Abstract
Background:
Efforts to increase opioid use disorder (OUD) treatment have focused on primary care. We assessed primary care physicians’ preparedness to identify and treat individuals with OUD and barriers to increasing buprenorphine prescribing.
Methods:
We conducted a cross-sectional survey from January–August 2020 which assessed perceptions of the opioid epidemic; comfort screening, diagnosing, and treating individuals with OUD with medications; and barriers to obtaining a buprenorphine waiver and prescribing buprenorphine in their practice. Primary care physicians were sampled from the American Medical Association Physician Master File (n = 1000) and contacted up to 3 times, twice by mail and once by e-mail.
Results:
Overall, 173 physicians (adjusted response rate 27.3 %) responded. While most were somewhat or very comfortable screening (80.7 %) and diagnosing (79.3 %) OUD, fewer (36.9 %) were somewhat or very comfortable treating OUD with medications. One third of respondents were in a practice where they or a colleague were waivered and 10.7 % of respondents had a buprenorphine waiver. The most commonly cited barriers to both obtaining a waiver and prescribing buprenorphine included lack of access to addiction, behavioral health, or psychiatric co-management, lack of experience treating OUD, preference not to be inundated with requests for buprenorphine, and the buprenorphine training requirement.
Conclusions:
While most primary care physicians reported comfort screening and diagnosing OUD, fewer were comfortable treating OUD with medications such as buprenorphine and even fewer were waivered to do so. Addressing provider self-efficacy and willingness, and identifying effective, coordinated, and comprehensive models of care may increase OUD treatment with buprenorphine.
Keywords: Opioid use disorder, Primary care, Buprenorphine, Treatment
1. Introduction
In the United States, conservative estimates indicate that at least 5–6 million people report a lifetime history of opioid use disorder (OUD) (Martins et al., 2017; Saha et al., 2016). Medications, including methadone, buprenorphine, and extended release injectable naloxone, are the most effective treatment for OUD, save lives, and reduce the social and health consequences of OUD (National Academies of Sciences, Engineering, and Medicine, 2019). However, only one-third of individuals with OUD report receiving any substance use disorder treatment in the past year (Jones and McCance-Katz, 2019a), and far fewer receive treatment with medications for OUD (Substance Abuse and Mental Health Services Administration, 2018; Giroir et al., 2020).
Since primary care physicians have a critical role in identifying and managing OUD (Saloner et al., 2018), national efforts to expand OUD treatment have focused on this group of providers’ use of buprenorphine (US Department of Health and Human Services, n.d.). Buprenorphine has several advantages that make it well-suited for use by primary care physicians: unlike methadone, buprenorphine can be prescribed in a physician’s office, and unlike naltrexone, use of buprenorphine does not require prolonged abstinence from opioids prior to treatment initiation. To prescribe buprenorphine for the treatment of OUD, physicians are required by the Drug Addiction and Treatment Act of 2000 (DATA 2000) to complete an 8 h training and receive a waiver from the Drug Enforcement Administration. Despite the advantages of OUD treatment with buprenorphine, previous research has documented gaps in capacity to prescribe buprenorphine relative to treatment need (Jones et al., 2015), low interest among primary care providers in obtaining a buprenorphine waiver (McGinty et al., 2020), and evidence that waivered physicians do not prescribe buprenorphine to as many patients as their waivers permit (Huhn and Dunn, 2017; Jones and McCance-Katz, 2019b).
As the opioid epidemic continues to worsen, scaling up use of medications for OUD treatment is a national priority. In recent years, the Federal government has increased funding for prevention, treatment, and recovery efforts, including $7.6 billion in fiscal year 2019 (Bipartisan Policy Center, 2019). Large national investments are likely to continue. The US Department of Health and Human Services recently issued practice guidelines which exempt eligible practitioners from federal certification requirements related to training, counseling, and other ancillary services that are part of the process for obtaining a waiver to treat up to 30 patients with buprenorphine (US Department of Health and Human Services, 2021). Congress could also pursue more comprehensive legislative changes to DATA 2000 to reduce or eliminate certain barriers to buprenorphine prescribing (Olsen et al., 2021; Weimer et al., 2021). Additionally, the COVID-19 pandemic, and related social distancing and stay-at-home orders, have amplified challenges for overdose prevention (Alter and Yeager, 2020; Centers for Disease Control and Prevention, 2020) and maintaining treatment services for individuals with OUD and other substance use disorders (Dunlop et al., 2020). Thus, understanding primary care physicians’ attitudes and readiness to treat OUD can help identify education and training needs to improve patient care (National Academies of Sciences, Engineering, and Medicine, 2019). We assessed primary care physicians’ preparedness to identify and treat individuals with opioid use disorder, as well as barriers to increased buprenorphine prescribing.
2. Materials and methods
2.1. Participants
We sampled 1000 primary care physicians from the American Medical Association Physician Masterfile. The Masterfile is the largest available database of practicing physicians in the U.S. and includes osteopathic and allopathic providers. We included family physicians, general practitioners, and internal medicine physicians in our sample. To ensure the survey was geographically representative of areas with varying degrees of opioid-related mortality, we stratified states into tertiles based on 2017 overdose mortality rates (Centers for Disease Control and Prevention, n.d.) (eTable 1), the most recent data available at the time of survey planning, and sampled one-third of physicians in our sample from each tertile based on the state of their practice location.
2.2. Survey design and administration
We designed a 39-question survey informed by a prior survey examining primary care physicians’ knowledge, attitudes, and beliefs about the opioid epidemic (Hwang et al., 2016, 2015; Rutkow et al., 2015). We developed additional survey items regarding identification and treatment of OUD based on our own expertise, as well as a previously published investigation (Jones and McCance-Katz, 2019b). Survey items were iteratively piloted and pretested for content and clarity with a small number of primary care physicians.
