study, 272 participants; very low‐certainty evidence).
At six months, the risk of persistent perforation is probably similar with the use of VTs or laser myringotomy (narrative synthesis of 6 studies, 581 participants; moderate‐certainty evidence).
Authors' conclusions
There may be small short‐ and medium‐term improvements in hearing and persistence of OME with VTs, but it is unclear whether these persist after longer follow‐up.
The RCTs included do not allow us to say when (or how much) VTs improve hearing in any specific child. However, interpretation of the evidence is difficult: many children in the control groups recover spontaneously or receive VTs during follow‐up, VTs may block or extrude, and OME may recur. The limited evidence in this review also affects the generalisability/applicability of our findings to situations involving children with underlying conditions (e.g. craniofacial syndromes) or the use of long‐acting tubes.
Consequently, RCTs may not be the best way to determine whether an intervention is likely to be effective in any individual child. Instead, we must better understand the different OME phenotypes to target interventions to children who will benefit most, and avoid over‐treating when spontaneous resolution is likely.
Keywords: Adolescent; Child; Child, Preschool; Humans; Anti-Bacterial Agents; Anti-Bacterial Agents/therapeutic use; Hearing Loss; Neoplasm Recurrence, Local; Neoplasm Recurrence, Local/drug therapy; Otitis Media with Effusion; Otitis Media with Effusion/etiology; Tympanic Membrane Perforation; Tympanic Membrane Perforation/complications; Tympanic Membrane Perforation/drug therapy
Plain language summary
Ventilation tubes (grommets) for otitis media with effusion (OME or 'glue ear') in children
Key messages
‐ From the studies included in this review, we are uncertain to what extent ventilation tubes improve hearing. Glue ear is a fluctuating condition, with high rates of spontaneous resolution and recurrence, which makes it difficult to study in a clinical trial.
‐ Ventilation tubes may slightly reduce the number of children who have glue ear after three to six months of follow‐up. It is not clear whether they also have an effect over longer periods of time.
‐ Insertion of ventilation tubes can lead to a persistent hole in the eardrum (tympanic membrane perforation), ranging from 0% to 12% in the studies that we assessed.
What is OME?
Glue ear (or 'otitis media with effusion', OME) is a relatively common condition affecting young children. Fluid collects in the middle ear, which may cause hearing impairment. As a result of their poor hearing, children may be behind in their speech and may have difficulties at school.
How is OME treated?
Most of the time OME does not need any treatment and the symptoms will get better with time. In children with persistent OME, different treatments have been used, including medications or surgery (insertion of grommets, with or without adenoidectomy). Ventilation tubes (grommets) are tiny plastic or silicon tubes, which are inserted in the eardrum under general anaesthesia. The tube allows fluid to drain out of the middle ear and allows air to enter.
What did we want to find out?
We wanted to identify whether insertion of ventilation tubes was better than no treatment, or other types of treatment (such as medicines or hearing aids), for children with OME. We also wanted to see if there were any unwanted effects associated with having ventilation tubes inserted.
What did we do?
We searched for studies that compared ventilation tubes with either no treatment or a different treatment, in children with OME. We compared and summarised the study results, and rated our confidence in the evidence, based on factors such as study methods and sizes.
What did we find?
We included 19 studies with a total of 2888 participants. We considered the majority of the evidence we found to be uncertain, because of the relatively small number of children included and some issues with the conduct of the studies. The evidence from the studies done so far does not allow us to say when, and by how much, ventilation tubes will improve hearing in any specific child.
We looked for studies that compared ventilation tubes to different types of treatment, including no treatment, delayed treatment with ventilation tubes (if needed), hearing aids, antibiotics or creating a small hole in the eardrum (called 'myringotomy'). We did not find any studies that compared ventilation tubes to hearing aids, but we did find evidence for the other comparisons.
Ventilation tubes may reduce the number of children with persistent OME after three to six months of follow‐up. This benefit was not seen after longer follow‐up. However, many children in the 'control group' (who were planned to receive no treatment) either recovered spontaneously or received ventilation tubes during the follow‐up period. This makes it hard to assess the evidence after longer follow‐up.
We did not find any evidence about quality of life, so we do not know if ventilation tubes have any impact on this.
We were not able to combine the results of different studies to calculate how often an eardrum perforation may occur. However, the studies reported this side effect in between 0% and 12% of children who received ventilation tubes.
What are the limitations of the evidence?
We did not have enough information to identify whether certain groups of children would benefit from ventilation tubes (for example, children with Down syndrome or cleft palate, children with severe hearing loss or those in a certain age group). In clinical practice, different types of ventilation tubes are available, which last for different lengths of time ‐ we did not identify any studies that specifically looked at the use of long‐acting ventilation tubes, where the benefits and harms may be different. Further work needs to be done to identify which children with OME would benefit from treatment, and which children are likely to recover spontaneously.
How up‐to‐date is this evidence?
The evidence is up‐to‐date to January 2023.
Summary of findings
Summary of findings 1. Ventilation tubes compared to no treatment for OME in children.
| Ventilation tubes compared to no treatment for OME in children | ||||||
| Patient or population: children aged 6 months to 12 years with OME Setting: outpatient Intervention: ventilation tubes Comparison: no treatment | ||||||
| Outcomes | Relative effect (95% CI) | Anticipated absolute effects* (95% CI) | Certainty of the evidence (GRADE) | Comments | ||
| With no treatment | With ventilation tubes | Difference | ||||
|
Hearing ‐ return to normal hearing Randomised by ear: normal defined as < 15 dB Assumed CC = 0.5 Follow‐up: 12 months (medium‐term) № of participants: 72 (1 RCT) |
OR 1.13 (0.46 to 2.74) | 51.4% | 54.4% (32.7 to 74.3) | 3.0% more (18.7 fewer to 22.9 more) | ⊕⊝⊝⊝ Very low1 | The evidence is very uncertain about the effect of ventilation tubes on return to normal hearing at 12 months when compared with no treatment. |
| Disease‐specific quality of life | No evidence was identified for this outcome. | |||||
|
Presence/persistence of OME Randomised by child Adjusted for non‐independence of within‐individual measurements, assumed ICC = 0.5 Follow‐up: 6 months (medium‐term) № of participants: 54 (1 RCT) |
RR 0.30 (0.14 to 0.65) | 68.0% | 20.4% (9.5 to 44.2) | 47.6% fewer (58.5 fewer to 23.8 fewer) | ⊕⊕⊝⊝ Low2 | Ventilation tubes may result in a large reduction in the risk of persistence at 6 months when compared with no treatment. |
|
Adverse event: persistent perforation Randomised by ear, assumed CC = 0.5 Follow‐up: 12 months (medium‐term) № of participants: 144 (1 RCT) |
OR 0.85 (0.38 to 1.91) | 9.7% | 8.4% (3.9 to 17.1) | 1.3% fewer (5.8 fewer to 7.3 more) | ⊕⊝⊝⊝ Very low3 | The evidence is very uncertain about the effect of ventilation tubes on the likelihood of eardrum perforation or retraction at 12 months when compared with no treatment. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CC: correlation coefficient; CI: confidence interval; ICC: intracluster correlation coefficient; OME: otitis media with effusion; OR: odds ratio; RCT: randomised controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
1Downgraded by one level for a risk of performance bias. Downgraded by one level for inconsistency, as the I2 was substantial (73%). Downgraded by one level for indirectness, as the definition of 'normal hearing' was particularly strict (< 15 dB). Downgraded by two levels for imprecision as the optimal information size (OIS) was not reached (< 300 events) and the confidence intervals crossed two decision thresholds (OR 0.80 and 1.25).
2Downgraded by one level for serious risk of performance and detection bias. Downgraded by one level for serious imprecision as the OIS was not reached (< 300 events).
3Downgraded by one level for a risk of performance bias. Downgraded by two levels for imprecision as the optimal information size (OIS) was not reached (< 300 events) and the confidence intervals crossed two decision thresholds (OR 0.80 and 1.25).
Summary of findings 2. Early ventilation tubes compared to watchful waiting (treatment later if required) for OME in children.
| Early ventilation tubes compared to watchful waiting (treatment later if required) for OME in children | ||||||
| Patient or population: children aged 6 months to 12 years with OME Setting: outpatient Intervention: early ventilation tubes Comparison: watchful waiting (treatment later if required) | ||||||
| Outcomes | Relative effect (95% CI) | Anticipated absolute effects* (95% CI) | Certainty of the evidence (GRADE) | Comments | ||
| With watchful waiting | With early ventilation tubes | Difference | ||||
|
Hearing ‐ return to normal hearing Randomised by child Follow‐up: by age 9 to 11 years (long‐term) № of participants: 391 (1 RCT) |
RR 0.98 (0.94 to 1.03) | 94.9% | 93.0% (89.2 to 97.7) | 1.9% fewer (5.7 fewer to 2.8 more) | ⊕⊝⊝⊝ Very low1 | The evidence is very uncertain about the effect of early ventilation tubes on the return to normal hearing in the long term, when compared to watchful waiting (ventilation tubes later if required). |
| Disease‐specific quality of life | No evidence was identified for this outcome. | |||||
|
Presence/persistence of OME Randomised by child Follow‐up: from 18 months to over 6 years (long‐term) № of participants: 584 (3 RCTs) |
RR 1.21 (0.84 to 1.74) | 12.2% | 14.8% (10.3 to 21.3) | 2.6% more (2 fewer to 9.1 more) | ⊕⊝⊝⊝ Very low2 | The evidence is very uncertain about the effect of early ventilation tubes on persistence of OME in the long term, when compared to watchful waiting (ventilation tubes later if required). |
|
Adverse event: persistent perforation Follow‐up: range 2 years to 3.75 years № of ears analysed: 1010 (2 RCTs) |
One study (follow‐up 3.75 years) yielded a RR for early ventilation tubes versus watchful waiting of 3.65 (95% CI 0.41, 32.38). One study (follow‐up 2 years) reported that lasting perforations are rare and at worst 1.26% (8/635 ears that had ventilation tubes inserted). | ⊕⊝⊝⊝ Very low3 | The evidence is very uncertain about the effect of early ventilation tubes on the risk of persistent perforation when compared to watchful waiting (ventilation tubes later if required). | |||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; OME: otitis media with effusion; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
1Downgraded by one level for serious risk of bias (performance bias), one level for serious indirectness (some children did not have a consecutive period of three months with OME before enrolment) and one level for serious imprecision (the optimal information size of 300 events was not reached).
2Downgraded by two levels for very serious risk of bias (due to performance bias and attrition bias), one level for serious indirectness (some children did not have a consecutive period of three months with OME before enrolment) and one level for serious imprecision (as the confidence interval crossed one decision threshold (RR 1.25)).
3Downgraded by one level for serious risk of bias (performance bias), one level for serious indirectness (some children did not have a consecutive period of three months with OME before enrolment) and one level for serious imprecision as a narrative synthesis was conducted, and no estimate of effect can be provided.
Summary of findings 3. Ventilation tubes compared to non‐surgical treatment for OME in children.
| Ventilation tubes compared to non‐surgical treatment for OME in children | ||||||
| Patient or population: children aged 6 months to 12 years with OME Setting: outpatient Intervention: ventilation tubes Comparison: non‐surgical treatment | ||||||
| Outcomes | Relative effect (95% CI) | Anticipated absolute effects* (95% CI) | Certainty of the evidence (GRADE) | Comments | ||
| With non‐surgical treatment | With ventilation tubes | Difference | ||||
|
Hearing ‐ mean final hearing threshold (4 months ‐ medium‐term) № of participants: 125 (1 RCT) |
— | The mean threshold without ventilation tubes was 17.8 dB | 11.8 dB | MD 5.98 lower (9.21 lower to 2.75 lower) | ⊕⊝⊝⊝ Very low1 | The evidence is very uncertain about the effect of ventilation tubes on the hearing threshold at 4 months, when compared to non‐surgical (antibiotic) treatment. |
| Disease‐specific quality of life | No evidence was identified for this outcome. | |||||
| Presence/persistence of OME | No evidence was identified for this outcome. | |||||
|
Adverse event: persistent perforation (18 months ‐ long‐term) № of participants: 60 (1 RCT) |
One study reported that none of 60 children who received ventilation tubes had a persistent perforation. Length of follow‐up was not reported directly, but assumed to be at the final examination at 18 months. | ⊕⊕⊝⊝ Low2 | Ventilation tubes may result in a low risk of persistent perforation at 18 months, when compared to non‐surgical (antibiotic) treatment. | |||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; OME: otitis media with effusion; RCT: randomised controlled trial | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
1Downgraded by two levels for risk of bias, due to very serious risk of performance and detection bias. Downgraded by one level for indirectness, as some children received a different (inferior) ventilation tube. Downgraded by one level for serious imprecision, as the optimal information size was not reached (400 participants).
2Not downgraded for risk of bias, as this outcome was felt to be sufficiently objective that it would not be impacted by performance or detection bias. Downgraded by one level for indirectness, as some children received a different (inferior) ventilation tube. Downgraded by one level for serious imprecision, as this was a narrative synthesis only.
Summary of findings 4. Ventilation tubes compared to myringotomy for OME in children.
| Ventilation tubes compared to myringotomy for OME in children | ||||||
| Patient or population: children aged 6 months to 12 years with OME Setting: outpatient Intervention: ventilation tubes Comparison: myringotomy | ||||||
| Outcomes | Relative effect (95% CI) | Anticipated absolute effects* (95% CI) | Certainty of the evidence (GRADE) | Comments | ||
| With myringotomy | With ventilation tubes | Difference | ||||
|
Hearing ‐ return to normal *Ventilation tubes versus laser myringotomy (6 to 12 months ‐ medium‐term) Adjusted for non‐independence of within‐individual measurements Assumed ICC of 0.5 № of participants: 132 (2 RCTs) |
RR 1.22 (0.59 to 2.53) | 63.6% | 77.6% (37.5 to 100) | 14.0% more (26.1 fewer to 97.4 more) | ⊕⊝⊝⊝ Very low1 | The evidence is very uncertain about the effect of ventilation tubes on the likelihood of a return to normal hearing at 6 to 12 months, when compared to laser myringotomy. |
| Disease‐specific quality of life | No evidence was identified for this outcome. | |||||
|
Presence/persistence of OME *Ventilation tubes versus laser myringotomy, randomised by ear (6 months ‐ medium‐term) Assumed CC of 0.5 № of participants: 272 (1 RCT) |
OR 0.27 (0.19 to 0.38) | 61% | 29.7% (22.9 to 37.3) |
31.3% fewer (38.1 fewer to 23.7 fewer) |
⊕⊝⊝⊝ Very low2 | The evidence is very uncertain about the effect of ventilation tubes on persistent OME at 6 months, when compared with laser myringotomy. |
|
Adverse event: persistent perforation Range of follow‐up: 3 months to 2 years № of participants: 581 (6 RCTs) |
The number of persistent perforations following insertion of ventilation tubes ranged from 1 ear to 4 ears, and from 1 to 3 children (D'Eredita 2006; Gates 1989; Sujatha 2015; To 1984). One study yielded a RR for persistent perforation (ventilation tubes versus laser myringotomy) of 1.00 (95% CI 0.06 to 15.56) at 6 months (Yousaf 2016). | ⊕⊕⊕⊝ Moderate3 | Ventilation tubes likely increase the risk of persistent perforation. When compared with laser myringotomy, there is likely to be little to no difference in risk at 6 months. | |||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CC: correlation coefficient; CI: confidence interval; ICC: intraclass correlation coefficient; OME: otitis media with effusion; OR: odds ratio; RCT: randomised controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
1Downgraded by two levels for risk of bias (performance and reporting bias). Downgraded by one level for serious inconsistency, as the I2 was 95%, with minimal overlap of confidence intervals. Downgraded by two levels for very serious imprecision as the optimal information size (OIS) was not reached (< 300 events) and two decision thresholds were crossed by the CI (RR 0.80 and 1.25).
2Downgraded by two levels for very serious risk of bias (performance, detection, reporting and attrition bias). Downgraded by one level for serious imprecision as the optimal information size (OIS) was not reached (< 300 events).
3Not downgraded for risk of bias, as this outcome was felt to be sufficiently objective that it would not be impacted by performance or detection bias. Downgraded by one level for serious imprecision, as this was a narrative synthesis only.
Background
Description of the condition
Otitis media with effusion (OME) is a common condition in early childhood. The condition, also known as 'glue ear' and serous otitis media, is defined as "the presence of fluid in the middle ear without signs or symptoms of acute infection" (Rosenfeld 2016).
A key clinical feature of OME is hearing loss, due to decreased mobility of the tympanic membrane and consequent loss of sound conduction (Rosenfeld 2016). When hearing loss persists, this may affect speech and language development, and lead to behavioural problems in some children (Bennett 1999; Bennett 2001). Other symptoms that may be attributable to OME include balance (vestibular) problems and ear discomfort (Rosenfeld 2016). When symptoms persist, they may lead to poor school performance and affect a child's daily activities, social interactions and emotions, possibly leading to a poorer quality of life for the child (Rosenfeld 2000).
It is thought that up to 80% of children have had OME by the age of four years, but a decline in prevalence is observed for children beyond six years of age (Williamson 2011). Most episodes of OME in children resolve spontaneously within three months, however approximately 35% of children will have more than one episode of OME and, furthermore, 5% to 10% of episodes will last for more than a year (Rosenfeld 2016). Children with OME following an episode of untreated acute otitis media (AOM) have a 59% rate of resolution by one month, rising to 74% by three months, while children with newly diagnosed OME of unknown duration demonstrate a resolution rate of 28% by three months and up to 42% by six months (Rosenfeld 2003). The condition is more prevalent in children with Down syndrome or cleft palate (Flynn 2009; Maris 2014). Atopy has been considered a potential risk factor for OME in children (Kreiner‐Møller 2012; Marseglia 2008; Zernotti 2017).
Diagnosis of OME is typically by clinical examination including (pneumatic) otoscopy and/or tympanometry in primary care. Following diagnosis, there will often be a period of active observation, for at least three months. During the observation period, the care provider may offer a non‐surgical intervention such as hearing aids or autoinflation. The UK National Institute for Health and Care Excellence (NICE) and the American Academy of Otolaryngology ‐ Head and Neck Surgery (AAO‐HNS) do not currently recommend the use of antibiotics, antihistamines, decongestants or corticosteroids for OME as there is insufficient evidence to suggest they are effective treatments (NICE 2008; Rosenfeld 2016). If OME has not resolved within the three‐month observation period, the child may be referred for further management/active intervention. This may include hearing aid provision or review by an ENT surgeon for consideration for myringotomy, ventilation tubes insertion and/or adenoidectomy. The choice of active intervention varies considerably. Earlier active intervention may be considered for children at increased risk of developmental difficulties (see Rosenfeld 2016 for a list of 'at‐risk' factors).
This Cochrane Review will focus on insertion of ventilation tubes as treatment for OME in children. This review forms part of a suite of five reviews of OME treatment that will address those interventions identified in a prioritisation exercise as being most important and in need of up‐to‐date Cochrane Reviews: namely, adenoidectomy, autoinflation, topical and oral steroids, and antibiotics (Cochrane ENT 2020).
Description of the intervention
NICE describes myringotomy and insertion of ventilation tubes (with or without adenoidectomy) as the most common surgical option for OME (NICE CKS 2021). Ventilation tubes (grommets) are tiny plastic tubes inserted in the tympanic membrane (under general anaesthetic in children). The procedure, undertaken by an ENT surgeon, involves making a small incision in the tympanic membrane (myringotomy), aspirating middle ear fluid as necessary and inserting the tube. The ventilation tube promotes middle ear ventilation and provides a passage for drainage of middle ear fluid. Generally, ventilation tubes eventually extrude into the external ear canal and the tympanic membrane closes (Venekamp 2018). In certain cases, early extrusion of the ventilation tubes occurs, and they may need replacing. While aspiration is common practice, there is little evidence to suggest that it is of benefit prior to ventilation tube insertion (Laina 2006).
Myringotomy can be performed alone without insertion of ventilation tubes, however when undertaken using 'cold steel' incision with a blade it results in rapid healing without maintenance of benefit. When undertaken using a laser to create a circular perforation in the tympanic membrane, healing and closure of the myringotomy perforation may take longer with more persisting benefits akin to a ventilation tube.
The role of adenoidectomy in addition to ventilation tubes has been assessed in a separate Cochrane Review (van den Aardweg 2010); this evidence will be updated as part of the new suite of five Cochrane Reviews of OME treatments and thus will not be assessed in this review.
How the intervention might work
For children with OME who suffer from hearing loss, the insertion of ventilation tubes helps the middle ear fluid to drain, aerates the middle ear and balances the pressures on each side of the tympanic membrane (Vanneste 2019), allowing for normal mobility and conduction of sound and thus improving the child's ability to hear. The improvement in hearing is immediate in the majority of cases, but occasionally complete resolution takes days to weeks. Ventilation tubes usually remain working within the tympanic membrane for 12 months on average (Rosenfeld 2016), and usually spontaneously extrude with healing of the tympanic membrane. Following this, the child may remain free from OME, however in a proportion of children OME can return and persist, requiring repeat insertion. Factors that can limit the effectiveness of ventilation tubes include blockage of the tube (with blood), difficulty or inability to place the tubes due to narrow ear canals (Down syndrome and cleft palate) and early extrusion.
A common problem with ventilation tubes is ear discharge (otorrhoea) (Schilder 2016), and in around 2% of cases when the ventilation tube is extruded the tympanic membrane does not heal and a perforation persists. There is some evidence that insertion of ventilation tubes may also result in long‐term damage to the tympanic membrane, such as tympanosclerosis or atrophy, and hearing loss (de Beer 2004; de Beer 2005).
Why it is important to do this review
A Cochrane Review assessing ventilation tubes for hearing loss associated with OME was published in 2010 (Browning 2010), updating an earlier review published in 2005. The 2010 review included 10 studies, three of which were randomised by ear (unilateral ventilation tube) and seven were randomised by child (bilateral ventilation tube or no ventilation tube). The authors concluded that the effect of ventilation tubes on hearing was small and diminished after six to nine months (by which time the hearing of children without ventilation tubes had improved due to natural resolution). The authors found few data on other outcomes, and identified a lack of trials conducted in children with established speech, language, learning or developmental problems. Since publication of the Cochrane Review in 2010, there have been two Health Technology Assessment (HTA) reports that include ventilation tubes (Berkman 2013; Steele 2017), and four other systematic reviews (Berkman 2013; Cheong 2012; Wallace 2014; Williamson 2011). Scoping searches for randomised controlled trials (RCTs) of ventilation tubes, which were last undertaken in January 2020, identified 12 abstracts of interest published since the last Cochrane Review. A prioritisation exercise undertaken in 2020 identified a review of ventilation tubes as a top priority (Cochrane ENT 2020). It is therefore timely to update the evidence.
Objectives
To assess the effects (benefits and harms) of ventilation tubes (grommets) for OME in children.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) and quasi‐randomised trials (where studies were designed as RCTs, but the sequence generation for allocation of treatment used methods such as alternative allocation, birth dates and alphabetical order). We included studies that randomised participants by ear, by participant or by cluster. We did not identify any cluster‐randomised or cross‐over trials for inclusion in this review.
Types of participants
The population of interest was children aged 6 months to 12 years with unilateral or bilateral otitis media with effusion, alternatively termed chronic otitis media with effusion (COME), glue ear, chronic or persistent middle ear effusion or serous otitis media. If a study included children aged younger than 6 months and/or older than 12 years, we only included the study if the majority of children fit our inclusion criteria, or if the trialists presented outcome data by age group. We included all children regardless of any comorbidity such as Down syndrome or cleft palate.
Clinical diagnosis of OME was confirmed by oto(micro)scopy or tympanometry or both. We included studies where children had OME for at least three months. We included studies of children who had previously had ventilation tubes inserted.
In some studies, the population of interest was children with acute otitis media (AOM) or recurrent acute otitis media (RAOM). Either of these populations may also have intermittent or chronic OME. However, we regarded children who present with AOM or RAOM as different populations to those who present with chronic OME (the focus of this review), and did not assume that interventions designed to treat one population would have the same efficacy in the others. We therefore excluded studies in which the population of interest was children with AOM or RAOM.
Types of interventions
Intervention
Insertion of ventilation tube performed either unilaterally or bilaterally. We did not assess different types of ventilation tubes or surgical approaches to insertion.
Comparators
In our protocol, we presented six comparisons of interest. However, after examining the comparisons of interest it was agreed that the comparisons with 'no treatment' and 'watchful waiting' are not the same and should not be treated as one comparison. The comparison with 'watchful waiting' requires an active process of monitoring the child's condition and treating them with ventilation tubes (such as bilateral) if deemed necessary at a later date.
As some studies included children with both bilateral and unilateral OME, we also decided to merge those comparisons where trials might include these participants. Hence, we were interested in the following five comparisons.
Ventilation tubes (bilateral or unilateral) versus no treatment
Early ventilation tubes versus watchful waiting (treatment later if required)
Ventilation tubes versus hearing aids
Ventilation tubes versus non‐surgical treatment
Ventilation tubes versus myringotomy alone
If study participants received other treatments (for example, adenoidectomy, intranasal steroids, oral steroids, antibiotics, mucolytics or decongestants), we included these studies if both arms received identical treatment.
Types of outcome measures
We analysed the following outcomes in the review, but we did not use them as a basis for including or excluding studies. We assessed all outcomes in the short term (≤ 3 months), medium term (> 3 months to ≤ 1 year) and long term (> 1 year). We assessed postoperative adverse events in the very short term (< 6 weeks).
Primary outcomes
-
Hearing, measured as:
the proportion of children whose hearing has returned to normal (defined by the trialists);
mean final hearing threshold (determined for the child or ear, depending on the unit of analysis);
change in hearing threshold from baseline (determined for the child or ear, depending on the unit of analysis).
We anticipated that trial data for these outcomes may be derived from a variety of assessment methods and subject to a variety of definitions. To avoid loss of important evidence, we extracted all such data for analysis. However, we gave consideration to the appropriateness of pooling different types of data in meta‐analysis. Our selection of primary outcomes was based principally upon clinical importance, but also permits applicability across a variety of age‐appropriate assessment methods, and considers the types of outcome data that are most likely to be available. Accordingly, we regarded the proportion of participants whose hearing has returned to normal as the most important measure of hearing impact. We considered medium‐ and long‐term outcome data as the most clinically important.
-
Disease‐specific quality of life measured using a validated instrument, for example:
OM8‐30 (Haggard 2003);
Otitis Media‐6 (Rosenfeld 1997).
Adverse event ‐ persistent perforation.
Secondary outcomes
Presence/persistence of OME.
-
Adverse events ‐ measured by the number of participants affected.
-
Tympanic membrane changes, such as:
atrophy;
atelectasis or retraction;
myringosclerosis;
tympanosclerosis.
-
Tube‐related, such as:
blockage;
extrusion;
granulation tissue formation;
otorrhoea/perforation;
displacement of the ventilation tube into the middle ear space.
-
Patient‐related, such as:
vomiting;
diarrhoea;
dry throat;
nasal stinging;
cough;
long‐term hearing loss;
postsurgical haemorrhage;
pain.
-
-
Receptive language skills, measured using a validated scale, for example:
Peabody Picture Vocabulary Test ‐ Revised (Dunn 2007);
relevant domains of the Reynell Developmental Language Scales (Reynell 1985);
relevant domains of the Preschool Language Scale (PLS) (Zimmermann 1992);
relevant domains of the Sequenced Inventory of Communication (SCID) (Hedrick 1984).
-
Speech development, or expressive language skills, measured using a validated scale, for example:
Schlichting test (Schlichting 2010);
Lexi list (Schlichting 2007);
relevant domains of the Reynell Developmental Language Scales (Reynell 1985);
relevant domains of the PLS (Zimmermann 1992);
relevant domains of the SCID (Hedrick 1984).
-
Cognitive development, measured using a validated scale, for example:
Griffiths Mental Development Scales (Griffiths 1996);
McCarthy General Cognitive Index (McCarthy 1972);
Bayley Scales of Infant and Toddler Development (Bayley 2006).
-
Psychosocial outcomes, measured using a validated scale, for example:
the Social Skills Scale of the Social Skills Rating System (Gresham 1990);
Child Behavior Checklist (Achenbach 2011);
Strengths and Difficulties Questionnaire (Goodman 1997);
Pediatric Symptom Checklist (Jellinek 1988).
Listening skills, for example listening to stories and instructions effectively. Given that there are few validated scales to assess listening skills in children with OME, we included any methods used by trialists.
-
Generic health‐related quality of life assessed using a validated instrument, for example:
EQ‐5D (Rabin 2001);
TNO AZL Children's QoL (TACQOL) (Verrips 1998);
TNO AZL Pre‐school children QoL (TAPQOL) (Fekkes 2000);
TNO AZL Infant Quality of Life (TAIQOL) (TNO 1997);
Infant Toddler Quality of Life Questionnaire (ITQOL) (Landgraf 1994);
Child Health Questionnaire (CHQ) (Landgraf 1996).
-
Parental stress, measured using a validated scale, for example:
Parenting Stress Index (Abidin 1995).
-
Vestibular function:
balance;
co‐ordination.
Number of doctor‐diagnosed acute otitis media episodes within a specified time frame.
These outcomes were identified as the most important in two studies that aimed to develop a core outcome set for children with OME (Bruce 2015; Liu 2020). As this review forms part of a suite of reviews of interventions for OME, not all outcomes will be relevant for all reviews.
Search methods for identification of studies
The Cochrane ENT Information Specialist conducted systematic searches for randomised controlled trials and controlled clinical trials. There were no language, publication year or publication status restrictions. We contacted original authors for clarification and further data if trial reports were unclear and arranged translations of papers where necessary. The date of the search was 20 January 2023.
Electronic searches
The Information Specialist searched:
the Cochrane ENT Register (searched via the Cochrane Register of Studies to 20 January 2023);
the Cochrane Central Register of Controlled Trials (CENTRAL 2023, Issue 1), searched via the Cochrane Register of Studies to 20 January 2023;
Ovid MEDLINE(R) Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R) (1946 to 20 January 2023);
Ovid EMBASE (1974 to 20 January 2023);
Web of Science, Web of Science (1945 to 20 January 2023);
-
ClinicalTrials.gov, www.clinicaltrials.gov:
searched via the Cochrane Register of Studies to 20 January 2023;
searched via www.clinicaltrials.gov to 20 January 2023;
-
World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP), https://apps.who.int/trialsearch/:
searched via the Cochrane Register of Studies to 20 January 2023;
searched via https://apps.who.int/trialsearch/ 20 January 2023.
The Information Specialist modelled subject strategies for databases on the search strategy designed for CENTRAL. The search strategies were designed to identify all relevant studies for a suite of reviews on various interventions for otitis media with effusion. Where appropriate, they were combined with subject strategy adaptations of the highly sensitive search strategy designed by Cochrane for identifying randomised controlled trials and controlled clinical trials (as described in the Technical Supplement to Chapter 4 of the Cochrane Handbook for Systematic Reviews of Interventions version 6.1) (Lefebvre 2020). Search strategies for major databases including CENTRAL are provided in Appendix 1.
Searching other resources
We scanned the reference lists of identified publications for additional trials and contacted trial authors where necessary. The Information Specialist also ran non‐systematic searches of Google Scholar to retrieve grey literature and other sources of potential trials.
We did not perform a separate search for adverse effects. We considered adverse effects described in included studies only.
Data collection and analysis
Selection of studies
The Cochrane ENT Information Specialist used Cochrane's Screen4Me workflow to help assess the search results. Screen4Me comprises three components:
Known assessments – a service that matches records in the search results to records that have already been screened in Cochrane Crowd and been labelled as 'a RCT' or as 'not a RCT'.
The machine learning classifier (RCT model) (Wallace 2017), available in the Cochrane Register of Studies (CRS‐Web), which assigns a probability of being a true RCT (from 0 to 100) to each citation. We assumed citations assigned a probability score below the cut‐point at a recall of 99% to be non‐RCTs. For those that scored on or above the cut‐point, we either manually dual screened these results or sent them to Cochrane Crowd for screening.
Cochrane Crowd is Cochrane's citizen science platform where the Crowd help to identify and describe health evidence. For more information about Screen4Me and the evaluations that have been done, please go to the Screen4Me website on the Cochrane Information Specialist's portal and see Marshall 2018, McDonald 2017, Noel‐Storr 2018 and Thomas 2017.
Two review authors (KG, CM) independently screened the remaining titles and abstracts to identify potentially relevant studies. At least two review authors (of KG, SM, CM, KW) then independently evaluated the full text of each potentially relevant study to determine whether it met the inclusion/exclusion criteria for this review. Any differences were resolved by discussion and consensus, with the involvement of a third author (of KG, CM, KW, SM) where necessary.
Screening eligible studies for trustworthiness
Two review authors (KG, KW) appraised all studies meeting our inclusion criteria for trustworthiness using a screening tool developed by Cochrane Pregnancy and Childbirth. This tool includes specified criteria to identify studies that are considered sufficiently trustworthy to be included in the review (see Appendix 2 and Figure 1). For any studies assessed as being potentially 'high risk', we attempted to contact the study authors to obtain further information or address any concerns. We had planned to exclude these studies from the review if we were unable to contact the authors, or there was persisting uncertainty about the study.
1.
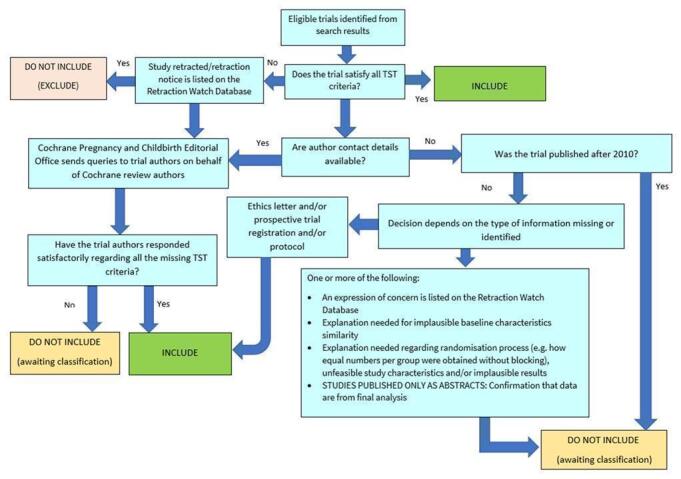
The Cochrane Pregnancy and Childbirth Trustworthiness Screening Tool
When using the trustworthiness tool, there were 11 studies where we had no concerns: Bernard 1991; Gates 1989; Koopman 2004; Maw 1983; Maw 1999; Paradise 2007; Rach 1991; Rovers 2000; Ruckley 1988; TARGET 2000; To 1984.
All the remaining studies had at least some concerns, although this was often due to a paucity of information, rather than a specific concern over trustworthiness:
We were unable to identify prospective trial registration for six studies (Elkholy 2021; Popova 2010; Sujatha 2015; Tao 2020; Velepic 2011; Yousaf 2016).
Four studies reported full follow‐up, without explanation to indicate how this was achieved (Elkholy 2021; Sujatha 2015; Velepic 2011; Yousaf 2016).
Three studies randomised equal numbers of participants to each group, without a description of blocked randomisation (D'Eredita 2006; Elkholy 2021; Sujatha 2015), and one did not provide information on the number randomised to each group (Dempster 1993).
We were unsure whether the number of studies with concerns reflected a genuine problem with the data from these studies, or whether the assessment tool was perhaps too sensitive. We note that this tool ‐ and others used for the same purpose ‐ has not yet been validated.
Consequently, we decided to include all the studies in the main analyses of this review, but we did investigate the effect of excluding studies with concerns over trustworthiness on the overall results (see Sensitivity analysis).
Data extraction and management
Two review authors (RC, KG, CM, AP, KW) independently extracted outcome data from each study using a standardised data collection form. Where a study had more than one publication, we retrieved all publications to ensure complete extraction of data. Any discrepancies in the data extracted by the two authors were checked against the original reports, and differences were resolved through discussion and consensus, with recourse to a third author (CM, KG, KW, SM) where necessary. If required, we contacted the study authors for clarification of any unclear or missing data. We included key characteristics of the studies, such as the study design, whether randomised by individual or by body part (see Unit of analysis issues), setting, sample size, population and the methods for defining or collecting outcome data in the studies.
We extracted data on study findings according to treatment assignment, irrespective of whether study participants complied with treatment or received the treatment to which they were randomised.
In addition to extracting pre‐specified information about study characteristics and aspects of methodology relevant to risk of bias, we extracted the following summary statistics for each trial and outcome:
For continuous data: the mean values, standard deviation and number of patients for each treatment group at the different time points for outcome measurement. Where endpoint data were not available, we extracted the values for change‐from‐baseline data instead. If values for the individual treatment groups were not reported, where possible we extracted summary statistics (e.g. mean difference) from the studies.
For binary data: we extracted information on the number of participants experiencing an event, and the number of participants assessed at that time point. If values for the individual treatment groups were not reported, where possible we extracted summary statistics (e.g. risk ratio) from the studies.
For ordinal scale data: if the data appeared to be normally distributed, or if the analysis performed by the investigators indicated that parametric tests were appropriate, then we treated the outcome measure as continuous data. Alternatively, if data were available, we converted these to binary data for analysis.
We pre‐specified time points of interest for the outcomes in this review. Where studies reported data at multiple time points, we took the longest available follow‐up point within each of the specific time frames. For example, if a study reported an outcome at 4 months, 8 months and 12 months of follow‐up then the 12‐month data was included for the time point > 3 months to ≤ 1 year. For adverse events, some studies reported frequency data for events and it may not be possible to determine whether these events occurred in one participant on one occasion or more than one occasion. In such circumstances we reported the data narratively.
Assessment of risk of bias in included studies
Two authors (RC, KG, CM, AP, KW) undertook risk of bias assessment of the included studies independently, with the following taken into consideration, as guided by Higgins 2011:
sequence generation;
allocation concealment;
blinding of participants and personnel;
blinding of outcome assessment;
incomplete outcome data;
selective outcome reporting;
other sources of bias.
We used the Cochrane risk of bias tool in RevMan 5.4 (RevMan 2020), which involves describing each of these domains as reported in the study and then assigning a judgement about the adequacy of each entry: 'low', 'high' or 'unclear' risk of bias.
Measures of treatment effect
We summarised dichotomous data, such as presence of OME, as risk ratios (RR) and 95% confidence intervals (CI) and we summarised continuous data as mean difference (MD) and 95% CI. For the outcomes presented in the summary of findings tables, we have provided both relative and absolute measures of effect. If individual patient data (IPD) were available we planned to use these in our analyses, however this was not possible.
Unit of analysis issues
Studies included in this review randomised either by participant or by ear. We identified whether randomisation was conducted at the level of the participant or the ear, and ‐ for those studies that randomised by participant ‐ we assess whether the study included one or two ears from each participant. Given that there are likely to be some carry‐over effects of disease and treatment from one ear to the other in a child, we analysed the outcomes separately for randomisation by ear or by child. For studies that randomised by ear, we only assessed the outcomes of hearing, adverse events, presence of OME and number of AOM episodes. The remaining outcomes are only relevant for studies randomised by child, where we can consider the more global effect of hearing difficulty.
If we had identified cluster‐randomised trials, we would have assumed that the data from participants was no longer independent and adjusted our analyses accordingly, using the design effect approach as detailed in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2021). If we had identified cross‐over RCTs then we would have included data from the first phase of the trial only. However, this was not necessary for the review. We did identify some multi‐arm trials in this review. Where necessary, we pooled data from separate arms to provide the comparisons of interest for this review.
Dealing with missing data
We attempted to contact study authors by email where data on an outcome of interest to the review were not reported but the methods described in the paper suggested that the outcome was assessed. We did the same if not all data required for meta‐analysis were reported.
Assessment of heterogeneity
We assessed clinical heterogeneity by examining the included studies for potential differences in the types of participants recruited, interventions or controls used, and the outcomes measured. We assessed statistical heterogeneity by considering both the I² statistic (which calculates the percentage of variability that is due to heterogeneity rather than chance, with values over 50% suggesting substantial heterogeneity) and the P value from the Chi² test (Higgins 2021).
Assessment of reporting biases
We assessed reporting bias as within‐study outcome reporting bias and between‐study publication bias.
Outcome reporting bias (within‐study reporting bias)
We assessed within‐study reporting bias by comparing the outcomes reported in the published report against the study protocol or trial registry, when this could be obtained. If the protocol or trial registry entry was not available, we compared the outcomes reported to those listed in the methods section of the published report. If results were mentioned but not reported in a way that allowed analysis (e.g. the report only mentions whether the results were statistically significant or not), we sought further information from the study authors. If no further information could be found, we noted this as being a 'high' risk of bias. If there was insufficient information to judge the risk of bias we noted this as an 'unclear' risk of bias (Higgins 2011).
Publication bias (between‐study reporting bias)
We planned to produce a funnel plot to explore possible publication biases, if we were able to pool 10 or more studies in a single analysis. However, this was not possible, as too few studies were included in the meta‐analyses.
Data synthesis
Where two or more studies reported the same outcome, we performed a meta‐analysis using Review Manager (RevMan 2020). We report pooled effect measures for dichotomous outcomes as a risk ratio (RR) using the Mantel‐Haenszel methods. For continuous outcomes measured using the same scales we report the mean difference (MD). We used a random‐effects model.
Where it was not possible to pool the findings from studies in a meta‐analysis, we have presented the results of each study and provide a narrative synthesis of findings.
Subgroup analysis and investigation of heterogeneity
We planned to analyse the following subgroups if sufficient data were available in study reports:
children with mild hearing loss versus moderate or severe;
children with allergy versus those without (using the trialists' own definition);
children aged up to four years versus children aged four years and over;
children with previous ventilation tubes versus those without ventilation tubes;
children with cleft palate versus children without;
children with Down syndrome versus children without;
conventional cold steel versus other methods of myringotomy.
However, we did not find any data suitable for conducting these subgroup analyses. No studies provided subgroup data for children with different features (for example, for those with mild hearing loss, compared to those with moderate or worse hearing loss). Many of the studies did not provide sufficient background information (for example, on hearing level) for us to conduct subgroup analysis at the level of the individual study. Although we identified some studies that specifically recruited children aged up to four years or over four years, we had too few studies included in any meta‐analysis to provide accurate estimates of subgroup effects.
Sensitivity analysis
We carried out sensitivity analyses to assess whether our findings were robust to decisions made regarding the analyses and inclusion of studies. We performed sensitivity analyses to assess the following:
Impact of model chosen: we compared the results using a random‐effects versus a fixed‐effect model.
Inclusion of studies at high risk of bias: we compared the results including all studies versus excluding studies at overall high risk of bias, that is four or more of the seven domains of bias are rated as high risk (see Assessment of risk of bias in included studies). This applied to six studies (Elkholy 2021; Gates 1989; Koopman 2004; Popova 2010; Velepic 2011; Yousaf 2016).
Exclusion of studies with concerns over trustworthiness, as assessed by the Trustworthiness Tool (Figure 1). This applied to eight studies (D'Eredita 2006; Dempster 1993; Elkholy 2021; Popova 2010; Sujatha 2015; Tao 2020; Velepic 2011; Yousaf 2016).
Summary of findings and assessment of the certainty of the evidence
Two independent authors (KG, CM) used the GRADE approach to rate the overall certainty of evidence using GRADEpro GDT. The certainty of evidence reflects the extent to which we are confident that an estimate of effect is correct, and we have applied this in the interpretation of results. There are four possible ratings: high, moderate, low and very low. A rating of high certainty of evidence implies that we are confident in our estimate of effect and that further research is very unlikely to change our confidence in the estimate of effect. A rating of very low certainty implies that any estimate of effect obtained is very uncertain.
The GRADE approach rates evidence from RCTs that do not have serious limitations as high certainty. However, several factors can lead to the downgrading of the evidence to moderate, low or very low. The degree of downgrading is determined by the seriousness of these factors:
study limitations (risk of bias);
inconsistency;
indirectness of evidence;
imprecision; and
publication bias.
When assessing imprecision, we used a minimally important difference of a risk ratio (or odds ratio) of 0.8 or 1.25 for dichotomous outcomes. For most continuous data, we considered a minimally important difference to be half of the standard deviation for the control/comparator group. The exception to this was hearing thresholds, where we used a difference of 10 dB HL as the minimally important difference.
We constructed summary of findings tables for the comparisons below according to the recommendations described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2021):
ventilation tubes (bilateral or unilateral) versus no treatment;
early ventilation tubes versus watchful waiting (treatment later if required);
ventilation tubes versus hearing aids;
ventilation tubes versus non‐surgical treatment;
ventilation tubes versus myringotomy alone.
We included the following four outcomes in the summary of findings tables:
hearing;
disease‐specific quality of life;
presence/persistence of OME;
adverse event ‐ persistent perforation.
Results
Description of studies
Results of the search
The searches (September 2021 and January 2023) retrieved a total of 7441 records. This reduced to 4157 after the removal of duplicates. The Cochrane ENT Information Specialist sent all 4157 records to the Screen4Me workflow. The Screen4Me workflow identified 84 records as having previously been assessed: 50 had been rejected as not RCTs and 34 had been assessed as possible RCTs. The remaining 4073 references were sent to the RCT classifier, which rejected an additional 1514 records as not RCTs (with 99% sensitivity) and 116 records as possible RCTs. The Cochrane Crowd assessed 2443 of the remaining references, rejecting 1313 as not RCTs and identifying 1130 as possible RCTs. Following this process, the Screen4Me workflow rejected 2877 records and identified 1280 possible RCTs for title and abstract screening (see Table 5).
1. RCTs identified through Cochrane Crowd and the RCT Classifier.
| Possible RCTs | Rejected | |
| Known assessments | 34 | 50 |
| RCT classifier | 116 | 1514 |
| Cochrane Crowd | 1130 | 1313 |
| Total (n = 4157) | 1280 | 2877 |
RCT: randomised controlled trial
Of the 1280 possible RCTs identified via the Screen4Me workflow, we excluded 76 additional duplicates. We screened the titles and abstracts of the remaining 1204 records. We discarded 886 records and retrieved full‐text reports for 318 records. We subsequently discarded an additional 192 irrelevant records and removed an additional six duplicates.
We excluded 50 records (linked to 47 studies) with reasons recorded in the review (see Excluded studies).
We included 19 studies (63 records) where results were available (Bernard 1991; D'Eredita 2006; Dempster 1993; Elkholy 2021; Gates 1989; Koopman 2004; Maw 1983; Maw 1999; Paradise 2007; Popova 2010; Rach 1991; Rovers 2000; Ruckley 1988; Sujatha 2015; Tao 2020; TARGET 2000; To 1984; Velepic 2011; Yousaf 2016).
We identified three ongoing studies. See Characteristics of ongoing studies for further details.
We identified four studies that are awaiting assessment because we did not have enough information to determine eligibility (Diacova 2016; Marshak 1980; Maw 1986; Tawfik 2002). See Characteristics of studies awaiting classification.
A flow chart of study retrieval and selection is provided in Figure 2.
2.

