Abstract
Latinx sexual minority men (LSMM) face multilevel barriers to accessing HIV pre-exposure prophylaxis (PrEP). To address these barriers, we designed and implemented community-based organization (CBO)-PrEP, a collaborative community-based telehealth PrEP program for LSMM. We designed this PrEP delivery program through a collaborative process involving staff from local CBOs and a primary care-based HIV prevention program. Staff met weekly over a 3-month period to establish protocols for referrals, obtaining insurance coverage, and navigation to appointments and laboratory testing. To assess feasibility, we extracted electronic medical record data including demographics and clinical outcomes of PrEP care. Between December 2020 and May 2023, 102 individuals were referred to CBO-PrEP of which 85 had Hispanic/Latino as their ethnicity in their medical records; out of 102 individuals, 72 (70.6%) were scheduled for an initial appointment. Out of 72 individuals scheduled for an appointment, 58 (80.6%) were seen by a health care provider a median of 7.5 days after referral [interquartile range (IQR), 2–19]; 48 (82.6%) of initial appointments were through telemedicine, 10 (17.2%) were seen in person. Of the 48 patients who had a telehealth appointment, 36 (75%) underwent initial laboratory testing and 42 (87.5) were prescribed PrEP; all 10 patients who were seen in person underwent laboratory testing and were prescribed PrEP. PrEP prescriptions were received in a median of 17.5 days (IQR 4.5–33.5) after referral. CBO-PrEP successfully engaged LSMM, a population that is often hard to reach. Expanding collaborative approaches with CBOs could have a significant impact on improving PrEP uptake for LSMM and other priority populations.
Keywords: pre-exposure prophylaxis, men who have sex with men, Latino, community-based organization, implementation science
Introduction
Latinx sexual minority men (LSMM) are disproportionately impacted by HIV, accounting for one in four HIV diagnoses in the United States.1 Pre-exposure prophylaxis (PrEP) is highly effective at preventing HIV and is recommended for all people with increased vulnerability to HIV acquisition.2 However, few LSMM use it: nationally, only 14% of Hispanic/Latino individuals estimated to benefit from PrEP have received a prescription.3
Key structural barriers limit PrEP access for LSMM, including limited English proficiency, low rates of health insurance coverage, and lack of primary care,4 factors that may be compounded by immigration-related fears of accessing care.5,6 At the individual level, competing everyday demands, time/transportation, stigma and discrimination related to ethnicity, HIV, PrEP, sexual orientation, and gender identity create additional barriers to accessing PrEP.7–9
There is an emerging consensus that tailored, low-barrier approaches are necessary to increase PrEP uptake among the groups that could most benefit from it.10–12 One such low-barrier strategy is telemedicine, defined as the provision of health care remotely through telephone or video technology, which is increasingly being utilized in the United States and has demonstrated effectiveness for PrEP uptake and persistence.13–15 Telehealth can be leveraged to address prevalent barriers such as geographic distance, time, transportation, and stigma encountered in health care settings.16,17
However, published data on telemedicine-based PrEP are largely limited to non-Latinx persons, primarily or Black sexual minority men.13,14,18 A small telemedicine-based PrEP project in Los Angeles targeting young sexual minority men of color included only 10 Latinx individuals.19 Therefore, it remains unclear whether telemedicine-based PrEP can address barriers among LSMM.
In response to this critical gap, we developed community-based organization (CBO)-PrEP, a low-barrier telemedicine-based PrEP service tailored to LSMM. We collaborated with three CBOs serving LSMM in New York City (NYC), leveraging their community-engaged sex-positive approach to design a care delivery program that could address specific HIV prevention needs for LSMM in NYC. In this study, we describe the development and implementation of CBO-PrEP as well as its feasibility for engaging LSMM in PrEP.
Methods
Setting
Nearly 30% of NYC's residents are Latinxs, who represent >20 different ethnic/nationality groups and together make up the largest immigrant group in the city as well as the largest group of undocumented immigrants.20 Nearly half of Latinx households live in poverty;21 one third of working Latinxs are employed in the service industry (34%) and 22% lack health insurance.22–26 NYC is an epicenter of HIV; overall prevalence is 1.2% and is >2% in Bronx and Queens.27 Although Latinxs represent less than a third of the city's population, among 1594 new HIV diagnoses in 2021, 593 (37.2%) occurred among Latinx individuals: 485 (82%) were among men. Latinxs represented 44% of all new infections among men who have sex with men in NYC in 2021, a 14% increase from 2020.27,28
Nationally and in New York State, significant disparities exist with respect to PrEP use, with Latinx individuals using PrEP at a rate three times lower than White individuals.10 This disparity persists in NY despite the mandate that all health insurances cover PrEP-related clinical care and medications, existence of the New York State PrEP Patient Assistance Program (PrEP-AP) that covers PrEP-related clinical care, and medication assistance programs [from manufacturers and the Health Resources and Services Administration's (HRSA) Ready-Set-PrEP programs] that cover medication costs for most individuals without insurance coverage.29
CBO-PrEP development and refinement
CBO-PrEP was designed and first implemented as a collaboration between the Montefiore Prevention Program (MPP), a primary care-based HIV prevention service located in Bronx that provides free HIV testing and linkage to sexual health services, and the Oasis Community Pride Center (Oasis), a drop-in sexual health center run by the Latino Commission on AIDS (LCOA). Oasis is located in the Chelsea neighborhood of Manhattan, and provides a package of services that includes testing for HIV and other sexually transmitted infections (STIs), assistance with obtaining medical insurance and referral to PrEP, postexposure prophylaxis (PEP), and mental health care providers. After initially piloting CBO-PrEP with Oasis, we expanded to two additional CBOs, Voces Latinas (Voces) and Destination Tomorrow (DT).
