Abstract
Coercive control is an under researched type of intimate partner violence (IPV). The aims of this review were to (a) synthesize all available evidence regarding associations with coercive control and mental health outcomes including post-traumatic stress disorder (PTSD), complex PTSD, and depression; and (b) compare these with associations involving broader categories of psychological IPV. Primary studies which measured associations of coercive control with PTSD, complex PTSD, depression, or other mental health symptoms, were identified via a systematic search of electronic databases (PsycINFO, Medline, CINAHL, Scopus). Eligible studies involved observational designs and reported associations between coercive control and mental health outcomes, among participants who were at least 18 years old. Studies were published in peer-reviewed journals and English language. Random-effects meta-analyses were used to synthesize correlational data from eligible studies. The search identified 68 studies while data from 45 studies could be included in the meta-analyses. These indicated moderate associations involving coercive control and PTSD (r = .32; 95% confidence interval [.28, .37]) and depression (r = .27; [.22, .31]). These associations were comparable to those involving psychological IPV and PTSD (r = .34; [.25, .42]) and depression (r = .33; [.26, .40]). Only one study reported on the relationship between coercive control and complex PTSD and meta-analyses could not be performed. This review indicated that coercive control exposure is moderately associated with both PTSD and depression. This highlights that mental health care is needed for those exposed to coercive control, including trauma-informed psychological interventions.
Keywords: coercive control, intimate partner violence, psychological abuse, PTSD, complex PTSD, depression
Background
Intimate partner violence (IPV) is a public health concern that has been linked with long-term mental health consequences including post-traumatic stress disorder (PTSD), depression, anxiety, alcohol and substance use disorders, as well as suicidality (World Health Organization [WHO], 2017). IPV may include physical, sexual, and psychological abuse. Psychological IPV can include verbal aggression and intimidating and belittling behaviors, as well as coercive control (WHO, 2017). Coercive control is a form of abuse where the main goal is to degrade, isolate, and deprive a person of their rights to physical security, dignity, and respect, which puts the victim in a state of terror and entrapment, and includes tactics such as monitoring movements, social isolation, and restriction of access to financial resources, employment, education, or medical care (Pitman, 2016; Stark, 2007, 2013; Stark & Hester, 2019). For instance, abusers may use tactics involving threats to hurt or kill their victims, their children or pets, or isolating them from family, friends, and support services. Coercive control may also involve economic abuse, by threatening economic security and independence (Postmus et al., 2020), intimate partner stalking (Mechanic et al., 2008), as well as reproductive coercion, such as pregnancy coercion or interference with contraception (Miller et al., 2010).
Psychometric measures often differentiate between behaviors attributed to broad forms of all psychological IPV (e.g., belittling, verbal aggression), versus specific dimensions of coercive control (e.g., monitoring, isolation) using subscales. For example, the Psychological Maltreatment of Women Inventory (PMWI; Tolman, 1989) provides one of the main measures of psychological IPV which distinguishes coercive controlling behaviors. It includes the emotional/verbal abuse (PMWI-EV) subscale, which captures general forms of psychological IPV, and the dominance/isolation (PMWI-DI) subscale, which captures more targeted features of coercive control.
As coercive control is both a distinct construct and a dimension of broader psychological IPV, it can be unclear whether an abusive behavior occurs in the context of coercive control (Dutton & Goodman, 2005). For instance, verbal threats may or may not reflect coercive control, depending on whether or not these occur in the context of a broader pattern of controlling, isolating, and degrading behaviors. This aligns with Johnson’s (2008) contextual distinction between psychological couple violence which occurs (a) situationally, such as eruptions of heated arguments (potentially involving threats) that are spontaneous and often mutual, and (b) coercive control (referred to by Johnson as intimate terrorism), which is characterized as an enduring pattern of violence, domination, intimidation, isolation, and control. Verbal threats can thus reflect situational couple violence or they can occur within the enduring pattern of domination that characterizes coercive control.
Importantly, coercive control is both highly prevalent, occurring in up to 58% of IPV relationships, and a particularly insidious form of IPV that likely has more severe mental health implications than situational psychological IPV, or even physical IPV that is not embedded in the context of coercive control (Crossman et al., 2016; Kennedy et al., 2018; Stark, 2007). Many studies have shown positive associations between coercive controlling behaviors, including specific forms of economic abuse, stalking, and reproductive coercion, with mental health outcomes including PTSD, depression, and other mental health symptoms. However, the findings are mixed. For example, Beck et al. (2011) have found small associations (r = .18), Hines and Douglas (2011) found moderate (r = .37), and Taft et al. (2005) found large associations (r = .56) for coercive control and PTSD. The mixed results are likely associated with methodological differences such as study settings, measures, and sample sizes.
Systematic reviews and meta-analyses can synthesize the effects of individual studies to overcome the limitations of single studies. To our knowledge, no previous systematic review and meta-analysis has investigated the associations with coercive control and mental health outcomes or compared these effects with the mental health outcomes of general psychological IPV (Pill et al., 2017; Stark & Hester, 2019). Most meta-analyses to date have not focused on psychological IPV and have either solely focused on the mental health implications of physical IPV exposure (e.g., Golding, 1999; Spencer et al., 2019; Stith et al., 2004), or have combined different types of IPV (e.g., Beydoun et al., 2012; Devries et al., 2013; Trevillion et al., 2012). These previous meta-analyses have revealed small to moderate mean correlations between physical or combined IPV and PTSD, depression, anxiety, suicidality, and drug and alcohol use, with the most robust evidence with PTSD and with depression (Devries et al., 2013; Golding, 1999; Spencer et al. 2019; Stith et al., 2004). For instance, Golding (1999) found moderate correlations involving physical IPV with PTSD (r = .34) and depression (r = .35), while Spencer et al.’s (2019) recent meta-analysis also found moderate correlations with physical IPV and PTSD (r = .34) and depression (r = .25). Importantly, previous meta-analyses have not distinguished between effects of psychological IPV and coercive control. In part, this may be because the unique impacts of psychological IPV have only been relatively recently more broadly recognized, and because the dimensions of psychological IPV, particularly coercive control, may be more difficult to distinguish and differentiate, when compared to physical IPV (Heise et al., 2019).
Given that meta-analyses have found evidence of the mental health impacts of physical and combined IPV, and the absence of prior systematic reviews of the mental health correlates of coercive control, there is a clear and pressing need for additional systematic examinations of this evidence. This is particularly important as most existing interventions for IPV survivors focus on safety and crisis management, and there is presently a lack of evidence-based psychological programs to support the long-term recovery of those who have been exposed to IPV, particularly coercive control (Hameed et al., 2020). A better understanding of the unique mental health consequences of coercive control would help to inform the development of such evidence-based psychological interventions, and to inform policy and legislation to promote long-term support and recovery (Crossman & Hardesty, 2018).
Moreover, the prolonged and chronic pattern of terror and entrapment of coercive control suggests that such exposures could be uniquely associated with complex PTSD (CPTSD) symptoms (Pill et al., 2017). The latest edition of the International Statistical Classification of Diseases and Related Health Problems (11th ed.; [ICD-11], WHO, 2019) includes a diagnostic classification for CPTSD which includes symptoms associated with (a) affective dysregulation, (b) negative self-concept, and (c) disturbances in relationships, which are additional to the diagnostic criteria of PTSD. An essential criterion for an ICD-11 CPTSD diagnosis is the “exposure to an event or series of events of an extremely threatening or horrific nature, most commonly prolonged or repetitive events from which escape is difficult or impossible” (WHO, 2019), which may include prolonged exposure to IPV. Given the chronic terror and entrapment experiences that characterize coercive control, with a typical length of IPV relationships ranging from 15 to 24 months, the likelihood of developing CPTSD in response to coercive control exposure may be high (Kennedy et al., 2018). This may explain in part the more detrimental mental health outcomes compared to other types of IPV (Crossman et al., 2016; Stark, 2007). In fact, it is possible that coercive control may have stronger associations with CPTSD compared to other types of IPV that reflect situational couple violence, because of the prolonged exposure to interpersonal trauma (Cloitre, 2021; Herman, 1992). Therefore, research into the associations between coercive control and CPTSD is important to inform development of effective treatment approaches to deal with the psychological consequences of experiencing coercive control (Karatzias & Cloitre, 2019). However, as far as we are aware, there is no systematic review to-date that has examined the relationship between coercive control and CPTSD.
Objectives of the Present Study
In this systematic review and meta-analysis we aimed to address limitations of past research by synthesizing the effects of individual studies to provide more precise estimates of the mental health impacts of coercive control on PTSD, CPTSD, and depression. We also add to research by comparing the mental health impact of coercive control with broader dimensions of any psychological IPV. As previous meta-analyses have consistently found small to moderate correlations with physical (or combined types of IPV) and PTSD and depression, and because of the potentially more detrimental mental health impacts of coercive control, when compared to psychological IPV, it was predicted that coercive control would be positively correlated with PTSD, CPTSD, and depression, and that, the strength of these associations, particularly those of CPTSD, would be stronger compared to those of general psychological IPV.
Method
Registration and Protocols
The protocol for this systematic review and meta-analysis was preregistered with the International Prospective Register of Ongoing Systematic Reviews (PROSPERO) database in June 2021 (registration number: CRD42021252071), while reporting was aligned with guidelines from Preferred Reported Items for Systematic Reviews and Meta-analyses (PRISMA; Page et al., 2021).
Literature Search Strategy
Primary studies examining the associations between coercive control and mental health measures were identified via electronic searches of databases including PsycINFO, Medline, CINAHL, and Scopus. These searches were conducted in May 2021. The search terms for each database are shown in Supplemental Appendix A. All records identified by the search were downloaded into Endnote (Version X9) to remove duplicates. After removing duplicates, the remaining records were uploaded into Covidence Systematic Review Software (2021). Both the title and abstract and the full text screening stages involved two independent reviewers. An exclusion hierarchy was developed by the first reviewer and discussed with the second reviewer before screening. If full text papers could not be obtained, corresponding authors were contacted to obtain full text papers. If authors could not be reached or they did not provide the full text paper, the study was excluded (only two full text papers could not be obtained).
Inclusion Criteria
Studies were included if they were empirical studies involving observational designs that reported on relationships involving measures of exposure to coercive controlling behaviors and any measure of mental health symptoms or diagnoses (including self-report measures and clinical interviews). Eligible studies had to be written in English language, published in peer reviewed journals, while participants had to be at least 18 years old. There were no exclusions on the basis of gender, ethnicity, regions/country, or publication year. Experimental or intervention studies, and studies that did not report primary quantitative data (e.g., case studies, case series, qualitative studies, reviews, editorials, book chapters) were excluded. Studies were also excluded if the violence was not perpetrated by an intimate partner (e.g., instead perpetrated by another family member), they only reported IPV perpetration, did not differentiate between types of IPV, or did not report any measure of coercive control, or did not report this separately from psychological IPV or other types of IPV. Only studies that measured controlling behaviors were included. Studies that only included measures that do not distinguish dimensions of coercive control, namely the Conflict Tactics Scale (CTS; Straus, 1990), Revised Conflict Tactics Scale (CTS2; Straus et al., 1996), the Severity of Violence Against Women Scale (SVAWS; Marshall, 1992), and the Danger Assessment (Campbell et al., 2009) were excluded. Studies that included measures of coercive control in addition to these scales were included and are listed in the results.
Quality Assessment
The risk of bias was assessed with the JBI Critical Appraisal Checklist for Analytical Cross Sectional Studies (Joanna Briggs Institute, 2017). The quality of all studies was assessed by the first reviewer, while a second reviewer independently assessed 31% of the studies (21 out of 68) which were randomly assigned by selecting every third study in alphabetical order.
Data Extraction and Coding
The research team developed a coding sheet that included the study design, country, sample size, and gender, recruitment source, sample characteristics, IPV and coercive control measures, mental health measures, statistical methods, and effect sizes. If effect sizes were not reported as either correlations or odds ratios with confidence intervals (CIs), or they could not be computed from the reported data, an email request for the data was sent to the corresponding authors. If the authors did not respond after 1 month or if they were not able to provide the data, the study was excluded from the meta-analysis.
