Abstract
Background
Pregnant women who have gestational diabetes mellitus (GDM) are more prone to adverse pregnancy outcomes. We estimated the prevalence of GDM in Iran.
Methods
Web of Science, Scopus, PubMed, Google Scholar, and Persian databases (SID, Magiran, Irandoc, and) were searched using the MeSH and non-MeSH terms in abstract, title, or keywords of articles until June 2021, with no limitation in time. Random effects models were applied to summarize the GDM prevalence in Iran. The obtained data were quantitatively analyzed to determine an effect size for each paper. The pooled effect size was introduced as prevalence and 95% confidence interval. Sensitivity analyses and subgroup analyses were done to determine heterogeneity. Publication bias was assessed by the classic fail-safe N and Egger test.
Results
A total of 53 papers were considered for meta‐analysis, involving 56,521 Iranians. The total GDM prevalence in Iran was 7.6% (95% CI, 6.1%–9.4%).
Conclusion
This meta-analysis was the newest to estimate the GDM prevalence among Iranian women. Our results suggest a high prevalence of GDM in Iran, showing that Iran might have many GDM patients.
Keywords: Prevalence, Gestational Diabetes Mellitus, Iran
↑What is “already known” in this topic:
Gestational diabetes depends on age, race, body composition, ethnicity, and screening and diagnostic criteria. The prevalence of gestational diabetes mellitus (GDM) varies from 5% to 25.5% worldwide, and approximately 90% of cases of GDM occur during pregnancy.
→What this article adds:
The total prevalence of GDM in Iran was 7.6% (95% CI, 6.1%–9.4%). Considering the imposition of high costs on the health system, increasing prevalence, and adverse outcomes on mothers and infants, one of the most important research aims is to achieve a cost-effective approach according to the characteristics of different cities for training, measuring, preventing, and controlling GDM in Iran.
Introduction
Diabetes is defined as high blood glucose levels caused by a lack of insulin secretion or by biological dysfunction (1). The World Health Organization (WHO) introduces GDM as "any level of early or early diagnosis of glucose intolerance in pregnancy" (2). Diabetes has become the third "silent killer" in the world after cancer and cardiovascular disease due to the increase in disease and mortality among the human race. The increasing prevalence of type 2 diabetes is significantly elevated in adults, particularly in women diagnosed during childbirth (3). GDM depends on age, race, body composition, ethnicity, and screening and diagnostic criteria. The prevalence of gestational diabetes varies from 5% to 25.5% worldwide, and in the United States, it affects 1 in 10 pregnant women, and approximately 90% of cases of gestational diabetes occur during pregnancy (4). However, the prevalence of GDM is higher in Asian women compared with American women. In Europe, the prevalence of GDM varies and in some populations, more than 20% of pregnancies are recorded (5). The GDM prevalence reached 14% of pregnancies among American women (6). The International Diabetes Federation reported in 2014 that the global prevalence of GDM varied between 1% and 14% (7). Diabetes during pregnancy affects both the mothers’ health and the fetus’ growth (8). One of the main causes of premature birth or even infant mortality is gestational diabetes. Diabetic mothers are more prone to miscarriage (9).
As a result of economic development and improvement of living standards, along with more attention to GDM screening, an increase in the incidence of GDM has been observed. Iran has a high prevalence of diabetes and the increasing GDM prevalence in Iran is also worrying. Therefore, a meta-analysis is needed to quantitatively aggregate the results of relevant studies. Therefore, we conducted a systematic review and meta-analysis of studies on the prevalence of GDM in Iran.
Methods
Study Protocol
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement (10) was applied.The study protocol was registered at the international prospective register of systematic reviews database (PROSPERO) ( https://www.crd.york.ac.uk/prospero; CRD42021259379) on June 2021.
Search strategy
Using a systematic search, studies on the prevalence of gestational diabetes in Iran were found. We searched the Web of Science, Scopus, PubMed, Google Scholar, and Persian databases (Magiran, SID, IranDo) using the MeSH and non-MeSH terms in the abstract, title, or keywords of articles until December 2022, with no time limitation. The search strategy was (Prevalence OR Incidence) AND (“Diabetes, Gestational” OR “Diabetes, Pregnancy-Induced” OR “Diabetes, Pregnancy Induced” OR “Pregnancy-Induced Diabetes” OR “Gestational Diabetes” OR “Gestational Diabetes” OR “Diabetes Mellitus, Gestational” OR “Gestational Diabetes Mellitus” OR “GDM”) AND (Iran (with no limitation in time.
Eligibility Criteria
Original English and Persian papers investigating the prevalence of gestational diabetes in Iran were included. Studies with incomplete or non-extractable data were excluded.
Study Selection
Two authors (S.Z.D. and S.S.) reviewed the retrieved papers for exclusion and inclusion criteria and discrepancies were discussed and resolved by a third author (S.R.Kh.). Also, the references of the obtained studies and related review articles were manually reviewed for possible missing articles in the electronic search.
Qualitative Study
The Newcastle–Ottawa quality assessment scale was applied to score the included studies. It addresses 3 major study designs in analytical epidemiology, namely, case-control, cohort, and cross-sectional studies.
Data Extraction
The authors’ name, publication year, name of the journal, country of origin, duration of data collection, GMD prevalence, 95% CI, and sample size were extracted from the studies.
Statistical Analysis
Data analysis was done using comprehensive meta-analysis software (CMA; Version 3.3.070) to determine the effect size. The pooled effect size was introduced as prevalence and 95% confidence interval by the random effects model. There was significant heterogeneity between studies evidenced by the P value of the Q-statistic ˂ 0.10 and the I2 statistic of ˃ 50% (11, 12). Thus, meta-regressions and subgroup analyses were applied to determine the possible sources of heterogeneity. The tau-squared (Tau2) statistic was used to assess the between-study variance ( 13). Also, a sensitivity analysis was performed through the removal of studies one by one and assessing the P value of the pooled effect (leave-one-out sensitivity analysis). The Egger and Begg tests investigated publication bias. P ˂ 0.05 was considered significant.