Included studies
A full description of each study is available in Characteristics of included studies, and a summary across all studies can be seen in Table 6.
2. Features of included studies.
| Study ID | Participants | Setting | Intervention | Comparator | Concomitant treatment | Follow‐up (main outcomes reported at this time) | Notes |
| Bernard 1991 | Children aged 2.5 to 7 years with OME and unsuccessful treatment with 2 courses of antibiotics (n = 139) | Single centre, USA | Bilateral myringotomy and insertion of ventilation tubes | Antibiotics (sulfisoxazole, 75 mg/kg divided into 2 daily doses for 6 months) | None reported | 18 months | — |
| D'Eredita 2006 | Children aged 2 to 6 with OME (n = 30) | Single centre, Italy | Cold myringotomy and ventilation tube insertion (unclear if bilateral or unilateral) | Laser myringotomy | Ofloxacin solution 3 times daily for 5 days | 12 months | — |
| Dempster 1993 | Children aged 3.5 to 12 years with bilateral OME (n = 78) | Single centre, UK | Unilateral ventilation tube | No ventilation tube | Half of the children in this study also underwent adenoidectomy | 11 months | Children received a ventilation tube in one ear, and no treatment in the other |
| Elkholy 2021 | Children aged 5 to 15 years with OME (n = 40) | Single centre, Egypt | Ventilation tube insertion (unclear if bilateral or unilateral) | No treatment | Children also underwent adenoidectomy | 2 weeks | Additional follow‐up to 12 months, but no useable data were reported after 2 weeks |
| Gates 1989 | Children aged 4 to 8 years with persistent OME for 60 days after a 10‐day course of erythromycin and sulfisoxazole, and a 30‐day course of pseudoephedrine hydrochloride (n = 578) | Multicentre, USA | Bilateral ventilation tubes or Adenoidectomy plus bilateral ventilation tubes |
Myringotomy or Adenoidectomy plus myringotomy |
— | 2 years | 4‐arm trial |
| Koopman 2004 | Children aged < 11 years with bilateral OME (n = 208) | Multicentre, Netherlands | Ventilation tube | Laser myringotomy | — | 6 months | Children received one intervention in each ear |
| Maw 1983 | Children aged 2 to 9 years with bilateral OME (n = 145) | Single centre, UK | Ventilation tubes | No treatment | Half of the children in this study also underwent adenoidectomy | 3 years | — |
| Maw 1999 | Children aged 9 months to 4.5 years with bilateral OME (n = 182) | Single centre, UK | Bilateral ventilation tubes | Watchful waiting | — | Up to 7 years | 21% of participants in the watchful waiting group received surgery before 9 months. By 18 months, only 85% of participants in this group had been listed for, or already received surgery. |
| Paradise 2007 | Children aged < 3 years with OME (n = 429) | Multicentre, USA | Ventilation tubes | Watchful waiting | — | Up to 11 years | 45% of those in the watchful waiting group had received ventilation tubes by the age of 9 to 11 years |
| Popova 2010 | Children (mean age 5 years) with bilateral OME (n = 90) | Single centre, Bulgaria | Ventilation tubes | Myringotomy | All participants received adenoidectomy | 12 months | — |
| Rach 1991 | Children aged 2 to 4 years with OME (n = 43) | Single centre, Netherlands | Ventilation tubes | No treatment | — | 4 years | After 6 months, some children in the 'no treatment group' underwent VT insertion, therefore data from later time points are included in the comparison of VT with watchful waiting |
| Rovers 2000 | Children (mean age 19.5 months) who failed 3 successive hearing tests, with bilateral OME (n = 187) | Multicentre, Netherlands | Ventilation tubes | Watchful waiting | — | 12 months | — |
| Ruckley 1988 | Children aged 4 to 9 years with bilateral OME (n = 40) | Single centre, UK | Ventilation tube | Thermal myringotomy | Adenoidectomy | 3 months | Children received one intervention in each ear |
| Sujatha 2015 | Children aged 3 to 10 years with OME (n = 50) | Single centre, India | Ventilation tube | Myringotomy | Adenoidectomy. Systemic antibiotics, analgesics, anti‐inflammatories and decongestant nasal drops for 7 days. | 12 months | — |
| Tao 2020 | Children aged 4 to 12 years with bilateral OME (n = 178) | Single centre, China | Ventilation tube | Myringotomy | Adenoidectomy | 12 months | — |
| TARGET 2000 | Children aged 3.25 to 6.75 with bilateral OME (n = 248) | Multicentre, UK | Bilateral ventilation tubes alone | Watchful waiting | — | 2 years | Additional study arm included in the companion review on adenoidectomy (MacKeith 2023) |
| To 1984 | Children aged < 14 years with bilateral OME (n = 54) | Single centre, UK | Ventilation tube | Myringotomy | Adenoidectomy | 1 to 5 years | Children received one intervention in each ear |
| Velepic 2011 | Children (mean age 5.5 years) with predominantly bilateral OME (n = 87) | Single centre, Croatia | Ventilation tube | Watchful waiting (ventilation tube after 3 months if required) | Adenoidectomy | 6 months | — |
| Yousaf 2016 | Children aged 4 to 12 years with OME and hearing level > 30 db HL (n = 82) | Single centre, Pakistan | Ventilation tube | Laser myringotomy | — | 6 months | — |
Study design
All the included studies were described as randomised controlled trials. Most were parallel‐group studies including two arms (Bernard 1991; D'Eredita 2006; Elkholy 2021; Maw 1999; Paradise 2007; Popova 2010; Rach 1991; Rovers 2000; Sujatha 2015; Tao 2020; Velepic 2011; Yousaf 2016). TARGET 2000 included a third arm, but these data were not relevant for this review (as they assessed adenoidectomy).
Three further studies were also two‐arm trials that recruited children with bilateral OME ‐ one ear of each child was assigned to the intervention, and the other ear was assigned to the comparator group (Koopman 2004; Ruckley 1988; To 1984).
Three studies with four arms were included. One compared ventilation tubes to myringotomy, and ventilation tubes plus adenoidectomy to adenoidectomy alone (Gates 1989). The two further studies randomised children with bilateral OME to adenoidectomy or no adenoidectomy, then assigned different interventions to each ear (Dempster 1993; Maw 1983). For the purposes of this review we have only made a comparison of those who received ventilation tubes to no ventilation tubes.
Location
Six studies were conducted in the UK (Dempster 1993; Maw 1983; Maw 1999; Ruckley 1988; TARGET 2000; To 1984), three in the USA (Bernard 1991; Gates 1989; Paradise 2007) and three in the Netherlands (Koopman 2004; Rach 1991; Rovers 2000). A single study was conducted in each of the following countries: Bulgaria (Popova 2010), China (Tao 2020), Croatia (Velepic 2011), Egypt (Elkholy 2021), India (Sujatha 2015), Italy (D'Eredita 2006) and Pakistan (Yousaf 2016).
Participants
Sample size
The size of the studies varied considerably, with the smallest study including only 30 participants (D'Eredita 2006). Nine studies recruited between 40 and 100 participants (Dempster 1993; Elkholy 2021; Maw 1983; Popova 2010; Rach 1991; Ruckley 1988; Sujatha 2015; To 1984; Velepic 2011; Yousaf 2016) and six studies included between 100 and 250 participants (Bernard 1991; Koopman 2004; Maw 1999; Rovers 2000; Tao 2020; TARGET 2000). Only two studies recruited more than 250 participants: Gates 1989 (578 participants) and Paradise 2007 (429 participants).
Age
Four studies recruited very young children:
Paradise 2007 included children aged less than three years.
Maw 1999 included children aged between nine months and four years.
Rach 1991 included children aged two to four years with bilateral OME.
Rovers 2000 included children who had failed a routine hearing screening test at the age of nine months, and subsequently failed follow‐up tests. The mean age of participants at recruitment was 19.5 months.
Most studies recruited slightly older children, typically aged between 3 and 12 years of age (Bernard 1991; D'Eredita 2006; Dempster 1993; Elkholy 2021; Gates 1989; Koopman 2004; Ruckley 1988; Sujatha 2015; Tao 2020; TARGET 2000; To 1984; Yousaf 2016). Three studies did not give age restrictions as part of their inclusion criteria, but the baseline characteristics of the participants indicated that the mean age was approximately five to six years (Maw 1983; Popova 2010; Velepic 2011).
Hearing loss
Many of the studies required participants to have confirmed hearing loss on entry to the trial. However, the requirements varied considerably.
One study recruited children who failed a hearing test ‐ with no response to sounds presented at 35 dB (Rovers 2000).
One study required a hearing level of more than 30 dB HL (Yousaf 2016).
Five studies included children with a hearing loss of at least 25 dB HL (Bernard 1991; Dempster 1993; Maw 1983; Maw 1999; Tao 2020).
Two studies recruited children with hearing loss of > 20 dB HL (Popova 2010; TARGET 2000).
One study stated that the air‐bone gap should be at least 25 dB (Sujatha 2015).
One study required parents to have noticed impaired hearing, but did not use a specific threshold for recruitment (Koopman 2004).
Eight studies did not explicitly state the level of hearing impairment that was necessary for enrolment in the study (D'Eredita 2006; Elkholy 2021; Gates 1989; Paradise 2007; Rach 1991; Ruckley 1988; To 1984; Velepic 2011).
Previous treatment
Most studies specifically excluded individuals who had previously received ventilation tubes and/or adenoidectomy (Bernard 1991; D'Eredita 2006; Dempster 1993; Elkholy 2021; Gates 1989; Tao 2020; TARGET 2000; To 1984; Velepic 2011). Some children enrolled in the study Koopman 2004 had previously undergone adenoidectomy, ventilation tube insertion or tonsillectomy.
A few studies specifically recruited children who had failed some form of medical therapy ‐ typically antibiotics, with or without decongestants (Bernard 1991; Elkholy 2021; Gates 1989; Paradise 2007; Sujatha 2015), whilst two studies recruited children early in their presentation with OME, although it was not clear whether they may have received some form of medical therapy at presentation (Ruckley 1988; TARGET 2000).
No information on previous treatment was provided by six studies (Maw 1983; Maw 1999; Popova 2010; Rach 1991; Rovers 2000; Yousaf 2016).
Other health issues
The majority of studies specifically excluded children with congenital risk factors for OME, including cleft palate and Down syndrome (Bernard 1991; D'Eredita 2006; Dempster 1993; Elkholy 2021; Gates 1989; Maw 1999; Popova 2010; Rach 1991; Rovers 2000; Sujatha 2015; Tao 2020; TARGET 2000; Velepic 2011).
Interventions and comparisons
Comparison 1: Ventilation tubes versus no treatment
We identified four studies for this comparison. Two studies compared outcomes within the same individual ‐ comparing insertion of a ventilation tube in one ear, to no surgery on the other ear (Dempster 1993; Maw 1983). One study compared outcomes for bilateral ventilation tube insertion (in both ears of the same individual) to no treatment (in other children) (Rach 1991). In the study Elkholy 2021, randomisation was also at the level of the individual child, but we were uncertain whether children received bilateral or unilateral ventilation tubes.
Children in Dempster 1993 were also randomised to receive adenoidectomy or no adenoidectomy. For this review, we have presented data separately (for those who did or did not receive adenoidectomy), but have also presented a pooled estimate of the overall effect of ventilation tube insertion. All children recruited to Elkholy 2021 also received adenoidectomy.
In the study Rach 1991, randomisation was by child, but the individual ear was the unit of analysis for persistence of OME ‐ results have therefore been adjusted to account for the correlation between ears of the same individual.
Comparison 2: Early ventilation tubes versus watchful waiting
This comparison included six studies where some children were randomised to receive ventilation tubes immediately, and others were monitored but may have undergone ventilation tube insertion at a later stage, if appropriate.
Four studies enrolled very young children. Maw 1999 randomised children (mean age approximately three years) with bilateral OME to receive ventilation tubes or watchful waiting. Paradise 2007 randomised over 400 very young children (mean age 15 months) with either bilateral or unilateral OME to immediate ventilation tubes, or delayed ventilation tube insertion (after a wait of six to nine months). Rovers 2000 randomised young children (mean age approximately 19.5 months) with persistent bilateral OME to insertion of ventilation tubes or watchful waiting. Long‐term results from the study Rach 1991 (described above, children aged two to four) are also included in this comparison, as some participants in the control (no ventilation tube) group underwent ventilation tube insertion during the extended follow‐up period.
Two studies considered slightly older children. TARGET 2000 randomised children aged between approximately three and seven years, with bilateral OME, to insertion of ventilation tubes or watchful waiting. A third arm in this trial considered adenoidectomy ‐ data from this arm are relevant for a companion Cochrane Review on the role of adenoidectomy for OME (MacKeith 2023). Velepic 2011 randomised children with predominantly bilateral OME to receive ventilation tube insertion plus adenoidectomy, or adenoidectomy alone.
The child was the unit of analysis for all studies except for Velepic 2011, where the ear was the unit of analysis.
Comparison 3: Ventilation tubes versus hearing aids
None of the included studies assessed this comparison.
Comparison 4: Ventilation tubes versus non‐surgical treatment
A single study was identified for this comparison. Bernard 1991 was a single‐centre study from Canada, which randomised children to receive either bilateral myringotomy and ventilation tubes or to receive a six‐month course of antibiotics (sulfisoxazole). Participants were analysed according to their randomised group; however, it should be noted that 47.7% of participants in the medical treatment group did receive ventilation tubes over the course of follow‐up, due to 'treatment failure'.
Comparison 5: Ventilation tubes versus myringotomy
We identified nine studies for this comparison, but different techniques were used to carry out myringotomy.
Laser myringotomy
Two studies randomised children to receive either laser myringotomy or ventilation tubes (D'Eredita 2006; Yousaf 2016). Koopman 2004 enrolled children with bilateral OME, and children received a ventilation tube in one ear and laser myringotomy in the other.
Cold steel myringotomy
Four studies randomised children to receive either bilateral ventilation tubes or cold‐steel myringotomy (Gates 1989; Popova 2010; Sujatha 2015; Tao 2020). In addition, half of the children in Gates 1989 and all the children in Popova 2010 received adenoidectomy. One further RCT randomised children with bilateral OME to receive a ventilation tube in one ear and cold steel myringotomy in the other (To 1984).
Thermal myringotomy
Ruckley 1988 randomised children with bilateral OME to receive a ventilation tube in one ear and thermal myringotomy in the other ear.
Types of ventilation tubes
Studies included in this review used a variety of different ventilation tubes (although some did not report the exact type of tube used: Elkholy 2021; Maw 1999; Paradise 2007; Velepic 2011; Yousaf 2016). The majority of studies that did specify the ventilation tube type reported the use of short‐acting ventilation tubes (including Reuter bobbins, Donaldson, Shah and Shepherd tubes). Only two studies explicitly mentioned the use of longer‐term ventilation tubes, and these were only used in a subset of study participants (Bernard 1991; Koopman 2004). It should be noted that the use of short‐acting tubes is likely to impact on the efficacy of the intervention, particularly for longer‐term outcomes.
Outcomes
Hearing
Return to normal hearing
As with other reviews in this suite, few studies reported our preferred outcome measure for hearing ‐ the proportion of children in whom hearing returns to normal. This outcome was only measured by three studies (D'Eredita 2006; Dempster 1993; Paradise 2007). Dempster 1993 and Paradise 2007 defined 'normal hearing' as < 15 dB HL, whilst D'Eredita 2006 did not provide a definition.
Final hearing thresholds or change in hearing threshold
The majority of studies assess hearing using mean final hearing thresholds. We have concerns about whether this is an appropriate method to assess hearing, as it may give misleading results ‐ particularly in a condition where there is a high rate of spontaneous resolution. A small mean change in hearing may actually be consistent with a large improvement in hearing for a subset of children (and little change for those who had spontaneous improvement).
Most studies assessed mean hearing thresholds using pure tone audiometry, typically over a range of frequencies (Bernard 1991; Dempster 1993; Maw 1983; Maw 1999; Paradise 2007; Popova 2010; TARGET 2000; To 1984). Rovers 2000 assessed hearing using a portable visual reinforcement audiometry set, which measured the minimal response level (not a mean hearing level) in the better‐hearing ear. Three studies assessed the air‐bone gap when assessing hearing (Ruckley 1988; Sujatha 2015; Velepic 2011).
Disease‐specific quality of life
We did not identify any studies that assessed disease‐specific quality of life.
Adverse event: persistent perforation
A small number of studies provided some information about the rate of persistent tympanic membrane perforation.
Presence/persistence of OME
Persistence of OME was assessed in the majority of studies. However, the methods used to identify persistent OME varied ‐ with the use of different combinations of tympanometry, otoscopy and audiometry findings. This may result in some heterogeneity in the effect estimates seen.
Adverse events: tympanic membrane changes, tube‐related, patient‐related
Few studies appeared to systematically assess and report on the presence of adverse effects. The data obtained were often not suitable for meta‐analysis, as we had insufficient information on the number of events or denominators, or outcomes were only reported for one group.
Receptive language skills
Four studies conducted some kind of assessment of receptive language skills (Maw 1999; Paradise 2007; Rach 1991; Rovers 2000). This outcome was assessed using the Reynell test, the WOLD test, reading fluency Woodcock Reading Mastery Tests, Woodcock‐Johnson III Tests of Achievement and tests of phonological processing.
Expressive language skills
The same four studies also assessed expressive language skills, using the Reynell test, WOLD and Schlichting test scores (Maw 1999; Paradise 2007; Rach 1991; Rovers 2000).
Cognitive development
This outcome was assessed in Maw 1999 (using the Griffiths practical reasoning test and the WISC‐III short form) and Paradise 2007 (with the Wechsler Abbreviated Scale of Intelligence, and the calculation subset of the Woodcock‐Johnson III Tests of Achievement).
Psychosocial outcomes
The study Maw 1999 considered a number of behavioural outcomes, assessed with the Richman Behaviour Checklist, which is completed by the child's parents (range 0 to 24, higher scores represent worse behaviour, and a threshold of ≥ 10 has been suggested as a cut‐off to determine behavioural problems). Rovers 2000 used the Erikson Scale of Parent‐Child interaction and Paradise 2007 used the Disruptive Behavior Disorders Rating Scale and Child Behavior Checklist to assess this outcome.
Listening skills
This outcome was not assessed by any of the included studies.
Generic health‐related quality of life
A single study included an assessment of generic health‐related quality of life, using the TAIQOL questionnaire (Rovers 2000).
Parental stress
A single study measured this outcome, using the Parenting Stress Index (Paradise 2007).
Vestibular function
This outcome was not assessed by any of the included studies.
Doctor‐diagnosed acute otitis media episodes
This outcome was assessed by only two studies (Bernard 1991; Popova 2010).
Excluded studies
We excluded 50 records (linked to 47 studies). The main reasons for exclusion are listed below.
Eighteen studies were not randomised controlled trials, or did not analyse participants according to their randomised groups (Ah‐Tye 2001; Bozkurt 2004; Englender 1999; Ferrara 2005; Gibson 1996; Hassmann 2004; Iino 1989; Kremer 1979; Liu 2004; MRC Multicentre Otitis Media Study 2004; MRC Multicentre Otitis Media Study 2008; Paradise 1997; Parlea 2012; Sanyaolu 2020; Shubich 1996; Stenstrom 2005; Uvarova 2001; Youssef 2013).
-
Fifteen studies recruited an incorrect population, including:
11 studies in which the duration of OME was unknown, or was definitely less than three months (Black 1990; El Begermy 2022; Bulman 1984; Hammaren‐Malmi 2005; Lildholdt 1983; Mandel 1989; Markou 2004; NCT00629694; Rohail 2006; Shishegar 2007; Skinner 1988);
three studies in which participants had recurrent acute otitis media, not OME (Gebhart 1981; Kujala 2012; Paradise 1990);
one study where participants had acute otitis media (Nguyen 2004).
Twelve studies assessed an intervention other than ventilation tubes. Some of these studies were relevant for other reviews in this suite (Ardehali 2008; Choung 2008; Hao 2019; Jabeen 2019; Mandel 1992; Marchisio 1998; Maw 1993; Moller 1990; NCT05545345; Tao 2020; Xu 2016; Yousaf 2014).
One study used an incorrect comparator, where ventilation tubes were compared to balloon dilatation of the Eustachian tube (Li 2020).
One study was terminated/withdrawn before any results were available (Demant 2017).
Risk of bias in included studies
We had concerns over the potential for bias in all the included studies in this review. See Figure 3 for a summary of the risk of bias across the studies, and Figure 4 for detailed judgements on individual studies.
3.

4.

Allocation
Most studies provided sufficient information regarding the randomisation procedure for us to be confident that a random method was employed. However, seven studies did not provide this information (Bernard 1991; D'Eredita 2006; Dempster 1993; Popova 2010; To 1984; Velepic 2011; Yousaf 2016). One study used quasi‐randomisation, where participants were allocated to groups according to the order of recruitment to the study (Elkholy 2021), leading to a high risk of selection bias. Only five studies provided a description of methods used to conceal group allocation (Dempster 1993; Gates 1989; Maw 1999; Ruckley 1988; TARGET 2000). We judged the remaining studies at unclear risk of selection bias, as insufficient information was available to determine whether group allocation may have been predicted.
Blinding
None of the included studies appeared to blind participants and study personnel to the intervention received, and only three studies described blinding of outcome assessors (Maw 1999; Paradise 2007; TARGET 2000).
Incomplete outcome data
The risk of bias was mixed for this domain. We considered nine studies to provide sufficient follow‐up data that attrition bias was not a concern (Bernard 1991; D'Eredita 2006; Elkholy 2021; Paradise 2007; Sujatha 2015; Tao 2020; To 1984; Velepic 2011; Yousaf 2016). We rated five studies at high risk of attrition bias, due to the level of dropout over the course of the study (Gates 1989; Koopman 2004; Maw 1999; Popova 2010; Rovers 2000). For the remaining studies, there was either insufficient information to judge whether dropout posed a risk of attrition bias, or we were uncertain whether the extent of dropout would be enough to cause a risk here.
Selective reporting
We considered five studies to be at risk of selective reporting, mainly due to incomplete reporting of primary outcome measures (D'Eredita 2006; Koopman 2004; Ruckley 1988; Yousaf 2016). We also rated the study Velepic 2011 at high risk, as it was unclear whether outcome data were provided for follow‐up at three months or six months, and raw data were not reported for some outcomes (only P values). The time of follow‐up affects interpretation of the outcomes as ventilation tubes were inserted for all participants in the control group who did not have resolution of the effusion after three months.
We rated most of the remaining studies at unclear risk of bias, as no registered protocol was available with which to compare the published reports.
Other potential sources of bias
We identified some additional issues with several studies, which we considered to be a potential risk of bias:
Bernard 1991 used two different types of ventilation tubes over the course of the study, and reported that one was better than the other at improving hearing loss. Data were not available for the different types of ventilation tubes. In addition, many children (48%) in the control (antibiotics) group also received a ventilation tube over the course of the trial, which may bias the findings towards the null.
Elkholy 2021 only provided useable outcome data after two weeks of follow‐up, which is too short to assess the effect of ventilation tubes and no intervention for many outcomes.
Gates 1989 permitted parents to choose a different treatment to the one randomised. This occurred for 5.5% of participants. In addition, many children undergoing medical (49%) or surgical (22%) treatment underwent a second course of the same treatment during the trial.
Popova 2010 appeared to use a 'per protocol' analysis, rather than 'intention‐to‐treat'.
Ruckley 1988 conducted follow‐up at three months, which may be too short to adequately assess the effect of the intervention.
TARGET 2000 retrospectively published the trial protocol, raising the possibility of publication bias. In addition, this was an MRC‐funded, multicentre trial and yet not all outcomes stated in the trial registration were published.
To 1984 indicated that most, but not all, children in the control group received a myringotomy. Ideally data would have been available separately for these groups, to include in the comparison of ventilation tubes versus no treatment and ventilation tubes versus myringotomy. The mixed control group may bias the results, if the effect sizes for ventilation tubes versus myringotomy and no treatment differ.
Velepic 2011 only recruited children who regularly attended check‐ups, which may have led to a risk of selection bias.
Yousaf 2016 randomised participants at the level of the child, but reported results at the level of the individual ear. This fails to account for correlation between ears of the same individual, and may lead to confidence intervals that are too precise.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
Comparison 1: Ventilation tubes versus no treatment
Four studies were included in this comparison (Dempster 1993; Elkholy 2021; Maw 1983; Rach 1991).
Hearing
Return to normal hearing at 3 to 12 months follow‐up
One study compared the proportion of ears in which hearing returned to normal levels (defined as < 15 dB HL) at 12 months follow‐up. The odds ratio (OR) for return to normal hearing was 1.13 in favour of ears that had received ventilation tubes, but the evidence is very uncertain (95% confidence interval (CI) 0.46 to 2.74; 54% versus 51%; 1 study, 72 participants; Analysis 1.1; very low‐certainty evidence).
1.1. Analysis.

Comparison 1: Ventilation tubes versus no treatment, Outcome 1: Return to normal hearing, randomised by ear (medium‐term)
As there is likely to be some correlation in this outcome between ears of the same individual, we attempted to account for this in the analysis. The main analysis was conducted assuming a correlation coefficient of 0.5 between ears of the same individual. However, we conducted sensitivity analyses to determine whether changing the assumed correlation would have a significant impact on the results, and it did not (Analysis 5.1; Analysis 5.2).
5.1. Analysis.

Comparison 5: Sensitivity analyses: Ventilation tubes versus no treatment, Outcome 1: Sensitivity analysis: Return to normal hearing, randomised by ear (medium‐term); CC = 0.3
5.2. Analysis.

Comparison 5: Sensitivity analyses: Ventilation tubes versus no treatment, Outcome 2: Sensitivity analysis: Return to normal hearing, randomised by ear (medium‐term); CC = 0.7
We also noted that the threshold for 'normal hearing' of < 15 dB HL was lower than we had pre‐specified in our protocol. The authors of Dempster 1993 also reported the proportion of ears in which hearing returned to < 25 dB HL. If this threshold was used as 'normal hearing' then there was no difference between the groups, with an OR of 1.00 for ears that received a ventilation tube (Analysis 5.3).
5.3. Analysis.

Comparison 5: Sensitivity analyses: Ventilation tubes versus no treatment, Outcome 3: Sensitivity analysis: Return to normal hearing, randomised by ear (medium‐term). Normal defined as < 25 dB; CC = 0.5
Final hearing threshold at 3 to 12 months follow‐up
Two studies compared the final hearing threshold for ears that had received a ventilation tube, compared to ears that had not, at 12 months follow‐up. The mean difference in hearing level was ‐3.47 dB HL lower (better) for ears that had received a ventilation tube (95% CI ‐9.97 to 3.03; 2 studies, 129 participants; Analysis 1.2; very low‐certainty evidence).
1.2. Analysis.

Comparison 1: Ventilation tubes versus no treatment, Outcome 2: Mean final hearing threshold, randomised by ear (medium‐term)
As above, when we accounted for correlation between the ears of the same individual using a variety of correlation coefficients, the effect size seen was very similar (Analysis 5.4; Analysis 5.5).
5.4. Analysis.

Comparison 5: Sensitivity analyses: Ventilation tubes versus no treatment, Outcome 4: Sensitivity analysis: Mean final hearing threshold, randomised by ear (medium‐term); CC = 0.3
5.5. Analysis.

Comparison 5: Sensitivity analyses: Ventilation tubes versus no treatment, Outcome 5: Sensitivity analysis: Mean final hearing threshold, randomised by ear (medium‐term); CC = 0.7
Change in hearing threshold at 3 to 12 months follow‐up
A single study assessed this outcome at 12 months follow‐up. The mean change in hearing level was ‐0.16 dB HL lower (better) for those ears that received a ventilation tube, compared to those that did not, but the evidence is very uncertain (95% CI ‐3.28 to 2.97; 1 study, 72 participants; Analysis 1.3; very low‐certainty evidence).
1.3. Analysis.

Comparison 1: Ventilation tubes versus no treatment, Outcome 3: Change in hearing threshold from baseline, randomised by ear (medium‐term)
Accounting for correlation between ears of the same individual made a very modest difference to the effect estimate, ranging from ‐0.10 to ‐0.21 dB HL lower (Analysis 5.6; Analysis 5.7).
5.6. Analysis.

Comparison 5: Sensitivity analyses: Ventilation tubes versus no treatment, Outcome 6: Sensitivity analysis: Change in hearing threshold from baseline, randomised by ear (medium‐term); CC = 0.3
5.7. Analysis.

Comparison 5: Sensitivity analyses: Ventilation tubes versus no treatment, Outcome 7: Sensitivity analysis: Change in hearing threshold from baseline, randomised by ear (medium‐term); CC = 0.7
Disease‐specific quality of life
No data were identified for this outcome.
Adverse event: persistent perforation
One study reported on perforation or retraction of the tympanic membrane (Dempster 1993). The odds ratio for perforation/retraction was 0.85 for those ears that had received a ventilation tube, compared to those that did not (95% CI 0.38 to 1.91; 8.3% versus 9.7%; 1 study, 72 participants; Analysis 1.4; very low‐certainty evidence).
1.4. Analysis.

Comparison 1: Ventilation tubes versus no treatment, Outcome 4: Adverse event: perforation/retraction, randomised by ear (medium‐term)
As above, when we accounted for correlation between the ears of the same individual using a variety of correlation coefficients, the effect size seen was very similar (Analysis 5.8; Analysis 5.9).
5.8. Analysis.

Comparison 5: Sensitivity analyses: Ventilation tubes versus no treatment, Outcome 8: Sensitivity analysis: Adverse event: perforation/retraction, randomised by ear (medium‐term); CC = 0.3
5.9. Analysis.

Comparison 5: Sensitivity analyses: Ventilation tubes versus no treatment, Outcome 9: Sensitivity analysis: Adverse event: perforation/retraction, randomised by ear (medium‐term); CC = 0.7
Presence/persistence of OME
Three studies assessed this outcome. The unit of analysis was different for these trials (Rach 1991 and Elkholy 2021 analysed per child, Dempster 1993 analysed per ear), therefore we have presented the results separately.
Randomised per child
< 6 weeks follow‐up
The risk ratio for persistence of OME after just two weeks of follow‐up was 0.33 (95% CI 0.08 to 1.46; 10% versus 30%; 1 study, 40 participants; Analysis 1.5; very low‐certainty evidence).
1.5. Analysis.

Comparison 1: Ventilation tubes versus no treatment, Outcome 5: Persistence of OME: randomised by child (very short‐term)
3 to 12 months follow‐up
After six months, one study reported a risk ratio of 0.30 for persistence of OME in ears that had received ventilation tubes (95% CI 0.14 to 0.65; 20% versus 68%; 1 study, 40 participants; Analysis 1.6; low‐certainty evidence). Although the trial was randomised by child, the unit of analysis was the individual ear. Using different intracluster correlation coefficients as part of a sensitivity analysis had little impact on the overall result (Analysis 5.10; Analysis 5.11).
1.6. Analysis.

Comparison 1: Ventilation tubes versus no treatment, Outcome 6: Persistence of OME: randomised by child (medium‐term)
5.10. Analysis.

Comparison 5: Sensitivity analyses: Ventilation tubes versus no treatment, Outcome 10: Sensitivity analysis: Persistence of OME: randomised by child (medium‐term); ICC = 1.0
5.11. Analysis.

Comparison 5: Sensitivity analyses: Ventilation tubes versus no treatment, Outcome 11: Sensitivity analysis: Persistence of OME: randomised by child (medium‐term); ICC = zero
Randomised per ear
3 to 12 months follow‐up
One study identified an odds ratio of 0.66 for the persistence of OME in ears that had received ventilation tubes, compared to ears of the same individual that did not have a ventilation tube fitted (95% CI 0.24 to 1.85; 49% versus 58%; 1 study, 72 participants; Analysis 1.7; very low‐certainty evidence). We note considerable heterogeneity in the effect between the two different subgroups of children included in this study. The effect size was substantial for those who did not receive adenoidectomy (OR 0.39, 95% CI 0.20 to 0.77), but was trivial for those who did receive adenoidectomy (OR 1.11, 95% CI 0.58 to 2.12).
1.7. Analysis.

Comparison 1: Ventilation tubes versus no treatment, Outcome 7: Persistence of OME: randomised by ear (medium‐term)
As above, when we accounted for correlation between the ears of the same individual using a variety of correlation coefficients, the effect size seen was very similar (Analysis 5.12; Analysis 5.13).
5.12. Analysis.

Comparison 5: Sensitivity analyses: Ventilation tubes versus no treatment, Outcome 12: Sensitivity analysis: Persistence of OME: randomised by ear (medium‐term); CC = 0.3
5.13. Analysis.

Comparison 5: Sensitivity analyses: Ventilation tubes versus no treatment, Outcome 13: Sensitivity analysis: Persistence of OME: randomised by ear (medium‐term); CC = 0.7
Other adverse events
Not all the adverse events reported were amenable to meta‐analysis. We have therefore summarised a number of adverse events in Table 7 and Table 8. Additional information is shown in Appendix 3.
3. Adverse events: primary and secondary outcomes ‐ tympanic membrane changes and tube‐related.
| Comparison and studies | Primary outcome | Secondary outcomes | ||||||
| 1. Tympanic membrane changes | 2. Tube‐related | |||||||
| Persistent perforation | Tympanosclerosis | Myringosclerosis | Infection | Foreign body reaction | Other | Otorrhoea | Tube functioning | |
| Ventilation tubes (VT) versus no treatment | ||||||||
| Dempster 1993 | VT: 6/72 (8.3%) No VT: 7/72 (9.7%) (described as persistent perforation or retraction) |
VT: 28/72 (39%) No VT: 1/72 (1.4%) | x | x | x | x | x | See Effects of interventions |
| Maw 1983 | x | x | x | x | x | x | x | x |
| Rach 1991 | x | x | x | x | x | x | x | VT 9/44 (20.5%) in situ short‐term (< 3 months) 26/44 (59.1%) in situ medium‐term (≥ 6 months) |
| Early VT versus watchful waiting (treatment later if required) | ||||||||
| TARGET 2000 | VT (with and without adenoidectomy): 8/635 (0.01%) ≥ 6 months See Effects of interventions |
VT (with and without adenoidectomy): 128/635 (20%) WW 0 ≥ 6 months See Effects of interventions |
x | x | x | x | x | VT functioning ears: 259/327 (79%), non‐functioning/extruded 68/327 (21%) = 3 months VT functioning ears: 57/316 (55%), non‐functioning/extruded 259/316 (45%) = 12 months VT functioning ears: 9/300 (3%), non‐functioning/extruded 291/300 (97%) = 24 months See Effects of interventions |
| Maw 1999 | x | x | x | x | x | x | x | x |
| Paradise 2007 | See Analysis 2.16 | See Analysis 2.17; Analysis 2.18; Analysis 2.19 | ||||||
| Rach 1991 (long‐term data) | x | x | x | x | x | x | x | x |
| Rovers 2000 | x | x | x | x | x | x | VT 42.9%, WW 14.3% short‐term (3 months) VT 37.6%, WW 16.5% medium‐term (12 months) Children with a specific number of episodes. VT 0 episodes 16/93 (17%), 1 episode 28 (30%), 2 episodes 26 (28%), > 3 episodes 23 (25%) WW 0 episodes 58 (62%), 1 episode 23 (24%), 2 episodes 8 (9%), > 3 episodes 5 (5%), 12 months Cumulative ≥ 1 episodes VT 83% (95% CI 75 to 91%) WW 38% (28 to 48%) (P = 0.001), 12 months See Effects of interventions |
VT 92% in situ 3 mo. VT 30% in situ 12 months. See Effects of interventions |
| Velepic 2011 | See Analysis 2.9 | x | Total of 42/161 (26%) ears see Effects of interventions | x | x | 1. Attic retraction: total of 79/161 (49%) ears showed attic retraction 2. Tensa retractions with/without malleus rotation total of 36/161 (22%) ears 3. Scars of the ear drum total of 46/161 (29%) See Effects of interventions |
x | x |
| VT versus non‐surgical treatment | ||||||||
| Bernard 1991 | VT: 0/60 (0%) 18 months | x | VT: 17/60 (28.3%) Antibiotic 4/65 (6.1%) 18 months | VT: 17/60 (28.3%) 18 months | VT: 17/60 (28.3%) 18 months | x | VT 26/60 (43.3%) (with and without gram negative bacterial culture) 18 months |
x |
| VT versus myringotomy alone | ||||||||
| ACTRN12611001073998 | No data available as yet | |||||||
| D'Eredita 2006 | VT: 1/15 (6.7%) LM: no data reported for LM |
x | x | x | x | x | LM: 2 short‐term (2 months) VT: 4 very short‐term (30 days) and medium‐term (3 months) See Effects of interventions |
x |
| Gates 1989 | In 6 children (3 post myringotomy and 3 post‐VT) (group allocations not reported) See Effects of interventions |
x | x | x | Number (proportion) of children with x episodes of purulent otorrhoea Myringotomy 0: 83/107 (78%) 1: 14/107 (13%) 2: 7/107 (6%) > 3: 3/107 (3%) VT 0: 92/129 (71%) 1: 23/129 (18%) 2: 6/129 (5%) > 3: 8/129 (6%) Adenoidectomy + M 0: 115/130 (89%) 1: 11/130 (9%) 2: 2/130 (1%) > 3: 2/130 (1%) Ad + VT 0: 95/125 (76%) 1: 25/125 (20%) 2: 3/125 (2%) > 3: 2/125 (2%) Assumed to be cumulative, over 2 years See Analysis 4.14 |
|||
| Koopman 2004 | x | x | x | x | x | x | See Effects of interventions | x |
| Popova 2010 | x | x | x | x | x | x | Ad + VT: 0 episodes 25/42 (60%), 1 episode 10/42 (24%), 2 episodes 5/42 (12%), 3 episodes 1/42 (2%), 4 or more episodes 1/42 (2%) Ad + M: 0 episodes 36/36 (100%), medium‐term (12 months) See Effects of interventions |
VT 7/42 (17%) experienced a blockage, medium‐term 12 months See Effects of interventions |
| Ruckley 1988 | x | VT 0/36 (0%), TM 0/36 (0%) (short‐term 3 months) | x | x | x | x | x | VT 2/36 (5.5%) |
| Sujatha 2015 | VT: R ear: 3/25 L ear: 3/25 Myringotomy R ear: 0/25 L ear: 0/25 12 months |
R ear 12 months: Tympanosclerotic patch Myringotomy 1/25 (4%) VT 2/25 (8%) L ear: 12 months: Tympanosclerotic patch Myringotomy 0/25 VT 1/25 (4%) |
x | x | x | R ear: 3 months: Retraction Myringotomy 22/25 (88%) 12 months: Retraction Myringotomy 7/25 (28%) VT 14/25 (56%) L ear: 3 months: Retraction Myringotomy 22/25 (88%) 12 months: Retraction Myringotomy 6/25 (24%) VT 12/25 (48%) |
x | R ear 3 months VT all in situ 6 months VT 1/25 in situ L ear 3 months VT all in situ 1 blocked 6 months VT 1/25 in situ |
| Tao 2020 | VT: 12 months: 4 ears/4 patients |
VT: 12 months: 6 ears/5 patients (calcified plaques) |
x | x | x | x | x | 2 weeks VT No VT falling out No obstruction 3 months VT 7 ears/4 patients VT falling out 3 ears/3 patients obstruction of VT 6 months: VT 20 ears/11 patients VT falling out 6 ears/5 patients obstruction of VT 12 months: VT 98 ears/11 patients VT falling out 2 ears/2 patients obstruction of VT |
| To 1984 | Authors state "One ear which had received a grommet was improving but was still abnormal." Presumed 1/54 for VT | VT 9/54, Myringotomy 1/54 timing of follow‐up not reported | x | x | x | Retraction segments VT 2/54 Myringotomy 1/54 24 months long‐term | x | x |
| Yousaf 2016 | See Analysis 4.5 | x | x | x | x | 1. Hypertrophic scar, see Analysis 4.18 2. Retraction of tympanic membrane, see Analysis 4.17 |
LM 2 (3%) VT 5 (7.3%) |
6/68 (13%) 30 days 53/68 (78%) 6 months |
Ad: adenoidectomy; CI: confidence interval; L: left; LM: laser myringotomy; M: myringotomy; R: right; TM: thermal myringotomy; VT: ventilation tube; WW: watchful waiting
4. Adverse events: secondary outcomes: patient‐related.
| Comparison and studies | Secondary outcomes | |||||
| 3. Patient‐related | ||||||
| Serious medication‐related adverse effects | Allergic reaction (appearing within 7 days of starting treatment) | Nausea | Vomiting | Otalgia | Post‐surgical haemorrhage | |
| Ventilation tubes (VT) versus no treatment | ||||||
| Dempster 1993 | x | x | x | x | x | x |
| Maw 1983 | ||||||
| Rach 1991 | x | x | x | x | x | x |
| Early VT versus watchful waiting (treatment later if required) | ||||||
| TARGET 2000 | x | x | x | x | x | 1/165 (0.6%) children that had adenoidectomy had to return to theatre due to postoperative haemorrhage. (Note: N exceeds number allocated to Ad group because of cross‐overs from other groups) |
| Maw 1999 | x | x | x | x | x | x |
| Paradise 2007 | x | x | x | x | x | x |
| Rach 1991 (long‐term data only) | x | x | x | x | x | x |
| Rovers 2000 | x | x | x | x | x | x |
| Velepic 2011 | x | x | x | x | x | x |
| VT versus non‐surgical treatment | ||||||
| Bernard 1991 | Sulfonamide: 0/65 (0%) 18 months | Sulfonamide: 4/65 (6.2%) 18 months | Sulfonamide: 2/65 (3.1%) 18 months | Sulfonamide: 0/65 (0%) 18 months | x | x |
| VT versus myringotomy alone | ||||||
| ACTRN12611001073998 | No data available as yet | |||||
| D'Eredita 2006 | x | x | x | x | x | x |
| Gates 1989 | x | x | x | x | x | 1/251 after adenoidectomy (unclear why 251). Returned to operating theatre for control. |
| Koopman 2004 | x | x | x | x | LM 1/208 (0.5%) during first 2 days post LM | x |
| Popova 2010 | x | x | x | x | x | x |
| Ruckley 1988 | x | x | x | x | TM 1/36 (2.8%) VT not reported very short‐term | x |
| Sujatha 2015 | x | x | x | x | x | x |
| Tao 2020 | x | x | x | x | x | x |
| To 1984 | x | x | x | x | x | x |
| Yousaf 2016 | x | x | x | x | x | LM 0, VT 9 (13%) |
LM: laser myringotomy; TM: thermal myringotomy; VT: ventilation tube
Tympanic membrane changes
One study reported a Peto OR of 10.09 for tympanosclerosis in ears that had received a ventilation tube, compared to those that had not (95% CI 4.48 to 22.70; 1 study, 72 participants; Analysis 1.10; low‐certainty evidence).
1.10. Analysis.

