What you need to know.
The clinical picture is the most important factor in assessing the significance of results of blood tests assessing cobalamin (B12) status because there is no “gold standard” test to define deficiency
Neurological symptoms resulting from B12 deficiency may take several months or even years to resolve completely
Measuring serum biomarkers such as B12 or methylmalonic acid is neither helpful nor indicated in assessing or monitoring clinical improvement, neither is titration of injection frequency based on biomarker assessment
Self-administration of intramuscular B12 injections can lead to greater patient satisfaction and better health outcomes
What is vitamin B12?
Vitamin B12 (cobalamin) is a water soluble vitamin required for several physiological processes, including normal nervous system functioning, and red blood cell development and maturation. It has antioxidant effects, is a co-factor in mitochondrial energy metabolism, and contributes to DNA synthesis, the methylation cycle, and epigenetic regulation.1 2 B12 is present in foods of animal origin, such as meat, eggs, and milk, or via food fortification. Healthy adults require an average intake of 4-7 mcg daily to maintain B12 status.3 4
Indications for B12 treatment, administration routes, and preparations
Treatment with B12 may be required for a variety of reasons (table 1).
Table 1.
Main indications and administration routes for B12 treatment
| Indication | Typical administration route |
|---|---|
| Prevention of B12 deficiency caused by insufficient dietary intake of B12. This is the most prevalent cause of B12 deficiency.4-6 Dietary intake might be limited in some people with vegetarian and vegan diets (if they do not regularly consume B12 fortified foods), in people with eating disorders, and some people with alcohol use disorder4-6 | Oral supplementation |
| Symptomatic B12 deficiency caused by dietary insufficiency7-9 | Intramuscular B12 therapy is usually initiated with the aim of progressing to oral supplements once symptoms have resolved |
| Prevention of B12 deficiency caused by the use of medications that interfere with B12 absorption (eg, metformin, proton pump inhibitors, H2 receptor blockers, antacids) | Consider oral prophylactic supplementation, with the reasonable anticipation that deficiency is likely to develop with time |
| Symptomatic B12 deficiency caused by impaired B12 absorption. This may be caused by autoimmunity; ageing related reduced B12 absorption; gastric atrophy; small bowel disease; chronic pancreatitis; Helicobacter pylori or Giardia lamblia infection; previous partial gastrectomy/gastric bypass/reduction surgery/small intestinal resection | Lifelong intramuscular injections are the default therapy10-13 |
| Nitrous oxide toxicity | Intramuscular injections14 |
| Cyanide poisoning | Intravenous administration of hydroxocobalamin |
(as long as the causative factor for B12 deficiency persists, therapy should be continued)
Evidence from animal and human studies shows that B12 also has neuroprotective and anti-inflammatory properties,15 and intervention studies in humans have reported beneficial effects of better B12 status or B12 therapy in multiple sclerosis,16 Parkinson’s disease,17 myalgic encephalomyelitis,18 autism,19 and (administering very high doses of methylcobalamin) in amyotrophic lateral sclerosis.20
Subcutaneous administration is sometimes recommended when intramuscular injections are contraindicated, for instance, in people using anticoagulants. Comparative studies between intramuscular and subcutaneous administration are lacking.21
In some countries, nasal or sublingual B12 preparations are available; however, their bioavailability is low,22 and long term efficacy studies in symptomatic B12 deficiency are lacking. Several combination preparations of different B12 forms and combinations with vitamins B1 and B6 are available. Table 2 summarises some of the available preparations; however, availability varies between countries.
Table 2.
Examples of available vitamin B12 preparations
| Preparations for parenteral administration | Oral preparations (most oral preparations are labelled as food supplements and some as prescription-only medication) | Intranasal sprays | Sublingual preparations |
|---|---|---|---|
| Hydroxocobalamin Cyanocobalamin Cyanocobalamin in tannin suspension (available in a few countries) Methylcobalamin Adenosylcobalamin Combination of thiamine, pyridoxine and cyanocobalamin |
Cyanocobalamin Methylcobalamin Adenosylcobalamin Combination of methyl- and adenosylcobalamin Combination of methyl- and adenosylcobalamin with folate Combination of thiamine, pyridoxine, and cyanocobalamin Other combination preparations |
Hydroxocobalamin Cyanocobalamin Methylcobalamin |
Cyanocobalamin Combination of cyano-, adenosyl-, and methylcobalamin Combination of cyano- and methylcobalamin, or of methyl- and adenosylcobalamin |
Determining whom to treat
A deficiency of B12 may lead to a variety of symptoms. The classic presentation of symptomatic B12 deficiency occurs in Addison-Biermer’s disease, and is characterised by megaloblastic anaemia.9 This type of anaemia was the first condition to be linked to B12 deficiency, and probably because of that, many doctors have the misconception that B12 deficiency is ruled out in patients without anaemia. This, in turn, has led to delayed diagnosis, notably in people presenting solely with neurological symptoms.6 8 23 24 25 However, in many people, neurological and neuropsychological or cognitive symptoms (box 1, fig 1) are the main presenting symptoms.23 Anaemia is present in fewer than 20% of people with B12 deficiency.26 Cobalamin analogue formation maybe related to more prominent neurological manifestations.30
Box 1. Frequently reported signs and symptoms of B12 deficiency9 23 26 27 28 29 .
Brain function: “Brain fog,” memory problems, cognitive impairment, insomnia, headaches (especially migraine), behavioural changes, learning problems, nominal aphasia
Mood: Mood swings, irritability, depression, anxiety, hallucinations, delusions, psychosis
Sensory: Peripheral paraesthesia (“pins and needles”), numbness, neuropathic pains, poor balance, reduced vibration sense or proprioception (joint position sense), tinnitus, ataxia, taste impairment, sometimes myelopathy
Constitutional: Fatigue, anaemia (either macrocytic, or normocytic when also iron deficient or associated with thalassaemia minor), other cytopenia, abdominal complaints, malabsorption, failure to thrive, weight loss, diarrhoea, hyperpigmentation, glossitis, (aphthous) stomatitis, infertility, urinary tract infections
Motor: Muscle weakness, altered reflexes (increased in degeneration of the spinal cord, reduced when peripheral neuropathy dominates), spasticity, seizures, cardiomyopathy
Autonomic: Urinary and/or faecal incontinence, postural hypotension or dizziness, erectile dysfunction
Fig 1.