Results
Description of the Included Studies
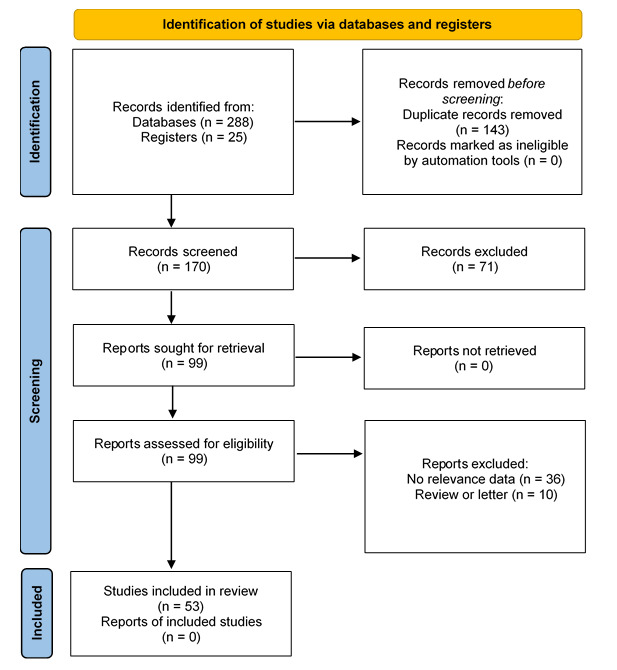
Figure 1 shows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2020 flow diagram of the process of study selection. We retrieved 313 original journal articles (199 from Scopus, 30 from PubMed, 6 from Web of Science, 53 from Persian databases, and 25 in the references of related articles), of which 53 articles had the inclusion criteria for the qualitative assessment (14-65). The quality score of the studies ranged from 8 to 10 according to the Newcastle–Ottawa quality assessment scale. Hence, all 53 articles were considered for the quantitative meta-analysis.
Figure 1.
Flow and Characteristics of the Included Studies
The characteristics of the 53 articles included in the meta-analysis with a total sample size of 56,521 are summarized in Table 1. All of the papers reported the prevalence of GDM in Iran. The articles were published between 1999 and 2021. According to geographical locations, 16 studies were performed in Tehran, (16, 17, 19, 24-27, 33, 34, 41, 45, 46, 48, 57, 62, 66), 4 in Isfahan, (30, 35 , 59, 67), 4 in Mazandaran, (15, 21, 28, 38), 3 in Kermanshah, (36, 50, 51), 4 in Yazd, (58, 60, 61, 65), 3 in Hamadan, (20, 23 , 63), 2 in Khuzestan, (54, 55), 2 in Kerman, (47, 53), 2 in Urmia, (29, 42), 2 in Fars, (14, 64); and 1 study was conducted in each of the following cities and provinces: Ardabil, Hormozgan, South Khorasan, Bushehr, Golestan, Ilam, Alborz, Lorestan, Semnan, Sistan and Baluchestan and Zanjan (22, 31, 32, 37, 39, 43, 44, 49, 52, 56, 68). All the studies have reported the prevalence of gestational diabetes (Figure 2).
Table 1. Characteristics of the studied papers in the meta-analysis.
| First Author | Year | Sample size | Place | Study Design | Prevalence | Newcastle - Ottawa Quality Assessment Scale |
|---|---|---|---|---|---|---|
| Manafi, M (42) | 2013 | 84 | Urmia | Cross-Sectional | 0.119 | 9 |
| Khodaei, S (52) | 2003 | 102 | Khorramabad | Cross-Sectional | 0.0686 | 9 |
| Nazari Robati, F (47) | 2017 | 160 | Shahdad-Kerman | Cross-Sectional | 0.125 | 9 |
| Kashi. Z (38) | 2007 | 200 | Sari | Cross-Sectional | 0.103 | 10 |
| Ekhtiari, A (24) | 2016 | 271 | Tehran | Cross-Sectional | 0.24 | 9 |
| Shafi poor, M (53) | 2013 | 290 | Rafsanjan | Cross-Sectional | 0.093 | 10 |
| Ghasemi-kakalar, S (29) | 2018 | 301 | Urmia | Cross-Sectional | 0.1628 | 9 |
| Shahdadi, H (56) | 2016 | 363 | Zabol | Cross-Sectional | 0.047 | 9 |
| Etminan-Bakhsh, M (25) | 2020 | 400 | Tehran | Cross-Sectional | 0.115 | 9 |
| Vakili, M (61) | 2014 | 400 | Yazd | Cross-Sectional | 0.12 | 10 |
| Asnafi, N (15) | 2006 | 401 | Babol | Cross-Sectional | 0.047 | 9 |
| Abolfazl, M (14) | 2008 | 420 | Shiraz | Cohort | 0.167 | 9 |
| Kamali, S (37) | 2003 | 450 | Zanjan | Cohort | 0.029 | 9 |
| Dorostkar, H (23) | 2015 | 493 | Razan | Cross-Sectional | 0.122 | 10 |
| Jalilian, N (36) | 2010 | 504 | Kermanshah | Cross-Sectional | 0.007 | 9 |
| Borzouei, S (20) | 2018 | 534 | Hamadan | Cross-Sectional | 0.395 | 9 |