Voces Latinas (Voces) is located in Jackson Heights, Queens, a neighborhood with a high concentration of recently arrived Latinx immigrants. The organization offers a range of sexual health services geared to the Latinx community, including HIV testing and referral to PrEP and PEP services. DT is located in South Bronx, a predominantly Black and Latinx area in NYC, and provides comprehensive sexual health and gender-affirming services including HIV testing and referrals to PrEP and PEP. All three CBOs have programs and outreach strategies focused on LSMM, some of the staff at each organization are LSMM, and each CBO offers services in Spanish and English; MPP provides live interpretation services when the medical provider or patient navigator does not speak Spanish.
The CBO-PrEP model was designed through a collaborative equitable process by a core team consisting of two medical providers, a health services researcher and a patient navigator from the MPP, and the director of programming at Oasis, and the director of monitoring, evaluation and learning at Oasis/LCOA.
The core team met weekly from June to December 2020 to determine which CBO and MPP personnel would be involved and the extent of their roles, establish communication and patient hand-off protocols between the MPP and CBO navigators, develop workflows for verifying insurance status and the process for obtaining insurance coverage (through PrEP-AP or other insurance if eligible) if needed, determine scheduling availability of providers, identify commercial laboratories that accept PrEP-AP, and develop workflows for placing orders for and navigating patients to commercial laboratories.
Through this process, we centered CBO-PrEP on three broad implementation strategies with high potential to address structural and individual barriers impacting access to PrEP for LSMM: (1) telemedicine appointments, (2) conavigation delivered in partnership between CBO and health center staff, and (3) offering patients flexible care options (e.g., PrEP-related diagnostic testing at a network of commercial laboratories with locations throughout NYC, evening appointments and bilingual navigation staff) (Table 1).
Table 1.
Components of Community-Based Organization-Pre-Exposure Prophylaxis and Barriers Addressed
| Strategy | Barriers addressed |
|---|---|
| Telehealth | Distance to clinic, lack of transportation, limited time availability, competing demands, discomfort in health settings. |
| Conavigation | Complexity of health care system, lack of insurance, limited awareness of available benefits. |
| Commercial laboratories | Distance to clinic, lack of transportation, limited time availability, competing demands, discomfort in health settings. |
| Cultural competency | Immigration concerns, stigma in health settings, cultural and language barriers, low medical literacy. |
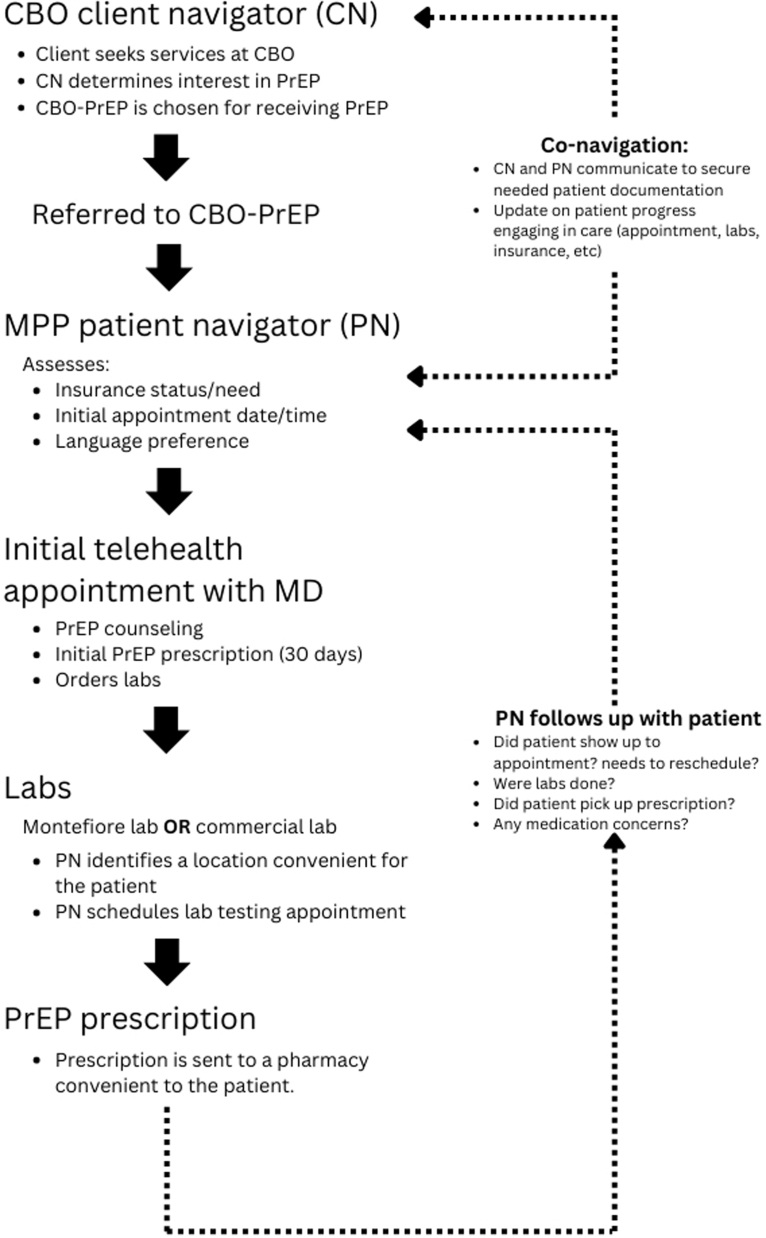