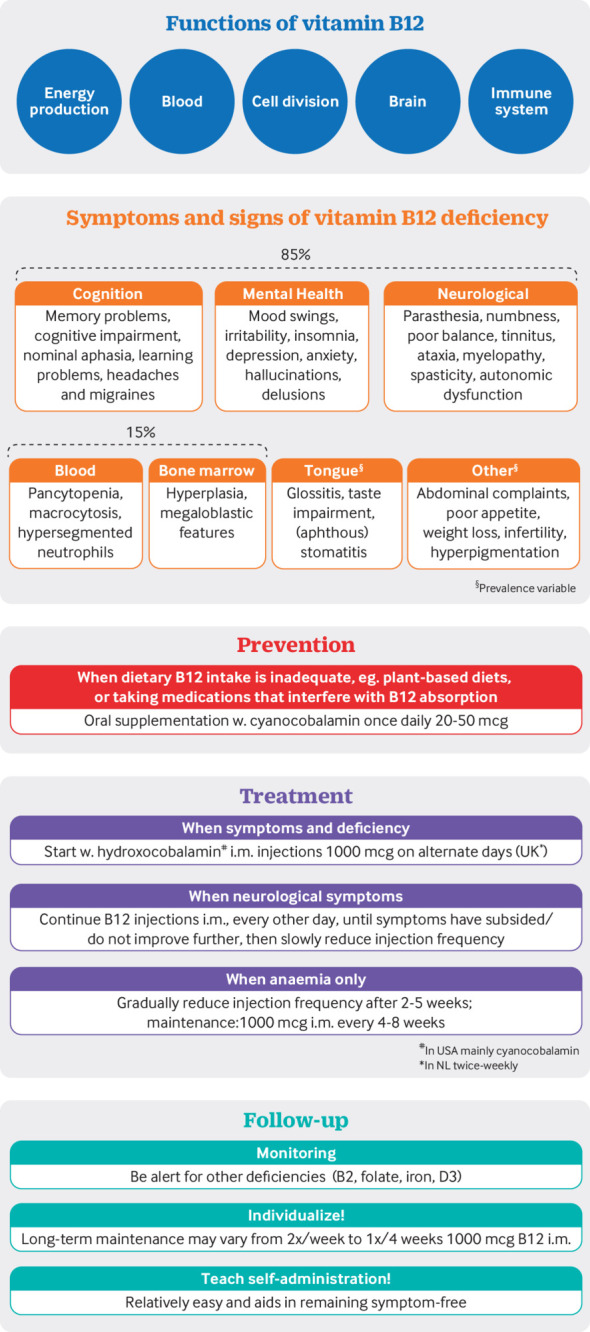
Vitamin B12: Functions, deficiency and treatment
Diagnosing B12 deficiency can be challenging because no single specific measurement exists to reliably diagnose or refute the presence of B12 deficiency11 12 26 27 (box 2). A serum B12 concentration below 148 pmol/L (depending on the assay) with symptoms (box 1) is a strong indication of deficiency and is sufficient to start treatment.11 However, symptoms may also be present in individuals with serum B12 >148 pmol/L.
Box 2. Factors influencing the accuracy of results of serum B12 and related biomarkers.
Considerable variability exists between the different commercially available serum B12 assays.31
Day-to-day variation of serum B12 may occur; for example, a concentration of 150 pmol/L on one day may be 120 pmol/L another day.
A serum B12 concentration within the normal limit, ie, above 148 pmol/L, does not exclude deficiency.
Serum B12 concentrations may be influenced by specific genetic polymorphisms or mutations; currently, more than 15 single nucleotide polymorphisms are known to influence serum B12.32 33 34 35
Oral B12 supplementation may result in serum B12 concentrations within or sometimes above the “normal” range without reducing symptoms, which can obscure the correct diagnosis.
Holo-transcobalamin (holoTC), the biologically active form of vitamin B12 in blood, also has a wide window with indeterminate levels,36 and the reference values strongly depend on the assay method.37
Measuring serum concentrations of MMA and homocysteine may be helpful in establishing B12 deficiency, especially in people with borderline serum B12 levels, ie, those between 148 and 300 pmol/L.36 38 39 However, MMA was normal in 52% of individuals with holoTC concentrations below 20 pmol/L, the latter being indicative of deficiency.40 Additionally, specific genetic polymorphisms41 and recent treatment with antibiotics may result in false normal MMA levels,42 and MMA is also elevated with impaired renal function.43
Serum homocysteine is less specific for B12 deficiency, and can also be elevated in folate deficiency, vitamin B6 deficiency, vitamin B2 deficiency, and impaired renal function, hypothyroidism, and by certain medications.44
Additionally, in patients who are already taking some form of oral B12 supplementation, demonstrating B12 deficiency can be a challenge, even when symptoms are typical (including those of neuropathy-like paraesthesia and numbness) as serum B12 concentrations may be just within, or sometimes above, the “normal” range.26 Serum B12, homocysteine, and methylmalonic acid (MMA) levels (box 2) are unreliable predictors of B12 responsive neuropathy (neurological disorders that respond to B12 supplementation).45 46 47 In these situations, expert opinion suggests that clinicians consider discussing with their patients a therapeutic trial of B12 injections.7 11 47
How is B12 deficiency treated?
The therapeutic goals of B12 treatment are the reversal of metabolic abnormalities and the prevention or reduction of clinical symptoms (fig 1). Treatment depends in part on the severity of symptoms and the cause of the deficiency. In individuals with symptomatic B12 deficiency despite normal dietary B12 intake, B12 malabsorption is the most likely cause and should guide parenteral therapy.