Data Analyses
Quantitative estimates of associations with measures of coercive control or other forms of IPV with mental health measures were synthesized via a series of random-effects meta-analyses, which account for both within-study and between-study variance and allows for greater generalizability of results (Borenstein et al., 2010). Comprehensive Meta-Analysis Version 3 software (Borenstein et al., 2014) was used for these quantitative syntheses. Only cross-sectional studies or longitudinal studies that reported relevant effect sizes at a single time-point (typically study baseline) were included in the meta-analyses. Random effects meta-analyses were performed for associations with coercive control (including economic abuse, stalking, reproductive coercion) with PTSD and depression. Only one study measured CPTSD and meta-analyses for this outcome could not be completed. To examine the strength of associations of coercive control with PTSD and depression, in comparison with the association of psychological IPV with PTSD and depression, additional random effects meta-analyses for the correlations of psychological IPV with PTSD and depression were performed. Only studies that also measured coercive control were included in this comparison, as only these studies met the inclusion criteria for this review.
A Pearson’s r correlation coefficient was selected as the effect size index for purposes of reporting and were interpreted based on Cohen’s (1988) guidelines whereby r values around 0.10 indicate a small, 0.30 are medium, and values around 0.50 a large effect. Only bivariate effect sizes that could be transformed into a Pearson’s r correlation coefficient, such as unadjusted odds ratios and independent group means and standard deviations, were included in the meta-analysis. When a study reported a standardized regression coefficient (β) without reporting a correlation coefficient, the β was imputed as the correlation coefficient (assuming a bivariate model) (Peterson & Brown, 2005). When a study only reported the correlation coefficient for subgroups (e.g., according to gender or ethnicity) without providing a correlation coefficient for the total sample, all subgroup correlation coefficients were transformed using Fisher’s Z, and back-transformed after calculating the mean Z value to retrieve the average correlation coefficient (Corey et al., 1998).
Heterogeneity was assessed with the Q and I2 statistics, where and I2 value of 25% indicated low, of 50% moderate, and of 75% high heterogeneity (Higgins et al., 2003). A series of exploratory subgroup analyses considering (a) types of coercive control measure (general coercive control measures vs. specific economic abuse, stalking and reproductive coercion measures) and (b) study settings (domestic violence support services/shelters vs. community) were performed to examine potential sources of heterogeneity. Subgroup analyses were only performed when at least six studies were available to be included in a subgroup. Therefore, subgroup analyses comparing gender or countries could not be performed. Statistical significance of subgroup differences was inferred when the 95% CIs for point estimates for each subgroup did not overlap (Cumming & Finch, 2005).
Publication bias was assessed with three tests. First, Duval and Tweedie’s (2000) trim and fill test, which estimates the number of studies missing on the left or right side of the funnel plot, and also estimates the effect size if such hypothetical studies were included. Second, Rosenthal’s (1979) classic fail-safe N test, which calculates how many studies with nonsignificant results would be needed to make the mean effect size nonsignificant. A large fail-safe N suggests that there is no risk of publication bias. Rosenthal recommends that the minimum fail-safe N can be computed by first multiplying the number of effect sizes by 5 and then adding 10 to that number. Finally, Orwin’s (1983) fail-safe N identifies the number of potentially missing studies with an effect size of r = .00 needed to reduce the mean effect size of each mental health outcome below a small effect size of r = .10.
Results
Search Results
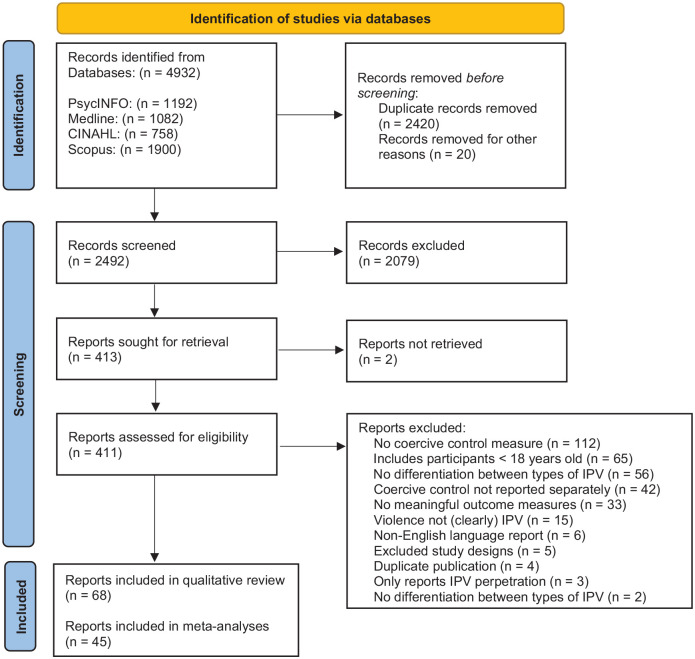
The combined database search identified a total of 4932 records. After removing 2440 duplicates, there were 2,492 records (PsycINFO = 1,175, Medline = 476, CINAHL = 208, Scopus = 633) imported into Covidence for title and abstract screening. After title and abstract screening, 2,079 records were excluded as ineligible, while 413 studies were passed on to full text screening. After the full text review a further 345 studies were excluded (see Supplemental Appendix B for a list of excluded studies) and 68 eligible studies were remaining. Every title, abstract, and full text record was screened by two independent reviewers. Conflicts were resolved through discussion and consensus. The reviewers identified that the main reasons for conflict were the heterogeneity and overlap of psychological abuse and coercive control measures. Data from 45 studies was available for inclusion in the meta-analyses. The PRISMA flow chart (Figure 1) depicts a summary of the study selection process.
Figure 1.
Preferred Reported Items for Systematic Reviews and Meta-analyses flow chart of study selection based on Page et al. (2021).
Description of Studies
The included studies examined associations involving coercive control (including economic abuse, stalking and reproductive coercion) with PTSD, CPTSD, depression, suicidality, anxiety, drug and alcohol use, and transdiagnostic mental health, using a variety of coercive control and mental health measures. Most studies (76%) recruited only women (k = 52), while 19% included women and men (k = 13), including one study where female and male participants identified as lesbian, gay, bisexual, or transgender. Only 3% of studies included only male participants (k = 3), including one study that focused on gay, bisexual, and other men who have sex with men. The vast majority (81%) of studies were conducted in developed countries, with 68% in the United States (n = 46). The latter included one study that also included participants from Puerto Rico. These were followed by 6% of studies from Canada (n = 4), and 6% from Europe (Denmark: n = 2, Sweden: n = 2), and Australia (n = 1). Other studies were from South America (Brazil: n = 2), Africa (South Africa: n = 3, Cote d’Ivoire: n = 1, Nigeria: n = 1, Kenya: n = 1, Tanzania: n = 1), Asia (Hong Kong: n = 1, Malaysia: n = 1, South Korea: n = 1) and the Middle East (Jordan: n = 1). Participants were recruited from a variety of settings, including shelters and domestic violence support services, the community, healthcare settings, and universities. These and other key characteristics included in the qualitative synthesis are summarized in Table 1.
Table 1.
Description of Studies Included in the Systematic Review in Alphabetical Order.
| Study | Country | Study Type | Recruitment | Sample | Age Range (M; SD) | Type | IPV Measures | Mental Health Constructs and Measures | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Coercive control | Psychological | Physical/sexual | Constructs | Measures | |||||||
| * Ahmad et al. (2018) | Malaysia | CS | Com: Post-natal health care facilities | 5,727 w | ≥18 | CC | WHOMCS-CC items | WHOMCS | WHOMCS | Postnatal depression | EPDS (Malaysian) |
| Alexander et al. (2019) | USA | CS | Com: Community support services | 188 w | 18–24 (21.3; 2.2) | RC | 10-items (Miller et al., 2010) | PTSD, depression | PCPTSD, CESD-SF | ||
| * Anderson (2008) | USA | CS 2nd | Com: NVAWS national survey | 4,575 w | 18–88 | CC | NVAWS-CC items | PTSD, depression | IES (adapted), NVAWS 8 depression items | ||
| Anderson et al. (2017) | USA | CS | Com: HIV clinic | 67 w | 18–45 | RC | 10-items (Miller et al., 2010) | PTSD, depression | PCL-C, CESD | ||
| Basile et al. (2004) | USA | CS—2nd | NVAWS: IPV subgroup | 380 w | <18 (40) | ST | NVAWS-ST Items |
NVAWS verbal abuse + CC |
CTS | PTSD | IES (adapted) |
| *Beck et al. (2011) | USA | CS | IPV survivors—university research clinic | 63 w | 18–64 (36.75; 11.62) | CC | PMWI-DI | PMWI-EV | Interview devised by authors | PTSD | CAPS for DSM-IV |
| * Broughton and Ford-Gilboe (2017) | Canada | LO—2nd | IPV—subsample from WHES | 157 w | 20–64 (40.6; 9.6) | CC | WEB | Depression | CESD | ||
| * BubriskiMcKenzie and Jasinski (2013) | USA | CS 2nd | Com: IPV sample CWHRS | 705 w | ≥18 Bl: (31.07; 9.46) His: (29.08; 7.79 |
CC | CWHRS Power and Control Scale | CTS2 | PTSD, Depression | PSS-I CWHRS-based on MOS | |
| Coker et al. (2002) | USA | CS—2nd | Com: NVAWS national survey | 6,790 w 7,122 m | 18–65 | CC | NVAWS-CC items | NVAWS-verbal abuse | CTS | Depression Drug and Alcohol Use | SF-36 NVAWS Drug and Alcohol items |
| * Damra and Abujilban (2021) | Jordan | CS | Com: hospital gynecology/obstetric service | 300 w | 18–49 (32; 6.4) | CC | WHOMCS-CC items | WHOMCS | WHOMCS | Depression | BDI for Jordanian culture |
| * Dokkedahl et al. (2021) | Denmark | CS | Shelter | 147 w | ≥18 (34.6; 10.1) | CC | PMWI-DI | PMWI-EV | CTS2 | PTSD | ITQ, HTQ, TSC-26 |
| * Dutton and Painter (1993) | Canada | LO | IPV—shelters, support programs | 75 w | ≥18 (31.4) | PMWI-DI | PMWI-EV | CTS | PTSD | TSC-33 | |
| Dutton et al. (1999) | USA | CS | DV support service | 149 w | 18–58 (30) | CC | PMWI-DI | PMWI-EV | CTS2 | PTSD, Depression | PSS-SR, CESD |
| * Emery et al. (2019) | South Korea | CS | Com | 462 w | ≥18 | CC | NVAWS-CC items | Alcohol Use | CAGE | ||
| Fleming et al. (2012) | USA | CS | Com | 192 w | ≥18 (55.04; 3.92) | ST | NVAWS-ST items | CTS2 | CTS2 | PTSD | PCL-C |
| * Gibbs et al. (2018) | South Africa | CS | Com | 677 w | 18–30 (23.7) | EA | WHOMCS-CC | WHOMCS | Depression Suicidal Ideation | CESD SI: 1-item |
|
| Gou et al. (2019) | Canada | LO | Com | 98 w 98 m |
≥18 w: (29.98; 5.49) m: (32.03; 5.51) | CC | PMWI-DI | CTS2 | CESD | ||
| Grace et al. (2020) | USA | CS | University students | 354 w | ≥18 (20.88; 2.31) | CC, RC | 2 RC questions CAS |
CAS | CAS | Depression Drug and Alcohol Use |
CESD-R MFDAQ |
