Abstract
Introduction
The Re-Evaluating the Inhibition of Stress Erosions (REVISE) Trial aims to determine the impact of the proton pump inhibitor pantoprazole compared with placebo on clinically important upper gastrointestinal (GI) bleeding in the intensive care unit (ICU), 90-day mortality and other endpoints in critically ill adults. The objective of this report is to describe the rationale, methodology, ethics and management of REVISE.
Methods and analysis
REVISE is an international, randomised, concealed, stratified, blinded parallel-group individual patient trial being conducted in ICUs in Canada, Australia, Saudi Arabia, UK, US, Kuwait, Pakistan and Brazil. Patients≥18 years old expected to remain invasively mechanically ventilated beyond the calendar day after enrolment are being randomised to either 40 mg pantoprazole intravenously or an identical placebo daily while mechanically ventilated in the ICU. The primary efficacy outcome is clinically important upper GI bleeding within 90 days of randomisation. The primary safety outcome is 90-day all-cause mortality. Secondary outcomes include rates of ventilator-associated pneumonia, Clostridioides difficile infection, new renal replacement therapy, ICU and hospital mortality, and patient-important GI bleeding. Tertiary outcomes are total red blood cells transfused, peak serum creatinine level in the ICU, and duration of mechanical ventilation, ICU and hospital stay. The sample size is 4800 patients; one interim analysis was conducted after 2400 patients had complete 90-day follow-up; the Data Monitoring Committee recommended continuing the trial.
Ethics and dissemination
All participating centres receive research ethics approval before initiation by hospital, region or country, including, but not limited to – Australia: Northern Sydney Local Health District Human Research Ethics Committee and Mater Misericordiae Ltd Human Research Ethics Committee; Brazil: Comissão Nacional de Ética em Pesquisa; Canada: Hamilton Integrated Research Ethics Board; Kuwait: Ministry of Health Standing Committee for Coordination of Health and Medical Research; Pakistan: Maroof Institutional Review Board; Saudi Arabia: Ministry of National Guard Health Affairs Institutional Review Board: United Kingdom: Hampshire B Research Ethics Committee; United States: Institutional Review Board of the Nebraska Medical Centre. The results of this trial will inform clinical practice and guidelines worldwide.
Trial registration number
Keywords: Clinical Trial, Gastroduodenal disease, Adult intensive & critical care, Adult gastroenterology, Bleeding disorders & coagulopathies
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This 4800-patient randomised clinical trial at low risk of bias will evaluate the effect of pantoprazole versus placebo on clinically important gastrointestinal bleeding (primary efficacy outcome), 90-day mortality (primary safety outcome) and other relevant endpoints.
Blinded to allocation, outcomes will be adjudicated (clinically important gastrointestinal bleeding), classified (ventilator-associated pneumonia) and validated (Clostridioides difficile infection severity).
Patient and family engagement in a mixed-method study will inform a novel secondary outcome of patient-important bleeding.
Patients not receiving invasive mechanical ventilation are excluded; trial results are not necessarily applicable to spontaneously breathing patients and those receiving non-invasive ventilation.
Enrolment of heterogenous patients in eight countries will enhance the generalisability of the findings.
Introduction
To prevent gastrointestinal (GI) bleeding from stress-induced ulceration during critical illness, physicians prescribe stress ulcer prophylaxis for over 70% of patients in the intensive care unit (ICU).1 However, more recently, clinicians have questioned the effect of acid suppression for seriously ill patients. The randomised clinical trials that first provided support for stress ulcer prophylaxis with acid-suppressing medications were conducted several decades ago, in an era characterised by different practices. Since then, concerns have emerged including that histamine-2-receptor antagonists (H2RAs) and proton pump inhibitors (PPIs), may increase the risk of pneumonia and Clostridioides difficile infection—two healthcare-associated infections that may confer greater morbidity, mortality and costs than upper GI bleeding.2
Two large trials recently rejuvenated interest in this topic.3 4 In October 2018, the Stress Ulcer Prevention in the ICU (SUPICU) trial3 randomised 3298 patients to pantoprazole or placebo and found no difference in the primary outcome of 90-day mortality, nor the secondary composite outcome (GI bleeding, pneumonia, C. difficile infection, and acute myocardial ischemia). Pantoprazole reduced GI bleeding rates (4.2% vs 2.5%, p=0.006); however, many of these bleeds did not result in hypotension, transfusion, endoscopy or other interventions. Subgroup analysis suggested that patients with higher illness severity receiving pantoprazole may have an increased risk of death at 90-day compared with those receiving placebo (relative risk (RR) 1.13; 95% CI 0.99 to 1.30, interaction p=0.05)—an effect not observed in less severely ill patients. Further misgivings about widespread PPI use were raised in January 2019 when a cluster crossover trial of 26 771 patients evaluating PPIs against the active comparator of H2RAs also suggested an increased risk of death in the most severely ill subgroup of patients receiving PPIs.4
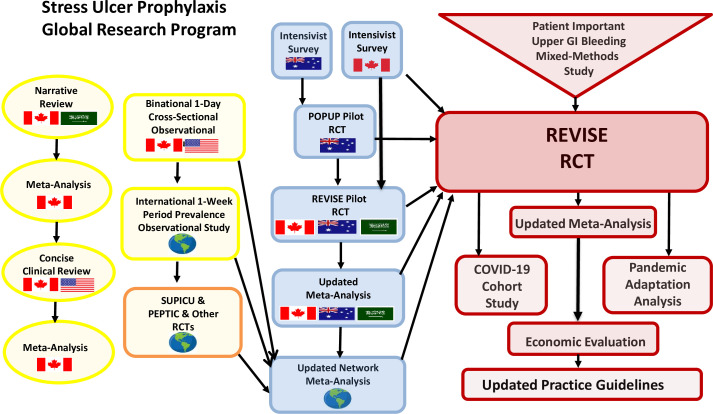
Building on prior studies through international collaboration,2 3 5–14 the Re-Evaluating the Inhibition of Stress Erosions (REVISE) Trial was developed. The objective is to determine the effect of pantoprazole versus placebo on the primary efficacy outcome (clinically important upper GI bleeding), and the primary safety outcome (90-day all-cause mortality).15 Secondary outcomes include ventilator-associated pneumonia (VAP), C. difficile infection, new renal replacement therapy (RRT), ICU and hospital mortality, and patient-important GI bleeding. The REVISE protocol was designed within the Stress Ulcer Prophylaxis Research Program (figure 1), in collaboration with the Canadian Critical Care Trials Group,16 Australian and New Zealand Intensive Care Society Clinical Trials Group17 and international colleagues (Protocol# CCT38473; Version 3.0, 10 April 2019).18
Figure 1.