The three key treatment areas are outlined below.
Insufficient dietary intake
To prevent deficiency, oral cyanocobalamin supplementation once daily 20-50 mcg or 50-150 mcg is most commonly recommended.4 48 In some countries, methyl- and adenosylcobalamin-containing preparations are available; however, one observational study suggests better efficacy with cyanocobalamin than with methylcobalamin.49 Exercise caution when using combination preparations to avoid excessive folate or B6 intake. With advancing age, B12 absorption declines, and a higher supplemental B12 dose may be needed. Yearly monitoring of B12 status and suitable adjustment of the supplementation dose is recommended.50
For symptomatic deficiency (box 1) caused by insufficient dietary intake, intramuscular B12 therapy is usually initiated with the aim of progressing to oral supplements once symptoms have resolved.7 8 9
Symptomatic deficiency in people with B12 malabsorption
Suggested treatment schemes differ considerably between countries. The British National Formulary (BNF), for example, differentiates the prescription of hydroxocobalamin according to presenting symptoms, eg, “For neurological involvement, it is advised to administer hydroxocobalamin by intramuscular injection, initially 1 mg once daily on alternate days until no further improvement, then 1 mg every 2 months.” In the Netherlands, pharmacotherapeutic guidelines51 recommend (for the same neurological symptoms or abnormalities) administration of 1000 mcg once or twice weekly for up to two years. Little robust, reliable evidence supports current recommended dosing schedules, and no clinical studies assess the effectiveness and optimal dosing of intramuscular cobalamin preparations for symptom relief, other than studies assessing attained serum B12 concentrations and sometimes haematological response.52 53 54 Studies as early as the 1960s reported considerable differences between individuals in pharmacodynamics52 53 54 55 56 and dose requirements.57 Some patients may require a more frequent injection regimen, especially those with neurological symptoms, varying from twice weekly to every 2-4 weeks to become and remain asymptomatic. A possible explanation may be the large inter-individual difference in biliary B12 excretion. More than two thirds of the B12 excreted in bile is reabsorbed in the small intestine, but this reabsorption is reduced in people with pernicious anaemia or other causes of B12 malabsorption.58 59
Nitrous oxide toxicity
The Association of British Neurologists has recently issued guidance on recognising and managing nitrous oxide toxicity associated with B12 deficiency.14 It recommends rapid initiation of alternate-day intramuscular hydroxocobalamin therapy, and maintenance of this treatment until all symptoms have resolved or there is no further neurological improvement, with long term B12 therapy depending on the presence of deficiency on presentation, together with total abstinence from the use of nitrous oxide.
How well does B12 therapy work?
Treatment with B12 injections is efficacious in restoring normal metabolism, alleviating symptoms, and reversing haematological and some neurological complications of deficiency.23 Anaemia usually resolves within six to eight weeks, but coexisting iron deficiency may be present and need oral iron supplementation7 and, in severe cases, parenteral iron infusion. Neurological symptoms may take several months or even years to resolve completely. Evidence from observational studies suggests that with longer symptom duration and more profound B12 deficiency, the likelihood that neurological symptoms will not completely resolve increases.28 People often continue to experience mild neurological symptoms such as poor memory, impaired concentration, and fatigue even after “adequate” B12 replacement (eg, therapy according to the BNF suggested treatment regimen)9 17 29 and many patients report they need additional treatment. Biomarkers normalise more rapidly than an improvement or reversal of (neurological) symptoms. Additionally, symptoms may reappear without changes in biomarker status.
Some controversies exist about long-term parenteral B12 treatment. These are outlined below.
Oral versus intramuscular administration
It is suggested that passive absorption of B12 following sufficiently high oral doses (2000 mcg) can result in up to 10-12 mcg being absorbed daily7 and may allow serum B12 concentrations to normalise. However, passive absorption may be well below 1% in many patients,60 and high biliary B12 excretion may add to a negative B12 balance.59 Prospective studies on this topic have focused mainly on normalising serum B12 concentrations and should be interpreted with caution since the specific goal of treatment in symptomatic B12 deficiency is alleviating symptoms.9 23 26 A recent Cochrane Review found that available studies only provide very low quality evidence that oral B12 is as efficacious as intramuscular B12 in improving symptoms.13 A recent survey of 204 patients suggested that oral B12 was associated with less effective symptom improvement than parenteral treatment.61 In practice, some patients may be able to switch to very high dose (ie, 2000 mcg daily) oral supplementation instead of continuing parenteral administration, but it is impossible to predict in whom this can be done safely, and many are at risk of worsening symptoms which may become permanent.24
Patient experiences
Data from a review of patient experiences and surveys involving more than 2200 patients with B12 deficiency in the UK indicate that many patients have concerns related to healthcare quality, safety, and treatment,62 63 64 with nearly two thirds of respondents reporting that their treatment is insufficient to manage symptoms.24 25 Some patients may experience recurrence or worsening of symptoms when the interval between injections is extended or extended too quickly, and report that continuation of frequent intramuscular hydroxocobalamin injections, varying between twice weekly and once every three to four weeks,65 is needed to remain asymptomatic. Why certain patients require more frequent treatment is not understood.
In an online survey, almost one third of 683 participants reported cancellation of B12 injections during the covid-19 lockdowns, with subsequent worsening of symptoms and often with negative emotions and feelings including anger, fear, disappointment, feeling let down, and feeling undervalued.66 In contrast, those who were self-administering B12 injections or who were rapidly taught to do so reported a noticeable improvement in their symptoms and quality of life, with some benefiting from increasing the frequency of injections to suit their personal need.65 66
What are the harms?
Strong evidence, from decades of treating individuals with inborn errors of B12 metabolism, supports the safety of parenteral, lifelong, even high dose hydroxocobalamin, sometimes even at very high doses.67 68 Long term epidemiological studies also indicate that treatment with pharmacological B12 doses and the corresponding increase in serum B12 do not increase mortality.69 Data on the safety of cyanocobalamin, when administered with high frequency (ie, one to two times a week) for a longer period of time, are lacking.