| * Groves et al. (2012) | South Africa | CS | Com: HIV | 1,500 w | ≥18 (27.29; 5.36) | CC | SRPS | adapted WHOMCS |
adapted WHOMCS |
Depression, Anxiety | HSCL-25 |
| Hardesty et al. (2019) | USA | LO | Com: mothers who filed for divorce | 135 w | 20.83–53.92 (35.22; 7.02) | CC | PMWI-DI | CTS2 | PTSD, Depression |
PCL-C-SF CESD-SF |
|
| Hayes and Kopp (2020) | USA | CS—2nd | Com: National NISVS | 7,433 w 6266 m |
≥18 | CC RC | Number of CC, RC past year | Number of psych. IPV past year | Number of physical IPV past year | Mental Health | Self-rated |
| * Hazen et al. (2008) | USA | CS | Com: Healthcare service users | 282 w | 18–45 (27.74; 7.12) | CC | PMWI-DI-SF | PMWI-EV-SF | CTS2 | Depression, Anxiety | BSI |
| * Hedin and Janson (1999) | Sweden | CS | Com: Antenatal clinics | 207 w | 18–35 (29.5, 4.5) | CC | PMWI-DI | PMWI-EV | SVAWS | PTSD, Anxiety | TSC-33 STAI |
| * Hines and Douglas (2011) | USA | CS | IPV support services (help-seeking group), Com |
822 m (302 IPV 520 com) | 18–59 IT: (40.49; 8.97) Com: (43.68; 10.88) |
CC | PMWI-DI | CTS2 | CTS2 | PTSD | PCL-C |
| * Hines and Douglas (2012) | USA | CS | IPV services (help-seeking group), Com | 822 m (302 IPV 520 Com) |
18–59 help-seek. (40.49; 8.97) Com: (43.68; 10.88) |
CC | PMWI-DI | CTS2 | CTS2 | Drug and Alcohol Use | NWS Alcohol and Drug Use scale |
| * Hines and Douglas (2018) | USA | CS | IPV support services (help-seeking group), Com |
2,212 m (611 IPV, 1601 Com) |
18–59 IPV: (43.89; 9.18), Com: (41.77; 11.35) |
CC | PMWI-DI | CTS2 | CTS2 | PTSD, Depression | PCL-C, CESD |
| * Ireland et al. (2017) | Australia | CS | Com: LGBTI | 287 LGBTI w and m | ≥18 (34.8; 11.2) | CC | MMEA (extended 44 items) | MMEA (extended 44 items) |
MMEA (extended 44 items) |
PTSD, Depression, Anxiety | PCL-C-SF, HAD |
| * Johnson and Leone (2005) | USA | CS—2nd | Com: NVAWS national survey |
4,967 w (81 IT) |
18–97 (44.55; 13.89) | CC | NVAWS-CC items | 12-items adapted from CTS | PTSD, Depression | IES (adapted), 8-items depression scale (based on SF-36) | |
| Johnson et al. (2014) | USA | CS—2nd | Com: NVAWS national survey | 7,782 w 6,908 m |
18–97 (46.91; 15.67) | CC | 12-items CC-Scale like PMWI | 12-items adapted from CTS | Depression | 8-items depression scale (based on SF-36) | |
| * Jones (2020) | USA | CS | Prison | 337 w | 18–65 | CC | based on CCMIPV | PTSD | PCL-C | ||
| * Jones et al. (2005) | USA | CS | DV services, medical and com | 172 w | 18–40 | CC | PMWI-DI-SF | PMWI-EV-SF, SOSPS | PTSD, Depression, Anxiety | PSDSWB BDI, BAI | |
| * Kapiga et al. (2017) | Tanzania | CS | Com | 1,021 w | 19–70 | CC, EA | WHOMCS-CC, EA items | WHOMCS | WHOMCS | Mental Health | SRQ-20 |
| * Lawrence et al. (2009) | USA | LO | Com: married couples | 103 w 103 m |
18–55 w: (25; 4.3) m: (26.4; 4.7) | CC | MMEA-RE | MMEA-total | Depression, Anxiety | BDI-II, BAI | |
| * Leone (2011) | USA | CS 2nd | CWHRS abused women subsample | 369 w | ≥18 (31; 9.62) | CC | PCS | PTSD, Depression, Suicidality |
PSS-I, MOS-4 items SI + SA combined 1item | ||
| * Levine and Fritz (2016) | Canada | CS | Shelter | 51 w | 19–58 (37) | CC | CBS-R | CTS2 | PTSD, Depression | PCL-C, BDI-II |
|
| * Lovestad et al. (2017) | Sweden | CS | Com: population sample | 573 w | 18–65 (42.7: 13.01) | CC | CBS-isolating control | WHOMCS | WHOMCS | Depression | self-report of 5 DSMIV indicators |
| * Ludermir et al. (2010) | Brazil | CS | Com: pregnant women from a family health program | 1,045 w | 18–49 | CC | WHOMCS-CC | WHOMCS | WHOMCS | Postnatal Depression | EPDS |
| * Ludermir et al. (2010) | Brazil | CS | Com: pregnant women from a family health program | 1,045 w | 18–49 | CC | WHOMCS-CC | WHOMCS | WHOMCS | Postnatal Depression | EPDS |
| Ludermir et al. (2014) | Brazil | CS | Com: pregnant women from a family health program | 1,120 w | 18–49 | CC | WHOMCS-CC | WHOMCS | WHOMCS | Mental Health | SRQ-20 |
| McCauley et al. (2014) | Cote d'Ivoire | CS | Com | 953 w | ≥18, (37.4) | RC | Based on Miller et al. (2010) | PTSD | HTQ | ||
| Mechanic et al. (2000) | USA | CS | DV support services | 114 w | 19–59 (35; 7.9) | (CC) ST |
SBC (PMWI-DI) | PMWI-EV | CTS2 | PTSD, Depression | PDS, BDI-II |
| * Mechanic et al. (2008) | USA | CS | DV support services | 413 w | 18–62 (34.5; 8.1) | CC, ST | PMWI-DI, SBC | PMWI-EV | PTSD, Depression | PDS, BDI-II | |
| Mutiso et al. (2020) | Kenya | CS | Com: Healthcare services | 5,448 w 2,862 m |
18–60+ | CC | WHOMCS-CC items |
WHOMCS | WHOMCS | Mental Health | MINI Plus |
| Newton (2021) | USA | CS | Com | 69 w | ≥18 (54.53; 3.19) | CC | PMWI-DI-SF | PMWI-DI-SF | CTS2 | PTSD—peritraumatic emotions | CAPS for DSM-IV |
| * Nielsen et al. (2016) | USA | CS | Com: Coparenting | 147 w | 20–54 (35.2) | CC | PMWI-DI-SF | PMWI-EV-SF | CTS2 | PTSD, Depression | PCL, CESD-SF |
| * Norwood and Murphy (2012) | USA | CS 2nd | DV support services | 216 w | 18–70 (34.0, 10.1) | CC | MMEA-RE | MMEA-total | CTS2 | PTSD | PCL-C-IPV |
| * Nnawulezi and Murphy (2019) | USA | CS | DV support services (archival data) | 228 w | 18–70 (34.23; 10.09) | CC | MMEA-RE | MMEA-total | CTS2 | PTSD | PCL-C-IPV |
| * Ogunbajo et al. (2020) | Nigeria |
CS |
Com |
389 m |
≥18 |
CC |
IPV-GBM monitoring controlling |
IPV-GBM |
IPV-GBM |
Depression, Suicidality, Anxiety |
CESD SI-1-item, SA-1-item GAD-7 |
| Peltzer et al. (2013) | South Africa | CS | IPV survivors who obtained a protective order | 268 w | 18–62 (28.8; 8.0) | ST | SVS, 10 items from HARASS |
SVAWS | SVAWS | PTSD, Depression Alcohol Use | PCL-C, CESD AUDIT-C |
| * Petra (2020) | USA | CS | Com | 222 w | 24–63 (33) | CC | MASIC-CC subscale | WAST | Depression, Anxiety | DASS-21 | |
| * Pickover et al. (2017) | USA | CS | IPV survivors, mental health research clinic | 284 w | ≥18 (37.84; 12.08) | CC | PMWI-DI-SF | PMWI-EV-SF | CTS2 | PTSD, Anxiety | LEC, IPV-related DSMIV-TR, ADIS-IV |
| Postmus et al. (2012) | USA | LO | Com | 2,305 w | ≥18 (25.8; 6.1) |
EA | Any EA in year 1 | Any psych. IPV in year 1 |
Any physic. IPV in year 1 |
Depression | CIDI-SF |
| Prospero (2008) | USA | CS | University students | 609 (361 w, 248 m) |
≥18 (21.44; 4.58) | CC | CBS-R | CTS2 | CTS2 | Mental Health | SQ |
| Prospero (2009) | USA | CS | University students | 573 (332 w, 241 m) |
≥18 (21.4; 4.37) |
CC | CBS-R | CTS2 | CTS2 | Mental Health | SQ |
| * Prospero and Kim (2009a) | USA | CS | University students | 560 (325 w, 235 m) |
≥18 (21.4; 4.37) |
CC, EA | CBS-R | CTS2 | CTS2 | Depression, Anxiety | SQ |
| Prospero and Kim (2009b) | USA | CS | University students | 676 (419 w, 257 m) |
≥18 (21.6; 4.66) |
CC, EA | CBS-R | CTS2 | CTS2 | Mental Health | SQ |
| * Reich et al. (2015) | USA | CS | IPV survivors—mixed recruitment | 105 w | ≥18 (36.94;12.68) | CC | PMWI-DI-SF | PMWI-EV-SF | CTS2 | PTSD | CAPS for DSM-IV |
| * Sackett and Saunders (1999) | USA | CS | DV support services | 60 w | ≥18 (34.7; 9.1) | CC | PPA-JC |
PPA | Depression, Anxiety | BDI 6-item Anxiety Scale |
|
| Sauber and O'Brien (2020) | USA | CS | DV support services, community | 147 w | ≥18 (34.7; 9.1) |
EA | SEA-12 | ABI | ABI | PTSD, Depression | PCL-C, CESD |
| Strauss et al. (2019) | USA | CS | University students | 357 (290 w, 67 m) |
18–25 (18.64; 1.13) | ST | 32-item validated ST measure | Alcohol and Drug Use | AUDIT DUDIT | ||
| * Street and Arias (2001) | USA | CS | Shelter | 63 w | 19–64 (32) | CC | PMWI-DI | PMWI-EV | CTS | PTSD, Depression | CMS, SCL-90-R |
| Stylianou (2018) | USA, Puerto Rico | LO | DV support services | 457 w | ≥18 (36; 9.15) |
EA | SEA-12 | ABI-R | ABI-R | Depression | CESD |
| * Taft et al. (2005) | USA | LO | Partners of IPV perpetrator group program participants | 96 w | 18–59 (34.0; 8.6) | CC | MMEA-RE | MMEA-total | CTS | PTSD | DIS for DSM-III |
| * Tiwari et al. (2015) | Hong Kong | CS | DV support services | 613 w | ≥20 | CC | CBS-R (Chinese) | C-AAS | PTSD, Depression | PCL-C (Chinese) BDI-II (Chinese) | |
| Voth Schrag et al. (2019) | USA | CS | University students | 435 w | ≥18 (27; 9.9) | EA | SEA-12 | ABI-R | PTSD, Depression |
PCL-5 LEC-5, CESD-SF |
|
| * Weaver and Etzel (2003) | USA | CS | DV support services | 62 w | ≥18 (34; 8.4) | CC | PMWI-DI-SF | PMWI-EV-SF | CTS2 | PTSD, Depression * | PDS, BDI-II |
| Wolf et al. (2018) | Denmark | CS | ST support services, groups | 196 w | 27–70 (40.82; 6.93) | ST | SBC | PMWI | PTSD | HTQ, TSC-33 | |
| * Wolford-Clevenger et al. (2017) | USA | CS | University students | 208 (107 w, 101 m) |
18–29 (19.61; 11.09) | CC | MMEA-RE | MMEA | CTS2 | Depression, Suicidal Ideation | PDSQ |
| * Wolford-Clevenger and Smith (2017) | USA | CS | Shelter | 134 w | 19–67 (32.50; 8.21) | CC | CIPRS | CTS2 (modified) | PTSD, Depression, Suicidal Ideation and Attempts | PCL-C, DASS-21 SI: MSSI SA: L-SASI |
|