Stress Ulcer Prophylaxis Research Program. In preparation for this trial, with national and international collaborators, we developed this stress ulcer prophylaxis research programme. We published several reviews and meta-analyses on acid suppression. We contributed to an international period prevalence epidemiological study which assisted with some Re-Evaluating the Inhibition of Stress Erosions (REVISE) trial estimates. We completed two surveys about stress ulcer prophylaxis in Australia and Canada. We completed two pilot randomised trials in preparation for REVISE. The 214-patient, single-centre Australian Pantoprazole versus Placebo for Stress Ulcer Prophylaxis (POP-UP) Pilot trial achieved three objectives related to exploring overt signals of benefit or harm, ascertaining whether the study drug could be administered promptly after commencing mechanical ventilation, and estimating relevant outcome event rates. A second 91-patient, international REVISE Pilot Trial achieved three feasibility objectives related to rates of recruitment, informed consent and protocol adherence. Other international studies provided key evidence to help inform the design of the main REVISE Trial. PEPTIC, Proton Pump Inhibitors vs Histamine-2-Receptor Blockers for Ulcer Prophylaxis Treatment in the Intensive Care Unit; RCT, randomized clinical trial; SUPICU, Stress Ulcer Prevention in the ICU.
Background and rationale
The current impact of PPIs for patients in the ICU is unclear. In the 4011 critically ill patients enrolled in seven randomised trials comparing PPI to no PPI, only 118 cases of clinically important bleeding, 565 cases of pneumonia and 48 cases of C. difficile were observed. Our updated network meta-analysis,14 using the Grading of Recommendations Assessment Development and Evaluation (GRADE) methodology,19 incorporating direct3 and indirect4 evidence further highlighted uncertainties regarding the net effect of PPIs across outcomes of mortality, pneumonia, C. difficile infections, and even—because of very small effects in lower-risk groups—GI bleeding. The certainty of evidence regarding GI bleeding reduction for three of four bleeding risk subgroups (low, high and highest risk) was moderate given the potential for risk of bias.20 All four risk groups shared the same relative effect estimate and credible interval (CrI) (RR 0.46, 95% CrI 0.29 to 0.66). For the moderate risk group, where the certainty of evidence was high, the CrI spanned a range from a 2.1% absolute reduction in bleeding to a 1.0% absolute reduction, illustrating imprecision and contributed to a low certainty evidence rating. Thus, the BMJ Rapid Recommendation initiative20 issued a weak recommendation against stress ulcer prophylaxis administration in patients at low bleeding risk of bleeding, and a weak recommendation for those at higher bleeding risk.
Regarding the risk of VAP (network RR 1.08, CrI 0.88 to 1.45) and of C. difficile infection (network RR 0.76, CrI 0.28 to 2.16), existing trials have failed to exclude important harm with PPIs. Regarding mortality, the network meta-analysis RR of 1.03 is consistent with a small increased risk of death with PPIs. Given the baseline mortality of ICU patients, the CrI of 0.93 to 1.14 includes an important mortality increase; for a baseline of 30%, a 14% relative increase would represent a 4.2% absolute increase. By adding REVISE results to the network meta-analysis, we hope to decrease imprecision of estimates, establishing an increased risk, or a trivial or no increase in mortality.
Based on these considerations, after grant funding and before launching the trial, protocol modifications were made to reflect the foregoing recent evidence. The trial was changed to a superiority design instead of a non-inferiority design. The primary safety outcome of mortality was included in response to subgroup analyses of earlier trials suggesting concern in patients at high-risk of death.21 22 The follow-up was extended from 60-day to 90-day mortality to better inform future meta-analyses. Patients and families were actively engaged in a study to refine the secondary endpoint of patient-important bleeding, outlined in the patient engagement section of this report.23 The sample size was increased from 3600 to 4800 patients, informed by the updated network meta-analysis.14 Relevant regulatory agencies, ethics boards and the Data Safety & Monitoring Committee reapproved the protocol. Enrolment began in July 2019.
Methods and analysis
Design
REVISE is a randomised, stratified, concealed, blinded, parallel-group trial.
Inclusion criteria
Adults≥18 years old receiving invasive mechanical ventilation.
Expected to remain mechanically ventilated beyond the calendar day after randomisation.
Exclusion criteria
Already invasively mechanically ventilated>72 hours during this hospital admission.
Acid suppression for active GI bleeding or high risk of bleeding (eg, current bleeding, peptic ulcer bleeding within 8 weeks, recent severe esophagitis, Barrett’s oesophagus, Zollinger-Ellison syndrome); (dyspepsia or gastroesophageal reflux is not an exclusion criterion).
Acid suppression in the ICU for>1 PPI or H2RA daily dose equivalent.
Dual antiplatelet therapy, or combined antiplatelet use and therapeutic anticoagulation.
Pantoprazole contraindication per local product information (in Australia: being treated with the HIV protease inhibitors atazanavir or nelfinavir, being treated with high-dose methotrexate (ie, >300 mg as part of a chemotherapy regimen), and documented cirrhosis or severe liver disease (eg, as indicated by an international normalised ratio>5.0 due to underlying liver disease); in Canada: being treated with rilpivirine or atazanavir, and patients who are hypersensitive to pantoprazole, substituted benzimidazoles, or to any ingredient in the formulation). Palliative care or anticipated withdrawal of life support.
Pregnancy.
Previous enrolment in REVISE, a related trial, or trial prohibiting coenrolment.
Patient, substitute decision-maker (SDM) or physician declines.
Informed consent
Research staff and investigators in the ICU screen patients for eligibility. Once eligibility is confirmed, the protocol allows either a priori informed consent or informed consent to continue. Consent encounters accord with guidelines.24 When not possible to obtain consent prior to randomisation, eligible patients are enrolled without prior consent (deferred consent). As soon as possible and appropriate thereafter, the patient or SDM is informed of the patient’s participation and offered the option to consent to continue or withdraw from the trial at any time. The patient or SDM may withdraw consent for receipt of study drug and/or for data collection. If withdrawal of study drug is requested, it is stopped and permission to use trial-related data is sought. Consent models and labels vary by region. In Canada and the UK, for those randomised under a deferred consent model, patients or SDMs can withdraw consent for continued participation whereas in Kuwait, they can opt out of continued participation. In some settings, telephone consent allows witnessed verbal a priori consent or consent to continue with signature confirmation as soon as possible. An example consent form approved by Clinical Trials Ontario is found in online supplemental appendix 1.
bmjopen-2023-075588supp001.pdf (337.9KB, pdf)
Randomisation
When notified by research staff or investigators about eligible patients, research pharmacists or designated unblinded staff not caring for patients use a password-protected website to access the central computerised randomisation programme to ensure concealed 1:1 allocation using randomly permuted variable unspecified block sizes. Randomisation is stratified by centre and prehospital acid suppression (ie, prior PPI or H2RA or not), generating start or no start, and continue or discontinue strata. The latter stratification will allow exploration of possible rebound hypersecretion of gastric acid on acid suppression termination25 and possible microbiome modification by long-term acid suppression which may modify infection risk.26
Interventions
Patients are randomly assigned to receive locally sourced intravenous pantoprazole 40 mg reconstituted with 0.9% sodium chloride (NaCl) or matched placebo (0.9% NaCl). Research pharmacists or designated unblinded staff prepare blinded placebo and study drug labelled per local regulations, dispensed to the ICU for daily bedside nurse administration.