Comparison 1: Ventilation tubes versus no treatment, Outcome 10: Adverse event: tympanosclerosis, randomised by ear (medium‐term)
Tube‐related changes
Rach 1991 found that in the short term (< 3 months), 9/44 (20.5%) ventilation tubes were in situ and in the medium term (six months), 18/44 (40.9%) of the tubes had extruded in the ventilation tube only group (assessed by otoscopy). Maw 1983 reported that some ventilation tubes were reinserted, but no data are presented for the number of extrusions/reinsertions. Dempster 1993 reported that, at the 12‐month follow‐up visit, 31% of ventilation tubes were still functioning.
Patient‐related changes
No patient‐related adverse events were reported.
Receptive language skills
A single study assessed this outcome, using the Reynell test. There was a 0.07 greater mean improvement in the Z score for children who had received bilateral ventilation tubes, as compared to those who did not receive ventilation tubes, but the evidence is very uncertain (95% CI ‐0.26 to 0.4; 1 study, 43 participants; very low‐certainty evidence). We have used Cohen's effect size to interpret these scales, where a change of 0.2 represents a small effect, 0.5 a medium effect and 0.8 a large effect. See Analysis 1.8.
1.8. Analysis.

Comparison 1: Ventilation tubes versus no treatment, Outcome 8: Mean improvement in comprehensive language, randomised by child (medium‐term)
Speech development/expressive language skills
The same study assessed this outcome, also using the Reynell test. There was a 0.12 greater mean improvement in the Z score for children who had received bilateral ventilation tubes as compared to those who did not receive ventilation tubes, but the evidence is very uncertain (95% CI ‐0.27 to 0.51; 1 study, 43 participants; Analysis 1.9; very low‐certainty evidence).
1.9. Analysis.

Comparison 1: Ventilation tubes versus no treatment, Outcome 9: Mean improvement in expressive language, randomised by child (medium‐term)
Other outcomes
No data were identified regarding cognitive development, psychosocial outcomes, listening skills, generic health‐related quality of life, parental stress, vestibular function or the number of doctor‐diagnosed episodes of acute otitis media.
Comparison 2: Early ventilation tubes versus watchful waiting
We included six studies in this comparison. All randomised individual children to receive immediate ventilation tube insertion, or to undergo a period of watchful waiting ‐ with later insertion of ventilation tubes as required.
Hearing
Return to normal hearing
Long‐term follow‐up (> 1 year)
A single study assessed the proportion of children in whom hearing returned to normal by the age of 9 to 11 years, defined as a hearing threshold of ≤ 15 dB HL (Paradise 2007). The risk ratio for return to normal hearing in those with early ventilation tube insertion was 0.98 (95% CI 0.94 to 1.03; 93% compared to 95%; 1 study, 391 participants; Analysis 2.1; very low‐certainty evidence).
2.1. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 1: Return to normal hearing, randomised by child (long‐term)
Mean final hearing threshold
≤ 3 months follow‐up
One study assessed final hearing threshold at three months, and found a mean difference of ‐11.90 dB HL favouring early ventilation tube insertion, but the evidence is very uncertain (95% CI ‐14.19 to ‐9.61; 1 study, 215 participants; Analysis 2.2; very low‐certainty evidence).
2.2. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 2: Mean final hearing threshold, randomised by child (short‐term)
3 to 12 months follow‐up
Two studies conducted follow‐up at 9 to 12 months. Overall, the mean difference in hearing level was ‐1.89 dB HL in favour of early ventilation tubes, but the evidence is very uncertain (95% CI ‐7.32 to 3.54; 2 studies, 351 participants; I2 = 74%; Analysis 2.3; very low‐certainty evidence).
2.3. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 3: Mean final hearing threshold (air conduction), randomised by child (medium‐term)
One further study also assessed this outcome but used air‐bone gap (rather than air‐conduction thresholds). In addition, outcomes were reported per ear (despite randomisation at the level of the individual child). Therefore, we have had to adjust the results to account for the correlation between ears of the same individual. These results have not been pooled, but show a similar result of very low certainty, with a mean difference of ‐1.18 dB HL in favour of early ventilation tubes (95% CI ‐2.9 to 0.54; 1 study, 87 participants with data from 161 ears; Analysis 2.4; very low‐certainty evidence). Sensitivity analyses using a different intracluster correlation coefficient showed very similar results (Analysis 6.1; Analysis 6.2).
2.4. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 4: Mean final hearing threshold (air‐bone gap), randomised by child, analysed by ear (medium‐term)
6.1. Analysis.

Comparison 6: Sensitivity analyses: Early ventilation tubes versus watchful waiting, Outcome 1: Sensitivity analysis: Mean final hearing threshold (air‐bone gap), randomised by child, analysed by ear (medium‐term); ICC = 1.0
6.2. Analysis.

Comparison 6: Sensitivity analyses: Early ventilation tubes versus watchful waiting, Outcome 2: Sensitivity analysis: Mean final hearing threshold (air‐bone gap), randomised by child, analysed by ear (medium‐term); ICC = zero
Long‐term follow‐up (> 1 year)
Three studies conducted follow‐up at between 18 months and approximately 3.5 years. The mean difference in hearing threshold for those receiving early ventilation tubes was 0.36 (95% CI ‐0.41 to 1.13; 3 studies, 633 participants; I2 = 0%; Analysis 2.5; low‐certainty evidence). Sensitivity analyses using a different correlation coefficient for the study Paradise 2007 showed very similar results (Analysis 6.3; Analysis 6.4).
2.5. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 5: Mean final hearing threshold, randomised by child (long‐term)
6.3. Analysis.

Comparison 6: Sensitivity analyses: Early ventilation tubes versus watchful waiting, Outcome 3: Sensitivity analysis: Mean final hearing threshold, randomised by child (long‐term); CC for Paradise 2007 of 0.3
6.4. Analysis.

Comparison 6: Sensitivity analyses: Early ventilation tubes versus watchful waiting, Outcome 4: Sensitivity analysis: Mean final hearing threshold, randomised by child (long‐term); CC for Paradise 2007 of 0.7
Paradise 2007 also assessed hearing using the children's version of the 'hearing in noise' test, where a child repeats sentences heard in a quiet room, and with competing noise. Each sentence is repeated at increasing loudness levels until the child can hear and repeat it. As above, the differences between the two groups are trivial and the evidence is very uncertain (mean difference ranged from 0 dB to 0.4 dB higher; 1 study, 391 participants; Analysis 2.6; very low‐certainty evidence).
2.6. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 6: Hearing in noise test, randomised by child (long‐term)
Change in hearing threshold from baseline
3 to 12 months follow‐up
One study assessed the change in hearing over the course of the study. The mean difference in hearing threshold between the two groups was ‐4.60 dB HL in favour of early ventilation tubes at between 9 and 12 months of follow‐up, but the evidence is very uncertain (95% CI ‐8.57 to ‐0.63; 1 study, 176 participants; Analysis 2.7; very low‐certainty evidence).
2.7. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 7: Change in hearing threshold from baseline, randomised by child (medium‐term)
This study also reported a multivariate analysis of the difference in hearing improvement between the two groups, adjusted for baseline hearing level and age. Here the mean difference was ‐1.6 dB better for those receiving early ventilation tubes, but the evidence is very uncertain (95% CI ‐0.62 to 3.82; 1 study, 166 participants; Analysis 2.8; very low‐certainty evidence).
2.8. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 8: Adjusted mean difference in hearing improvement, randomised by child (medium term)
Disease‐specific quality of life
No data were identified for this outcome.
Adverse event: persistent perforation
3 to 12 months follow‐up
One study assessed the rate of persistent tympanic membrane perforations after six months of follow‐up but reported no events in either group (risk difference 0, 95% CI ‐0.03 to 0.03; 1 study, 161 participants; Analysis 2.9; very low‐certainty evidence).
2.9. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 9: Adverse event: persistent perforation, randomised by child (medium‐term)
In TARGET 2000, of 635 ears that had a ventilation tube inserted, eight had a perforation recorded at least six months after surgery. However, of the four who attended later appointments, all had healed.
Long‐term follow‐up (> 1 year)
One study assessed the rate of perforation after approximately 3.5 years of follow‐up. The risk ratio for perforation for those who had received early ventilation tubes was 3.65 (95% CI 0.41 to 32.38; 1 study, 281 participants, but data are reported according to ears affected and adjusted for correlation between ears of the same individual; Analysis 2.10; very low‐certainty evidence).
2.10. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 10: Adverse event: persistent perforation, randomised by child (long‐term)
Presence/persistence of OME
3 to 12 months follow‐up
Three studies assessed this outcome but used slightly different ways of assessing and reporting persistent OME. Velepic 2011 assessed persistence of OME in both ears using otoscopy at six months follow‐up and found a risk ratio of 0.39 for participants who had undergone early ventilation tube insertion (95% CI 0.09 to 1.72; 5% versus 13%; 1 study, 87 participants; Analysis 2.11; very low‐certainty evidence).
2.11. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 11: Presence/persistence of OME, randomised by child, measured by otoscopy (medium‐term)
Maw 1999 used tympanometry to assess the presence of OME in the better ear at nine months of follow‐up and found a risk ratio of 0.52 for those who had undergone early ventilation tube insertion (95% CI 0.37 to 0.71; 37% versus 70%; 1 study, 154 participants; Analysis 2.12; low‐certainty evidence). Finally, Paradise 2007 reported on the percentage of days during follow‐up that OME persisted for in each group. OME persisted for 19% fewer days in those who had received early ventilation tubes, but the evidence is very uncertain (95% CI 23% fewer to 15% fewer; 1 study, 316 participants; Analysis 2.13; very low‐certainty evidence).
2.12. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 12: Presence/persistence of OME, randomised by child, measured by tympanometry (medium‐term)
2.13. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 13: Presence/persistence of OME, mean percentage of days, randomised by child (medium‐term)
Long‐term follow‐up (> 1 year)
Three studies assessed the presence or persistence of OME after long‐term follow‐up using tympanometry (from 18 months to over six years) and found a risk ratio of 1.21 for those who had undergone early ventilation tube insertion (95% CI 0.84 to 1.74; 15% versus 12%; 3 studies, 584 participants; I2 = 0%; Analysis 2.14; very low‐certainty evidence).
2.14. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 14: Presence/persistence of OME, randomised by child (long‐term)
One of these studies also presented an adjusted effect estimate, accounting for baseline differences in gender, age, housing status, maternal education and mother's parity. The odds ratio for abnormal tympanometry was 0.99 (95% CI 0.35 to 2.83; 1 study, 65 participants; Analysis 2.15; very low‐certainty evidence).
2.15. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 15: Presence/persistence of OME, adjusted OR, randomised by child (long‐term)
Adverse events
Adverse events were reported inconsistently by the different studies, and many were not amenable to analysis. We have therefore summarised a number of adverse events in Table 7 and Table 8. Additional information is shown in Appendix 3.
Receptive language skills
Three studies assessed receptive language skills at medium‐term (Maw 1999; Rovers 2000) and long‐term follow‐up (Maw 1999; Paradise 2007). This outcome was assessed using the Reynell test, the WOLD test, reading fluency Woodcock Reading Mastery Tests, Woodcock‐Johnson III Tests of Achievement and tests of phonological processing. Overall, outcomes on these tests either showed a trivial difference between the two groups, or slight benefit for those who received early ventilation tubes (see Analysis 2.20; Analysis 2.21; Analysis 2.22; Analysis 2.23; Analysis 2.24; Analysis 2.25; Analysis 2.26; Analysis 2.50; Analysis 2.51 and Table 9). However, we assessed all the evidence as very low certainty.
2.20. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 20: Receptive language development, Reynell test, randomised by child (medium‐term)
2.21. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 21: Receptive language development, Reynell test, adjusted MD (medium‐term)
2.22. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 22: Receptive language, Reynell test, randomised by child (long‐term)
2.23. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 23: Receptive language: Reynell test, long‐term, adjusted MD
2.24. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 24: Receptive language: WOLD adjusted OR (long‐term)
2.25. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 25: Receptive language, mean difference (months) in improvement in Reynell test score (equivalent age‐real age): medium‐term
2.26. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 26: Receptive language, adjusted mean difference (months) in improvement in Reynell test score (equivalent age ‐ real age): medium‐term
2.50. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 50: Literacy (long‐term)
2.51. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 51: Phonological awareness (long‐term)
5. Developmental outcomes at age 9 to 11 from Paradise 2007 with GRADE assessment.
| Test | Reported test properties, working MID | Early VT mean score ± SD (n) | WW mean score ± SD (n) | MD (95% CI) | GRADE certainty of evidencea |
| Literacy | |||||
| Woodcock Reading Mastery Tests: | The normative mean standard score is 100 ± 15. Higher scores indicate more favourable results. Working MID of 15. | ||||
| Word identification subtest | 98 ± 11 (195) | 99 ± 12 (196) | ‐1.00 (‐3.28 to 1.28) | Very low | |
| Word Attack subtest | 103 ± 13 (195) | 104 ± 14 (196) | ‐1.00 (‐3.68 to 1.68) | Very low | |
| Passage Comprehension subtest | 98 ± 12 (195) | 99 ± 12 (196) | ‐1.00 (‐3.38 to 1.38) | Very low | |
| Oral reading fluency test: | Higher scores indicate more favourable results. Working MID of 15. | ||||
| Children in grade 3 | 78 ± 36 (37) | 87 ± 41 (37) | ‐9.00 (‐26.58 to 8.58) | Very low | |
| Children in grade 4 | 89 ± 36 (87) | 89 ± 38 (97) | 0.00 (‐10.70 to 10.701) | Very low | |
| Children in grade 5 | 97 ± 36 (54) | 102 ± 37 (51) | ‐5.00 (‐18.98 to 8.98) | Very low | |
| Children in grade 6 | 102 ± 32 (12) | 96 ± 43 (9) | 6.00 (‐27.42 to 39.42) | Very low | |
| Woodcock–Johnson III Tests of Achievement: | In both subtests, raw scores are converted to standard scores according to the child’s age. The normative mean standard score on both subtests is 100 ± 15. Higher scores indicate more favourable results. Working MID of 15. | ||||
| Spelling subtest | 96 ± 13 (194) | 97 ± 16 (196) | ‐1.00 (‐3.89 to 1.89) | Very low | |
| Writing Samples subtest | 104 ± 14 (192) | 105 ± 15 (195) | ‐1.00 (‐3.89 to 1.89) | Very low | |
| Phonological awareness | |||||
| Comprehensive Test of Phonological Processing: | In both subtests, raw scores are converted to standard scores according to the child’s age. The normative mean standard score on each subtest is 10 ± 3. Higher scores indicate more favourable results. Working MID of 3. | ||||
| Elision subtest | 8.6 ± 4.9 (195) | 8.7 ± 3.0 (196) | ‐0.10 (‐0.91 to 0.71) | Very low | |
| Rapid Letter Naming subtest | 9.3 ± 2.5 (193) | 9.6 ± 2.4 (196) | ‐0.30 (‐0.79 to 0.19) | Very low | |
| Attention, impulsivity and psychosocial function | |||||
| Disruptive Behavior Disorders Rating Scale | The items are scored on a 4‐point scale (0, “not at all”; 1, “just a little”; 2, “pretty much; 3, “very much) and are averaged for comparison with normative data. For boys 9 or 10 years of age, the normative mean score for the inattention factor is 1.01 ± 0.91; for the impulsivity and overactivity factor, 0.86 ± 0.81; and for the oppositional defiant factor, 0.69 ± 0.77. For boys 11 through 14 years of age, the corresponding values are 1.01 ± 0.96, 0.85 ± 0.88 and 0.73 ± 0.86. Normative data for girls are not available. Higher scores indicate less favourable results. Working MID of 0.96 (inattention), 0.88 (impulsivity and overactivity) and 0.86 (oppositional defiant factor). | ||||
| Inattention factor: | |||||
| Parent's rating | 0.70 ± 0.63 (194) | 0.65 ± 0.66 (196) | 0.05 (‐0.08 to 0.18) | Very low | |
| Teacher's rating | 0.71 ± 0.74 (190) | 0.67 ± 0.75 (192) | 0.04 (‐0.11 to 0.19) | Very low | |
| Impulsivity and overactivity factor: | |||||
| Parent's rating | 0.67 ± 0.57 (194) | 0.57 ± 0.54 (196) | 0.10 (‐0.01 to 0.21) | Very low | |
| Teacher's rating | 0.48 ± 0.63 (190) | 0.40 ± 0.52 (192) | 0.08 (‐0.04 to 0.20) | Very low | |
| Oppositional defiant factor: | |||||
| Parent’s rating | 0.57 ± 0.58 (194) | 0.52 ± 0.53 (196) | 0.05 (‐0.06 to 0.16) | Very low | |
| Teacher’s rating | 0.33 ± 0.56 (190) | 0.33 ± 0.58 (192) | 0.00 (‐0.11 to 0.11) | Very low | |
| Child Behavior Checklist: | Scores on each of the 8 component scales and a Total Problem score are calculated and converted to T scores. The normative mean T score on each scale and for Total Problems is 50 ± 10. Only the Total Problem scores are shown here. Higher scores indicate less favourable results. Working MID of 10. | ||||
| Total Problems score, parent’s rating | 51 ± 12 (194) | 49 ± 12 (196) | 2.00 (‐0.38 to 4.38) | Very low | |
| Total Problems score, teacher’s rating | 52 ± 11 (189) | 50 ± 11 (191) | 2.00 (‐0.21 to 4.21) | Very low | |
| Impairment Rating Scales: | A score of 3 or higher is considered to be indicative of clinically meaningful impairment. Working MID of 3. | ||||
| Overall functioning, parent’s rating | 0.82 ± 1.42 (194) | 0.68 ± 1.33 (196) | 0.14 (‐0.13 to 0.41) | Very low | |
| Overall functioning, teacher’s rating | 2.04 ± 2.24 (190) | 1.78 ± 2.19 (192) | 0.26 (‐0.18 to 0.70) | Very low | |
| Social Skills Rating System: | The normative mean standard score is 100 ± 15. Higher scores indicate more favourable results. Working MID of 15. | ||||
| Social Skills scale, parent’s version | 96 ± 19 (194) | 98 ± 18 (194) | ‐2.00 (‐5.68 to 1.68) | Very low | |
| Social Skills scale, teacher’s version | 98 ± 13 (184) | 99 ± 13 (186) | ‐1.00 (‐3.65 to 1.65) | Very low | |
| Visual Continuous Performance Test: | Normative data are not available. Higher scores indicate less favourable results. Working MID of 2. | ||||
| Inattention | 9.7 ± 8.5 (195) | 9.5 ± 8.5 (196) | 0.20 (‐1.49 to 1.89) | Very low | |
| Impulsivity | 8.8 ± 16.5 (195) | 8.2 ± 15.6 (196) | 0.60 (‐2.58 to 3.78) | Very low | |
| Auditory Continuous Performance Test: | Normative data are not available. Higher scores indicate less favourable results. Working MID of 2. | ||||
| Inattention | 11.1 ± 7.2 (155) | 11.4 ± 8.0 (153) | ‐0.30 (‐2.00 to 1.40) | Very low | |
| Impulsivity | 3.3 ± 8.7 (154) | 4.2 ± 12.1 (153) | ‐0.90 (‐3.26 to 1.46) | Very low | |
| Intelligence and academic achievement | |||||
| Wechsler Abbreviated Scale of Intelligence | The normative mean score is 100 ± 15. Higher scores indicate more favourable results. Working MID of 15. | 96 ± 13 (195) | 96 ± 14 (196) | 0.00 (‐2.68 to 2.68) | Very low |
| Calculation subtest of the Woodcock–Johnson III Tests of Achievement | The normative mean score is 100 ± 15. Higher scores indicate more favourable results. Working MID of 15. | 99 ± 13 (194) | 99 ± 13 (195) | 0.00 (‐2.58 to 2.58) | Very low |
CI: confidence interval; MD: mean difference; MID: minimum important difference; SD: standard deviation; VT: ventilation tubes; WW: watchful waiting
aGRADING for risk of bias, inconsistency, indirectness and publication bias was the same for each effect estimate (downgraded two levels for performance bias, no downgrade, downgraded one level for population indirectness and no downgrade, respectively). Imprecision was downgraded by one level for each effect estimate as the optimal information size was not attained, and downgraded a further level when two decision thresholds were crossed by the CI.
Speech development/expressive language skills
The same studies also assessed expressive language skills at medium‐term (Maw 1999; Rovers 2000) and long‐term follow‐up (Maw 1999), using the Reynell test, WOLD and Schlichting test scores. Again, the difference between the two groups was largely trivial or showed a very slight benefit for early ventilation tubes, but the evidence is very uncertain (see Analysis 2.27; Analysis 2.28; Analysis 2.29; Analysis 2.30; Analysis 2.31; Analysis 2.32; Analysis 2.33). Some additional data from Paradise 2007 are reported in Table 9.
2.27. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 27: Expressive language development: Reynell test (medium‐term)
2.28. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 28: Expressive language development: Reynell test, medium‐term, adjusted MD
2.29. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 29: Expressive language development: Reynell test (long‐term)
2.30. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 30: Expressive language development: Reynell test, long‐term, adjusted MD
2.31. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 31: Expressive language: WOLD adjusted OR (long‐term)
2.32. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 32: Expressive language, MD (months) in improvement in Schlichting test score (equivalent age‐real age): medium‐term
2.33. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 33: Expressive language, adjusted mean difference (months) in improvement in Schlichting test score (equivalent age‐real age): medium‐term
A number of other aspects of language development were assessed by Maw 1999 after long‐term follow‐up, including repetition of nonsense words (using the CN/Rep), reading ability (using the WORD test), spelling ability (using 15 age‐appropriate words to spell) and an assessment of the ability to delete phonemes when repeating a word (using the Auditory Analysis Test). Again, the evidence for these outcomes is very uncertain (see Analysis 2.34; Analysis 2.35; Analysis 2.36; Analysis 2.37).
2.34. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 34: Non‐word repetition total score, adjusted OR (long‐term)
2.35. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 35: Reading, WORD test, adjusted OR (long‐term)
2.36. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 36: Spelling, ALSPAC test, adjusted OR (long‐term)
2.37. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 37: Phoneme deletion, adjusted OR (long‐term)
Cognitive development
Maw 1999 assessed cognitive development at nine months (using the Griffiths practical reasoning test) and 18 months (using the WISC‐III short form), but the evidence is very uncertain (Analysis 2.38; Analysis 2.39). Paradise 2007 also assessed cognition (with the Wechsler Abbreviated Scale of Intelligence, and the calculation subset of the Woodcock‐Johnson III Tests of Achievement). No difference was seen between the two groups, but the evidence was very low‐certainty. Some additional data from Paradise 2007 are reported in Table 9.
2.38. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 38: Cognitive development: Griffiths practical reasoning (medium‐term)
2.39. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 39: Cognitive development: IQ (WISC‐III UK short form) adjusted OR (long‐term)
Psychosocial outcomes
Maw 1999 considered a number of behavioural outcomes, assessed with the Richman Behaviour Checklist, which is completed by the child's parents (range 0 to 24, higher scores represent worse behaviour, and a threshold of ≥ 10 has been suggested as a cut‐off to determine behavioural problems). At medium‐term follow‐up, scores were very slightly lower (better) for those who received early ventilation tubes (mean difference ‐0.65, 95% CI ‐1.85 to 0.55; 1 study, 150 participants; Analysis 2.40) and the risk ratio for behavioural problems was lower for those receiving early ventilation tubes (RR 0.63, 95% CI 0.42 to 0.96; 1 study, 150 participants; Analysis 2.41). However, the evidence is very low certainty and adjustment for potential confounding factors (including hearing level) resulted in a change in the direction of the effect. The adjusted odds ratio was 1.16 for behavioural problems in those who received early ventilation tubes, although the confidence intervals were extremely wide and the evidence is very uncertain (95% CI 0.27 to 4.90; 1 study, 150 participants; Analysis 2.42; very low‐certainty evidence).
2.40. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 40: Behaviour, Richman score (medium‐term)
2.41. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 41: Behaviour, Richman score, dichotomised (medium‐term)
2.42. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 42: Behaviour, Richman score, adjusted OR (medium‐term)
At longer‐term follow‐up (18 months), behavioural scores were very slightly worse for those who received early ventilation tubes, but the difference between the groups may be trivial, and the evidence is very uncertain (1 study, 123 participants; Analysis 2.43; Analysis 2.44; Analysis 2.45). Similar results were seen in Paradise 2007 when rating behaviour, social skills and continuous performance tests (see Analysis 2.52; Analysis 2.53; Analysis 2.54 and Table 9).
2.43. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 43: Behaviour, Richman score (long‐term)
2.44. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 44: Behaviour, Richman score, dichotomised (long‐term)
2.45. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 45: Behaviour: SDQ teacher report, total, adjusted OR (long‐term)
2.52. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 52: Attention, impulsivity and psychosocial function, long‐term (1): disruptive behaviour disorders, child behaviour and impairment rating
2.53. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 53: Attention, impulsivity and psychosocial function, long‐term (2): social skills
2.54. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 54: Attention, impulsivity and psychosocial function, long‐term: Visual and auditory continuous performance
Interaction between parents and children was also assessed in Rovers 2000, and a trivial difference was seen in outcomes between the two groups, but the evidence is very uncertain (see Analysis 2.46; Analysis 2.47).
2.46. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 46: Parent‐child interaction: Erickson child scale (medium‐term)
2.47. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 47: Parent‐child interaction: Erickson parent scale (medium‐term)
Generic health‐related quality of life
One study assessed quality of life using the TAIQOL questionnaire (Rovers 2000). A trivial difference was found between the groups across all domains studied, but the evidence is very uncertain (see Analysis 2.48).
2.48. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 48: Generic health‐related quality of life: TAIQOL (medium‐term)
Parental stress
A single study measured this outcome, using the Parenting Stress Index, but there was no evidence of a difference in parental stress between the two groups after long‐term follow‐up and the evidence is very uncertain (mean difference 0, 95% CI ‐4.12 to 4.12; 1 study, 383 participants; Analysis 2.49; very low‐certainty evidence).
2.49. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 49: Parental stress, Parental Stress Index, short form (long‐term)
Other outcomes
No data were identified regarding listening skills, vestibular function or the number of doctor‐diagnosed episodes of acute otitis media.
Comparison 3: Ventilation tubes versus hearing aids
No studies were identified that assessed this comparison.
Comparison 4: Ventilation tubes versus non‐surgical treatment
This comparison included a single study that compared ventilation tubes to antibiotics (Bernard 1991).
Hearing
Final hearing threshold
At short‐term follow‐up (two months) the mean final hearing threshold was ‐9 dB HL lower (better) for those who received ventilation tubes, as compared to medical treatment, but the evidence is very uncertain (95% CI ‐12.61 to ‐5.39; 1 study, 125 participants; Analysis 3.1; very low‐certainty evidence). At medium‐term follow‐up (four months), the mean difference was ‐5.98 dB HL lower (95% CI ‐9.21 to ‐2.75; 1 study, 125 participants; Analysis 3.2; very low‐certainty evidence).
3.1. Analysis.

Comparison 3: Ventilation tubes versus non‐surgical treatment, Outcome 1: Mean final hearing threshold (short‐term)
3.2. Analysis.

Comparison 3: Ventilation tubes versus non‐surgical treatment, Outcome 2: Mean final hearing threshold (medium‐term)
Disease‐specific quality of life
No data were available for this outcome.
Adverse event ‐ persistent perforation
Bernard 1991 reported that none of the 60 children who received ventilation tubes developed persistent perforation at 18 months of follow‐up.
Presence/persistence of OME
No data were available for this outcome.
Adverse events
The prevalence of most adverse events was only reported for those who had received ventilation tubes. Data on adverse events reported in this study are presented in Table 7 and Table 8, and Appendix 3.
Number of doctor‐diagnosed acute otitis media (AOM) episodes
At medium‐term follow‐up, the number of doctor‐diagnosed episodes of AOM was lower in those who received ventilation tubes, with a mean difference of ‐0.23 episodes fewer, but the evidence is very uncertain (95% CI ‐0.42 to ‐0.04; 1 study, 125 participants; Analysis 3.4; very low‐certainty evidence). The difference between the two groups was trivial after long‐term follow‐up (mean difference ‐0.05 episodes fewer, 95% CI ‐0.31 to 0.21; 1 study, 125 participants; Analysis 3.5; very low‐certainty evidence).
3.4. Analysis.

Comparison 3: Ventilation tubes versus non‐surgical treatment, Outcome 4: Number of doctor‐diagnosed AOM episodes (medium‐term)
3.5. Analysis.

Comparison 3: Ventilation tubes versus non‐surgical treatment, Outcome 5: Number of doctor‐diagnosed episodes of AOM (long‐term)
Other outcomes
No data were identified regarding receptive language skills, expressive language skills, cognitive development, psychosocial outcomes, listening skills, generic health‐related quality of life, parental stress or vestibular function.
Comparison 5: Ventilation tubes versus myringotomy alone
We identified nine studies for this comparison, but they used different techniques to carry out myringotomy (D'Eredita 2006; Gates 1989; Koopman 2004; Popova 2010; Ruckley 1988; Sujatha 2015; Tao 2020; To 1984; Yousaf 2016).
Hearing
Return to normal hearing
Two studies assessed the proportion of participants in whom hearing returned to normal (at six months and one year of follow‐up). The risk ratio for return to normal hearing was 1.22 for those who received ventilation tubes compared to laser myringotomy (95% CI 0.59 to 2.53; 74% versus 64%; 2 studies, 120 participants but data reported per ear; I2 = 95%; Analysis 4.1; very low‐certainty evidence). Sensitivity analysis with the use of different intracluster correlation coefficients made very little difference to the overall estimates (see Analysis 7.1; Analysis 7.2).
4.1. Analysis.

Comparison 4: Ventilation tubes versus myringotomy, Outcome 1: Hearing returned to normal: VT versus laser myringotomy (medium‐term)
7.1. Analysis.

Comparison 7: Sensitivity analyses: Ventilation tubes versus myringotomy, Outcome 1: Sensitivity analysis: Hearing returned to normal: VT versus laser myringotomy (medium‐term); ICC = 1.0
7.2. Analysis.

Comparison 7: Sensitivity analyses: Ventilation tubes versus myringotomy, Outcome 2: Sensitivity analysis: Hearing returned to normal: VT versus laser myringotomy (medium‐term); ICC = zero
Final hearing threshold
≤ 3 months follow‐up
Two studies assessed this outcome in the short term, but we did not pool the results as one study reported the number of ears affected, and one reported the number of children affected. Both found a trivial difference between the groups in final hearing threshold at short‐term follow‐up (mean difference for those receiving ventilation tubes 0.2 dB HL higher for one study (95% CI 1.71 to 2.11; 156 participants) and 4.3 dB HL lower for the other study (95% CI ‐8.55 to ‐0.05; 108 participants)) (Analysis 4.2; Analysis 4.3 and see sensitivity analyses Analysis 7.5; Analysis 7.6), but the evidence is very uncertain.
4.2. Analysis.

Comparison 4: Ventilation tubes versus myringotomy, Outcome 2: Mean final hearing threshold, randomised by child (short‐term). Adjusted for non‐independence of within‐individual measurements; assumed ICC of 0.5
4.3. Analysis.

Comparison 4: Ventilation tubes versus myringotomy, Outcome 3: Mean final hearing threshold, randomised by ear (short‐term)
7.5. Analysis.

Comparison 7: Sensitivity analyses: Ventilation tubes versus myringotomy, Outcome 5: Sensitivity analysis: Mean final hearing threshold (medium‐term); ICC = 1.0
7.6. Analysis.

Comparison 7: Sensitivity analyses: Ventilation tubes versus myringotomy, Outcome 6: Sensitivity analysis: Mean final hearing threshold (medium‐term); ICC = zero
3 to 12 months follow‐up
One study also assessed hearing at 12 months of follow‐up and, again, found a trivial difference between the groups, but the evidence is very uncertain (MD 0.80 dB HL, 95% CI ‐0.87 to 2.47; 1 study, 156 participants; Analysis 4.4; very low‐certainty evidence).
4.4. Analysis.

Comparison 4: Ventilation tubes versus myringotomy, Outcome 4: Mean final hearing threshold (medium‐term)
Disease‐specific quality of life
No data were available for this outcome.
Adverse event: persistent perforation
Three studies clearly reported the rate of persistent perforation in both groups of participants, allowing a comparison to be made between the groups. After three months, Yousaf 2016 identified one perforation in the ears that received laser myringotomy, and two in the ears that received ventilation tubes. Accounting for the potential for correlation between ears of the same individual gave a risk ratio of 1.00 (95% CI 0.06 to 15.56; 1 study, 90 ears; Analysis 4.5; moderate‐certainty evidence), although if the correlation between ears was less than the risk ratio would be higher (see Analysis 7.7; Analysis 7.8).
4.5. Analysis.

Comparison 4: Ventilation tubes versus myringotomy, Outcome 5: Adverse event: persistent perforation (medium‐term)
7.7. Analysis.

Comparison 7: Sensitivity analyses: Ventilation tubes versus myringotomy, Outcome 7: Sensitivity analysis: Persistent perforation (medium‐term); ICC = 1.0
7.8. Analysis.

Comparison 7: Sensitivity analyses: Ventilation tubes versus myringotomy, Outcome 8: Sensitivity analysis: Persistent perforation (medium‐term); ICC = zero
There appeared to be an increased risk of perforation with ventilation tubes compared with cold‐steel myringotomy at 12 months of follow‐up, but the confidence intervals were extremely wide and the evidence is very uncertain (Peto OR 8.09, 95% CI 1.78 to 36.79; 2 studies, 208 participants; I2 = 0%; Analysis 4.6; very low‐certainty evidence). In addition, Gates 1989 reported that six children had a persistent perforation of the tympanic membrane: three in the myringotomy group and three who received ventilation tubes. However, the number assessed in each group was not reported, therefore we could not include these data in the meta‐analysis.
4.6. Analysis.

Comparison 4: Ventilation tubes versus myringotomy, Outcome 6: Adverse event: persistent perforation cold‐steel myringotomy (medium‐term)
In D'Eredita 2006, one child in the ventilation tubes group required “myringoplasty to close a persistent TM perforation after 1 year”. No data were reported for the myringotomy group, but it is unclear whether this is because no persistent perforations occurred, or this outcome was not assessed in the group.
Presence/persistence of OME
≤ 3 months follow‐up
Two studies assessed the persistence of OME in the short term but used different types of myringotomy. Yousaf 2016 compared ventilation tubes to laser myringotomy and found a risk ratio of 1.40 for persistence of OME in those receiving ventilation tubes, although the confidence interval was wide and the evidence is very uncertain (95% CI 0.48 to 4.12; 14% versus 10%; 1 study, 90 participants; Analysis 4.7; very low‐certainty evidence). Sensitivity analyses to account for the correlation between ears made little difference to the overall estimates (Analysis 7.9; Analysis 7.10).
4.7. Analysis.

Comparison 4: Ventilation tubes versus myringotomy, Outcome 7: Persistence of OME: VT versus laser myringotomy (short‐term)
7.9. Analysis.

Comparison 7: Sensitivity analyses: Ventilation tubes versus myringotomy, Outcome 9: Sensitivity analysis: Persistence of OME: VT versus laser myringotomy (short‐term); ICC = 1.0
7.10. Analysis.

Comparison 7: Sensitivity analyses: Ventilation tubes versus myringotomy, Outcome 10: Sensitivity analysis: Persistence of OME: VT versus laser myringotomy (short‐term); ICC = zero
Ruckley 1988 compared ventilation tubes with thermal myringotomy. The result was a Peto OR of 0.11 for persistence of OME in those receiving ventilation tubes (95% CI 0.02 to 0.53; 0% versus 19%; 1 study, 72 participants; Analysis 4.8; very low‐certainty evidence).
4.8. Analysis.

Comparison 4: Ventilation tubes versus myringotomy, Outcome 8: Persistence of OME: VT versus thermal myringotomy, randomised by ear (short‐term)
3 to 12 months follow‐up
Three studies considered persistence of OME at medium‐term follow‐up. The point estimate for each study showed a benefit for ventilation tubes as compared to myringotomy; however, the confidence intervals were very wide, and the evidence is all of very low certainty:
Ventilation tubes versus cold‐steel myringotomy: RR 0.69 (95% CI 0.20 to 2.36; 1 study, 78 participants; Analysis 4.9; very low‐certainty evidence).
Ventilation tubes versus laser myringotomy: RR 0.32 (95% CI 0.15 to 0.67; 1 study, 90 participants; Analysis 4.10; very low‐certainty evidence). Sensitivity analysis to account for correlation between ears of the same individual made little difference to the overall effect estimates (Analysis 7.11; Analysis 7.12).
Ventilation tubes versus laser myringotomy, randomised by ear: OR 0.27 (95% CI 0.19 to 0.38; 1 study, 272 ears; Analysis 4.11; very low‐certainty evidence). Sensitivity analysis to account for correlation between ears of the same individual made little difference to the overall effect estimates (Analysis 7.13; Analysis 7.14).
4.9. Analysis.

Comparison 4: Ventilation tubes versus myringotomy, Outcome 9: Persistence of OME: VT versus cold‐steel myringotomy (medium‐term)
4.10. Analysis.

Comparison 4: Ventilation tubes versus myringotomy, Outcome 10: Persistence of OME: VT versus laser myringotomy (medium‐term)
7.11. Analysis.

Comparison 7: Sensitivity analyses: Ventilation tubes versus myringotomy, Outcome 11: Sensitivity analysis: Persistence of OME: VT versus laser myringotomy (medium‐term); ICC = 1.0
7.12. Analysis.

Comparison 7: Sensitivity analyses: Ventilation tubes versus myringotomy, Outcome 12: Sensitivity analysis: Persistence of OME: VT versus laser myringotomy (medium‐term); ICC = zero
4.11. Analysis.

Comparison 4: Ventilation tubes versus myringotomy, Outcome 11: Persistence of OME: VT versus laser myringotomy, randomised by ear (medium‐term)
7.13. Analysis.

Comparison 7: Sensitivity analyses: Ventilation tubes versus myringotomy, Outcome 13: Sensitivity analysis: Persistence of OME: VT versus laser myringotomy, randomised by ear (medium‐term); CC = 0.3
7.14. Analysis.

Comparison 7: Sensitivity analyses: Ventilation tubes versus myringotomy, Outcome 14: Sensitivity analysis: Persistence of OME: VT versus laser myringotomy, randomised by ear (medium‐term); CC = 0.7
One study assessed persistence of OME slightly differently, considering the number of days before the recurrence of OME in each group. Gates 1989 reported a mean difference of 173.88 days longer before recurrence in those who received ventilation tubes as compared to myringotomy (95% CI 150.19 to 197.56; 1 study, 389 participants; Analysis 4.12; very low‐certainty evidence).
4.12. Analysis.

Comparison 4: Ventilation tubes versus myringotomy, Outcome 12: Persistence of OME: mean days to first recurrence
Long‐term follow‐up (> 1 year)
One study considered persistence of OME in the long term and found little difference between the two groups after two years of follow‐up (RR 0.97, 95% CI 0.90 to 1.05; 83% versus 85%; 1 study, 491 participants; Analysis 4.13; very low‐certainty evidence).
4.13. Analysis.

Comparison 4: Ventilation tubes versus myringotomy, Outcome 13: Persistence of OME (long‐term)
Tao 2020 also reported recurrence of OME at 3, 6 and 12 months. However, they also describe additional "conservative treatment" received by these patients. It is not clear what this conservative treatment is, and whether it was balanced across the two groups, so we have not presented these findings.
Adverse events
Details are reported in Appendix 3, Table 7 and Table 8.
Doctor‐diagnosed episodes of acute otitis media
Only one study assessed the occurrence of acute otitis media during the follow‐up period. This was reported as the proportion of participants who experienced a specific number of episodes over the course of 12‐month follow‐up. The evidence is all of very low certainty.
No episodes of AOM for those receiving ventilation tubes compared to myringotomy: RR 0.95 (95% CI 0.73 to 1.25; 1 study, 78 participants; Analysis 4.15).
One episode of AOM for those receiving ventilation tubes compared to myringotomy: RR 1.00 (95% CI 0.37 to 2.71; 1 study, 78 participants; Analysis 4.15).
Two episodes of AOM for those receiving ventilation tubes compared to myringotomy: RR 0.86 (95% CI 0.18 to 3.99; 1 study, 78 participants; Analysis 4.15).
Three episodes of AOM for those receiving ventilation tubes compared to myringotomy: Peto OR 6.41 (95% CI 0.13 to 326.59; 1 study, 78 participants; Analysis 4.16).
Four or more episodes of AOM for those receiving ventilation tubes compared to myringotomy: Peto OR 6.41 (95% CI 0.13 to 326.59; 1 study, 78 participants; Analysis 4.16).
4.15. Analysis.

Comparison 4: Ventilation tubes versus myringotomy, Outcome 15: Zero, one or two episodes of AOM in 12 months
4.16. Analysis.