The final workflow for CBO-PrEP referrals consisted of the following steps (Fig. 1): (1) clients interested in PrEP meet with a CBO navigator who provides culturally responsive information (i.e., emphasizing the needs and priorities of the client, offering materials in Spanish with visual representations of diverse Latinx individuals) about PrEP, determines insurance status and provides guidance for applying for insurance or PrEP-AP New York's PrEP if needed; (2) the CBO navigator then contacts the MPP navigator, who schedules a telehealth appointment (or, if preferred, an in-person appointment at a Montefiore health center) with a provider at a time convenient for the patient, confirms the patient's insurance status, facilitates applying for coverage and for medication assistance if needed, and assists with selecting a pharmacy and location for diagnostic tests; (3) the patient has a medical appointment with a physician who reviews relevant medical and sexual history, determines candidacy for PrEP, provides counseling on appropriate use of PrEP, and orders relevant laboratory tests; and (4) the MPP navigator follows up with the patient to address any issues concerning insurance or laboratory testing, ensure prescriptions were obtained at the pharmacy, and schedule a follow-up appointment.
FIG. 1.
CBO-pre-exposure prophylaxis process for patients referred from a CBO site to a Montefiore primary care HIV prevention clinic. CBO, community-based organization.
Between appointments, the MPP navigator also reminds patients of their next appointment through a text message, phone call, email, or MyChart (electronic health record patient portal) messages and reschedules when needed.
In December 2020, we launched CBO-PrEP: the staff at Oasis and MPP were trained on the CBO-PrEP protocol, and Oasis staff began to navigate clients to the program. The core team continued to meet monthly throughout 2021 to discuss and resolve emerging issues in the workflow and protocols. Starting in January 2022, CBO-PrEP was expanded to two additional CBOs, Voces and DT.
Data collection and analysis
We extracted the following information from patients' electronic medical records: age, insurance status, borough of residence, preferred language, appointment dates, date of and number of contacts with the MPP navigator, laboratory test results, and PrEP prescriptions (including dates and number of pills prescribed). When available in the medical record, we also extracted gender of sexual partners, condom use (documented as always, inconsistent, or never), history of any STI, and receptive and insertive anal sex practices. We also qualitatively reviewed electronic health records (EMR) documentation from medical appointment visits and provider and MPP patient navigator notes to identify reasons for missed appointments and discontinuation from care. Data were stored in a deidentified password-protected Excel database.
To assess feasibility, we measured the proportions of individuals referred to CBO-PrEP who were linked to care, scheduled for an appointment, seen by a provider, and who received a PrEP prescription. Additional outcomes of interest included time from referral to first appointment, time from referral to PrEP prescription, the proportions using telemedicine or in-person appointments, and the proportions who underwent diagnostic testing at an MPP facility or a commercial laboratory.
The study was approved by the Albert Einstein College of Medicine Institutional Review Board, which granted a waiver of informed consent for analysis of routine clinical data.