The colour stability of reconstituted pantoprazole or placebo formulations from 5 companies up to 5 days without unblinding has been verified.27 These clear, colourless indistinguishable solutions are dispensed daily until 90 days after randomisation or until death, mechanical ventilation discontinuation, or clinically important GI bleeding.
When patients receive study drug, open-label PPI or H2RA use is documented and considered a protocol violation unless clinically indicated. Study drug continues regardless of feeding status.28–30 Study drug may be temporarily or permanently discontinued if a definite pantoprazole indication or contraindication develops. Regardless of study drug exposure, all patients are followed unless consent to follow-up is withdrawn. Study drug is restarted if invasive mechanical ventilation is reinstituted during the index ICU admission.
All other patient management during and following the trial is at the treating team’s discretion.
Risk of bias
To protect against selection bias, prognostic imbalance, detection, performance and measurement bias, loss to follow-up, missing data and other threats to validity, 18 strategies for trial conduct, analysis and dissemination phases were incorporated (table 1). Patients, families, clinicians and research personnel (staff, investigators and adjudicators) are blinded. The analyst and biostatisticians remain blinded until the main analysis is complete. Unblinding is not permitted other than in emergency situations, requiring Methods Center contact.
Table 1.
Strategies to minimise bias
| Stage and type of bias | Strategy implemented |
| Protocol development | |
| Design bias | Extensive international scientific, clinical and ethical input on the protocol; patient and family input to refine the patient-important bleeding outcome |
| Corporate conflicts of interest | Peer-review funded trial; locally sourced pantoprazole |
| Procedural bias | Standard operating procedures guide protocol implementation; central statistical monitoring is ongoing throughout the trial |
| Omission bias | Eligibility criteria are broad; enrolment is in five continents |
| Surveillance bias | Rigorous training of research personnel |
| Detection of ventilator-associated pneumonia (VAP) | To avoid biased choice of VAP definition: VAP reporting has one main and several alternate definitions |
| Protocol implementation | |
| Prognostic imbalance | At point of randomisation, patients are stratified for prehospital acid suppression which may influence outcomes |
| Selection bias | Allocation is concealed; research personnel screening, consenting, and enrolling patients are unaware of randomisation sequence |
| Detection and performance bias | Patients, families, all clinical and research personnel are blinded |
| Measurement bias | Primary efficacy outcome: Clinically important GI bleeding is centrally adjudicated by two physicians trained in study procedures, and blinded to allocation and centre |
| Loss to follow-up | Primary Safety Outcome: for 90-day mortality status, multiple methods used for patients discharged alive before 90 days; all other outcomes are hospital based as recorded in medical charts |
| Missing data | Each research record is reviewed and validated at least three times by Methods Center staff |
| Analysis | |
| False claims of benefit | A priori statistical approach is very conservative for stopping early for apparent benefit before full sample size reached |
| False claims of no difference | A priori statistical approach does not include stopping early for futility before full sample size reached |
| Confirmation bias | Analyst is blinded to allocation until after the final analysis |
| Analytic bias | Analysis will adhere to the intention-to-treat principle |
| Dissemination | |
| Reporting bias | Trial reporting will adhere to trial registration (NCT03374800), protocol and statistical analysis plan |
| Publication bias | Results will be disseminated through many knowledge translation strategies including peer-review journals |
These are the strategies we protocolised to minimise bias in four different phases of the trial.
Data collection
Research staff collect baseline data about the patients (eg, illness severity, comorbidities, prehospital acid suppression), and daily data up to 90 days post randomization while in the ICU. This includes advanced life supports received, key laboratory values (eg, haemoglobin, international normalised ratio (INR), platelet count); cointerventions (eg, enteral nutrition, anticoagulants, non-steroidal anti-inflammatory agents, corticosteroids), and relevant hospital reports (eg, endoscopy, radiology, surgery). Research staff follow patients daily to document study drug receipt or reasons for non-administration, while tracking trial outcomes as listed below. The duration of mechanical ventilation, ICU and hospital stay, and mortality are documented. Patients discharged alive from hospital before 90 days are followed for 90 days; vital status is obtained by patient, family or family physician contact, regional obituary or health-record review. No biological specimens are collected. The case report forms with additional details are found in online supplemental appendix 2.
bmjopen-2023-075588supp002.pdf (351.3KB, pdf)
Enrolled patients are assigned a unique numerical code. Enrolment logs with identifiers are retained at each site. Research pharmacists or designated unblinded staff not caring for patients enter study drug dispensing details into a secure web-based electronic data-capture system (iDataFax, Seattle, Washington). Blinded research staff upload clinical data without personal health information. An audit trail tracks any data modifications.
Primary outcomes
Primary efficacy outcome
Clinically important upper GI bleeding occurring in the ICU or resulting in ICU readmission during the index hospital stay up to 90-days post randomisation.
Clinically important GI bleeding requires the presence of overt GI bleeding, defined as one of the following:
Haematemesis.
Overt oro/nasogastric bleeding (frank blood or coffee-ground oro/nasogastric aspirate).
Melena.
Haematochezia.
Plus one of the following in the absence of other causes:
Haemodynamic change defined as a spontaneous decrease in mean arterial pressure or non-invasive systolic or diastolic blood pressure of >20 mm Hg, or an orthostatic increase in pulse rate of >20 beats/min and a decrease in systolic blood pressure of >10 mm Hg, with or without vasopressor initiation or increase.
Vasopressor initiation.
Haemoglobin decrease of >2 g/dL (20 g/L) within 24 hours of bleeding.
Transfusion of>2 units packed red blood cells within 24 hours of bleeding.
Therapeutic intervention (eg, therapeutic endoscopy, angioembolisation, surgery).
Our bleeding definition builds on prior studies,31 32 explicitly incorporating vasopressor initiation or increase3 and endoscopy. Research staff prospectively collect data related to GI bleeding, allowing central duplicate blinded adjudication, described below.
Primary safety outcome
All-cause mortality at 90 days post randomisation, ascertained by patient or SDM contact for those discharged alive before 90 days.
