Abstract
Gender minority (GM) youth are at heightened risk for psychopathology, purportedly due to their experiences of GM stressors. However, few studies have examined how GM stressors are associated with depression and anxiety among GM youth. Furthermore, no prior studies have investigated how experiences of GM stressors differ across gender identity and race/ethnicity within a diverse sample of GM youth. A nationwide online cross-sectional survey of 1,943 14- to 18-year-old GM adolescents (66.91% White, 11.73% multiracial, 8.49% Latinx, 7.10% Black, 3.09% Asian, 1.49% American Indian/Alaskan Native) in the U.S. assessed GM stressors (prejudice events, expectations of rejection, internalized transnegativity, and concealment) and mental health. Structural equation modeling was used to examine how GM stressors, and depressive and anxiety symptoms, differ across gender identity and race/ethnicity. Higher levels of each GM stressor were related to higher depressive symptoms. Prejudice events, expectations of rejection, and concealment were related to higher anxiety symptoms. Transmasculine and transfeminine youth reported higher levels of GM prejudice events and expectations of rejection, and higher mental health symptoms, than nonbinary youth. Findings were relatively consistent across racial/ethnic identities, with the exception that Black GM adolescents reported fewer GM prejudice events and expectations of rejection and indirectly exhibited lower mental health symptoms as compared to White GM youth. Researchers and clinicians should be attuned to how intersectional identities are related to stress and mental health among diverse GM youth. Recommendations for individual and structural-level interventions are discussed.
Keywords: gender minority, race/ethnicity, minority stress, depression, anxiety, adolescence
Empirical work documents that gender minority (GM) youth (youth whose gender identity differs from their sex assigned at birth) are more likely to experience depression and anxiety than their cisgender peers (Becerra-Culqui et al., 2018). Over half of GM youth meet diagnostic criteria for a depressive disorder (Becerra-Culqui et al., 2018). Similarly, 37% to 48% of GM youth meet criteria for an anxiety disorder (Becerra-Culqui et al., 2018; Chodzen et al., 2019). The minority stress model posits that disparities among sexual and gender minority (SGM) individuals are related to persistent stressors associated with a marginalized identity (Brooks, 1981; Meyer, 2003; Meyer, 2010). Despite mounting evidence of high risk for mental health problems among GM adolescents (Chodzen et al., 2019; Veale et al., 2017), prior research has not systematically examined how GM stressors are related to internalizing mental health symptoms among GM adolescents. Furthermore, little work has examined how minority stress experiences differ across gender and racial/ethnic identities.
Minority Stress Theory and Intersectionality
Minority stress theory proposes that mental health disparities related to SGM identities are explained by exposure to minority stressors (Brooks, 1981; Meyer, 2003; Meyer, 2010). The minority stress model was originally developed for sexual minority adults but has been adapted for GM populations (Hendricks & Testa, 2012). Stressors experienced by SGM individuals have been theorized as two distinct types: distal and proximal. Distal stressors are those that occur in the environment and include prejudice events—experiences of discrimination or victimization due to one’s GM status. Proximal stressors refer to three types of internal processes. First, GM individuals may experience expectations of rejection, including persistent worries about whether they will be safe, rejected, or accepted by strangers, peers, family members, and systems in their daily lives (e.g., healthcare facilities). Secondly, GM individuals may struggle with internalized transnegativity, or the internalization of negative beliefs about GM individuals, leading to negative self-perceptions and attitudes, such as a deeply felt sense that one is “wrong” or “bad” for being transgender. Realizing one’s GM identity necessitates a brave unlearning of these beliefs, which can be an arduous and ever-evolving process. Lastly, concealment involves hiding one’s current GM identity, sex assigned at birth, or gender history, often to avoid discrimination, rejection, or stigmatization. Concealment can be affirming by allowing GM individuals to “pass” or blend in as cisgender but can also be stressful because it may precipitate feelings of inauthenticity, worries about being “found out,” and sadness or frustration around not being accepted (Rood et al., 2017a). The minority stress model proposes that all four minority stressors work in concert to drive mental health disparities among SGM individuals (Brooks, 1981; Meyer, 2003; Meyer, 2010).
It is important to note that minority stress occurs not only on individual and interpersonal but also systemic levels. For example, anti-transgender legislation targeting youth is increasing, with more than 300 anti-LGBTQ+ pieces of legislation being considered across the U.S. as of September 2022 (“Anti LGBTQ+ Bills”, 2022). Anti-LGBTQ+ legislation has been found to have negative effects on the health and well-being of GM individuals (Horne et al, 2022) and is a particular concern for GM youth and their parents (Abreu et al., 2022; Barbee et al., 2022). Therefore, when GM youth encounter minority stressors in their daily lives, they are doing so within the context of a broader society which is not structured to support them and, in some places, is actively working to undermine them.
Many prior studies of GM youth have operationalized GM youth as one monolithic, homogenous population. However, recent evidence indicates psychosocial experiences and mental health symptoms vary across gender identity subgroups. Some studies have found that nonbinary/genderqueer youth (youth whose gender identity falls outside the male–female binary) generally experience more mental health symptoms than GM individuals with binary identities, including transmasculine and transfeminine youth (Grossman et al., 2016; Lefevor et al., 2019; Thorne et al., 2019). However, more evidence is needed to understand how minority stress experiences differ across gender identity subgroups.
Intersectionality theory (Collins, 2000; Crenshaw, 1989), a Black feminist framework that has increasingly been integrated across psychological research (Buchanan & Wiklund, 2020; Cole, 2009), provides a framework for contextualizing the unique experiences of GM youth across multiple social identities (e.g., gender, race/ethnicity, class). Multiple forms of minority stressors, both distal and proximal, are perpetuated by interlocking structural systems of power, privilege, and oppression (Brooks, 1981; Collins, 2000; Crenshaw, 1989) that shape GM youth’s experiences. Such stressors uniquely contribute to the mental health of GM youth of color (youth who identify with a marginalized racial/ethnic identity), both in terms of risk and resiliency.
Some research suggests that SGM adolescents of color report higher depressive symptoms compared to heterosexual adolescents (Bostwick et al., 2014). Studies have also found that SGM people of color are more likely to experience discrimination and victimization and also experience it more frequently, leading to higher depressive symptoms than White SGM adults (Calabrese et al., 2015; Everett et al., 2019). Systematic reviews focused exclusively on race-related experiences among adolescents indicate that racial discrimination is associated with increased psychopathology (Priest et al., 2013; Stirling et al., 2015). These experiences likely intersect with GM-related discrimination to create unique intersectional experiences (Mereish et al., 2022) for GM youth of color. Nonetheless, other studies have found that SGM youth of color have lower rates of psychopathology than White SGM youth (Toomey et al., 2017). For example, prior analyses of the current dataset found fewer depressive symptoms and self-injurious thoughts and behaviors among Black SGM adolescents compared to White SGM adolescents (Fox et al., 2020). Given mixed findings, additional investigations of how minority stressors are related to mental health symptoms among GM adolescents of color are required.
In this study, we systematically evaluate the original minority stress model (Brooks, 1981; Meyer, 2003; Meyer, 2010) by assessing the role of gender-specific forms of minority stress in the mental health of racially/ethnically diverse GM adolescents. Notably, we do not directly assess intersectional minority stressors (e.g., gendered racial discrimination) that may reflect unique experiences for GM youth of color. However, this study provides an important step toward understanding gender-related minority stressors among diverse GM youth, particularly because most prior studies of GM stress have not considered GM youth of color, resulting in discrepant findings related to their experiences.
GM Stressors Among GM Youth
Studies of GM adolescents are necessary because experiences of GM stressors during adolescence may differ from other life stages in several important ways. First, although no studies have examined when mental health disparities between GM and cisgender youth begin, disparities between heterosexual and sexual minority youth begin in early adolescence (Marshal et al., 2013), so investigating adolescence may provide more insight into the origin of disparities. Second, adolescence is a period of identity formulation and social development. Uncovering and accepting one’s GM identity may itself be a stressful experience. SGM youth often report losing social support after coming out, and a third of GM youth report being victimized due to their gender identity (Hatchel et al., 2019). Third, most adolescents live with and financially rely on parents or other family members, and half of all GM youth experience stress related to parental rejection (Grossman et al., 2021). Higher parental support is associated with better health and academic outcomes, fewer depressive symptoms, and less SGM-identity disclosure stress (Grossman et al., 2021; Johns et al., 2018). For these reasons, experiences of GM stressors during adolescence may differ from–and in some cases, be more severe than–these experiences in adulthood.
Distal Stressors
Most of the literature on GM stressors and mental health focuses on distal stressors. GM prejudice events are related to higher psychological distress, depressed mood, and suicidal ideation among youth (Veale et al., 2017; Wilson et al., 2016). The likelihood of discrimination and its subsequent impact on youth mental health appears to differ across GM identities. Some studies have found that nonbinary and genderqueer youth are harassed, abused, and experience traumatic events at higher rates than binary GM youth (Lefevor et al., 2019). Others have found that binary GM adults report more discrimination than nonbinary adults (Poquiz et al., 2021). More research is needed to determine which subgroups of GM youth are at greatest risk of discrimination-related harm.
Similarly, rates of discrimination and subsequent mental health symptoms may differ for GM youth with different racial/ethnic identities. In a study of GM adolescents, being a person of color did not moderate the relationship between peer victimization and mental health issues (Hatchel et al., 2019). Yet, research examining the impact of racial/ethnic discrimination and gender victimization among SGM adolescents found that exposure to stressors based on race/ethnicity and SGM status predicted negative mental health outcomes, indicating that SGM adolescents of color could experience poorer mental health (Swann et al., 2020).