Note. Study type: CS = cross-sectional; LO = longitudinal; 2nd = secondary data analysis; Sample: w = women; m = men; Age: M = mean; SD = standard deviation; IPV = intimate partner violence; DV = domestic violence; PTSD = post-traumatic stress disorder; Type of coercive control: CC = coercive control; EA = economic abuse; RC = reproductive coercion; ST = stalking. Recruitment: Com = community sample (i.e., not specific IPV sample); NVAWS = National Violence Against Women survey (Tjaden & Thoennes, 1999); NISVS = The National Intimate Partner and Sexual Violence Survey (Smith et al., 2017); CWHRS = Chicago Women’s Health Risk Study (Block, 2000); WHES = Women’s Health Effects Study (Ford-Gilboe et al. 2009). IPV Measures: ABI = The Abusive Behavior Inventory (Shepard & Campbell, 1992); ABI-R = Abuse Behavior Inventory–Revised (Postmus et al. 2016b); CAS = Composite Abuse Scale (Hegarty et al.,1999, 2005); CAAS = Chinese Abuse Assessment Screen (Tiwari et al., 2007); CBS = Controlling Behaviors Scale (Graham-Kevan & Archer, 2003a); CBS-R = Controlling Behaviors Scale-Revised (Graham-Kevan & Archer, 2003b); CCMIPV = Coercive Control Measure for IPV (Dutton et al., 2005); CIPRS = Coercion in Intimate Partner Relationships Scale (Dutton et al., 2007); CTS = Conflict Tactics Scale (Straus, 1990); CTS2 = Revised Conflict Tactics Scale (Straus et al., 1996); HARASS = Harassment of battered women (Sheridan, 1998); IPV-GBM = Intimate Partner Violence among Gay and Bisexual Men Scale (Stephenson & Finneran, 2013); MASIC = Mediator’s Assessment of Safety Issues and Concerns (Pokman et al., 2014); MMEA = Multidimensional Measure of Emotional Abuse (Murphy et al., 1999); MMEA-RE restrictive engulfment subscale; PCS = Power and Control Scale (Leone et al., 2007); PMWI, PMWI-SF = Psychological Maltreatment of Women Inventory (Tolman, 1989;1999) with PMWI-DI = dominance/isolation subscale, PMWI-EV = emotional/verbal abuse subscale; PPA = Profile of Psychological Abuse (Sacket & Saunders, 1999); SEA-12 = Scale of Economic Abuse-12 (Postmus et al., 2016a); SBC = Stalking Behavior Checklist (Coleman, 1997); SRPS = Sexual Relationship Power Scale (Pulerwitz et al., 2002); SVAWS = Severity of Violence Against Women Scale (Marshall, 1992); SVS = Stalking Victimization Survey (Tjaden & Thoennes, 1999); WAST = Woman Abuse Screening Tool (Brown, 1996); WEB = Women’s Experiences with Battering (Smith et al., 1999); WHOMCS = WHO Multi-country Study on Women's Health and Domestic Violence Against Women (Garcia-Moreno et al., 2005). PTSD: CAPS = Clinician-Administered PTSD Scale (Blake et al., 1990); CMS = The Civilian Mississippi Scale for PTSD (Vreven et al., 1995); DIS = Diagnostic Interview Schedule for DSM-III (Robins et al., 1982); HTQ = Harvard Trauma Questionnaire (Mollica et al., 1992); IES = Impact of Event Scale (Weiss & Marmar, 1997); ITQ = International Trauma Questionnaire (Cloitre et al., 2018); LEC = Life Events Checklist (Gray et al., 2004); LEC-5 = Life Events Checklist for DSM-5 (Weathers et al., 2013a); PCL = PTSD Checklist (Blanchard et al., 1996); PCL-C = PTSD Checklist-Civilian (Weathers et al., 1993); PCL-C-SF = PTSD Checklist-Civilian Short Form (Lang & Stein, 2005); PCL-C-IPV = PTSD Checklist-Civilian Modified to IPV experience (Weathers et al., 1993); PCL-5 = The PTSD Checklist for DSM-5 (Weathers et al., 2013b); PCPTSD = Primary Care Post-Traumatic Stress Disorder Screen (Prins et al., 2003); PDS = The Posttraumatic Diagnostic Scale (Foa et al., 1997); PSDSWB = Posttraumatic Stress Disorder Scale for Battered Women (Saunders, 1994); PSS-I = PTSD Symptom Scale Interview (Foa, et al., 1993a); PSS-SR = PTSD Symptom Scale Self-Report Version (Foa, et al., 1993b); TSC-33 = The Trauma Symptom Checklist (Briere & Runtz, 1989); TSC-26 = The Revised Trauma Symptom Checklist (Krog & Duel, 2003). Depression, Suicidality, Anxiety, Mental Health: ADIS-IV = Anxiety Disorders Interview Schedule-IV (Brown et al., 1994); BAI = Beck Anxiety Inventory (Beck et al., 1988); BDI = Beck Depression Inventory (Beck et al., 1961); BDI-II = Beck Depression Inventory (Beck et al., 1996); BSI = Brief Symptom Inventory (Derogatis, 1993); CESD = Center for Epidemiologic Depression Scale (Radloff, 1977); CESD-SF = CESD Short Form (Andresen et al., 1994); CESD-R = (Eaton et al., 2004); CIDI-SF = International Diagnostic Interview, Short Form (Kessler et al., 1998); DASS-21 = The Depression Anxiety Stress Scale 21 (Lovibond & Lovibond, 1995); EPDS = Edinburgh postnatal depression scale (Cox et al., 1987); GAD-7 = Generalized Anxiety Disorder 7-item (Spitzer et al., 2006); HAD = Hospital Anxiety and Depression Scale (Zigmond & Snaith, 1983); HSCL-25= Hopkins Symptom Checklist (Parloff et al., 1954; Winokur et al., 1984); MINI Plus = International Neuropsychiatric Interview (Sheehan et al., 1997); MOS = Medical Outcome Study (Hays et al., 1995); PDSQ = Psychiatric Diagnostic Screening Questionnaire (Zimmerman & Mattia, 2001); L-SASI = Lifetime-Suicide Attempt Self-Injury Count (Linehan et al., 2006); SA = Suicide Attempt SCL-90-R = Symptom Checklist 90 (Derogatis, 1983); SF-36 = Short-Form Health Survey (Ware & Sherbourne, 1992); SI = Suicidal Ideation; SQ = Symptom Questionnaire (Kellner, 1987); SRQ-20 = Self-reporting Questionnaire (Beusenberg et al.,1994); STAI = State-Trait Anxiety Inventory (Spielberger et al., 1983); Alcohol and Drug Use: AUDIT = Alcohol Use Disorders Identification Test (Saunders et al., 1993); AUDIT-C = Alcohol Consumption Questions (Bush, 1998); CAGE = CAGE questionnaire (Ewing, 1984); DUDIT = Drug Use Disorders Identification test (Stuart et al., 2003); MFDAQ = Monitoring the future drug and alcohol questionnaire (Bachman et al., 2011); NWS = National Women’s Study (Kilpatrick et al., 1997). References for these measures are provided in Supplemental Appendix D.
Studies included in the meta-analysis.
Coercive Control Measures
Coercive control was measured with a range of scales and subscales. The domination/isolation subscale of the PMWI-DI (Tolman, 1989) or its short form (PMWI-SF-DI; Tolman, 1999) were most frequently used (n = 17). The Controlling Behaviors Scale-Revised (Graham-Kevan & Archer, 2003) was the second most frequently used measure (n = 7), followed by the Multidimensional Measure of Emotional Abuse (MMEA; Murphy et al., 1999) (n = 6), particularly the Restrictive Engulfment Subscale (MMEA-RE). Several studies in Non-Western countries used the controlling behaviors questions from the WHO Multi-country Study on Women’s Health and Domestic Violence Against Women (Garcia-Moreno et al., 2005)(n = 6). Other studies used the power and control questions that were developed for the National Violence Against Women survey (Tjaden & Thoennes, 1999)(n = 5). Each of the remaining studies used a different scale: Composite Abuse Scale (Hegarty et al.,1999, 2005), Women’s Experiences with Battering (Smith et al., 1999), Scale of Power and Control (Block, 2000), Power and Control Scale (Leone et al., 2007), controlling questions from the Intimate Partner Violence among Gay and Bisexual Men Scale (IPV-GBM; Stephenson & Finneran, 2013), coercive control subscale of the Mediator’s Assessment of Safety Issues and Concerns (Pokman et al., 2014), Sexual Relationship Power Scale (Pulerwitz et al., 2002), coercive tactics subscale from the Coercion in Intimate Partner Relationships Scale (Dutton et al., 2007), coercive control questions from The National Intimate Partner and Sexual Violence Survey (Smith et al., 2017),the Jealous/Control Scale from the Profile of Psychological Abuse (Sackett & Saunders, 1999) and a modified version of Dutton et al.’s (2005) Coercive Control Measure for IPV. Specific measures of economic abuse, stalking, and reproductive coercion are also identified in Table 1.
Mental Health Measures
PTSD symptom severity was measured by 31 studies and was most frequently measured with the PTSD Checklist-Civilian (Weathers et al., 1993). Depression was measured by 38 studies, the most frequently used measure was the Center for Epidemiologic Depression Scale (Radloff, 1977). Notably, only one study (Dokkedahl et al., 2021) measured CPTSD by using the International Trauma Questionnaire (Cloitre et al., 2018). The mental health measures of all studies included in the qualitative synthesis are summarized in Table 1.
Quality Assessment
The reviewers initially obtained a 90% agreement and any conflicts in the quality assessment that remained were discussed and resolved by consensus. The most common risk of bias was that studies did not clearly report or address potential confounds. A summary table of the quality assessment for all studies included in the qualitative synthesis is included in Supplemental Appendix C. The appraisal tool does not offer guidance about cut-off scores to assess the overall level of risk of bias for each study and we could therefore not establish the overall risk of bias for each study (Munn et al., 2020).
Meta-Analyses
A total of 45 studies with 107 effect sizes addressed associations involving coercive control with PTSD and depression and were included across a series of random effects meta-analyses. The numbers of studies, effect size estimates (weighted mean correlations), 95% CIs, and heterogeneity statistic (I2) for these meta-analyses are summarized in Table 2. Forest plots for each meta-analysis are included in Supplemental Appendix E.
Table 2.
Results of Random-Effects Meta-Analyses.
| Association | Studies k | Effect Sizes k | r | 95% CI | I2 (%) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Women | Men | Both | Range | Mean | ||||
| PTSD | |||||||||
| Coercive control | 30 | 31 | 28 | 2 | 1 | −.08 to .56 | .32* | [.28, .37] | 71.77* |
| Psychological IPV | 19 | 19 | 17 | 1 | 1 | −.15 to .64 | .34* | [.25, .42] | 88.48* |
| Depression | |||||||||
| Coercive control | 35 | 38 | 31 | 3 | 4 | −.09 to .59 | .27* | [.22, .31] | 87.20* |
| Psychological IPV | 18 | 19 | 15 | 2 | 2 | −.08 to .60 | .33* | [.26, .40] | 85.45* |
Note. Coercive control includes economic abuse, stalking, reproductive coercion. IPV = intimate partner violence; PTSD = post-traumatic stress disorder.
p ≤ .001
Coercive Control, PTSD, and Depression
The meta-analyses involving coercive control and PTSD identified a significant moderate positive association (r = .32; 95% CI [.28, .37]) when pooled across studies, with high heterogeneity, Q(20) = 97.62, I2 = 79.51%, p < .001. The meta-analyses involving coercive control and depression showed a significant moderate positive correlation (r = .27; [.22, .31]) when pooled across studies, with high heterogeneity, Q(37) = 289.02, I2 = 87.20%, p < .001).
Subgroup analyses
Subgroup analyses for studies addressing associations involving coercive control with PTSD and depression were performed to examine sources of heterogeneity. These analyses included comparisons according to (a) types of coercive control measure (general coercive control measures vs. specific economic abuse, stalking and reproductive coercion measures) and (b) study settings (domestic violence support services/shelters vs. community). The inspection of the 95% CIs showed a statistically significant difference in the strength of mean correlations between coercive control and PTSD according to study settings, with a stronger pooled association observed in studies of domestic violence support services/shelters settings (r = .40; 95% CI [.35, .45]), when compared to community settings (r = .26; [.16, .35]). There were no other significant effects. Findings for all performed subgroup analyses including pooled correlations, 95% CIs and heterogeneity (I2) of studies are summarized in Supplemental Appendix F.