Secondary outcomes
Incidence of VAP: is diagnosed in patients who received invasive mechanical ventilation for >48 hours when there is a new, progressive or persistent radiographic infiltrate plus at least 2 of the following without other obvious cause: (1) fever (temperature >38°C) or hypothermia (temperature <36°C); (2) leucopenia (<4.0×106/L) or leucocytosis (>12.0×106 /L); (3) purulent sputum or (4) gas exchange deterioration.33 34 Research staff prospectively collect data allowing central classification by the Clinical Pulmonary Infection Score,35 and other definitions as below.
Incidence of C. difficile infection is defined as clinical features (diarrhoea (>3 episodes of unformed stools36 or Bristol type 6 or 737) ileus, or toxic megacolon) and either microbiological evidence of toxin-producing C. difficile or pseudomembranous colitis on colonoscopy38 in hospital within 90 days.
New RRT is defined as initiation of new RRT in the ICU.
ICU mortality is defined as all-cause mortality in the ICU during the index hospitalisation within 90 days.
Hospital mortality is defined as all-cause mortality during the index hospitalisation within 90 days.
Patient-important GI bleeding is focused on GI bleeding characteristics that are important to patients and families.23 The criteria will be derived from a mixed-method study involving interviews and focus groups of ICU survivors and family members not involved in REVISE, eliciting perspectives on concerning bleeding features for incorporation into the database to define this outcome.
Tertiary outcomes
Total units of red blood cells transfused in the ICU.
Peak serum creatinine level in the ICU.
Duration of mechanical ventilation (days).
ICU length of stay (days).
Hospital length of stay (days).
Central adjudication, classification and validation of morbidity outcomes
Clinically important GI bleeding
Research staff and investigators will identify all possible GI bleeding events, complete the bleeding case report form and submit redacted clinical notes, laboratory data and procedural reports. All GI bleeding events will be adjudicated by at least two investigators from of a 10-member GI bleeding adjudication committee to determine if the event meets the definition of clinically important GI bleeding and to confirm GI bleeding site. Initial calibration of the committee members will involve independent review by all 10 members (blinded to study drug and centre) case report forms and source data for the first 10 bleeding patients. Committee members will convene and discuss their assessments, clarify reasons for disagreements and arrive at consensus for each event. If consensus does not ensue, this process will be repeated until it does. Subsequent bleeding events will be independently adjudicated by one primary adjudicator (for all events) and a secondary adjudicator (randomly assigned, stratified by study drug). Adjudicators will be blinded to allocation and centre. Disagreements will resolve by discussion and consensus or a third researcher if necessary.
Ventilator-associated pneumonia
Local research staff and investigators will report any lower respiratory tract infections on the pneumonia outcome case report form. Data will be classified in duplicate by the Clinical Pulmonary Infection Score35 and other definitions (eg, American College of Chest Physicians,33 34 Centers for Disease Control,39 the International Sepsis Forum40) and by invasive microbiological confirmation.41 Disagreements will resolve by discussion and consensus or a third researcher if necessary.
In addition, early VAP is defined as arising on days 3, 4 or 5 after mechanical ventilation is initiated, and late VAP as arising on day 6 of mechanical ventilation or later, including up to 2 days after mechanical ventilation discontinuation.42 Pneumonia arising 3 or more days after mechanical ventilation discontinuation will be considered post extubation pneumonia. We do not report ventilator-associated conditions (VACs) or infection-related VACs, as surveillance metrics are modifiable by volume status and ventilator settings and do not reliably predict VAP.43
C. difficile infection
C. difficile outcome case report forms will be validated in duplicate by two researchers assessing severity (non-severe, severe, fulminant).38 Disagreements will resolve by discussion and consensus or a third researcher if necessary.
Trial process metrics
We will report informed consent rates and coenrolment rates, and any need for unblinding.
In terms of protocol adherence, we will report days of study drug exposure, and reasons for non-administration of study drug. Protocol deviations will include administration of open-label PPI or H2RA, missed doses of study drug, or dispensing the wrong study drug (eg, pantoprazole given instead of placebo or vice versa).
Patient and public involvement
Patients and families will be involved in several ways. We completed two pilot trials, documenting consent rates of 98.1%11 and 77.8%.12 Second, enrolled patients who regain capacity after critical illness are notified about the trial and approached for consent to continued participation. A mixed-method study eliciting perspectives of patients and families not involved in REVISE is refining the secondary outcome of patient-important bleeding.23 Fourth, in the UK, patients are involved at all stages as per the Health Research Authority standards44; patients reviewed the protocol, provided feedback and supported approval. When REVISE results are available, lay language summaries, visual abstracts and infographics will be created by patient partners for traditional media (paper, radio, television) and public social media feeds (X, blogs).
Sample size
The sample size of 4800 patients was chosen on the basis of plausible baseline risks of GI bleeding, plausible RR reductions, a target of 85% power and feasible enrolment. The best estimate of the GI bleeding event rate in the placebo arm ranging from 3% to 6% is based on the following: an international period-prevalence study (2.6%; 95% CI 1.6 to 3.6)1; the REVISE Pilot trial (placebo 6.1%; 95% CI 2.1 to 16.5)12; and the SUPICU trial placebo rate of 4.2%.3 The RR associated with pantoprazole was 0.6 in the SUPICU trial. Table 2 highlights sample size considerations for clinically important upper GI bleeding. The table presents combinations of RR reductions ranging from 30% to 50%, and baseline risks between 3% and 6% for which we will achieve 85% power. With a baseline risk of 3% and an RR reduction of 50%, the absolute benefit will be a 1.5% difference. Other highlighted cells correspond to absolute risk reduction of greater than 1.5%. In summary, across the range of plausible baseline risks, 4800 patients will provide at least 85% power to detect effects of pantoprazole as large as, or greater than, the smallest clinically important reduction in GI bleeding.
Table 2.
Sample size with respect to clinically important bleeding outcome
| True underlying relative risk (PPI vs placebo) | ||||
| 0.7 | 0.6 | 0.5 | ||
| Event rate in placebo group | 3% | 47.1% | 74.6% | 92.6% |
| 4% | 60.1% | 86.6% | 97.8% | |
| 5% | 70.7% | 93.4% | 99.4% | |
| 6% | 79.1% | 96.9% | 99.9% | |
This table highlights consideration for clinically important gastrointestinal (GI) bleeding. It presents combinations of relative risk reductions ranging from 30% to 50%, and baseline risks between 3% and 6% for which we will achieve 85% power. With a baseline risk of 3% and a relative risk reduction of 50%, the absolute benefit of will be a 1.5% difference. Other highlighted cells correspond to absolute risk reduction of greater than 1.5%. In summary, across the range of plausible baseline risks in the shaded boxes, 4800 patients will provide at least 85% power to detect effects of pantoprazole as large as, or greater than, this small important reduction in clinically important GI bleeding. This sample size reflects feasible enrolment in an acceptable 4-year time frame, accounting for any non-compliance or loss to follow-up, in the context of hybrid serial funding for Re-Evaluating the Inhibition of Stress Erosions.