We used a modified Dillman approach to field our survey (Dillman, 1978). First, in January 2020, we mailed the survey to all 1000 sampled participants. The mailing included a cover letter describing the purpose of the study, a $2 cash incentive, a paper-based survey, and a self-addressed stamped envelope. Approximately 8 weeks later, in March 2020, we contacted non-respondents again by mailing them another copy of the survey with a self-addressed stamped envelope. Due to the COVID-19 pandemic, we contacted second-wave non-respondents for whom email addresses were available by email in June 2020 with a final invitation to participate using an adapted web-based version of the survey (Qualtrics). To encourage survey participation, we shortened the web-based questionnaire after considering item response rates on the paper survey, the variability within each item, and the centrality of the question to the main goals of the survey.
The questionnaire and survey protocol were approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board. Strict procedures were used to protect participants’ confidentiality throughout all phases of the work.
2.3. Statistical analysis
We linked survey data with demographic information from the AMA Masterfile. We considered physicians ineligible if the mailed survey was returned to the sender or the emailed survey invitation bounced back (American Association for Public Opinion Research, 2016). Among a random sample of 100 non-respondents, we conducted internet searches to confirm their physical mailing address. Those whose addresses could not be confirmed were considered noncontacts. We extrapolated the rate of noncontact to the remaining nonrespondents to determine the adjusted response rate.14
In order to help assess non-response bias, we compared characteristics of survey respondents with eligible non-respondents based on key participant characteristics available for all subjects, including age, sex, state tertile, and primary care specialty using t-tests for continuous and chi-square tests for categorical variables.
We used descriptive statistics to examine the distribution of each variable and bivariate analyses to examine the distribution of key items across state tertiles of overdose deaths. We focused on respondents’ perceptions of the magnitude of the opioid epidemic, as well as their comfort and self-reported experiences identifying and treating individuals with OUD. In the subset of respondents who had treated at least one patient with OUD in the past year, we examined their comfort level identifying and treating individuals with OUD.
3. Results
3.1. Participant characteristics
Of the 1000 physicians sampled, 167 mailed surveys were returned to sender and 12 emailed invitations bounced back (eFig. 1). After removal of these individuals from the denominator, the crude response rate was 21.1 % (173/821). We were unable to confirm the physical mailing addresses for 29 of 100 randomly selected non-respondents. Extrapolating this rate of noncontact to remaining non-respondents, 188 additional individuals were removed from the denominator, resulting in an adjusted response rate of 27.3 % (173/633).
Of the 173 physicians who completed the survey, 148 responded to the first mailing initiated in January 2020, 14 responded to the second mailing initiated in March 2020, and 11 completed the web-based questionnaire between June and August 2020.
Survey respondents and non-respondents did not differ by age, sex, state tertile, or primary care specialty (eTable 2). Among survey respondents, the mean age was 52 years, 43.4 % were female and three fourths were non-Hispanic white (Table 1). Overall, 34.1 % practiced in urban, 35.3 % practiced in suburban, and 28.2 % practiced in rural communities. Among respondents, 37.0 %, 28.9 %, and 34.1 % were from states in the first (lowest), second, and third (highest) tertiles of drug overdose mortality. More than half (53.8 %) were family medicine physicians, 45.1 % were internal medicine physicians, and 1.2 % were general practitioners. Overall, 37.3 % worked in an academic medical center or teaching hospital. Approximately one third (33.5 %) practiced in solo or small group practices. Among all respondents, 41.4 % reported pharmaceutical company representatives visit their primary site of clinical practice.
Table 1.
Respondent demographic and practice characteristics.
| Overall (N = 173) | |
|---|---|
| Age, years (SE) | 52 (1) |
| Female | 43.4 % |
| Race/ethnicity | |
| Non-Hispanic white | 75.3 % |
| Non-Hispanic Black | 8.4 % |
| Hispanic | 6.6 % |
| Asian | 13.9 % |
| Geography | |
| Urban | 34.1 % |
| Suburban | 35.3 % |
| Rural | 28.2 % |
| State drug overdose death rate (2017) | |
| Tertile 1 (lowest) | 37.0 % |
| Tertile 2 | 28.9 % |
| Tertile 3 (highest) | 34.1 % |
| Primary care specialty | |
| Internal medicine | 45.1 % |
| Family medicine | 53.8 % |
| General practice | 1.2 % |
| Work in an academic medical center or teaching hospital | 37.3 % |
| Practice type* | |
| Solo or small group practice | 33.5 % |
| Managed care organization | 17.1 % |
| Academic medical center-based practice | 24.1 % |
| Federally Qualified Health Center (FQHC) | 8.8 % |
| Public or government-based practice | 9.4 % |
| Other | 17.7 % |
| Number of patients seen in a typical month, Mean (SE) | 253 (15) |
| Number of physicians and nurse practitioners, Mean (SE) | 64 (38) |
| Percent annual pay from number of patients you see | |
| 0–25% | 54.1 % |
| 26–50% | 8.2 % |
| 51–75% | 1.3 % |
| 76–100% | 36.5 % |
| Pharmaceutical company representatives visit practice | 41.4 % |
Categories not mutually exclusive and responses may sum to >100 %.
3.2. Physician readiness to treat opioid use disorder
Overall, more than 90 % of respondents said opioids were a moderate or big problem in their community and nearly 60 % reported at least one unique patient in their practice in the past year had lost a family member or friend to an opioid overdose (Table 2). In the past year, 90.6 % of physicians reported seeing at least one patient with OUD in their practice and 53.9 % reported treating a patient with OUD.