| Rahimi, G (49) | 2004 | 601 | Ardebil | Cross-Sectional | 0.013 | 9 |
| Bojnordi, S (19) | 2021 | 613 | Tehran | Case-Control | 0.23 | 8 |
| Zangeneh, M (63) | 2018 | 620 | Hamadan | Cross-Sectional | 0.086 | 9 |
| Ghadiri, M (28) | 2018 | 627 | Sari | Cross-Sectional | 0.042 | 9 |
| MirFeizi, m (43) | 2008 | 668 | Karaj | Cross – Sectional | 0.186 | 9 |
| Shahbazian,BH (55) | 2012 | 678 | Ahvaz | Cross – Sectional | 0.074 | 9 |
| Dolatian, M (22) | 2020 | 734 | Ilam | Cross-Sectional | 0.098 | 9 |
| Shahbazian,H (54) | 2016 | 750 | Ahvaz | Cohort | 0.299 | 9 |
| Hadaegh, F (31) | 2004 | 800 | Bandar Abbas | Cross-Sectional | 0.063 | 9 |
| Navayi, L (46) | 2002 | 820 | Tehran | Cross-Sectional | 0.023 | 9 |
| Karimi, F (68) | 2003 | 910 | Bushehr | Cohort | 0.0175 | 9 |
| Babaniamansour S (17) | 2021 | 925 | Tehran | Cross-Sectional | 0.127 | 10 |
| Shirazian, N (57) | 2009 | 971 | Tehran | Cohort | 0.074 | 9 |
| Hedayati, H (32) | 2012 | 980 | Birjand | Cross-Sectional | 0.051 | 9 |
| Hosseini, E (72) | 2018 | 1000 | Isfahan | Cohort | 0.093 | 9 |
| Hosseini, E. (67) | 2018 | 1000 | Isfahan | Prospective Cohort | 0.1 | 9 |
| Bouzari, Z (21) | 2013 | 1004 | Babol | Cross-Sectional | 0.0805 | 9 |
| Soheilukhah, S (58) | 2010 | 1071 | Yazd | Cohort | 0.102 | 9 |
| Tabatabaei, A (59) | 2007 | 1112 | Isfahan | Cross – Sectional | 0.0676 | 9 |
| Niroomand, M (48) | 2019 | 1117 | Tehran | Cross-Sectional | 0.156 | 9 |
| Garshaspi, E (27) | 2004 | 1200 | Tehran | Cross-Sectional | 0.069 | 9 |
| Vakili, M (60) | 2016 | 1209 | Meibod-Yazd | Cross-Sectional | 0.271 | 9 |
| Rahimi, M (50) | 2017 | 1272 | Kermanshah | Cross-Sectional | 0.0881 | 9 |
| Mohammadzadeh,F (44) | 2015 | 1276 | Gorgan | Cross-Sectional | 0.049 | 9 |
| Keshavarz, M (39) | 2003 | 1310 | Shahrood | Cross-Sectional | 0.048 | 10 |
| Rahimi, M (51) | 2010 | 1720 | Kermanshah | Cross-Sectional | 0.0343 | 9 |
| Garshasbi, A (26) | 2008 | 1804 | Tehran | Cohort | 0.068 | 9 |
| Zahedi, M (62) | 2020 | 1894 | Tehran | Cohort | 0.183 | 9 |
| Goli, M (30) | 2013 | 2014 | Isfahan | Cross-Sectional | 0.038 | 9 |
| Momenzadeh, F (45) | 2015 | 2033 | Tehran | Cross Sectional | 0.068 | 10 |
| Larijani, B (66) | 1999 | 2100 | Tehran | Cross-Sectional | 0.045 | 9 |
| Atashzadeh, F (16) | 2006 | 2221 | Tehran | Cross – Sectional | 0.048 | 9 |
| Hossein-Nezhad, A (34) | 2007 | 2416 | Tehran | Cross-Sectional | 0.047 | 9 |
| Larijani, B (41) | 2002 | 2416 | Tehran | Cross-Sectional | 0.0223 | 10 |
| Hematyar, M (33) | 2008 | 5107 | Tehran | Cross-Sectional | 0.033 | 9 |
| Rashidi, H (65) | 2021 | 3202 | Yazd | Cross-Sectional | 0.033 | 9 |
| Rezaee, E (64) | 2021 | 953 | Gerash | Cross-Sectional | 0.04 | 9 |
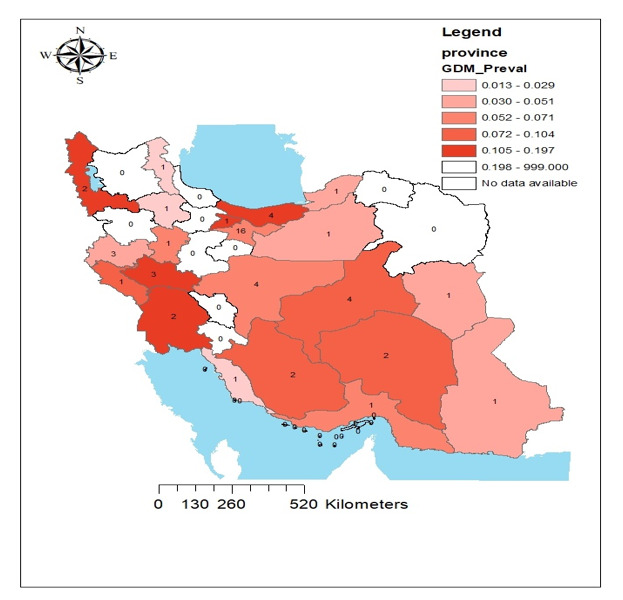
Figure 2.
Prevalence of gestational diabetes mellitus in Iran by province. The numbers on the map indicate the number of studies conducted in each province.
Findings of Individual Studies
The highest prevalence (39.5) was declared from Hamadan in 2018 (20). The lowest prevalence (0.7) was declared from Kermanshah in 2010 (36).