Results
Between December 2020 and May 2023, 102 individuals were referred to CBO-PrEP. Median age was 29.5 years and 75 (73.5%) identified their gender as male (Table 2). Among all patients, 18 (17.6%) had private health insurance, 15 (14.7%) had Medicaid or Medicare, and 69 (67.6%) were uninsured at the time of referral. Most patients (43, 42.2%) resided in Queens and 62 (60.8%) indicated Spanish as their preferred language. Among 46 men whose medical records contained information on sexual partners, 41 (89%) reported exclusively having male sexual partners, and 39 (85%) reported receptive anal intercourse. Among 38 records with documented information on condom use, 29 (76.3%) reported inconsistent condom use, and of 44 patients with documented STI history, 23 (52%) reported ever having an STI.
Table 2.
Demographic Characteristics of Community-Based Organization-Pre-Exposure Prophylaxis Patients, N = 102
| Age (median, std dev) | 29.5 (9.9) |
| Gender | |
| Male | 75 (73.5%) |
| Female | 24 (23.5%) |
| Trans female | 3 (2.9%) |
| Ethnicity | |
| Latinx/Hispanic | 85 (83.3%) |
| Not Latinx/Hispanic | 5 (4.9%) |
| Not recorded | 12 (11.8%) |
| Insurance at time of referral | |
| Private | 18 (17.6%) |
| Medicaid | 13 (12.7%) |
| Medicare | 2 (2%) |
| Uninsured | 69 (67.6%) |
| Borough | |
| Bronx | 22 (21.6%) |
| Manhattan | 15 (14.7%) |
| Brooklyn | 15 (14.7%) |
| Queens | 43 (42.2) |
| Staten island | 2 (2%) |
| Other | 5 (4.9%) |
| Referring CBO | |
| Oasis | 44 (43.1% |
| Destination tomorrow | 13 (12.7%) |
| Voces Latinas | 43 (42.2%) |
| Other | 2 (2%) |
| Spanish preferred | 62 (60.9%) |
CBO, community-based organization.
Out of 102 referred patients, 9 were never engaged in care due to lack of response to the navigator's contact attempts, declining PrEP, or deciding to obtain PrEP from a different provider. Seventy-two (70.6%) patients were scheduled for an initial appointment with a median of two contacts from the MPP patient navigator; three did not show up to their appointments and were lost to care after the MPP navigator was unable to reach them again (Table 3). The median number of days from referral to the first scheduled appointment was 6.5 [interquartile range (IQR), 2–13].
Table 3.
Outcomes of initial Pre-Exposure Prophylaxis engagement for Community-Based Organization-Pre-Exposure Prophylaxis Patients (N = 102)
| Had a scheduled appointmenta | |
| Yes | 72 (70.6%) |
| Attended appointment (n = 72) | |
| Yes | 58 (80.6%) |
| Patient navigator telephone contact with patients before appointment, median (IQR) | 2 (1–4) |
| Days from referral to scheduled appointment, median (IQR) | 6.5 (2–13) |
| Days from referral to kept appointment, median (IQR) | 7.5 (2–19) |
| Initial appointment modality (n = 58) | |
| Telemedicine | 48 (82.6%) |
| Office visit | 10 (17.2%) |
| No. of patients prescribed PrEP | 52 (51.0%) |
| Days from referral to PrEP prescription, median (IQR) | 17.5 (4.5–33.5) |
| Initial laboratories location | |
| Labcorp | 20 (43.5%) |
| Montefiore | 26 (56.5%) |
Scheduled appointment could have been cancelled by the patient or provider, or patient did not show to appointment.
IQR, interquartile range; PrEP, pre-exposure prophylaxis.
Of the 72 patients scheduled for an appointment, 58 (80.6%) were seen by a health care provider a median of 7.5 days after referral (IQR 2–19); 48 (82.6%) of these initial appointments were through telemedicine. Of the 48 patients who had a telehealth appointment, 36 (75%) underwent initial laboratory testing and 42 (87.5%) were prescribed PrEP; all 10 patients who were seen in person underwent laboratory testing and were prescribed PrEP. A total of 52 patients (87.7%) received a PrEP prescription a median of 17.5 days (IQR 4.5–33.5) after referral.
As of May 2023, among 58 patients seen for an initial appointment and with at least 4 months of follow-up time, 42 (72.4%) were seen for a second appointment, of whom 29 were telemedicine based. Diagnostic tests were completed for 21 patients (50.0%), including 7 (33.3%) done at a commercial laboratory. Of 37 patients due for a third appointment, 28 (75.6%) patients saw a provider, of whom 20 (71.4%) were telemedicine based. Out of 28 patients, diagnostic tests were completed for 17 (60.7%) patients; 3 (10.7%) used a commercial laboratory.
A total of 20 patients seen at least once for a medical appointment discontinued from care. Reasons for discontinuation included changing providers outside of Montefiore, change in insurance, moving out of New York state, and experiencing side effects.