Psychological IPV, PTSD, and Depression
The random-effects meta-analysis showed a significant moderate positive association between psychological IPV and PTSD (r = .34; 95% CI [.25, .42]) with high heterogeneity between studies, Q(18) = 156.23, I2 = 88.48%, p < .001. The random-effects meta-analysis between psychological IPV and depression showed a significant moderate positive association between psychological IPV and depression (r = .33; 95% CI [.26, .40]) with high heterogeneity between studies, Q(18) = 124.36, I2 = 85.45%, p < .001. Inspection of the 95% CIs suggests that there are no statistically significant differences in the associations between coercive control and psychological IPV in relation to PTSD and depression (see Table 2).
Publication Bias
All analyses were found to be robust against the risk of publication bias. The results of the Duval and Tweedie’s (2000) trim and fill test, the classic fail-safe N test (Rosenthal, 1979), and Orwin’s (1983) fail-safe N test for each meta-analysis are summarized in Supplemental Appendix G.
Discussion
This review examined the mental health implications of coercive control and identified moderate associations with measures of PTSD and depression symptom severity, when considered across all available studies. The overall strength of these associations were comparable to those involving broader measures of psychological IPV with both PTSD and depression. Furthermore, the strength of the associations were comparable to those for physical IPV and combined IPV found in previous meta-analyses. For instance, Spencer et al.’s (2019) large meta-analysis found small to moderate correlations between physical IPV and PTSD (r = .34), as well as depression (r = .25).
It was unexpected that associations of coercive control with PTSD and depression would not be clearly stronger than associations involving other types of IPV (including broader measures of psychological IPV), and there are several possible explanations for this. First, considering the difficulties of distinguishing coercive control from broader dimensions of psychological IPV in psychometric measures, construct overlap remains likely and could explain similar effects (Dutton & Goodman, 2005). Relatedly, the psychometric measures and subscales that were used to measure coercive control in this review may not have fully captured whether a behavior occurred in the context of coercive control. For instance, many measures may not fully capture whether respondents experience a threat that is embedded in a chronic pattern of power and control (Johnson, 2008). Second, the chronic pattern of terror and the effects of entrapment that characterize coercive control may be difficult to quantify, and they may not be as clearly measured in psychometric instruments compared to the occurrence of specific behaviors (Dokkedahl et al., 2019). Nevertheless, the similar strength of links involving coercive control and broader dimensions of psychological IPV and physical IPV with mental health symptoms reported in previous meta-analyses, suggests that these dimensions of coercive control are just as important and detrimental as physical IPV.
It was not possible to investigate whether coercive control was associated with CPTSD symptom severity, as only one eligible study measured CPTSD (Dokkedahl et al., 2021). This study reported a small positive correlation (r = .23) between coercive control and CPTSD, with stronger links also observed between broader psychological IPV and CPTSD when compared to physical IPV in a shelter sample of 147 women. This dearth of empirical studies, along with Dokkedahl et al.’s initial findings and emerging evidence from qualitative studies (Baird et al., 2019; Salter et al., 2020), as well as strong conceptual reasons for expecting CPTSD symptoms to develop in response to coercive control (Cloitre, 2021; Herman, 1992; WHO, 2019), suggests an urgent need for more research into the relationship between coercive control and CPTSD.
Finally, combined subgroup analyses of economic abuse, reproductive coercion, and stalking did not indicate any meaningful differences compared to general coercive control, but these types of coercive control were not reviewed separately and may have unique impacts that could not be investigated in this review. Notably, subgroup analyses indicated that the associations between coercive control and PTSD were stronger in domestic violence support service/shelter settings compared to community settings, suggesting that the incidence and/or impact of coercive control may be greater in domestic violence crisis response settings.
Limitations
The present study had several limitations, and the findings have to be interpreted accordingly. First, the findings included in the meta-analyses were cross-sectional and a direct causal link between coercive control and mental health could not be established. Second, the overall level of quality in the body of evidence could not be assessed with certainty and clear conclusions about the quality of the evidence could not be drawn. Third, most of the data in the included studies were derived from self-report measures and may be subject to under or overreporting. We also limited our search to English language reports, which has limited the access to evidence from non-English speaking countries and cultures. Moreover, the majority of studies used symptom severity measures. Only 7.35% of the studies included in the qualitative synthesis, and only 4.44% of the studies included in the meta-analyses used diagnostic instruments (Beck et al., 2011; Mutiso et al., 2020; Newton, 2021; Pickover et al., 2017; Reich et al. 2015). Thus, there was less clear evidence for a direct link between coercive control and mental health diagnoses. Finally, high heterogeneity suggests that other study features that could not be examined in this review may account for this variability. For instance, 76% of the studies focused solely on women, and only three studies focused on men and two on gender diverse populations and subgroup analyses could not be performed. Differences in female, male, and gender diverse populations may help to explain some of the heterogeneity.
Conclusion
Despite these limitations, the findings of this review provide important evidence for the mental health implications of coercive control exposure. This was the first meta-analysis that examined the associations involving coercive control and mental health. Results indicate that coercive control exposure is moderately associated with PTSD and depression symptom severity. The strength of these associations were comparable to those involving measures of broader psychological IPV in the present meta-analyses, and to those for physical IPV found in previous meta-analyses. Key findings are summarized in Table 3.
Table 3.
Summary of Critical Findings.
| • Coercive control exposure was moderately associated with PTSD and depression symptom severity • The strength of these associations was comparable to those involving measures of broader psychological IPV The strength of these associations was comparable to those for physical IPV found in previous meta-analyses |
Note. IPV = intimate partner violence; PTSD = post-traumatic stress disorder.
Implications
These findings have important implications for clinical practice research, policy, and legislation.
Implications for Clinical Practice
This meta-analysis provided evidence that coercive control exposure is linked to PTSD and depression, suggesting that coercive control exposure can have long-term mental health implications and that individuals who have been exposed to coercive control would likely benefit from psychological support. However, presently most IPV interventions focus on safety and crisis management (Neave et al., 2016). Subgroup analyses indicated a stronger link between coercive control and PTSD in domestic violence service/shelter settings suggesting that there is a need to include short-term mental health support in crisis response services. Moreover, evidence-based interventions are urgently needed to support long-term recovery, and clinicians need to be trained and supported so that they can provide effective short- and long-term care.
Implications for Research
First, the complexity of the coercive control construct and the difficulty to fully and distinctly capture it in most commonly used psychometric measures suggests the need to use more comprehensive measures of coercive control in primary studies. Equally, qualitative research approaches may be well suited to address the nuances in behaviors, such as verbal threats, to determine if they occur within the context of situational couple violence or coercive control. Third, this review identified a lack of empirical studies that have investigated the relationship between coercive control and CPTSD, and more research is needed. Finally, most of the studies were conducted in developed countries and predominantly focused on women in heterosexual relationships. More primary studies in developing countries, and studies with gender diverse samples are needed.
Implications for Policy and Legislation
The findings highlight that policy makers and legislators need to consider the mental health impacts of coercive control when implementing policies and legislations surrounding the criminalization of coercive control, and to provide funding for trauma-informed mental health services that support the long-term recovery of those who have been exposed to coercive control. The implications for clinical practice, research, and policy and legislation are summarized in Table 4.
Table 4.
Implications for Clinical Practice, Research, Policy, and Legislation.
| Implications for Clinical Practice • Coercive control exposure is linked to PTSD and depression, suggesting long-term mental health implications that require mental health support • Trauma-informed interventions are needed to support long-term recovery • A stronger link between coercive control and PTSD in domestic violence service/shelter settings suggests a need to include short-term trauma-informed mental health care in crisis response services • Clinicians need to be trained and supported so that they can provide effective short- and long-term care. Implications for Research • Coercive control is difficult to capture in most commonly used psychometric measures and more comprehensive measures of coercive control need to be used in primary studies • Research into the development of more specific coercive control measures is needed • Qualitative research approaches may be well suited to address the nuances in behaviors, such as verbal threats, to determine if they occur within the context of situational couple violence or coercive control. • There is lack of empirical studies that have investigated the relationship between coercive control and CPTSD, and more research is needed • More research in developing countries is needed • More research with gender diverse samples is needed Implications for Policy and Legislation • The mental health impacts of coercive control need to be considered in policies and legislations surrounding the criminalization of coercive control Funding for trauma-informed mental health care that supports the long-term recovery of those who have been exposed to coercive control is needed |
Note. IPV = intimate partner violence; PTSD = post-traumatic stress disorder; CPTSD = complex post-traumatic stress disorder.
Supplemental Material
Supplemental material, sj-docx-1-tva-10.1177_15248380231162972 for The Trauma and Mental Health Impacts of Coercive Control: A Systematic Review and Meta-Analysis by Susanne Lohmann, Sean Cowlishaw, Luke Ney, Meaghan O’Donnell and Kim Felmingham in Trauma, Violence, & Abuse
Author Biographies
Susanne Lohmann is a clinical psychologist registrar and a clinical psychology PhD candidate with the University of Melbourne. Her research focuses on the trauma and mental health impacts of intimate partner violence exposure with a particular focus on coercive control.
Sean Cowlishaw, PhD, is a senior research fellow with the Phoenix Australia Centre for Posttraumatic Mental Health, in the Department of Psychiatry at the University of Melbourne. He is also an Honorary Senior Research Fellow with the Bristol Medical School at the University of Bristol. He has primary expertise in post-traumatic mental health and Intimate Partner Violence.
Luke Ney, PhD, is postdoctoral research fellow at Queensland University of Technology, Australia. He graduated from the University of Tasmania with a PhD in Psychology in 2021. He is an expert in trauma, fear, memory, cannabinoid pharmacology, and analytical chemistry.
Meaghan O’Donnell, PhD, is the head of research at the Phoenix Australia, Centre for Posttraumatic Mental Health, which tests new and emerging treatments to promote recovery following trauma exposure, and professor in the Department of Psychiatry, University of Melbourne. She has published widely in the area of post-traumatic mental health.
Kim Felmingham, PhD, is professor and chair of clinical psychology, in the School of Psychological Sciences, at the University of Melbourne. She is a clinical psychologist and researcher with expertise identifying the mechanisms underlying post-traumatic stress disorder, post-traumatic mental health and trauma-focused treatments.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: SL received funding from a PhD graduate research scholarship from the University of Melbourne.
ORCID iD: Susanne Lohmann  https://orcid.org/0000-0002-1478-4534
https://orcid.org/0000-0002-1478-4534
Supplemental Material: Supplemental material for this article is available online.
References
References marked with an asterisk indicate studies included in the meta-analyses.
