Abstract
Healthy sleep is essential for physical and mental health, and social wellbeing; however, across the globe, and particularly in developing countries, national public health agendas rarely consider sleep health. Sleep should be promoted as an essential pillar of health, equivalent to nutrition and physical activity. To improve sleep health across the globe, a focus on education and awareness, research, and targeted public health policies are needed. We recommend developing sleep health educational programmes and awareness campaigns; increasing, standardising, and centralising data on sleep quantity and quality in every country across the globe; and developing and implementing sleep health policies across sectors of society. Efforts are needed to ensure equity and inclusivity for all people, particularly those who are most socially and economically vulnerable, and historically excluded.
Introduction
WHO defines health as “a state of complete physical, mental and social wellbeing and not merely the absence of disease or infirmity”. Like nutrition and physical activity, sleep is also an essential pillar of health.1 Sleep is a complex neurobehavioural state involving widespread changes in the brain and systemic physiology. The depth, duration, continuity, and timing of sleep are regulated by the interaction of a homoeostatic process (the reflection of accumulated wakefulness), and the circadian system (an endogenous and self-sustaining 24 h rhythm that influences nearly all tissues, organs, and physiological systems, including those that govern cardiometabolic, immune, neurological, endocrine, and mental function).
Decades of research have investigated why we sleep. Today, we know that sleep is critical to numerous biological functions that optimise adaptation and function throughout the body, from genes to behaviour. Furthermore, environmental and social factors influence sleep and, together with biological factors, can affect multiple dimensions of sleep.2 Such dimensions of sleep include sleep duration, efficiency (ie, the percentage of consolidated vs fragmented sleep), timing, and regularity, and have been evaluated in relation to health outcomes both independently and in combination. Functional outcomes of sleep include alertness and sleepiness, quality and satisfaction, impairment at school or work, and impairment of interpersonal relationships. Despite major advances in our understanding of sleep, the importance of sleep health is still under-recognised by most national public health agendas and educational institutions (including research institutions) around the world. This Viewpoint presents a contemporary, evidence-based, urgent call to action to incorporate sleep health into global public health policies. Furthermore, we provide recommendations on strategies and approaches to enhance education, research, and the development of policies to improve sleep health in all populations, including those who have been historically excluded from such policies.
Global disparities in sleep data: sleep duration as an example
Sleep health influences every facet of human function and is essential to optimise cardiometabolic, immune, brain, and mental health. To illustrate how disturbed sleep is associated with a broad set of health outcomes, we present data on one important dimension of sleep health: sleep duration. To estimate the extent of global disparity in sleep health data, we examined published data as described in the appendix (pp 1–3). Results of our literature review of 194 WHO member states (figure) show that only 43 (22%) had collected and published population-level sleep duration data. The complete literature search by country can be found in the appendix (pp 4–28). This paucity of sleep duration data is in contrast to the abundance of global data for other health risk behaviours such as poor nutrition, physical inactivity, smoking, or alcohol consumption, which can be found on the WHO, Global Burden of Disease, and the US Centers for Disease Control and Prevention (CDC) websites. This discrepancy in data for health risk behaviours is especially concerning given that sleep deficiency is an established risk factor for numerous health outcomes.