Proximal Stressors
Preliminary evidence suggests proximal stressors contribute to mental illness above and beyond the effect of distal stressors among SGM adults (Cogan et al., 2021; Meyer, 2003); however, studies tend to focus on SGM samples broadly rather than GM samples in particular, use composite measures of stressors, or examine a single proximal stressor in isolation. For example, higher composite proximal stressor scores, as well as a latent minority stress construct incorporating both proximal and distal stressors, have been linked to higher depressive symptoms in samples of SGM youth and young adults (Fulginiti et al., 2021; Hunter et al., 2021). Only one study has investigated the relationship between expectations of rejection and depression and anxiety symptoms among an all-GM sample of youth and found that the association did not reach significance (Chodzen et al., 2019). In the same sample, GM youth reporting higher levels of internalized transnegativity were more likely to meet criteria for depression and anxiety. To date, no studies have investigated concealment among a sample of GM youth.
Furthermore, very few studies have attended to heterogeneity within samples of GM youth, often due to small sample sizes. Regarding gender identity, limited evidence suggests that transfeminine and nonbinary adolescents report more negative future expectations and less pride than transmasculine adolescents (Poquiz et al., 2021), suggesting different proximal stress experiences among these groups that have not yet been linked to mental health outcomes. Additionally, in a previous study of the current dataset which did not examine the full minority stress model, Black and Latinx youth were less likely to have disclosed their gender identity to parents and reported lower gender-related expectations of rejection than White youth (Fox et al., 2020). However, researchers have not previously examined how differential levels of stressors relate to mental health symptoms among GM youth in this sample. Furthermore, no prior studies have concurrently measured expectations of rejection, internalized transnegativity, and concealment among GM youth of color.
The Current Study
Little attention has been paid to how specific GM stressors could confer risk for mental health symptoms among diverse GM youth, and proximal GM stressors are particularly under-addressed. Furthermore, few studies have explored differences in GM youth’s experiences across intersecting social identities (e.g., gender identity and race/ethnicity). Intersectionality theory demands that gender minority youth are not treated as a homogenous group. Therefore, the aims of the current study are threefold. First, we examine the full minority stress model (Brooks, 1981; Meyer, 2003; Meyer, 2010) among GM youth for the first time, and hypothesize that gender-related minority stressors will be related to mental health symptoms. Second, we explore differences in the experiences of adolescents with different GM identities (e.g., transmasculine, transfeminine, nonbinary, and questioning youth). Third, we investigate how the associations between GM stressors and mental health symptoms differ for GM youth across racial/ethnic identities, including Black, Asian, Latinx, American Indian/Alaskan Native, multiracial, and White GM youth. Due to the exploratory nature of the second and third aims, no hypotheses are specified.
We use cross-sectional data to address our research questions. While examining mediation with cross-sectional data has limitations, we believe the study makes a critical preliminary contribution to the existing literature on mental health among GM youth as the first to examine GM stressors and mental health symptoms with an intersectional lens. GM youth are a highly stigmatized and hidden population that have been underexamined in prior research because they are difficult to recruit into research studies, especially when parental permission is required. Given these challenges, few high-quality datasets exist focusing on the health of GM adolescents and, to our knowledge, no extant longitudinal studies of GM adolescents focus on minority stress. Because of these limitations inherent in existing literature, our cross-sectional data make a needed contribution.
Method
Participants
Participants were 1,943 GM adolescents from the U.S. (ages 14–18, Mage = 15.91, SDage = 1.22). Data were collected as part of a large nationwide, cross-sectional study of adolescent health which included both cisgender and GM adolescents (see Salk et al., 2020). The current analytic sample includes only participants who self-identified as GM and included 6.79% transfeminine, 50.95% transmasculine, 32.94% nonbinary assigned female at birth (AFAB), 4.32% nonbinary assigned male at birth (AMAB), and 4.99% questioning youth. Most participants (66.91%) self-identified as White, 7.10% as Black, 8.49% as Latinx, 3.09% as Asian, 11.73% as multiracial, 1.49% as American Indian/Alaskan Native, and 0.51% as another racial/ethnic identity. Most participants (96.7%) identified as sexual minority, with 18.9% identifying as gay or lesbian, 47.9% as bisexual or pansexual, 28.6% as queer, questioning, or another SM identity, and only 3.3% identifying as straight or heterosexual. The average subjective social status of participants was 5.40 (range = 1–10; SD = 1.54).
Procedure
Recruitment advertisements were posted on Facebook and Instagram in the summer and fall of 2018, inviting adolescents ages 14–18 to participate in an anonymous online study. Multiple steps were performed to ensure high quality data (see Supplementary Material A and Salk et al., 2020 for details). The final sample included adolescents from all 50 states, Washington, D.C., and Puerto Rico. To oversample GM youth, some advertisements were presented to users associated with interest tags such as “Genderqueer” and “Transgender.” The study received a waiver of parental consent from the University of Pittsburgh Human Research Protection Office to ensure the safety of transgender teens who were not out to their parents.
Measures
Sociodemographic Identity Variables.
Participants indicated their gender by checking all that apply from a list of 17 options; they indicated their assigned sex at birth by indicating “male”, “female”, or “intersex.” Participants were categorized as transfeminine if they identified as male to female transgender/MTF, trans female/trans feminine, and/or a combination of male sex assigned at birth and “female” gender identity. Participants were categorized as transmasculine if they identified as female to male transgender/FTM, trans male/trans masculine, and/or a combination of female sex assigned at birth and “male” gender identity. Those who identified with one or more nonbinary identities (e.g., genderqueer, gender expansive, androgynous, nonbinary, two-spirited, agender) but no binary identities were included in the nonbinary AMAB or nonbinary AFAB group, depending on their sex assigned at birth. Regardless of sex assigned at birth, if an adolescent only indicated “not sure” for their gender identity, they were categorized as questioning.
Participants indicated their race/ethnicity by checking all that apply from a list including White, Black, Hispanic/Latino, Asian/Pacific Islander, American Indian/Alaskan Native, or “other” race/ethnicity. Participants who indicated multiple racial/ethnic groups were categorized as “multiracial.” The “another racial/ethnic identity” group included only participants who could not be recategorized into another group based on their lack of a clear write-in response. Although these respondents were retained in the model, we do not report parameter estimates for this group because they are not interpretable, due to small cell size and heterogeneity within the group. As a proxy for socioeconomic status, participants completed the MacArthur Ladder of subjective social status (SSS) for youth (Goodman et al., 2001). Participants were presented with a picture of a ladder with 10 rungs and asked to “imagine that this ladder pictures how American society is set up” with those at the top having relatively more money, higher education, and high-status jobs than those lower down. Participants indicated where on the ladder (1 = worst off, 10 = best off) they and their family would be.
Prejudice Events.
Four items captured the frequency (in the past six months) of four transgender-specific bullying or harassment victimization experiences: “teased or bullied,” “hit or beaten up,” “treated rudely or unfairly,” and “called bad names” (Burton et al., 2013; α = 0.83). Items were adapted from a measure of sexual orientation-specific victimization and reworded to address prejudice events experienced due to one’s actual or assumed transgender identity. Responses included 1 = Never, 2 = Once or twice, 3 = A few times, 4 = Many times.
Expectations of Rejection.
Participants indicated agreement with four statements about expecting social rejection based on their gender identity, including wondering about being judged by others, feeling uncomfortable being judged, thinking a lot about how one’s gender identity affects others’ perceptions of oneself, and expecting poor treatment because of one’s gender identity (α = 0.81). Items were adapted from the acceptance concerns subscale of the Lesbian, Gay, and Bisexual Identity Scale (Mohr & Kendra, 2011) and rephrased to focus on gender identity rather than sexual orientation. Responses ranged from 1 = Strongly disagree to 6 = Strongly agree. Higher scores indicated greater expectations of rejection.
Internalized Transnegativity.
The 3-item Gender Identity Acceptance subscale of the Transgender Congruence Scale (Kozee et al., 2012) was used to assess participants’ feelings about their gender identity (α = 0.85). Participants responded to three statements about feelings of pride and acceptance (e.g., “I have accepted my gender identity”) on a scale from 1 = Strongly disagree to 5 = Strongly agree. One edit was made to the original scale to phrase all items positively (i.e., “I am proud of my gender identity” rather than “I am not proud…”) to improve readability and comprehension for adolescents (Omrani et al., 2019). Higher scores reflected higher pride in gender identity or lower internalized transnegativity.
Concealment.
Participants were asked “Who knows about your gender identity?” and checked all that applied from a list including: Parents/primary caregivers, friends, teachers, and “no one knows about my gender identity.” Participants were coded as 0 if they reported no one knew about their gender identity, 1 if they reported friends were aware of their gender identity, and 2 if parents and/or teachers were aware, with higher scores indicating lower concealment. Differentiating concealment and disclosure across different categories of relationships is a common approach to assessing identity disclosure among LGBTQ+ adults and adolescents (Mohr & Fassinger, 2000; Watson et al., 2015).
Mental Health Symptoms.