Discussion
LSMM in NYC and elsewhere face substantial barriers to accessing comprehensive HIV prevention services, including PrEP. Research to enhance engagement in PrEP and other HIV prevention modalities among LSMM supports the implementation of strategies that address cost, logistical barriers, PrEP-related stigma, and syndemic challenges to service use.30–34 Following this approach, we designed and implemented CBO-PrEP, a program targeting these barriers by integrating culturally competent community-engaged services provided by CBOs with flexible options for patients (e.g., telemedicine, evening appointment times, diverse laboratory testing options, and access to services in Spanish).
We found CBO-PrEP to be highly feasible: a considerable proportion of patients were engaged in PrEP care rapidly after referral, most through telemedicine, and a large majority received a PrEP prescription. Notably, many patients were uninsured and with low English proficiency, populations that are often particularly hard to engage in care.35,36 The program also successfully reached young LSMM (24–34 years), an age group with elevated HIV incidence rates.1,12,37 Our findings highlight CBO-PrEP's potential to reach LSMM not currently engaged in HIV prevention services, thereby reducing persistent inequities in PrEP utilization, and ultimately contributing to a reduction in HIV incidence.
CBO-PrEP leveraged telehealth to address barriers related to geographic distance, time availability, and stigma encountered in health care settings by LSMM. Telehealth is an increasingly utilized modality for PrEP that is acceptable and convenient for many patients.16 However, prior studies have reported that Latinx individuals, particularly those with limited English proficiency, are less likely to use telehealth, a disparity that was exacerbated during the COVID-19 pandemic.38–40
Our results demonstrate the feasibility of community-based culturally sensitive telehealth as a strategy to engage LSMM in PrEP care, with clinical outcomes comparable with several other studies investigating telehealth for PrEP.13,14 Although at least one demonstration project intentionally targeted Black and LSMM in Los Angeles,19 that program was small (n = 25), included only 10 LSMM, and did not report follow-up data. Our real-world findings build on prior research to demonstrate that a telehealth program for LSMM can result in sustained engagement.
PrEP navigation is an established strategy to overcome structural barriers to care that both CBOs and health centers have successfully utilized to improve engagement.41–43 An innovative feature of CBO-PrEP was the use of conavigation to bridge CBO clients to clinical care, with CBO and health center navigators collaborating on both sides and communicating to resolve emerging issues for patients. Because CBO navigators were able to reach health center counterparts easily through text, phone, or email, and work together to obtain insurance coverage and determine appointment preferences, LSMM in CBO-PrEP were rapidly linked to PrEP.
The median time from initial referral to first appointment was 6.5 days, substantially faster than that reported by programs in Atlanta (16 weeks)18 or Los Angeles (6 weeks),19 which targeted Black and LSMM. Nonetheless, we have encountered delays in appointment scheduling related to missed connections between navigators and difficulty contacting patients. To address these barriers, we have implemented an online referral tool, and texting (rather than calling) patients, interventions that have demonstrated efficacy for PrEP and other care.44,45
There is a broad consensus that community engagement is critical to expanding PrEP and other HIV prevention efforts targeting LSMM.12,46,47 For the CBO-PrEP program, we leveraged ongoing community–academic partnerships to engage CBO patients in a locally relevant culturally appropriate manner, soliciting continuous input from CBO staff on best ways to communicate with clients, conduct outreach, and provide clinical care. CBO–academic partnerships are common for HIV prevention and care interventions.
However, few have incorporated CBO input into designing care delivery strategies or directly included CBOs in delivering care. Our three CBO partners have an established history of working with sexual and gender minority Latinxs in NYC. In practice, this encompasses outreach, education, and continued engagement strategies that each CBO has developed and tailored over time to work with distinct communities.
Routine laboratory monitoring testing is an essential part of PrEP initiation and maintenance but can make persistence in PrEP difficult for some individuals due to required travel time, transportation, and insurance status.11,48,49 CBO-PrEP offered patients the option to test at more conveniently located commercial laboratories, and almost half chose to do so. Although this option added flexibility for patients, we observed lower rates of complete laboratory testing among patients who used telehealth for their appointments, suggesting additional strategies may be needed to make this option viable. We also encountered challenges such as lost laboratory orders and refusal to process self-collected samples that varied by site, sometimes delaying the process for patients and requiring further assistance from the MPP navigator.
Although core components of CBO-PrEP can likely be adapted to many settings, there are important limitations to this program's generalizability. The large urban setting of NYC made the use of commercial laboratories feasible, since these are available throughout the city. In addition, when this option was not preferred by patients, they could use a robust public transportation system to visit an MPP clinic. In addition, the success of CBO-PrEP in linking a large number of uninsured patients to PrEP was facilitated by New York State's PrEP-AP,29 which provides broader coverage than many other states.