PPI, proton pump inhibitor.
Table 3 highlights sample size implications for 90-day mortality. The estimates of RR are informed by SUPICU in which the upper confidence limit around the increased mortality in the high-risk group (using the illness severity metric of the Simplified Acute Physiology Score (SAPS) II>53) included a value of 1.30. Among the first 25% of patients enrolled, the mortality rate was 44% across both groups in the comparable high risk of death group of concern (using the illness severity metric of the Acute Physiology and Chronic Health Evaluation (APACHE) II score>25). Our power calculations are based on the estimated 40% of REVISE patients who will fall in the high-risk group (~1920 patients). The table presents combinations of RRs ranging from 1.1 to 1.3, and baseline risks between 4% and 38%, demonstrating power of >70% for combinations of higher levels of baseline risk and RR increase. The RR of 1.13 is the point estimate in patients with high illness severity in SUPICU.3 In summary, across the range of higher baseline risks, 4800 patients will provide at least 70% power to detect effects of pantoprazole at levels that would likely preclude use of pantoprazole in patients at higher risk of death.
Table 3.
Sample size with respect to 90-day mortality
| True underlying relative risk (PPI vs placebo) | |||||
| 1.1 | 1.13 | 1.2 | 1.3 | ||
| Event rate in placebo group | 38% | 38.0% | 57.9% | 91.5% | 99.9% |
| 40% | 40.9% | 61.7% | 93.7% | >99.9% | |
| 42% | 43.9% | 65.6% | 95.5% | >99.9% | |
| 44% | 47.1% | 69.4% | 96.9% | >99.9% | |
This table highlights sample size implications for 90-day mortality. The estimates of relative risk are informed by Stress Ulcer Prevention in the ICU (SUPICU) in which the upper confidence limit around the increased mortality in the high-risk group (SAPS II>53) included a value of 1.30. Among the first 25% of patients enrolled, the mortality rate was 44% across both groups in the comparable high-risk of death group of concern (APACHE II score>25). Our power calculations are based on the 40% of REVISE patients who will fall in the high-risk group (1920 patients). The table presents combinations of relative risks ranging from 1.1 to 1.3, and baseline risks between 38% and 44%, showing power of >70% for combinations of higher levels of baseline risk and relative risk increase. The relative risk of 1.13 is the observed point estimate in patients with high illness severity in the SUPICU Trial. In summary, across the range of higher baseline risks, 4800 patients will provide at least 70% power to detect effects of pantoprazole at levels that would preclude use of the drug in patients with high illness severity—those at higher risk of death.
APACHE, Acute Physiology and Chronic Health Evaluation; PPI, proton pump inhibitor; SAPS, Simplified Acute Physiology Score;
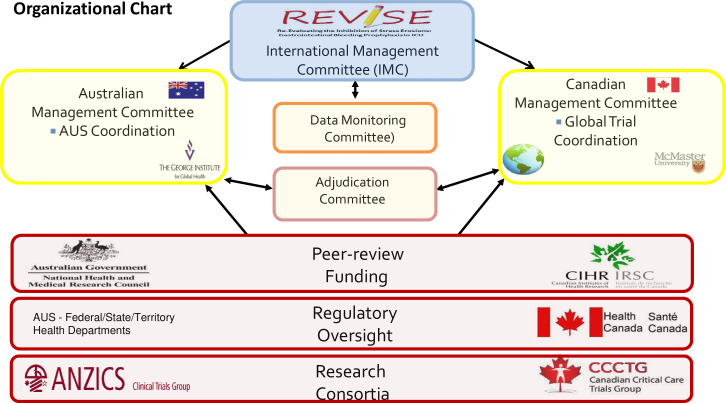
Trial management
Two methods centres with extensive experience running international clinical trials oversee REVISE, at McMaster University in Hamilton, Canada and The George Institute for Global Health in Sydney, Australia for Australian sites (figure 2). Methods centre teams meet at least twice monthly to harmonise approaches, track progress and share management efficiencies. Within Canada, the Québec Lead investigator ensures valid scientific cross-cultural, bilingual alignment with provincial ethical and regulatory directives. Methods centre personnel train local investigators and research staff on the protocol, ensure optimal conduct and validate all data at least thrice.
Figure 2.
Organisational chart. In this figure, we depict the organisation and management relationships for the international REVISE Trial.
Central statistical monitoring will occur twice annually at McMaster University. Site-specific data monitoring and auditing will follow national guidance.
On trial completion, original research records will be retained at participating sites in accordance with relevant regulations. Study drug will be destroyed per jurisdictional regulations. The database will be maintained for at least 15 years.
Statistical analysis
The main analyses will be conducted by analysing patients in the group to which they were allocated regardless of protocol adherence, per the intention-to-treat principle. We will compare the time to the primary and secondary binary outcomes using Cox proportional hazards regression with threshold p values of 0.05. Randomisation is stratified for centre and prehospital acid suppression. Because APACHE II score is strongly associated with mortality, to maximise statistical efficiency, we will also adjust for baseline APACHE II score for the mortality outcome. For binary outcomes, we will report HRs with 95% CIs as well as the absolute risk increase or decrease and 95% CIs. For continuous outcomes, we will use linear regression on the original scale or on the log-scale. Subgroup analyses will be conducted for the primary efficacy outcome and primary safety outcome in five a priori subgroup pairs: (1) prehospital acid suppression (PPIs or H2RAs) versus none, (2) illness severity per APACHE II score of>25 or <25, (3) medical versus surgical/trauma ICU admitting diagnosis, (4) SARS-CoV-2 positive versus negative status, and (5) female versus male.
Peer-review funding
Global enrolment in REVISE is supported by serial hybrid peer-review funding including three grants from the Canadian Institutes of Health Research, one of which is the Accelerating Clinical Trials Fund, and the Hamilton Academy of Health Sciences Organization. The National Health and Medical Research Council of Australia grant funds enrolment in Australia. REVISE was approved by the National Institute for Health Research in the UK supported by the Clinical Research Network. The funders have no role in the conception, design, conduct, oversight, analysis, interpretation, write-up, or approval of the manuscript, or decision to submit for publication.
Ethics and dissemination
Data monitoring committee
The independent REVISE Data Monitoring Committee (DMC) requested review of 90-day mortality results after 1200 patients were recruited (25% enrolment), recommending trial continuation. The formal interim analysis was conducted after 2400 patients (50% enrolment) had 90-day mortality ascertainment. To maintain the overall type-I error rate for the interim analysis, a Haybittle-Peto stopping rule with a critical value of 3 SD and fixed conservative α=0.001 was used.45 46 After examining recruitment, consent, coenrolment, protocol adherence and all trial outcomes, the DMC advised the Steering Committee to continue enrolment.