Depressive symptoms were measured with the 20-item Center for Epidemiologic Studies Depression Scale (CES-D; (Radloff, 1977), which has been used previously with adolescents (Garrison et al., 1991). Participants indicated how frequently in the past week they experienced depressive symptoms on a four-point Likert scale. The CES-D was reduced to a 10-item version while fitting the measurement model (α = 0.83; see Supplementary Material B). Anxiety symptoms were assessed with the 7-item Generalized Anxiety Disorder-7 (GAD-7; Spitzer et al., 2006), which has been validated among adolescents (Mossman et al., 2017). Participants indicated how frequently in the past two weeks they have experienced anxiety symptoms on a four-point Likert scale (α = 0.91).
Analysis Plan
Bivariate associations between all variables were examined, including differences across gender identity subgroups and race/ethnicity for continuous variables. Structural equation modeling was used in Mplus Version 8 (Muthén & Muthén, 2017). A measurement model was calculated and modified as necessary (see Supplementary Material B for measurement model approach and results). A structural model was fit to examine hypothesized associations between latent constructs and measured variables. Paths from sociodemographic identity variables, including age, SSS, gender identity, sexual orientation, and race/ethnicity, to each of the four minority stressors were estimated. Paths between each minority stressor and mental health symptoms were estimated separately for depressive and anxiety symptoms while also including sociodemographic covariates within each path (see Figure 1 for key hypothesized paths). Paths were estimated using maximum likelihood estimation, and missing data were accounted for using full information maximum likelihood (FIML). Missingness was almost exclusively due to early termination of the survey, so missing data should be considered missing at random. Under FIML, all cases are included and contribute to estimates within the model regardless of missingness (Enders & Bandalos, 2001). Gender identity, race/ethnicity, and sexual orientation were coded with transmasculine youth, White youth, and bisexual and pansexual youth as reference groups, respectively, because they were the largest subgroups.
Figure 1.
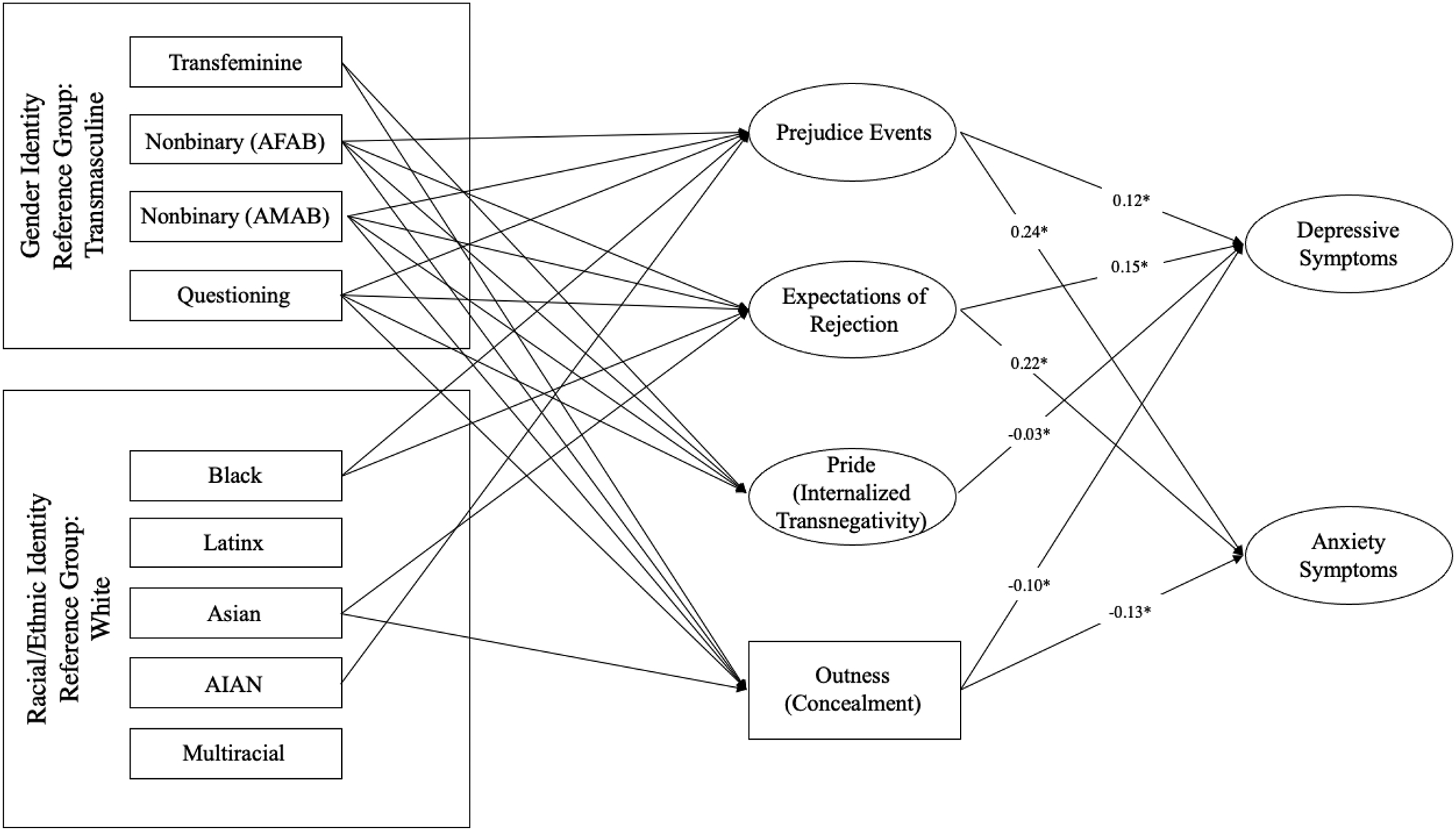
Structural model from sociodemographic identity variables to gender minority (GM) stressors to depressive and anxiety symptoms.
Note: For readability, not all covariatcs are shown. Direct effects from sociodemographic identity variables to GM stressors are available in Table 2. AFAB = assigned female at birth; AMAB = assigned male at birth; AIAN = American Indian/Alaskan Native.
Indirect effects between gender identity, race/ethnicity, and mental health symptoms via level of each minority stressor were assessed. To assess the significance of indirect effects, 95% confidence intervals were estimated using a bootstrapping procedure with 20,000 iterations that was not bias-corrected (Fritz et al., 2012). Indirect effects were considered significant if the confidence interval did not include zero. Importantly, in all analyses, gender and race/ethnicity are used to represent the interpersonal and contextual experiences of members of each social identity group, rather than presumed direct causes of psychosocial phenomena. In addition to examining indirect effects of subgroup identities on mental health symptoms via minority stressors within the structural equation model, we also conducted post hoc sensitivity analyses to examine moderation of associations between minority stressors and mental health symptoms by both gender identity subgroup and race/ethnicity (see Supplementary Material C).
Transparency and Openness
We describe data exclusions, manipulations, and measures in the study in Salk et al. (2020). Due to the risk of deductive disclosure with the minoritized population studied, deidentified data are only available from the study team through a data sharing agreement. Study analysis code is available from the authors upon request. This study was not preregistered.
Results
Preliminary Analyses
Correlations between continuous variables, as well as means, standard deviations, and missingness for each variable are included in Table 1. See Supplementary Material D for a description of bivariate associations. Age, SSS, and SM status were significantly associated with variables of interest and were included as covariates within the structural model.
Table 1.
Means, standard deviations, number of respondents, and correlations among study measures.
| Variable | 1. Age | 2. SSS | 3. Prejudice events | 4. Exp. of rejection | 5. Pride (internalized transnegativity) | 6. Outness (concealment) | 7. Depressive symptoms (CES-D 10) | 8. Anxiety symptoms (GAD-7) |
|---|---|---|---|---|---|---|---|---|
| 1. Age | ||||||||
| 2. Subjective Social Status (SSS) | .006 | |||||||
| 3. Prejudice events | −.062* | −.200* | ||||||
| 4. Expectations of rejection | −.043 | −.097* | .292* | |||||
| 5. Pride (internalized transnegativity) | .083* | −.064* | .011 | −.161* | ||||
| 6. Outness (concealment) | .116* | −.028 | .244* | .088* | .192* | |||
| 7. Depressive symptoms (CES-D 10) | −.026 | −.160* | .252* | .306* | −.138* | −.088* | ||
| 8. Anxiety symptoms (GAD-7) | −.016 | −.131* | .281* | .266* | −.088* | −.053 | .708* | |
| Mean (M) | 15.92 | 5.402 | 1.646 | 4.551 | 3.871 | 1.596 | 17.17 | 13.787 |
| Minimum | 14 | 1 | 1 | 1 | 1 | 0 | 0 | 0 |
| Maximum | 18 | 10 | 4 | 6 | 5 | 2 | 29 | 21 |
| Standard deviation (SD) | 1.221 | 1.537 | .733 | 1.109 | 1.054 | .615 | 6.080 | 5.644 |
| Respondents (n) | 1,943 | 1,790 | 1,079 | 1,633 | 1,632 | 1,725 | 1,363 | 1,033 |
Note.
p < .05
Direct Effects in Structural Model
Significant direct effects are represented in Figure 1, and all direct effects are reported within Table 2. Within the structural model, higher levels of GM prejudice events, expectations of rejection, and concealment of gender identity were related to higher levels of both depressive and anxiety symptoms. Higher levels of internalized transnegativity were related to higher depressive symptoms but were unrelated to anxiety symptoms. Because temporality between minority stressors and mental health symptoms cannot be firmly established with cross-sectional data, we also tested an alternative structural model with minority stressors as mediators and mental health symptoms as outcomes. Our original model evidenced stronger fit to our observed data than this alternative model (see Supplementary Material E).