Coverage continues to be a barrier to access in different states with less robust PrEP-APs and without Medicaid expansion.50 In all settings, the use of telehealth requires access to technology, comfort using videoconferencing platforms, and a reliable internet connection, factors that could limit the success of a program such as CBO-PrEP among individuals with no access to these technologies.
Together with CBO partners, we developed and implemented a telehealth-based model for accessing PrEP tailored to LSMM. CBO-PrEP harnessed the cultural expertise of CBOs serving Latinx communities and the clinical capabilities of a large healthcare system to successfully link and engage LSMM in PrEP. By simultaneously addressing multilevel barriers experienced by LSMM, this model engaged individuals from populations that are often hard to reach, including those with limited English proficiency, young persons, and the uninsured. Expanding such cooperative approaches, including facilitating reimbursements for effective health center–CBO partnerships, could have a significant impact on improving PrEP uptake for LSMM and other priority populations.
Acknowledgments
We thank the teams at the Latino Commission on AIDS, Voces Latina, and Destination Tomorrow for their collaboration in this project.
Authors' Contributions
E.A.A. wrote the initial draft of the article, implemented program strategies, and analyzed data. J.R. is the principal investigator, developed the study concept and design, analyzed data, and edited the article. G.B., G.M., V.V.P., and E.N. contributed to the development of the study concept and design. All authors contributed to the interpretation of the data, made critical revisions to the article, and approved the final article draft.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
This study was supported by a pilot grant and an End the HIV Epidemic supplement from the Einstein-Rockefeller-CUNY Center for AIDS Research (P30 AI124414). The funder had no role in the design of the study and collection, analysis, and interpretation of data and in writing the article.
References
- 1. Centers for Disease Control and Prevention. HIV and Hispanic/Latino People: HIV Diagnosis. 2023. Available from: https://www.cdc.gov/hiv/group/racialethnic/hispanic-latino/diagnoses.html [Last accessed: May 5, 2023].
- 2. Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med 2010;363(27):2587–2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas, 2019. Vol. 26. 2021. HIV Surveillance Supplemental Report 2021. Available from: www.cdc.gov/hiv/library/reports/hiv-surveillance.html
- 4. Cohen RA, Terlizzi EP, Cha AE, Martinez ME. Health insurance coverage: Early release of estimates from the National Health Interview Survey, January–June 2020. National Center for Health Statistics; 2021. [Google Scholar]
- 5. Rhodes SD, Mann L, Simán FM, et al. The impact of local immigration enforcement policies on the health of immigrant Hispanics/Latinos in the United States. Am J Public Health 2015;105(2):329–337; doi: 10.2105/ajph.2014.302218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bonacci RA, Smith DK, Ojikutu BO. Toward greater pre-exposure prophylaxis equity: Increasing provision and uptake for Black and Hispanic/Latino individuals in the U.S. Am J Prev Med 2021;61(5 Suppl 1):S60–S72; doi: 10.1016/j.amepre.2021.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Harkness A, Lozano A, Bainter S, et al. Engaging Latino sexual minority men in PrEP and behavioral health care: Multilevel barriers, facilitators, and potential implementation strategies. J Behav Med 2023;46(4):655–667; doi: 10.1007/s10865-022-00371-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. García M, Harris AL. PrEP awareness and decision-making for Latino MSM in San Antonio, Texas. PLoS One 2017;12(9):e0184014; doi: 10.1371/journal.pone.0184014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Golub SA. PrEP stigma: Implicit and explicit drivers of disparity. Curr HIV/AIDS Rep 2018;15(2):190–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Epidemic. Et. ETE Dashboard. Ending the AIDS epidemic. 2022. Available from: https://etedashboardny.org/ [Last accessed: November 29, 2022].