Ethics
Relevant Research Ethics Boards (REBs) and/or Human Research Ethics Committees of each participating hospital and/or region approved REVISE. These include: Australia: Northern Sydney Local Health District Human Research Ethics Committee and Mater Misericordiae Ltd Human Research Ethics Committee; Brazil: Comissão Nacional de Ética em Pesquisa; Canada: Hamilton Integrated Research Ethics Board; Kuwait: Ministry of Health Standing Committee for Coordination of Health and Medical Research; Pakistan: Maroof Institutional Review Board; Saudi Arabia: Ministry of National Guard Health Affairs Institutional Review Board: United Kingdom: Hampshire B Research Ethics Committee; United States: Institutional Review Board of the Nebraska Medical Center.
Protocol implementation and database training accords with the International Council for Harmonisation Guidelines for Good Clinical Practice and other locally applicable regulations.
Adverse events
Key adverse events and serious adverse events (SAEs) relevant to REVISE are already predefined primary or secondary trial outcomes. Beyond these events, ICU patients can develop many other complications due to critical illness or its treatment, which may be life threatening or fatal. However, they do not constitute adverse events or SAEs unless considered by the treating clinicians to possibly relate to the study drug. REVISE follows guidance for rational reporting of SAEs in investigator-initiated ICU trials of drugs in common use.47 The trial report will document all deaths and report only SAEs meeting the foregoing five published recommendations, regardless of local reporting requirements.
COVID-19 pandemic
After the pandemic was declared, REVISE paused for variable periods of time at each centre. We proposed ethical principles for concurrent conduct of research that is and is not pandemic-focused, whenever safe, feasible and locally approved.48 Relevant to patients with49 and without COVID-19, enrolment restarted as soon as possible without protocol modification, ensuring local research capacity, protocol fidelity and infection control.
Data deposition and curation
The dataset will be used for secondary observational studies addressing additional hypothesis-driven questions (eg, predictors of GI bleeding). Access for REVISE investigators will follow a submitted rationale, analysis plan and management committee approval. Requests for access to the dataset by external investigators will be considered following a submitted rationale, analysis plan and approval by the management committee and REBs, as relevant. Requirements will be stipulated in a prespecified data sharing agreement. Only deidentified data will be provided and will be transferred via a secure web portal.
Knowledge translation
REVISE will provide low risk-of-bias estimates that more than double trial evidence on the impact of pantoprazole on outcomes, increasing the strength of inferences regarding clinically important GI bleeding, mortality, VAP and C. difficile infection. REVISE will not provide direct evidence about pantoprazole’s effect on patients requiring non-invasive ventilation or no ventilatory support. Given contemporary critical care practice, we anticipate that a small proportion of enrolled patients will receive no enteral nutrition, such that inferences about this population may be limited.
We will publish the main results within 1 year of the last patient follow-up, presenting concurrently at an international congress. We will host videoconferences and regional rounds, and disseminate abstracts and slide-decks to local quality councils, provincial and state organisations, national policy makers and professional groups. Interested websites will feature multilingual REVISE results. Findings will be communicated through conventional academic channels (eg, abstracts, posters, peer-review manuscripts) and at professional fora (eg, grand rounds, teaching sessions, in-services, quality improvement councils). We will update our meta-analysis, and results will be incorporated into guidance documents such as BMJ Rapid Recommendations and Surviving Sepsis Guidelines.
Status
REVISE study was launched in response to multiprofessional stakeholder interests, serving public, professional and policy needs. As of 1 May 2023, 4124 patients have been recruited in 63 centres. Led by two seasoned research consortia, supported by the Canadian Community ICU Research Network,50 and energised by international collaborators, prevailing uncertainty about acid suppression has fuelled recruitment. By October 2023, 4800 patients are anticipated, with 90-day follow-up ascertained by January 2024.
REVISE readdresses the benefits, harms or disutility of acid suppression in invasively mechanically ventilated patients the ICU, aligned with the Declaration of Helsinki stating that ‘even the best-proven interventions’ must be continually re-evaluated through research for their safety, effectiveness, efficiency, accessibility and quality.51
Supplementary Material
Footnotes
Twitter: @icuresearch2, @LauzierFrancoi1, @naomihammond, @fengxie_mac
Correction notice: This article has been corrected since it was published. ORCID ids of few authors have been added. Online supplemental appendix 2 has been corrected.
Contributors: Concept and design: AAF, WA, YA, LB, MJC, DJC, AD, SE, SF, GG, RH, NH, MH, DH-A, MI, DJ, SK, FL, JCM, JMu, JMy, MO, AP, DR, GR, LS, LT, BV, FX, PY, NZ. Acquisition, analysis, or interpretation of data: DJC, NEH, MH, DH-A, SK, LS, LT, NZ. Drafting of the manuscript: DJC, AD, GG, MH, DH-A, FL, LT, PY, NZ. Critical revision of the manuscript for important intellectual content: AAA-F, WA, YA, LB, MJC, SE, SF, RH, NEH, MI, DJ, SK, JCM, JMu, JMy, MO, AP, DR, GR, LS, BV, FX. Statistical analysis: LB, DJC, SF, GG, DH-A, LT. Obtained funding: AAA-F, WA, YA, LB, MJC, DJC, AD, SE, SF, GG, RH, NEH, DH-A, DJ, SK, FL, JCM, JMu, JMy, MO, AP, DR, GR, LT, BV, PY, FX, NZ. Administrative, technical, or material support: WA, DJC, AD, SF, GG, NEH, MH, DH-A, SK, DR, LS, AP, LT, NZ. Data Integrity: DJC, MH, DH-A, SK, LS, NZ.