Comparison 4: Ventilation tubes versus myringotomy, Outcome 16: Three or more episodes of AOM in 12 months
Other outcomes
No data were identified regarding cognitive development, psychosocial outcomes, listening skills, generic health‐related quality of life, parental stress or vestibular function.
Sensitivity analysis
The results of all sensitivity analyses performed are presented in Table 10.
6. Sensitivity analyses.
| Outcome | Main analysis result (95% CI) | Sensitivity analysis | Sensitivity analysis result (95% CI) |
| Ventilation tubes versus no treatment | |||
| Return to normal hearing | |||
| 1.1 Return to normal hearing, randomised by ear (medium‐term) | OR 1.13 (0.46 to 2.74) | Correlation coefficient 0.3 instead of 0.5 | OR 1.13 (0.46 to 2.74) |
| 1.1 Return to normal hearing, randomised by ear (medium‐term) | OR 1.13 (0.46 to 2.74) | Correlation coefficient 0.7 instead of 0.5 | OR 1.13 (0.47 to 2.75) |
| 1.1 Return to normal hearing, randomised by ear (medium‐term) | OR 1.13 (0.46 to 2.74) | Normal hearing defined as < 25 dB HL instead of < 15 dB HL | OR 1.00 (0.57 to 1.76) |
| Final hearing threshold | |||
| 1.2 Mean final hearing threshold, randomised by ear (medium‐term) | MD ‐3.47 (‐9.97 to 3.03) | Correlation coefficient 0.3 instead of 0.5 | MD ‐3.47 (‐10.01 to 3.06) |
| 1.2 Mean final hearing threshold, randomised by ear (medium‐term) | MD ‐3.47 (‐9.97 to 3.03) | Correlation coefficient 0.7 instead of 0.5 | MD ‐3.49 (‐10.37 to 3.38) |
| 1.2 Mean final hearing threshold, randomised by ear (medium‐term) | MD ‐3.47 (‐9.97 to 3.03) | Fixed‐effect model | MD ‐3.31 (‐5.09 to ‐1.54) |
| 1.2 Mean final hearing threshold, randomised by ear (medium‐term) | MD ‐3.47 (‐9.97 to 3.03) | Exclusion of studies with concerns over trustworthiness | MD ‐9.90 (‐13.00 to ‐6.80) |
| Change in hearing threshold from baseline | |||
| 1.3 Change in hearing threshold from baseline, randomised by ear (medium‐term) | MD ‐0.16 (‐3.28 to 2.97) | Correlation coefficient 0.3 instead of 0.5 | MD ‐0.10 (‐3.22 to 3.01) |
| 1.3 Change in hearing threshold from baseline, randomised by ear (medium‐term) | MD ‐0.16 (‐3.28 to 2.97) | Correlation coefficient 0.7 instead of 0.5 | MD ‐0.21 (‐3.34 to 2.92) |
| Persistent tympanic membrane perforation | |||
| 1.4 Adverse event: perforation/retraction, randomised by ear (medium‐term) | OR 0.85 (0.38 to 1.91) | Correlation coefficient 0.3 instead of 0.5 | OR 0.85 (0.33 to 2.21) |
| 1.4 Adverse event: perforation/retraction, randomised by ear (medium‐term) | OR 0.85 (0.38 to 1.91) | Correlation coefficient 0.7 instead of 0.5 | OR 0.91 (0.45 to 1.86) |
| 1.4 Adverse event: perforation/retraction, randomised by ear (medium‐term) | OR 0.85 (0.38 to 1.91) | Fixed‐effect model | OR 0.85 (0.38 to 1.91) |
| Persistence of OME | |||
| 1.6 Persistence of OME: randomised by child, analysed by ear (medium‐term) | RR 0.30 (0.14 to 0.65) | Intracluster correlation of 1.0, instead of 0.5 | RR 0.27 (0.11 to 0.70) |
| 1.6 Persistence of OME: randomised by child, analysed by ear (medium‐term) | RR 0.30 (0.14 to 0.65) | Intracluster correlation of 0, instead of 0.5 | RR 0.30 (0.16 to 0.56) |
| 1.7 Persistence of OME: randomised by ear (medium‐term) | OR 0.66 (0.24 to 1.85) | Correlation coefficient 0.3 instead of 0.5 | OR 0.66 (0.24 to 1.83) |
| 1.7 Persistence of OME: randomised by ear (medium‐term) | OR 0.66 (0.24 to 1.85) | Correlation coefficient 0.7 instead of 0.5 | OR 0.66 (0.24 to 1.83) |
| 1.7 Persistence of OME: randomised by ear (medium‐term) | OR 0.66 (0.24 to 1.85) | Fixed‐effect model | OR 0.68 (0.42 to 1.09) |
| Ventilation tubes versus watchful waiting (treatment later if required) | |||
| Final hearing threshold | |||
| 2.3 Mean final hearing threshold (air conduction), randomised by child (medium‐term) | MD ‐1.89 (‐7.32 to 3.54) | Fixed‐effect model | MD ‐0.74 (‐3.08 to 1.59) |
| 2.4 Mean final hearing threshold (air‐bone gap), randomised by child, analysed by ear (medium‐term) | MD ‐1.18 (‐2.86 to 0.50) | Intracluster correlation of 1.0, instead of 0.5 | MD ‐1.18 (‐3.08 to 0.72) |
| 2.4 Mean final hearing threshold (air‐bone gap), randomised by child, analysed by ear (medium‐term) | MD ‐1.18 (‐2.86 to 0.50) | Intracluster correlation of 0, instead of 0.5 | MD ‐1.18 (‐2.58 to 0.22) |
| 2.5 Mean final hearing threshold, randomised by child (long‐term) | MD 0.36 (‐0.41 to 1.13) | Correlation coefficient 0.3 instead of 0.5 | MD 0.37 (‐0.37 to 1.11) |
| 2.5 Mean final hearing threshold, randomised by child (long‐term) | MD 0.36 (‐0.41 to 1.13) | Correlation coefficient 0.7 instead of 0.5 | MD 0.35 (‐0.45 to 1.16) |
| 2.5 Mean final hearing threshold, randomised by child (long‐term) | MD 0.36 (‐0.41 to 1.13) | Fixed‐effect model | MD 0.36 (‐0.41 to 1.13) |
| Persistent tympanic membrane perforation | |||
| 2.10 Adverse event: persistent perforation, randomised by child (long‐term) | RR 3.65 (0.41 to 32.38) | Intracluster correlation of 1.0, instead of 0.5 | RR 2.73 (0.29 to 25.97) |
| 2.10 Adverse event: persistent perforation, randomised by child (long‐term) | RR 3.65 (0.41 to 32.38) | Intracluster correlation of 0, instead of 0.5 | RR 2.73 (0.56 to 13.43) |
| Persistence of OME | |||
| 2.11 Presence/persistence of OME, randomised by child, measured by otoscopy (medium‐term) | RR 0.39 (0.09 to 1.72) | Intracluster correlation of 1.0, instead of 0.5 | RR 0.49 (0.11 to 2.22) |
| 2.11 Presence/persistence of OME, randomised by child, measured by otoscopy (medium‐term) | RR 0.39 (0.09 to 1.72) | Intracluster correlation of 0, instead of 0.5 | RR 0.40 (0.12 to 1.34) |
| 2.14 Presence/persistence of OME, randomised by child (long‐term) | RR 1.21 (0.84 to 1.74) | Fixed‐effect model | RR 1.22 (0.84 to 1.77) |
| Adverse events | |||
| 2.16 Adverse event: tympanosclerosis (long‐term) | RR 0.91 (0.33 to 2.55) | Intracluster correlation of 1.0, instead of 0.5 | RR 0.91 (0.27 to 3.08) |
| 2.16 Adverse event: tympanosclerosis (long‐term) | RR 0.91 (0.33 to 2.55) | Intracluster correlation of 0, instead of 0.5 | RR 0.83 (0.36 to 1.92) |
| 2.17 Adverse event: fibrosis (long‐term) | RR 0.61 (0.10 to 3.60) | Intracluster correlation of 1.0, instead of 0.5 | RR 0.46 (0.04 to 4.97) |
| 2.17 Adverse event: fibrosis (long‐term) | RR 0.61 (0.10 to 3.60) | Intracluster correlation of 0, instead of 0.5 | RR 0.68 (0.15 to 3.03) |
| 2.18 Adverse event: segmental atrophy (long‐term) | RR 2.83 (1.81 to 4.43) | Intracluster correlation of 1.0, instead of 0.5 | RR 2.92 (1.72 to 4.96) |
| 2.18 Adverse event: segmental atrophy (long‐term) | RR 2.83 (1.81 to 4.43) | Intracluster correlation of 0, instead of 0.5 | RR 2.85 (1.97 to 4.13) |
| 2.19 Adverse event: retraction pocket with other abnormality (long‐term) | RR 0.91 (0.06 to 14.41) | Intracluster correlation of 1.0, instead of 0.5 | RR 0.91 (0.06 to 14.43) |
| 2.19 Adverse event: retraction pocket with other abnormality (long‐term) | RR 0.91 (0.06 to 14.41) | Intracluster correlation of 0, instead of 0.5 | RR 0.91 (0.06 to 14.64) |
| Psychosocial outcomes | |||
| 2.46 Parent‐child interaction: Erickson child scale (medium‐term) | MD ‐0.34 (‐0.56 to ‐0.12) | Correlation coefficient 0.3 instead of 0.5 between five domains assessed | MD ‐0.34 (‐0.53 to ‐0.15) |
| 2.46 Parent‐child interaction: Erickson child scale (medium‐term) | MD ‐0.34 (‐0.56 to ‐0.12) | Correlation coefficient 0.7 instead of 0.5 between five domains assessed | MD ‐0.34 (‐0.58 to ‐0.10) |
| 2.47 Parent‐child interaction: Erickson parent scale (medium‐term) | MD ‐0.42 (‐0.67 to ‐0.17) | Correlation coefficient 0.3 instead of 0.5 between five domains assessed | MD ‐0.42 (‐0.64 to ‐0.20) |
| 2.47 Parent‐child interaction: Erickson parent scale (medium‐term) | MD ‐0.42 (‐0.67 to ‐0.17) | Correlation coefficient 0.7 instead of 0.5 between five domains assessed | MD ‐0.42 (‐0.70 to ‐0.14) |
| Ventilation tubes versus myringotomy | |||
| Return to normal hearing | |||
| 4.1 Hearing returned to normal: VT versus laser myringotomy (medium‐term) | RR 1.22 (0.59 to 2.53) | Intracluster correlation of 1.0, instead of 0.5 | RR 1.21 (0.59 to 2.48) |
| 4.1 Hearing returned to normal: VT versus laser myringotomy (medium‐term) | RR 1.22 (0.59 to 2.53) | Intracluster correlation of 0, instead of 0.5 | RR 1.22 (0.62 to 2.40) |
| 4.1 Hearing returned to normal: VT versus laser myringotomy (medium‐term) | RR 1.22 (0.59 to 2.53) | Fixed‐effect model | RR 1.33 (1.09 to 1.63) |
| 4.1 Hearing returned to normal: VT versus laser myringotomy (medium‐term) | RR 1.22 (0.59 to 2.53) | Exclusion of studies at high risk of bias | RR 1.00 (0.88 to 1.13) |
| Final hearing threshold | |||
| 4.2 Mean final hearing threshold, randomised by child (short‐term) | RR 0.20 (‐2.13 to 2.53) | Intracluster correlation of 1.0, instead of 0.5 | RR 0.20 (‐2.50 to 2.90) |
| 4.2 Mean final hearing threshold, randomised by child (short‐term) | RR 0.20 (‐2.13 to 2.53) | Intracluster correlation of 0, instead of 0.5 | RR 0.20 (‐1.71 to 2.11) |
| 4.4 Mean final hearing threshold (medium‐term, pure tone audiometry) | MD 0.80 (‐0.87 to 2.47) | Intracluster correlation of 1.0, instead of 0.5 | MD 0.80 (‐1.13 to 2.73) |
| 4.4 Mean final hearing threshold (medium‐term, pure tone audiometry) | MD 0.80 (‐0.87 to 2.47) | Intracluster correlation of 0, instead of 0.5 | MD 0.80 (‐0.57 to 2.17) |
| Persistent tympanic membrane perforation | |||
| 4.5 Adverse event: persistent perforation (medium‐term) | RR 1.00 (0.06 to 15.56) | Intracluster correlation of 1.0, instead of 0.5 | RR 1.00 (0.06 to 15.45) |
| 4.5 Adverse event: persistent perforation (medium‐term) | RR 1.00 (0.06 to 15.56) | Intracluster correlation of 0, instead of 0.5 | RR 2.00 (0.19 to 21.54) |
| 4.6 Adverse event: persistent perforation cold‐steel myringotomy (medium‐term) | Peto OR 8.09 (1.78 to 36.79) | Exclusion of studies with concerns over trustworthiness | Peto OR 7.39 (0.15 to 372.38) |
| Persistence of OME | |||
| 4.7 Persistence of OME: VT versus laser myringotomy (short‐term) | RR 1.40 (0.48 to 4.12) | Intracluster correlation of 1.0, instead of 0.5 | RR 1.50 (0.46 to 4.92) |
| 4.7 Persistence of OME: VT versus laser myringotomy (short‐term) | RR 1.40 (0.48 to 4.12) | Intracluster correlation of 0, instead of 0.5 | RR 1.43 (0.58 to 3.53) |
| 4.10 Persistence of OME: VT versus laser myringotomy (medium‐term) | RR 0.32 (0.16 to 0.64) | Intracluster correlation of 1.0, instead of 0.5 | RR 0.35 (0.17 to 0.74) |
| 4.10 Persistence of OME: VT versus laser myringotomy (medium‐term) | RR 0.32 (0.16 to 0.64) | Intracluster correlation of 0, instead of 0.5 | RR 0.33 (0.18 to 0.60) |
| 4.11 Persistence of OME: VT versus laser myringotomy, randomised by ear (medium‐term) | OR 0.27 (0.19 to 0.38) | Correlation coefficient 0.3 instead of 0.5 | OR 0.27 (0.18 to 0.42) |
| 4.11 Persistence of OME: VT versus laser myringotomy, randomised by ear (medium‐term) | OR 0.27 (0.19 to 0.38) | Correlation coefficient 0.7 instead of 0.5 | OR 0.27 (0.21 to 0.36) |
| Adverse events | |||
| 4.20 Adverse event: retraction of TM: VT versus laser myringotomy (medium‐term) | RR 2.67 (0.75 to 9.48) | Intracluster correlation of 1.0, instead of 0.5 | RR 3.50 (0.77 to 15.85) |
| 4.20 Adverse event: retraction of TM: VT versus laser myringotomy (medium‐term) | RR 2.67 (0.75 to 9.48) | Intracluster correlation of 0, instead of 0.5 | RR 2.75 (0.92 to 8.21) |
| 4.22 Adverse event: otorrhoea: VT versus laser myringotomy (medium‐term) | RR 4.00 (0.46 to 34.57) | Intracluster correlation of 1.0, instead of 0.5 | RR 3.00 (0.33 to 27.66) |
| 4.22 Adverse event: otorrhoea: VT versus laser myringotomy (medium‐term) | RR 4.00 (0.46 to 34.57) | Intracluster correlation of 0, instead of 0.5 | RR 2.50 (0.50 to 12.44) |
CI: confidence interval; MD: mean difference; OME: otitis media with effusion; OR: odds ratio; RR: risk ratio; TM: tympanic membrane; VT: ventilation tube
Discussion
There are some certainties in otitis media with effusion (OME). Firstly, this is a fluctuating condition with a high rate of spontaneous resolution, but also a high rate of recurrence over time. The impact of OME on any individual child is very variable, and consequently the need for treatment differs. So far, attempts to understand the condition better with prognostic studies have been unsuccessful.
In undertaking this review and using the GRADE approach to assess the certainty of evidence according to Cochrane methodology (Higgins 2021), we have encountered a high degree of uncertainty ‐ the GRADE approach not only considers methodological rigour of the studies but also precision of the effect estimates, applicability of the results and consistency in estimates between different studies. Despite the large number of studies included in the review, limited pooling of data was possible. Relatively small numbers of participants were included in many analyses, resulting in wide confidence intervals for measures of effect.
There are still key questions that remain unanswered in this common disease. Resolving these uncertainties is absolutely critical to enable research in this area to progress.
Firstly, we need to identify which children will undergo spontaneous resolution of OME, through a better understanding of prognostic factors in the disease. This would allow treatments to be targeted to those children in whom OME is more likely to be persistent, and impact language and development. Many of the studies included in this review recruited a variety of children ‐ some with unilateral OME, and some with mild hearing loss. It is possible that these children are less likely to benefit from any intervention to treat OME, as the disease may have little impact on their development and quality of life. Including these children in trials may result in an under‐estimate of the efficacy of the intervention, and bias the overall results towards the null.
In addition, although our primary outcome measure was hearing, we are aware that this is not the only important factor in this disease. Children with identical levels of hearing loss from OME may have very different outcomes in terms of the impact of the disease on development and quality of life. Again, a clearer understanding of the disease process and different subgroups of children with OME would help to identify those children who are at risk of poor long‐term outcomes.
Summary of main results
All the evidence identified in this review was either low‐ or very low‐certainty, showing that we have little confidence in the overall estimates of effect.
Ventilation tubes compared to no treatment
There were very few trials that assessed this comparison, as it does not reflect routine clinical practice where patients would be offered either immediate surgery or a period of watchful waiting. After 12 months, there appeared to be little to no difference in the proportion of children whose hearing returned to normal with or without ventilation tubes. The mean difference in hearing threshold was also small, although we have concerns about the use of mean hearing thresholds to assess hearing in this context (see below). Persistence of OME appeared slightly lower after six months follow‐up for those who received ventilation tubes, but the evidence was very uncertain after one year. Little difference was seen between the two groups for receptive and expressive language skills. Very few data on adverse events were available. See also Table 1.
Early ventilation tubes compared to watchful waiting
After long‐term follow‐up (> 1 year), there was little to no difference in the proportion of children whose hearing had returned to normal. When final hearing threshold was assessed, there may be a benefit to ventilation tubes at short‐term (three months) follow‐up, but this reduced after longer‐term follow‐up, and the overall certainty of evidence is very low. This may be due to the high proportion of children in the control group who underwent surgery during the follow‐up period. Persistence of OME appeared to be reduced after six to nine months for those who received ventilation tubes, but the evidence is very uncertain, and this effect was not seen after longer‐term follow‐up. Very limited data on adverse events were available. Evidence for expressive language skills, receptive language skills, cognitive development, psychosocial outcomes, parental stress and generic quality of life is all of very low certainty, with little to no difference observed between the two groups. See also Table 2.
Ventilation tubes versus non‐surgical treatment
A single study compared ventilation tubes to long‐term antibiotic treatment. The mean final hearing threshold was slightly better for those who received ventilation tubes, but the evidence is very uncertain. Very few data were reported for adverse events or other pre‐defined outcome measures. See Table 3.
Ventilation tubes compared to myringotomy
There may be a slight increase in the proportion of children whose hearing returned to normal with ventilation tubes (as compared to myringotomy) but the evidence is very uncertain. Little to no difference in the mean final hearing threshold was seen but, as described below, we are uncertain if this method of assessing hearing is appropriate for this condition. The rate of persistent tympanic membrane perforation is probably increased with ventilation tubes as compared to myringotomy. After medium‐term follow‐up, ventilation tubes may slightly reduce the rate of persistent OME, but the evidence is again very uncertain, and this effect was not seen at longer‐term follow‐up. Very few data on adverse events were available. See Table 4.
Overall completeness and applicability of evidence
The focus of this review was to summarise the evidence from randomised controlled trials (RCTs). However, in a condition such as OME ‐ with very variable effects on individual children, fluctuating symptoms and little understanding of important prognostic factors ‐ an RCT may not be the preferred study design. The review does not include data from large cohort studies, which have highlighted the fluctuation of symptoms of OME in those both with and without ventilation tubes (Zielhuis 1990).
In keeping with other Cochrane Reviews in this suite, we noted that very few studies reported our preferred outcome measure for hearing ‐ the number of children who returned to normal hearing. We have concerns that assessment of hearing using the mean difference in final hearing threshold (or mean change in hearing threshold) may not be the most appropriate way to assess hearing. OME has a high spontaneous resolution rate. Consequently, we would anticipate that the change in hearing threshold for most children will be similar across the groups, as many children will improve with or without treatment. Therefore, even if a subset of children had substantial benefit from the intervention, the overall mean difference between the two groups would appear to be small. When assessed using the mean difference, the marked benefit seen in a subgroup of participants is ‘diluted’ by the children who get better regardless of treatment. Therefore, an apparently small mean difference between the two groups may actually be consistent with a substantial change in the number of children in whom hearing returns to normal.
Interpreting the results of the comparison between ventilation tube insertion and watchful waiting is challenging. This situation is commonly encountered in clinical practice, where children, their parents and healthcare professionals may need to decide between immediate insertion of ventilation tubes or a further period of watchful waiting. However, the high rate of ventilation tube insertion in the watchful waiting group means that it is difficult to understand the effect of ventilation tubes. The similarities between the intervention and control groups after long‐term follow‐up may be because of spontaneous improvement in symptoms, but also may be because of the high rate of intervention in the control group. In addition, ventilation tubes become blocked, and will extrude over time, and OME can recur. Comparing the prevalence of OME in those who received and did not receive ventilation tubes therefore becomes more difficult to interpret after longer‐term follow‐up.
The results of this review should be assessed in conjunction with those of the companion Cochrane Review regarding the use of adenoidectomy for OME (MacKeith 2023). It is possible that there are synergistic effects of ventilation tubes and adenoidectomy when treating OME. Many of the studies included in this review provided adenoidectomy as a background intervention to all children. The effect of ventilation tubes on OME may be modified in children who also receive adenoidectomy. For example, if children receiving adenoidectomy already have a high rate of resolution for OME, then any additional benefit of ventilation tubes may not be clearly identified.
It should be noted that almost all the studies included in this review used short‐acting ventilation tubes (such as Shepard, Shah minivent and Donaldson tubes) (Bernard 1991; D'Eredita 2006; Dempster 1993; Gates 1989; Koopman 2004; Maw 1983; Popova 2010; Rach 1991; Rovers 2000; Ruckley 1988; Sujatha 2015; Tao 2020; TARGET 2000; To 1984). Therefore, it is possible that the reduction in benefit for longer‐term follow‐up can be explained by the type of standard (short‐term) ventilation tubes used in the majority of included studies. This may mean that our review findings are not applicable to children treated with other types of tubes. Although we included RCTs of any type of ventilation tube, we did not identify studies that specifically used long‐term ventilation tubes and thus we are unable to comment on the efficacy and safety of the long‐acting tubes. Even within studies that considered standard ventilation tubes, there may be differences in extrusion rate over time, which could impact on their duration of efficacy.
Finally, we aimed to include all children with OME and conduct subgroup analyses to determine if the efficacy and harms of treatment may vary amongst different subgroups, such as children with co‐morbidities (e.g. allergies), children with Down syndrome, or children with cleft palate. However, the majority of studies did not include children with craniofacial syndromes and these pre‐planned subgroup analyses were not pursued. Therefore, it is important to note that the findings of this review may not be applicable to children with craniofacial syndromes, who have a higher risk of OME.
Quality of the evidence
We considered most of the evidence included in this review to be very low‐certainty. This was predominantly due to concerns over the risk of bias in the studies included, particularly the risk of performance and detection bias. However, many studies also had unclear ratings for the risk of selection bias, attrition bias or reporting bias. In addition, many of the studies included relatively few participants, which led to wide confidence intervals and imprecision in the overall effect estimates. We had some concerns regarding indirectness in the evidence. This was sometimes related to the population included ‐ for example, some children did not have a continuous period of OME for three months before enrolment (Paradise 2007). We also had some concerns over one study where a particularly stringent definition of normal hearing (< 15 dB HL) was used (Dempster 1993).
We have included five RCTs that were conducted since the publication of Browning 2010, the previous Cochrane Review on this topic (Elkholy 2021; Popova 2010; Sujatha 2015; Tao 2020; Yousaf 2016). However, despite the availability of additional data, the evidence concerning the effects of ventilation tubes for OME in children remains uncertain. Many of the new trials recruited small numbers of participants and conducted short follow‐up, providing little additional evidence for decision‐makers.
Potential biases in the review process
We have attempted to minimise the potential for bias during the review process by adhering to the Cochrane Handbook for Systematic Reviews of Interventions throughout the conduct of this review. We conducted comprehensive searches and ensured that study selection, data extraction and GRADE assessment were carried out by at least two independent authors, to ensure reproducibility of findings.
We acknowledge that there is little consensus on the definition of 'normal hearing'. Consequently, our selection of a hearing threshold of ≤ 20 dB HL as 'normal' was based on discussion between the author team, review of earlier studies and a pragmatic choice of outcome measure. However, we were as inclusive as possible with this outcome measure, and have included data where the authors provided an alternative definition of normal hearing. If we had rigidly used a definition of ≤ 20 dB HL then the data included in this review would have been even more sparse.
Agreements and disagreements with other studies or reviews
The results of this review are similar to those from the previous Cochrane Review on this topic, which included 10 studies (Browning 2010). At that time, the authors concluded that the effects of ventilation tubes on hearing appear to be small, and reduce after six to nine months. The time with effusion (analogous to our outcome 'persistence of OME') was reduced for those who received ventilation tubes. Again, this benefit was smaller after longer follow‐up.
In accordance with current Cochrane standards, we have now used the GRADE approach to assess the certainty of the evidence; the previous Cochrane Review on this topic pre‐dated the GRADE criteria. This approach means that our conclusions appear less certain than the previous review, but it should be noted that the evidence has not changed, it is simply that we are looking at the data with a new approach.
Authors' conclusions
Implications for practice.
There may be small short‐ and medium‐term improvements in hearing and persistence of otitis media with effusion (OME) with ventilation tubes, but it is unclear whether there are lasting benefits when children are followed up for longer periods of time. There is a risk of complications from surgery, including persistent tympanic membrane perforation. The extent of this risk is unclear but is likely to be small. As part of shared decision‐making with patients around the uncertainty of longer‐term benefits from ventilation tubes, it would be important to highlight that these results may not represent the outcomes when longer‐term ventilation tubes are used, both in terms of benefits and harms.
Most of the studies in this review used short‐acting ventilation tubes (two studies explicitly mentioned the use of long‐acting ventilation tubes), and many studies specifically excluded children with risk factors for OME, such as cleft palate or Down syndrome. Therefore, we do not have any information on the efficacy or safety of longer‐acting ventilation tubes, or the effects of ventilation tubes in children with underlying syndromes or developmental delays. We were unable to carry out our planned subgroup analyses to determine if the effect of ventilation tubes may vary across children of different ages, different levels of hearing loss or with co‐morbidities. These are important considerations for generalisability/applicability that should be kept in mind when discussing treatment options with individual patients and their families/carers.
Implications for research.
This review forms part of a suite of five reviews that consider interventions for otitis media with effusion (OME) (Galbraith 2023; MacKeith 2023; MacKeith 2022; Mulvaney 2023a; Mulvaney 2023b). Here we present implications for research in this field, which are shared across the suite of reviews:
As OME is a fluctuating condition with high rates of resolution and recurrence, and a highly variable impact on children, clinical trials (and, in particular, randomised controlled trials) may not be the research design of choice. Instead, evidence may be better obtained from surgical or clinical registries (for example, see Schmalbach 2021) or prospective cohort studies, with the use of 'big data'. These data sets may also be used to help identify subgroups of children who are at greater risk of persistent disease or long‐term consequences of OME. A clearer understanding of possible subgroups of children is needed to better target interventions to those who need them most, whilst avoiding over‐treatment for those in whom spontaneous resolution is anticipated.
Adverse effects of interventions are important, and should always be assessed. However, randomised controlled trials are also not the best method to consider these, especially when events are rare. Observational studies with longer follow‐up and larger numbers of participants are needed to provide more robust evidence on the frequency of side effects. It is important to note that the protocol, inclusion criteria and search strategy used for this review would have excluded these types of studies. It is therefore possible that evidence of this type may exist. With this in mind, we would advocate a review of observational data, to assess whether evidence regarding longer‐term outcomes and adverse events is already available. This may be particularly important when assessing harms from serious but rare adverse events.
It is encouraging that a core outcome set has been developed in this field (Bruce 2015; Liu 2020). Guidance on how to measure the different outcomes would also be helpful for future research.
Comparison of mean hearing thresholds is widely used in research to assess the impact of different interventions on hearing. However, this outcome measure risks underestimating the potential impact of interventions on hearing. Small changes in mean hearing thresholds may be consistent with a substantial improvement in the number of children whose hearing returns to normal, particularly in a condition with a high spontaneous resolution rate. We would encourage researchers to assess hearing with the proportion of children in whom hearing returns to normal, in preference to mean hearing thresholds.
History
Protocol first published: Issue 3, 2022
Acknowledgements
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to Cochrane ENT (closed in March 2023). The views and opinions expressed herein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
We are grateful to the 20 Cochrane Crowd screeners for screening 2443 records to identify 1130 possible RCTs, and reject 1313 references as not RCTs. We are particularly grateful to Bernardo Costa, Stefanie Rosumeck, Nikolaos Sideris, Susanna Wisniewski, Anna Resolver, Lai Ogunsola, Shammas Mohammed, Sarah Moore, Brian Duncan, Mohammad Aloulou, Ana‐Marija Ljubenković, Vighnesh D, Ahlam Jamal Alhemedi, Neetu Bhadra, Amin Sharifan, Abu Emmil Qawarizmi Bin Abu Sofian, Helen Ramsay, Dinah Amoah, Maike Scherhans and Natalya Clark for screening more than 200 records each.
Editorial and peer reviewer contributions
Cochrane ENT supported the authors in the development of this review. Our grateful thanks to Jenny Bellorini, Managing Editor, and Samantha Cox, Information Specialist, from Cochrane ENT, without whom the development of these reviews would not have been possible.
The following people conducted the editorial process for this review:
Sign‐off Editor (final editorial decision): Richard Rosenfeld, Department of Otolaryngology‐Head and Neck Surgery, State University of New York Downstate Health Sciences University, USA.
Managing Editor (selected peer reviewers, collated peer reviewer comments, provided editorial guidance to authors, edited the article): Joey Kwong, Cochrane Central Editorial Service.
Editorial Assistant (conducted editorial policy checks, supported editorial team): Lisa Wydrzynski, Cochrane Central Editorial Service.
Copy Editor (copy editing and production): Jenny Bellorini, Cochrane Central Production Service.
Peer reviewers (provided comments and recommended an editorial decision): Cyril Page, ENT and Head & Neck Surgery Department, University Hospital of Amiens, France (clinical/content review); Kimberly Luu, University of California San Francisco (clinical/content review); Jessica Scaife, Surgical Intervention Trials Unit, Nuffield Department of Surgical Sciences, University of Oxford (consumer review); Nuala Livingstone, Cochrane Evidence Production and Methods Directorate (methods review); Jo Platt, Cochrane Evidence Production and Methods Directorate (search review).
Appendices
Appendix 1. Search strategies
The search strategies were designed to identify all relevant studies for a suite of reviews on various interventions for otitis media with effusion.
| CENTRAL (CRS) | Cochrane ENT Register (CRS) | MEDLINE (Ovid) |
| 1 MESH DESCRIPTOR Otitis Media with Effusion EXPLODE ALL AND CENTRAL:TARGET 2 ("otitis media" adj6 effusion):AB,EH,KW,KY,MC,MH,TI,TO AND CENTRAL:TARGET 3 (OME):TI,TO AND CENTRAL:TARGET 4 (Secretory otitis media):AB,EH,KW,KY,MC,MH,TI,TO AND CENTRAL:TARGET 5 (Serous otitis media):AB,EH,KW,KY,MC,MH,TI,TO AND CENTRAL:TARGET 6 (Middle‐ear effusion):AB,EH,KW,KY,MC,MH,TI,TO AND CENTRAL:TARGET 7 (glue ear):AB,EH,KW,KY,MC,MH,TI,TO AND CENTRAL:TARGET 8 (middle‐ear perfusion):AB,EH,KW,KY,MC,MH,TI,TO AND CENTRAL:TARGET 9 MESH DESCRIPTOR Otitis Media AND CENTRAL:TARGET 10 (otitis media):TI,TO AND CENTRAL:TARGET 11 #9 OR #10 AND CENTRAL:TARGET 12 (((effusion or Recurrent or persistent or serous or secretory or perfusion) adj3 otitis)):AB,EH,KW,KY,MC,MH,TI,TO AND CENTRAL:TARGET 13 #11 AND #12 AND CENTRAL:TARGET 14 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #13 AND CENTRAL:TARGET |
1 MESH DESCRIPTOR Otitis Media EXPLODE ALL AND INREGISTER 2 ("otitis media" OR OME OR "glue ear" OR middle‐ear effusion OR middle‐ear perfusion):AB,EH,KW,KY,MC,MH,TI,TO AND INREGISTER 3 #1 OR #2 4 (effusion or Recurrent or persistent or serous or secretory or perfusion):AB,EH,KW,KY,MC,MH,TI,TO AND INREGISTER 5 #3 AND #4 |
1 exp Otitis Media with Effusion/ 2 ("otitis media" adj6 effusion).ab,ti. 3 OME.ti. 4 Secretory otitis media.ab,ti. 5 Serous otitis media.ab,ti. 6 Middle‐ear effusion.ab,ti. 7 Glue ear.ab,ti. 8 middle‐ear perfusion.ab,ti. 9 Otitis Media/ 10 otitis media.ti. 11 9 or 10 12 ((effusion or Recurrent or persistent or serous or secretory or perfusion) adj3 otitis).ab,ti. 13 11 and 12 14 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 13 15 randomized controlled trial.pt. 16 controlled clinical trial.pt. 17 randomized.ab. 18 placebo.ab. 19 drug therapy.fs. 20 randomly.ab. 21 trial.ab. 22 groups.ab. 23 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 24 exp animals/ not humans.sh. 25 23 not 24 26 14 and 25 |
| Embase (Ovid) | Web of Science (Web of knowledge) | Trial registries (CRS) |
| 1 exp secretory otitis media/ 2 ("otitis media" adj6 effusion).ab,ti. 3 OME.ti. 4 Secretory otitis media.ab,ti. 5 Serous otitis media.ab,ti. 6 Middle‐ear effusion.ab,ti. 7 glue ear.ab,ti. 8 middle‐ear perfusion.ab,ti. 9 otitis media/ 10 otitis media.ti. 11 9 or 10 12 ((effusion or Recurrent or persistent or serous or secretory or perfusion) adj3 otitis).ab,ti. 13 11 and 12 14 1 or 2 or 4 or 5 or 6 or 7 or 8 or 13 15 (random* or factorial* or placebo* or assign* or allocat* or crossover*).tw. 16 (control* adj group*).tw. 17 (trial* and (control* or comparative)).tw. 18 ((blind* or mask*) and (single or double or triple or treble)).tw. 19 (treatment adj arm*).tw. 20 (control* adj group*).tw. 21 (phase adj (III or three)).tw. 22 (versus or vs).tw. 23 rct.tw. 24 crossover procedure/ 25 double blind procedure/ 26 single blind procedure/ 27 randomization/ 28 placebo/ 29 exp clinical trial/ 30 parallel design/ 31 Latin square design/ 32 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 33 exp ANIMAL/ or exp NONHUMAN/ or exp ANIMAL EXPERIMENT/ or exp ANIMAL MODEL/ 34 exp human/ 35 33 not 34 36 32 not 35 37 14 and 36 |
11 #10 AND #9 Indexes=SCI‐EXPANDED, CPCI‐S Timespan=All years 10 #8 OR #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1 Indexes=SCI‐EXPANDED, CPCI‐S Timespan=All years 9 TS=(randomised OR randomized OR randomisation OR randomisation OR placebo* OR (random* AND (allocat* OR assign*) ) OR (blind* AND (single OR double OR treble OR triple) )) Indexes=SCI‐EXPANDED, CPCI‐S Timespan=All years 8 (TI=(otitis media) ) AND TS=((effusion or Recurrent or persistent or serous or secretory or perfusion) NEAR/3 otitis) Indexes=SCI‐EXPANDED, CPCI‐S Timespan=All years 7 TOPIC: ((middle‐ear perfusion) ) Indexes=SCI‐EXPANDED, CPCI‐S Timespan=All years 6 TOPIC: ((glue ear) ) Indexes=SCI‐EXPANDED, CPCI‐S Timespan=All years 5 TOPIC: ((Middle‐ear effusion) ) Indexes=SCI‐EXPANDED, CPCI‐S Timespan=All years 4 TOPIC: ((Serous otitis media) ) Indexes=SCI‐EXPANDED, CPCI‐S Timespan=All years 3 TOPIC: ((Secretory otitis media) ) Indexes=SCI‐EXPANDED, CPCI‐S Timespan=All years 2 TITLE: (OME) Indexes=SCI‐EXPANDED, CPCI‐S Timespan=All years 1 TOPIC: ("otitis media" NEAR/6 effusion) Indexes=SCI‐EXPANDED, CPCI‐S Timespan=All years |
1 ("otitis media" OR OME OR "glue ear" OR middle‐ear effusion OR middle‐ear perfusion):AB,EH,KW,KY,MC,MH,TI,TO AND CENTRAL:TARGET 2 (effusion or Recurrent or persistent or serous or secretory or perfusion):AB,EH,KW,KY,MC,MH,TI,TO AND CENTRAL:TARGET 3 #1 AND #2 4 http*:SO AND CENTRAL:TARGET 5 (NCT0* or ACTRN* or ChiCTR* or DRKS* or EUCTR* or eudract* or IRCT* or ISRCTN* or JapicCTI* or JPRN* or NTR0* or NTR1* or NTR2* or NTR3* or NTR4* or NTR5* or NTR6* or NTR7* or NTR8* or NTR9* or SRCTN* or UMIN0*):AU AND CENTRAL:TARGET 6 #4 OR #5 7 #3 AND #6 |
| ClinicalTrials.gov | ICTRP | |
| (EXPAND[Concept] "otitis media" OR EXPAND[Concept] "glue ear" OR middle‐ear ) AND (effusion OR Recurrent OR persistent OR serous OR secretory OR perfusion ) | Interventional Studies | (otitis media AND effusion) OR glue ear OR middle‐ear effusion OR middle‐ear perfusion |
Appendix 2. Tool for screening eligible studies for scientific integrity/trustworthiness
This screening tool has been developed by Cochrane Pregnancy and Childbirth. It includes a set of predefined criteria to select studies that, based on available information, are deemed to be sufficiently trustworthy to be included in the analysis.
| Criteria questions | Assessment | Comments and concerns | |
| High risk | Low risk | ||
| Research governance | |||
| Are there any retraction notices or expressions of concern listed on the Retraction Watch Database relating to this study? | Yes | No | |
| Was the study prospectively registered (for those studies published after 2010) If not, was there a plausible reason? | No | Yes | |
| When requested, did the trial authors provide/share the protocol and/or ethics approval letter? | No | Yes | |
| Did the trial authors engage in communication with the Cochrane Review authors within the agreed timelines? | No | Yes | |
| Did the trial authors provide IPD data upon request? If not, was there a plausible reason? | No | Yes | |
| Baseline characteristics | |||
| Is the study free from characteristics of the study participants that appear too similar? (e.g. distribution of the mean (SD) excessively narrow or excessively wide, as noted by Carlisle 2017) |
No | Yes | |
| Feasibility | |||
| Is the study free from characteristics that could be implausible? (e.g. large numbers of women with a rare condition (such as severe cholestasis in pregnancy) recruited within 12 months) | No | Yes | |
| In cases with (close to) zero losses to follow‐up, is there a plausible explanation? | No | Yes | |
| Results | |||
| Is the study free from results that could be implausible? (e.g. massive risk reduction for main outcomes with small sample size)? | No | Yes | |
| Do the numbers randomised to each group suggest that adequate randomisation methods were used (e.g. is the study free from issues such as unexpectedly even numbers of women ‘randomised’ including a mismatch between the numbers and the methods, if the authors say ‘no blocking was used’ but still end up with equal numbers, or if the authors say they used ‘blocks of 4’ but the final numbers differ by 6)? | No | Yes | |
| For abstracts only: | |||
| Have the study authors confirmed in writing that the data to be included in the review have come from the final analysis and will not change? | No | Yes | |
Appendix 3. Additional detail on adverse effects
Comparison 1: Ventilation tubes (VT) versus no treatment
VT versus no treatment
Rach 1991 found that in the short term (< 3 months) 9/44 (20.5%) VT were in situ and in the medium term (6 months) 18/44 (40.9%) of the tubes had extruded in the VT only group (assessed by otoscopy).
Maw 1983 reports that some VTs were reinserted, but no data are presented for the number of extrusions/reinsertions.
Dempster 1993 reported that at 12 months tympanosclerosis had occurred in 28 ears (39%) in the VT group but in none of the ears without VT. In addition, at 12 months, six ears (8.3%) in the VT group and seven ears (9.7%) in the no treatment group showed signs of perforation/retraction. At the 12‐month follow‐up visit, 31% of VT were still functioning.
Comparison 2: Ventilation tubes versus watchful waiting
In the TARGET 2000 trial, of 635 ears that had a VT inserted, eight had a perforation recorded at least six months after surgery. However, of the four who attended later appointments, all had healed. Of ears receiving a VT, either with or without adenoidectomy, 128/635 (20%) showed tympanosclerosis while none were reported in the watchful waiting group. For ears receiving VT, in the short term, 259/327 ears (79%) were functioning while 68/327 (21%) were either non‐functioning or extruded; in the medium term (12 months) 57/316 ears (55%) were functioning while 259/316 (18%) were either non‐functioning or extruded; and in the long term (24 months) 9/300 ears (3%) were functioning while 291/300 (97%) were either non‐functioning or extruded. Data are presented only for ears when the otoscopy and tympanometry results agree. One child (1/165 (0.6%)) who underwent an adenoidectomy had to return to theatre for postoperative haemorrhage (Note: the total number exceeds the number allocated to adenoidectomy because of cross‐overs from other groups).
Maw 1999 did not report adverse events.
Paradise 2007 assessed assessed a number of adverse events after long‐term follow‐up. The results were as follows:
-
Tympanosclerosis
Risk ratio (RR) 0.91 for those undergoing early ventilation tube insertion (95% confidence interval (CI) 0.33 to 2.55; 1 study, 391 participants, but data adjusted to account for non‐independence of within‐individual measurement; Analysis 2.16; very low‐certainty evidence).
-
Fibrosis
RR 0.61 for those undergoing early ventilation tube insertion (95% CI 0.10 to 3.60; 1 study, 391 participants, but data adjusted to account for non‐independence of within‐individual measurement; Analysis 2.17; very low‐certainty evidence).
-
Segmental atrophy
RR 2.83 for those undergoing early ventilation tube insertion (95% CI 1.81 to 4.43; 1 study, 391 participants, but data adjusted to account for non‐independence of within‐individual measurement; Analysis 2.18; very low‐certainty evidence).
-
Retraction pocket with other abnormality
RR 0.91 for those undergoing early ventilation tube insertion (95% CI 0.06 to 14.50; 1 study, 391 participants, but data adjusted to account for non‐independence of within‐individual measurement; Analysis 2.19 very low‐certainty evidence).
2.16. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 16: Adverse event: tympanosclerosis (long‐term)
2.17. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 17: Adverse event: fibrosis (long‐term)
2.18. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 18: Adverse event: segmental atrophy (long‐term)
2.19. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 19: Adverse event: retraction pocket with other abnormality (long‐term)
Rach 1991 did not report adverse events after long‐term follow‐up (relevant for this comparison).
Rovers 2000 presented data on the proportion of children with parental reports of otorrhoea in the short term (three months), with 42.9% in the VT group and 14.3% in the watchful waiting group. In the medium term (12 months), 37.6% in the VT group reported otorrhoea while 16.5% did in the watchful waiting group. Rovers 2000 also reported the number of children with a specific number of episodes of otorrhoea at 12 months. In the VT group, 16/93 (17%) of children reported no episodes of otorrhoea, 28 (30%) reported one episode, 26 (28%) reported two episodes and 23 (25%) reported more than three episodes. In the watchful waiting group, 58 (62%) reported no episodes of otorrhoea at 12 months, 23 (24%) reported one episode, eight (9%) reported two episodes and five (5%) reported three episodes. In terms of the cumulative proportion of children with one or more episodes of otorrhoea at 12 months, this was 83% in the VT group (95% CI 75 to 91%) and 38% (28 to 48%) in the watchful waiting group (P = 0.001). At three months, 92% of VT were in situ, and 30% at 12 months.
Velepic 2011 presented data for a number of adverse events, but data were presented for all participants rather than for each group. In terms of attic retractions, 74/161 (46%) ears presented as mild retractions (type I and II according to Sudhoff and Tos), while in 5/161 (3.1%) ear retractions were severe (type III and IV). A total of 82/161 (51%) ears showed no attic retraction. Velepic 2011 reported that when the two groups were compared, ears in the adenoidectomy only group more frequently reported normal ears in terms of attic retraction compared to ears receiving adenoidectomy and VT (Chi2 = 4.592; ss = 1; P = 0.032). Tensa retractions/malleus rotation was observed in 36/161 ears (22.4%). There was no statistically significant difference in the incidence between the two groups (Chi2 = 0.263; ss = 1; P = 0.608). Scars of the ear drum were observed in 46/161 ears (28.6%) and were found significantly more frequently in the group receiving VT (Chi2 = 28.107; ss = 1; P < 0.001). Myringosclerosis was observed in 42/161 ears (26.1%), but there was no significant difference in the incidence observed between the two groups (Chi2 = 0.171; ss = 1; P = 0.680). Data on persistent perforation are shown in Analysis 2.9.
Comparison 3: Ventilation tubes versus myringotomy
All adverse events reported by Bernard 1991 are included in Table 7 and Table 8. Comparative data were available for myringosclerosis, with a risk ratio of 4.60 for those who received ventilation tubes (95% CI 1.64 to 12.91; 1 study, 125 participants; Analysis 3.3; very low‐certainty evidence).
3.3. Analysis.