Table 2.
Identification and treatment of opioid use disorder.
| Percent | |
|---|---|
| How big of a problem is the opioid epidemic in your community | |
| A big problem | 44.9 % |
| A moderate problem | 46.7 % |
| A small problem | 8.4 % |
| No problem at all | 0.0 % |
| Number of unique patients in your practice in the past year who have lost a family member or friend to an opioid overdose | |
| 0 | 43.8% |
| 1–5 | 33.3% |
| 6–10 | 9.2 % |
| 11–20 | 6.5% |
| 21–50 | 5.2% |
| >50 | 2.0% |
| Number of unique patients in your practice in the past year with OUD | |
| 0 | 9.4 % |
| 1–10 | 42.8% |
| 11–50 | 32.1% |
| 51–100 | 12.6% |
| >100 | 3.1 % |
| Treated anyone with OUD in the past year | 53.9 % |
| For the most recent treated with OUD, which of the following did you do with respect to their OUD* | |
| Refer or co-manage them with an addiction specialist | 63.3 % |
| Manage their OUD within the practice | 46.7 % |
| Encourage a 12-step program (e.g., Narcotics Anonymous) | 41.1 % |
| Treat them with buprenorphine for OUD | 30.0 % |
| Treat them with naltrexone for OUD | 16.7 % |
| Treat them with methadone for OUD through an opioid treatment program | 7.8 % |
| Anyone in practice waivered to prescribe buprenorphine | 33.5 % |
| Physician waivered to prescribe buprenorphine† | 10.7 % |
| Practice accepts insurance for buprenorphine treatment‡ | 83.0 % |
| Referral relationship with any providers that offer addiction treatment | 58.8 % |
Among those who had treated someone with OUD in the past year (N = 90). Responses not mutually exclusive and may sum to >100 %.
Question not asked on web-based survey and responses exclude 11 web-based respondents (N = 162).
Among those in practices where they or a colleague are waivered to prescribe buprenorphine (N = 56).
Only one third of all respondents (33.5 %) reported they or a practice colleague were waivered to prescribe buprenorphine for OUD treatment, and 10.7 % physicians reported that they had a waiver to prescribe buprenorphine. Among physicians in practices with at least one waivered prescriber, 83.0 % reported accepting insurance for buprenorphine treatment.
Most physicians said they were somewhat or very comfortable screening patients for OUD (80.7 %) and diagnosing patients with OUD (79.3 %) (Fig. 1). However, fewer (36.9 %) said they were somewhat or very comfortable treating patients with OUD with medications, with 1 in 5 physicians reporting they were not at all comfortable with treating patients with OUD with medications. In the subset who had treated a patient with OUD in the past year, 87.7 % were somewhat or very comfortable screening patients for OUD, 86.5 % were somewhat or very comfortable diagnosing patients with OUD, and 52.3 % were somewhat or very comfortable treating patients with OUD with medications, while 6.8 % were not at all comfortable treating patients with OUD with medications.
Fig. 1.
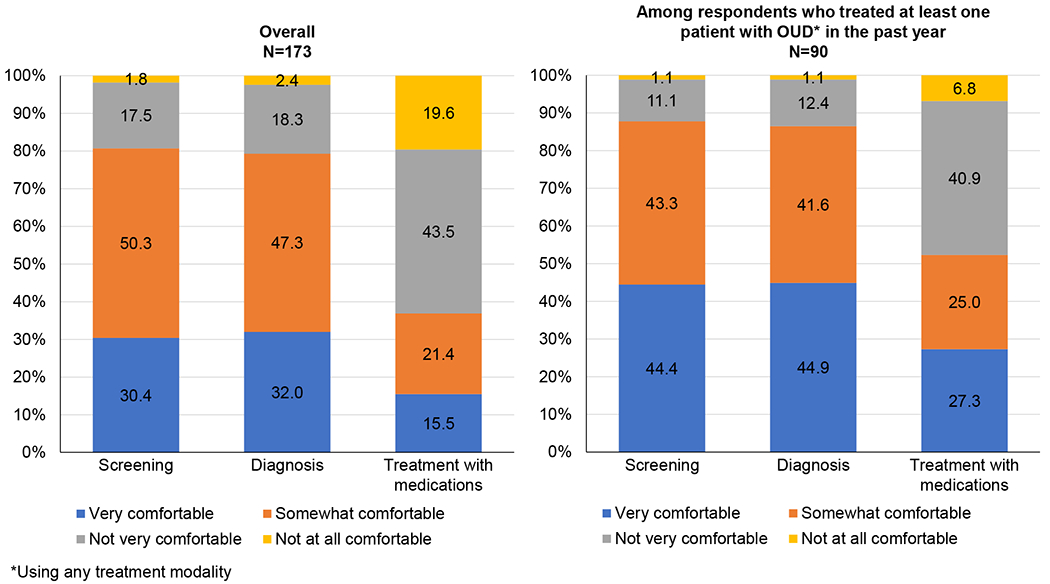
Physician comfort screening, diagnosing, and treating opioid use disorder.
This figure shows the proportion of primary care physicians overall and the proportion of those who had treated at least one patient with OUD in the past year using any treatment modality who are very comfortable, somewhat comfortable, not very comfortable, or not at all comfortable screening for OUD, diagnosing OUD, and treating OUD with medications.