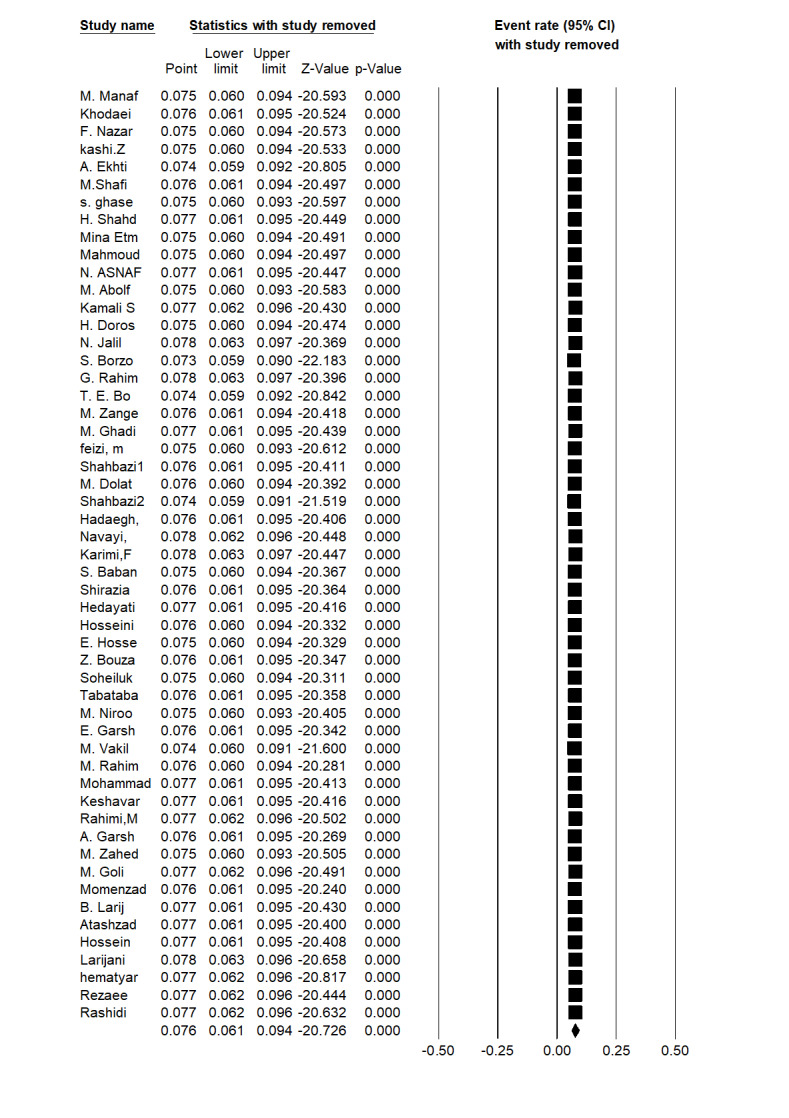
The forest plot summarizing the pooled prevalence is depicted in Figure 3. Using a random effects model, 53 studies were included in the meta‐analysis, including 56,521 Iranian participants. The total prevalence of GDM in Iran was 7.6% (95% CI 6.1%–9.4%). This pooled effect was robust in the leave-one-out sensitivity analysis (Figure 4). However, a significant between-study heterogeneity was found (Q-statistic P < 0.001; I2 = 98.08%).
Figure 3.
Forest plot of the random‑effect meta‑analysis for the prevalence of gestational diabetes in Iran
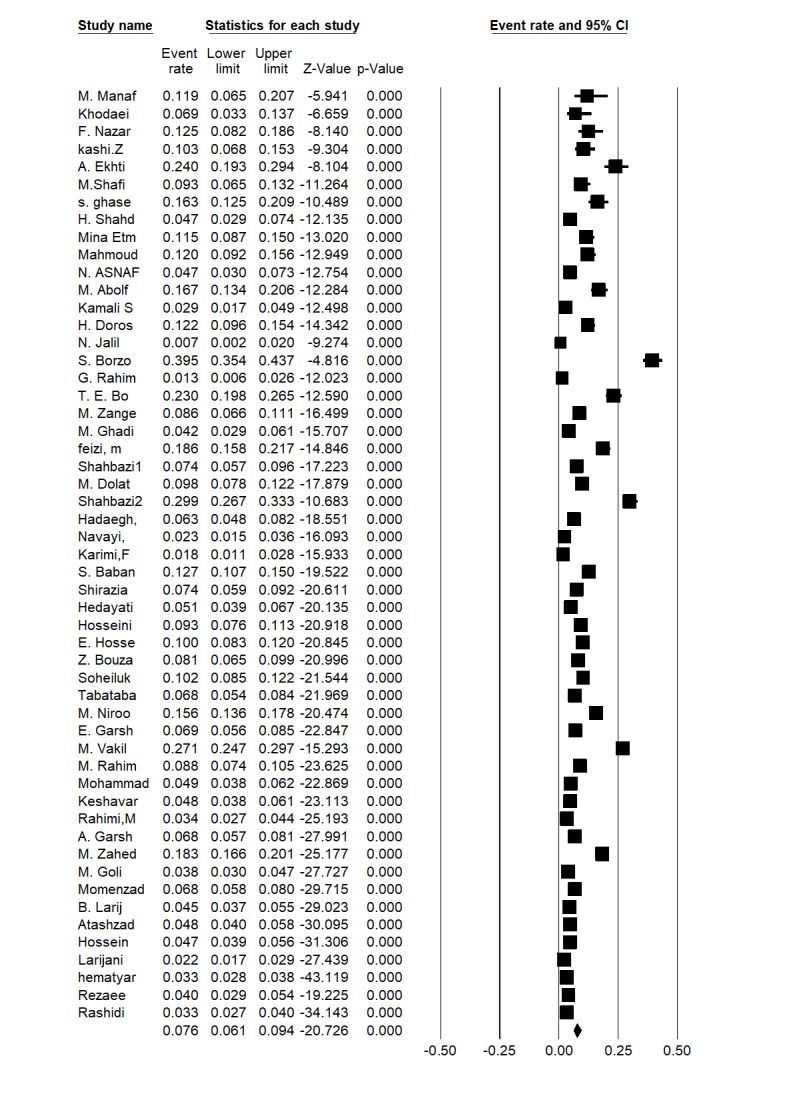
Figure 4.
The results of the leave-one-out sensitivity analysis
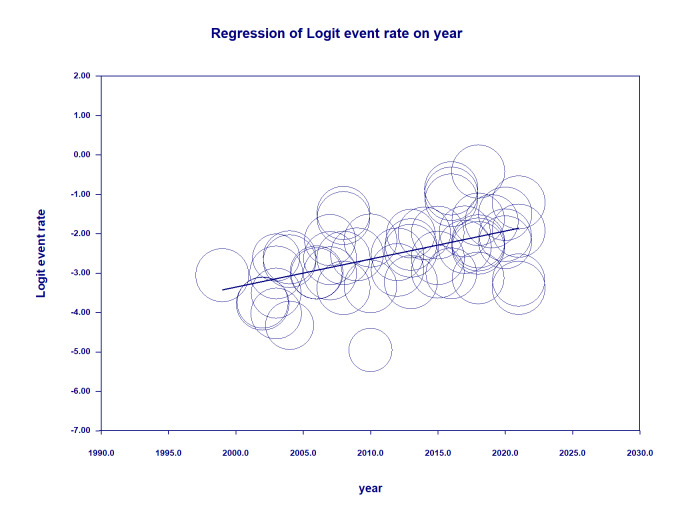
Meta-regression analysis was done to evaluate the association between the prevalence of GDM in Iran and the publication year of the study. The results suggested that the prevalence of GDM in Iran increased over time (Figure 5 ).