Table 2.
Direct effects of sociodemographic identity variables, gender minority stressors, and depressive and anxiety symptoms.
| Parameter | Estimate | SE | p |
|---|---|---|---|
| Prejudice events | |||
| Age | −0.06 | 0.02 | .01 |
| SSS (Subjective Social Status) | −0.10* | 0.02 | <.01 |
| Transfeminine | 0.03 | 0.11 | .78 |
| Nonbinary (AFAB) | −0.47* | 0.06 | <.01 |
| Nonbinary (AMAB) | −0.32* | 0.13 | .01 |
| Questioning | −0.71* | 0.12 | <.01 |
| Black | −0.20* | 0.10 | .04 |
| Latinx | 0.01 | 0.09 | .87 |
| Asian | −0.10 | 0.16 | .52 |
| American Indian/Alaskan Native | 0.56* | 0.24 | .02 |
| Multiracial | 0.03 | 0.08 | .66 |
| Gay/lesbian | 0.03 | 0.07 | .66 |
| Queer, questioning, or another SM | 0.03 | 0.06 | .65 |
| Heterosexual | −0.27 | 0.15 | .07 |
| Expectations of rejection | |||
| Age | −0.04* | 0.02 | .03 |
| SSS | −0.05 | 0.02 | <.01 |
| Transfeminine | 0.09 | 0.10 | .39 |
| Nonbinary (AFAB) | −0.30* | 0.05 | <.01 |
| Nonbinary (AMAB) | −0.37* | 0.12 | <.01 |
| Questioning | −0.69* | 0.12 | <.01 |
| Black | −0.24* | 0.09 | .01 |
| Latinx | 0.04 | 0.09 | .68 |
| Asian | −0.28* | 0.14 | .05 |
| American Indian/Alaskan Native | 0.10 | 0.20 | .60 |
| Multiracial | −0.04 | 0.07 | .55 |
| Gay/lesbian | −0.02 | 0.06 | .80 |
| Queer, questioning, or another SM | 0.03 | 0.05 | .58 |
| Heterosexual | −0.15 | 0.14 | .28 |
| Pride (internalized transnegativity) | |||
| Age | 0.07* | 0.02 | <.01 |
| SSS | −0.04* | 0.02 | .03 |
| Transfeminine | 0.30* | 0.13 | .02 |
| Nonbinary (AFAB) | 0.18* | 0.06 | <.01 |
| Nonbinary (AMAB) | 0.47* | 0.15 | <.01 |
| Questioning | −0.58* | 0.14 | <.01 |
| Black | 0.24* | .11 | .03 |
| Latinx | 0.16 | 0.10 | .13 |
| Asian | 0.24 | 0.17 | .16 |
| American Indian/Alaskan Native | 0.08 | 0.24 | .73 |
| Multiracial | −0.01 | 0.09 | .89 |
| Gay/lesbian | 0.02 | 0.08 | .80 |
| Queer, questioning, or another SM | 0.17* | 0.07 | <.01 |
| Heterosexual | −0.22 | 0.17 | .19 |
| Outness (concealment) | |||
| Age | 0.05* | 0.01 | <.01 |
| SSS | −0.01 | 0.01 | .32 |
| Transfeminine | −0.16* | 0.06 | .01 |
| Nonbinary (AFAB) | −0.43* | 0.03 | <.01 |
| Nonbinary (AMAB) | −0.46* | 0.07 | <.01 |
| Questioning | −0.97* | 0.07 | <.01 |
| Black | −0.08 | 0.05 | .15 |
| Latinx | −0.10 | 0.05 | .05 |
| Asian | −0.18* | 0.08 | .02 |
| American Indian/Alaskan Native | −0.08 | 0.11 | .49 |
| Multiracial | −0.03 | 0.04 | .47 |
| Gay/lesbian | 0.04 | 0.04 | .31 |
| Queer, questioning, or another SM | 0.04 | 0.03 | .16 |
| Heterosexual | 0.14 | 0.08 | .08 |
| Depressive symptoms (CES-D 10) | |||
| Age | 0.02 | 0.01 | 0.14 |
| SSS | −0.03* | 0.01 | <.01 |
| Transfeminine | −0.04 | 0.05 | .40 |
| Nonbinary (AFAB) | 0.04 | 0.03 | .19 |
| Nonbinary (AMAB) | 0.004 | 0.06 | .95 |
| Questioning | 0.12 | 0.07 | .07 |
| Black | 0.06 | 0.05 | .18 |
| Latinx | −0.03 | 0.05 | .49 |
| Asian | 0.004 | 0.08 | .95 |
| American Indian/Alaskan Native | −0.08 | 0.10 | .40 |
| Multiracial | 0.04 | 0.04 | .32 |
| Gay/lesbian | −0.01 | 0.03 | .83 |
| Queer, questioning, or another SM | −0.05 | 0.03 | .10 |
| Heterosexual | −0.13 | 0.07 | .07 |
| Prejudice events | 0.12* | 0.02 | <.01 |
| Expectations of rejection | 0.15* | 0.02 | <.01 |
| Pride (internalized transnegativity) | −0.03* | 0.01 | .02 |
| Outness (concealment) | −0.10* | 0.02 | <.01 |
| Anxiety symptoms (GAD-7) | |||
| Age | 0.03 | 0.02 | .18 |
| SSS | −0.03 | 0.02 | .09 |
| Transfeminine | −0.10 | 0.10 | .32 |
| Nonbinary (AFAB) | 0.13* | 0.05 | .02 |
| Nonbinary (AMAB) | 0.07 | 0.11 | .53 |
| Questioning | 0.22 | 0.12 | .06 |
| Black | 0.11 | 0.08 | .20 |
| Latinx | −0.15 | 0.08 | .08 |
| Asian | −0.06 | 0.14 | .63 |
| American Indian/Alaskan Native | 0.05 | 0.20 | .79 |
| Multiracial | −0.02 | 0.07 | .69 |
| Gay/lesbian | −0.07 | 0.06 | .27 |
| Queer, questioning, or another SM | −0.13* | 0.05 | .01 |
| Heterosexual | −0.11 | 0.13 | .39 |
| Prejudice events | 0.24* | 0.03 | <.01 |
| Expectations of rejection | 0.22* | 0.03 | <.01 |
| Pride (internalized transnegativity) | −0.01 | 0.02 | .59 |
| Outness (concealment) | −0.13* | 0.04 | <.01 |
Note.
p < .05. SM = sexual minority identity.
Nonbinary and questioning youth reported lower levels of GM prejudice events and expectations of rejection than transmasculine youth, and post hoc analyses indicated these groups reported lower levels of these stressors than transfeminine youth. Transmasculine youth reported lower levels of concealment than all other gender identity subgroups. Transmasculine youth also reported higher levels of internalized transnegativity than other subgroups with the exception of questioning youth, who reported higher levels than transmasculine youth. Black youth reported lower levels of GM prejudice events, expectations of rejection, and internalized transnegativity than White youth, and American Indian/Alaskan Native youth reported higher levels of GM prejudice events than White youth. Asian youth also reported lower levels of GM expectations of rejection and higher concealment than White youth. In the model predicting anxiety symptoms while controlling for all GM stressors and covariates, nonbinary youth AFAB reported higher levels of anxiety symptoms than transmasculine youth. See Supplementary Material F for a discussion of direct effects with respect to SSS and SM status. No other direct effects were found.
Indirect Effects in Structural Model
Transfeminine youth exhibited higher depressive and anxiety symptoms than transmasculine youth via higher levels of concealment. Both subgroups of nonbinary youth (AFAB and AMAB) exhibited higher depressive and anxiety symptoms via higher levels of concealment and lower levels of depressive and anxiety symptoms via lower levels of GM prejudice events and expectations of rejection. Nonbinary youth AMAB exhibited lower levels of depressive symptoms via lower levels of internalized transnegativity than transmasculine youth. Questioning youth exhibited higher levels of concealment and internalized transnegativity as well as lower levels of GM prejudice events and expectations of rejection compared to transmasculine youth. In turn, higher levels of concealment predicted higher depressive and anxiety symptoms. Higher levels of internalized transnegativity predicted higher levels of depressive symptoms, and lower GM prejudice events and expectations of rejection predicted lower depressive and anxiety symptoms. With regard to racial/ethnic subgroup indirect effects, Black youth exhibited lower depressive and anxiety symptoms via lower GM prejudice events and expectations of rejection than White youth. Asian youth exhibited higher levels of depressive and anxiety symptoms via higher concealment. No other indirect effects between racial/ethnic subgroup membership and mental health symptoms via GM stressors were detected. All indirect effects are reported in Table 3.
Table 3.