3.3. Treatment of opioid use disorder
Among physicians who reported treating a patient with OUD in the past year, 63.3 % reported they referred or comanaged their most recent patient with OUD with an addiction specialist, 46.7 % of physicians reported managing OUD within their practice, and 41.1 % reported encouraging a 12-step program such as Narcotics Anonymous. Buprenorphine was the most common medication treatment utilized as 30.0 % reported treating their most recent patient with OUD with buprenorphine, followed by naltrexone (16.7 %). Additionally, 7.8 % reported their most recent patient with OUD was treated with methadone provided through an opioid treatment program.
Among physicians who had treated a patient with OUD in the past year, 81.9 % were somewhat or very confident in the safety of the care their patients received for OUD and 68.7 % were somewhat or very confident in the effectiveness of care their patients received for OUD (Fig. 2). However, large minorities of physicians reported being not very confident or not at all confident in the comprehensiveness (37.4 %), timeliness (41.0 %), and patient-centeredness (28.9 %) of OUD care received.
Fig. 2.
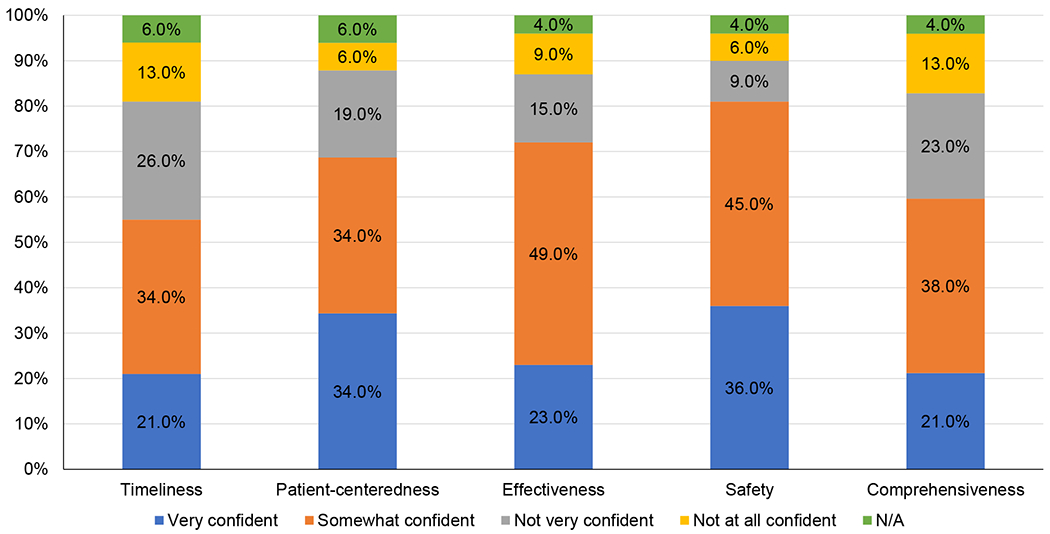
Physician confidence in the quality of care patients with opioid use disorder receive*.
*Among those who had treated someone with OUD in the past year. Question not asked on web-based survey. (N = 83).
Among primary care physicians who had treated at least one patient with OUD in the past year, this figure shows the proportion who were very confident, somewhat confident, not very confident, or not at all confident in the quality of care for OUD that their patients received in terms of timeliness, patient-centeredness, effectiveness, safety, and comprehensiveness.
3.4. Barriers to buprenorphine treatment
The most commonly cited barriers to obtaining a buprenorphine waiver were lack of experience treating OUD (61.1 %), preference not to be inundated with requests for buprenorphine (45.8 %), lack of access to addiction, behavioral health, or psychiatric co-management (41.2 %), and requirements for eight-hour training to obtain a waiver (35.9 %) (Table 3).
Table 3.
Barriers to obtaining buprenorphine waiver and increasing buprenorphine prescribing.
| Obtaining buprenorphine waiver* N = 162 |
Increasing buprenorphine prescribing*,† N = 45 |
|
|---|---|---|
| Poor reimbursement or other insurance barriers (e.g., prior authorization, step therapy) | 9.2 % | 27.3 % |
| Lack of access to addiction, behavioral health, or psychiatric co-management | 41.2 % | 47.7 % |
| Too little experience treating opioid use disorder | 61.1 % | 34.1 % |
| Lack of eligible patients with opioid use disorder within the practice | 19.1 % | 18.2 % |
| Preference not to be inundated with requests for buprenorphine | 45.8 % | 31.8 % |
| Concern about the risk of buprenorphine misuse or diversion | 25.2 % | 22.7 % |
| Requirements for eight-hour training to obtain buprenorphine “waiver” | 35.9 % | 27.3 % |
| Presence of better treatments for OUD than buprenorphine | 3.1 % | 4.6 % |
| Resistance from practice partners, staff, or lack of institutional support | 21.4 % | 22.7 % |
| Federal or state regulations related to buprenorphine | 17.6 % | 27.3 % |
Responses to these survey questions allowed participants to select all that apply and may sum to >100 %.
Question not asked on web-based survey and responses exclude 11 web-based respondents.
Among those in practices where they or a colleague are waivered to prescribe buprenorphine.
Among those in a practice where they or a colleague were waivered to prescribe buprenorphine, the most common barriers to increasing buprenorphine prescribing were lack of access to addiction, behavioral health, or psychiatric co-management (47.7 %), lack of experience treating OUD (34.1 %), preference not to be inundated with requests for buprenorphine (31.8 %), and requirements for eight-hour training to obtain a waiver (27.3 %), poor reimbursement or other insurance barriers (27.3 %), and federal or state regulations related to buprenorphine (27.3 %).