Adverse drug reactions include skin reactions like acne or rosacea; their frequency is unknown. In our experience, some people have successfully switched to a cobalamin preparation without benzylalcohol (a preservative in some parenteral B12 preparations) and have seen their skin problems resolve. Isolated allergy cases are reported, with some successfully treated by desensitisation.70 Transient hypokalaemia during initial B12 treatment in individuals with severe anaemia is usually mild and without clinical consequences.7
Contraindications
Preparations containing benzylalcohol are contraindicated for use in children and pregnant women.71 Cyanocobalamin is associated with worsening of visual problems, and is therefore contraindicated in people with the mitochondrial disorder Leber’s hereditary optic neuropathy.72 Cyanocobalamin (but not hydroxocobalamin) is also contraindicated in renal insufficiency.73
Tips for safer prescribing
Pregnancy and breastfeeding
Continued or new B12 therapy of women with deficiency during pregnancy and lactation is mandatory and safe.74 B12 deficiency increases the risk of adverse pregnancy outcomes, including early pregnancy loss, neural tube defects, pre-eclampsia, preterm birth, and low birth weight,75 76 as well as insulin resistance and adiposity.77 It also may lead to neurological complications in newborns, such as hypotonia, failure to thrive, central apnoeas, and seizures.78 79
Children
Evidence based treatment advice on treatment in children is lacking; each case is judged individually.11 Solid evidence on the safety of parenteral, lifelong, high dose hydroxocobalamin is available from decades of treating patients with inborn errors of B12 metabolism (eg, cobalamin C deficiency).67 68
Symptom monitoring
Monitor symptoms regularly (eg, every two to three months) as they may reappear, even after several months, if injection frequency is reduced. Measuring serum biomarkers such as B12 or MMA is neither helpful nor indicated in assessing or monitoring clinical improvement.38 Base the injection frequency on symptoms, and not on biomarker assessment.
Shared decision making
Use shared decision making to establish a long term frequency of B12 injections for each patient and teach them how to self-inject.80
How cost effective is B12?
Oral cyanocobalamin is cost effective for treating diet related B12 deficiency. A hydroxocobalamin vial for parenteral administration containing 1000 mcg costs less than £1. The main costs of intramuscular B12 therapy are associated with the administration of the injection itself, when this is done by a nurse specialist or GP. Many patients have successfully learnt to self-administer B12 by intramuscular injection, which reduces both healthcare costs and burden on GP practices, and allows people who are B12 deficient to optimise their treatment regimen.65 66
Case example.
A man in his 70s presents with a nine month history of difficulty walking and climbing stairs, numbness and pain in his lower limbs, and paraesthesia in his hands. He received a diagnosis of B12 deficiency 10 years ago, and during the covid-19 pandemic he switched from intramuscular hydroxocobalamin 1000 mcg once monthly to oral B12 supplementation. At the current presentation he has serum B12 (209 pmol/L), which is within the normal range (148-600 pmol/L), however MMA is elevated at 1100 nmol/L (a measurement taken in 2017 was 117 nmol/L, normal <300 nmol/L). He had no other haematological abnormalities at initial presentation or at his current relapse. Hydroxocobalamin injections are resumed twice weekly (self-administrated) because of the severity of the neuropathy. It takes more than 12 months for his symptoms to resolve.
Tips for patients.
If you have limited dietary intake of B12 and experience symptoms listed in box 1, you might have B12 deficiency.
Consider regular oral supplementation if you have a limited dietary intake of B12 or are taking medications that interfere with B12 absorption.
Where possible, avoid suddenly reducing the B12 dose or injection frequency, as too rapid dose reduction may worsen symptoms or lead to symptom recurrence.26 Instead, gradually increase the interval between B12 injections over the course of several months while monitoring symptoms.
If you require regular intramuscular B12 injections, consider being taught how to self-administer these.
Consider creating an individualised treatment plan with the support of your doctor tailored to help you become or remain symptom-free (dose and frequency will vary between individuals from twice weekly to once every two to three months).
Education into practice.
Practice
How often do you evaluate B12 deficiency related symptoms in individuals at high risk of developing this, such as vegetarians and vegans, or people with increased risk of B12 malabsorption, such as individuals with type 1 diabetes or Hashimoto hypothyroidism?
Think about the last time you talked to a patient using intramuscular B12 therapy. Did you discuss the optimum frequency of hydroxocobalamin injections in their specific situation? And have you considered teaching the patient to self-inject? How might you alter your discussion next time?
How patients were involved in the creation of this article.
This article has been shared with Martyn Hooper, chairperson of the Pernicious Anaemia Society (PAS), for comments and feedback. Input from Martyn and other patients, some being members of the PAS, is much appreciated. They suggested recommendations for reporting specific signs and symptoms often mentioned by members/patients; however, as this is a therapeutics article, these recommendations are not included. They also reported on the barriers patients experience in healthcare (which can also be found in the scientific literature,25 66) and several additional case descriptions.
.
Search strategy.
We searched PubMed (NLM database) with the terms “B12” OR “cobalamin” AND “deficiency” OR “therapeutics” OR “supplementation” for relevant publications of clinical observations and studies published from 1950 to 2022. We prioritised systematic reviews and studies on the benefits, harms, and cost effectiveness of B12 supplementation. We also searched clinical guidelines and our personal archives of references, and screened the reference lists of studies retrieved by the searches.
Further resources.
Multiple speakers: Treating pernicious anaemia—getting it tight. Pernicious Anaemia Society 2019 Conference. https://pernicious-anaemia-society.org/conference-2019-presentations/
B12 main facts. https://www.youtube.com/watch?v=DeV2jzofjXQ
How to convert ng/L (or pg/mL) values to pmol/L vitamin B12 and vice versa:
1 ng/L is equivalent to 0.7378 pmol/L
1 pmol/L is equivalent to 1.3554 ng/L.
Advisers to this series are Robin Ferner and Patricia McGettigan.