Indirect effects between sociodemographic identity variables, depressive symptoms, and anxiety symptoms through gender minority stressors.
| Indirect effect | Depressive symptoms (CES-D 10) | Anxiety symptoms (GAD-7) | ||
|---|---|---|---|---|
| Unstandardized estimates | 95% CI | Unstandardized estimates | 95% CI | |
| Through prejudice events | ||||
| Transmasculine | Reference group | - | Reference group | - |
| Transfeminine | 0.004 | −0.024 – 0.033 | 0.008 | −0.048 – 0.066 |
| Nonbinary (AFAB) | −0.055* | −0.079 – −0.034 | −0.111* | −0.153 – −0.076 |
| Nonbinary (AMAB) | −0.037* | −0.072 – −0.005 | −0.076* | −0.143 – −0.010 |
| Questioning | −0.082* | −0.121 – −0.046 | −0.166* | −0.234 – −0.100 |
| White | Reference group | - | Reference group | - |
| Black | −0.023* | −0.047 – −0.003 | −0.046* | −0.090 – −0.007 |
| Latinx | 0.002 | −0.020 – 0.025 | 0.004 | −0.041 – 0.050 |
| Asian | −0.012 | −0.044 – 0.021 | −0.024 | −0.089 – 0.041 |
| American Indian/Alaskan Native | 0.065 | 0.000 – 0.143 | 0.132 | −0.001 – 0.283 |
| Multiracial | 0.004 | −0.015 – 0.023 | 0.008 | −0.030 – 0.047 |
| Through expectations of rejection | ||||
| Transmasculine | Reference group | - | Reference group | - |
| Transfeminine | 0.014 | −0.015 – 0.042 | 0.020 | −0.021 – 0.060 |
| Nonbinary (AFAB) | −0.048* | −0.070 – −0.030 | −0.068* | −0.100 – −0.040 |
| Nonbinary (AMAB) | −0.057* | −0.104 – −0.015 | −0.080* | −0.150 – −0.021 |
| Questioning | −0.106* | −0.161 – −0.059 | −0.149* | −0.235 – −0.079 |
| White | Reference group | - | Reference group | - |
| Black | −0.036* | −0.072 – −0.006 | −0.051* | −0.103 – −0.008 |
| Latinx | 0.005 | −0.018 – 0.030 | 0.008 | −0.027 – 0.042 |
| Asian | −0.043 | −0.098 – 0.008 | −0.060 | −0.139 – 0.011 |
| American Indian/Alaskan Native | 0.016 | −0.059 – 0.086 | 0.022 | −0.085 – 0.121 |
| Multiracial | −0.006 | −0.029 – 0.015 | −0.009 | −0.041 – 0.021 |
| Through pride (internalized transnegativity) | ||||
| Transmasculine | Reference group | - | Reference group | - |
| Transfeminine | −0.009 | −0.021 – 0.000 | −0.004 | −0.020 – 0.010 |
| Nonbinary (AFAB) | −0.005 | −0.012 – 0.000 | −0.002 | −0.011 – 0.006 |
| Nonbinary (AMAB) | −0.013* | −0.029 – −0.001 | −0.006 | −0.029 – 0.015 |
| Questioning | 0.016* | 0.002 – 0.036 | 0.007 | −0.018 – −0.036 |
| White | Reference group | - | Reference group | - |
| Black | −0.007 | −0.017 – 0.000 | −0.003 | −0.013 – 0.008 |
| Latinx | −0.004 | −0.013 – 0.001 | −0.002 | −0.012 – 0.006 |
| Asian | −0.007 | −0.021 – 0.004 | −0.003 | −0.020 – 0.009 |
| American Indian/Alaskan Native | −0.002 | −0.017 – 0.010 | −0.001 | −0.014 – 0.009 |
| Multiracial | 0.000 | −0.005 – 0.006 | 0.000 | −0.004 – 0.005 |
| Through outness (concealment) | ||||
| Transmasculine | Reference group | - | Reference group | - |
| Transfeminine | 0.002* | 0.004 – 0.031 | 0.021* | 0.004 – 0.045 |
| Nonbinary (AFAB) | 0.043* | 0.020 – 0.076 | 0.057* | 0.020 – 0.096 |
| Nonbinary (AMAB) | 0.045* | 0.021 – 0.077 | 0.060* | 0.019 – 0.109 |
| Questioning | 0.096* | 0.048 – 0.149 | 0.127* | 0.044 – 0.216 |
| White | Reference group | - | Reference group | - |
| Black | 0.007 | −0.004 – 0.020 | 0.010 | −0.005 −0.029 |
| Latinx | 0.009 | 0.000 – 0.021 | 0.013 | 0.000 – 0.030 |
| Asian | 0.018* | 0.001–0.041 | 0.024* | 0.001 – 0.058 |
| American Indian/Alaskan Native | 0.008 | −0.012 – 0.030 | 0.010 | −0.017 – 0.043 |
| Multiracial | −0.003 | −0.012 – 0.005 | −0.004 | −0.017 – 0.007 |
Note.
p < .05
Discussion
The primary aim of our study was to examine the full minority stress model among a nationwide sample of GM adolescents for the first time (Brooks, 1981; Meyer 2003; Meyer 2010). We found that GM stressors were systematically associated with depressive and anxiety symptoms. Adolescents who reported higher GM prejudice events, expectations of rejection, internalized transnegativity, and concealment reported higher depressive symptoms. Similarly, each GM stressor, with the exception of internalized transnegativity, was significantly associated with anxiety symptoms. These results are in line with past evidence that GM stressors, when examined in isolation, are associated with psychopathology among SGM youth (Chodzen et al., 2019; Hunter et al., 2021; Veale et al., 2017; Wilson et al., 2016). Direct effects between GM stressors and mental health outcomes were significant in the context of the full model, highlighting that the different components of the minority stress model explain unique variance in depressive symptoms and anxiety. Thus, research that examines only one type of GM stressor, or aggregates across distinct stressors, may miss important contributors to GM adolescents’ mental health.
Differences Across Gender Identity
We observed significant differences in minority stress experiences and, in turn, mental health symptoms across GM youth of diverse gender identities. Although past work has been mixed (Lefevor et al., 2019; Poquiz et al., 2021; Sterzing et al., 2017), in the current study, transmasculine and transfeminine youth reported more GM prejudice events and GM expectations of rejection than nonbinary youth, and higher levels of these stressors were indirectly related to higher depressive and anxiety symptoms. This difference could be explained by a higher level of outness among transmasculine and transfeminine youth (Caba et al., 2022), leading them to experience more stigmatization earlier on. Meanwhile, nonbinary youth may be more likely to conceal their identity during adolescence and therefore may be more likely to be perceived as maintaining a gender expression consistent with their sex assigned at birth (Poquiz et al., 2021). Given higher cultural visibility of binary GM identities, it is also possible that transmasculine and transfeminine youth realize they are transgender at an earlier age, allowing for transition—and associated gender-related discrimination—at an earlier age. Thus, although transitioning earlier is associated with better mental health outcomes (dickey et al., 2022), it may also be associated with greater stigmatization during a developmental period where social acceptance is key to adjustment (Hatchel et al., 2019). Nevertheless, we found that youth AFAB who have nonbinary identities reported higher anxiety symptoms than youth AFAB who are transmasculine in multivariate analyses accounting for GM stressors, so it is possible that a psychosocial process outside of GM stressors is related to heightened anxiety symptoms among nonbinary youth AFAB. These disparities could be related to nonbinary-specific forms of minority stress, such as lower cultural visibility and the structural invalidation of nonbinary identities. More research is needed to determine the mechanisms of these disparities.
Transmasculine youth reported higher internalized transnegativity than nonbinary (AFAB and AMAB) and transfeminine youth and reported the lowest levels of concealment. If transmasculine youth are more likely to come out during adolescence, they might experience stigmatization earlier, which could increase their internalized transnegativity while still early in their gender development. Qualitative work with GM adults has similarly demonstrated that negative social messages can have a negative impact on one’s feelings about their gender (Rood et al., 2017b).
Youth in the current study who were questioning their gender identity reported the highest levels of internalized transnegativity across GM subgroups. To date, there has been a dearth of literature on youth who are questioning their gender identity. Nevertheless, the findings are intuitive—youth who are not sure of their GM identity may be more likely to report higher levels of negative internalized beliefs about transgender identities. Given the cross-sectional design of the current study, the opposite may be true: higher levels of internalized transnegativity may lead to less self-trust and self-efficacy around recognizing and affirming one’s GM identity. Because almost all transgender people were at one point questioning their identity, future longitudinal research should focus on how the process of moving from questioning to recognizing one’s gender identity affects GM youth’s mental health.
Differences Across Race/Ethnicity
Overall, results of the structural equation model were consistent across racial/ethnic identities, with some notable exceptions. First, significant direct and indirect effects were found for Black youth’s experiences of GM stressors, depressive symptoms, and anxiety symptoms. Compared to White GM youth, Black GM youth reported lower levels of GM prejudice events, expectations of rejection, and internalized transnegativity and also exhibited lower depressive and anxiety symptoms via these lower GM stressors. Prior research has identified factors that may promote resilience among Black youth, including that parents of Black youth provide racial socialization preparing them to cope with experiences of discrimination (Hughes et al., 2006; Neblett et al., 2012). Asian GM youth reported lower expectations of rejection and higher concealment of gender identity than White GM youth and exhibited lower depressive and anxiety symptoms via lower GM concealment compared to White youth. Higher levels of concealment—and thus opportunities to experience discrimination—among Asian GM youth may explain lower expectations of rejection. American Indian/Alaskan Native GM youth reported higher levels of GM prejudice events than White GM youth. These findings are supported by prior work indicating that American Indian/Alaskan Native GM adults are more likely to report elevated experiences of major discrimination than White GM adults (Miller & Grollman, 2015), and more frequent mental distress than White cisgender adults (Robertson et al., 2021). There were no other significant indirect effects for racial/ethnic differences in mental health via minority stressors.