Comparison 3: Ventilation tubes versus non‐surgical treatment, Outcome 3: Adverse event: myringosclerosis (long‐term)
Comparison 4: Ventilation tubes versus myringotomy
In the D'Eredita 2006 trial, participants were asked to report “any complications noted during the post‐operative period” in a questionnaire. D'Eredita 2006 reported that 59 of 60 questionnaires (98.3%) were returned. Given that there were 30 children participating in the trial, it is not clear whether participants were asked to complete one questionnaire on two occasions for each child or one questionnaire for each ear on one occasion. It is therefore not clear whether the adverse events reported relate to children or ears. Parents reported six episodes of otorrhoea: two in the laser myringotomy group at two months post surgery, and four in the VT group at 30 days and three months post surgery. The otorrhoea responded to topical antibiotic‐containing drops.
Gates 1989 reported necrosis of the long process of the incus in one child who received a VT and the child underwent a myringostapediopexy. It is not clear to which treatment group the child was randomised. A tube fell into the middle ear in three instances and became trapped when the tympanic membrane healed. In such cases, repeat myringotomy was performed, the tube removed and a new one inserted. The time point of assessment was not stated but assumed to be two years. Gates 1989 reported the number (proportion) of children with the number of episodes of otorrhoea (see Analysis 4.14).
4.14. Analysis.

Comparison 4: Ventilation tubes versus myringotomy, Outcome 14: Adverse events: otorrhoea (long‐term)
Koopman 2004 reported that 1/208 (0.5%) children in the laser myringotomy group complained of severe otalgia during the first two days post laser myringotomy. There were no signs of inflammation, and the condition was treated with oral analgesics. Otorrhoea occurred more frequently in the VT ear than in the laser myringotomy ear (P = 0.002), but the number of events and denominators were not reported.
Popova 2010 reported episodes of otorrhoea per child in the medium term (12 months). For children receiving adenoidectomy and VT, 25/42 (60%) reported no episodes of otorrhoea, 10/42 (24%) reported one episode, 5/42 (12%) reported two episodes, 1/42 (2%) reported three episodes and 1/42 (2%) reported four or more episodes. In the children receiving adenoidectomy and myringotomy, all children 36/36 (100%) reported no episodes of otorrhoea. Of the 42 children receiving VT, seven (17%) experienced a blockage.
Ruckley 1988 found no evidence of tympanosclerosis in any ear receiving either treatment. In the short term (three months), 2/36 ears (5.5%) receiving VT were blocked. In the very short term (two weeks), one child complained of mild otalgia in the ear receiving thermal myringotomy (see Analysis 4.5).
Sujatha 2015 reported adverse events by ear. In the right ear, in the group receiving myringotomy alone, 22 (88%) showed retracted tympanic membrane at three months, and at one year seven (28%) were retracted and one (4%) showed tympanosclerotic patch. In those receiving VT, at one year, 14 (56%) were retracted, two (8%) showed tympanosclerotic patch and three (12%) tympanic membranes showed perforation in the anterior quadrant. This is significant by Fisher's exact test (P < 0. 01) (Fig. 3).
In the left ear, in the group receiving myringotomy alone, after one year, six (24%) showed retracted tympanic membranes whereas those receiving VT showed retraction in 12 cases (48%), tympanosclerotic patch in one (4%) and perforation in three (12%). All perforations were in the anterior quadrant. This comparison between groups showed a significant difference by Fisher's exact test (P < 0. 05).
In the right ear, all VT were in situ at the third month visit and all but one were expelled at the end of six months. In the left ear, the VT was present in all patients in the third month follow‐up, and it was expelled in all except one at the six‐month visit. In one case, a VT got blocked at the third month and it was removed under local anaesthesia.
Tao 2020 reported that at two weeks follow‐up, of those receiving myringotomy, five ears/four patients showed tympanic effusion, while in those receiving VT, non‐purulent effusions could be seen in the ear canals in eight ears/seven patients, and the re‐examination after one week showed that all the ears were dry. A re‐examination six months after the operation showed that in those receiving myringotomy, three ears/two patients received tympanostomy again and at 12 months, two ears/two patients received tympanostomy again after the failure of conservative treatment.
To 1984 reported that 9/54 (17%) receiving a VT experienced tympanosclerosis while 1/54 ears (2%) receiving a myringotomy experienced tympanosclerosis. The timing of the follow‐up was not reported. In terms of retraction segments, 0/54 ears receiving VT and 1/54 receiving a myringotomy experienced retraction segments assessed at nine months, while 2/54 ears (4%) receiving VT and 1/54 receiving a myringotomy experienced retraction segments assessed in the long term (24 months). In terms of persistent perforation, one ear receiving VT experienced this between 9 and 21 months and no ears receiving myringotomy (see Analysis 4.7).
§In Yousaf 2016, in terms of post‐surgical haemorrhage, those receiving laser myringotomy reported no cases but nine (13%) in the VT group reported this. Yousaf 2016 reported that for ears receiving VT 6/68 (13%) had extruded in the very short term (30 days) while 53/68 (78%) had extruded in the medium term (six months).
Retraction of the tympanic membrane: RR 2.33 for those receiving ventilation tubes as compared to laser myringotomy (95% CI 0.64 to 8.46; 1 study, 90 participants; Analysis 4.17; very low‐certainty evidence). Sensitivity analysis to account for correlation between ears of the same individual made little difference to the overall effect estimates (Analysis 7.15; Analysis 7.16).
Hypertrophic scar of the tympanic membrane: OR 7.50 for those receiving ventilation tubes as compared to laser myringotomy (95% CI 0.46 to 121.15; 1 study, 90 participants; Analysis 4.18; very low‐certainty evidence)
Otorrhoea: RR 3.00 for those receiving ventilation tubes as compared to laser myringotomy (95% CI 0.32 to 27.76; 1 study, 90 participants; Analysis 4.19; very low‐certainty evidence). Sensitivity analysis to account for correlation between ears of the same individual made little difference to the overall effect estimates (Analysis 7.17; Analysis 7.18).
4.17. Analysis.

Comparison 4: Ventilation tubes versus myringotomy, Outcome 17: Adverse event: retraction of TM: VT versus laser myringotomy (medium‐term)
7.15. Analysis.

Comparison 7: Sensitivity analyses: Ventilation tubes versus myringotomy, Outcome 15: Sensitivity analysis: Retraction of TM: VT versus laser myringotomy (medium‐term); ICC = 1.0
7.16. Analysis.

Comparison 7: Sensitivity analyses: Ventilation tubes versus myringotomy, Outcome 16: Sensitivity analysis: Retraction of TM: VT versus laser myringotomy (medium‐term); ICC = zero
4.18. Analysis.

Comparison 4: Ventilation tubes versus myringotomy, Outcome 18: Adverse event: hypertrophic scar of TM: VT versus laser myringotomy (medium‐term)
4.19. Analysis.

Comparison 4: Ventilation tubes versus myringotomy, Outcome 19: Adverse event: otorrhoea: VT versus laser myringotomy (medium‐term)
7.17. Analysis.

Comparison 7: Sensitivity analyses: Ventilation tubes versus myringotomy, Outcome 17: Sensitivity analysis: Otorrhoea: VT versus laser myringotomy (medium‐term); ICC = 1.0
7.18. Analysis.

Comparison 7: Sensitivity analyses: Ventilation tubes versus myringotomy, Outcome 18: Sensitivity analysis: Otorrhoea: VT versus laser myringotomy (medium‐term); ICC = zero
Data and analyses
Comparison 1. Ventilation tubes versus no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Return to normal hearing, randomised by ear (medium‐term) | 1 | Odds Ratio (IV, Random, 95% CI) | 1.13 [0.46, 2.74] | |
| 1.1.1 Randomised by ear: normal defined as < 15 dB; CC = 0.5 (medium‐term) | 1 | Odds Ratio (IV, Random, 95% CI) | 1.13 [0.46, 2.74] | |
| 1.2 Mean final hearing threshold, randomised by ear (medium‐term) | 2 | Mean Difference (IV, Random, 95% CI) | ‐3.47 [‐9.97, 3.03] | |
| 1.2.1 Correlation coefficient = 0.5 | 2 | Mean Difference (IV, Random, 95% CI) | ‐3.47 [‐9.97, 3.03] | |
| 1.3 Change in hearing threshold from baseline, randomised by ear (medium‐term) | 1 | Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐3.28, 2.97] | |
| 1.4 Adverse event: perforation/retraction, randomised by ear (medium‐term) | 1 | Odds Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.4.1 Correlation coefficient 0.5 | 1 | Odds Ratio (IV, Random, 95% CI) | 0.85 [0.38, 1.91] | |
| 1.5 Persistence of OME: randomised by child (very short‐term) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.6 Persistence of OME: randomised by child (medium‐term) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.6.1 Adjusted for non‐independence of within‐individual measurements, assuming ICC of 0.5 | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.7 Persistence of OME: randomised by ear (medium‐term) | 1 | Odds Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.7.1 Correlation coefficient = 0.5 | 1 | Odds Ratio (IV, Random, 95% CI) | 0.66 [0.24, 1.85] | |
| 1.8 Mean improvement in comprehensive language, randomised by child (medium‐term) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.9 Mean improvement in expressive language, randomised by child (medium‐term) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.10 Adverse event: tympanosclerosis, randomised by ear (medium‐term) | 1 | 144 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 10.09 [4.48, 22.70] |
Comparison 2. Early ventilation tubes versus watchful waiting (treatment later if required).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Return to normal hearing, randomised by child (long‐term) | 1 | 391 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.94, 1.03] |
| 2.2 Mean final hearing threshold, randomised by child (short‐term) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.3 Mean final hearing threshold (air conduction), randomised by child (medium‐term) | 2 | 351 | Mean Difference (IV, Random, 95% CI) | ‐1.89 [‐7.32, 3.54] |
| 2.4 Mean final hearing threshold (air‐bone gap), randomised by child, analysed by ear (medium‐term) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.4.1 Adjusted for non‐independence of within‐individual measurements, assuming ICC of 0.5 | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.5 Mean final hearing threshold, randomised by child (long‐term) | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.5.1 Assumed correlation coefficient for Paradise 2007 (left and right ear data combined) of 0.5 | 3 | 633 | Mean Difference (IV, Random, 95% CI) | 0.36 [‐0.41, 1.13] |
| 2.6 Hearing in noise test, randomised by child (long‐term) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.6.1 Competing noise from the front (dB) | 1 | 391 | Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.13, 0.53] |
| 2.6.2 Competing noise from the right (dB) | 1 | 391 | Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.54, 0.54] |
| 2.6.3 Competing noise from the left (dB) | 1 | 391 | Mean Difference (IV, Random, 95% CI) | 0.40 [‐0.10, 0.90] |
| 2.7 Change in hearing threshold from baseline, randomised by child (medium‐term) | 1 | 176 | Mean Difference (IV, Random, 95% CI) | ‐4.60 [‐8.57, ‐0.63] |
| 2.8 Adjusted mean difference in hearing improvement, randomised by child (medium term) | 1 | Mean Difference (IV, Random, 95% CI) | 1.60 [‐0.62, 3.82] | |
| 2.9 Adverse event: persistent perforation, randomised by child (medium‐term) | 1 | 161 | Risk Difference (M‐H, Random, 95% CI) | 0.00 [‐0.03, 0.03] |
| 2.10 Adverse event: persistent perforation, randomised by child (long‐term) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.10.1 Adjusted for non‐independence of within‐individual measurements: ICC 0.5 | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.11 Presence/persistence of OME, randomised by child, measured by otoscopy (medium‐term) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.11.1 Adjusted for non‐independence of within‐individual measurements, assuming ICC of 0.5 | 1 | 113 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.09, 1.72] |
| 2.12 Presence/persistence of OME, randomised by child, measured by tympanometry (medium‐term) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.13 Presence/persistence of OME, mean percentage of days, randomised by child (medium‐term) | 1 | 316 | Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.23, ‐0.15] |
| 2.14 Presence/persistence of OME, randomised by child (long‐term) | 3 | 584 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.84, 1.74] |
| 2.15 Presence/persistence of OME, adjusted OR, randomised by child (long‐term) | 1 | Odds Ratio (IV, Random, 95% CI) | 0.99 [0.35, 2.83] | |
| 2.16 Adverse event: tympanosclerosis (long‐term) | 1 | 375 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.33, 2.55] |
| 2.16.1 Adjusted for non‐independence of within‐individual measurements: ICC 0.5 | 1 | 375 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.33, 2.55] |
| 2.17 Adverse event: fibrosis (long‐term) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.17.1 Adjusted for non‐independence of within‐individual measurements: ICC 0.5 | 1 | 375 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.10, 3.60] |
| 2.18 Adverse event: segmental atrophy (long‐term) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.18.1 Adjusted for non‐independence of within‐individual measurements. Assumed ICC 0.5 | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.19 Adverse event: retraction pocket with other abnormality (long‐term) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.19.1 Adjusted for non‐independence of within‐individual measurements; assumed ICC 0.5 | 1 | 374 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.06, 14.41] |
| 2.20 Receptive language development, Reynell test, randomised by child (medium‐term) | 1 | Mean Difference (IV, Random, 95% CI) | 0.31 [‐0.03, 0.65] | |
| 2.21 Receptive language development, Reynell test, adjusted MD (medium‐term) | 1 | Mean Difference (IV, Random, 95% CI) | 0.39 [0.04, 0.74] | |
| 2.22 Receptive language, Reynell test, randomised by child (long‐term) | 1 | Mean Difference (IV, Random, 95% CI) | 0.26 [‐0.08, 0.60] | |
| 2.23 Receptive language: Reynell test, long‐term, adjusted MD | 1 | Mean Difference (IV, Random, 95% CI) | 0.17 [‐0.21, 0.55] | |
| 2.24 Receptive language: WOLD adjusted OR (long‐term) | 1 | Odds Ratio (IV, Random, 95% CI) | 1.58 [0.59, 4.24] | |
| 2.25 Receptive language, mean difference (months) in improvement in Reynell test score (equivalent age‐real age): medium‐term | 1 | Mean Difference (IV, Random, 95% CI) | 1.01 [‐0.14, 2.16] | |
| 2.26 Receptive language, adjusted mean difference (months) in improvement in Reynell test score (equivalent age ‐ real age): medium‐term | 1 | Mean Difference (IV, Random, 95% CI) | 0.71 [‐0.28, 1.70] | |
| 2.27 Expressive language development: Reynell test (medium‐term) | 1 | Mean Difference (IV, Random, 95% CI) | 0.38 [‐0.00, 0.76] | |
| 2.28 Expressive language development: Reynell test, medium‐term, adjusted MD | 1 | Mean Difference (IV, Random, 95% CI) | 0.42 [0.02, 0.82] | |
| 2.29 Expressive language development: Reynell test (long‐term) | 1 | Mean Difference (IV, Random, 95% CI) | 0.31 [‐0.07, 0.69] | |
| 2.30 Expressive language development: Reynell test, long‐term, adjusted MD | 1 | Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.28, 0.56] | |
| 2.31 Expressive language: WOLD adjusted OR (long‐term) | 1 | Odds Ratio (IV, Random, 95% CI) | 2.10 [0.78, 5.65] | |
| 2.32 Expressive language, MD (months) in improvement in Schlichting test score (equivalent age‐real age): medium‐term | 1 | Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐2.19, 1.13] | |
| 2.33 Expressive language, adjusted mean difference (months) in improvement in Schlichting test score (equivalent age‐real age): medium‐term | 1 | Mean Difference (IV, Random, 95% CI) | 0.96 [‐0.43, 2.35] | |
| 2.34 Non‐word repetition total score, adjusted OR (long‐term) | 1 | Odds Ratio (IV, Random, 95% CI) | 1.69 [0.64, 4.47] | |
| 2.35 Reading, WORD test, adjusted OR (long‐term) | 1 | Odds Ratio (IV, Random, 95% CI) | Subtotals only | |
| 2.36 Spelling, ALSPAC test, adjusted OR (long‐term) | 1 | Odds Ratio (IV, Random, 95% CI) | 0.90 [0.33, 2.45] | |
| 2.37 Phoneme deletion, adjusted OR (long‐term) | 1 | Odds Ratio (IV, Random, 95% CI) | 0.84 [0.32, 2.20] | |
| 2.38 Cognitive development: Griffiths practical reasoning (medium‐term) | 1 | Mean Difference (IV, Random, 95% CI) | 2.40 [‐3.78, 8.58] | |
| 2.39 Cognitive development: IQ (WISC‐III UK short form) adjusted OR (long‐term) | 1 | Odds Ratio (IV, Random, 95% CI) | Totals not selected | |
| 2.40 Behaviour, Richman score (medium‐term) | 1 | 150 | Mean Difference (IV, Random, 95% CI) | ‐0.65 [‐1.85, 0.55] |
| 2.41 Behaviour, Richman score, dichotomised (medium‐term) | 1 | 150 | Risk Ratio (M‐H, Random, 95% CI) | 0.63 [0.42, 0.96] |
| 2.42 Behaviour, Richman score, adjusted OR (medium‐term) | 1 | Odds Ratio (IV, Random, 95% CI) | 1.16 [0.27, 4.90] | |
| 2.43 Behaviour, Richman score (long‐term) | 1 | 123 | Mean Difference (IV, Random, 95% CI) | 0.90 [‐0.27, 2.07] |
| 2.44 Behaviour, Richman score, dichotomised (long‐term) | 1 | 123 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.62, 2.40] |
| 2.45 Behaviour: SDQ teacher report, total, adjusted OR (long‐term) | 1 | Odds Ratio (IV, Random, 95% CI) | 2.05 [0.62, 6.74] | |
| 2.46 Parent‐child interaction: Erickson child scale (medium‐term) | 1 | 165 | Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.56, ‐0.12] |
| 2.47 Parent‐child interaction: Erickson parent scale (medium‐term) | 1 | 165 | Mean Difference (IV, Random, 95% CI) | ‐0.42 [‐0.67, ‐0.17] |
| 2.48 Generic health‐related quality of life: TAIQOL (medium‐term) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.48.1 Vitality | 1 | 165 | Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐1.95, 1.75] |
| 2.48.2 Appetite | 1 | 165 | Mean Difference (IV, Fixed, 95% CI) | 0.40 [‐3.77, 4.57] |
| 2.48.3 Communication | 1 | 165 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐5.11, 5.71] |
| 2.48.4 Motoric | 1 | 165 | Mean Difference (IV, Fixed, 95% CI) | 0.00 [‐2.51, 2.51] |
| 2.48.5 Social | 1 | 165 | Mean Difference (IV, Fixed, 95% CI) | 0.00 [‐2.49, 2.49] |
| 2.48.6 Anxiety | 1 | 165 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐3.04, 3.64] |
| 2.48.7 Aggression | 1 | 165 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐5.82, 6.42] |
| 2.48.8 Eating | 1 | 165 | Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐1.63, 1.43] |
| 2.48.9 Sleeping | 1 | 165 | Mean Difference (IV, Fixed, 95% CI) | 0.00 [‐5.70, 5.70] |
| 2.49 Parental stress, Parental Stress Index, short form (long‐term) | 1 | 383 | Mean Difference (IV, Random, 95% CI) | 0.00 [‐4.12, 4.12] |
| 2.50 Literacy (long‐term) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.50.1 Woodcock Reading Mastery Tests: Word Identification subtest | 1 | 391 | Mean Difference (IV, Random, 95% CI) | ‐1.00 [‐3.28, 1.28] |
| 2.50.2 Woodcock Reading Mastery Tests: Word Attack subtest | 1 | 391 | Mean Difference (IV, Random, 95% CI) | ‐1.00 [‐3.68, 1.68] |
| 2.50.3 Woodcock Reading Mastery Tests: Passage Comprehension subtest | 1 | 391 | Mean Difference (IV, Random, 95% CI) | ‐1.00 [‐3.38, 1.38] |
| 2.50.4 Oral reading fluency test: Children in grade 3 | 1 | 74 | Mean Difference (IV, Random, 95% CI) | ‐9.00 [‐26.58, 8.58] |
| 2.50.5 Oral reading fluency test: Children in grade 4 | 1 | 184 | Mean Difference (IV, Random, 95% CI) | 0.00 [‐10.70, 10.70] |
| 2.50.6 Oral reading fluency test: Children in grade 5 | 1 | 105 | Mean Difference (IV, Random, 95% CI) | ‐5.00 [‐18.98, 8.98] |
| 2.50.7 Oral reading fluency test: Children in grade 6 | 1 | 21 | Mean Difference (IV, Random, 95% CI) | 6.00 [‐27.42, 39.42] |
| 2.50.8 Woodcock–Johnson III Tests of Achievement: Spelling subtest | 1 | 390 | Mean Difference (IV, Random, 95% CI) | ‐1.00 [‐3.89, 1.89] |
| 2.50.9 Woodcock–Johnson III Tests of Achievement: Writing Samples subtest | 1 | 387 | Mean Difference (IV, Random, 95% CI) | ‐1.00 [‐3.89, 1.89] |
| 2.51 Phonological awareness (long‐term) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.51.1 Comprehensive Test of Phonological Processing: Elision subtest | 1 | 391 | Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.91, 0.71] |
| 2.51.2 Comprehensive Test of Phonological Processing: Rapid Letter Naming subtest | 1 | 389 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.79, 0.19] |
| 2.52 Attention, impulsivity and psychosocial function, long‐term (1): disruptive behaviour disorders, child behaviour and impairment rating | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.52.1 Disruptive Behavior Disorders Rating Scale: Inattention factor: Parent's rating | 1 | 390 | Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.08, 0.18] |
| 2.52.2 Disruptive Behavior Disorders Rating Scale: Inattention factor: Teacher's rating | 1 | 382 | Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.11, 0.19] |
| 2.52.3 Disruptive Behavior Disorders Rating Scale: Impulsivity and overactivity factor: Parent's rating | 1 | 390 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.01, 0.21] |
| 2.52.4 Disruptive Behavior Disorders Rating Scale: Impulsivity and overactivity factor: Teacher's rating | 1 | 382 | Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.04, 0.20] |
| 2.52.5 Disruptive Behavior Disorders Rating Scale: Oppositional defiant factor: Parent's rating | 1 | 390 | Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.06, 0.16] |
| 2.52.6 Disruptive Behavior Disorders Rating Scale: Oppositional defiant factor: Teacher's rating | 1 | 382 | Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.11, 0.11] |
| 2.52.7 Child Behavior Checklist: Total Problems score, parent’s rating | 1 | 390 | Mean Difference (IV, Random, 95% CI) | 2.00 [‐0.38, 4.38] |
| 2.52.8 Child Behavior Checklist: Total Problems score, teacher’s rating | 1 | 380 | Mean Difference (IV, Random, 95% CI) | 2.00 [‐0.21, 4.21] |
| 2.52.9 Impairment Rating Scales: Overall functioning, parent’s rating | 1 | 390 | Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.13, 0.41] |
| 2.52.10 Impairment Rating Scales: Overall functioning, teacher’s rating | 1 | 382 | Mean Difference (IV, Random, 95% CI) | 0.26 [‐0.18, 0.70] |
| 2.53 Attention, impulsivity and psychosocial function, long‐term (2): social skills | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.53.1 Attention, impulsivity and psychosocial function: Social Skills Rating System: parent version | 1 | 388 | Mean Difference (IV, Random, 95% CI) | ‐2.00 [‐5.68, 1.68] |
| 2.53.2 Attention, impulsivity and psychosocial function: Social Skills Rating System: teacher version | 1 | 370 | Mean Difference (IV, Random, 95% CI) | ‐1.00 [‐3.65, 1.65] |
| 2.54 Attention, impulsivity and psychosocial function, long‐term: Visual and auditory continuous performance | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.54.1 Visual Continuous Performance Test: Inattention | 1 | 391 | Mean Difference (IV, Random, 95% CI) | 0.20 [‐2.66, 3.06] |
| 2.54.2 Visual Continuous Performance Test: Impulsivity | 1 | 391 | Mean Difference (IV, Random, 95% CI) | 0.60 [‐2.58, 3.78] |
| 2.54.3 Auditory Continuous Performance Test: Inattention | 1 | 308 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐2.00, 1.40] |
| 2.54.4 Auditory Continuous Performance Test: Impulsivity | 1 | 307 | Mean Difference (IV, Random, 95% CI) | ‐0.90 [‐3.26, 1.46] |
| 2.55 Intelligence and academic achievement (long‐term) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.55.1 Wechsler Abbreviated Scale of Intelligence | 1 | 391 | Mean Difference (IV, Random, 95% CI) | 0.00 [‐2.68, 2.68] |
| 2.55.2 Calculation subtest of the Woodcock–Johnson III Tests of Achievement | 1 | 389 | Mean Difference (IV, Random, 95% CI) | 0.00 [‐2.58, 2.58] |
2.55. Analysis.

Comparison 2: Early ventilation tubes versus watchful waiting (treatment later if required) , Outcome 55: Intelligence and academic achievement (long‐term)
Comparison 3. Ventilation tubes versus non‐surgical treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Mean final hearing threshold (short‐term) | 1 | 125 | Mean Difference (IV, Random, 95% CI) | ‐9.00 [‐12.61, ‐5.39] |
| 3.2 Mean final hearing threshold (medium‐term) | 1 | 125 | Mean Difference (IV, Random, 95% CI) | ‐5.98 [‐9.21, ‐2.75] |
| 3.3 Adverse event: myringosclerosis (long‐term) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.4 Number of doctor‐diagnosed AOM episodes (medium‐term) | 1 | 125 | Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.42, ‐0.04] |
| 3.5 Number of doctor‐diagnosed episodes of AOM (long‐term) | 1 | 125 | Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.31, 0.21] |
Comparison 4. Ventilation tubes versus myringotomy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Hearing returned to normal: VT versus laser myringotomy (medium‐term) | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1.1 Adjusted for non‐independence of within‐individual measurements; assumed ICC of 0.5 | 2 | 132 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.59, 2.53] |
| 4.2 Mean final hearing threshold, randomised by child (short‐term). Adjusted for non‐independence of within‐individual measurements; assumed ICC of 0.5 | 1 | 104 | Mean Difference (IV, Random, 95% CI) | 0.20 [‐2.13, 2.53] |
| 4.3 Mean final hearing threshold, randomised by ear (short‐term) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.4 Mean final hearing threshold (medium‐term) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.4.1 Pure tone audiometry at 12 months. Adjusted for non‐independence of within‐individual measurements; assumed ICC of 0.5 | 1 | 104 | Mean Difference (IV, Fixed, 95% CI) | 0.80 [‐0.87, 2.47] |
| 4.4.2 Air‐bone gap at 12 months | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | 4.50 [0.76, 8.24] |
| 4.5 Adverse event: persistent perforation (medium‐term) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.5.1 Adjustment for non‐independence of within‐individual measurements: assumed ICC of 0.5 | 1 | 102 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.06, 15.56] |
| 4.6 Adverse event: persistent perforation cold‐steel myringotomy (medium‐term) | 2 | 208 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 8.09 [1.78, 36.79] |
| 4.7 Persistence of OME: VT versus laser myringotomy (short‐term) | 1 | 102 | Risk Ratio (M‐H, Random, 95% CI) | 1.40 [0.48, 4.12] |
| 4.7.1 Adjusted for non‐independence of within‐individual measurements; assumed ICC of 0.5 | 1 | 102 | Risk Ratio (M‐H, Random, 95% CI) | 1.40 [0.48, 4.12] |
| 4.8 Persistence of OME: VT versus thermal myringotomy, randomised by ear (short‐term) | 1 | 72 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.11 [0.02, 0.53] |
| 4.9 Persistence of OME: VT versus cold‐steel myringotomy (medium‐term) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.10 Persistence of OME: VT versus laser myringotomy (medium‐term) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.10.1 Adjusted for non‐independence of within‐participant measurements; assumed ICC of 0.5 | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.11 Persistence of OME: VT versus laser myringotomy, randomised by ear (medium‐term) | 1 | Odds Ratio (IV, Random, 95% CI) | Totals not selected | |
| 4.11.1 Correlation coefficient of 0.5 assumed | 1 | Odds Ratio (IV, Random, 95% CI) | Totals not selected | |
| 4.12 Persistence of OME: mean days to first recurrence | 1 | 389 | Mean Difference (IV, Random, 95% CI) | 173.88 [150.19, 197.56] |
| 4.13 Persistence of OME (long‐term) | 1 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.90, 1.05] |
| 4.14 Adverse events: otorrhoea (long‐term) | 1 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 1.58 [0.98, 2.53] |
| 4.15 Zero, one or two episodes of AOM in 12 months | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.15.1 Zero episodes | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.15.2 One episode | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.15.3 Two episodes | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.16 Three or more episodes of AOM in 12 months | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Totals not selected | |
| 4.16.1 Three episodes | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Totals not selected | |
| 4.16.2 Four or more episodes | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Totals not selected | |
| 4.17 Adverse event: retraction of TM: VT versus laser myringotomy (medium‐term) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.17.1 Adjusted for non‐independence of within‐individual measurements; assumed ICC of 0.5 | 1 | 102 | Risk Ratio (M‐H, Random, 95% CI) | 2.67 [0.75, 9.48] |
| 4.18 Adverse event: hypertrophic scar of TM: VT versus laser myringotomy (medium‐term) | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 4.19 Adverse event: otorrhoea: VT versus laser myringotomy (medium‐term) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.19.1 Adjusted for non‐independence of within‐individual measurements; assumed ICC of 0.5 | 1 | 102 | Risk Ratio (M‐H, Random, 95% CI) | 4.00 [0.46, 34.57] |
Comparison 5. Sensitivity analyses: Ventilation tubes versus no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Sensitivity analysis: Return to normal hearing, randomised by ear (medium‐term); CC = 0.3 | 1 | Odds Ratio (IV, Random, 95% CI) | 1.13 [0.46, 2.74] | |
| 5.1.1 Sensitivity analysis: normal defined as < 15 dB; CC = 0.3 | 1 | Odds Ratio (IV, Random, 95% CI) | 1.13 [0.46, 2.74] | |
| 5.2 Sensitivity analysis: Return to normal hearing, randomised by ear (medium‐term); CC = 0.7 | 1 | Odds Ratio (IV, Random, 95% CI) | 1.13 [0.47, 2.75] | |
| 5.2.1 Sensitivity analysis: normal defined as < 15 dB; CC = 0.7 | 1 | Odds Ratio (IV, Random, 95% CI) | 1.13 [0.47, 2.75] | |
| 5.3 Sensitivity analysis: Return to normal hearing, randomised by ear (medium‐term). Normal defined as < 25 dB; CC = 0.5 | 1 | Odds Ratio (IV, Random, 95% CI) | 1.00 [0.57, 1.76] | |
| 5.3.1 Sensitivity analysis: normal defined as < 25 dB; CC = 0.5 (medium‐term) | 1 | Odds Ratio (IV, Random, 95% CI) | 1.00 [0.57, 1.76] | |
| 5.4 Sensitivity analysis: Mean final hearing threshold, randomised by ear (medium‐term); CC = 0.3 | 2 | Mean Difference (IV, Random, 95% CI) | ‐3.47 [‐10.01, 3.06] | |
| 5.4.1 Sensitivity analysis: correlation coefficient = 0.3 | 2 | Mean Difference (IV, Random, 95% CI) | ‐3.47 [‐10.01, 3.06] | |
| 5.5 Sensitivity analysis: Mean final hearing threshold, randomised by ear (medium‐term); CC = 0.7 | 2 | Mean Difference (IV, Random, 95% CI) | ‐3.49 [‐10.37, 3.38] | |
| 5.5.1 Sensitivity analysis: correlation coefficient = 0.7 | 2 | Mean Difference (IV, Random, 95% CI) | ‐3.49 [‐10.37, 3.38] | |
| 5.6 Sensitivity analysis: Change in hearing threshold from baseline, randomised by ear (medium‐term); CC = 0.3 | 1 | Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐3.22, 3.01] | |
| 5.7 Sensitivity analysis: Change in hearing threshold from baseline, randomised by ear (medium‐term); CC = 0.7 | 1 | Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐3.34, 2.92] | |
| 5.8 Sensitivity analysis: Adverse event: perforation/retraction, randomised by ear (medium‐term); CC = 0.3 | 1 | Odds Ratio (IV, Random, 95% CI) | 0.85 [0.33, 2.21] | |
| 5.8.1 Sensitivity analysis: correlation coefficient = 0.3 | 1 | Odds Ratio (IV, Random, 95% CI) | 0.85 [0.33, 2.21] | |
| 5.9 Sensitivity analysis: Adverse event: perforation/retraction, randomised by ear (medium‐term); CC = 0.7 | 1 | Odds Ratio (IV, Random, 95% CI) | 0.91 [0.45, 1.86] | |
| 5.9.1 Sensitivity analysis: correlation coefficient = 0.7 | 1 | Odds Ratio (IV, Random, 95% CI) | 0.91 [0.45, 1.86] | |
| 5.10 Sensitivity analysis: Persistence of OME: randomised by child (medium‐term); ICC = 1.0 | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.27 [0.11, 0.70] |
| 5.10.1 Sensitivity analysis: assuming ICC of 1.0 (complete correlation between ears) | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.27 [0.11, 0.70] |
| 5.11 Sensitivity analysis: Persistence of OME: randomised by child (medium‐term); ICC = zero | 1 | 81 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.16, 0.56] |
| 5.11.1 Sensitivity analysis: assuming ICC of 0.0 (no correlation between ears) | 1 | 81 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.16, 0.56] |
| 5.12 Sensitivity analysis: Persistence of OME: randomised by ear (medium‐term); CC = 0.3 | 1 | Odds Ratio (IV, Random, 95% CI) | 0.66 [0.24, 1.83] | |
| 5.12.1 Sensitivity analysis: correlation coefficient = 0.3 | 1 | Odds Ratio (IV, Random, 95% CI) | 0.66 [0.24, 1.83] | |
| 5.13 Sensitivity analysis: Persistence of OME: randomised by ear (medium‐term); CC = 0.7 | 1 | Odds Ratio (IV, Random, 95% CI) | 0.66 [0.24, 1.83] | |
| 5.13.1 Sensitivity analysis: correlation coefficient = 0.7 | 1 | Odds Ratio (IV, Random, 95% CI) | 0.66 [0.24, 1.83] |
Comparison 6. Sensitivity analyses: Early ventilation tubes versus watchful waiting.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Sensitivity analysis: Mean final hearing threshold (air‐bone gap), randomised by child, analysed by ear (medium‐term); ICC = 1.0 | 1 | 87 | Mean Difference (IV, Random, 95% CI) | ‐1.18 [‐3.08, 0.72] |
| 6.1.1 Sensitivity analysis: assuming ICC of 1.0 (complete correlation between ears) | 1 | 87 | Mean Difference (IV, Random, 95% CI) | ‐1.18 [‐3.08, 0.72] |
| 6.2 Sensitivity analysis: Mean final hearing threshold (air‐bone gap), randomised by child, analysed by ear (medium‐term); ICC = zero | 1 | 160 | Mean Difference (IV, Random, 95% CI) | ‐1.18 [‐2.58, 0.22] |
| 6.2.1 Sensitivity analysis: assuming ICC of 0.0 (no correlation between ears) | 1 | 160 | Mean Difference (IV, Random, 95% CI) | ‐1.18 [‐2.58, 0.22] |
| 6.3 Sensitivity analysis: Mean final hearing threshold, randomised by child (long‐term); CC for Paradise 2007 of 0.3 | 3 | 633 | Mean Difference (IV, Random, 95% CI) | 0.37 [‐0.37, 1.11] |
| 6.3.1 Sensitivity analysis: CC for Paradise 2007 (left and right ear data combined) of 0.3 | 3 | 633 | Mean Difference (IV, Random, 95% CI) | 0.37 [‐0.37, 1.11] |
| 6.4 Sensitivity analysis: Mean final hearing threshold, randomised by child (long‐term); CC for Paradise 2007 of 0.7 | 3 | 633 | Mean Difference (IV, Random, 95% CI) | 0.35 [‐0.45, 1.16] |
| 6.4.1 Sensitivity analysis: CC for Paradise 2007 (left and right ear data combined) of 0.7 | 3 | 633 | Mean Difference (IV, Random, 95% CI) | 0.35 [‐0.45, 1.16] |
| 6.5 Sensitivity analysis: Persistent perforation, randomised by child (long‐term); ICC = 1.0 | 1 | 281 | Risk Ratio (M‐H, Random, 95% CI) | 2.73 [0.29, 25.97] |
| 6.5.1 Sensitivity analysis: ICC 1.0 (complete correlation between ears) | 1 | 281 | Risk Ratio (M‐H, Random, 95% CI) | 2.73 [0.29, 25.97] |
| 6.6 Sensitivity analysis: Persistent perforation, randomised by child (long‐term); ICC = zero | 1 | 562 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.73 [0.56, 13.43] |
| 6.6.1 Sensitivity analysis: ICC zero (no correlation between ears) | 1 | 562 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.73 [0.56, 13.43] |
| 6.7 Sensitivity analysis: Persistence of OME, randomised by child, measured by otoscopy (medium‐term); ICC = 1.0 | 1 | 87 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.11, 2.22] |
| 6.7.1 Sensitivity analysis: assuming ICC of 1.0 (complete correlation between ears) | 1 | 87 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.11, 2.22] |
| 6.8 Sensitivity analysis: Persistence of OME, randomised by child, measured by otoscopy (medium‐term); ICC = zero | 1 | 161 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.12, 1.34] |
| 6.8.1 Sensitivity analysis: assuming ICC of 0.0 (no correlation between ears) | 1 | 161 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.12, 1.34] |
| 6.9 Sensitivity analysis: Tympanosclerosis (long‐term); ICC = 1.0 | 1 | 281 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.27, 3.08] |
| 6.9.1 Sensitivity analysis: ICC 1.0 (full correlation between ears) | 1 | 281 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.27, 3.08] |
| 6.10 Sensitivity analysis: Tympanosclerosis (long‐term); ICC = zero | 1 | 562 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.36, 1.92] |
| 6.10.1 Sensitivity analysis ICC zero (no correlation between ears) | 1 | 562 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.36, 1.92] |
| 6.11 Sensitivity analysis: Adverse event: fibrosis (long‐term); ICC = 1.0 | 1 | 281 | Risk Ratio (M‐H, Random, 95% CI) | 0.46 [0.04, 4.97] |
| 6.11.1 Sensitivity analysis: ICC 1.0 (complete correlation between ears) | 1 | 281 | Risk Ratio (M‐H, Random, 95% CI) | 0.46 [0.04, 4.97] |
| 6.12 Sensitivity analysis: Adverse event: fibrosis (long‐term); ICC = zero | 1 | 562 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.15, 3.03] |
| 6.12.1 Sensitivity analysis: ICC zero (no correlation between ears) | 1 | 562 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.15, 3.03] |
| 6.13 Sensitivity analysis: Segmental atrophy (long‐term); ICC = 1.0 | 1 | 281 | Risk Ratio (M‐H, Random, 95% CI) | 2.92 [1.72, 4.96] |
| 6.13.1 Sensitivity analysis: ICC 1.0 (complete correlation between ears) | 1 | 281 | Risk Ratio (M‐H, Random, 95% CI) | 2.92 [1.72, 4.96] |
| 6.14 Sensitivity analysis: Segmental atrophy (long‐term); ICC = zero | 1 | 562 | Risk Ratio (M‐H, Random, 95% CI) | 2.85 [1.97, 4.13] |
| 6.14.1 Sensitivity analysis: ICC zero (no correlation between ears) | 1 | 562 | Risk Ratio (M‐H, Random, 95% CI) | 2.85 [1.97, 4.13] |
| 6.15 Sensitivity analysis: Retraction pocket with other abnormality (long‐term); ICC = 1.0 | 1 | 281 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.06, 14.43] |
| 6.15.1 Sensitivity analysis: ICC 1.0 (complete correlation between ears) | 1 | 281 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.06, 14.43] |
| 6.16 Sensitivity analysis: Retraction pocket with other abnormality (long‐term); ICC = zero | 1 | 562 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.06, 14.64] |
| 6.16.1 Sensitivity analysis: ICC zero (no correlation between ears) | 1 | 562 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.06, 14.64] |
| 6.17 Sensitivity analysis: Parent‐child interaction: Erickson child scale (medium‐term); CC = 0.3 | 1 | 165 | Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.53, ‐0.15] |
| 6.18 Sensitivity analysis: Parent‐child interaction: Erickson child scale (medium‐term); CC = 0.7 | 1 | 165 | Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.58, ‐0.10] |
| 6.19 Sensitivity analysis: Parent‐child interaction: Erickson parent scale (medium‐term); CC = 0.3 | 1 | 165 | Mean Difference (IV, Random, 95% CI) | ‐0.42 [‐0.64, ‐0.20] |
| 6.20 Sensitivity analysis: Parent‐child interaction: Erickson parent scale (medium‐term); CC = 0.7 | 1 | 165 | Mean Difference (IV, Random, 95% CI) | ‐0.42 [‐0.70, ‐0.14] |
6.5. Analysis.

Comparison 6: Sensitivity analyses: Early ventilation tubes versus watchful waiting, Outcome 5: Sensitivity analysis: Persistent perforation, randomised by child (long‐term); ICC = 1.0
6.6. Analysis.

Comparison 6: Sensitivity analyses: Early ventilation tubes versus watchful waiting, Outcome 6: Sensitivity analysis: Persistent perforation, randomised by child (long‐term); ICC = zero
6.7. Analysis.

Comparison 6: Sensitivity analyses: Early ventilation tubes versus watchful waiting, Outcome 7: Sensitivity analysis: Persistence of OME, randomised by child, measured by otoscopy (medium‐term); ICC = 1.0
6.8. Analysis.

Comparison 6: Sensitivity analyses: Early ventilation tubes versus watchful waiting, Outcome 8: Sensitivity analysis: Persistence of OME, randomised by child, measured by otoscopy (medium‐term); ICC = zero
6.9. Analysis.