- 11. Siegler A, Sullivan P. The PrEP laboratory service gap: Applying implementation science strategies to bring PrEP coverage to scale in the United States. J Law Med Ethics 2022;50(S1):40–46; doi: 10.1017/jme.2022.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rodriguez-Diaz CE, Martinez O, Bland S, et al. Ending the HIV epidemic in US Latinx sexual and gender minorities. Lancet 2021;397(10279):10.43–1045; doi: 10.1016/s0140-6736(20)32521-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hoth AB, Shafer C, Dillon DB, et al. Iowa TelePrEP: A public-health-partnered telehealth model for human immunodeficiency virus preexposure prophylaxis delivery in a rural state. Sex Transm Dis 2019;46(8):507–512; doi: 10.1097/olq.0000000000001017. [DOI] [PubMed] [Google Scholar]
- 14. Player MS, Cooper NA, Perkins S, Diaz VA. Evaluation of a telemedicine pilot program for the provision of HIV pre-exposure prophylaxis in the Southeastern United States. AIDS Care 2022;34(12):1499–1505; doi: 10.1080/09540121.2021.2018567. [DOI] [PubMed] [Google Scholar]
- 15. Zhang C, Fiscella K, Przybylek S, et al. Telemedicine experience for PrEP care among PrEP-eligible women and their primary care providers during the first year of the COVID-19 pandemic in the United States. Trop Med Infect Dis 2 2022;7(10)doi: 10.3390/tropicalmed7100280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wong KYK, Stafylis C, Klausner JD. Telemedicine: A solution to disparities in human immunodeficiency virus prevention and pre-exposure prophylaxis uptake, and a framework to scalability and equity. Mhealth 2020;6:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rousseau E, Julies RF, Madubela N, et al. Novel platforms for biomedical HIV prevention delivery to key populations—Community mobile clinics, peer-supported, pharmacy-led PrEP delivery, and the use of telemedicine. Curr HIV/AIDS Rep 2021;18(6):500–507; doi: 10.1007/s11904-021-00578-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rolle CP, Rosenberg ES, Siegler AJ, et al. Challenges in translating PrEP interest into uptake in an observational study of young black MSM. J Acquir Immune Defic Syndr 2017;76(3):250–258; doi: 10.1097/qai.0000000000001497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Refugio ON, Kimble MM, Silva CL, et al. Brief report: PrEPTECH: A telehealth-based initiation program for HIV pre-exposure prophylaxis in young men of color who have sex with men. A pilot study of feasibility. J Acquir Immune Defic Syndr 2019;80(1):40–45; doi: 10.1097/qai.0000000000001873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. NYC Mayor's Office of Immigrant Affairs. A demographic snapshot: NYC's Latinx immigrant population. 2021. Available from: https://www.nyc.gov/assets/immigrants/downloads/pdf/Hispanic-Immigrant-Fact-Sheet.pdf [Last accessed: April 4, 2023].
- 21. UCLA Latino Policy & Politics Institute. 15 facts about Latino well-being in New York. 2023. Available from: https://latino.ucla.edu/research/15-facts-latinos-new-york/ [Last accessed: May 1, 2023].
- 22. Poverty Tracker Research Group at Columbia University. State of Poverty and Disadvantage in New York City. Volume 3. 2020. Available from: https://static1.squarespace.com/static/610831a16c95260dbd68934a/t/6113f3b27a11e63e811521a9/1628697527573/POVERTY_TRACKER_REPORT25.pdf
- 23. New York State Department of Health. New York City Health Indicators by Race/Ethnicity, 2018–2020. Available from: https://www.health.ny.gov/statistics/community/minority/county/newyorkcity.htm [Last accessed: May 5, 2023.
- 24. U.S. Census Bureau. QuickFacts. New York City, New York. Available from: https://www.census.gov/quickfacts/newyorkcitynewyork [Last accessed: May 5, 2023].
- 25. Latino Commission on AIDS. NYC Hispanic/Latinx Health Action Agenda 2021–2025. Our Health-Our Future. 2023. Available from: https://www.latinoaids.org/publications/nyc-latino-health-action-agenda-2021-2025.pdf [Last accessed: May 5, 2023].
- 26. Greer S, Naidoo M, Hinterland K, et al. Health of Latinos in NYC. 2017:1–32. Available from: https://www.nyc.gov/assets/doh/downloads/pdf/episrv/2017-latino-health.pdf [Last accessed: October 20, 2023].
- 27. New York City Department of Health and Mental Hygiene. New York City HIV/AIDS Annual Surveillance Statatistics 2021. Available from: https://www.nyc.gov/assets/doh/downloads/pdf/ah/surveillance2021-tables-all.pdf [Last accessed: May 5, 2023].
- 28. New York City Department of Health and Mental Hygiene. New York City HIV/AIDS Annual Surveillance Statistics 2020. Available from: https://www.nyc.gov/assets/doh/downloads/pdf/ah/surveillance2020-tables-all.pdf [Last accessed: May 5/2023].
- 29. New York State Department of Health AIDS Institute. Payment options for adults and adolescents for pre-exposure prophylaxis (PrEP). Available from: https://www.health.ny.gov/diseases/aids/general/prep/docs/prep_payment_options.pdf [Last accessed: May 5, 2023].