Importantly, analyses in the present study used gender and racial/ethnic identity as proxies for unique, identity-dependent sociocultural experiences. In other words, identities do not cause minority stressors or mental health outcomes—differences in these experiences by gender and race/ethnicity are the result of a complex set of interpersonal and contextual factors, including stereotypes, stigma, and histories of oppression differentially affecting social groups (Lett et al., 2022). Addressing differences in psychological outcomes across social identity groups is a useful tool for understanding how these sociocultural forces manifest differently for youth with diverse intersecting marginalized identities. However, results from the present study should not be interpreted as indicating that gender or racial/ethnic identities directly cause mental health experiences.
Additionally, this study did not assess GM youth of color’s appraisal of stressors related to having a marginalized racial/ethnic identity and a marginalized gender identity. In addition to GM stressors, GM youth of color—and Black GM youth in particular—may be further impacted by racism-based stressors that are associated with depressive symptoms among adolescents of color (Carter et al., 2017). Mereish and colleagues (2022) found that subtle and intersectional forms of minority stress (factoring in youth’s intersectional racial/ethnic and gender identities) may increase risk for internalizing symptoms among SGM adolescents of color. Future research with GM youth of color should assess experiences of discrimination related to both gender identity and race/ethnicity to capture the full range of Black GM adolescents’ proximal and distal stressors and related mental health outcomes. Furthermore, protective factors among GM youth of color are an important avenue for future research.
Implications
Individual-Level Interventions
Despite their high risk for experiencing mental health symptoms during adolescence, almost no interventions have been developed to help GM youth cope with GM stressors. Only one study has evaluated such an intervention, finding that cognitive-behavioral approaches have the potential to improve depressive symptoms by increasing coping skills in the face of discrimination and stigmatization (Austin et al., 2018). Nevertheless, potentially promising treatments include those developed to decrease internalized transnegativity among GM adults (Israel et al., 2021) as well as treatments for decreasing mental health symptoms among GM youth in general, such as mindfulness-based (Iacono et al., 2022), Internet-based (Steinke et al., 2017), and parent-based interventions (Matsuno & Israel, 2021). Interventions specifically designed to augment the coping capacity of GM youth in the face of GM stressors could have the potential to reduce mental health symptoms in this vulnerable population.
Importantly, all treatments for GM youth must incorporate understandings of intersectionality to effectively support diverse GM populations. GM youth’s experiences are shaped by their social positionality as it relates to power, privilege, and oppression across race/ethnicity, gender identity and sexual orientation, class, and ability or disability, among other identity statuses. GM youth’s unique social positions result in benefits (e.g., resiliency) as well as risks. For example, SGM youth generally report lower rates of mental healthcare service utilization than heterosexual peers, and SM youth of color report more difficulty accessing mental health services than white peers (Cook et al, 2016; Macapagal et al., 2016). Marginalized youth may have difficulty accessing care due to structural barriers (Roulston et al., 2022) and experiences of heteronormativity or racism in therapy (Williams & Fish, 2017). Improving access to care could attenuate the potentially deleterious effects of minority stress among GM youth.
Structural Interventions
While mental health treatments can help individual GM adolescents cope with GM stressors, structural interventions can work to eradicate gender-based oppression and structural stigma that contribute to the GM stressors youth are exposed to, thereby potentially improving their mental health. Structural stigma refers to the societal norms (e.g., cisnormativity—or the expectation that all people are or ought to be cisgender) and institutional policies that limit access to resources among GM populations. GM youth consistently report experiencing high levels of structural stigma (Hatzenbuehler & Pachankis, 2016). The internalization of structural stigma by cisgender and GM individuals likely contributes to the perpetuation of prejudice events and related increased levels of expectations of rejection, internalized transnegativity, identity concealment, and health disparities for GM youth. For example, the recent onslaught of anti-transgender legislation targeting U.S. GM youth (e.g., the criminalization of gender-affirming medical care) may have a broad range of negative impacts for GM youth, including increased mental health symptoms, suicide risk, and internalized stigma (Abreu et al., 2022).
However, promising findings indicate that GM youth who experience gender-affirming support across multiple contexts (e.g., home, school, work) are less likely to experience negative mental health symptoms such as depressive symptomatology and suicidality (Russell et al., 2018). It is critical that GM youth receive protections and support that affirm their gender identity and expression through policy interventions that target educational, healthcare, and legal systems. For example, policies and practices that support and protect GM youth can include allowing name and gender changes on legal documentation, school files, and medical records. In school-based settings, policymakers and school personnel can enact and uphold non-discriminatory and anti-bullying policies that provide GM youth with equitable access to school facilities and resources (e.g., gender-affirming bathrooms, gender and sexuality alliances). Further, policymakers can support GM youth’s well-being in healthcare contexts by prohibiting discriminatory policies that ban or limit access to developmentally appropriate, gender-affirming healthcare. It is important to work directly with GM youth by centering their voices to elucidate the issues most relevant to them.
Limitations
The current study had several limitations. Importantly, the current study included a majority White sample (66.91%) and did not directly assess intersectional minority stressors (e.g., gendered racial discrimination) that are uniquely related to being a GM person of color. Future studies should assess minority stressors at the intersection of multiple axes of oppression (e.g., heterosexism, sexism, racism, classism) within GM and racial/ethnic communities. Our study also incorporated measures of internalized transnegativity and concealment that evidenced psychometric reliability and validity in this sample yet may not be perfect approximations of the constructs (Jackson & Mohr, 2016). Future work should focus on developing and validating scales to assess minority stress constructs among GM adolescents.
Second, all results were based on cross-sectional data, and caution should be taken when interpreting the directions of some associations within the SEM model. We have taken multiple steps to address these limitations within our SEM model, including using stationary variables as the “predictor” variables in our models, including gender identity and race and ethnicity. Prior research has shown that mediation analyses using cross-sectional data can produce biased parameter estimates when all three variables are changing over time, but this limitation does not apply when the “predictor” variable is constant over time (Maxwell & Cole, 2007). In addition, because our “predictor” variables were minority identities, these variables logically precede the occurrence of minority stress temporally. However, bidirectional effects or an opposite direction of effects cannot be ruled out between minority stress experiences and mental health symptoms. For example, youth reporting depressive symptoms might be more likely to report expectations of future rejection due to depressive cognitions and biases towards negative events. We tested an alternative model which provided evidence that our original model is a stronger fit to our observed data than this hypothesized alternative model. From a clinical perspective, clinicians should be cautious when attempting to restructure thoughts surrounding minority stressors so as to not invalidate GM youth’s lived experiences. Future studies of longitudinal cohorts should assess how minority stressors change over time and influence long-term mental health outcomes.
Furthermore, our limited findings related to indirect effects between racial/ethnic identity and mental health symptoms via GM stressors could be due to relatively low statistical power in some subgroups. Future studies with larger samples of GM youth of color are needed to determine the stability of these effects. Finally, and critically, future work is needed not only to understand the associations between intersectional minority stressors and internalizing symptoms, but also to explore racially/ethnically diverse GM adolescents’ resilience and resistance to experiences of oppression (Singh et al., 2014).
Conclusion
This is the first study to apply the minority stress model (Brooks, 1981; Meyer, 2003; Meyer, 2010) in a nationwide sample of GM adolescents. We found significant support for the minority stress model, as GM stressors were systematically associated with internalizing symptoms. Furthermore, our results suggest that some GM youth could be more vulnerable to mental health symptoms because they experience more GM stressors, although temporal precedence cannot be determined in this cross-sectional study. Future longitudinal studies should assess intersectional forms of minority stress among GM youth, and culturally informed individual and structural interventions should be developed to address minority stress among GM adolescents.
Supplementary Material
General Scientific Summary.
Gender minority youth are at heightened risk for depression and anxiety compared to cisgender peers. This study supports the theory that mental health symptoms among gender minority youth are associated with unique stressful experiences related to having a marginalized gender identity during adolescence. Risk for these stressful experiences and related mental health symptoms vary by gender identity and, to some extent, race/ethnicity.
Acknowledgments
We have no known conflicts of interest to disclose. These results were previously presented at the Association for Psychological Science 2022 Conference. The study (PRO18030522) received a waiver of parental consent from the University of Pittsburgh Human Research Protection Office. Due to the risk of deductive disclosure with the minoritized population studied, deidentified data are only available from the study team through a data sharing agreement. Primary analyses were conducted using Mplus (Muthén & Muthén, 2017), Version 8. Study analysis code is available from the authors upon request. This study was not preregistered. This material is based upon work supported by the National Science Foundation (NSF) Graduate Research Fellowship under Grant No. 1940700 awarded to Anne J. Maheux. Any opinion, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the NSF.
References
- Abreu RL, Sostre JP, Gonzalez KA, Lockett GM, Matsuno E, & Mosley DV (2022). Impact of gender-affirming care bans on transgender and gender diverse youth: Parental figures’ perspective. Journal of Family Psychology. Advance online publication. 10.1037/fam0000987cv [DOI] [PubMed] [Google Scholar]
- Anti-LGBTQ+ Bills in 2022. (2022). Human Rights Campaign. Retrieved September 10, 2020, from https://www.hrc.org/resources/state-maps/anti-lgbtq-bills-in-2022.