Figure 5.
Meta-regression between publication year of studies and GDM prevalence in Iran
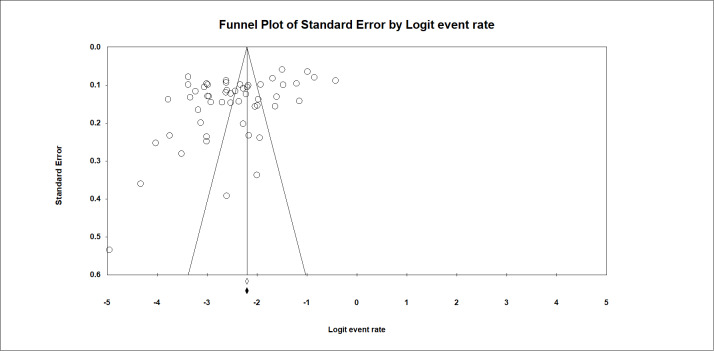
The funnel plot in Figure 6 shows no significant publication bias considering Egger linear regression (intercept = –7.93; S.E. = 2.48; 95% CI: –12.91 to –2.95; t = 3.20; df = 51; 2-tailed P = 0.002) and Begg rank correlation (Kendall’s Tau with continuity correction = –0.13; z = 1.34; 2-tailed P = 0.18). Duval and Tweedie “trim-and-fill” correction caused the imputation of 1 potentially missing study as well as an adjusted effect size of 0.099 (95% CI: 0.096–0.102). According to the “fail-safe N” test, 8386 studies were needed to turn the effect size into a nonsignificant value.
Figure 6.
The funnel plot of the meta-analysis
Discussion
Diabetes is a major threat to health. The WHO reported diabetes as the eighth cause of death in 2016, which will be the fourth cause in 2030 (18). We tried to determine the GDM prevalence in Iran. A total of 53 studies performed on 56,521 women between 1999 and 2021 entered the final stage. The GDM prevalence in Iran was 7.6%, which is lower than previous reviews (11.5%) in Asia (69) and Eastern Mediterranean (12.9%) (70), which can be attributed to the similarity in sociodemographic features of some of the studied countries. In this study, Kermanshah showed a lower prevalence (0.7%) of GMD. (36) Also, the prevalence of GDM was higher in Hamadan (39.5%) (20). This could be due to the time of the study, as well as various diagnostic criteria of GDM. The fact that more women of reproductive age are obese and overweight results in the increasing prevalence of GDM. Other factors causing this difference are the ethnic and racial variation in the population of different cities, as the prevalence of GDM in the Asian race was more than in European Whites and African Americans of the same age (71). We faced a limitation because we analyzed data on the crude prevalence without considering the effect of confounders, like social, demographic, and geographical factors. This was because various studies have used different confounding factors and similarity in this regard is scarce.
Conclusion
Despite the high diversity of methods, our results indicated a high GDM prevalence in Ahvaz, which indicates more interest of policymakers in timely screening and appropriate management of the disease. Concerning increasing the prevalence and adverse outcomes on mothers and infants, and imposition of high costs on the health system, one of the most important research points is to achieve a cost-effective approach according to characteristics of different cities of Iran to train, prevent, measure, and control GDM in Iran. Policymakers should take measures to raise the awareness of pregnant women and families about the warning signs of GDM.
Conflict of Interests
The authors decle that they have no competing interests.
Acknowledgment
The authors gratefully acknowledge the Health Sciences Research Center of Torbat Heydariyeh University of Medical Sciences for its valuable cooperation and coordination.
Cite this article as : Sadeghi S, Khatibi SR, Mahdizadeh M, Peyman N, Zare Dorniani S. Prevalence of Gestational Diabetes in Iran: A Systematic Review and Meta-analysis. Med J Islam Repub Iran. 2023 (24 Jul);37:83. https://doi.org/10.47176/mjiri.37.83
References
- 1.Choudhury AA, Devi Rajeswari. Gestational diabetes mellitus - A metabolic and reproductive disorder. Biomed Pharmacother. 2021;143:112183. doi: 10.1016/j.biopha.2021.112183. [DOI] [PubMed] [Google Scholar]
- 2.Macaulay S, Dunger DB, Norris SA. Gestational diabetes mellitus in Africa: a systematic review. PLoS One. 2014;9(6):e97871. doi: 10.1371/journal.pone.0097871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Knox CA, Delaney JA, Winterstein AG. Anti-diabetic drug utilization of pregnant diabetic women in us managed care. BMC Pregnancy Childbirth. 2014;14:28. doi: 10.1186/1471-2393-14-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim HY, Kim J, Noh E, Ahn KH, Cho GJ, Hong SC. et al. Prepregnancy hemoglobin levels and gestational diabetes mellitus in pregnancy. Diabetes Res Clin Pract. 2021;171:108608. doi: 10.1016/j.diabres.2020.108608. [DOI] [PubMed] [Google Scholar]
- 5.Egan AM, Vellinga A, Harreiter J, Simmons D, Desoye G, Corcoy R. et al. Epidemiology of gestational diabetes mellitus according to IADPSG/WHO 2013 criteria among obese pregnant women in Europe. Diabetologia. 2017;60(10):1913. doi: 10.1007/s00125-017-4353-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tobias DK, Zhang C, Chavarro J, Olsen S, Bao W, Bjerregaard AA. et al. Healthful dietary patterns and long-term weight change among women with a history of gestational diabetes mellitus. Int J Obes (Lond) 2016;40(11):1748. doi: 10.1038/ijo.2016.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Qiu H, Yu HY, Wang LY, Yao Q, Wu SN, Yin C. et al. Electronic Health Record Driven Prediction for Gestational Diabetes Mellitus in Early Pregnancy. Sci Rep. 2017;7(1):16417. doi: 10.1038/s41598-017-16665-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shen Z, Yang C, Zhu P, Tian C, Liang A. Protective effects of syringin against oxidative stress and inflammation in diabetic pregnant rats via TLR4/MyD88/NF-κB signaling pathway. Biomed Pharmacother. 2020;131:110681. doi: 10.1016/j.biopha.2020.110681. [DOI] [PubMed] [Google Scholar]