Comparison 6: Sensitivity analyses: Early ventilation tubes versus watchful waiting, Outcome 9: Sensitivity analysis: Tympanosclerosis (long‐term); ICC = 1.0
6.10. Analysis.

Comparison 6: Sensitivity analyses: Early ventilation tubes versus watchful waiting, Outcome 10: Sensitivity analysis: Tympanosclerosis (long‐term); ICC = zero
6.11. Analysis.

Comparison 6: Sensitivity analyses: Early ventilation tubes versus watchful waiting, Outcome 11: Sensitivity analysis: Adverse event: fibrosis (long‐term); ICC = 1.0
6.12. Analysis.

Comparison 6: Sensitivity analyses: Early ventilation tubes versus watchful waiting, Outcome 12: Sensitivity analysis: Adverse event: fibrosis (long‐term); ICC = zero
6.13. Analysis.

Comparison 6: Sensitivity analyses: Early ventilation tubes versus watchful waiting, Outcome 13: Sensitivity analysis: Segmental atrophy (long‐term); ICC = 1.0
6.14. Analysis.

Comparison 6: Sensitivity analyses: Early ventilation tubes versus watchful waiting, Outcome 14: Sensitivity analysis: Segmental atrophy (long‐term); ICC = zero
6.15. Analysis.

Comparison 6: Sensitivity analyses: Early ventilation tubes versus watchful waiting, Outcome 15: Sensitivity analysis: Retraction pocket with other abnormality (long‐term); ICC = 1.0
6.16. Analysis.

Comparison 6: Sensitivity analyses: Early ventilation tubes versus watchful waiting, Outcome 16: Sensitivity analysis: Retraction pocket with other abnormality (long‐term); ICC = zero
6.17. Analysis.

Comparison 6: Sensitivity analyses: Early ventilation tubes versus watchful waiting, Outcome 17: Sensitivity analysis: Parent‐child interaction: Erickson child scale (medium‐term); CC = 0.3
6.18. Analysis.

Comparison 6: Sensitivity analyses: Early ventilation tubes versus watchful waiting, Outcome 18: Sensitivity analysis: Parent‐child interaction: Erickson child scale (medium‐term); CC = 0.7
6.19. Analysis.

Comparison 6: Sensitivity analyses: Early ventilation tubes versus watchful waiting, Outcome 19: Sensitivity analysis: Parent‐child interaction: Erickson parent scale (medium‐term); CC = 0.3
6.20. Analysis.

Comparison 6: Sensitivity analyses: Early ventilation tubes versus watchful waiting, Outcome 20: Sensitivity analysis: Parent‐child interaction: Erickson parent scale (medium‐term); CC = 0.7
Comparison 7. Sensitivity analyses: Ventilation tubes versus myringotomy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 Sensitivity analysis: Hearing returned to normal: VT versus laser myringotomy (medium‐term); ICC = 1.0 | 2 | 112 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.59, 2.48] |
| 7.1.1 Sensitivity analysis: ICC of 1.0 (complete correlation between ears) | 2 | 112 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.59, 2.48] |
| 7.2 Sensitivity analysis: Hearing returned to normal: VT versus laser myringotomy (medium‐term); ICC = zero | 2 | 166 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.62, 2.40] |
| 7.2.1 Sensitivity analysis: ICC of zero (no correlation between ears) | 2 | 166 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.62, 2.40] |
| 7.3 Sensitivity analysis: Mean final hearing threshold, randomised by child (short‐term); ICC = 1.0 | 1 | 78 | Mean Difference (IV, Random, 95% CI) | 0.20 [‐2.50, 2.90] |
| 7.4 Sensitivity analysis: Mean final hearing threshold, randomised by child (short‐term); ICC = zero | 1 | 156 | Mean Difference (IV, Random, 95% CI) | 0.20 [‐1.71, 2.11] |
| 7.5 Sensitivity analysis: Mean final hearing threshold (medium‐term); ICC = 1.0 | 1 | 78 | Mean Difference (IV, Random, 95% CI) | 0.80 [‐1.13, 2.73] |
| 7.5.1 Sensitivity analysis: ICC 1.0 (complete correlation between ears) | 1 | 78 | Mean Difference (IV, Random, 95% CI) | 0.80 [‐1.13, 2.73] |
| 7.6 Sensitivity analysis: Mean final hearing threshold (medium‐term); ICC = zero | 1 | 156 | Mean Difference (IV, Random, 95% CI) | 0.80 [‐0.57, 2.17] |
| 7.6.1 Sensitivity analysis: ICC zero (no correlation between ears) | 1 | 156 | Mean Difference (IV, Random, 95% CI) | 0.80 [‐0.57, 2.17] |
| 7.7 Sensitivity analysis: Persistent perforation (medium‐term); ICC = 1.0 | 1 | 82 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.06, 15.45] |
| 7.7.1 Sensitivity analysis: ICC = 1 (complete correlation between ears) | 1 | 82 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.06, 15.45] |
| 7.8 Sensitivity analysis: Persistent perforation (medium‐term); ICC = zero | 1 | 136 | Risk Ratio (M‐H, Random, 95% CI) | 2.00 [0.19, 21.54] |
| 7.8.1 Sensitivity analysis: ICC of zero (no correlation between ears) | 1 | 136 | Risk Ratio (M‐H, Random, 95% CI) | 2.00 [0.19, 21.54] |
| 7.9 Sensitivity analysis: Persistence of OME: VT versus laser myringotomy (short‐term); ICC = 1.0 | 1 | 82 | Risk Ratio (M‐H, Random, 95% CI) | 1.50 [0.46, 4.92] |
| 7.9.1 Sensitivity analysis: ICC of 1.0 (complete correlation between ears) | 1 | 82 | Risk Ratio (M‐H, Random, 95% CI) | 1.50 [0.46, 4.92] |
| 7.10 Sensitivity analysis: Persistence of OME: VT versus laser myringotomy (short‐term); ICC = zero | 1 | 136 | Risk Ratio (M‐H, Random, 95% CI) | 1.43 [0.58, 3.53] |
| 7.10.1 Sensitivity analysis: ICC of zero (no correlation between ears) | 1 | 136 | Risk Ratio (M‐H, Random, 95% CI) | 1.43 [0.58, 3.53] |
| 7.11 Sensitivity analysis: Persistence of OME: VT versus laser myringotomy (medium‐term); ICC = 1.0 | 1 | 82 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.17, 0.74] |
| 7.11.1 Sensitivity analysis: ICC of 1.0 (complete correlation between ears) | 1 | 82 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.17, 0.74] |
| 7.12 Sensitivity analysis: Persistence of OME: VT versus laser myringotomy (medium‐term); ICC = zero | 1 | 136 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.18, 0.60] |
| 7.12.1 Sensitivity analysis: ICC of zero (no correlation between ears) | 1 | 136 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.18, 0.60] |
| 7.13 Sensitivity analysis: Persistence of OME: VT versus laser myringotomy, randomised by ear (medium‐term); CC = 0.3 | 1 | Odds Ratio (IV, Random, 95% CI) | 0.27 [0.18, 0.42] | |
| 7.13.1 Sensitivity analysis: correlation coefficient of 0.3 assumed | 1 | Odds Ratio (IV, Random, 95% CI) | 0.27 [0.18, 0.42] | |
| 7.14 Sensitivity analysis: Persistence of OME: VT versus laser myringotomy, randomised by ear (medium‐term); CC = 0.7 | 1 | Odds Ratio (IV, Random, 95% CI) | 0.27 [0.21, 0.36] | |
| 7.14.1 Sensitivity analysis: correlation coefficient of 0.7 assumed | 1 | Odds Ratio (IV, Random, 95% CI) | 0.27 [0.21, 0.36] | |
| 7.15 Sensitivity analysis: Retraction of TM: VT versus laser myringotomy (medium‐term); ICC = 1.0 | 1 | 82 | Risk Ratio (M‐H, Random, 95% CI) | 3.50 [0.77, 15.85] |
| 7.15.1 Sensitivity analysis: ICC of 1.0 (complete correlation between ears) | 1 | 82 | Risk Ratio (M‐H, Random, 95% CI) | 3.50 [0.77, 15.85] |
| 7.16 Sensitivity analysis: Retraction of TM: VT versus laser myringotomy (medium‐term); ICC = zero | 1 | 136 | Risk Ratio (M‐H, Random, 95% CI) | 2.75 [0.92, 8.21] |
| 7.16.1 Sensitivity analysis: ICC of zero (no correlation between ears) | 1 | 136 | Risk Ratio (M‐H, Random, 95% CI) | 2.75 [0.92, 8.21] |
| 7.17 Sensitivity analysis: Otorrhoea: VT versus laser myringotomy (medium‐term); ICC = 1.0 | 1 | 82 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.33, 27.66] |
| 7.17.1 Sensitivity analysis: 1.0 (complete correlation between ears) | 1 | 82 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.33, 27.66] |
| 7.18 Sensitivity analysis: Otorrhoea: VT versus laser myringotomy (medium‐term); ICC = zero | 1 | 136 | Risk Ratio (M‐H, Random, 95% CI) | 2.50 [0.50, 12.44] |
| 7.18.1 Sensitivity analysis: ICC of zero (no correlation between ears) | 1 | 136 | Risk Ratio (M‐H, Random, 95% CI) | 2.50 [0.50, 12.44] |
7.3. Analysis.

Comparison 7: Sensitivity analyses: Ventilation tubes versus myringotomy, Outcome 3: Sensitivity analysis: Mean final hearing threshold, randomised by child (short‐term); ICC = 1.0
7.4. Analysis.