Figure: Paucity of sleep duration data across the globe.
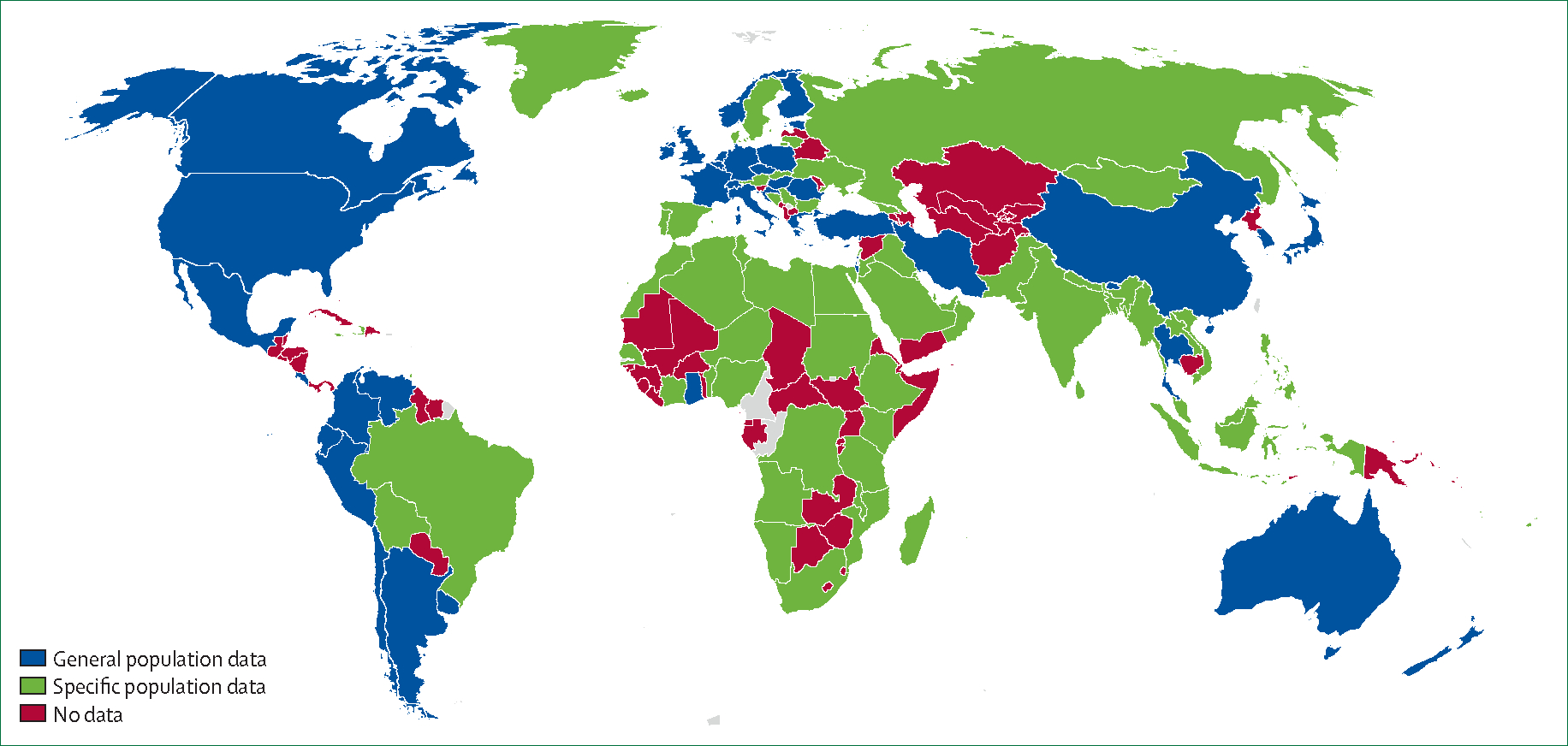
We did a literature search to determine which countries have data on sleep duration. Out of 194 WHO state members, 43 (22%) had general (blue) population data on sleep duration, 69 (36%) had sleep duration data in at least one specific (green) population (eg, lorry drivers or athletes), and the remaining 82 (42%) had no (red) sleep duration data. The disconcerting absence of general population sleep data in 78% of countries suggests that developing countries are unlikely to have sleep health on their national health agenda, despite being disproportionately affected by adverse environmental and social determinants of sleep health. This paucity of global data on sleep duration should serve as a wakeup call to national and international health organisations as such data are urgently needed to inform sleep health policies and practices that will not only improve population health but, possibly, impact health inequities. See appendix pp 4–28 for raw data.
Consequences of sleep deficiency are a threat to health
Healthy sleep allows us to enjoy good physical and mental health, and experience a general sense of wellbeing. The European Academy of Neurology3 and WHO have recognised sleep as a determinant of brain health,4 and the American Heart Association recently added sleep duration as one of Life’s Essential Eight factors for optimal cardiovascular health.5
Sleep deficiency, defined as insufficient sleep (eg, duration of sleep <6 h per night), sleep disturbances (eg, irregular sleep and nightmares), or sleep disorders (eg, insomnia, sleep apnoea, and restless legs syndrome), adversely affects health across the entire lifespan. First, children are particularly vulnerable to sleep deficiency6 that leads to behavioural problems7 early in life, and has been associated with sleep deficiency into adulthood.8 The appendix (p 29) provides sleep disturbance data among adolescents from the global school-based student health survey in 93 countries which shows an estimated average prevalence of 9·6%, ranging from 3·0% in Myanmar to 28·2% in Samoa (for data by country, see appendix pp 30–31). Second, insufficient sleep is associated with several adverse clinical consequences. Data from the CDC (appendix p 32) show that the prevalence of less than 7 h sleep per 24 h period overlaps with poor general health, poor mental health, poor brain health (ie, increased stroke), obesity, and high blood pressure. Lastly, sleep deficiency has been associated with allcause mortality9–11 with potential mechanisms related to telomere length12 and systemic inflammation.13 As experimental and within-person longitudinal observational studies continue to be conducted to determine causal relationships, it is crucial that we collect sleep data concurrently with nutrition, physical inactivity, smoking, and binge drinking data, and that we do so in all countries. Such an approach would be a crucial step towards achieving global health equity. We report references in this section by study type and level of evidence (appendix pp 33–35).
Economic burden
Sleep deficiency has economic costs related to its negative effects on health, wellbeing, safety, and productivity. Thus, disturbed sleep threatens not only global health but also the national health budget of every country across the globe. The economic toll of sleep deficiency can be expressed in terms of financial costs (eg, health care, workplace and motor vehicle accidents, productivity losses, forgone taxation revenue, and welfare payments) and non-financial costs (eg, loss of life quality and premature death). An analysis of the costs of inadequate sleep in the 2016–17 financial year in Australia estimated a total financial cost of US$17·9 billion (representing 1·6% of Australian gross domestic product) and a non-financial cost of $27·3 billion (representing 4·6% of the total Australian burden of disease for the year).14 Although most countries are still without comprehensive sleep health data, a 2017 study15 developed a model to forecast the effect of insufficient sleep on the economies of Canada, the USA, the UK, Germany, and Japan. The resultant financial loss was estimated to be $680 billion per year.