- *Ahmad N. A., Silim U. A., Rosman A., Mohamed M., Chan Y. Y., Mohd Kasim N., Yusof M., Abd Razak M. A., Omar M., Abdul Aziz F. A., Jamaluddin R., Ismail F., Ibrahim N., Aris T. (2018). Postnatal depression and intimate partner violence: A nationwide clinic-based cross-sectional study in Malaysia. BMJ Open, 8(5), e020649. 10.1136/bmjopen-2017-020649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Alexander K. A., Willie T. C., McDonald-Mosley R., Campbell J. C., Miller E., Decker M. R. (2019). Associations between reproductive coercion, partner violence, and mental health symptoms among young Black women in Baltimore, Maryland. Journal of Interpersonal Violence, 36(17–18), NP9839–NP9863. https://doi.org/https://dx.doi.org/10.1177/0886260519860900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Anderson K. L. (2008). Is partner violence worse in the context of control? Journal of Marriage and Family, 70(5), 1157–1168. 10.1111/j.1741-3737.2008.00557.x [DOI] [Google Scholar]
- *Anderson J. C., Grace K. T., Miller E. (2017). Reproductive coercion among women living with HIV: An unexplored risk factor for negative sexual and mental health outcomes. AIDS, 31(16), 2261–2265. 10.1097/QAD.0000000000001620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baird S. L., Alaggia R., Jenney A. (2019). “Like Opening Up Old Wounds”: Conceptualizing intersectional trauma among survivors of intimate partner violence. Journal of Interpersonal Violence, 36(17-18), 8118–8141. https://doi.org/https://doi.org/10.1177/0886260519848788 [DOI] [PubMed] [Google Scholar]
- *Basile K. C., Arias I., Desai S., Thompson M. P. (2004). The differential association of intimate partner physical, sexual, psychological, and stalking violence and posttraumatic stress symptoms in a nationally representative sample of women. Journal of Traumatic Stress, 17(5), 413–421. https://doi.org/http://dx.doi.org/10.1023/B:JOTS.0000048954.50232.d8 [DOI] [PubMed] [Google Scholar]
- *Beck J., McNiff J., Clapp J. D., Olsen S. A., Avery M. L., Hagewood J. (2011). Exploring negative emotion in women experiencing intimate partner violence: Shame, Guilt, and PTSD. Behavior Therapy, 42(4), 740–750. https://doi.org/http://dx.doi.org/10.1016/j.beth.2011.04.001 [DOI] [PubMed] [Google Scholar]
- Beydoun H. A., Beydoun M. A., Kaufman J. S., Lo B., Zonderman A. B. (2012). Intimate partner violence against adult women and its association with major depressive disorder, depressive symptoms and postpartum depression: A systematic review and meta-analysis. Social Science & Medicine, 75(6), 959–975. 10.1016/j.socscimed.2012.04.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block C. (2000). Chicago Women’s Health Risk Study, 1995–1998. [Computer File ICPSR]. Chicago: Illinois Criminal Justice Information Authority. [Google Scholar]
- Borenstein M., Hedges L. V., Higgins J. P., Rothstein H. R. (2010). A basic introduction to fixed-effect and random-effects models for meta-analysis. Research Synthesis Methods, 1(2), 97–111. 10.1002/jrsm.12 [DOI] [PubMed] [Google Scholar]
- Borenstein M., Hedges L., Higgins J., Rothstein H. (2014). Comprehensive meta-analysis (version 3). Biostat. [Google Scholar]
- *Broughton S., Ford-Gilboe M. (2017). Predicting family health and well-being after separation from an abusive partner: Role of coercive control, mother's depression and social support. Journal of Clinical Nursing, 26(15–16), 2468–2481. https://doi.org/http://dx.doi.org/10.1111/jocn.13458 [DOI] [PubMed] [Google Scholar]
- *Bubriski-McKenzie A., Jasinski J. L. (2013). Mental health effects of intimate terrorism and situational couple violence among black and Hispanic women. Violence Against Women, 19(12), 1429–1448. https://doi.org/http://dx.doi.org/10.1177/1077801213517515 [DOI] [PubMed] [Google Scholar]
- Campbell J. C., Webster D. W., Glass N. (2009). The danger assessment: Validation of a lethality risk assessment instrument for intimate partner femicide. Journal of Interpersonal Violence, 24(4), 653–674. 10.1177/0886260508317180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloitre M. (2021). Complex PTSD: Assessment and treatment. European Journal of Psychotraumatology, 12(sup1), 1866423. 10.1080/20008198.2020.1866423 [DOI] [Google Scholar]
- Cloitre M., Shevlin M., Brewin C. R., Bisson J. I., Roberts N. P., Maercker A., Karatzias T., Hyland P. (2018). The International Trauma Questionnaire: development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatrica Scandinavica, 138(6), 536–546. 10.1111/acps.12956 [DOI] [PubMed] [Google Scholar]
- Cohen J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Lawrence Erlbaum. [Google Scholar]
- *Coker A. L., Davis K. E., Arias I., Desai S., Sanderson M., Brandt H. M., Smith P. H. (2002). Physical and mental health effects of intimate partner violence for men and women. American Journal of Preventive Medicine, 23(4), 260–268. https://doi.org/http://dx.doi.org/10.1016/S0749-3797%2802%2900514-7 [DOI] [PubMed] [Google Scholar]
- Corey D. M., Dunlap W. P., Burke M. J. (1998). Averaging correlations: Expected values and bias in combined Pearson rs and Fisher's z transformations. The Journal of general psychology, 125(3), 245–261. [Google Scholar]
- Covidence Systematic Review Software. (2021). [Computer software]. Veritas Health Innovation. https://www.covidence.org/
- Crossman K. A., Hardesty J. L. (2018). Placing coercive control at the center: What are the processes of coercive control and what makes control coercive? Psychology of Violence, 8(2), 196–206. 10.1037/vio0000094 [DOI] [Google Scholar]
- Crossman K. A., Hardesty J. L., Raffaelli M. (2016). “He could scare me without laying a hand on me”: Mothers’ experiences of nonviolent coercive control during marriage and after separation. Violence Against Women, 22(4), 454–473. 10.1177/1077801215604744 [DOI] [PubMed] [Google Scholar]
- Cumming G., Finch S. (2005). Inference by eye: Confidence intervals and how to read pictures of data. American Psychologist, 60(2), 170–180. 10.1037/0003-066X.60.2.170 [DOI] [PubMed] [Google Scholar]
- *Damra J. K., Abujilban S. (2021). Violence against women and its consequences on women's reproductive health and depression: A Jordanian sample. Journal of Interpersonal Violence, 36(5/6), NP3044–NP3060. 10.1177/0886260518770649 [DOI] [PubMed] [Google Scholar]
- Devries K. M., Mak J. Y., Bacchus L. J., Child J. C., Falder G., Petzold M., Astbury J., Watts C. H. (2013). Intimate partner violence and incident depressive symptoms and suicide attempts: A systematic review of longitudinal studies. PLoS Med, 10(5), e1001439. 10.1371/journal.pmed.1001439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dokkedahl S., Kok R. N., Murphy S., Kristensen T. R., Bech-Hansen D., Elklit A. (2019). The psychological subtype of intimate partner violence and its effect on mental health: protocol for a systematic review and meta-analysis. Systematic Reviews, 8(1), 198. 10.1186/s13643-019-1118-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Dokkedahl S., Kristensen T. R., Murphy S., Elklit A. (2021). The complex trauma of psychological violence: cross-sectional findings from a Cohort of four Danish Women Shelters. European Journal of Psychotraumatology, 12(1), 1863580. 10.1080/20008198.2020.1863580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Dutton D. G., Painter S. (1993). The battered woman syndrome: Effects of severity and intermittency of abuse. American Journal of Orthopsychiatry, 63(4), 614–622. https://doi.org/http://dx.doi.org/10.1037/h0079474 [DOI] [PubMed] [Google Scholar]
- *Dutton M. A., Goodman L. A., Bennett L. (1999). Court-involved battered women's responses to violence: The role of psychological, physical, and sexual abuse. Violence and Victims, 14(1), 89–104. [PubMed] [Google Scholar]
- Dutton M. A., Goodman L. A. (2005). Coercion in intimate partner violence: Toward a new conceptualization. Sex Roles, 52(11–12), 743–756. 10.1007/s11199-005-4196-6 [DOI] [Google Scholar]
- Dutton M. A., Goodman L. A., Terrell D., Schmidt R. J., Fujimoto A. (2007). Coercion in intimate partner relationships (CPR): A measure of demands, surveillance, coercive tactics, and behavioral response to coercive tactics. Final report submitted to National Institute of Justice. [Google Scholar]
- Duval S., Tweedie R. (2000). Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics, 56(2), 455–463. 10.1111/j.0006-341x.2000.00455.x [DOI] [PubMed] [Google Scholar]
- *Emery C. R., Wu S., Yang H., Lee H., Kim J., Chan K. L. (2019). Informal control by family and risk markers for alcohol abuse/dependence in Seoul. Journal of Interpersonal Violence, 34(5), 1000–1020. https://doi.org/http://dx.doi.org/10.1177/0886260516647003 [DOI] [PubMed] [Google Scholar]
- Endnote. (2013). (Version X9) [Computer software]. Clarivate. https://endnote.com/
- *Fleming K. N., Newton T. L., Fernandez-Botran R., Miller J. J., Burns V. E. (2012). Intimate partner stalking victimization and posttraumatic stress symptoms in post-abuse women. Violence Against Women, 18(12), 1368–1389. https://doi.org/http://dx.doi.org/10.1177/1077801212474447 [DOI] [PubMed] [Google Scholar]
- García-Moreno C., Jansen H. A., Ellsberg M., Heise L., Watts C. (2005). WHO multi-country study on women’s health and domestic violence against women. World Health Organization. [DOI] [PubMed] [Google Scholar]
- *Gibbs A., Dunkle K., Jewkes R. (2018). Emotional and economic intimate partner violence as key drivers of depression and suicidal ideation: A cross-sectional study among young women in informal settlements in South Africa. PLoS ONE, 13(4), e0194885. https://doi.org/http://dx.doi.org/10.1371/journal.pone.0194885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golding J. M. (1999). Intimate partner violence as a risk factor for mental disorders: A meta-analysis. Journal of Family Violence, 14(2), 99–132. 10.1023/a:1022079418229 [DOI] [Google Scholar]
- *Gou L. H., Duerksen K. N., Woodin E. M. (2019). Coercive control during the transition to parenthood: An overlooked factor in intimate partner violence and family wellbeing?. Aggressive Behavior, 45(2), 139–150. https://doi.org/http://dx.doi.org/10.1002/ab.21803 [DOI] [PubMed] [Google Scholar]
- *Grace K. T., Perrin N. A., Clough A., Miller E., Glass N. E. (2020). Correlates of reproductive Coercion among college women in abusive relationships. American College of Nurse-Midwives (ACNM) 65th Annual Meeting & Exhibition, May 29-June 02, 2020. Journal of Midwifery & Women's Health, 65(5), 717–718. 10.1111/jmwh.13178 [DOI] [Google Scholar]
- Graham-Kevan N., Archer J. (2003). Intimate terrorism and common couple violence. A test of Johnson’s predictions in four British samples. Journal of Interpersonal Violence, 18(11), 1247-1270. 10.1177/0886260503256656 [DOI] [PubMed] [Google Scholar]
- Groves A. K., Kagee A., Maman S., Moodley D., Rouse P. (2012). Associations between intimate partner violence and emotional distress among pregnant women in Durban, South Africa. Journal of Interpersonal Violence, 27(7), 1341–1356. 10.1177/0886260511425247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hameed M., O'Doherty L., Gilchrist G., Tirado-Munoz J., Taft A., Chondros P., Feder G., Tan M., Hegarty K. (2020). Psychological therapies for women who experience intimate partner violence. Cochrane Database of Systematic Reviews, 7, CD013017. 10.1002/14651858.CD013017.pub2 [DOI] [PMC free article] [PubMed]
- *Hardesty J. L., Ogolsky B. G., Raffaelli M., Whittaker A. (2019). Relationship dynamics and divorcing mothers' adjustment: Moderating role of marital violence, negative life events, and social support. Journal of Social and Personal Relationships, 36(11–12), 3651–3672. https://doi.org/http://dx.doi.org/10.1177/0265407519833178 [Google Scholar]
- *Hayes B. E., Kopp P. M. (2020). Gender differences in the effect of past year victimization on self-reported physical and mental health: Findings from the 2010 National Intimate Partner and Sexual Violence Survey. American Journal of Criminal Justice, 45(2), 293–312. https://doi.org/http://dx.doi.org/10.1007/s12103-019-09510-7 [Google Scholar]