Funding: REVISE is funded by peer-reviewed grants (Canadian Institutes of Health Research 201610PJT-378226-PJT-CEBA-18373, Canadian Institutes of Health Research 202207CL3-492565-CTP-CEBA-19215), and the Canadian Institutes for Health Research Accelerating Clinical Trials Fund (ACT Consortium RFA-1 Application), as well as the Hamilton Academy of Health Sciences Organization (HAH-22-009), and funds from St. Joseph’s Healthcare Hamilton and McMaster University. The National Health and Medical Research Council of Australia grant (GNT1124675) funds enrolment in Australia. REVISE was approved by the National Institute for Health Research (NIHR) in the UK as a Portfolio Study (CPMS ID 45782), eligible for support from the NIHR Clinical Research Network (https://www.nihr.ac.uk/researchers/collaborations-services-and-support-for-your-research/run-your-study/crn-portfolio.htm). This trial received no support from the commercial or private sector. The funders/sponsors have no role in the conception, design, conduct, oversight, analysis, interpretation, write-up, review or approval of the manuscript, or decision to submit the manuscript for publication. Career Award Funding: WA holds a Mid-Career Award from the Department of Medicine at McMaster University. DJC holds a Research Chair in Knowledge Translation in Critical Care from the Canadian Institutes for Health Research. SE holds a National New Investigator Award from the Heart and Stroke Foundation of Canada. SF holds a Leadership Fellowship from the National Health and Medical Research Council of Australia. NEH holds an Emerging Leadership Fellowship from the National Health and Medical Research Council of Australia. FL is a recipient of a Research Career Award from the Fonds de la recherche du Québec-Santé. JCM holds the Unity Health Chair in Trauma Research. JMy holds a Leadership Fellowship from the National Health and Medical Research Council of Australia. BV holds a Leadership Fellowship from the National Health and Medical Research Council of Australia. PY holds a Clinical Research Practitioner Fellowship from the Health Research Council of New Zealand.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. Krag M, Perner A, Wetterslev J, et al. Prevalence and outcome of gastrointestinal bleeding and use of acid suppressants in acutely ill adult intensive care patients. Intensive Care Med 2015;41:833–45. 10.1007/s00134-015-3725-1 [DOI] [PubMed] [Google Scholar]
- 2. Cook DJ, Guyatt GH. Gastrointestinal bleeding prophylaxis for hospitalized patients. N Engl J Med 2018;378:2506–16. 10.1056/NEJMra1605507 [DOI] [PubMed] [Google Scholar]
- 3. Krag M, Marker S, Perner A, et al. Pantoprazole in patients at risk for gastrointestinal bleeding in the ICU. N Engl J Med 2018;379:2199–208. 10.1056/NEJMoa1714919 [DOI] [PubMed] [Google Scholar]
- 4. PEPTIC Investigators for the ANZICS-CTG . Effect of stress ulcer prophylaxis with PPIs vs H2RAs on In- hospital mortality among ICU patients. JAMA 2020. 10.1001/jama.2019.22190 [DOI] [Google Scholar]
- 5. Alhazzani W, Alenezi F, Jaeschke RZ, et al. Proton pump inhibitors versus Histamine-2-receptor antagonists for stress ulcer prophylaxis in critically ill patients: a systematic review and meta-analysis. Crit Care Med 2013;41:693–705. 10.1097/CCM.0b013e3182758734 [DOI] [PubMed] [Google Scholar]
- 6. Barletta JF, Kanji S, MacLaren R, et al. American-Canadian consortium for intensive care drug utilization (ACID) investigators. Pharmacoepidemiology of stress ulcer prophylaxis in the United States and Canada. J Crit Care 2014;29:955–60. 10.1016/j.jcrc.2014.06.025 [DOI] [PubMed] [Google Scholar]
- 7. Eastwood GM, Litton E, Bellomo R, et al. Opinions and practice of stress ulcer prophylaxis in Australian and New Zealand intensive care units. Crit Care Resusc 2014;16:170–4. 10.1016/S1441-2772(23)01468-0 [DOI] [PubMed] [Google Scholar]
- 8. Alshamsi F, Belley-Cote E, Cook D, et al. Efficacy and safety of proton pump inhibitors for stress ulcer prophylaxis in critically ill patients: a systematic review and meta-analysis of randomized trials. Crit Care 2016;20:120. 10.1186/s13054-016-1305-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Barletta J, Bruno JJ, Buckley MS, et al. Concise definitive review: stress ulcer prophylaxis. Crit Care Med 2016;44:1395–405. [DOI] [PubMed] [Google Scholar]
- 10. Shears M, Alhazzani W, Marshall JC, et al. Stress ulcer prophylaxis in critical illness: a national survey. Can J Anaesth 2016;63:718–24. 10.1007/s12630-016-0612-3 [DOI] [PubMed] [Google Scholar]
- 11. Selvanderan SP, Summers MJ, Finnis ME, et al. Pantoprazole or placebo for stress ulcer prophylaxis (POP-UP): randomized double-blind exploratory study. Crit Care Med 2016;44:1842–50. 10.1097/CCM.0000000000001819 [DOI] [PubMed] [Google Scholar]
- 12. Alhazzani W, Guyatt G, Alshahrani M, et al. Withholding pantoprazole for stress ulcer prophylaxis in critically ill patients: a pilot randomized clinical trial and meta-analysis. Crit Care Med 2017;45:1121–9. 10.1097/CCM.0000000000002461 [DOI] [PubMed] [Google Scholar]
- 13. Alhazzani W, Alshamsi F, Belley-Cote E, et al. Efficacy and safety of stress ulcer prophylaxis in critically ill patients: a network meta-analysis of randomized trials. Intensive Care Med 2018;44:1–11. 10.1007/s00134-017-5005-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wang Y, Ge L, Ye Z, et al. Efficacy and safety of gastrointestinal bleeding prophylaxis in critically ill patients: an updated systematic review and network meta-analysis of randomized trials. Intensive Care Med 2020;46:1987–2000. 10.1007/s00134-020-06209-w [DOI] [PubMed] [Google Scholar]
- 15. Clinicaltrials.gov registry . Re-evaluating the inhibition of stress Erosions in the ICU (REVISE). Available: https://www.clinicaltrials.gov/study/NCT03374800 [Accessed 1 May 2023].
- 16. The Canadian Critical Care Trials Group (CCCTG) . Available: http://www.CCCTG.ca [Accessed 1 May 2023].
- 17. The Australian and New Zealand Intensive Care Unit Clinical Trials Group (ANZICS-CTG) . Available: http://www.ANZICS.com [Accessed 1 May 2023].