Cardiometabolic disorders
During sleep, the body replenishes and repairs itself through cell and tissue growth, while enhancing its ability to maintain energy balance.16 Insufficient sleep has been linked to increased risk of gestational diabetes,17 obesity,18 diabetes,19 coronary artery disease, and cardiovascular mortality.20 The loss of even 1 h of sleep during the transition to Daylight Saving Time is followed by a significant increase in risk of a heart attack over the next 3 days, which supports recommendations to adopt permanent standard time in countries that engage in clock changes, such as the USA.21,22 Furthermore, sleep disorders, such as obstructive sleep apnoea with severe nocturnal hypoxaemia, might increase risk of atrial fibrillation23 and mortality in heart failure,24 and are predictors of poor prognosis after myocardial infarction.25
The immune system, infections, and cancer
Sleep supports a healthy, balanced immune response,26 including the innate response,27 which is the first line of defence against bacteria and viruses.28 Sleep deficiency has been associated with impaired immune response to vaccinations,29 and increased risk of COVID-19,30 tuberculosis,31 and the common cold.32 Conversely, COVID-19,33 HIV,34 tuberculosis,35 and malaria36 can cause sleep deficiency. Furthermore, because the immune system has an important role in fighting cancer,37 sleep deprivation can lead to an impaired immune response that might result in increased cancer progression or mortality.38
Neurological disorders
Sleep is essential for memory consolidation39—a fundamental requirement for survival and high-level functioning.40 Sleep disturbances contribute to cognitive decline and increased risk of Alzheimer’s disease and related dementia,10 with potential mechanisms, including sleep insufficiency, that decrease clearance of amyloid β waste,41 possibly via an impaired glymphatic pathway.42 Furthermore, sleep disorders such as obstructive sleep apnoea and insomnia not only increase the risk of stroke and negatively affect outcomes, but also are highly prevalent in patients with stroke.43
Psychiatric and psychological disorders
Sleep is important in regulating emotions and maximising psychosocial wellbeing.44 Not only do underlying psychiatric disorders disrupt sleep, but sleep deficiency also increases the risk of anxiety disorders, major depression, post-traumatic stress disorder, bipolar disorder, substance use disorders, and suicide.45–49 In older people who are at risk of depression, cognitive behavioural therapy for insomnia might reduce the long-term incidence of depressive symptoms,50 suggesting that sleep deficiency might be causally related to subsequent mental health conditions.
Traffic and occupational accidents
Sleep disorders (eg, obstructive sleep apnoea,51 narcolepsy, and insomnia) and night-time shift work can make it difficult to maintain wakefulness under low-stimulation conditions, such as driving. Uncontrolled microsleeps while driving a vehicle might result in serious or fatal accidents.52,53 Furthermore, sleep deficiency can also result in slowed reaction times, impaired judgement, and cognitive impairment.54 Together, these deficits lead to suboptimal productivity54 and more accidents56,57 in the workplace.
COVID-19
Since the emergence of the COVID-19 pandemic, there has been an even more urgent need to examine sleep and circadian health, given their connection with COVID-19. Overall, the pandemic has had a negative effect on sleep health through various pathways, from increased anxiety and depression58 to disruptions in the circadian system and sleep patterns.59,60 A systematic review and meta-analysis61 that examined 493 475 participants from 49 countries between Nov 1, 2019, and July 15, 2021, reported a global prevalence of sleep disturbance at 40·49%, with the most affected groups being individuals with COVID-19, children, and adolescents. A large-scale study60 comprising 14 countries assessed sleep and daytime problems before and during the pandemic in 22 151 participants. Collectively, the prevalence of sleep and daytime problems increased by 10%. Importantly, COVID-19 itself did not account for this entire increase, with only 3% reporting having had COVID-19, whereas 42·2% faced confinement, and 55·9% faced financial hardships. Furthermore, a harmonised international survey62 comprising more than 22 330 adults from the general population, representing 13 countries, found a clinical insomnia prevalence of 36·7%, with 25·6% reporting probable anxiety, and 23·1% reporting probable depression. These findings of a relationship between mental ill health and COVID-19 are supported by an evaluation of data from a health insurance database in the USA,63 where the records of more than 17·2 million adults showed an increase in benzodiazepine receptor agonist hypnotics, selective serotonin reuptake inhibitors, and serotonin and norepinephrine reuptake inhibitors during the COVID-19 pandemic.
Sleep disturbances have emerged as an important feature in people with post-COVID-19 condition (also known as long COVID)64 that includes circadian rhythm disruptions.65 Additionally, SARS-CoV-2-positive participants were found to sleep 60·9 min longer than SARS-CoV-2-negative participants,66 and those with prolonged COVID-19 symptoms were more likely to have insomnia.67 The International COVID sleep study, involving 16 countries and 13 628 participants, revealed a high prevalence of fatigue (61·3%), insomnia symptoms (49·6%), and excessive daytime sleepiness (35·8%) among individuals with long COVID.68 Lastly, the COVID-19 pandemic disproportionately affected frontline health-care workers69 and minoritised racial and ethnic groups,70 further worsening global sleep health disparities.
Environmental and social determinants of sleep health disproportionately affect socioeconomically disadvantaged groups
Historically excluded groups are disproportionately affected by adverse environmental and social determinants of health—including sleep health—in both developing and developed countries.71 For example, minoritised racial and ethnic populations and those with lower socioeconomic status in the USA are more likely to have sleep deficiency.72 Across the globe, environmental determinants, such as perceived neighbourhood safety, objective neighbourhood characteristics (eg, degree of urbanisation), and screen time, have adverse effects on sleep.73 Furthermore, lower social class in Nigeria is predictive of shorter sleep duration in children.74 Thus, it is imperative that we address equity in sleep health across countries, groups (eg, women and children), individuals with lower socioeconomic status, minoritised racial and ethnic groups, and sexual minorities.