- 9.Bequer L, Gómez T, Molina JL, Álvarez A, Chaviano C, Clapés S. Experimental diabetes impairs maternal reproductive performance in pregnant Wistar rats and their offspring. Syst Biol Reprod Med. 2018;64(1):60–70. doi: 10.1080/19396368.2017.1395928. [DOI] [PubMed] [Google Scholar]
- 10.Parums DV. review articles, systematic reviews, meta-analyses, and the updated preferred reporting items for systematic reviews and meta-analyses (PRISMA) 2020 guidelines. Med Sci Monit. 2021;27:e934475. doi: 10.12659/MSM.934475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ghorbani M, Najafi Saleh, Barjasteh-Askari F, Nasseri S, Davoudi M. The effect of gas versus charcoal open flames on the induction of polycyclic aromatic hydrocarbons in cooked meat: a systematic review and meta-analysis. J Environ Health Sci. 2020;18(1):345. doi: 10.1007/s40201-020-00457-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dianatinasab M, Joulaei H, Ghorbani M, Zarei N, Rezaeian S, Fararouei M. et al. Prevalence of Tuberculosis in HIV-positive Prisoners: A Systematic Review and Meta-analysis. AIDS Rev. 2018;20(2):114. doi: 10.24875/AIDSRev.M18000023. [DOI] [PubMed] [Google Scholar]
- 13.Rezaianzadeh A, Ghorbani M, Rezaeian S, Kassani A. Red meat consumption and breast cancer risk in premenopausal women: A systematic review and meta-analysis. Middle East J Cancer. 2018;9(1):5–12. [Google Scholar]
- 14.Abolfazl M, Hamidreza TS, Narges M, Maryam Y. Gestational diabetes and its association with unpleasant outcomes of pregnancy. Pakistan J Med. 2008;24(4):566. [Google Scholar]
- 15.Asnafi N, Taheri B. Incidence of Gestational Diabetes Mellitus in Babol (North of Iran) (2002-03) J Gorgan Univ Med Sci. 2006;8 [Google Scholar]
- 16.Atashzadeh Shorideh. Frequency of gestational diabetes and its related factors in pregnant women attended to Tehran University of Medical Sciences obstetrics and gynecology clinics 2000-2001. J Rafsanjan Univ Med Sci. 2006;5(3):175. [Google Scholar]
- 17.Babaniamansour S, Aliniagerdroudbari E, Afrakhteh M, Hosseinpanah F, Farzaneh F, Niroomand M. Can fasting plasma glucose replace oral glucose-tolerance test for diagnosis of gestational diabetes mellitus. Diabetol Int. 2021;12(3):277. doi: 10.1007/s13340-020-00484-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Badakhsh M, Daneshi F, Abavisani M, Rafiemanesh H, Bouya S, Sheyback M. et al. Prevalence of gestational diabetes mellitus in Eastern Mediterranean region: a systematic review and meta-analysis. Endocrine. 2019;65(3):505. doi: 10.1007/s12020-019-02026-4. [DOI] [PubMed] [Google Scholar]
- 19.Bojnordi TE, Hantoushzadeh S, Sabzevary M, Heidari Z. A case-control study to predict the risk of gestational diabetes mellitus by initial fasting blood sugar or past gestational history. Int J Reprod Biomed (Yazd) 2021;19(4):381. doi: 10.18502/ijrm.v19i4.9064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Borzouei S, Rabiei S, Esna Ashari, Zareeighane Z, Biglari M. The Relationship between Gestational Diabetes and Risk Factors in Pregnant Women in Hamadan. Pajouhan Sci J. 2018;17(1):30. [Google Scholar]
- 21.Bouzari Z, Yazdani S, Abedi Samakosh, Mohammadnetaj M, Emamimeybodi S. Prevalence of gestational diabetes and its risk factors in pregnant women referred to health centers of Babol, Iran, from September 2010 to March 2012. Iran J Obstet Gynecol Infertil. 2013;16(43):6–13. [Google Scholar]
- 22.Dolatian M, Sharifi N, Mahmoodi Z, Taheri S, Rezaei N, Rashidian T. Investigating the association of food insecurity, psychological factors, and social support with gestational diabetes in pregnant women in Ilam Province, Iran. Iran J Endocrinol Metab. 2020;22(1):52–61. [Google Scholar]
- 23.Dorostkar H, Zare NZ, Mahvar AA, Goodarzi MT. Prevalence of gestational diabetes mellitus in different age groups in Razan, Iran 2014. J Mazandaran Univ Med Sci. 2015;25(127):74–81. [Google Scholar]
- 24.Ekhtiari A, Langari H, Yarjanli M. Prevalence of gestational diabetes mellitus and fetomaternal outcomes using one step screening method. J Mazandaran Univ Med Sci. 2016;26(142):167. [Google Scholar]
- 25.Etminan-Baksh M, Tadi S, Hatami M. Prevalence of Gestational Diabetes Mellitus and Its Associated Risk Factors in Boo-Ali Hospital, Tehran. Galen Med J. 2020;9:1642. doi: 10.31661/gmj.v9i0.1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Garshasbi A, Faghihzadeh S, Naghizadeh MM, Ghavam M. Prevalence and risk factors for gestational diabetes mellitus in Tehran. J Family Reprod Health. 2008 Jun;2(2):75–80. [Google Scholar]
- 27.Garshaspi E, Khoshniat Nikoo, Abbasian M, Radjabipour B, Fallah N. The Prevalence of Gestational Diabetes: Comparison Between Carpenter–Coustan and Nddg. Iran J Endocrinol Metab. 2004;4(1):43. [Google Scholar]
- 28.Ghadiri M, Aarabi M, Alizadeorimi F, Akha O, Khani S, Bahar A. et al. Prevalence of Gestational Diabetes According to One-Step and Two-Step Screening in Sari Rural Areas, 2012-2014. J Mazandaran Univ Med Sci. 2018;28(159):46–55. [Google Scholar]