Patient consent: The case in this article is based on a real case, and written consent has been obtained and submitted as a supplementary file.
Competing interests: The BMJ has judged that there are no disqualifying financial ties to commercial companies. The authors declare the following other interests:
Bruce H.R. Wolffenbuttel: Consultation for Novo Nordisk on GLP1 scientific data and results, and involved in a Novo Nordisk Post-marketing surveillance study on semaglutide use in type 2 diabetes.
Speaker honorarium from Springer MedNet, for a presentation on new insight into genetics and genomics in diabetes diagnosis and treatment.
Scientific adviser for a healthcare start-up, Nuevo Care, initiating a dedicated clinic for individuals with B12 deficiency.
Scientific adviser for a digital health start-up, Ancora Health, offering preventive health programmes.
Member of the Post-Graduate Education Committee of the European Association for the Study of Diabetes.
Coordinator/organiser for Post-Graduate Educations and Webinars, Diabetes (Alpha Omega Congress) & Endocrinology (BIG5 Endocrinology course).
Member of the editorial board of the Journal of Diabetes and Current Topics in Diabetes.
P Julian Owen: none.
Mary Ward: Principal investigator on investigating the effect of riboflavin on markers of vascular health in adults with a genetic predisposition to hypertension, supported by Dutch State Mining (DSM)—Health and Biosciences division.
We (Ulster University) have been awarded a patent for the treatment of hypertension with Riboflavin. EP2139488A1 USE OF RIBOFLAVIN IN THE TREATMENT OF HYPERTENSION; an intellectual Property License Agreement was signed with DSM, which provides exclusive use of pharmaceutical claims under patent rights in China, Mexico, Japan, Canada, and Europe.
Ralph Green: none.
Contributorship statement and guarantor: Planning of the manuscript: BHRW, PJO, MW, RG. Discussions on manuscript contents: all authors. Writing the first draft: BHRW. Editing for important content and approval of the final manuscript: all authors. Guarantor of the paper: all authors.
Provenance and peer review: commissioned; externally peer reviewed.
This is one of a series of occasional articles on therapeutics for common or serious conditions, covering new drugs and old drugs with important new indications or concerns. To suggest a topic, please email us at practice@bmj.com
References
- 1. Nielsen MJ, Rasmussen MR, Andersen CB, Nexø E, Moestrup SK. Vitamin B12 transport from food to the body’s cells-a sophisticated, multistep pathway. Nat Rev Gastroenterol Hepatol 2012;9:345-54. 10.1038/nrgastro.2012.76. [DOI] [PubMed] [Google Scholar]
- 2. Green R. Vitamin B12 deficiency from the perspective of a practicing hematologist Blood 2017;129:2603-11. 10.1182/blood-2016-10-569186. [DOI] [PubMed] [Google Scholar]
- 3. Bor MV, von Castel-Roberts KM, Kauwell GP, et al. Daily intake of 4 to 7 microg dietary vitamin B-12 is associated with steady concentrations of vitamin B-12-related biomarkers in a healthy young population Am J Clin Nutr 2010;91:571-7. 10.3945/ajcn.2009.28082. [DOI] [PubMed] [Google Scholar]
- 4. Niklewicz A, Smith AD, Smith A, et al. CluB-12 . The importance of vitamin B12 for individuals choosing plant-based diets Eur J Nutr 2023;62:1551-9. 10.1007/s00394-022-03025-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rizzo G, Laganà AS, Rapisarda AM, et al. Vitamin B12 among vegetarians: status, assessment and supplementation Nutrients 2016;8:767. 10.3390/nu8120767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Benham AJ, Gallegos D, Hanna KL, Hannan-Jones MT. Intake of vitamin B12 and other characteristics of women of reproductive age on a vegan diet in Australia. Public Health Nutr 2021;24:4397-407. 10.1017/S1368980021001695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Carmel R. How I treat cobalamin (vitamin B12) deficiency Blood 2008;112:2214-21. 10.1182/blood-2008-03-040253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Green R. Anemias beyond B12 and iron deficiency: the buzz about other B’s, elementary, and nonelementary problems. Hematology Am Soc Hematol Educ Program 2012;2012:492-8. 10.1182/asheducation.V2012.1.492.3800162. [DOI] [PubMed] [Google Scholar]
- 9. Green R, Allen LH, Bjørke-Monsen AL, et al. Vitamin B12 deficiency Nat Rev Dis Primers 2017;3:17040. 10.1038/nrdp.2017.40. [DOI] [PubMed] [Google Scholar]
- 10. Hillman RS. Hematopoietic agents: growth factors, minerals and vitamins. Goodman & Gilman’s The Pharmacological Basis of Therapeutics. McGraw-Hill, 1990: 1311-40. [Google Scholar]
- 11. Devalia V, Hamilton MS, Molloy AM, British Committee for Standards in Haematology . Guidelines for the diagnosis and treatment of cobalamin and folate disorders Br J Haematol 2014;166:496-513. 10.1111/bjh.12959. [DOI] [PubMed] [Google Scholar]
- 12. Sukumar N, Saravanan P. Investigating vitamin B12 deficiency BMJ 2019;365:l1865. 10.1136/bmj.l1865. [DOI] [PubMed] [Google Scholar]
- 13. Wang H, Li L, Qin LL, Song Y, Vidal-Alaball J, Liu TH. Oral vitamin B12 versus intramuscular vitamin B12 for vitamin B12 deficiency Cochrane Database Syst Rev 2018;3:CD004655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Association of British Neurologists Clinical Practice Guide. Nitrous Oxide-Induced Subacute Combined Degeneration of the Cord. https://www.theabn.org/resource/collection/6750BAE6-4CBC-4DDB-A684-116E03BFE634/N2O-SACD_Guidelines_-_ABN_-_12.02_-_1.1.11_-_AP_FINAL_FOR_RELEASE.pdf