Environmental determinants
Sleep quantity and quality can be disrupted by many environmental factors (eg, light, temperature, noise, and air quality), each of which differentially affects socially disadvantaged groups. Relevant to planetary health, adverse physical and social environmental determinants related to climate change have been associated with short sleep duration and poorer sleep quality.75 Warmer night-time temperatures in particular have been shown to shorten sleep, with older people and residents of low-income countries (along with disadvantaged communities within high-income countries) already living in hotter climates being disproportionally affected.76 Consequences of environmental and social stress such as ecoanxiety (ie, the anxiety people experience related to current or future harm caused by climate change) can increase cortisol and norepinephrine, increase sympathetic nervous system activity, adversely affect sleep, and thereby increase the risk of myriad negative health outcomes.77
Social determinants
Sleep deficiency generally mirrors the level of social disadvantage or exclusion, and the social determinants of sleep health vary between and within countries or regions. For example, sleep deficiency might result from psychological stress, financial strain,72,78 modern tech nology (eg, video games or streaming services), hunger, or threat to safety. Another example is the increasing demand for a workforce that is available at all hours of the day or night, creating a cadre of night-shift workers with irregular sleep schedules and sleep deficiency.
Collectively, disadvantaged social and physical environments, combined with individual vulnerability, might have synergistic effects on economic costs. For example, a person with post-traumatic stress disorder might also have sleep deficiency and poor daytime functioning, and, consequently, increased workplace absenteeism and health-care use.79 Thus, improving sleep health could contribute to achieving overall health equity.80
Recommendations to promote sleep health across the globe
The health benefits of good sleep and the adverse consequences of sleep deficiency are abundantly clear. Although more global data will refine our knowledge base, we know enough to act now, leveraging better global sleep to achieve better global health. We recommend three concrete actions for local, regional, national, and international health organisations.
Educate: promote sleep and circadian health education and awareness
Transforming the worldview of sleep begins with education. Global efforts by numerous universities and professional organisations are already under way to actively promote sleep education and training. This commitment has contributed to 35 journals indexed in PubMed with sleep in the title; however, we need to go beyond this effort to increase access to care and treatment for sleep and circadian disorders. One step is the further integration of sleep health recommendations into medical specialties, as exemplified by the European Academy of Neurology and the American Heart Association. Another step is to develop sleep health curricula for primary and secondary education. The US National Institutes of Health has developed an electronic bookshelf where more than 135 books on sleep and circadian health can be translated and adapted for national and local contexts with global application, available via the World Sleep Society. Lastly, coordinated efforts involving international agencies (eg, WHO), national and international professional organisations, and local governments (eg, labour and transportation organisations) are essential to raise global awareness about sleep and circadian health. We must join public and population-based sleep health education and awareness campaigns, akin to what has been done for diet and nutrition or physical activity education.
Research: collect and centralise standard sleep and circadian data in every country
Effectively formulating sleep health policies tailored to national and regional contexts necessitates the collection of comprehensive global sleep and circadian data. Initial efforts might include collaboration with existing cohorts (eg, Burden of Obstructive Lung Disease81) and adding sleep duration and timing questions. In addition, including culturally appropriate sleep questionnaires (a list of widely used questionnaires can be found in the appendix pp 36–37) in existing population-based surveys could also promote this effort. We advise researchers, when selecting questions about sleep health, to consider questions that assess as many dimensions of sleep as possible (panel). Likewise, we recommend assessments of circadian preference, tendency, and timing. Standardising and centralising sleep and circadian data will not only enhance our knowledge and understanding of sleep but will also allow us to track and evaluate progress. Funding such data collection efforts would probably require and benefit from input and cooperation from professional sleep organisations and national and international health agencies.
Implement public health policies: include sleep health initiatives to advance public health agendas
Although sleep is relevant to all sectors of society, including housing, urban planning, and the labour market, it is essential to the UN’s Sustainable Development Goal 3 (Ensure healthy lives and promote wellbeing for all at all ages). Until sleep is recognised as a health priority by WHO, countries are less likely to include sleep in their national health agenda. National and international sleep societies also play a crucial advisory role in transforming how sleep is perceived, and the adoption of global strategies to collect appropriate sleep data. Bold recommendations are required for sleep to be prioritised as a pillar of health in agendas, policies, and practices. Finally, health equity must be a cross-cutting theme at the centre of all sleep-related public health initiatives across the globe.
Conclusion
Despite the strength of evidence showing that sleep has a critical influence on all aspects of human health, the importance of sleep health remains under-recognised globally. We call for action to enhance awareness and promote participation in the collection of crucial sleep data on a global scale. Such data are necessary to drive the implementation of sleep health policies that, in turn, will improve worldwide population health and help address health inequities.
Supplementary Material
Panel: Recommended sleep measurements.
Sleep can be measured by dimensions that characterise every individual, as well as by the presence of specific sleep disorders. We recommend, when possible, both sleep dimensions and sleep disorders be measured in national and global epidemiological assessments. Techniques for assessment include validated questionnaires (appendix pp 36–37), a sleep history, and wearables and nearables. We also recommend, when possible, studies of sleep health and sleep disorders measure functional consequences as outcome measures.