- 29.Ghasemi Kakalar, Sohrabi M, Amiri P, Mazahri M. GDM prevalence in 301 pregnant women in nikkhah cilinc_urmia. Stud Med Sci. 2018;29(9):687. [Google Scholar]
- 30.Goli M, Firouze F. Prevalence of gestational diabetes and the effectiveness of risk factors in screening it in patients referred to health centers. J Holist Nurs. 2013;24(3):56–63. [Google Scholar]
- 31.Hadaegh F, Kher Andish, Rahimi S, Touhidi M. Prevalence of gestational diabetes in pregnant women of Bandar Abbas. Iran J Endocrinol Metab. 2004;6(3):225. [Google Scholar]
- 32.Hedayati H, Khazaee T, Mogarrab M, Sharifzadeh GR. Prevalence of gestational diabetes mellitus and overt diabetes in perganant women in birjand. Mod Care J. 2012;8(4 (32)):238. [Google Scholar]
- 33.Hematyar M, Khabiri M. Prevalence of gestational diabetes and comparison of mean maternal age in healthy and gestational diabetic patients at Javaheri hospital (2003-2006) J Inflam Dis. 2008;12(1):69–73. [Google Scholar]
- 34.Hossein-Nezhad A, Maghbooli Z, Vassigh AR, Larijani B. Prevalence of gestational diabetes mellitus and pregnancy outcomes in Iranian women. Taiwan J Obstet Gynecol. 2007;46(3):236. doi: 10.1016/S1028-4559(08)60026-1. [DOI] [PubMed] [Google Scholar]
- 35.Hosseini E, Janghorbani M, Aminorroaya A. Incidence, risk factors, and pregnancy outcomes of gestational diabetes mellitus using one-step versus two-step diagnostic approaches: A population-based cohort study in Isfahan, Iran. Diabetes Res Clin Pract. 2018;140:288. doi: 10.1016/j.diabres.2018.04.014. [DOI] [PubMed] [Google Scholar]
- 36.Jalilian N, Fakheri T, Yari M, Daeechin S. Study of relative frequency of pregnancy diabetes in women referring to clinic of societal of medicine in Kermanshah. Proceedings of the 1st National Women's Health Conference; The 1st National Women's Health Conference; 2010. [Google Scholar]
- 37.Kamali S, Shahnam F, Poormemari M. Gestational diabetes mellitus diagnosed with a 75-gram oral Glucose tolerance test and adverse pregnancy outcomes. J Adv Med Biomed Res. 2003;11(43):17–25. [Google Scholar]
- 38.Kashi Z, Borzouei S, Akha O, Moslemizadeh N, Zakeri HR, Mohammad Pour. et al. Diagnostic Value of Fasting Plasma Glucose in Screening of Gestational Diabetes Mellitus. Int J Endocrinol Metab. 2007;5(1 (13)) [Google Scholar]
- 39.Keshavarz M. Prevalence of gestational diabetes mellitus in shahrud township. J Mazandaran Univ Med Sci. 2003;13(41):90. [Google Scholar]
- 40.Keshavarz M, Cheung NW, Babaee GR, Moghadam HK, Ajami ME, Shariati M. Gestational diabetes in Iran: incidence, risk factors and pregnancy outcomes. Diabetes Res Clin Pract. 2005;69(3):279. doi: 10.1016/j.diabres.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 41.Larijani B, Azizi F, Bastanhagh M, Pajouhi M, Hoseinnezadeh A. The prevalence of gestational diabetes mellitus in young women. Iran J Endocrinol Metab. 2002;4(1):23. [Google Scholar]
- 42.Manafi M, Khadem-Ansari MH. Gestational diabetes mellitus in Iranian women: A rising rate. Acta Endocrinol. 2013;9(1):71. [Google Scholar]
- 43.MirFeyzi M, Azarian A, Mirheydari M. Prevalence of gestational diabetes and its risk factors in pregnant women living in Karaj in 2008. J Diabetes Metab Disord. 2008;9(4):376. [Google Scholar]
- 44.Mohammadzadeh F, Eshghinia S, Vakili MA. The prevalence of gestational diabetes mellitus and its related risk factors in Gorgan, north of Iran. Selective or universal screening test is cost-effective? Int J Diabetes Dev Ctries. 2015;35(3):225. [Google Scholar]
- 45.Momenzadeh F, Mokhlesi S, Mohebbi S, Moghddam Banaem. Gestational diabetes and its risk factors for pregnant women in Tehran. Int J Trop Med. 2015;10:30. [Google Scholar]
- 46.Navayi L, Kimiagar M, Kheirkhahi M, Azizi F. Investigating diabetes epidemiology among pregnant women in Tehran province villages. Pajouhesh dar Pezeshki. 2002;26(3):223. [Google Scholar]
- 47.Nazari Robati, Khanjani N, Tabasi Nejad, Rezabeigi davarani, Mohseni M. The Prevalence of Gestational Diabetes and Factors Affecting it in a Health Care Center. Health_Based Res. 2017;2(4):307. [Google Scholar]
- 48.Niroomand M, Afsar J, Hosseinpanah F, Afrakhteh M, Farzaneh F, Serahati S. Comparison of the International Association of Diabetes in Pregnancy Study Group Criteria with the Old American Diabetes Association Criteria for Diagnosis of Gestational Diabetes Mellitus. Int J Endocrinol Metab. 2019;17(4):e88343. doi: 10.5812/ijem.88343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rahimi G. The Prevalence of Gestational Diabetes in Pregnant Women eferring to Ardabil Health Centers, 2003. J Ardabil Univ Med Sci. 2004;4(13) [Google Scholar]
- 50.Rahimi M, Karami Moghadam. The prevalence of gestational diabetes mellitus and its related risk factors using one-step method in Kermanshah, 2016. Iran J Obstet Gynecol Infertil. 2017;20(4):1–4. [Google Scholar]
- 51.Rahimi Mehr, Dinari Z, Najafi F. Prevalence of gestational diabetes and its risk factors in kermanshah 2009. J Kermanshah Univ Med Sci. 2010;14(3 (47)) [Google Scholar]
- 52.Sepideh K, Kaviani M, Akbari S. Evaluation of the prevalence of gestational diabetes mellitus in 24-28 weeks pregnant women in one of the private clinics in Khorram abad in 2003 . Khorram abad : Lorestan University of Medical Sciences; 2003. [MD. thesis] [Google Scholar]