- Austin A, Craig SL, & D’Souza SA (2018). An AFFIRMative cognitive behavioral intervention for transgender youth: Preliminary effectiveness. Professional Psychology: Research and Practice, 49(1), 1–8. 10.1037/pro0000154 [DOI] [Google Scholar]
- Barbee H, Deal C, & Gonzales G (2022). Anti-transgender legislation—a public health concern for transgender youth. JAMA Pediatrics, 176(2), 125–126. 10.1001/jamapediatrics.2021.4483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becerra-Culqui TA, Liu Y, Nash R, Cromwell L, Flanders WD, Getahun D, Giammattei SV, Hunkeler EM, Lash TL, Millman A, Quinn VP, Robinson B, Roblin D, Sandberg DE, Silverberg MJ, Tangpricha V, & Goodman M (2018). Mental health of transgender and gender nonconforming youth compared with their peers. Pediatrics, 141(5). 10.1542/peds.2017-3845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostwick WB, Meyer I, Aranda F, Russell S, Hughes T, Birkett M, & Mustanski B (2014). Mental health and suicidality among racially/ethnically diverse sexual minority youths. American Journal of Public Health, 104(6), 1129–1136. 10.2105/AJPH.2013.301749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks VR (1981). Minority stress and lesbian women. Lexington Books. [Google Scholar]
- Buchanan NCT, & Wiklund LO (2020). Why clinical science must change or die: integrating intersectionality and social justice. Women and Therapy, 43(3–4), 309–329. 10.1080/02703149.2020.1729470 [DOI] [Google Scholar]
- Burton CM, Marshal MP, Chisolm DJ, Sucato GS, & Friedman MS (2013). Sexual minority-related victimization as a mediator of mental health disparities in sexual minority youth: A longitudinal analysis. Journal of Youth and Adolescence, 42(3), 394–402. 10.1007/s10964-012-9901-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caba AE, Mallory AB, Simon KA, Rathus T, & Watson RJ (2022). Complex outness patterns among sexual minority youth: A latent class analysis. Journal of Youth and Adolescence, 54, 746–765. 10.1007/s10964-022-01580-x [DOI] [PubMed] [Google Scholar]
- Calabrese SK, Meyer IH, Overstreet NM, Haile R, & Hansen NB (2015). Exploring discrimination and mental health disparities faced by Black sexual minority women using a minority stress framework. Psychology of Women Quarterly, 39(3), 287–304. 10.1177/0361684314560730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter RT, Lau MY, Johnson V, & Kirkinis K (2017). Racial discrimination and health outcomes among racial/ethnic minorities: A meta-analytic review. Journal of Multicultural Counseling and Development, 45(4), 232–259. 10.1002/jmcd.12076 [DOI] [Google Scholar]
- Chodzen G, Hidalgo MA, Chen D, & Garofalo R (2019). Minority stress factors associated with depression and anxiety among transgender and gender-nonconforming youth. Journal of Adolescent Health, 64(4), 467–471. 10.1016/j.jadohealth.2018.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cogan CM, Scholl JA, Lee JY, & Davis JL (2021). Potentially traumatic events and the association between gender minority stress and suicide risk in a gender-diverse sample. Journal of Traumatic Stress, 34, 977–984. 10.1002/jts.22728 [DOI] [PubMed] [Google Scholar]
- Cole ER (2009). Intersectionality and research in psychology. American Psychologist, 64(3), 170–180. 10.1037/a0014564 [DOI] [PubMed] [Google Scholar]
- Collins PH (2000). Gender, Black feminism, and Black political economy. The Annals of the American Academy of Political and Social Science, 568(1), 41–53. 10.1177/000271620056800105 [DOI] [Google Scholar]
- Cook B, Trinh NH, Li Z, Hou SS, & Progovac AM (2016). Trends in racial-ethnic disparities in access to mental health care, 2004–2012. Psychiatric Services, 68(1), 9–16. 10.1176/appi.ps.201500453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crenshaw K (1989). Demarginalizing the intersection of race and sex: A Black feminist critique of antidiscrimination doctrines, feminist theory, and antiracist politics. University of Chicago Legal Forum, 8, 139–167. [Google Scholar]
- dickey LM, Thomas K, Andert B, Ibarra N, & Budge SL (2022). The relationship between realization of transgender identity and transition processes with nonsuicidal self-injury in transgender populations. Psychiatry Research, 310, 114332. 10.1016/j.psychres.2021.114332 [DOI] [PubMed] [Google Scholar]
- Enders CK, & Bandalos DL (2001). The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling, 8(3), 430–457. 10.1207/S15328007SEM0803_5 [DOI] [Google Scholar]
- Everett BG, Steele SM, Matthews AK, & Hughes TL (2019). Gender, race, and minority stress among sexual minority women: An intersectional approach. Archives of Sexual Behavior, 48(5), 1505–1517. 10.1007/s10508-019-1421-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox KR, Choukas-Bradley S, Salk RH, Marshal MP, & Thoma BC (2020). mental health among sexual and gender minority adolescents: Examining interactions with race and ethnicity. Journal of Clinical and Counseling Psychology, 88(5), 402–415. 10.1037/ccp0000486.Mental [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritz MS, Taylor AB, & MacKinnon DP (2012). Explanation of two anomalous results in statistical mediation analysis. Multivariate Behavioral Research, 47(1), 61–87. 10.1080/00273171.2012.640596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fulginiti A, Rhoades H, Mamey MR, Klemmer C, Srivastava A, Weskamp G, & Goldbach JT (2021). Sexual minority stress, mental health symptoms, and suicidality among LGBTQ youth accessing crisis services. Journal of Youth and Adolescence, 50(5), 893–905. 10.1007/s10964-020-01354-3 [DOI] [PubMed] [Google Scholar]
- Garrison CZ, Addy CL, Jackson KL, McKeown RE, & Waller JL (1991). The CES-D as a screen for depression and other psychiatric disorders in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 30(4), 636–641. 10.1097/00004583-199107000-00017 [DOI] [PubMed] [Google Scholar]
- Goodman E, Adler NE, Kawachi I, Frazier AL, Huang B, & Colditz GA (2001). Adolescents’ perceptions of social status: development and evaluation of a new indicator. Pediatrics, 108(2), E31. 10.1542/peds.108.2.e31 [DOI] [PubMed] [Google Scholar]
- Grossman AH, Park JY, Frank JA, & Russell ST (2021). Parental responses to transgender and gender nonconforming youth: Associations with parent support, parental abuse, and youths’ psychological adjustment. Journal of Homosexuality, 68(8), 1260–1277. 10.1080/00918369.2019.1696103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman AH, Park JY, & Russell ST (2016). Transgender youth and suicidal behaviors: Applying the interpersonal psychological theory of suicide. Journal of Gay and Lesbian Mental Health, 20(4), 329–349. 10.1080/19359705.2016.1207581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatchel T, Valido A, De Pedro KT, Huang Y, & Espelage DL (2019). Minority stress among transgender adolescents: The role of peer victimization, school belonging, and ethnicity. Journal of Child and Family Studies, 28(9), 2467–2476. 10.1007/s10826-018-1168-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, & Pachankis JE (2016). Stigma and minority stress as social determinants of health among lesbian, gay, bisexual, and transgender youth: Research evidence and clinical implications. Pediatric Clinics of North America, 63(6), 985–997. 10.1016/j.pcl.2016.07.003 [DOI] [PubMed] [Google Scholar]
- Hendricks ML, & Testa RJ (2012). A conceptual framework for clinical work with transgender and gender nonconforming clients: An adaptation of the minority stress model. Professional Psychology: Research and Practice, 43(5), 460–467. 10.1037/a0029597 [DOI] [Google Scholar]
- Horne SG, McGinley M, Yel N, & Maroney MR (2022). The stench of bathroom bills and anti-transgender legislation: Anxiety and depression among transgender, nonbinary, and cisgender LGBQ people during a state referendum. Journal of Counseling Psychology, 69(1), 1–13. 10.1037/cou0000558 [DOI] [PubMed] [Google Scholar]
- Hughes D, Rodriguez J, Smith EP, Johnson DJ, Stevenson HC, & Spicer P (2006). Parents’ ethnic-racial socialization practices: A review of research and directions for future study. Developmental Psychology, 42(5), 747–770. 10.1037/0012-1649.42.5.747 [DOI] [PubMed] [Google Scholar]
- Hunter J, Butler C, & Cooper K (2021). Gender minority stress in trans and gender diverse adolescents and young people. Clinical Child Psychology and Psychiatry, 26(4), 1182–1195. 10.1177/13591045211033187 [DOI] [PubMed] [Google Scholar]
- Iacono G, Craig SL, Crowder R, Brennan DJ, & Loveland EK (2022). A qualitative study of the LGBTQ+ youth affirmative mindfulness program for sexual and gender minority youth. Mindfulness, 13(1), 222–237. 10.1007/s12671-021-01787-2 [DOI] [Google Scholar]
- Israel T, Choi AY, Lin YJ, Matsuno E, Goodman JA, Kary KG, & Merrill C. R. S.f (2021). Reducing internalized transnegativity: Randomized controlled trial of an online intervention. Psychology of Sexual Orientation and Gender Diversity, 8(4), 429–439. 10.1037/sgd0000447 [DOI] [Google Scholar]
- Jackson SD, & Mohr JJ (2016). Conceptualizing the closet: Differentiating stigma concealment and nondisclosure processes. Psychology of Sexual Orientation and Gender Diversity, 3(1), 80. 10.1037/sgd0000147 [DOI] [Google Scholar]