- 15. Scalabrino G. The multi-faceted basis of vitamin B12 (cobalamin) neurotrophism in adult central nervous system: lessons learned from its deficiency Prog Neurobiol 2009;88:203-20. 10.1016/j.pneurobio.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 16. Nozari E, Ghavamzadeh S, Razazian N. The effect of vitamin B12 and folic acid supplementation on serum homocysteine, anemia status and quality of life of patients with multiple sclerosis Clin Nutr Res 2019;8:36-45. 10.7762/cnr.2019.8.1.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. McCaddon A. Vitamin B12 in neurology and ageing; clinical and genetic aspects. Biochimie 2013;95:1066-76. 10.1016/j.biochi.2012.11.017. [DOI] [PubMed] [Google Scholar]
- 18. Regland B, Forsmark S, Halaouate L, et al. Response to vitamin B12 and folic acid in myalgic encephalomyelitis and fibromyalgia. PLoS One 2015;10:e0124648. 10.1371/journal.pone.0124648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hendren RL, James SJ, Widjaja F, Lawton B, Rosenblatt A, Bent S. Randomized, placebo-controlled trial of methyl B12 for children with autism J Child Adolesc Psychopharmacol 2016;26:774-83. 10.1089/cap.2015.0159. [DOI] [PubMed] [Google Scholar]
- 20. Oki R, Izumi Y, Fujita K, et al. Japan Early-Stage Trial of Ultrahigh-Dose Methylcobalamin for ALS (JETALS) Collaborators . Efficacy and safety of ultrahigh-dose methylcobalamin in early-stage amyotrophic lateral sclerosis: a randomized clinical trial. JAMA Neurol 2022;79:575-83. 10.1001/jamaneurol.2022.0901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Elangovan R, Baruteau J. Inherited and acquired vitamin B12 deficiencies: Which administration route to choose for supplementation? Front Pharmacol 2022;13:972468. 10.3389/fphar.2022.972468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tillemans MP, Donders EM, Verweij SL, Van der Hoeven RT, Kalisvaart KJ. Effect of administration route on the pharmacokinetics of cobalamin in elderly patients: a randomized controlled trial Curr Ther Res Clin Exp 2014;76:21-5. 10.1016/j.curtheres.2014.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lindenbaum J, Healton EB, Savage DG, et al. Neuropsychiatric disorders caused by cobalamin deficiency in the absence of anemia or macrocytosis N Engl J Med 1988;318:1720-8. 10.1056/NEJM198806303182604. [DOI] [PubMed] [Google Scholar]
- 24. Seage CH, Glover E, Mercer J. Receiving a diagnosis of pernicious anemia: exploring experiences of relationships with health professionals. J Patient Exp 2020;7:766-70. 10.1177/2374373519883497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hooper M, Hudson P, Porter F, McCaddon A. Patient journeys: diagnosis and treatment of pernicious anaemia. Br J Nurs 2014;23:376-81. 10.12968/bjon.2014.23.7.376. [DOI] [PubMed] [Google Scholar]
- 26. Wolffenbuttel BHR, Wouters HJCM, Heiner-Fokkema MR, van der Klauw MM. The many faces of cobalamin (vitamin B12) deficiency Mayo Clin Proc Innov Qual Outcomes 2019;3:200-14. 10.1016/j.mayocpiqo.2019.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hunt A, Harrington D, Robinson S. Vitamin B12 deficiency BMJ 2014;349:g5226. 10.1136/bmj.g5226. [DOI] [PubMed] [Google Scholar]
- 28. Healton EB, Savage DG, Brust JC, Garrett TJ, Lindenbaum J. Neurologic aspects of cobalamin deficiency Medicine (Baltimore) 1991;70:229-45. 10.1097/00005792-199107000-00001. [DOI] [PubMed] [Google Scholar]
- 29. Briani C, Dalla Torre C, Citton V, et al. Cobalamin deficiency: clinical picture and radiological findings Nutrients 2013;5:4521-39. 10.3390/nu5114521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Carmel R, Karnaze DS, Weiner JM. Neurologic abnormalities in cobalamin deficiency are associated with higher cobalamin “analogue” values than are hematologic abnormalities. J Lab Clin Med 1988;111:57-62. [PubMed] [Google Scholar]
- 31. Mackenzie F, Devalia V. Laboratory performance of serum B12 assay in the United Kingdom (UK) as assessed by the UK National External Quality Assessment Scheme for Haematinics: implications for clinical interpretation. Blood 2018;132(Supplement 1):2230-30. 10.1182/blood-2018-99-110597 30463993 [DOI] [Google Scholar]
- 32. Carmel R, Parker J, Kelman Z. Genomic mutations associated with mild and severe deficiencies of transcobalamin I (haptocorrin) that cause mildly and severely low serum cobalamin levels Br J Haematol 2009;147:386-91. 10.1111/j.1365-2141.2009.07855.x. [DOI] [PubMed] [Google Scholar]
- 33. Oussalah A, Besseau C, Chery C, et al. Helicobacter pylori serologic status has no influence on the association between fucosyltransferase 2 polymorphism (FUT2 461 G->A) and vitamin B12 in Europe and West Africa Am J Clin Nutr 2012;95:514-21. 10.3945/ajcn.111.016410. [DOI] [PubMed] [Google Scholar]
- 34. Surendran S, Adaikalakoteswari A, Saravanan P, Shatwaan IA, Lovegrove JA, Vimaleswaran KS. An update on vitamin B12-related gene polymorphisms and B12 status Genes Nutr 2018;13:2. 10.1186/s12263-018-0591-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Velkova A, Diaz JEL, Pangilinan F, et al. The FUT2 secretor variant p.Trp154Ter influences serum vitamin B12 concentration via holo-haptocorrin, but not holo-transcobalamin, and is associated with haptocorrin glycosylation Hum Mol Genet 2017;26:4975-88. 10.1093/hmg/ddx369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Harrington DJ. Laboratory assessment of vitamin B12 status J Clin Pathol 2017;70:168-73. 10.1136/jclinpath-2015-203502. [DOI] [PubMed] [Google Scholar]