- 53.Shafiepoor M, Mortazavi M, Moradi S. Comparison of the prevalence of gestati998onal diabetes based on new indicators introduced by the international groups of the Diabetes Study Association with previous criteria. I J Diabetes Metab. 2013;12(4):302. [Google Scholar]
- 54.Shahbazian H, Nouhjah S, Shahbazian N, Jahanfar S, Latifi SM, Aleali A. et al. Gestational diabetes mellitus in an Iranian pregnant population using IADPSG criteria: incidence, contributing factors and outcomes. Diabetes Metab Syndr. 2016;10(4):242. doi: 10.1016/j.dsx.2016.06.019. [DOI] [PubMed] [Google Scholar]
- 55.Shahbazian HB, Shahbazian N, Yarahmadi M, Saiedi S. Prevalence of gestational diabetes mellitus in pregnant women referring to gynecology and obstetrics clinics. Jundishapur J Microbiol. 2012;11(2 (77)):113. [Google Scholar]
- 56.Shahdadi H, Rahnama M, Absalan A, Fahimzadeh L, MohammadPourhodki R, Moghadam K. et al. Evaluation of the prevalence of gestational diabetes among pregnant women in Zabol city in 2015. J Diabetes Nurs. 2016;4(1):64–71. [Google Scholar]
- 57.Shirazian N, Emdadi R, Mahboubi M, Motevallian A, Fazel-Sarjuei Z, Sedighpour N. et al. Screening for gestational diabetes: usefulness of clinical risk factors. Arch Gynecol Obstet. 2009;280(6):933. doi: 10.1007/s00404-009-1027-y. [DOI] [PubMed] [Google Scholar]
- 58.Soheilykhah S, Mogibian M, Rahimi-Saghand S, Rashidi M, Soheilykhah S, Piroz M. Incidence of gestational diabetes mellitus in pregnant women. Iran J Reprod Med. 2010;8(1):24. [Google Scholar]
- 59.Tabatabaei A, Fallah Z, Haghighi S, Farmani M, Horri N, Eslamian Z. et al. Prevalence and Risk Factors for Gestational Diabetes Mellitus in Pregnant Women of Isfahan, Iran. Iran J Endocrinol Metab. 2007;9(3):251. [Google Scholar]
- 60.Vakili M, Modaressi M, Zhabi R, Aghakoochak A. Prevalence of gestational diabetes and its risk factors in Meibod-Yazd 2013-2014. J Community Health Res. 2016;5(4):270. [Google Scholar]
- 61.Vakili M, Rahimi Pardanjani, Alipour N, Taheri M, Baeradeh N, Hashemi A. The prevalence of gestational diabetes and associated factors in pregnant women referred to health care centers of Yazd in 2012. J Sabzevar Univ Med Sci. 2014;21(6):1214. [Google Scholar]
- 62.Zahedi M, Kazemian E, Ramezani-Tehrani F, Tohidi M, Azizi F, Khalili D. et al. Assessment of the simultaneous effect of hypothyroidism and thyroid autoimmunity with gestational diabetes on the incidence of type 2 diabetes. BMC Endocr Disord. 2020;20(1) doi: 10.1186/s12902-020-00627-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zangeneh M, Mohamadi N, Kolahi T, Roshanei G, Khodaveisi M, Shayan A. Prevalence Of Gestational Diabetes Mellitus In Perganant Women Rreferred Totheraputic And Health Centers In Hammadan Town, Iran In The 2015. Iran J Endocrinol Metab. 2018;17(3):139. [Google Scholar]
- 64.Rezaee E, Mohammadi F, Boozhmehrani MJ, Bagheri P. The Prevalence of Gestational Diabetes Mellitus in Pregnant Women Referred to Amir al-Mu'minin Hospital of Gerash City, Fars Province, Iran. Int J Med Lab. 2021;8(3):162. [Google Scholar]
- 65.Rashidi H, Rezaianzadeh A, Tabatabaee SHR, Mousavi SA. Prevalence and Risk Factors of Gestational Diabetes Mellitus in Yazd Province, Iran. J Midwifery Reprod Health. 2021;9(3):2828. [Google Scholar]
- 66.Larijani B, Azizi F, Pazhouhi M, Bastanhagh M, Marsousi V, Hossein Nezhad. et al. Prevalence of gestational diabetes in pregnant women referred to hospitals of Tehran University of Medical Sciences 1373-1372. Iran J Endocrinol Metab. 1999;1(2):125. [Google Scholar]
- 67.Hosseini E, Janghorbani M, Shahshahan Z. Comparison of risk factors and pregnancy outcomes of gestational diabetes mellitus diagnosed during early and late pregnancy. Midwifery. 2018;66:64. doi: 10.1016/j.midw.2018.07.017. [DOI] [PubMed] [Google Scholar]
- 68.Karimi F, Nabipoor I, Jaafari M, Gholazmzadehi F. Selective screening for gestational diabetes mellitus in bushehr, based on a 50-gram clucose challenge test. Iran J Endocrinol Metab. 2003;2(1):45–51. [Google Scholar]
- 69.Lee KW, Ching SM, Ramachandran V, Yee A, Hoo FK, Chia YC. et al. Prevalence and risk factors of gestational diabetes mellitus in Asia: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2018;18(1):494. doi: 10.1186/s12884-018-2131-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhu Y, Zhang C. Prevalence of Gestational Diabetes and Risk of Progression to Type 2 Diabetes: a Global Perspective. Curr Diab Rep. 2016;16(1):7. doi: 10.1007/s11892-015-0699-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Makgoba M, Savvidou MD, Steer PJ. An analysis of the interrelationship between maternal age, body mass index and racial origin in the development of gestational diabetes mellitus. BJOG. 2012;119(3):276. doi: 10.1111/j.1471-0528.2011.03156.x. [DOI] [PubMed] [Google Scholar]
- 72. Hosseini E , Janghorbani M , Aminorroaya A . Incidence, risk factors, and pregnancy outcomes of gestational diabetes mellitus using one-step versus two-step diagnostic approaches: A population-based cohort study in Isfahan, Iran . Diabetes Res Clin Pract . 2018;140:288–294. doi: 10.1016/j.diabres.2018.04.014. [DOI] [PubMed] [Google Scholar]