- *Hazen A. L., Connelly C. D., Soriano F. I., Landsverk J. A. (2008). Intimate partner violence and psychological functioning in Latina women. Health Care for Women International, 29(3), 282–299. https://doi.org/http://dx.doi.org/10.1080/07399330701738358 [DOI] [PubMed] [Google Scholar]
- *Hedin L. W., Janson P. O. (1999). The invisible wounds: the occurrence of psychological abuse and anxiety compared with previous experience of physical abuse during the childbearing year. Journal of Psychosomatic Obstetrics & Gynecology, 20(3), 136–144. [DOI] [PubMed] [Google Scholar]
- Hegarty K., Bush R., Sheehan M. (2005). Composite Abuse Scale: Further development and assessment of reliability and validity of a multidimensional partner abuse measure in clinical settings. Violence Victims, 20(5), 529–547. 10.1891/vivi.2005.20.5.529 [DOI] [PubMed]
- Hegarty K., Sheehan M., Schonfeld C. (1999). A multidimensional definition of partner abuse: Development and preliminary validation of the Composite Abuse Scale. Journal of Family Violence, 14(4), 399–415. 10.1023/A:1022834215681 [DOI] [Google Scholar]
- Heise L., Pallitto C., Garcia-Moreno C., Clark C. J. (2019). Measuring psychological abuse by intimate partners: Constructing a cross-cultural indicator for the Sustainable Development Goals. SSM Population Health, 9, 100377. 10.1016/j.ssmph.2019.100377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman J. L. (1992). Trauma and Recovery. Basic Books [Google Scholar]
- Higgins J. P., Thompson S. G., Deeks J. J., Altman D. G. (2003). Measuring inconsistency in meta-analyses. Bmj, 327(7414), 557–560. https://doi.org/https://doi.org/10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Hines D. A., Douglas E. M. (2011). Symptoms of posttraumatic stress disorder in men who sustain intimate partner violence: A study of helpseeking and community samples. Psychology of Men & Masculinity, 12(2), 112–127. https://doi.org/http://dx.doi.org/10.1037/a0022983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Hines D. A., Douglas E. M. (2012). Alcohol and drug abuse in men who sustain intimate partner violence. Aggressive Behavior, 38(1), 31–46. https://doi.org/http://dx.doi.org/10.1002/ab.20418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Hines D. A., Douglas E. M. (2018). Influence of intimate terrorism, situational couple violence, and mutual violent control on male victims. Psychology of Men & Masculinity, 19(4), 612–623. https://doi.org/https://dx.doi.org/10.1037/men0000142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Ireland J. L., Birch P., Kolstee J., Ritchie A. (2017). Partner abuse and its association with emotional distress: A study exploring LGBTI relationships. International Journal of Law and Psychiatry, 54, 107–117. 10.1016/j.ijlp.2017.06.005 [DOI] [PubMed] [Google Scholar]
- Joanna Briggs Institute. (2017). JBI Critical Appraisal Checklist for Analytical Cross Sectional Studies. https://jbi.global/sites/default/files/2019-05/JBI_Critical_Appraisal-Checklist_for_Analytical_Cross_Sectional_Studies2017_0.pdf
- Johnson M. P. (2008). A typology of domestic violence: Intimate terrorism, violent resistance, and situational couple violence. Northeastern University Press. [Google Scholar]
- *Johnson M. P., Leone J. M. (2005). The differential effects of intimate terrorism and situational couple violence: Findings from the national violence against women survey. Journal of Family Issues, 26(3), 322–349. https://doi.org/http://dx.doi.org/10.1177/0192513X04270345 [Google Scholar]
- *Johnson M. P., Leone J. M., Xu Y. (2014). Intimate terrorism and situational couple violence in general surveys: Ex-spouses required. Violence Against Women, 20(2), 186–207. https://doi.org/http://dx.doi.org/10.1177/1077801214521324 [DOI] [PubMed] [Google Scholar]
- *Jones M. S. (2020). Exploring coercive control, PTSD, and the use of physical violence in the pre-prison heterosexual relationships of incarcerated women. Criminal Justice and Behavior, 47(10), 1299–1318. 10.1177/0093854820920661 [DOI] [Google Scholar]
- *Jones S., Davidson W. S., II, Bogat G., Levendosky A., von Eye A. (2005). Validation of the subtle and overt psychological abuse scale: An examination of construct validity. Violence and Victims, 20(4), 407–416. https://doi.org/http://dx.doi.org/10.1891/vivi.2005.20.4.407 [PubMed] [Google Scholar]
- *Kapiga S., Harvey S., Muhammad A. K., Stockl H., Mshana G., Hashim R., Hansen C., Lees S., Watts C. (2017). Prevalence of intimate partner violence and abuse and associated factors among women enrolled into a cluster randomised trial in northwestern Tanzania. BMC Public Health, 17(1), 190. https://doi.org/https://dx.doi.org/10.1186/s12889-017-4119-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karatzias T., Cloitre M. (2019). Treating adults with complex posttraumatic stress disorder using a modular approach to treatment: Rationale, evidence, and directions for future research. Journal of Trauma and Stress, 32(6), 870–876. 10.1002/jts.22457 [DOI] [PubMed] [Google Scholar]
- Kennedy A. C., Bybee D., Mccauley H. L., Prock K. A. (2018). Young women’s intimate partner violence victimization patterns across multiple relationships. Psychology of Women Quarterly, 42(4), 430–444. 10.1177/0361684318795880 [DOI] [Google Scholar]
- *Lawrence E., Yoon J., Langer A., Ro E. (2009). Is psychological aggression as detrimental as physical aggression? The independent effects of psychological aggression on depression and anxiety symptoms. Violence and Victims, 24(1), 20–35. https://doi.org/http://dx.doi.org/10.1891/0886-6708.24.1.20 [DOI] [PubMed] [Google Scholar]
- *Leone J. M. (2011). Suicidal behavior among low-income, African American female victims of intimate terrorism and situational couple violence. Journal of Interpersonal Violence, 26(13), 2568–2591. https://doi.org/http://dx.doi.org/10.1177/0886260510388280 [DOI] [PubMed] [Google Scholar]
- Leone J. M., Johnson M. P., Cohan C. L. (2007). Victim help seeking: Differences between intimate terrorism and situational couple violence. Family Relations, 56(5), 427–439. 10.1111/j.1741-3729.2007.00471.x [DOI] [Google Scholar]
- *Levine A. R., Fritz P. A. (2016). Coercive control, posttraumatic stress disorder, and depression among homeless women. Partner Abuse, 7(1), 26–43. https://doi.org/http://dx.doi.org/10.1891/1946-6560.7.1.26 [Google Scholar]
- *Lovestad S., Love J., Vaez M., Krantz G. (2017). Prevalence of intimate partner violence and its association with symptoms of depression; a cross-sectional study based on a female population sample in Sweden. BMC Public Health, 17(1), 335. https://doi.org/https://dx.doi.org/10.1186/s12889-017-4222-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Ludermir A. B., Lewis G., Valongueiro S. A., de Araujo T. V. B., Araya R. (2010). Violence against women by their intimate partner during pregnancy and postnatal depression: A prospective cohort study. The Lancet, 376(9744), 903–910. https://doi.org/http://dx.doi.org/10.1016/S0140-6736%2810%2960887-2 [DOI] [PubMed] [Google Scholar]
- *Ludermir A. B., Valongueiro S., Araujo T. V. (2014). Common mental disorders and intimate partner violence in pregnancy. Revista de Saude Publica, 48(1), 29–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall L. L. (1992). Development of the severity of violence against women scales. Journal of Family Violence, 7, 103–121. https://doi.org/https://doi.org/10.1007/BF00978700 [Google Scholar]
- *McCauley H. L., Falb K. L., Streich-Tilles T., Kpebo D., Gupta J. (2014). Mental health impacts of reproductive coercion among women in Cote d'Ivoire. International Journal of Gynaecology & Obstetrics, 127(1), 55–59. https://doi.org/https://dx.doi.org/10.1016/j.ijgo.2014.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Mechanic M. B., Uhlmansiek M. H., Weaver T. L., Resick P. A. (2000). The impact of severe stalking experienced by acutely battered women: An examination of violence, psychological symptoms and strategic responding. Violence and Victims, 15(4), 443–458. https://doi.org/http://dx.doi.org/10.1891/0886-6708.15.4.443 [PMC free article] [PubMed] [Google Scholar]
- *Mechanic M. B., Weaver T. L., Resick P. A. (2008). Mental health consequences of intimate partner abuse: A multidimensional assessment of four different forms of abuse. Violence Against Women, 14(6), 634–654. https://doi.org/http://dx.doi.org/10.1177/1077801208319283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller E., Decker M. R., Mccauley H. L., Tancredi D. J., Levenson R. R., Waldman J., Schoenwald P., Silverman J. G. (2010). Pregnancy coercion, intimate partner violence and unintended pregnancy. Contraception, 81(4), 316–322. 10.1016/j.contraception.2009.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munn Z., Barker T. H., Moola S., Tufanaru C., Stern C., McArthur A., Stephenson M., Aromataris E. (2020, Oct). Methodological quality of case series studies: an introduction to the JBI critical appraisal tool. JBI Evidence Synthesis, 18(10), 2127–2133. 10.11124/JBISRIR-D-19-00099 [DOI] [PubMed] [Google Scholar]
- Murphy C. M., Hoover S. A., Taft C. (1999, November). The multidimensional measure of emotional abuse: Factor structure and subscale validity. Paper presented at the annual meeting of the Association for the Advancement of Behavior Therapy, Toronto, Canada. [Google Scholar]
- *Mutiso V., Musyimi C., Rebello T., Gitonga I., Tele A., Pike K., Ndetei D. (2020). Predictors of intimate partner violence in patients attending general health services at rural health facilities in Makueni County, Kenya. Mental Health and Prevention, 20, 200191. 10.1016/j.mhp.2020.200191 [DOI]
- Neave M., Faulkner P., Nicholson T. (2016). Royal commission into family violence: Summary and recommendations. Victorian Government Printer. [Google Scholar]
- *Newton T. L. (2021). In their own words: Women’s memories of felt emotions during worst incidents of intimate partner abuse. Journal of Trauma & Dissociation, 22(5), 563–580. https://doi.org/https://dx.doi.org/10.1080/15299732.2020.1869649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Nielsen S. K., Hardesty J. L., Raffaelli M. (2016). Exploring variations within situational couple violence and comparisons with coercive controlling violence and no violence/no control. Violence Against Women, 22(2), 206–224. https://doi.org/http://dx.doi.org/10.1177/1077801215599842 [DOI] [PubMed] [Google Scholar]
- *Nnawulezi N., Murphy C. (2019). Understanding formal help-seeking among women whose partners are in abuser intervention programs. Psychology of Violence, 9(4), 383–391. https://doi.org/http://dx.doi.org/10.1037/vio0000126 [Google Scholar]
- *Norwood A., Murphy C. (2012). What forms of abuse correlate with PTSD symptoms in partners of men being treated for intimate partner violence? Psychological Trauma: Theory, Research, Practice, and Policy, 4(6), 596–604. https://doi.org/http://dx.doi.org/10.1037/a0025232 [Google Scholar]
- *Ogunbajo A., Oginni O. A., Iwuagwu S., Williams R., Biello K., Mimiaga M. J. (2020). Experiencing intimate partner violence (IPV) is associated with psychosocial health problems among gay, bisexual, and other men who have sex with men (GBMSM) in Nigeria, Africa. Journal of Interpersonal Violence, 37(9–10), NP7394–NP7425. https://doi.org/https://dx.doi.org/10.1177/0886260520966677 [DOI] [PubMed]
- Orwin R. G. (1983). A Fail-SafeN for effect size in meta-analysis. Journal of Educational Statistics, 8(2), 157–159. 10.3102/10769986008002157 [DOI] [Google Scholar]
- Page M. J., Mckenzie J. E., Bossuyt P. M., Boutron I., Hoffmann T. C., Mulrow C. D., Shamseer L., Tetzlaff J. M., Akl E. A., Brennan S. E., Chou R., Glanville J., Grimshaw J. M., Hróbjartsson A., Lalu M. M., Li T., Loder E. W., Mayo-Wilson E., Mcdonald S., . . .Moher D. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ, n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed]