Dimensions of sleep
Sleep duration
Efficiency (consolidated vs fragmented sleep)
Timing
Regularity
Sleep quality or satisfaction
Sleep disorders
Insomnia
Sleep-related breathing disorders (eg, obstructive sleep apnoea)
Hypersomnia (eg, narcolepsy)
Sleep-related movement disorders (eg, restless legs syndrome)
Circadian rhythm sleep–wake disorders (eg, shift work sleep disorder)
Parasomnia (eg, rapid eye movement behaviour disorder)
Functional consequences of sleep
Sleepiness and alertness
Quality of life
Impairment at work or school
Impaired interpersonal function
Acknowledgments
We thank Allan O’Bryan, Lindsay Jesteadt, and Michael Mutschelknaus from the World Sleep Society for their support. This Viewpoint uses data from the GSHS. GSHS is supported by WHO and the CDC. We thank the CDC for allowing us to use their national interactive data. We acknowledge funding by the National Institutes of Health (NIH)1R01HL142981-01A1 and VA BLRD 1I01BX004872-01 (to DCL), (NIH)R01HL160619 (to VKS), (NIH)R01HL140580, (NIH)P01AG011412, (NIH)R01HD097786, and (NIH)R01AG068579 (to PCZ); and by the Intramural Program at the NIH, National Institute of Environmental Health Sciences (Z1A ES103325) and by the Intramural Research Program of the NIH, National Institute on Minority Health and Health Disparities (to CLJ). FH was supported by the National Natural Science Foundation of China (NSFC 82020108001). YAM was supported by The National Health and Medical Research Council of Australia Investigator Grant (2009776) and Jack Brockhoff Foundation (outside of this work). CMM is supported by grants from the Canadian Institutes of Health Research (483689, 483692, and 148410). The funders had no role in this Viewpoint.
Declaration of interests
DCL serves on the scientific advisory board for Apnimed. CMM has received research grants from Eisai, Idorsia, and Lallemand Health; and is a scientific advisory board member and consultant for Eisai and Idorsia. VKS is a consultant for Jazz, Apnimed, Bayer, Lilly, Zoll, and Huxley; and is a scientific advisory board member for Sleep Number. PCZ is a consultant for Eisai, Idorsia, Harmony Bioscience, Jazz, Sleep Number, and CVS Caremark; and serves as President of the World Sleep Society. PRE is a consultant for Invicta Medical. All other authors declare no competing interests.
Contributor Information
Diane C Lim, Miami Veterans Affairs, Healthcare System, Miami, FL, USA; Division of Pulmonary, Critical Care and Sleep Medicine, University of Miami, Miami, FL, USA.
Arezu Najafi, Occupational Sleep Research Center, Baharloo Hospital, Tehran University of Medical Sciences, Tehran, Iran; Sleep Breathing Disorders Research Center, Tehran University of Medical Sciences, Tehran, Iran.
Lamia Afifi, Clinical Neurophysiology Unit, School of Medicine, Cairo University Hospitals, Cairo, Egypt.
Claudio LA Bassetti, Department of Neurology, Inselspital, University of Bern, Bern, Switzerland.
Daniel J Buysse, Center for Sleep and Circadian Science, Department of Psychiatry, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA.
Fang Han, Department of Sleep Medicine, Peking University People’s Hospital, Beijing, China.
Birgit Högl, Department of Neurology, Medical University of Innsbruck, Innsbruck, Austria.
Yohannes Adama Melaku, Flinders Health and Medical Research Institute: Sleep Health, College of Medicine and Public Health, Flinders University, Adelaide, SA, Australia; Cancer Epidemiology Division, Cancer Council Victoria, Melbourne, VIC, Australia.
Charles M Morin, Department of Psychology, and CERVO Brain Research Center, Université Laval, Quebec City, QC, Canada.
Allan I Pack, Sleep Division, Department of Medicine, University of Pennsylvania, Philadelphia, PA, USA.
Dalva Poyares, Psychobiology Department, Sleep Medicine Division, Universidade Federal de São Paulo, São Paulo, Brazil.
Virend K Somers, Department of Cardiovascular Medicine, Mayo Clinic, Rochester, MN, USA.
Peter R Eastwood, Health Futures Institute, Murdoch University, Perth, WA, Australia.
Phyllis C Zee, Division of Sleep Medicine, Center for Circadian and Sleep Medicine, Department of Neurology, Feinberg School of Medicine, Northwestern University, Chicago, IL, USA.
Chandra L Jackson, Epidemiology Branch, National Institute of Environmental Health Sciences, National Institutes of Health, US Department of Health and Human Services, Research Triangle Park, NC, USA; Division of Intramural Research, National Institute on Minority Health and Health Disparities, National Institutes of Health, US Department of Health and Human Services, Bethesda, MD, USA.
References
- 1.Cassidy S, Chau JY, Catt M, Bauman A, Trenell MI. Cross-sectional study of diet, physical activity, television viewing and sleep duration in 233,110 adults from the UK Biobank; the behavioural phenotype of cardiovascular disease and type 2 diabetes. BMJ Open 2016; 6: e010038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Buysse DJ. Sleep health: can we define it? Does it matter? Sleep 2014; 37: 9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bassetti CLA, Endres M, Sander A, et al. The European Academy of Neurology Brain Health Strategy: one brain, one life, one approach. Eur J Neurol 2022; 29: 2559–66. [DOI] [PubMed] [Google Scholar]
- 4.WHO. Optimizing brain health across the life course: WHO position paper. Aug 9, 2022. https://www.who.int/publications/i/item/9789240054561 (accessed Sept 1, 2023).