3.5. Opioid use disorder treatment by state burden of drug overdose deaths
There was no statistically significant difference across state tertiles of drug overdose mortality in the proportion of physicians who responded that opioids were a big problem in their community (p = 0.48) (Table 4). About half of physicians in each state tertile had treated anyone with OUD in the past year. There were no statistically significant differences by state tertile in physicians’ level of comfort screening, diagnosing, or treating patients with OUD. Those in the third tertile were somewhat more likely to have a referral relationship with any provider that offers addiction treatment (p = 0.14).
Table 4.
Identification and treatment of opioid use disorder by state tertile of drug overdose mortality.
| Tertile 1 (lowest rate) N = 64 |
Tertile 2 N = 50 |
Tertile 3 (highest rate) N = 59 |
P value | |
|---|---|---|---|---|
| How big of a problem is the opioid epidemic in your community, % | 0.48 | |||
| A big problem | 37.1 | 48.9 | 50.0 | |
| A moderate problem | 53.2 | 40.4 | 44.8 | |
| A small problem | 9.7 | 10.6 | 5.2 | |
| No problem at all | 0.0 | 0.0 | 0.0 | |
| Treated anyone with OUD in the past year, % | 55.6 | 51.0 | 54.5 | 0.89 |
| Somewhat or very comfortable screening patients for OUD, % | 87.5 | 78.0 | 75.4 | 0.21 |
| Somewhat or very comfortable diagnosing patients with OUD, % | 82.5 | 83.7 | 71.9 | 0.24 |
| Somewhat or very comfortable treating patients with OUD using medications, % | 38.1 | 40.8 | 32.1 | 0.64 |
| Referral relationship with any providers that offer addiction treatment, % | 55.7 | 57.4 | 63.2 | 0.14 |
| Anyone in practice waivered to prescribe buprenorphine, % | 40.3 | 28.6 | 30.4 | 0.35 |
| Physician waivered to prescribe buprenorphine*, % | 9.1 | 11.6 | 11.4 | 0.91 |
| Practice accepts insurance for buprenorphine treatment†, % | 84.0 | 81.8 | 82.4 | 0.98 |
| Barriers to increasing buprenorphine prescribing*,†, % | ||||
| Lack of access to addiction, behavioral health, or psychiatric co-management, % | 57.1 | 54.5 | 25.0 | 0.18 |
| Too little experience treating opioid use disorder, % | 38.1 | 27.3 | 33.3 | 0.83 |
| Lack of eligible patients with opioid use disorder within the practice, % | 19.0 | 18.2 | 16.7 | 0.99 |
| Preference not to be inundated with requests for buprenorphine, % | 38.1 | 36.4 | 16.7 | 0.42 |
Question not asked on web-based survey and responses exclude 11 web-based respondents.
Among those in practices where they or a colleague are waivered to prescribe buprenorphine.
There were no significant differences by state tertile in the proportion of physicians in practices with at least one waivered buprenorphine prescriber (p = 0.35) or the proportion of waivered physicians (p = 0.91). Among those in practices where they or a colleague were waivered, the proportion who reported their practice accepts insurance for buprenorphine was similar across the three tertiles of states (>80 %). Among those in practices where they or a colleague were waivered to prescribe buprenorphine, 57.1 % of physicians in the first and 54.5 % of physicians in the second state tertile reported lack of access to addiction, behavioral health, or psychiatric co-management as a barrier to increasing buprenorphine prescribing compared to 25.0 % of those in the third state tertile (p = 0.18). There was no difference in the proportion of physicians who reported having too little experience (p = 0.83), lack of eligible patients (p = 0.99), or a preference not to be inundated with requests for buprenorphine (p = 0.42) as barriers to increasing buprenorphine prescribing.
4. Discussion
In this recent national survey of primary care physicians, the vast majority indicated opioids were a problem in their community and 90 % had seen a patient with OUD in their practice in the past year. Primary care physicians were generally comfortable screening and diagnosing OUD, but much less comfortable treating OUD with medications. Overall, 1 in 5 physicians expressed that they were not at all comfortable using medications to treat OUD, though this proportion was lower among those who had treated a patient with OUD (using any treatment modality) in the past year. Although buprenorphine was the medication used most frequently, we found just one third of respondents were in a practice where they or a colleague were waivered to prescribe buprenorphine and only one in ten respondents was waivered to prescribe buprenorphine. These findings underscore the ubiquity of the opioid epidemic in the U.S. and highlight important opportunities to expand the use of medications for opioid use disorder treatment (MOUD) among primary care physicians.
Primary care physicians are in a unique position to expand access to buprenorphine (Haffajee et al., 2018; Saloner et al., 2018). However, there are documented gaps in buprenorphine treatment capacity and prescribing (Jones et al., 2015). In our study, 10.7 % of primary care physicians reported they were waivered to prescribe buprenorphine, an estimate that closely matches another recent survey which found 10.6 % of primary care physicians were waivered to prescribe buprenorphine (McGinty et al., 2020). The proportion of physicians waivered to prescribe buprenorphine did not differ by state tertile of drug overdose mortality, though other studies have illustrated buprenorphine physician supply is higher and has increased to a greater extent in states with higher opioid overdose mortality rates (Knudsen et al., 2017).
As policy solutions are considered to expand access to buprenorphine for OUD treatment, our analysis identifies important barriers to address. The Department of Health and Human Services published Practice Guidelines for the Administration of Buprenorphine for Treating Opioid Use Disorder in April 2021, which exempt eligible practitioners from federal certification requirements related to training, counseling, and other ancillary services that are part of the process for obtaining a waiver to treat up to 30 patients with buprenorphine (US Department of Health and Human Services, 2021). Because the need for OUD treatment has outpaced the supply of waivered physicians, and because the waiver perpetuates stigma around the treatment of OUD with medications and implies addiction treatment is outside mainstream medicine, there have been numerous calls to eliminate the waiver requirement (Fiscella et al., 2019; Olsen et al., 2021). In our study, the 8 -h training requirement was cited as a barrier to obtaining a buprenorphine waiver and to increasing buprenorphine prescribing. However, our analysis also identified other barriers to obtaining a buprenorphine waiver and increasing buprenorphine prescribing, including lack of experience treating OUD, lack of access to addiction, behavioral health, or psychiatric co-management, and a preference not to be inundated with buprenorphine requests.