- 37. Nexo E, Hoffmann-Lücke E. Holotranscobalamin, a marker of vitamin B12 status: analytical aspects and clinical utility Am J Clin Nutr 2011;94:359S-65S. 10.3945/ajcn.111.013458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Solomon LR. Cobalamin-responsive disorders in the ambulatory care setting: unreliability of cobalamin, methylmalonic acid, and homocysteine testing Blood 2005;105:978-85, author reply 1137. 10.1182/blood-2004-04-1641. [DOI] [PubMed] [Google Scholar]
- 39. Spence JD. Metabolic vitamin B12 deficiency: a missed opportunity to prevent dementia and stroke Nutr Res 2016;36:109-16. 10.1016/j.nutres.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 40. Herrmann W, Obeid R. Utility and limitations of biochemical markers of vitamin B12 deficiency Eur J Clin Invest 2013;43:231-7. 10.1111/eci.12034. [DOI] [PubMed] [Google Scholar]
- 41. Molloy AM, Pangilinan F, Mills JL, et al. A common polymorphism in HIBCH influences methylmalonic acid concentrations in blood independently of cobalamin Am J Hum Genet 2016;98:869-82. 10.1016/j.ajhg.2016.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Bain MD, Jones M, Borriello SP, et al. Contribution of gut bacterial metabolism to human metabolic disease. Lancet 1988;1:1078-9. 10.1016/S0140-6736(88)91898-3. [DOI] [PubMed] [Google Scholar]
- 43. Iqbal N, Azar D, Yun YM, Ghausi O, Ix J, Fitzgerald RL. Serum methylmalonic acid and holotranscobalamin-II as markers for vitamin B12 deficiency in end-stage renal disease patients Ann Clin Lab Sci 2013;43:243-9. [PubMed] [Google Scholar]
- 44. Kim J, Kim H, Roh H, Kwon Y. Causes of hyperhomocysteinemia and its pathological significance Arch Pharm Res 2018;41:372-83. 10.1007/s12272-018-1016-4. [DOI] [PubMed] [Google Scholar]
- 45. Graber JJ, Sherman FT, Kaufmann H, Kolodny EH, Sathe S. Vitamin B12-responsive severe leukoencephalopathy and autonomic dysfunction in a patient with “normal” serum B12 levels J Neurol Neurosurg Psychiatry 2010;81:1369-71. 10.1136/jnnp.2009.178657. [DOI] [PubMed] [Google Scholar]
- 46. Julian T, Syeed R, Glascow N, Angelopoulou E, Zis P. B12 as a treatment for peripheral neuropathic pain: a systematic rdeview Nutrients 2020;12:2221. 10.3390/nu12082221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Solomon LR. Vitamin B12-responsive neuropathies: a case series Nutr Neurosci 2016;19:162-8. 10.1179/1476830515Y.0000000006. [DOI] [PubMed] [Google Scholar]
- 48.Scenario: management of anaemia - vitamin B12 and folate deficiency. https://cks.nice.org.uk/topics/anaemia-b12-folate-deficiency/management/management/
- 49. Zugravu CA, Macri A, Belc N, Bohiltea R. Efficacy of supplementation with methylcobalamin and cyancobalamin in maintaining the level of serum holotranscobalamin in a group of plant-based diet (vegan) adults Exp Ther Med 2021;22:993. 10.3892/etm.2021.10425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Porter KM, Hoey L, Hughes CF, et al. Associations of atrophic gastritis and proton-pump inhibitor drug use with vitamin B12 status, and the impact of fortified foods, in older adults. Am J Clin Nutr 2021;114:1286-94. 10.1093/ajcn/nqab193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. National Health Care Institute TNHhwfn . https://www.farmacotherapeutischkompas.nl/
- 52. Chalmers JN, Shinton NK. Comparison of hydroxocobalamin and cyanocobalamin in the treatment of pernicious anaemia. Lancet 1965;2:1305-8. 10.1016/S0140-6736(65)92336-6. [DOI] [PubMed] [Google Scholar]
- 53. Tudhope GR, Swan HT, Spray GH. Patient variation in pernicious anaemia, as shown in a clinical trial of cyanocobalamin, hydroxocobalamin and cyanocobalamin-zinc tannate. Br J Haematol 1967;13:216-28. 10.1111/j.1365-2141.1967.tb08734.x. [DOI] [PubMed] [Google Scholar]
- 54. Bastrup-Madsen P. Treatment of vitamin B12 deficiency. Evaluation of therapy with cyanocobalamin, hydroxocabalamin, and depot cobalamin Betolvex. Scand J Gastroenterol Suppl 1974;29:89-95. [PubMed] [Google Scholar]
- 55. N.N. To-day’s Drugs . To-day’s drugs. Br Med J 1963;2:225-7. 10.1136/bmj.2.5351.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Hertz H, Kristensen HP, Hoff-Jorgensen E. Studies on vitamin B12 retention. Comparison of retention following intramuscular injection of cyanocobalamin and hydroxocobalamin. Scand J Haematol 1964;1:5-15. 10.1111/j.1600-0609.1964.tb00001.x. [DOI] [PubMed] [Google Scholar]
- 57. Neumark E. International Congress of Haematology, Cambridge, 1950. Acta Haematol 1951;5:302-17. [DOI] [PubMed] [Google Scholar]
- 58. Grasbeck R, Nyberg W, Reizenstein P. Biliary and fecal vit. B12 excretion in man: an isotope study. Proc Soc Exp Biol Med 1958;97:780-4. 10.3181/00379727-97-23879. [DOI] [PubMed] [Google Scholar]
- 59. Doets EL, In’t Veld PH, Szczecinska A, et al. Systematic review on daily vitamin B12 losses and bioavailability for deriving recommendations on vitamin B12 intake with the factorial approach. Ann Nutr Metab 2013;62:311-22. [DOI] [PubMed] [Google Scholar]
- 60. Berlin H, Berlin R, Brante G. Oral treatment of pernicious anemia with high doses of vitamin B12 without intrinsic factor. Acta Med Scand 1968;184:247-58. 10.1111/j.0954-6820.1968.tb02452.x. [DOI] [PubMed] [Google Scholar]