- 30. Harkness A, Satyanarayana S, Mayo D, et al. Scaling up and out HIV prevention and behavioral health services to Latino sexual minority men in South Florida: Multi-level implementation barriers, facilitators, and strategies. AIDS Patient Care STDs 2021;35(5):167–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Watson RJ, Morgan E, Sherman J, et al. Pre-exposure prophylaxis (PrEP) use, anticipated PrEP stigma, and bisexual identity among a Black and Hispanic/Latino sexual and gender diverse sample. Behav Med 2023/07/03 2023;49(3):283–291; doi: 10.1080/08964289.2022.2048249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Robles G, Hong C, Yu M, Starks TJ. Intersecting communities and PrEP uptake among US-based Latinx sexual minority men. J Racial Ethn Health Disparities 2022;9(6):2157–2163; doi: 10.1007/s40615-021-01154-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rhodes SD, Alonzo J, Mann-Jackson L, et al. A peer navigation intervention to prevent HIV among mixed immigrant status Latinx GBMSM and transgender women in the United States: Outcomes, perspectives and implications for PrEP uptake. Health Educ Res 2020;35(3):165–178; doi: 10.1093/her/cyaa010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Shorrock F, Alvarenga A, Hailey-Fair K, et al. Dismantling barriers and transforming the future of pre-exposure prophylaxis uptake in young Black and Latinx sexual minority men and transgender women. AIDS Patient Care STDs 2022;36(5):194–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Srikanth K, Killelea A, Strumpf A, et al. Associated costs are a barrier to HIV preexposure prophylaxis access in the United States. Am J Public Health 2022;112(6):834–838; doi: 10.2105/ajph.2022.306793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Horridge DN, Oh TS, Alonzo J, et al. Barriers to HIV testing within a sample of Spanish-speaking Latinx gay, bisexual, and other men who have sex with men: Implications for HIV prevention and care. Health Behav Res 2019;2(3). [PMC free article] [PubMed] [Google Scholar]
- 37. Guilamo-Ramos V, Thimm-Kaiser M, Benzekri A, et al. The invisible US Hispanic/Latino HIV crisis: Addressing gaps in the national response. Am J Public Health 2020;110(1):27–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hsueh L, Huang J, Millman AK, et al. Disparities in use of video telemedicine among patients with limited English proficiency during the COVID-19 pandemic. JAMA Netw Open 2021;4(11):e2133129–e2133129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Price JC, Simpson DC. Telemedicine and health disparities. Clin Liver Dis (Hoboken) 2022;19(4):144–147; doi: 10.1002/cld.1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Rodriguez JA, Saadi A, Schwamm LH, et al. Disparities in telehealth use among California patients with limited English proficiency: Study examines disparities in telehealth use among California patients with limited English proficiency. Health Affairs 2021;40(3):487–495. [DOI] [PubMed] [Google Scholar]
- 41. Mayer KH, Chan PA, Petal R, et al. Evolving models and ongoing challenges for HIV preexposure prophylaxis implementation in the United States. J Acquir Immune Defic Syndr 2018;77(2):119–127; doi: 10.1097/qai.0000000000001579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Pathela P, Jamison K, Blank S, et al. The HIV pre-exposure prophylaxis (PrEP) cascade at NYC sexual health clinics: Navigation is the key to uptake. J Acquir Immune Defic Syndr 2020;83(4):357–364; doi: 10.1097/qai.0000000000002274. [DOI] [PubMed] [Google Scholar]
- 43. Goedel WC, Bessey S, Lurie MN, et al. Projecting the impact of equity-based pre-exposure prophylaxis implementation on racial disparities in HIV incidence among men who have sex with men. AIDS 2020;34(10):1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Siegler AJ, Steehler K, Sales JM, et al. A review of HIV pre-exposure prophylaxis streamlining strategies. Curr HIV/AIDS Rep 2020;17(6):643–653; doi: 10.1007/s11904-020-00528-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Wu AW, Weston CM, Ibe CA, et al. The Baltimore community-based organizations neighborhood network: Enhancing capacity together (CONNECT) cluster RCT. Am J Prev Med 2019;57(2):e31–e41; doi: 10.1016/j.amepre.2019.03.013. [DOI] [PubMed] [Google Scholar]
- 46. Centers for Disease Control and Prevention. Ending the HIV epidemic in the U.S. (EHE). Available from: https://www.cdc.gov/endhiv/index.html [Last accessed: January 7, 2023].
- 47. Fielding-Miller R, Kim S, Bowles J, et al. “We're already doing this work”: Ethical research with community-based organizations. BMC Med Res Methodol 2022;22(1):237; doi: 10.1186/s12874-022-01713-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Chasco EE, Hoth AB, Cho H, et al. Mixed-methods evaluation of the incorporation of home specimen self-collection kits for laboratory testing in a telehealth program for HIV pre-exposure prophylaxis. AIDS Behav 2021;25(8):2463–2482; doi: 10.1007/s10461-021-03209-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Calabrese SK. Interpreting gaps along the preexposure prophylaxis cascade and addressing vulnerabilities to stigma. Am J Public Health 2018;108(10):1284–1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. D'Angelo AB, Lopez-Rios J, Flynn AW, et al. Insurance-and medical provider-related barriers and facilitators to staying on PrEP: Results from a qualitative study. Transl Behav Med 2021;11(2):573–581. [DOI] [PMC free article] [PubMed] [Google Scholar]