Another recent survey found 38 % of primary care physicians supported eliminating the requirement to complete the 8-h training and register with the Federal government to prescribe buprenorphine (McGinty et al., 2020). This may be a reflection of our findings that physicians feel they need more experience treating OUD and support to prescribe buprenorphine, though in both studies, few had obtained a waiver and had ever prescribed buprenorphine. Over 60 % of physicians in our study responded having too little experience treating addiction was a barrier to obtaining a buprenorphine waiver and 34.1 % of physicians in a practice with at least one waivered prescriber reported lack of experience treating addiction was a barrier to increasing buprenorphine prescribing. Previous studies among primary care physicians have also found insufficient education, training, and experience is a major barrier to buprenorphine prescribing (Barry et al., 2009; Cunningham et al., 2007; Haffajee et al., 2018; Mendoza et al., 2016). Additionally, among those who are waivered but lack training in addiction medicine, insufficient training was cited as a barrier to prescribing, particularly without access to specialist support (Mendoza et al., 2016). These findings highlight the need to invest in education in addiction medicine, including training physicians earlier, such as during medical training (McCance-Katz et al., 2017; Sharfstein and Olsen, 2019), and integrating experience treating OUD into all phases of health professional training (Fiscella et al., 2019). Practicing physicians should be encouraged and incentivized to prescribe buprenorphine and complete any needed training, such as through continuing education, maintenance of certification, or working with mentors in practice (Weimer et al., 2021). Such efforts should also be integrated into health systems changes facilitating specialist support.
Consistent with prior research, we found lack of access to addiction, behavioral health, or psychiatric co-management was a common barrier to obtaining a buprenorphine waiver and increasing buprenorphine prescribing (Andrilla et al., 2017; Cioe et al., 2020; Haffajee et al., 2018; Hutchinson et al., 2014; Jones and McCance-Katz, 2019b). Fewer than 60 % of physicians in our study reported having a referral relationship with providers offering addiction treatment. These barriers could be addressed by embedding addiction medicine providers in primary care practices and expanding emerging comprehensive service delivery models that provide for integrated care (Brooklyn and Sigmon, 2017). Future research can also help identify effective models of primary care management of OUD, including effective coordination and integration, and best practices for implementation (Chou et al., 2016; Saloner et al., 2018).
A high proportion of physicians also expressed a preference not to be inundated with requests for buprenorphine. Low physician willingness to prescribe buprenorphine has been found in other studies (Huhn and Dunn, 2017). Among waivered physicians, lack of patient demand has also been cited as a reason for not prescribing buprenorphine or prescribing to maximum patient limits (Jones and McCance-Katz, 2019b). These findings may reflect physician and patient stigma around use of MOUD and indicate a need to address both physician and patient understanding of buprenorphine treatment (Madras et al., 2020).
During the COVID-19 public health emergency, the Drug Enforcement Administration has expanded the ability to initiate and prescribe buprenorphine for current and new patients with OUD via telephone or telemedicine visit (US Department of Justice, 2020). While it is unknown whether this flexibility will be permitted moving forward, some patient-level barriers to buprenorphine treatment may be reduced or eliminated as a result of this new flexibility and may drive the development of new models of OUD care. This further highlights the need to address physician- and practice-level barriers identified in our study to increase buprenorphine treatment capacity.
Our study has limitations. First, our adjusted response rate was 27.3 %. While we attempted to reach participants several times, the COVID-19 pandemic likely impacted the response rate, as well as our ability to perform additional mailings. However, we did not find differences in the characteristics of respondents and non-respondents. Second, we shortened the web-based version of the survey to reduce participant burden and encourage participation. While excluding web-based respondents from certain questions could introduce selection bias, only 11 participants of 173 completed the web-based survey. Third, our results could be affected by recall bias, such as the numbers of patients seen or how the most recent patient with OUD was treated. Fourth, the results could be affected by social desirability bias, though given the nature of the questions asked, the socially desirable response was not always clear. Finally, while the survey was developed with experts and reviewed with a small group of primary care physicians, we did not formally validate the questions. Our study also has a number of strengths. The survey was conducted anonymously to maintain confidentiality of responses and encourage accurate reporting. The sample includes physicians from states with higher and lower rates of drug overdose deaths; from urban, suburban, and rural areas; and who have been in practice for varying lengths of time.
5. Conclusions
Our survey indicates primary care physicians believe they can effectively identify and diagnose OUD, but are less comfortable treating OUD with medications. While buprenorphine was the most commonly used medication, there are barriers to increasing its use among both physicians who were previously waivered to prescribe buprenorphine and those who were not. Addressing barriers such as provider self-efficacy and willingness to treat patients with OUD with buprenorphine, and identifying effective, coordinated, and comprehensive models of OUD treatment to support primary care providers in providing MOUD may help improve patient outcomes.
Supplementary Material
Funding
This study was funded by a Liptiz Public Health Policy Award from the Institute for Health and Social Policy at the Johns Hopkins Bloomberg School of Public Health.