Comparison 7: Sensitivity analyses: Ventilation tubes versus myringotomy, Outcome 4: Sensitivity analysis: Mean final hearing threshold, randomised by child (short‐term); ICC = zero
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bernard 1991.
| Study characteristics | ||
| Methods | Single‐centre, parallel‐group RCT with 18 months of follow‐up Randomised by child |
|
| Participants |
Location: Canada, single centre Setting of recruitment and treatment: otolaryngology clinic at the Children’s Hospital of Eastern Ontario Study dates: not reported Sample size:
Participant (baseline) characteristics: Age, years:
Gender
Hearing loss at baseline
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
Intervention Bilateral myringotomy and insertion of VTs at the anterior‐inferior quadrant of the tympanic membrane by the same otolaryngologist 10 participants had Reuter bobbin ventilation tubes; the remaining 58 had Richard T ventilation tubes N = 68 Comparison Sulfisoxazole 75 mg/kg divided into 2 daily doses for 6 months N = 71 |
|
| Outcomes | Proportion with normal/impaired hearing (not extracted because of insufficient data) Mean final hearing threshold
Adverse events:
AOM episodes |
|
| Funding sources | "This work was funded by the National Health and Welfare Research and Development Program, Ottawa, Canada (grant 6606‐2944‐42). The sulfisoxazole was kindly provided by Hoffmann Laroche Canada Ltd." | |
| Declarations of interest | No declaration was made. | |
| Notes |
Research integrity checklist: No retraction notices identified Prospective registration not applicable (published before 2010) Baseline characteristics are not excessively similar Plausible loss to follow‐up reported No implausible results The number randomised to each group was not identical |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method used for sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | No attempt to conceal allocation was reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel is not reported. There is a strong possibility that participants and personnel could identify which treatment a participant received and hence change their behaviour as a result. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | The only outcome reported to have been conducted blind to treatment allocation was tympanometry, “tympanometry was conducted only at 18 months to keep the audiologist “blind” to treatment group”. However, the other outcomes of episodes of AOM and some adverse events, such as rash and nausea, are more likely to be influenced by lack of blinding. Thus, some outcomes are at low risk of detection bias and others are at high risk, giving an overall rating of high. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 8 of 68 (12%) participants in the VT group and 6 of 71 (8%) in the control group were lost to follow‐up. Reasons for loss to follow‐up were reported as participants moving out of town and parental refusal to attend follow‐up appointments. |
| Selective reporting (reporting bias) | Unclear risk | No protocol or trial registration was found. All outcomes specified in the published paper were reported. |
| Other bias | High risk |
|
D'Eredita 2006.
| Study characteristics | ||
| Methods | 2‐arm, parallel group, non‐blinded, single‐centre, non‐blinded RCT with 12 months follow‐up Randomised by child |
|
| Participants |
Location: Italy, single centre Setting of recruitment and treatment: Division of Paediatric Otolaryngology, in a tertiary paediatric care institution Study dates: January 2001 to January 2003 Sample size:
Participant (baseline) characteristics: Age (years):
Gender:
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
VT group: cold myringotomy, middle ear secretions were suctioned and a Teflon Shah tube inserted Laser myringotomy: laser myringotomy using diode laser, then middle ear secretions suctioned. Laser settings were 2 W power, 0.5 second pulse duration, with 5 pulses in the contact mode used with 600 mm thick fibre, which tapers to a 300 mm tip. Use of additional interventions: Following VT or LM, "middle ear secretions were suctioned. Ofloxacin 0.3% otic solution (Floxin otic1, Daiichi Pharmaceutical Corp., Montvale, NJ) was then instilled in each ear, and was prescribed for use at home thrice daily for 5 days." |
|
| Outcomes | Hearing returned to normal
Persistent perforation Otorrhoea |
|
| Funding sources | Not reported | |
| Declarations of interest | Not reported | |
| Notes |
Research integrity checklist: No retraction notices identified Prospective registration not applicable (published before 2010) Baseline characteristics show identical numbers of males/females No loss to follow‐up was reported Hearing was assessed as normal in all children at follow‐up, which may be implausible The number randomised to each group was identical, and no information on how randomisation was performed |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Thirty children ... with OME for at least 3 months duration were randomized into study (CDLM) and control (M&T) groups." No details provided. |
| Allocation concealment (selection bias) | Unclear risk | No details provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel is not reported. There is a strong possibility that participants and personnel could identify which treatment a participant received and hence change their behaviour as a result. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details provided. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The only missing data seems to be one of 60 parent‐completed questionnaires. No children were lost to follow‐up. |
| Selective reporting (reporting bias) | High risk | "Patients were scheduled for post‐operative office evaluation at day 10, 20, 30, 40, 60 and 80, and then at month 3, 4, 5, 6, 8, and 12. During each visit, myringotomy patency and tube status were assessed ….. All patients underwent a post‐operative age‐appropriate audiometric evaluation with tympanometry at month 6, and then again at 1‐year follow‐up." No protocol is available. The main outcome of middle ear ventilation is presented graphically. However, data presented in the text are sparse. Few outcome data are presented for tympanometry and audiometric testing at 6 and 12 months. |
| Other bias | Unclear risk | No details given as to how potential participants were identified for the study. The instructions given to parents on completing the questionnaire, the validity of the questionnaire and the reliability of outcome assessments were not reported. The risk of detection bias is therefore unclear. |
Dempster 1993.
| Study characteristics | ||
| Methods | Single‐centre RCT with 11 months follow‐up Randomised by child for adenoidectomy; subsequently, 1 ear was randomly selected to receive a ventilation tube Data of relevance for this review are for the comparison of unilateral ventilation tube versus no treatment in ears of the same individual (either with no additional surgery, or with a background of adenoidectomy) |
|
| Participants |
Location: UK, single centre Setting of recruitment and treatment: paediatric hospital clinic in Glasgow Study dates: August 1986 to February 1989 Sample size:
Participant (baseline) characteristics: Age, years, SD (range):
Gender
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
Intervention and comparisons Ventilation tube insertion:
Control group:
The comparison was made between the ears of the same individual (operated versus un‐operated side). Note that half of the children in this trial also underwent adenoidectomy. For the purposes of this review, we have displayed the data from children who underwent adenoidectomy separately from those who did not undergo adenoidectomy. However, the data have been pooled together, to show the overall effect of ventilation tubes (with or without adenoidectomy). |
|
| Outcomes | Proportion of ears with hearing returned to normal
Mean final hearing threshold (air conduction and air‐bone gap)
Mean change in hearing threshold Proportion of ears with persistence of OME
Adverse events:
|
|
| Funding sources | Not reported | |
| Declarations of interest | No declaration is made | |
| Notes |
Research integrity checklist: No retraction notices identified Prospective registration not applicable (published before 2010) No excessive similarities in baseline characteristics Plausible loss to follow‐up reported No implausible results The number randomised to each group was not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided on how the allocation sequence was generated. |
| Allocation concealment (selection bias) | Low risk | "These 78 children were then admitted to hospital within ten days and randomly allocated by a serially numbered envelope system..." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No information provided on blinding of participants and personnel. There is a strong possibility that participants and personnel could identify which treatment a participant received and hence change their behaviour as a result. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | “At six and 12 months post‐surgery, the presence or absence of otitis media in the non‐grommeted ear was record by the validated otoscopist who was blind as to whether adenoidectomy had been performed and by tympanometry.” There was no report of blinding for either tympanometric or audiometric assessment. The outcomes are not sufficiently objective to discount the possibility of ascertainment bias. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "Six children defaulted either at the six or 12 month assessment visits, leaving 72 (92 per cent) children with complete clinical, audiometric and tympanometric data for the pre‐operative and these post‐operative visits." Six of the 78 (8%) randomised children were lost to follow‐up. The distribution of those 6 across groups is not reported. Precise reasons for losses to follow‐up were not reported. It is therefore difficult to judge the potential for attrition bias. |
| Selective reporting (reporting bias) | Unclear risk | No protocol or trial registration was found. The published paper reports all expected outcomes. |
| Other bias | Unclear risk | It is unclear whether (for VT versus no treatment) comparisons were made within each individual child. The data are presented as if comparisons were made at whole trial arm level, as in a parallel‐group trial. There could therefore be a unit of analysis error, which could result in spuriously wide confidence intervals. |
Elkholy 2021.
| Study characteristics | ||
| Methods | Single‐centre, parallel‐group RCT with 1 year of follow‐up Randomised by child |
|
| Participants |
Location: Egypt, single centre Setting of recruitment and treatment: ENT and paediatric outpatient clinics at Al‐Azhar University Hospital, Cairo Study dates: September 2018 to March 2020 Sample size:
Participant (baseline) characteristics: Age, years (SD):
Sex
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
Intervention: Ventilation tube insertion (unclear if one or both ears, type of ventilation tube not stated) and adenoidectomy N = 20 Comparator: Adenoidectomy alone N = 20 |
|
| Outcomes | Persistence of OME at 2 weeks follow‐up | |
| Funding sources | Not stated | |
| Declarations of interest | The authors state that they have no conflict of interest | |
| Notes |
Research integrity checklist: No retraction notices identified Prospective registration was not identified Baseline characteristics are not excessively similar No reason is given for full follow‐up No implausible results were identified The number randomised to each group was identical, and there is no description of block randomisation |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | “Included children were randomly divided into two groups based on the consecutive number of enrollments those with odd number were included into group A while those of even number were included in group B”. Quasi‐randomised allocation. |
| Allocation concealment (selection bias) | High risk | “Included children were randomly divided into two groups based on the consecutive number of enrollments those with odd number were included into group A while those of even number were included in group B”. Quasi‐randomised allocation, allowing group allocation to be predicted. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and study personnel would have been aware of the group allocation. No blinding was used. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No indication is given that outcome assessors were blinded. Outcomes were assessed by study personnel, therefore we assume they were aware of the group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Full follow‐up is reported. |
| Selective reporting (reporting bias) | Unclear risk | No protocol was available to assess the intended reporting plan. |
| Other bias | High risk | Data were only available after 2 weeks of follow‐up, which is too short to fully assess the benefit of this intervention. Data from later time points were incompletely reported, precluding their inclusion in the review. |
Gates 1989.
| Study characteristics | ||
| Methods | Parallel‐group, 4‐arm, multicentre RCT with 2 years duration of follow‐up Randomised by child This study included a comparison of ventilation tubes, myringotomy and adenoidectomy. For the purposes of analysis, we have compared children who received ventilation tubes with those who received myringotomy, and also compared children who received ventilation tubes plus adenoidectomy to those who received myringotomy plus adenoidectomy. |
|
| Participants |
Location: USA, multicentre Setting of recruitment and treatment: hospital‐based otitis media study centre in the US. Inpatient and outpatient management. 14 participating otolaryngologists in 5 hospitals. Study dates: not reported Sample size:
Participant (baseline) characteristics: Age, years
Gender
Hearing loss at baseline
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
Intervention and comparisons Bilateral myringotomy
N = 127 VT
N = 150 Adenoidectomy and myringotomy
N = 151 Adenoidectomy and VT
N = 150 |
|
| Outcomes |
Primary outcomes relevant to this review:
Secondary outcomes relevant to this review:
|
|
| Funding sources | Supported by National Institutes of Health/National Institute of Neurological and Communicative Disorders and Stroke (NINCDS) contract NO1 NS 02328 and a grant in kind from Ross Laboratories | |
| Declarations of interest | None reported | |
| Notes |
Research integrity checklist: No retraction notices identified Prospective registration not applicable (published before 2010) Baseline characteristics are not excessively similar Plausible loss to follow‐up reported No implausible results The number randomised to each group was not identical |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "If informed consent was given, the child was assigned randomly by the project statistician, using tables of random numbers, to one of four groups...". This method would be expected to produce an adequate balance of prognostic factors across groups. However, two issues were reported, that might have interfered with the balance produced by randomisation: (1) parents of children were free after randomisation to choose an alternative treatment; and (2) there were fewer patients in group 1 because entry was stopped early at the request of the Safety and Data Monitoring Board. However, reported patient characteristics were adequately balanced across groups, suggesting that randomisation was adequate. |
| Allocation concealment (selection bias) | Low risk | "If informed consent was given, the child was assigned randomly by the project statistician, using tables of random numbers, to one of four groups...". As allocation was undertaken by the statistician, allocation was probably concealed. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Parents of children were informed of treatment allocation. Surgeons could not be blinded. There is a strong possibility that personnel could identify which treatment a participant received and hence change their behaviour as a result. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Despite otoscopists being blind to treatment allocation and outcome data, treatment allocation would be obvious in instances when a VT was visible. Otoscopic assessments have a degree of subjectivity. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Despite losses to follow‐up being of similar proportions across groups, and despite the characteristics of those losses being similar to those who were not lost to follow‐up, the very high attrition rate of 189/578 (33%) constitutes a major loss of data, exceeding the effect size for outcomes relating to persistence of effusion. |
| Selective reporting (reporting bias) | Low risk | No protocol was available, but pre‐specified outcomes were reported. |
| Other bias | High risk | The parents of 27 of the 491 randomised children (5.5%) chose a treatment other than that to which their child was randomised. Of 491 children, 240 (49%) received medical retreatment for chronic effusion. Of 491 children, 109 (22%) met the criteria for surgical retreatment. Given the number of children receiving retreatment, there is the strong possibility of contamination within the trial. |
Koopman 2004.
| Study characteristics | ||
| Methods | 2‐arm, multicentre, parallel‐group RCT with 6‐month follow‐up Randomised by ear |
|
| Participants |
Location: Netherlands, 7 sites Setting of recruitment and treatment: paediatric hospital Study dates: July 1999 to September 2001 Sample size: 208 children (416 ears)
Participant (baseline) characteristics: Age (mean (SD) years): 4.2 (2.3) (for all 208 children) Gender: males 108/208 (52%), females 100/208 (48%) Duration of disease: 6 months (range 3 to 12 months) Treatment used before trial entry: adenoidectomy, tonsillectomy and grommets in 24.5%, 11.1% and 23.6% of patients, respectively Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | All participants had one intervention in each ear Laser myringotomy: performed with a Sharplan CO2‐flashscanner laser using a handheld device and video screen (ESC Sharplan Medical Systems, Tel Aviv, Israel). The power setting varied from 7 to 20 W, and the diameter of the circular perforation varied from 1.8 to 2.6 mm, with an aim for the largest diameter possible (2.6 mm in 159 of 208 patients). The laser myringotomy was performed in the anteroinferior part of the tympanic membrane without aspiration of fluid. Ventilation tube: inserted using cold‐knife myringotomy, a ventilation tube with a 1.1 mm internal diameter (Donaldson) was used (94%). In case of OME with atelectasis of the middle ear, a Goode‐T Tube (6%) was inserted in the anteroinferior part of the tympanic membrane. Use of additional interventions: adenoidectomy in combination with tonsillectomy was performed on 16 children. Otorrhoea persisting for more than 1 week was treated by ear drops consisting of either dexamethasone/framycetin/gramicidin or ofloxacin, depending on the culture, whereas otorrhoea with fever was treated with oral antibiotics only (amoxicillin). During administration of medication, the child was seen weekly until recovery. |
|
| Outcomes | Proportion of children with persistence of OME Adverse events
|
|
| Funding sources | The Sophia Foundation For Medical Research and The Revolving Fund Sophia Children’s Hospital, Erasmus Medical Centre, Rotterdam, Theia Foundation, and Silver Cross Company | |
| Declarations of interest | "The authors declare that there is no conflict of interest of any kind in this study" | |
| Notes |
Research integrity checklist: No retraction notices identified Prospective registration not applicable (published before 2010) Baseline characteristics are not relevant (split‐body trial) Plausible loss to follow‐up reported No implausible results The number randomised to each group was identical as this was a split‐body trial |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Assignment of the side for laser myringotomy or tube insertion was made randomly by computer‐generated lists in balanced blocks of six to assure an even distribution of surgical procedure for left and right ears." |
| Allocation concealment (selection bias) | Unclear risk | No method of allocation concealment was reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Surgeons could not be blinded. There is a strong possibility that personnel could identify which treatment a participant received and hence change their behaviour as a result. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information provided on blinding of outcome assessors. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The rate of loss to follow‐up was high: "A total of 55 (26%) children quit the study (41 lost to follow‐up, 14 failures). The frequency of control visits was the main reason for discontinuation of follow‐up." There was no detailed account of reasons for losses to follow‐up. The proportion of missing outcomes (26%) compared with observed event risk (e.g. proportion effusion‐free after laser myringotomy at 3 months 37.1%) could be enough to induce clinically relevant bias in intervention effect estimate. |
| Selective reporting (reporting bias) | High risk | One or more outcomes of interest in the review (e.g. otorrhoea and perforation) are reported incompletely, and thus cannot be entered in a meta‐analysis. |
| Other bias | Unclear risk | A follow‐up period of 6 months may be too short to assess a clinically meaningful outcome of persistence of OME. |
Maw 1983.
| Study characteristics | ||
| Methods | Randomised, parallel‐group, single‐blind controlled trial of adenotonsillectomy or adenoidectomy or no pharyngeal surgery, with 3 years of follow‐up Randomised by ear (split‐body randomisation was used to place a VT in 1 ear of each participant) For the purposes of this review, we have included data comparing the ear with the ventilation tube to the un‐operated, contralateral ear in the same participant. Only participants who did not receive additional surgery were included in this analysis. |
|
| Participants |
Location: UK, single centre Setting of recruitment and treatment: UK inpatient and ENT outpatient setting in Bristol Study dates: recruitment started in July 1979; end date not reported Sample size: Note that this is the sample size for relevant arms included in this review, not the total sample size for the whole trial (N = 192)
Participant (baseline) characteristics: Age, years, SD (range): 5.31 years (SD 1.22) Gender: 32 males (57%), 24 females (43%) Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
Intervention and comparisons Ventilation tube insertion:
Control:
Background treatments: no additional surgery was used for participants included in this review. Other participants in the study did undergo adenoidectomy or adenotonsillectomy. |
|
| Outcomes | Final hearing threshold (operated and un‐operated ear) | |
| Funding sources | Not reported | |
| Declarations of interest | Not reported | |
| Notes |
Research integrity checklist: No retraction notices identified Prospective registration not applicable (published before 2010) No excessive similarities in baseline characteristics Plausible loss to follow‐up reported. No implausible results The number randomised to each group was similar but not identical |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "From tables of random numbers, the children were allocated as follows: adenotonsillectomy 47; adenoidectomy 47; no‐surgery 56." |
| Allocation concealment (selection bias) | Unclear risk | The method of concealment is not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Surgeons could not be blinded. There is a strong possibility that personnel could identify which treatment a participant received and hence change their behaviour as a result. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | "The accuracy of A. R. M. (the clinical investigator) in otoscopic diagnosis has been assessed and reported previously." The lead researcher undertook the pneumatic otoscopy. Blinding of audiometric and tympanometric assessments was not reported and therefore assessments are unlikely to be blinded. Audiometry is open to subjective assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The attrition rate was similar in each group of interest (24% and 23% at 1 year, and 53% and 52% at 3 years, in the adenoidectomy plus unilateral VT group and the unilateral VT group, respectively). The reasons for attrition were largely unreported and could have been related to the outcomes of interest. |
| Selective reporting (reporting bias) | Low risk | No published protocol has been found, but it appears that all pre‐specified outcomes are reported. |
| Other bias | Low risk | None identified. |
Maw 1999.
| Study characteristics | ||
| Methods | Parallel‐group, single‐centre, 2‐arm RCT with up to 7 years of follow‐up Randomised by child |
|
| Participants |
Location: UK, single centre Setting of recruitment and treatment: paediatric hospital clinic in Bristol Study dates: November 1993 to January 1996 Sample size:
Participant (baseline) characteristics: Age, years, SD (range):
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
Intervention and comparisons Ventilation tubes: Surgery was by insertion of bilateral ventilation tubes (type of tube not stated). In children with clinical evidence of nasal obstruction because of adenoid enlargement, adenoidectomy was also done. In the early‐surgery group, if hearing difficulty returned, otoscopy showed recurrence of effusions, with type B or C2 tympanograms during follow‐up, tube reinsertion would be performed, if desired, within 6 weeks. Watchful waiting Participants were advised that ‐ if the need for an operation was recognised at the 9‐month assessment ‐ surgery would be done within 6 weeks of that date. Approximately 21% of participants received surgery before 9 months of follow‐up. By 18 months, only 15% of participants in this group had not been listed for, or already received, surgery. |
|
| Outcomes | Final hearing threshold (right ear, left ear, best ear, worst ear)
Proportion of children with persistence of OME by otoscopy and tympanometry in one or both ears, and in the best ear Receptive language skills (Reynell Language Scales) Speech development (Reynell Language Scales) Cognitive development (Griffiths Mental Development Scales) Psychological outcomes (Goodman) Listening skills |
|
| Funding sources | “The trial was funded by the South and West NHS Research and Development Directorate.” | |
| Declarations of interest | No declaration is made | |
| Notes |
Research integrity checklist: No retraction notices identified Prospective registration not applicable (published before 2010) No excessive similarities in baseline characteristics Plausible loss to follow‐up reported No implausible results The number randomised to each group was not identical |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Randomisation was performed using a random number table to generate numbers in an office distant from the hospital”. |
| Allocation concealment (selection bias) | Low risk | “Numbers were placed in sealed envelopes”. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Surgeons could not be blinded. There is a strong possibility that personnel could identify which treatment a participant received and hence change their behaviour as a result. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “Tympanometry and hearing tests at randomisation and 9‐month and 18‐month follow‐up visits were done by audiological scientists or technicians who were masked to the children’s treatment status”. "Audiological Scientists, Reynell Language and Griffith Mental Development scale testers were blind to allocation of treatment group. The Richman Behaviour Checklist was completed by parents.” Therefore, there is the potential for psychological outcomes (those assessed using the Richman Behaviour Checklist and behaviour total scores as reported by parents) to have been influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Twenty participants were lost to follow‐up (4 in the VT group, 16 in the watchful waiting group) by final follow‐up when participants were 7 years of age. It is unclear whether it is the same participants who were lost to follow‐up at each follow‐up period, as the number of participants for whom outcome data are available fluctuates throughout the years. There is an imbalance in numbers of missing data across intervention groups, and there is likely to be an imbalance in reasons for missing data across intervention groups. For example, the authors note that “mothers of lower educational achievement provided complete data on these factors less often than other mothers” (Hall 2009, p 17). Additionally, the authors note that “the validity of the results needs to be considered in the light of a number of factors […] loss to follow‐up – although relatively low (9% in the early surgery and 18% in the watchful waiting group) – could introduce some degree of bias”. |
| Selective reporting (reporting bias) | Unclear risk | No published protocol or trial registrations were found. For the outcome mean final hearing threshold for best ears at 9 months follow‐up, 2 different sets of data at the same follow‐up time point are presented in Maw 1999 vs Maw 2000. The authors note data were available for more children in Maw 2000 than in Maw 1999 for some outcomes, but it is unclear why this is the case. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Paradise 2007.
| Study characteristics | ||
| Methods | Multicentre RCT with 11 years of follow‐up Randomisation by child |
|
| Participants |
Location: multiple sites in the USA Setting of recruitment and treatment: recruited from 2 urban hospitals, 2 small‐town/rural and 4 suburban private paediatric practices Study dates: recruitment from May 1991 to December 1995 Sample size:
Participant (baseline) characteristics: Age, months: mean 15 months for the whole cohort (median 14 months) Gender:
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
Intervention and comparisons Early treatment (VT) Children were scheduled to have ventilation tubes inserted as soon as possible (n = 216 randomised; 195 completed follow‐up and 164 had received ventilation tubes by the age of 9 to 11 years). The type of ventilation tube was not stated. Watchful waiting/late treatment (VT) Children were scheduled to have ventilation tubes after a 6‐month delay (if bilateral effusion persisted) or after a 9‐month delay (if unilateral effusion persisted) (n = 213 randomised; 196 completed follow‐up and 88 had received ventilation tubes by the age of 9 to 11 years). |
|
| Outcomes | Proportion of children with hearing returned to normal
Mean final hearing threshold (left ear, right ear) Persistence of OME (none, unilateral, bilateral, indeterminate) Adverse event:
Receptive language skills Speech development Cognitive development Psychological development Listening skills Parental stress |
|
| Funding sources | “Supported by grants from the National Institute of Child Health and Human Development and the Agency for Healthcare Research and Quality (HD26026 and HD42080), from the University of Pittsburgh Competitive Medical Research Fund, and from the Children’s Hospital of Pittsburgh Research Advisory Committee and by gifts from GlaxoSmithKline and Pfizer.” | |
| Declarations of interest | None declared | |
| Notes | No retraction notices identified Prospective registration not applicable (published before 2010) No excessive similarities in baseline characteristics Plausible loss to follow‐up reported No implausible results Block randomisation was used to ensure balanced allocation to the 2 groups |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Assignments were made by designated nonclinical staff members using separate, computer‐generated lists of random numbers.” |
| Allocation concealment (selection bias) | Unclear risk | “Assignments were made by designated nonclinical staff members using separate, computer‐generated lists of random numbers.” It is unclear the role these staff members played in the study and thus it is difficult to judge whether their knowledge of the sequence influenced allocation and had a possible effect on outcomes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Surgeons could not be blinded. There is a strong possibility that personnel could identify which treatment a participant received and hence change their behaviour as a result. The parents of the child would know the allocation and it might affect their behaviour or decision to use adjunctive treatments. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Examiners and analysts carrying out developmental tests were unaware of the children’s medical histories and treatment group assignments at follow‐up when participants were 9 to 11 years of age, but no information about blinding of other outcome assessors, such as audiologists, is provided. Examiners, transcriptionists and analysts were blinded to the children’s health histories including receipt of tympanostomy tubes at follow‐up when participants were 6 years of age, but no information about blinding of other outcome assessors, such as audiologists, is provided. All otomicroscopic examinations were conducted by a paediatric otolaryngologist who was unaware of children’s history and study group assignment, and audiologists were unaware of children’s otoscopic diagnoses at follow‐up when participants were 5 years of age. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | At age 3, 206 of 216 (95%) who had early treatment underwent developmental tests and 196 of 213 (92%) who had late treatment underwent developmental tests. At age 4, 204 of 216 (94%) who had early treatment underwent developmental tests and 193 of 213 (91%) who had late treatment underwent developmental tests. No reasons are given for attrition/exclusion but low levels. |
| Selective reporting (reporting bias) | Low risk | There is a trial registration for study of 9‐ to 11‐year olds. It appears that all pre‐specified outcomes are reported for each time of assessment. |
| Other bias | Low risk | There does not appear to be any other source of bias. |
Popova 2010.
| Study characteristics | ||
| Methods | Parallel‐group, single‐centre RCT with 12‐month follow‐up Randomisation by child |
|
| Participants |
Location: Bulgaria, single centre Setting of recruitment and treatment: ENT department of University Hospital "Queen Jovanna", Sofia, Bulgaria Study dates: 2007 to 2009 Sample size:
Participant (baseline) characteristics: Age, years, SD:
Gender
Hearing threshold at baseline
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
Intervention and comparisons Adenoidectomy and VT
N = 42 Adenoidectomy and myringotomy
N = 36 |
|
| Outcomes | Mean final hearing threshold Proportion of children with persistence of OME Adverse events:
Episodes of AOM |
|
| Funding sources | No details are given | |
| Declarations of interest | "Authors report no conflict of interest in the publication of the article" | |
| Notes |
Research integrity checklist: No retraction notices identified Prospective registration was not identified (published in 2010) Baseline characteristics are not excessively similar Plausible loss to follow‐up reported No implausible results The number randomised to each group was not identical |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details are given. |
| Allocation concealment (selection bias) | Unclear risk | No details are given. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Surgeons could not be blinded. There is a strong possibility that personnel could identify which treatment a participant received and hence change their behaviour as a result. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding of outcome assessment is reported, so we assume no blinding and therefore a high risk of bias. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | “Ninety patients with bilateral OME were enrolled initially in our study. Seventy‐eight of them (156 ears) attended all of the appointed examinations during the whole follow‐up period and remaining twelve were excluded.” Data are not available for these 12 participants, including which intervention they received. It is possible that the reason for missing data for these participants could be related to true outcome. |
| Selective reporting (reporting bias) | Unclear risk | No protocol or trial registration has been found. The authors did not clearly state the outcomes they would be assessing in the study. |
| Other bias | High risk | “All 5 patients with recurrence from the A+M group were treated conservatively with medications as described previously [9] and subsequently on one of them a tympanostomy tube was inserted, which followed to his exclusion from the A+M group.” Thus, this study appears to have adopted a per protocol analysis. |
Rach 1991.
| Study characteristics | ||
| Methods | Single‐centre RCT with 6‐month follow‐up, and additional follow‐up of developmental outcomes for up to 4 years Randomisation by child |
|
| Participants |
Location: Netherlands, single centre Setting of recruitment and treatment: recruitment from GP surgeries, trial run from ENT clinic Study dates: not reported Sample size:
Participant (baseline) characteristics: Age, years, SD (range):
Gender
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
Ventilation tubes Standard (silicone ventilating tubes, Donaldson design). Insertion was performed bilaterally under general anaesthetic in the antero‐inferior quadrant of the tympanic membrane N = 22 Comparator No treatment N = 21 Note that some participants in this group may have undergone ventilation tube placement during the extended follow‐up period (after a 6‐month delay, and up to 7 to 8 years of age). Results until 6 months of follow‐up are therefore included in Comparison 1 (VT versus no treatment) but results from extended follow‐up are included in Comparison 2 (VT versus watchful waiting). |
|
| Outcomes | Proportion of ears with persistence of OME Adverse events:
Receptive language skills (Reynell)
Expressive language skills (Reynell)
|
|
| Funding sources | This study was supported by a grant from the Dutch Prevention fund (no. 28‐924). | |
| Declarations of interest | None declared | |
| Notes |
Research integrity checklist: No retraction notices identified Prospective registration not applicable (published before 2010) No baseline characteristics are reported, therefore unable to assess Loss to follow‐up is unclear, but may be zero No implausible results Numbers allocated to each group are similar but not identical |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomized allocation was performed for the first five children entering the trial; each subsequent child was allocated to the treatment group which would lead to the smallest imbalance of the four determinants noted above." As the process of minimisation is described, this is low risk. |
| Allocation concealment (selection bias) | Unclear risk | No details on allocation concealment provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Surgeons could not be blinded. There is a strong possibility that personnel could identify which treatment a participant received and hence change their behaviour as a result. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | A rating of low risk of bias would be appropriate for grading the certainty of evidence for developmental test outcomes (receptive language skills and expressive language skills), because the authors report that “All tests were performed and scored by one speech therapist, without previous knowledge of the child's history”. However, there was no report of blinding to treatment allocation for tympanometry. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Information on loss to follow‐up is not reported, although the data reported indicate no loss to follow‐up. However, the authors note “The total group from whom two language tests could be obtained comprised 52 children”, indicating that only participants in the original prospective longitudinal study who had the necessary data at baseline and follow‐up were included in this study. Therefore, there is potential that participants who were not available for follow‐up were excluded from the study, although this is not reported in the exclusion criteria (criteria only list “not visiting the GP after referral” and “no referral by the GP to the ENT outpatient clinic” as exclusion reasons related to this issue). Authors do not give any further information, so it is difficult to judge the potential for attrition bias. |
| Selective reporting (reporting bias) | Low risk | There is no published protocol, but it does not appear that selective reporting has occurred. |
| Other bias | Unclear risk | A follow‐up period of 6 months is too short a time to show a real difference in language development, although other outcomes may be unaffected. |
Rovers 2000.
| Study characteristics | ||
| Methods | Multicentre, randomised, controlled, parallel‐group, open trial with 12 months of follow‐up Randomised by child |
|
| Participants |
Location: Netherlands, multicentre study Setting of recruitment and treatment: 13 ENT hospital outpatient clinics in the Netherlands Study dates: recruitment from 1996 to 1998 Sample size:
Participant (baseline) characteristics: Age, years, SD (range):
Gender
Mean hearing threshold
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
Ventilation tube insertion Bevel Bobbins ventilation tubes were used Number randomised: 93; number completed: 90 Watchful waiting 10 children received treatment with ventilation tubes during the follow‐up period (11.6%) Number randomised: 94; number completed: 86 |
|
| Outcomes | Change in hearing threshold
Difference in hearing improvement Persistence of OME Adverse events
Receptive language skills (Reynell)
Speech development (Schlichting)
Erickson scale of parent‐child interaction
Generic HRQoL
|
|
| Funding sources | The Dutch Investigative Medicine Fund of the National Health Insurance Board | |
| Declarations of interest | None reported | |
| Notes |
Research integrity checklist: No retraction notices identified Prospective registration not applicable (published before 2010) Baseline characteristics are similar, but this is to be expected due to the balanced allocation procedure Plausible loss to follow‐up reported No implausible results Balanced allocation was reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “To increase comparability at baseline, a balanced allocation procedure was employed with five balancing factors: sex, age, season at randomization, educational level of the mother, and hospital.” Minimisation was used. |
| Allocation concealment (selection bias) | Unclear risk | The method of concealment is not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Surgeons could not be blinded. There is a strong possibility that personnel could identify which treatment a participant received and hence change their behaviour as a result. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | “During the trial, tympanometry and audiometry were performed by experienced audiologists (who were not blinded to the assignment of a child).” Some outcomes are likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Follow‐up of 176/187 (94%), which is a high percentage; however, 8 were lost from the WW group and only 3 from the VT group. Furthermore 10 from the WW group went on to have VT. |
| Selective reporting (reporting bias) | Unclear risk | No protocol was available for comparison. |
| Other bias | Low risk | No protocol was available, but all pre‐specified outcomes were reported. |
Ruckley 1988.
| Study characteristics | ||
| Methods | 2‐arm, parallel‐group, single‐centre RCT with 3 months follow‐up Randomised by ear |
|
| Participants |
Location: Scotland, single centre Setting of recruitment and treatment: hospital Study dates: not reported Sample size: 40 children (80 ears)
Participant (baseline) characteristics: Age: 5 years 10 months (range 4 to 9 years) Gender: males 23/40 (58%), females 17/40 (42%) Duration of disease: ≥ 3 months Baseline hearing loss (measured as the mean air‐bone gap for the frequencies 0.25 kHz, 0.5 kHz, 1 kHz, 2 kHz and 4 kHz): VT 21.4 dB (SD 6.5) thermal myringotomy group 21.0 dB (SD 6.6) Inclusion criteria:
Exclusion criteria: not reported |
|
| Interventions | All participants received one intervention in each ear Ventilation tube: myringotomy, with a conventional myringotomy knife, followed by aspiration of fluid and insertion of a Shepherd grommet Thermal myringotomy: using the Xomed thermovent device, followed by fluid aspiration Use of additional interventions: all participants received adenoidectomy |
|
| Outcomes |
Primary outcome: hearing assessed using air conduction and bone conduction Secondary outcomes: appearance of tympanic membranes, patency of VT and thermal perforation, any otological symptoms, recurrence of middle ear fluid |
|
| Funding sources | Not reported | |
| Declarations of interest | Not reported | |
| Notes |
Research integrity checklist: No retraction notices identified Prospective registration not applicable (published before 2010) Baseline characteristics are not relevant (this is a split‐body trial) Plausible loss to follow‐up reported No implausible results The number randomised to each group was identical, as this was a split‐body trial |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Immediately prior to surgery a coin was spun in order to determine in a random fashion which ear was to be treated by thermal myringotomy." |
| Allocation concealment (selection bias) | Low risk | The need for allocation concealment is obviated by using a simple method of randomisation at the point of intervention. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Surgeons could not be blinded. There is a strong possibility that personnel could identify which treatment a participant received and hence change their behaviour as a result. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding is reported and the authors do not clearly state who undertook outcome assessments. Otoscopy is sufficiently subjective for there to be a high risk of detection bias. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "Of the 40 children who entered the study complete results were obtained in 36. Four children failed to attend for regular post‐operative review and were not included in the final results." As this study randomised by ear, loss of outcome data was equal for each intervention group. We do not know if the reasons for loss to follow‐up were due to the intervention. |
| Selective reporting (reporting bias) | High risk | A study protocol is not available. One or more outcomes of interest in the review, e.g. otalgia, are reported incompletely. |
| Other bias | High risk | A follow‐up period of 3 months is too short a time to assess the effect of the intervention. |
Sujatha 2015.
| Study characteristics | ||
| Methods | Randomised, parallel‐group, open trial with 12 months of follow‐up Randomised by child |
|
| Participants |
Location: India, single centre Setting of recruitment and treatment: tertiary care hospital in Kerala Study dates: January 2013 to December 2013 Sample size:
Participant (baseline) characteristics: Age (years): mean age 5.8 years (SD 1.8) Gender: 22 males (44%), 28 females (56%) Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | Ventilation tube group:
Myringotomy group:
Interventions used in both groups:
|
|
| Outcomes | Final hearing threshold at 12 months (air‐bone gap) Tympanic membrane perforation Persistence of OME at 12 months Adverse events |
|
| Funding sources | Kerala State board of medical research | |
| Declarations of interest | No competing interests are declared | |
| Notes |
Research integrity checklist: No retraction notices or expressions of concern were identified No prospective trial registration was identified Baseline characteristics were not excessively similar Full follow‐up was reported No implausible results were noted Equal numbers of participants were allocated to each group |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “They were randomized into group A and group B as per randomisation table.” |
| Allocation concealment (selection bias) | Unclear risk | No information on how/whether the allocation sequence was concealed. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | There was no mention of whether the trial was open or blinded. It is therefore assumed to be open. Outcomes could be influenced by a lack of blinding. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | There was no mention of whether the trial was open or blinded. It is therefore assumed to be open. Outcomes could be influenced by a lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Full follow‐up was reported. |
| Selective reporting (reporting bias) | Unclear risk | A trial protocol was not available for assessment. |
| Other bias | Unclear risk | Potential detection bias, as the accuracy and reliability of tympanometry, PTA and otoscopy were not reported. |
Tao 2020.
| Study characteristics | ||
| Methods | 2‐arm, randomised, parallel‐group, open, controlled trial with 12 months of follow‐up Randomised by child |
|
| Participants |
Location: China, single centre Setting of recruitment and treatment: ENT Department, Guangzhou Women and Children's Medical Center Study dates: January 2016 to June 2018 Sample size:
Participant (baseline) characteristics: Age (years): VT plus adenoidectomy mean 7.0 (SD 1.9) years; LM plus adenoidectomy mean 7.2 (SD 2.4) years Gender: VT males 42/87 (48%), females 45/87 (52%); LM males 42/82 (51%), females 40/82 (49%) Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
Ventilation tube:
Myringotomy:
Interventions administered to both groups:
|
|
| Outcomes | Persistent perforation Persistence of OME ‐ these data were not used in the review, as data were only reported for one group at 3 months follow‐up, and data from later time points will be affected by the use of different additional treatments in each arm. Adverse events |
|
| Funding sources | Not reported | |
| Declarations of interest | — | |
| Notes |
Research integrity checklist: No retraction notices or expressions of concern were noted No prospective trial registration was identified Baseline characteristics were not excessively similar between the two groups Plausible loss to follow‐up was reported No implausible results were found Different numbers of participants were allocated to each group |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “All patients were randomly divided into two groups, namely Group A and B, according to the sequence generated by a computer program when they were admitted to the hospital.” |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to assess. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | There was no report of blinding. Blinding of patients and personnel may not have been feasible for operative interventions. However, lack of blinding could influence outcomes. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | There was no report of blinding. Blinding of patients and personnel may not have been feasible for operative interventions. However, lack of blinding could influence outcome interpretation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition rate. |
| Selective reporting (reporting bias) | Unclear risk | No protocol was available to assess. |
| Other bias | Unclear risk | Insufficient detail in the report to assess whether an important risk of bias exists. |
TARGET 2000.
| Study characteristics | ||
| Methods | 3‐arm, multicentre, parallel‐group RCT with 2‐year follow‐up Randomised by child For this review we have included data relevant to the comparison of ventilation tube insertion with watchful waiting. Additional data on adenoidectomy are relevant to a companion review (MacKeith 2023). |
|
| Participants |
Location: UK, 11 sites Setting of recruitment and treatment: otorhinolaryngology departments Study dates: April 1994 to January 1998 Sample size:
Participant (baseline) characteristics: Age (mean (SD) months): VTs 62.5 (10.2), VTs + ad 64.5 (10.3), WW 62.9 (10.4) Gender: VTs males 60/126 (48%), females 66/126 (52%); VTs + ad males 61/128 (48%), females 67/128 (52%); WW males 62/122 (51%), females 60/122 (49%) Hearing threshold at baseline (at visit 2) (mean (SD) dB): VTs 32.2 (6.0), VTs + ad 31.7 (6.4), WW 33.5 (6.4) AOM episodes (> 6 per year): VTs 5/126 (4%), VTs + ad 5/127 (4%), WW 8/122 (7%) Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
Bilateral VTs: Bilateral Shepard VTs were inserted following myringotomy and fluid aspiration Bilateral VT with adenoidectomy: Bilateral ventilation tubes were inserted, as above, and adenoidectomy was performed by curettage Watchful waiting: Children were not allocated to any surgery. However, over the 2‐year follow‐up period, 57% of participants in this group actually underwent surgery. |
|
| Outcomes | Mean final hearing threshold
Mean change in hearing from baseline Adverse events:
|
|
| Funding sources | Medical Research Council; Trial Registration Number: ISRCTN35793977 | |
| Declarations of interest | Authors reported "None to declare" | |
| Notes |
Research integrity checklist: No retraction notices identified Prospective registration not applicable for earliest publications (published before 2010). Registration was noted for the most recent publication. Baseline characteristics were not excessively similar between the groups Plausible loss to follow‐up was reported No implausible results Numbers allocated to each group are not identical |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "For each centre, the first five children were randomised according to a computer‐generated random number sequence. Thereafter, the minimisation procedure balanced the treatment allocations across four dichotomous factors: boy, girl; <5.25, >5.25 years old at initial visit; manual, non‐manual occupation of head of household and baseline hearing <25 dB HL, >25 dB HL." |
| Allocation concealment (selection bias) | Low risk | "Randomisation was performed by telephone call from the nurse ⁄ research assistant to the statistician at the MRC Institute of Hearing Research and allocation immediately communicated to the parent,” and “This basis of minimisation was not divulged to centres and may be regarded as completely concealed.” |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No information provided on blinding of participants and personnel. There is a strong possibility that participants and personnel could identify which treatment a participant received and hence change their behaviour as a result. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “Audiometry was performed by audiologists, independently of the otolaryngologist and research nurse. Clinic pressures meant that these testers, whilst not blinded in the strictest sense, were not aware of the child’s allocation, nor in a position to be influenced by such information were it present.” |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Losses to follow‐up were 55/376 randomised (14.6%) overall with 19/122 (15.6%) in the medical management group, 17/126 (13.5%) in the VT group and 19/128 (14.8%) in the VT + Ad group. Complete data were available for only 76/122 (62.3%), 85/126 (67.5%) and 92/128 (71.9%) in the medical management, VT and VT + Ad groups, respectively. Reasons for loss to follow‐up after randomisation were not reported. |
| Selective reporting (reporting bias) | Unclear risk | The trial entry on ISRCTN registry states that “general health, economic impact, behavioural assessment and quality of life” would be assessed. Data on these are published (no economic data) but no details given of the scales used to assess the outcomes. |
| Other bias | High risk | The trial registration was retrospectively published, raising the possibility of publication bias. In addition, this was an MRC funded, multicentre trial and yet not all outcomes stated in the trial registration were published. |
To 1984.
| Study characteristics | ||
| Methods | 2‐arm RCT with at least 12 months follow‐up (mean follow‐up of 2 years (range 1 to 5 years)) Randomised by ear |
|
| Participants |
Location: UK Setting of recruitment and treatment: no details given Study dates: March 1976 to June 1982 Sample size: 54 children
Participant (baseline) characteristics: Age (mean): 7 years and 6 months (range 47 months to 14 years) Gender: males 29/54 (54%), females 25/54 (46%) Duration of disease: not reported but mean follow‐up before operation 7.2 months Treatment used before trial entry: unspecified "medical measures" Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
Ventilation tube: insertion of a Shepherd grommet; 22 in the better ear* (9 right and 13 left), 25 in the worse ear* (11 right and 14 left), 7 in which both ears were equal (2 right and 5 left) (*where these refer to comparisons of audiograms) Myringotomy: "most participants" had myringotomy in the contralateral ear Use of additional interventions: all participants received adenoidectomy if adenoids had not previously been removed (n = 9), and were present (n = 1 no adenoids) |
|
| Outcomes | Primary outcome: hearing level Secondary outcomes: adverse events: perforation, retraction segments, tympanosclerosis | |
| Funding sources | Not reported | |
| Declarations of interest | No declarations are made | |
| Notes |
Research integrity checklist: No retraction notices identified Prospective registration not applicable (published before 2010) Baseline characteristics are not relevant (split‐body trial) No loss to follow‐up was reported No implausible results The number randomised to each group was identical as this was a split‐body trial |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Those who did not respond were submitted to the removal of adenoids (if present) and the insertion of a Shepard grommet in one ear chosen at random.” No information is provided about the process used for randomly selecting an ear. |
| Allocation concealment (selection bias) | Unclear risk | "Those who did not respond were submitted to the removal of adenoids (if present) and the insertion of a Shepard grommet in one ear chosen at random." No information is provided about concealment of allocation. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Surgeons could not be blinded. There is a strong possibility that personnel could identify which treatment a participant received and hence change their behaviour as a result. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | “The patients were under the care of 2 consultants working independently and the results were reviewed by an independent observer.” It is unclear if this means that the observer was blinded to group allocation, or was simply a separate assessor. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Follow‐up appears to be 100% at 12 months for hearing threshold data. Adverse events are reported at later follow‐up times but no information is provided on how many had dropped out. It appears that the number of dropouts after 1 year could have been many: "Twenty‐three children have been discharged from follow‐up having been well and with normal ears for about a year; some of them have had further surgical treatment on one or both sides. The mean follow‐up for this group is 27 months." For adverse event outcomes, the risk of bias for this domain is high. |
| Selective reporting (reporting bias) | Unclear risk | No protocol or trial registration was found. The published paper reports all expected outcomes. |
| Other bias | High risk | “In the other ear, myringotomy was usually performed; those cases in the present trial in which myringotomy was not performed were not considered to introduce a significant variation, as Bennett & Chakraborty showed that myringotomy did not produce a more beneficial effect than adenoidectomy alone.” As the contralateral ear was sometimes treated with myringotomy, and sometimes not, it is unclear whether the study really compared a VT to no treatment, or to myringotomy. |
Velepic 2011.
| Study characteristics | ||
| Methods | Parallel‐group, single‐centre RCT with 6 months follow‐up Randomised by child, analysis by ear This trial randomised participants to receive ventilation tubes and adenoidectomy, or adenoidectomy alone. However, those in the adenoidectomy group were also offered ventilation tube insertion after 3 months, if appropriate. Therefore, we have included this as a comparison of early ventilation tube insertion versus watchful waiting. |
|
| Participants |
Location: Croatia, single centre Setting of recruitment and treatment: ENT clinic Study dates: 2004 to 2010 Sample size:
A total of 87 children were included in the study, indicating that most had bilateral disease. Participant (baseline) characteristics: Age, years:
Gender
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
Ventilation tube plus adenoidectomy: Operations were performed under general anaesthetic. Adenoidectomy was performed using Beckmann’s adenotome. Myringotomy was performed under the control of an operational microscope. It included incision in the posteroinferior quadrant of the eardrum. After the incision, the effusion was aspirated and the tube was inserted (type of tube not stated). If during the follow‐up period CSOM recurred, the tubes were reinserted. Adenoidectomy alone: Participants underwent adenoidectomy. However, if there was no resolution of the effusion after 3 months, myringotomy and implantation of ventilation tube(s) was performed. It is not clear how many participants in this group actually underwent VT tube insertion. |
|
| Outcomes | Final hearing threshold
Adverse event
Proportion of children with persistence of OME, identified using "eardrum examination with an operational microscope" |
|
| Funding sources | “There was no sponsorship for this study” | |
| Declarations of interest | “Authors report no conflict of interest in the publication of the article. There were no financial and personal relationships with other people or organizations that could inappropriately influence (bias) their work.” | |
| Notes |
Research integrity checklist: No retraction notices identified Prospective registration was not identified (published in 2011) No excessive similarities in baseline characteristics No loss to follow‐up was reported No implausible results The number randomised to each group was not identical |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Children were randomly divided into two groups depending on the treatment method”. No details on how the allocation sequence was generated are provided. We note a large discrepancy in the number of ears allocated to each group, and this is not explained in the article. |
| Allocation concealment (selection bias) | Unclear risk | No details on allocation concealment are provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Surgeons could not be blinded. There is a strong possibility that personnel could identify which treatment a participant received and hence change their behaviour as a result. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No information on blinding of outcome assessors is provided for any of the assessments, and the outcomes are not sufficiently objective to discount the possibility of ascertainment bias. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data missing on one ear (1/161). No information given as to how many children/ears completed the trial. |
| Selective reporting (reporting bias) | High risk | No protocol or trial registration was found. The published paper reports all expected outcomes; however, results are not reported separately per group for adverse events outcomes (although P values have been provided). It is unclear whether outcome data are provided for follow‐up at 3 months or 6 months. The time of follow‐up would affect interpretation of the outcomes due to the insertion of tympanostomy tubes for all participants in the no tympanostomy tube group who did not have resolution of the effusion after 3 months. |
| Other bias | High risk | “For 87 children, 37 girls and 50 boys, their parents had signed an informed consent and had regularly come to check‐ups. Those children were enrolled in the research.” There is the possibility of selection bias as the authors chose children who had regularly come to check‐ups and the outcomes for these children may be different to outcomes for those children who do not regularly attend. A follow‐up of 6 months may be too short to detect a true effect of each intervention. |
Yousaf 2016.
| Study characteristics | ||
| Methods | Parallel‐group, single‐centre RCT with 6‐month follow‐up Randomisation by child |
|
| Participants |
Location: Pakistan, single centre Setting of recruitment and treatment: ENT clinic in Pakistan Study dates: February 2012 to January 2015 Sample size:
Participant (baseline) characteristics: None reported Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
VT A myringotomy lancet was used to create an opening for the insertion of ventilation tubes in the intervention group (type of tube not stated) N = 40 children (68 ears) Laser myringotomy Performed using an operating microscope. A diode laser of 980 nm wavelength with a fibre‐optic delivery system was used to perform the myringotomy. The opening was made in the anteroinferior quadrant of the tympanic membrane with a 0.6 mm bare diode fibre, projecting 3 mm from the handpiece edge. Laser energy was delivered with 5 shots in a circular manner with power of 5 W in 0.5 seconds single‐pulse mode. The size of the opening varied from 2 mm to 2.5 mm. N = 42 children (68 ears) |
|
| Outcomes | Improvement in hearing (definition unclear) Final hearing threshold (for a subset only with persistent effusion) Change in hearing threshold (for a subset only) Adverse events
|
|
| Funding sources | Not reported | |
| Declarations of interest | No declaration is made | |
| Notes |
Research integrity checklist: No retraction notices identified Prospective registration was not identified Baseline characteristics are not reported Follow‐up was apparently complete No implausible results The number of children randomised to each group was not identical (although the number of ears included was identical) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “These patients were randomly allocated to either of the 2 groups.” No information is provided regarding generation of the randomisation sequence. The inclusion of identical numbers of affected ears in each group, despite apparent randomisation at the level of the individual child, raises some concerns about the randomisation process. |