- *Peltzer K., Pengpid S., McFarlane J., Banyini M. (2013). Mental health consequences of intimate partner violence in Vhembe district, South Africa. General Hospital Psychiatry, 35(5), 545–550. https://doi.org/http://dx.doi.org/10.1016/j.genhosppsych.2013.04.001 [DOI] [PubMed] [Google Scholar]
- Peterson R. A., Brown S. P. (2005). On the use of beta coefficients in meta-analysis. Journal of Applied Psychology, 90(1), 175–181. 10.1037/0021-9010.90.1.175 [DOI] [PubMed] [Google Scholar]
- *Petra M. (2020). The salience of intimate partner violence to coping and social support for intimate partners of people with addictions. Alcoholism Treatment Quarterly, 38(3), 306–324. https://doi.org/http://dx.doi.org/10.1080/07347324.2019.1681332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Pickover A. M., Lipinski A. J., Dodson T. S., Tran H. N., Woodward M. J., Beck J. G. (2017). Demand/withdraw communication in the context of intimate partner violence: Implications for psychological outcomes. Journal of Anxiety Disorders, 52, 95–102. 10.1016/j.janxdis.2017.07.002 [DOI] [PubMed] [Google Scholar]
- Pill N., Day A., Mildred H. (2017). Trauma responses to intimate partner violence: A review of current knowledge. Aggression and Violent Behavior, 34, 178–184. 10.1016/j.avb.2017.01.014 [DOI] [Google Scholar]
- Pitman T. (2016). Living with coercive control: Trapped within a complex web of double standards, double binds and boundary violations. British Journal of Social Work. 10.1093/bjsw/bcw002 [DOI]
- Pokman V., Rossi F. S., Holtzworth-Munroe A., Applegate A. G., Beck C. J. A., D’Onofrio B. M. (2014). Mediator’s Assessment of Safety Issues and Concerns (MASIC). Assessment, 21(5), 529–542. 10.1177/1073191114528372 [DOI] [PubMed] [Google Scholar]
- Postmus J. L., Hoge G. L., Breckenridge J., Sharp-Jeffs N., Chung D. (2020). Economic abuse as an invisible form of domestic violence: A multicountry review. Trauma, Violence, & Abuse, 21(2), 261-283. 10.1177/1524838018764160 [DOI] [PubMed] [Google Scholar]
- *Postmus J. L., Huang C. -C., Mathisen-Stylianou A. (2012). The impact of physical and economic abuse on maternal mental health and parenting. Children and Youth Services Review, 34(9), 1922–1928. https://doi.org/http://dx.doi.org/10.1016/j.childyouth.2012.06.005 [Google Scholar]
- *Prospero M. (2008). The effect of coercion on aggression and mental health among reciprocally violent couples. Journal of Family Violence, 23(3), 195–202. https://doi.org/http://dx.doi.org/10.1007/s10896-007-9143-6 [Google Scholar]
- *Prospero M. (2009). Sex-symmetric effects of coercive behaviors on mental health?: Not exactly. Journal of Interpersonal Violence, 24(1), 128–146. https://doi.org/http://dx.doi.org/10.1177/0886260508315778 [DOI] [PubMed] [Google Scholar]
- *Prospero M., Kim M. (2009. a). Ethnic difference in the effects of coercion on mental health and the use of therapy. Journal of Social Work Practice, 23(1), 77–91. https://doi.org/http://dx.doi.org/10.1080/02650530902723332 [Google Scholar]
- *Prospero M., Kim M. (2009. b). Mutual partner violence: Mental health symptoms among female and male victims in four racial/ethnic groups. Journal of Interpersonal Violence, 24(12), 2039–2056. https://doi.org/http://dx.doi.org/10.1177/0886260508327705 [DOI] [PubMed] [Google Scholar]
- Pulerwitz J., Amaro H., De Jong W., Gortmaker S. L., Rudd R. (2002). Relationship power, condom use and HIV risk among women in the USA. AIDS Care, 14, 789-800. https://doi:10.1080/0954012021000031868 [DOI] [PubMed] [Google Scholar]
- Radloff L. S. (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- *Reich C. M., Blackwell N., Simmons C. A., Beck J. (2015). Social problem solving strategies and posttraumatic stress disorder in the aftermath of intimate partner violence. Journal of Anxiety Disorders, 32, 31–37. https://doi.org/http://dx.doi.org/10.1016/j.janxdis.2015.02.007 [DOI] [PubMed] [Google Scholar]
- Rosenthal R. (1979). The file drawer problem and tolerance for null results. Psychological Bulletin, 86(3), 638–641. 10.1037/0033-2909.86.3.638 [DOI] [Google Scholar]
- *Sackett L. A., Saunders D. G. (1999). The impact of different forms of psychological abuse on battered women. Violence and Victims, 14(1), 105–117. https://doi.org/http://dx.doi.org/10.1891/0886-6708.14.1.105 [PubMed] [Google Scholar]
- Salter M., Conroy E., Dragiewicz M., Burke J., Ussher J., Middleton W., Vilenica S., Martin Monzon B., Noack-Lundberg K. (2020). “A deep wound under my heart”: Constructions of complex trauma and implications for women’s wellbeing and safety from violence (Research Report, 12/2020). ANROWS. [Google Scholar]
- *Sauber E. W., O’Brien K. M. (2020). Multiple losses: The psychological and economic well-being of survivors of intimate partner violence. Journal of Interpersonal Violence, 35(15–16), 3054–3078. https://doi.org/https://dx.doi.org/10.1177/0886260517706760 [DOI] [PubMed] [Google Scholar]
- Smith P. H., Smith J. B., Earp J. A. L. (1999). Beyond the Measurement Trap: A Reconstructed Conceptualization and Measurement of Woman Battering. Psychology of Women Quarterly, 23(1), 177–193. 10.1111/j.1471-6402.1999.tb00350.x [DOI] [Google Scholar]
- Smith S. G., Chen J., Basile K. C., Gilbert L. K., Merrick M. T., Patel N., Walling M., Jain A. (2017). The National Intimate Partner and Sexual Violence Survey (NISVS): 2010–2012 state report. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. [Google Scholar]
- Spencer C., Mallory A. B., Cafferky B. M., Kimmes J. G., Beck A. R., Stith S. M. (2019). Mental health factors and intimate partner violence perpetration and victimization: A meta-analysis. Psychology of Violence, 9(1), 1–17. 10.1037/vio0000156 [DOI] [Google Scholar]
- Stark E. (2007). Interpersonal violence. Coercive control: How men entrap women in personal life. Oxford University Press. [Google Scholar]
- Stark E. (2013). Coercive control. Violence Against Women: Current Theory and Practice in Domestic Abuse, Sexual Violence and Exploitation, 25(1), 17–33. [Google Scholar]
- Stark E., Hester M. (2019). Coercive control: Update and review. Violence Against Women, 25(1), 81–104. https://doi.org/https://doi.org/10.1177/1077801218816191 [DOI] [PubMed] [Google Scholar]
- Stephenson R., Finneran C. (2013). The IPV-GBM Scale: A New Scale to Measure Intimate Partner Violence among Gay and Bisexual Men. PLOS ONE, 8(6), e62592. 10.1371/journal.pone.0062592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stith S. M., Smith D. B., Penn C. E., Ward D. B., Tritt D. (2004). Intimate partner physical abuse perpetration and victimization risk factors: A meta-analytic review. Aggression and Violent Behavior, 10(1), 65–98. 10.1016/j.avb.2003.09.001 [DOI] [Google Scholar]
- Straus M. A. (1990). The Conflict Tactics Scales and its critics: An evaluation and new data on validity and reliability. In Straus M. A., Gelles R. J. (Eds.), Physical violence in American families: Risk factors and adaptations to violence in 8,145 families. 49–73. Transaction Publishing. [Google Scholar]
- Straus M. A., Hamby S. L., Boney-McCoy S., Sugarman D. B. (1996). The Revised Conflict Tactics Scale (CTS2). Journal of Family Issues, 17(3), 283–316 https://doi.org/https://doi-org.ezp.lib.unimelb.edu.au/10.1177/019251396017003001 [Google Scholar]
- *Strauss C. V., Haynes E. E., Cornelius T. L., Shorey R. C. (2019). Stalking victimization and substance use in college dating relationships: An exploratory analysis. Journal of Interpersonal Violence, 34(14), 2878–2896. https://doi.org/https://dx.doi.org/10.1177/0886260516663899 [DOI] [PubMed] [Google Scholar]
- *Street A. E., Arias I. (2001). Psychological abuse and posttraumatic stress disorder in battered women: Examining the roles of shame and guilt. Violence and Victims, 16(1), 65–78. [PubMed] [Google Scholar]
- *Stylianou A. M. (2018). Economic abuse experiences and depressive symptoms among victims of intimate partner violence. Journal of Family Violence, 33(6), 381–392. https://doi.org/http://dx.doi.org/10.1007/s10896-018-9973-4 [Google Scholar]
- *Taft C. T., Murphy C. M., King L. A., Dedeyn J. M., Musser P. H. (2005). Posttraumatic stress disorder symptomatology among partners of men in treatment for relationship abuse. Journal of Abnormal Psychology, 114(2), 259–268. https://doi.org/http://dx.doi.org/10.1037/0021-843X.114.2.259 [DOI] [PubMed] [Google Scholar]
- *Tiwari A., Chan K. L., Cheung D. S., Fong D. Y., Yan E. C., Tang D. H. (2015). The differential effects of intimate terrorism and situational couple violence on mental health outcomes among abused Chinese women: A mixed-method study. BMC Public Health, 15, 314. https://doi.org/https://dx.doi.org/10.1186/s12889-015-1649-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tjaden P., Thoennes N. (1999). Extent, nature, and consequences of intimate partner vio- lence: Findings from the National Violence Against Women Survey. National Institute of Justice/Centers for Disease Control and Prevention. [Google Scholar]
- Trevillion K., Oram S., Feder G., Howard L. M. (2012). Experiences of domestic violence and mental disorders: A systematic review and meta-analysis. PLoS One, 7(12), e51740. 10.1371/journal.pone.0051740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolman R. M. (1989). The development of a measure of psychological maltreatment of women by their male partners. Violence and Victims, 4(3), 159–177. 10.1891/0886-6708.4.3.159 [DOI] [PubMed] [Google Scholar]
- Tolman R. M. (1999). The Validation of the Psychological Maltreatment of Women Inventory. Violence and Victims, 14(1), 25–37. 10.1891/0886-6708.14.1.25 [DOI] [PubMed] [Google Scholar]
- *Voth Schrag R. J., Robinson S. R., Ravi K. (2019). Understanding pathways within intimate partner violence: Economic abuse, economic hardship, and mental health. Journal of Aggression, Maltreatment & Trauma, 28(2), 222–242. https://doi.org/http://dx.doi.org/10.1080/10926771.2018.1546247 [Google Scholar]
- Weathers F. W., Litz B. T., Herman D. S., Huska J. A., Keane T. M. (1993). The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Paper presented at the International Society for Traumatic Stress Studies, San Antonio, TX. [Google Scholar]
- *Weaver T. L., Etzel J. C. (2003). Smoking patterns, symptoms of PTSD and depression: Preliminary findings from a sample of severely battered women. Addictive Behaviors, 28(9), 1665–1679. https://doi.org/http://dx.doi.org/10.1016/j.addbeh.2003.08.041 [DOI] [PubMed] [Google Scholar]
- *Wolf N. M., Lokkegaard S. S., Elklit A. (2018). Psychological distress and attachment insecurity of stalked mothers. Journal of Interpersonal Violence, 36(13–14), 6487–6511. https://doi.org/https://dx.doi.org/10.1177/0886260518819883 [DOI] [PubMed] [Google Scholar]
- *Wolford-Clevenger C., Grigorian H., Brem M., Florimbio A., Elmquist J., Stuart G. L. (2017). Associations of emotional abuse types with suicide ideation among dating couples. Journal of Aggression, Maltreatment & Trauma, 26(9), 1042–1054. https://doi.org/http://dx.doi.org/10.1080/10926771.2017.1335821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Wolford-Clevenger C., Smith P. N. (2017). The conditional indirect effects of suicide attempt history and psychiatric symptoms on the association between intimate partner violence and suicide ideation. Personality and Individual Differences, 106, 46–51. https://doi.org/http://dx.doi.org/10.1016/j.paid.2016.10.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2017). Intimate partner and sexual violence against women: Fact sheet. https://www.who.int/news-room/fact-sheets/detail/violence-against-women
- World Health Organization. (2019). International statistical classification of diseases and related health problems (11th ed.). World Health Organization. https://icd.who.int/ [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-tva-10.1177_15248380231162972 for The Trauma and Mental Health Impacts of Coercive Control: A Systematic Review and Meta-Analysis by Susanne Lohmann, Sean Cowlishaw, Luke Ney, Meaghan O’Donnell and Kim Felmingham in Trauma, Violence, & Abuse