Footnotes
Declaration of Competing Interest
GCA is past Chair of FDA’s Peripheral and Central Nervous System Advisory Committee; is a co-founding Principal and equity holder in Monument Analytics, a health care consultancy whose clients include the life sciences industry as well as plaintiffs in opioid litigation; and is a past member of OptumRx’s National P&T Committee. This arrangement has been reviewed and approved by Johns Hopkins University in accordance with its conflict of interest policies. The statements, findings, conclusions, views, and opinions contained and expressed herein are not necessarily those of IQVIA or any of its affiliated or subsidiary entities.
Appendix A. Supplementary data
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.drugalcdep.2021.108811.
References
- Alter A, Yeager C, 2020. COVID-19 Impact on US National Overdose Crisis (Accessed 1.4.2021). http://odmap.org/Content/docs/news/2020/ODMAP-Report-May-2020.pdf.
- American Association for Public Opinion Research, 2016. Standard Definitions Final Dispositions of Case Codes and Outcome Rates for Surveys.
- Andrilla CHA, Coulthard C, Larson EH, 2017. Barriers rural physicians face prescribing buprenorphine for opioid use disorder. Ann. Fam. Med 15, 359–362. 10.1370/afm.2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry DT, Irwin KS, Jones ES, Becker WC, Tetrault JM, Sullivan LE, Hansen H, O’Connor PG, Schottenfeld RS, Fiellin DA, 2009. Integrating buprenorphine treatment into office-based practice: a qualitative study. J. Gen. Intern. Med 24, 218–225. 10.1007/sll606-008-0881-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bipartisan Policy Center, 2019. Tracking Federal Funding to Combat the Opioid Crisis (Accessedl.4.2021). https://bipartisanpolicy.org/report/combating-the-opioid-crisis-2020/.
- Brooklyn JR, Sigmon SC, 2017. Vermont hub-and-Spoke model of care for opioid use disorder: development, implementation, and impact. J. Addict. Med 11, 286–292. 10.1097/ADM.0000000000000310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, 2020. Overdose Deaths Accelerating During COVID-19 [Press release]. https://www.cdc.gov/media/releases/2020/p1218-overdose-deaths-covid-19.html.
- Centers for Disease Control and Prevention (CDC), n.d. 2017. Drug Overdose Death Rates | Drug Overdose | CDC Injury Center; [WWW Document]. URL https://www.cdc.gov/drugoverdose/data/statedeaths/drug-overdose-death-2017.html (Accessed 9.2.20). [Google Scholar]
- Chou R, Korthuis TP, Weimer M, Bougatsos C, Blazina I, Zakher B, Grusing S, Devine B, McCarty D, 2016. Medication-assisted treatment models of care for opioid use disorder in primary care settings. Agency Healthc. Res. Qual. Technical Brief No. 28. (Prepared by the Pacific Northwest Evidence-based Practice Center under Contract No. 290-2015-00009-I.) AHRQ Publication No. 16(17)-EHC039-EF. Rockville, MD: Agency for Healthcare Research and Quality. December 2016. www.effectivehealthcare.ahrq.gov/reports/final.cfm. [PubMed] [Google Scholar]
- Cioe K, Biondi BE, Easly R, Simard A, Zheng X, Springer SA, 2020. A systematic review of patients’ and providers’ perspectives of medications for treatment of opioid use disorder. J. Subst. Abuse Treat 119, 108146. 10.1016/j.jsat.2020.108146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham CO, Kunins HV, Roose RJ, Elam RT, Sohler NL, 2007. Barriers to obtaining waivers to prescribe buprenorphine for opioid addiction treatment among HIV physicians. J. Gen. Intern. Med 22, 1325–1329. 10.1007/si1606-007-0264-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillman D, 1978. Mail and Telephone Surveys: The Total Design Method. John Wiley & Sons, New York (NY). [Google Scholar]
- Dunlop A, Lokuge B, Masters D, Sequeira M, Saul P, Dunlop G, Ryan J, Hall M, Ezard N, Haber P, Lintzeris N, Maher L, 2020. Challenges in maintaining treatment services for people who use drugs during the COVID-19 pandemic. Harm Reduct. J 17 (26) 10.1186/sl2954-020-00370-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiscella K, Wakeman SE, Beletsky L, 2019. Buprenorphine deregulation and mainstreaming treatment for opioid use disorder: X the X waiver. JAMA Psychiatry 76, 229–230. 10.1001/jamapsychiatry.2018.3685. [DOI] [PubMed] [Google Scholar]
- Giroir B, McCance-Katz EF, Collins FS, Jones CM, 2020. Agency Priority Goal Action Plan: Reducing Opioid Morbidity and Mortality (Accessed 27 April 2021). https://trumpadministration.archives.performance.gov/health_and_human_services/FY2020_july_Reducing_Opioid_Morbidity_and_Mortality_Q1-2.pdf.