- 61. Kornic PA, Harty MMJ, Grant JA. Influence of treatment parameters on symptom relief in individuals with vitamin B12 deficiency. Annu Res Rev Biol 2017;11:1-8 10.9734/ARRB/2016/31711 [DOI] [Google Scholar]
- 62. Tyler N, Giles S, Daker-White G, McManus BC, Panagioti M. A patient and public involvement workshop using visual art and priority setting to provide patients with a voice to describe quality and safety concerns: vitamin B12 deficiency and pernicious anaemia. Health Expect 2021;24:87-94. 10.1111/hex.13152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Tyler N, Hodkinson A, Ahlam N, Giles S, Zhou A, Panagioti M. Patient safety, self-injection, and B12 deficiency: a UK cross-sectional survey. Br J Gen Pract 2022;72:e891-8. 10.3399/BJGP.2021.0711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Cotton M, McCaddon A. Examining the diagnosis and treatment experiences of people living with autoimmune gastritis and pernicious anemia. J Patient Exp 2023;10:23743735231151767. 10.1177/23743735231151767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Warren J. Pernicious anaemia: self-administration of hydroxocobalamin in the covid-19 crisis BMJ 2020;369:m2380. 10.1136/bmj.m2380. [DOI] [PubMed] [Google Scholar]
- 66. Seage CH, Semedo L. How do patients receiving prescribed B12 injections for the treatment of PA perceive changes in treatment during the Covid-19 pandemic? A UK-based survey study. J Patient Exp 2021;8:2374373521998842. 10.1177/2374373521998842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Huemer M, Diodato D, Schwahn B, et al. Guidelines for diagnosis and management of the cobalamin-related remethylation disorders cblC, cblD, cblE, cblF, cblG, cblJ and MTHFR deficiency. J Inherit Metab Dis 2017;40:21-48. 10.1007/s10545-016-9991-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Scalais E, Osterheld E, Geron C, et al. Parenteral hydroxocobalamin dose intensification in five patients with different types of early onset intracellular cobalamin defects: clinical and biochemical responses. JIMD Rep 2019;49:70-9. 10.1002/jmd2.12055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Wolffenbuttel BHR, Heiner-Fokkema MR, Green R, Gans ROB. Relationship between serum B12 concentrations and mortality: experience in NHANES. BMC Med 2020;18:307. 10.1186/s12916-020-01771-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Caballero MR, Lukawska J, Lee TH, Dugué P. Allergy to vitamin B12: two cases of successful desensitization with cyanocobalamin. Allergy 2007;62:1341-2. 10.1111/j.1398-9995.2007.01389.x. [DOI] [PubMed] [Google Scholar]
- 71.EMA/CHMP/272866/2013 CfHMPC. Benzyl alcohol and benzoic acid group used as excipients. https://www.ema.europa.eu/en/documents/report/benzyl-alcohol-benzoic-acid-group-used-excipients-report-published-support-questions-answers-benzyl/chmp/508188/2013-t_en.pdf
- 72.ULC. MP. Prescribing information cyanocobalamin injection, USP (vitamin B12) https://pdf.hres.ca/dpd_pm/00026115.PDF
- 73. Spence JD. B vitamin therapy for homocysteine: renal function and vitamin B12 determine cardiovascular outcomes. Clin Chem Lab Med 2013;51:633-7. 10.1515/cclm-2012-0465. [DOI] [PubMed] [Google Scholar]
- 74.Hydroxocobalamin. https://cks.nice.org.uk/topics/anaemia-b12-folate-deficiency/prescribing-information/hydroxocobalamin/
- 75. Rogne T, Tielemans MJ, Chong MF, et al. Associations of maternal vitamin B12 concentration in pregnancy with the risks of preterm birth and low birth weight: a systematic review and meta-analysis of individual participant data Am J Epidemiol 2017;185:212-23. 10.1093/aje/kww212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Behere RV, Deshmukh AS, Otiv S, Gupte MD, Yajnik CS. Maternal vitamin B12 status during pregnancy and its association with outcomes of pregnancy and health of the offspring: a systematic review and implications for policy in India Front Endocrinol (Lausanne) 2021;12:619176. 10.3389/fendo.2021.619176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Yajnik CS, Deshmukh US. Maternal nutrition, intrauterine programming and consequential risks in the offspring. Rev Endocr Metab Disord 2008;9:203-11. 10.1007/s11154-008-9087-z. [DOI] [PubMed] [Google Scholar]
- 78. Aguirre JA, Donato ML, Buscio M, et al. Serious neurological compromise due to vitamin B12 deficiency in infants of vegan and vegetarian mothers. Arch Argent Pediatr 2019;117:e420-4. [DOI] [PubMed] [Google Scholar]
- 79. Cortés-Albornoz MC, García-Guáqueta DP, Velez-van-Meerbeke A, Talero-Gutiérrez C. Maternal nutrition and neurodevelopment: a scoping review. Nutrients 2021;13:3530. 10.3390/nu13103530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Carmona C, Crutwell J, Burnham M, Polak L, Guideline Committee . Shared decision-making: summary of NICE guidance BMJ 2021;373:n1430. 10.1136/bmj.n1430. [DOI] [PubMed] [Google Scholar]
- 81.Metformin and reduced vitamin B12 levels: new advice for monitoring patients at risk. https://www.gov.uk/drug-safety-update/metformin-and-reduced-vitamin-b12-levels-new-advice-for-monitoring-patients-at-risk?utm_source=e-shot&utm_medium=email&utm_campaign=DSU_June2022Main1
- 82. Staley K, Ahmadi KR, Carter K, et al. Research priorities in pernicious anaemia: James Lind Alliance Priority Setting Partnership BMJ Open 2022;12:e065166. 10.1136/bmjopen-2022-065166. [DOI] [PMC free article] [PubMed] [Google Scholar]