- 5.Lloyd-Jones DM, Ning H, Labarthe D, et al. Status of cardiovascular health in US adults and children using the American Heart Association’s new “Life’s Essential 8” metrics: prevalence estimates from the National Health and Nutrition Examination Survey (NHANES), 2013 through 2018. Circulation 2022; 146: 822–35. [DOI] [PubMed] [Google Scholar]
- 6.Kajeepeta S, Gelaye B, Jackson CL, Williams MA. Adverse childhood experiences are associated with adult sleep disorders: a systematic review. Sleep Med 2015; 16: 320–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Melaku YA, Appleton S, Reynolds AC, et al. Association between childhood behavioral problems and insomnia symptoms in adulthood. JAMA Netw Open 2019; 2: e1910861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McWhorter KL, Parks CG, D’Aloisio AA, Rojo-Wissar DM, Sandler DP, Jackson CL. Traumatic childhood experiences and multiple dimensions of poor sleep among adult women. Sleep 2019; 42: zsz108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Omichi C, Koyama T, Kadotani H, et al. Irregular sleep and allcause mortality: a large prospective cohort study. Sleep Health 2022; 8: 678–83. [DOI] [PubMed] [Google Scholar]
- 10.Robbins R, Quan SF, Weaver MD, Bormes G, Barger LK, Czeisler CA. Examining sleep deficiency and disturbance and their risk for incident dementia and all-cause mortality in older adults across 5 years in the United States. Aging 2021; 13: 3254–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang YH, Wang J, Chen SH, et al. Association of longitudinal patterns of habitual sleep duration with risk of cardiovascular events and all-cause mortality. JAMA Netw Open 2020; 3: e205246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tempaku P, Hirotsu C, Mazzotti D, et al. Long sleep duration, insomnia, and insomnia with short objective sleep duration are independently associated with short telomere length. J Clin Sleep Med 2018; 14: 2037–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Irwin MR, Olmstead R, Carroll JE. Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiatry 2016; 80: 40–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hillman D, Mitchell S, Streatfeild J, Burns C, Bruck D, Pezzullo L. The economic cost of inadequate sleep. Sleep 2018; 41: zsy083. [DOI] [PubMed] [Google Scholar]
- 15.Hafner M, Stepanek M, Taylor J, Troxel WM, van Stolk C. Why sleep matters-the economic costs of insufficient sleep: a crosscountry comparative analysis. Rand Health Q 2017; 6: 11. [PMC free article] [PubMed] [Google Scholar]
- 16.Min S, Masanovic B, Bu T, et al. The association between regular physical exercise, sleep patterns, fasting, and autophagy for healthy longevity and well-being: a narrative review. Front Psychol 2021; 12: 803421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Facco FL, Grobman WA, Reid KJ, et al. Objectively measured short sleep duration and later sleep midpoint in pregnancy are associated with a higher risk of gestational diabetes. Am J Obstet Gynecol 2017; 217: 447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Covassin N, Singh P, Somers VK. Keeping up with the clock: circadian disruption and obesity risk. Hypertension 2016; 68: 1081–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Itani O, Jike M, Watanabe N, Kaneita Y. Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep Med 2017; 32: 246–56. [DOI] [PubMed] [Google Scholar]
- 20.Covassin N, Singh P. Sleep duration and cardiovascular disease risk: epidemiologic and experimental evidence. Sleep Med Clin 2016; 11: 81–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Janszky I, Ljung R. Shifts to and from daylight saving time and incidence of myocardial infarction. N Engl J Med 2008; 359: 1966–68. [DOI] [PubMed] [Google Scholar]
- 22.Malow BA. It is time to abolish the clock change and adopt permanent standard time in the United States: a Sleep Research Society position statement. Sleep 2022; 45: zsac236. [DOI] [PubMed] [Google Scholar]
- 23.Blanchard M, Gerves-Pinquie C, Feuilloy M, et al. Association of nocturnal hypoxemia and pulse rate variability with incident atrial fibrillation in patients investigated for obstructive sleep apnea. Ann Am Thorac Soc 2021; 18: 1043–51. [DOI] [PubMed] [Google Scholar]
- 24.Oldenburg O, Wellmann B, Buchholz A, et al. Nocturnal hypoxaemia is associated with increased mortality in stable heart failure patients. Eur Heart J 2016; 37: 1695–703. [DOI] [PubMed] [Google Scholar]
- 25.Xie J, Sert Kuniyoshi FH, Covassin N, et al. Nocturnal hypoxemia due to obstructive sleep apnea is an independent predictor of poor prognosis after myocardial infarction. J Am Heart Assoc 2016; 5: e003162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zee PC, Turek FW. Sleep and health: everywhere and in both directions. Arch Intern Med 2006; 166: 1686–88. [DOI] [PubMed] [Google Scholar]
- 27.De Lorenzo BH, de Oliveira Marchioro L, Greco CR, Suchecki D. Sleep-deprivation reduces NK cell number and function mediated by β-adrenergic signalling. Psychoneuroendocrinology 2015; 57: 134–43. [DOI] [PubMed] [Google Scholar]