- Haffajee RL, Bohnert ASB, Lagisetty PA, 2018. Policy pathways to address provider workforce barriers to buprenorphine treatment. Am. J. Prev. Med 54, S230–S242. 10.1016/j.amepre.2017.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huhn AS, Dunn KE, 2017. Why aren’t physicians prescribing more buprenorphine? J. Subst. Abuse Treat 78, 1–7. 10.1016/j.jsat.2017.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchinson E, Catlin M, Andrilla CHA, Baldwin LM, Rosenblatt RA, 2014. Barriers to primary care physicians prescribing buprenorphine. Ann. Fam. Med 12, 128–133. 10.1370/afm.1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang CS, Turner LW, Kruszewski SP, Kolodny A, Alexander GC, 2015. Prescription drug abuse: a national survey of primary care physicians. JAMA Intern. Med 175, 302–304. 10.1001/jamainternmed.2014.6520. [DOI] [PubMed] [Google Scholar]
- Hwang CS, Turner LW, Kruszewski SP, Kolodny A, Alexander GC, 2016. Primary care physicians’ knowledge and attitudes regarding prescription opioid abuse and diversion. Clin. J. Pain 32, 279–284. 10.1097/AJP.0000000000000268. [DOI] [PubMed] [Google Scholar]
- Jones CM, McCance-Katz EF, 2019a. Co-occurring substance use and mental disorders among adults with opioid use disorder. Drug Alcohol Depend. 197, 78–82. 10.1016/j.drugalcdep.2018.12.030. [DOI] [PubMed] [Google Scholar]
- Jones CM, McCance-Katz EF, 2019b. Characteristics and prescribing practices of clinicians recently waivered to prescribe buprenorphine for the treatment of opioid use disorder. Addiction 114, 471–482. 10.1111/add.14436. [DOI] [PubMed] [Google Scholar]
- Jones CM, Campopiano M, Baldwin G, McCance-Katz E, 2015. National and state treatment need and capacity for opioid agonist medication-assisted treatment. Am. J. Public Health 105, e55–e63. 10.2105/AJPH.2015.302664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knudsen HK, Havens JR, Lofwall MR, Studts JL, Walsh SL, 2017. Buprenorphine physician supply: relationship with state-level prescription opioid mortality. Drug Alcohol Depend. 173, 55–64. 10.1016/j.drugalcdep.2016.08.642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madras BK, Ahmad NJ, Wen J, Sharfstein J, 2020. Improving Access to Evidence-Based Medical Treatment for Opioid Use Disorder: Strategies to Address Key Barriers Within the Treatment System. NAM Perspect. 10.31478/202004b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins SS, Sarvet A, Santaella-Tenorio J, Saha T, Grant BF, Hasin DS, 2017. Changes in US lifetime heroin use and heroin use disorder prevalence from the 2001-2002 to 2012-2013 national epidemiologic survey on alcohol and related conditions. JAMA Psychiatry 74, 445–455. 10.1001/jamapsychiatry.2017.0113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCance-Katz EF, George P, Scott NA, Dollase R, Tunkel AR, McDonald J, 2017. Access to treatment for opioid use disorders: medical student preparation. Am. J. Addict 26, 316–318. 10.1111/ajad.12550. [DOI] [PubMed] [Google Scholar]
- McGinty EE, Stone EM, Kennedy-Hendricks A, Bachhuber MA, Barry CL, 2020. Medication for opioid use disorder: a national survey of primary care physicians. Ann. Intern. Med 173, 160–162. 10.7326/ml9-3975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendoza S, Rivera-Cabrero AS, Hansen H, 2016. Shifting blame: Buprenorphine prescribers, addiction treatment, and prescription monitoring in middle-class America. Transcult. Psychiatry 53, 465–487. 10.1177/1363461516660884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine, 2019. Medications for Opioid Use Disorder Save Lives, Medications for Opioid Use Disorder Save Lives. Washington, DC. 10.17226/25310. [DOI] [Google Scholar]
- Olsen Y, Fitzgerald RM, Wakeman SE, 2021. Overcoming barriers to treatment of opioid use disorder. JAMA 325, 1149–1150. 10.1001/jama.2021.1741. [DOI] [PubMed] [Google Scholar]
- Rutkow L, Turner L, Lucas E, Hwang C, Caleb Alexander G, 2015. Most primary care physicians are aware of prescription drug monitoring programs, but many find the data difficult to access. Health Aff. 34, 484–492. 10.1377/hlthaff.2014.1085. [DOI] [PubMed] [Google Scholar]
- Saha TD, Kerridge BT, Goldstein RB, Chou SP, Zhang H, Jung J, Pickering RP, Ruan WJ, Smith SM, Huang B, Hasin DS, Grant BF, 2016. Nonmedical prescription opioid use and DSM-5 nonmedical prescription opioid use disorder in the United States. J. Clin. Psychiatry 77, 772–780. 10.4088/JCP.15ml0386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saloner B, Stoller KB, Alexander GC, 2018. Moving addiction care to the mainstream — improving the quality of buprenorphine treatment. N. Engl. J. Med 379, 4–6. 10.1056/NEJMpl804059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharfstein JM, Olsen Y, 2019. Making amends for the opioid epidemic. JAMA 321, 1446–1447. 10.1001/jama.2019.3505. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, 2018. National Survey of Substance Abuse Treatment Services (N-SSATS): 2017 Data on Substance Abuse Treatment Facilities. [Google Scholar]
- US Department of Health and Human Services, 2021a. Practice guidelines for the administration of buprenorphine for treating opioid use disorder. Federal Register 86, 22439–22440. https://www.federalregister.gov/documents/2021/04/28/2021-08961/practice-guidelines-for-the-administration-of-buprenorphine-for-treating-opioid-use-disorder#citation-1-p22440. [Google Scholar]
- US Department of Health and Human Services, n.d. Strategy to Combat Opioid Abuse, Misuse, and Overdose: A Framework Based on the Five Point Strategy. https://www.hhs.gov/opioids/sites/default/files/2018-09/opioid-fivepoint-strategy-20180917-508compliant.pdf (Accessed 1.4.2021).
- US Department of Justice, 2020. (No Title) [WWW Document]. URL https://www.deadiversion.usdoj.gov/GDP/(DEA-DC-022)(DEA068) DEA SAMHSA buprenorphinetelemedicine (Final) +Esign.pdf (accessed 9.2.20).
- Weimer MB, Wakeman SE, Saitz R, 2021. Removing one barrier to opioid use disorder treatment: is it enough? JAMA 325, 1147–1148. 10.1001/jama.2021.0958. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