- 18. Chan A-W, Tetzlaff JM, Altman DG, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med 2013;158:200–7. 10.7326/0003-4819-158-3-201302050-00583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924–6. 10.1136/bmj.39489.470347.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ye Z, Reintam Blaser A, Lytvyn L, et al. Gastrointestinal bleeding prophylaxis for critically ill patients: a clinical practice guideline. BMJ 2020:l6722. 10.1136/bmj.l6722 [DOI] [PubMed] [Google Scholar]
- 21. Barkun A, Bardou M. Proton-pump inhibitor prophylaxis in the ICU - benefits worth the risks. N Engl J Med 2018;379:2263–4. 10.1056/NEJMe1810021 [DOI] [PubMed] [Google Scholar]
- 22. Rice TW, Kripalani S, Lindsell CJ. Proton pump inhibitors vs histamine-2-receptor blockers for stress ulcer prophylaxis in critically ill patients: issues of Interpretability in pragmatic trials. JAMA 2020;323:611–3. 10.1001/jama.2019.22436 [DOI] [PubMed] [Google Scholar]
- 23. Cook DJ, Swinton M, Krewulak KD, et al. What counts as patient-important upper gastrointestinal bleeding in the ICU? A mixed-methods study protocol of patient and family perspectives. BMJ Open 2023;13:e070966. 10.1136/bmjopen-2022-070966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Smith OM, McDonald E, Zytaruk N, et al. Enhancing the informed consent process for critical care research: strategies from a thromboprophylaxis trial. Intensive Crit Care Nurs 2013;29:300–9. 10.1016/j.iccn.2013.04.006 [DOI] [PubMed] [Google Scholar]
- 25. Helgadottir H, Bjornsson ES. Problems associated with deprescribing of proton pump inhibitors. Int J Mol Sci 2019;20:5469. 10.3390/ijms20215469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Freedberg DE, Lebwohl B, Abrams JA. The impact of proton pump inhibitors on the human gastrointestinal microbiome. Clin Lab Med 2014;34:771–85. 10.1016/j.cll.2014.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Zytaruk N, Wallace C, Copland M, et al. Colour stability testing for Pantoprazole formulations: can blinding be maintained in a randomized trial? Canadian critical care forum 2017 abstracts. Can J Anaesthesia 2018;65. [Google Scholar]
- 28. Kazamias P, Kotzampassi K, Koufogiannis D, et al. Influence of enteral nutrition-induced splanchnic hyperemia on the septic origin of splanchnic ischemia. World J Surg 1998;22:6–11. 10.1007/s002689900341 [DOI] [PubMed] [Google Scholar]
- 29. Braga M, Gianotti L, Gentilini O, et al. Early postoperative enteral nutrition improves gut oxygenation and reduces costs compared with total parenteral nutrition. Crit Care Med 2001;29:242–8. 10.1097/00003246-200102000-00003 [DOI] [PubMed] [Google Scholar]
- 30. Ephgrave KS, Kleiman-Wexler RL, Adair CG. Enteral nutrients prevent stress ulceration and increase Intragastric volume. Crit Care Med 1990;18:621–4. 10.1097/00003246-199006000-00009 [DOI] [PubMed] [Google Scholar]
- 31. Cook DJ, Fuller HD, Guyatt GH, et al. Risk factors for gastrointestinal bleeding in critically ill patients. N Engl J Med 1994;330:377–81. 10.1056/NEJM199402103300601 [DOI] [PubMed] [Google Scholar]
- 32. Cook D, Guyatt G, Marshall J, et al. A comparison of sucralfate and ranitidine for prevention of upper gastrointestinal bleeding in patients requiring mechanical ventilation. N Engl J Med 1998;338:791–7. 10.1056/NEJM199803193381203 [DOI] [PubMed] [Google Scholar]
- 33. Grossman RF, Fein A. Evidence-based assessment of diagnostic tests for ventilator-associated pneumonia: executive summary. Chest 2000;117:177S–181S. 10.1378/chest.117.4_suppl_2.177s [DOI] [PubMed] [Google Scholar]
- 34. Morrow LE, Kollef MH, Casale TB. Probiotic prophylaxis of ventilator-associated pneumonia. Am J Respir Crit Care Med 2010;182:1058–64. 10.1164/rccm.200912-1853OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Pugin J, Auckenthaler R, Mili N, et al. Diagnosis of ventilator-associated pneumonia by bacteriologic analysis of bronchoscopic and nonbronchoscopic blind bronchoalveolar lavage fluid. Am Rev Respir Dis 1991;143:1121–9. 10.1164/ajrccm/143.5_Pt_1.1121 [DOI] [PubMed] [Google Scholar]
- 36. U.S. Department of Health and Human Services, National Institutes of Health . Diarrhea. n.d. Available: https://www.niddk.nih.gov/health-information/digestive-diseases/diarrhea
- 37. Lewis SJ, Heaton KW. Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol 1997;32:920–4. 10.3109/00365529709011203 [DOI] [PubMed] [Google Scholar]
- 38. McDonald LC, Gerding DN, Johnson S, et al. Clinical practice guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis 2018;66:e1–48. 10.1093/cid/cix1085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 2008;36:309–32. 10.1016/j.ajic.2008.03.002 [DOI] [PubMed] [Google Scholar]
- 40. Calandra T, Cohen J, International Sepsis Forum Definition of Infection in the ICU Consensus Conference . The international sepsis forum consensus conference on definitions of infection in the intensive care unit. Crit Care Med 2005;33:1538–48. 10.1097/01.ccm.0000168253.91200.83 [DOI] [PubMed] [Google Scholar]
- 41. Johnstone J, Meade MA, Lauzier F, et al. Effect of probiotics on ventilator-associated pneumonia in critically ill patients: a randomized trial. JAMA 2021;326:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Torres A, Niederman MS, Chastre J, et al. Summary of the international clinical guidelines for the management of hospital-acquired and ventilator-acquired pneumonia. ERJ Open Res 2018;4:00028-2018. 10.1183/23120541.00028-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Pouly O, Lecailtel S, Six S, et al. Accuracy of ventilator-associated events for the diagnosis of ventilator-associated lower respiratory tract infections. Ann Intensive Care 2020;10:6. 10.1186/s13613-020-0624-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Health Research Authority Standards for Public Involvement in Research, National Health Services, UK . Available: https://www.hra.nhs.uk/planning-and-improving-research/best-practice/public-involvement [Accessed 1 May 2023].
- 45. Haybittle JL. Repeated assessment of results in clinical trials of cancer treatment. Br J Radiol 1971;44:793–7. 10.1259/0007-1285-44-526-793 [DOI] [PubMed] [Google Scholar]
- 46. Peto R, Pike MC, Armitage P, et al. Design and analysis of randomized control trials requiring prolonged observations of each patient. Br J Cancer 1976;34:585–612. 10.1038/bjc.1976.220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Cook D, Lauzier F, Rocha MG, et al. Serious adverse events in academic critical care research. CMAJ 2008;178:1181–4. 10.1503/cmaj.071366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Cook DJ, Kho ME, Duan EH, et al. Principles guiding non-pandemic critical care research during a pandemic. Crit Care Med 2020;48:1403–10. 10.1097/CCM.0000000000004538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Lee SW, Ha EK, Yeniova AÖ, et al. Severe clinical outcomes of COVID-19 associated with PPIs: a nationwide cohort study with propensity score matching. Gut 2021;70:76–84. 10.1136/gutjnl-2020-322248 [DOI] [PubMed] [Google Scholar]
- 50. Gehrke P, Binnie A, Chan SPT, et al. Fostering community hospital research. CMAJ 2019;191:E962–6. 10.1503/cmaj.190055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. World Medical Association . Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 2013;310:2191–4. 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-075588supp001.pdf (337.9KB, pdf)
bmjopen-2023-075588supp002.pdf (351.3KB, pdf)