- 28.Haspel JA, Anafi R, Brown MK, et al. Perfect timing: circadian rhythms, sleep, and immunity - an NIH workshop summary. JCI Insight 2020; 5: e131487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schmitz NCM, van der Werf YD, Lammers-van der Holst HM. The importance of sleep and circadian rhythms for vaccination success and susceptibility to viral infections. Clocks Sleep 2022; 4: 66–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huang B, Niu Y, Zhao W, Bao P, Li D. Reduced sleep in the week prior to diagnosis of COVID-19 is associated with the severity of COVID-19. Nat Sci Sleep 2020; 12: 999–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kou T, Wang Q, Lv W, et al. Poor sleep quality is associated with a higher risk of pulmonary tuberculosis in patients with a type 2 diabetes mellitus course for more than 5 years. Jpn J Infect Dis 2019; 72: 243–49. [DOI] [PubMed] [Google Scholar]
- 32.Prather AA, Janicki-Deverts D, Hall MH, Cohen S. Behaviorally assessed sleep and susceptibility to the common cold. Sleep 2015; 38: 1353–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord 2020; 277: 55–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.O’Brien KE, Riddell NE, Gómez-Olivé FX, Rae DE, Scheuermaier K, von Schantz M. Sleep disturbances in HIV infection and their biological basis. Sleep Med Rev 2022; 65: 101571. [DOI] [PubMed] [Google Scholar]
- 35.Raj JP, Ramesh N. Quality of sleep among patients diagnosed with tuberculosis-a cross-sectional study. Sleep Breath 2021; 25: 1369–77. [DOI] [PubMed] [Google Scholar]
- 36.Nevin RL, Croft AM. Psychiatric effects of malaria and anti-malarial drugs: historical and modern perspectives. Malar J 2016; 15: 332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gonzalez H, Hagerling C, Werb Z. Roles of the immune system in cancer: from tumor initiation to metastatic progression. Genes Dev 2018; 32: 1267–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Garbarino S, Lanteri P, Bragazzi NL, Magnavita N, Scoditti E. Role of sleep deprivation in immune-related disease risk and outcomes. Commun Biol 2021; 4: 1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Klinzing JG, Niethard N, Born J. Mechanisms of systems memory consolidation during sleep. Nat Neurosci 2019; 22: 1598–610. [DOI] [PubMed] [Google Scholar]
- 40.Reyes-Resina I, Samer S, Kreutz MR, Oelschlegel AM. Molecular mechanisms of memory consolidation that operate during sleep. Front Mol Neurosci 2021; 14: 767384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Insel PS, Mohlenhoff BS, Neylan TC, Krystal AD, Mackin RS. Association of sleep and β-amyloid pathology among older cognitively unimpaired adults. JAMA Netw Open 2021; 4: e2117573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Helakari H, Korhonen V, Holst SC, et al. Human NREM sleep promotes brain-wide vasomotor and respiratory pulsations. J Neurosci 2022; 42: 2503–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bassetti CLA, Randerath W, Vignatelli L, et al. EAN/ERS/ESO/ESRS statement on the impact of sleep disorders on risk and outcome of stroke. Eur J Neurol 2020; 27: 1117–36. [DOI] [PubMed] [Google Scholar]
- 44.Vaingankar JA, Müller-Riemenschneider F, Chu AHY, et al. Sleep duration, sleep quality and physical activity, but not sedentary behaviour, are associated with positive mental health in a multiethnic Asian population: a cross-sectional evaluation. Int J Environ Res Public Health 2020; 17: 8489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Baglioni C, Battagliese G, Feige B, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord 2011; 135: 10–19. [DOI] [PubMed] [Google Scholar]
- 46.Gregory AM, Caspi A, Eley TC, Moffitt TE, Oconnor TG, Poulton R. Prospective longitudinal associations between persistent sleep problems in childhood and anxiety and depression disorders in adulthood. J Abnorm Child Psychol 2005; 33: 157–63. [DOI] [PubMed] [Google Scholar]
- 47.Freeman D, Sheaves B, Waite F, Harvey AG, Harrison PJ. Sleep disturbance and psychiatric disorders. Lancet Psychiatry 2020; 7: 628–37. [DOI] [PubMed] [Google Scholar]
- 48.Liu JW, Tu YK, Lai YF, et al. Associations between sleep disturbances and suicidal ideation, plans, and attempts in adolescents: a systematic review and meta-analysis. Sleep 2019; 42: zsz054. [DOI] [PubMed] [Google Scholar]
- 49.Vandekerckhove M, Wang YL. Emotion, emotion regulation and sleep: an intimate relationship. AIMS Neurosci 2017; 5: 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Irwin MR, Carrillo C, Sadeghi N, Bjurstrom MF, Breen EC, Olmstead R. Prevention of incident and recurrent major depression in older adults with insomnia: a randomized clinical trial. JAMA Psychiatry 2022; 79: 33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tregear S, Reston J, Schoelles K, Phillips B. Obstructive sleep apnea and risk of motor vehicle crash: systematic review and meta-analysis. J Clin Sleep Med 2009; 5: 573–81. [PMC free article] [PubMed] [Google Scholar]
- 52.Watson NF, Morgenthaler T, Chervin R, et al. Confronting drowsy driving: the American Academy of Sleep Medicine perspective. J Clin Sleep Med 2015; 11: 1335–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Higgins JS, Michael J, Austin R, et al. Asleep at the wheel-the road to addressing drowsy driving. Sleep 2017; 40: zsx001. [DOI] [PubMed] [Google Scholar]
- 54.Williamson AM, Feyer AM. Moderate sleep deprivation produces impairments in cognitive and motor performance equivalent to legally prescribed levels of alcohol intoxication. Occup Environ Med 2000; 57: 649–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Glick DR, Abariga SA, Thomas I, et al. Economic impact of insufficient and disturbed sleep in the workplace. PharmacoEconomics 2023; 41: 771–85. [DOI] [PubMed] [Google Scholar]