- Johns MM, Beltran O, Armstrong HL, Jayne PE, & Barrios LC (2018). Protective factors among transgender and gender variant youth: A systematic review by socioecological level. Journal of Primary Prevention, 39(3), 263–301. 10.1007/s10935-018-0508-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozee HB, Tylka TL, & Bauerband LA (2012). Measuring transgender individuals’ comfort with gender identity and appearance: Development and validation of the transgender congruence scale. Psychology of Women Quarterly, 36(2), 179–196. 10.1177/0361684312442161 [DOI] [Google Scholar]
- Lefevor GT, Boyd-Rogers CC, Sprague BM, & Janis RA (2019). Health disparities between genderqueer, transgender, and cisgender individuals: An extension of minority stress theory. Journal of Counseling Psychology, 66(4), 385–395. 10.1037/cou0000339 [DOI] [PubMed] [Google Scholar]
- Lett E, Asabor E, Beltrán S, Cannon AM, & Arah OA (2022). Conceptualizing, contextualizing, and operationalizing race in quantitative health sciences research. The Annals of Family Medicine, 20(2), 157–163. 10.1370/afm.2792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macapagal K, Bhatia R, & Greene GJ (2016). Differences in healthcare access, use, and experiences within a community sample of racially diverse lesbian, gay, bisexual, transgender, and questioning emerging adults. LGBT Health, 3(6), 434–442. 10.1089/lgbt.2015.0124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshal MP, Dermody SS, Cheong JW, Burton CM, Friedman MS, Aranda F, & Hughes TL (2013). Trajectories of depressive symptoms and suicidality among heterosexual and sexual minority youth. Journal of Youth and Adolescence, 42(8), 1243–1256. 10.1007/s10964-013-9970-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuno E, & Israel T (2021). The parent support program: Development and acceptability of an online intervention aimed at increasing supportive behaviors among parents of trans youth. Journal of GLBT Family Studies, 17(5), 413–431. 10.1080/1550428X.2020.1868369 [DOI] [Google Scholar]
- Maxwell SE, & Cole DA (2007). Bias in cross-sectional analyses of longitudinal mediation. Psychological Methods, 12(1), 23. [DOI] [PubMed] [Google Scholar]
- Mereish EH, Parra LA, Watson RJ, & Fish JN (2022). Subtle and intersectional minority stress and depressive symptoms among sexual and gender minority adolescents of color: Mediating role of self-esteem and sense of mastery. Prevention Science, 23, 142–153. 10.1007/s11121-021-01294-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. 10.1037/2329-0382.1.s.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH (2010). Identity, stress, and resilience in lesbians, gay men, and bisexuals of color. The Counseling Psychologist, 38(3), 442–454. 10.1177/0011000009351601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller LR, & Grollman EA (2015). The social costs of gender nonconformity for transgender adults: Implications for discrimination and health. Sociological Forum, 30(3), 809–831. 10.1111/socf.12193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr JJ, & Fassinger R (2000). Measuring dimensions of lesbian and gay male experience. Measurement and Evaluation in Counseling and Development, 33(2), 66–90. 10.1080/07481756.2000.12068999 [DOI] [Google Scholar]
- Mohr JJ, & Kendra MS (2011). Revision and extension of a multidimensional measure of sexual minority identity: The lesbian, gay, and bisexual identity scale. Journal of Counseling Psychology, 58(2), 234–245. 10.1037/a0022858 [DOI] [PubMed] [Google Scholar]
- Mossman SA, Luft MJ, Schroeder HK, Varney ST, Fleck DE, Barzman DH, Gilman R, Delbello MP, & Strawn JR (2017). The Generalized Anxiety Disorder 7-item (GAD-7) scale in adolescents with generalized anxiety disorder: Signal detection and validation. Annals of Clinical Psychiatry, 29(4), 227–234. [PMC free article] [PubMed] [Google Scholar]
- Muthén B, & Muthén L (2017). Mplus. In Handbook of Item Response Theory (pp. 507–518). Chapman and Hall/CRC. [Google Scholar]
- Neblett EW, Rivas-Drake D, & Umaña-Taylor AJ (2012). The promise of racial and ethnic protective factors in promoting ethnic minority youth development. Child Development Perspectives, 6(3), 295–303. 10.1111/j.1750-8606.2012.00239.x [DOI] [Google Scholar]
- Omrani A, Wakefield-Scurr J, Smith J, & Brown N (2019). Survey development for adolescents aged 11–16 years: A developmental science based guide. Adolescent Research Review, 4(4), 329–340. 10.1007/s40894-018-0089-0 [DOI] [Google Scholar]
- Poquiz JL, Coyne CA, Garofalo R, & Chen D (2021). Comparison of gender minority stress and resilience among transmasculine, transfeminine, and nonbinary adolescents and young adults. Journal of Adolescent Health, 68(3), 615–618. 10.1016/j.jadohealth.2020.06.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Priest N, Paradies Y, Trenerry B, Truong M, Karlsen S, & Kelly Y (2013). A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Social Science and Medicine, 95, 115–127. 10.1016/j.socscimed.2012.11.031 [DOI] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- Robertson L, Akré E-R, & Gonzales G (2021). Mental health disparities at the intersections of gender identity, race, and ethnicity. LGBT Health, 8(8), 526–535. 10.1089/lgbt.2020.0429 [DOI] [PubMed] [Google Scholar]
- Rood BA, Maroney MR, Puckett JA, Berman AK, Reisner SL, & Pantalone DW (2017a). Identity concealment in transgender adults: A qualitative assessment of minority stress and gender affirmation. American Journal of Orthopsychiatry, 87(6), 704–713. 10.1037/ort0000303 [DOI] [PubMed] [Google Scholar]
- Rood BA, Reisner SL, Puckett JA, Surace FI, Berman AK, & Pantalone DW (2017b). Internalized transphobia: Exploring perceptions of social messages in transgender and gender-nonconforming adults. International Journal of Transgenderism, 18(4), 411–426. 10.1080/15532739.2017.1329048 [DOI] [Google Scholar]
- Roulston C, McKetta S, Price M, Fox KR, & Schleider JL (2022). Structural correlates of mental health support access among sexual minority youth of color during COVID-19. Journal Of Clinical Child And Adolescent, 53, 1–10. 10.1080/15374416.2022.2034633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell ST, Pollitt AM, Li G, & Grossman AH (2018). Chosen name use is linked to reduced depressive symptoms, suicidal ideation, and suicidal behavior among transgender youth. Journal of Adolescent Health, 63(4), 503–505. 10.1016/j.jadohealth.2018.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh AA, Meng SE, & Hansen AW (2014). “I am my own gender”: Resilience strategies of trans youth. Journal of Counseling and Development, 92(2), 208–218. 10.1002/j.1556-6676.2014.00150.x [DOI] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, & Löwe B (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Steinke J, Root-Bowman M, Estabrook S, Levine DS, & Kantor LM (2017). Meeting the needs of sexual and gender minority youth: Formative research on potential digital health interventions. Journal of Adolescent Health, 60(5), 541–548. 10.1016/j.jadohealth.2016.11.023 [DOI] [PubMed] [Google Scholar]
- Sterzing PR, Ratliff GA, Gartner RE, McGeough BL, & Johnson KC (2017). Social ecological correlates of polyvictimization among a national sample of transgender, genderqueer, and cisgender sexual minority adolescents. Child Abuse and Neglect, 67, 1–12. 10.1016/j.chiabu.2017.02.017 [DOI] [PubMed] [Google Scholar]
- Stirling K, Toumbourou JW, & Rowland B (2015). Community factors influencing child and adolescent depression: A systematic review and meta-analysis. Australian and New Zealand Journal of Psychiatry, 49(10), 869–886. 10.1177/0004867415603129 [DOI] [PubMed] [Google Scholar]
- Swann G, Stephens J, Newcomb ME, & Whitton SW (2020). Effects of sexual/gender minority- and race-based enacted stigma on mental health and substance use in female assigned at birth sexual minority youth. Cultural Diversity & Ethnic Minority Psychology, 26(2), 239–249. 10.1037/cdp0000292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorne N, Witcomb GL, Nieder T, Nixon E, Yip A, & Arcelus J (2019). A comparison of mental health symptomatology and levels of social support in young treatment seeking transgender individuals who identify as binary and non-binary. International Journal of Transgenderism, 20(2–3), 241–250. 10.1080/15532739.2018.1452660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toomey RB, Huynh VW, Jones SK, Lee S, & Revels-Macalinao M (2017). Sexual minority youth of color: A content analysis and critical review of the literature. In Journal of Gay and Lesbian Mental Health, 21(1), 3–31 10.1080/19359705.2016.1217499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veale JF, Peter T, Travers R, & Saewyc EM (2017). Enacted stigma, mental health, and protective factors among transgender youth in Canada. Transgender Health, 2(1), 207–216. 10.1089/trgh.2017.0031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson RJ, Wheldon CW, & Russell ST (2015). How does sexual identity disclosure impact school experiences? Journal of LGBT Youth, 12(4), 385–396. 10.1080/19361653.2015.1077764 [DOI] [Google Scholar]
- Williams ND, & Fish JN (2020). The availability of LGBT-specific mental health and substance abuse treatment in the United States. Health Services Research, 55(6), 932–943. 10.1111/1475-6773.13559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson EC, Chen YH, Arayasirikul S, Raymond HF, & McFarland W (2016). The impact of discrimination on the mental health of trans*female youth and the protective effect of parental support. AIDS and Behavior, 20(10), 2203–2211. 10.1007/s10461-016-1409 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