| Allocation concealment (selection bias) | Unclear risk | No details on allocation concealment provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Surgeons could not be blinded. There is a strong possibility that personnel could identify which treatment a participant received and hence change their behaviour as a result. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | There was no report of blinding to treatment allocation for any assessment. The outcomes are not sufficiently objective to discount the possibility of ascertainment bias. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Information on loss to follow‐up is not reported, although percentage data for all outcomes indicate no loss to follow‐up |
| Selective reporting (reporting bias) | High risk | No registered protocol was identified, therefore we are unable to compare the reported results to a pre‐specified analysis plan. Hearing was reportedly assessed with pure tone audiogram and tympanogram, but is insufficiently reported, with only the number “improved” in each group, and no clear explanation of what constitutes improvement. |
| Other bias | High risk | Randomisation seems to have occurred at the level of the individual child. Therefore, those with bilateral disease received the same intervention in both ears. However, results are reported at the level of the individual ear. This fails to account for correlation between the ears in the outcome, and may over‐estimate the precision of the estimates. |
AOM: acute otitis media CSOM: chronic suppurative otitis media dB: decibels ENT: ear, nose and throat GP: general practitioner HL: hearing loss ITT: intention‐to‐treat LM: laser myringotomy MRC: Medical Research Council OM: otitis media OME: otitis media with effusion PTA: pure tone audiometry RCT: randomised controlled trial SD: standard deviation SE: standard error TM: tympanic membrane VT: ventilation tube WW: watchful waiting
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Ah‐Tye 2001 | ALLOCATION: randomisation not retained |
| Ardehali 2008 | INTERVENTION: treatment with antibiotics, and is relevant for another review in this suite (Mulvaney 2023a). |
| Black 1990 | PARTICIPANTS: unknown duration of OME |
| Bozkurt 2004 | ALLOCATION: not randomised |
| Bulman 1984 | PARTICIPANTS: wrong patient population. Unknown duration of OME. |
| Choung 2008 | INTERVENTION: treatment with steroids, and is relevant for another review in this suite (Mulvaney 2023b) |
| Demant 2017 | OTHER: study withdrawn/terminated |
| El Begermy 2022 | PARTICIPANTS: unclear duration of OME |
| Englender 1999 | ALLOCATION: not randomised |
| Ferrara 2005 | ALLOCATION: not randomised |
| Gebhart 1981 | PARTICIPANTS: wrong patient population (recurrent acute otitis media) |
| Gibson 1996 | ALLOCATION: not randomised |
| Hammaren‐Malmi 2005 | PARTICIPANTS: did not have OME of at least 3 months duration |
| Hao 2019 | INTERVENTION: treatment with adenoidectomy, and is relevant for another review in this suite (MacKeith 2023) |
| Hassmann 2004 | ALLOCATION: not randomised |
| Iino 1989 | ALLOCATION: not randomised |
| Jabeen 2019 | INTERVENTION: treatment with adenoidectomy, and is relevant for another review in this suite (MacKeith 2023) |
| Kremer 1979 | ALLOCATION: not randomised |
| Kujala 2012 | PARTICIPANTS: had recurrent acute otitis media, not OME |
| Li 2020 | COMPARISON: balloon dilatation of the Eustachian tube (inappropriate comparator) |
| Lildholdt 1983 | PARTICIPANTS: unknown duration of OME |
| Liu 2004 | ALLOCATION: not randomised |
| Mandel 1989 | PARTICIPANTS: wrong patient population |
| Mandel 1992 | PARTICIPANTS: wrong patient population |
| Marchisio 1998 | INTERVENTION: treatment with antibiotics, and is relevant for another review in this suite (Mulvaney 2023a) |
| Markou 2004 | PARTICIPANTS: unknown duration of OME |
| Maw 1993 | INTERVENTION: patients had adenotonsillectomy |
| Moller 1990 | INTERVENTION: treatment with antibiotics, and is relevant for another review in this suite (Mulvaney 2023a) |
| MRC Multicentre Otitis Media Study 2004 | ALLOCATION: not randomised |
| MRC Multicentre Otitis Media Study 2008 | ALLOCATION: not randomised |
| NCT00629694 | PARTICIPANTS: unknown duration of OME |
| NCT05545345 | INTERVENTION: treatment with adenoidectomy, and is relevant for another review in this suite (MacKeith 2023) |
| Nguyen 2004 | PARTICIPANTS: patients with AOM as well as OME |
| Paradise 1990 | PARTICIPANTS: patients had RAOM |
| Paradise 1997 | ALLOCATION: not randomised |
| Parlea 2012 | ALLOCATION: not randomised |
| Rohail 2006 | PARTICIPANTS: unknown duration of OME |
| Sanyaolu 2020 | ALLOCATION: not randomised |
| Shishegar 2007 | PARTICIPANTS: wrong patient population |
| Shubich 1996 | ALLOCATION: not randomised |
| Skinner 1988 | PARTICIPANTS: wrong patient population |
| Stenstrom 2005 | ALLOCATION: not randomised |
| Tao 2004 | COMPARISONS: wrong intervention |
| Uvarova 2001 | ALLOCATION: not randomised |
| Xu 2016 | INTERVENTION: treatment with adenoidectomy, and is relevant for another review in this suite (MacKeith 2023) |
| Yousaf 2014 | COMPARISONS: comparing two types of myringotomy |
| Youssef 2013 | ALLOCATION: not randomised |
AOM: acute otitis media OME: otitis media with effusion RAOM: recurrent acute otitis media
Characteristics of studies awaiting classification [ordered by study ID]
Diacova 2016.
| Methods | — |
| Participants | — |
| Interventions | — |
| Outcomes | — |
| Notes | Extensive efforts to obtain full text were unsuccessful. The available text is ambiguous in that it defines the design as "a prospective observational study", but then goes on to describe random treatment assignment. |
Marshak 1980.
| Methods | — |
| Participants | — |
| Interventions | — |
| Outcomes | — |
| Notes | Unable to obtain full‐text |
Maw 1986.
| Methods | — |
| Participants | — |
| Interventions | — |
| Outcomes | — |
| Notes | Unable to obtain full‐text |
Tawfik 2002.
| Methods | — |
| Participants | — |
| Interventions | — |
| Outcomes | — |
| Notes | Unable to obtain full‐text |
Characteristics of ongoing studies [ordered by study ID]
ACTRN12611001073998.
| Study name | Surgery for otitis media in Indigenous Australian children |
| Methods | RCT Australia, multicentre 12‐month follow‐up |
| Participants | Children with chronic OM |
| Interventions | Adenoidectomy with VT Adenoidectomy with myringotomy |
| Outcomes | Trial registration 2011 No data published as of August 2022 |
| Starting date | — |
| Contact information | — |
| Notes | — |
NCT02546518.
| Study name | A comparison of surgical and a new non‐surgical treatment methods for secretory otitis media in children |
| Methods | Parallel‐group RCT |
| Participants | 80 children with unilateral or bilateral secretory otitis media of at least 3 months duration, and an intact tympanic membrane |
| Interventions | Ventilation tubes compared to Moniri Otovent (autoinflation device) |
| Outcomes | Change in hearing level measured using age suitable audiogram (1 month, 3 months, 6 months) Change in middle ear pressure using tympanometry (1 month, 3 months, 6 months) Presence of fluid in the middle ear, assessed with otomicroscopy (1 month, 3 months, 6 months) Health economics ‐ number of days of parental leave needed (6 months) Otitis Media Questionnaire‐14 (1 month, 3 months, 6 months) Number of healthcare or hospital visits with ear‐related issues (6 months) |
| Starting date | April 2017 |
| Contact information | Mohammed Al‐Azzawe: mohammed.al‐azzawe@vgregion.se Hasse Ejnell: hasse.ejnell@vgregion.se |
| Notes |
NCT04584073.
| Study name | Secretory otitis media in adenoids hypertrophy patients |
| Methods | Randomised trial, 3‐month follow‐up |
| Participants |
Location: Egypt Setting of recruitment and treatment: ENT department, university hospital Study dates: October 2020 to December 2022 (estimated) Sample size:
Inclusion criteria: Any case presenting with secretory otitis media with adenoid hypertrophy, meeting the following criteria:
Exclusion criteria: Patients with the following criteria will be excluded from the study:
|
| Interventions |
|
| Outcomes | Primary outcome measures
|
| Starting date | October 2020 |
| Contact information | Dr Ahmed Ayman Ahmed: Ahmed.20123777@med.au.edu.eg Professor Ahmed Abd El‐Hay El‐Hussiney: alhussiniahmad@aun.edu.eg |
| Notes | — |
ENT: ear, nose and throat OM: otitis media OME: otitis media with effusion RCT: randomised controlled trial VT: ventilation tube
Differences between protocol and review
In the protocol for this review we planned to assess the following six comparisons (MacKeith 2022):
bilateral ventilation tubes versus no treatment/watchful waiting;
bilateral ventilation tubes versus hearing aids;
bilateral ventilation tubes versus non‐surgical treatment;
bilateral ventilation tubes versus myringotomy alone;
unilateral ventilation tubes versus no treatment/watchful waiting;
unilateral ventilation tubes versus myringotomy alone in the other ear/other children.
However, two issues arose whilst conducting the review. Firstly, we agreed that the comparators 'no treatment' and 'watchful waiting' for this review were different. No treatment indicates that it was intended that children in the comparator arm would not receive treatment during the study. Watchful waiting suggests a more active follow‐up, with intervention at a later stage as required. We therefore considered it appropriate to separate these comparisons.
The second issue was that studies often included a mixture of children with unilateral and bilateral OME, therefore the distinction between unilateral and bilateral ventilation tube insertion was not relevant.
We therefore revised our comparisons to the following:
ventilation tubes (bilateral or unilateral) versus no treatment;
early ventilation tubes versus watchful waiting (treatment later if required);
ventilation tubes versus hearing aids;
ventilation tubes versus non‐surgical treatment;
ventilation tubes versus myringotomy alone.
Contributions of authors
Samuel MacKeith: drafted the protocol. Screened the search results and selected studies. Reviewed the analyses and reviewed and edited the text of the review.
Caroline A Mulvaney: drafted the protocol. Screened the search results and selected studies, conducted data extraction, carried out statistical analyses and GRADE assessment. Drafted the text of the review.
Kevin Galbraith: drafted the protocol. Screened the search results and selected studies, conducted data extraction, carried out statistical analyses and GRADE assessment. Drafted the text of the review.
Katie Webster: screened the search results and selected studies, conducted data extraction. Drafted the text of the review.
Rachel Connolly: conducted data extraction. Reviewed the analyses and reviewed and edited the text of the review.
Aye Paing: conducted data extraction. Reviewed the analyses and reviewed and edited the text of the review.
Tal Marom: reviewed the protocol. Reviewed the analyses and reviewed and edited the text of the review.
Mat Daniel: reviewed the protocol. Reviewed the analyses and reviewed and edited the text of the review.
Roderick P Venekamp: co‐wrote and edited the protocol. Reviewed the analyses and reviewed and edited the text of the review.
Maroeska Rovers: co‐wrote and edited the protocol. Reviewed the analyses and reviewed and edited the text of the review.
Anne GM Schilder: co‐wrote and edited the protocol. Reviewed the analyses and reviewed and edited the text of the review.
Sources of support
Internal sources
No sources of support provided
External sources
-
National Institute for Health Research, UK
Infrastructure funding for Cochrane ENT
Declarations of interest
Samuel MacKeith: ENT private practice (employment); sees patients with general ENT problems in NHS and private practice; Assistant Co‐ordinating Editor of Cochrane ENT 2020‐2023, but had no role in the editorial process for this review.
Caroline A Mulvaney: none known.
Kevin Galbraith: none known.
Katie Webster: none known.
Rachel Connolly: National Institute for Health and Care Excellence (employment: systematic reviewer on the upcoming NICE guideline on otitis media with effusion in under 12s).
Aye Paing: none known.
Tal Marom: no relevant interests; Attending Otolaryngologist.
Mat Daniel: Aventa Med (stock; consultant); Nottingham University Hospitals NHS Trust (employment: ENT consultant); published research papers relevant to the interventions in the work; co‐author of the TARGET trial.
Roderick P Venekamp: no relevant interests; work as a GP; editorial board member of Cochrane ARI and ENT, but had no role in the editorial process for this review.
Maroeska M Rovers: no relevant interests; involved in the KNOOP‐3 study on the effectiveness of ventilation tubes performed in the Netherlands (sponsored by ZonMw).
Anne GM Schilder: joint Co‐ordinating Editor of Cochrane ENT until April 2020, but had no role in the editorial process for this review.; treats patients with OME in her NHS practice. Her evidENT team at the UCL Ear Institute is supported by the National Institute of Health Research (NIHR) University College London Hospitals (UCLH) Biomedical Research Centre (BRC), with research projects being supported by the NIHR, Wellcome Trust, RNiD, ENT UK and industry; National Specialty Lead for the NIHR Clinical Research Network ENT and Surgical Specialty Lead for ENT for the Royal College of Surgeons of England's Clinical Research Initiative; in her role as director of the NIHR UCLH BRC Deafness and Hearing Problems Theme, she advises CRO, biotech and pharma companies in the hearing field on clinical trial design and delivery.
New
References
References to studies included in this review
Bernard 1991 {published data only}
- Bernard PA, Stenstrom RJ, Feldman W, Durieux-Smith A. Randomized, controlled trial comparing long-term sulfonamide therapy to ventilation tubes for otitis media with effusion. Pediatrics 1991;88(2):215-22. [CENTRAL: CN-00077175] [PMID: ] [PubMed] [Google Scholar]
- Feldman W, Bernard P, Smith A, Stenstrom R. Sulfonamide prophylaxis vs ventilation tubes in hearing-loss due to recurrent otitis-media with effusion (Rome) - preliminary-results of a randomized controlled trial. Clinical and Investigative Medicine-medecine Clinique et Experimentale 1987;4:A33. [CENTRAL: CN-02494379] [Google Scholar]
- Feldman W, Bernard P, Smith A, Stenstrom R. Sulfonamide prophylaxis vs ventilation tubes in hearing-loss due to recurrent otitis-media with effusion - preliminary-results of a randomized controlled trial. American Journal of Diseases of Children 1987;4:389-9. [CENTRAL: CN-02494378] [Google Scholar]
D'Eredita 2006 {published data only}
- D'Eredità R, Shah UK. Contact diode laser myringotomy for medium-duration middle ear ventilation in children. International Journal of Pediatric Otorhinolaryngology 2006;70:1077-80. [DOI: 10.1016/j.ijporl.2005.11.003] [DOI] [PubMed] [Google Scholar]
Dempster 1993 {published data only}
- Dempster JH, Browning GG, Gatehouse SG. A randomized study of the surgical management of children with persistent otitis media with effusion associated with a hearing impairment. Journal of Laryngology and Otology 1993;107(4):284-9. [CENTRAL: CN-00094188] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Dempster JH, Browning GG, Gatehouse SG. A randomized study of the surgical management of children with persistent otitis media with effusion associated with a hearing impairment. Journal of Laryngology and Otology 1993;107(4):284-9. [DOI: 10.1017/s0022215100122844] [DOI] [PubMed] [Google Scholar]
Elkholy 2021 {published data only}
- Elkholy TA, El-gaber A, Mohammed F, Al-Agamy DMM, Elhady M. Impact of adenoidectomy alone or with ventilation tube for treatment of secretory otitis media in children. Al-azhar International Medical Journal 2021;2(8):53-8. [CENTRAL: CN-02518323] [Google Scholar]
Gates 1989 {published data only}
- Gates GA, Avery CA, Cooper JC, Prihoda TJ, Cooper JCJ. Chronic secretory otitis media: effects of surgical management. Annals of Otology, Rhinology & Laryngology. Supplement 1989;138:2-32. [CENTRAL: CN-00057471] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Gates GA, Avery CA, Prihoda TJ, Cooper JC. Effectiveness of adenoidectomy and tympanostomy tubes in the treatment of chronic otitis media with effusion. New England Journal of Medicine 1987;317(23):1444-51. [CENTRAL: CN-00051110] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Gates GA, Avery CA, Prihoda TJ. Effect of adenoidectomy upon children with chronic otitis media with effusion. Laryngoscope 1988;98(1):58-63. [CENTRAL: CN-00051547] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Gates GA, Wachtendorf C, Hearne EM, Holt GR. Treatment of chronic otitis media with effusion: results of tympanostomy tubes. American Journal of Otolaryngology 1985;6(3):249-53. [CENTRAL: CN-00038728] [PMID: ] [DOI] [PubMed]
Koopman 2004 {published data only}
- Koopman JP, Blom H, Hoeve H, Mulder P. Laser myringotomy versus ventilation tubes in children with chronic otitis media with effusion: a randomized trial for efficacy and outcome prediction. In: 8th International Symposium on Recent Advances in Otitis Media. 2003:136. [CENTRAL: CN-00449322]
- Koopman JP, Reuchlin AG, Kummer EE, Boumans LJ, Rijntjes E, Hoeve LJ, et al. Laser myringotomy versus ventilation tubes in children with otitis media with effusion: a randomized trial. Laryngoscope 2004;114(5):844-9. [CENTRAL: CN-00469076] [PMID: ] [DOI] [PubMed] [Google Scholar]
Maw 1983 {published data only}
- Maw AR, Herod F. Otoscopic, impedance, and audiometric findings in glue ear treated by adenoidectomy and tonsillectomy. A prospective randomised study. Lancet 1986;1(8495):1399-402. [CENTRAL: CN-00043077] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Maw AR, Parker A. Surgery of the tonsils and adenoids in relation to secretory otitis media in children. Acta Oto-laryngologica. Supplementum 1988;454:202-7. [CENTRAL: CN-00057952] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Maw AR. Age and adenoid size in relation to adenoidectomy in otitis media with effusion. American Journal of Otolaryngology 1985;6(3):245-8. [CENTRAL: CN-00038727] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Maw AR. Chronic otitis media with effusion (glue ear) and adenotonsillectomy: prospective randomised controlled study. British Medical Journal (clinical Research Ed.) 1983;287(6405):1586-8. [CENTRAL: CN-00032849] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maw AR. Chronic otitis media with effusion and adeno-tonsillectomy--a prospective randomized controlled study. International Journal of Pediatric Otorhinolaryngology 1983;6(3):239-46. [CENTRAL: CN-00034535] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Maw AR. Factors affecting adenoidectomy for otitis media with effusion (glue ear). Journal of the Royal Society of Medicine 1985;78(12):1014-8. [CENTRAL: CN-00040567] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maw AR. Otitis media with effusion (glue ear). A prospective randomized study 1 year following adenoidectomy and tonsillectomy. Clinical Otolaryngology and Allied Sciences 1984;9:130. [CENTRAL: CN-00262086] [Google Scholar]
- Maw AR. The long term effect of adenoidectomy on established otitis media with effusion in children. Auris, Nasus, Larynx 1985;12(Suppl 1):S234-6. [CENTRAL: CN-00043248] [EMBASE: 16731316] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Parker AJ. No peak-peak tympanometric conversion in relation to radiographic palatal airway size in children with otitis media with effusion (OME). Clinical Otolaryngology 1989;14:172. [CENTRAL: CN-00262390] [DOI] [PubMed] [Google Scholar]
Maw 1999 {published data only}
- Hall AJ, Maw AR, Steer CD. Developmental outcomes in early compared with delayed surgery for glue ear up to age 7 years: a randomised controlled trial. Clinical Otolaryngology 2009;34(1):12-20. [CENTRAL: CN-00699827] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Maw R, Wilks J, Harvey I, Peters TJ, Golding J, Wiks J. Early surgery compared with watchful waiting for glue ear and effect on language development in preschool children: a randomised trial. Lancet 1999;353(9157):960-3. [CENTRAL: CN-00166722] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Maw R, Wilks J, Harvey I, Peters TJ, Golding J, Wiks J. Early surgery compared with watchful waiting for glue ear and effect on language development in preschool children: a randomised trial. Lancet 1999;353(9157):960-3. [DOI] [PubMed] [Google Scholar]
- Maw R, Wilks J, Harvey I, Peters TJ, Golding J. Randomised controlled trial of early surgery versus watchful waiting for glue ear: the effect of langauge development in pre-school children. Journal of Laryngology 1999;113(23 Suppl):40. [CENTRAL: CN-00292554] [Google Scholar]
- Wilks J, Maw R, Peters TJ, Harvey I, Golding J. Randomised controlled trial of early surgery versus watchful waiting for glue ear: the effect on behavioural problems in pre-school children. Clinical Otolaryngology and Allied Sciences 2000;25(3):209-14. [CENTRAL: CN-00330781] [PMID: ] [DOI] [PubMed] [Google Scholar]
Paradise 2007 {published data only}
- Johnston LC, Feldman HM, Paradise JL, Bernard BS, Colborn DK, Casselbrant ML, et al. Tympanic membrane abnormalities and hearing levels at the ages of 5 and 6 years in relation to persistent otitis media and tympanostomy tube insertion in the first 3 years of life: a prospective study incorporating a randomized clinical trial. Pediatrics 2004;114(1):e58-67. [CENTRAL: CN-00490067] [PMID: ] [DOI] [PubMed] [Google Scholar]
- NCT00365092. Middle ear disease before age 3, treatment with ear tubes, and literacy and attentional abilities at ages 9 to 11 [Early otitis and literacy and attention at 9 to 11 years]. clinicaltrials.gov/show/NCT00365092 (first received 15 August 2006). [CENTRAL: CN-02013311]
- Paradise J, Dollaghan C, Campbell T, Feldman H. Early vs delayed tube placement for persistent middle-ear effusion in the first three years of life: effects on cognition, language, speech and behavior at ages 4 and 6 years. In: 8th International Symposium on Recent Advances in Otitis Media. Fort Lauderdale, FL, USA, 3-7 June, 2003. 2003:219. [ABSTRACT NO.: B57] [CENTRAL: CN-00449362]
- Paradise JL, Campbell TF, Dollaghan CA, Feldman HM, Bernard BS, Colborn DK, et al. Developmental outcomes after early or delayed insertion of tympanostomy tubes. New England Journal of Medicine 2005;353(6):576-86. [CENTRAL: CN-00523784] [EMBASE: 2005369617] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paradise JL, Colborn DK, Bernard BS, Hakos LM, Guerra NJ, et al. Comparison of the early results of tympanostomy tube placement and of nonsurgical management in infants with persistent otitis media. In: Recent Advances in Otitis Media. 6th International Symposium on Recent Advances in Otitis Media, Jun 04-08, 1995, Ft Lauderdale, Florida. 1996:201. [CENTRAL: CN-00634260]
- Paradise JL, Dollaghan CA, Campbell TF, Feldman HM, Bernard BS, Colborn DK, et al. Otitis media and tympanostomy tube insertion during the first three years of life: developmental outcomes at the age of four years. Pediatrics 2003;112(2):265-77. [CENTRAL: CN-00439773] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Paradise JL, Feldman HM, Campbell TF, Dollaghan CA, Colborn DK, Bernard BS, et al. Early versus delayed insertion of tympanostomy tubes for persistent otitis media: developmental outcomes at the age of three years in relation to prerandomization illness patterns and hearing levels. Pediatric Infectious Disease Journal 2003;22(4):309-14. [CENTRAL: CN-00431844] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Paradise JL, Feldman HM, Campbell TF, Dollaghan CA, Colborn DK, Bernard BS, et al. Early vs late tube placement for persistent middle-ear effusion (MEE) in the first 3 years of life: effects on language, speech sound production, and cognition at age 3 years. Pediatric Research 2000;47(4):216A. [CENTRAL: CN-00383898] [Google Scholar]
- Paradise JL, Feldman HM, Campbell TF, Dollaghan CA, Colborn DK, Bernard BS, et al. Effect of early or delayed insertion of tympanostomy tubes for persistent otitis media on developmental outcomes at the age of three years. New England Journal of Medicine 2001;344(16):1179-87. [CENTRAL: CN-00327417] [EMBASE: 32319492] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Paradise JL, Feldman HM, Campbell TF, Dollaghan CA, Rockette HE, Pitcairn DL, et al. Tympanostomy tubes and developmental outcomes at 9 to 11 years of age. New England Journal of Medicine 2007;356(3):248-61. [CENTRAL: CN-00575011] [EMBASE: 2007-01205-003] [PMID: ] [DOI] [PubMed] [Google Scholar]
Popova 2010 {published data only}
- Popova D, Varbanova S, Popov TM. Comparison between myringotomy and tympanostomy tubes in combination with adenoidectomy in 3-7-year-old children with otitis media with effusion. International Journal of Pediatric Otorhinolaryngology 2010;74(7):777-80. [CENTRAL: CN-00767591] [PMID: ] [DOI] [PubMed] [Google Scholar]
Rach 1991 {published data only}
- Rach GH, Zielhuis GA, Baarle PW, den Broek P. The effect of treatment with ventilating tubes on language development in preschool children with otitis media with effusion. Clinical Otolaryngology and Allied Sciences 1991;16(2):128-32. [CENTRAL: CN-00076714] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Schilder AGM, Manen JG, Zielhuis GA, Grievink EH. Long-term results of a randomized controlled trial of surgery for otitis media with effusion. In: Sade J , editors(s). Infections in Childhood Ear, Nose and Throat Aspects: Proceedings of the 3rd International Conferenceof the European Working Group for Pediatric Otorhinolargyngology, Jerusalem, Israel: Nov 7-12, 1993. 1994.
- Zielhuis GA, Rach GH, den Broek P. Screening for otitis media with effusion in preschool children. Lancet 1989;1(8633):311-4. [DOI] [PubMed] [Google Scholar]
Rovers 2000 {published data only}
- Hartman M, Rovers MM, Ingels K, Zielhuis GA, Severens JL, Wilt GJ. Economic evaluation of ventilation tubes in otitis media with effusion. Archives of Otolaryngology--Head & Neck Surgery 2001;127(12):1471-6. [CENTRAL: CN-00369148] [EMBASE: 2001440522] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Rovers M, Ingels K, Wilt GJ, den Broek P, Zielhuis G. The effects of ventilation tubes: a randomized clinical trial. In: Recent Advances in Otitis Media, Proceedings. 2001:411-4. [CENTRAL: CN-02494418]
- Rovers M, Zielhuis G, Hartman M, Ingels K, Straatman H, Van Der Wilt G. The effect of early screening and treatment with ventilation tubes in infants with persistent otitis media with effusion. In: ISTAHC Annual Meeting. Vol. 16. 2000:063. [CENTRAL: CN-00452876]
- Rovers MM, Krabbe PF, Straatman H, Ingels K, Wilt GJ, Zielhuis GA. Randomised controlled trial of the effect of ventilation tubes (grommets) on quality of life at age 1-2 years. Archives of Disease in Childhood 2001;84(1):45-9. [CENTRAL: CN-00327716] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rovers MM, Straatman H, Ingels K, Wilt GJ, den Broek P, Zielhuis GA. Generalizability of trial results based on randomized versus nonrandomized allocation of OME infants to ventilation tubes or watchful waiting. Journal of Clinical Epidemiology 2001;54(8):789-94. [CENTRAL: CN-00349653] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Rovers MM, Straatman H, Ingels K, Wilt GJ, den Broek P, Zielhuis GA. The effect of short-term ventilation tubes versus watchful waiting on hearing in young children with persistent otitis media with effusion: a randomized trial. Ear and Hearing 2001;22(3):191-9. [CENTRAL: CN-00362609] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Rovers MM, Straatman H, Ingels K, Wilt GJ, den Broek P, Zielhuis GA. The effect of ventilation tubes on language development in infants with otitis media with effusion: a randomized trial. Pediatrics 2000;106(3):E42. [CENTRAL: CN-00299394] [PMID: ] [PubMed] [Google Scholar]
- Rovers MM, Zielhuis K, Ingels H, Straatman G. The effect of early screening and treatment with ventilation tubes in infants with persistent otitis media with effusion. Clinical Otolaryngology and Allied Sciences 2003;28(2):158. [CENTRAL: CN-00452877] [Google Scholar]
Ruckley 1988 {published data only}
- Ruckley RW, Blair RL. Thermal myringotomy (an alternative to grommet insertion in childhood secretory otitis media?). Journal of Laryngology and Otology 1988;102(2):125-8. [CENTRAL: CN-00452878] [PubMed] [Google Scholar]
Sujatha 2015 {published data only}
- Sujatha S, Venugopalan PG. Evaluation of effectiveness of myringotomy and myringotomy with ventilation tube insertion as treatment of otitis media with effusion in children. Journal of Evolution of Medical and Dental Sciences 2015;4(29):5003-9. [Google Scholar]
Tao 2020 {published data only}
- Tao J, Luo R, Chen Y, Hou C, Hao Q. Myringotomy or tympanostomy tube insertion, comparison of surgical treatment of adenoid hypertrophy and otitis media with effusion in children. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2020;34(3):207-10. [DOI: 10.13201/j.issn.2096-7993.2020.03.005] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
TARGET 2000 {published data only}
- Browning G. TARGET trial of alternative regimes for glue ear treatment: analysis 2. In: 8th International Congress of Paediatric Otorhinolaryngology (ESPO). Oxford, UK, 11-14 September, 2002. 2002:60. [CENTRAL: CN-00431582]
- Browning GG. Patient-centred oucomes of a surgical RCT of otitis media with effusion at one year. Laryngo-Rhino-Otologie 2000;79(Suppl 1):S35-6. [CENTRAL: CN-00526378] [Google Scholar]
- Browning GG. Two-year outcome of ventilation tubes in a randomized controlled trial of persistent childhood otitis media with effusion. Clinical Otolaryngology and Allied Sciences 2001;26(4):342-4. [CENTRAL: CN-02494417] [DOI] [PubMed] [Google Scholar]
- Haggard MP, Gannon MM, Birkin JA, Bennett KE, Nicholls EE, Spencer H, et al. Adjuvant adenoidectomy in persistent bilateral otitis media with effusion: hearing and revision surgery outcomes through 2 years in the TARGET randomised trial. Clinical Otolaryngology 2012;37(2):107-16. [CENTRAL: CN-00896356] [EMBASE: 364670938] [PMID: ] [DOI] [PubMed] [Google Scholar]
- ISRCTN35793977. Trial of alternative regimens in glue ear treatment - effectiveness of surgery for otitis media with effusion in 3.5-7 year olds using multiple developmental and economic measures combined with classical clinical measures. www.controlled-trials.com/ISRCTN35793977 (first received 2000). [CENTRAL: CN-00725114]
- MRC Multicentre Otitis Media Study Group. Surgery for persistent otitis media with effusion: generalizability of results from the UK trial (TARGET). Trial of Alternative Regimens in Glue Ear Treatment. Clinical Otolaryngology and Allied Sciences 2001;26(5):417-24. [CENTRAL: CN-00374837] [EMBASE: 32995195] [PMID: ] [DOI] [PubMed] [Google Scholar]
- MRC Multicentre Otitis Media Study Group. The role of ventilation tube status in the hearing levels in children managed for bilateral persistent otitis media with effusion. Clinical Otolaryngology and Allied Sciences 2003;28(2):146-53. [CENTRAL: CN-00431744] [EMBASE: 2003174240] [PMID: ] [DOI] [PubMed] [Google Scholar]
To 1984 {published data only}
- To SS, Pahor AL, Robin PE. A prospective study of the use of unilateral grommets in chronic bilateral secretory otitis media. Clinical Otolaryngology and Allied Sciences 1984;9:130-1. [CENTRAL: CN-00262088] [DOI] [PubMed] [Google Scholar]
- To SS, Pahor AL, Robin PE. A prospective trial of unilateral grommets for bilateral secretory otitis media in children. Clinical Otolaryngology and Allied Sciences 1984;9(2):115-7. [CENTRAL: CN-00035295] [PMID: ] [DOI] [PubMed] [Google Scholar]
Velepic 2011 {published data only}
- Velepic M, Starcevic R, Bonifacic M, Ticac R, Kujundzic M, Udovic DS, et al. The clinical status of the eardrum: an inclusion criterion for the treatment of chronic secretory otitis media in children. International Journal of Pediatric Otorhinolaryngology 2011;75(5):686-90. [CENTRAL: CN-00784332] [EMBASE: 51315541] [PMID: ] [DOI] [PubMed] [Google Scholar]
Yousaf 2016 {published data only}
- Yousaf M, Malik SA, Haroon T. Laser myringotomy versus ventilation tubes in otitis media with effusion. Journal of Ayub Medical College, Abbottabad 2016;28(4):773-5. [CENTRAL: CN-01380598] [EMBASE: 619635268] [PMID: ] [PubMed] [Google Scholar]
References to studies excluded from this review
Ah‐Tye 2001 {published data only}
- Ah-Tye C, Paradise JL, Colborn DK. Otorrhea in young children after tympanostomy-tube placement for persistent middle-ear effusion: prevalence, incidence, and duration. Pediatrics 2001;107(6):1251-8. [CENTRAL: CN-00348427] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ardehali 2008 {published data only}
- Ardehali MM, Seraj JM, Asiabar MK, Adibi H. The possible role of gastroesophageal reflux disease in children suffering from chronic otitis media with effusion. Acta Medica Iranica 2008;46(1):33-7. [CENTRAL: CN-00708224] [EMBASE: 351792703] [Google Scholar]
Black 1990 {published data only}
- Black NA, Sanderson CF, Freeland AP, Vessey MP. A randomised controlled trial of surgery for glue ear. BMJ (Clinical Research Ed.) 1990;300(6739):1551-6. [CENTRAL: CN-00069039] [PMID: ] [DOI] [PMC free article] [PubMed]
Bozkurt 2004 {published data only}
- Bozkurt MK, Calguner M. The efficacy of CO2 laser myringotomy in serous otitis media. Kulak Burun Bogaz Ihtisas Dergisi: KBB [Journal of Ear, Nose, and Throat] 2004;12(3-4):55-9. [CENTRAL: CN-00523128] [PMID: ] [PubMed] [Google Scholar]
Bulman 1984 {published data only}
- Bulman CH, Brook SJ, Berry MG. A prospective randomized trial of adenoidectomy vs grommet insertion in the treatment of glue ear. Clinical Otolaryngology and Allied Sciences 1984;9(2):67-75. [CENTRAL: CN-00174952] [EMBASE: 1984176580] [PMID: ] [DOI] [PubMed] [Google Scholar]
Choung 2008 {published data only}
- Choung YH, Shin YR, Choi SJ, Park K, Park HY, Lee JB, et al. Management for the children with otitis media with effusion in the tertiary hospital. Clinical and Experimental Otorhinolaryngology 2008;1(4):201-5. [CENTRAL: CN-00671567] [DOI] [PMC free article] [PubMed] [Google Scholar]
Demant 2017 {published data only}
- Demant MN, Jensen RG, Jakobsen JC, Gluud C, Homoe P. The effects of ventilation tubes versus no ventilation tubes for recurrent acute otitis media or chronic otitis media with effusion in 9 to 36 month old Greenlandic children, the SIUTIT trial: study protocol for a randomized controlled trial. Trials 2017;18(1):30. [CENTRAL: CN-01304999] [EMBASE: 614107422] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT02490332. The effects of ventilation tubes - The SIUTIT Trial [The effects of ventilation tubes versus no ventilation tubes for recurrent acute otitis media or chronic otitis media with effusion in 9 to 36 month old Greenlandic children - a randomised clinical trial]. clinicaltrials.gov/show/NCT02490332 (first received 3 July 2015). [CENTRAL: CN-02043426]
El Begermy 2022 {published data only}
- El Begermy MA, El Begermy MM, Kassamy H. The effect of endoscopic peritubal adenoidectomy vs myringotomy with ventilation tubes insertion in management of otitis media with effusion in children. Egyptian Journal of Ear, Nose, Throat and Allied Sciences 2022;23(23):1-10. [CENTRAL: CN-02518322] [Google Scholar]
Englender 1999 {published data only}
- Englender M, Somech E, Harell M. Laser myringotomy (L-myringotomy) and ventilating tubes: a preliminary comparative study. Lasers in Medical Science 1999;14(1):62-6. [CENTRAL: CN-00431622] [DOI] [PubMed] [Google Scholar]
Ferrara 2005 {published data only}
- Ferrara S, Sammartano D, Ferrara P. Long-term management of recurrent otitis media with effusion in children. In: XVIII IFOS World Congress; 2005 Jun 25-30, Rome (Italy). 2005. [CENTRAL: CN-00526409]
Gebhart 1981 {published data only}
- Gebhart DE. Tympanostomy tubes in the otitis media prone child. Laryngoscope 1981;91(6):849-66. [CENTRAL: CN-00025323] [EMBASE: 1981143267] [PMID: ] [DOI] [PubMed] [Google Scholar]
Gibson 1996 {published data only}
- Gibson PG, Stuart JE, Wlodarczyk J, Olson LG, Hensley MJ. Nasal inflammation and chronic ear disease in Australian Aboriginal children. Journal of Paediatrics and Child Health 1996;32(2):143-7. [CENTRAL: CN-00131589] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hammaren‐Malmi 2005 {published data only}
- Hammaren-Malmi S, Saxen H, Tarkkanen J, Mattila PS. Adenoidectomy does not significantly reduce the incidence of otitis media in conjunction with the insertion of tympanostomy tubes in children who are younger than 4 years: a randomized trial. Pediatrics 2005;116(1):185-9. [CENTRAL: CN-00528797] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hao 2019 {published data only}
- Hao J, Chen M, Liu B, Yang Y, Liu W, Ma N, et al. Compare two surgical interventions for otitis media with effusion in young children. European Archives of Oto-rhino-laryngology 2019;276(8):2125-31. [CENTRAL: CN-01956237] [EMBASE: 627898353] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Hao J, Chen M, Liu B, Yang Y, Liu W, Ma N, et al. Correction to: compare two surgical interventions for otitis media with effusion in young children [Correction to: Compare two surgical interventions for otitis media with effusion in young children (European Archives of Oto-Rhino-Laryngology, (2019), 276, 8, (2125-2131), 10.1007/s00405-019-05421-9)]. European Archives of Oto-rhino-laryngology 2019;276(8):2133-4. [CENTRAL: CN-02080898] [EMBASE: 628234545] [PMID: 31214828] [Google Scholar]
Hassmann 2004 {published data only}
- Hassmann E, Skotnicka B, Baczek M, Piszcz M. Laser myringotomy in otitis media with effusion: long-term follow-up. European Archives of Oto-rhino-laryngology 2004;261(6):316-20. [CENTRAL: CN-00497408] [DOI] [PubMed] [Google Scholar]
Iino 1989 {published data only}
- Iino Y, Ishitoya J, Ikeda M, Ito Y, Usami M, Kawashiro N, et al. Factors on delayed recovery of otitis media with effusion in children--clinical and bacteriological study. Nihon Jibiinkoka Gakkai Kaiho 1989;92(8):1183-91. [CENTRAL: CN-00063873] [PMID: ] [DOI] [PubMed] [Google Scholar]
Jabeen 2019 {published data only}
- Jabeen F, Chaudhry S, Ahmed Z, Khalil N, Amin B, Rizvi SS. Comparison of rate of recurrence of otitis media with effusion in children treated by myringotomy and ventilating tube insertion with patients treated by additional adenoidectomy. Rawal Medical Journal 2019;44(3):513-6. [CENTRAL: CN-02007003] [EMBASE: 2002854226] [Google Scholar]
Kremer 1979 {published data only}
- Kremer M, Podoshin L, Fradis M. Treatment of serous otitis media with tympanic ventilation tubes. Ear, Nose, & Throat Journal 1979;58(5):203-9. [PMID: ] [PubMed] [Google Scholar]
Kujala 2012 {published data only}
- Kujala T, Alho OP, Kristo A, Uhari M, Renko M, Pokka T, et al. Quality of life after surgery for recurrent otitis media in a randomized controlled trial. Pediatric Infectious Disease Journal 2014;33(7):715-9. [CENTRAL: CN-00995945] [EMBASE: 2014406374] [PMID: ] [DOI] [PubMed] [Google Scholar]
Li 2020 {published data only}
- Li H, Zhou Y, Huang J, Zhang L, Lou Z. Treatment of secretory otitis media with balloon dilation and tympanostomy tube insertion: a randomized controlled trial. Basic & Clinical Pharmacology & Toxicology 2020;127(Suppl 1):292-3. [CENTRAL: CN-02230226] [EMBASE: 633830686] [Google Scholar]
Lildholdt 1983 {published data only}
Liu 2004 {published data only}
- Liu L, Sun YG, Ma L, Zhao W, Wu R. Effect of ventilation tube insertion on otitis media with effusion in cleft palate children. Zhonghua Er Bi Yan Hou Ke za Zhi 2004;39(4):216-8. [CENTRAL: CN-00549233] [EMBASE: 39714817] [PubMed] [Google Scholar]
Mandel 1989 {published data only}
Mandel 1992 {published data only}
- Mandel EM, Rockette HE, Bluestone CD, Paradise JL, Nozza RJ. Efficacy of myringotomy with and without tympanostomy tubes for chronic otitis media with effusion. Pediatric Infectious Disease Journal 1992;11(4):270-7. [CENTRAL: CN-00338034] [PMID: ] [DOI] [PubMed] [Google Scholar]
Marchisio 1998 {published data only}
- Marchisio P, Principi N, Passali D, Salpietro DC, Boschi G, Chetri G, et al. Epidemiology and treatment of otitis media with effusion in children in the first year of primary school. Acta Oto-laryngologica 1998;118(4):557-62. [CENTRAL: CN-00154484] [EMBASE: 1998254893] [PMID: ] [DOI] [PubMed] [Google Scholar]
Markou 2004 {published data only}
- Markou K, Vlachtsis K, Kyriafinis G, Petridis D, Daniilidis I. Long-term results of adenoidectomy and ventilation tube insertion in the surgical treatment of chronic otitis media with effusion. International Journal of Pediatric Otorhinolaryngology 2004;68(5):684. [CENTRAL: CN-00477460] [Google Scholar]
Maw 1993 {published data only}
- Maw R, Bawden R, Maw AR. Spontaneous resolution of severe chronic glue ear in children and the effect of adenoidectomy, tonsillectomy, and insertion of ventilation tubes (grommets). BMJ (Clinical Research Ed.) 1993;306(6880):756-60. [CENTRAL: CN-00093062] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moller 1990 {published data only}
- Moller P, Dingsor G. Otitis media with effusion: can erythromycin reduce the need for ventilating tubes? Journal of Laryngology and Otology 1990;104(3):200-2. [CENTRAL: CN-00067688] [PMID: ] [DOI] [PubMed] [Google Scholar]
MRC Multicentre Otitis Media Study 2004 {published data only}
- MRC Multicentre Otitis Media Study Group. Speech reception in noise: an indicator of benefit from otitis media with effusion surgery. Clinical Otolaryngology and Allied Sciences 2004;29(5):497-504. [CENTRAL: CN-00497404] [EMBASE: 39287082] [PMID: ] [DOI] [PubMed] [Google Scholar]
MRC Multicentre Otitis Media Study 2008 {published data only}
- MRC Multicentre Otitis Media Study Group. An extension of the Jerger classification of tympanograms for ventilation tube patency--specification and evaluation of equivalent ear-canal volume criteria. Ear and Hearing 2008;29(6):894-906. [CENTRAL: CN-00682310] [EMBASE: 550156802] [PMID: ] [DOI] [PubMed] [Google Scholar]
NCT00629694 {published data only}
- NCT00629694. Adenoidectomy, myringotomy and tubes' insertion vs adenoidectomy and myringotomy alone in children with otitis media with effusion and adenoid hypertrophy. clinicaltrials.gov/show/NCT00629694 (first received 6 March 2008). [CENTRAL: CN-00726812]
NCT05545345 {published data only}
- NCT05545345. Adjuvant adenoidectomy for the treatment of chronic OME in children [Adjuvant adenoidectomy plus tympanostomy tube placement for the treatment of chronic OME in children]. clinicaltrials.gov/show/NCT05545345 (first received 19 September 2022). [CENTRAL: CN-02462316]
Nguyen 2004 {published data only}
- Nguyen LH, Manoukian JJ, Yoskovitch A, Al-Sebeih KH, Al Sebeih KH. Adenoidectomy: selection criteria for surgical cases of otitis media. Laryngoscope 2004;114(5):863-6. [CENTRAL: CN-00469074] [PMID: ] [DOI] [PubMed] [Google Scholar]
Paradise 1990 {published data only}
- Paradise JL, Bluestone CD, Rogers KD, Taylor FH, Colborn DK, Bachman RZ, et al. Efficacy of adenoidectomy for recurrent otitis media in children previously treated with tympanostomy-tube placement. Results of parallel randomized and nonrandomized trials. JAMA 1990;263(15):2066-73. [CENTRAL: CN-00066665] [PMID: ] [PubMed]
Paradise 1997 {published data only}
- Paradise J, Campbell T, Dollaghan C, Feldman H, Bernard B, Colborn K, et al. Receptive vocabulary, cognition, and parent-rated behavior at age 3 years in relation to otitis media in the first 3 years of life. In: Abstract Book of the Association of Health Service Research. Vol. 14. 1997:350-1. [CENTRAL: CN-00452820]
Parlea 2012 {published data only}
- Parlea E, Georgescu M, Calarasu R. Tympanometry as a predictor factor in the evolution of otitis media with effusion. Journal of Medicine and Life 2012;5(4):452-4. [CENTRAL: CN-00850240] [EMBASE: 369159817] [PMID: ] [PMC free article] [PubMed] [Google Scholar]
Rohail 2006 {published data only}
- Rohail A, Gill ZI, Butt MR. A comparison of medical treatment versus surgical treatment for the management of otitis media with effusion. Annals of King Edward Medical College 2006;12(1):64-7. [CENTRAL: CN-00597368]
Sanyaolu 2020 {published data only}
- Sanyaolu LN, Cannings-John R, Butler CC, Francis NA. The effect of ventilation tube insertion on quality of life in children with persistent otitis media with effusion. Clinical Otolaryngology 2020;45(2):239-47. [CENTRAL: CN-02217143] [EMBASE: 2004053181] [PMID: ] [DOI] [PubMed] [Google Scholar]
Shishegar 2007 {published data only}
- Shishegar M, Hoghoghi H. Comparison of adenoidectomy and myringotomy with and without tube placement in the short term hearing status of children with otitis media with effusion: a preliminary report. Iranian Journal of Medical Sciences 2007;32(3):169-72. [CENTRAL: CN-00708699] [EMBASE: 351270400] [Google Scholar]
Shubich 1996 {published data only}
- Shubich I. Otitis media with effusion and allergy control in children: a prospective study. In: Sixth International Symposium on Otitis Media; 1996, Fort Lauderdale (FL). 1996:173-4. [CENTRAL: CN-00452904]
Skinner 1988 {published data only}
- Skinner DW, Lesser TH, Richards SH. A 15-year follow-up of a controlled trial of the use of grommets in glue ear. Otolaryngology and Allied Sciences 1989;14:169. [DOI] [PubMed] [Google Scholar]
- Skinner DW, Lesser THJ, Richards SH. A 15 year follow-up of a controlled trial of the use of grommets in glue ear. Clinical Otolaryngology and Allied Sciences 1988;13(5):341-6. [EMBASE: 18269160] [DOI] [PubMed] [Google Scholar]
Stenstrom 2005 {published data only}
- Stenstrom R, Pless IB, Bernard P. Hearing thresholds and tympanic membrane sequelae in children managed medically or surgically for otitis media with effusion. Archives of Pediatrics & Adolescent Medicine 2005;159(12):1151-6. [CENTRAL: CN-00532329] [PMID: ] [DOI] [PubMed] [Google Scholar]
Tao 2004 {published data only}
- Tao LH, He D-H, Huang Y-D. Effects of adenoidectomy in treatment of secretory otitis media in children. Journal of Clinical Pediatric Surgery 2004;4:253-5. [CENTRAL: CN-00849652] [Google Scholar]
Uvarova 2001 {published data only}
- Uvarova N. Comparison of the results of treatment of otitis media with effusion after myringotomy with and without ventiliation tube. In: 4th Extraordinary International Symposium on Recent Advances in Otitis Media; 2001 Apr 16-20, Sendai (Japan). 2001:165. [ABSTRACT NO.: 122] [CENTRAL: CN-00362633]
Xu 2016 {published data only}
- Xu WM, Ye YH. Effect of tympanostomy tube insertion with adenoidectomy for children with recurrent otitis media with effusion. Lin Chuang Er Bi Yan Hou Tou Jing Wai Ke za Zhi [Journal of Clinical Otorhinolaryngology, Head, and Neck Surgery] 2016;30(23):1873-5. [CENTRAL: CN-01614396] [EMBASE: 622451696] [PMID: ] [DOI] [PubMed] [Google Scholar]
Yousaf 2014 {published data only}
- Yousaf M, Malik SA, Zada B. Laser and incisional myringotomy in otitis media with effusion-a comparative study. Journal of Ayub Medical College, Abbottabad 2014;26(4):441-3. [CENTRAL: CN-01043373] [PMID: ] [PubMed] [Google Scholar]
Youssef 2013 {published data only}
- Youssef TF, Ahmed MR. Laser-assisted myringotomy versus conventional myringotomy with ventilation tube insertion in treatment of otitis media with effusion: long-term follow-up. Interventional Medicine and Applied Science 2013;5(1):16-20. [CENTRAL: CN-01043520] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies awaiting assessment
Diacova 2016 {published data only}
- Diacova S, McDonald TJ, Ababii I. Clinical, functional, and surgical findings in chronic bilateral otitis media with effusion in childhood. Ear, Nose, & Throat Journal 2016;95(8):E31-7. [CENTRAL: CN-01339417] [EMBASE: 614412861] [PMID: ] [PubMed] [Google Scholar]
Marshak 1980 {published data only}
- Marshak G, Neriah ZB. Adenoidectomy versus tympanostomy in chronic secretory otitis media. Annals of Otology, Rhinology, and Laryngology. Supplement 1980;89(3 Part 2):316-8. [DOI] [PubMed] [Google Scholar]
Maw 1986 {published data only}
- Maw AR. Adenoidectomy and adenotonsillectomy for otitis media with effusion in children: a prospective randomized controlled study (Masters thesis). Bristol, UK: University of Bristol, 1986. [CENTRAL: CN-00849155] [Google Scholar]
Tawfik 2002 {published data only}
- Tawfik S, Belal A, Sorour W. A comparative study of the different treatment modalities of otitis media with effusion in children. In: 8th International Congress of Paediatric Otorhinolaryngology (ESPO). Oxford, UK, 11-14 September, 2002. 2002:151. [ABSTRACT NUMBER: P2.26] [CENTRAL: CN-00508402]
References to ongoing studies
ACTRN12611001073998 {unpublished data only}
- ACTRN12611001073998. Surgery for otitis media in Indigenous Australian children [A 12 month, multi-centred, randomized trial to compare the outcomes of two surgical and one medical intervention on chronic Otitis Media in Indigenous children living in remote communities of Australia. Medicine V surgery sub-study]. www.anzctr.org.au/ACTRN12611001073998.aspx (first received 17 October 2011). [CENTRAL: CN-01012938]
NCT02546518 {published data only}
- NCT02546518. A comparison of surgical and a new non-surgical treatment methods for secretory otitis media in children- hearing and socioeconomic aspects. clinicaltrials.gov/show/nct02546518 (first received 11 September 2015). [CENTRAL: CN-01102072]
NCT04584073 {published data only}
- NCT04584073. Secretory otitis media in adenoids hypertrophy patients [Comparison between the fate of secretory otitis media in patients with adenoids hypertrophy undergoing adenoidectomy alone or with myringotomy or with myringotomy and tympanostomy tube application]. clinicaltrials.gov/show/NCT04584073 (first received 12 October 2020). [CENTRAL: CN-02181953]
Additional references
Abidin 1995
- Abidin RR. Parenting Stress Index: Professional Manual. 3rd edition. Odessa, FL: Psychological Assessment Resources, 1995. [Google Scholar]
Achenbach 2011
- Achenbach TM. Child Behavior Checklist. In: Kreutzer JS, DeLuca J, Caplan B, editors(s). Encyclopedia of Clinical Neuropsychology. New York, NY: Springer, 2011. [DOI: 10.1007/978-0-387-79948-3_1529] [DOI] [Google Scholar]
Bayley 2006
- Bayley N. Bayley Scales of Infant and Toddler Development. 3rd edition. San Antonio, TX: Harcourt Assessment, Inc, 2006. [Google Scholar]
Bennett 1999
- Bennett KE, Haggard MP. Behaviour and cognitive outcomes from middle ear disease. Archives of Disease in Childhood 1999;80:28-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bennett 2001
- Bennett KE, Haggard MP, Silva PA, Stewart IA. Behaviour and developmental effects of otitis media with effusion into the teens. Archives of Disease in Childhood 2001;85:91-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Berkman 2013
- Berkman ND, Wallace IF, Steiner MJ, Harrison M, Greenblatt AM, Lohr KN, et al. Otitis Media with Effusion: Comparative Effectiveness of Treatments. Vol. Report No.: 13-EHC091-EF. Rockville (MD): Agency for Healthcare Research and Quality (US), 2013. [PMID: ] [PubMed] [Google Scholar]
Browning 2010
- Browning GG, Rovers MM, Williamson I, Lous J, Burton MJ. Grommets (ventilation tubes) for hearing loss associated with otitis media with effusion in children. Cochrane Database of Systematic Reviews 2010, Issue 10. Art. No: CD001801. [DOI: 10.1002/14651858.CD001801.pub3] [DOI] [PubMed] [Google Scholar]
Bruce 2015
- Bruce I, Harman N, Williamson P, Tierney S, Callery P, Mohiuddin S, et al. The management of Otitis Media with Effusion in children with cleft palate (mOMEnt): a feasibility study and economic evaluation. Health Technology Assessment 2015;19(68):1-374. [DOI: 10.3310/hta19680] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cheong 2012
- Cheong KH, Hussain SS. Management of recurrent acute otitis media in children: systematic review of the effect of different interventions on otitis media recurrence, recurrence frequency and total recurrence time. Journal of Laryngology & Otology 2012;126(9):874-85. [DOI] [PubMed] [Google Scholar]
Cochrane ENT 2020
- Cochrane ENT. Otitis media with effusion: a project to prioritise Cochrane systematic reviews. https://ent.cochrane.org/otitis-media-effusion-ome-glue-ear 2020 (accessed 3 November 2021).
de Beer 2004
- Beer B, Schilder AGM, Zielhuis GA, Ingels K, Graamans K. Hearing loss in young adults who had ventilation tube insertion in childhood. Annals of Otology, Rhinology, and Laryngology 2004;113(6):438-44. [DOI: 10.1177/000348940411300604] [DOI] [PubMed] [Google Scholar]
de Beer 2005
- Beer BA, Schilder AGM, Zielhuis GA, Graamans K. Natural course of tympanic membrane pathology related to otitis media and ventilation tubes between ages 8 and 18 years. Otology & Neurotology 2005;26(5):1016-21. [DOI: 10.1097/01.mao.0000185058.89586.ed] [DOI] [PubMed] [Google Scholar]
Dunn 2007
- Dunn LM, Dunn DM. Peabody Picture Vocabulary Test (PPVT™-4). 4th edition. Pearson Education, 2007. [Google Scholar]
Fekkes 2000
- Fekkes M, Theunissen NC, Brugman E, Veen S, Verrips EGH, Koopman HM, et al. Development and psychometric evaluation of the TAPQOL: a health-related quality of life instrument for 1–5-year-old children. Quality of Life Research 2000;9:961-72. [DOI: 10.1023/a:1008981603178] [DOI] [PubMed] [Google Scholar]
Flynn 2009
- Flynn T, Möller C, Jönsson R, Lohmander A. The high prevalence of otitis media with effusion in children with cleft lip and palate as compared to children without clefts. International Journal of Pediatric Otorhinolaryngology 2009;73:1441-6. [DOI: 10.1016/j.ijporl.2009.07.015] [DOI] [PubMed] [Google Scholar]
Galbraith 2023
- Galbraith K, Mulvaney CA, MacKeith S, Marom T, Daniel M, Venekamp RP, et al. Autoinflation for otitis media with effusion (OME) in children. Cochrane Database of Systematic Reviews 2023, Issue 9. Art. No: CD015253. [DOI: 10.1002/14651858.CD015253.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Goodman 1997
- Goodman R. The Strengths and Difficulties Questionnaire: a research note. Journal of Child Psychology and Psychiatry 1997;38:581-6. [DOI: 10.1111/j.1469-7610.1997.tb01545.x] [DOI] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- GRADEpro GDT. Hamilton (ON): McMaster University (developed by Evidence Prime), accessed 27 February 2023. Available at gradepro.org.
Gresham 1990
- Gresham FM, Elliott SN. Social Skills Rating System. Circle Pines, MN: American Guidance Service, 1990. [Google Scholar]
Griffiths 1996
- Griffiths R. The Griffiths mental development scales from birth to two years, manual, the 1996 revision. Henley: Association for Research in Infant and Child Development, Test Agency, 1996. [Google Scholar]
Haggard 2003
- Haggard MP, Smith SC, Nicholls EE. Quality of life and child behaviour. In: Rosenfeld RM, Bluestone CD, editors(s). Evidence-based Otitis Media. 2nd edition. Hamilton, Ontario: BC Decker Inc, 2003:401-29. [https://researchonline.lshtm.ac.uk/id/eprint/15108] [Google Scholar]
Hedrick 1984
- Hedrick DL, Prather EM, Tobin AR. Sequenced Inventory of Communication Development. Seattle, WA: University of Washington Press, 1984. [Google Scholar]
Higgins 2011
- Higgins JPT, Altman DG, Sterne JAC (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
Higgins 2021
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (updated February 2021). Cochrane, 2021. Available from training.cochrane.org/handbook. [DOI] [PMC free article] [PubMed]
Jellinek 1988
- Jellinek MS, Murphy JM, Robinson J, Feins A, Lamb S, Fenton T. Pediatric Symptom Checklist: screening school-age children for psychosocial dysfunction. Journal of Pediatrics 1988;112(2):201-9. [DOI: 10.1016/s0022-3476(88)80056-8] [DOI] [PubMed] [Google Scholar]
Kreiner‐Møller 2012
- Kreiner-Møller E, Chawes BL, Caye-Thomasen P, Bønnelykke K, Bisgaard H. Allergic rhinitis is associated with otitis media with effusion: a birth cohort study. Clinical and Experimental Allergy 2012;42(11):1615-20. [DOI: 10.1111/j.1365-2222.2012.04038.x] [DOI] [PubMed] [Google Scholar]
Laina 2006
- Laina V, Pothier DD. Should we aspirate middle‐ear effusions prior to insertion of ventilation tubes? Journal of Laryngology and Otology 2006;120:818-21. [DOI: 10.1017/S0022215106002118] [DOI] [PubMed] [Google Scholar]
Landgraf 1994
- Landgraf JM. The Infant/Toddler Child Health Questionnaire: conceptual framework, logic content, and preliminary psychometric results. Boston: Health Act, 1994. [Google Scholar]
Landgraf 1996
- Landgraf JL, Abetz L, Ware JE. The CHQ User’s Manual. Boston: The Health Institute, New England Medical Center, 1996. [Google Scholar]
Lefebvre 2020
- Lefebvre C, Glanville J, Briscoe S, Littlewood A, Marshall C, Metzendorf M-I, et al. Technical Supplement to Chapter 4: Searching for and selecting studies. Higgins JPT, Thomas J, Chandler J, Cumpston MS, Li T, Page MJ, et al, editors(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.1 (updated September 2020). Cochrane, 2020. Available from training.cochrane.org/handbook.
Liu 2020
- Liu PZ, Ismail-Koch H, Stephenson K, Donne AJ, Fergie N, Derry J, et al. A core outcome set for research on the management of otitis media with effusion in otherwise-healthy children. International Journal of Pediatric Otorhinolaryngology 2020 ;134:Article 110029. [DOI: 10.1016/j.ijporl.2020.110029] [DOI] [PubMed]
MacKeith 2023
- MacKeith S, Mulvaney CA, Galbraith K, Marom T, Daniel M, Venekamp RP, et al. Adenoidectomy for otitis media with effusion (OME) in children. Cochrane Database of Systematic Reviews 2023, Issue 10. Art. No: CD015252. [DOI: 10.1002/14651858.CD015252.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Maris 2014
- Maris M, Wojciechowski M, Van de Heyning P, Boudewyns A. A cross-sectional analysis of otitis media with effusion in children with Down syndrome. European Journal of Pediatrics 2014;173:1319-25. [DOI: 10.1007/s00431-014-2323-5] [DOI] [PubMed] [Google Scholar]
Marseglia 2008
- Marseglia GL, Pagella F, Caimmi D, Caimmi S, Castellazzi AM, Poddighe D, et al. Increased risk of otitis media with effusion in allergic children presenting with adenoiditis. Otolaryngology – Head and Neck Surgery 2008;138(5):572-5. [DOI: 10.1016/j.otohns.2008.01.020] [DOI] [PubMed] [Google Scholar]
Marshall 2018
- Marshall J, Noel-Storr AH, Kuiper J, Thomas J, Wallace BC. Machine learning for identifying randomized controlled trials: an evaluation and practitioner's guide. Research Synthesis Methods 2018;9(4):602-14. [DOI: 10.1002/jrsm.1287] [DOI] [PMC free article] [PubMed] [Google Scholar]
McCarthy 1972
- McCarthy D. Manual for the McCarthy Scales of Children's Abilities. New York: Psychological Corp, 1972. [Google Scholar]
McDonald 2017
- McDonald S, Noel-Storr AH, Thomas J. Harnessing the efficiencies of machine learning and Cochrane Crowd to identify randomised trials for individual Cochrane reviews. In: Global Evidence Summit; 2017 Sep 13-17; Cape Town, South Africa. 2017.
Mulvaney 2023a
- Mulvaney CA, Galbraith K, MacKeith S, Marom T, Daniel M, Venekamp RP, et al. Antibiotics for otitis media with effusion (OME) in children. Cochrane Database of Systematic Reviews 2023, Issue 10. Art. No: CD015254. [DOI: 10.1002/14651858.CD015254.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mulvaney 2023b
- Mulvaney CA, Galbraith K, MacKeith S, Marom T, Daniel M, Venekamp RP, et al. Topical and oral steroids for otitis media with effusion (OME) in children. Cochrane Database of Systematic Reviews 2023, Issue 10. Art. No: CD015255. [DOI: 10.1002/14651858.CD015255.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
NICE 2008
- NICE. Otitis media with effusion in under 12s: Otitis media with effusion in under 12s: surgery (CG60). Available at: https://www.nice.org.uk/guidance/cg60 2008.
NICE CKS 2021
- NICE. Otitis media with effusion (Clinical Knowledge Summary). Available at: https://cks.nice.org.uk/topics/otitis-media-with-effusion/ 2021.
Noel‐Storr 2018
- Noel-Storr AH. Cochrane Crowd: new ways of working together to produce health evidence. In: Evidence Live; 2018 Jun 18-20; Oxford, UK. 2018.
Rabin 2001
- Rabin R, Charro F. EQ-5D: a measure of health status from the EuroQol Group. Annals of Medicine 2001;33(5):337-43. [DOI: 10.3109/07853890109002087] [DOI] [PubMed] [Google Scholar]
RevMan 2020 [Computer program]
- Review Manager (RevMan). Version 5.4. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2020.
Reynell 1985
- Reynell JH. Reynell Development Language Scales Manual. 2nd edition. Windsor, UK: NFER-NELSON, 1985. [Google Scholar]
Rosenfeld 1997
- Rosenfeld RM, Goldsmith AJ, Tetlus L, Balzano A. Quality of life for children with otitis media. Archives of Otolaryngology - Head & Neck surgery 1997;123:1049-54. [DOI: 10.1001/archotol.1997.01900100019002] [DOI] [PubMed] [Google Scholar]
Rosenfeld 2000
- Rosenfeld RM, Bhaya MH, Bower CM, Brookhouser PE, Casselbrant ML, Chan KH, et al. Impact of tympanostomy tubes on child quality of life. Archives of Otolaryngology - Head & Neck Surgery 2000;126:585-92. [DOI] [PubMed] [Google Scholar]
Rosenfeld 2003
- Rosenfeld RM, Kay D. Natural history of untreated otitis media. Laryngoscope 2003;113:1645-57. [DOI: 10.1097/00005537-200310000-00004] [DOI] [PubMed] [Google Scholar]
Rosenfeld 2016
- Rosenfeld RM, Shin JJ, Schwartz SR, Coggins R, Gagnon L, Hackell JM, et al. Clinical practice guideline: otitis media with effusion (update). Otolaryngology - Head & Neck Surgery 2016;154:S1-S41. [DOI: 10.1177/0194599815623467] [DOI] [PubMed] [Google Scholar]
Schilder 2016
- Schilder AGM, Chonmaitree T, Cripps AW, Rosenfeld RM, Casselbrant ML, Haggard MP, et al. Otitis media. Nature Reviews Disease Primers 2016;2(1):16063. [DOI: 10.1038/nrdp.2016.63] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schlichting 2007
- Schlichting JEPT, Lutje Spelberg HC. Lexilijst Begrip: An Instrument to Investigate Language Comprehension in Children aged 15-25 Months in the Context of Early Identification. Amsterdam: Pearson Assessment & Information BV, 2007. [Google Scholar]
Schlichting 2010
- Schlichting JEPT, Lutje Spelberg HC. Schlichting Test for Language Comprehension; Instruction Manual. Woooden: Bohn Stafleu van Loghum, 2010. [Google Scholar]
Schmalbach 2021
- Schmalbach CE, Brereton J, Bowman C, Denneny JC. American Academy of Otolaryngology–Head and Neck Surgery/Foundation Reg-ent Registry: Purpose, Properties, and Priorities. Otolaryngology–Head and Neck Surgery 2021;164(5):964-71. [DOI] [PubMed] [Google Scholar]
Steele 2017
- Steele D, Adam GP, Di M, Halladay C, Pan I, Coppersmith N, et al. Tympanostomy tubes in children with otitis media. Comparative Effectiveness Review No. 185 (Prepared by the Brown Evidence-based Practice Center under Contract No. 290-2015-00002-I.). AHRQ Publication No. 17-EHC003-EF. Rockville, MD: Agency for Healthcare Research and Quality, 2017. [DOI: 10.23970/AHRQEPCCER185] [DOI] [PubMed] [Google Scholar]
Thomas 2017
- Thomas J, Noel-Storr AH, Marshall I, Wallace B, McDonald S, Mavergames C, et al, Living Systematic Review Network. Living systematic reviews 2: combining human and machine effort. Journal of Clinical Epidemiology 2017;91:31-7. [DOI: 10.1016/j.jclinepi.2017.08.011] [DOI] [PubMed] [Google Scholar]
TNO 1997
- TNO—Prevention and Health/LUMC. TAIQOL—Questionnaire for parents of children aged 1—5 years. Leiden, The Netherlands: Leiden University Medical Center, 1997. [Google Scholar]
van den Aardweg 2010
- den Aardweg MTA, Schilder AGM, Herkert E, Boonacker CWB, Rovers MM. Adenoidectomy for otitis media in children. Cochrane Database of Systematic Reviews 2010, Issue 1. Art. No: CD007810. [DOI: 10.1002/14651858.CD007810.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vanneste 2019
- Vanneste P, Page C. Otitis media with effusion in children: pathophysiology, diagnosis, and treatment. A review. Journal of Otolaryngology - Head & Neck Surgery 2019;14(2):33-9. [DOI: 10.1016/j.joto.2019.01.005] [DOI] [PMC free article] [PubMed] [Google Scholar]
Venekamp 2018
- Venekamp RP, Mick P, Schilder AGM, Nunez DA. Grommets (ventilation tubes) for recurrent acute otitis media in children. Cochrane Database of Systematic Reviews 2018, Issue 5. Art. No: CD012017. [DOI: 10.1002/14651858.CD012017.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Verrips 1998
- Verrips GH, Vogels AGC, Verloove-Vanhorick SP, Fekkes M, Koopman HM, Kamphuis RP, et al. Health-related quality of life measure for children - the TACQOL. Journal of Applied Therapeutics 1998;1(4):357-60. [Google Scholar]
Wallace 2014
- Wallace IF, Berkman ND, Lohr KN, Harrison MF, Kimple AJ, Steiner MJ. Surgical treatments for otitis media with effusion: a systematic review. Pediatrics 2014;133(2):296-311. [DOI: 10.1542/peds.2013-3228] [DOI] [PubMed] [Google Scholar]
Wallace 2017
- Wallace BC, Noel-Storr A, Marshall IJ, Cohen AM, Smalheiser NR, Thomas J. Identifying reports of randomized controlled trials (RCTs) via a hybrid machine learning and crowdsourcing approach. Journal of the American Medical Informatics Association 2017;24(6):1165-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Williamson 2011
- Williamson I. Otitis media with effusion in children. BMJ Clinical Evidence 2011;2011:0502. [PMID: ] [PMC free article] [PubMed] [Google Scholar]
Zernotti 2017
- Zernotti ME, Pawankar R, Ansotegui I, Badellino H, Croce JS, Hossny E, et al. Otitis media with effusion and atopy: is there a causal relationship? World Allergy Organization Journal 2017;10(1):37. [DOI: 10.1186/s40413-017-0168-x] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zielhuis 1990
- Zielhaus GA, Rach GH, den Broek P. The occurrence of otitis media with effusion in Dutch pre-school children. Clinical Otolaryngology & Allied Sciences 1990;15(2):147-53. [DOI] [PubMed] [Google Scholar]
Zimmermann 1992
- Zimmerman IL, Steiner VG, Pond RE. Preschool Language Scale-3. San Antonio, TX: The Psychological Corporation, 1992. [Google Scholar]
References to other published versions of this review
MacKeith 2022
- MacKeith S, Mulvaney CA, Galbraith K, Marom T, Daniel M, Venekamp RP, et al. Ventilation tubes (grommets) for otitis media with effusion (OME) in children. Cochrane Database of Systematic Reviews 2022, Issue 3. Art. No: CD015215. [DOI: 10.1002/14651858.CD015215] [DOI] [PMC free article] [PubMed] [Google Scholar]