- 56.Sutherland C, Smallwood A, Wootten T, Redfern N. Fatigue and its impact on performance and health. Br J Hosp Med 2023; 84: 1–8. [DOI] [PubMed] [Google Scholar]
- 57.Elliott KC, Lincoln JM, Flynn MA, et al. Working hours, sleep, and fatigue in the agriculture, forestry, and fishing sector: a scoping review. Am J Ind Med 2022; 65: 898–912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021; 398: 1700–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Partinen M, Bjorvatn B, Holzinger B, et al. Sleep and circadian problems during the coronavirus disease 2019 (COVID-19) pandemic: the International COVID-19 Sleep Study (ICOSS). J Sleep Res 2021; 30: e13206. [DOI] [PubMed] [Google Scholar]
- 60.Partinen M, Holzinger B, Morin CM, et al. Sleep and daytime problems during the COVID-19 pandemic and effects of coronavirus infection, confinement and financial suffering: a multinational survey using a harmonised questionnaire. BMJ Open 2021; 11: e050672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jahrami HA, Alhaj OA, Humood AM, et al. Sleep disturbances during the COVID-19 pandemic: a systematic review, meta-analysis, and meta-regression. Sleep Med Rev 2022; 62: 101591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Morin CM, Bjorvatn B, Chung F, et al. Insomnia, anxiety, and depression during the COVID-19 pandemic: an international collaborative study. Sleep Med 2021; 87: 38–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Milani SA, Raji MA, Chen L, Kuo YF. Trends in the use of benzodiazepines, z-hypnotics, and serotonergic drugs among US women and men before and during the COVID-19 pandemic. JAMA Netw Open 2021; 4: e2131012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Premraj L, Kannapadi NV, Briggs J, et al. Mid and long-term neurological and neuropsychiatric manifestations of post-COVID-19 syndrome: a meta-analysis. J Neurol Sci 2022; 434: 120162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Goldstein CA, Kagan D, Rizvydeen M, Warshaw S, Troost JP, Burgess HJ. The possibility of circadian rhythm disruption in long COVID. Brain Behav Immun Health 2022; 23: 100476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Donzella SM, Kohler LN, Crane TE, et al. COVID-19 infection, the COVID-19 pandemic, and changes in sleep. Front Public Health 2022; 9: 795320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Vargas I, Muench A, Grandner MA, Irwin MR, Perlis ML. Insomnia symptoms predict longer COVID-19 symptom duration. Sleep Med 2023; 101: 365–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Merikanto I, Dauvilliers Y, Chung F, et al. Sleep symptoms are essential features of long-COVID - comparing healthy controls with COVID-19 cases of different severity in the international COVID sleep study (ICOSS-II). J Sleep Res 2023; 32: e13754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Stewart NH, Koza A, Dhaon S, Shoushtari C, Martinez M, Arora VM. Sleep disturbances in frontline health care workers during the COVID-19 pandemic: social media survey study. J Med Internet Res 2021; 23: e27331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Alhasan DM, Gaston SA, Jackson CL. Structural inequity and racial/ethnic disparities in sleep health during the COVID-19 pandemic. In: BaHammam A, Pandi-Perumal SR, Jahrami H, eds. COVID-19 and sleep: a global outlook. Singapore: Springer Singapore, 2023: 165–93. [Google Scholar]
- 71.Slopen N, Lewis TT, Williams DR. Discrimination and sleep: a systematic review. Sleep Med 2016; 18: 88–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jackson CL, Walker JR, Brown MK, Das R, Jones NL. A workshop report on the causes and consequences of sleep health disparities. Sleep 2020; 43: zsaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hale L, Emanuele E, James S. Recent updates in the social and environmental determinants of sleep health. Curr Sleep Med Rep 2015; 1: 212–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Olorunmoteni OE, Fatusi AO, Komolafe MA, Omisore A. Sleep pattern, socioenvironmental factors, and use of electronic devices among Nigerian school-attending adolescents. Sleep Health 2018; 4: 551–57. [DOI] [PubMed] [Google Scholar]
- 75.Rifkin DI, Long MW, Perry MJ. Climate change and sleep: a systematic review of the literature and conceptual framework. Sleep Med Rev 2018; 42: 3–9. [DOI] [PubMed] [Google Scholar]
- 76.Minor K, Bjerre-Nielsen A, Jonasdottir SS, Lehmann S, Obradovich N. Rising temperatures erode human sleep globally. One Earth 2022; 5: 534–49. [Google Scholar]
- 77.Han KS, Kim L, Shim I. Stress and sleep disorder. Exp Neurobiol 2012; 21: 141–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Jackson CL, Redline S, Emmons KM. Sleep as a potential fundamental contributor to disparities in cardiovascular health. Annu Rev Public Health 2015; 36: 417–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Stefanovics EA, Potenza MN, Pietrzak RH. PTSD and obesity in U.S. military veterans: prevalence, health burden, and suicidality. Psychiatry Res 2020; 291: 113242. [DOI] [PubMed] [Google Scholar]
- 80.Hale L, Troxel W, Buysse DJ. Sleep health: an opportunity for public health to address health equity. Annu Rev Public Health 2020; 41: 81–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Emilsson OI, Janson C, Benediktsdóttir B, Júlíusson S, Gíslason T. Nocturnal gastroesophageal reflux, lung function and symptoms of obstructive sleep apnea: results from an epidemiological survey. Respir Med 2012; 106: 459–66. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


